Back Stability
This document was uploaded by user and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this DMCA report form. Report DMCA
Overview
Download & View Back Stability as PDF for free.
More details
- Words: 147,469
- Pages: 366
Loading documents preview...
Back Stability
Christopher M. Norris, MSc, MCSP Director, Norris Associates, Manchester, UK
Human Kinetics
Norris, Christopher M. Back stability I Christopher M. Norris. p.cm. Includes bibliographical references and index. ISBN 0-7360-008 I-X I. Backache--Treatment. 2. Backache--Prevention. 3. Backache--Exercise therapy. I. Title. RD771.158 N67 2000 617.5'64--dc21
99-089545
ISBN 0-7360-008 I-X
,
Copyright @ 2000 by Christopher M. Norris All rights reserved. Except for use in a review, the reproduction or utilization of this work in any form or by any electronic, mechanical, or other means, now known or hereafter invented, including xerography, photocopying, and recording, and in any information storage and retrieval system, is forbidden without the written permission of the publisher. Permission notices for material reprinted in this book from other sources can be found on page 263. Acquisitions Editor: Loam D. Robertson, PhD; Developmental Editor: Elaine Mustain; Writer: Brian Mustain; Assistant Editors: Derek Campbell, Melissa Feld, Maggie Schwarzentraub; Copyeditor: Lisa Morgan; Proofreader: Myla Smith; Indexer: Craig Brown; Permission Manager: Heather Munson; Graphic Designer: Fred Starbird; Graphic Artist: Yvonne Griffith; Cover Designer: Keith Blomberg; Photographer (cover): Tom Roberts; Art Manager: Craig Newsom; Illustrator: Kristin Mount; Printer: Edwards Brothers Printed in the United States of America
10 9
8 7
6
5 4
3
2
Human Kinetics Web site: www.humankinetics.com United States: Human Kinetics P.O. Box 5076 Champaign, IL 61825-5076 800-747-4457 e-mail: [email protected]
Australia: Human Kinetics 57A Price Avenue Lower Mitcham, South Australia 5062 08 8277 1555 e-mail: [email protected]
Canada: Human Kinetics 475 Devonshire Road, Unit 100 Windsor, ON N8Y 2L5 800-465-7301 (in Canada only) e-mail: [email protected]
New Zealand: Human Kinetics P.O. Box 105-231, Auckland Central 09-523-3462 e-mail: [email protected]
Europe: Human Kinetics Units C2IC3 Wira Business Park West Park Ring Road Leeds LSl6 6EB, United Kingdom +44 (0)113 2781708
e-mail: [email protected]
Contents Preface vi Acknowledgments
viii
·
Part I The Conce~tua1 Foundation
1
Chapter 1 What Is Back Stability? The Scope of the Problem A New Look at the Etiology and Treatment of Back Pain The Model Used in This Book: Lumbar Stabilization Summary
3 3 4 7 13
Chapter 2 Biomechanics of the Lumbar Spine Anatomy of the Vertebral Column Axial Compression Movements of the Lumbar Spine and Pelvis The Mechanics of Lifting Lifting Methods Summary
14 14 25 30 35 40 42
Chapter 3 Stabilization Mechanisms
43
in the Lumbar Spine
The Posterior Ligamentous System The Thoracolumbar Fascia Trunk Muscle Action Intra-Abdominal Pressure Mechanism Summary
·
Part II Exercises for Establishing Stabilitt Chapter 4 Teaching Your Clients the Basic Skills Teaching Your Clients to Control Pelvic Tilt Teaching Your Clients to Identify and Assume the Neutral Position
43 44 49 62 65
67 69 70 78
iii
iv
. Contents Teaching Your Clients to Use Abdominal Hollowing Teaching Your Clients to Contract the Multifidus Muscles at Will Summary
81 89 91
Chapter 5 Muscle Imbalance Basic Concepts Muscle Adaptation to Injury, Immobilization, and Training Training Specificity Changes in Muscle Length Principles of Muscle Stretching Stretching Target Muscles Summary
99 100 111 113 118
Chapter 6 Basic Abdominal Muscle Training Current Practice in Abdominal Training Modifications of Traditional Abdominal Exercises Ab Roller Exercises Summary
120 120 124 130 133
Chapter 7 Posture Optimal Postural Alignment Postural Stability and Body Sway Basic Postural Assessment Principles of Postural Correction Posture Types and How to Correct Them Summary
134 134 135 136 143 145 163
Part III. Building Back Fitness Chapter8 AdvancedStabilityTraining Superimposed Limb Movements and Balance Boards Stability Ball Exercises Proprioceptive Training Summary
92 92 96
165 167 168 186 197 201
Contents
Chapter 9 More Advanced Stability Training: Weight Training and Plyometrics Weight Training Using Plyometrics to Train for Power and Speed Summary
·
Part IV Putting It All Together
.
v
202 203 222 227
229
Chapter10 Buildinga BackStabilityProgram
231
for Your Client Preliminary Assessment of Your Client General Principles for Designing a Stability Program Parallel Tracks in Designing a Stability Program Designing an Advanced Stability Program Summary
231 234 235 237 246
Chapter 11 Preventing Back Injuries and Reinjuries Keep the Spine Vertical Principles of Lifting in the Home and on the Job Summary
247 247 248 254
Bibliography 255 Credits 263 Index 264 About the Author 272
Preface This book presents an approach to treating low back pain that is different from what you've seen before. I'd like to present a brief story to illustrate my point. One of the editorial staff who worked on this book had experienced severe back problems for over a quarter century. Only a few months before he saw this manuscript, he had completed a 12-week intensive weight-training program that he had hoped would help his back. It provided some relief, but not a great deal. After he had read the manuscript, this person began employing just a couple of the very elementary principles described in chapter 4 (specifically, hollowing his abdomen and intentionally tightening his multifidus muscles). He did not even do any of the exercises-he just practiced abdominal hollowing and multifidus tightening as he sat at his desk, or in his car, or as he walked through the supermarket. A month after he began this very minimal effort, he reported to me that his sharp sciatica pain had declined about 80% and that his periodic minor (but quite distressing) bowel incontinence, caused by impingement of vertebrae on a nerve, had declined from about a dozen episodes per week to about one every two weeks. While I certainly do not endorse this person's decision to do only the bare minimum in trying to alleviate his back problems, I note the story here to illustrate a single point: This approachworks! It works because it is based on sound anatomical, physiological, and neurological principles. While health professionals have long known that a large number of back problems arise because of muscle weakness, solving the problems simply by "doing strengthening exercises" is like telling a person with an infection to "take a lot of antibiotics" without targeting the medicine to the microbe. I have treated scores of "hunks" who had terrible problems with lower back pain. An individual can have unusually strong abdominal and back muscles while those unsung, unpublicized, invisible muscles that run alongside the spine-and that actually keep it stable-are. weak and stretched. This book shows you how to help your clients solve lower back problems by attending to the actual anatomical structures that control the problem-and these are not merely the gross, obvious muscles that make one look good at the beach. They are nearly invisible muscles such as the transversus abdominis and the multifidus; invisible tendons that have become inelastic; and hidden nerves carrying invisible impulses, all of
vi
Preface
.
vii
which can be trained surprisingly well (I'll teach you how) to stabilize the back even when your client isn't thinking about it. I have honed the techniques described in this book over many years, during which I have helped thousands of clients who for the most part had not been significantly helped with traditional approaches. If you ever treat, advise, coach, train, massage, or in any other way deal with people who have lower back pain, this book is for you. If you're a physical therapist, a massage therapist, a chiropractor, an athletic trainer, or a sports physician, this book may well prove vital to your professional practice. Even if you are a casual reader and are not able to understand the more technical aspects, you at least can benefit from learning the basic moves that stabilize the back, as in chapter 4. Because the body is a complex unit of closely interconnecting systems, any treatment must address the whole, even though it targets a single system. Thus, back stability is part of a holistic approach centering on muscle balance. Muscles affect the support of the spine, posture, and both our ability to move and the way that we move. If we examine the biomechanical factors at work in the back, we can see that there are three elements that combine to restore the muscle balance that is vital to back stability: correction of segmental control, shortening and strengthening lax muscles, and lengthening tight muscles. In Back Stability, I will explain these three elements to you, and I'll show you how to order them according to each client's symptoms, using them to construct a program uniquely tailored for that client. In part I ("The Conceptual Foundation"), I lead you through the anatomical, physiological, and neurological underpinnings of back pain, and of both traditional and newer approaches to treating it. I help you understand why traditional approaches so often don't work, and why the back stabilization method is so successful. Then, in part II ("Exercises for Establishing Stability"), I show you how to teach your clients the basic skills for back stabilization. In part III ("Building Back Fitness"), I teach you a wide range of exercises that will help your clients prevent recurrence of back pain and rehabilitate their backs (when appropriate) for strenuous on-the-job lifting or for challenging sports activities. Finally, in part IV ("Putting It All Together"), I discuss how you decide which assessments, exercises, etc., to prescribe for which clients. Be sure you don't begin applying the material herein to your clients till after you've studied chapter 10 since that's the roadmap that helps you navigate the exercises with a particular client in mind. Chapter 11,while short, is vital, as it briefly points out how you should coach your clients to avoid reinjuring their backs. Simple stick figures rather than lifelike line drawings have been used to represent human beings in the illustrations of those exercises in which the
viii
. Preface
position of the pelvic girdle might otherwise be difficult for a layperson to understand. This device makes it easier for your clients to see the required position of the pelvic girdle in those particular exercises. When more lifelike drawings were deemed clearer, we have used them. Therefore you, the practitioner, can use the book as a teaching tool, showing your clients the drawings as you explain the exercises to them, and they will be able to see clearly what the desired positions are. Christopher
M. Norris
Acknowledgments I
would like to thank Brian Mustain for translating British English into American English and for unraveling the "knotted ball of wool" that formed my thoughts, and Elaine Mustain for maintaining the book's momentum when all seemed lost. In addition to the references quoted in this book, I acknowledge the work of several individuals in the field of back stability-including Carolyn Richardson, Gwendolen Jull, Paul Hodges, and Julie Hides from the University of Queensland, Australia; Vladamir Janda and Karl Lewit from the University of Prague, Czech Republic; Shirley Sahrmann from the University of Washington, U.S.A.; and Mark Comerford from Kinetic Control, England. I would also like to thank the staff at Norris Associates, Manchester, England, for sharing their clinical experience in the field of back stability.
PART
II
The Concet!fttal Foundation Because the approach used in this book differs somewhat from what you have seen in the past, it is important that you understand the theoretical basis for what you read. I begin in chapter 1 ("What Is Back Stability?") with a general introduction to the problems of back pain and back instability. In one sense, the true "problem" is that some health professionals fail to understand that instability IS the problem for many instances of low back pain! People who suffer from back pain may be subjected to manipulation, instructed to perform exercises, told to "work out"; they may be given chemicals to relax their muscles and poked with electric needles-all intended to alleviate their pain. But surprisingly few professionals understand that a great deal of low back pain occurs for one simple reason: the spine is not supported by the tissues surrounding it and therefore "wobbles" in ways that impinge on nerves and in general do bad things to a person's quality of life. Traditional approaches are often quite helpful-but there are some clients for whom they simply do not address the root problem of back pain completely. The purpose of this book is to teach you how to deal with back pain by helping your clients stabilize their spines. From discussion of the basic etiology of pain in chapter 1, I proceed in chapter 2 ("Biomechanics of the Lumbar Spine") to an explanation of how the spine works: its anatomy, its movements, even the physics of lifting. Then, in chapter 3 ("Stabilization Mechanisms in the Lumbar Spine"), I show you how the anatomical lessons of the first two chapters lead logically to certain specific, but frequently ignored, treatments. I hope you will digest these three chapters thoroughly-without their conceptual foundation, the rest of the book will appear to be little more than one more listing of exercises. If you appreciate the anatomical and physiological underpinnings of the following chapters, however, you will see that the "how to" chapters will open for your clients a world of new possibilities that traditional programs cannot provide.
11
What Is Back Stabili!Yl Back pain is a universal problem, particularly important in the largely sedentary Western world. New information about this condition is stimulating new ways to manage it, focusing particularly on new approaches to exercise.
THE SCOPE OF THE PROBLEM As many as 80% of individuals in the Western world will suffer at least one disabling episode of low back pain during their lives; at any time, as many as 35% of the population suffers from some kind of back pain (Frymoyer and Cats-Baril 1991). The cost is tremendous, both financially and in terms of personal suffering. Most individuals with low back pain recover within six weeks, but 5-15% of subjects progress to permanent disability, accounting for up to 90% of total expenditures for this condition (Liebenson 1996). Unfortunately, recurrence of back pain after an acute episode is common. Over 60% of individuals suffering an acute episode of low back pain will experience another bout within a year, and 45% of these will have a second recurrence within the following four years (Liebenson 1996). As many as 15% of individuals with low back pain progress to permanent disability, and 60% suffer from a recurrence of pain within one year.
KEY POINT:
Back pain is universal. Sufferers in the United States spend $60 billion per year treating it (Frymoyer and Gordon 1989) and receive $27 billion for permanent disability. The rate of increase in back pain is 14 times greater than the population growth, and during a period when disability awards for all conditions rose by 347%, awards for back pain increased by 2,680% (Frymoyer and Cats-Baril 1991). 3
4
.
Back Stability
In the United Kingdom, 46.5 million working days were lost through back pain in 1989-representing a cost to the National Health Service of £0.5 billion ($840 million) per year and an even larger cost to industry of £5.1 billion ($8.59 billion) in lost production (CSP 1998; Tye and Brown 1990). In 1994-1995, 14 million people in the UK visited their doctors for back pain and lost 116 million working days.
A NEW LOOK AT THE ETIOLOGY AND TREATMENT
OF BACK PAIN
In spite of the tremendous increase in the number of back pain sufferers in the past two decades, popular understanding about the nature of back pain has remained somewhat static. It is commonly believed that back pain results from a structural injury or fault that must be corrected in order to reduce pain and restore full function. According to this viewpoint, normal function is impossible-or even dangerous-until the defective structure has changed (Zusman 1998). While it is true that many individuals with low back pain exhibit structural changes, CT (computerized tomography) scans reveal similar "positive findings" in up to 50% of normal, asymptomatic subjects (Boden et al. 1990; Jensel et al. 1994)! It is the same with radiographic changes in the lumbar spine: as many individuals without pain show evidence of disc degeneration as do those with pain (Nachemson 1992). Moreover, studies with cadavers have shown no correlation between structural changes in the lumbar spine and a history of low back pain (Videman et al. 1990), and large disc lesions with nerve compression may be totally asymptomatic (SaaI1995). .:f:a":.l'JI.'.~ Structural changes in the spine are as likely in asymptomatic individuals as in those with low back pain and loss of function.
Nonorganic Causes of Back Pain At least three sources of back pain do not originate in the sufferer's body: iatrogenic, forensic, and behavioral (compare Zusman 1998).
.
Iatrogenic factors (brought on by the practitioner) include labels of disability and the consequences of deconditioning through prolonged (bed) rest. For example, a label such as "prolapsed disc" is far more threatening to a patient than "simple back pain," even though the total amount of pain experienced by the patient may be the same in both cases. Labels that imply disease or disability such as "arthritis" also suggest
What Is Back Stability?
.
5
severe conditions even though a mild form of the pathology may be present. Alternatives such as "slight roughening" or "normal wear and tear" are less threatening. Although avoiding stressful activities on the back is important, and limited rest has its place, prolonged bed rest has been shown to be counterproductive. Deyo et a1. (1986) compared two days of bed rest with two weeks of bed rest. They found both periods to be equally effective in terms of pain reduction, but the two-week period led to significant "negative effects due to immobilization" (such as weakening and stiffness around the spine) that were not present in the two-day period. Forensic factors (associated with legal proceedings) contribute significantly to chronic back pain. In a study of 2,000 back pain patients (Long 1995), involvement in litigation was the only factor that accurately predicted that a person would not rapidly return to work. Two important behavioral factors are perceived disability and anticipation of pain. 1. Perceived disability. Patients often fail to take part in daily activities because they believethey are physically incapable of doing the taskalthough structural changes in their spines do not bear out this belief (Zusman 1998). Perceived disability is often associated with a mistaken fear of reinjury (Vlaeyen et a1. 1995). 2. Anticipation of pain. Often the anticipation of pain rather than pain itself is enough to limit activity and create protective behaviors (Zusman 1998). The physical changes brought about by the fear of pain can be measured on surface EMG (sEMG). Main and Watson (1996) applied experimental noxious stimuli to the upper trapezius on normal subjects and on those with back pain. Normal subjects showed the expected reflex increase in sEMG activity in the trapezius muscles. Those with back pain, however, showed the reaction not in the upper trapezius, but in the lumbar regionsuggesting that the subjects viewed any pain as an inherent part of their back condition even when the pain was in fact occurring in another part of their bodies.
.
.
Perceived disability and the anticipation of pain contribute significantly to loss of function.
KEY POINT:
A New Model for Low Back Pain Management Most people traditionally have perceived back pain as a structural condition that requires rest to recover. New information is challenging this approach, however, viewing back pain at least in part as a functional change .
6
.
BackStability
that requires functional management. Exercise is at the forefront of this new approach. The Traditional Model Rest is still the most common treatment for back pain, despite the fact that prolonged bed rest has been shown to be harmful. Controlled exercises restore function, reduce both distress and perceived disability, diminish pain, and promote a return to work (Waddell 1987). Rest has little effect on the natural history of back pain and may actually increase its severity (Twomey and Taylor 1994). For back pain without significant radiation, bed rest probably should be limited to a maximum of two days. Longer periods are almost certainly counterproductive due to the negative effects of whole-body immobilization (Spitzer et al. 1987). Surgery is effective in only a small group of low back pain patients. Waddell (1987) argued that surgical intervention can help only 1% of patients. Comparing surgically and conservatively treated patients suffering from disc prolapse, Weber (1983) found no difference in outcome after two years. Aggressive conservative management can successfully treat over 80% of patients with clinically diagnosed sciatica and radiological evidence of nerve root entrapment (Bush et al. 1992). According to Allan and Waddell (1989), "disc surgery. . . [has left] more tragic human wreckage in its wake than any other operation in history." The New Model In proposing a new model for the treatment of low back pain, Waddell (1987) recommended that the patient's role should change from one of resting and being a passive recipient of treatment to an active role of sharing responsibility for restoration of function. Rehabilitation professionals increasingly are adopting this philosophy, using exercise programs to enhance lumbar stabilization Oull and Richardson 1994b; Norris 1995a; O'Sullivan et al. 1997). Here are some examples:
·
For a herniated lumbar disc. A rehabilitation program that emphasized skill-basedexercisetherapy for the spine effectively treated herniated lumbar discs (Saal and Saa11989) and rehabilitated football players with back injury (SaaI1988). The program aimed to restore automatic control of muscular stabilization of the trunk by teaching subjects to maintain a correct lumbar pelvic position (Le., "neutral position"-see following discussion) while performing progressively more complex tasks. In a study by Skall et al. (1994), intensive exercise when pain was not a limiting factor was more effective than mild mobilizing exercise five weeks following disc surgery. A one-year follow-up showed a trend favoring the intensive exercise group. Even when the diagnosis is uncertain, progressive exercis~onsisting of strengthening, proprioceptive training, and aerobic training-may restore
What Is Back Stability?
.
7
pain-free function (Deutsch 1996). Pain, physical dysfunction, and psychosocial dysfunction improved following a 1D-week exercise program for chronic low back pain patients studied by Risch et al. (1993), whereas all three factors worsened for those who remained inactive.
.
100 90 80 70 60 50 40 30 20 10
Control Exercise
.q
",,
&
,,
Pain intensity
group group
----
I
,, " boo-.......0
0
0
o 35
Pain description
30 25 20 15
.
~~ ,
10
---''II> '0..........- -0
0
0
5
o 50 45 40 35 30 25 20 15 10 5
o
Pre
Post
3 mo. Functional measure
,
.,,
.
I
" '\:>-.-.-
0
0
For
spondylolysis
or
spondylolisthesis. A back stability program targeting the anterolateral abdomina Is and multifidus was more effective than conventional rehabilitation in patients with radiographic diagnosis of spondylolysis or spondylolisthesis (O'Sullivan et al. 1997). In this study, one group of patients underwent a 1D-week program of gym work (including trunk curl exercises), general exercises such as swimming, and pain-relieving modalities. A second group, which engaged only in back stability exercises, showed a statistically significant reduction in pain intensity, pain descriptor scale, and functional disability that was maintained at a 3D-month follow-up (figure 1.1). This trial provides the strongest evidence so far in the literature regarding the effectiveness of stabilization programs for the lumbar spine. I have expanded some of these techniques for use in this book.
0
THE MODEL 'I--r 6 mo. 30 mo.
Figure 1.1 A comparison of conventional exercise and stability exercise effects on spondylolys isl s pondylol isthes is. Adapted from O'Sullivanet al. 1997.
USED IN THIS BOOK: LUMBAR STABILIZATION
This book presents a program of back treatment based on the
8
.
Back Stability
new model of active patient participation. The most important concept underlying the program is that of lumbar back stability versus lumbar back instability. Instability of the lumbar spine is not the same as hypermobility. In both conditions the range of motion is greater than norma!. However, instability is present when there is "an excessive range of abnormal movement for which there is no protective muscular contro!." There is no instability in hypermobility, however, since the "excessive range of movement. . . has complete muscular control" (Maitland 1986). The essential feature of stability
is therefore
the ability of the body to control the whole range of motion
of a joint, in this case the lumbar spine.
~.
Stability of ajoint implies the body's ability to control the entire range of motion around that joint.
An unstable lumbar spine cannot maintain correct vertebral alignment. Because the unstable segment is less stiff (less resistant to movement), movement within the spinal column increases even under minor loadsthereby altering both the quality and quantity of motion. Unstable lumbar spines often reveal no clinical damage to the spinal cord or nerve roots and no incapacitating deformity. If untreated, however, an unstable spine may irritate or damage neural tissue, leading to positive neurological signs on clinical examination. Positive neurological examination therefore does not preclude prescription of stabilization exercise since instability may indeed be the cause of the positive findings. The excessive movement in an unstable spine may either stretch or compress pain-sensitive structures, leading to inflammation (Kirkaldy-Willis 1990; Panjabi 1992). A number of physical signs can suggest instability in a clinical assessment, as outlined in "Physical Signs of Instability," below. See also "Preliminary Assessment of Your Client," page 231. Physical
.
Signs of Instability
Step deformity (spondylolisthesis) or rotation deformity (spondylolisis)
on standing,
which reduces on lying
. Transverse band of muscle spasm, which reduces on lying
. Localized muscle twitching while shifting weight from one leg to the other . . Alteration to passive intervertebral motion testing, suggesting excessive mobility in the sagittal plane Juddering
or shaking during forward bending
Source; Paris 1985; Maitland 1986
What Is Back Stability?
.
9
Stable Movement and Position of the Lumbar Spine Both the gross and fine positions of the lumbar spine are vital to back stability and may be described in terms of "neutral zone" and "neutral position." Control of these positions requires an interplay among several body systems and forms the basis of the back stability program.
Movement in the Neutral Zone Lumbar instability may be defined as an excessive range of motion without muscular control. Another way to visualize instability is as a loss of stiffness (Pope and Panjabi 1985)-not the negative condition we refer to when we speak of "a stiff back:' but rather a positive factor referring to the amount of resistance a structure (in this case, the spine) provides in order to move against a force. (Imagine a bodybuilder arm wrestling a weakling, and consider whose arm would be more stiff/stable.) Less stiffness leads to more movement from application of the same force. If a back is not stiff enough, it will buckle and move under very little force, resulting in compression or stretching of sensitive structures. Pain is the consequence. Panjabi et al. (1989)proposed the concept of the neutral zone-the zone in which movement occurs at the beginning of the range of motion before any effective resistance is offered from either the muscular system or the spinal column. The neutral zone represents the range of motion that lacks effective restraint, either active or passive. It is the vertebral displacement that occurs before resistance is offered. A grossly unstable spinal segment has quite a large neutral zone (figure 1.2). Physiotherapists use this concept when they Vertebra in neutral position ~.~ anterior cc ~~movement 15 .(i) cn~ 1:J c:
+
posterior movement ~\!!.
~
~*
Q)
:J
£
llJ cc
Neutral zone-. Figure 1.2 The neutral zone.
10
. Back Stability
assess lumbar joint movements by palpation-they note the onset either of motion resistance or of pain as they move the joint. In the case of the lumbar spine in the prone position, movement of this type is usually in a posteroantero (PA) direction. Note that the resistance felt by physiotherapists is mainly passive and does not necessarily represent significant resistance offered by muscle contraction. The passive stability system (ligaments and bone contour) reduces motion toward the end of the neutral zone. Our strategy, however, is to reduce the size of the neutral zone by increasing muscle stability. Exercise that increases muscle stability may reduce motion within the neutral zone before the passive elements even come into play. Note that neutral zone motion is different from the total range of motion-€ven though stabilizing exercise increases muscle "stiffness," it does not correspondingly reduce the total range of motion. Panjabi (1992) investigated the relationship between total range to neutral zone range by studying the effect of external fixation on the cervical spine in cadavers-and noted that neutral zone motion declined over 70% in association with a decrease of only 40% in total range of motion. In reducing the size of the neutral zone, the back stability program decreases the amount of motion that occurs when minimal forces are imposed on the spine (Le., those same forces that, when experienced hour after hour, can produce the compression/ stretching that lead to back pain). A stable back is not constantly buffeted by minor stresses related to mere sitting, standing, etc., such as those that occur in individuals with unstable spines. Instability alters both the quality and quantity of lumbar motion.
KEY POINT:
Neutral Position of the Lumbar Spine The neutral position of the lumbar spine is different from the neutral zone. Lumbar neutral position refers to an overall movement of the lumbar spine rather than to individual movements between vertebrae. Lumbar neutral position is midway between full flexion and full extension as brought about by posterior and anterior tilting of the pelvis. Teaching patients to identify and maintain the neutral position of their lumbar spines is a key component of each stage of the back stability program, since the neutral position places minimal stress on body tissues. Also, because postural alignment is optimal, the neutral position is generally the most effective position from which trunk muscles can work. The neutral position of the lumbar spine is important in all stages of the back stability program because it minimizes stress.
KEY POINT:
What Is Back Stability?
.
11
Achieving and Maintaining Spinal Stability Three interrelated systems maintain spinal stability (figure 1.3). Inert tissues (in particular, ligaments) provide passive support; contractile tissues give active support; and neural control centers coordinate sensory feedback from both systems (Panjabi 1992). Since one or two systems may compensate for reduced stability in another, the active system may sometimes increase its contribution to stability in order to minimize stress on the passive system (Tropp et a!. 1993). When the goal of rehabilitation is healing of the spine, appropriate exercise-by enabling the active system to take more of the total load placed on the back-can permit the passive system to repair itself. The net result is decreased pain and increased function. Conversely, continually loading the passive system without proper support from the active system can increase the time to recovery and lead to further tissue damage. Simply developing muscle strength, however, is insufficient. To provide maximum relief to the passive system, one must augment both of the other systems (i.e., the active and neural control systems). Yetmany popular strength exercises for the trunk actually increase mobility in this region to dangerously high levels (Norris 1993, 1994a). Rather than improving stability, exercises of this type may reduce it and therefore exacerbate symptoms-€specially those associated with inflammation. An example is the bilateral straight-leg-raise movement where both legs are lifted simultaneously from a supine lying position. Although individuals performing this exercise may indeed strengthen their abdominal muscles, they often fail to maintain pelvic alignment. Anterior tilting of the pelvis leads to lumbar facet compression and overstretches the anterior spinal
Figure 1.3 The spinal stabilizing system consists of three interrelating subsystems. Reprinted, by permission, from M.M.Panjabi, 1992, "The stabilisation of the spine. Part 1. Function, dysfunction, adaptation, and enhancement," Journal of Spinal Disorders 5(4): 383-389.
12
.
Back Stability
tissues. In this case, the anterior longitudinal ligament of the spine may be overstretched, reducing the effect of an important passive stabilizing structure. Passive Support Passive support of the lumbar region is provided by the stretching (especially of ligaments) and compression of soft tissues. A compressed ligament is more relaxed and offers less support. In full lumbar extension, for example, as may occur when standing with an anteriorly tilted pelvis, the lumbar facet joints are loaded and compressed. The anterior structures, including the anterior longitudinal ligament, are stretched: stability is provided (passively) through elastic recoil of this ligament and because facet joints of the spine are forcibly closed. Developing Active Lumbar Stability Poor postural control can leave the spine vulnerable to injury by placing excessive stress on the body tissues (Kendall et al. 1993). In the lumbar spine, the trunk muscles protect spinal tissues from excessive motion. To do this, however, the muscles surrounding the trunk must be able to cocontract isometrically when appropriate (Richardson et al. 1990). The synergistic interaction between various trunk muscles is complex: some muscles act as prime movers to create the gross movements of the trunk, while others function as stabilizers (fixators) and neutralizers to support the spinal structures and control unwanted movements. Rehabilitation through active lumbar stabilization not only deals with the torqueproducing capacity of muscles, as is true of many traditional programs, but also seeks to enable a subject to unconsciously and consistently coordinate an optimal pattern of muscle activity Oull and Richardson 1994a). Developing the Neural System The neural system links the passive and active systems. Upon detecting movement within the neutral zone, the neural system relays information to the active system (muscles) about the position and direction of movement. The muscles' ability to contract and maintain stability (i.e., to increase stiffness and reduce the size of the neutral zone) depends on the speed and accuracy with which the information is relayed. The vital aspects of neural system development are therefore accuracy of movement and speed of reaction. Thus the stability program emphasizes accuracy of movement early on; speed comes later.
What Is Back Stability? . 1 3
SUMMARY
· · · . ·
Low back pain is a massive challenge to health-care professionals and a major financial drain on Western economies. Low back pain produces alterations in behavior patterns that can exacerbate the condition. The traditional structural approach to treating back pain must be balanced with restoration of function. New approaches to treating back pain emphasize the use of exercise ra ther than rest.
Back stability consists of three interrelating control systems: active, passive, and neural. . Although traditional exercise systems that work the trunk may strengthen muscle, they also may reduce total back stability. · Enhancing the active and neural systems can partially compensate for decrements in the passive system.
·
Enhanced movement accuracy and muscle reaction speed are vital to full rehabilitation of the back.
2 Biomechanics of the Lumbar Spine In order to explain how the back is stabilized, I must briefly review some important aspects of spinal anatomy. Chapter 1 describes the passive stability system-the "brakes" provided by inert tissues that will stretch only a certain amount (both individually and as systems of tissues) before they restrict further movement. In this chapter, I describe this passive system for each of the major physiological movements of the lumbar spine and then use the example of lifting to illustrate the importance of stability.
ANATOMY
OF THE VERTEBRAL
COLUMN
The gross anatomy of the lumbar spine includes vertebral bones, joints, and discs, plus the sacroiliac joints. Although none of these structures moves in isolation, it should prove helpful if I describe them individually.
The Bones and Their Joints The adult human vertebral column comprises 33 vertebrae. Five vertebrae are fused to form the sacrum and four are fused to form the coccyx. The remaining 24 movable vertebrae are divided among the cervical (7), thoracic (12) and lumbar (5) regions (figure 2.1). Any two neighboring vertebrae make up a spinal segment (figure 2.2). To understand how the vertebrae fit together in the spine, one must know the parts of the typical vertebra. The two vertebrae within a spinal segment are attached (articulated) by both joints and ligaments. There are three joints-the articulating triadconsisting of the disc, which forms the joint between the bodies of adjacent vertebrae, and the two facet joints (also called zygapophyseal or apophyseal joints), where the inferior articular processes on either side of the upper vertebra come together with the superior articular processes on either side of the lower vertebra. 14
Biomechanics of the Lumbar Spine
2.1 The vertebral column. Reprinted from Watkins 1999. Figure
.
15
Figure 2.2 A typical spinal segment. Reprinted
from
Watkins
1999.
A spinal segment comprises two adjacent vertebrae, articulating with each other through the intervertebral disc and two facet joints. The articulations form a triad.
KEY POINT: I
The disk and its associated facet joints are intimately linked both structurally and functionally. Degeneration of the intervertebral disc as a result of injury can lead to degeneration of the neighboring facet joints (Vernon-Roberts 1992); and as we shall see later, the ligamentous support to both structures is continuous. We can compare the spinal segment to a simple leverage system (Kapandji 1974), with the facet joints forming a fulcrum. The posterior tissues (ligamentous and muscular) and the anteriorly placed disc resist both compressive and tensile forces. The ligaments themselves may be categorized into three interrelating functional groups as shown in table 2.1.
Ligaments The neural arch ligaments consist mainly of the ligamentum flavum and the interspinous ligament, with the supraspinous and inter transverse
16
. Back Stability
Table 2.1
Ligaments
of the Spinal Segment
Neural arch Ligamentum flavum Interspinous ligament Supraspinous ligament Intertransverse ligament
. .. .
Capsular
.
Ventral
Facet joint capsule
(reinforced by the ligamentum flavum)
. .
Anterior longitudinal ligament Posterior longitudinal ligament
Adapted, by permission, from EH. Willard, 1997, The muscular, ligamentous and neural structure of the low back and its relation to back pain. In Movement stability and low back pain, edited by A. Vleeming, V. Mooney, T. Dorman, C. Snijders, and R. Stoeckart (Edinburgh: Churchill Livingstone).
a
Anterior longitudinal ligament
b
Left intertransverse ligament
Left ligamentum flavum
Figure 2.3 Ligaments of the spinal segment (a) side view, (b) superior view.
ligaments providing additional support (figure 2.3 a and b). Although these four ligaments are traditionally described as separate structures, they are actually merged at their edges and act functionally as a single unit. This is an extremely important point, as it bears significantly on the question of how one stabilizes the back. On dissection, when the bony components of the neural arch are removed, the neural arch ligaments can be seen to maintain their continuity (Willard 1997). The lateral fibers of the ligamentum f1avum are continuous with the facet joint capsule (YongHing et al. 1976) and form the rear wall of the spinal canal. The anterior border of the interspinous ligament is a continuation of the ligamentum f1avum, while the posterior border of this ligament is thickened into the supraspinous ligament. The supraspinous ligament merges with the thoracolumbar fascia (TLF) (figure 2.4), which in turn connects
TeymsYou .ShPEti(l$.now ~ articulate to join or connect loosely to allow motion between the connection, such as a joint caudal any tail-like structure contralateral fibers fibers originating in or affecting the opposite side of the body distraction force a force that separates a joint surface without injury or dislocation extension a movement that straightens a limb to a parallel or nearparallel position fascia a sheet of fibrous tissue under the skin that encloses muscles as well as separates and supports them; connects the skin with the tissue beneath it flexion bending or being bent; opposite of extension innominate bone the hip bone composed of the ilium, ischium, and pubis; forms the pelvis investing fascia fascia that surrounds rather than connects or separates ischemic deficiency of blood to a body part due to an obstruction in or a narrowing of the blood vessels lamina of vertebral arch the posterior portion of the arch that provides a base for the spine lateral flexion bending or being bent to the side lordosis inward curvature of the cervical and lumbar spines occiput the back part of the head vertebral pedicle the bony process that extends posteriorly from the body of a vertebra; one of the paired parts of the vertebral arch that connect the lamina to the vertebral body pelvic inlet the upper opening of the pelvis pelvic outlet the lower opening of the pelvis periosteum a thick, fibrous membrane covering all the bones of the body except at the joints prolapse downward displacement sagittal rotation turning from the front to the back sagittal plane a vertical plane through the body that divides it into the left and right side Schmorls node an irregular or hemispherical bone defect in the body of a vertebra, which a spinal disk herniates into trabecula fibrous cord of connective tissue that extends into an organ's wall to serve as support ventral front side of the body
17
18
.
Back Stability
Ligamentum
flavum
Superior articular process
Figure 2.4 Interspinous-supraspinous-thoracolumbar (1ST)ligamentous complex. The 1STcomplex supports the lumbar spine by anchoring the thoracolumbar fascia and multifidus sheath to the facet joint capsules
with the deep abdominal muscles (see page 57). The force generated by the deep abdominal muscles therefore can be transmitted through the TLF, via the supraspinous ligament, directly into the ligamentum flavum-preventing this ligament from buckling towards the spinal cord. This is one way the deep abdominals assist in spinal stabilization. Note that it is not only abdominal muscles that affect the spine. The interspinous ligament merges with the supraspinous ligament and then into the TLF, forming the interspinous-supra spinous-thoracolumbar (1ST) ligamentous complex (Willard 1997). The 1STcomplex attaches the fascia of the back to the lumbar spine. The importance of this system is that tension developed in the extremities is transmitted to the vertebral column, making the seemingly distant limb musculature essential to the rehabilitation of spinal function. The intertransverse ligament, although small, becomes more important caudally as it expands into the iliolumbar ligament, the importance of which I will discuss later. Force from the extremity muscles is transmitted to the spine via ligaments and fasciae, which ultimately attach to the vertebrae themselves. The deep abdominal muscles have
KEY POINT:
lth:. g~eate~tcapacityto stabilizethe spine. _
_
__ _
j
The capsule of the facet joint is reinforced posteriorly by the multifidus muscle and anteriorly by the ligamentum flavum. It is surrounded by fascia which is itself continuous with that covering the ligamentum flavum and the investing fascia of the vertebral body. The facet joint capsule there-
Biomechanics of the Lumbar Spine
.
19
fore can be seen as a "bridge" of connective tissue between the ligaments of the neural arch and those of the vertebral body (Willard 1997) (figure 2.5). The anterior longitudinal ligament (ALL) and posterior longitudinal ligament (PLL) lie ventrally within the spinal segment. The ALL is the stronger of the two and extends from the occiput to the sacrum where it merges with the sacroiliac joint capsule. The ALL has two sets of fibers (Bogduk and Twomey 1991). The superficial fibers span several vertebral segments, while the deep fibers attach loosely to the annulus of the spinal disc (figure 2.6). The PLL exists in the cervical spine as the tectorial membrane and extends caudally to the periosteum of the sacrum. It expands as it passes the intervertebral discs and narrows around the vertebral body. Because it is considerably weaker than the ALL, the main ligamentous restriction to flexion is not from the PLL but from the ligamentum flavum and the facet joint capsule into which it merges. The ligamentum flavum and facet joint capsules combine to offer 52% of the resistance to flexion in the lumbar spine (Bogduk and Twomey 1991). The structural pairing of the PLL and the ligamentum flavum is functionally obvious as well. Load-deformation (stress-strain) curves plotted for the two ligaments are similar (Panjabi and White 1990), suggesting in this case that the two ligaments may have a similar purpose.
Ligamentum
flavum
Multifidus muscle
Figure 2.5 Facet joint capsule. Reprinted from Watkins 1999.
Figure 2.6 Vertical section through pedicles in lumbar region: posterior aspect of vertebral bodies showing attachment of posterior longitudinal ligament to spinal discs. Reprinted from Watkins 1999.
20
. Back Stability
The longitudinal ligaments are viscoelastic, meaning that they stiffen when loaded rapidly. They do not store all the energy used to stretch them because they lose some as heat, a feature known as hysteresis. When loaded repeatedly, these ligaments become even stiffer, and the hysteresis is less marked, making them more prone to fatigue failure (Hukins 1987). The supraspinous and interspinous ligaments are farther from the flexion axis and therefore need to stretch more than the posterior longitudinalligament when they resist flexion. With age, all ligaments gradually lose their ability to absorb energy (Tkaczuk 1968). The stiffest ligament in the spine is the posterior longitudinalligament; the most flexible is the supraspinous (Panjabi et al. 1987). The ligamentum flavum in the lumbar spine is "pretensioned" (possesses tension at rest) when the spine is in its neutral position, a situation that compresses the spinal disc. This ligament has the highest percentage of elastic fibers of any tissue in the body (Nachemson and Evans 1968) and contains nearly twice as much elastin as collagen. The anterior longitudinalligament and joint capsules are among the strongest ligamentous tissues in the body, while the interspinous and posterior longitudinalligaments are the weakest (Panjabi et al. 1987). The ligamentum f1avum is the most elastic ligament in the body and the main ligament limiting flexion. It forms the anterior portion of the facet joint capsule.
KEY POINT:
Spinal Discs There are 24 intervertebral discs lying between successive vertebrae, making the spine an alternatively rigid then elastic column. The amount of flexibility in a particular spinal segment is determined by the size and shape of the disc and by the resistance to motion of the soft tissue that supports the spinal joints. The discs increase in size as they descend the column, the lumbar discs having an average thickness of 10 mm, twice that of the cervical discs. The disc shapes are accommodated to the curvatures of the spine and to the shapes of the vertebrae. The greater anterior widths of the discs in the cervical and lumbar regions reflect the curvatures of these areas. Each disc comprises three closely related components-the annulus fibrosis, nucleus pulposus, and cartilage end plates (figure 2.7). The annulus comprises layers of fibrous tissue arranged in concentric bands-about 20-like those in an onion. The fibers within each band are parallel, with the various bands angled at 45° to each other. The bands are more closely packed anteriorly and posteriorly than they are laterally, and those innermost are the thinnest. Fiber orientation, although partially determined at birth, is influenced by torsional stresses in the adult (Palastanga
Biomechanics of the Lumbar Spine
.
21
Anterior Nucleus
pulposus
Annulus fibrosus
Posterior Figure through
2.7 (a) Concentric a disc.
bands
of annular
fibers.
(b) Horizontal
section
Reprinted, by permission, from j. Watkins, 1999, Structure and function of the musculoskeletal system (Champaign, IL: Human Kinetics), 142.
et al. 1994). The posterolateral regions have a more irregular makeuppossibly one reason why they become weaker with aging and more predisposed to injury. KEY POINT: I
The spinal discs have fewer concentric bands
posterolaterally than in other regions, and these are irregularmaking this region of the disc more susceptible to injury.
The annular fibers pass over the edge of the cartilage end plate of the disc and are anchored to the bony rim of the vertebra and to its periosteum and body. The attaching fibers are actually interwoven with the fibers of the bony trabeculae of the vertebral body. The outer layer of fibers blend with the posterior longitudinal ligament; some authors claim that the anterior longitudinal ligament has no such attachment (Vernon-Roberts 1987). Resting on the surface of the vertebra, the hyaline cartilage end plate is approximately 1 mm thick at its outer edge and becomes thinner toward its center. The central portion of the end plate acts as a semipermeable membrane to facilitate fluid exchange into and out of the disc; it also protects the vertebral body from excessive pressure. In early life, canals from the vertebral body penetrate the end plate, but these disappear after the age of 20 to 30. The end plate then starts to ossify and become more brittle, while the central portion thins and, in some cases, is completely destroyed. The nucleus pulposus is a soft hydrophilic (water-attracting) substance taking up about 25% of the total disc area. It is continuous with the annulus, but the nuclear fibers are far less dense than those of the annulus. Mucopolysaccharides called proteoglycans fill the spaces between the collagen fibers of the nucleus, giving the nucleus its water-retaining capacity
. BackStability
22
and making it mechanically plastic. Metabolically very active, the area between the nucleus and annulus is sensitive both to physical force and to chemical/hormonal influence (Palastanga et al. 1994). Although the collagen volume of the nucleus remains unchanged, the proteoglycan content decreases with age-leading to a net reduction in water content. In early life, the water content may be as high as 80-90%, but this decreases to about 70% by middle age. The lumbar discs are the largest avascular structures in the body. The nucleus obtains fluids by passive diffusion from the margins of the vertebral body and across the cartilage end plate-particularly across the center of the end plate, which is more permeable than the periphery. Intense anaerobic activity within the nucleus (Holm et al. 1981) can lead to lactate buildup and low oxygen concentration, placing the nuclear cells at risk. Inadequate ATP levels may lead to cell death. Some researchers hypothesize that regular exercise involving movement of the spine may improve the nutrition of the disc-and over the years might not only improve the general health of discs, but even slow the loss of height due to water loss from discs. KEY POINT: The lurTihar spinal discs are avascular and depend on fluid exchange by passive diffusion. Regular movement/ activity is vital to this process.
:
Facet Joints The facet joints are synovial joints (cushioned by synovia, a viscous fluid) between the inferior articular process of one vertebra and the superior articular process of its neighbor. As with other typical synovial joints, they have articular cartilage, a synovial membrane to contain the fluid, and a joint capsule; but they also have a number of unique features (Bogduk and Twomey 1991). The facet joint capsule holds about 2 ml of synovial fluid. Its anterior wall is formed by the ligamentum flavum; posteriorly, the capsule is reinforced by the deep fibers of the multifidus muscle. At its superior and inferior poles, the joint leaves a small gap, creating the subscapular pockets. These are filled with fat, contained within the synovial membrane. Within the subscapular pocket lies a small foramen for passage of the fat in and out of the joint as the spine moves. Within the capsule, there are three structures of interest. The first is the connective tissue rim, a thickened wedge-shaped area that makes up for the curved shape of the articular cartilage in much the same way as the menisci of the knee do. The second structure is an adipose tissue pad, a 2-mm fold of synovium filled with fat and blood vessels. The third structure is the fibroadipose meniscoid, a 5-mm leaf-like fold that projects from the inner sur-
Biomechanics of the Lumbar Spine.
23
faces of the superior and inferior capsules. The last two structures have a protective function. Flexion leaves some of the articular facets' cartilage exposed-both the adipose tissue pad and the fibro-adipose meniscus cover the exposed regions (Bogduk and Engel 1984). With aging, cartilage of the facet joint can split parallel to the joint surface, pulling a portion of joint capsule with it. The split cartilage, with its attached piece of capsule, forms a false intra-articular meniscoid (Taylor and Twomey 1986). Flexion normally draws the fibro-adipose meniscus out from the joint, and it moves back in with extension. If the meniscus fails to move back, it will buckle and remain under the capsule, causing pain (Bogduk and Jull 1985). A mobilization or manipulation that combines flexion and rotation may relieve pain by allowing the meniscoid to move back into its original position.
The Sacroiliac Joint As with the lumbar spine, the sacroiliac joint (SIJ)-the rather large surface where the sacrum (the five fused bottom vertebrae of the spine) fits into the pelvis (figure 2.8)-is stabilized by several ligaments that connect to muscles within the region. The iliolumbar ligament attaches to the transverse process of 1.5, and in some subjects to those of L4 as well (Willard 1997), and passes anteromedially to the iliac crest and the surface of the a
Iliolumbar ligaments Anterior sacroiliac ligament
Right innominate bone (ilium,ischium, and pubis)
b
Sacrotuberous ligament
Iliolumbar ligaments
Pubic arch c Iliac crest Posterior sacroiliac ligament
Sacrospinous ligament Ischial tuberosity Sacrotuberous ligament Figure 2.8 The sacroiliac joint and its supporting ligaments: (a) anterior aspect; (b) posterior aspect; and (c) left aspect of medial section through the pelvis. Reprinted, by permission, from J. Watkins, 1999, Structure and function of the musculoskeletal system (Champaign, IL:Human Kinetics), 1972.
24
.
Back Stability
ilium. The iliolumbar ligament resists movement between the sacrum and lumbar spine, particularly that of lateral flexion. When the ligament is cut, movement of the lumbar spine (L5) on the sacrum increases significantly-lateral flexion by nearly 30%; and flexion, extension, and rotation by 18-23% (Yamamoto et al. 1990). The superior aspect of the SIJcapsule is an extension of the iliolumbar ligament, while the anterior portion of the capsule merges into the sacrotuberous ligament. The sacrotuberous ligament has a triangular shape extending between the posterior iliac spines, SIJ capsule, and coccyx (figure 2.8). Importantly, the tendon of biceps femoris (the large muscle at the back of the upper leg) extends over the ischial tuberosity to attach to the sacrotuberous ligament (Vleeming et al. 1989); the ligament also attaches into some of the deepest fibers of the multifidus muscle (the multifidus runs vertically down the entire length of the back, on either side of the spine) (Willard 1997). Movement at the sacroiliac joint is described as nutation and countemutation (table 2.2). The sacrotuberous ligament resists nutation of the sacrum, while the long dorsal sacroiliac ligament resists countemutation. Even though it is difficult to discern this from observing most anatomical diagrams, the sacrum is not fused with the pelvis-so when I speak of movement of the sacrum, I mean motion within the pelvis as opposed to motion of the pelvis, where the entire structure is moving on the hip. Greater movement ranges have been reported in nonweightbearing than weightbearing movements. Nonweightbearing movements have exhibited as much as 12° innominate rotation during flexion, together with 8 mm translation during extension (Lavignolle et a!. 1983); weightbearing movements were reduced to 2.5° rotation and 1.6 mm maximal translaTable 2.2
Movement
of the Sacroiliac
Nutation Anterior tilting of sacrum Sacral base moves down and forward, apex moves up Size of pelvic outlet increased, pelvic inlet decreased Occurs in standing
.. .
. . Increased as lumbar lordosis increased
.
Iliac bones pulled together,
impacted . Superior aspect of pubis compressed
SIJ
Joint (SIJ)
Counternutation Posterior tilting of sacrum Sacral base moves up and back, apex moves down Pelvic inlet increased, outlet red uced . Occurs in nonweightbearing position such as lying Increased as lumbar lordosis decreased (flatback posture) Iliac bones move apart, SIJdistracted
. .
. . .
. Inferioraspect of pubiscompressed
Biomechanics of the Lumbar Spine
.
25
tion (Sturesson et al. 1989).In a study of healthy individuals aged 20-50 years, Jacob and Kissling (1995) found average rotational motion at the SI] to be 2°, whereas symptomatic patients averaged 6°. Nutation of the SIJ is an anterior tilting of the sacrum on the fixed innominate bones. The sacral base moves down and forward, while the sacral apex moves up, increasing the pelvic outlet. Nutation occurs in standing and increases as lordosis deepens. By pulling the iliac bones together, nutation compresses the SI] as well as the superior portion of the pubic symphasis. Countemutation is the opposite movement, with the sacral base moving up and back and the apex moving downward. This movement occurs in nonweightbearing situations, such as lying prone, and increases as the lordosis is reduced and the low back is flattened. During countemutation, the iliac bones move apart, the pelvic inlet increases, and the pelvic outlet reduces (Kesson and Atkins 1998). A variety of movements occur about the SI] during trunk actions (Lee 1994). During forward bending of the trunk, the pelvis tilts anteriorly and the sacrum moves into extension (coccyx moving backward; i.e., nutation around an oblique axis), causing the iliac crests and posterior superior iliac spines (PSIS) to approximate (i.e., press toward each other) and the ischial tuberosities and the anterior superior iliac spines (ASIS) to separate. During side bending, the trunk laterally flexes and the pelvis shifts to the opposite direction to maintain balance. With left lateral flexion and right pelvic shift, the right innominate bone rotates posteriorly, and the left innominate rotates anteriorly. The sacrum rotates to the right. During trunk rotation, the pelvis rotates in the same direction; therefore, with left trunk rotation, the right innominate anteriorly rotates and the left posteriorly rotates. The sacrum is driven into left rotation.
AXIAL COMPRESSION Vertical loading of the lumbar spine (axial compression) occurs during upright (standing or sitting) postures, exacerbating certain forms of back pain. Knowledge of loading can help us to design safer exercise programs for the back pain sufferer.
Compression
of the Vertebral
Bodies
Within the vertebra itself, compressive force is transmitted by both the cancellous (spongy) bone of the vertebral body and its cortical bone shell. Until about the age of 40, the cancellous bone contributes about 25-55% of the vertebra's strength. As aging-related decreases in bone density lead to a decline in the proportion of cancellous bone, the cortical bone shell carries a greater proportion of load (Rockoff et al. 1969). As the vertebral body is compressed, a net flow of blood out of it (Crock and Yoshizawa
26
. BackStability
1976) reduces bone volume and dissipates energy (Roaf 1960). Blood returns slowly as the force is reduced-leaving a latent period after the initial compression and diminishing the shock-absorbing properties of the bone. Exercises that involve prolonged periods of repeated shock to the spine (e.g., jumping on a hard surface) are therefore more likely to damage vertebrae than those that load the spine for short periods and allow recovery of the vertebral blood flow before repeating a movement.
.
Blood flows-out of the vertebral body with loading, decreasing its shock-absorbing properties. Exercises I that repeatedly load the spine without allowing recovery can therefore lead to accumulated stress.
KEY POINT:
Compression of Intervertebral Discs During standing, 12-25% of axial compression forces are transmitted between adjacent vertebrae by the facet joints (see discussion on page 28); the intervertebral disc absorbs the rest of the force (Miller et al. 1983). The annulus fibrosis of a healthy disc resists buckling; even if a disc's nucleus pulposus has been removed, its annulus alone can exhibit a loadbearing
capacity similar to that of the fully intact discfor a brief period (Markolfand Morris 1974). When exposed to prolonged loading however, the collagen
lamellae of the annulus eventually buckle (see figure 2.7). Throughout the waking day, discalloading diminishes a person's height until the forces inside the disc equal the load forces (Twomey and Taylor 1994). By reducing axial loading, lying down permits restoration of the former spinal length. Lying in a flexed position speeds the regain of lost height as the lumbar discs are distracted (unloaded) during flexion (Tyrrell et al. 1985). Application of an axial load compresses the fluid nucleus of the disc, causing it to expand laterally. This lateral expansion stretches the annular fibers, preventing them from buckling. The degree of discal compression depends on the weight imposed and the rate of loading. A 100kg axial load can compress a disc by 1.4 mm and cause a lateral expansion of 0.75 mm (Hirsch and Nachemson 1954). The stretch in the annular fibers stores energy, which is released when the compression stress is removed. The stored energy gives the disc a certain springiness, which helps to offset any deformation that occurred in the nucleus. A force applied rapidly is not lessened by this mechanism, but its rate of application is slowed, giving the spinal tissues time to adapt. Deformation of the disc occurs more rapidly at the onset of axial load application, the majority of its deformation occurring within 10 minutes of onset. After this time, deformation continues but slows to a rate of about 1 mm per hour (Markolf and Morris 1974),leading to loss of height throughout the day. Under constant loading the discs exhibit "creep" (i.e., they
Biomechanics
of the
Lumbar
Spine
.
27
continue to deform even though the load is not increasing). Because compression causes a rise in fluid pressure, fluid is actually lost from both the nucleus and the annulus. About 10% of the water within the disc can be squeezed out by this method (Kraemer et al. 1985), the exact amount dependent on the size and duration of the applied force. When the compressive force is reduced, the fluid is absorbed back through pores in the cartilage end plates of the vertebra. Exercises that axially load the spine reduce a person's height through discal compression-squat exercises in weight training, for example, can create compression loads in the L3-L4 segment of 6-10 times bodyweight (Cappozzo et al. 1985). Researchers have observed average height losses of 5.4 mm over a 25-minute period of general weight training, and 3.25 mm after a 6-km run (Leatt et al. 1986) (figure 2.9). Static axial loading of the spine with a 40-kg barbell over a 20minute period can reduce a subject's height by as much as 11.2mm (Tyrrell et al. 1985). Clearly, exercises that involve this degree of spinal loading are unsuitable for individuals with discal pathology. The vertebral end plates of the discs are compressed centrally and are able to undergo less deformation than either the annulus or the cancellous bone. The end plates are therefore likely to fail (fracture) under high compression (Norkin and Levangie 1992). Discs subjected to very high compressive loads can show permanent deformation without herniation (Farfan et al. 1976; MarkoH and Morris 1974). However, such compression forces may lead to Schmorls node formation (Bernhardt et al. 1992): the disc end plate (which joins the disc to the vertebral body) ruptures, and nuclear material from the disc passes through to the vertebral body itself. Bending and torsional stresses on the spine, when combined with compression, are more damaging than compression alone, and degenerated discs are particularly at risk. Average failure torques for normal discs are
D D
15
E
.s
10
Weight
training 6-km run
.40-k9 ~static load
.E
C> 0ij; I
5
o
Activity
Figure 2.9 Discal compression
and height loss during exercise.
28
. Back Stability
25% higher than for degenerative discs (Farfan et al. 1976). Degenerative discs also demonstrate poorer viscoelastic properties and therefore a reduced ability to attenuate shock. The proteoglycan of the disc's nucleus makes it hydrophilic, and its ability to transmit load relies on high water content; yet proteoglycan content declines from about 65% in early life to about 30% by middle age (Bogduk and Twomey 1987). When the proteoglycan content of the disc is high (up to age 30 in most subjects), the nucleus pulposus is gelatinous, producing a uniform fluid pressure. After this age, the lower water content of the disc leaves the nucleus unable to build as much fluid pressure. Less central pressure is produced, and the load is distributed more peripherally, eventually causing the annular fibers to become fibrillated and to crack (Hirsch and Schajowicz 1952). The net result is that a disc's reaction to compressive stress declines with age (figure 2.10). The age-related changes in discs cause greater susceptibility to injury. This fact-<:ombined with a general reduction in fitness and changes in trunk movement patterns related to activities of daily living-greatly increases the risk of injury in older individuals. Encourage previously inactive persons over the age of 40 to engage in trunk exercises, under the supervision of a physiotherapist, before attending fitness classes.
Compression
of Facet Joints
The orientations of facet joints differ among various regions of the spine, thereby altering the available motion. In the mid- and lower cervical spine, for example, rotation and lateral flexion are limited but flexion and extension are possible. In the thoracic spine, flexion and extension are limited but lateral flexion and rotation are free. At the thoracolumbar junction (T12-Ll), rotation is the only movement that is limited; in the lumbar spine, both rotation and lateral flexion are limited. a
b
Figure 2.10 Age-related changes in lumbar discs. (a) Maximal disc height and end plate length of youth. (b) Reduced measurements through aging.
Biomechanics of the Lumbar Spine
.
29
The superior / inferior alignment of the facet joints in the lumbar spine means that, during axial loading in the neutral position, the joint surfaces slide past each other. Note, however, that anywhere between T9 and T12, the orientation of the facet joints may change from those characteristic of the thoracic spine to those of the lumbar spine. Therefore, the level at which particular movements will occur can vary considerably among subjects. During lumbar movements, displacement of the facet joint surfaces causes them to impact, or press together. Because the sacrum is inclined and the body and disc of L5 are wedge shaped, during axial loading L5 is subjected to a shearing force. This force is resisted by the more anterior orientation of the L5 inferior articular processes. As the lordosis increases, moreover, the anterior longitudinal ligament and the anterior portion of the annulus fibrosis are stretched, providing tension to resist the bending force. Additional stabilization is provided for the L5 vertebra by the iliolumbar ligament, attached to the L5 transverse process. This ligament, together with the facet joint capsules, stretches to resist the distraction force. Once the axial compression force stops, release of the stored elastic energy in the spinal ligaments re-establishes the neutral lordosis. With compression of the lordotic lumbar spine, or in cases where gross disc narrowing has occurred, the inferior articular processes may impact on the lamina of the vertebra below (see figure 2.11). In this case, the lower joints (L3/4, L4/5, L5/S1) may bear as much as 19% of the compression force, while the upper joints (Ll/2, L2/3) bear only 11% (Adams et al. 1980).
Figure 2.11 Results of compression on discs and facet joints. (a) Normal disc thickness and alignment of superior and inferior articular processes. (b) Reduced disc thickness resulting in increased compression load on facet joint. (c) Extra.articular impingement of facet joint. Reprinted, by permission, from J. Watkins, 1999, Structure and function of the musculoskeletal system (Champaign, IL:Human Kinetics), 146.
30
.
Back Stability
MOVEMENTS
OF THE LUMBAR
SPINE AND PELVIS
Much of the material for this section comes from Norris (1995a) and Norris (1998), to which I refer you for further reading.
Flexion and Extension Both disc height and the horizontal length of the vertebral end plate affect the range of motion attainable during sagittal plane movement of the lumbar spine. Greatest range of motion occurs with a combination of maximum disc height and maximum end plate length (figure 2.10). Since this alignment most often occurs in young females, it is they who possess the greatest ranges of motion at the lumbar spine. With aging, disc height and end plate length become more similar between the sexes, equalizing the available range of motion for males and females in old age (Twomey and Taylor 1994). Q) During flexion movements, the C> C anterior annulus of a lumbar disc co .J::. is compressed, whereas the posU Q) terior fibers are stretched. Simi:; larly, the nucleus pulposus of the disc is compressed anteriorly, c. Q) whereas pressure is relieved over .2: OJ its posterior surface. Since the a; c: total volume of the disc remains unchanged, however, its pressure a should not increase. The increases in pressure seen with posture Q) changes are due not to the bendC> C ing motion of the bones within co .J::. the vertebral joint itself but to the U !!? soft tissue tension created to con::> (/) (/) trol the bending. If the pressure Q) ~ at the L3 disc for a 70-kg standc. Q) ing subject is said to be 100%, su.2: OJ pine lying reduces the pressure to a; c: 25%. The pressure variations inb crease dramatically as soon as the Figure 2.12 Pressure changes in the lumbar spine is flexed and tissue third lumbar disc: (a) in different posi- tension increases (figure 2.12). The sitting posture increases intions; (b) in different muscle-strengthening exercises. tradiscal pressure to 140%, whereas sitting and leaning forFrom Norris 1998. (/) (/) Q)
Biomechanics of the Lumbar Spine
.
31
ward with a lO-kg weight in each hand increases pressure to 275% (Nachemson 1992). The selection of an appropriate starting position for trunk exercises is therefore of great importance. Spinal exercise from a slumped sitting posture, for example, places considerably more stress on spinal discs than the same movement beginning from crook lying (lying on the back with the knees and hips flexed, feet flat on the floor). The posterior annulus stretches during flexion, whereas the nucleus is compressed onto the posterior wall. Since the posterior portion of the annulus is the thinnest part, the combination of stretch and pressure to this area may result in discal bulging or herniation. Because layers of annular fibers alternate in direction, rotation movements stretch only half of the fibers at any given time. The disc is more easily injured during a combination of rotation and flexion, which stretches all the fibers at the same time. As the lumbar spine flexes, the lordosis flattens and then reverses at its upper levels. Reversal of lordosis does not occur at LS-S1 (Pearcy et al. 1984). Flexion of the lumbar spine involves a combination of anterior sagittal rotation and anterior translation. As sagittal rotation occurs, the articular facets move apart, permitting the translation movement to occur. Translation is limited by impaction of the inferior facet of one vertebra on the superior facet of the vertebra below. As flexion increases, or if the spine is angled forward on the hip, the surface (i.e., the top) of the vertebral body faces more vertically, increasing the shearing force due to gravity. The forces involved in facet impaction therefore increase to limit translation of the vertebra and stabilize the lumbar spine. Because the facet joint has a curved articular facet, the load is not concentrated evenly across the whole surface but is focused on the anteromedial portion of the facets (figure 2.13). The sagittal rotation movement of the facet joint causes the joint to open and is therefore limited by the stretch of the joint capsule. The posteriorly placed spinal ligaments are also tightened. Adams et al. (1980) used mathematical modeling to analyze the forces that limit sagittal rotation within the lumbar spine. They found that the disc contributes 29% of the limit to movement, the supraspinous and interspinous ligaments 19%, and the facet joint capsules 39%. In one experiment, the researchers cut (and thereby "released") various posterior tissues in cadavers in order to measure the effects of those tissues on flexion range. Range of motion increased about 40 when the posterior ligaments were released and 90 when the capsule was released. Releasing the pedicles increased the flexion range by 240 in young (14-22 years) subjects. Cutting all the posterior elements increased the flexion range by 100% in the young subjects but by only 60% in the elderly (61-78 years) subjects. During sustained flexion, tissue overstretch results in creep-gradually increasing the range of motion as tissues elongate over time. With aging, the amount of creep is greater, but recovery takes longer (Twomey and
32
. Back Stability Taylor 1994). Occupations that involve prolonged flexion with little recovery (e.g., bricklaying or sitting with poor posture) provide little chance for the overstretched tissue to recover, leading to chronic adaptation of both soft tissue and bone. Such individuals suffer from a high incidence of chronic postural back pain with many acute episodes (Twomey et al. 1988). Sustained flexion results in creep of the lumbar tissues (Le., a gradual increase in range of motion over time). Prolonged flexion with inadequate tissue recovery can lead to chronic adaptation and consequent pain.
KEY POINT:
During extension, anterior structures are under tension, whereas posterior structures are first taken off c stretch and then compressed (depending on the range of motion). Extension movements subject the vertebral bodies to posterior sagittal rotation. The inferior articular processes move downward, causing them to impact against the lamina of the vertebra below. Once the bony block has occurred, if further load is applied, the upper vertebra will axially rotate by pivoting on the impacted inferior articular process. The inferior articular process will move backward, overstretching and possibly damaging the joint capsule (Yang and King 1984). Repeated moveFigure 2.13 The lower lumbar spine and sacrum in (a) standing, ments of this type eventually can lead (b) extension, and (c) flexion. to erosion of the laminal periosteum Reprinted, by permission, from J. (Oliver and Middleditch 1991). At the Watkins, 1999, Structure and function site of impaction, the joint capsule may of the musculoskeletal system (Chamcatch between the opposing bones, crepaign, IL:Human Kinetics), 147.
Biomechanics of the Lumbar Spine.
33
ating another source of pain (Adams and Hutton 1983). Since structural abnormalities can alter a vertebra's axis of rotation, considerable variation exists among subjects (Klein and Hukins 1983).
Rotation and Lateral Flexion During rotation, torsional stiffness is provided by the outer layers of the annulus, by the orientation of the facet joints, and by the cortical bone shell of the vertebral bodies themselves. Moreover, the annular fibers of the disc are stretched as their orientation permits-since alternating layers of fibers are angled obliquely to each other, some fibers will be stretched while others relax. A maximum range of 3° of rotation can occur before the annular fibers will be microscopically damaged and a maximum of 12° before tissue failure (Bogduk and Twomey 1987). The spinous processes separate during rotation, stretching the supraspinous and interspinous ligaments. Impaction occurs between the opposing articular facets on one side, causing the articular cartilage to compress by 0.5 mm for each 1° of rotation and providing a substantial buffer mechanism (Bogduk and Twomey 1987). If rotation continues beyond this point, the vertebra pivots around the impacted facet joint, causing posterior and lateral movement. The combination of movements and forces stress the impacted facet joint by compression, the spinal disc by torsion and shear, and the capsule of the opposite facet joint by traction. The disc provides only 35% of the total resistance (Farfan et al. 1976). When the lumbar spine is laterally flexed, the annular fibers toward the concavity of the curve are compressed and begin to bulge, while those on the convexity of the curve are stretched. The contralateral fibers of the outer annulus and the contralateral intertransverse ligaments help to resist extremes of motion (Norkin and Levangie 1992). Lateral flexion and rotation occur as coupled movements. In the neutral position, rotation of the upper four lumbar segments is accompanied by lateral flexion to the opposite side; rotation of the L5-S1 joint, however, occurs with lateral flexion to the same side. The nature of the coupling varies with the degree of flexion and extension. In the neutral position, rotation and lateral flexion occur to the opposite side, called "type I movement" (i.e., right rotation is coupled with left lateral flexion). But when the lumbar spine is in flexion or extension, rotation and lateral flexion occur in the same direction, called "type II movement" (i.e., right rotation is coupled with right lateral flexion). In the concavity of lateral flexion, the inferior facet of the upper vertebra slides downward on the superior facet of the vertebra below, reducing the area of the intervertebral foramen on that side. On the convexity of the laterally flexed spine, the inferior facet slides upwards on the superior facet of the vertebra below, increasing the diameter of the intervertebral foramen.
34
.
Back Stability
Lumbar-Pelvic Rhythm When people bend forward as though to touch their toes, the movement comes from both the pelvis and the lumqar spine. The pelvis anteriorly tilts on the femur, while the lumbar spine flexes on the pelvis. The combined movement of both lumbar and pelvic motion is called "lumbarpelvic rhythm." With the lumbar spine held immobile and the knees locked, the pelvis can tilt only to roughly 90° hip flexion (hamstring tightness limits further movement). To touch the floor, one must also flex the lumbar spine. Similarly, with the pelvis held immobile, lumbar flexion is limited to about 30-40°, with most movement occurring at the lower lumbar segments. Therefore, to achieve full forward bending, one must move both body segments. When flexing to midrange levels during daily living, individuals can significantly reduce their lumbar flexion by using anterior pelvic tilt. Reduced ability to anteriorly tilt the pelvis increases the need to flex the lumbar spine, opening the possibility of postural pain through repetitive loading of the lumbar tissues. When a person bends forward from a standing position, the pelvis and lumbar spine rotate in the same direction. Lumbar flexion accompanies anterior tilt of the pelvis (figure 2.14a). In the upright posture, the feet and shoulders are static, and the pelvis and lumbar spine move in opposite directions (figure 2.14b)-lumbar extension compensates for an anteriorly tilted pelvis in order to maintain the head and shoulders in an upright orientation. Table 2.3 describes the relationship between various pelvic movements and the corresponding hip joint action. b
Figure 2.14 (a) Lumbar-pelvic rhythm in open chain formation occurs in the same direction. Anterior pelvic tilt accompanies lumbar flexion. (b) Lumbarpelvic rhythm in closed kinetic chain formation occurs in opposite directions. Anterior pelvic tilt is compensated by lumbar extension. From Norris 1998.
Biomechanics of the Lumbar Spine
.
35
Table 2.3 Relationship of Pelvis, Hip Joint, and Lumbar Spine During Right Lower-Extremity Weightbearing and Upright Posture Pelvic
motion
Anterior
pelvic
Posterior
Accompanying joint motion tilt
pelvic
tilt
hip
Compensatory lumbar motion
Hip flexion
Lumbar extension
Hip extension
Lateral drop)
pelvic
tilt (pelvic
Right hip adduction
Lumbar flexion Right lateral flexion
Lateral hitch)
pelvic
tilt (hip
Right hip abduction
Left lateral
Right hip MR
Rotation
to the left
Right hip LR
Rotation
to the right
Forward Backward
rotation
rotation
MR = medial rotation; LR = lateral rotation. Reprinted, by permission, from c.c. Norkin and P.K. Levangie, and function: A comprehensive analysis, 2d ed. (Philadelphia:
flexion
1992, joint structure Davis).
Controlling Spinal Range of Motion If the trunk is moving slowly, a subject feels tissue tension at the end range and is able to stop a movement short of the full end range-thereby protecting the spinal tissues from overstretching. However, rapid trunk movements can build up sufficient momentum to push the spine to the full end range, thereby stressing the spinal tissues. Many amateur and even professional sports directors, teachers, and coaches have their charges engage in rapid and ballistic warm-up exercises, performed with high numbers of repetitions. These activities can lead to excessive flexibility and a reduction in passive stability of the spine.
THE MECHANICS
OF LIFTING
Many individuals engage in some sort of lifting throughout the day. This section briefly describes the mechanical factors and the muscle work involved in lifting. See chapter 11 for proper lifting techniques.
Lifting As a Set of Torques Lifting an object from the ground actually represents a rather complex mechanical problem. One must create a set of torques (technically, torque = force x distance to axis of rotation), involving both the body and the object to be lifted, that will produce the desired outcome (figure 2.15). The forces created during flexion by leverage, body weight, and muscle force-plus those created by the weight being lifted-must be overcome
36
.
Back Stability
by an opposing extension force created by the hip extensor muscles as they contract upon the spine.
·
If the spine is not stable, posterior pelvic tilting brought about by the hip extensors (gluteus maximus and the hamstrings) merely increases the flexion of the spine.
Hip extension
·
Object lifted Figure lifting.
2.15
The mechanics
of
If the spine is stable, the power (cre-
ated when the hip extensors posteriorly tilt the pelvis) is transmitted by the erector spinae along the length of the spine to the upper limb, which then delivers the force to the object being lifted.
The hip extensor muscles are better suited than the erector spinae to initiate a lift from a flexed position. A ISO-pound athlete develops a torque of about 10,000 inch-pounds in lifting a 450-pound weight. Although the hip extensors can generate a torque of about 15,000 inch-pounds, the erector spinae can generate only 3,000, or 30% of that required to perform the lift (Farfan 1988). Note that the bulk of the muscles creating the force (gluteus maxim us) are some distance from the limb controlling the movement (compare this arrangement with the fingers: the muscles that flex and extend the fingers are located not right above the fingers, where they would be in the way, but in the forearm). When prescribing exercises within the back stability program to help re-educate a person in correct lifting habits, emphasize use of the hip extensors (spinal extensors are far less important in this case), working with a stable spine. The hip hinge action, which emphasizes the gluteals, is a good exercise to use (see page 72). Modeling the spine as a cantilever system according to standard mechanical principles, one can calculate the torques of various forces acting on the spine during lifting. Where the leverage is in equilibrium, the sum of the torques is zero, with flexion forces exactly balancing extension forces. It is possible to calculate both the force needed to lift an object and the resulting compression force on the lumbar spine (Sullivan 1997). In order to lift a weight, the muscles and connective tissues in the lumbar spine must counteract the flexion caused by the weight by providing an equal amount of extension (figure 2.15). However, since the weight is far from the fulcrum while the lower back muscles and tissues are very near to it, the muscles and tissues have much less leverage and must therefore exert much more force than just the weight of the object being lifted. Meanwhile, the vertebral joints experience a compression
Biomechanics of the Lumbar Spine
.
37
that is the sum of this force and the weight of the object. That sum is much greater than the weight alone and can be very large indeed! Yet, using postmortem measurements of actual vertebral strength, Perey (1957) estimated that lifting a weight heavier than 110 kg (242.5 lb.) would exceed the compressive strength of vertebrae. Such calculations clearly indicate that the spinal column alone cannot bear excessively large weights without undergoing severe damage. In order to reduce the compressive force acting on the spinal column when lifting large amounts of weight (as, for example, in Olympic weight lifting), an individual must substantially strengthen all the vertebral reinforcing mechanisms reviewed in chapter 3. The spinal column itself is not strong enough to bear the compression force from lifting heavy weights. The force created by the torque of lifting heavy weights can be many, many times the force of the weight itself-the muscles and connective tissues of the lumbar spine must bear the large majority of the forces involved. If these soft tissues are not sufficiently trained, severe injury can result.
KEY POINT:
The Flexion Relaxation Response
in Lifting
When a subject flexes the spine during a lift, the erector spinae are electrically silent just short of full flexion (Kippers and Parker 1984). This phenomenon, called the flexion relaxation responseor critical point, is the result of elastic recoil (rebound) of the posterior ligaments and musculature. This point does not occur in all individuals (see below) and occurs later in the range of motion when weights are carried (Bogduk and Twomey 1991). During the final stages of flexion and from 2-100extension (Sullivan 1997), movement occurs by recoil of the stretched tissues rather than by active muscle work. During bending, the erector spinae are electrically silent just short of full flexion. This phenomenon is the "flexion relaxation response."
KEY POINT:
If the erector spinae are in spasm, chronic low back pain often obliterates the flexion relaxation response. Failure of the muscles to relax prevents adequate perfusion with fresh blood and can lead to local ischemic muscle pain. Interestingly, during a squat lift with the back perfectly straight, the latissimus dorsi contracts powerfully at the beginning of the lift-perhaps to initiate extension by pulling on the thoracolumbar fascia (McGill and Norman 1986; Sullivan 1997). With extremely heavy lifts of any type, as subjects flex forward to the point of electrical silence, the
38
. Back Stability
positions of the vertebrae suggest that they do not reach the point at which the ligaments would be loaded (i.e., stretched or tensioned greater than at rest) (Cholewicki and McGill 1992). The electrical silence of the muscles and the anatomical alignment of the vertebral segments suggest that the final degrees of flexion as well as the first degrees of extension occur through elastic recoil of the spinal extensor muscles. The length/tension relationship in muscles (figure 2.16) shows that a muscle loses active tension as it is stretched-but even toward the end of the range of movement, there is little decrease in total tension since an increase in passive force (recoil, as happens with a stretched rubber band) largely makes up for the decrease in active contraction. As the spine returns from a fully flexed position, the ligaments may produce some 50 N . m of tension while the recoiling muscles produce 200 N . m. The combined extensor forces of the two passive systems represents the major component of the "posterior ligamentous system" supporting the spine (Bogduk and Twomey 1991).
Arch Model of the Spine Instead of representing the spine as a cantilever system as just described, one can use the model of an arch (Aspden 1987, 1989).The ends (abutments) of the arch are provided caudally by the sacrum and cranially by a combination ofbodyweight and muscular /ligamentous forces. The principle difference between a lever and an arch is that the lever is externally supported, whereas the arch is intrinsically stable. Any load positioned on the convex surface of the arch will create an internal thrust line that runs in a straight
......./
.Total
"
.'
,
,,
, ,,
,,
, ,,
,,
Muscle length
Figure 2.16 The length-tension From Norris 1998.
relationship
in muscles.
Active
Biomechanics ofrhe
Lumbar Spine.
39
line to the arch abutments (figure 2.17a). For the arch to remain stable, the thrust line must stay within the physical boundaries of the arch. The deeper within the arch the thrust line stays, the more stable the arch will be. In the case of the spine, the thrust line is positioned within the vertebral bodies. Because a lOO-kg weight lifted in a stooped position (lordosis lost) creates a thrust line outside the spine (figure 2.17b), the arch is unstable. By tensing the back extensor and abdominal muscles at the same time, however, one can create intra-abdominal pressure (lAP) that moves the thrust line back into the spine and increases spinal stability (figure 2.17c).
b
Figure 2.17 (a) General mechanics of an arch. A load on the convex surface of an arch creates an internal thrust line. For stability, the thrust line must stay within the depth of the arch ring. (b) Applying the arch model to the spine. Lifting a heavy weight in a stooped position creates a thrust line that moves outside the arch of the spine, making the spine unstable. (e) lAP acting on the anterior surface of the spine and adjustment of lordosis moves the thrust line back within the vertebral bodies. Reprinted, by permission, from C. Norris, 1995, "Spinal stabilisation," Physiotherapy journa/Bl(3):
4-12.
40
. Back Stability
Moreover, an individual can use the spinal muscles (which are intrinsic to the arch) to adjust the lordosis, so that the thrust line continually remains within the arch of the spine. The stiffness of the spine (resistance to bending) also is increased through the thoracolumbar fascia (TLF) and hydraulic amplifier mechanisms. Some writers believe the arch model of the spine seriously underestimates the compressive forces on the spine (Adams 1989). For further discussion of lAP and other stabilizing mechanisms, see chapter 3.
LIFTING
METHODS
There are two basic ways to lift something: in the squat lift, a person bends the knees and back; in the stoop lift, the legs remain straight and the back alone bends. Because the legs are apart and bent with the squat lift, an individual can hold the object closer to the body's line of gravity-thereby reducing the length of the lever arm from the body's line of gravity to the center of gravity of the object. The disadvantage of the squat lift is that individuals are lifting more of their bodies (the legs and trunk as opposed to the trunk alone) and therefore must expend more energy than with a stoop lift. The erector spinae are more active in positions where the lordosis is maintained (Delitto et al. 1987)-after they have attained a fully erect position when lifting a heavy weight, people tend to lean back in order to balance the weight and to use their hip flexor muscles to resist further spinal extension and to stabilize their spines. In a squat lift, a person can hold a weight closer to the body's center of gravity, thereby reducing the torque on the spine.
KEY POINT:
In addition to differentiating between the squat lift and stoop lift, we must also examine the difference between using a squat lift with the back lordotic (lumbar spine minimally extended) and with the back flat (lumbar spine minimally flexed). Lumbar curvature is calculated as the angle formed between the surface of the vertebral body of L1 and that of the sacrum (figure 2.18). The population mean value of this angle is 50°, although in children it is increased to 67° and in young males to as much as 74° (Bogduk and Twomey 1991) depending on posture type. The lordosis naturally results from the shapes of the vertebrae and disks of the lumbar spine. The L5-S1 vertebral disc is wedge shaped, its posterior height typically about 7 mm less than its anterior. The L5 vertebral body also is wedge shaped, its posterior height typically 3 mm less than its anterior. The remainder of the lordosis occurs because the discs themselves (not the vertebral bodies) are wedge shaped. The sacrum is angled at about 30° to the horizontal, and changes to this angle affect the sacroiliac joint.
Biomechanics
of the Lumbar
Spine
.
41
Because the orientation of the vertebrae differ between the squat and stoop L1 lifts, the load distribution is affected. The lengths of various trunk muscles also difL2 fer between the two lifts. Since the depth of the lumbar discs (6-12 mm) is considL3 erably smaller than the vertical height of the lumbar vertebrae (30-45 mm), even minimal changes in vertebral angles can L4 greatly deform the discs. A flexion angle of 10-12°, for example, stretches the posL5 terior annulus by more than 50% (Adams and Dolan 1997). Repeated loading in a lordotic posture can cause compressive stress within the posterior annulus of a disc and load the adjacent facet joints. Maximal flexion (up to the elastic limit) Sacrum can thin the posterior annulus and cause posterior prolapse. Minimal flexion (flatback), however, which brings the verteCoccyx~ bral bodies into vertical alignment, equalizes compressive stress across the Figure 2.18 The curvature of whole disc and unloads the facets the lumbar spine can be designated by the angle (Q) formed (Adams et al. 1994). At 60-80% of maxibetween lines through the surmum flexion, the posterior tissues exert face of L 1 and the sacrum. a substantial extensor torque--yet there Adapted, by permission, from J.K. is only a small compression effect on the Loudon, S.L. Bell, and J,M. Johnston, lumbar discs. Moreover, tension in the 1998, The clinical orthopedic assessment guide (Champaign, IL: Human thoracolumbar fascia helps to stabilize Kinetics), 54. the sacroiliac joint-and contraction of the gluteal muscles, the abdominals, and latissimus dorsi all increase the TLF tension in a flatback posture. To lift a heavy object, one optimally should use a squat lift while maintaining the neutral position of the spine. The spine is likely to flatten as the weight is taken, and this technique should prevent hyperflexion as long as the object is pulled toward the pelvis. KEY POINT: Have your client perform squat lifts when lifting an object, bringing the object in toward the pelvis. As your client begins to raise the weight, her lumbar spine flattens to minimally compress the lumbar discs and unload the facet joints. In this position, tissue recoil provides substantial extension power.
. BackStability
42
SUMMARY
· .
A spinal segment, comprising two adjacent vertebrae, is comparable to a simple leverage system, connected and held together by ligaments. Because spinal ligaments are interconnected with fasciae surrounding back muscles, which in turn eventually merge with ligaments and muscles as distant as the extremities of limbs, movements of most parts of the body can affect the stability of the spine. The deep abdominal muscles in particular are very important in keeping the spine stable (Le., keeping vertebrae in line even during heavy lifting). Spinal discs, between each pair of vertebrae, absorb stress through stretching of the elastic fibers in the outer annulus and through cushioning by the highly plastic, hydrophilic nucleus pulposus. With age, the nucleus loses water content and the fibers lose elasticity. The facet joints are synovial joints between the inferior articular process of one vertebra and the superior articular process of its neighbor. Their articular cartilage can become brittle with age. Within the vertebra itself, compressive force is transmitted by both the cancellous (spongy) bone of the vertebral body and its cortical bone shell. Cancellous tissue declines with age. The vertebrae themselves, however, can bear only a small fraction of the load placed on the spine by heavy weights without experiencing serious injury. In order to successfully bear heavy weight, the spine must be stabilized by muscles and ligaments.
. . . . .
~ Stabilization Mechanisms in the Lumbar S1!ine Devoid of its musculature, the human spine is inherently unstable. The spine of a fresh cadaver stripped of muscle can sustain a load of only 4-5 lb. before it buckles into flexion (Panjabi et al. 1989). Moreover, the center of gravity of the upper body (when standing upright) lies at stemallevel (Norkin and Levangie 1992). This combination of flexibility and weight distribution is approximately comparable to balancing a 75-pound weight at the end of a 14-inch flexible rod (Farfan 1988). From the strictly mechanical standpoint, discs don't contribute as much as one might think to the spine's strength: lifting heavy objects imposes on the lower lumbar spine a compressive force that greatly exceeds the failure load of the vertebral discs unless additional support is present (Bartelink 1957; Bradford and Spurling 1945; Morris et al. 1961). By reducing the compression forces on lumbar discs, several mechanisms help stabilize the spine (Norris 1995a). These mechanisms, on which this chapter focuses, include the posterior ligamentous system, several processes involving the thoracolumbar fascia, actions of trunk muscles, and intra-abdominal pressure.
THE POSTERIOR
LIGAMENTOUS
SYSTEM
The interspinous and supraspinous ligaments, facet joint capsules, and thoracolumbar fascia (TLF) together provide passive support for the spine sufficient to balance between 24% and 55% of imposed flexion stress (Adams et al. 1980). In the unstretched position, collagen fibers within the anterior and posterior longitudinal ligaments and the ligamentum flavum (see figure 2.3, page 16) are aligned haphazardly. When the ligaments are stretched as the spine flexes or extends, however, the collagen fibers become aligned and the ligament becomes stiffer (Hukins et al. 1990; Kirby et al. 1989). Prestressed by 10-13% at rest, the ligaments retract when cut (Hukins et al. 1990). The 43
44
. Back Stability
longitudinal ligaments therefore maintain a compressive force along the axis of the spine, causing it to act somewhat like a prestressed beam (Aspden 1992).The ligaments are viscoelastic (Le.,they stiffen when loaded rapidly). Rapid loading therefore increases the thrust within the spine and tends to approximate (bring closer together) the vertebrae, enhancing spinal stability. Power created by the hip extensors posteriorly tilts the pelvis and is transmitted through the spine to the thorax and upper limbs via the ligamentous system. Some authors have maintained that for this passive mechanism to work, the spine must remain flexed. They argued that if the spine extends, tightness of the posterior ligaments will decrease and their ability to stabilize the spine will be lost (McGill and Norman 1986). More recently, however, it has been shown that the spine need not become kyphotic before it can create tension by stretching the tissues (Gracovetsky et al. 1990). The posterior ligamentous system alone can sustain a maximum torque of only about 50 N . m (Bogduk and Twomey 1991), less than 25% of that of the contracting erector spinae. However, two passive systems are at work here (see page 38). In addition to the recoil from the posterior ligamentous sytem, the erector spinae are also recoiling. At the point of full flexion, these muscles no longer contract (they are electrically silent), but they do exert a force through recoil much like that of a giant elastic band. The force that the erector spinae create through recoil is about 200 N . m equal to their potential contractile force. The combined posterior musculoligamentous system therefore provides a substantial stabilizing mechanism in full flexion.
~
The posterior ligaments of the spine can sustain 50 N . m of torque and resist over 50% of the flexion stress imposed on the spine. The passive tension (elastic recoil) in the stretched erector spinae can create 200 N . m of torque, equal to their maximum contraction.
THE THORACOLUMBAR
FASCIA
The thoracolumbar fascia performs a number of important functions during back stability, which I briefly review here. Note that the fascia also acts to stabilize the sacroiliac joints.
Structure of the Thoracolumbar
Fascia
The thoracolumbar (lumbardorsal) fascia (TLF) has three layers that cover the muscles of the back (figure 3.1). The anterior layer derives from fascia covering the quadratus lumborum and attaches to the transverse processes
Stabilization Mechanisms in the Lumbar Spine.
45
-Terms YouSh'OUltI Kn-ow=: aponeurosis connective tissue that attaches muscle to bone approximate (verb) to move or bring objects closer together contralateral originating in or affecting the opposite side of the body fascicle a small bundle of nerve or muscle fibers hoop pressure the inward pressure exerted by the muscles surrounding the trunk ipsilateral on the same side (of the body) kyphotic convex curvature of the thoracic spine creating a hunchback lamina a thin flat layer or membrane raphe, lateral a ridge along the side of the erector spinae muscles formed by the connective tissue of the latissimus dorsi, internal obliques. and transversus abdominus
(Bogduk and Twomey 1991). The middle layer, behind the quadratus lumborum, attaches both to the transverse processes and to the intertransverse ligaments. Laterally, it extends to cover transversus abdominis. The posterior layer, which envelops the erector spinae, attaches from the spinous processes and wraps around the back muscles to blend with the rest of the TLF laterally to the iliocostalis. The point at which the layers blend is the lateral raphe. The superficial layer of the TLF is continuous with the latissimus dorsi and gluteus maximus. Sometimes a few fibers attach to parts of the external oblique and trapezius, and some cross the body midline (Vleeming et al. 1995). At L4-LS level, fibers from latissimus dorsi and gluteus maximus differ in orientation, giving the superficial layer of the TLF a crosshatched appearance. This appearance may even extend down to the LS-S2 level (Vleeming et al. 1997).The fibers of the deep layer are continuous with the sacrotuberous ligament (and through it to the biceps femoris muscle of the upper leg); and they attach to the posterior superior iliac spines, the iliac crests, and the sacroiliac ligaments (see figure 2.8, page 23). In the thoracic region, fibers of the serratus posterior inferior are continuous with the TLF (figure 3.2).
Thoracolumbar
Fascia Mechanism
In addition to its passive role, the TLF has two further capacities that involve muscle contraction. The transversus abdominis, through its attachment to the lateral raphe, pulls on the TLF. Although both attach to the lateral raphe (figure 3.3), the deep laminae of the TLF angle upward, while
Transversus
Psoas
CD Anterior @ Middle @ Posterior
Figure
3.1
abdominis
layer Erector
layer
spinae
layer Cross
section
of trunk
showing
thoracolumbar
fascia
(TLF).
Trapezius Serratus posterior inferior (beneath latissimus dorsi)
Latissimus
dorsi
Internal oblique and transversus abdominis
External oblique
Gluteus maximus
Figure
46
3.2 Muscle attachments
into the thoracolumbar
fascia (TLF).
Stabilization Mechanisms in the Lumbar Spine.
47
Superficial lamina ofTLF Lateral raphe
Figure 3.3 The thoracolumbar fascia mechanism. Through its attachment to the lateral raphe, the transversus abdominis pulls on the TLF.The angulation of both the deep and superficial layers of the TLF creates a net force that tends to approximate the vertebrae.
the superficial laminae angle downward. As the transversus abdominis contracts and pulls on the lateral raphe, the deep and superficial fibers of the TLF pull laterally for the most part, although some force is transmitted along the length of the TLF. Originally, this approximating force was calculated as 57% of the force applied to the lateral raphe (Macintosh and Bogduk 1987), an increase in force termed the "gain" of the TLF (Gracovetsky et al. 1985). However, more detailed anatomical investigation has revealed that the torque created by contraction of transversus abdominis onto the TLF is between 3.9 and 5.9 N . m-compared to that from the back extensors of 250-280 N . m (Macintosh et al. 1987). Rather than actively extending the spine through the approximating force represented by "gain," then, the primary importance of the TLF seems to be providing passive resistance to flexion.
Thoracolumbar
Fascia as Hydraulic Amplifier
The TLF exerts an even greater stabilizing effect through its role in the socalled hydraulic amplifier effect (Gracovetsky et al. 1977). The posterior layer of the TLF is retinacular tissue (i.e., very strong reinforcing connective tissue) that envelops the erector spinae. As the erector spinae contract, the TLF resists the expansion of the bellies of the shortening muscles by increasing tension in the fascia. Some believe that the predominant antiflexion effect of the TLF occurs via this hydraulic amplifier effect rather than by
48
.
Back Stability
its pull on the transversus abdominis (Macintosh et al. 1987). Restriction of the radial expansion of the erector spinae by the TLF has been shown to increase the stress generated by these muscles by as much as 30% (Hukins et al. 1990).
Thoracolumbar Fascia Coupling and the Sacroiliac Joint A combination of form closure and force closure stabilizes the sacroiliac joint (51])(Vleeming et al. 1990). Form closure arises from the anatomical alignment of the bones of the ilium and sacrum, where the sacrum forms a kind of keystone between the wings of the pelvis (Norris 1998). Force closure results from muscles pulling laterally onto fascia and ligaments that pass over the joint. The combination of form and force closure creates a very useful self-locking mechanism within the 51J. Any activity that weakens these forms of closure can create pathological symptoms in the 51J. Nutation (see table 2.2 on page 24) tensions the 51Jligaments, pulling the posterior parts of the iliac bones together and increasing 51Jcompression. Two ligaments are of special importance to self locking-the sacrotuberous ligament connecting the sacrum to the ischial tuberosity, and the long dorsal sacroiliacligament from the third and fourth sacral segments to the posterior superior iliac spines (PSIS). Both ligaments blend over the posterolateral aspect of the sacrum to form an expansion approximately 20 mm wide and 60 mm long. The ligaments attach to the posterior layer of the TLF and to the aponeurosis of the erector spinae. Nutation tensions the sacrotuberous ligament, while counternutation tensions the long dorsal sacroiliac (51)ligament. The 51 ligament is tensioned by contraction of the biceps femoris and of the gluteus maximus. Force closure of the 51] opens the possibility of treating 51Jlesions with exercise therapy either passively (automobilization) or actively through contraction of the biceps femoris, gluteus maxim us, latissimus dorsi, or erector spine. Clearly, if muscle affects the 51J, as has been shown by Vleeming's work (Vleeming et al. 1995a), training these muscles could improve 51Jfunctions. Moreover, any muscle that tensions the TLF should also affect force closure of the 51J. When the erector spinae contract, they pull the sacrum forwardinducing nutation of the 51]and tensing the interosseous and sacrotuberous ligaments. The iliac portion of the muscle tends to pull the cranial aspect of the 51Jtogether, whereas the action of nutation pulls the caudal aspect apart. The gluteus maxim us can compress the 51Jdirectly and indirectly through its attachment to the sacrotuberous ligament. This occurs particularly when the gluteus maximus contracts with the contralateral
Stabilization Mechanisms in the Lumbar Spine
.
49
latissimus dorsi and both muscles tension the TLF, whose fibers join the two muscles. Tension in the sacrotuberous ligament is increased by tensioning the long head of biceps femoris. This occurs most noticeably in a flexed trunk or stooped position, in which the sacrotuberous ligament is also tensioned by the sacral portion of the erector spinae and the gluteus maxim us. 51] pain frequently occurs during and after pregnancy, when laxness of the 51] ligaments reduces form closure of the joints. Female gymnasts experience similar problems: the inherent hyperflexibility of gymnastics generally increases the laxity of the pelvic ligaments, reducing the form closure that they produce. The increased muscular stability resulting from the muscular demands of the sport is compensated for by the laxness, as long as the women continue their activity. When their muscle strength declines after they stop practicing the sport, the 51] is left unstable and open to pathology. SI] pain of this type is often helped by using a pelvic belt; it may also be helped by improving force closure of the 51] by using stabilization techniques for the lumbar spine and enhancing gluteal muscle strength using the hip hinge action (see page 77). Specific exercise can improve stability of the sacroiliac joint by restoring the natural mechanisms of form closure and force closure.
KEY POINT:
TRUNK
MUSCLE ACTION
Facilitating co-contraction of the muscles surrounding the lumbar spineincluding the erector spinae, transversus abdominis, multifidus, and the oblique abdominals-may enhance spinal stability (Richardson et al. 1990).
Spinal Extensor Muscles The spinal extensors may be broadly categorized into superficial muscles (the erector spinae) that travel the length of the lumbar spine and attach to the sacrum and pelvis, and deep, or intersegmental (unisegmental) muscles (multifidi, interspinales, and intertransversarii) that span the spaces between the individual lumbar segments. The intersegmental muscles, being more deeply placed, are closer to the center of rotation of the spine and have a shorter lever arm than the superficial muscles. However, their closeness to the center of rotation means that the change in length of intersegmental muscles is less for any given change in the spine's angular position; and the muscles' shorter length gives them a faster reaction time, creating a smoother and more efficient stabilizing control system (Panjabi et al. 1989). The intersegmental nature
so
.
Back Stability
of these muscles also means that they are able to "fine tune" the spinal movements by acting on individual lumbar segments rather than the whole spine (Aspden 1992). Being larger in size and further from the center of rotation, the superficial muscles are better placed to create gross sagittal rotation movements, while the intersegmental muscles are of greater importance to spinal stability (Panjabi et al. 1989). Furthermore, because the smaller intersegmental muscles have about seven times the number of muscle spindles (Bastide et al. 1989) than the larger muscles have, they have a greater proprioceptive role (see following discussion). Deep (Intersegmental) Muscles Of the deeply placed intersegmental muscles, the multifidus is most important for lumbar stability. The fibers of multifidus are arranged segmentally, and each fascicle of a given vertebra has a separate innervation by the medial branch of the dorsal ramus of the vertebra below (Macintosh and L1 Bogduk 1986). The primary function of each multifidus fascicle may be to control L2 lordosis at its particular vertebral level and to independently counteract any imposed loading (Aspden 1992). The action of the L3 multifidus can be resolved into a small horizontal and very much larger vertical L4 component (figure 3.4), which (as is clear when viewed from the side) acts at 90° to L5 the spinous processes. This configuration enables multifidus to produce posterior sagittal rotation (rocking) of the lumbar vertebrae (Macintosh and Bogduk 1986). This action neutralizes spinal flexion caused as a secondary action when the Sacrum oblique abdominals produce spinal rotation. Because the line of action of the long fascicles of multifidus lies behind the lumCOCCyxL bar spine, the muscle also increases lumbar lordosis. Multifidus is active through Figure 3.4 Lateral view showthe whole range of flexion, during rotaing the line of action of multifidus, with its vertical alignment. tion in either direction, and during extenAdapted, by permission, from J.K. sion movements of the hip (Valencia and Loudon, 5.L. Bell,andJ,M.Johnston, Munro 1985). Posterior sagittal rotation J 998, The clinical orthopedic assessment guide (Champaign, IL: occurs during all flexion movements, in order to resist the anterior sagittal rotation Human Kinetics), 54.
Stabilization Mechanisms in the Lumbar Spine
.
51
that naturally accompanies flexion. The importance of multifidus in producing this action is therefore essential to stability of the lumbar spine in normal movements. Panjabi's (1992) description of instability (as a reduction in stiffness within the neutral zone of the lumbar spine) is particularly relevant to multifidus function. Multifidus is a muscle well positioned to enhance segmental stiffness in the neutral zone and contributes nearly 70% of the stiffness resulting from muscle contraction (Wilke et al. 1995). Real-time ultrasound imaging has revealed marked asymmetry of the multifidus in patients with low back pain (Hides et al. 1994). Crosssectional area (CSA) of the multifidus was markedly reduced on the ipsilateral side to symptoms, the site of reduction corresponding to the level of lumbar lesion as assessed by manual therapy palpation. The muscle also showed a rounder shape, suggesting muscle spasm. The suggested mechanism for the CSA reduction was by inhibition through perceived pain via a long loop reflex. The level of vertebral pathology may have been targeted to protect the damaged tissues from movement. The authors suggested that the rapid muscle wasting (less than 14 days in 20 of the 26 patients studied) may have resulted from spasm-induced reduction in circulation to the muscle. In addition to changes in muscle bulk, Biedermann et al. (1991) observed altered fiber types in the multifidus of low back pain (LBP) patients; patients who tended to decrease their physical and social activities as a result of LBP showed a reduced ratio of slow twitch to fast twitch muscle fibers. This could be the muscle's adaptive response to changes in functional demand placed on it, and/ or the injury may have caused a shift in recruitment patterns of motor units of the paraspinal muscles, with the fast twitch motor units being recruited before the slow twitch units. Pathologic changes in the multifidus following low back pain include a motheaten appearance of type I fibers (Hides et al. 1996) and an increase in fatty deposits (Parkkola et al. 1993). Recovery of multifidus function following low back pain does not occur automatically following the resolution of pain and resumption of normal daily activity. In a study comparing medical treatment alone (1-3 days' bed rest, analgesics, and anti-inflammatory medication) with medical treatment plus specific exercise therapy to the multifidus, Hides et al. (1996) showed that multifidus activity could be retrained. Subjects who had experienced first-episode acute low back pain showed an average of 24% reduction in CSA to the multifidus on the painful side. The difference between painful and painless sides changed from nearly 17% after 4 weeks to 14% after 10 weeks in those subjects receiving medical treatment alone. For those who received additional exercise therapy, however, the mean values were 0.7% at 4 weeks dropping
to 0.24% after 10 weeks (figure 3.5).
S2 . Back Stability
30
No exercise
therapy
25 % difference in cross-sectional area between sides
-----
20
Exercise
therapy
15
10 5 o o
Figure Reprinted
~
3.5 from
Ultrasound Hides
2 Weeks
imaging
results
3
4
of multifidus
muscle
recovery.
et al. 1996.
Low back pain leads to reduced cross-sectional area in the multifidus muscle. As the pain reduces, recovery not automatic-rehabilitation is required.
Superficial
Muscles
The lumbar
erector spinae
consists of two muscles:
is
the iliocostalis
and
the longissimus (figure 3.6). Each of these muscles has two components arising from both the thoracic and lumbar spine. Functionally, therefore, the erector spinae can be considered in four distinct groups: lumbar longissimus, lumbar iliocostalis, thoracic longissimus, and thoracic iliocostalis (Macintosh and Bogduk 1987). The force produced by the lumbar longissimus can be resolved into a large vertical vector and a smaller horizontal vector (figure 3.7). However, the fascicle attachments are closer to the axis of Iliocostalis thoracis sagittal rotation than those of multifidus, so Longissimus thoracis their effect on posteSerratus rior sagittal rotation is posterior inferior less. Because the horizontal vectors of lumIliocostalis lumborum bar longissimus are directed backward, Longissimus lumborum the muscle is able to Quadratus lumborum draw the vertebrae backward into posterior translation and Figure 3.6 Muscles of the back. restore the anterior
Stabilization Mechanisms in the Lumbar Spine.
53
translation that occurs with lumbar flexion. The upper lumbar fascicles are better equipped to facilitate posterior sagittal rol2 tation, whereas the lower levels are better suited to resist anterior translation. The lumbar iliocostalis has a similar l3 action to that of the lumbar longissimus. In addition, the muscle cooperates with l4 multifidus to neutralize flexion caused when the abdominals rotate the trunk. The thoracic longissimus can indirectly l5 increase lumbar lordosis via its effect on the aponeurosis of the erector spinae. It also indirectly laterally flexes the lumbar spine through its lateral flexion of the thoracic spine. Sacrum The thoracic iliocostalis attaches not to the lumbar vertebrae but to the iliac crest. On contraction, these fascicles increase lordosis; through their additional leverage Coccyx~ from the ribs, they indirectly laterally flex Figure 3.7 lateral view of the the lumbar spine. During contralateral lumbar spine, showing the line of the lumbar iliocostalis and rotation, the ribs separate, stretching the thoracic iliocostalis which can therefore act lumbar longissimus, and their more oblique orientation. Note as a limiting factor to this movement. On the greater horizontal force contraction, the thoracic iliocostalis will vector (H) and smaller verical de-rotate the rib cage and lumbar spine force vector (V) of the lower fifrom a position of contralateral rotation. bers of these muscles. It is probably the endurance rather than Adapted, by permission, from J.K. the strength of the erector spinae that is Loudon,S.L.Bell,andJ,M.Johnston, 199B, The clinical orthopedic as- important to LBP rehabilitation. Endursessment guide (Champaign, IL: ance has been used as a predictor for susHuman Kinetics), 54. ceptibility to LBP (Beiring-Sorensen 1984). Moreover, subjects with a history of LBP may have reduced endurance of the back extensors compared to normal subjects, but similar strength Gorgensen and Nicolaisen 1987). As fatigue increases, subjects with LBP show reduced precision and control of trunk movements. Loss of torque from the trunk muscles in these subjects is relatively less than the loss of control and precision (Pamianpour et al. 1988), indicating that a rehabilitation program should include restoration of endurance for the spinal extensors. Selective recruitment of the torque-producing superficial muscles from the stabilizing deep muscles is also important for rehabilitation of active lumbar stabilization (Ng and Richardson 1994). l1
54
.
Back Stability
The quadratus lumborum (figure 3.6) can be an important back stabilizer in certain circumstances (McGill et al. 1996). The muscle lies deeper than the erector spinae and has medial and lateral fibers. The medial fibers connect the lumbar transverse processes to the ilium and iliolumbar ligament or the 12th rib, while the lateral fibers directly connect the ilium and iliolumbar ligament and 12th rib (Bogduk and Twomey 1991). The quadratus lumborum has a small extensor torque and a larger lateral flexion torque and is able to stabilize the lumbar spine via its segmental attachments (McGill et al. 1996). EMG with fine wire electrodes has shown the muscle to be more active during lateral bending than during extension and especially active in upright standing and unilateral carrying (McGill et al. 1996). Side-support actions shift some of the loading of the muscles from the discs and facet joints of the lumbar spine to the side (McGill 1998). This role of the quadratus lumborum as a potential stabilizer of the lumbar spine expands the traditionally recognized role of the muscle as a prime mover of side flexion and as an auxiliary muscle of respiration.
The Iliopsoas The iliopsoas (figure 3.8) consists of the separate psoas and iliacus muscles. The psoas major arises from the vertebral bodies and discs of the lumbar and 12th thoracic vertebrae and from their transverse processes. The muscle passes downward and laterally, beneath the inguinalligament, to blend with the fibers of iliacus and then to Psoas attach onto the posterior aspect of the lesser trochanter of the femur. The iliacus is a large triangular muscle on the anterior Iliacus aspect of the pelvis. It arises primarily from the upper and posterior portions of the iliac fossa, but some fibers have been found on the sacrum and anterior sacroiliac ligament (Palastanga et al. 1994). The fibers from iliacus pass downward and medially to blend with those of psoas major and attach into the lesser trochanter, Figure 3.8 The iliopsoas muscle, compris- a few fibers merging with the ing the psoas and the iliacus, anterior view. joint capsule.
Stabilization Mechanisms in the Lumbar Spine.
55
The iliopsoas flexes the hip; with the hip fixed, it anteriorly tilts the pelvis and flexes the lumbar spine. Although these actions are minimal, the psoas major extends the upper lumbar spine and flexes the lower lumbar spine (Bogduk et al. 1992); far more important is its production of compression and shear forces over the lumbar spine. The individual fascicles of psoas spiral anteromedially and are all of similar lengths. The lines of action of these fascicles run very close to the axis of rotation of the lumbar spine, giving the muscle fascicles very small torque arms and reducing the muscle's ability to flex the trunk on the stationary hip. However, the compression and shear forces created by the psoas on the lumbar spine are considerable and may even equal full trunk weight. The shearing force exerted on 15-51 by maximum contraction of a single psoas muscle is nearly twice that exerted on this joint by trunk weight in normal upright standing (Bogduk et al. 1992). Because the two components of iliopsoas have a separate innervation (psoas from the anterior rami and Ll-3, and iliacus from the femoral nerve), they can be activated separately. In a study using fine wire electrodes guided by high-resolution ultrasound, Andersson et al. (1995) showed selective recruitment of iliacus during contralateral leg extension from single-leg standing. No postural activity was seen in either muscle during relaxed standing or with the whole trunk flexed to 30°. When the contralateral hand was loaded (34-kg weight), psoas was active but iliacus was electrically silent. During sitting with a straight back, psoas was active but iliacus relatively silent; while in relaxed sitting, both muscles were inactive. Both muscles showed moderate activity when subjects sat with an anteriorly tilted pelvis and an increased lordosis. During abdominal exercise, both muscles were active during straight-leg sit-ups-with even higher activity during sit-ups with the knees and hips flexed to 90° (crunch position). However, little activity was seen when subjects performed trunk curls from the crunch position. During straight-leg raising, both muscles were active when the ipsilateral leg was lifted; both were inactive when the contralateral leg lifted (table 3.1).
Abdominal Muscles The abdominal muscle group consists of four muscles, divided into two groups. The deep (anterolateral) abdominals are transversus abdominis and internal oblique; the superficial (front) abdominals are the rectus abdominis and external oblique.
Anatomy of the Superficial Abdominals The rectus abdominis (figure 3.9) is positioned vertically at the front of the abdomen. It attaches from the symphasis pubis and pubic crest and runs to the xiphoid process and 5/6/7th ribs, being broader superiorly. The lateral border (semilunaris) can be seen in lean subjects, as can the central separation between the two muscles, the linea alba. Of the three
~ ,.
56 .")f ck Stability
. f
"
.'0;
.!~
""15,,
.}''i
e 3.1
Psoas and Iliacus Activity Measured on EMG
s a Percentage
.
0 f Maximum
Starting position Single-leg standing Same. leg flexion (90") Opposite-leg extension (30") Same-leg abduction Standing Standing with trunk flexed to 300
Psoas %
Iliacus %
0 99
0 99
0
26
36 0
S6 0
0
0
Standing opposite hand loaded Sitting with straight back
11 9
0 4
Relaxed sitting Sitting, hyperlordosis and pelvic tilt
0 17
0 22
Sit-up, straight legs
52
42
Sit-up, legs 4S0 to floor
88
60
Trunk curl, legs straight
0
0
4 59
0 58
Trunk curl, legs 900 (end range) Straight-leg. raising (bilateral) Data from Andersson et al. 1995.
noticeable tendinous intersections of this muscle, one is level with the umbilicus, one is level with the xiphoid, and one is midway between the two. Each rectus muscle is enclosed within a fibrous sheath (the rectus sheath) formed from the aponeuroses of the internal and external oblique muscles and of the transversus abdominis. These aponeuroses join centrally to form the linea alba. The rectus sheath changes at a level midway between the pubic symphasis and the umbilicus. In the upper area of the muscle, above this point, the aponeurosis of internal oblique splits into two, one part passing behind the rectus and the other in front. The aponeurosis of transversus abdominis fuses with the posterior portion of the sheath, while the aponeurosis of external oblique fuses with the anterior sheath. In the lower portion of the muscle (below the midpoint between the pubis and umbilicus), the oblique abdominal and transversus abdominis aponeuroses pass in front of the rectus, and as a result the rectus is less visible in this region (Palastanga et al. 1994). The external oblique (figure 3.9) is positioned on the anterolateral aspect of the abdomen, with its fibers running downward and medially. It attaches from the outer borders of the lower eight ribs (and their costal cartilages) and then passes toward the midline. The muscle interdigitates
Stabilization Mechanisms in the Lumbar Spine'
Serratus muscle
Rectus
57
anterior
sheath
Linea alba
External oblique muscle (cut away)
Inguinal
Figure
ligament
3.9 Muscles of the abdomen
I (intermediate
dissection).
with the serratus anterior (above) and latissimus dorsi (below). The lateral fibers are almost vertical and attach to the iliac crest, while the medial fibers attach into the rectus sheath. The lower border of the muscle aponeurosis passes between the pubic tubercle and the anterior superior iliac spine to form the inguinal ligament. Anatomy of the Deep Abdominals The internal oblique (figure 3.9) is deep to the external oblique and attaches from the lateral two-thirds of the inguinal ligament and the anterior two-thirds of the iliac crest. It also takes attachment from the thoracolumbar fascia. The fibers fan outward and upward (the posterior fibers being almost vertical) to attach to the inferior borders of the lower four ribs. The anterior fibers pass medially to help form the rectus sheath (figure 3.10). The portion of the muscle that attaches to the inguinal ligament joins its neighboring fibers from transversus abdominis to form the conjoint tendon. The transversus abdominis (figure 3.10) is the deepest of the sheet-like abdominal muscles and attaches from the lateral third of the inguinalligament and the anterior two-thirds of the inner lip of the iliac crest (Palastanga et aI. 1994). In addition, it has an attachment from the thoracolumbar fascia (where it merges with internal oblique to form the lateral raphe) and
58
.
Back Stability
Anterior layer of rectus sheath
Transversus
abdominis muscle
(cut)
Transversalis
fascia
Figure
3.10
Muscles
of the abdomen
II (deep
dissection).
from the lower six ribs, where it interdigitates with the diaphragm. Its fibers pass horizontally to merge into the rectus sheath (figure 3.11), with the lower fibers attaching to the inguinal ligament and merging with the fibers of the internal oblique to form the conjoint tendon. The lower part of the transversus abdominis forms into the transversalis fascia in which lies the deep inguinal ring. Functions of the Abdominals The rectus abdominis and lateral fibers of external oblique are the prime movers of trunk flexion; the internal oblique and transversus abdominis are the major stabilizers (Miller and Medeiros 1987). The rectus and external oblique are superficial muscles that often dominate trunk actions. The transversus and internal oblique are more deeply placed, and patients often are unable to contract them voluntarily. The rectus abdominis flexes the trunk by approximating the pelvis and rib cage. EMG investigation has shown that trunk flexion emphasizes the supraumbilical portion, whereas posterior pelvic tilt shows greater activity in the infra umbilical portion (Guimaraes et a1.
Stabilization Mechanisms in the Lumbar Spine.
59
1991; Lipetz and Cutin 1970).Abdominal hollowing activates the internal oblique and transversus muscles (Richardson Transversalis fascia Rectus abdominis muscle et al. 1992), and the transversus acts at the Figure 3.11 Cross section of the rectus sheath. initiation of movement to stabilize the trunk in overhead and lower-limb actions (Hodges and Richardson 1996). In resisted actions such as sport or lifting, the abdominal muscles essentially function to stabilize the trunk and provide a firm base of support for the arms and legs to work against. If stability is poor (in relation to total power of the subject), some of the energy of the limb actions can displace the pelvis and trunk instead of providing the desired limb movement. Compare what would happen if a baseball batter wearing sneakers were standing on ice when he connected with the ball, rather than having his feet dug into firm ground-much of the energy of the swing would be lost, and his body would twist awkwardly. In the same way, if trunk stability is poor, limb power suffers and additional stress is placed on the spinal tissues if they move to full end range. Consider an overhead lifting action performed with an unstable spine (figure 3.12, a and b): if the pelvis tilts forward, lumbar lordosis increases and the abdominal muscles overstretch as the lumbar spine moves into full extension (see page 34). In this case, what trunk stability is present comes from facet joint approximation and elastic recoil of noncontractile tissues (passive stability) rather than from muscle action (active stability) (see
Skin
a
b
Figure 3.12 Trunk stability in overhead lifting: (a) active stability of the trunk through tight abdominals and level pelvis. re-
sulting in reduced stress on lumI I
~
L\
bar tissues; (b) passive stability of the trunk through lax abdominals and tilted pelvis, resulting in increased stress on lumbar tissues. From C. Norris, 199B, Diagnosis and management, 2d ed. (Oxford: Butterworth Heinemann), 175. Reprinted by permission of Butterworth Heinemann Publishers, a division of Reed Educational & Professional Publishing Ltd.
60
.
Back Stability
page 30). The fundamental key to safe and effective abdominal training in sport is to train for trunk stability before training for trunk muscle performance. In this way, the exercises are performed on a spine made stable by muscle rather than placing excessive stress on spinal joints before muscle stability has had time to build up. KEY POINT: -stability
forriiS1he -foundation o(ili"irunkexercise. Individuals should train for trunk stability before [ !,!:a,!!1ing for muscle perform~nce. _
Patterns of Coordination Among the Abdominals During Spinal Movement In terms of spinal stabilization, the contraction speed of the abdomina Is is more critical than their strength when they react to a force tending to displace the lumbar spine (Saal and SaaI1989). Moreover, the ability of a patient to dissociate deep abdominal function from that of the superficial abdominals is important, and the key to lumbar stabilization appears to be the ratio rather than the intensity of muscle activity. Abdominal hollowing (rather than a sit-up movement) works the transversus abdominis and internal oblique (not the rectus abdominis and the external oblique) (Richardson et aI. 1992). Patients with chronic low back pain (CLBP) are poorer at using the internal oblique than the rectus abdominis and external oblique, reflecting a shift in the pattern of motor activity (O'Sullivan et aI. 1997).As CLBP patients attempt an abdominal hollowing action, they tend to substitute the superficial muscles that override the deep abdominals. When expressed as a ratio of internal oblique over rectus abdominis (IO/RA), the value from the control group (non-LBP) was 8.74 while the CLBP group had a ratio of only 2.41-indicating a much larger proportional contribution to hollowing by the internal oblique in the control group (figure 3.13). Pain inhibition in
(!)
ero
.
0.9 0.8
o Internal
0.7
~ WI/)5- 0.6 Q) c:
0.5
m
0.4
g
'§!:
C/)~
Rectus abdominis oblique
0.3 0.2 0.1
o
Control
CLBP
Figure 3.13 Abdominal muscle activation in chronic low back pain (CLBP). Data from O'Sullivan et al. 1997.
Stabilization Mechanisms in the Lumbar Spine
.
61
the subjects with CLBPmay have led to altered muscle recruitment and compensatory strategies (O'Sullivan et al. 1997). EMG measurements of trunk muscles have shown that the muscles do not simply work as prime movers of the spine but show antagonistic activity during various movements. The oblique abdomina Is are more active than predicted, to help stabilize the trunk. In a study by Zetterberg et al. (1987), subjects' abdominal muscle activities during maximum trunk extension ranged from 32% to 68% of their longissimus activities. As would be expected, the ipsilateral muscles showed maximum activity in resisted lateral flexion-but the contralateral muscles were also active at about 1020% of the maximum values. The coordinated patterns among the abdominal muscles are taskspecific. But the only muscle that is active in all patterns is the transversus abdominis. During maximum voluntary isometric trunk extension, transversus abdominis is the only one of the abdominal muscles to show marked activity. It is also the muscle most consistently related to changes in intra-abdominal pressure (lAP) (Cresswell et al. 1992). The transversus abdominis not only contracts whenever the trunk moves in any direction-its activity always precedes the contraction of the other trunk muscles in the normal (non-LBP) subject (Cresswell et al. 1994). Transversus abdominis is the only abdominal muscle to be active in trunk movements in all directions. Its activity always precedes that of the other abdominal muscles in normal subjects.
KEY POINT:
When people engage in repeated movements, their bodies anticipate the predictable load and the muscles brace themselves accordingly. Using fine wire electrodes, Hodges and Richardson (1996) assessed abdominal muscle action during 10 repetitions of shoulder flexion, extension, and abduction. They found that transversus abdominis contracted before the shoulder muscles by as much as 38.9 milliseconds. The reaction time for the deltoid was on average 188 msec, with the abdominal muscles (except transversus) following the deltoid contraction by 9.84 msec. With subjects who had a history of low back pain, however, the contraction of the transversus failed to precede that of the deltoid, indicating that the subjects had lost the anticipatory nature of stability (figure 3.14). These highly significant data reveal a uniform dysfunction in the motor control of transversus abdominis in people with low back painthe problem is not simply one of muscle strength. It appears that the anticipatory nature of transversus may be lost in those with low back pain, leaving open the possibility that this mechanism may be redeveloped therapeutically.
62
.
Back Stability Controls
Subjects
with back pain
150
~
(!) en 100 ::E5LJ.J"' 50
~f,j ~ ~
~8.:.
0
-50
-100 -150
. D
o
Flexion Abduction Extension
Figure 3.14 Activity of transversus abdominis muscle during shoulder movements. Note that subjects with back pain had a longer transversus reaction time. Point 0 represents the onset of shoulder movement.
Patients With chronic low back pain exhibit a motor control deficit (alteration in muscle reaction timing and anticipatory bracing) in the transversus abdominis.
KEY POINT:
A number of authors have highlighted contraction of the abdominal muscles before the initiation of limb movement as an example of a feedforward postural reaction (Friedli et al. 1984; Aruin and Latach 1995). In these cases, as would be expected, the erector spinae and the external oblique contract before arm flexion, while the rectus abdominis contracts before arm extension. In each case, the trunk muscles act to limit the reactive body movement toward the moving limb. Contraction of the transversus before the other abdominal muscle has been described by Cresswell et al. (1994) in response to trunk movements, but anticipatory contraction during limb movements is a newer finding. The transversus abdominis seems to be contracting during posture not simply to bring the body back closer to the posture line but to increase the stiffness of the lumbar region and enhance stability (Hodges et al. 1996).
INTRA.ABDOMINAL
PRESSURE MECHANISM
Intra-abdominal pressure (lAP) is sometimes described as intratruncal pressure (Watkins 1999), although the latter term includes both intra-abdominal and intrathoracic pressure. Intrathoracic pressure is created during inspiration by expanding the lungs within the ribcage to coincide with a lift or other effort. Although intrathoracic pressure can be useful in competitive sport, I do not emphasize it within this text because the rather complex coordination between it and abdominal hollowing (described later) makes
Stabilization Mechanisms in the Lumbar Spine
.
63
it unsuitable for most rehabilitation programs. Timing inspiration with effort, moreover, can lead to use of the Valsalva maneuver where the breath is held to maintain increased intrathoracic pressure. If done during exercise, the Valsalva can raise blood pressure to dangerous levels (Linsenbardt et al. 1992), an inappropriate situation given the poor health status of many individuals with back pain. lAP involves synchronous contraction of the abdominal muscles, the diaphragm, and the muscles of the pelvic floor. The deep abdominals (transversus abdominis and internal oblique) are the more important of the abdominal muscle groups in this respect since they are visceral compressors rather than flexors. Although they have no name for it, most people experience lAP in everyday life-as, for example, when the muscles contract reflexively to defend the abdomen from a direct blow. The theoretical basis for the lAP mechanism is that pressure within the abdomen, acting against the pelvis and diaphragm, provides additional extensor torque to the spine (figure 3.15)-moreover, the "inflated balloon" acts on a torque arm that is as much as three times greater than that of the erector spinae. Intra-abdominal pressure is created by synchronous contraction of the abdominal muscles, the diaphragm, and th~_muscles of the pelvic floor.
KEY POINT:
j
Contraction of the transversus abdominis and the internal oblique increases lAP, providing the glottis is closed. Imagine the trunk as a cylinder. The top of the cylinder is formed by the diaphragm, the bottom the pelvic floor, and the walls the deep abdominals (transversus and internal oblique). As the abdominal wall is pulled in and up, the walls of the cylinder are effectively pulled in. If a deep breath is taken, the diaphragm is lowered, compressing the cylinder from the top. Providing the pelvic floor (the bottom of the cylinder) is intact, the cylinder is "pressurized" and made more solid. In this way, it is able to resist any bending stress applied to it. The lAP is greater if the breath is held following a deep inspiration (Valsalva maneuver) as the diaphragm is lower and the comparative size of the abdominal cavity (the cylinder) is reduced. During Figure 3.15 Intra-abdominal pressure mechanism. Pressure within the abdomen acting against the pelvis and diaphragm provides additional extensor torque to the spine.
64
.
Back Stability
lifting, the pelvic floor muscles (the floor of the cylinder) contract to maintain pelvic integrity and prevent urination. The Valsalva maneuver is therefore appropriate in heavy lifting as long as it occurs only briefly. It must be borne in mind, however, that the blood pressure changes may not be desirable in subjects with poor cardiopulmonary health. Heavy lifting for this group is, therefore, not recommended. Making the trunk into a more solid cylinder reduces axial compression and shear loads and transmits loads over a wider area (Twomey and Taylor 1987). lAP may also help to protect the spine from excessive indirect loads (those not acting directly on the spine but through limb loading), with the muscles acting to involuntarily fix the rib cage. lAP is greater when heavy lifts are performed and when the lift is rapid (Davis and Troup 1964). Abdominal muscle strength affects lAP-strong athletes can produce very large lAP values (Harman et al. 1988). Yet strengthening the abdominal muscles with movements such as sit-ups does not permanently increase lAP (Hemborg et al. 1983)since these exercises usually do not mimic the coordination among abdominal muscles that is inherent in the lAP mechanism (Oliver and Middleditch 1991). Investigating the effect of abdominal muscle training on lAp, Hemborg et al. (1985)used isometric trunk curl and twist exercises. Increased recruitment of motor units in the oblique abdominal muscles clearly demonstrated muscle strengtheningyet EMG activity of these muscles decreased during lifting, implying that the subjects did not make functional use of their increased ability to recruit more motor units. The differentiation between increased strength and functional ability is an important one. If an exercise is not specific to a task being carried out, the physiological adaptation of the musculoskeletal system may be inappropriate. See page 99 for more discussion of training specificity. KEY POINT: -sit-'up exercises 'Willnot permanentlyraise intra-
.
abdominal pressure. A number of important criticisms has been made against the lAP mechanism when it has been presented as the only stabilizing process for the spine (Bogduk and Twomey 1987). First, to fully stabilize the spine during the lifting of heavy weights, the lAP would have to exceed the systolic pressure within the aorta, effectively cutting off the blood flow to the viscera and lower limbs. Competitive weight lifters have been known to black out when lifting extremely heavy weight, perhaps because of very high lAP (McGill et al. 1990).At the onset of a lift, there is an initial rapid rise in lAP-known as the snatch pressure-that may last for less than 0.5 second. The pressure declines during the remainder of the lift. Hemborg et al. (1985) calculated that a peak lAP of 250 mm Hg would be required to
Stabilization Mechanisms in the Lumbar Spine.
65
lift a 100-kg weight. Second, the muscle force required to create a sufficiently high lAP is greater than the hoop pressure possible from the abdominal muscles (Gracovetsky et al. 1985). Third, if the rectus abdominis contracts to increase lAP, it produces a flexion torque that counteracts the antiflexion effect of lAP created as the diaphragm and pelvic floor spread apart. These criticisms of lAP have led to reexamination of its contribution to back stability. Originally, lAP was believed to reduce the compression acting on the lumbar spine by as much as 40% (Eie 1966), but more recent studies have shown this to be only 7% (McGill et al. 1990). Inira-abdominal pressure has been estimated to reduce the compression acting on the lumbar spine by only 7%.
KEY POINT:
Bogduk and Twomey (1991) have considered a further effect of lAP in controlling axial rotation while lifting. Most mathematical models describe lifting in the sagittal plane only. From the functional standpoint, however, lifting is a multi plane activity, requiring stability to rotation as well as flexion-extension. If the internal and external obliques contract to control rotation, lAP may increase as a secondary effect.
SUMMARY
· · ·
The human spine is inherently unstable without its musculature. The interspinous and supraspinous ligaments, facet joint capsules, and thoracolumbar fascia (TLF) together provide passive support for the spine sufficient to balance between 24% and 55% of imposed flexion stress.
·
The posterior ligamentous through elastic recoil.
the spine passively
and
The TLF stabilizes the spine through three primary mechanisms: (1) passive resistance through its connections with the transversus abdominis muscle; (2) hydraulic amplification, as it restricts expansion of the erector spinae; and (3) "form closure" and "force closure" of the sacroiliac joint.
· · .
system stabilizes
Of the deep intersegmental muscles, the for stabilizing the spine by helping neutralizing spinal flexion. Following therapy is required to restore multifidus
multifidus is most important to control lordosis and for lower-back injury, exercise function.
Of the superficial back muscles, the erector spinae are most significant for back stabilization. It is their endurance rather than their strength that is particularly important. Of the abdominal muscles, the internal oblique and transversus abdominis are the major back stabilizers rather than the more
. Back Stability
66
·
·
superficial external oblique and rectus abdominis. The ratio in which these muscles are used is more important that mere muscle strength. The key to effective abdominal training in sport is to train for trunk stability before training for trunk muscle performance. Individuals with low back pain tend to favor the more external abdominal muscles. Abdominal hollowing (rather than sit-ups), however, activates the internal oblique and transversus muscles-and since an important aim of rehabilitation is to help patients learn to dissociate use of the deeper muscles from use of the more superficial muscles, learning to practice abdominal hollowing is a vital part of rehabilitation.
PART
ITIT
Exercises for Establishing Stabititt Chapter 4 ("Teaching Your Clients the Basic Skills") is probably the most important chapter in this book. If you do no more than help your back pain clients to master all the movements in that chapter, you may well help them more than they would have been by a lifetime of standard weight training, exercises, massages, manipulations, etc. But teaching your clients pelvic tilt, abdominal hollowing, how to assume the neutral lumbar position, and how to contract the multifidus (the essence of chapter 4) is just the beginning. The skills described in chapter 4 get your clients to the point where you can proceed with the rest of their treatment plans. You will want to identify and correct muscle imbalance as it is the source of much back pain and instability. Chapter 5 ("Muscle Imbalance") tells you how to diagnose imbalance and how to correct it. Chapter 6 ("Basic Abdominal Muscle Training") shows you how to teach your clients to train the abdominal muscles that most strongly affect low back pain-and these are not just the muscles that some therapists target when they assign "ab workouts" in order to deal with back problems. Your clients can do abdominal crunches until they have the most beautiful "six pack" on Malibu Beach and still be wracked with back pain. I show you how to target all the important structures (and they are not all muscles-you need to help your clients train their neurological responses as well!). In chapter 7 ("Posture"), I show you how to determine if your clients have less-than-ideal posture and how to correct the different kinds of abnormal posture that can be a major factor in low back pain.
67
4 Teaching Your Clients the Basic SkiDs Before your clients can follow rigorously the programs and practices discussed later in this book, they must have certain fundamental abilities. This chapter will help you understand how to teach your clients these skills. Muscle action can stabilize the trunk effectively only if the trunk is a solid cylinder. In chapter 3, we saw that the deep (lateral) abdominal muscles (transversus abdominis and internal oblique) were the most important of the abdominal group for achieving this aim, whereas the multifidus is the most important of the back muscles. Our initial aim is to reeducate these muscles to gain voluntary control over their actions.
-
KEY POINT: The back stability program begins with muscle reeducation. Before proceeding to the exercises described in later chapters, your clients should be able to control pelvic tilt; to identify and assume the neutral position of the lumbar
spine; to perform abdominal hollowing; and to voluntarily I contract the multifidus muscle.
1 I
I
Once your clients have achieved voluntary control, they are more able to use the muscles with minimal effort-the aim in all these exercises is for contraction intensities of only 30-40% of maximum, which can be easily sustained. Your clients must then learn to build the endurance of the muscles, aiming to perform 10 repetitions and hold each for 10 seconds. They also must learn to recognize the neutral position of the lumbar spine, to detect when the lumbar spine has moved away from this neutral position, and to correct the position of the lumbar spine using a pelvic tilting action.
69
.
70
Back Stability
TEACHING YOUR CLIENTS TO CONTROL PELVIC TILT If you determine that your clients' lumbar-pelvic alignment is incorrect, you will need to teach them how to tilt and hold their pelvises in order to correct the misalignment. As you begin treatment, remember that for some, touching may be a sensitive issue. Be alert for words or body language that indicate tension in your client. Before you touch the client, explain clearly what you are going to do and be sure that she is comfortable with the proposed action. If not, try a different approach. With extra-sensitive clients, by proceeding gradually, you can usually establish the trust necessary to pursue the most helpful therapeutic course. Always bear in mind that therapist-client trust is an essential ingredient for successful treatment; do everything you can to establish and maintain that trust.
Segmental Control The ability to dissociate the movement of one body segment from that of a neighboring segment is dependent on stabilization ability and adequate muscle length. The central requirement of segmental control as it applies to back stability is that the pelvis be able to tilt independently of the lumbar spine in both frontal and sagittal planes. The combination of movements of the hip on the pelvis and of the lumbar spine on the pelvis increases the range of motion of this body area. The relationship between lumbar and pelvic movement is called lumbar-pelvic rhythm (see page 34). During forward flexion in standing, when the legs are straight, movement of the pelvis on the hip is limited to about 90° hip flexion. Any further movement, allowing the subject to touch the ground, must occur at the lumbar spine. For lumbar-pelvic rhythm to function correctly, movement of the pelvis on the hip should be equal to or greater than movement of the lumbar spine on the pelvis. In people with a history of back pain, however, the ability to perform pelvic tilting (pelvis moving on hip) is often lost-almost all the movement during forward bending comes from the lumbar spine, which shows excessive flexion laxity but limited, or often blocked, extension. In the lower trunk, the ability to dissociate lumbar movement from pelvic movement is therefore important, and correction of faulty lumbar-pelvic rhythm is vital. KEY POINT: ThecibTlitYto-dissociatemovementof'tnefumDar
't
spine from movement of the pelvis is essential for the healthy functioning of the back.
1
-----
Your Clients the Basic Skills.
Teaching
71
Assessing Lumbar.Pelvic Dissociation You can use a variety of exercises to assess lumbar-pelvic rhythm; you may subsequently use the same exercises as part of the rehabilitation process. There is no stated "goal" for each of the following exercises because they all have basically the same goal: to allow you to assess your clients' abilities to dissociate lumbar from pelvic movement.
Knee Raising in Standing The subject stands at a right angle to a wall bar for support, flexing his hip beyond 90° by raising his thigh to his chest and allowing his knee to bend. The movement should ideally occur in three phases. Initially there should be no pelvic or lumbar movement, with phase I consisting of hip flexion alone (a). During phase II, the pelvis should begin to posteriorly tilt as the hip approaches 90°. The lordosis should flatten, but the lumbar spine movement should not be excessive (b). In phase III, no further hip or pelvic movement is available, and the final position is obtained by lumbar flexion alone (c). When control of lumbar-pelvic rhythm is poor, lumbar flexion and pelvic rotation often occur early in phase I, with thoracic movement noticeable as the subject dips his chest downward toward the knee (d).
~
,. ,,
a
c
,
When lumbar flexion occurs early in the movement, the action of knee raising in standing can be used as a stability exercise in itself. Instruct your client to raise his knee initially by performing 10-20° hip flexion while maintaining stability of the lumbar-pelvic region and avoiding any pelvic tilt. To progress the overload of the exercise, increase the range of hip motion to 30-45° and slow the action so that the knee raise takes a total of 10seconds.
..-.
72
.
Back Stability
Passive
Assessment
of Pelvic
Tilt
While your client is standing, grip her below the waist with your forearm placed around the pelvic rim. Place your other hand flat on the sacrum, and use your shoulder to stabilize her thoracic spine. Move your client's pelvis into anterior and then into posterior tilt, assessing how far you can move it in either direction. If your client demonstrates a flatback posture, the amount of anterior tilt will be reduced; if she demonstrates a lordotic posture, the corresponding amount of posterior tilt will be limited.
Assessing
Lumbar-Pelvic
Rhythm
in Prone
Kneeling
The subject sits back toward his ankles. Again, the action should occur in three phases. In phase I, no lumbar or pelvic movement should occur (a); in phase II, posterior pelvic tilt and hip flexion occur (b); and in phase III, lumbar flexion and some thoracic flexion finish the action (c). Faulty lumbar-pelvic rhythm often shows up immediately when lumbar flexion and posterior pelvic tilt occur immediately (d). ._
o ~
~, .~ ~
o
t
...
'-:'" 0
a
The Hip Hinge Movement
.._ ,~ -- I. .
'..
~:
.-"..-,
t
Io I
C
~ .
d:
.._...... I0
I
I
in Standing
This activity permits you to observe your client's ability to isolate pelvic motion from that of the lumbar spine in the more functional position of standing. Your first aim is to assess the client's forward flexion since the relative contribution of anterior pelvic tilt to this movement is important. With normal lumbar-pelvic rhythm, unlocked knees and anterior pelvic tilt reduce the amount of lumbar flexion required to reach downward to below waist height, as when continued
Teaching Your Clients the Basic Skills.
73
The Hip Hinge Movement in Standing, continued standing and working at a low bench (a). Where pelvic tilt is limited, greater lumbar flexion is required. Throughout the day, the number of lumbar flexion movements is greatly increased, leading to accumulated stress on the body tissues in this area (b).
Assessing
Pelvic Motion Control
in the Frontal Plane: The Trendelenburg
Sign
When one leg supports all the body weight, the hip abLax ductors (mainly gluteus meabductor dius) of the supporting leg muscles....... work to prevent the pelvis Tight from dipping (a). When these adductor muscles muscles are unable to hold an inner-range contraction, a b the pelvis dips downward toward the lifted leg, effectively adducting the weightbearing limb (b). Persistent use of this action in the swayback posture can lead to an imbalance, combining lengthening of the hip abductors and shortening of the hip adductors.
Recognizing
False Hip Abduction
In a nonweightbearing situation, inactivity of the gluteus medius shows as a false hip abduction movement. Normally when the upper leg is lifted from side lying, the pelvis remains level and the hip moves on this stable base (a). When the hip abductors are weak, the subject is unable to abduct the leg correctly (b).
continued
74
.
Back Stability
Recognizing False Hip Abduction, continued
Instead, his pelvis tilts laterally on the spine using the trunk side flexors, which give the false appearance of hip abduction. Although the leg lifts, the relationship between the femur and pelvis remains unchanged, with close inspection showing the movement isolated to the lower spine.
Regaining Correct Lumbar.Pelvic Rhythm The restoration of correct lumbar-pelvic rhythm is essential for the correct functioning of this region. Rehabilitation of this mechanism begins with your client recognizing the action of pelvic tilt and being able to maintain the neutral lumbar spine. Control of lumbar-pelvic rhythm is used extensively during static loading of the stabilizing system covered in chapter 8 and during the rehabilitation of lifting in chapter 9. The following exercises will help your client gain the essential control of pelvic tilt that is necessary for basic back stability. The last two exercises use a gym ball and will prepare your client for the more advanced gym ball exercises described in chapter 9. The pelvic tilt mechanism-is an important key-to movements of the lumbar-pelvic region.
KEY POINT:
Assisted
Pelvic Tilting While Standing
.1'{t1~,.. For subjects
who are unable to initiate a pelvic tilt.
Promote passive movement while your clients are standing by gripping around their pelvic rim and supporting their sacrum with the flat of your opposite hand (as in "Passive Assessment of Pelvic Tilt," page 72). Push the pelvis into anterior tilt and then into posterior tilt, and have your clients attempt to return to the neutral position each time (i.e., to reproduce the passive motion) in order to enhance proprioceptive input to this area.
Teaching
Assisted .f['7~'.
Your Clients the Basic Skills.
75
Pelvic Tilt While Sitting
For subjects who are currently unable to perform a pelvic tilt while sitting. The action is especially useful for individuals whose flatback posture causes pain after prolonged sitting.
Stand in front of your client and place a webbing belt around her waist. Gripping the belt, place your hand over her sternum to prevent upper body sway. As you pull the belt, her lumbar lordosis increases and her pelvis tends to tilt anteriorly. This action is made easier if your client sits on a wedge-in this case, the ischial tuberosities are higher than the pubic bone, and the pelvis is forced into anterior tilt. Initially, most of the power comes from your pulling on the belt, but gradually the belt provides less and less assistance as the subject becomes able to perform the tilting action by herself.
Assisted .f['H.
Pelvic Tilt From Crook Lying Position
For subjects who are unable to perform a full active tilt by themselves in any position.
The subject begins in the crook lying position, as for the heel slide maneuver on page 106. Grip his pelvis over the pelvic rim on each side, and push the pelvis into anterior and then posterior tilt. Encourage your subject to visualize the effect of the tilt on the lumbar spine as the lordosis is increased and reduced. Have him attempt first to follow the action using his own musculature (abdominals and gluteals), then gradually reduce your force in tilting the pelvis until he is performing the action independently. Once your client can perform the action regularly in crook lying, he should attempt the same movements in the standing position. Begin with passive control (you provide the force for movement), then have your client gradually assume active control. Eventually have him perform pelvic tilting in a variety of starting positions including 4-point kneeling, 2-point kneeling, sitting, and supine lying. In each case the action of pelvic tilt is important, and the ability to reproduce the neutral lumbar position is essential.
continued
76
.
Back Stability
Assisted Pelvic Tilt From Crook Lying Position, continued
Hip Hinge Action in High (2-Point) Kneeling (Assisted) .1'Ie1~'. Uses a pelvic tilt action to move the spine forward and backward. Once your subject can perform pelvic tilting well, she should combine it with classic "hip hinge" actions-where the trunk moves on the hip in a hinge action, and the spine remains straight. With your client in the 2-point kneeling position, assist her in performing the pelvic tilt. Encourage her to follow this movement with her shoulders, keeping her spine stable and avoiding any increase or decrease in lumbar lordosis. She should gently draw her abdominal muscles in (hollowing, see page 85) and maintain this minimal contraction (a feeling of "tightness" only) throughout the movement. The essence of this action is to angle the spine forward and backward from the hip without flexing or extending the spine. The movement is made easier if the subject visualizes a rod tipping forward and backward from a single point (the hip) rather than a rope bending. You should provide gentle pressure on the back of your client's shoulders to initiate forward angulation of the spine and pressure over the front of the shoulder to initiate backward angulation. In each case, the spine remains straight, and the action comes from the spine (acting as a single unit) moving on the hip through pelvic tilting.
Teaching Your Clients the Basic Skills
.
77
Hip Hinge (Table Support) .f{"~,,, A progression on assisted hip hinge. The subject stands facing a couch or other object placed just below waist level, with his hands on the couch surface (a). With his knees unlocked to relax the hamstring muscles, he performs the hip hinge action described in the previous exercise, using pelvic tilt and a fully stable spine. As he leans forward, he supports some of his weight with his hands, thus reducing spinal loading. After your client has mastered this supported action, he should move to the free standing position (b).
Controlled .f{"~,,,
Forward Bending
Teaches segmental control of the lumbar-pelvic region as a precursor to lifting.
Once an individual has mastered the hip hinge actions, permit him a small degree of lumbar flexion-have him perform normal forward bend actions, with the pelvis initiating the action and both the pelvis and lumbar spine contributing equally throughout the first half of the range of motion.
Sitting Pelvic Tilt Using Gym Ball .f{"~'"
Teaches anterior-posterior
pelvic tilt control.
See chapter 9 for more thorough discussion of gym ball exercises and for more advanced exercises. The ball used is a standard 65-cm ball. Instruct your client to sit on the ball with her knees apart, feet flat on the floor. Both hips and knees should be flexed to about 90°. She should then tilt her pelvis alternately in both anterior and posterior directions, making sure that her shoulders and thoracic spine remain inactive. At first, she should attempt only small
continued
78
.
Back Stability
Sitting Pelvic Tilt Using Gym Ball. continued
ranges of movement; as she gradually works up to larger ranges, the ball should roll forward and backward slightly.
Sitting Lateral Tilt Using Gym Ball .1'111.'1. Teaches lateral pelvic tilt control.
Instruct your client to sit on the ball, as in the previous exercise, and to use lateral tilting to roll the ball from side to side, transferring the body weight from one ischial tuberosity to the other. Again, the shoulders should remain still throughout the action. The aim is to control the movement throughout the range using a smooth action and to avoid "falling into" the end-range position.
TEACHING YOUR CLIENTS TO IDENTIFY AND ASSUME THE NEUTRAL POSITION Teaching clients to identify and maintain the neutral position of their lumbar spines is important for each stage of the back stability program since the neutral position places minimal stress on body tissues. Lumbar neutral position is midway between full flexion and full extension as brought about by posterior and anterior tilting of the pelvis. The discs and facet joints are minimally loaded in this position, and the soft tissues surrounding the lumbar spine are in elastic equilibrium. Because postural alignment is optimal in this position, it is generally the most effective position from which trunk muscles can work. In the normal (nonpathological) person, the neutral position corresponds to lumbar alignment in an optimal posture. Individuals with suboptimal posture may increase or reduce their pelvic tilt, causing corresponding changes in the depth of lumbar lordosis. In either case, the neutral position remains midway between end-range flexion and end-range extension-in cases of postural malalignment, however, part of the treatment aim is to restore optimal posture by rebalancing the length of the surrounding soft tissueelements.Subjects can find neutral position passively (as you move the pelvis) or actively (subject moves her own pelvis through muscle action). Refer to "Optimal Posture Alignment" in chapter 7 (page 134) for more thorough treatment of the neutral position while standing. In kneeling,
Teaching
Your Clients the Basic Skills
.
79
your subject attempts similar lumbar alignment by slightly hollowing the lumbar spine. A flatback or excessive lordosis both mean that the subject has moved away from the neutral position and will need to reposition by tilting the pelvis. With time, your clients will be able to recognize the neutral position and maintain it as appropriate. In the early stages of the program, however, you will need to constantly remind them of their spinal alignment. Proprioceptive exercises will help your client learn to assume neutral position at will.
Proprioception-Basic
Concepts
Because proprioception is vital to the process of back stability during later stages of rehabilitation (Norris 1998), your clients should begin appropriate proprioceptive exercises at the start of their treatment programs. Lephart and Fu (1995) define proprioception as a specialized variation of touch encompassing the sensations of both joint movement and joint position. During acute injury, the reflexes initiated by displacement of mechanoreceptors and muscle spindles occurs far more rapidly than that brought about by pain (nociception) (Barrack and Skinner 1990). Effusion (escape of fluid) from joints contributes to a reduction in mechanoreceptor discharge, resulting in inhibition of muscular contraction. This inhibition commonly occurs in the vastus medialis (VMO) of the knee, for example, where just 60 ml of intra-articular effusion may result in 30-50% inhibition of quadriceps contraction (Kennedy et a1. 1982). Proprioceptive deficits parallel joint degeneration (Barrett et a1.1991),but it is unclear whether this is a cause or a result of degeneration (Lephart and Fu 1995). Proprioceptive exercise is useful from the early stages of rehabilitation to restore normal functioning of the proprioceptive control of the back. And it is nowhere more useful than in helping your clients master assuming neutral position. From a clinical standpoint, proprioception consists of three interrelating components (Beard et a1. 1994) that represent activity at spinal, brain stem, and higher centers (Tyldesley and Grieve 1989)(table 4.1). Individuals
Table 4.1
Components
of Proprioception
Level of neural system
Component
of proprioception
controlled
Spinal Brain stem Higher
Regulates muscle stiffness Controls static joint positioning Controls kinesthesia (movement sense)
80
.
Back Stability
beginning back stability training should focus on brain stem activities, characterized especially by static joint positioning, for they must cultivate this ability before proceeding to more advanced training.
Static Joint Positioning Static joint position sense helps to maintain posture and balance at the brain stem level. Input for these actions is from joint proprioception, from the vestibular centers in the ears, and from the eyes. Balance and postural exercise with the eyes open or closed can enhance static joint position sense. Reproduction of passive positioning (RPP) and reproduction of active positioning (RAP) are exercises in which an individual tries to place a joint back in its starting position after either active or passive movement.
Reproduction .1'I'l'1.
of Passive
Positioning
To teach individuals how to maintain neutral position improving the accuracy of body segment position.
by
Four-point kneeling is the best starting position for restoring RPP during back stability training. Have your client kneel, with the lumbar spine in neutral position. After you passively move the spine away from neutral, instruct your client to place the spine back into the neutral position. Initially, you should work with single movements from flexion back to neutral and then extension back to neutral; then progress to combinations of movements-flexion-extension and lateral flexion and then back to neutral, for example. The aim is to increase the precision of movements so that the individual is able to accurately reproduce the neutral position alignment after each movement away from this starting position. After your client has mastered RPP in the 4-point kneeling position, move to other positions-especially those common to daily activities, such as sitting and standing.
Reproduction .I'IIT~'.
of Active
Positioning
To teach individuals how to maintain neutral position improving the accuracy of movement.
by
After your client has become proficient in passive positioning, he should initiate his own movements. Instruct him to begin in neutral position, move away from this position using single movements, and then move back into the neutral starting position. It sometimes works best if he continued
Teaching Your Clients the Basic Skills
.
81
Reproduction of Active Positioning, continued
begins RAP with a sitting or standing position-that way he can practice in front of a mirror, with his hands flat over his lower abdomen and sacrum to monitor pelvic tilt. Eventually, he uses no mirror and performs the movement without monitoring the action with his hands. Again, use a variety of movements from several starting positions.
performing-exercises to'improVer~'pfoauc~':, ion of passive or active positioning (RPP/RAP),your client hould focu.s=, onpreci~io.n",,,-.,,,,,;,:;,,,,;'~'''Aof movelT)~nt. . ". ;_~; ,,;ill, ~I~c-;-"ii;;",~i_ ~'!I;>"'_'i,,::': '1<--'. -;'<;['" i''':,;u,"
KEY POINT:
"'.Wnen
'
TEACHING YOUR CLIENTS TO USE ABDOMINAL HOLLOWING Individuals with low back pain must re-educate their muscles by learning to isolate the deep (lateral) abdominals from the superficial abdominals. This requires a hollowing action of the abdomen, using the internal oblique and transversus abdominis muscles (Lacote et al. 1987) rather than the traditional lumbar flexion movements (e.g., sit-ups) that emphasize the upper rectus (O'Sullivan et al. 1998). Before they can proceed with the exercises described later in this book, your clients must be able to perform abdominal hollowing well and cons-istently. Because the concept of abdominal hollowing is probably less familiar than other major points in this chapter, I shall devote a disproportionately large portion of the chapter to this discussion.
Abdominal Hollowing--General
Considerations
The basic process of abdominal hollowing is in theory simple and the same in all positions: the subject pulls the belly in and up at the navel without moving the rib cage, the pelvis, or the spine. Everything else in this section merely elaborates on that basic action and on how you can best help your clients to learn it well. In comparison with mobilizer muscles (see page 92), stability muscles are better suited to endurance (postural holding) and better recruited at low resistance levels. Contraction intensities of 30-40% of the maximum voluntary contraction (MVC) work best for the deep (lateral) abdominal muscles. Your clients initially will have little control over the intensity of their contractioris. Often they will begin with minimal contractions, then build to high intensities (60-70% MVC). This is acceptable during the early stages of learning and enables your clients to "feel the muscles working."
82
.
BackStability
They eventually must gain accurate control, however, and you should instruct your clients to master changing the intensity of contraction in all hollowing exercises. An effective way to achieve this mastery is to ask for a maximal contraction, then tell your clients to relax by half, and then half again. Once they have achieved minimal contraction, they should then build up the intensity again, in steps, to the maximum. Only when they can control hollowing with minimal muscle intensity over a period of time (10 repetitions each of 30-40% MVC, held for 10 seconds) should they progress to more advanced exercises. The position in which the movements are performed is important. Have your clients assume the neutral position of the spine whenever possibleinitially, you will need to position your client correctly (you may want to read ahead to the section on "Optimal Postural Alignment" in chapter 7 [page 134] for the optimal position while standing). If your clients are kneeling, have them try to achieve proper alignment by slightly hollowing the lumbar spine-a flatback or excessive lordosis both mean that the subject has moved away from the neutral position and should appropriately reposition by tilting the pelvis. Eventually, your clients will be able to maintain the neutral position throughout their exercises. ~-Have yo'Ur"'dierits maintain-the "ii'e'i:itralpo'Sit1'On([' ;he spine throughout all the exercises in this ch.apter. :
Abdominal Hollowing-Starting
Positions
Different individuals require different starting positions, depending on their weight, degree of injury, flexibility, and so on. Standing (wall support) and 4-point kneeling are probably the easiest positions for most people. Four-point kneeling places the fibers of the transversus abdominis muscle vertically. It thereby initiates some stretching in the transversus, making contraction of this muscle easier. The 4-point kneeling position is usually more comfortable than the other positions for people with back pain. On the other hand, 4-point kneeling requires control of structures in the spine, shoulders, and hips, whereas lying positions require control over only spinal structures. Since controlling a single body segment is considerably easier than controlling three, many people (especially those with poor body control, and especially when unsupervised) find exercises in the lying position easier to perform. Moreover, because 4-point kneeling places compression on the patellae and the wrists, individuals with pathology in these joints (such as arthritis) may need to modify the kneeling position. Modifications include (a) placing the open fist on the ground rather than the flat of the hand to reduce the wrist extension stress, (b) placing extra padding beneath the shins and leaving the patellae free,
Teaching Your Clients the Basic Skills
.
83
(c) taking the body weight on the forearms rather than the wrists, and (d) supporting the upper body with the chest on a chair in order to reduce the upper body weight transmitted to the arms and wrists. Obese subjects often have trouble performing abdominal hollowing in a kneeling position-the sheer weight of their abdominal tissue presents too large an overload for their deep abdomina Is to work against. For obese individuals, the standing (wall support) position is better: although it is usually a progression from kneeling (standing provides no stretch facilitation of the deep abdominals), obese individuals can control the action more easily. They can use their hands to palpate the abdominal wall, and the action of "pulling the tummy in" is often rather familiar in the standing position. Prone lying is not suitable for obese individuals with poor abdominal muscle tone because of the compression of excess body tissue in this position. Lean people often like the prone position, however, since it provides many sensory cues-the act of hollowing to draw the abdominal wall away from the supporting surface gives useful tactile feedback (especially if a pressure biofeedback unit is used, as described later in this chapter). You must use your own judgment to select appropriate starting positions for clients, taking into account body size, body condition, age, and pathology. Be flexible-experiment with different starting positions until your client feels comfortable with the exercise.
Abdominal .I'("~'.
Hollowing: 4-Point Kneeling
To isolate the transversus abdominis and internal oblique.
Because the transversus fibers are aligned horizontally, 4-point kneeling allows the abdominal muscles to sag, facilitating stretch. Position your client with her lumbar spine in a neutral position, her head looking at the floor, not forward, and her ears horizontally aligned to her shoulder joint. Her hip should be directly above the knee, her shoulder directly above the hand. The hands and knees are shoulder-width apart. Instruct your client to focus her attention on her navel area, and to pull that region "in and up" while breathing normally. This action dissociates activity in the internal obliques and transversus from that of the rectus abdominis (Richardson et al. 1992). The exercise is thus useful for re-educating the stabilizing function of the abdominals when the rectus abdominis has become the dominant muscle of the group.
84
.
Back Stability
Abdominal
Hollowing: Standing
.f'['1~,..A progression from 4-point kneeling, or an initial position for obese individuals or others for whom 4-point kneeling is uncomfortable. Some subjects find 4-point kneeling difficult to control and tend to round their spines as they attempt abdominal hollowing. In this case, wall-supported standing is a more appropriate starting position. Your client should stand with his feet six inches from a wall and his back against the wall, while maintaining a neutral spinal position (a). An easy way to monitor neutral position is for your client to place one hand behind his back (over the sacrum) and the other in front of the abdomen, enabling him to monitor the position of his pelvis. He can also use his front hand to feel the contraction of the abdominal muscles as he initiates hollowing and a draws the abdominal wall away from his hand. In an obese or poorly toned subject, the weight of the digestive organs will pull the abdominal wall out and down (visceral ptosis). If this occurs, position a belt below his navel (b), instructing him to contract the lateral abdominals and to pull the abdominal wall "in and up," trying to create a space between the abdomen and the belt. Since motor programming links lateral abdominal action and pelvic floor action as part of the intraabdominal pressure mechanism, pelvic floor contracb tions are also useful to aid learning of abdominal hollowing. Instruct your client to pull in the pelvic floor as though trying to stop himself from urinating. In men, the action of "lifting the penis" is also useful imagery.
Linkingabdominai hollowing w'ithpelvic floor ; contractions is a useful way to enhance learning in both males L:.n~~ales._ __
KEY POINT:
It is important that your clients be able to differentiate the abdominal hollowing action from pelvic tilting. Be careful to ensure that your clients do not flatten their backs completely against the wall as that would indicate posterior pelvic tilting through action of the rectus abdominis. Once a client has performed wall-standing abdominal hollowing cor-
Teaching Your Clients the Basic Skills.
85
rectly to repetition, have him repeat the action without wall support. There should be no movement of the spine, pelvis, or rib cage.
Abdominal
.fI"~'.
Hollowing:
For subjects
2-Point Kneeling and Sitting
who are already
able to maintain
lumbar position and control body sway.
the neutral
Two-point kneeling and sitting (stool) can help lead up to free standing, as they require greater body segment control than either lying or 4-point kneeling. This is because in both 2-point kneeling and sitting, the upper part of the trunk is unsupported, while in 4-point kneeling, the arms support the upper trunk. Individuals must be more active in controlling the upper trunk when it is unsupported, paying attention to the hollowing action as well as to the position of the lumbar spine (maintaining neutral position) and the position of their shoulders (avoiding body sway). These positions are also the starting points for the hip hinge actions described later. Have your clients pay close attention to movement of the rib cage, as well as to shoulder position, pelvic tilt, and maintenance of a neutral lordosis. Instructing your client to "sit tall" or "kneel tall" can facilitate correct alignment; this concept is also helpful in correcting whole-body posture while standing.
Abdominal .fllm.
Hollowing:
Lying
Suitable for lean individuals perform hollowing.
and those already
able to
In prone lying, abdominal hollowing pulls the abdominal wall away from the floor-a practical cue for the beginning subject. Use of a pressure
continued
86
.
Back Stability
Abdominal Hollowing: Lying, continued
biofeedback unit can be very helpful (consult a medical supply catalog). Note that the pressure biofeedback unit is useful only for assessment and not for continuing exercises. Place the bladder of the feedback unit below the navel, its lower edge in line with the anterior superior iliac spines. As your client performs hollowing, the dial of the biofeedback unit will show a decline in his body's pressure on the bladder. Once your client has mastered this action, you can link it with hip extension movements, if you wish, to provide abdominal-gluteal co-contraction. Abdominal hollowing in supine lying permits an individual to feel the muscle activity and the pelvic position; again, pressure biofeedback may be useful. Have your client assume the crook lying position, with his fingers flat against the lateral abdominals below his navel. Explain that no pelvic tilt should occur during lateral abdominal contraction-you can check this by palpating the anterior superior iliac spine. You can use pressure biofeedback to monitor the depth of the lordosis: flattening of the back (posterior pelvic tilt) shows as increasing pressure on the dial and indicates activity of the rectus abdominis; excessive hollowing shows as reduced pressure and indicates loss of stability associated with anterior pelvic tilt. As your client performs abdominal hollowing, the pressure biofeedback unit should register no more than a 5-mm Hg increase in pressure-at this level of pressure the internal oblique, the transversus abdominis, and the diaphragm are all recruited together. Higher values (up to 15 mm Hg) will not increase the recruitment of the deep abdominals but will increase the activity of both the diaphragm and the rectus abdominis (Allison et al. 1998).
Tips for Teaching Abdominal Hollowing Multisensory cues can facilitate learning (Miller and Medeiros 1987). You can provide auditory cues by giving your clients frequent feedback about their performance; to create visual cues, encourage people to look at their muscles as they function and to place a mirror on the floor/couch below the abdomen; for kinesthetic cues, encourage subjects to "feel" the particular action-for example, ask them to "feel the stomach being pulled in." Muitlsensory cueing involves increased sensory input through auditory, visual, kinesthetic, and tactile stimuli, I i~o_nlunction with v~ualization of correct e~er:ise techni~~
KEY POINT:
:
J
Tactilecues for abdominal hollowing can come from you and/ or from a belt touching your client's abdomen. The first technique involves palpation. Place the heel of your hand over the client's anterior superior iliac spine and point your fingers toward the pubic bone (figure 4.1). Your
Teaching Your Clients the Basic Skills.
87
fingertips will then fall over the retroaponeurotic triangle, which is the most superficial position of transversus abdominis (Walters and Partridge 1957).At this point the external obliqje is aponeurotic and, so, not electrically active. This point may be used for siting the electrode of a surface EMG unit. Since the muscles are sheetlike, they will flatten rather than bulge when they contract. One way to facilitate the contraction is to instruct your clients to "stop me from pushing in" as you palpate the abdominal wall. A second way Figure 4.1 Palpation of the is have them cough (visceral compression) deep abdominals-the retro- and hold the muscle contraction they feel aponeurotic triangle-to teach beneath your fingers. This "cough and abdominal hollowing. hold" procedure is also useful in conjunction with surface EMG-as the muscle contraction shows on the EMG unit, encourage the subject to maintain the contraction while breathing normally. Continue with this exercise until your client can hold the contraction for a single 3D-second repetition or for 10 repetitions of 10 seconds each. Then encourage your client to reduce the contraction intensity of the muscle to the minimum required to maintain the hollow abdomen position. Another tip for tactile cues in the 4-point kneeling position: fasten a webbing belt around your client's abdomen below the navel, with the muscles relaxed and sagging (figure 4.2). The belt should be just tight enough to touch the skin but not to pull in the muscles. Have your client hollow the abdomen, pull the muscles away from the belt, and then relax them completely to fill the belt again. Figure 4.2 Using a belt to teach abSome people may be unable to dominal hollowing. draw the muscles away from the belt; others may contract their muscles too strongly, making the abdominal wall rigid and leading to aninability to relax the muscles again to fill the belt. Several days' practice will give your clients full muscle control over both actions. Once they can achieve the appropriate contraction, have them build up the holding time to 10-30 seconds while breathing normally.
88
. Back Stability
A final learning technique is visualization of correct exercise technique following your demonstration. For this "mental practice," your clients should relax and "see" themselves performing the exercise in their imagination. Such visualization has been shown to benefit development of both motor skills (Fansler et al. 1985) and strength (Cornwall et al. 1991). To help your "clients visualize the hollowing action, help them understand the workings of the transversus abdominis and internal oblique musclesyou can use simple diagrams of the muscles and then demonstrate their location using palpation. Analogies such as "personal muscle corset" or "cylinder of muscles" can be helpful. Abdominal Hollowing: Common Errors Be sure that your client's rib cage, shoulders, and pelvis remain still throughout the hollowing action (figure 4.3a). The contour of the abdomen will flatten if a person takes and holds a deep breath, but you will notice the chest expansion (figure 4.3b). If this occurs, instruct your client to exhale and then hold the resulting chest position while performing the exercise. Placing a belt around the lower chest provides helpful feedback about chestmovement (Richardson and Hodges 1996). If your client is using the external oblique to brace the abdomen, which is also an incorrect technique, the lower ribs will be depressed, and you may observe a horizontal skin crease across the upper abdomen (figure 4.3c). When this occurs, instruct your client to perform pelvic floor contraction at the same time as abdominal hollowing, but to avoid contracting the gluteus maximus (use of which leads in this case to inappropriate motor patterns for trunk stability during dynamic sports activity).
Lower ribs stay still a
Figure 4.3 Abdominal are incorrect.
Rib cage depressed
Rib cage lifted
c
b hollowing
in standing:
(a) is correct,
and (b) and (c)
Teaching Your Clients the Basic Skills
.
89
In kneeling, lying, and sitting positions, pressing onto the floor with the feet indicates a failure to isolate the deep abdominal action from that of the hip muscles. Placing your client's feet on a bathroom scale will provide clear feedback about hip extension pressure-ideally, the scales should show no increase in weight during the exercise. Your clients should maintain a neutral lumbar position during abdominal hollowing and refrain from significant movement of ribs, pelvis, or hips.
KEY POINT:
TEACHING YOUR CLIENTS TO CONTRACT THE MULTIFIDUS MUSCLES AT WILL Multifidus is the key stabilizer muscle within the spinal extensor group (page 50). Subjects with low back pain often lose the ability to contract this muscle (probably through pain inhibition), and they do not regain the ability spontaneously (Hides et al. 1996). Two kinds of exercises will help increase your client's basic back stability. The first focuses solely on the multifidus muscles, with an emphasis on helping your client learn to recognize what it feels like to tension/relax only those particular muscles. The second, using the techniques of proprioception, focuses not only on the multifidus but also on the lateral abdominals, which of course are also vital for basic stability.
The Basic Exercise for Multifidus Contraction Your help is essential for your client to learn adequate control of this muscle.
Multifidus Contraction .f{.1~'"
To learn to use the multifidus other muscles.
at will and separately
from
Your client begins in a prone lying position while you palpate his lower back medial to the longissimus at L4 and L5levels. Identify the spinous processes and slide your fingers laterally into the hollow between the spinous process and the longissimus bulk. Assess the difference in muscle consistency, and then determine your client's ability to isometrically contract the multifidus in a "setting" action. Once the individual can consciously contract the muscle, encourage him to use multifidus setting continued
90
. Back Stability
Multifidus Contraction, continued
in a sitting position with a neutral lumbar spine. He should become able to symmetrically contract the two multifidus muscles and sustain the contraction for 10-30 seconds.
Rhythmic Stabilization Rhythmic stabilization involves gross action of the multifidus in conjunction with the lateral abdominals. Rhythmic stabilization is a PNF (proprioceptive neuromuscular facilitation) technique that involves alternating isometric contractions of the agonist and antagonist muscles, building up to co-contraction (Sullivan et al. 1982). The general idea is simple: first, you apply a resistance in one direction and your client contracts her muscle against the resistance. Once you feel that the contraction has reached a maximum, instantaneously apply your resistance in the opposite direction-at which point she contracts the antagonist muscle, with no momentary relaxation between the two contractions. In this way, the muscle pairs are contracting to gradually higher levels. The following exercise uses this technique in teaching your client to contract the multifidus.
Rhythmic Stabilization of Multifidus and Lateral Abdominals in Side Lying Position .f{'7~'.
To encourage your client to contract lateral abdominals simultaneously.
the multifidus
and
With your client in the crook side lying position, palpate the intervertebral joints to ascertain the midpoint of the movement range at the spinal level where you have found pain/pathology (Maitland 1986). Remember that the multifidus muscle is unisegmental-that is, each fascicle stretches over only a single segment of the lumbar spine. Wasting of the muscle occurs at the same level as the segment of pathology (Hides et al. 1994). To place the relevant muscle fascicle at its optimum length, you must move the painful segment into its midrange. If you feel inadequate to do this, ask an experienced orthopedic physical therapist to work with you.
The exercise consists of you pushing forward on your client's pelvis and backward onto the shoulder while your client resists the action. Then reverse the action: while you push backward on the pelvis and forward onto the shoulder, she continues to resist the action, not allowing herself to relax even for a second. The action can be more localized by an orthopedic physical therapist who can palpate the specific spinal continued
Teaching
Your Clients the Basic Skills.
91
Rhythmic Stabilization of Multifidus and Lateral Abdominals in Side Lying Position, continued
level that requires resistance to rotation. General resisted rotation can be performed for the whole spine by having a partner help you use this exercise at home. The exercise is repeated 5-10 times at each of three treatment sessions.
Teaching Tips for Multifidus Contraction Initially, you will palpate with your thumb and the knuckle of your first finger placed on either side of the lumbar spinous process at any one level. Instruct your client to "feel the muscle swelling" without actively flexing the lumbar spine (figure 4.4). You may want to suggest that your client practice this action with his own thumbs so he'll have some feedback for home practice. While sitting, he should press into the extensor region with his thumbs at the side of the spinous processes. Figure 4.4 Palpating to The pressure should be steady but deep. The assist your client in detectaim is to feel the muscle swelling against his ing multifidus contraction. digital pressure without allowing his pelvis to From Norris 1998. tilt or his spine to arch. Angling the trunk forward at the hip (hip hinge action) will contract the longissimus and enable your client to distinguish between the longissimus fibers (more lateral) and the multifidus. Performing abdominal hollowing at the same time will improve the multifidus contraction.
.
SUMMARY Safely improving back stability requires that an individual learn to contract certain muscles voluntarily and independently-in particular, the deep abdominal muscles (transversus abdominis and internal oblique) and the multifidus muscles of the back.
.
Such independent muscle control enables an individual 1. to control pelvic tilt (i.e., to voluntarily move the pelvis independently of the spine); 2. to support the spine with contracted multifidus; 3. to support the spine with abdominal hollowing; and 4. to achieve the neutral position of the lumbar spine, from which position most exercises in this book should begin.
.
This chapter teaches you, the therapist,
these skills.
how to help your clients learn
S Muscle Imbalance Muscle imbalance occurs when a particular agonist is significantly stronger than its antagonist, or when one or the other is abnormally shortened or stretched. The body's attempts to compensate for imbalance generally exacerbate the problem and can lead to serious disability. This chapter first presents general theory about muscle balance and imbalance. It then shows you how to identify such problems and how to treat them. Much of the material for this section is modified from Norris (1998), to which you are referred for further reading.
BASIC CONCEPTS We can categorize muscles into two nondistinct groups Ganda and Schmid 1980; Richardson 1992): (1) Muscles that primarily stabilize a joint and approximate the joint surfaces are known as stabilizers or "postural muscles." (2) Muscles primarily responsible for movement (those which develop angular rotation more effectively than the stabilizers), are called mobilizers or "task muscles."
CTermsYOUShoulil1<now
~
diastasis separation of normally joined parts. pseudoparesis apparent weakness brought on by increased tone in a muscle antagonist.
Stabilizers (postural muscles) primarilyfix a joint'" and prevent movement. Mobilizers (task muscles) primarily create movement.
KEY POINT:
I
Stability muscles tend to be more deeply placed in the body and are usually monoarticular (one-joint) muscles, whereas mobilizers are on the whole superficial and are often biarticular (two-joint) muscles. For example, in the leg, the rectus femoris is classified as a mobilizer, while the other Chapter 5 exercise descriptions adapted from Norris 1998. 92
Muscle Imbalance.
93
quadriceps muscles are stabilizers. Stabilizer function is more slow-twitch (type I) or tonic in nature, whereas that of the mobilizers tends toward fast-twitch (type II) action. This physiology suits the functional requirements of the muscles-enabling mobilizers to contract and develop maximal tension rapidly but also to fatigue quickly. The stabilizer muscles build tension slowly and perform well at lower tensions over longer periods, being more fatigue-resistant. Stabilizers can be subdivided into primary and secondary types Gull 1994) (table 5.1). The primary stabilizers (e.g., multifidus, transversus abdominis, and vastus medialis oblique) have very deep attachments, lying close to the axis of rotation of the joint. In this position, they are unable to contribute any significant torque but will approximate the joint.
Table 5.1
Muscle Types
The following characteristics are not absolute but are only tendencies within these sometimes inexact categories of muscles. Stabilizers Mobilizers Primarily responsible for movement, Primarily responsible for stabilizing including angular rotation and approximating joints Examples: rectus femoris. hamExamples: multifidus, transversus strings abdominis, vastus medialis oblique
.
.
.
.
Primary stabilizers . Deep, close to joint . Slow twitch
.
Usuallymonoarticular (1 joint)
Secondary stabilizers
. . . .
Intermediate
depth Slow twitch Usually mono-
articular Primary source of torq ue ments multipinnate
. torque . . Build tension slowly, more fatigue resistant No significant Short fibers
. .
.
Better activated at low levels of resistance More effective in closed chain movement In muscle imbalance, tend to weaken and lengthen
. Superficial . Fast twitch
.Often biarticular (2 joints) .
.
Secondary
source of torque
Build tension rapidly, fatigue quickly . Better activated at high levels of resistance More effective in open chain movements In muscle imbalance, tend to tighten and shorten
.
.
94
. Back Stability
In addition, many of these smaller muscles have important proprioceptive functions (8astide et al. 1989). The secondary stabilizers (e.g., gluteals and oblique abdominals) are the main torque producers, being large monoarticular muscles attaching via extensive aponeurosis. Their multipinnate fiber arrangement makes them powerful and able to absorb large amounts of force through eccentric action. The mobilizers (e.g., rectus femoris and hamstrings) act as stabilizers only in conditions of extreme need. They are fusiform in shape-a less powerful fiber arrangement, but one able to produce large ranges of motion. Stabilizer muscles are better activated at low resistance levels-about 30-40% of the maximum voluntary contraction (MVC)-while mobilizer muscles are generally better activated above this level. Re-educating the muscles of back stability therefore calls for low-level contractions, not the extreme workouts well-meaning therapists sometimes prescribe for lower back pain. In addition, stabilizer muscles respond better to closed kinetic chain actions, where movement occurs proximally on a stabilized distal segment; in standing, this would be with the foot on the ground for the lower limb, or the hand on a wall for the upper limb. Mobilizer function is more effective in an open chain situation, where free movement occurs without distal fixation. In the lower limb, the swing phase of gait is open chain; in the upper limb, throwing is a prime example. The structure and functional characteristics of the two muscle categories makes the stabilizers better equipped for postural holding and antigravity function. The mobilizers are better designed for rapid ballistic movements. Two fundamental changes appear when there is muscle imbalance: (1) tightening of mobilizer (two-joint) muscles and (2) loss of endurance (holding) within the inner range of motion of the (single-joint) stabilizer muscles, which arises from their being abnormally stretched. These two changes are used as tests for the degree of muscle imbalance present. Since the changes in length and tension alter muscle pull around a joint, they may draw the joint out of alignment. Changes in body segment alignment and the degree of segmental control (the ability to move one body segment without moving any others) form the basis of the third type of test used when assessing muscle imbalance. The mixture of tightness and weakness in muscle imbalance alters body segment alignment and changes the equilibrium point of a joint. Normally, the equal resting tone of agonist and antagonist muscles allows the joint to assume a balanced resting position, with the joint surfaces evenly loaded and the joint's inert tissues not excessively stressed. However, if the muscles on one side of a joint are tight and the opposing muscles are lax, the joint will be pulled out of alignment toward the tight muscle (figure 5.1). This alteration in alignment throws weightbearing stress onto a smaller region of the joint surface, increasing pressure per unit area. Further, the inert tissues on the shortened (closed) side of the joint will contract over time.
.
Muscle Imbalance
95
Normal
a Joint
Joint
Figure 5.1 Posture and muscle imbalance. (a) Equal muscle tone gives correct joint alignment. (b) Unequal muscle tone pulls joint out of alignment, resulting in faulty posture. Reprinted from Griffin 1998.
a ()
b
c
I I I
I I I I
ID
:-;
I
.,
'.
I
I
I I I,
I I
:E)
()
Figure 5.2 Relative flexibility. When the attached tighter cord (A-B) moves less than the looser cord From Norris 1998.
cords (B-C).
I
are stretched,
the
Imbalance also leads to a lack of accurate segmental control. The combination of stiffness (hypoflexibility) in one body segment and laxity (hyperflexibility) in an adjacent segment leads to relative flexibility (White and Sahrmann 1994). In a chain of movement, the body seems to take the path of least resistance, with the more flexible segment always contributing more to the total movement range. Consider two pieces of rubber tubing of unequal strengths that are attached to one another (figure 5.2). If the movement begins at C and A is fixed, the more flexible area B-C moves more. This will still be the case if C is held immobile and A moves. Taking this example into the body, figure
5.3
shows
areas
a toe-touching
of interest
for relative
exercise.
flexibility
The
two
are the
a
Figure 5.3 Relative stiffness in the body. bine equal
pelvic
tilt and spinal flexion. stressing the more lax spinal tissues. (0) From Norris 1998.
(a) Forward flexion should com(b) Tight hamstrings limit pelvic tilt,
96
. BackStability
hamstrings and lumbar spine tissues. As we flex forward, movement should occur through a combination of anterior pelvic tilt and lumbar spinal flexion. Many people have tight hamstrings and excessively lax lumbar tissues due to excessive bending (lumbar flexion) during everyday activities. During this flexing action, greater movement (and therefore greater tissue strain) always occurs at the lumbar spine. Relative stiffness in this case makes the toe-touching exercise ineffective as a hamstring stretch unless the trunk muscles are tightened to stabilize the lumbar spine.
~
Muscle imbalance can iead to changes in-b-oth
functionand structure of the body tissues.
MUSCLE ADAPTATION TO INJURY, AND TRAINING
IMMOBILIZATION,
Different kinds of muscles react differently to injury and immobilization. Primary stabilizers such as multifidus and transversus abdominis, for example, react quickly (by inhibition) to pain and swelling (see table 5.2). Table 5.2 Stabilizer and Mobilizer That Affect the Lower Back
Muscles marked
with'
Muscles
can act as both stabilizers
and mobilizers,
situations. Stabilizers
Mobilizers
. Primary stabilizers Multifidus Transversus abdominis Internal oblique Gluteus medius Vastus medialis Serratus anterior Lower trapezius Deep neck flexors . Secondary stabilizers Gluteus maximus Quadriceps Iliopsoas' Subscapularis Infraspinatus Upper trapezius' Quadratus lumborum'
. Iliopsoas' . Hamstrings . Rectus femoris . Tensor fasciae Hip adductors Piriformis
. . . . . . . .
lata (TFL)
. Rectus abdominis External oblique Quadratus lumborum' Erector spinae Sternomastoid Upper trapezius' Levator scapulae . Rhomboids . Pectoralis minor . Pectoralis major . Scalenes
in different
Muscle Imbalance.
97
There are even more clear differences in reactions to reduced usage, which has been studied extensively using immobilized limbs. The greatest tissue changes occur within the first few days of disuse. Strength loss can be as much as 6% per day for the first eight days, with minimal loss after this period (Appell 1990). Type I and type II muscle fibers differ considerably in response to disuse, with type I fibers showing greater reduction in size and greater loss of total fiber numbers than type II. In fact, the number of type II fibers actually increases-demonstrating a process of selective atrophy of the type I fibers (Templeton et al. 1984). However, not all muscles show an equal amount of type I fiber atrophy. Atrophy is largely related to change in use relative to normal function, with the initial percentage of type I fibers that a muscle contains being a good indicator of likely atrophy pattern. Those muscles with a predominantly antigravity function, which cross one joint and have a large proportion of type I fibers (e.g., the soleus and vastus medialis muscles) show greatest selective atrophy. Predominantly slow twitch antigravity muscles that cross multiple joints are next in order of atrophy (e.g., erector spinae). Finally, the phasic, predominantly fast type II muscles (e.g., biceps) can be immobilized with less loss of strength than the other two groups (Lieber 1992). Training also causes selective changes in muscle. In the knee, rapid flexion-extension actions can selectively increase activity in the rectus femoris and hamstrings (biarticular mobilizers) but not in the vasti (monoarticular stabilizers). In a study by Richardson and Bullock (1986) comparing speeds of 75°/sec and 195°/sec, mean muscle activity for the rectus femoris increased from 23.0 f.I. V to 69.9 f.I. V. In contrast, muscle activity for the vastus medialis increased from 35.5 f.I. V to only 42.3 f.I.V (figure 5.4). The pattern of muscle activity was also noticeably different after training. The rectus femoris and hamstrings displayed phasic (on-and-off) activity at the fastest speeds, while the vastus medialis show~d a tonic (continuous) pattern. The graphs in figure 5.5 show an EMG trace of the electrical activity produced when a muscle contracts. The general trend of the graph shape is important, rather than each individual line. Note that there are clear groups of electrical spikes for the rectus femoris and the hamstrings, indicating that activity occurred in these muscles at specific points in the total movement. For the vastus medialis there are no clear groups, indicating that the activity occurred continually throughout the movement. Ng and Richardson (1990) found similar changes even in the more functional closed kinetic chain position. A four-week training period of rapid plantar flexion (in standing position) gave significant increases in jump height (gastrocnemius, biarticular) but also significant losses of static function of the soleus (monoarticular). Recruitment patterns of lower back muscles also change depending on the type of training used (O'Sullivan et al. 1998). Subjects followed a
98
. 8ack Stability 70-
o 75°/sec .1500/sec .195°/sec
60-
:~ (;
~50-
co Q)
40U ::> 30'" :2 20 10
n Vastus lateralis
Rectus femoris
Vastus medialis
Lateral hamstring
Figure 5.4 Muscle activity changes with increases in speed. Reprinted from Richardson and Bullock 1986.
Rectus femoris Hamstrings
Vastus medialis 0°
Knee angle
Figure 5.5 Muscle activity patterns during rapid alternating knee flexionextension. Note that biarticular muscles are phasic, while monoarticular muscles are tonic. Reprinted from Richardson and Bullock 1986.
lO-week training program involving either abdominal hollowing (15 minutes daily, progressed with limb loading) or gym exercise that included trunk curls. EMG activity of the internal oblique (more important for back stability) increased in the hollowing group, whereas that of the rectus abdominis remained relatively unchanged. Trunk curls (but
Muscle Imbalance
1000
1000
~~ 500
500
. 99
w~
o
Before
After
Before
o
After
.
After
Abdominal
Trunk curl
D
Before
Before
After
hollowing
Rectus abdominis Internal
oblique
Figure 5.6 Altered abdominal Data from O'Sullivan et al. 1998.
muscle
not hollowing) led to an increase duction in activity of the internal
TRAINING
recruitment
pattern
with
in rectus abdominis activity oblique (figure 5.6).
training.
and
a re-
SPECIFICITY
The aforementioned differences in responses of stabilizer and mobilizer muscles illustrate the importance of training specificity. Responses to training closely correspond to the type of exercise used. For example, if runners want to reduce their marathon running time, sprint training will not be effective. This is because sprinting is primarily an anaerobic activity (energy supplied from stores within the body), whereas marathon training is predominantly aerobic (energy supplied by using oxygen and food as fuel). We can say in this case that, although the sprint training caused an increase in fitness, the aspect of fitness that improved was not strictly relevant to the event that the training was designed for. The training was not specific to the event. In the same way, we have seen that high-speed muscle training leads to recruitment of mobilizer muscles. In the example from Richardson and Bullock (1986) described previously, the rectus femoris increased its activity markedly at high-speed (195°/sec) movements. If we used this highspeed training to try to improve the vastus medialis, it would not be very effective. Specificity can be remembered by a simple mnemonic, S.A.I.D., which stands for Specific Adaptation to Imposed Demand. The change occurring in the body (the adaptation) is specific to (exactly matches) the training used (the imposed demand). You can adequately address your clients'
100
.
Back Stability
muscle imbalances only by using quite specific exercises-which, of course, require equally accurate, specific assessments of which muscles need what kind of treatment. The tests described later in this chapter will help you make such appropriate assessments. '""Training specificity dictates that, when de5'i'Qriing an exercise program for a client, you must consider the
KEY POINT: I
functional requirements, contraction type, and speed of contraction of a muscle.
CHANGES IN MUSCLE
LENGTH
Changes in muscle length do not occur in a uniform manner throughout the body. An overly simplistic but useful description is that stabilizer muscles tend to "weaken" (sag), whereas mobilizers tend to "shorten" (tighten). Exercise therapy aimed at muscle must therefore be selective rather than general, seeking to lengthen (stretch) tight mobilizer muscles and shorten/build endurance of inactive stabilizer muscles.
Chronic Muscle Lengthening The weakening of stabilizer muscles has been termed stretch weakness (Kendall et al. 1993): the muscle remains in an elongated position, beyond its normal resting position but within its normal range. This is different from overstretch, in which the muscle is elongated beyond its normal range. The length-tension relationship of a muscle (page 38) dictates that a stretched muscle, where the actin and myosin filaments are pulled apart, can exert less force than a muscle at normal resting length. Where the stretch is maintained, however, this short-term response (reduced force output) becomes a long-term adaptation: the muscle adds more sarcomeres to its ends in an attempt to move its actin and myosin filaments closer together (figure 5.7). This adaptation, known as an increase in serial sarcomere number (SSN), can lengthen a muscle by up to 20% (Gossman et al. 1982). The length-tension curve of an adaptively lengthened muscle moves to the right (figure 5.8). The peak tension such a muscle can produce in the laboratory is up to 35% greater than that of a normal length muscle (Williams and Goldspink 1978). However, this peak tension occurs at approximately the position where the muscle has been immobilized (point a, figure 5.8). If the strength of the lengthened muscle is tested with the joint in midrange or inner range (point b, figure 5.8), as is common in clinical practice, the muscle cannot produce its peak tension and appears "weak." For this reason, manual muscle tests appear to be more accurate indicators of positional strength than measures of total strength (Sahrmann 1987).
-
Figure 5.7 Muscle length adaptation. (0) Normal muscle length. (b) In stretched muscle, the filaments move apart, resulting in loss of muscle tension. (c) Normal filament alignment is restored by increases in serial sarcomere number (SSN), resulting in chronic abnormal muscle length. From Norris 1998.
10
Shortened Control Lengthened
a ,.,---....
8
§ c: o 'w c: $
6
~
4
U
2
,.,~/ , ,
, ,,
,
, ,,
,
, ,,
,
, ,,
,
,,"
1 0
1 0
% muscle belly length of control
Figure 5.8 Effects of immobilizing positions (see text for explanation).
a muscle in shortened
and lengthened
From Norris 1998.
101
102
.
Back Stability
In the laboratory, a lengthened muscle returns to its optimal length within approximately one week if placed in a shortened position (Goldspink 1992). Clinically, restoration of optimal length may be achieved by immobilizing the muscle in its physiological rest position (Kendall et al. 1993) and/or by exercising it in its shortened (inner-range) position (Sahrmann 1990). Enhancement of strength is not the priority in this situation-indeed, the load on the muscle may need to be reduced to ensure correct alignment of the various body segments and correct performance of the relevant movement pattern. SSN may be partly responsible for changes in muscle strength without parallel changes in hypertrophy (Koh 1995). A number of factors influence SSN, which exhibits marked plasticity. For example, immobilization of rabbit plantarflexors in a lengthened position showed an 8% increase in SSN in only four days; applying electrical stimulation to increase muscle force led to an even greater increase (Williams et al. 1986). Stretching a muscle appears to affect SSN significantly more than does immobilization in a shortened position. Following immobilization in a shortened position for two weeks, the mouse soleus decreased SSN by almost 20% (Williams 1990). However, stretching for just one hour per day in this study not only eliminated the SSN reduction, but actually increased SSN by nearly 10%. Eccentric stimuli appear to cause a greater adaptation of SSN than concentric stimuli. Morgan and Lynn (1994) subjected rats to uphill or downhill running and found SSN in the vastus intermedius to be 12% greater in the eccentric-trained rats after one week. Koh (1995) has suggested that, if SSN adaptation occurs in humans, strength training may produce such a change if it is performed at a joint angle different from that at which the maximal force is produced during normal activity. The lengthened muscle is not weak-it merely lacks the ability to maintain full contraction within the inner range. This shows up clinically as a difference between the active and passive inner ranges. If the joint is passively placed in full anatomical inner range, the subject is unable to hold the position. Sometimes the position cannot be held at all, but more usually the contraction cannot be sustained, indicating a lack in slow twitch endurance capacity. Clinically, reduction of muscle length is seen as the enhanced ability to hold an inner-range contraction. This mayor may not represent a reduction in SSN but is a required functional improvement in postural control for muscles that are abnormally lengthened. Muscle shortening appears in the dorsiflexors of equestrians, who clearly do not hold the shortened position permanently, as with splinting, but rather show a training response. Following pregnancy, SSN increases in the rectus abdominis in combination with diastasis. Again, length of the muscle gradually reduces in the months following birth. Inner-range training, then, is likely to shorten a lengthened muscle (Goldspink 1996).
Muscle Imbalance
. 103
Assessing Stretched MusclesTesting Inner-Range Holding Ability We have seen from figure 5.8 that the length-tension curve of a lengthened muscle moves to the right, indicating that it is unable to produce significant power within the full inner range. This fact forms the basis of the assessment of stabilizer muscle length by inner-range holding tests. Tests for the most important stabilizing muscles are described below. Lower Back and Hip Muscles-inner-Range Hoiding Tests The ability of a stabilizer to maintain a low-load isometric contraction over a period of time is vital to its antigravity function and may be assessed using the standard muscle test position (Richardson 1992; Richardson and Sims 1991). In all the following assessments, ask your clients to maintain a contraction in full inner range, the key factor being the length of time they can maintain the static hold before developing jerky (phasic) movements. In each case, you will place the limb passively into the full inner range. If the limb drops upon release, the passive range of motion differs from the active range-an important indicator of poor stabilizer function. Full stabilizing function is present only when a subject can maintain the innerrange position for 10 repetitions of 10 seconds' duration Ou1l1994). In all the tests, it is important that your subjects attempt all 10 repetitions; often they will perform the first two or three normally, with the deficit becoming apparent only in later repetitions.
Assessing
Muscle
Balance
in the Iliopsoas
While sitting, your client flexes her hip while maintaining 90° knee flexion so that the foot is lifted clear of the ground. Have her hold this position as long as she can, while you record the time at which phasic movements begin. Note also the position of the pelvis and lumbar spine. Where the iliopsoas is lengthened, one of two things may happen: (1) If lumbar stability is poor, the pelvis will drop back into posterior tilt, flattening or even reversing the lumbar lordosis. (2) If lumbar stability is good, your client will be able to maintain the neutral position of the lumbar spine and pelvis-but the knee will simply drop, indicating that the hip flexor muscles have lengthened (but not necessarily weakened) and are unable to hold the full inner-range position.
104
. Back Stability
Assessing
Muscle
Balance
in the Gluteus
Maximus
,,----.. Have your client lie in a prone , -position with her knee flexed to 90°. Then she should lift her \/ , hip to the inner range of ex-----tension and hold it steady (right; b, below). Using palpation, note the order of muscle contraction during the hip extension. Normally, the hamstrings should contract first, followed by the gluteus maxim us, then the contralateral erector spinae, and finally the ipsilateral erector spinae (Lewit 1991). In many cases of imbalance, the gluteus is poorly recruited or even inhibited (pseudoparesis) by tightness in the opposing hip flexors (Janda 1986). Where this is the case, the order of muscle contraction changes. If the gluteals do not function adequately, the hamstrings dominate the movement-little gluteal activity is apparent, and the muscle mass remains flaccid. Note how long your client can hold the position steady before phasic movement begins. Performing the test with the knee bent reduces the contribution that the hamstrings make to the movement by shortening them. The contribution of the gluteus is therefore more apparent. Your ability to see and feel the subtle changes that indicate the order of muscle contraction, however, takes time to develop. Until you have gained experience in this area of examination, you can use dual-channel EMG to show the intensity and timing of muscle contraction. Note: watch carefully to see if your client performs a false hip extension movement; in this action, the pelvis anteriorly tilts due to powerful action of the erector spinae, and the relationship between the hip and pelvis remains the same (c). Thoroughly explain to your client which muscles she should be using to perform this activity and in which order. If she tends to make a false hip extension, hold her pelvis down while she raises her leg using only her gluteals, so that that she learns what the correct movement feels like.
a ,, ,
o c
/' \v "-.:. '7"
Muscle Imbalance
Assessing
Muscle
Balance
in the Gluteus
.
105
Medius
The action in this test is combined hip abduction, with slight lateral rotation to emphasize the posterior fibers of the muscle. Have your client lie on her side with her upper knee flexed. Instruct her to abduct and externally rotate her upper leg so that the femur is at a 45° angle to the ground and her knee is flexed about 45° (dotted lines in figure). Then have her rotate her chest toward the examination table while keeping her upper leg in place Oull1994). Deep Abdominal Muscles-inner-Range Holding Tests Rather than deal with specific abdominal muscles as I did with the hip muscles, I think it more useful in this section to focus on the entire system of deep abdominal muscles that affect lumbar stability and that often are abnormally stretched (and therefore weak in their inner ranges). You can test clients' ability to hold the inner range of the deep abdomina Is (1) by assessing their abilities to hollow the abdomen, and (2) by monitoring lumbar lordosis and pelvic tilt while overloading the stability system. You can assess both actions by accurate palpation and motion recording, but I recommend use of pressure biofeedback, which will make the assessment considerably easier. Note that the pressure biofeedback unit is more useful for assessment rather than for continuing exercises. To assess limb function relative to lumbar-pelvic stability, you can use a number of starting positions-two of which I will describe in detail.
Prone Abdominal
Hollowing Test
Using
Pressure
Biofeedback
.I'{"~'.
To asse.ss client's ahility to hold the inner range of the deep ahdomlnals.
With your subject lying prone, place the pressure biofeedback unit beneath his abdomen with the J upper edge of the device's bladder below his navel. Inflate the unit to ~70 mm Hg, and instruct your client to perform abdominal hollowing (see chapter 4). The aim is to reduce the pressure reading on the biofeedback unit by 6-10 mm Hg continued
~
106
. Back Stability
Prone Abdominal Hollowing Test Using Pressure Biofeedback. continued
and to be able to maintain this contraction for 10 repetitions of 10 seconds each while breathing normally (Richardson and Hodges 1996).
Heel Slide Maneuver Using Pressure
Biofeedback
.,{l1~'" Assess the deep abdominals' ability to maintain spinal stability. The subject begins in a crook lying position with the spine in a neutral position and the pressure biofeedback unit positioned beneath his lower spine. While you palpate the anterior superior iliac spine (ASIS), instruct him to gradually straighten one leg, sliding the heel along the ground to take the weight off the limb. During this action, the hip flexors are working eccentrically and pulling on the pelvis and lumbar spine. If the strong pull of these muscles is sufficient to displace the pelvis, you will be able to feel the pelvis tilt; moreover, the pressure shown on the dial of the biofeedback unit will change. If your client cannot complete the action without any alteration of pelvic tilt or depth of lordosis, palpate the abdominal muscle action. Often subjects will substitute their rectus abdominis and/ or external oblique in an attempt to fix the pelvis rather than using transversus abdominis and internal oblique. Where this is the case, these deeper abdominal muscles will need to be re-educated.
Assessing
Shortened Muscles
Mobilizer muscles have a tendency to tighten. TIghtness in the hamstrings (mobilizers), for example, is common, while tightness in the gluteals (stabilizers) is rare. In addition to reducing range of motion, muscle tightening may lead to development of trigger points (Travell and Simmons 1983)small hypersensitive regions within a muscle that stimulate afferent nerve fibers, causing pain. The sensation created is a deep tenderness with an overlying increase in tone, creating a palpably tender band of muscle. When palpated deeply, the trigger point creates a local muscle spasm, the "jump sign" Ganda 1993). Because tight muscles have a lowered irritability threshold, they are activated earlier than normal in a movement sequence-and they have less slack to take up before contraction begins. In addition, tight muscles have increased afferent input via the stretch receptors (Sahrmann 1990).
Muscle Imbalance
.
107
There are several important reasons why you should assess the tightness of your client's mobilizer muscles. First, since limited range of motion may not allow sufficient movement for correct body segment alignment, limbs may be pulled into positions that stress joint surfaces and collateral ligaments. Second, tightness in a muscle may, through reciprocal innervation, inhibit the opposing muscle through the process of pseudoparesis Oanda 1986). Third, stability must be relative to flexibility. Consider the straight-leg raise (SLR) exercise (see page 109): poor stability can lead the pelvis to tilt very early in the range of motion. Normally, the pelvis only tilts when the hamstring muscles reach the end of their stretch-they are fully 'wound up' -and this may not occur until 80-90° hip flexion. If pelvic tilt is seen before this (in a flexible individual), an imbalance exists. The individual's level of stability is not sufficient for her level of flexibility-she has lost active muscular control over a portion of her total range of motion, a fundamental feature in the difference between hypermobility and instability. If you find muscle tightness, you can use the test movements as starting positions for stretching. But before prescribing stretching exercises, be sure that they will not place excessive strain on adjacent body parts because of relative stiffness. Your clients often will require some stability work before beginning the stretches. The need for stability work is indicated if the subject's alignment is degraded (partially lost) as a stretch is applied. To assess tightness in those muscles that are most likely to exacerbate lower back problems, there are four principal tests--each of which in its own way will help you to assess restriction of pelvic motion: (1) the modified Thomas test, (2) the straight-leg raise (SLR) test, (3) the Ober test, and (4) the tripod test. Carefully note whether any of the movements in these tests reproduces the pain for which the patient has sought treatment; note also if the range is significantly less than the optimal position. (For the Thomas test, optimum is for the femur of the lower leg to drop down to the horizontal, and the tibia of the same leg to drop to the vertical. For the SLR, the optimal value is 70-80° from the horizontal; and for the Ober test, the upper leg should drop down to the level of the couch.) In either case, the muscle will require specific stretching.
The Thomas Test .fl:t1.,.
To assess/correct femoris.
tightness in the iliopsoas and rectus
The patient begins in crook lying at the end of the examination table. Instruct her to lift both knees up to her chest, keeping her back flattened continued
108 . Back Stability
The Thomas Test, continued
to a point where the sacrum just begins to lift away from the examination table surface, but not farther. You can monitor the movement of the pelvis and lumbar spine using a pressure biofeedback unit. As she holds one leg close to the chest to maintain the pelvic position, have her lower the other leg over the end of the table, maintaining a 90° angle at the knee (a). Optimal alignment occurs with the femur horizontal and aligned with the sagittal plane (no abduction) and with the subject's shoulder, hip, and knee more or less in line. The tibia should hang vertically (90° knee flexion) and be aligned with the sagittal plane (no hip rotation-see c). If the femur rests a above the horizontal and the knee is flexed less than 90°, tightness may be present in either the iliopsoas or rectus femoris. If the rectus is tight, straightening the knee will take the stretch off the muscle and the leg will drop down (b). If the knee is straightened and the leg stays in place, it indicates tightness in the iliopsoas. Use palpation to distinguish between the psoas and iliacus. Psoas can be palpated deep in the abdomen at the side of the lumbar spine. Iliacus is found on the inner side of the pelvis. Both muscles take experience to palpate, as they lie beneath the abdominal con- c tents (see figure 3.lOb, page 58).
The Ober Test .f'[t1~,..
To assess both the length of tensor fasciae lata muscle and the tightness of the iliotibial band.
The modified Ober test begins in side lying with the pelvis in a neutral position (a). Have your client bend her lower leg to improve overall body continued
Muscle Imbalance
.
109
The Ober Test, continued
stability while you stabilize the pelvis to avoid lateral pelvic dipping. The examination table should be low enough to allow you to place pressure through the subject's iliac crest in the direction of the lower shoulder. You may monitor the position of the spine and pelvis using pressure biofeedback. While she maintains the neutral pelvic position, have your client abduct the upper leg to 15° above the horizontal and then extend her hip about 15°. She should then adduct it while maintaining extension. For an athlete, optimal muscle length would be confirmed if she is able to lower the upper leg to the level of the table; the nonathlete should be able to lower the leg to the horizontal (b). A false reading is obtained if the pelvis is allowed to tip and the lumbar spine to laterally flex. You can still proceed with the test when hip extension is limited, but you should further assess the hip tightness to determine if it results from muscular, capsular, or osteological factors-an examination for which you should refer the subject to an orthopedic physical therapist.
The Straight-Leg .f{tH.
Raise (SLR) Test
To assess tightness
in hamstrings.
Have your client lie supine on the examination table, one leg slightly bent. Have her raise the other leg while keeping it completely straight. Palpate the anterior rim of the pelvis to note the point at which the pelvis begins to posteriorly tilt due to hamstring tightness-this is the point at which a stable base is no longer being provided for the hamstrings to stretch against. Two body segments are moving here; this is a prime example of relative flexibility, as mentioned on page 95. As the maximal continued
110
.
Back Stability
The Straighr-Leg Raise (SLR) Test, continued
range of hamstring flexibility is reached, the pelvis will begin to tilt posteriorly, bringing the ischial tuberosity of the pelvis forward in an attempt to reduce tension in the hamstrings. Look for pelvic tilt, which will occur before the hamstrings are fully stretched to their end range. For example, if your client can stretch the hamstrings to 90° hip flexion, does the pelvis move at 80-90° as it should because the tension in the hamstrings is maximal? Or does the pelvis begin to tilt at perhaps 4050°, when the tension in the hamstrings is only moderate? The latter case indicates a lack of muscular control over the pelvisthe individual is unable to create the stable pelvic base (using the trunk stabilizers) for the stretched hamstrings to pull against.
The Tripod Test .1'{'1~'. To assess/correct imbalanced hamstrings. Have your client sit on the examination table with his lumbar spine in the neutral position and his feet hanging off the edge. As he straightens one leg, note two measures: (1) the point at which posterior pelvic tilting occurs, and (2) the total range of combined motion at both hip and knee. For optimal performance, the lumbar spine should remain neutral and should allow the knee to straighten to within 10° of full extension while the femur remains horizontal. If you find muscle tightness, you can use the test movements as starting positions for stretching.
Muscle Imbalance
PRINCIPLES
OF MUSCLE
.
111
STRETCHING
Five methods of stretching are generally recognized: ballistic, static, active, and two PNF (proprioceptive neuromuscular facilitation) techniques (table 5.3). PNF stretching has been adopted by the sporting world from neurological physiotherapy treatments. By alternately contracting and relaxing muscles, these techniques capitalize on various muscle reflexes to achieve a greater level of relaxation during the stretch. The back stability program uses two PNF techniques: contract-relax (CR), and contractrelax-agonist-contract (CRAC). PNF stretching was believed at one time to be the most effective type of stretching (Etnyre and Abraham 1986; Holt and Smith 1983), with CRAC methods generally being better than CR. The data are not consistent, however. Moore and Kukulka (1991) found CRAC to cause more pain than either CR or static stretching; moreover, they found that static stretching appeared to be the most effective of all the techniques, leading to less pain and more range of motion. 1recommend that you select stretching techniques on a client-by-client basis. Test to see what works best for each individual. The advantage of static stretching, of course, is that it does not require your presence or that of anyone else. Table 5.3
Principal Stretching Techniques
Method
. .
Action Rapid jerking actions at end of range to force the tissues to stretch. Slowly and passively stretching the muscle to full range, and maintaining this stretched position for a set
.
Ballistic
.
Static
period-usually from 15 to 30
. Active .
Contract-relax
.
seconds.
. Contracting the agonist muscle to full inner range to impart a stretch (CR)
Contract-relax-agonist-contract (CRAC)
'
.
on the antagonist. Isometrically contracting the stretched muscle, then relaxing and passively stretching the muscle still farther. This action is usually performed by a partner. The same as CR. except that during the final stages of the stretching phase. the muscle opposite the one being stretched is contracted.
.
112
.
Back Stability
Here are the basic five stretching methods: 1. Ballistic stretching involves taking the limb to the end of its movement range and adding repetitive bouncing movements. This method is increasingly out of favor since it appears that it may cause injury and muscle soreness (Etnyre and Lee 1987). Although not recommended for regular training, ballistic stretching may have a place in the final stages of rehabilitation for athletes whose sport requiresballistic actions (e.g., high kicks in martial arts practice) (Norris 1998). 2. During static stretching, a muscle is stretched to the point of slight discomfort and held there for an extended period. A holding time of 30 seconds has been shown to be optimal, with 15 seconds being less effective and 60 seconds being not more effective (Bandy and Irion 1994). Repeating the stretch is important, with the greatest stretching effects occurring within the first four repetitions (Taylor et al. 1990). Easily remembered, basic guidelines for static stretching are 5 repetitions, holding each for 30 seconds, with a 3D-second rest period between each movement. 3. Active stretching involves pulling a limb into full inner range so that the antagonist muscle is stretched passively while the agonist is strengthened. This type of stretch can be important when correcting muscle imbalance. The inner-range contraction helps shorten a lengthened (lax) muscle, while the shortened muscle is stretched using a functionally relevant movement. Webright et al. (1997) found static and active stretching equally effective when used daily for a six-week period. Static stretching involves less coordination and fewer repetitions than active stretching, so it is more appropriate to early treatment stages. Active stretching involves more complex coordination and requires greater segmental control, making it more useful in later stages of rehabilitation. 4. The CR (contract-relax) PNF technique involves lengthening a muscle until a comfortable stretch is felt. From this position, the muscle is isometrically contracted and held for a set period. The muscle is relaxed again, then taken to a new lengthened position until the subject again feels the full stretch. The rationale behind the CR method is that the contracted muscle will relax as a result of autogenic inhibition, as the Golgi tendon organ (GTO) fires to inhibit tension. Some authors argue that a maximal isometric contraction is needed to initiate relaxation through the GTO mechanism Uanda 1992). Others recommend the use of minimal isometric contractions (Lewit 1991), which seem more appropriate in situations where pain is present. A window of opportunity exists after isometric muscle contraction-since the stretch reflex is suppressed for about 10 seconds following isometric contraction (Moore and Kukulka 1991), the stretch must be imposed during this time. 5. With the CRAC (contract-relax-agonist-contract) PNF technique, the muscle is stretched as just described-but in the final stages of the stretch,
Muscle Imbalance
.
113
the opposing muscle groups are isometrically contracted to make use of reciprocal inhibition of the agonist and to reduce its tension. To illustrate each of these procedures, consider stretching the hamstrings. 1.A ballisticstretch could involve keeping the leg straight while standing and vigorously reaching for the toes with a bouncing action. While the rapid action may actually tighten the muscle by increasing its tone, it may stretch other soft tissues-including the noncontractile muscle elements, muscle tendons, and ligaments surrounding the hip, knee, and spine. In this particular exercise, moreover, repeated spinal flexion may increase intradiscal pressure within the lumbar discs, potentially leading to discal migration (McKenzie 1981) or discal herniation. For this reason, ballistic stretching should only be performed in the presence of good lumbar stability and optimal segmental alignment. 2. An easy static stretch for the hamstrings involves lying supine on the floor in a doorway, with the hips just inside the door frame. With the leg farthest from the door frame flat on the ground and the back in neutral position, raise the other leg, keeping it straight, until it rests on the door frame. To increase/ decrease the stretch, move the body closer to or farther away from the door frame. The stretch is held for 30 seconds. 3.An active stretchcould be performed by standing, holding on to a wall bar for support, and lifting the straight leg upward using the force of the hip flexors. 4. An individual could perform the CR technique for the hamstrings while lying on his back. A training partner lifts his leg, keeping the knee straight. After holding the stretch for 10seconds, the athlete contracts his hamstrings by pulling the straight leg down toward the floor against his partner's resistance. He holds the tension for 10 to 20 seconds-sufficient time to allow the GTO to override the stretch reflex. He then releases the tension, and the training partner reapplies the stretch. 5. The CRAC technique takes this stretch even further: as the stretch is applied, the athlete tries to increase the stretch himself by pulling the straight leg up toward his head, tensing his hip flexors. In so doing, the hamstrings are relaxed still further through reciprocal inhibition, and the stretch becomes even more effective.
STRETCHING
TARGET
MUSCLES
Several mobilizer muscles within the lumbar-pelvic region are commonly tight and may require stretching. It is generally best to begin with passive static stretching, followed by contract-relax techniques. Finally, the opposing muscles are shortened to full inner range to stretch
the antagonist actively.
114
. Back Stability
Thomas
Test Stretch
.1'1".'. To stretch the hip flexors. This stretch is performed from the Thomas test position (see page 107). Any firm surface may be used at home, such as a sturdy coffee table. Your client should hold one knee tightly to her chest and allow the other leg to rest in a stretched position near the horizontal. To increase the emphasis on the rectus femorus muscle, the knee of the lower (horizontal) leg may be bent. Throughout the movement the back must remain flat on the table and the pelvis must not be allowed to move. She should hold the stretched position for 10-20 seconds, and then lower the leg slowly. Raising into the stretch position and recovering from it should be performed with control, taking 5 seconds in each direction. Reverse the legs and repeat the cycle two more times. Have her perform this stretch daily until she can perform the Thomas test satisfactorily.
Half Lunge .1'111.'. To stretch
the hip flexors.
Have your client take up the half-kneeling position, with one hand on a chair to aid balance and the other hand pressing into the lumbar spine on the side of the dependent leg (the one with the knee on the floor). Instruct him to keep his abdomen hollowed throughout the exercise in order to keep the lumbar spine in neutral position. Tell him to lunge his body forward, forcing the dependent hip into extension while avoiding increasing the lordosis. Hold this stretched position for 10 seconds. Instruct your client to perform this exercise three times a day, each session comprising 10 lunges on each side.
Muscle Imbalance
.
115
Hip Hitch .lIel~''- To work the trunk side flexors on the side of the weightbearing leg. This exercise is used in preparation for the Ober stretch, to enable the subject to control the pelvis with the trunk side flexors. Your client should stand with her hands on a tabletop for support at home, or a bar in the clinic. Instructing her to keep her legs straight throughout the movement, have her make one leg shorter than the other by laterally tilting her pelvis. It may help by suggesting that she imagine she is drawing the rim of her pelvis vertically upward on the side of the shortening leg, raising her heel slightly off the ground. To avoid simply coming up onto the toes, have your client dorsiflex (pull up) her foot-this way you can assess movement of the whole leg in one section. Tell her to keep her upper body from swaying and to relax her shoulders. Once she has mastered this action, have her practice it unsupported (hand off the tabletop), then lying supine, and finally while lying on her side. In each case, the knee must be kept straight throughout the movement, with the action coming from pelvic movement alone. When using the side lying position, she should place her upper hand on her upper hip to provide resistance (since there is no gravity to resist), and she should pull her upper leg up as she simultaneously pushes the leg that is against the floor down (as if she's trying to make that leg as long as possible). Instruct your client to perform this exercise three times a day, with five repetitions for each side from each of the three starting positions (standing, supine, side lying).
Ober
Test Stretch
.lIeN'-Stretch (TFL).
the iliotibial band (lTB) and tensor fasciae lata
The ITB and TFL can become overactive and tight to compensate for a weak or inactive gluteus medius muscle. When this occurs, tightness in the ITB-TFL can cause friction of this structure over the greater trochanter of the femur or the lateral epicondyle of the femur. Both of these areas continued
116
.
Back Stability
Ober Test Stretch, continued
are common sites for ITB friction syndrome-a common overuse condition, particularly among distance runners, that results from muscle imbalance. Beginning in a side-lying position, your client first performs the hip hitch as just described. Then he continues with the Ober test actions (see page 108): he abducts the upper leg to 15° above the horizontal, extends it to 15°, then lowers it into adduction (toward the floor or couch) while maintaining an immobilepelvis. The exercise is complex because it requires the control of two body parts simultaneously. Supervise your client closely, (1) watching the pelvic rim to note any unwanted pelvic movement and (2) noting if the hip extension is being maintained. When the hip extension is lost, the leg falls forward into flexion and the stretch is lost from the TFL. If your client is unable to maintain stability of his pelvis, assist him by holding the pelvis in place with your hands.
Active Knee Extension,
Holding Thigh
.1'[17.'. To stretch the hamstrings. Have your client lie supine, then raise one leg to 90° hip flexion, comfortably bent at the knee, and hold it with her hands beneath the thigh. Then instruct her to straighten the leg as much as possible. The sensation should be one of a deep stretching sensation rather than acute pain. The discomfort should reduce as the stretch is held. She should hold the stretch for 30 seconds. Instruct her to perform this stretch at home three times a day, with two repetitions for each leg at each session.
Active
.1'[.'.'.
Knee
Extension,
To strengthen
Pushing
Against
Thigh
hip flexors, hip
extensors, and hamstrings.
This action stretches the hamstrings while activating the quadriceps against a resistance. Increasing the quadriceps activity should reduce the hamstring tone through reciprocal innervation. continued
Muscle Imbalance
.
117
Active Knee Extension, Pushing Against Thigh, continued
Have your client lie supine and, with one knee comfortably bent, raise that leg until it is at a 600angle to the floor. Instruct him then to straighten the leg, and then slowly raise the straightened leg till it is vertical (900 hip flexion). He should keep the leg completely straight and use only his hip flexor muscles to raise the leg (no use of the hands this time!), without allowing the knee to bend. Once the leg is vertical (or as near vertical as your client can raise it), have him place his hand on the leg just above the knee and use it as a fulcrum to straighten the leg just a little bit more. This is especially helpful in stretching the hamstrings. He should hold this position for 30 seconds. Tell your client to do this exercise three times a day, using three repetitions for each leg per session.
Tripod Stretch .f{'7~'.
To stretch the hamstrings.
Have your client sit upright on the edge of a table, her lumbar spine in its neutral position, her feet hanging over the edge of the table. She should maintain abdominal hollowing throughout the exercise. Have her straighten one leg, to stretch the hamstrings against the stable base of the unmoving pelvis. She should hold the leg straight for 15 seconds, then slowly lower it. Instruct your client to perform this exercise three times a day, with three repetitions per leg per session.
Trunk Side Flexor Stretch .f{'H.
To stretch the quadratus the oblique abdominals.
lumborum
and lateral portion
of
These muscles are commonly tight after prolonged periods of sitting or bed rest. Have your client stand with his back against a wall, his feet shoulder-width apart, his hands clasped behind the head. He should keep his abdomen hollowed throughout the exercise. Instruct him to slowly bend his spine (and only his spine) to one side, being very careful to keep his pelvis level and his knees straight. Until he learns what the continued
. Back Stability
118
Trunk Side Flexor Stretch. continued
proper movement feels like, you should place your hands on his pelvis and let him know when it's bending. Tell him to reach his upper elbow as far toward the ceiling as he can, in an attempt to "lengthen his spine," and to hold this position for 30 seconds. Then he should repeat the exercise to the other side. The height of the upper elbow indicates the range of motion obtained, and the comparative range of each side will reveal your client's degree of symmetry. Instruct your client to do this stretch three times a day on each side.
J.'7:,\
~
':. ,
"'-'
r/
'
J
.
"
Four-Point Kneeling Stretch .fle,,-,.
To stretch the erector spinae.
,:-_... The erector spinae muscles also can tighten :~ during long periods of sitting or bed rest. Have your client assume a 4-point kneeling position. Emphasize that, throughout this exercise, she must move only her spine, with her shoulders remaining over her hands and her hips remaining over her knees at all times. Have her tilt her pelvis posteriorly and continue flexing her spine until her face points toward the groin. She should hold this position for 30 seconds, then slowly relax back toward the starting position. Instruct your client to perform this exercise three times a day, with six repetitions per session.
~~
.
SUMMARY Muscles can be divided roughly, although not unambiguously, into stabilizer or mobilizer muscles. Stabilizer muscles tend to be deep, to contain mainly slow-twitch fibers,
. .
to control only one joint, and primarily to prevent movement while stabilizing a joint. They are the primary postural muscles. Mobilizer muscles tend to be more superficial, to contain mainly fasttwitch fibers, to act over two joints, and primarily
to create movement.
Muscfe Imbalance
·
.
119
Disuse, long-term bed rest, and injury can cause muscle systems to become imbalanced-with an agonist shortened while its antagonist is stretched.
·
To train specific muscles, you must carefully target those muscles in your exercise prescriptions; exercises meant to improve back stability often fail to do so because they target the wrong muscles (especially the deep stabilizer muscles).
·
You can treat such imbalance by prescribing exercises that strengthen/ shorten the stretched muscle and stretch the shortened muscle; this chapter describes a number of such exercises.
~ Basic Abdominal Muscle Training Much of the back stability program involves working on the abdominal muscles. Especially for your clients who want to take abdominal training further (to enhance performance rather than merely to build stability), you must offer training that is both safe and effective. First I want to discuss currently popular abdominal exercises and assess their effects on the muscles and tissue. Then I will present modifications to improve the safety and effectiveness of such exercises.
CURRENT
PRACTICE
IN ABDOMINAL
TRAINING
Abdominal training can be dangerous, whether for competitive sport or for general fitness. In sport, athletes often adhere with almost religious fervor to traditional but potentially harmful training methods. In the general population, fashion often dictates which movements are in favoryet many popular exercises lack reliable scientific foundation. Before you can prescribe the most appropriate trunk exercises for your clients, you must understand what the traditional exercises actually achieve. To this end I will begin by briefly analyzing the two major categories of abdominal exercises: the sit-up and the leg raise.
The Sit-Up In the sit-up, an individual comes from a supine lying to a long sitting position using hip flexion, usually combined with trunk flexion. In a classic sit-up, the rectus abdominis shows activity as soon as the head lifts (Walters and Partridge 1957), and as a consequence the rib cage is depressed anteriorly. This initial period of flexion emphasizes the supra umbilical portion of the rectus; the infra umbilical portion contracts later, with the internal oblique (Kendall et al. 1993). As the internal oblique contracts, it pulls on the lower ribs, increasing the infrasternal angle by causing the ribs to flare out. 120
Basic Abdominal Muscle Training
.
121
Fixation of the pelvis is provided by the hip flexors, especially the iliacus through its attachment to the pelvic rim. The strong pull of the hip flexors is partially counteracted by the pull of the lateral fibers of external oblique and the infra umbilical portion of the rectus abdominis, which tend to tilt the pelvis posteriorly. Action of the external oblique, if powerful enough, compresses the ribs and reduces the infrasternal angle once more (Kendall et al. 1993). Problems Resulting From Poor Conditioning Initiation of the sit-up action sometimes leads to "bow stringing" in poorly toned individuals. For the superficial abdominals (rectus abdominis and external oblique) to pull flat, the deep abdominals (transversus abdominis and internal oblique) must be able to pull on the rectus sheath to hold the abdominal wall down. Many people, however, have lost the ability to coordinate action of both the superficial and deep abdominals, which this action requires-the two sets of abdominal muscles are imbalanced, with poorly recruited deep abdominals and dominant superficial abdominals. When this is the case, the abdominal wall appears to dome and the athlete may lift the trunk with the lumbar spine extended or flat rather than flexed (figure 6.1). Weak deep abdominal muscles cannot hold the rectus abdominis down as it contracts, leading to "doming" of the abdominal wall.
KEY POINT:
a
b Figure 6.1 Trunk alignment during a sit-up exercise. (a) Strong deep abdominals flatten abdominal wall. (b) Weakened deep abdominals allow abdominal wall "doming," while lengthened superficial abdominals allow anterior pelvic tilt and hollowing of the back. From Norris 1998.
122
.
BackStability
Poorly conditioned subjects also tend to use the hip extensors to momentarily tilt the pelvis posteriorly at the beginning of a sit-up, prestretching the hip flexors. This gives the hip flexors a mechanical advantage before hip flexion occurs and reduces both the work required of the abdomina Is and the conditioning effect of the exercise on the abdominals. During this phase, the abdominal muscles work eccentrically (Ricci et al. 1981). Effects of Foot Fixation If a person attempts a sit-up from the supine position without allowing trunk flexion, the legs tend to lift up from the supporting surface-this occurs because the legs constitute roughly one-third of total body weight whereas the trunk contributes two-thirds. The upper body's center of gravity moves toward the hip as the abdominal muscles flex the spine, reducing the lever arm of the trunk and enabling the subject to perform the sit-up without lifting the legs (figure 6.2). When the abdominal muscles are weak and lengthened, maximum spinal flexion does not occur because the muscles are unable to pull the lumbar spine into full inner range-the lever arm of the trunk remains long, and the legs lift. The point at which this occurs in the movement depends on a subject's weight and height. If the feet are fixed, however, the hip flexors can pull powerfully without causing the legs to lift. The act of foot fixation itself, in fact, may facilitate the iliopsoas Oanda and Schmid 1980). To pull against the fixation point, one must use active dorsiflexion-which simulates the gait pattern at heel contact, increasing activity in the tibialis anterior, quadriceps, and iliopsoas (a pattern known as flexor synergy during gait) (Atkinson 1986). , ...-......, I
,---_
I... \ " "',..-' ",
, ,-, , , ,, , ~r- , , ,.... , , ...'" , , , , "
,,
Figure 6.2 As the trunk flexes, the center of gravity of the upper body moves caudally. From Norris 1998.
Basic Abdominal Muscle Training.
The hip flexor muscles contract powerfully in a traditional sit-up. Fixing the foot causes the hip flexors to work even harder, without significantly increasing the work on the abdominal muscles.
KEY POINT:
123
1
The Straight-Leg Raise The bilateral straight-leg raise (SLR) creates only slight activity in the upper rectus, although the lower rectus contributes a greater proportion of the total abdominal work in this exercise than with the sit-up (Lipetz and Cutin 1970). The rectus works isometrically to fix the pelvis against the strong pull of iliopsoas (Silvermetz 1990). The iliopsoas contracts with maximum force when the lever arm of the leg is greatest (near the horizontal) and reduces as the leg is lifted toward the vertical. Problems Resulting From Poor Conditioning In subjects with weaker abdominals, the pelvis tilts and the lumbar spine hyperextends during the SLR. This forced hyperextension dramatically increases stress on the facet joints, especially those in the lumbar spine. The movement is likely to be limited by impaction of the inferior articular processes on the laminae of the vertebrae below (see chapter 2) or, in some cases, by contact between the spinous processes (Twomey and Taylor 1987). Rapid action of this kind can damage the facet joint structures. Once the facet and lamina are touching each other, further loading causes axial rotation of the superior vertebra (Yang and King 1984); the superior vertebra then pivots, causing the inferior articular process to move backward, overstretching the joint capsule. Effects of Arm Fixation When the legs are lifted in an SLR, the body position is less secure because its base of support is smaller. People tend to rock toward the side of the lifted leg (where one leg is lifted) or to struggle to keep their backs on the floor (where both legs are lifted). Fixing the arms by holding onto an overhead object (e.g., gym bench) with the arms, or by pressing down with the flats of the hands with the arms by the side, improves the security of the starting position. The disadvantage of fixing the arms, however, is that people can pull harder with their hip flexors without realizing they have lost their lumbar alignment. This is especially true of the bilateral leg raise action. At the beginning of this action the leverage from the legs is maximal, as they are horizontal. Without fixing their arms, poorly conditioned subjects may be unable to lift their legs at all-thereby self-limiting potential stress on the lumbar spine. With arms fixed, however, they may be able to lift their legs by rapidly pulling
124
. Back Stability
with their arms and "jerking" their legs up with a rapid contraction of the hip flexors. Once the legs move toward the vertical, their leverage is reduced and the movement can be continued-leading people to believe (wrongly) that, since they completed the action, they must have performed it correctly. The jerking action is extremely dangerous, however, due to the compression and shear forces it imposes on the lumbar spine. For SLRs, then, permit your clients to fix their arms only when they will perform the exercises in a slow and controlled fashion, and only after you have chosen the exercise most appropriate for their specific body condition. Straight-leg actions are inappropriate for poorly conditioned subjects or for those with a history of back pain.
MODIFICATIONS ABDOMINAL
OF TRADITIONAL EXERCISES
Your clients will find it easier to learn modifications of exercises they already know than to learn totally new procedures. Such modifications also may be more acceptable to "experienced trainers" than if you try to convince them to change their ways completely. Remember that in every case your clients should begin with their abdomens hollowed and their lumbar spines in neutral position. Except where otherwise noted, have your clients perform 8-10 reps of each exercise once a day, three days per week. Except where otherwise noted, the initial movement of each exercise should take about 2-3 seconds; your clients should hold the position for 1-3 seconds; then should perform the reverse movement in 2-3 seconds. Note, however, that these are mere guidelines. If at any time your clients are not working hard enough, increase the overload by slowing down the exercise or increasing the number of repetitions. If they are working too hard, reduce the overload. As your clients become more proficient at a given exercise, they can increase the number of repetitions, perform the movements more slowly, and/ or increase the time for the holding period. Remember to emphasize to your clients that, when moving slowly, they must breathe normally (no holding their breaths!). The limiting factor is not how many times individuals can superficially perform an exercise-but rather how well they can do it while stilI maintaining
Modifications
proper spinal alignment
and abdominal
hal/owing.
of the Sit-Up
Bending the knees and hips to alter the starting position of the sit-up affects both passive and active actions of the hip flexors, and the biomechanics of the lumbar spine. Supine lying stretches the iliopsoas, aligning it with the horizontal (figure 6.3). As the muscle contracts in this position,
Basic Abdominal Muscle Training.
125
trunk lifting is at a mechanical disadvantage and vertebral compression is at its greatest-the ratio of lifting to compression is approximately 1:10 (Watson 1983). Flexing the knees pulls the iliopsoas more vertically, reducing the ratio of trunk lifting to vertebral compression to 2:5 in crook lying and 1:1 in bench lying. If flexion historically has exacerbated clients' back pain (consult with their physical therapists on this), they can use fewer repetitions (2 or 3) while increasing the exercise timing (8-12 seconds in each direction). This schedule reduces the number of flexion movements but maintains the overload on the muscle. With 450 hip flexion, tension in the iliopsoas is 70-80% of its maximum; with the hips and knees flexed to 900,the figure reduces to 40-50% Gohnson and Reid 1991). Note, however, that the iliopsoas develop passive tension due to elastic recoil. Since the iliopsoas are not fully stretched when the hips are flexed, they cannot passively limit the posterior tilt of the pelvis. Instead, to fix the pelvis and provide a stable base for the abdominals to pull on when the hips are flexed, the hip flexors contract earlier in the situp action. This contraction has reduced intensity (Walters and Partridge 1957), however, due to the length-tension relationship of the muscle.
Pull of iliopsoas
Trunk
lifting 1:10
t~
.
Vertebral compression 2:5
1:1
Figure 6.3 Flexing the hip lengthens the moment arm of the iliopsoas, enabling the muscle to complete the sit-up action with less force. Thus, verte. bral compression is reduced. From Norris 1998.
126
. BackStability
With the legs straight in the traditional sit-up position, the iliopsoas are stretched and can passively limit posterior tilting of the pelvis. The stretched position also enables the iliopsoas to exert greater force during hip flexion-which means that, if the abdominal muscles are too weak to maintain the position of the pelvis, the stronger hip flexors will hyperextend the lumbar spine and cause the pelvis to tilt forward, thus lengthening the abdominals and hyperextending the lumbar spine. This type of action is therefore unsuitable for postural re-education if the aim is to shorten lengthened abdominal muscles.
Bent Knee Sit-Up .1I.m.
To strengthen the abdominals while reducing the action of the hip flexors.
Have your client begin with the crook lying position, knees flexed to 90° and hips flexed to 45°. He should lift his trunk, moving from the hip alone, and either at the same time or slightly later should flex his hips. Suggest that he imagine himself as a hinge pivoting on the hip joint. The action must be slow and controlled, without strain. A pure bent knee sit-up requires keeping the spine straight, moving it around the fixed hip, and reducing the action of the hip flexors. Tell your client that, if he feels his back muscles straining instead of his abdomina Is, he should stop the exercise and perform abdominal hollowing before resuming the exercise.
Trunk Curl .''117.'. To shorten and strengthen the rectus abdominis. In this exercise there is no hip flexion, the lumbar spine remaining in contact with the supporting surface. Have your client assume the crook lying position, knees flexed to 90° and hips flexed to 45°. continued
Basic Abdominal Muscle Training'
127
Trunk Curl, continued
Instruct him to "roll through the spine," performing cervical flexion until the chin comes toward the chest, followed by thoracic flexion, until only the lumbar spine remains on the supporting surface. He then should reverse these actions, first lowering the thoracic spine from bottom to top and finally releasing the cervical spine so that the head is gently lowered back onto the supporting surface.
Bench Curl .f{17.:.'" To strengthen the upper abdominals (supraumbilical portion of rectus abdominis with the lateral fibers of external oblique) while reducing the pull of the hip flexors and lessening the stresses on the lumbar spine. The bench curl is performed from a starting position of 90° flexion at both the hip and the knee, with the calves supported on a bench or chair. Since shortening the hip flexors in this way reduces their ability to contribute to the movement, hip flexor action does not obscure the action of the abdominals. Instruct your client to "roll through the spine" just as in the trunk curl.
Modifications
of the Straight-Leg Raise
As none of the abdominal muscles actually crosses the hip, these muscles are not prime movers for the SLR. The SLR is nevertheless important for abdominal training because it enhances the pelvic stabilizing function of the infra umbilical portion of the rectus abdominis and lateral external oblique. Several modifications of the bilateral straight-leg raise can help reduce stress on the lumbar spine.
128
.
Back Stability
Heel Slide (see also discussion of this action in chapter 8) .f'[,,~,.
To statically overload the abdominal muscles, increasing the emphasis on the deep abdominals.
Have your client assume a crook lying position, then straighten one leg while keeping the heel on the ground and sliding the leg into extension. Instruct her to place her hands over her lower abdomen on either side of the navel, her fingertips 5-6 inches apart. She should perform abdominal hollowing and keep the abdominal muscles tight beneath her hands as she slowly performs the leg action over a period of about 3-5 seconds (see page 170).
Leg Lowering .fI'l'1.
To increase the static overload on the abdominal while maintaining a neutral spine.
Instructyourclienttoliesu-
muscles
-
pine with hips flexed to 90° but with the knees extended so that the straightened legs are vertical. Tell him to slowly lower his legs until the pelvis begins to tilt. As soon as this occurs, he should raise the legs again to 90° hip flexion. Each cycle should take about 3-5 seconds. The advantage of this exercise over the standard straight-leg raise is one of changing leverage. With the standard leg raising action, the subject starts with maximum leverage on the leg, forcing the hip flexors and abdomina Is to work maximally from the very beginning. With leg lowering, the starting position provides minimum leverage. As the legs are lowered away from the vertical, leverage increases-but the subject is able to control the descent of the legs and avoid the position of maximal leverage that would cause the spine to hyperextend. Should a client find the leg lowering difficult to control, tell him to bend his knees in order to reduce leverage on the leg; or have him perform the exercise close to a wall, so he cannot fully lower the legs.
Basic Abdominal Muscle Training
.
129
Bench Lying Pelvic Raise .fI.1~'"
To strengthen the abdominal muscles, especially the lower (infraumbilical) portion of rectus abdominis.
Instruct your client to lie supine and flex both hips and knees 90o-a position she will main, tain throughout the movement. 5he should place her arms by her sides, hands flat on the table or floor. Have her lift her buttocks from the ground by flexing her lumbar spine, while keeping her legs relatively inactive. Although in this movement the lumbar spine is flexed as with the trunk curl, the movement occurs from "below upward" with the L551 joint moving first followed by flexion of each successively higher lumbar segment. The trunk curl provides the reverse movement (above downward) (McKenzie 1981).
i(........
~~~o /
Wall Bar Hanging Leg Raise .fll1~'" To strengthen the lower rectus, with increasing leg leverage, while providing traction for the lumbar spine. Performing leg raises while hanging from a wall bar considerably reduces the leverage forces on the lumbar spine and provides traction. Explain to your client that he must hold a neutral pelvic position throughout all versions of this exercise, preventing anterior tilt of the pelvis, and (except in the last variation) pressing the small of his back into the wall bars. There are three forms of the exercise: 1. Instruct your client to stand with his back against the wall bar, place his arms overhead, and hold onto a bar above head height. Then, avoiding any jerking action, he should slowly take his weight onto his arms and, keeping his legs straight, raise his feet slightly off the ground (a). Tell him to feel the stretch through the whole of his spine-and to tighten his abdominal muscles while pressing his lower back into the wall bar and breathing normally. Instruct him to hold this position for 2-3 seconds, and then release it slowly. continued
130
.
Back Stability
Wall Bar Hanging Leg Raise, continued
b
a
2. The action then progresses to include hip and knee flexion. For this exercise, instruct your client to bend his knees and raise them until he has achieved 90° hip flexion (Le., knees level with hips), while still keeping the lumbar spine in contact with the wall bars. Be sure that he doesn't jerk his knees up-the movement should be slow, lasting about 3-5 seconds. Suggest that he focus his attention on his abdominal muscles, pulling them in as he moves his legs. After holding the 90° flexed position for 2-3 seconds, he should slowly lower his legs to the starting position. 3. The final progression of this exercise requires flexing the lumbar spine to lift the back away from the support of the wall bars. This action, while working the abdominals hard, also strengthens and possibly shortens the hip flexors. Once your client has reached the 90° flexed position as in the previous exercise, instruct him to round his spine in order to slowly lift his tailbone away from the wall bar (b). Emphasize that, in the reverse movement, your client must not allow his body to "fall" and strike his tailbone hard onto the wall bar.
AB ROLLER
EXERCISES
The ab roller can help your clients re-educate their muscles for the trunk curl action (spinal flexion) as distinct from the sit-up movement (straight spine moving on a fixed femur). The frame allows only trunk flexion, while the subject's lumbar spine remains in contact with the ground.
Basic Abdominal Muscle Training
.
131
Basic Crunch .,{l7~'.
To work the abdominal muscles in general, with increased emphasis on inner-range activity of the upper abdominals.
Instruct your client to lie on her back with her knees bent and feet flat on the floor (crook lying), her head and neck on the neck rest of the machine. She should either grasp the centers of the curled handles at the sides of the device's arms or hold her arms straight with her wrists against the horizontal piece that connects the handles-whichever is more comfortable for her. Tell her to curl her trunk ("basic crunch"), keeping her head on the pad and gently assisting the movement by extending the shoulder. Her focus should be on pulling the abdominal wall in (hollowing). There is a tendency with this exercise for people to rapidly "pump" the movement-an error that adds considerable momentum to the spine and may forcibly overstretch the posterior tissues. Make sure that the exercise stays slow and controlled, following the earlier-stated principle that each movement should last 2-3 seconds. With time, your client will gain sufficient control to rest her elbows on the machine pads and press down with her elbows (shoulder extension), gripping only lightly with her open hand on the machine frame.
Reverse Crunch .f{t7~'.'ntense
strengthening
for the lower rectus abdominis.
This action emphasizes the lower portion of rectus abdominis. Instruct your client to raise her legs (one at a time) into a vertical position and maintain this position throughout the exercise. The exercise action is to vertically lift the leg as though trying to reach the toes to the ceiling, while keeping the upper body still. In so doing, she will lift her sacrum from the floor, a movement which combines posterior pelvic tilt with lower lumbar flexion. The movement must be slow and controlled with no lunging or bouncing.
132
.
Back Stability
Double
Crunch
.1'['7.:.'"To strengthen the upper and lower rectus abdom;n;s. The double crunch movement combines the actions of the trunk curl and the leg raise, working both the upper and lower portions of the rectus abdominis. Since two body areas work together for this exercise, it requires a greater degree of coordination than the other crunches. Starting position is the same as that of the basic crunch. Instruct your client to simultaneously (1) raise her knees toward her chest, posteriorly tilting the pelvis; and (2) raise her upper body (as in the basic crunch) to flex the spine. The lumbar spine remains on the floor, while the shoulders and sacrum both lift off the floor. She should perform the action slowly and precisely, avoiding the excess momentum on the spine that rapid "pumping" actions cause. Make sure that she neither holds her breath nor hyperventilates (breathes too rapidly). If she does hyperventilate, she should rest on her side and not attempt to stand up until the lightheadedness has passed.
Side Crunch .1'[.7.:.'" To strengthen the oblique abdom;nals the rectus abdom;n;s.
wh;le also working
Have your client begin in the basic crunch position, then lower her knees to one side; she should raise her arms up straight and cross them, her wrists resting on the horizontal bar as in one version of the basic crunch. Instruct her to perform, from this altered starting position, the same actions as in the basic crunch-to curl her trunk, keeping her head on the pad. Since asymmetry is common in this body region, your client may find that one side is stronger or more flexible than the other; as she continues with this exercise (assuming she uses correct form), the asymmetry should resolve and both sides should perform equally.
Basic Abdominal Muscle Training.
133
SUMMARY
· · · · ·
Popular abdominal exercises can be only moderately effective, or even dangerous, for some people with lower back injuries. Poorly conditioned individuals tend to place emphasis on the wrong muscles to perform straight-leg raises and sit-ups; modified versions of these exercises force them to use the correct muscles. Poorly conditioned subjects, or those with a history of back pain, should avoid straight-leg abdominal exercises altogether. It is generally more productive for you to introduce your clients to modifications of exercises they already know than to try to teach them totally new movements. This chapter introduces specific abdominal exercises that are both safe and maximally effective for functional abdominal training.
7 Posture Because postural alignment reflects changes in muscle length, it is the first form of assessment you will generally use to determine muscle imbalance. Before you can diagnose changes in alignment, however, you need a standard of optimal posture. The body moves continually around the optimal position in a process called body sway, and back stability is an essential component of this mechanism. In this chapter, I describe four principal types of posture.
OPTIMAL
POSTURAL
ALIGNMENT
Posture is the arrangement of body parts in a state of balance that protects the supporting structures of the body against injury or progressive deformity-a definition given in 1947 by the Posture Committee of the American Academy of Orthopaedic Surgeons (Cailliet 1983). A good posture is therefore effortless, nonfatiguing, and painless when the individual remains erect for reasonable periods (Cailliet 1981). Muscles function most efficiently in such an alignment, and the joints are optimally positioned (Bullock-Saxton 1988). Optimal posture combines both minimal muscle work and minimal joint loading. It is the combination of these two factors that is important-where optimal posture is lost (for example in "slouched standing"), the muscle activity is clearly reduced, but there is a significant increase in joint loadmg. Minimizing joint loading over time is important-articular cartilage gains its nutrition through intermittent loading (Norris 1998), and an even distribution of force is preferable to point pressure. Contact pressure is directly proportional to the transmitted force, but inversely proportional to area (McConnell 1993). Distributing force over a larger area by optimizing segmental alignment, therefore, reduces joint surface compression and lessens the risk of degenerative changes to a joint. The aim of any posture should be to reduce total energy expenditure and lessen stress on the supporting body structures. 134
Posture
.
135
_ Terms-You Shoultl Know ~ lateral malleolus the lower end of the fibula that forms the projection of the ankle tragus cartilaginous projection over the external opening of the ear
A good posture reduces total energy expenditure I and lessens the stress on the supporting body structures.
KEY POINT:
-
-
-
Any change in the alignment of one body segment automatically causes neighboring segments to move in an attempt to maintain stability. If one body segment moves forward, for example, another must move backward to keep the line of gravity of the body (LOG) within the base of support (figure 7.1). Over time, changes in force per unit area cause tissue adaptation (Norkin and Levangie 1992). Changes in serial sarcomere number within muscles (see chapter 5), for example, are adaptations to postural changes over time. Shortening ligaments lead to reduced range of motion, while lengthening ligaments reduce a joint's passive stability. Static posture-when the body is stationary-reflects the alignment of body segments and can reflect both changes in load distribution across joints and resting muscle length. Such postures include standing, sitting, and lying. Dynamic posture-body position during movement-can give information about body segment alignment, muscle actions, and motor skill. Typical dynamic postures are walking, running, jumping, and lifting. You can use both description of position (kinematic) and of force (kinetic) to assess posture.
POSTURAL
STABILITY
AND BODY SWAY
When standing erect, the human body has a small base of support due to its bipedal stance and comparatively high center of gravity (approximately
m m ctJ
-0
o ctJ-
Figure 7.1 When one body segment moves out of alignment, a neighboring segment moves in the opposite direction to maintain the line of gravity within the base of support.
136
.
Back Stability
at the second sacral segment). Humans are thus relatively unstable in comparison with quadrupeds with their larger base of support and lower center of gravity. Maintaining an erect posture takes surprisingly little energy, however, as a result of constant motion brought about by postural control. This motion (postural sway) depends on kinesthesis, or "motion sense" (Kent 1994), which enables us to detect the position of our body parts through organs of proprioception, vision, the vestibular apparatus in the inner ear, and skin receptors. Normal postural sway consists of a small continuous motion in the sagittal plane. This oscillation of the center of gravity results from alternating muscle activity-possibly a relief mechanism to reduce lower-limb fatigue and to aid blood flow (BullockSaxton et al. 1991). Excessive postural sway generally reveals poor balance and stability, a situation commonly seen in the elderly and inactive. Heavier people also may exhibit greater body sway (Sugano and Takeya 1970), as may taller individuals (Murray et al. 1975).Training usually can reduce postural sway. In the elderly, strength training may improve stability and limit postural sway (Hughes et al. 1996); following ankle injury, postural sway increases. By using balance and coordination training, body sway may be reduced to normal values once more (Bernier and Perrin 1998). Levels of postural sway can predict risk of recurrent falls among frail nursing home residents (Thapa et al. 1996). Lord and colleagues (1996) reduced fracture risk in women (ages 60-85) using a general aerobic exercise program whose effect was to improve postural sway rather than to change bone density.
BASIC POSTURAL ASSESSMENT You can assess static posture through comparisons to a standard reference line (Kendall et al. 1993), which represents the line of gravity. A weight board can help identify both the center of gravity (COG) and the vertical extension of this point to the ground (line of gravity). Find the horizontal distance from the edge of the board to the subject's line of gravity (d) by multiplying the combined weight of subject and board by the total length of the board (L) and dividing the result by the subject's body weight (W). See Luttgens and Wells (1982) for full details of this method. As the vertical extension of the COG, the LOG must pass within the body's base of support to maintain stability. The closer the body segments are to the LOG, the less torque there is around a joint. Where the LOG passes through the joint axis, no torque is created around that joint. If the LOG passes some distance from the joint axis, gravitational torque would tend to move the body segment toward the line of gravity were the segment not counterbalanced by elastic recoil of soft tissue and muscle action (Norkin and Levangie 1992). With the LOG anterior to the joint axis, the
Posture
.
137
proximal segment of the body connected to the joint tends to move anteriorly (figure 7.2); posterior motion tends to occur when the LOG is posterior to the joint axis. In the standard posture (viewed from the side), the subject is positioned with a plumb line representing the LOG, passing just in front of lateral malleolus (the bulge on the outside of the ankle). In an ideal posture, this line should pass just anterior to the midline of the knee and then through the greater trochanter, bodies of the lumbar vertebrae, shoulder joint, bodies of the cervical vertebrae, and the lobe of the ear (figure 7.3). Since the LOG is anterior to the ankle joint, gravity is continuously pulling the tibia anteriorly. This would result in enough dorsiflexion to unbalance the body were it not for constant opposing resistance provided by muscle action from the soleus (Nor kin and Levangie 1992). The LOG passes in front of the knee joint axis (but behind the patella), forcing the femur anteriorly and creating an extension torque resisted by the posterior knee structures. Table 7.1 shows the gravitational torques created by the position of the LOG and the opposing structures resisting these torques. When viewed from the front, with the feet 3-4 inches (10 cm) apart, the LOG should bisect the body into two equal halves. The anterior superior iliac spines (ASIS) should be approximately in the same horizontal plane, and the pubis and ASIS should be in the same vertical plane (Kendall et al. 1993). This alignment defines the neutral lumbar-pelvic alignment, which typically is about 5° to the horizontal. The joint axes of the hips, knees, and ankles should be equidistant from the LOG, and the LOG should transect the vertebral bodies (Nor kin and Levangie 1992). The gravitational torque imposed on one side of the body should equal that of the other side. Anatomical landmarks that provide comparisons for horizontal level on the right and left sides of the body include the knee creases, buttock
Gravity line Figure
7.2 When the gravity
line falls outside
segment tends to move toward the gravity line.
a joint,
the proximal
body
138
. BackStability
Figure 7.3 The standard reference line for posture. Reprinted, by permission, fromJ.C. Griffin, 1998, Client-centered exercise prescription (Champaign, Il: Human Kinetics), 66.
creases, pelvic rim, inferior angle of the scapulae, acromion processes, ears, and the external occipital protuberances. You also can observe alignment of the spinous processes and rib angles; minor scoliosis becomes more evident when assessed in Adam's position (forward flexion in standing). Unequal distances between arms and trunk (referred to as the keyhole), various skin creases, or unequal muscle bulk should prompt you to closer examination. You should also assess foot and ankle alignment. Figure 7.4 provides a simple checklist for postural assessment in the clinic. View the subject from behind and assess the symmetry of each of the body parts shown in the first column of figure 7.4 by comparing the right and left sides of the body. Record your observations in the section headed Notes (e.g., "head tilted to right," "left shoulder higher than right," or "left scapula lower"). These notes will highlight the region of the body that requires local testing of muscle length and joint movement by yourself or another therapist. Another way to assess static posture is to use a posture grid. The posture grid again uses a plumb line as a reference, but the subject stands behind a screen divided into 10-cm squares to aid inspection of body part alignment. To ensure reliability of the plumb line assessment for a given client, you must perform it at the same time of day to help remove diurnal variability (Tyrrell et al. 1985). Have subjects stand with their feet 10 em apart. They should walk on the spot (10
Posture
Table 7.1
Normal Alignment
in the Sagittal
Joints
Gravitational torque
forces
Passive opposing forces
Active opposing forces
Ligamentum nuchae; tectorial membrane
Posterior neck muscles
Cervical
Flexion Anterior Anterior to transverse axis for flexion and extension Extension Posterior
Thoracic
Anterior
Flexion
Posterior longitudinalligament; ligamentum flavum; supraspinous ligament
Lumbar
Posterior
Extension
Anterior longitudinalligament
Sacroiliac Anterior joint
Flexion type motion
Sacrotuberous ligament; sacrospinous ligament; sacroiliac ligament
Hip joint
Posterior
Extension
Knee joint
Anterior
Extension
Iliofemoral ligament Posterior joint capsule
Ankle joint
Anterior
Dorsiflexion
Atlantooccipital
13 9
Plane Opposing
Line of gravity
.
Anterior longitudinalligament Extensors
Iliopsoas
Soleus
Reprinted, by permission, from c.c. Norkin and P.K.Levangie, 1992, Joint structure and function: A comprehensive analysis, 2d ed. (Philadelphia: Davis). paces) and then come to rest, to aid general body relaxation. Instruct your clients to maintain their "normal" posture rather than to seek to modify or improve it. You can refine whole-body posture analysis by measuring alignment of individual body segments. You can assess pelvic tilt with a pelvic inclinometer, which measures the angle of pelvic tilt relative to the horizontal. The inclinometer consists of a protractor mounted on a base plate and attached to a pair of bone calipers. The inclinometer reads 0° when the caliper arms are horizontal. The end of the arms are positioned over the posterior superior iliac spine and the anterior superior iliac spine of one side of the body. The inclinometer dial shows the angle of pelvic tilt in the
Position
of body part
Head
Shoulder
Notes
position
level
Position of shoulder blade alignment
Skin creases at waist and spinal alignment
level
of bullock creases
level of knee creases
Calf muscle bulk and Achilles alignment
Flat foot or high arch
Figure
7.4
Assessing
standing
posture
from
From C. Norris, 199B, Diagnosis and management, Heinemann). Reprinted by permission of Butterworth of Reed Educational & Professional Publishing Ltd.
140
behind. 2d ed. Heinemann
(Oxford: Butterworth Publishers, a division
Posture
.
141
sagittal plane. This method of assessing pelvic tilt appears to be accurate to within::!: %0 (Toppenberg and Bullock 1986). Inclinometers are highly reliable and quite valid in comparison with lateral radiographs (Crowell et al. 1994). Pelvic tilt and lumbar lordosis are intimately linked, with changes in pelvic tilt causing significant alteration in the depth of the lordosis (Day et al. 1984). Bullock-Saxton (1993) demonstrated that inclinometer measurement is repeatable in both normal and symptomatic females: subjects were measured three times on a single day with three-minute intervals between consecutive tests, and then over three separate days with a four-day rest period between each test. You can use a flexible ruler to measure the depth of lordosis. Locate the spinous process of the second sacral segment (52), which lies between the posterior superior iliac spines. Palpate each spinous process from 52, counting back to the first lumbar vertebra (Ll) (figure 7.5). Record the length
L1
L2
L3
L4
L5
Figure 7.5 S2 lies between the posterior superior iliac spines. Palpate each spinous process cephalically from S2 up to L1. Use a flexible ruler to assess the depth of lumbar lordosis.
\
142
. Back Stability
(radius) of the traced curvature (L) of the lordosis from Ll to 52 and the depth of the lordosis (H) from the line joining Ll-52 to the deepest part of the lordotic curve, as shown on figure 7.5. Calculate the lordotic index (8) using the arctan formula, 8
=4 arctan(2H/L).
Arctan is a trigonometric term that can be calculated on most scientific calculators or computer spreadsheet programs. The flexible ruler method of assessing lordosis is highly reliable, as verified by lateral radiographs (Hart and Rose 1986; Lovell et a1. 1989). Lordosis measured in this manner showed average (mean) values of 50.9° in normal individuals and 40.4° in subjects who demonstrated lower abdominal weakness, confirmed as an inability to maintain alignment on supine leg lowering tasks (Levine et a1. 1997). Detect head position relative to trunk position with a stadiometer, an apparatus used to measure horizontal displacement of body segments relative to each other. The stadiometer consists of two or more sliding arms mounted on a vertical frame. The arms may be raised or lowered to the level of the body segments being measured, and then adjusted forward and backward (horizontally). A scale on the side of the horizontal arm shows the distance of each body segment from the vertical arm. Record the craniovertebral (CV) angle by measuring the degree of forward shift of the head, which pulls the suboccipital region into hyperextension (Watson 1994). The CV angle is that formed between a horizontal line through the C7 spinous process and the tragus (the prominence on the inner side of the ear) (figure 7.6). The average CV angle in asymptomatic subjects is 50° (range 48.6-52.0°); people who complain of cervical headaches have reduced angles (44.3°) (Watson 1994), indicating a head-heldforward posture as described by McKenzie (1990).
Figure 7.6 Using a stadiometer
to measure the craniovertebral
(CV) angle.
Posture.
143
Local "low-tech" measures of posture can be valid, reliable, and reproducible.
KEY POINT:
PRINCIPLES
OF POSTURAL
CORRECTION
Correcting posture requires a combination of several factors, embracing the approach to muscle imbalance described in chapter 5. Shortened muscles must be stretched, and lengthened muscle shortened. Static and PNF techniques can stretch muscles, while inner-range holding techniques can shorten lengthened muscles and build postural holding time. You must use principles of motor skill training (Norris 1998). Make use of the three stages of motor skill training to help your clients regain segmental control (table 7.2). In the cognitive stage, your client must learn objectively the requirements of a skill. In terms of postural reeducation, this often involves passive positioning of optimal postureyou place your clients passively into the optimal postural alignment by correcting pelvic tilt, for example, and instruct them to hold this position. This passive positioning is repeated several times until your clients are able to recreate the optimal position themselves. This signifies that they have progressed to the second stage of skill training (motor). During the second stage, the key factor is that individuals can identify their own mistakes. In the case of posture this means that they can consciously move into the optimal posture. Once they have achieved this ability, they are ready to perform a home-exercise program designed to build endurance Table 7.2
Stages of Motor Skill Learning
Cognitive
Motor
Automatic
.Movement "runs by movement . Stage of understanding .Effective itself' now obtained .tion Independent of atten. Movement more .Environmental cues important demands consistent . Action very fast . Use information from . Able to identify own past experiences . Poorly coordinated .mistakes Proprioception more important than visual . Unable to identify own mistakes
. .
Visual/verbal cues more important than proprioceptive Much coaching
needed
144
. Back Stability
of the postural muscles. Only after many thousands of repetitions of a movement will a person move into the third and final stage of motor training (automatic). Now, he is able to maintain an optimal postural alignment without conscious control because the action has become automatic. The process of learning to drive a car illustrates the three stages of motor learning. When we first learn to drive, the actions are difficult and we must concentrate on many separate activities. The actions become easier with repetition, as we begin to integrate the independent actions into a whole. Eventually, driving becomes largely automatic. Similarly, the separate components of postural control must be corrected individually and then pieced together to form a more complex single movement. By dividing the total movement into a number of component sequences, you can help your client learn the action more easily. Correcting a posture so that the correction becomes automatic is extremely difficult. If poor posture is held by shortened tissue, stretching can sufficiently lengthen tissue so that posture can change permanentlyassuming that the tissue is not allowed to shorten again through poor postural alignment. If poor posture is the result of muscle weakness brought on through injury (wasting or pain inhibition), muscle strengthening may successfully optimize posture. For many cases of poor stability, progressive exercises and proprioceptive training can effectively enhance stability and produce positive postural changes. When posture has been suboptimal for many years, however, full correction probably is not possible. Certainly improvements can be made, and these may be clinically significant (especially in relieving pain), but they will be limited. As an example of postural re-education, consider how you might treat common lordotic posture. This posture combines lack of active lumbar stability, lengthening of the rectus abdominis, and shortening of both hamstrings and hip flexors; moreover, the gluteus maximus often is poorly recruited. Re-education begins with stabilization training for the back, emphasizing use of the deep abdominals. Once your client has enhanced her basic stability, she should stretch her hamstrings. She could then combine the two separate activities, using a hamstring stretch in sitting position while maintaining spinal alignment. Following work to improve recruitment of the gluteals, stretch the hip flexors, and shorten the rectus abdominis, she should begin whole-body postural re-education using standing, walking, and sitting movements. Finally, she would begin proprioceptive training as described on page 197. Especially in the early stages of learning, you could use taping to give your client feedback. The taping performs two functions: First, structural taping or bracing can support a hypermobile segment of the body; second, functional taping can provide tactile feedback. In the latter case, skin
Posture.
145
drag will remind your client that her posture has moved away from the optimal alignment (place breathable undertaping under zinc oxide tape to protect the skin) (Norris 1994b).
POSTURE TYPES AND HOW TO CORRECT THEM There are four classic abnormal posture types (figure 7.7). In the lordotic posture, the main feature is excessive anterior pelvic tilt (a). Anterior displacement of the pelvis characterizes the swayback (b), while the flatback has slight posterior pelvic tilting and loss of lumbar lordosis (c). In the kyphotic posture the thoracic curve is excessive (d).
lordotic
Posture
In the classic lordotic or "hollow back" posture, the greater trochanter remains on the LOG, but the pelvis tilts anteriorly, moving the anterior superior iliac spine (ASIS) forward and downward in relation to the pubic bone. The abdominal muscles and gluteals are typically lengthened and have poor tone. Over time, the hip flexors may shorten, and pelvic tilt is limited by tightness in the overactive and tight hamstrings (Jull and Janda 1987). In an extreme lordotic posture seen in chronic obesity, the lumbar spine rests in extension with the lumbar facet joints impacted; the elastic recoil of the hamstrings allows the pelvis to hang. Janda and Schmid (1980) call this posture the pelvic crossed syndrome: high contact pressures occur in the facet joints, with the inferior articular processes impinging on the lamina
)
a Figure
7.7 Classic abnormal
(c) flatback;
and (d) kyphotic.
d
c
b
posture
types:
(a) lordotic;
(b) swayback;
146
.
Back Stability
below. Increased weightbearing of the facet joints in turn reduces the compression force on the lumbar discs (Adams et al. 1994). Lordotic posture is common in dancers and in young gymnasts, for whom it is a requirement of the sport. It is the posture most noticeable in women after childbirth, especially multiple births. In the case of childbirth, however, lengthening of the rectus abdominis through serial sarcomere adaptation is accompanied by diastasis, which mayor may not resolve spontaneously. Correction of lordotic posture requires shortening the abdominal muscles and lengthening the hip flexors. The rectus abdominis must be shortened by combining a posterior pelvic tilt with spinal flexion-but only after developing effective deep abdominal muscles to prevent bowstringing, where the abdominal muscles contract and bulge outward instead of pulling flat. This is different from the diastasis that occurs during pregnancy. With bowstringing there is no long-term structural change in the muscle, nor does the linea alba (the tendinous line between the two rectus abdominis muscles) split.
Modified Trunk Curl .f{t7~,. To shorten and strengthen the rectus abdominis muscle. The modified trunk curl action can help correct lordotic posture. Where full inner-range motion is lacking due to muscle lengthening, your client can perform the modified trunk curl in progressive stages. In stage 1, he lies supine with the knees bent and then posteriorly tilts his pelvis. Then have him curl up as far as he is able, combining spinal flexion with posterior pelvic tilt to fully shorten the rectus abdominis muscle. For stage 2, your client needs assistance either from you or from himself. You can gently pull your client into a slightly higher position, or he can pull himself higher by gripping his thighs. The extra lift should be no more than 1 or 2 inches (2.5-5.0 cm) and must be performed slowly and with care to avoid jolting the spine. Have your client hold the upper position with an isometric contraction for stage 4 (stage 3 is for those who can't perform stage 4), gradually building up the holding time from 1-2 seconds to 4-5 and finally to 10 seconds, at all times breathing normally. Individuals unable to hold the upper position should practice eccentric lowering, which represents stage 3: after they are lifted into the upper position and released, they should slow their descent back to the floor as much as possible. Initially they may almost fall back to the floor in less than 1 second. With practice, they should be able to lower themselves more slowly, taking 1-2 and then 4-5 and finally a full 10 seconds to lower continued
Posture
.
147
Modified Trunk Curl, continued
themselves. When they have achieved this level of strength, they can progress to holding the full upper position as for stage 4. How will you know if the abdominal muscles are lengthened and require shortening by this full inner-range holding method? In chapter 5, we saw that the length-tension curve moves to the right for lengthened muscles (see figure 5.8, page 101), indicating that they are unable to hold a joint at full inner range (i.e., to close the joint fully). When your clients perform the trunk curl, they are attempting full spinal flexion. If, in an attempt to pull the spine into full flexion, they fall back away from the inner-range position while performing the extra lift (with your help or by pulling on their thighs), you can safely conclude that the muscle is lengthened and requires this type of training to shorten it. Normally, full-range flexion of the spine is not recommended for general back care. Individuals with lordotic posture, however, have been maintaining the lumbar spine in extension. Full flexion is therefore a treatment of choice for such individuals and is widely used within physical therapy practice (McKenzie 1981).
Gluteus Maximus Inner-Range Exercise _fl,,,.,.
To contract and fully shorten the gluteus maximus.
The gluteus maxim us muscles must be tightened and shortened by working them in inner range (page 104). Have your client lie prone and flex one knee to 90°. She should then extend her hip, trying to emphasize the action of the gluteal muscles. If she is unable to lift the leg into full inner range, lift the leg for her. Then she should try either to hold this position (isometric) or to control the leg as it descends (eccentric). She eventually should attain full inner-range holding ability, with holding times built up from 3-5 seconds to 30-60 seconds. Take a gradual, progressive approach for those who are unable to lift the leg, always remembering to adapt the program to your client's individual level of progress. Begin with muscle re-education, encouraging your client simply to contract the gluteus in prone lying. Use of EMG feedback and manual muscle stimulation is helpful at this stage if the individual is completely unable to perform a static contraction. Tapping or brushing the gluteus with the fingers adds to multisensory cueing, making the task easier by increasing the amount of information that accompanies the movement. By making the contractions forceful, your client can increase the holding time until she can contract and hold the muscle for 10 seconds. Once she can do that, the next step is to lift the continued
J48
.
Back Stability
Gluteus Maximus Inner-Range Exercise, continued
femur into 10-150extension and place the knee on a block or cushion to maintain the extended hip position. She then contracts and holds the muscle as before, but in this new starting position. Eventually, she will develop sufficient strength so that you can remove the cushion and ask her to hold the extended position by herself. If your client is unable to hold this nonsupported position, have her use eccentric lowering. After you have raised her hip into 150extension, instruct her to hold it there as you release the leg. Encourage her to use the same intensity of muscle contraction as for the first two movements. If she is unable to hold the leg into extension (i.e., off the examination table), she should try to lower it in a controlled way rather than allowing it to drop. Have her gradually increase the time required to lower the leg to at least 10 seconds. The next stage is for your client to forcibly contract the gluteal muscles and simultaneously try to lift the leg off the table into extension. Suggest that she bend the knee to reduce the hamstrings' contribution to extension. Begin with 2-5 repetitions, lifting the leg as high as possible without allowing the pelvis to tilt. Try placing your hand just above your client's heel on the lifting leg and then encouraging her to lift the leg until her heel touches your hand. The final progression is first to lift the leg to full extension and hold this inner-range position for a full 10 seconds and then to perform 10 repetitions of this movement. If clients have both poor tone in the gluteals and poor control of hip extension in the prone position, have them begin a progression of exercises leading toward the goal of performing 10 repetitions, with each contraction held 10 seconds, at each exercise session. For the first week, they should perform the exercises only every other day to reduce the likelihood of muscle soreness. They should perform 2 sets of 10 repetitions, one in the morning and one in the evening, for the first two exercise days, then 3 sets (morning, late afternoon, and evening) on the next two exercise days. Instruct clients to work gradually on increasing reps and holding time-perhaps starting with 3 repetitions, held as long as possible, then alternating between adding to the number of reps and increasing the holding time. Once they can hold a full contraction in both prone position and in extension, they should do the exercises 10 times twice per day for two days followed by 10 reps three times per day for two days. They should take a full day's rest after each four-day cycle. They should follow the sequence of 2 sets/ day for two days, then 3 sets/day for two days, followed by one day of rest, for each progression until they can consistently perform 10 reps at each session, holding each rep for 10 seconds. continued
Posture
.
149
Gluteus Maximus Inner-Range Exercise, continued
Although this kind of inner-range exercise may shorten the previously lengthened rectus abdominis and gluteus maxim us, excessive pelvic tilt will be corrected only if the tight hip flexors are stretched to release the pull on the pelvis through the iliacus muscle. Tightness of the hip flexors (if due to increased muscle tone rather than to adaptive shortening of connective tissue) inhibits the activity of the hip extensors through a process called pseudoparesis Oanda 1986). When this is the case, an individual must reduce muscle tone in the hip flexors before engaging in exercises to strengthen the hip extensors. The Thomas test (page 114) can show if the hip flexors are tight and whether the rectus femoris or iliopsoas is the tighter muscle. You also can prescribe the Thomas test for initial stretching of the hip flexors, later using the half lunge to combine lumbar stability with hip flexor stretching.
Half Lunge (without chair-see .I{el".
To stretch
page 114)
the hip flexors while maintaining
back stability.
Instruct your clients to assume a half-kneeling position and to tighten their abdominal muscles (using a hollowing action) to stabilize the pelvis. From this position, they should press the pelvis forward to force the trailing hip into extension. Providing the pelvis is not allowed to anteriorly tilt, the hip flexors will be stretched. Prescribe twice-daily exercise for four days, 10 repetitions per session, holding the position 20-30 seconds for each repetition. Instruct your clients to rest for a day, then repeat the four-day cycle until they have gained the desired range of motion, or until range improvement has stopped. The long-term maintenance exercise schedule should be 10 repetitions, three times per week. A chair may be useful for the client to hold (page 114) if they find the balance of this exercise difficult.
Back Flattening .1{e7.:.'. Stretches hip flexors and strengthens/builds the abdominal muscles, while re-educating
endurance in posture control.
Once an individual has corrected the muscle imbalance of the lordotic posture, he should practice assuming optimal posture. A back flattening exercise can help. Have your client stand with his back flat against a wall and his feet 6 inches (15 cm) from the wall. He should then tighten continued
150
.
Back Stability
Back Flattening,
continued
the abdominal muscles and gluteals in order to posteriorly tilt the pelvis, while his legs remain fully extended. The posterior pelvic tilting will effectively stretch the hip flexors. He can gradually increase the holding time, starting at 3-5seconds and building to 30-60 seconds, breathing normally Tighten throughout the exercise. Prescribe exercises abdominals i .' twice daily for 10 repetitions, with each , repetition held 5 seconds, and a rest day Streichtight ~ hipflexors taken after every four exercise days. \, Strengthening the abdominal muscles is , , not sufficient to correct a lordotic posture. Unless a person modifies hip flexor tightness and corrects abnormal lengthening of abdominal muscles, abdominal strength changes will have little effect on pelvic tilt or lumbar lordosis. Walker et al. (1987) and Levine et al. (1997) both examined the effects of abdominal strengthening alone and found no changes in postural variables.
t
I
Swayback In the swayback or "slouched" posture, the pelvis remains level, but the hip joint is pushed forward, the greater trochanter lying anterior to the LOG. Whereas in normal posture the sternum is the most anterior structure, now the pelvis has shifted and become the more anterior body segment, with the LOG moving from the ankle to the midfoot and toes (see figure 7.7b, page 145). The hip is effectively extended, lengthening the hip flexors, and the body "hangs" on the hip ligaments and anterior hip structures. The lordosis now changes shape from an even curve to a deeper, shorter curve with a prominent crease normally at L3 level. The kyphosis is now longer and may extend into the lumbar spine. The lower lumbar region is flatter than normal, and the pelvis may be minimally posteriorly tilted. A person with this posture will often be able to point to the exact point of pain, which normally occurs after prolonged standing. Swayback is common in youth and is the most common posture in young (18-28 years) athletes (Norris and Berry 1998). The rectus abdominis remains relatively unchanged in the swayback posture because the pubic bone and lower ribs in general retain their anatomical relationship. However, due to the direction of the fibers of the oblique abdomina Is, the external oblique is lengthened and the internal oblique unchanged or shortened (figure 7.8); in the latter case, it is the upper fibers that are affected (Kendall et al. 1993).
Posture
. 151
The swayback posture may be combined with dominance of one leg in standing ("hanging on the hip"), especially in adolescents. In this case, weakness in the gluteus medius allows the pelvis to tip laterally, a situation partially compensated by increased tone in the tensor fasciae latae. Shortening is seen in the iliotibial band (ITB), with a prominent groove apparent on the lateral aspect of the thigh, as the tight fascial band pulls on the skin. You can assess tightness in the ITB using the Ober test (see page 108), which you may also use to Figure 7.8 Changing length of the stretch the tight muscle. Assess the oblique abdominals in swayback ability of the gluteus medius to mainposture. tain pelvic stability in single-leg standing by using the Trendelenburg sign test (see page 73). Page 105 shows the inner-range holding test position of this muscle in side lying. Correction of swayback relies on two essential points of the posture type: the pelvis is the most anteriorly placed structure instead of the sternum, and the posture results in height loss. To correct the posture, you must help your client change the relative alignment of chest and pelvis.
Correction of Swayback Posture .f{'1~'.
For re-education of body segment positioning.
Have your client stand with his pelvis against the top of a table; from this position he presses his chest forward, shifting it as a single segment and avoiding any spinal flexion. At the same time, he performs abdominal hollowing to reeducate the flat abdomen alignment. If you have observed single-leg dominance with the swayback posture, help your client correct it by stretching the adductor muscle group pn the tight side, and enhancing the endurance of the abductors (gluteus medius) on the lax side. Symmetry between the two legs is essential. Use the Ober test (page 108) on both legs to determine the length of the hip abductors. continued
152
. Back Stability
Correction of Swayback Posture, continued
Determine hip adductor length by passively stretching your client's straightened leg into an abducted position, with a total of 900 hip abduction (450 on each leg) being desirable. You can use the following two exercises both to assess the range of hip abduction and to develop it. The first assesses tightness in only the short adductors inserting above the knee (adductor longus, adductor brevis, adductor magnus) because the knee is allowed to bend. The second targets the long adductor inserting below the knee (gracilis) by keeping the knee straight throughout the stretch.
Sitting Bilateral Hip Adductor Stretch .f{t1~,.. To stretch the hip adductors, excluding the gracilis. Have your client sit on the floor on a folded towel (2 inches thick), her back supported against a wall. She should place the soles of her feet together, grip the feet, and press down on her knees using her elbows, holding the full stretch for 5-10 seconds while maintaining back alignment. A desirable range of motion is for the knees to fall to within 3-4 inches of the floor. Prescribe 10 repetitions daily.
Sitting .f'lt1~,..
Wide Splits To stretch all the hip adductor
muscles.
Have your client sit on the floor in an upright posture with her arms behind her, hands on the floor to stop her from leaning back too far, legs straight. The body should be as vertical as possible. Instruct her to abduct her legs as far as possible, allowing the pelvis to posteriorly tilt. This posterior tilt will take the stretch off the adductors slightly, enabling the subject to get into the position comfortably. Then, she can increase the stretch by maintaining the position of the feet and pressing the hands against the floor to lengthen the trunk (the instructor can use the instruction "grow taller" or "try to reach your head up to continued
Posture.
153
Sitting Wide Splits. continued
the ceiling"). As this occurs, the subject attempts to anteriorly tilt the pelvis which will move the pubic bone (the upper insertion of the adductor muscles) backwards and so increase the stretch. A desirable range of motion is a total of 90° hip abduction between both legs. She should hold the full stretch for 5-10 seconds. Prescribe 10 repetitions daily. Because swayback posture is common in youth, but not associated with marked muscle tightening or weakening, it is difficult to correct. The emphasis is on re-education, with postural awareness playing an important part in the process. You can increase postural awareness by the use of proprioception during the spinal lengthening exercise below.
Spinal Lengthening .f{l1~'.
To improve awareness of body position.
Your client needs a partner for this exercise. As your client stands in his normal resting posture, his partner places a hand 1-2 inches (2.5-5.0 cm) above the crown of the client's head. Instruct your client to lengthen his spine (the instruction is to" grow taller"), attempting to touch his partner's hand with the top of his head. He must not look up (cervical extension) in an attempt to lengthen his neck, and must not stand on his toes! Once he has mastered this action, he should attempt the same lengthening action without the help of a partner. The action is again to "grow taller." Placing a light book or beanbag on the head helps to give sensory feedback and can help him focus his attention on moving the top of his head upward. Initially he practices simple lengthening at whatever speed is comfortable, with the beanbag on the head. Eventually he should slow the lengthening action, attempting to hold the lengthened position for 5-10 seconds while breathing normally (some people take a deep breath and hold it-this must not be allowed, as it can lead to lightheadedness). The lengthened position should be relatively relaxed and not stiff-comparisons with a puppet rather than a wooden stick can illustrate the difference between stability (spine lengthened and continued
154
.
Back Stability
Spinal Lengthening, continued
aligned) and rigidity (spine fixed). When your client is able to perform the movement and hold the corrected body position, he can progress to walking while holding the lengthened position, and then to simple activities such as sitting/standing from a chair to increase the variety of movements. In order to provide sensory feedback when the swayback posture is incorrectly stretching the muscle, try applying nonelastictape on the skin over the external oblique, taking up any skin slack. Attach the tape to the lower lateral aspect of the abdomen, out toward the anterior rim of the pelvis. Pull the tape tight from this point up to the posterolateral aspect of the lower ribs. Although the tape is not strong enough to prevent the pelvis from moving forward in relation to the rib cage, it will remind your client when this is happening and encourage him to correct the posture. The more times he makes the correction, the more likely it is that optimal postural alignment will become automatic. Either a physical therapist or athletic trainer should apply the tape, and it should be done immediately following the spinal lengthening exercise above, to encourage maintaining correct alignment between exercise bouts. Another way to reinforce automatic alignment is to build correction into daily activities. Encourage your client to perform the pelvis-chest realignment exercise regularly throughout the day. Office workers, for example, can perform the exercise whenever the telephone rings, and students can perform it each time a bell rings to end class. If the iliopsoas is lengthened by the extended position of the hip (the Thomas test will reveal this; see chapter 5) its inner-range holding must be redeveloped.
Sitting, Hip Flexor Shortening .f{"~'.
To shorten the iliopsoas and rectus femoris muscles and build their endurance. While your client is sitting, you should passively flex the hip to the maximum degree possible without pain-or to approximately 110°, or to the point where the pelvis just begins to posteriorly rotate. Instruct your client to hold this position for 10 seconds, while maintaining a continued
Posture
.
155
Sitting, Hip Flexor Shortening, continued
neutral lordosis. Inability to hold at full inner range for 10 repetitions (10 seconds each) is a sign of postural lengthening. If the iliopsoas is lengthened, the leg may drop and/or the pelvis drop back into posterior tilt, moving the iliopsoas into its lengthened position. Your client can redevelop inner-range holding of the iliopsoas by using first eccentric and then isometric inner-range hip flexor exercises while maintaining a neutral lordosis. In the preceding exercise position, your client should try to lift her leg to full flexion. Then you should try to lift the leg farther (increasing hip flexion), without altering the position of the spine or pelvis. Remember that a lengthened muscle cannot contract powerfully to pull a limb into its fully closed (inner-range) position. If your client's hip flexors are lengthened, further passive movement will be possible because she will not have been able to pull her own leg into full inner range. Have her attempt to hold this new (passive) inner-range position. If she is able to do so, instruct her to build up holding time from 1-2 seconds to 10 seconds while performing the exercise daily for two weeks-her target is 10 repetitions of the 10-second hold. If your client is not able to hold the passive inner-range position, she should use controlled lowering (eccentric). From the passive inner-range position, she attempts to slow the descent of the leg after you release it from its fully flexed position. She should continue the controlled lowering until she can slow the descent sufficiently to hold the leg still. She then progresses to holding at reducing joint angles. For example, assume that the active inner-range position (with your client using her own muscles) is 90° hip flexion, and the passive inner-range position (as you lift the leg farther into flexion) is 120°. The target for active flexion! holding is about 110°.You lift her leg to 120° hip flexion and release the leg. She then controls the lowering back to the 90° starting position. Once she can do this consistently, you lift her leg to 90-100° and she attempts to hold it. Once she can hold this position, you repeat the exercise, beginning again with the 110-120° passive flexion. She should perform each holding or lowering exercise only five times before taking a rest period since the muscle fatigues quickly with this exercise and alignment will be lost. Prescribe 3 sets of 5 repetitions twice daily for four days (a family member can provide the passive flexion), followed by a single day of rest, then another five-day cycle, and so on. The goal is the ability to actively flex the leg to 110° and hold it for 10 seconds for each exercise set.
156
.
Back Stability
Flatback With the flatback posture, the main problem is lack of mobility in the lumbar spine and a flattening of the lordosis (lumbar flexion). This posture reflects the extension dysfunction described by McKenzie (1981) and is common in chronic low back pain after extended periods of inactivity. The pelvis may be posteriorly tilted in comparison to the reference line, and the lumbar tissues are often thickened and immobile. The flatback posture is also seen in subjects who practice a high number of sit-up type exercises (repeated lumbar flexion). In this case the lumbar spine may be mobile-but the rectus abdominis is strong and tight, and is by far the dominant member of the abdominal muscle group. Flatback is corrected by regaining appropriate mobility in the lumbar spine through passive and active extension movements.
Passive
.'{If.'.
Back Extension in Lying Position
To improve spine.
the passive
range of extension
in the lumbar
Performed in the lying position, extension exercises first mobilize the upper lumbar levels, a with proportionally less caudal movement (McKenzie 1981). Instruct your client to lie prone on the lab table (or floor), with his hands by his shoulders in a pushb up position (a). He should extend his arms while keeping his pelvis on the table, thereby forcing extension of the spine (b). Initially, some people may need to push up only with their forearms on the table, gradually building up to full arm extension. To emphasize the motion of the spine rather than the pelvis, try fixing the pelvis to the table with a webbing belt. If your client experiences any pain in the lumbar region during this exercise, refer him to a physical therapist (PT). Often, instead of the whole '. lumbar spine being stiff to extension, one or two vertebrae may be stiffer than others. These stiff units require a specific manual therapy techcontinued
Posture
.
157
Passive Back Extension in Lying Position, continued
nique of "joint mobilization" either before or during the exercise program. When a specific stiff area has started to move (the PT will assess this), you can move the webbing belt up or down within the lumbar region to form a fulcrum around which the movement occurs. In this way, the extension action is focused more exactly on a single lumbar joint. See that your clients practice the passive extension movement often, but for only a short time each session, to allow the movement to develop without causing too much reactionary pain. Suggest 10 repetitions every two hours throughout the waking day, with a full day's rest after every four days. The exercise should continue until the individual has achieved the desired movement range.
Pelvic Tilt Re-Education, Sitting .f{t7~,. To regain both range and quality of movement in the lumbar spine. If the lower lumbar spine has reduced extension, the pelvic tilting action may be effective in correcting it. Instruct your client to sit on a low stool with his feet on the ground. Keeping his shoulders still, he should try to tilt his pelvis forward and down. Tell him to think of his pelvis as a bowl full of water, and that by tilting the bowl he can pour the water onto the ground between his feet. He should try to bring the backside of the bowl up as he pushes the front of it down, always keeping his shoulders still and his sternum up. When the motion is especially poor, provide passive assistance. Wrap a webbing belt around your client's waist and, fixing the sternum, pull the lumbar spine into extension as he attempts to tilt his pelvis (see page 75, "Assisted Pelvic Tilting While Sitting"). Refer to chapter 4 for a fuller discussion of pelvic tilt.
Kyphotic
Back
In the kyphotic posture, the shoulder joint moves anteriorly to the posture line, increasing the thoracic kyphosis. In optimal upper body alignment
158
. Back Stability
(table 7.3), the scapulae should be approximately the width of three fingers from the spine, and the medial borders of the scapulae should be vertical. Assess optimal positioning of the shoulder by comparing the head of the humerus in relation to the acromion process. In optimal positioning, no more that one-third of the humeral head should be anterior to the point of the acromion. The humerus should be held with the cubital fossa (elbow crease) at 45° to the sagittal plane in relaxed standing. A smaller angle indicates excessive medial rotation, indicating tightness in the medial rotators (especially the pectoralis major) and lengthening of the lateral rotators. Visualizing how this would appear from above may be helpful. When the arm is held in medial rotation, the crease of the elbow is orientated more forward and inward; when lateral rotation is greater than normal, the elbow crease faces farther outward. Deviation from the ideal is often described as a "round-shouldered" posture, a blanket term that covers a number of scenarios. TIghtness in the anterior structures pulls the shoulder forward, away from the posture line. The weight of the arm moves farther from the upper body's center of gravity, dramatically increasing the leverage forces transmitted to the thorax. Eventually, thoracic kyphosis increases. Tightness in the pectoralis minor pulls on the coracoid process, tilting the scapula forward (figure 7.9a). Tightness in the pectoralis major causes both excessive medial rotation at the glenohumeral joint and anterior displacement of the humeral head (figure 7.9b). Lengthening of the lower trapezius and serratus anterior may cause excessive abduction (figure 7.9c) and downward rotation (figure 7.9d) of the scapula. Excessive elevation (figure 7.ge) and upward rotation may result from tightness in the upper fibers of the trapezius. Correction of kyphotic posture depends on flexibility of the thoracic spine. Where the kyphosis appears fixed and thoracic motion is grossly reduced, thoracic joint mobilization is required as a first step. Once some mobility has been gained passively by manual therapy, you can use exerTable 7.3
Correct Alignment of the Shoulder Girdle
From behind
. .
Medial border of scapula vertical
Medial border of scapula no more than three finger breadths from the spinous processes Spine of scapular T3/T4 level,
. inferior angle at T7
. Scapula flat against thoracic wall
From the side Line from ear canal to center of shoulder joint is perpendicular to floor No more than one-third of head of humerus anterior to acromion
. .
. Humerus held with elbow crease 45° to sagittal plane
Posture
I
I
I
I
I
I
I I
a
I
I
,I
.
159
,, , ,,, ,, ,, ,, ,
,, ,, ,, ' e Figure 7.9 Postural changes
around the shoulder.
cise therapy to maintain the newly gained motion. The stemallift action (page 162) is the exercise of choice. If the subject is younger and the thoracic spine is mobile, only scapular repositioning is required.
Thoracic Joint Mobilization 1Jf['1~'. To increase mobility of thoracic joints, using manual therapy, in preparation for exercise therapy. With your client in the prone lying position, work with a PT to use posterior-anterior vertebral pressures (PAVP) or gross extension pressures to isolate the thoracic spine. With your client sitting, you can combine mobilization with overpressure. Have her sit facing a treatment table, with her arms folded and placed on the table. As you press the thoracic spine into extension, instruct her to try to follow the action. If thoracic mobility is quite limited, at first you will simply press the spine passively into extension. As your client gains mobility, encourage her to follow your motion with her own active movement while you gradually reduce the pressure you apply. The first step in this active process is for the subject to be able to "feel" the movement. Many people with a kyphotic posture have a poor ability to control the quality of motion in the thoracic spine, and this type of guided exercise can help them improve their control. If your client is still unable to perform active thoracic extension even after regaining passive extension, suggest a visualization technique: encourage her to imagine herself performing the action. continued
160
. Back Stability
Thoracic Joint Mobilization, continued
Either you or a model should perform the action correctly. You can also use video to enable your client to see the action from behind, while a mirror provides a view from the front. Then have her repeat her attempt at active thoracic extension. She may need to cycle through a series of visualization sessions, passive extension, and attempts at active extension before she can finally sense what active extension feels like. Once that happens, she can proceed to daily exercises. The subject should perform the exercise daily for 10-15 repetitions. In the early stages as mobility is very poor, some soreness can be expected following the exercise, so a greater number of repetitions should not be performed.
Scapula Repositioning .fl:I1.'. To improve control of scapular retraction and depression. If the thoracic spine is mobile, you can correct kyphotic posture by repositioning the scapulae-shortening the shoulder retractors and enhancing the scapular stabilizers (especially lower trapezius and serratus anterior). The aim here is to improve control of movement rather than simply to increase strength. By improving strength, muscle endurance, and movement quality (coordination and timing), these exercises differ from many traditional weight-training programs whose primary aims are gains in strength and muscle size. With your client lying prone, passively place his scapula into optimal alignment-the medial borders vertical, three finger widths from the spine. The scapula should be firmly anchored to the thorax (by action of the serratus anterior and lower trapezius muscles) rather than being separated from the rib cage. Frequently this involves passively depressing and adducting the scapula, but the amount of passive movement of the scapula that is required depends on the postural alignment of the subject. More movement is needed in subjects who have grossly abducted scapulae (medial border of scapula 5-6 inches [13-15 em] from the spine) than for those with minimal abduction (medial border 3-4 inches [8-10 em] from the spine) (Mottram 1997; Norris 1998). Initially, encourage your client to hold the new position for 1-2 seconds. Often the tendency is for the subject to "brace" the shoulders back continued
Posture
.
161
Scapula Repositioning, continued
hard. Discourage this reaction since it requires maximal muscle activity. Encourage your client to "let go" until the scapula just begins to move away from the corrected position, and then to hold the muscles slightly tight. Progressively increase the amount of time that this position is held with minimal muscle work, from 1-2 to 3-4 and eventually 10 seconds. The aim is to build up to 10 reps, holding each for 10 seconds, with the minimal amount of scapular muscle work that is required to maintain good scapular alignment. Tight anterior structures must be stretched to allow the shoulders to retract fully. Check for tightness in the pectoralis major and pectoralis minor, and if necessary prescribe stretching exercises as detailed in the following sections.
Door Frame Stretch .flI1~'" Stretch pectoralis major muscles. Instruct your client to lean forward onto a doorframe, his arms horizontal, his forearms vertical against the frame. He then pushes his arms back into extension by leaning into the doorway opening, holding the position for 20 seconds. Have your client do this exercise 3 times a day, with 2 repetitions each time.
Weight .fllm..
Bag Passive Stretch pectoralis
Stretch minor muscles.
A tight pectoralis minor can pull the scapula down and forward. Have your client lie in a supine position. Place a 3- to 5-lb weight bag over the anterior aspect of her shoulder. She should relax and allow the bag to press the shoulder back into position for 30 seconds. The weight bag continued
162
.
Back Stability
Weight Bag Passive Stretch, continued
will help press the shoulder back into retraction, passively stretching the anterior structures. To use a contractrelax technique, the client presses the shoulder into protraction for 2 seconds, trying to lift the weight bag, and then relaxes for 5-10 seconds, allowing the weight bag to press the shoulder farther back. Astatic stretch may also be used with the client simply lying relaxed, allowing the weight bag to press her shoulders back.
Sternal Lift Exercise .I'!"~'.
Combines thoracic extension and scapular repositioning.
While sitting, your client should lift his sternum using thoracic extension (rather than simply taking a deep breath) (a). At the same time, he should draw the scapulae down and in toward their optimal alignment. He may prefer to perform the action against a wall, where the movement should be one of "rolling" the thoracic spine up the wall while keeping the lumbar spine stable and avoiding any increase in the depth of the lumbar lordosis (b). b a If the client's lumbar spine stability is particularly poor and he. is unable to avoid hyperflexion, modify the starting position by having him sit on a bench, with his feet on a chair to bring the femur above the horizontal. This position posteriorly tilts the pelvis and flattens or reverses the lumbar lordosis.
Posture
. 163
SUMMARY
· · ·· ·
Posture is the arrangement of body parts in a state of balance that protects the supporting structures of the body against injury or progressive deformity. Postural sway consists of a small continuous motion in the sagittal plane-an oscillation of the center of gravity that may reduce lowerlimb fatigue and aid blood flow.
·
Excessive postural sway generally reveals poor balance and stability. You can assess clients' postures by use of a plumb line or a posture grid. There are four basic types of abnormal posture: 1. Lordotic posture is characterized by excessive anterior pelvic tilt. 2. Swayback is characterized by anterior displacement of the pelvis. 3. Flatback is characterized by slight posterior pelvic tilting and loss of lumbar lordosis. 4. Kyphosis is characterized by excessive thoracic curve. This chapter describes how to assess different abnormal posture types and presents exercises that can help correct them.
PART
nnn
BuildinL Back Fitness If you bring a client all the way through the assessments and exercises in the previous chapters, he or she should have a basically stable back, with no pain. Some clients need more, however-namely, those whose demands in the workplace or in sport activities require extraordinary strength, speed, or accuracy of movement. Chapter 8 ("Advanced Stability Training") presents exercises that will build on the training already achieved, using body movements alone, using balance boards, using stability balls, or employing proprioceptive training to increase accuracy of muscle control. Chapter 9 ("More Advanced Stability Training: Weight Training and Plyometrics") is for those clients who need the most rigorous training possible for their backs because of extremely heavy sport/workplace demands. Please note: the approaches used in chapters 8 and 9 are specifically for people who have had lowerback problems and/ or who need to prevent such problems in the future. Study the chapters with that in mind-the material does NOT merely restate what you've read before about weight training, etc. Because these chapters approach advanced training from the viewpoint of increasing your client's back stability, and not simply with the idea of building pretty muscles or increasing overall strength, they will be invaluable to your clients who have major concerns about their backs.
165
~ Advanced Stabilig Training Atter your clients have used the procedures and exercises of previous chapters to achieve basic back stability, they are ready (if they wish) to build on that stability. By now they should have learned to control pelvic tilt; to automatically assume the neutral position; to maintain abdominal hollowing (at 30-40% of the maximum effort); and to contract the multifidus at will-or, in quantitative terms, to perform the basic procedures in chapter 4 with variable intensity for 10 repetitions, holding each repetition for 10 seconds. With your help, they should have begun correcting muscle imbalances using the approaches in chapter 5. They should have developed their abdominal strength using the exercises in chapter 6. They should be able to maintain proper posture as described in chapter 7. Many people-who are relatively sedentary and whose back stability is rarely challenged through workplace or leisure-time activities-may have little motivation to proceed with additional training. Others will want to go further, however, especially if they are involved in sports or if they face heavy physical demands on the job. In this chapter, I cover exercises for developing even greater back stability. Chapter 9 goes further still, but your clients should master the material in this chapter before moving to the very strenuous work in that chapter. The first class of exercises in this chapter simply adds layers of complexity onto movements your clients will already know from other chapters. But there is also an entire series of exercises using a stability ball (or "gym ball"), which was introduced briefly in chapter 4-many people find these exercises more "user friendly" for their home workouts. Finally, I cover a small core of proprioceptive exercises-training that is advanced beyond what your clients have seen thus far, and that provides a kind of transition between some of the later exercises in the first section and the plyometric exercises in chapter 9.
167
168
. Back Stability
Very important: for each of the exercises in this chapter, your clients should gently contract their deep abdominal muscles to perform abdominal hollowing and maintain this contraction throughout the exercise. By now, moreover, they should be able to voluntarily contract the multifidus muscles--especially if they began the program as sufferers from chronic low back pain. They should begin all exercises in the neutral position.
SUPERIMPOSED LIMB MOVEMENTS AND BALANCE BOARDS Each of the following exercises involves limb movements that are superimposed on a basically stable back that the exercises of chapter 4 can create (Le., in these exercises an individual tightens the back stability muscles and then moves the limbs upon the stable base). As your clients focus their attention on limb movements, they will become more able to control their back stability muscles without conscious thought. This kind of automatic response occurs only with long repetition of the exercises. You should find it surprisingly easy to observe the point at which your clients are exerting automatic control. If they perform a limb-loading exercise such as the standing single-leg raise or the crook lying heel slide, for example, movement of the pelvis will reveal lack of back stability. In this case, you would retreat a couple of steps and have your clients practice the hollowing actions to enhance their ability to stabilize the spine. Once they have built up endurance of these muscles and can hold the abdominal contraction for 10 repetitions of 10 seconds each, you would once again try adding limb movements to the basic exercises. If they can now successfully control limb movements while avoiding unwanted pelvic movement (maintaining the lumbar spine's neutral position throughout the action), you will know that they are gaining automatic control of the stabilizing muscles-they no longer have to focus their attention on these muscles and can now concentrate on accurate positioning of the limb. For each of the following exercises, your client should progress in a single session only to the point at which he can no longer maintain neutral position, correct pelvic tilt, or maintain abdominal hollowing. Have him do the exercise daily for four days, rest one day, then resume the pattern, gradually increasing the progression or the number of repetitions until he eventually can do the exercise in its most challenging form for 10 reps, holding (where appropriate) for 10 seconds each time. Obvi-
Advanced Stability Training
.
169
ously, all one-sided movements should be performed on both right and left sides, one being the mirror image of the other. Each exercise should be performed in a slow, controlled fashion, maintaining the neutral position of the spine throughout the exercise. Since limb leverage changes when arms/legs are bent and straightened, your clients will necessarily have to vary the amount of abdominal work they use to maintain the neutral position. It is this variation that makes the difference (in terms of skill) between the holding exercises, such as abdominal hollowing, and these more advanced exercises that involve limb movements upon the stable trunk base.
Determining the Starting Position An individual's starting position depends on his physical characteristics and abilities. You should always be open, moreover, to changing the starting position if you perceive that your first choice may not have been the best-which will be the case if your client is not succeeding with an exercise. Some exercises are easier than others because they involve less muscle work. For example, in the heel slide movement, the ground partially takes the weight of the leg, while in the single-leg raise, the subject lifts the whole of the leg weight. The former exercise is therefore easier in terms of pure muscle work. Some movements may be more comfortable for certain subjects. Since lying positions are more supported than kneeling, for example, many people feel more secure in lying. The program generally follows a neurodevelopmental progression (Le., the sequence that children go through when they learn to sit, stand, and walk). In the present case, we go from ground support, to apparatus support, and finally to increasingly complex free exercises.
Exercises in the Crook Lying Position The crook lying position, which was used to perform abdominal hollowing and pelvic tilting, is a good starting position for superimposed limb movements. As an individual straightens the leg or lowers it to the ground, the overload placed on the trunk becomes progressively greater-the individual must therefore vary the intensity of muscular stabilization to maintain the neutral position. This variation in muscle contraction intensity increases the person's cOlltrolrather than simply strength or endurance capacity.
170
. Back Stability
Heel Slide-the
Basic Movement
.1'{17.'. To place minimal, but progressive,
limb loading on the trunk.
Instruct your client to slowly straighten one leg, with the heel resting on the ground. This movement is easier if the heel is on a slippery surface (a cloth if on a polished floor, or a piece of shiny paper if on carpet). The moment the pelvis anteriorly tilts and the lordosis increases, the movement must stop and the leg be drawn back into flexion once more.
Leg Lowering .1'{17.'. Limb loading as a progression from the heel slide. Instruct your client to flex both her hips to 90° so that her thighs are vertical to the ground, while keeping her knees relaxed. She should then slowly extend one hip until her foot touches the ground. Have her gradually extend the knee farther in subsequent repetitions, so that the foot touches the ground farther from the buttock, increasing the limb leverage and therefore progressing the resistance. The exercise is performed daily for four days and then a single day's rest is taken. She should continue this sequence until she can perform the exercise with the leg almost straight. Once she can perform the exercise with the leg almost straight, she can progress to single-leg raises.
Advanced Stability Training.
171
Single Bent-Leg Raises .f{"~'.
Progression from leg lowering.
Beginning in the crook lying position, your client should lift one leg-still bent at the knee-while the other rests on the floor. He brings the knee up as far as he can without moving out of neutral position, then lowers it. Then he repeats with the other leg. As a progression on this action, have him begin lifting one leg just before the other limb has touched the ground so that momentarily they are both off the floor at the same time. Finally, he should lift and lower both legs together, initially with minimal limb leverage (Le., with knees well bent) and finally with increasing leverage (legs increasingly straightened). The maximum leverage will vary with each individual. For most well-conditioned individuals, 90-120"knee extension is appropriate. At no time should the pelvis anteriorly tilt, and at no time should the abdominal muscles be allowed to bowstring (bulge outward rather than maintain a flat or hollow contour). I do not recommend progressing all the way to bilateral straight-leg raises-the compression and shear forces imposed by the psoas muscle upon the lumbar spine make this unsuitable for use in rehabilitation following low back pain.
. maintained
The neutral position of the lumbar spine must be throughout the exercises. If the pelvis tilts and neutral position is lost, the exercise must be stopped, and the client should revert to an earlier stage of the exercise in which the pelvic tilt was accurately controlled. Be certain also that your clients keep their abdomens hollowed throughout the exercises.
KEY POINT: I
Prone Lying Gluteal Brace .1'['7~'. Co-contraction of trunk stabilizers with gluteals. Instruct your client to lie prone, then to dorsiflex one foot, with the toes bent up toward the knee. She should then slightly flex both her knee (about 10°) and her hip (also about 10°). She then contracts her gluteal muscles to lift the femur into extension to the horizontal position (with the foot remaining on the ground), straightening the knee.
~~
172
.
Back Stability
Prone
Bent-Leg
Lift
.I'{,,~,. Active movement of an unsupported leg on the stable trunk. In the prone lying position, your client should flex one leg to 90° at the knee. Instruct your client to set her abdominal muscles and contract the gluteals to lift the leg from the floor. To prevent passive anterior pelvic tilt, the maximum hip extension should be only 15°. This position places the hamstring muscles at a mechanical disadvantage, reducing the tension they can create and therefore throwing greater stress onto the gluteals. To increase the isolation of the gluteals from the hamstrings, have your client slowly flex her knee while maintaining hip extensionthis causes the gluteals to act isometrically as hip stabilizers while the hamstrings acts isotonically as prime knee flexors.
Bridge
From
.I'{"~'. Using
Crook
Lying
leg power to lift the trunk while maintaining
neutral lumbar position.
a
In a crook lying position, your client should tighten his gluteal muscles and then lift his pelvis from the ground, aiming to form a straight line from shoulders to hips and then to the knees. This exercise tends to induce movement in the sagittal plane (anterior-posterior pelvic tilt, and/ or lumbar flexion-extension). Lifting one leg (see next exercise) imposes an additional rotary stress, tending to cause movement within the transverse plane.
Advanced Stability Training
.
173
Bridge With Leg Lift .I'{IJ~'. A progression from bridge from crook lying. Instruct your client to assume the bridge position, starting from lying. Then he lifts one leg, avoiding the tendency for the pelvis toward the unsupported side. Placing a stick across the anterior rior iliac spines of the pelvis gives useful feedback for keeping the level.
crook to fall supepelvis
Exercises in 4.Point Kneeling Position The 4-point kneeling position is initially stable since four symmetrical points (both hands and both knees) bear the weight. As one arm or one leg is lifted to reduce support to three points, the body is less stable and the stability muscles must now work harder to maintain trunk alignment and stop the body from tipping.
Four-Point
Body Sway
.I'{IJ.,. Learning to maintain neutral position as the limbs are moved. Instruct your client, who begins in the standard 4-point position, to sway the body forward and back, moving at the shoulders and hips only. As she passes the critical point of 90° hip flexion, be sure that her lumbar spine remains in its neutral position. As soon as she begins to lose the neutral lumbar position, she should reverse the movement back into full 4-point kneeling. The aim is to gradually work farther and farther back (increasing hip flexion) while maintaining a neutral spine.
174
.
Back Stability
Four-Point Pelvic Shift .f'[11.'. Learning to unload the limbs prior to lifting them. After assuming the 4-point position, your client should shift to the side to take the weight of the far leg. She then barely lifts the leg on this side from the supporting surface, leaving only one knee in contact with the ground. Be sure that she lifts the leg a maximum of 1-2 inches (2.5-5.0em). Some people find the subtlety of this movement difficult and tend to lift the leg by 6-8 inches (15-20cm)-but this imposes an unwanted rotation on the spine and must be discouraged. Placing a stick across the upper pelvis (level with the posterior superior iliac spines) is helpful. With the required subtle movement, the stick will stay in place. If the leg is lifted too far, however, pelvic rotation will cause the stick to fall.
Four-Point Leg Flexion/Extension .f'[I1.,. Controlling back stability in the presence of limb movement. Your client should begin as for the previous exercise, shifting weight to one leg. Instruct him to move the unloaded leg into flexion! extension and abduction! adduction, while maintaining a neutral lumbar spine and keeping the lower leg parallel to the floor. He should use only small movements, the knee moving forward/backward and side to side by only 2-3 inches (5-8 em). Larger movements will require greater changes in pelvic tilt and are more difficult to control. The movements should be slow to avoid excessive limb momentum-no more than 1 or 2 complete limb movements per second.
Four-Point Kneeling Leg Lift .1'111.'. Maintainingstability movement.
during increasing
complexities
of leg
From the basic 4-point kneeling position, your client should extend one leg completely, keeping the foot on the ground (a). The next step is to lift the leg until it is parallel to the floor (b). Finally, instruct him to alternately flex and extend the raised leg at the knee, keeping the raised thigh continued
Advanced Stability Training.
175
Four-PointKneeling Leg Lift. continued
parallel to the floor. The foot should remain in a middle (neutral) position, toes and foot neither fully pointed (plantarflexed) nor fully pulled up (dorsiflexed)-holding the shin or calf muscles tight can cause muscle cramping. a Several alignment faults are common in this final movement. First, while your client is focusing on the limb movement, he may forget to maintain contraction of the trunk stabilizing muscles-leading b the abdominal wall to bulge because the hollowing action is lost. As this happens, the pelvis may anteriorly tilt, pulling the lumbar spine into excessive extension (back hollowing). Finally, if the gluteals have poor endurance, the client may start to rely on his hamstrings to maintain the extended hip position: as the hamstrings begin to flex the knee, he loses the hip extension position and the leg drops below the horizontal. In each case, you should stop the procedure and return to the previous exercise.
Four-Point Kneeling Arm and Leg Lift .fI.H.'ncreasing taining
back
the complexity stability.
of limb
movements
while
main-
Have your client begin as with the kneeling leg lift above. But this time, once the leg reaches the horizontal, he should also lift the diagonally opposite arm. Watch to see that his shoulder does not sag or drop down on this side; the scapula should not move as the elbow bends to unload the arm. Once your client's hand has cleared the ground, he should lift the arm forward toward the horizontal.
Exercises in the Side Lying Position We saw in chapter 7 that, in the frontal plane, the gluteus medius may lack endurance and inner-range holding ability, leading both the tensor fasciae lata/iliotibial band (TFL/ITB) and the hip adductors to tighten. In the side lying position, we are attempting to work the gluteus medius and to stretch the adductors, while maintaining stability of the pelvis and lumbar spine
176
.
Back Stability
in the frontal plane. The stability is achieved by contraction of the lateral abdominals and the quadratus lumborum acting together.Where lateral abdominal function is poor, the quadratus lumborum can become overactive and tight. Each of the following exercises overloads the quadratus lumborum and the oblique abdominal muscles on the upper side of the body. The movements must be reversed to provide a symmetrical overload.
Side Lying Knee Lift .f'll7~'" Maintaining trunk stability in the frontal (side flexion) plane during limb movement. Have your client begin the exercise in side lying, and align her pelvis so that the line joining the two anterior superior iliac spines is vertical. She must maintain this alignment throughout the exercise. Do not allow lateral movement of the pelvis. Instruct her to place the foot of her top leg on the floor in front of the shin of her lower leg. Then she should lift the top knee by abducting and externally rotating her hip, keeping the foot in place on the ground. Palpate the posterior fibers of gluteus medius above and behind the greater trochanter to make sure they are contracting. Give your client feedback until she is able to tell when she is contracting these fibers as she lifts her knee. Once she is able to feel the appropriate contraction, have her attempt to lift to full inner range, but stop her immediately if the pelvis begins to move out of alignment.
Side Lying Leg Rotation .f{e7~'" Maintaining trunk stability hip rotation. The second exer-
cise combines abduction and
trunk
ability stab il-
~
\ ~
and isolating pelvic control from
-
-
ii' ~
ity, while isolating hip movement from that of the pelvis. From the stabilized side lying position, your client should hold her upper leg straight and abduct it to the horizontal. continued
Advanced Stability Training
.
177
Side Lying Leg Rotation, continued
Tell her to then externally rotate the entire leg from the hip, turning the foot toward the ceiling and then back to pointing forward. Have your client perform 3-5 rotations before lowering the leg, unless she loses alignment of the pelvis-in which case she should lower her leg immediately.
Side Lying Leg Abduction .fl:IH.
Controlling hip abduction on a stable trunk.
The third exercise represents true abduction upon a stable base. Have your client assume the stable side lying position, then lift his upper leg into abduction while avoiding flexion and external rotation. Encourage him to "lengthen his leg" to avoid lateral pelvic movement, and then to abduct his leg as high as he can without experiencing discomfort, up to a maximum of 45° from the horizontal. All the movement should be in the hip-tell him to avoid lumbar-pelvic movement. He may have to work up gradually to the 45-degree target.
Side Lying Spine Lengthening .fl:lm.
Controlling the quadratus the oblique abdominals.
lumborum
and lateral fibers of
Side lying is also a useful starting position for strong co-contraction of the abdominal muscles with minimal compressive and shear forces on the lumbar spine (McGill 1997). Have your client lie on his left side, his thighs in line with his body but his knees flexed 90°, with his upper body supported on his left elbow to side flex the spine. He should then straighten his spine against the force of gravity, leaving the body supported on the forearm of the underneath arm and hip.
178
.
Back Stability
Side Lying Hip Lift .1{'1~'" Progression from side lying spine lengthening_ Have your client assume the position for the side lying spine lengthening. Then have him lift his hips, leaving the body supported on the forearm of the underneath arm and the knees.
Side Lying
Body Lift
.1{11~'. Final progression for developing control of quadratus lumborum and lateral fibers of oblique abdominals. Again, have your client assume the position for the side lying spine lengthening. Instruct him to straighten his knees and cross the upper leg in front of the lower leg. Then he should lift his body to the full side support position, leaving the body supported on the forearm of the underneath arm and the feet. Encourage him to "lengthen his body" and to "broaden his shoulders" to avoid their "falling" into scapular adduction-the aim being to form a straight line from the feet, through the pelvis, to the shoulders.
Exercises in the Standing Position The standing position is clearly important for the activities of daily living. The aim of the following exercises is to add limb and thoracic movements to the stable lumbar spine and to add whole spinal movements to the stable hip. You can monitor changes in the depth of lordosis by having your client lean against a wall-feet 4-6 inches (10-15 cm) forward of the
Advanced Stability Training
.
179
wall, his buttocks and scapulae on the wall-while you place the bladder of a pressure biofeedback unit between his lumbar spine and the wall.
Standing Sternal Lift .lIe1.:.'" To help correct excessive thoracic kyphosis by extending the thoracic spine in isolation. The idea of this first sequence of exercises is to teach your client to move the thoracic spine independently from the nonmoving, stable lumbar spine. Instruct your client to stand facing a table, his thighs pressed against the edge to prevent anterior shift of the pelvis into a swayback position. Have him lift the sternum up and forward, while drawing the scapulae down. Suggest that he place one hand in front of his sternum to monitor the sternal lift action. The anterior upward movement and posterior downward movement work like two guide wires pulling a wheel with its axle in the chest. The action is to flatten the thoracic curve rather than simply expand the chest or extend the lumbar spine. If your client finds it difficult to isolate the thoracic from the lumbar movement, have him try the same action while sitting-he should place his feet on a low stool to bring his knees above the level of the hips, thereby flexing the lumbar spine and reversing the lumbar lordosis. This action reduces the available extension in the lumbar spine and focuses the action to the thoracic area. After he has mastered the action in a sitting position, have him work on it while standing (see "Sternal Lift Exercise," page 162).
Pelvic Shift With Unloading .lIe1.:.'" To build isolation of leg movements on a stable base-a precursor to standing leg lifting in the frontal plane. Initially your client should stand with his side to a wall for support (gripping wall bars is also OK). As he develops skill in the movement, he should do it in a freestanding position. Instruct him to "lengthen his spine" ("grow taller"); to shift his pelvis to the left while maintaining alignment (a); then to unload the right leg by slightly flexing the knee and lifting the heel, while keeping the toe on the floor (b).
a Pelvic shift to unload leg
b Leg lift
180
.
Back Stability
Pelvic Shift With Leg Lift .r{'1~'"
To teach pelvic control and stability in single-leg standing.
Ask your client to shift her pelvis to the left, so that her body weight is over the left leg only, then slowly lift her right leg no more than 4-6 inches (10-15 em) while maintaining alignment in all three planes-there should be no posterior tilt of the pelvis, no hip drop, and no spinal rotation. Figure b (a) in "Pelvic Shift With Unloading" shows the a Lateral Anterior correct form; here, figure (a) shows lateral pelvic pelvicdip pelvic dip tilt (incorrect!); figure (b) illustrates anterior pelvic tilt (incorrect!). The action is one of pure hip flexion upon a stable back: the supporting leg supports the pelvis, and the pelvis supports the back. The knee should be raised no more than 45° from the horizontal. If your client finds the movement difficult to control, let her practice at first with her back supported by a wall. The sequence of pelvic shift, leg unloading, and knee lift are the same, but the back remains against the wall throughout the movement.
Standing Hip Abduction .r{'1~'"
Learning performing
to maintain stability
in the frontal
plane
while
hip abduction.
Your client begins by standing with her back 2-4 inches (5-10 em) from a wall. If your client loses pure abduction as the movement progresses (i.e., if she uses any flexion or extension), she will know immediately because the leg
will move closer to or farther
a
b
away from the wall. Instruct her to shift her pelvis to the right, unloading the left leg (a). Then, maintaining alignment, she should abduct the left leg by 10-20° (b). Be sure that she does not laterally tilt her pelvis or spine (c). She should gradually increase the abduction range to a maximum of 45°. Reduce the range or stop the exercise as soon as alignment is lost.
Advanced Stability Training.
Standing
181
Hip Hinge
.f{e1~'. Learning to move the spine and pelvis as a single unit on the hip. Have your client stand about 4 inches (10 cm) from a table. She may place her hands on the table only to help guide her movement, not to bear weight. Instruct her to bend from the hip, keeping her spine straight, until the spine is angled 30-45° from the vertical. It is often easier if your client focuses attention on her sacrum and imagines it moving from a b near vertical to near horizontal-tell her to "push her tail away." Once she has mastered this movement, she should do it without table support. Two kinds of feedback may be helpful. First, she can monitor pelvic tilt by placing the flat of one hand over the lower (infra umbilical) abdomen and the back of the other hand over the sacrum (a). The action is to tilt the pelvis while maintaining the relationship of the lumbar spine to the pelvis-the palm of the back hand should end up facing toward the ceiling. The second feedback method uses a long, straight stick. As your client places one hand over her sacrum and the other between her shoulder blades, she should grip the stick with both hands. She must keep her spine on the stick as she performs the hip hinge action (b). Rounding the spine (a typical error) increases pressure of the spinous processes on the stick; hollowing the spine increases the gap between the spine and the stick.
Exercises in the Sitting Position Incorrect sitting positions often cause low back pain, especially that of postural origin. But, while sitting at home or work, one can also conveniently practice the following exercises throughout the day. The first exercise uses the process of relative flexibility to overload the stabilizing system. The sitting position used in these exercises must reflect the optimal alignment of body segments. The hips should be at 70° flexion; the knees should be below the hips and slightly wider than shoulder-width apart (bringing the knees together posteriorly tilts the pelvis through soft tissue tension). About 70% of the body's weight should rest on the ischial tuberosities, 30% on the pubis. The gravity line for the upper body should pass from
182
. Back Stability
the center of the hip joint to the shoulder joint and ear canal, with the spine evenly distributed along the gravity line. Your instructions to hollow the abdomen and "lengthen the spine" will help bring about the correct alignment. If you wish, you can monitor the depth of the lumbar lordosis with pressure biofeedback, placing the bladder of the unit between the lumbar spine and the chair back. (Note that the sitting position used in this case is not what most people use in everyday activities; they can have their backs against the chair for use with a pressure bladder by slightly straddling the seat with their legs, which, as you recall, are to be somewhat spread, with knees lower than hips.)
Sitting Hamstring Stretch .l1:tJ.,. Maintaining pelvic position against the pull of the hamstrings. For the first exercise, instruct your client to straighten one leg to stretch the hamstrings, while maintaining lumbar-pelvic alignment. As soon as the pelvis posteriorly tilts (to bring the ischial tuberosity forward and take the stretch off the hamstrings), stop the exercise because alignment has been lost. Progress the exercise by gradually straightening the leg further (while maintaining alignment) until the knee can be locked fully with the hip at 70° flexion (see "Tripod Stretch," page 117).
Sitting _It.,.,.
Sternal
Lift
Performing active thoracic extension lumbar extension.
and isolating
it from
Instruct your client to raise her sternum while drawing the scapulae down, as in the standing sternal lift on page 179. The movement is one of thoracic spine extension rather than deep inspiration. To assist the learning process, place the flat of your hand on your client's sternum and "draw it up," while placing the thumb and forefingers of your opposite hand on the inferior angles of the scapulae and "draw it down." If breathing control proves to be problematic, encourage your client to breathe out as she begins the sternal lift. Many people mistakenly extend the lumbar spine rather than the thoracic spine. If this occurs with your client, let her practice the exercise with her feet on a small stool to bring her knees above hip level-this position reverses the lumbar lordosis and throws the extension force high up the spine to the thoracic continued
Advanced Stability Training
.
183
Sitting Sternal Lift. continued
region. Once she has mastered the movement in this position, try the standard position again (see "Sternal Lift Exercise," [a], page 162).
Sitting Knee Raise Maintaining pelvic position I!imIpull of the hip flexors.
against the
In this third exercise, we overload the stability muscles by using the pull of the iliopsoas to displace the lumbar spine. Instruct your client to raise one knee, in stages, to about 3 inches above the horizontal, while maintaining lumbar-pelvic alignment. Be sure that he avoids posterior pelvic tilt. Initially, he should gradually unload the limb by lifting just the heel. If he is able to maintain good alignment, have him proceed to lift the entire leg.
Sitting Knee and Arm Raise .1'{'1~''''ncreasing
the complexity to challenge coordination.
Have your client flex one arm to 90°. Holding a small (7.5-10 lb., or 3-5 kg) dumbbell in the hand increases the overload; he should keep the dumbbell moving rather than holding it still. Combining alternate arm and leg movements is a useful progression-the right arm is lifted at the same time as the left knee to provide a diagonal stress on the body; this is then reversed with the left arm and right knee being raised.
Repeated Pelvic Tilting Exercises Using Balance Boards Moving the pelvis beneath an immobile trunk is an excellent teaching method to improve control of the neutral position, to reduce muscle reaction speed, and to enhance general stability. Using a "rocker board" (moves like a see-saw), and progressing to a "wobble board" (mounted on a hemisphere-moves in any direction), is an effective (and rather fun) way to perform such exercises.
184
. BackStability
Simple Pelvic Tilt, Progressing to Use of Balance Boards
Em
For advanced control of pelvic tilt.
At first, have your client sit in the optimal position (see page 181)on a wooden bench or stool with his feet on the floor. Instruct him to tilt his pelvis alternately in the anterior and then posterior direction, while maintaining the position of his shoulders and thoracic spine. The aim is to isolate the pelvis and lower lumbar spine from the thoracic spine, and the shoulders from the upper lumbar spine. Progress the exercise by having your client perform it while sitting first on a rocker board (like a see-saw, moves in only one plane-shown in the next exercise section), and then on a wobble board (mounted on a sphere, moves in any direction-see page 185, "Neutral Position Maintenance").
Pelvic Rock on Rocker Board .f{I1~'. Progression from simple pelvic tilt. Initially place the rocker in the frontal plane to facilitate anterior and posterior tilting of the pelvis. Changing the rocker orientation of the board to the sagittal plane will facilitate lateral tilting. In each case, the lumbarpelvic movement must be isolated from that of the upper body. To begin working for muscle reaction speed, apply pressure on the shoulders to push your client off balance while he tries to stay upright on the rocker board. Alternate the orientation of the board, between frontal and sagittal planes. You'll know when to stop any given session when your client is no longer able to maintain neutral position or maintain abdominal hollowing. Build up to 2 minutes in both planes before progressing to the wobble board.
Advanced Stability Training.
185
Pelvic Rock on Wobble Board IIm%i!!IMultiplane (sagittal. frontal. and transverse) stability in sitting_ Initially, have your client merely sit on the wobble board and attempt to maintain the optimal sitting position. Have him progress to single plane actions (flexion/extension and lateral flexion). Once he has mastered these actions, instruct him to "tip the board around a clock face" (i.e., to tilt to 1 o'clock and then back to neutral, to 2 o'clock and back to neutral, to 3 o'clock and back to neutral, etc.). Encourage him to use slow, deliberate movements, taking perhaps 2-5 seconds to reach each position of the clock, holding that position for 2 seconds, taking 2-5 seconds to return to neutral, holding neutral position for 2 seconds, and then beginning the next phase.
Neutral Position Maintenance IIm%i!!I Building stability reaction speed in sitting_ Finally, you should try to knock your client off balance while he maintains the neutral position on a wobble board. Initially use slow-onset pressure, working gradually up to rapid pressure from a variety of directions. Have your client close his eyes to faci!itate anticipatory muscle action and muscle contraction speed. The progression here is one of time. Initially, try to prolong the movement for 30 seconds, then 60 seconds, stopping each time when alignment is lost or the client loses his balance.
Sitting
Hip Hinge
IIm%i!!I Moving spine and pelvis
as a single
unit on the hip_
The final exercise is the hip hinge (compare "Standing Hip Hinge," page 181). As in all these sitting exercises, be sure your client begins continued
186
.
Back Stability
Sitting Hip Hinge, continued
in the optimal sitting position, with the knees astride to facilitate pelvic tilt (see description under "Exercises in the Sitting Position," page 181). Have him tip the whole of his upper body forward as a single unit, moving the pelvis and spine on the fixed femU[ He should initiate the action by leaning his whole body forward to change the sitting weight distribution. In optimal sitting, approximately 30% of the body weight is taken on the pubic bones and 70% on the ischial tuberosities, provided that the knees are aligned below the hip and the femurs are angled below the horizontal. As your client leans forward, he takes weight from the ischial tuberosities and places it onto the pubic bone, ending with 70-80% of his weight on the pubic bone. To lean back, he reverses the weight transference. To facilitate the action, suggest that he perform it while sitting on a rocker board. In each case the pelvis and spine should move as one unit, avoiding any change in lordosis.
STABILITY
BALL EXERCISES
In addition to or even instead of the exercises in the previous section, your clients can obtain advanced levels of stability by exercises with stability balls (also called gym balls). These exercises require quite complex movements and will help increase the stability already obtained through previous exercises in this book. They also can strengthen stability muscles that otherwise might not be exercised. At first your clients should use the ball under your supervision, but later they can use it at home-it is an inexpensive and effective apparatus for back stability. Several authors have described general exercises on the gym ball, and these publications make useful follow-up material (Hyman and Liebenson 1996; Lester and Posner-Mayer 1993; Norris 1995a).
Advanced Stability Training.
187
A 26-inch (65-cm) gym ball facilitates the optimal sitting position for most people. Your clients should be able to sit on the ball with their femurs horizontal and their hips and knees both at approximately 900 flexion. Feet should be shoulder-width apart and flat on the floor to enable free pelvic tilting and provide a wide base of support. The ball should be inflated so that it feels firm but will give slightly when a person sits on it. Use higher inflation pressures for heavier clients. Deflating the ball slightly will increase the base of support. You can reduce the ball's tendency to roll by setting it on a "collar"-a plastic ring on the floor. When you need to increase your clients' confidence or provide support, place the ball between two chairs: either position the chair backs toward the ball so that your clients can lightly touch the chair with arms outstretched at shoulder level; or, for even more support, position the seats toward the ball so your clients can place the flats of their hands on the seat surface. As with all exercises, your clients should warm up and stretch before engaging in these activities. During all exercises they should maintain the neutral position of their spines and keep their abdomens hollowed. They should perform mirror images of anyone-sided exercises, so the body is worked symmetrically. The progression with stability ball exercises is similar to that for previous exercises: begin with 8-10 repetitions, for example, then increase to 12-15. Note that the gym ball introduces balance as an additional variable. Even if your clients are not fatigued, if they lose alignment or lose their balance and become unstable (and therefore likely to slip off the ball), they must stop, rest, and start again using a lower number of repetitions. If gym ball exercises are the only ones your clients are doing, they should perform all of the following exercises during each session. I suggest at least three but no more than five sessions per week, for at least 1016 weeks. At first have your clients use a slow count of 4 or 5 to move into the holding position; hold the designated position for a count of 5; then use a count of 4 or 5 to move back into the starting position. They can progress by adding reps and/or by adding to the holding time. Determine the limits for a given exercise by observing the point at which your clients just begin to lose spinal alignment or abdominal hollowing, or to lose their balance-then instruct them to stay just below that level of timing or rep number for at least a week before trying to add holding time or reps. They should always stay just a little bit within their maximum capacity, as determined by their ability to maintain alignment and abdominal hollowing.
J88
. Back Stability
Sitting Knee Raise .fI.m.
Maintaining stability in the presence of hip movement on a reduced base of support.
While sitting upright on the gym ball, your client should lift a single knee from 90° hip flexion to 120° hip flexion. She must make the action slow and deliberate, maintaining her body position throughout, and avoiding the temptation to "fall toward" the lifting leg.
Abdominal Slide .fllT,:.'. Controlling moving.
the action of the rectus abdominis
while
Instruct your client to tilt her pelvis backward from a sitting position on the ball, then to roll back until her spine rests on the ball. The action is to roll through the spine-the ischial tuberosities begin on the ball, but the weight is transferred to the coccyx and sacrum and eventually to the lumbar spine. The final holding position is with the trunk slightly flexed and the abdominal muscles contracted in a half-sitting position.
Half-Sitting Arm and Leg Movements .fI'N.
Maintaining stability unstable position.
while moving arms and legs in an continued
Advanced Stability Training
.
189
Half-Sitting Arm and Leg Movements, continued
Have your client perform the abdominal slide action just described, but maintain the position when his trunk is at 45° to the horizontaL Then he should raise one arm while lowering the other. Once he can do this in a controlled fashion, with the trunk remaining in alignment, have him rest his arms, then lift one leg while lowering the other. He should try to keep the thigh of the leg being raised parallel to the ground (i.e., only the lower leg should move). Finally, he should perform arm and leg movements together-the right arm and left leg lifting together, and vice versa. To make the exercise even more challenging, suggest that your client hold small dumbbells in his hands as he does the movements.
Lying Trunk Curl Over Ball .f[,,~,.
Strengthens upper rectus abdominis muscles.
Instruct your client to begin with his thoracolumbar spine supported on the ball, his arms at his side. He should move from this sligh tl y flexed position to spinal extension, relaxing over the balL He then performs a curling movement while performing abdominal hollowing and pressing his lumbar spine onto the ball surface. Once he can perform the basic exercise well, increase the difficulty by having him hold his arms by the side of his head or even completely overhead.
190
. Back Stability
Lying Trunk Curl With Leg Lift .I'{t:r..,. Strengthens upper and lower abdominals. From the "lying trunk curl over ball" position, your client should lift one leg while maintaining the stable position, trying to keep the thigh parallel to the other thigh. The movement is easier if the ball rests closer to the shoulders with the waist at the ball's edge rather than at the ball's center. Lying over the ball, in fact, is an excellent way to stretch the whole spine into extension as part of postural correction of a flatback posture.
Basic Superman .1'{t7~,. Strengthens the spinal and hip extensors. Have your client lie prone with his abdomen on the ball, and his feet astride and flat against a wall. He should tighten his abdominal muscles to form a firm surface pressing against the ball and retract his head (tuck the chin in without looking down). He should retract and depress his shoulders in order to draw his arms downward and back, then extend his thoracic spine to bring his chest off the ball. Have him hold the innerrange position for 5-10 seconds.
Superman With Arms .1'{t1~,. Strengthens spinal extensors; helps shoulder retractors contribute more to movement. From the basic superman movement, instruct your client to extend first one and then both arms overhead to increase the overload for both trunk and shoulders. Holding a light ball or balloon between his hands can help give him the feeling of lengthening his body. Observe carefully to make sure that your client doesn't lose alignment and hyperextend his spine. There should be a straight line through the heels, knees, hips, shoulders, and hands. continued
Advanced Stability Training.
191
Superman With Arms, continued
Bridge .I'[IJ~'.
To simultaneously extensors.
strengthen
both hip extensors
and spinal
Have your client lie with her shoulders and back on the ball and her feet flat on the floor, knees apart. At first, place a small stool under her buttocks and instruct her to raise and lower her body from the stool using hip extension force. Once she is able to hold the raised position, remove the stool. Instruct her to hold the position, making sure that her lumbar spine is in its optimal position; she should gradually build up the holding time to 30 seconds.
Bridge With Pelvic Tilt .1'['1.'1. Strengthens back and hip extensors of pelvic tilt.
while improving
control
While your client holds the bridge position, have her perform a pelvic tilt. She can intensify the bridge movement by combining anterior tilt with lowering her buttocks onto the floor, and a posterior tilt with lifting herself back into the bridge position. This exercise helps teach the subtleties of muscle control involved in minor adjustments in pelvic tilt. It is especially helpful to clients who can only perform a tilt as an "all-or-nothing" movement using maximal force to bring about a full tilt.
192
. Back Stability
Bridge With Leg Lift .f{"~'.'ncreases bridge.
overload-especially
of lower abdominals-during
Have your client perform the standard bridge exercise-but once he is in the high position, he should lift one knee to bring the foot off the ground. Be sure that he maintains spinal alignment, avoiding the temptation to tip the pelvis toward the lifted leg. If he finds it difficult to keep his pelvis level, place a stick across the front of the pelvis just below the level of the anterior superior iliac spines. If the pelvis tilts too far, the stick will fall off!
Bridge .f{'1~'.
With
Leg Lift and Extension
Strengthens lower abdominals
while increasing
leg control.
Have your client perform the standard bridge and lift the right knee so that the right foot clears the floor, avoiding the tendency to allow the pelvis to tilt to the right. At the high position, he should gradually straighten the right leg until it is completely in line with the spine. After maintaining this position for 2-3 seconds, he slowly bends the leg and lowers it till his foot is back on the ground.
Bridge .f{'1~'.
With Therapist Strengthens
Pressure
hip and trunk stability
stability with continuously directions.
variable
muscles by challenging overload
from
multiple
While your client performs the standard bridge, you should kneel at his side. Push against his pelvis from above/below and side/side. Rapid pushes will decrease muscle reaction time, training the muscles to contract more quickly without loss of intensity.
Advanced Stability Training.
Reverse
193
Bridge
.f!I7~'" Strengthens back and hip muscles while increasing leg motion control. Your client's feet and calves should rest on the ball, with her trunk on the floor. Instruct her to abduct her arms to about 30. to aid balance. Then she should lift her hips to make a straight line from the shoulders to the hips and feet.
Reverse Bridge and Roll .f!'1~'"
Strengthens trunk and hip muscles, while increasing leg motion control.
Once your client is in the high position of the reverse bridge movement, she should roll the ball toward herself by flexing her knees and hips; then roll it away by extending the legs again.
Heel Bridge .f!I7~'" Increases overload in the bridge position. Instruct your clien t to assume the high position of the reverse bridge, with this difference: only her heels should be on the ball. Instruct her to push each heel alternately into the ball-this entails pushing down with the whole leg to activate the hamstrings and gluteals, rather than simply flexing the knee to work the hamstrings alone.
194
. BackStability
Single-Leg .f{'N.
Heel
Bridge
Provides maximal overload in the bridge position.
Your client's trunk should be on the floor, and only her heels should be on the ball. Have her lift one leg and hold it away from the ball. Then have her perform a single-leg heel bridge by pushing her heel into the ball and lifting her buttocks off the floor. She should hold the position for 5-10 seconds, then lower her body under control to the starting position.
Heel
Bridge
With
Leg Raise,
Ball Rolling
.f{I1~'. Provides maximal overload in the bridge position, while increasing leg movement control. Instruct your client to begin as with the previous exercise, up through the point of raising one leg. At this point, she should roll the ball toward herself by flexing her knee and hip; then roll it away by extending her leg again.
Prone
Fall
.f{'1~'.
Provides co-contraction
for the hip and trunk muscles.
Have your client place his thighs on the ball, with his legs together and his hands on the floor. He should lengthen his body to achieve a neutral spine, and retract his head to maintain cervical alignment. He should begin with the ball close to his pelvis, and then walk his hands forward so that the ball moves down his legs toward the knees. By shifting the body's center of gravity farther from the center of the ball, this movement increases the leverage effect.
Advanced Stability Training.
195
Prone Fall With Arm Lift ."tN.'ncreases
overload in prone fall.
Have your client begin with the prone fall movement. Then he should lift one hand about 0.5 inches (1.3 em) from the floor without allowing the shoulder girdle to dip down. He then lifts the arm first to the side and eventually forward, pointing the hand and lengthening the whole body.
Prone Fall With Single-Leg Lift ."t7.:.'.'ncreases overload (especially for gluteals) in prone fall, while training for abdominal-gluteal co-contraction. Have your client begin with the prone fall movement, then lift one leg to 15° hip extension, keeping the knee locked. Instruct him to perform alternate single-leg lifts; to train for speed as well as strength, have him gradually increase the speed of the lifts. Eventually he should do them as fast as he can without losing correct alignment.
Wall Sit ."t7.:.'.
To prepare the body for lifting, while strengthening to provide power for the lift.
the legs
Your client performs the following exercise with the ball sandwiched between his back and a wall. This has two main advantages over simply leaning against the wall. First, vertical movement is easier because the rolling of the ball removes the friction between the individual's back continued
196
. Back Stability
Wall Sit, continued
and the wall. Second, these exercises require more control since the subject is leaning on a mobile object rather than a fixed wall. The greater degree of control builds more automatic stability (i.e., the individual need not focus so much on the stability muscles in order to keep them stable). While your client stands with his back toward the wall, his feet about 2.5 feet (0.75 m) from the wall, place the gym ball between the wall and the lumbar region of his back. Instruct him to lower his body to the sitting position while rolling the ball down the wall. Once he achieves 90° hip and knee flexion (a), he should hold the position for 5-10 seconds and then roll back up to the starting position. He can then progress to the single-leg wall sit (b).
Free Squat .flaB.
Teaches whole-body
control during vertical movement.
Place the gym ball on a collar to stop it from rolling. Have your client stand in front of the ball, feet astride. She should slowly squat, keeping her back aligned, until she sits on the ball, then slowly stand up again.
Arm Lift in 4-Point Kneeling .fle7.:.,.'ncreases
overall stability during shoulder movements.
Decrease the ball pressure for kneeling actions so that it will fit comfortably under your client's abdomen in 4-point kneeling. Once your client is kneeling over the ball, instruct him to lift first one (a) and then both continued
Advanced Stability Training
.
197
Arm Lift in 4.Point Kneeling, continued
arms to the horizontaL Tell him to "lengthen his body" through the arms and hold the fully extended position for 5-10 seconds. The next progression is for the client to extend his spine and lift his arms behind himself to the horizontal (b).
b
Double-Leg
Raise
.f'('7.'.'ncreases strength of hip and spine extensors, while promot. ing trunk stability. Your client begins as with the previous exercise, but with the ball lower down the body toward the hips. Have him first lift one leg to the horizontal, maintaining good body alignment throughout the action. He can then progress to lifting both legs. If your client's legs are especially heavy, his arms may lift from the floor during this exercise. To prevent this, he should hold onto a low object such as the legs of a heavy gym bench. He should hold the fully extended position for 5-10 seconds.
PROPRIOCEPTIVE The aim of most of the to move/position their become stable, and (2) second goal is virtually
TRAINING
training in this book is for your clients (1) to learn muscles in such a way that their lower backs will to keep their backs in the stable position. And the unattainable unless your clients' bodies learn to
198
. BackStability
do what is necessary without conscious thought. The movements, the postures, and the balance must be more automatic. This is the goal of proprioceptive training.
Theory of Proprioception Because I believe it is important that you know the underlying mechanisms behind the activities you prescribe for your clients, the next few paragraphs provide a brief overview of proprioception. Movement Sense Kinesthetic awareness, or "movement sense," includes the detection of both joint displacement and change in velocity (Le.,acceleration). It is commonly assessed by measuring the threshold to detection of passive motion (TIDPM): individuals simply state when they feel movement has begun. One cannot act to correct imbalance until one is aware that there is an imbalance. The awareness can be conscious or unconscious, however, and the corrective action likewise can be intentional or automatic. The purpose of proprioceptive training is to help individuals learn both to detect and to correct imbalances without conscious awareness that they are doing so. Consciously performed joint-positioning activities, especially at end range, will enhance the development of automatic control and cognitive awareness (Lephart and Fu 1995). Regulation of Muscle Stiffness Dynamic joint stability (Le., the body's ability to constantly make unconscious "microcorrections" to keep a joint stable) occurs via reflexes at the spinal level. And reflexes by definition are not conscious or intentional movements. A common illustration is the body's response when your finger touches a hot skillet. The incoming nerve stimulus (afferent, Le., going "toward" the central nervous system) doesn't even make it to the brain-rather, it gets only as far as the spinal cord before it is processed and an appropriate outgoing (efferent, i.e., going "away from" the central nervous system) signal is sent to the muscles: "Move your hand!" In fact, you end up moving your hand without thinking about it because your brain had nothing to do with the reaction-it all occurred in a "closed loop" of signals between your hand and your spinal cord. The ideal situation as far as back stability is concerned is that you have such "closed loop" efferent signals constantly going out to your stability muscles: the receptor nerves detect a slight increase in instability, they send messages to the spinal cord, and instantaneously outgoing "efferent" signals are sent out to tweak a multifidus muscle, to slightly increase tension in your left internal oblique muscle, etc. It
Advanced Stability Training
.
199
all happens dozens of times a second without your even thinking about it. Such is the goal of proprioceptive exercises. It is possible to "train" your nervous system to be more sensitive to incoming messages that say "stability is weakening" and to provide more automatic outgoing signals that instruct which muscles to change in which way. If such a fine-tuned system seems unimaginable, try this experiment: open a water faucet at least halfway, place a drinking glass under it, and keep the glass as perfectly level as you can. You'll find that you can keep it quite still. Now consider the complexity of the nerve signals involved in the task you just completed. Thousands of times a second, afferent signals left your hand with the message, "The cup has just gotten heavier." And thousands of times a second, efferent signals returned from your central nervous system: "OK, tighten such-and-such muscles a teensy bit more." But it all happens so fast, and the microadjustments are so smooth, that for the most part your hand is able to hold the drinking glass stable. This is a closed loop system. Your brain isn't significantly involved. The signals go to your spinal cord, they are processed, and the return messages head immediately back to your hand. Proprioceptive exercises involve sudden alterations in joint position in order to train the body's reflexes. Chapter 7 provided exercises to help your clients learn simply to reproduce passive positioning of body segments. The training in this section is similar to those activities, but on a very fast track! In order to thoroughly follow an individual's progress, you theoretically can measure the precise onset of muscle contraction in relation to joint displacement-unfortunately, however, you most likely would need to refer your client to a physical therapy department or specialist biomechanics lab to make accurate measurements. Yet, with experience, you can assess onset of muscle contraction to some degree by palpating the muscle during a passive movement test. This type of examination, while not exact, can be useful for muscle re-education. The aim is simply to note if the muscles are able to limit joint displacement and effectively stabilize the joint.
Benefits of Training Using TIDPM and reproduction of passive positioning (RPP), Barrack et al. (1983) found decreased kinesthesia with increasing age (Le., the closed loop system for stability works less well). Injury further reduces proprioceptive input due to prolonged inactivity and damage to proprioceptive nerve endings within the injured tissues. A number of authors have stressed the importance of proprioceptive training in rehabilitation following injury to the knee (Barrack et al. 1983; Beard et al. 1994), ankle (Freeman et al. 1965; Konradsen and Ravn 1990; Lentell et al. 1990), and shoulder
200
. Back Stability
(Lephart et al. 1994; Smith and Brunolli 1990). The functional importance of proprioceptive training has also been emphasized during rehabilitation of the spine (Irion 1992; Lewit 1991; Norris 1995a), although its use in spinal rehabilitation is less common than for other areas of the body. Proprioception and accompanying reflexes may indeed be enhanced with training. Barrack et al. (1983) found enhanced kinesthesia in trained dancers, and Lephart and Fu (1995) demonstrated the same in intercollegiate gymnasts. Both types of athletes practice free exercise using body weight as resistance and using complex multijoint activities. This type of training appears appropriate for proprioceptive rehabilitation. Proprioception and stabilizing reflexes may be enhanced by using training that involves complex multijoint activities.
KEY POINT:
The basis of proprioceptive training for the back is maintenance of stability against
a rapidly
applied force tending
to displace
the spine. In most cases,
you can instruct your clients to practice one or more of the following exercises for at least five minutes a day, four or five days per week. The limiting factor is whether or not your clients can keep their spines stable (they should stop before they lose stability). They should do the most advanced exercise(s) of which they are capable, as quickly as they are able-remember, the idea is to train their reflexes to act with such extreme speed that maintaining spinal stability will be as smooth an operation as your holding the glass motionless as it fills under a tap.
Rapid Displacement
in Sitting
.1"111.01.Develop muscle reaction speed for back stability. Have your client sit on a stool with her spine optimally aligned. A training partner stands behind her and presses against her shoulders from multiple directions to flex, extend, and laterally flex the spine. Initially the pressure should be even, but gradually it should become varied in both direction and force. The aim is for your client to be able to rapidly stabilize the spine before the spine moves away from its neutral position. Instruct her to relax her trunk muscles between repetitions (which should last about a minute each), rather than hold them rigidly braced throughout the whole exercise. If you have it available, you may want to use surface EMG to monitor changing muscle tone. As your client's reactions become more proficient, the movements should become fasterbut she must always maintain good alignment.
Advanced Stability Training.
201
Muscle Reaction Speed Using a Mobile Platform .1'1:11.'. Further develop
muscle reaction
speed for back stability.
Instruct your client to assume a 2-point kneeling position on a balance board and to align his lumbar spine into its neutral position. Then a training partner should push him off balance so that the platform tilts. The aim is to maintain lumbar stability as the board tilts, while keeping the edges of the board off the ground. Start with a rocker board (allows single-plane motion), advancing later to a domed balance board (wobble board) that allows trip lane motion. You may also want to use other mobile platforms such as the Fitter ski trainer (Fitter International Inc., Calgary, Alberta, Canada), the slide trainer (Forza Fitness Equipment, London, England), or a mini trampette (available in most large sports stores). Again, increase the speed of the movements as your client becomes more proficient.
Throw-Catch Activities
on a Mobile Surface
.1'1:11.'. Develop rapid-onset back stability. Throw-catch activities using a basketball or medicine ball will increase the challenge to the stabilizing system. The aim is to align the lumbar spine optimally while balancing on the mobile surface. As your client catches the ball, she must maintain spinal alignment in spite of the platform's motion. Instruct your client to increase the speed of the exercises as she becomes more proficient.
SUMMARY
· · · ·
Once individuals
have achieved
basic back stability
through
the
exercises in previous chapters, they can begin building greater stability and training their backs for sports or on-the-job lifting by using the advanced exercises in this chapter. Advanced stability exercises, with movement of limbs on the stable trunk, will greatly increase an individual's ability to maintain stability automatically, without conscious thought.
back
Exercises with gym balls also help develop automatic stability and help develop muscles that previous, more basic, exercises may not affect. Proprioceptive exercises can be very useful in training your clients' reflexes to automatically (unconsciously) keep the spine stable.
9 More Advanced
Stabilig Training! Weight Training and Plyometrics If one's
goal is merely to develop adequate back stability, special equipment is unnecessary. People with sport and occupational injuries, however, require limb strength in addition to back stability in order to complete their rehabilitation-especially if they are to resume on-the-job lifting tasks or sports activities in which the body works against resistance. Weight training has several important advantages for those with lower back problems. First, it can increase the limb strength that some people need. Second, it can further enhance trunk muscle strength/stability to the level often required in sports-especially contact sports where abdominal strength can have a protective function for the internal organs. Finally, weight training can help to guard against further back injury. When we use weight training for back stability, we are strengthening muscles upon an already stable base-weight training is appropriate only for individuals who have already re-educated and built up endurance within the stabilizing muscles. Weight training takes the process further, adding greater resistance both to strengthen muscle and to challenge the stability system itself. The target muscles are those of the trunk, the limb muscles attaching to the trunk, and the limb muscles that provide the power for lifting. Plyometric exercises also can enhance strength and stability, with the added benefit of training for very fast reaction times. Your clients can use plyometrics in place of weight training if they wish, although I suggest a combination of both if they can afford the time. They need good stability before beginning either kind of training-but since the speed of movement in plyometrics is far greater than that in basic weight training, your clients will need better stability to begin plyometrics than to begin using machine weights.
202
Weight Training and Plyometrics
.
203
Weight training or plyometric exercise for greater back stability is appropriate only for those who have already developed good back stability using exercises described earlier in this book.
KEY POINT:
WEIGHT TRAINING Emphasize to your clients that the weight training you are giving them is specifically part of a back stability program, and therefore the activities will be somewhat different from those they may see other people doing in the weight rooms. Make sure they understand that they must follow your instructions, resisting the temptation to emulate the practices of other exercisers.
Before You Start Before introducing any of these weight-training exercises, give your clients the following instructions: (1) They must keep the whole spine correctly aligned and the lumbar spine in neutral position. (2) They should perform abdominal hollowing to tighten the stabilizing muscles and provide a stable base upon which the limbs can move. (3) They should exhale when lifting a weight, rather than holding their breaths, and be careful that deep breathing does not lead to hyperventilation and associated dizziness. Weight training involves three types of muscle work. The weight is lifted through concentric muscle action, held steady by isometric action, and lowered under control by eccentric action. Your clients should use all three phases. Remind them that the common practice of lifting the weight rapidly and then dropping it minimizes eccentric and isometric action, both of which are vital to stability work. A ratio of lifting for a count of 3, holding for a count of 2, and lowering for a count of 4 will emphasize each type of muscle work. Your clients should feel comfortably challenged during these exercises rather than excessively strained. Their breathing rates will increase, but they should be able to talk normally at all times-if they are fighting for breath, the exercise intensity is too great for rehabilitation and you should stop the exercise. Individuals may sweat lightly and experience mild reddening/ darkening of the skin; but excessive red coloration and bulging of veins in the face and neck are indications that the exercise intensity is too great, and the exercise should be stopped. See that a therapist or trainer supervises your clients during the initial stages of weight training, until both parties are confident that the exercise techniques are correct.
204
. Back Stability
Safety Check All exercise equipment has risks that must be minimized (see "Safety Checklist for Weight Training," below). The risks fall broadly into two categories: those associated with moving machinery, and those associated with the lifting action itself. Here are the rules you should present to your clients, and the explanations you should give them for why the rules are important:
·
Control the weights. Moving weights carry considerable momentum. Unless the weights are kept under control throughout the full range of motion, there is considerable risk to joints and body tissues. When a limb reaches the end of its motion range, the ligaments and muscles surrounding it become tight and limit further movement. Movements that are too rapid lead to loss of control-the joint stops moving at the end of the motion range, but the inertia of the weight forces the joint further against the tightening support tissues, causing severe trauma or overuse injury. With a traumatic injury, tissues are suddenly tom and function is lost-the athlete sometimes feels the body part "tear" or "give." Bleeding and swelling result. Overuse injuries are more insidious. The tissues undergo microtrauma as they are continually pulled further than their normal range allows. The resulting low-grade inflammation in some cases gives rise to formation of scar tissue, and in others may actually pull a tendon attachment away from the bone. When this happens the bone membrane (periosteum) may be lifted and the area may calcify, giving a cloudy appearance on X ray. In either case, the message is clear: when using Safety Checklist
for Weight Training
.. .. . Remove jewelry.
Always warm up before training. Check machinery before use. Set up machinery to suit your height and weight. Tie back long hair and be careful with loose clothing.
..
Wearserviceable footwear-no flip-flops! Use correct exercise techniques and keep the weight under control. Watch your body alignment-keep a neutral, stable spine.
. .. Keep abdomen hollowed during exercises. Practice good back care-lift correctly.
..
Train within your own limitations.
Never train through an injury-see
a physical therapist.
Adapted, by permission, from eM. Norris, 1995, Weight training: Principles and practice (London: A & C Black).
Weight Training and Plyometrics
.
205
weight-training apparatus, your clients must always move the weights in a controlled fashion. When using weight-training equipment, your clients must move the weights in a controlled, slow manner. Tell them, "Make sure you control the weight; don't let it control you'"
KEY POINT:
·
Wear appropriate clothing. Even though most machines have guards, fingers and especially hair and clothing can be trapped in the moving weight stack with severe results. Instruct your clients to tie back long hair when they use machine weights and to keep loose clothing well away from the machines. They should remove watches, large rings, and dangling jewelry. Good sports shoes will help protect their feet-the weight gym is no place for beach shoes or flip-flops! Toes can be stubbed and free weights dropped onto feet. As well as giving your lower limbs better alignment, sports shoes offer the first line of defense against foot injuries. Adjust the equipment. Most good weight-training machines allow users to adjust the unit for the shape and size of their bodies. Make sure that the machine is set up beforeit is used, and that the user knows exactly how the machine works before beginning the exercise. Know your limits. Remind your clients to train well within their limits. An old adage says, "Never sacrifice technique for weight." Lifting a weight that is too heavy can impair both technique and body alignment and increase the risk of injury.
· ·
·
Listen to your body. Your clients must not train with an injury unless they are following a structured rehabilitation program. The key is to listen to the body, especially pain. Never allow an individual to exercise through increasing pain. If a movement hurts and is continued slowly, the pain may diminish-in which case the person is probably suffering from stiffness that is working loose. If pain increases, however, the movement must stop. Caution: remember that some rapid, repeated actions may "reduce" pain simply because the exercise hurts more than the injury! Alert your clients to this possibility, and remind them to stop such movements immediately if they even suspect a masking effect. KEY POINT:
Never exercise through increasing pain.
Machine Exercises A major advantage of machine exercises is that they usually allow only singleplane motions and are therefore easy to coordinate (pulleys are an exception-
206
.
Back Stability
because they allow motion in three planes, they require more complex coordination). Have your clients use "pyramid training," with light resistance for the first sets to prepare the muscles for higher overload. They generally should employ slow repetitions to make the movement exact, and light resistances in order to build endurance. Obviously, they should do all exercises using both left and right sides of their bodies-they should simply follow mirror-image instructions for anyone-sided exercises described in the next section. Once your clients have mastered the basic movements for any of these exercises, using fairly light weights, prescribe a progressive program similar to the following, taking your clients' individual needs into account: for each machine, determine the weight with which the clients can perform 15 full repetitions and still have enough energy left to do 3 or 4 more before reaching exhaustion. Prescribe 12-15 reps per exercise session, three sessions per week, skipping at least one day between sessions. After two weeks, they can increase the weight, again according to how much they can lift using 15 full reps and not quite be at the point of exhaustion. Let them follow this program-12-15 reps / session, three sessions / week, for a period of at least 16 weeks, never increasing the weights past the point where they can do 15 reps and still feel they can do several more. Remember, this is not a program of building photogenic bodies-it is a program designed to further increase back stability and help prevent future back problems. You can prescribe higher numbers of repetitions (20-25) to enhance muscle endurance rather than strength. Although 12-15 repetitions will produce some increase in both muscle strength and muscle endurance, higher numbers of reps are required for muscle endurance with minimal joint loading. This is relevant for clients whose clinical conditions preclude their handling larger weights. Those with high blood pressure or severe osteoporosis, for example, may require higher numbers of repetitions with very little resistance. This type of workout will help your clients learn the proper movement without overloading the joints. The weight your clients lift should always feel comfortable and lightly challenging to them. If a weight feels too heavy, it will lead to poor exercise technique-and body alignment will suffer. If you see this happening, reduce the weight.
Lateral Pulldown .1'(t1~,.. To strengthen the latissimus dorsi (which tensions the thoracolumbar fascia, an essential component of stabilization). For the lat pulldown, one may lower the bar either behind the shoulders or to sternal level on the chest. Either position can be used, and both have continued
Weight Training and Plyometrics
.
207
Lateral Pulldown, continued
advantages and disadvantages. Pulling the bar behind the neck will increase your client's shoulder mobility, as that position requires a higher degree of external rotation at the shoulder than pulling the bar to the chest. Since external rotation is often limited, this is a desirable form of mobility training. Remember, however, that the seventh cervical vertebra has a very prominent spinous process (the point of bone pressing out through the skin), and your clients must take care not to strike this point with the bar. To lessen the likelihood of this happening, they should pass the bar behind the head by 2-3 inches (5-8 cm) rather than letting it brush the hair. In this way, the bar will miss the cervical spine and come to rest across the shoulders. Individuals unable to adopt this position should pull the bar to the upper chest. The action is a smooth pull downward, placing the bar (in the first case) behind the neck and across the shoulders. The head should be tilted forward slightly, and the bar must not strike the cervical vertebrae but rest across the middle fibers of the trapezius. The lowering action of the weight pulls the bar up again. Instruct your clients not to permit the weights to rest together at the end of the movement, so that useful traction will be maintained in the latissimus dorsi and the thoracolumbar fascia. Bringing the bar in front of the body to the top of the sternum reduces the range of external rotation and extension at the shoulder and is especially useful for less flexible individuals and those with a history of shoulder subluxation or dislocation. Although you may permit your clients to use whatever grip seems most comfortablewide, narrow, pronated, supinated, or midposition-keep the following in mind: using a narrow grip either on a standard wide bar or a box frame (with elbows in pronated or mid position) will allow the elbows to pass close to the sides of the body as the bar is pulled down; and, according to Weider (1989), keeping the elbows in will thicken the latissimus dorsi rather than broaden it. Using a supinated grip reduces the emphasis on the latissimus dorsi and emphasizes the biceps brachii.
208
. Back Stability
Cable Crossover .I{"~,,,
To strengthen the latissimus dorsi and pectoralis major.
The movement begins with both arms abducted. The feet are apart, slightly wider than shoulder width. The action is to exhale and pull both arms into adduction to the sides of the body. An alternate approach is to pull the arms forward across the chestthis technique increases the adduction range and emphasizes the pectoralis major. The elbows should be slightly bent throughout the movement, to reduce stress on the elbow joint.
Back Extension
(Machine)
.1{11~'" Strengthens
the erector
spinae (full range).
The back extension machine can help rehabilitate and strengthen the back extensors but can cause problems if faulty technique is used. It requires close supervision. Permit clients to use this machine only after they have mastered the hip hinge action and pelvic tilt movements (both in chapter 4). Have your client adjust the machine so that knees and hips are bent to 70-80° and the pivot point of the machine is aligned with the hip joint axis. The movement begins with a posterior tilt of the pelvis, moving the seat contact point from the ischial tuberosities back onto the sacrum. The action is movement of the pelvis on the stationary femur, with the back stabilized and immobile throughout the early part of the movement. Only when the second half of the movement range begins should the spine move into extension.
Weight Training and Plyometrics
.
209
Back Extension (Frame) .1'[t1~,.. Strengthens the erector spinae (limited range). The back hyperextension frame is useful in both the early and advanced stages of training but can be dangerous if used incorrectly. The exercise position is similar to the superman (pages 190-191). Quality supervision is vital. Be doubly sure that your client maintains the neutral position at all times during this exercise and is performing abdominal hollowing. Place a bench or stool in front of the machine, level with your client's shoulders. He should place his hands on the stool in a push-up position, with his legs locked onto the machine pads. He lifts first one hand and then both hands from the stool, placing his arms by his sides. Have him perform this action 10 times, resting his arms on the stool between each movement. Once he can perform this action in a controlled manner, add spinal extension. He should begin in the neutral position (with or without stool support), move into extension, lifting the shoulders about 2-3 inches (5-8 em) above the hip only, then back to neutral, and finally down into flexion. Avoid full inner-range extension, to reduce loading on the lumbar facet joints. Note that this action can injure an individual with poor back stability. At the beginning of the movement, if the abdominal muscles are relaxed, the pelvis will anteriorly tilt and the lumbar spine hyperextend, compressing the lumbar facet joints without sufficient intra-abdominal pressure to reduce the loading. Back stability and good alignment control are essential prerequisites for performing this exercise.
Seated Rowing .,{l7~'"
To strengthen scapular retractors (middle trapezius, lower trapezius, serratus anterior) and glenohumeral extensors (triceps)-bilateral.
Instruct your client to perform this exercise with her knees bent, in order to relax the hamstrings and allow the pelvis to anteriorly tilt sufficiently for her lumbar spine to remain in neutral position. The action is upper arm extension, keeping the elbows in to the sides of the body. The scapulae should adduct, and the thoracic spine extend in the stemallift action (chapter 7). When lowering the weight, she should not allow it to pull the thoracic spine into flexion.
210
. Back Stability
Single Arm Pulley Row .,{t1~'" Strengthens scapular retractors and shoulder extensors (as in seated rowing~unilateral. Because this exercise combines back extension and rotation with shoulder extension, it offers a significant challenge to the stabilizing system of the back. Have your client stand in a lunge position to the left of the pulley, with the left foot forward and the 0 handle of the low pulley gripped in the right hand. He should place his left hand on the left knee for support and angle his body forward (trunk on hip) at 45°. He then pulls the right arm into extension at the shoulder-and, as the pulley hand approaches his chest, he slightly rotates his trunk to the right and extends the thoracic spine (a) (stemallift action, see chapter 7). Using a low pulley position (pulley at mid-shin level) requires the exerciser to lean over slightly, increasing the workload on the spinal extensors (b). This is suitable only where alignment is good and the individual can keep his spine straight throughout the action. Placing the pulley at waist height negates the requirement to lean forward, taking the workload off the spinal extensors and reducing leverage on the spine. Use the waist-high position if your client's alignment is poor.
n
a
b
low Pulley Spinal Rotation .f['1~'"
Strengthens
oblique abdominals.
One can perform spinal rotation exercises in lying, sitting, or standing positions. For the lying exercise (a), have your client assume a half-crook lying position perpendicular to the direction of pull, flexing the leg closer to the pulley. Attach the cable of the pulley to
a continued
Weight Training and Plyometrics
Low Pulley
Spinal
Rotation,
.
211
continued
the flexed knee with a leather or webbing strap. The action is to rotate the spine so that the bent knee passes over the straight leg and onto the floor. In the sitting position (b), your client sits on a stool, facing perpendicular to the pulley, with .. her left side about 18 inches (0.5 m) from the pulley. She should flex her right arm 90° at the elbow, holding it across her body. After adjusting the level of the lower pulley so that it is level with her elbow, she should grip the D handle of the pulley with her right hand. The action is to b rotate her trunk to the right, keeping her hips, legs, and arm immobile so the weight of the pulley unit is lifted by the trunk action alone. The standing exercise is similar to the sitting. She again adjusts the pulley to elbow level and folds the outer arm across her body, her feet apart to maintain a wide base of support.
Rotary Torso Machine .1'(t1~,. To strengthen oblique abdominals while avoiding end-range movements.
Position the rotation lock to allow full rotation range but not to overstretch the spine. If rotation is painful or the range is limited, set the lock of the machine to avoid the painful end-range position. The action is a smooth rotation into full muscular inner range. Have your client hold the position and then slowly release it, avoiding the temptation to drop the weights rapidly and spin the machine. Reset the machine for the opposite rotation, remembering that range and strength are not necessarily symmetrical. Remember also that the full inner-range position into which an individual's muscles can pull (physiologicalinner range) is generally less than the full inner range into which he can be taken passively (anatomical inner range). As long as the motion is smooth and not too fast, your client is in no danger of overly stressing the facet joints of the spine during this exercise. If the motion is too rapid, however, the momentum of the machine can take the spine past physiological inner range and into anatomical inner range, loading the facet joints unnecessarily.
212
.
Back Stability
Abdominal
Machine
.f'(I1.". Strengthens the rectus abdom;n;s. Several abdominal machines are available on the market, but most provide resistance to trunk flexion, emphasizing the supraurnbilical portion of the rectus abdominis. Some provide additional resistance for the hip flexors working the infraumbilical portion of rectus abdominis as well. If possible, align the pivot of the machine with the center or lower portion of the lumbar spine rather than the hips. It is important that the rectus abdorninis does not bulge outward or "bowstring" during the action, but abdominal hollowing (practiced in all these exercises) will alleviate this potential problem. Have your client grip the machine arms, holding his elbows in throughout the action. Instruct him to "roll into flexion," keeping his back on the backrest and avoiding the tendency to lean forward. The movement begins by pulling the sternum down rather than forward. The eccentric component of the movement is important, so lowering the weight has to be slow and controlled.
Trunk Flexion With High Pulley (Pulley Crunch) .IIIH.
Strengthens
the rectus abdom;n;s.
Instruct your client either to kneel (2-point kneeling) or to sit, with his back to the machine, holding the 0 handle of the machine in both hands behind or in front of the neck (either is correctthe client should choose the most comfortable position). He should shuffle forward until he has taken up the slack in the machine cable. The action is to flex the trunk alone rather than the trunk on the hip (hip hinging), with the movement pointing the head downward toward the knees rather than forward in front of the knees. The action must be slow and controlled. Very little movement is available, so it is essential that the machine cable is tight before the action begins.
Weight Training and Plyometrics
.
21 3
Free Weight Exercises In the context of a back stability program, free weights are only for people whose bodies have heavy demands for strength and speed-generally, individuals who perform either medium or heavy manual handling on their jobs, or who are involved in strenuous sports. Free weights are also helpful in late-stage rehabilitation because of the complexity of skills they require (as compared with machine weights). It is best if, before beginning this stage, your clients have mastered the machine weight exercises just described, as those exercises help build the strength needed in these more complex free weight movements. They must do the exercises in this section only under strict supervision until they have perfected the actions. Give special consideration to clients younger than 18 or older than 60 years of age because their skeletons and joint structures are generally more prone to injury that those of other people. These individuals should exercise only under the supervision of a physical therapist or trainer who is specially trained to teach these groups.
~I
Individuals must demonstrate
good stability,
segmental control, and whole-body alignment before beginning late-stage rehabilitation exercises.
Special Concerns Regarding Free Weights Because free weight exercises combine both speed and weight, they expose the body to high levels of momentum (the product of mass X velocity). It's easy to stop a fast-moving arm if you have a pencil in your hand; but an arm moving at the same speed with a 20-pound weight in the hand can end up with torn tissues if the movement is not controlled. It is important that your sports-oriented clients-whether they swing objects such as racquets, or move their bodies quickly-learn to control momentum forces. The same is true for clients involved in moving or lifting heavy objects on the job. Before allowing individuals to begin free weight exercises, establish the following prerequisites and ground rules:
·
Your clients must have good stability and alignment. They must be able to maintain a neutral spinal position against limb resistance, as illustrated by good performance on the heel slide action (chapter 8, page 170). They must be able to maintain good alignment throughout the free weight-training program, keeping their lumbar spines in or near the neutral position at all times-the thoracic spine should be at its optimal position for each client, with shoulders held back comfortably (but not rigidly braced) and the chin held in.
214
.
Back Stability
· · ·
They must have good stability endurance. They should be able to perform 10 repetitions of each of the exercises in chapter 4, holding each rep for 10 seconds. They should have mastered all the machine weight exercises in the previous section of this chapter. They must warm up and stretch thoroughly before each weight session. First, they should lightly exercise (treadmill, stationary bike, etc.) till they just begin to sweat. Second, they should perform comprehensive stretching exercises that will take every major joint (hip, knee, shoulder, and spine) through its full range of motion. Third, they should rehearse each exercise by performing the first set at a light weight before adding further resistance. · They must stretch adequately after each weight-lifting session.
· At the beginning, a qualified trainer should supervise all free weight exercises, until both client and trainer are satisfied that the exercise technique is good.
·
Within the context of a back stability program, your clients should perform all free weight exercises progressively-first using light weights, then taking a rest period, then progressing to medium weights, another rest period, and finally heavy weights.
·
Free weight exercises as part of a stability program are not competitive; they are intended to progressively develop your clients' abilities to perform work against a resistance at speed. Clients should not compete with each other to see who can lift the most weight. Basic Free Weight Exercises For best results, have your clients go through all the following exercises in a single session. These exercises are appropriate for most individuals who fulfill the preliminary requirements just described. All the movements should be slow and well controlled. In the next section, I will describe more advanced exercises for people who need a great deal of "explosive power." Remember that the exercises are designed to build adequate strength, not bulk. Refer to Baechle (1994)for more detailed descriptions of the teaching points for these exercises. Because free weight exercises require more balance and coordination than do machine exercises, less weight should be used. Prescribe about 10-12 repetitions for each exercise, using a final weight that is comfortable for that number of reps (i.e., if the individual can perform 20 repetitions, the weight is too light; if he/she can perform only 5 reps, it is too heavy). For each exercise, your client should perform 2 or 3 sets of 10-12 repetitions: use a moderate weight (perhaps half the final weight) for the first set, three-fourths the final weight for the second,
.
Weight Training
and Pfyometrics
.
21 5
and the full weight only during the third set. In this way, the muscles gradually become accustomed to handling the weight. Your clients should rest after each set until their breathing rates and heart rates return to normalnever let them start a fresh set while their hearts are pounding or they are out of breath. Explain to your more impatient clients that this type of training is designed to "encourage" strength adaptation, not to "force" it. Training should be slow and controlled rather than fast and furious. Prescribe 2 or 3 sets for each exercise, three sessions per week, skipping at least one day between sessions. After two weeks, they may increase the target weight, again according to how much they can lift comfortably. Let them follow this program-2 or 3 sets of 10-12 reps, three sessions/weekfor a period of at least 16 weeks, never increasing the weights to the point where they feel exhausted. Remember that exercises described for just one side should be done on both sides, and that the instructions for the side not described are, of course, the mirror image of the instructions given.
Lying Barbell Row .flt1~'"
To strengthen shoulder retractors and increase thoracic spine extension (correct kyphotic posture).
Instruct your client to lie prone on top of a gym bench, with a light barbell (about 22.5-32.5 lb., or 10-15 kg) beneath the bench. She should grip the barbell at arm's length and lift it until it touches the underside of the ! bench. She may hold her elbows either close to the sides of her chest or with arms abducted to 90°-the narrow position places greater work on the latissimus dorsi, while the wider grip emphasizes the posterior deltoids and scapular stabilizers.
Dumbbell .fltH..
Row
Helps correct asymmetry between the shoulder retractors (middle and lower trapezius, serratus anterior).
You can recognize asymmetry by your client's inability to lift the same amount of weight, or to perform the same number of repetitions, with each arm. Have your client assume the half-kneeling position on a gym bench, his right arm and right knee on the bench and his left leg straight continued
216
.
Back Stability
Dumbbell Row, continued
with his left foot on the ground. He should grip a dumbbell (whatever weight feels comfortable to him) with his left hand, then pull (lift) it toward him, brushing the side of his body with his elbow. He should stop the movement when the dumbbell approaches his chest. As he pulls the upper arm into extension, the scapula is adducted; he should hold the inner-range position for 2-3 seconds before lowering the weight.
Good Morning .1'('1:.'" Works the spinal extensors statically and the hip extensors dynamically. This is basically a hip hinge action (several variations are in chapter 4) performed with a weight. Instruct your client to stand with her feet just wider than shoulder-width apart. Her knees should be unlocked to relax the hamstrings slightly and allow free pelvic tilt. With a light barbell (about 22.5 lb., or 10 kg) across her shoulders, she should tilt her pelvis anteriorly (always maintaining the alignment of the spine to the pelvis) so that her trunk angles forward to 45°. Watch carefully to be sure she does not allow her spine to flex, moving the axis of rotation from the hip joint to the mid lumbar spine-this stresses the spine considerably and can increase intradiscal pressure sufficiently to cause severe injury.
Squat .1'('1:.'" Teaches correct spinal alignment and strengthens quadriceps, hamstrings, and gluteals.
the
Have your client practice the correct form and movement using a light wooden pole (e.g., broom handle) until she has perfected the technique. The beginning weight should be 10-30% of body weight, depending on body build-stronger clients can use the larger value. Instruct your clicontinued
Weight Training and Plyometrics
.
217
Squat, continued
ent always to use a squat rack, so she can take the bar in the standing position. Her feet should be shoulder-width apart, toes turned out slightly. She should step under the bar, her hips directly under her shoulders, and, gripping the bar with hands slightly wider than shoulder width, place it across the back of her shoulders (over the posterior deltoids and trapezius). She should perform a sternal lift action and straighten both legs to lift the bar off the rack-then take a small step backward to clear the bar from the rack. Throughout the movement, your client should look up and keep her spine nearly vertical. The action is to flex hips and knees simultaneously, keeping the weight of the bar over the center of the foot rather than the toes. Instruct her to lower the bar under control until her thighs are parallel to the ground. After a momentary pause in this lower position to assist balance (but no bounce!), she reverses her actions to lift the bar. Watch to be sure her upward movement is controlled (no increase in speed toward the end of the action) and her knees stay over the foot rather than moving apart or together. Table 9.1 lists common errors associated with the squat. Table 9.1
Common Errors When Performing a Squat
Technique modification Error Knees come inward ("knock-kneed" Foot may be hyperpronating; conposition). sider more supportive footwear.
Knees stay behind feet throughout movement.
Practice a knee-bend position onto a bench in front of a mirror. Check if dorsiflexion range is limited in the ankle, and use a wooden block beneath the heels. Practice sitting onto a bench, pressing the knee forward onto the instructor's hand. continued
218
. Back Stability
Squat, continued
Table 9.1
(continued)
Error
Technique
Back angles
too far forward.
Spine flexes in thoracic
region.
modification
Press the knee forward, and aim to keep the spine more vertically aligned. Practice the basic squat motion sideon to a mirror. Ensure that adequate thoracic extension range is available, and practice the sternal lift motion in isolation. Strengthen the shoulder retractors and stretch the shoulder protractors (page 161).
Anterior pelvic tilt is exaggerated and lumbar lordosis increases.
Strengthen the abdominal muscles, and check for tightness in the hip flexors (chapter 7, pages 144-1 SO). Practice back flattening (chapter 7, page 149) against a wall.
Heel lifts.
Ensure that the weight of the bar is taken through the center of the foot, not through the toes. Check for adequate dorsiflexion range in the ankle, and use a wooden block beneath the heel.
Bar dips to one side.
Practice the squat in front of a mirror, and use a horizontal line drawn on the mirror to line up the reflection of the barbell.
Bouncing
Practice squatting onto a bench or
in the low position.
stool, lowering final position.
Barbell
gradually
into the
Lunge
.f{t1~,.. Helps improve spinal alignment and leg power, but with less spinal compression than in a squat. The start position is with the bar across the shoulders as for the squat. Because only one leg leads the movement, less weight (less than half) is used than in a squat-and so less spinal compression is created. Have your client stand with feet shoulder-width apart, the feet marking the end of an imaginary rectangle on the floor in front of him (shoulderwidth wide and twice shoulder-width long). As in the squat, he should perform a stemallift action while maintaining spinal alignment. Instruct him to step directly forward with the right leg (as though placing his continued
Weight Training and Plyometrics
.
219
Barbell Lunge, continued
foot along the long edge of the rectangle), then bend his knees so that the knee of the leading leg obscures the foot and that of the trailing leg moves toward the ground, stopping when it is 2-4 inches (5-10 cm) above the floor. The side of the trailing knee should be 6-14 inches (15-35 cm) from the inner edge of the heel of the leading foot. To stand up again, he pushes off the leading leg, bringing the leading foot back to its shoulder-width start position. The movement must not involve "falling" into the lower position or "jumping" into the upright position. Throughout the movement, your client should look up and forward, and the bar should remain horizontal.
Free Weight Exercises for Explosive Power Because of unusually heavy demands at work or in strenuous sport activities, some individuals require a high degree of explosive strength (Le., movement against a resistance [the weight] performed at speed [rapid resisted movements]). A variety of free weight exercises can help develop explosive power in the late stages of a sport-specific or workplace-specific back stability program. In order to perform these exercises, your clients must have progressed through the full back stability program and have good segmental control and spinal alignment. They should have mastered the machine exercises and basic free weight exercises in the previous section of this chapter. Have them rehearse all of the power movements using a wooden pole. Although you should still prescribe 2 or 3 sets of 10-12 reps, the first set should be with an empty bar to be doubly sure that the technique is correct and to train the muscles in the correct movements. Your primary guide for subsequent
sets must be spinal alignment
rather than the amount
of weight
the client can comfortably lift. If alignment is degraded, stop the exercise and reduce the weight, even if the client feels the resulting weight is "too light." Remember: the aim here is rehabilitation, not competitive weight lifting or body sculpting. For advanced free weight exercises, determine the amount of weight not according to how much your client can lift-rather, by how much your client can lift and still maintain correct alignment of the spine.
KEY POINT:
220
. Back Stability
Hang Clean .f["~,,,
Stage I power training.
Have your client begin with the barbell (held with hands pronated) resting on the middle of the thighs. For this exercise you should hand the bar to your client, who is already in the basic position illustrated by (a). Her body should be angled forward (30-45°) at the hips, and her spine straight. Knees and hips should be flexed, ankles dorsiflexed. The action is divided into two phases: the upward movement and the catch. During the upward movement, have your client hold her trunk erect and lift the bar explosively in a single "jump" action, extending the hips and knees and plantarflexing the ankles, without allowing her feet to come off the ground. Her shoulders should stay directly over the bar, and the path of the bar should be as close to the body as possible. At the point of maximum plantarflexion of the ankle, her shoulders will begin to shrug to continue the upward path of the bar (b). During the catch phase, which follows the shoulder shrug as a continuous motion, the client maintains the upward movement by flexing her arms. The elbows drop under the bar, forcing the wrists into extension to allow the bar to rest on the now horizontal palms (c). The elbows point directly forward, and the bar rests over the anterior aspect of the shoulders. As the bar touches the shoulders, your client should slightly flex her knees and hips to absorb shock and prevent a sudden jolt of the bar as she catches it on her shoulders. Instruct your client to lower the bar all the way to the ground, at first simply by reversing her earlier actions-she dips beneath the bar by bending her knees slightly, then allows her elbows to drop, with the bar staying close to the body as it is lowered. Her knees should bend so her body is not pulled into spinal flexion as the bar approaches the ground.
a
b
Weight Training
and Plyometrics
.
221
Power Clean .I'{IJ~'. Stage" power training. The power clean is a progression from the hang clean, with your client now lifting the weight from the floor rather than from the thighs. The barbell rests either on the floor or on two racks about 10-20 inches (25-50 cm) high. Instruct your client to stand with feet shoulder-width apart and knees inside the arms, feet flat and turned out slightly. It is important with this exercise that your client wears supportive training shoes-preferably a weight-lifting boot or high-cut cross-training shoes with broad, stable heels. Your client should grasp the bar with hands slightly wider than shoulderwidth apart, arms straight. She should squat down so that her shins are almost in contact with the bar, her knees over the center of her feet, her shoulders over or slightly in front of the bar (a). A common error with this movement is to get closer to the bar by flexing the spine, using only limited knee and hip flexion. This markedly increases the stress on the spine and must be avoided. The lift consists of three uninterrupted phases: (1) Instruct your client to extend her knees and move her hips forward as she raises her shoulders. Her shins should stay back (a common error with novices is to hit the knees with the bar), always maintaining the alignment of her back. The line of the bar's movement should be vertical, with her heels staying on the ground and the bar passing close to her body (b). Her shoulders should stay back, either over or slightly in front of the bar, and she should position her head to look straight ahead or slightly up. (2) For the "scoop," she drives her hips forward, keeping her shoulders over the bar and her elbows fully extended. The trunk is nearly vertical at this stage (c). This movement brings the bar to the midpoint of the thighs. (3) The exercise continues here as if it were the hang clean, through the upward movement and catch phases of that exercise (see illustrations for hang clean, previous page). The action is one of continuous movement, with no significant pauses between sections. Although the bar maintains its momentum, your client should never lose control of the movement. She should lower the bar in a vertical path, bending her knees to prevent her spine from being pulled into flexion.
222
.
Back Stability
Dead Lift .f{lN.
To improve back and hip strength, and add power for lifting.
The exercise begins with the bar on the floor (novices may use low racks at first, until they gain control through the full range of the exercise). Your client should stand with feet flat on the floor (heels must not lift) and shoulder-width apart, knees inside the arms, gripping the bar with hands pronated and slightly wider than shoulder-width apart, elbows pointing out to the sides. (Some athletes use an alternate grip, with one forearm pronated and the other supinated, i.e., knuckles down. If your client finds this grip more comfortable, by all means let him use itonly suggest that he alternate which hand is pronated and which supinated.) Have him position the bar over the balls of his feet, almost touching the shins, with his shoulders over or slightly ahead of the bar and his spine aligned in its neutral position (a). The movement begins by extending the knees and driving the hips forward. At the same time, your client raises his shoulders so that the alignment of his back remains unchanged. The path of the bar is initially vertical, and it is held close to the body at all times (b). The elbows must not bend, as that will cause a loss of power, and the shoulders should stay over or slightly in front of the bar. The head should be placed so that your client looks forward. Feet should remain flat. As the knees approach full extension, the back begins to move on the hip, maintaining spinal alignment (c). Have your client lower the bar with a squat motion, still maintaining the spine erect, keeping the bar close to the shins.
c
USING PLYOMETRICS TO TRAIN FOR POWER AND SPEED For most recreational athletes, almost any kind of training with more rapid movements (such as those in the free weight exercises) will suffice to im-
Weight Training and Plyometrics
.
223
prove speed. For clients who participate in higher levels of sports competition, however, or who simply want greater fitness gains than they have obtained after mastering everything in this book through chapter 8, proceed to the following plyometric exercises. These exercises can boost both reaction time and response time to high levels. There is no simplistic formula to help you decide, in consultation with your clients, whether they should do the exercises in this section in addition to the weight-training work just described, or instead of the weighttraining exercises. Together, you must weigh your clients' precise needs and goals. The main considerations will probably center around your clients' needs either for especially quick, strong reactions (e.g., hockey goalies or rodeo athletes), or for simple strength that must be explosive, but not necessarily blinding in its speed (e.g., football players or iron workers). If your client has the time and inclination, prescribe both kinds of exercise; if he has neither, but still wants to do more advanced work, choose either the weight training or the plyometrics. In order for you to understand the physiology behind the exercises, I need to present a bit of theoretical background. First, a few definitions: Power is the rate at which work is performed (work/time). Within the context of sports, Kent (1994) defined power as the ability to transform physical energy into force at a fast rate. Speed is simply the rate of movement. Reaction time is the time from the presentation of a stimulus to the initiation of a response. In terms of muscle work for stabilization, muscle reaction time is the time between the onset of a passive movement that disrupts stability and the initiation of muscle contraction to restabilize the joint. Response time combines both reaction time and movement time, the latter dependent on a variety of factors such as energy availability, nerve conduction, and actin/ myosin coupling. Good muscle reactiontime is vital to improving joint stability. Following ligamentous injury, for example, it is the reaction time of the supporting peroneus muscles that is the deciding factor for the return of full functionnot just the strength of the muscles (Freeman et al. 1965; Konradsen and Ravn 1990). And following knee injury, the important factor for rehabilitation is the reaction time of the hamstring muscles to resist anterior displacement of the tibia-not the strength of those muscles (Beard et al. 1994). The stretch-shorten cycle is important for anyone who trains for power and speed. Normally, the muscle supplies force through purely chemical means as actin and myosin filaments bond to cause the muscle to shorten. When an eccentric contraction (controlled lengthening) precedes a concentric action, however, force increases dramatically. Observe how a batter always swings his arms back immediately before swinging at a baseball. Or compare a squat jump (jumping from a static squatting position) with a countermovement jump (standing, dropping into a squat position, and then jumping). The height gained with the latter is greater than that from the former. Enoka (1988) measured average heights of 32.4 cm for
224
.
Back Stability
squat jumps, but 36.4 cm for countermovement jumps-more than 12% greater. The increased height comes from two sources: release of stored elastic energy, and additional chemical energy through a preload effect. In a countermovement, the extra energy gained relative to a standard movement comes from the release of stored elastic energy within the muscle, and from the preload effect.
KEY POINT:
Elastic energy results from passive stretching of the elastic components of the muscle. The muscle membranes (endomysium, epimysium, etc.) are noncontractile, but they are elastic and will recoil when released from a stretch, as will muscle tendons. The combined recoil of membranes and tendons provides a significant amount of energy. It takes time for actin and myosin coupling to occur. Chemical energy increases in a countermovement because, when the muscle is contracted eccentrically before it is contracted concentrically, the additional time permits more coupling-which leads to release of more chemical energy. Providing extra time to allow chemical reactions to occur creates the preload effect. Think of elastic energy as the muscle's springing back or recoiling like an elastic band-it is passive, and physical; whereas preload is like giving the muscle a running start on the chemical processes that lead to earlier contraction-it is active, and chemical. Three factors are important to energy release during concentric-eccentric coupling (Enoka 1988): 1. Time. If there is a delay between stretching the muscle and concentric contraction, some of the stored energy is dissipated. During the delay, actin and myosin filaments become detached and reattach farther along the muscle fiber under less stretch. 2. Magnitude. If the stretch magnitude is too great, fewer crossbridges are able to remain attached, and less elastic energy is available. 3. Velocity. A more rapid stretch (greater velocity) creates more elastic energy. To create maximum power with concentric-eccentric coupling, an individual must be warmed up; and a rapid eccentric movement must be followed immediately by a rapid concentric movement with no rest between the two phases. Any standard exercise can be performed in this way, and the exercises created are known as plyometrics. Yet not all exercises should be included in a plyometric workout since leverage forces and momentum acting on the spine can be dangerous: beware especially of rapid endrange motion on the spine and long lever movements.
Weight Training and Plyometrics
.
225
Before You Start Before progressing to the following plyometric exercises, your clients must
· ·
demonstrate good basic stability-able to perform the heel slide exercise (chapter 8, page 170) 10 times, and in general to perform adequately the exercises in chapter 4;
·
demonstrate good power and control in the trunk-able to perform gym ball exercises, including the superman (chapter 8, page 190) and bridge (chapter 8, page 191); and have good overall general fitness-demonstrated by regular, moderateto-intense exercise over the previous six to eight weeks. The exercise intensity should have been sufficient to raise the heart rate above 100 beats per minute. Each exercise session should have lasted for a minimum of 20 continuous minutes, with three periods of exercise per week.
Plyometric Exercises A number of exercises are useful. Be certain that your clients are supervised during all of them until both subjects and trainers are satisfied that your clients have learned the proper technique. Have your clients perform each exercise (for both right and left sides if it is asymmetrical) a maximum of 20 times per session, stopping earlier if they lose alignment or abdominal hollowing. They should try from one to three sessions per week for at least eight weeks, gradually increasing the speed of their movements as they are able. After the eight-week period, your clients may stop using plyometrics unless they are competitive athletes who require explosive strength to aid performance-in which case their strength coaches should prescribe the advanced plyometric exercises, tailoring them to the athletes' particular sports or events.
Plyometric Side Bend Using a Punching Bag .1'111.-'. Develops power and speed of the trunk side flexors while maintaining back stability. Instruct your client to stand with his left side toward a punching bag, feet shoulder-width apart, with his left arm abducted to 90°. He should flex his trunk to the left and push (not hit) the bag with his straight left arm. As the bag swings back, he takes its weight with his straight arm, then side flexes to the right to decelerate the swing of the bag (stopping short of full range!). The left side flexion begins the motion again. The action is reversed with the subject standing with his right side toward the bag.
226
. Back Stability
Plyometric
Flexion
and Extension Using a Punching Bag .1'{11~'" Develops power and speed in the trunk flexors and extensors while maintaining back stability. Have your client stand facing the punching bag, then push the bag with one or both hands. He should follow the movement through, using trunk flexion only, to 45°. He remains in this flexed position, and, as the bag swings back, he takes the bag with his arms straight (but unlocked) and flexes the arms, extending his trunk minimally and transferring his body weight to his back foot to cushion the momentum of the moving bag.
Twist and Throw With Medicine Ball .l'{lm.. Develops power and speed of the trunk rotators while maintaining back stability. Your client should stand in an aligned posture, with stabilized trunk and minimal abdominal hollowing. A training partner, facing in the same direction as your client, stands about three feet to her right, holding a medicine ball. While your client rotates her trunk to the right, her partner throws the medicine ball to her. As she catches the ball, she should rotate to the left, prestretching the oblique abdominals. She stops the movement short of full range, rotates back to the right, and throws the ball back to her partner.
Medicine .I'{IH..
Ball Trunk
Curl
Develops power and speed in the trunk flexors while maintaining back stability.
This exercise is a modification of the trunk curl (chapter 6, page 126). Instruct both your client and his training partner to lie on a mat with continued
Weight Training and Plyometrics
.
227
Medicine Ball Trunk Curl, continued
their knees bent (crook lying), such that their ankles are almost touching. They should then raise their trunks (without significantly moving their legs) to a stable upright position. The training partner throws a medicine ball to your client, who catches it while in the upright position, holding it close to his chest, but then moves back into the lower trunk curl position. He should stop the movement short of full range (his back should not touch the ground), then "bounce" back with a concentric trunk curl and throw the ball back to his partner. Increase the range of the curling action by having your client lie over a cushion-this allows the trunk to move into extension before moving into flexion. Be sure that movement stops short of full range in each direction in order to reduce joint loading.
Leg Raise .1'(.1.'1.
Throw
To develop
power and speed in the lower abdominals.
Make sure your client can easily perform the wall bar hanging leg raise (page 129) before attempting this movement. Your client should hang from a gymnasium beam with a ball beneath him. ,, Instruct him to grip the ball between both feet, then flex his hips and spine to throw the ball forward to a waiting partner. The partner places the ball back between your client's feet while the hips are still flexed to 90°. Your client then lowers his legs to prestretch the lower abdominals before repeating the movement.
SUMMARY
·
It is imperative that individuals be able to consistently hollow their abdomens, contract their multifidus muscles at will, and maintain neutral position before they attempt these exercises.
.
228
·
· · ·
Back Stability
After (and only after) your client has attained basic back stability using exercises presented earlier in this book, he/she can progress to using (1) machine exercises and/ or (2) plyometric exercises, each of which can further stabilize the back and help prevent future injury. Basic free weight exercises are useful for people whose jobs or sport activities demand greater back stability than that created by the earlier exercises. Advanced free weight exercises are appropriate for those whose jobs or sport activities are extremely demanding and require "explosive strength." Plyometric exercises are particularly useful for individuals who need
veryfast reaction times along with strength in their movements.
·
Because the material in this chapter is specifically designed for individuals with a history of low back pain, the exercises may differ from those you might prescribe for other individuals.
PART
ITW
Putting It All Together Although chapters 1 through 9 provide everything you really need to know in order to prescribe a very effective back stability program for virtually any client, I have summarized some ideas in chapter 10 ("Building a Back Stability Program for Your Client") that should help you synthesize the theoretical and practical material more easily. In chapter 10, you'll learn more about how to deal with pain since you generally will need to take care of that before even attempting to prescribe exercises. And I provide general tips about how to decide which exercises to prescribe for whom. Possibly the most helpful part of this chapter is the four case histories, which help you understand how to deal with four different kinds of client, from your first meeting until you discharge them. Chapter 11, "Preventing Back Injuries and Reinjuries," advocates a more proactive approach to dealing with your clients' daily activities. It is very common for people to reinjure themselves by lifting objects they had no business lifting, or by lifting them in the wrong way. Some therapists merely hand clients a pamphlet that describes proper lifting procedures, but most clients do not take written material alone very seriously. Chapter 11shows you how to teach your clients to avoid reinjury, with the suggestion that you actually do a bit of role-playing in order to help your clients internalize the theoretical principles.
229
1l((D
Building a Back Stabili!I Prog!am for Your Client We have corne full circle from the preface and seen how the three components of muscle imbalance-correction of segmental control, shortening and strengthening lax muscles, and lengthening tight muscles--combine to produce back stability. Although there is a great deal of highly varied material in previous chapters, you should nevertheless find it rather easy to tailor a unique back stability program to each client, taking these three components into account as they are needed for each individual. It is largely a question of (1) assessing where the problems lie and (2) prescribing appropriate exercises to correct the problems. Yet before you even think about a back stability program for a given individual, make sure that you should be treating the individual in the first place.
PRELIMINARY
ASSESSMENT OF YOUR
CLIENT
Especially for individuals who have experienced serious cardiovascular illness, you must decide whether exercise is appropriate at all. It is rare, but occasionally you may see someone whose general health is in such a state that the slightest additional stress could be catastrophic. If you have any doubts about an individual, be sure to have him or her obtain clearance through a medical doctor before proceeding with therapy. Note also that, although a back stability program is generally suitable for even the very unfit, it is contraindicated in some cases where people are not able to practice it correctly. If hypertensive individuals cannot be taught to hollow without holding their breath, for example, then hollowing is clearly contraindicated. And advanced exercises using weights are contraindicated in cases of reduced bone density.
Pain If clients are in pain when they first corne to you, manage the pain before proceeding with any muscle training. If you are qualified to treat the pain, 231
232
.
Back Stability
then apply whatever treatments you deem appropriate. If you are not qualified, refer clients to someone who is and work jointly with that therapist. Pain can inhibit muscle contraction and can affect alignment by making people take up positions that are less painful, but that reinforce poor alignment. It is certainly true that back stability exercise can lead to significant pain relief (e.g., multifidus training can release back spasms), but such activities work best when used as an adjunct to pain-relieving treatments. Where pain is extreme, elimination of the pain may become the primary aim of treatment. Pain that occurs through muscle spasm, or through trigger points in tight muscles, may be relieved by treatments that reduce muscle tone-various physical therapy treatments, manual therapy, and/or stretching. See Norris (1999) for details of these types of treatment. Where pain is the result of persistent overstress on a hypermobile segment, focus initial treatments on segmental control and stability. You may have to create stability passively at first (through taping or splinting), until your client has gained sufficient control of the muscular stabilizing system.
Diagnostic
Triage
Diagnostic triage categorizes low back pain into three types: simple back ache; nerve root pain (the nerve root is the "T" junction of the nerve as it joins to the spinal cord-pain from this area indicates compression of the nerve by a spinal disc or other structure); or possibly serious pathology requiring referral to a specialist (Waddell et al. 1997). See "Diagnostic Triage," page 233. I do not generally recommend referral to a specialist for simple back ache, and clients with nerve root compression do not usually require referral
if their
pain resolves within four weeks of its on-
set. Clients with possibly serious pathology require prompt referral, while those with likely cauda equina syndrome (involving a group of fine nerves at the base of the spinal cord) require immediate referral. For individuals with simple back ache or nerve root compression, you generally can begin back stability exercises immediately (with or without other physical therapy treatment). Those with serious pathology, however, may require surgical intervention before you begin back stability exercise, but please note the discussion in chapter 1, page 6, concerning the appropriateness of surgery on low back pain. Back stability exercise is a necessity as follow-up therapy for those with a previous history of back pain but no current pain, and as a preventive therapy for clients with no history of back pain (table 10.1).
Diagnostic
Triage
Diagnostic triage is the differential diagnosis between 1. Simple back pain (nonspecific low back pain-Le., pain with no specific cause) 2. Nerve root compression 3. Possibly serious spinal pathology (such as bone damage, infection, carcinoma, or pain traveling/referred from the abdomen or gastro/ urinary systems) 1. Simple
back ache: specialist referral not required
Patient aged 20-55 years Pain restricted to lumbosacral region, buttocks, or thighs Pain is "mechanical" (Le., pain changes with and can be relieved by movement) Patient otherwise in good health (no temperature, nausea/dizziness, weight loss, etc.)
2. Nerve root pain: specialist
referral not generally first four weeks, if the pain is resolving
required
within
Unilateral (one side of the body) leg pain that is worse than low back pain Pain radiates into the foot or toes Numbness and paresthesia (altered feeling) in the same area as pain Localized neurological signs (such as reduced tendon jerk and positive nerve tests) 3. Red flags (caution) promptly to specialist
for possibly
serious
spinal
pathology:
refer
Patient under 20 or over 55 years of age Nonmechanical pain (Le., pain does not improve with movement) Thoracic pain Past history of carcinoma, steroid drugs, or HIV Patient unwell or has lost weight Widespread neurological signs Obvious structural deformity (such as bone displacement after an accident, or a lump which has appeared recently) Sphincter disturbance (unable to pass water or incontinent) Gait disturbance (unable to walk correctly) Saddle anesthesia (no feeling in crotch area between the legs) Cauda equina syndrome (refer to specialist immediately-i.e., same da0 If in doubt, always refer the patient to an orthopedic physical therapist. Adapted, by permission, from G. Waddell, G. Feder, and M. Lewis, 1997, "Systematic reviews of bed rest and advice to stay active for acute low back pain:' British Journal of General Practice 47: 647-652. 233
.
234
Back Stability
Table 10.1
Use of Back Stability
Exercises
Type of back pain
Back stability
Simple
Begin immediately; fully functional.
Nerve
Serious
root compression
No history
continue
until
Begin as pain allows; refer to specialist if no marked progress within four weeks.
pathology
Previous
exercise
Use back stability surgical/medical
back pain now resolved of back pain
exercise after intervention.
Use back stability full function.
exercise
to restore
Use back stability risk of developing
exercise to reduce back pain.
Reprinted, by permission, from G. Waddell, G. Feder, and M. Lewis, 1997, "Systematic reviews of bed rest and advice to stay active for acute low back pain," British journal of General Practice 47: 647-652.
GENERAL
PRINCIPLES FOR DESIGNING A STABILITY PROGRAM
There are a few basic principles that apply in every situation:
· .
If you are not trained to properly diagnose back ailments, proceed no further until you've referred your client to a trained therapist-then work as closely with that therapist as you can, prescribing exercises appropriate to the therapist's diagnoses. Remember the general principle that bed rest is counterproductive
(see
chapter 1). Except in unusual circumstances, get your clients up and performing controlled activities as quickly as possible after an injury. Start back stability work as soon as possible after you have determined
·
· ·
that such a program is appropriate for an individual. The longer people are unstable, the more likely they are to develop compensatory postures that will need to be retrained. Always pay close attention to pain-it can be a very reliable guide. In
a careful series of assessments, it can tell you where the problems lie; throughout an individual's program, it can tell you when to stop a given exercise. Remember
the principle of specificity: prescribe
specific activities
for
specific problems/goals. This is why careful assessment is so important. Many therapists have a one-size-fits-all program. I have heard about many unhappy individuals, especially in the United States, who have visited physicians because of back pain-and the way the
Building a Back Stability Program for Your Client.
235
doctor "treated" them was to hand them a "back care pamphlet" and instruct them to do all the exercises in it! After reading part I of this book, you know that you must deal with each individual according to his or her precise symptoms. Remember the principle of overload: if the overload is not great enough, there will be no training effect; your client will merely be engaging in physical activity rather than training. Too great an overload, however, will break down tissue; and since the body cannot adapt sufficiently to match the imposed stress, overuse injury results. Carefully following the exercise programs presented in this book will enable you to achieve a training effect with your clients and to avoid overtraining injuriesa particular danger with those who have experienced low back pain or back injury.
.
Be sure that you always have a clear vision of your goal for each individual, and of the best path to reach that goal. That path should consider all systems-muscle tightness/laxness, posture, strength, flexibility,reaction speed, skill, and even emotional factors. Be careful that you do not fall into the common trap of overemphasizing a single aspect of fitness or rehabilitation. This is especially easy to do when strong-willed, generally knowledgeable clients make it clear that they have a certain problem and they want it fixed in a certain way ("I hurt my back at work, and I need to do some weight training so I can lift boxes again. . ."). Working one system in isolation can do more harm than good. Excessive flexibility in relation to strength, for example, may lead to instability of a joint. Individuals with increased strength, but without parallel improvement in muscle reaction speed, may be unable to use their extra strength in functional situations (Konradsen and Ravn 1990). Increases in either strength or flexibility that fail to improve skill may make injury more likely (Tropp et al. 1993). PARALLEL
TRACKS
A STABILITY
IN DESIGNING PROGRAM
Because the body is a complex unit of closely interconnecting systems, any approach to treatment must be holistic, even if it targets a single system. In training clients for back stability, we constantly intertwine our focuses on correcting segmental control, shortening and strengthening lax muscles, and lengthening tight muscles. The order in which you use these exercises, of course, will depend on your clients' symptoms. You ideally want to pay attention to all these areas at all times. When time constraints require that you teach only one or two exercises, stretches, etc., at a time, simply focus first on the most problematic area. In the accompanying case histories, note how I generally started with just one or two exercises, aiming to solve the most acute problem first.
236
.
Back Stability
The following sections provide suggestions for parallel exerciseprogressions. Don't (for example) just look at basic stability, proceed to correct it, and finally go on to other items only after your client can do a great hip hinge. Assess basic stability, deep abdominal control, muscle imbalance, and posture when you first see a client. At first, you may need to deal only with the most glaring deficiency, as the case histories illustrate. By your third or fourth treatment session, you generally will want to prescribe appropriate measures to correcteachdeficiency at the same time, working on each "track" during each session, and prescribing home exercises for each area. This is not as time consuming as it sounds, as many of the exercises in this book address several aims at the same time.
Assess
Back Stability
Your first task upon seeing a new client is to learn how stable her back is-and, to the degree it is not stable, to determine wherein lies the instability and to begin creating stability through appropriate activities described in chapter 4. Almost all prescriptive journeys begin in chapter 4. Your clients should not advance to actual strengthening or even stretching exercises until they have mastered the movements in that chapter. The best way to begin assessment is with the heel slide (page 170): if the pelvis tilts, your client has an unstable back and you should begin by teaching her abdominal hollowing (chapter 4, page 83). If her pelvis does not move during the heel slide, indicating a degree of stability, begin by teaching your client to control pelvic tilt (chapter 4, page 74) and to assume/ maintain the neutral position (chapter 4, page 78), without ignoring abdominal hollowing, of course. She should progress through pelvic tilt actions, to supported hip hinge exercises, and finally to free hip hinge exercises (all in chapter 4). Once your client demonstrates adequate segmental control by being able to independently control her pelvis and spine, let her progress to the good morning exercise, first without and finally with light barbell weights (chapter 9, page 216).
Assess the Degree of Deep Abdominal Control Can your client perform abdominal hollowing in the prone kneeling position? If not, follow the instructions under "Teaching Your Clients to Use Abdominal Hollowing" in chapter 4 (page 81), especially the subsection on teaching tips (page 86). Once he has mastered abdominal hollowing in all positions, help him gradually build up his strength and endurance till he can perform the movement for 10 reps, 10 seconds each, in the kneeling position. For more advanced abdominal control, he can progress to limb-loading exercises in chapter 8--€specially the heel slide (page 170) and leg lowering (page 170).
Building
Assess
a Back Stability Program for Your Client.
237
Muscle Imbalance
For each client, go through all the assessments in chapter 5 under" Assessing Stretched Muscles" (page 103) and under" Assessing Shortened Muscles" (page 106).Then proceed to correct whatever deficiency you find. For stretched or weakened abdominal muscles, for example, prescribe appropriate exercises (look at the "goal" statements) from chapter 6 under "Modifications of Traditional Abdominal Exercises" (page 124) and" Ab Roller Exercises" (page 130). For tightened muscles, refer to "Stretching Target Muscles" in chapter 5 (page 113). If clients have both tight muscles and an unstable back, I suggest that you begin with stretching exercisesyour clients first must learn tofind the neutral position before they take the second step in doing exercises to help them maintain neutral position. Some clients, especially the elderly, will have chronic muscle tightness that is virtually impossible to cure completely. Yetyou are unlikely to meet someone whom you can't help at all-€ven if you cannot help people achieve optimal posture, you probably can help them move more freely, increase their range of motion, and experience less discomfort.
Assess Posture Assessing posture goes hand-in-hand with checking muscle balance and can often give the first indication of which muscles may need to be tested for imbalance. Select the procedures under "Basic Postural Assessment" (chapter 7, page 136) that you find most useful given your availability of equipment, and thoroughly assess your client's posture. If you suspect a muscle is lengthened, test its inner-range holding ability (e.g., test the gluteals for lordotic posture); if you think it is tight, use specific tests of muscle length (e.g., for lordotic posture use the Thomas test for tight hip flexors). Then train the muscle accordingly, using inner-range holding for lengthened muscles and static or PNF stretching for tight muscles. See "Principles of Postural Correction" (page 143) and "Posture Types and How to Correct Them" (page 145).
DESIGNING AN ADVANCED STABILITY PROGRAM After clients have achieved basic back stability, they may wish to press on with more intense work because of heavy physical demands from work or from athletic activities. Chapters 8 and 9 are for such individuals.
In General, Be Specific The single most important concept is to determine, in close consultation with clients, precisely what their needs/ goals are. Does she have to lift 50pound grain bags all day at work? Is he a tennis player whose body is
238
.
Back Stability
constantly twisted and exposed to very rapid loads? Is your client a doorman who spends eight hours each day standing up and moving relatively little? Is she a caregiver who must bend over and lift bedridden patients many times a day? Every individual's specific needs will call for specific exercises to strengthen, stretch, increase reaction speed, increase accuracy of movement, or whatever. And there is no way I can suggest sequences of exercises to cover all possibilities. That is why each exercise is preceded by a "goal" statement. Once you have determined specific goals for a client, select the exercises in chapters 8 and 9 that match those goals. Choosing the exercises is relatively straightforward. Where you must be very careful is in your exercise prescriptions. I have provided basic guidelines for the exercises in each chapter, either with introductory remarks or with the exercises themselves. But these are no more than guidelines. Carefully monitor your clients as they first perform any exercise, not only to be sure they are performing the exercises correctly, but also to be sure they are performing enough reps and using sufficient load to challenge their muscles, but not to excessively load them.
Tips for Designing
Weight-Training Programs
In addition to the rather specific instructions I provide for the weighttraining exercises, here are a few more strategies you can use to guide your prescriptions of exercises. The order in which weight-training exercises are performed in a single exercise session is important. In general, have your clients work large muscle groups first with multijoint exercises, and smaller groups second using isolation movements. A multijoint exercise is one that works a number of muscles, including those with a large muscle mass. For example, the bench press works the pectoral muscles and the triceps. Because the triceps are far smaller than the pectorals, they fatigue first and so are the limiting factor in the exercise. If the triceps are worked first, fewer bench press movements are possible and the pectoral muscles will not be sufficiently challenged. Another method of combining exercises is to use a superset (i.e., to work the muscles on one side of a limb, and then immediately [without a rest] work those on the opposing side). This type of training keeps the blood within a body part, while the individual muscles themselves have some rest. A typical superset routine would involve biceps-triceps-biceps. One way to provide maximum challenge to muscles is to use pyramid training. Have your client perform 12 repetitions with an average weight for the first set, 10 reps with a heavier weight for the second set, and finally 8 reps with the heaviest weight he can manage for the final set. In this way, the muscle is worked maximally, but only when it is thoroughly warmed up. See Norris (1995b) for further details of weight-training programs.
Building a Back Stability Program for Your Client.
CASE
239
HISTORY
The Overweight
Client
A 42-year-old man with a history of persistent back pain, AH worked on a production line. He was about 56 pounds overweight, with marked lordotic posture. The goal of my treatment was first to reduce pain and then to restore postural balance. In the first treatment session, I instructed AH to perform supine lying lumbar flexion, bringing the knees to the chest with overpressure to encourage flexion of the lumbar spine. The principle here was that AH's lordotic posture was placing an excessive extension stress on his low back. The flexion exercise that I used was designed to neutralize this. With repetition (15-25 reps), his low back pain eased. I showed him how to get onto and off the floor without bending and advised him to practice this exercise every two hours of the waking day for two days. I gave AH general advice concerning back care and resting, used standard physical therapy modalities to reduce local pain, and referred him to a dietician to begin a weight-loss program. By the second treatment session two days later, AH's pain was markedly reduced. I started him on a general aerobic exercise session with his back supported-he used static cycling (seat and handlebar adjusted to minimize back str~ss) and a ski trainer to perform heart-rate-controlled exercise for 15-20 minutes every other day. At the second session, I also started AH on stability training, beginning with abdominal hollowing in the 4-point kneeling position and using a webbing belt around his abdomen. Since AH was unable to perform abdominal hollowing correctly, I provided a surface EMG unit to give feedback. It took 40 minutes to re-educate deep abdominal contraction using surface EMG, palpation, and voice encouragement. But since AH was still unable to perform the exercise unaided, I did not yet prescribe abdominal hollowing as a home exercise. AH continued with his back care and aerobic training for two more days. During his third treatment session, AH was able to perform abdominal hollowing with a 5- to 7-second hold for 3 repetitions. We had to work hard to help him refrain from holding his breath-I encouraged him to count out loud as he performed abdominal hollowing, to show that he was breathing normally. AH progressed in hollowing his abdomen but found it difficult to control the neutral position of his spine without my feedback. I taught him abdominal hollowing in wall-support standing to allow him to practice at home without having to think about his spine. He used a belt, focusing on pulling his abdomina Is in and up from the belt. He particularly liked this exercise, as it began to give his abdominal wall a flatter appearance-and, combined with weight loss, AH's physical appearance began to be leaner. continued
I'
240
I
.
Back Stability
Case History, continued We repeatedly set goals: goals for weight loss, numbers of repetitions performed, holding time of exercises, and heart-rate-monitored exercise. AH's low back pain had now gone, and he progressed from abdominal hollowing in standing to standing posterior pelvic tilt. Since his cardiopulmonary fitness (measured as heart-rate recovery) had improved with a decline in percent body fat (38% to 30%), I had him increase his aerobic activity. He still used nonweightbearing or partial weightbearing activities in the gymnasium to reduce joint loading, but now he began walking (on grass/gravel with shock absorbing sports shoes) for 15-20 minutes daily. In an attempt to shorten AH's rectus abdominis, to his standing posterior pelvic tilt I added posterior tilt in the lying position, held for 20-30 seconds (breathing normally). AH had short hip flexors and hamstrings, and he stretched them using the half-kneeling hip flexor stretch and active knee extension. AH built up his stability work with kneeling activities (knee raise, 10 repetitions on each leg, holding for 10 seconds) and began hollowing his abdomen regularly during his walking. I discharged AH from physical therapy to a personal trainer at a local gymnasium, where he incorporated stability work into a general fitness and weight-loss program. Points to Note V' AH had mechanical back pain brought on by his lordotic posture. V' Posture correction began with weight loss. V' Because AH was initially unable to perform correct abdominal hollowing, I did not give this as a home exercise. V' Surface EMG proved useful in initially teaching abdominal hollowing. V' We repeatedly used goal setting. V' Since AH liked the standing abdominal intensely.
hollowing exercise, I used it
V' AH used aerobic training to aid general fitness as well as specific back stability. V' The back stability program formed a focus for more general lifestyle changes. V' When discharged from physical therapy care, AH continued stability program in another setting. CASE
Poor Stability
the back
HISTORY
in an Athlete
Twenty-six-year-old HC trains daily in a gymnasium, using either weighttraining apparatus (40 minutes) plus cardiopulmonary apparatus (20 mincontinued
Building
a Back Stability Program for Your Client.
241
Case History, continued utes), or step aerobics (60 minutes). One day she complained of low back pain the morning after training. X-ray examination of the low back and pelvic joints showed no abnormality, and blood tests were normal. She was referred to me for physical therapy three months after the onset of pain. Her lumbar spine and sacroiliac joints were unremarkable upon examination, but repeated lumbar extension-especially anterior pelvic tilt-caused pain. Kinesiological examination (movement analysis) showed poor lumbar stability with overhead movements and with hip extension actions in standing. HC stated that two exercises in particular gave rise to her pain following workouts: standing hip extension on a "multihip" unit that targets the gluteals and repeated overhead pressing actions in standing with an aerobics bar. Examination of these moves showed that her pelvis moved rapidly into anterior tilt and remained in that position throughout the exercises. In assessing He's abdominal musculature, I found high tone in the superficial abdomina Is, with marked muscular definition of the rectus abdominis (the "six pack"). Yet she performed poorly on stability tests, being unable to perform abdominal hollowing in 4-point kneeling while maintaining a neutral lumbar spine. In the heel slide action monitored by a pressure biofeedback unit, HC was unable to perform more than 3 repetitions before her pelvis tilted anteriorly. In 4-point kneeling, leg lifting actions caused marked muscle quivering, demonstrating poor performance. He's gross segmental control was also poor-she was unable to perform a controlled hip hinge action. She moved not into spinal flexion (like most people) but into extension, anteriorly tilting her pelvis and hyperextending her lumbar spine. In her first treatment session, I had her perform supine knee and hip flexion, to press the lumbar spine into flexion. I told her to do these movements at the end of each workout period. I temporarily removed the overhead press and hip extension exercises from her gym program. Following her first two workout periods after the first session, HC noted reduced pain in the mornings. I used video feedback to show HC her performance in the hip extension and overhead exercises. She was surprised, having been unaware of her lack of alignment. I had HC try to perform abdominal hollowing in 4-point kneeling, and she was able to perform the exercise within 2-3 minutes of being shown the movement. She then used abdominal hollowing in wallsupport standing, progressing to free standing after 2 sets of 10 repetitions. She used abdominal hollowing in free standing and free (stool) sitting during her gym workouts, performing a single set with a 3D-second hold, breathing normally. HC progressed quickly (within two weeks) to supine lying heel slide and finally to supine lying foot drop (2 sets, 10 reps, 3D-second hold). I prescribed 4-point kneeling knee movements to improve stability control. continued
242
.
Back Stability
Case History, continued By the third treatment session (10 days after beginning treatment), noting that HC was able to perform abdominal hollowing for 10 reps, holding each for 30 seconds, I prescribed the hip hinge action. Initially I had her use controlled pelvic tilt in crook lying. In that same session, she progressed to pelvic tilt in wall-support standing, and finally in free standing. She performed the hip hinge with a stick held along the length of the spine to give feedback about spinal position. Initially she performed the exercise next to a mirror, then without a mirror, then without a stick, and finally with her eyes closed (to overload proprioception). HC had mastered the hip hinge action by her fourth treatment session-at which point I had her perform overhead pressing actions with a stick, and perform hip extensions on the multihip unit with minimal weight. Her goal was to maintain abdominal hollowing and a neutral lumbar alignment throughout the exercise. I incorporated stability principles of abdominal hollowing (30% max contraction) and neutral lumbar alignment into all of He's exercise activities. PoiniS to' Note V' HC had excellent cosmetic appearance of her abdominal region (superficial abdominals), but poor deep abdominal control. V' She was unable to maintain neutral lumbar alignment, she had high muscle tone.
even though
V' I used extensive movement analysis and made a point of observing the exercises that HC practiced in her gym. V' She had poor segmental control, moving into extension rather than flexion as is more common. V' Video feedback permitted HC to see her alignment. use of a stick increased feedback.
Mirrors and the
V' HC was a regular exerciser and had good body visualization. able to pick up new exercise techniques very quickly. V' Deep abdominal training and segmental formed the basis of her program.
She was
control (hip hinge action)
V' I waited until after HC was pain free to begin the basic stability program.
CASE
HISTORY
Acute
Pain
DB, 34 years old, came to me with acute simple low back pain that was localized to the lower lumbar region and minimally referred into the right buttock. The pain was mechanical in nature, made worse by lumbar flexion continued
Building
a Back Stability Program for Your Client.
243
Case History. continued
and better by lumbar extension. Initially I treated the pain, using physical therapy and lumbar manipulation. Then I had her begin multifidus contractions in left side lying, while I palpated the right multifidus and encouraged her to attempt to "swell" the muscle beneath my fingers. Although unable to perform this action at first, by the end of the second treatment session she was minimally able to contract the multifidus. I had her perform rhythmic stabilizations in left side lying-I placed pressure over her pelvis and shoulder to encourage spinal rotation and instructed DB to resist this motion with slight muscle contraction. As contraction built in intensity, I changed my hand position to resist spinal rotation in the opposite direction. The combination of rhythmic stabilization and isolated multifidus contractions gave substantial pain relief, with pain reducing from 8 to 3 on a subjective scale (10 = most intense pain, 1 = least intense). In the second treatment session, I introduced abdominal hollowing. As DB lay prone, I instructed her to draw her abdomen in, in an attempt to pull her tummy away from the surface of the treatment table. Since DB was at first unable to perform this action, I used pressure biofeedback, placing the bladder of the biofeedback unit beneath her abdomen just above the top of her pelvis and inflating the bladder sufficiently for DB to feel pressure over the abdomen. I instructed her to draw in her abdomen in an attempt to pull away from the biofeedback unit, thereby reducing the pressure on the bag. I wanted DB to perform the exercise at home, but since she was unable to identify when she was performing abdominal hollowing correctly, I brought her husband into the treatment session and showed him how to assist her. At home, DB placed a folded towel beneath her abdomen in the same position that the biofeedback bladder had occupied. I instructed DB's husband to gently try to slide the towel out from beneath DB's abdomen, while his wife drew in her abdomen sufficiently to take her weight from the towel and permit it to be pulled away. I instructed her to repeat this exercise 3 times daily, performing 10 reps each time. Once DB was able to perform the hollowing action unaided in the prone lying position, I had her progress to abdominal hollowing in kneeling and sitting positions. While aiding DB in her back stability training, I also instructed her on general back care, with emphasis on correct sitting and resting postures. I also taught her basic lifting techniques for use in the home. She progressed through the early stages of the back stability program using the heel slide, kneeling leg lift, and hip hinge actions. I then referred her to an exercise instructor at a local health club, to perform a general exercise program incorporating back stability principles. Points fo Note Because DB was in intense pain, I used physical therapy for pain relief at the beginning of her first session, before introducing her to stability exercises later in the session. continued
244
. Back Stability
Case History, cOl1til1ued
V On the first day, I began teaching her to control the multifidus, helped in pain relief. V I used pressure biofeedback and palpation.
which
v I showed a family member how to assist with DB's abdominal hollowing exercises at home. v DB continued her back stability training at a health club, along with general fitness activities.
CASE
Patient
HISTORY
Unwilling
to Exercise
SD was a 53-year-old manual worker in a food company. About 42 pounds overweight, he had marked abdominal sagging and chronic back pain that was localized to the lower lumbar region. His erector spinae muscles were tight and thickened. When standing, SD had a flattened lumbar curve, showing a typical "flatback" posture. Examination of range of movement revealed a lack of lumbar extension, and grossly limited pelvic tilt during I forward flexion movements. The pelvis contributed little to forward bending since most forward movement came from the upper lumbar and lower thoracic spine. Examination of SD's lifting techniques showed repeated bending actions with his legs straight, and adoption of poor resting positions with marked spinal flexion. SD had attended his company's manual handling course and even a refresher course, but his line manager confirmed SD's unwillingness to practice correct handling procedures on a regular basis. My initial physical therapy treatment targeted pain relief, but I also wanted to make SD contribute to his own treatment by taking part in exercise. It required considerable persuasion to convince SD to begin exercising! I taught him passive extension procedures that involved his lying on the floor and pressing with his arms to encourage restoration of a normal lumbar curve. During this exercise, his pain reduced in intensity, and localized to the lumbar region, shrinking in size. To encourage correct bending, I placed 15-inch-long strips of nonelastic tape on either side of his spine, from the pelvic region to the mid thoracic area. As SD bent forward, the I tape tightened on the skin, restricting spinal flexion and encouraging him to bend from the knees. I taught SD pelvic tilting, first passively and then actively, during the first treatment session. Although I instructed him to continue practicing at home, he showed little willingness to do so. I therefore instructed him to visit the company medical center daily, to practice his exercises under supervision of a physical therapy assistant or nurse. He did this each working day for two weeks.
cOl1til1ued
Building
a Back Stability Program for Your Client.
245
Case History, continued In his second treatment session, I started SO on a single abdominal hollowing exercise, choosing hollowing in wall-supported standing (with a webbing belt) since it was easiest for him to perform. With the use of a mirror, palpation, and surface EMG feedback, he was able to perform consistent hollowing by his third treatment session. I then encouraged him to practice hollowing without aids in wall-support standing, instructing him to draw his abdominal wall away from the waistband of his trousers (without holding his breath) and to hold the contraction for 5-10 seconds. I told him to repeat the exercise 3 times daily for 10 repetitions. By our third session, the combination of increased flexibility to pelvic tilt and back taping made SO bend more correctly. I assigned hamstring stretching exercises (active knee extension) in a lying position-lO reps, holding each for 10 seconds, during his treatment sessions on alternate working days. I also referred him to the company occupational health nurse for advice on diet and monitored weight loss. Video feedback helped SO learn correct bending techniques; and he practiced the hip hinge action (with a stick placed along the length of the spine) first with and then without video feedback. After four treatment sessions and 10 days of supervised exercise, SO was pain free. (But I also discovered that SO stopped practicing his exercise program two weeks after treatment began!) I encouraged him to perform the hollowing procedure when walking to his tea break (morning and afternoon) and his lunch break. The action was to contract the muscles to pull away from the waistband, hold the contraction while taking 10 steps, relax for 10 steps, and begin over againa technique known as "postural walking." I told him to continue this contraction-and-rest procedure for the full length of the walk (about 5 minutes). Because this action was easy to perform and was built into SO's daily activity, he received it well. Three months after his first appointment, SO was still practicing the postural walking procedure daily. He reported a feeling of "strength" in his abdomen, with the added advantage of increased tone and a flatter stomach. Points to Note If' SO had a flatback posture and chronic back pain. If' Previous to my seeing him, SO had received only medication and passive physical treatments. If' He had taken no active part in the care of his own back condition. If' Back taping encouraged him to move more correctly. If' Because SO was unwilling to exercise on his own, I arranged for him to do his exercises at work under supervision of a PT assistant. If' Although he did not continue abdominal hollowing exercises at home, he liked the "postural walking" approach-which we therefore built into his daily activities.
.
246
· · · ·
Back Stability
SUMMARY When you first see a client, assess him or her for basic stability, posture, alignment, segmental control, and muscle imbalance.
Treat pain before proceeding with stability exercises. In many cases, your first several sessions will address only the most severe deficiency. By the third or fourth session, if not earlier, you generally will want to focus on all aspects of stability, prescribing exercises for any area where there is a deficit.
·
Prescribe specific exercises for specific goals; there is no such thing as a "general" prescription for back stability.
·
The principle of specificity applies also to advanced
·
stability exercises.
When prescribing procedures from chapters 8 or 9, target them to your clients' specific goals and needs, whether they are related to the workplace or to the playing field. Four case histories provide step-by-step examples of treatment programs for individuals with varying kinds of problems.
1l1l Preventing Back Injuries and Reinjuries It is surprising how many people go to a great deal of effort to follow a rehabilitation program after a back injury, only to reinjure the back by doing something foolish at home or at work. I strongly urge you to take a few minutes to go over the information in this chapter with your clients so that they will have an increased probability of maintaining the progress you've helped them achieve. In the large majority of cases, according to my experience, you will meet with mild resistance or even boredom, because most people will say (at least to themselves if not to you), "Yes, yes, I know all that, use your legs and not your back, don't bend over. . . ." Yet a significant number of these same people will end up doing something outrageously silly because they haven't internalized proper safety procedures. I suggest that you actually role play these ideas with your clients. After leading them through the information in this chapter, take just 5 or 10 minutes to point to various objects and say, "All right, let's say you have to carry that chair into the next room and set it against the wall. Plan it out for me, explain to me the proper lifting/carrying procedure, then show me how you would position yourself for the lift." (I don't suggest letting anyone do a heavy or awkward lift, for reasons of liability.)
KEEP THE SPINE VERTICAL Merely reaching over a table can tremendously leverage the stress on the spine. Picking up a mug of coffee from the opposite side of a table, for example, can produce more force against the intervertebral disks than lifting a 20-pound weight next to one's body. Remember, torque = force x the length of the lever arm. If the spine remains vertical, leverage is minimal. If the spine is allowed to move toward the horizontal, higher leverage forces increase the tendency for the spine to flex, loading the spinal tissues. An analogy: when a flexible fishing rod is held vertically, it remains 247
248
.
Back Stability
straight; if you tilt it, it bends under its own weight. In order to keep the rod straight in a tilted or horizontal position, you must support its weight. The same principle applies to the back. If you want to move your back away from the vertical, you should support it by placing your hand onto a nearby tabletop or chair or whatever, or onto your knee if nothing else is available. The additional support greatly reduces the stress on the spine and enables you to maintain correct alignment. Repeated flexion also adds to spinal stress, greatly increasing discal pressure and continually stretching the posterior spinal tissues. Over time, repeated flexion can lead to tissue breakdown. Microtrauma of this type gives rise to classical postural pain syndromes (McKenzie 1981). Instruct your clients to reduce their total amount of bending in anyone day by using more effective movements and by improving general back care. Figure 11.1 shows examples of poor general back care, along with alternatives for reducing stress on the spine.
~
Support the spine whenever it is not vertical, and reduce the total amount of bending.
PRINCIPLES
OF LIFTING IN THE AND ON THE JOB
HOME
Both at home and at work, your clients should follow the principles of good back stability in any lifting or other manual tasks. Most simply stated, they must plan their actions carefully and minimize the forces of the lift.
Planning Planning prevents surprises. One of the most common reasons for lifting injuries is failure to assess the entire situation before trying to move an object. Tell your clients they must evaluate three areas: 1. Assess the environment. Note the floor surface. Is it uneven? Is it wet? Are there potential trip hazards? They should plan the entire path over which they will carry the object. Does the path involve going through a doorway? If so, is it accessible and open? Is it wide enough? (It is amazing how often people will carry a couch or desk up to a doorway, only to discover the opening is too small!) Where is the object to be placed? If it is to go on a table, is there room for it or do other items need to be moved first? 2. Assess the object. The distribution of the object's weight can be even more important than the absolute weight. The heaviest part of the object should be held close to the body to reduce the leverage effect, and
Correct
/'
Incorrect
X
Vacuuming
Removing clothes from the dryer
Reaching for object on a high shelf
Lifting (or even talking with) a small child
Figure 11.1
Proper
and improper
back care in the home. 249
250
. BackStability
individuals must feel comfortable with the weight lifted in relation to their own health status, training, and capability. They should consider the size and shape of the object: a light object that is very bulky or that may shift (e.g., a container of powder or fluid) offers a greater potential for injury. They must also consider any possible danger from the contents-if a container holds acid, or a scalding liquid, what would happen in the event of an unforeseen accident? 3. Assess themselves. Do they feel confident that a lift is within their capability? Individuals with a knee injury, for example, may not be able to bend their knees sufficiently to lift the object in a correct manner. Are there any relevant medical conditions? Pregnant women should severely restrict their lifting; and individuals with heart disease, low back pain, or hip pathology will have reduced capacities. Many people injure their backs by trying to lift objects they suspected were too heavy for them. I often hear something like "I was afraid I couldn't lift it, but it had to be moved and I didn't have time to find help" when I examine people following back injuries. Especially in men, "machismo" is a very common and very dangerous attitude. Emphasize to your clients that it is in no way "wimpy" to admit they should not lift a given item. Such a statement in fact shows great wisdom and maturity. If special training is generally needed before a certain kind of lift, and if a person has not received that training, he certainly must not attempt it. In general, aspect of a lift, they should not attempt it. KEY POINT: the slightest safely.
if individuals
are unsure
about
any
individuals should not attempt any lift if they have doubts about their abilities to perform the lift
Minimizing the Stress of a Lift There are several ways to reduce the physical stress of a lift. The Safe Zone The center of gravity of the human body typically lies at the 52/53 level. Pulling an object near to this "safe zone" reduces the leverage forces acting on the body; allowing the object to move farther away from this point increases the leverage and therefore the stress. If holding an object within the safe zone next to the pelvis represents 100% lifting capacity, this capacity is reduced by 20% when the object is held a forearm's length from the body, and by 75% when the object is lifted at arm's length. Teach your clients to pull objects they are lifting toward the body's center of gravity at the sacrum-to pull them into the safe zone as soon as possible and keep them there as long as possible. When lifting something
Preventing
Back Injuries
and Reinjuries
.
251
from the floor, they should pull it in toward the body early in the lift by sliding the object along the floor. Only when the object is pulled close to the safe zone should the lift begin. Although it may not be possible to keep the object within the safe zone during the entire lift, the longer it is held there, the better. If a lift takes a total of 15 seconds to complete, it will be performed far more safely if the object is within the safe zone for 12 of the 15 seconds than if it is there for only 5 seconds. Since the lift takes the same total time in each case, lifting safely will not slow a person down. KEY POINT: I
Pull an object into the "safe zone" (near the
sacrum) as soon as possible during a lift, and keep it there for as long as possible.
Appropriate Stance and Grip Instruct your clients to use two hands when lifting a heavy object from the floor. They should stand at the comer of the object, with the feet at 90° to each other (figure 11.2). With this foot position, the knees pass to the
Figure 11.2 Double-handed
lift.
252
.
Back Stability
sides of the object as they are bent. At least one foot must stay flat on the floor, to aid stability. The hands should grip under the object ("hook grip") rather than merely at its sides, to avoid their slipping-elbows in to aid power; knees bent; the back aligned and near vertical for the majority of the lift (only when the object is approaching the floor, when the individual is setting it down, is the back allowed to flex slightly). Individuals should look up as they lift, to aid the general feeling of back extension; and their hips should remain below the shoulders at all times. For certain heavy, large objects such as a sack of grain or a bag of concrete (figure 11.3), suggest a modification of the double-handed lift called
@ Figure 11.3 (1) Bend knees to get close to the sack, gripping it at the top; (2) rapidly straighten the legs and pull the sack up high; (3) dip down beneath the sack as its momentum continues to carry it upward; (4) straighten the legs to stand up, holding the sack high against the chest.
Preventing Back Injuries and Reinjuries
.
253
a snatch lift. The snatch lift uses speed and momentum to reduce the strength needed for the lift, but is only possible for objects that can be grasped at the top. It is highly effective, but requires great skill and therefore practice. Since it is performed rapidly, there is little margin for error. The person lifting uses a position similar to that used for the double-handed lift, except the squat is not as deep. Gripping the object at its top, the individual keeps his back straight and his legs somewhat bent. The action is to rapidly straighten the legs and raise onto the toes (as with the power clean exercise, page 221) while pulling the object upward. Most of the power for the lift comes from the legs, the arm pull being used mostly to transmit the power and guide the path of the object. The object's momentum carries it upward-and at the height of its movement (when its weight feels minimal), the individual changes his grip to place his hands under the object and pull it firmly into the safe zone. Single-handed lifts are appropriate for lighter objects (figure 11.4). The individual should assume a lunge position, with feet shoulder-width apart and one foot forward of the other. If the right hand is used to lift, the left foot leads the movement and the left hand may be placed on the left knee for support. The back remains in its neutral position and is kept near the vertical throughout the lift. The knee of the forward leg should pass just over the foot, but no farther, so that the tibia of the leading leg is nearly vertical-this way the individual will be pressing her hand down on a more stable lower leg. If the leading foot is dorsiflexed too far, the hand pressing down on the knee will increase the range of dorsiflexion and make it more difficult to raise the body from the ground. Pushing and pulling activities can also place considerable stress on the back if they are performed incorrectly. It is essential that back alignment is maintained, and that the power for the movement comes from the legs rather than from the spine. Instruct your clients to begin a push either facing forward with their hands on the object and their arms straight, or facing backward with their backs flat against the object. In either case, they should keep their pelvises in neutral position and produce most of the power for pushing/pulling in the legs-power that is directed through the straight, stable spine to the object being moved. Make sure your clients know to take only small steps during the push/pull-overly large steps will overstretch the body and pull the spine out of alignment.
Figure 11.4 Single-handed
lift.
.
254
Back Stability
SUMMARY
· ·
Individuals should keep their spines vertical, or as near vertical as possible, during a lift. Repeated spinal flexion during lifting can lead to serious breakdown of tissues. Whenever the spine is not vertical, it should be supported by placing a hand either on a stable object or on the bent knee. Before lifting any object, individuals should plan the move: they should assess the environment, the object, and their own capabilities.
· ·
· ·
. .
If there is any doubt in individuals'
minds that they can safely lift/
carry an object, they should refrain from doing so. The "safe zone" is near the sacrum, since the average person's center of gravity is at approximately the S2/S3level. Lifted objects should be brought to the safe zone as quickly as possible, and remain there as long as possible. Individuals should use two hands to lift heavy objects. When lifting lighter objects with only one hand, they should place the free hand on a bent knee to provide support for the spine. The "snatch lift" is useful for lifting heavy objects that can be grasped at the top, but the movement is difficult and should be practiced before it is used.
Bibliography Adams, M. 1989. Letter to the editor. Spine 14:1272. Adams, M.A., and Dolan, P. 1997. The combined function of the spine, pelvis, and legs when lifting with a straight back. In Movement, stability and low back pain, ed. A. Vleeming. V. Mooney, T. Dorman, e. Snijders, and R Stoeckart. New York: Churchill Livingstone. Adams, M.A, and Hutton, W.e. 1983. The mechanical function of the lumbar apophyseal joints Spine 8:327-30. Adams, M.A.; Hutton, w.e.; and Stott,J.R.R. 1980. The resistance to flexion of the lumbar intervertebral joint. Spine 5:245-53. Adams, M.A.; McNally, D.5.; Chinn, H.; and Dolan, P. 1994. Posture and the compressive strength of the lumbar spine. Clinical Biomechanics 9:5-14. Allan, D.B., and Waddell, G. 1989. An historical perspective on tow back pain and disability. Acta Orthop Scand (Suppl) 60:1-5. Allison, G.; Kendle, K.; Roll, S.; Schupelius, J.; Scott, Q.; and Panizza, J. 1998. The role of the diaphragm during abdominal hollowing exercises. Australian Journal of Physiotherapy 44:95-102. Andersson, E.; Oddsson, L.; Grundstrom, H.; and Thorstensson, A 1995. The role of the psoas and iliacus muscles for stability and movement of the lumbar spine, pelvis and hip. Scandinawln Journal of Medicine and Science in Sports 5:1()'16. Appell, H.J. 1990. Muscular atrophy following immobilisation: a review. Sports Medicine 10:42-58. Aruin, AS., and Latach, M.L. 1995. Directional specificity of postural muscles in feed-forward postural reactions during fast voluntary ann movements. Experimental Brain Research 103:323-32. Aspden, R.M. 1987. Intra-abdominal pressure and its role in spinal mechanics. Clinical Biomechanics 2:168-74. Aspden, RM. 1989. The spine as an arch. A new mathematical model. Spine 14:266-74. Aspden, R.M. 1992. Review of the functional anatomy of the spinal ligaments and the lumbar erector spinae muscles. Clinical Anatomy 5:372-87. Atkinson, H.W. 1986. Principles of treatment. In Cash's textbaok of neurology for physiotherapists, 4th edition, ed. P.A Downie. London: Faber and Faber. Baechle, T.R 1994. Essentials of strength training and conditioning. Champaign, II.: Human Kinetics. Bandy, W.D., and Irion, J.M. 1994. The effect of time on static stretch of the flexibility of the hamstring muscles. Physical Therapy 74:845-52. Barrack, R.L., and Skinner, H.B. 1990. The sensory function of knee ligaments. In Knee ligaments: structure, function, and injury, ed. D. Daniel. New York: Raven Press. Barrack, RL.; Skinner, H.B.; and Brunet, G. 1983. Joint kinesthesia in the highly trained knee. Journal of Sports Medicine and Physical Fitness 24:18-20. Barrett, D.5.; Cobb, AG.; and Bentley, G. 1991. Joint proprioception in normal, osteoarthritic, and replaced knees. Journal of Bone and Joint Surgery 73B:53-56. Bartelink, D.L. 1957.The role of abdominal pressure in relieving the pressure on the lumbar intervertebral discs. Journal of Bone and Joint Surgery 398:718-25. Bastide, G.; Zadeh, J.; and Lefebre, D. 1989. Are the little muscles what we think they are? Surgical aud Radiological Anatomy 11:255-56. Beard, D.J.; Kyberd, P.J.; O'Connor, J.J.; Fergusson, e.M.; and Dodd, C.A.F. 1994. Reflex hamstring contraction latency in anterior cruciate ligament deficiency. JournalofOrthopaedicResearch12:219-28. Beiring-Sorensen, R. 1984. Physical measurement as risk indicators for low back trouble over a one year period. Spine 9:106-19. Bernhardt, M.; White, A.A.; Panjabi, M.M. 1992. Lumbar spine instability. In The lumbar spine and back pain. 4th ed., ed. M.l.V. Jayson. Edinburgh: Churchill Livingstone. Bernier, J.N., and Perrin, D.H. 1998. Effect of coordination training on proprioception of the functionally unstable ankle. Journal of Orthopedic and Sports Physical Therapy 27:264-75. Biedermann, H.J.; Shanks, G.L.; Forrest, W.J.; and Inglis, J. 1991. Power spectrum analyses of electromyographic activity. Spine 16:1179-84. Boden, S.D.; Davis, D.O.; and Dina, T.S. 1990. Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects. Journal of Bone and Joint Surgery [Ami 72:403. Bogduk, N.; and Engel. R 1984. The menisci of the lumbar zygapophyseal joints. A review of their anatomy and clinical significance. Spine 9:454-60. Bogduk, N.; and Jull, G. 1985. The theoretical pathology of acute locked back: a basis for manipulative therapy. Manual Medicine 1:78-82. 255
256
.
Bibliography
Bogduk,
N.; Pearcy, M.; and Hadfield, G. 1992. Anatomy and biomechanics of psoas major. Clinical 7:109-19. Bogduk, N., and Twomey, L.T. 1987. Clinical anatomy of the lumbar spine. Edinburgh: Churchill Livingstone. Bogduk, N., and Twomey, L.T. 1991. Clinical anatomy of the lumbar spine. 2d ed. Edinburgh: Churchill Biomec1umics
Livingstone.
Bradford,
F.K., and Spurling,
Bullock-Saxton,
RG. 1945. The intervertebral
J. 1988. Normal
and
abnormal
postures
disc. Springfield, in the sagittal
low back pain. Physiotherapy Practice 4:94-104. Bullock-Saxton,). 1993. Postural alignment in standing: a repeatability iotherapy 39:25-29. Bullock-Saxton, J.E.; Bullock, M.I.; Tod, C; Riley, D.R; and Morgan, young adult men and women. New Zealand journal of Physiotherapy Bush, K.; Cowan, N.; and Katz, D.E. 1992. The natural history of sciatica
IL: Charles C Thomas.
plane
and
their
study. Australian
relationship journal
to
of Phys-
A.E. 1991. Postural stability in 3:7-10. associated with disc pathology: a prospective study with clinical and independent radiographic follow up. Spine 17:1205-12. Cailliet, R 1981. Low back pain syndrome. 3d ed. Philadelphia: Davis. Cailliet, R 1983. Soft tissue pain and disability. Philadelphia: Davis. Chartered Society of Physiotherapy (CSP). 1998. Low backpain. Information for sufferers. [Online]. Available: http:.I'www.csp.org.uk [October 15, 1999]. Cappozzo, A.; Felici, F.; Figura, F.; and Gazzani, F. 1985. Lumbar spine loading during half-squat exercises. Medicine and Science in Sports and Exercise 17(5):613-20. Cholewicki, J., and McGill, S.M. 1992. Lumbar posterior ligament involvement during extremely heavy lifts estimated from fluoroscopic measurements. journal of Biomechanics 25(1):17-28. Comerford, M. 1995. Muscle imbalance. Course notes. Nottingham School of Physiotherapy. Comerford, M. 1998. Dynamic stability. Physiotools compatible computer programme. Physiotools development office. Pihapolku F. 02420. Jorvas. Finland. Cornwall, M.W.; Melinda, P.B.; and Barry, S. 1991. Effect of mental practice on isometric muscular strength. journal of Orthopedic and Sparts Physical Therapy 13:217-23. Cresswell, A.G.; Grundstrom, H.; and Thorstensson, A. 1992. Observations on intra-abdominal pressure and patterns of abdominal intra-muscular activity in man. Acta Physiol Scand 144:409-18. Cresswell, A.G.; Oddsson, L.; and Thorstensson, A. 1994. The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure whiJe standing. Experimental Brain Research 98:336-41. Crock, H.V., and Yoshizawa, H. 1976. The blood supply of the lumbar vertebral column. Clinical Orthopaedics 115:6-21. Crowell, RD.; Cummings, G.5.; Walker,J.R; and TIllman, L.J. 1994. Intra tester and intertester reliability and validity of measures on innominate bone inclination. Journal of Orthopedic and Sports Physical Therapy Davis,
20:88-97.
P.R., and
Troup,
JD.G.
1964. Pressures
Ergonomics 7:465-74. Day, J.W.; Smidt, G.L.; and Lehmann, 64:510-16. Delitto, R.S.; Rose,
S.J.; and
lifting. Physical Therapy Deutsch,
F.E. 1996. Isolated
of Manipulative Deyo, RA.; Diehl, New
England
in the trunk
cavities
T. 1984. Effect of pelvic
pulling.
tilt on standing
pushing,
posture.
and
Physical
lifting. Therapy
Apts, D.W. 1987. Electromyographic analysis of two techniques for squat 67:1329-34. lumbar strengthening in the rehabilitation of chronic low back pain. Journal
and Physiological Therapeutics 19:124-33. A.K.; and Rosenthal, M. 1986. How many Journal
when
of Medicine
days
of bed
rest for acute
low back
pain.
315:1064.
Eie, N. 1966. Load capacity of the low back. Journal of Oslo City Hospitals 16:73-98. Enoka, R.M. 1988. Neuromechanical basis of kinesiology. Champaign, IL: Human Kinetics. Etnyre, B.R., and Abraham, L.D. 1986. H-reflex changes during static stretching and two variations proprioceptive 010gy63:174-79. Etnyre, B.R., and
neuromuscular Lee,
E.J. 1987.
facilitation Comments
techniques.
Electroencephalography
on proprioceptive
Research Quarterly for Exercise and Sport 58:184-88. Fansler, CL.; Poff, CL.; and Shepard, K.F. 1985. Effects of mental Physical T.herapy 65:1332-38. Farfan, H.F. 1988. Biomechanics of the lumbar spine. In Managing Willis. London: Churchill Livingstone.
neuromuscular practice
and Clinical
Neurophysi-
facilitation
stretching.
on balance
in elderly
of
women.
low back pain. 2d ed., ed. W.H. Kirkaldy-
Farfan, H.F.; Osteria, V.; and Lamy, C 1976. The mechanical etiology of spondylolysis and spondylolisthesis. Clinical Orthopedics and Related Research 117:40-55. Freeman, M.A.R.; Dean, M.R.E.; and Hanham, I.W.F. 1965. The etiology and prevention of functional instability of the foot. Journal of Bone and joint Surgery 478(4):678-85.
.
Bibliography
257
Friedli, WG.; Hallet, M.; and Simon, S.R. 1984. Postural adjustments associated with rapid voluntary arm movements. Electromyographic data. Journal of Neurology, Neurosurgery and Psychiatry47:611-22. Frymoyer, J.W., and Cats-Baril, W.L. 1991. An overview of the incidences and costs of low back pain. Orthopedic Clinics of North America 22:263. Frymoyer, J.W., and Gordon, S.L. 1989. Symposium on new perspectives on low back pain. Park Ridge, IL: American Academy of Orthopedic Surgeons. Goldspink, G. 1992. Cellular and molecular aspects of adaptation in skeletal muscle. In Strength and power in sport, ed. P.V. Komi. Oxford: Blackwell. Goldspink, G. 1996. Personal communication. Gossman, M.R.; Sahrmann, S.A; and Rose, S.J. 1982. Review of length associated changes in muscle. Physical Th£rapy 62: 1799-808. Gracovetsky, S.; Farfan, H.E; and Helleur, C 1985. The abdominal mechanism. Spine 10:317-24. Gracovetsky, S.; Kary, M.; Levy, S.; Ben Said, R.; Pitchen, I.; and Helie, J. 1990. Analysis of spinal and muscular activity during flexion/extension and free lifts. Spine 15:1333-39. Gracovetsky, S.; Farfan, H.E; and Lamy, C. 1977. A mathematical model of the lumbar spine using an optimal system to control muscles and ligaments. Orthopaedic Clinics of North America 8:135-53. Guimaraes, ACS.; Vaz, M.A.; De Campos, M.LA.; and Marantes, R. 1991. The contribution of the rectus abdominis and rectus femoris in twelve selected abdominal exercises. Journal of Sports Medicine and Physical Fitness 31:222-30. Harman E.; Frykman, P.; Clagett, B.; and Kraemer, W 1988. Intra-abdominal and intra-thoracic pressures during lifting and jumping. Medicine and Science in Sports and Exercise 20:195-201. Hart, D.L, and Rose, S.J. 1986. Reliability of a non-invasive method for measuring the lumbar curve. Journal of Orthopedic and Sports Physical Therapy 8:180-84. Hemborg, B.; Moritz, U.; and Hamberg, J. 1983. Intra-abdominal pressure and trunk muscle activity during lifting---
165-72. Hirsch,
C and Schajowicz,
Orthopaedica Scandinavica Hirsch, C., and Nachemson,
F. 1952. Studies 22:184-89. A. 1954. New
Orthopaedica Scandinavica 23:254-83 Hodges, P.W., and Richardson, CA. 1996.
on structural
changes
in the lumbar
annulus
fibrosis.
observations
on mechanical
behaviour
of lumbar
Contraction
of transversus
abdominis
invariably
Acta
discs.
Acta
precedes
movement of the upper and lower limb. In Proceedings of the 6th Illternational Conference of the International Federation of Orthopaedic Manipulative Therapists. Lillehammer, Norway. Hodges, P.; Richardson, C; and Jull, G. 1996. Evaluation of the relationship between laboratory and clinical tests of transversus Holm, S.; Maroudas, A.; Urban,
abdominis function. Physiotherapy J.PG.; Selstam, G.; and Nachemson,
Research International 1:30-40. A. 1981. Nutrition of the intervertebral
disc: solute transport and metabolism. Cotlnect Tissue Res 8:101-19. Holt, L.E., and Smith, R. 1983. The effect of selected stretching programs on active and passive flexibility. Mar, CA: Research Center for Sport. Hughes, M.A.; Duncan, r.W; Rose, OK; Chandler, J.M.; and Studenski, S.A. 1996. The relationship postural
sway
to sensorimotor
function,
functional
performance,
and
disability
in the elderly
Del of Ar-
chives of Physical Medicine and Rehabilitation 77:567-72. Hukins, D.W.L. 1987. Properties of spinal materials. In The lumbar spine and back pain, ed. M.I.V. Jayson. Edinburgh: Churchill Livingstone. Hukins, D.W.L.; Aspden, R.M.; and Hickey, D.5. 1990. Thoracolumbar fascia can increase the efficiency of the erector spinae muscles. Clinical Biomechanics Hyman, J., and Liebenson, C. 1996. Spinal stabilization
5:30-34. exercise
ed. C Liebenson. Baltimore: Williams & Wilkins. Irion, J .M. 1992. Use of the gym ball in rehabilitation of spinal
program.
dysfunction.
In Rehabilitation In Orthopaedic
of the spine,
physical
therapy
clinics of North America. Oxford: Churchill Livingstone. Jacob, H.A.C, and Kissling, R.O. 1995. The mobility of the sacroiliac joints in healthy volunteers between 20 and 50 years of age. Clinical Biomechanics 10:352-61. Janda, V. 1986. Muscle weakI1l.'Ss and inhibition pseudoparcsis in back pain syndromes. In Modern manual therapy, ed. G. Grieve. Edinburgh: Churchill Livingstone.
258
. Bibliography
Janda, V. 1992. Muscle imbalance and musculoskeletal pain. Course notes. University of Oxford. UK. Janda, V. 1993. Muscle strength in relation to muscle length, pain and muscle imbalance. In Muscle strength. International perspectives in physical therapy, ed. K. Harms-Ringdahl. Edinburgh: Churchill Livingstone. Janda v., and Schmid, H.J.A. 1980. Muscles as a pathogenic factor in back pain. Proceedings of the International Federation of Orthopaedic Manipulative Therapists, 4th Conference, 17-18. New Zealand. Jensel, M.C.; Brant-Zawadzki, M,N.; and Obuchowki, N. 1994. Magnetic resonance imaging of the lumbar spine in people without back pain. New England Journal of Medicine 2:69. Johnson, C., and Reid, J.G. 1991. Lumbar compressive and shear forces during various curl up exercises. Clinical Biomechanics 6:97-104. Jorgensen, K., and Nicolaisen, T. 1987. Trunk extensor endurance: determination and relation to lowback trouble. Ergonomics 30:259-67. Jull, G.A. 1994. Headaches of cervical origin. In Physical therapy of the cervical and thoracic spine, ed. R. Grant. New York: Churchill Livingstone. Jull, G.A., and Janda, V. 1987. Muscles and motor control in low back pain: assessment and management. In Physical therapy of the low back, ed. L.T. Twomey. New York: Churchill Livingstone. Jull, G., and Richardson, CA. 1994a. Active stabilisation of the trunk. Course notes. University of Edinburgh. Jull, G.A., and Richardson, CA. 1994b. Rehabilitation of active stabilization of the lumbar spine. In Physical therapy of the low back. 2d ed., ed. L.T. Twomey and L.T. Taylor. Edinburgh: Churchill Livingstone. Kapandji, I. 1974. The physiology of joints, vol. 3. The spine. London: Churchill Livingstone. Kendall, EP.; McCreary, E.K.; and Provance, P.G. 1993. Muscles. Testing and function. 4th ed. Baltimore: Williams & Wilkins. Kennedy, J.C; Alexander, I.J.; and Hayes, K.C 1982. Nerve supply of the human knee and its functional importance. American Journal of Sports Medicine 10:329. Kent, M. 1994. The Oxford dictionary of sports science and medicine. Oxford: Oxford University Press. Kesson, M., and Atkins, E. 1998. Orthopaedic medicine. A practical approach. Oxford: Butterworth Heinemann. Kippers, V., and Parker, A.W. 1984. Posture related to myoelectric silence of erectores spinae during trunk flexion. Spine 9:74045. Kirby, M.C; Sikoryn, T.A.; Hukins, D.W.L.; and Aspden, R.M. 1989. Structure and mechanical properties of the longitudinal ligaments and ligamentum flavum of the spine. Journal of Biomedical Engineering 11:192-96. Kirkaldy-Willis, W.H. 1990. The lumbar spine. New York: Saunders. Klein, J .A., and Hukins, D. w.L. 1983. Relocation of the bending axis during flexion-extension of the lumbar intervertebral discs and its implications for prolapse. Spine 8: 659-64. Koh, T.J. 1995. Do adaptations in serial sarcomere number occur with strength training? Human Movement Science 14:61-77. Konradsen, L., and Ravn, J.B.1990. Ankle instability cause by prolonged peroneal reaction time. Acta Orthop Scand 61:388-90. Kraemer, J.; Kolditz, D.; and Gowin, R. 1985. Water and electrolyte content of human intervertebral discs under variabJe load. Spine 10:69-71. Lacote, M.; Chevalier, A.M.; Miranda, A.; Sleton, J.P.; and Stevenin, P. 1987. Clinical evaluation of muscle function. Edinburgh: Churchill Livingstone. Lavignolle, B.; Vital, J.M.; and Senegas, J. 1983. An approach to the functionaJ anatomy of the sacroiliac joints in vivo. Anatomia Clinica 5:169-76. Leatt. P.; Reilly, T.; and Troup, J.G.D. 1986. Spinal loading during circuit weight-training and running. British Journal ofSparts Medicine 20(3):119-24. Lee, D.G. 1994. Kinematics of the pelvic joints. In Grieves modern manual therapy, ed. J.D. Boyling and N. Palastanga. Edinburgh: Churchill Livingstone. LenteJl, G.L.; Katzman, L.L.; and Walters, M.R. 1990. The relationship between muscle function and ankle stability. Journal of Orthopedic and Sports Physical Therapy 11:605-11. !.ephart, S.M., and Fu, EH. 1995. The role of proprioception in the treatment of sports injuries. Sparts Exerciseand Injury 1:96-102. !.ephart, S.M.; Warner, J.P.; Borsa, P.A.; and Fu, EH. 1994. Proprioception of the shoulder in normal, unstable, and surgical individuals. Journal of Shoulder and Elbow Surgery 3:224-28. Lester, M.N., and Posner-Mayer, J. 1993. Spinal stabilisatio,,: utilizing the Swiss ball video. Denver: Ball Dynamics. Levine, D.; Walker, J.R.; and TIllman, L.J. 1997. The effect of abdominal muscle strengthening on pelvic tilt and lumbar lordosis. Physiotherapy Theory and Practice 13:217-26.
Bibliography.
259
Lewit, K. 1991. Manipulative therapy in rehabilitation of the locomotor system. 2d ed. Oxford: Butterworth Heinemann. Liebenson, C. 1996. Rehabilitation of the spine. Baltimore: Williams & Wilkins. Lieber, R.L. 1992. Skeletal muscle structure and function. Baltimore: Williams & Wilkins. Linsenbardt, S.T.; Thomas, TR.; and Madsen, R.w. 1992. Effect of breathing techniques on blood pressure response
to resistance
exercise.
British
/ouma1
of Sports
Medicine
26:97-100.
Lipetz, S., and Gutin, B. 1970. An electromyographic study of four abdominal exercises. Medicine and Science in Sports and Exercise 2:35-38. Long, D.M. 1995. Effectiveness of therapies currently employed for persistent low back and leg pain. Pain Forum 4:122-25. Lord,S.R.;Ward,J.A.; Williams, P.;and Zivanovic, E. 1996. The effects of a community exercise program on fracture risk factors in older women. Osteoporosis International 6:361-67. Lovell, F.W.; Rothstein, j.M.; and Personius, w.j. 1989. Reliability of clinical measurements of lumbar lordosis taken with a nexible rule. Physical TIIerapy 69:96-105. Luttgens, K.; and Wells, K. 1982. Kinesiology. Scientific basis alld human motion. 7th ed. Philadelphia: Saunders College Publishing. Macintosh,j.E., and Bogduk, N. 1986. The biomechanics of the lumbar multifidus. Clinical Biomechanics 1:205-13. Macintosh, j.E., and Bogduk, N. 1987. The anatomy and function of the lumbar back muscles and their fascia. In Physical therapy of the low back, ed. L.T Twomey. New York: Churchill Livingstone. Macintosh, j.E.; Bogduk, N.; and Gracovetsky, S. 1987. The biomechanics of the thoracolumbar fascia. Clillical Biomechallics 2:78-83. Main, c.j., and Watson, P.j. 1996. Guarded movements: development of chronicity. Journal ofMusculoskeletal Pain 4:163-70. Maitland, G.D. 1986. Vertebral manipulatioll. 5th ed. London: Butterworths. Markolf, K.L., and Morris, j.M. 1974. The structural components of the intervertebral disc. Journal of Balle alld Joint Surgery 56A:675-87. McConnell, J. 1993. Promoting effective segmental alignment. In Kry issues ill musculoskeletal physiotherapy, ed. J. Crosbie and j. McConnell. Oxford: Butterworth Heinemann. McGill, S.M. 1997. Distribution of tissue loads in the low back during a variety of daily and rehabilitation tasks. Journal of Rehabilitatioll Researcll alld Development 34:448-58. McGill, S.M. 1998. Low back exercises: evidence for improving exercise regimens. Physical TIIerapy 78:7546S. McGill, S.M., and Norman, R.W. 1986. Partitioning of the L4-LS dynamic moment into disc, ligamentous, and muscular components during lifting. Spine 11:666-78. McGill, S.M.; Norman, R.W.; and Sharratt, M.T 1990. The effect of an abdominal belt on trunk muscles activity and intra-abdominal pressure during squat lifts. Ergonomics 33:147-60. McGill, S.M.; Juker, D.; and Kropf. P. 1996. Quantitative intramuscular myoelectric activity of quadratus lumborum during a wide variety of tasks. Clinical Biomechanics 11:170-72. McKenzie, R.A. 1981. The lumbar spille. Mechanical diagnosis and therapy. Lower Hutt, New Zealand: Spinal Publications. McKenzie, R.A. 1990. TIle ceroical and tlJOraricspine. Mechanical diagnosis and therapy. Lower Hutt, New Zealand: Spinal Publications. Miller, j.A.A.; Haderspeck, K.A.; and Schultz, A.B. 1983. Posterior element loads in lumbar motion segments. Spine 8:331-37. Miller, M.L, and Medeiros, j.M. 1987. Recruitment of internal oblique and transversus abdominis muscles during the eccentric phase of the curl-up exercise. Physical Therapy 67:1213-17. Moore, M.A., and Kukulka, CG. 1991. Depression of Hoffman reflexes following voluntary contraction and implications for proprioceptive neuromuscular facilitation therapy. Physical Therapy 71:321-33. Morgan, D.L., and Lynn, R. 1994. Decline running produces more sarcomeres in rat vastus intermedius muscle fibers than does incline running. Journal of Applied Physiology 77:1439-44. Morris, j.M.; Lucas, 0.8.; and Bresler, B. 1961. Role of the trunk in stability of the spine. Journal of Balle alld Joint Surgery (Am) 43A:327-51. Mottram, S.L. 1997. Dynamic stability of the scapula. Mallual Therapy 2:123-31. Murray, M.P.; Seireg, A.; and Sepic, S.B. 1975. Normal postural stability and steadiness: quantitative assessment. Journal of Balle alld Joint Surgery S7 A:S10-16. Nachemson, A.L. 1992. Newest knowledge of low back pain. Clinical Orthopaedics 279:8. Nachemson, A., and Evans, j. 1968. Some mechanical properties of the third lumbar laminar ligament (ligamentum flavum). Journal of Biomechanics 1:211. Ng, G., and Richardson, CA. 1990. The effects of training triceps surae using progressive speed loading. Physiotherapy Practice 6:77-84.
260
.
Bibliography
Ng, G., and extension Norkin, CC, delphia: Norris, CM. Norris, CM.
Richardson, C 1994. EMG study of erector spinae and multifidus in two isometric back exercises. Australian Journal of Physiotherapy 40:115-21. and Levangie, P.K. 1992. Joint structure and function. A comprehensive analysis. 2d ed. PhilaDavis. 1993. Abdominal muscle training in sport. British Journal of Sports Medicine 27:19-27. 1994b. Abdominal training. Dangers and exercise modifications. Physiotherapy in Sport
14:10-14. Norris, CM. 1994c. Taping: components, applications and mechanisms. Sports Exercise and Injury 1:14-17. Norris, CM. 1995a. Spinal stabilisation 2. Limiting factors to end-range motion in the lumbar spine. Physiotherapy 81 :4-12. Norris, CM. 1995b. Weight training. Principles and practice. London: A&C Black. Norris, CM. 1997. Abdominal training. London: A&C Black. Norris, CM. 1998. Sports Injuries. Diagnosis and management. 2d ed. Oxford: Butterworth Heinemann. Norris, CM. 1999. Functional load abdominal training: part 1. Journal of Bodywork and Movement Therapies 3(3):150-58. Norris, CM., and Berry, S. 1998. Occurrence of common lumbar posture types in the student sporting population: an initial evaluation. Sports, Exercise, and Injury 4:15-18. O'Sullivan, P.B.; Twomey, L.T.; and Allison, G.T. 1997. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine 22:2959-67. O'Sullivan, P.B.; Twomey, L.; and Allison, G.T. 1998. Altered abdominal muscle recruitment in patients with chronic back pain following a specific exercise intervention. Journal of Orthopedic and Sports Physical Therapy 27:114-24. Oliver, J., and Middleditch, A. 1991. Functional anatomy of the spine. Oxford: Butterworth Heinemann. Palastanga, N.; Field, D.; and Soames, R 1994. Anatomy and human movement. 2d ed. Oxford: Butterworth Heinemann. Panjabi, M.M. 1992. The stabilizing system of the spine. Part 1. Function, dysfunction, adaptation, and enhancement. Journal of Spinal Disorders 5:383-89. Panjabi, M.M.; Abumi, K.; Duranceau, J.; and Oxland, T. 1989. Spinal stability and intersegmental muscle forces. A biomechanical model. Spine 14:194-200. Panjabi, M.M.; Hult, J.E.; and White, A.A. 1987. Biomechanics studies in cadaveric spines. In The lumbar spine and back pain, ed. M.l.V.Jayson. Edinburgh: Churchill Livingstone. Panjabi, M.M., and White, A.A. 1990. Physical properties and functional biomechanics of the spine. In Clinical biomechanics of the spine, ed. A.A. White and M.M. Panjabi. Philadelphia: Lippincott. Paris, S.V. 1985. Physical signs of instability. Spine 10:277-79. Parkkola, R; Rytokoski, U.; and Kormano, M. 1993. Magnetic resonance imaging of the discs and trunk muscles in patients with chronic low back pain and healthy control subjects. Spine 18:830-36. Pamianpour, M.; Nordin, M.; Kahanovitz, N.; and Frankel, V. 1988. The triaxial coupling of torque generation of trunk muscles during isometric exertions and the effect of fatiguing isoinertial movements on the motor output and movement patterns. Spine 13:982-92. Pearcy, p.; Portek, I.; and Shepherd, J. 1984. Three dimensional X ray analysis of normal movement in the lumbar spine. Spine 9:294-97. Perey, 0.1957. Fracture of the vertebral end plate in the lumbar spine. Acta Orthap Scand (Suppl) 25:1-101. Pope, M.H., and Panjabi, M.M. 1985. Biomechanical definitions of instability. Spine 10:255-56. Ricci, B.; Marchetti, M.; and Figura, F. 1981. Biomechanics of sit up exercises. Medicine and Science in Sports and Exercise 13:54-59. Richardson, CA. 1992. Muscle imbalance: principles of treatment and assessment. Proceedings of the New Zealand Society of Physiotherapists Challenges Conference. Christchurch, New Zealand. Richardson, CA., and Bullock, M.1. 1986. Changes in muscle activity during fast, alternating flexionextension movements of the knee. Scandinavian Journal of Rehabilitation Medicine 18:51-58. Richardson, CA., and Hodges, P. 1996. New advances in exercise to rehabilitate spinal stabilisation. Course notes. University of Edinburgh. Richardson, C; Jull, G.; Toppenburg, R; and Comerford, M. 1992. Techniques for active lumbar stabilisation for spinal protection: a pilot study. Australian Journal of Physiotherapy 38:105-12. Richardson, CA., and Sims, K. 1991. An inner range holding contraction: an objective measure of stabilising function of an antigravity muscle. Proceedings of the World Confederation for Physical Therapy, 11th International Congress. London. Richardson, C; Toppenberg, R.; and Jull, G. 1990. An initial evaluation of eight abdominal exercises for their ability to provide stabilisation for the lumbar spine. Australian Journal of Physiotherapy 36:6-11. Risch, 5.V.; Norvell, N.K.; Pollock, M.L.; Risch, E.D.; Langer, H.; Fulton, M.; Graves, J.E.; and Leggett, S.H. 1993. Lumbar strengthening in chronic low back pain patients. Physical and psychological
benefits. Spine 18:232-38.
Bibliography.
261
Roaf, R. 1960. A study of the mechanics of spinal injuries. Journal of Bone and Joint Surgery 42B:810-23. Rock~ff, S.F.i Sweet, E.; and Bleustein, J. 1969. The relative contribution of trabecular and cortical bone to the strength of human lumbar vertebrae. Calcified Tissue Research 3:163-75. SaaI. J.A. 1988. Rehabilitation of football players with lumbar spine injury. Physician and Sports medicine 16:61-67. Saal, J.A. 1995. The pathophysiology of painful lumbar disorder. Spine 20:180-83. Saal, J.A., and Saal, JS. 1989. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. Spine 14:431-37. Sahrmann, S.A. 1987. Posture and muscle imbalance: faulty lumbar-pelvic alignment and associated musculoskeletal pain syndromes. In Postgraduate advances in physical therapy. Berryvill, VA: Forum Medicum. Sahrmann, S.A. 1990. Diagnosis and treatment of movement related pain syndromes associated with muscle and movement imbalances. Course notes. Washington University. Silvermetz, M.A. 1990. Pathokinesiology of supine double leg lifts as an abdominal strengthener and suggested alternative exercises. Athletic Trianing 25:17-22. Skall, F.H.; Manniche, C; and Nielsen, CJ. 1994. Intensive back exercises 5 weeks after surgery of lumbar disk prolapse. A prospective randomized multicenter trial with a historical control group. Ugeskr Laeger 156:643-46. Smith, R.L., and Brunolli, J. 1990. Shoulder kinesthesia after anterior glenohumeral joint dislocation. Physical Therapy 69: I 06-12. Spitzer, W.O.; Le Blanc, F.E.; and Dupuis, M. 1987. Scientific approach to the assessment and management of activity related spinal disorders: a monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine 12 (Suppl 7). Sturesson, 8.; Selvik, G.; and Uden, A. 1989. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine 14:162-65. Sugano, H., and Takeya, T. 1970. Measurement of body movement and its clinical application. Japanese Journal of Physiology 20:296-308. Sullivan, MS. 1997. Lifting and back pain. In Physical therapy of the low back,ed. L.T. Twomey and J.R Taylor. Edinburgh: Churchill Livingstone. Sullivan, P.E.; Markos, P.O.; and Minor, M.A.D. 1982. An integrated approach to therapeutic exercise. Reston, VA: Reston Publishing. Swanepoel, M.W.; Adams, L.M.; and Smeathers, J.E. 1995. Human lumbar apophyseal joint damage and intervertebral disc degeneration. Annals of the Rheumatic Diseases 54:182-88. Taylor, D.C; Dalton, j.; 5oaber, A.V.; and Garrett, W.E. 1990. The viscoelastic properties of muscle-tendon units. American Journal of Sports Medicine 18:300-09. Taylor, J.R, and Twomey, L.T. 1986. Age changes in lumbar zygapophyseal joints. Spine 11:739-45. Templeton, G.H.; Padalino, M.; and Manton, J. 1984. Influence of suspension hypokinesia on rat soleus muscle. Journal of Applied Physiology 56:278-86. Thapa, P.B.; Gideon, P.; Brockman, K.G.; Fought, RL.; measures
of balance
as fall predictors
in ambulatory
and
Ray, W.A.
nursing
home
1996. Clinical residents.
and Journal
biomechanical of Gerontology
51:239-46. Tkaczuk, H. 1968. Tensile properties of human lumbar longitudinal ligaments. Acta Orthop Scand 115 (Suppl). Toppenburg, R.M., and Bullock, M.l. 1986. The interrelation of spinal curves, pelvic tilt and muscle lengths in the adolescent female. Australian Journal of Physiotherapy 32:6-12. Travell, J.G., and Simmons, D.G. 1983. Myofascial pain and dysfunction. Baltimore: Williams & Wilkins. Tropp, H.; Alaranta, H.; and Renstrom, P.A.F.H. 1993. Proprioception and coordination training in injury prevention. In Sports injuries: basicprinciples of prevention and care. IOC Medical Commission publication, ed. P.A.F.H. Renstrom. London: Blackwell Scientific. Twomey, L.T., and Taylor, 1.R. 1987. Lumbar posture, movement and mechanics. In Physical therapy of the low back, ed. LT. Twomey. New York: Churchill Livingstone. Twomey, L.T., and Taylor, 1.R. 1994. Factors influencing ranges of movement in the spine. In Physical therapy of the low back. 2d ed., ed. L.T.Twomey and J.R Taylor. Edinburgh: Churchill Livingstone. Twomey, L.T.; Taylor, J.R.; and Oliver, M. 1988. Sustained flexion loading, rapid extension loading of the lumbar spine and the physical therapy of related injuries. Physiotherapy Practice 4:129-38. Tye, J., and Brown, V. 1990. Back pain-the ignored epidemic. London: British Safety Council. Tyldesley, B., and Grieve, 1.1. 1989. Muscles, nerves and movement: kinesiology in daily living. Oxford: Blackwell Scientific. Tyrrell, A.R; Reilly, T.; and Troup, JD.G. 1985. Circadian variation in stature and the effects of spinal loading. Spine 10:161-64. Valencia, P.P.,and Munro, R.R. 1985. An electromyographic study of the lumbar multifidus in man. Electromyography and Clinical Neurophysiology 25:205-21.
262
. Bibliography
Vernon-Roberts, B. 1987. Pathology of intervertebral discs and apophyseal joints. In Tile lumbar spine and back pain. ed. M.I. V. Jayson. Edinburgh: Churchill Livingstone. Vernon-Roberts, B. 1992. Age related and degenerative pathology of intervertebral discs and apophyseal joints. In The lumbar spine and back pain, ed. M.I.V. Jayson. Edinburgh: Churchill Livingstone. Videman, T.; Nurminen, M.; and Troup, j.D.G. 1990. Lumbar spine pathology in cadaveric material in relation to history of back pain, occupation, and physical loading. Spine 15:728-40. Vlaeyen, J.W.S.; Kole-Snijders, AM.J.; Boeren, RG.B.; and van Eek, H. 1995. Fear of movement/reinjury in chronic low back Vleeming, A; Mooney,
and its relation to behavioural performance. Pain 62:363-72. v.; Snijders, CJ.; Dorman, T.A; and Stoeckart, R. 1997. Movement pain
low back pain. New York: Churchill Livingstone. Vleeming. A; Pool-Goudzwaanl, A.L.; and Stoeckart, fascia: Vleeming.
its function in load A; Pool-Goudzwaanl,
transfer from spine AL.; Stoeckart,
rior layer of the thoracolumbar Vleeming. A; Stoeckart, R; and
to its dynamic Vleeming.
fascia: Snijders,
role in stabilizing
A.; Stoeckart,
R 1995a.
its function in load transfer C 1989. The sacrotuberous
A.CW.;
and
Snijders,
tion in the sacroiliac joint. Spine 15:130-32. Waddell, G. 1987. A new clinical model for the treatment Waddell, G.; Feder, G.; and Lewis, M. 1997. Systematic
acute low back pain. British ,ournal Walker,
M.L.;
Rothstein,
J.M.; Finucane,
dosis, pelvic tilt, and abdominal Walters,
C,
and
Partridge,
M. 1957.
Watson,
D.H.
flexor
1994.
Cervical
headache:
performance.
muscle
CJ.
from spine ligament:
Biomechanics 1990. Relation
and
of the thoracolumbar CJ.
1995. The poste-
to legs. Spine 20:753-58. a conceptual approach
4:201-03. between
form
and
func-
of low-back pain. Spine 12:632-44. reviews oibed rest and advice to stay active
of General Practice S.D.; and Lamb,
47:647-52. RL. 1987. Relationships between Physical Therapy 67:512-16.
muscle performance.
during exercise. American ,ournal Watkins, J. 1999. Structure and function
layer
to legs. Spine 20:753-58. R; Wingerden, J.P.; and Snijders,
the sacroiliac joint. Clinical
R; Volkers,
The posterior
stability
Electromyographic study of the differential of Physical Medicine 36:259-68. system.
an investigation
of natural
head
lumbar
abdominal
Champaign,
of the musculoskeletal
and
Kinetics.
upper
cervical
In Grieve's modern manual therapy. 2d ed., ed. J.D. Boyline
Palastanga. Edinburgh: Churchill Livingstone. Watson, J. 1983. An introduction for mechanics of human movement. Weber, H. 1983. Lumbar disc herniation: a controlled prospective
lor-
muscles
1L: Human
posture
for
and
N.
Lancaster, UK: MTP Press. study with ten years of observation.
Spine 8:131-38. Webright,
w.G.;
Randolph,
B.J.; and
Perrin,
D.H.
1997. Comparison
of nonballistic
active
knee
exten-
sion in neural slump position and static techniques on hamstring flexibility. Sparts Physical Therapy 26:7-13. Weider, J. 1989. Ultimate badybuilding. Chicago: Contemporary Books.
Journal of Orthopedic
White,
to management
S.G., and Sahrmann,
culoskeletal
Livingstone. Wilke, H.J.; Wolf, S.; Claes, with Willard,
S.A. 1994. A movement
pain. In Physical therapy of the cervical L.E.; Arand,
different muscle groups: F.H. 1997. The muscular,
system
balance
and thoracic
M.; and Weisend,
approach
and
of mus-
spine, ed. R Grant. New York: Churchill
A. 1995. Stability
increase
of the lumbar
spine
a biomechanical in vitro study. Spine 20:192-98. ligamentous and neural structure of the low back and its relation
to
back pain. In Movement stability and low back pain, ed. A. Vleeming. V. Mooney, T. Dorman, C Snijders, and R Stoeckart. Edinburgh: Churchill Livingstone. Williams, P.; Watt, P.; Bicik, V.; and Goldspink, G. 1986. Effect of stretch
combined
with electrical
tion on the type of sarcomeres produced at the ends of muscle Williams, P.E. 1990. Use of intennittent stretch in the prevention
fibers. Experimental of serial sarcomere
muscle. Annals of the Rheumatic Diseases 49:3]6-]7. Williams, P.E., and Goldspink, G. 1978. Changes in sarcomere
length
immobilised Yamamoto,
muscle.,ournal
I.; Panjabi,
M.M.;
of Anatomy 127:459-68. Oxland, T.R.; and Crisco,
the lumbosacral junction. Spine 15:1138-41. Yang, K.H., and King, A.1. 1984. Mechanism pain.
Spine
Yong-Hing, Zetterberg.
of facet load
and physiological
The role of the iliolumbar
transmission
as a hypothesis
properties
in
ligament
in
for low
back
9:557-65.
K.; Reilly, J.; and Kirkaldy-Willis, C; Andersson,
G.B.J.;
44:13-20.
W.H. 1976. The ligamentum
Schultz, A.B. 1987. The activity Spine 12:1035-40.
ing heavy physical loading. Zusman, M. 1998. Structure-oriented iotherapy
J.J. ]990.
stimula-
Neurology 93:500-09. loss in immobilised
and
beliefs and disability
flavum. Spine 1:226-34.
of individual
due to back pain. Australian
trunk
muscles ,ournal
dur-
of Phys-
Credits From J.e. Griffin, 1998, Client-centered exercise prescription (Champaign, ics): Figure 5.1 (page 95) reprinted, by permission, from p. 176.
IL: Human Kinet-
From J.A. Hides, e.A. Richardson, and G.A. Jull, 1996, "Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain," Spine 21 (23): Figure 3.5 (page 52) reprinted, by permission, from pp. 2763-2769. From National Strength and Conditioning Association, 1994, Essentials of strength conditioning and training (Champaign, IL:Human Kinetics): Exercise figure, a-c, "Hang Clean" (Page 220) adapted, by permission, from p. 394; Exercise figure, a.c, "Power Clean" (page 221) adapted, by permission, from p. 392; Exercise figure, a-c, "Dead Lift" (page 222) adapted, by permission, from p. 380. From e. Norris, 1995, "Spinal stabilisation," Physiotherapy Journal 81 (3): Exercise figure, a. c, "Assessing Muscle Balance in the Gluteus Maximus" (page 104) reprinted, by permission, from p. 26. From e. Norris, 1998, Diagnosis and management, 2d ed. (Oxford: 8utterworth Heinemann): Figure 2.12, a and b (page30); Figure 2.14, a and b (page 34); Figure 2.16 (page 3B) reprinted from p. 18; Exercise figure, a-d, "Knee Raising in Standing" (page 71); Exe,.. cise figure, a.d, "Assessing Lumba,..Pelvic Rhythm in Prone Kneeling" (page 72); Exercise figure, a and b, ''The Hip Hinge Movement in Standing" (page 72); Exercise figure, a and b, "Recognizing False Hip Abduction" (Page 73) reprinted from p. 167; Figure Figure 4.4 (page 91) reprinted from p_ 155; Chapter 5 exercise descriptions; 5.2 (page 95) and Figure 5.3 a (page 95) reprinted from p. 145; Figure 5.7 (page 101) and Figure 5.8 (page 101); Exercise figure, "Assessing Muscle Balance in the IliopMuscle Balance in the Glu. soas" (page 103); Exercise figure, top right, "Assessing teus Maximus" (page 104); Exercise figure, "Assessing Muscle Balance in the Glu. teus Medius" (page 105); Exercise figure, "Half Lunge" (page 114), Exercise figure, "Hip Hitch" (page 115), Exercise figure, "Active Knee Extension, Holding Thigh" (Page 116), Exercise figure, "Active Knee Extension, Pushing Against Thigh" (Page 116) and Exercise figure, ''Tripod Stretch" (page 117) reprinted from p. 175; Figure 6.1, a and b (page 121) reprinted from p. 176; Figure 6.2 (page 122) and Figure 6.3 (page 125) reprinted from p. 177; Exercise figure, "Leg Lowering" (page 128); Exe,.. cise figure, "Bench Lying Pelvic Raise" (page 129) and Exercise figure, a, "Wail Bar Hanging Leg Raise" (page 130) reprinted from p. 177; Exercise figure, "Plyometrlc Flexion and Extension Using a Punching Bag" (page 226) and Exercise figure, "Leg Raise Throw (Page 227) reprinted from p. 129. All reprinted by permission of Butterworth Heinemann Publishers, a division of Reed Educational & Professional Publishing Ltd. From CM. Norris, 1997. Abdominal Training (london: A & C Black): Exercise figure, "Correction of Swayback Posture" (page 151) and Exercise figure, a and b, "Passive Back Extension in Lying Position" (page 156) adapted, by permission, from p. 38. Illustrations by Jean Ashley. From P.B. O'Sullivan, l.T. Twomey, and G.T. Allison, 1997, "Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiological diagnosis of spondylolysis or spondylolisthesis," Spine 22 (24): Figure 1.1 (page 7) adapted, by permission, from pp.2959-2967. From e.A. Richardson and M.I. Bullock, 1986, "Changes in muscle activity during fast, alternating flexion-extension movements of the knee," Scandinavian Journal of Rehabilitation Medicine 18: Figure 5.4 (page98) and Figure 5.5 (page98), reprinted, by permission, from pp. 51-58. From J. Watkins, 1999, Structure and function of the musculoskeletal system (Champaign, IL: Human Kinetics): Figure 2.1 (page 15) reprinted from p. 61; Figure 2.2 (page 15) reprinted from p. 63; Figure 2.5 (page 19) reprinted from p. 145; Figure 2.6 (page 19) reprinted from p. 150. 263
Index Figures and tables are indicated by the italicized assessments have italicized page numbers.
letters
A abdominal hollowing: about 60; assessing 236; basic process 81; common errors 88-89; correct and incorrect positions 88; fourpoint kneeling 83; general considerations 81-82; importance 168; lying 85-86; with pelvic floor contractions 84; prone test using pressure biofeedback 105-106; standing 84; starting positions 82-86; teaching clients 81-89; teaching tips 86; two-point kneeling and sitting 85; with webbing belt 87f; in weight training 203 abdominal machine 212 abdominal muscles: activation in chronic low back pain 6Of; coordination during spinal movement 60-62; deep abdominals anatomy 57-58; deep dissection illustration 58f; "doming" of abdominal wall 121; functions 58-60; intermediate dissection illustration 57£; in resisted actions 59; superficial abdominals anatomy 55-57 abdominal slide 188 abdominal training: current practice 120-124; modifications of traditional exercises 124-130 abdominal wall "doming" 121 ab roller exercises 130-132 active knee extension: holding thigh 116; pushing against thigh 116-117 active lumbar stability 12 active positioning reproduction 80-81 active stretching 111!, 112, 113 acute pain case history 242-244 Adams, M. 31 Adam's position 138 adipose tissue pad 22-23 advanced training qualifications 167-168 aerobic exercise 99 aging: chronic muscle tightness 237; compression of vertebral bodies 25; disc changes 28; facet joint cartilage 23; and ligaments 20; lumbar disc changes 28f; and posture 136; proteoglycan content 22; tissue overstretch 31 Allan, D.B. 6 American Academy of Orthopaedic Surgeons
134 anaerobic exercise 99 Andersson, E. 55 annulus fibrosis 20-21,21f anterior pelvic tilt 34f anterolateral muscles 7 aponeurosis 45 approximate (verb), defined arch mechanics 39f
264
45
t and f follCJWing the page number.
Exercises
and
arctan formula 142 arm fixation 123-124 arm lift in four-point kneeling 196-197 articulate, defined 17 articulating triad 14 assessments: heel slide maneuver using pressure biofeedback 106; hip hinge movement in standing 72-73; knee raising in standing 71; lumbar-pelvic rhythm in prone kneeling 72; muscle balance in gluteus maximus 104; muscle balance in gluteus medius 105; muscle balance in iliopsoas 103; Ober test 108-109; passive assessment of pelvic tilt 72; pelvic motion control in frontal plane 73; prone abdominal hoUowing test using pressure biofeedback 105-106; recognizing false hip abduction 73-74; straight-leg raise test 109-110; Thomas test 107-108; tripod test 110 assisted
pelvic
tilt: from
crook
lying
position
75-
76; while sitting 75; while standing 74 atrophy 97 axial compression: of facet joints 28-29; of intervertebral discs 26-28; verterbal bodies 25-26
B back back back back back back
care, in home 249f extension (frame) 209 extension (machine) 208 flattening 149-150 muscles 52f pain: back stability exercises 234t; diagnostic triage 233; nonorganic causes 4-5; recurrence 3; scope of problem 3--4 back pain management: about 5-6; lumbar stabilization model 7-12; new model 6-7; traditional model 6 back stability assessment 236 back stability exercises 234t Baechle, T.R. 214 balance boards 168-169,183-186 ballistic stretching 1111, 112, 113 barbell lunge 218-219 Barrack, R.L. 199-200 basic crunch, ab roller 131 basic superman 190 bed rest 5, 234 behavioral factors 5 bench curl 127 bench lying pelvic raise 129 bending: erector spinae 37; sacroiliac joint 25; torsional stresses 27 bent knee sit-up 126 Biedermann, H.j. 51 blood flow, out of vertebral body 26
Index.
blood pressure, and Valsalva maneuver 63 body, listening to 205 body sway, and postural stability 135-136 Bogduk, M. 65 bones, vertebral column anatomy 14-15 brain stem activities 80 breathing, in weight training 203 bridge: from crook lying 172; with gym ball 191; with leg lift 173,192; with leg lift and extension 192; with pelvic tilt 191; with therapist pressure 192 Bullock, M.l. 97,99 Bullock-Saxton, J. 141
C cable crossover 208 capsular ligaments 16t, 18 cartilage end plates 20,22 case histories: acute pain 242-244; obese client 239-240; poor stability 240-242; unwillingness to exercise 244-245 cauda equina syndrome 232
caudal, defined 17 center of gravity, in postural assessment 136 chronic low back pain: and abdominal hollowing 60-61; abdominal muscle activation 6Of; motor control deficit in transversus abdominis 62 chronic muscle lengthening 100-102 clients (see also teaching clients): advanced training qualifications 167-168; postural re-education 144; preliminary assessment 231-234; training progression 168169,206,214; working with 71 closed loop system 198-199 clothing, for weight training 205 common beliefs 4 compressed ligament 12 concentric-eccentric coupling 224 conditioning: and traditional sit-up 121-122; and traditional straight-leg raise 123 connective tissue rim 22 contractile tissues 11 contract-relax-agonist-contract stretching 111t, 112, 113 contract-relax stretching 11It, 112, 113 contralateral, defined 45 contralateral fibers 17 controlled forward bending 77 correction of swayback posture 151-152 costs, of treatment 3-4 countermovement 224 countemutation, of sacroiliac joint 24t, 25 coupled movements 33 CRAC stretching lilt, 112, 113 craniovertebral angle 142, 142f creep: of discs 26-27; of lumbar tissues 31-32 Cresswell, A.G. 62 critical point 37.38 crook lying position exercises 169-173 CR stretching lilt, 112, 113
o dancers: and lordotic posture tive training 200
146; propriocep-
265
dead lift 222 deep abdominal muscles 57-58: inner-range holding tests 105-106 deep (intersegmental) muscles 50-52 deformation of disc 26-27 degenerative discs 28 Deyo, R.H. 5 diagnostic triage 232-234 disability; labels of 4-5; permanent 3 disc, defined 14 discal compression 26-28, 27f. 29f disc surgery 6 distraction force 17 door frame stretch 161 double crunch, ab roller 132 double-handed lift 251f double-leg raise 197 dumbbell row 215-216 dynamic posture 135
E elastic energy 224 electrical silence, of muscles 37-38 Enoka, R.M. 223-224 equipment, for weight training 205 erector spinae 37, 40 exercise: with axial loading 27; compression of vertebral bodies 26; controlled 6; disc compression and height losses 27f; lifting habit education 36; and sacroiliac joint stability 49; from sitting posture 31; and spinal stability 11-12; starting positions 31,82-86,169; training specificity 99 exercises: abdominal hollowing: four-point kneeling 83; abdominal hollowing: lying 85-86; abdominal hollowing: standing 84; abdominal hollowing: two-point kneeling and sitting 85; abdominal machine 212; abdominal slide 188; active knee extension, holding thigh 116; active
knee
extension,
pushing against
thigh 116-117; arm lift in four-point kneeling 196-197; assisted pelvic tilt from crook lying position 75-76; assisted pelvic tilt while sitting 75; assisted pelvic tilt while standing 74; back extension (frame) 209; back extension (machine) 208; back flattening 149-150; barbell lunge 218-219; basic crunch, ab roller 131; basic superman 190; bench curl 127; bench lying pelvic raise 129; bent knee sit-up 126; bridge from crook lying 172; bridge with gym ball 191; bridge with leg lift 173, 192; bridge with leg lift and extension 192; bridge with pelvic tilt 191; bridge with therapist pressure 192; cable crossover 208; controlled forward bending 77; correction of swayback posture 151-152; dead lift 222; door frame stretch 161; double crunch, ab roller 132; double-leg raise 197; dumbbell row 215-216; four-point body sway 173; four-point kneeling arm and leg lift 175; four-point kneeling leg lift 174-175; four-point kneeling stretch 118;
266 . Index
exercises (continued): four-point leg flexion/ extension 174; lour-point pelvic shilt 174; lree squat 196; gluteus maximus inner-range exercise 147-149; good morning 216; hall lunge 114; hall lunge (without chair) 149; hall-sitting arm and leg movements 188-189; hang clean 220; heel bridge 193; heel bridge with leg raise, ball rolling 194; heel slide 128; heel slide basic movement 170; hip hinge action in high kneeling 76; hip hinge with table support 77; hip hitch 115; lateral puUdown 206-207; leg lowering 128,170; leg raise throw 227; low pulley spinal rotation 210-211; lying barbell row 215; lying trunk curl over baU 189; lying trunk curl with leg lilt 190; medicine ball trunk curl 226-227; modified trunk curl 146-147; multiludus contraction 89-90; muscle reaction speed using mobile platform 201; neutral position maintenance 185; Dber test stretch 115-116; passive back extension in lying position 156-157; pelvic rock on rocker board 184; pelvic rock on wobble board 185; pelvic shilt with leg lilt 180; pelvic shilt with unloading 179; pelvic tilt re-education, sitting 157; plyometric lIexion and extension using punching bag 226; plyometric side bend using punching bag 225; power clean 221; prone bent-leg lilt 172; prone laU 194; prone laU with arm lilt 195; prone lall with single-leg lilt 195; prone lying gluteal brace 171; pulley crunch 212; rapid displacement in sitting 200; reproduction of active positioning 80-81; reproduction of passive positioning 80; reverse bridge 193; reverse bridge and roll 193; reverse crunch, ab roller 131; rhythmic stabilization 01 multifudus and lateral abdomina Is in side lying position 90-91; rotary torso machine 211; scapula repositioning 160161; seated rowing 209; side crunch, ab roller 132; side lying body lilt 178; side lying hip lilt 178; side lying knee lilt 176; side lying leg abduction 177; side lying leg rotation 176-177; side lying spine lengthening 177; simple pelvic tilt, progressing to balance boards 184; single arm pulley row 210; single-bent leg raises 171; single-leg heel bridge 194; sitting, hip lIexor shortening 154-155; sitting bilateral hip adductor stretch 152; sitting hamstring stretch 182; sitting hip hinge 185-186; sitting knee and arm raise 183; sitting knee raise 183, 188; sitting lateral tilt using gym baU 78; sitting pelvic tilt using gym ball 77-78; sitting sternal lilt 182-183; sitting wide splits 152-153; spinal lengthening 153-154; squat 216-218; standing hip abduction 180; standing hip hinge 181; standing sternal lilt 179; sternalliEt exercise 162;
superman, basic 190; superman with arms 190-191; Thomas test stretch 114; thoracic joint mobilization 159-160; throw-catch activities on mobile surface 201; tripod stretch 117; trunk curl 126127; trunk lIexion with high pulley 212; trunk side lIexor stretch 117-118; twist and throw with medicine ball 226; wall bar hanging leg raise 129-130; wall sit 195-196; weight bag passive stretch 161162 explosive power 219-222 extension 17,32-33 external oblique muscle 56-57,57f
F lacet joint capsule 19f lacet joints: about 14; axial compression 28-29; compression results 29f; 01 vertebral column 22-23 lalse hip abduction, recognizing 73-74 lascia 17 lascicle, delined 45 fast-twitch muscles 93 !ibro-adipose meniscoid 22-23 lIatback 145[ 156-157 lIexion 17,30-32 flexion relaxation response 37-38 flexor synergy during gait 122 lIuid loss 27 foot fixation 122 force closure 48 forensic back pain factors 5 form closure 48 lour-point body sway 173 lour-point kneeling 82: arm and leg lilt 175; exercises 173-175; leg lilt 174-175; stretch 118 four-point leg flexion/extension 174 four-point pelvic shift 174 lree squat 196 free weight concerns 213-214 exercises: about 213;basic 214-219; for explosive power 219-222
free weight
Fu, EH. 79,200 lunctional taping
144-145
G gender, and range of motion 30 gluteus maximus inner-range exercise 147-149 gluteus maximus muscle balance assessment 104 gluteus medius muscle balance assessment 105 good morning 216 gym ball exercises 186-197 gymnasts: and lordotic posture 146; proprioceptive training 200; and sacroiliac joint pain 49
H hall lunge 114 hall lunge (without chair) 149 half-sitting arm and leg movements hamstrings, stretching 113
hang clean 220
188-189
Index. heel bridge 193 heel bridge with leg raise, ball rolling 194 heel slide 128: basic movement 170; using pressure biofeedback 106 height losses 26,27, 27f Hemborg. B. 64-65 herniated lumbar disc 6-7 Hides, J.A. 51 hip extensor muscles 36, 122 hip flexor muscles 123 hip hinge 36; in high kneeling 76; in standing 72-73; with table support 77 hip hitch 115 hip joint, motion relationships with pelvis and lumbar spine 351 hip muscles, inner-range holding tests 103-105 Hodges, P. 61 holding 94 holistic treatment 235-236 hollow back 145. (set!also lordotic posture home back care 249f hoop pressure 45 hydraulic amplifier effect 47-48 hyperflexibility 95-96 hypoflexibility 95-96 hysteresis 20
I iatrogenic back pain factors 4-5 iliacus 54f 561 iliopsoas muscle: about 54-55; illustrated 54J; muscle balance assessment 103 immobilization: effects on muscles 101f; muscle adaptation 96-99 impaction 33 inclinometer 139,141 inert tissues 11 inguinal ligament 57f injury, muscle adaptation 96-99 injury prevention 247-253 inner-range holding ability 103-106 innominate bone 17 internal oblique muscle 57,57f interspinous-supraspinous-thoracolumbar complex 18f intervertebral discs, axial compression 26-28 intra-abdominal pressure mechanism 62-65,631 intradiscal pressure 301 intrathoracic pressure 62-63 intra truncal pressure 62 investing fascia 17 ipsilateral, defined 45 ischemic, defined 17
J Jacob, H.A.e. 25 Janda, V. 145-146 joint degeneration 79 joint loading, minimizing 134 joints, vertebral column anatomy joint stability 8
K Kent, M. 223 keyhole 138
14-15
267
kinesthesis 136, 198 Kissling. R.O. 25 knee raising in standing 71 Koh, T.J. 102 Kukulka, e.G. 111 kyphotic back 45, 145f 157-162
L lamina, lamina lateral lateral lateral lateral
defined 45 of vertebral arch 17 flexion 17,33 malleolus 135 pulldown 206-207 raphe 45 laxity 95-96 lean clients, and abdominal hollowing 83 leg lowering 128,170 leg raise throw 227 Lephart, S.M. 79, 200 Lifting: appropriate stance and grip 251-253; arch model of spine 38-40; flexion relaxation response 37-38; large objects 37, 252J; mechanics 35-40,36J; methods 40-41; minimizing stress 250-253; planning 248, 250; principles 248-253; safe zone 250-251; as set of torques 3537; with unstable spine 59; and Valsalva maneuver 64 Ligaments: elasticity 20; self locking 48; of spinal segment 16f 161; and spinal stability 11; of vertebral column 15-16, 18-20 limb strength 202 limits,
in weight
training
205
linea alba 57f line of gravity: gravitational torques maintaining 135fi in postural
137, 139t; assessment
136-137 long dorsal sacroiliac ligament 48 Lord, S.R. 136 Lordosis: defined 17; depth measurement 141142,141f lordotic index 142 lordotic posture 145-150, 145f low back pain: anticipatory nature of stability 61; incorrect sitting positions 181; and multifudus muscle 51-52; and superficial muscles 53 tower back muscles, inner-range holding tests
103-105 low-level contractions 94 low pulley spinal rotation 210-211 lumbar curvature 40,41f lumbar erector spinae 52 lumbar hypermobility 8 lumbar iliocostalis muscle 53 lumbar instability 8-10 lumbar longissumus muscle 52-53 lumbar neutral position 10, 78-79 lumbar-pelvic dissociation 71-74 lumbar-pelvic rhythm: about 34-35; assessing in prone kneeling 72; in closed kinetic chain 34f; correct function 70; in open chain 34J; regaining correct 74-78
268
.
Index
lumbar region 191 lumbar spine: biomechanics 14; flexion and extension 30-33; lateral view 53f; lumbar-pelvic rhythm 34-35; motion relationships with pelvis and hip joint 351; rotation and lateral flexion 33; stabilization mechanisms 43; stable movement and position 9-10; in standin~ extension, and flexion 321 lumbar stabilization model: about 7-8; spinal stability 11-12; stable movement and position 9-10 Luttgens, K. 136 lying, lost height restoration 26 lying abdominal hollowing 85-86 lying barbell row 215 lying trunk curl over ball 189 lying trunk curl with leg lift 190 Lynn, R. 102
M machine exercises 205-212 machismo, and lifting 250 McKenzie, R.A. 142,156 Main, Cj. 5 medicine balls 226-227 medicine ball trunk curl 226-227 men, range of motion 30 mobile surfaces 201 mobilizer muscles: about 92,94; affecting lower back 96/; characteristics 93/ modified trunk curl 146-147 momentum, and free weights 213 Moore, M.A. 111 Morgan, D.L. 102 motion sense 136 motor skiIlleaming stages 143/ motor skiU training 143-144 movement sense 198 multifudus contraction 89-90 multifudus muscle: contraction 89-91; exercise effects 51; exercises for contraction 8990; function 50-51; lateral view SOft medical treatment effects 51; targeting 7 multisensory cues 86 muscle activity: changes with speed increase 98f; patterns during rapid knee flexionextension 98f; in weight training 203 muscle balance assessment: in gluteus maximus 104; in gluteus medius 105; in iliopsoas 103 muscle imbalance: about 92; assessment 237; characteristics 94-96; and posture 95f muscle length: about 100; adaptation 101f; chronic muscle lengthening 100-102; shortened muscle assessment 106-110; stretched muscle assessment 103-106 muscle reaction speed using mobile platform
201 muscles:
of abdomen 57f; adaptation to injury, immobilization, and training 96-99; of back 52f; basic concepts 92-96; electrical silence 37-38; endurance vs. strength 206; immobilization effects 101f; lengthtension relationship 38f; in optimal
posture alignment 134; proprioceptive functions 94; re-ed uca tion 69; stretching principles 111-113; target stretching 113118; thoracolumbar fascia attachments 46f; transmission of force 18; types 93/; voluntary control 69; working large groups first 238 muscle stiffness regulation 198-199
N nerve root entrapment 6 nerve root pain 232,233 nervous system training 198-199 neural arch ligaments 15-16, 16t, 18 neural control centers 11 neural system, developing 12 neutral position: and abdominal hollowing 82; in crook lying position exercises 171; of lumbar spine 10,78-79; teaching clients 78-81; in weight training 203 neutral position maintenance 185 neutral zone 9-1O,9f Ng, G. 97 Norris, CM. 30,92, 232, 238 nucleus pulposus 20,21-22,211 nutation, of sacroiliac joint 24t, 25, 48
a Ober test 108-109, 151 Ober test stretch 115-116 obese clients 83,239-240 occiput 17 occupational considerations 32 overemphasis of single aspect 235 overhead lifting 59,59f overload principle 235 overstretch 100 overuse injury 204
p pain (see also back pain; chronic low back pain; low back pain): acute pain case history 242-244; anticipation of 5; assessing 231232; nerve root pain 232, 233; not exercising through 205; as reliable guide 234 palpation 86-87, 87j. 91f Panjabi, M.M. 9,10,51 parallel exercise progressions 236 passive back extension in lying position 156-157 passive positioning reproduction 80, 199-200 passive stability system 10 passive support, of lumbar region 12 pelvic crossed syndrome 145-146 pelvic inclinometer 139,141 pelvic inlet 17 pelvic motion control, assessing in frontal plane 73 pelvic rock on rocker board 184 pelvic rock on wobble board 185 pelvic shift with leg lift 180 pelvic shift with unloading 179 pelvic tilt: inclinometer assessment 139,141; passive assessment 72; repeated pelvic tilting exercises 183-186 pelvic tilt control: about 70; lumbar-pelvic dissociation 71-74; segmental control 70
Index.
pelvic tilt re-education, sitting 157 pelvis, motion relationships with hip joint and lumbar spine 351 Perey, O. 37 periosteum 17 permanent disability 3 physiology 238 plumb line, in postural assessment 137, 137f, 138139 plyometric exercises 225-227 plyometric flexion and extension using punching bag 226 plyometrics: about 202; for power and speed 222-225; preparation 225 plyometric side bend using punching bag 225 PNF stretching 111-113 poor conditioning: in traditional sit-up 121-122; in traditional straight-leg raise 123 poor stability, case history 240-242 posterior ligamentous system 43-44 postural muscles 92. (see also stabilizer muscles postural stability, and body sway 135-136 posture: anatomical landmarks 137-138; assessing 237; basic assessment 136-142; correction principles 143-145; dynamic posture 135; energy expenditure reduction 135; home-exercise programs 143-144; "low-tech" measurement 143; and muscle imbalance 95f; optimal alignment 134-135; re-education 144; standard reference 138J; standing posture assessment 140f; static posture
135 Posture Committee, American Academy of Orthopaedic Surgeons 134 posture grid 138-139 posture types: about 145; flatback 145f, 156-157; kyphotic back 45, 145f, 157-162; lordotic posture 145-150,1451; swayback 1451, 150-155 power: defined 223; in free-weight exercises 219-222; with plyometrics 222-227 power clean 221 preload effect 224 pressure biofeedback 105-106 primary mobilizer muscles 93t primary stabilizer muscles 93t principle of overload 235 principle of specificity 234-235 prolapse, defined 17 prone abdominal hollowing test using pressure biofeedback 105-106 prone bent-leg lift 172 prone fall 194: with arm lift 195; with single-leg lift 195 prone lying 83 prone lying gluteal brace 171 proprioception: basic concepts 79-80; components 79t; defined 79; kinesthesis 198; movement sense 198; regulation of muscle stiffness 198-199; theory 198-199; training benefits 199-200 proprioceptive neuromuscular facilitation 111113. (see also PNF stretching) proprioceptive training 197-201
269
proteoglycans 21-22,28 psoas 54f, 561 pulley crunch 212 punching bags 225-226 pyramid training 206, 238
Q quadratus
lumborum
muscle
54
R range of motion 30, 35 raphe, lateral 45 rapid displacement in sitting 200 reaction time 223 rectus abdominis muscle 55-56, 57f, 591 rectus sheath 57f, 58f, 591 reinjury prevention 247-253 relative flexibility 951 relative stiffness 951 repeated pelvic tilting exercises 183~186 repetitions, in weight training 206 reproduction of active positioning 80-81 reproduction of passive positioning 80, 199-200 response time 223 rest, as most common treatment 6 reverse bridge 193 reverse bridge and roll 193 reverse crunch, ab roller 131 rhythmic stabilization 90-91: of multifudus and lateral abdominals in side lying position
90-91 Richardson, C. 61 Richardson, C.A. 97, 99 Risch, S.V. 7 rocker boards 183, 184 rotary torso machine 211 rotation, of lumbar spine 33
round-shouldered posture 158 S joint: about 23-25; gymnasts' pain 49; illustrated 23J; movement 241; and thoracolumbar fascia coupling 48-49 sacrotuberous ligament 48 sacrum, in standing, extension, and flexion 32/ safety checklist, weight training 204 sagittal plane 17, 139/ sagittal rotation 17,31 S.A.I.D. (specific adaptation to imposed demand) 99-100 scapula repositioning 160-161 Schmid, H.j.A. 145-146 Schmorls node 17, 27 sciatica 6 seated rowing 209 segmental control 70, 94, 95 self-assessment in lifting 250 serial sarcomere number 100-102 serious spinal pathology 233 serratus anterior muscle 57! shortened muscle assessment 106-110 shoulder, postural changes around 159/ shoulder girdle alignment 158/ side crunch, ab roller 132 side lying body lift 178 side lying hip lift 178
sacroiliac
270
.
Index
side lying knee lift 176 side lying leg abduction 177 side lying leg rotation 176-177 side lying position exercises 175-178 side lying spine lengthening 177 simple pelvic tilt, progressing to balance boards 184 single arm pulley row 210 single aspect overemphasis 235 single-bent leg raises 171 single-handed lift 253f single-leg heel bridge 194 sitting, hip flexor shortening 154-155 sitting, intradiscal pressure 30-31 sitting bilateral hip adductor stretch 152 sitting hamstring stretch 182 sitting hip hinge 185-186 sitting knee and arm raise 183 sitting knee raise 183,188 sitting lateral tilt using gym ball 78 sitting pelvic tilt using gym ball 77-78 sitting position exercises 181-183 sitting sternal lift 182-183 sitting wide splits 152-153 sit-up: exercises 64; modified 124-127; traditional 120-122 Skall, EH. 6 skill-based exercise therapy 6-7 slouched posture 150. (see also swayback slow-twitch muscles 93 snatch lift 253 specific adaptation to imposed demand 99-100 specificity principle 234-235 speed: defined 223; with plyometrics 222-227 spinal discs: avascular nature 22; concentric bands 21; of vertebral column 20-22 spinal extensor muscles: about 49-50; deep (intersegmental) muscles 50-52; superficial muscles 52-54 spinal lengthening 153-154 spinal pathology 233 spinal range of motion 35 spinal segment 14,15/ spinal segment ligaments 16f, 16t spinal stability: achieving and maintaining 1112; and lifting 36; system 11/ spine: arch model 38-40; as cantilever system 36-37; keeping vertical 247-248; structural changes 4 spondylolisthesis 7, 7f spondylolysis 7,7/ squat 216-218 squat lift 40-41 stability ball exercises 186-197 stability program: advanced design 237-238; design principles 234-235; parallel tracks 235-237 stabilizer muscles: about 92-96; affecting lower back 96/; characteristics 93t stadiometer 142,142f standing: abdominal hollowing 82; axial compression 26 standing abdominal hollowing 84
standing assisted pelvic tilt 74 standing hip abduction 180 standing hip hinge 181 standing hip hinge movement 72-73 standing knee raising 71 standing position exercises 178-181 standing posture assessment 140f standing sternal lift 179 starting positions 31,82-86,169 static joint positioning 8D-81 static posture 135 static stretching I11t, 112, 113 sternal lift exercise 162 stiffness 95-96,198-199 stoop lift 40-41 straight-leg raise: modified 127-130; traditional 123-124 straight-leg raise test 109-110 stretched muscle assessment 103-106 stretching: principles 111-113; target muscles 113-118; techniques I11t stretch-shorten cycle 223-224 stretch weakness 100 structural injury 4 structural taping 144 superficial abdominal muscles 55-57 superficial spinal extensor muscles 52-54 superimposed limb movements 168-169 superman, basic 190 superman with arms 190-191 superset 238 surgery 6 sustained flexion 31-32 swayback 145f, 150-155, 151f symmetry, in postural assessment 138 synovia 22
T tactile cues 86-87 taping 144-145,244-245 task muscles 92. (see also mobilizer muscles) teaching clients: abdominal hollowing 81-89; advance preparation 69; modifications of exercises 124; multifudus contraction 89-91; multisensory cues 86; neutral position 78-81; pelvic tilt control 70-78; rhythmic stabilization 90-91; tactile cues 86-87; visualization 88 terminology 17,45,135 therapist referrals 234 Thomas test 107-108,237 Thomas test stretch 114 thoracic iliocostalis muscle 53 thoracic joint mobilization 159-160 thoracic longissimus muscle 53 thoracolumbar fascia: coupling and sacroiliac joint 48-49; cross section 46f; as hydraulic amplifier 47-48; muscle attachments to 46f; structure 44-45 thoracolumbar fascia mechanism 45,47,47/ threshold to detection of passive motion 198,199200 throw-catch activities on mobile surface201
Index' tightening 94 tightness, assessing 107 tissue microtrauma 204,248 tissue overstretch 31 torque: defined 35; lifting as set of 35-37; in posterior ligamentous system 44 trabecula 17 tragus 135 trainer qualifications 214,234 . . . training: abdominaUsee abdommal trammg); abdominal muscle recruitment 99J; advanced training qualifications 167-168; motor skill training 143-144; muscle adaptation 97-99; nervous system 198199; postural sway reduction 136; . progression 168-169,206,214; prop noceptive training 197-201; pyramid training 206, 238 training specificity 99-100 transversalis fascia 58! 59! transversus abdominis muscle 57-58, 58!, 61-62, 62f traumatic injury 204 treatment costs 3-4 Trendelenburg sign 73, 151 trigger points 106 tripod stretch 117 tripod test 110 trunk alignment, in traditional sit-up 121! trunk curl 126-127 trunk flexion, in traditional sit-up 132! trunk flexion with high pulley 212 trunk muscle action: abdominal muscles 55-60; coordination of abdominals during spinal movement 60-62; iliopsoas 54-55; spinal extensor muscles 49-54 trunk side flexor stretch 117-118 trunk stability, in overhead lifting 59-60, 59! TTDPM (threshold to detection of passive motion) 198,199-200 twist and throw with medicine ball 226 Twomey, L.T. 65
type type
II movement I movement
271
33 33
U unwillingness
to exercise
244-245
V Valsalva maneuver 63-64 ventral, defined 17 ventral ligaments 16/, 18-20 vertebral column IS! vertebral column anatomy: bones and joints 1415; facet joints 22-23; ligaments 15-16, 18-20; sacroiliac joint 23-25; spinal discs 20-22 vertebral compression 125/ vertebral pedicle 17 vertical spine 247-248 video feedback 241,245 visualization 88 Vleeming, A. 48 voluntary muscle control 69
W Waddell, G. 6 wall bar hanging leg raise 129-130 wall sit 195-196 Watson, P.). 5 webbing belt 87,87! Weber, H. 6 Webright, WG. 112 Weider,). 207 weight bag passive stretch 161-162 . weight training: about 202; free weight exercises 213-222; machine exercises 205-212; preparation 203; program design 238; safety 204 Wells, K. 136 wobble boards 183, 185 women, range of motion 30
Z Zetterberg,
C. 61
About the Author Christopher M. Norris, MSc, MCSp, has more than twenty years of experience as a physiotherapist and sport scientist. His specialty is exercise therapy. He is currently the director of Norris Associates in Manchester, UK. An expert on back stability, Norris is the author of four books. One of his books on sports injuries is in its second edition and has been adopted by most physiotherapy schools in the United Kingdom. He has taught for the British Association of Sports Medicine on flexibility training and back rehabilitation. In addition to serving as a consultant to major companies, Norris also published the first-ever review of back stability in a series of articles in Physiotherapy Journal. Norris is a member of the Chartered Society of Physiotherapy and the Society of Orthopaedic Medicine. He holds a certificate in occupational health physiotherapy, an advanced certificate in acupuncture, and a certificate in business administration. He and his wife Hildegard live in the Peak District National Park. He enjoys hill walking and ju jitsu.
272
1
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺍﺭﺍﺋﻪﻛﻨﻨﺪﻩ ﻛﺘﺎﺏ ﻭ ﻧﺮﻡﺍﻓﺰﺍﺭﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﺎﻥ ﻫﻤﮕﺎﻡ ﺑﺎ ﺗﻮﺳﻌﻪ ﻋﻠﻤﻲ ﻭ ﻓﺮﻫﻨﮕﻲ ﺟﻬﺎﻥ ﻣﻌﺎﺻﺮ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺭﻭﺯﺍﻓﺰﻭﻥ ﻛﺎﻣﭙﻴﻮﺗﺮ ﺩﺭ ﺑﻴﻦ ﺟﻮﺍﻣﻊ ﺑﺸﺮﻱ ﺧﺼﻮﺻ ًﹰﺎ ﺭﺷﺘﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻋﻠﻮﻡ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺑﻬﻴﻨﻪ ﺍﺯ ﺁﺧﺮﻳﻦ ﻳﺎﻓﺘﻪﻫﺎﻱ ﭘﺰﺷﻜﻲ ﺩﻧﻴﺎ ﻭ ﺍﺭﺍﺋﻪ ﺍﻳﻦ ﻳﺎﻓﺘﻪﻫـﺎ ﺩﺭ ﻗﺎﻟـﺐ ﻧـﺮﻡﺍﻓﺰﺍﺭﻫـﺎﻱ ﭘﺰﺷﻜﻲ ) VHS ، DVD ، VCD ، ebookﻭ (...ﻣﺎ ﺭﺍ ﺑﺮ ﺁﻥ ﺩﺍﺷﺖ ﻛﻪ ﺑﺎ ﮔﺮﺩﺁﻭﺭﻱ ﻭ ﺍﺭﺍﺋﺔ ﺍﻳﻦ ﻳﺎﻓﺘﻪﻫﺎ ﮔﺎﻣﻲ ﻛﻮﭼﻚ ﺩﺭ ﺭﺍﻩ ﺍﺭﺗﻘﺎﺀ ﺳﻄﺢ ﻋﻠﻤﻲ ﻣﺘﺨﺼﺼﻴﻦ ﻛﻠﻴﻪ ﺭﺷﺘﻪﻫﺎﻱ ﭘﺰﺷﻜﻲ ﻛﺸﻮﺭ ﺑﻪ ﺻﻮﺭﺕ ﺳﻤﻌﻲ ﻭ ﺑﺼﺮﻱ ﺑﺮﺩﺍﺭﻳﻢ .ﺍﻣﻴﺪ ﺍﺳﺖ ﻣﺸﻮﻕ ﻣﺎ ﺩﺭ ﺍﻳﻦ ﺭﺍﻩ ﺑﺎﺷﻴﺪ. ﻟﺬﺍ ﻋﻼﻗﻤﻨﺪﺍﻥ ﻣﻲﺗﻮﺍﻧﻨﺪ ﺑﺮﺍﻱ ﺩﺭﻳﺎﻓﺖ ﻫﺮ ﻳﻚ ﺍﺯ ﻣﺤﺼﻮﻻﺕ ﺍﺭﺍﺋﻪﺷﺪﻩ ﺑﻪ ﺍﺯﺍﺀ ﻫﺮ CDﻣﺒﻠﻎ ٥٠٠٠ﺗﻮﻣﺎﻥ ﺑﻪ ﺣﺴﺎﺏ ﺟﺎﺭﻱ ١٣٢٤٣٦ﺑﺎﻧﻚ ﺭﻓﺎﻩ ﻛﺎﺭﮔﺮﺍﻥ ﺷﻌﺒﻪ ﻣﻴﺪﺍﻥ ﺍﻧﻘﻼﺏ ﻛﺪ ﺷﻌﺒﻪ ١١٢ﺑﻪ ﻧﺎﻡ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﻭﺍﺭﻳﺰ ﻭ ﭘـﺲ ﺍﺯ ﻓﺎﻛﺲ ﻓﻴﺶ ﻓﻮﻕ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﺸﺎﻧﻲ ﺩﻗﻴﻖ ﻧﺴﺒﺖ ﺑﻪ ﺧﺮﻳﺪ ﺍﻗﻼﻡ ﻭ ﺩﺭﻳﺎﻓﺖ ﻛﺎﻻﻱ ﻣﻮﺭﺩ ﻧﻈﺮ ﺧﻮﺩ ﺍﻗﺪﺍﻡ ﻧﻤﺎﻳﻨﺪ .ﻻﺯﻡ ﺑﻪ ﺫﻛﺮ ﺍﺳﺖ ﻓﻘﻂ ﺑﻪ ﺳﻔﺎﺭﺷﺎﺗﻲ ﻛﻪ ﻭﺟﻪ ﻣﻮﺭﺩ ﺳﻔﺎﺭﺵ ﺑﻪ ﺣﺴﺎﺏ ﻓﻮﻕ ﺫﻛﺮ ﻭﺍﺭﻳﺰ ﺷﺪﻩ ﺗﺮﺗﻴﺐ ﺍﺛﺮ ﺩﺍﺩﻩ ﺧﻮﺍﻫﺪ ﺷﺪ ،ﻟـﺬﺍ ﺧﻮﺍﻫﺸﻤﻨﺪ ﺍﺳﺖ ﺍﺯ ﻭﺍﺭﻳﺰ ﻭﺟﻪ ﺑﻪ ﻫﺮ ﮔﻮﻧﻪ ﺣﺴﺎﺏ ﺩﻳﮕﺮﻱ ﺍﻛﻴﺪﺍ ﺧﻮﺩﺩﺍﺭﻱ ﻓﺮﻣﺎﺋﻴﺪ. ﻻﺯﻡ ﺑﻪ ﺫﻛﺮ ﺍﺳﺖ ﺩﺭ ﺻﻮﺭﺕ ﻧﻴﺎﺯ ﺑﻪ ﻫﺮﮔﻮﻧﻪ ﺍﻃﻼﻋﺎﺕ ﺗﻜﻤﻴﻠﻲ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺑﻪ ﻧﺸﺎﻧﻲ ﻣﺮﻛﺰ ﻣﺮﺍﺟﻌﻪ ﻭ ﻳﺎ ﺑﺎ ﺗﻠﻔﻦ ٦٩٣٦٦٩٦ﺗﻤﺎﺱ ﺣﺎﺻﻞ ﻧﻤﺎﻳﻴﺪ.
-١ﺭﺍﺩﻳﻮﻟﻮﮊﻱ
ﻋﻨﻮﺍﻥ CD
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
)3D Conformal Radiation Therapy A multimedia introduction to methods and techniques (Springer
ــــــ
1.1
)2.1 Abdominal and pelvic Ultrasound with CT and MR correlation (R. Brooke Jeffrey, Jr., M.D.
ــــــ
ﺍﻳﻦ ﻳﻚ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺷﻲ ﻗﻮﻱ ﺑﻤﻨﻈﻮﺭ Self teachingﻭ Self evaluationﺗﺸﺨﻴﺺﻫﺎﻱ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺷﻜﻢ ﻭ ﻟﮕﻦ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻛﻨﺎﺭ ﺗﺼﺎﻭﻳﺮ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ ﺑﻴﻤﺎﺭﻱ ،ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﻫﻤﺰﻣﺎﻥ CT Scanﻭ MRIﺑﺮﺍﻱ ﻓﻬﻢ ﻭ ﺩﺭﻙ ﺑﻬﺘـﺮ ﻣﻄﺎﻟـﺐ ﺍﺳـﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ، CDﻣﺒﺎﺣﺚ ﻣﺨﺘﻠﻒ ﺑﻪ ﺻﻮﺭﺕ Caseﻣﻄﺮﺡ ﮔﺮﺩﻳﺪﻩ ﻭ ﺿﻤﻦ ﺑﻴﺎﻥ ﺷﺮﺡ ﺣﺎﻝ ﺑﻴﻤﺎﺭ ،ﺗﺼﺎﻭﻳﺮ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ )ﻭ ﺩﺭ ﺻﻮﺭﺕ ﻟﺰﻭﻡ MRIﻭ (CT Scanﺑﻪ ﻧﻤﺎﻳﺶ ﮔﺬﺍﺷﺘﻪ ﺷﺪﻩ ﻭ ﺑﺎ Clickﺁﺭﺍﻳﺔ ،Textﻣﻄﺎﻟﺐ ﺗﺌﻮﺭﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ Caseﺑﺎ ﺑﻴﺎﻧﻲ ﺳـﺎﺩﻩ ﻭ ﺩﺭ ﻋﻴﻦ ﺣﺎﻝ ﻛﺎﻣﻞ ،ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻛﺎﺭﺑﺮ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ. ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ ﺍﻳﻦ CDﺑﺮ ﺣﺴﺐ ﻣﻮﺿﻮﻉ ﺑﻪ ﻗﺮﺍﺭ ﺟﺪﻭﻝ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﺪﺍﺩ Case
٧٨
ﻣﻮﺿﻮﻉ ﺳﻴﺴﺘﻢ ﮔﻮﺍﺭﺷﻲ
ﺗﻌﺪﺍﺩ Case
٣٥
ﻣﻮﺿﻮﻉ ﻛﻠﻴﻪ ﻭ ﻏﺪﻩ ﺁﺩﺭﻧﺎﻝ
ﺗﻌﺪﺍﺩ Case
٣٧
ﻣﻮﺿﻮﻉ ﭘﺎﻧﻜﺮﺍﺱ
ﺗﻌﺪﺍﺩ Case
١٢ ٧
ﻣﻮﺿﻮﻉ ﻃﺤﺎﻝ ﺭﺗﺮﻭﭘﺮﻳﺘﻮﺋﻦ
ﺗﻌﺪﺍﺩ Case
٤٠ ٤٦
ﻣﻮﺿﻮﻉ ﻛﻴﺴﺔ ﺻﻔﺮﺍ ﻭﻣﺠﺎﺭﻱ ﺻﻔﺮﺍﻭﻱ ﻟﮕﻦ
ﺗﻌﺪﺍﺩ Case
٦٧ ١٠
ﻣﻮﺿﻮﻉ ﻛﺒﺪ ﺣﺎﻣﻠﮕﻲ
)ACR - Chest (Learning file) (American college of Radiology ﺍﻳﻦ CDﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ:
2001 4- Airway Disease 8-Pediatric Chest 12- Immunocompromised Host
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
3- Vascular Disease 7- Chest Wall and Diaphragm 11- Pulmonary Infection
2- Cardiac Disease 6- Pleural Disease 10- Neoplasma and Tumors
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
3.1
1- chest Trauma 5- Mediastinal Masses 9- Normal Disease 13- Diffuse Disease
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
2 ACR - Gastrointestinal (Learning file) (American college of Radiology) (Igor Laufer, M.D., James M. Messmer, M.D.) (Learning file) (American college of Radiology) 5.1 ACR - Genitourinary ( ﺑﻮﺩﻩ ﻭ ﺩﺭﺻﻮﺭﺕ... ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻭ، CT Scan ، ﻣﻄﺎﻟﻌﺎﺕ ﺑﺎ ﻣﻮﺍﺩ ﺣﺎﺟﺐ، ﺗﺼﺎﻭﻳﺮ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ )ﻋﻜﺲﻫﺎﻱ ﺳﺎﺩﻩ، ﺩﺍﺭﺍﻱ ﺗﺎﺭﻳﺨﭽﻪ ﺑﺎﻟﻴﻨﻲCase ﻫﺮ. ﻣﻄﺮﺡ ﮔﺮﺩﻳﺪﻩﺍﻧﺪCase ﺗﻌﺪﺍﺩﻱ، ﺷﺎﻣﻞ ﻓﺼﻮﻝ ﻣﺘﻌﺪﺩﻱ ﺩﺭ ﺧﺼﻮﺹ ﺍﻭﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻣﻲﺑﺎﺷﺪ ﻭ ﺩﺭ ﻫﺮﻓﺼﻞCD ﺍﻳﻦ . ﺗﺸﺨﻴﺺ ﻧﻬﺎﻳﻲ ﻭ ﻫﻤﭽﻨﻴﻦ ﺗﻮﺿﻴﺤﺎﺕ ﻋﻠﻤﻲ ﺍﺿﺎﻓﻪ ﻣﺮﺗﺒﻂ ﺑﺎ ﺗﺸﺨﻴﺺ ﺑﺎ ﺍﻃﻼﻉ ﺷﺪ، ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﺭﺍﻳﻪﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﻣﻲﺗﻮﺍﻥ ﺍﺯ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ، ﺩﺭﻧﻬﺎﻳﺖ. ﻣﻄﻠﻊ ﮔﺮﺩﺩFinding ﻧﻤﻮﺩﻥ ﺑﺮﺭﻭﻱ ﺁﻳﻜﻮﻥClick ﺑﺎImaging ﻓﺮﺩ ﻣﻲﺗﻮﺍﻧﺪ ﺍﺯ ﻳﺎﻓﺘﻪﻫﺎﻱ،ﻧﻴﺎﺯ : ﻫﺎﻱ ﻣﻄﺮﺡ ﺷﺪﻩ ﺑﺮ ﺣﺴﺐ ﻫﺮ ﻓﺼﻞ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCase ﺗﻌﺪﺍﺩ 4.1
ﻣﻮﺿﻮﻉ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﻠﻴﻪ ﺑﺎﻟﻐﻴﻦ
ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case
١١٨
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﻠﻴﻪ ﺍﻃﻔﺎﻝ
ﺗﻌﺪﺍﺩ Case
٢٦
ﻣﻮﺿﻮﻉ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺣﺎﻟﺐ
ﺗﻌﺪﺍﺩ
ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case
Case
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﮊﻧﻴﻜﻮﻟﻮﮊﻳﻚ
١٧
ﻣﻮﺿﻮﻉ ﻏﺪﺩ ﺁﺩﺭﻧﺎﻝ
١٥
ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case
ﺳﻴﺴﺘﻢ ﺍﺩﺭﺍﺭﻱ ﺗﺤﺘﺎﻧﻲ ﺍﻃﻔﺎﻝ
١١
ﺗﻌﺪﺍﺩ
ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case
١٨
Case
ﺭﺗﺮﻭﭘﺮﻳﺘﻮﺋﻦ
١٠
ﻣﻮﺿﻮﻉ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺜﺎﻧﻪ
ﺗﻌﺪﺍﺩ Case
١٧
ﻣﻮﺿﻮﻉ
ﺗﻌﺪﺍﺩ Case
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﭘﺮﻭﺳﺘﺎﺕ
١٠
ﻣﻮﺿﻮﻉ ﺩﺳﺘﮕﺎﻩ ﺗﻨﺎﺳﻠﻲ ﺧﺎﺭﺟﻲ ﻣﺬﻛﺮ
1998 1998
ﺗﻌﺪﺍﺩ Case
١٦
6.1
ACR - Head & Neck (Learning file) (American college of Radiology)
1998
7.1
ACR - Neuroradiology (Learning file) (American college of Radiology)
1998 ــــــ
ACR - Nuclear medicine (Learning file) (American college of Radiology) (Paul Shreve, M.D. and James Corbett, M.D.) 9.1 ACR - Pediatric (Learning file) (American college of Radiology) (Beverly P. Wood, M.D., David C. Kushner, M.D.) : ﻣﺮﺗﺒﻂ ﺑﺎ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺍﻃﻔﺎﻝ ﺑﻮﺩﻩ ﻭ ﺩﺍﺭﺍﻱ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪTeaching File ﻓﻮﻕ ﻳﻚCD
8.1
ﻋﻨﻮﺍﻥ
Case ﺗﻌﺪﺍﺩ
Chest
٢٠٢ ٣١
ﺳﺮ ﻭ ﮔﺮﺩﻥ
ﻋﻨﻮﺍﻥ ﻗﻠﺐ ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ
Case ﺗﻌﺪﺍﺩ
٧٨ ٩٠
Case ﺗﻌﺪﺍﺩ
ﻋﻨﻮﺍﻥ ﮔﻮﺍﺭﺵ Skeletal
١٦٣ ٩٧
ﻋﻨﻮﺍﻥ ﭘﺎﻧﻜﺮﺍﺱ، ﻃﺤﺎﻝ،ﻛﺒﺪ
Case ﺗﻌﺪﺍﺩ
ﻋﻨﻮﺍﻥ
Case ﺗﻌﺪﺍﺩ
٧١
Genitourimary
١٠٩
10.1 ACR - Skeletal (B.J Manaster, M.D., Ph.D.) (Learning file) 1. Tumolrs 2. Arthritis 3. Trauma 4. Metabolic Congeaital 11.1 ACR
1998
ــــــ
- Ultrasound (Learning file) (American college of Radiology)
1998
12.1 Anatomy and MRI of the JOINTS (A Multiplanar Atlas) (William D. Middleton, Thomas L. Lawson)
(Department of Radiology Medical College of Wisconsin Milwaukee, Wisconsin) The Tmporomandibular
The Shoulder
The Wrist
The Finger
The Vertebral Column
The Hip
The Knee
The Ankle
TM
Brainiac! Medical Multimedia Systems Presents (Version 1.52) (An interactive digital atlas designed to assist in learning human neuroanatomy) Breast Implant Imaging (SALEKAN E-BOOK) (MICHAEL S. MIDDLETON, PH,D., M.D, MICHAEL P.MCNAMARA JR., M.D.) 13.1 9.9
(Serial # 316.34427)
:ﺍﻳﻦ ﻛﺘﺎﺏ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ A History and Overview of Breast Augmentation and Implant Imaging Basic Principles of Breast Implant Imaging Classification of Breast Implants Evaluation of Silicone Fluid Injecitons
Clinical Presentation Principles of Imaging Breast Implant Rupture and Soft-Tissue Silicone Practical Consideration in the Evaluaion of Implant Integrity Breast Cancer Imaging
14.1 Carotid Duplex Ultrasonography Extracranial and Intracranial
2000 2003
Methods of Imaging Artifacts of MR and Ultrasound Imaging of Breast Implants and Soft-Tissue Silicone Evaluation of Soft-Tissue Silicone from Ruptured Implants Surgical and Other Considerations
(Michael Jaff DO, Serge Kownator MD, Alain Voorons Audlovlsuel)
ــــــ
ﺣﻠﻘﺔ ﻭﻳﻠﻴﺲ ﺗﻨﻪ ﺑﺮﺍﻛﻴﻮﺳﻔﺎﻟﻴﻚ ﻭ ﻗﻮﺱ ﺁﺋﻮﺭﺕ ﻣﻮﺭﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ ﻭ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺛﺎﺑﺖ ﻭ ﻣﺘﺤﺮﻙ ﮔﻮﻳـﺎ )ﺑـﻪ ﺯﺑـﺎﻥ ﺍﻧﮕﻠﻴﺴـﻲ( ﺟﻬـﺖ ﻧﻤـﺎﻳﺶ ﺗﻜﻨﻴـﻚﻫـﺎﻱ، ﻭﺭﺗﺒﺮﺍﻝ، ﺳﺎﺏ ﻛﻼﻭﻳﻦ، ﻛﻠﻴﺎﺕ ﺍﻧﺠﺎﻡ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻛﺎﺭﻭﺗﻴﺪ، CD ﺩﺭ ﺍﻳﻦ : ﺭﺋﻮﺱ ﻣﻄﺎﻟﺐ ﻣﻮﺭﺩ ﺑﺤﺚ ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺪﻳﻦ ﻗﺮﺍﺭ ﺍﺳﺖ. ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ،ﺳﻮﻧﻮﮔﺮﺍﻓﻲﻫﺎﻱ ﻓﻮﻕ ﻭ ﻫﻤﭽﻨﻴﻦ ﭼﮕﻮﻧﮕﻲ ﺗﻔﺴﻴﺮ ﻧﺘﺎﻳﺞ ﺣﺎﺻﻞ ﺍﺯ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻓﻮﻕ ﻭ ﻫﻤﭽﻨﻴﻦ ﭼﮕﻮﻧﮕﻲ ﺗﻔﺴﻴﺮ ﻧﺘﺎﻳﺞ ﺣﺎﺻﻞ ﺍﺯ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻓﻮﻕﺍﻟﺬﻛﺮ ﺁﺷﻨﺎﻳﻲ ﺑﺎ ﺩﺳﺘﮕﺎﻩ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺳﺎﺏ ﻛﻼﻭﻳﻦ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﺳﻮﺑﺮﺍﻝ ﻭ ﺣﻠﻘﺔ ﻭﻳﻠﻴﺲ
ﺩﺳﺘﮕﺎﻩSetting ﭼﮕﻮﻧﮕﻲ ﺍﺳﻜﻦﻛﺮﺩﻥ ﻋﺮﻭﻕ ﻓﻮﻕﺍﻟﺬﻛﺮ ﻭ ﻧﺤﻮﺓ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻭﺭﺗﺒﺮﺍﻝ ﺿﺎﻳﻌﺎﺕ ﻣﺠﺎﻭﺭ
ﺷﺮﻳﺎﻥﻫﺎﻱ ﻛﺎﺭﻭﺗﻴﺪ ﺍﻛﺴﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻗﻮﺱ ﺁﺋﻮﺭﺕ ﻭ ﺗﻨﺔ ﺑﺮﺍﻛﻴﻮ ﺳﻔﺎﻟﻴﻚ Revaseularization ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﭘﺲ ﺍﺯ
. ﻣﻲﺑﺎﺷﺪPost-Test ﻭPre-Test ﺟﻬﺖ ﺍﺭﺯﻳﺎﺑﻲ ﻓﺮﺩ ﺍﺯ ﺧﻮﺩ ﺩﺍﺭﺍﻱCD ﺿﻤﻨﹰﺎ ﺍﻳﻦ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
3 ــــــ
)(Pamela T. Johnson, Alfred B. Kurtz
WITH CROSS-REFERENCES TO THE REQUISITES SERIES
15.1 CASE REVIEW Obstetric and Gynecologic Ultrasound
ﺍﻳﻦ CDﻣﺤﺘﻮﻱ Case ١٢٧ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺯﻧﺎﻥ ﻭ ﺯﺍﻳﻤﺎﻥ )ﺑﺼﻮﺭﺕ ﭘﺮﺳﺶ ﻭ ﭘﺎﺳﺦ( ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻫﻤﺮﺍﻩ ﺗﻮﺿﻴﺤﺎﺕ ﻭ ﺗﺼﺎﻭﻳﺮ ﻣﺮﺑﻮﻃﻪ ﺑﻮﺩﻩ ﻭ ﺩﺭ ﻓﻬﻢ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ Gynecologyﻭ Obstetricﺑﺴﻴﺎﺭ ﻣﻔﻴﺪ ﺧﻮﺍﻫﺪ ﺑﻮﺩ. ــــــ
)16.1 CD Roentgen (Michael McDermott, M.D., Thorsten Krebs, M.D.) (Williams & Wilkins
2000 ــــــ
17.1 Cerebral and Spinal Computerized Tomography )18.1 Cerebral MR Perfusion Imaging CD-ROM to complement the book (A. Gregory Sorensen, Peter Reimer) (Thieme
ﺍﻳﻦ CDﺩﺭ ﺯﻣﻴﻨﺔ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﭘﺮﻓﻮﺯﻳﻮﻥ ﻣﻐﺰﻱ ﺑﻮﺳﻴﻠﺔ MRIﺑﻪ ﺷﺮﺡ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﻭ ﻫﻤﭽﻨﻴﻦ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﺁﻧﻬﺎ ﭘﺮﺩﺍﺧﺘﻪ ﻭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺛﺎﺑﺖ ﻭ ﻣﺘﺤﺮﺕ ﺑﻪ ﺷﺮﺡ ﻣﻔﺎﻫﻴﻢ ﻣﺮﺗﺒﻂ ﺑﺎ ﺍﻳﻦ ﺭﻭﺵ ﺗﺸﺨﻴﺼﻲ ﻣﻲﭘﺮﺩﺍﺯﺩ. 19.1 CHEST X-RAY INTERPRETATION
2002
CDﺣﺎﺿﺮ ﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﺑﺮﻧﺎﻣﻪﻫﺎ )ﭼﻪ ﻛﺘﺎﺏ ﻭ ﭼﻪ (CDﺩﺭ ﻣﻮﺭﺩ ﭼﮕﻮﻧﮕﻲ ﺗﻔﺴﻴﺮ CXRﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ CDﺷﺎﻣﻞ ٣ﺑﺨﺶ Clinic -٣ seminar -٢ Library -١ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻋﻜﺲ ﺳﺎﻟﻢ ﺭﻳﻪ ﻫﻤـﺮﺍﻩ ﺑـﺎ ﺗﻮﺿـﻴﺤﺎﺕ ﻭ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻭ ﺑﺮﺍﻱ ﻓﻬﻢ ﻣﻄﻠﺐ ﻓﻴﻠﻢﻫﺎﻱ ٣ﺑﻌﺪﻱ animatoryﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺑﺨﺶ ﺍﻭﻝ Library :ﻳﺎ ﻛﺘﺎﺑﺨﺎﻧﻪ : ﺍﻟﻒ( ﺑﻴﻤﺎﺭﻱﻫﺎ ﺑﻪ ﺗﺮﺗﻴﺐ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﺳﭙﺲ CXRﻭ ﻣﺘﻦ ﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻥ ﺑﻴﻤﺎﺭﻱ ﻭ ﺗﻔﺴﻴﺮ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺏ :ﺍﺑﺘﺪﺍ ﻳﻚ ﻋﻜﺲ ﺭﻳﻪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺳﭙﺲ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺁﻥ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﺝ : Sings, clue :ﻋﻼﺋﻢ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﺗﻌﺮﻳﻒ ﻭ ﺩﺭ CXRﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻣﺎﻧﻨﺪ(…,westermark Sing, Sign) : ﺩ : Anatomy World :ﺁﻧﺎﺗﻮﻣﻲ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﺑﺎ ﻣﻘﺎﻃﻊ ﻃﻮﻟﻲ ﻭ ﻋﺮﺿﻲ ﻭ ﻫﻮﺭﻳﺰﻧﺘﺎﻝ ﺑﻪ ﺻﻮﺭﺕ 3Dﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻫ :ﺩﻳﻜﺸﻨﺮﻱ :ﺗﻌﺎﺭﻳﻒ ﻋﻼﺋﻢ ﻭ ﻧﺸﺎﻧﻪﻫﺎﻱ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻭ :CME Quiz :ﻋﻜﺲ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻲ ﻭ ﺷﺮﺡ ﺣﺎﻝ ﺑﻴﻤﺎﺭ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪ .ﺳﭙﺲ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﻳﺎﻓﺘﻪﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺭﺍ ﻣﺸﺨﺺ ﻧﻤﺎﻳﺪ. ﺑﺨﺶ ﺩﻭﻡ ﻳﺎ :Seminarﺑﻪ ٥ﺑﺨﺶ: -٢ Soft tissue -١ﺍﺳﺘﺨﻮﺍﻧﻬﺎ -٣ﭘﻠﻮﺭﻭﺩﻳﺎﻓﺮﺍﮔﻢ -٤ﺭﻳﻪ ﻭ -٥ﻣﺪﻳﺸﺎﻥ ﺗﻘﺴﻴﻢ ﺷﺪﻩ. ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﺍﺑﺘﺪﺍ ﻋﻜﺴﻲ ﺍﺯ ﺭﻳﻪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺷﺨﺺ ﺑﺎﻳﺪ ﻣﺤﻞ ﺿﺎﻳﻌﻪ ﻭ ﺗﺸﺨﻴﺺ ﺑﻴﻤﺎﺭﻱ ﺭﺍ ﻣﺸﺨﺺ ﺳﺎﺯﺩ .ﺩﺭ ﻣﻮﺭﺩ ﻗﺴﻤﺖ ﺭﻳﻪ ﺧﻮﺩ ﺑﻪ ٤ﺑﺨﺶ Searchﻭ Localizeﻭ describeﻭ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺗﻘﺴﻴﻢ ﺷﺪﻩ ﺍﺳﺖ. : Searchﻋﻜﺲ ﺭﻳﻪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﻣﺤﻞ ﺿﺎﻳﻌﻪ ﺭﺍ ﻧﺸﺎﻥ ﺩﻫﺪ ) ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻮﺱ( :Localizeﺍﺑﺘﺪﺍ ﻋﻼﻣﺖ ﻳﺎ ﻧﺸﺎﻧﻪ ﺑﻴﻤﺎﺭﻱ ﺩﺭ CXRﺷﺮﺡ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﻣﺤﻞ ﺁﻧﺮﺍ ﻧﺸﺎﻥ ﺩﻫﺪ. ﻼ ﺗﻮﺩﻩﺍﻱ ﺩﺭ CXRﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﺑﺘﻮﺍﻧﺪ ﺗﻌﻴﻴﻦ ﻛﻨﺪ ﺧﻮﺵ ﺧﻴﻢ ﺍﺳﺖ ﻳﺎ ﺑﺪ ﺧﻴﻢ. :Describeﺍﺑﺘﺪﺍ CXRﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﺍﺯ ﺑﻴﻦ ٢ﮔﺰﻳﻨﻪ ﻳﻜﻲ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﺪ ﻣﺜ ﹰ CXR :Differential diagnosisﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭﺳﭙﺲ ﺑﻴﻤﺎﺭﻳﻬﺎpattern ،ﻫﺎﻱ ﺑﻴﻤﺎﺭﻱ ﺑﻪ ﺻﻮﺭﺕ ﺗﺴﺖ ﭼﻨﺪ ﺟﻮﺍﺑﻲ ﺁﻭﺭﺩ ﺷﺪﻩ ﺍﺳﺖ. ﺑﺨﺶ ﺳﻮﻡ :Clinicﺍﻳﻦ ﺑﺨﺶ ﺭﺍ ﺑﺮﺍﻱ ﻛﻤﻚ ﺑﻪ ﺗﻘﺴﻴﻢ ﻗﺪﻡ ﺑﻪ ﻗﺪﻡ ﻭ ﻳﺎ ﻧﻮﺷﺘﻦ ﻳﻚ ﺗﻔﺴﻴﺮ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺍﺳﺖ. ﺑﻴﻤﺎﺭ ﺑﻪ ﻫﻤﺮﺍﻩ ﺷﺮﺡ ﺣﺎﻝ ،ﻣﻌﺎﻳﻨﻪ ﻓﻴﺰﻳﻜﻲ ﻭ CXRﻭ ﺩﺭ ﺻﻮﺭﺕ ﻟﺰﻭﻡ CT/MRIﺑﺮﻭﻧﻜﻮﺳﻜﻮﻳﻲ ﻭ ﺑﻴﻮﭘﺴﻲ ﻭ ﻧﻮﻛﺌﺎﺭﺩﺍﺳﻜﻦ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ. ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﺑﺮ ﺍﺳﺎﺱ ﻓﻮﺭﻳﺖ ﺗﻌﻴﻴﻦ ﺷﺪﻩ ﺍﺑﺘﺪﺍ ← Softtissueﺍﺳﺘﺨﻮﺍﻥ ← ﭘﻠﻮﺭﻭﺩﻳﺎﻓﺮﺍﮔﻢ ← ﺭﻳﻪ ← ﻣﺪﻳﺴﺘﺎﻥ ← ﻧﺎﻑ ﺭﻳﻪ ﻋﻜﺲ ﺭﺍ ﻣﻄﺎﻟﻌﻪ ﻧﻤﺎﻳﺪ ﺑﺮﺍﻱ ﻛﻤﻚ ﺑﻪ ﺗﻔﺴﻴﺮ ،ﺧﻮﺩ ﺑﺮﻧﺎﻣﻪ ﺑﺎ ﺗﻌﻴﻴﻦ ﺧﺼﻮﺻﻴﺎﺕ ﻣﻨﻄﻘﻪ ﺑﻪ ﻛـﺎﺭﺑﺮ ﺩﺭ ﺗﻔﺴـﻴﺮ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ﺑﺮﺍﻱ ﻣﺜﺎﻝ :ﺩﺭ ﻣﻮﺭﺩ ...... Softtissueﺑﺎﻓﺖ ﻧﺮﻡ ﺟﺪﺍﺭ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﺍﻓﺰﺍﻳﺶ ،ﻛﺎﻫﺶ ،ﻧﺮﻣﺎﻝ ﻭ ﻛﻠﻴﺴﻔﻴﻜﺎﺳﻴﻮﻥ ﻭ ﺍﺑﻨﺮﻣﺎﻝ airﻭ ....ﻣﻲﺑﺎﺷﺪ. )(Mosby
ــــــ
20.1 Comprehensive Reviw of Radiography
ﺍﻳﻦ CDﺑﻤﻨﻈﻮﺭ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ) (Self evaluationﺍﻓﺮﺍﺩ ﻣﺮﺗﺒﻂ ﺑﺎ ﺣﺮﻓﺔ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺗﺸﺨﻴﺼﻲ ﺩﺭ ﺯﻣﻴﻨﻪﻫﺎﻱ ﺯﻳﺮ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ: ﺗﻬﻴﻪ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﮔﺮﺍﻓﻲﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻛﺎﺭﻛﺮﺩ ﻭ ﻧﮕﻬﺪﺍﺭﻱ ﺍﺯ ﺩﺳﺘﮕﺎﻩﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺣﻔﺎﻇﺖ ﺍﺯ ﺍﺷﻌﻪ ﻧﮕﻬﺪﺍﺭﻱ ﻭ ﻣﺪﻳﺮﻳﺖ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺑﻴﻤﺎﺭﺍﻥ ﺭﻭﺵﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﭘﺲ ﺍﺯ ﻧﺼﺐ CDﻓﻮﻕ ،ﺩﺭ ﺷﺮﻭﻉ ،ﺷﺨﺺ ﺑﺎﻳﺴﺘﻲ ﻳﻜﻲ ﺍﺯ ﻣﺒﺎﺣﺚ ﭘﻨﺞﮔﺎﻧﻪ ﻓﻮﻕ ﺭﺍ ﺟﻬﺖ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﺪ ﻭ ﺑﻪ ﺩﻧﺒﺎﻝ ﺁﻥ ،ﺳﺆﺍﻻﺕ ﻫﺮ ﻣﺒﺤﺚ ﺑﺼﻮﺭﺕ ﭼﻨﺪﮔﺰﻳﻨﻪﺍﻱ ﻣﻮﺭﺩ ﺁﺯﻣﻮﻥ ﻗﺮﺍﺭ ﺧﻮﺍﻫﻨﺪ ﮔﺮﻓﺖ ﻭ ﺑﻪ ﺩﻧﺒﺎﻝ ﻫﺮ ﭘﺎﺳﺦ ،ﺗﻮﺿﻴﺤﺎﺕ ﻋﻠﻤﻲ ﻣﺮﺑﻮﻁ ﺟﻬـﺖ ﺍﺭﺗﻘﺎﺀ ﻋﻠﻤﻲ ﻓﺮﺩ ،ﺑﻪ ﻭﻱ ﺍﺭﺍﺋﻪ ﺧﻮﺍﻫﺪ ﮔﺮﺩﻳﺪ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
4 ــــــ
)21.1 Computed Body Tomography with MRI Correlation (Joseph K. T. Lee, Stuart S. Sagel, Robert J. Stanley, Jay P. Heiken) (3rd Edition) (LIPPINCOTT WILLIAMS & WILKINS
ــــــ 2000
)(Salekan E-Book
)(Matthias Hofer) (Thieme
22.1 CT Teaching Manual
)23.1 Diagnostic Imaging Expert (A CD-ROM Reference & Review) (Ralph Weissleder, Jack Witterberg, Mark J. Rieumont, Genevieve Bennett
ﺍﻳﻦ ﻳﻚ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺷﻲ ﺍﺯ ﻣﻄﺎﻟﺐ ﻣﺨﺘﻠﻒ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﺤﺴﻮﺏ ﻣﻲﺷﻮﺩ ﻭ ﺩﺭ ﺯﻣﻴﻨﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ،ﺑﻪ ﺑﺤﺚ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎ ﻭ ﺭﻭﺵﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ Imagingﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻧﻬﺎ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺍﻳـﻦ CDﺩﺍﺭﺍﻱ ﺁﺭﺍﻳـﻪﻫـﺎﻱ ﺫﻳـﻞ ﻣﻲﺑﺎﺷﺪ: 1- Chest 2- Breast
3- Cardiac 4- Obstetric
5- Gastrointestinal 6- Pediatric
7- Genitourinary 8- Nuclear Imaging
9- Musculoskeletal 10- Contrast agent
11- Neurologic
14- Vascular 13- Head and Neck 12- Imaging Physics
)24.1 DIAGNOSTIC ULTRASOUND A LOGICAL APPROACH (JOHN P. McGAHAN, BARRY B. GOLDBERG
ــــــ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ٣ﻗﺴﻤﺖ ﺍﺳﺖ:
-١ﻛﺘﺎﺏ Diagnostic Ultrasoundﻋﻼﻭﻩ ﺑﺮ ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﻭ ﺟﺰﺀ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮﺩ ﺩﻳﮕﺮ ﺷﺎﻣﻞ ﺩﻭ ﻓﻴﻠﻢ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻭ ﺩﺍﭘﻠﺮ ﻫﺮ ﺑﺨﺶ ﺑﻪ ﺻﻮﺭﺕ ﺯﻧﺪﻩ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. Selp-assessment -٢ﺑﻪ ﺻﻮﺭﺕ CMPﻭ ﺗﺴﺖﻫﺎﻱ ﭼﻨﺪﮔﺰﻳﻨﻪﺍﻱ ﻣﻲﺑﺎﺷﺪ. ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺣﺎﺿﺮ ﺷﺎﻣﻞ ٤١ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺷﺎﻣﻞ: -١ﻓﻴﺰﻳــــﻚ -٢ bioeffectsﺁﺭﺗﻔﻜــــﺖ ٣ﻭ -٤ﺭﻭﺵﻫــــﺎﻱ ﺗﻬــــﺎﺟﻤﻲ ﺑــــﺎ ﺳــــﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺭ )ﺑﻴﻮﭘﺴــــﻲ ،ﺁﺳﭙﻴﺮﺍﺳــــﻴﻮﻥ ﻭ ﺩﺭﻧــــﺎﮊ( ﻭ ﺩﺭ ﺑﻴﻤــــﺎﺭﻱﻫــــﺎﻱ ﺯﻧــــﺎﻥ ﻭ ﺯﺍﻳﻤــــﺎﻥ -٥ﺭﻭﺵﻫــــﺎﻱ ﺍﻭﻟﺘﺮﺍﺳــــﻮﻧﻮﮔﺮﺍﻓﻲ ﺣــــﻴﻦ ﻋﻤــــﻞ ﺟﺮﺍﺣــــﻲ :٦-١٨ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺣﺎﻣﻠﮕﻲ ،ﭘﻼﺳﻨﺘﺎ ﻭ Cervixﻭ ﺑﻨﺪ ﻧﺎﻑ ﻭ ﭘﺮﺩﻩ ﺁﻣﻨﻴﻮﺗﻴﻚ ،ﺳﺮ ﻭ ﺻﻮﺭﺕ ﻭ ﮔﺮﺩﻥ ﻭ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﺷﻜﻢ ﻭ ﻟﮕﻦ ﻭ ﺿﺮﺑﺎﻥ ﻗﻠﺐ ﻭ ﺍﻧﺪﺍﺯﻩﻫﺎﻱ ﺟﻨﻴﻦ ﻭ ﺣﺎﻣﻠﮕﻲ ﺩﻭﻗﻠﻮﺋﻲ ﻭ Small-for-date , large-for-dataﻭ .... ﺩﺭ ﺑﺨﺶﻫﺎﻱ ﺩﻳﮕﺮ ﻫﺮ ﺳﻴﺴﺘﻢ ﺑﺪﻥ ﺍﺯ ﻟﺤﺎﺽ ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ،ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ،ﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﻳﺎﻓﺘﻪﻫﺎ ﺑﻪ ﻧﺮﻣﺎﻝ ﻭ ﻏﻴﺮﻧﺮﻣﺎﻝ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ،ﺗﺸﺨﻴﺺ ﻳﺎﻓﺘﻪ ﻭ ﺭﺳﻴﺪﻥ ﺑﻪ ﻳﻚ ﺗﺸﺨﻴﺺ ﺑﺎﻟﻴﻨﻲ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ -١٩ﺩﺳﺘﮕﺎﻩ ﮔﻮﺍﺭﺵ )ﺣﻔـﺮﻩ ﭘﺮﻳﺘﻮﺍﻥ( -٢٠ﺍﺭﺯﻳﺎﺑﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺍﻋﻀﺎﺀ ﭘﻴﻮﻧﺪ ﺯﺩﻩ ﺷﺪﻩ )ﻛﺒﺪ – ﻛﻠﻴﻪ -ﭘﺎﻧﻜﺮﺍﺱ( -٢١ﻛﺒﺪ -٢٢ﻛﻴﺴﻪ ﺻﻔﺮﺍ ﻭ ﻣﺠـﺎﺭﻱ ﺻـﻔﺮﺍﻭﻱ -٢٣ﺭﺗﺮﻭﭘﺮﺗﻴـﻮﺍﻥ ﻭ ﭘـﺎﻧﻜﺮﺍﺱ ،ﻃﺤـﺎﻝ ،ﻟﻤـﻒ ﻧـﻮﺩ -٢٤ﺩﺳـﺘﮕﺎﻩ ﺍﺩﺭﺍﺭﻱ -٢٥ﭘﺮﻭﺳـﺘﺎﺕ -٢٧ Penis -٢٦ﺍﺳـﻜﺮﻭﺗﻮﻡ ﻭ testes -٣٠ Post meno Pausal Pelvis -٢٩ Female Pelvis -٢٨ﺳﻴﺴــﺘﻢ ﻋــﺮﻭﻕ ﻣﺤﻴﻄــﻲ -٣١ﻛﺎﺭﻭﺗﻴــﺪ -٣٥ Chest -٣٤ Brest -٣٣ trans cranial -٣٢ﺗﻴﺮﻭﺋﻴــﺪ ،ﭘﺎﺭﺍﺗﻴﺮﻭﺋﻴــﺪ ﻭ ﻏــﺪﺩ ﺩﻳﮕــﺮ -٣٦ﺳﻴﺴــﺘﻢ Skeletalﻭ Pediactric Head -٣٧ Softtissue -٤١ ultrasound-Guided Percutaneous tissue Ablation -٤٠ Three dimensional ultrasound -٣٩ Ultrasoud Contrast agent -٣٨ﺍﻭﻟﺘﺮﺍﺳﻮﻧﺪﺍﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﻻﺯﻡ ﺑﻪ ﺫﻛﺮ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻫﻨﮕﺎﻡ ﻧﺼﺐ ﺍﻳﻦ CDﺑﺎﻳﺴﺘﻲ ﺍﺯ ﻛﺪ ﻋﺒﻮﺭ RUSR 2335ﺍﺳﺘﻔﺎﺩﻩ ﺷﻮﺩ. )25.1 Diagnostic Ultrasound of Fetal Anomalies: Principles and Techniques (CD I,II
1999
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺷﻲ ﺩﺍﺭﺍﻱ ٢ﻋﺪﺩ CDﻣﻲﺑﺎﺷﺪ .ﺩﺭ CDﺷﻤﺎﺭﻩ ١ﺑﺎ ﺑﻬﺮﻩﮔﻴﺮﻱ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺛﺎﺑﺖ ﻭ ﻣﺘﺤﺮﻙ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺟﻨﻴﻦ ﻛﻪ ﺩﺍﺭﺍﻱ ﻛﻴﻔﻴﺖ ﻓﻮﻕﺍﻟﻌﺎﺩﻩ ﻋﺎﻟﻲ ﻣﻲﺑﺎﺷﻨﺪ ،ﺁﻧﻮﻣﺎﻟﻲﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻣﺎﺩﺭﺯﺍﺩﻱ ﺑﺼﻮﺭﺕ ﺗﻴﭙﻴﻚ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻳﻚ ،ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ CDﺷﻤﺎﺭﻩ ، ٢ﺍﻣﻜﺎﻥ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﺷﺨﺺ ﺑﻪ ﺻﻮﺭﺕ Caseﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻭ ﺑﻪ ﻃﺮﻳﻘﺔ Multiple Choice questionﻓﺮﺍﻫﻢ ﮔﺮﺩﻳﺪﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ، Caseﺗﻮﺿﻴﺤﺎﺕ ﻻﺯﻡ ﺩﺍﺩﻩ ﺷﺪﻩﺍﻧﺪ .ﻣﺒﺎﺣﺚ ﻭ ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ ٢ﻋﺪﺩ CDﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﻣﻲﺑﺎﺷﻨﺪ: ﻣﺒﺤﺚ ﻣﺒﺤﺚ ﻣﺒﺤﺚ ﻣﺒﺤﺚ ﻣﺒﺤﺚ ﺗﻌﺪﺍﺩ Case ﺗﻌﺪﺍﺩ Case ﺗﻌﺪﺍﺩ Case ﺗﻌﺪﺍﺩ Case ﺗﻌﺪﺍﺩ Case Headﺟﻨﻴﻦ ٣٦ ١٩ ٢ ﺟﻨﺴﻴﺖ ٤ ﺟﻨﻴﻦ ﺍﺳﻜﺘﺎﻝ ﺳﻴﺴﺘﻢ ١٦ Neural tube Amniotic Fluid ٢٠ ٣ ﻣﻮﺍﺭﺩ ﻣﺘﻔﺮﻗﻪ ٢ ﺩﺳﺘﮕﺎﻩ ﺍﺩﺭﺍﺭﻱ ﺟﻨﻴﻦ ١٢ Body wall Umblical Cord ﻗﻠﺐ ﺟﻨﻴﻦ ١٤ ﺻﻮﺭﺕ ﺟﻨﻴﻦ ٦ Chestﺟﻨﻴﻦ ١٢ ﺳﻴﺴﺘﻢ ﮔﻮﺍﺭﺷﻲ ﺟﻨﻴﻦ ٤ ــــــ
)26.1 EBUS (Endo Bronchial Ultrasound
2004
)27.1 Endoscopy and Gastrointestinal Radiology (Gregory G. Ginsberg, Michael L. Kochman Colonoscopy
Upper endoscopy
Percutaneous Management of Biliary Obstruction
Clinical Application of Magnetic Resonance Imaging in the Abdomen
Contrast Radiology
Endoscopiy Endoscopic Ultrasound
Computed Tomography and Ultrasound of the Abdomen and Gastrointestinal Tract
Endoscopic Retrograte Cholagiopancreatography
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
5 28.1 Essentials of Radiology
ــــــ
ﺩﺭ CDﻓﻮﻕ ،ﺿﺮﻭﺭﻳﺎﺕ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺗﺸﺨﻴﺼﻲ ﺑﺼﻮﺭﺕ Caseﻣﻄﺮﺡ ﮔﺮﺩﻳﺪﻩﺍﻧﺪ ﻭ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺗﻴﭙﻴﻚ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﻭ ﺗﻮﺻﻴﻒ ﺩﻗﻴﻖ ﻧﻤﺎﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ CDﺑﺮ ﺣﺴﺐ ﻣﻮﺿﻮﻉ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﺪﺍﺩ Case
ﻣﻮﺿﻮﻉ
ﺗﻌﺪﺍﺩ Case
ﻣﻮﺿﻮﻉ
٢٠ ١٦ ١ ١٣ ٢٨ ١٢
ﻣﺮﺍﻗﺒﺖ ﺑﺤﺮﺍﻧﻲ ﻛﻮﻟﻮﻥ ﻭ ﻧﺎﺣﻴﻪ LLQﺷﻜﻢ ﻣﻄﺎﻟﻌﺎﺕ ﻓﻠﻮﺭﻭﺳﻜﻮﭘﻴﻚ ﺷﻜﻢ ﺳﻴﺴﺘﻢ ﺍﺩﺭﺍﺭﻱ ﺗﻨﺎﺳﻠﻲ ﺳﻴﺴﺘﻢ ﺍﺳﻜﻠﺘﺎﻝ ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻣﻐﺰ
١٥ ٧ ٧ ٧ ٥ ٣
ﻧﺎﺣﻴﻪ RLQﺷﻜﻢ ﺭﻭﺓ ﺑﺎﺭﻳﻚ ﻗﻠﺐ ﮊﻧﻴﻜﻮﻟﻮﮊﻱ ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
TB
ﺗﻌﺪﺍﺩ Case
ﻣﻮﺿﻮﻉ
ﺗﻌﺪﺍﺩ Case
٨ ١٢ ٦ ١٢ ١٧ ١٨
ﺍﻧﺴﺪﺍﺩ ﻭ ﭘﺮﻓﻮﺭﺍﺳﻴﻮﻥ ﻧﺎﺣﻴﻪ RUQﺷﻜﻢ ﻣﻌﺪﻩ
٣٠ ١٢ ٦ ٩ ١٨ ١٦ ١٣
AIDS
ﺗﺮﻭﻣﺎ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ Breast
ﻣﻮﺿﻮﻉ
ﭘﻨﻮﻣﻮﻧﻲ ﻛﺎﻧﺴﺮ ﺭﻳﻪ ﻣﺮﻱ ﭘﻨﻮﻣﻮﻛﻮﻧﻴﻮﺯ ﺍﻃﻔﺎﻝ obstetrics
ﭘﺰﺷﻜﻲ ﻫﺴﺘﻪﺍﻱ
ــــــ
)29.1 Exam Preparation for Diagnostic Ultrasound Abdomen and OB/GYN (RogerC. Sanders, Jann D. Dolk, Nancy Smith Miner
ــــــ
)30.1 Image Data Bank RADIOGRAPHIC ANATOMY & POSITIONING (APPLETON & LANGE
1998
31.1 Imaging Atlas of Human Anatomy
)(Mosby
)(version 2.0
ﺑﺎ ﻛﻤﻚ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻗﺎﺩﺭ ﺧﻮﺍﻫﻴﺪ ﺑﻮﺩ ﻛﻪ ﺩﺭ ﻣﺪﺕ ﺑﺴﻴﺎﺭ ﻛﻮﺗﺎﻫﻲ ﺑﺎ ﺁﻧﺎﺗﻮﻣﻲ ﺑﺪﻥ ﺩﺭ ﺗﺼﺎﻭﻳﺮ ﻣﺨﺘﻠﻒ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ )ﻓﻴﻠﻢﻫﺎﻱ ﺳﺎﺩﻩ ،ﺗﺼﺎﻭﻳﺮ ﺑﺎ ﻛﻨﺘﺮﺍﺳـﺖ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴـﻚ MRI ، CT Scan ،ﻭ ﺳـﻮﻧﻮﮔﺮﺍﻓﻲ( ﺁﺷـﻨﺎ ﺷـﻮﻳﺪ .ﺭﻭﺵ ﻳـﺎﺩﮔﻴﺮﻱ ﺁﻧـﺎﺗﻨﻮﻣﻲ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ CDﺑﺴﻴﺎﺭ ﺁﺳﺎﻥ ﺑﻮﺩﻩ ﻭ ﺍﻣﻜﺎﻧﺎﺕ ﻣﺨﺘﻠﻔﻲ ﺍﺯ ﻗﺒﻴﻞ ﺑﺰﺭﮒﻧﻤﺎﻳﻲ ﺗﺼﻮﻳﺮ negative ،ﻛﺮﺩﻥ ﺗﺼﻮﻳﺮ ،ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﻭ ...ﺟﻬﺖ ﺍﻳﺠﺎﺩ ﻋﻼﻗﻤﻨﺪﺍﻥ ﺑﻴﺸﺘﺮ ﺩﺭ ﺍﻣﺮ ﻳﺎﺩﮔﻴﺮﻱ ﺩﺭ ﻧﻈﺮ ﮔﺮﻓﺘﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺿﻤﻨﹰﺎ ﺑﺎ ﺍﺳـﺘﻔﺎﺩﻩ ﺍﺯ ﺁﺭﺍﻳـﺔ ، noteﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺍﻃﻼﻋﺎﺕ ﻋﻠﻤﻲ ﺍﺿﺎﻓﻲ ﻣﺮﺗﺒﻂ ﺑﺎ ﺗﺼﻮﻳﺮ ﻣﻮﺭﺩ ﻣﻄﺎﻟﻌﻪ ﺩﺳﺘﻴﺎﺑﻲ ﭘﻴﺪﺍ ﻧﻤﻮﺩ. 1998
)32.1 Imaging of Diffuse Lung Disease (David A. Lynch, MB, John D. Newell Jr, MD, FCCP, Jin Seong Lee, MD
CDﺣﺎﺿﺮ ﺷﺎﻣﻞ ١١ﻓﺼﻞ ﺍﺯ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﻨﺘﺸﺮ ﺭﻳﻪ ) (DLNﻣﻲﺑﺎﺷﺪ .ﻛﻪ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﺷﺎﻣﻞ ﺗﻠﻔﻴﻘﻲ ﺍﺯ ﻣﻌﺎﻳﻨﻪ ،ﺷﺮﺡ ﺣﺎﻝ ،ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ ﺗﻔﺴﻴﺮ ﻋﻜﺲﺑﺮﺩﺍﺭﻱ ) MRI,CT-Xrayﻭ (....ﺩﺭ ﺍﻃﻔﺎﻝ ﻭ ﺑﺎﻟﻐﻴﻦ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫـﺎﻱ ﻣﻨﺘﺸـﺮ ﺭﻳﻪ ﻣﻲﺑﺎﺷﺪ. ﺑﻌﻀﻲ ﻓﺼﻮﻝ ﻛﺘﺎﺏ ﺷﺎﻣﻞ : ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ DLDﻛﻮﺩﻛﺎﻥ ﺗﺼﻮﻳﺮ ﺑﺮﺩﺍﺭﻱ ﻋﺮﻭﻕ ﺭﻳﻮﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻧﻔﻴﻠﺘﺮﺍﺗﻴﻮ ﺭﻳﻪ
ﭘﻴﻮﻧﺪ ﺭﻳﻪ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺁﻣﻔﻴﺰﻡ
ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﻐﻠﻲ ﻭ ﻣﺤﻴﻄﻲ ﻭDLD
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺭﺍﻫﻬﺎﻱ ﻫﻮﺍﺋﻲ
ﺍﺭﺯﻳﺎﺑﻲ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺑﻴﻤﺎﺭﻫﺎﻱ ﺭﻳﻪ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ DLDﻭ ﻣﻘﺎﻳﺴﻪ X-Ray,CTﺁﻧﻬﺎ ﺑﻪ ﻃﻮﺭ ﻣﺠﺰﺍ ﻣﻲﺑﺎﺷﺪ
ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ ﺑﺮﻧﺎﻣﻪ Acrobat Readerﺑﻮﺩﻩ ﻭ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﻧﮕﺎﻫﻲ ﺟﺪﻳﺪ ﺑﻪ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎﻱ ﺩﺍﺧﻠﻲ ،ﺭﻳﻪ ،ﻗﻠﺐ ﻭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻣﻲﺩﻫﺪ. ___
)33.1 Imaging of Spinal Trauma in Children (Lawrence R. Kuhns, M.D.) (University of Michigan Medical Center
ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ:
ATLAS OF SPINAL INJURIES IN CHILDREN Cervcal Spine Lumbar Spine Thoracic Spine Sacrococcygeal Spine Lumbar
ــــــ
Special Views and Techniques Experimental and Necropsy Data Sacral Injuries
Principles AND TECHNIQUES Normal Spine Variants and Anatomy Mechanisms and Patterns of Injury Thoracic Spine Injuries
Epidemiology Measurements Occipitocervical Injuries
)34.1 MAGNETIC RESONANCE IMAGING (Third Edition) (Dauld Stark, William Bradley
ﺳﻪ ﺟﻠﺪ ﻛﺘﺎﺏ David Starkﺩﺭ ﺍﻳﻦ CDﻣﻮﺟﻮﺩ ﻣﻴﺒﺎﺷﺪ.
2. Magnetic Resonance: Bioeffects and Safety
1. Generation and Manipulation of Magnetic Resonance Images
4. Principles of Echo Planar Imaging: Implications for Musculoskeletal System
3. Three-Dimensional Magnetic Resonance Rendering Technique
6. The Hip
5. MR Imaging of Articular Cartilage and of Cartilage Degneration
12. The Temporomandibular Joint
9. The Shoulder
8. The Ankle and Foot 13. Kinematic Magnetic Resonance Imaging 14. The Spine
7. The Knee
11. The Wrist and hand
10. The Elbow
15. Marrow Imaging 16. Bone and Soft-Tissue Tumors 17. Magnetic Resonance Imaging of Muscle Injuries
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
6 )35.1 Magnetic Resonance Imaging in Orthopedics and Sport Medicine (David W. Stoller
ــــــ
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻛﺎﺭﺑﺮﺩ MRIﺩﺭ ﺍﺭﺗﻮﭘﺪﻱ ﻭ ﻃﺐ ﻭﺭﺯﺵ ﻣﻲﺑﺎﺷﺪ ﻭ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖ: -١٦ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻥ ﻭ ﺑﺎﻓﺖ ﻧﺮﻡ MRI -١٧ﺁﺳﻴﺒﻬﺎﻱ ﻋﻀﻼﻧﻲ
-١١ﺗﻜﻨﻴﻚ ﺑﺎﺯﺳﺎﺯﻱ ﺟﻬﺖ MRIﺳﻪﺑﻌﺪﻱ -١٢ﻣﻔﺼﻞ ﺭﺍﻥ )(Hip -١٣ﺷﺎﻧﻪ -١٤ﻣﻔﺼﻞ ﻛﻤﭙﻮﺭﻭﻣﺎﻧﺪﻳﺒﻮﻻﺭ )(TMJ -١٥ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ MRIﺍﺯ ﻣﻐﺰ ﺍﺳﺘﺨﻮﺍﻥ
-٦ﺍﺛﺮﺍﺕ ﺑﻴﻮﻟﻮﮊﻳﻚ ﻭ ﺍﻳﻤﻨﻲ ﺩﺭ MRI
-١ﺗﻬﻴﺔ ﺗﺼﺎﻭﻳﺮ MRI
MRI -٧ﻋﻀﺮﻭﻑ ﻣﻔﺼﻠﻲ ﻭ ﺩﮊﻧﺮﺍﺳﻴﻮﻥ ﻋﻀﺮﻭﻓﻲ -٨ﻣﭻ ﭘﺎ ﻭ ﭘﺎ -٩ﻣﭻ ﺩﺳﺖ ﻭ ﺩﺳﺖ -١٠ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
-٢ﺍﺻﻮﻝ ﺗﺼﻮﻳﺮﺳﺎﺯﻱ Echo-Planarﺟﻬﺖ ﺳﻴﺴﺘﻢ ﻣﻮﺳﻜﻮﻟﻮﺍﺳﻜﻠﺘﺎﻝ -٣ﺯﺍﻧﻮ -٤ﺁﺭﻧﺞ Kinematic MRI -٥
2000
)(Ralphl. Smathers, M.D.
ﺩﺭ ﺍﻳﻦ CDﻣﻄﺎﻟﺒﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﺎﻣﻮﮔﺮﺍﻓﻲ ﺑﺎ ﻋﻨﺎﻭﻳﻦ ﺫﻳﻞ ﻣﻄﺮﺡ ﺷﺪﻩ ﺍﺳﺖ: ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ﭘﺴﺘﺎﻥ ﺗﻐﻴﻴﺮﺍﺕ ﺯﻣﺎﻥ ﻭ ﺁﺭﺗﻔﻜﺖﻫﺎ -ﺭﻭﺵﻫﺎﻱ ﺍﻧﺠﺎﻡ ﻣﺎﻣﻮﮔﺮﺍﻓﻲ )ﺑﻪ ﺻﻮﺭﺕ ﻟﻮﻛﺎﻟﻴﺰﻩ ﺑﺎ Needleﻭ ﻳﺎ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ(
ﺗﻐﻴﻴﺮﺍﺕ ﻓﻴﺒﺮﻭﻛﻴﺴﺘﻴﻚ ﻭ ﺗﻮﺩﻩﻫﺎﻳﻲ ﺑﺎ ﺣﺪﻭﺩ ﻣﺸﺨﺺ ﻭ ﺧﻮﺵﺧﻴﻢ -ﺑﺮﺭﺳﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﻴﺸﺮﻓﺘﻪ ﻭ ﻣﺘﺎﺳﺘﺎﺯ ﻭ ﻫﻤﭽﻨﻴﻦ ﺩﺭ ﻣﻮﺭﺩ ﺭﺍﺩﻳﻮﺗﺮﺍﭘﻲ
2001 Aortic Coarcation Miscellaneous
2001 ــــــ
Aortic Arch Anomalies Congenital venous anomalies
Aortic Arch Anomalies Aequised venous diseases
36.1 Mammography Diagnosis and Intervention
-ﺗﻮﺩﻩﻫﺎﻳﻲ ﺑﺎ ﺣﺪﻭﺩ ﻧﺎﻣﺸﺨﺺ ﻭ ﺗﻮﻣﻮﺭﻫﺎﻱ ﺑﺪﺧﻴﻢ ﻭ Aggressive
)37.1 MR Angiography Thoracic Vessels (O. Ratib & D. Didier Methods & Techniques Aortic Aneurysms Aortitis Pulmonary astesies diseases )38.1 MR Imagin Expert (Geir Torhim, Peter A. Rinck
4th Edition "This version is a special adaptation for "Magnetic Resonance in Medicine The Basic Textbook of the European Magnetic Redonance Forum )39.1 MRI of the BRAIN & SPINE (SCOT W. ATLAS) (LIPPINCOTT-ROVEN ﺍﻳﻦ CDﻳﻚ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺷﻲ ﭼﻨﺪﻣﻨﻈﻮﺭﻩ ﺑﻪ ﺣﺴﺎﺏ ﻣﻲﺁﻳﺪ ﺯﻳﺮﺍ ﺩﺭ ﺁﻥ ،ﻋﻼﻭﻩ ﺑﺮ ﺗﻮﺿﻴﺤﺎﺕ ﻻﺯﻡ ﻭ ﺩﺭ ﻋﻴﻦ ﺣﺎﻝ ﻣﺨﺘﺼﺮ ﺩﺭ ﻣﻮﺭﺩ ﻓﻴﺰﻳﻚ ﻭ ﺍﺻﻮﻝ MRIﻭ ﻫﻤﭽﻨﻴﻦ ﺗﻜﻨﻴﻜﻬﺎﻱ ﻣﺮﺑﻮﻃﻪ ،ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻣﺒﺤﺚ ﺑﺎﻟﻴﻨﻲ ﻧﻴﺰ ﺩﺭ ﻃﻲ ٣٢ﻓﺼﻞ ﺑﻪ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻳﺎﻓﺘﻪﻫﺎﻱ Imagingﭘﺮﺩﺍﺧﺘﻪ ﺷﺪﻩ ﻭ ﺑﻴﺶ ﺍﺯ ٤٠٠٠ﺗﺼﻮﻳﺮ MRIﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺑﺮﺣﺴﺐ ﻣﻮﺭﺩ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﺍﺳﺖ .ﺿﻤﻨﹰﺎ ﺑﺮﺍﻱ ﻓﻬﻢ ﺑﻬﺘﺮ ﻣﻄﺎﻟﺐ ،ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻫﺮ ﻣﻮﺿﻮﻉ ﺑﺎﻟﻴﻨﻲ ﻭ ﻳﺎ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺍﺯ ﺟﺪﺍﻭﻝ ﻣﻔﻴﺪ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻗﺴﻤﺖ ﺁﻧﺎﺗﻮﻣﻲ ﻧﻴﺰ ،ﻧﻮﺭﻭﺁﻧﺎﺗﻮﻣﻲ ﺑﻪ ﺻﻮﺭﺕ Sectionalﻭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺳﻪ ﺭﻭﺵ )ﺗﺼﺎﻭﻳﺮ ﺷﻤﺎﺗﻴﻚ +ﺗﺼﺎﻭﻳﺮ ﻃﺒﻴﻌﻲ +ﺗﺼﺎﻭﻳﺮ (MRIﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻧﻜﺘﺔ ﺑﺴﻴﺎﺭ ﺟﺎﻟﺐ ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ،ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﻣﻄﺎﻟﺐ ﻣﻄﺎﻟﻌﻪ ﺷﺪﻩ ﺑﻮﺳﻴﻠﻪ Caseﻫﺎﻱ ﻣﺘﻌﺪﺩ ﺍﺳﺖ ﻛﻪ ﺑﺮﺣﺴﺐ ﻣﻮﺿﻮﻉ ،ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡ ﺷﺪﻩ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡ ﺷﺪﻩ ٥ ٦ ٦ ٦ ٦ ٥ ٣ ٥ ٤ ٥
ﻣﻮﺿﻮﻉ ﺧﻮﻧﺮﻳﺰﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﻳﻨﺎﻝ ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﻛﺴﺘﺮﺍﺁﮔﺰﻳﺎﻝ ﻣﻐﺰ ﺍﻳﺴﻜﻤﻲ ﻭ ﺁﻧﻔﺎﺭﻛﺘﻮﺱ ﻣﻐﺰﻱ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺎﺩﺓ ﺳﻔﻴﺪ ﺗﻈﺎﻫﺮﺍﺕ ﺳﻴﺴﺘﻢ ﺍﻋﺼﺎﺏ ﻣﺮﻛﺰﻱ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻓﺎﻛﻮﻣﺎﺗﻮﺭﻫﺎ ﺳﻼﺗﻮﺭﺳﻴﻜﺎ ﻭ ﻧﺎﺣﻴﻪ ﭘﺎﺭﺍﺳﻼﺭ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻥ ﻛﻤﭙﻮﺭﺍﻝ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﮊﻧﺮﺍﻳﺘﻮ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻋﻔﻮﻧﻲ ﻭ ﺍﻟﺘﻬﺎﺑﻲ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻧﺌﻮﭘﻼﺳﺘﻴﻚ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻭ ﻧﺨﺎﻉ
ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡ ﺷﺪﻩ ٧ ٦ ٦ ٥ ٥ ٤ ٥ ٦ ٣ ٣ ٢
ﻣﻮﺿﻮﻉ ﺍﺧﺘﻼﻻﺕ ﺗﻜﺎﻣﻠﻲ ﻣﻐﺰ ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﺁﮔﺰﻳﺎﻝ ﻣﻐﺰ ﻣﺎﻟﻔﻮﺭﻣﺎﺳﻴﻮﻧﻬﺎﻱ ﻋﺮﻭﻗﻲ ﻭ ﺁﻧﻮﺭﻳﺴﻢﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻳﻨﺎﻝ ﺗﺮﻭﻣﺎﻱ ﺳﺮ ﻋﻔﻮﻧﺖﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻳﻨﺎﻝ Agingﻣﻐﺰ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻧﻮﺭﻭﺩﮊﻧﺮﺍﻳﺘﻮ ﻗﺎﻋﺪﺓ ﺟﻤﺠﻤﻪ ﺍﻭﺭﺑﻴﺖ ﻭ ﺳﻴﺴﺘﻢ ﺑﻴﻨﺎﻳﻲ ﺗﺮﻭﻣﺎﻱ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺁﻧﺎﻣﺎﻟﻴﻬﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻭ ﻧﺨﺎﻉ ﺍﺧﺘﻼﻻﺕ ﻋﺮﻭﻕ ﻧﺨﺎﻋﻲ
ــــــ
40.1 MRI der Extremitaten
2000
)41.1 Normal Findings in CT and MRI (Torsten B Moeller, Emil Reif) (Thieme
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
7 20.3 Obstetric Ultrasound Principles and Techniques
ــــــ
ﺩﺭ ﺍﻳﻦ CDﻣﻄﺎﻟﺐ ﺟﺎﻣﻊ ﻭ ﺍﺭﺯﻧﺪﻩﺍﻱ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﻬﺎﺭﺕﻫﺎﻱ ﻻﺯﻣﻪ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻣﺎﻣﺎﺋﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﻛﻪ ﻋﻨﺎﻭﻳﻦ ﺁﻥ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﻴﻴﻦ ﺳﻦ ﺣﺎﻣﻠﮕﻲ ﺑﺮ ﺍﺳﺎﺱ ﻣﻌﻴﺎﺭﻫﺎﻱ FL . BPDﻭ ACﻭ HCﻭ ﺟﺪﺍﻭﻝ ﺁﻧﻬﺎ ﺑﺮﺭﺳﻲ ﺁﻧﺎﺗﻮﻣﻲ ﺟﻨﻴﻦ ﻭ ﺁﻧﻮﻣﺎﻟﻲﻫﺎﻱ CNSﻭ Body ﺁﻧﺎﺗﻮﻣﻲ ﺭﺣﻢ ﻭ ﺁﺩﻧﻜﺲﻫﺎ ﻭ ﺍﻣﺒﺮﻳﻮ ﻭ ﻛﻴﺴﻪ ﺯﺭﺩﻩ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺑﺮ ﺍﺳﺎﺱ Gsﻭ CRLﻭ ﻧﺤﻮﺓ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻧﻬﺎ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ ﺑﺮ ﺍﺳﺎﺱ ﺩﻭﺭ ﺳﺮ ﻭ ﻧﺤﻮﻩ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻥ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ ﺑﺮ ﺍﺳﺎﺱ FLﻭ ACﻭ ﻧﺤﻮﻩ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻧﻬﺎ ﺗﻌﻴﻴﻦ ﻣﺤﻞ ﺟﻔﺖ ﻭ ﺣﺠﻢ ﻣﺎﻳﻊ ﺁﻣﻨﻴﻮﺗﻴﻚ ﻣﻄﺎﻟﺐ ﺟﺎﻟﺒﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺁﻧﺎﺗﻮﻣﻲ ﺟﻨﻴﻦ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ )ﻣﻌﺪﻩ -ﻛﻠﻴﻪ (........ ﺗﻌﻴﻴﻦ ﻣﺤﻞ ﻻﻧﻪﮔﺰﻳﻨﻲ ﺟﻔﺖ ﻭ ﺑﺮﺭﺳﻲ ﺭﻛﻮﻟﻤﺎﻥ ﻭ ﭘﻼﻧﺘﺎﭘﺮﻭﻳﺎ ﺍﻧﻔﺎﺭﻛﺘﻮﺱ ﻭ ﻭﺍﺭﻳﺎﺳﻴﻮﻥ ﻣﺤﻞ ﺧﺮﻭﺝ ﺑﻨﺪ ﻧﺎﻑ )(Cord Insertion ﺑﺮﺭﺳﻲ ﻟﻜﻴﻨﻴﻜﺎﻝ ﻭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ Case Studyﻭ ﻣﻄﺮﺡﻛﺮﺩﻥ ﺳﺆﺍﻻﺕ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺁﻧﻬﺎ ﻭ ﭘﺎﺳﺦ ﻣﺮﺑﻮﻃﻪ ﺗﻮﺿﻴﺤﺎﺗﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ) BPPﺑﻴﻮﻓﻴﺰﻳﻜﺎﻝ ﭘﺮﻭﻓﺎﻳﻞ(ــــــ
)(DAVID A. STRINGER, PAUL S. BABYN, MDCM
)(Second Edition
42.1 PEDIATRIC GASTROINTESTINAL IMAGING AND INTERVENTION
)43.1 Peripheral Musculoskeletal Ultrasound Interactive Atlas A CD-ROM (J. E. Cabay, B. Daenen) (R. F. Dondelinger
ــــــ
ﺁﻣﻮﺯﺵ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ MusculoSkeletalﻣﺤﺴﻮﺏ ﻧﻤﻮﺩ ﭼﺮﺍ ﻛﻪ ﺑﺎ ﻛﻤﻚ ﺗﺼﺎﻭﻳﺮ ﺛﺎﺑﺖ ﻭ ﻣﺘﺤﺮﻙ ﻣﺘﻌﺪﺩ ﻭ ﺗﻴﭙﻴﻚ ،ﺷﻤﺎ ﺭﺍ ﺑﻪ ﺧﻮﺑﻲ ﺑﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻻﺯﻡ ﺟﻬﺖ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻧﺴﻮﺝ ﻧﺮﻡ ﺳﻄﺤﻲ ﻭ ﺗﺼﺎﻭﻳﺮ ﻧﺮﻣﺎﻝ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱﻫﺎﻱ ﺍﻳﻦ ﺳﻴﺴﺘﻢ ﺁﺷﻨﺎ ﻣﻲﺳﺎﺯﺩ ﻭ ﺿـﻤﻨﹰﺎ ﺍﻣﻜـﺎﻥ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ) (Quizﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻓﺮﺍﻫﻢ ﺍﺳﺖ .ﺩﺭ ﻣﻨﻮﻱ ﺍﻳﻦ CDﺷﻤﺎ ﺑﺮﺍﻱ ﺑﺮﺭﺳﻲ ﺗﺼﺎﻭﻳﺮ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﻧﺮﻣﺎﻝ ﻭ ﻳﺎ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﺩﺭ ﺳﻴﺴﺘﻢ ﻣﻮﺳﻜﻮﻟﻮ ﺍﺳﻜﻠﺘﺎﻝ ﺍﺯ ﺩﻭ ﺷﻴﻮﺓ ﻣﺨﺘﻠﻒ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺑﻬﺮﻩﻣﻨﺪ ﺷﻮﻳﺪ: ﺍﻟﻒ -ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻨﻮﻱ :Generalﻛﻪ ﺩﺭ ﺍﻳﻦ ﺻﻮﺭﺕ ﺷﻤﺎ ﻳﻜﻲ ﺍﺯ itemﻫﺎﻱ ﺯﻳﺮ ﺭﺍ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﺋﻴﺪ: -١٠ﭘﻮﺳﺖ
-٩ﻋﺼﺐ
-٨ﻋﺮﻭﻕ
-٧ﻏﻀﺮﻭﻑ ﻓﻴﺒﺮﻭ
-٦ﻏﻀﺮﻭﻑ ﻫﻴﺎﻟﻴﻦ
-٥ﻛﭙﺴﻮﻝ ﻣﻔﺼﻠﻲ ﻭ ﺑﻮﺭﺱ
-٣ﻟﻴﮕﺎﻣﺎﻥ
-٤ﺍﺳﺘﺨﻮﺍﻥ ﻭ ﭘﺮﻳﻮﺳﺖ
-٢ﺗﺎﻧﺪﻭﻥ
-١ﻋﻀﻠﻪ
ﺏ -ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻨﻮﻱ :Regionﻛﻪ ﺩﺭ ﺍﻳﻦ ﺻﻮﺭﺕ ﺷﻤﺎ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻳﻜﻲ ﺍﺯ itemﻫﺎﻱ ﺯﻳﺮ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﺋﻴﺪ: 1- Ankle
2- Elbow
3- Foot
4- Hand
5- Hip
6- Knee
7- Shoulder
ــــــ 2002 ــــــ
8- Wrist
44.1 Principles of MRI
)(Jeery Papp) (Mosby )(UNIVERSITY OF FLORIDA COLLEGE OF MEDICINE DEPARTMENT OF RADIOLOGY
45.1 Quality Management in the Imaging sciences
Interactive Tutorial on Normal Radiology
46.1 RADIOLOGIC ANATOMY
ﻼ ﺍﮔﺮ ﻣﻲﺧﻮﺍﻫﻴﻢ ﺩﺭ ﻣﻮﺭﺩ (Lower Extremityﺍﻃﻼﻋﺎﺕ ﺁﻧﺎﺗﻮﻣﻴﻚ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺑﺪﺳﺖ ﺁﻭﺭﻳﻢ ﺑﺮ ﺭﻭﻱ ﺍﻧـﺪﺍﻡ ﺗﺤﺘـﺎﻧﻲ ﺷـﻜﻞ ﻣـﺬﻛﻮﺭ ﺑﺮﺍﻱ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ، CDﺍﺑﺘﺪﺍ ﺑﺎﻳﺪ ﺑﺮ ﺭﻭﻱ ﻗﺴﻤﺖ ﻣﻮﺭﺩ ﻧﻈﺮ ﺑﺮ ﺭﻭﻱ ﺷﻜﻞ ﺍﻧﺴﺎﻥ )ﺩﺭ ﻛﺎﺩﺭ ﺳﻤﺖ ﺭﺍﺳﺖ( Clickﺷﻮﺩ )ﻣﺜ ﹰ Clickﻣﻲﻛﻨﻴﻢ( ،ﺳﭙﺲ ﺩﺭ ﻛﺎﺩﺭ ﺳﻤﺖ ﭼﭗ ﻟﻴﺴﺖ ﻗﺴﻤﺖﻫﺎﻱ ﻛﻠﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﻧﺎﺣﻴﻪ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻣﻮﺭﺩ ﻣﻄﺎﻟﻌﻪ ﻇﺎﻫﺮ ﻣﻲﺷﻮﺩ ﻭ ﻣﺎ ﻣﻲﺗﻮﺍﻧﻴﻢ ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﻗﺴﻤﺖﻫﺎﻱ ﻛﻠﻲ ،ﻭﺍﺭﺩ ﺟﺰﺋﻴﺎﺕ ﺑﻴﺸﺘﺮ ﺁﻥ ﺷﻮﻳﻢ .ﺿﻤﻨﹰﺎ ﺩﺭ ﻗﺴﻤﺖ ﭘﺎﻳﻴﻦ ﻛﺎﺩﺭﻫـﺎﻱ ﻓـﻮﻕ ،ﺳـﻪ ﻋـﺪﺩ Iconﻛﺎﺭﺑﺮﺩﻱ ﺩﺭ ﻗﺴﻤﺖ ﻭﺳﻂ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﺑﺎ ﻛﻤﻚ ﺁﻧﻬﺎ ﻣﻲﺗﻮﺍﻥ ﺑﺘﺮﺗﻴﺐ ﺍﺯ ﺗﻜﻨﻴﻚ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﻗﺴﻤﺖ ﻣﻮﺭﺩ ﻧﻈﺮ ،ﺁﻧﺎﺗﻮﻣﻲ ﻃﺒﻴﻌﻲ ﻗﺴﻤﺖ ﻣﺬﻛﻮﺭ ﻭ ﻫﻤﭽﻨﻴﻦ ﻣﺴﺎﺋﻞ ﻛﻠﻴﻨﻴﻜﻲ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﻋﻀـﻮ ﻣـﻮﺭﺩ ﻣﻄﺎﻟﻌـﻪ ﺁﮔـﺎﻫﻲ ﻛﺎﻣـﻞ ﻳﺎﻓـﺖ .ﺿـﻤﻨﹰﺎ ﺍﻣﻜـﺎﻥ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ) (Self evaluationﺑﺮ ﺍﺳﺎﺱ ﻣﺒﺎﺣﺚ ﻣﻮﺭﺩ ﻧﻈﺮ ﻭﺟﻮﺩ ﺩﺍﺭﺩ .ﻧﻜﺘﺔ ﻗﺎﺑﻞ ﺗﻮﺟﻪ ﺩﺭ ﺍﻳﻦ ، CDﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻛﻠﻴﺔ ﺭﻭﺵﻫﺎﻱ ) Imagingﺍﺯ ﻗﺒﻴﻞ ، Plain Filmﻣﻄﺎﻟﻌﺎﺕ ﺑﺎ ﻣﻮﺍﺩ ﺣﺎﺟﺐ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴـﻚ MRI ، CTScan ،ﻭ (...ﺑـﺮﺍﻱ ﻧﺸـﺎﻥﺩﺍﺩﻥ ﺗﻜﻨﻴـﻚﻫـﺎﻱ ﻣﺨﺘﻠﻒ ﻣﺮﺑﻮﻁ ﺑﻪ Imagingﻫﺮ ﻋﻀﻮ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ( ﻃﺮﻳﻘﺔ ﻧﺼﺐ : hCDﺑﻌﺪ ﺍﺯ ﻗﺮﺍﺭﺩﺍﺩﻥ CDﺩﺭ CD-ROMﺩﺳﺘﮕﺎﻫﺘﺎﻥ ﺻﻔﺤﺔ Autoplay menuﺭﺍ ﺑﺒﻨﺪﻳﺪ ﺳﭙﺲ ﺑﻪ my computerﺭﻓﺘﻪ ﻭ ﺭﻭﻱ ﺩﺭﺍﻳﻮ CD-ROMﺩﺳﺘﮕﺎﻩ ﺧﻮﺩ ﺭﺍﺳـﺖﻛﻠﻴـﻚ ﻛﻨﻴـﺪ ﻭ ﮔﺰﻳﻨـﺔ Openﺭﺍ ﺍﻧﺨـﺎﺏ ﻛﻨﻴـﺪ ﺳﭙﺲ ﺭﻭﻱ * ، Setupﺩﺍﺑﻞ ﻛﻠﻴﻚ ﻛﻨﻴﺪ ﺻﻔﺤﻪﺍﻱ ﺑﺎ ﻧﺎﻡ radiologic Anatomy installationﻇﺎﻫﺮ ﻣﻲﺷﻮﺩ ﻣﺴﻴﺮ ﻧﺼﺐ ﺭﺍ ﻭﺍﺭﺩ ﻛﺮﺩﻩ ﻭ ﻳﺎ ﭘﻴﺶﻓﺮﺽ ﺭﺍ ﺑﺎ ﻛﻠﻴﻚ ﺑﺮ ﺭﻭﻱ OKﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ .ﺑﻌﺪ ﺍﺯ ﻧﺼﺐ ﭘﻴﻐـﺎﻣﻲ ﻣﺒﻨـﻲ ﺑـﺮ ﻧﺼـﺐ ﻛﺎﻣـﻞ CD ﻣﻲﺁﻳﺪ ﻛﻪ ﺁﻥ ﺭﺍ OKﻛﻨﻴﺪ ،ﺳﭙﺲ ﺍﺯ ﻣﻨﻮﻱ Startﺑﻪ Programﺭﻓﺘﻪ ﻭ ﺩﺭ radilogic Anatomyﻋﻨﻮﺍﻥ ﻣﺮﺑﻮﻃﻪ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ. * iconﻫﺎﻱ ﺩﻳﮕﺮﻱ ﺑﺎ ﻋﻨﺎﻭﻳﻦ ) (ssetup.apm ، setup.cfg ، ssetup ، Setup.ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﻣﺮﺑﻮﻁ ﺑﻪ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻧﻴﺴﺖ ﻟﻄﻔﹰﺎ ﻓﻘﻂ setup.exeﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ. )(International Medical Multimedia
ــــــ
47.1 Radiology Image Bank: Orthopedic Radiology
)48.1 Radiology on CD-ROM Diagnosis, Imaging, Intervention (Juan M. Taveras, MD, Joseph T. Ferrucci, MD
ــــــ ﺍﻳﻦ ، CDﻣﺠﻤﻮﻋﻪ ﻛﺎﻣﻠﻲ ﺍﺯ ﻛﺘﺎﺏ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Tavers
)ﻛﻪ ﻳﻜﻲ ﺍﺯ ﻣﻌﺘﺒﺮﺗﺮﻳﻦ ﻭ ﻛﺎﻣﻞﺗﺮﻳﻦ ﻣﺮﺍﺟﻊ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺭ ﺟﻬﺎﻥ ﻣﻲﺑﺎﺷﺪ( ﻫﻤﺮﺍﻩ ﺑﺎ ﺁﺧﺮﻳﻦ ﺗﻐﻴﻴﺮﺍﺕ ﺩﺍﺩﻩﺷﺪﻩ ﺗﺎ ﺳﺎﻝ 2001ﻣﻴﻼﺩﻱ ﺑﻮﺩﻩ ﻭ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﻋﻤﺪﺓ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: -٤ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Gastrointestinal
-٣ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Vascular
-٨ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Cardiac
Breast Imaging -٧ -١١ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Skeletal
2002 ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
-٢ﺳﻴﺎﺳﺖ ﺑﻬﺪﺍﺷﺘﻲ ﻭ ﻣﺪﻳﺮﻳﺖ ﺩﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ -٦ﻓﻴﺰﻳﻚ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ -١٠ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Adbomen
-١ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Pulmonary -٥ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Genitourinary
-٩ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺳﺮ ﻭ ﮔﺮﺩﻥ
)49.1 REVIEW FOR THE Radiography Examination (A & LERT) (McGrow-Hill's
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
8 50.1 Teaching Atlas of Mammography (Laszlo Tabar, Peter B. Dean) 51.1 The Basics of MRI of NMR
(Thieme)
ــــــ
(Joseph P. Hornak, Ph.D.)
ــــــ
52.1 The Encyclopaedia of Medical Imaging from NICER
ــــــ
53.1 THE MRI TEACHING FILE (Robert B. Lufkin, William G. Bradley, Jr., Michael Brant-Zawadzki)
2001
ﺗﻌـﺪﺍﺩ. ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﺷﺮﺡ ﺣﺎﻝ ﻭ ﻳﺎﻓﺘﻪﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺩﺍﺭﺍﻱ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻭ ﺗﺸﺨﻴﺺ ﻧﻬﺎﻳﻲ ﺑﻮﺩﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﺗﺸﺨﻴﺺ ﻧﻜﺎﺕ ﻣﻬﻢ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳـﺖCase ﻣﻲﺑﺎﺷﺪ ﻭ ﻫﺮMRI ﻫﺎﻱ ﻣﺘﻌﺪﺩ ﻣﺮﺑﻮﻁ ﺑﻪ ﻣﺒﺎﺣﺚ ﻣﺨﺘﻠﻒ ﺩﺭ ﺯﻣﻴﻨﺔCase ﻓﻮﻕ ﺩﺍﺭﺍﻱCD : ﺑﺼﻮﺭﺕ ﺟﺪﻭﻝ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪCD ﻫﺎﻱ ﻣﻄﺮﺡﺷﺪﻩ ﺑﺮ ﺣﺴﺐ ﻫﺮ ﻣﻮﺿﻮﻉ ﺩﺭ ﺍﻳﻦCase ﻣﻮﺿﻮﻉ
Case ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case ﺗﻌﺪﺍﺩ
ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻏﻴﺮﻧﺌﻮﭘﻼﺳﺘﻴﻚ ﻣﻐﺰ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺍﻃﻔﺎﻝ
٢٠١ ١٠٠ ١٠٠
ﻧﺌﻮﭘﻼﺳﻢﻫﺎﻱ ﻣﻐﺰﻱ ﺳﻴﺴﺘﻢ ﻋﻀﻼﻧﻲ ﺍﺳﻜﻠﺘﻲ ﺍﺻﻮﻝ ﻭ ﺁﺭﺗﻴﻔﻜﺖﻫﺎ
١٠٢ ١٠٠ ١٠٠
ﻣﻐﺰMRA ﺗﻨﻪ
١٠ ١٠٢
ﺳﺮ ﻭ ﮔﺮﺩﻥ ﺳﻴﺴﺘﻢ ﻗﻠﺒﻲﻋﺮﻭﻗﻲ
١٠٠ ١٠٤
54.1 THE RADIOLOGIC CLINICS OF NORTH AMERICA High-Resolution CT of the Lung II (DAVID A. LYNCH, MD)
(NUMBER 1 VOLUME 40)
ــــــ
: ﺭﻳﻪ ﺍﺳﺖHRCT ﻣﻲﺑﺎﺷﺪ ﻭ ﺩﺍﺭﺍﻱ ﻣﺒﺎﺣﺚ ﻋﻤﺪﺓ ﺫﻳﻞ ﺩﺭﺧﺼﻮﺹThe Radiologic clinics of North America ﺑﺮﮔﺮﺩﺍﻥ ﺷﻤﺎﺭﻩ ﺍﻭﻝ ﺟﻠﺪ ﭼﻬﻠﻢ ﺍﺯ ﻣﺠﻤﻮﻋﺔ ﻛﺘﺎﺑﻬﺎﻱCD ﺍﻳﻦ ﻭ ﺑﺮﻭﻧﺸﻜﺘﺎﺯﻱAir Way ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱCT Scan ﺩﺭ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺷﻐﻠﻲ ﻭ ﻣﺤﻴﻄﻲ ﺭﻳﻪHRCT ﻧﻘﺶ( ﺭﻳﻪquantitative) ﻛﻤﻴﺘﻲCT -
Peripheral Airways ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱHRCT Drug-Induced ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺭﻳﻮﻱHRCT -
ﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻣﻔﻴﺰﻡCT Scan Non-TB ﻭTB ﻣﺮﺑﻮﻁ ﺑﻪ ﻋﻔﻮﻧﺘﻬﺎﻱ ﻣﺎﻳﻜﻮﺑﺎﻛﺘﺮﻳﺎﻳﻲCT Scan -
ﺩﺭ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺭﻳﻮﻱ ﺍﻃﻔﺎﻝHRCT ﻧﻘﺶ ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺗﺮﻭﻣﺒﻮﺁﻣﺒﻮﻟﻴﻚ ﺭﻳﻮﻱCT Scan -
ﻧﺪﻭﻝ ﻣﻨﻔﺮﺩ ﺭﻳﻮﻱ-
55.1 THE RADIOLOGIC CLINICS OF NORTH AMERICA Imaging of Musculoskeletal and Spinal Infections • PRINCIPLES AND TECHNIQUES 1. Epidemiology 3. Normal Spine Variants and Anatomy 2. Thoracic Spine Injuries 4. Experimental and Necropsy Data • ATLAS OF SPINE INJURIES IN CHILDREN 1. Cervcal Spine 2. Thoracic Spine 3. Lumbar Spine
56.1 THE RADIOLOGIC CLINICS OF NORTH AMERICA
5. Measurements 6. Special Views and Techniwques
1999 7. Sacral Injuries 8. Occipitocervical Injuries
9- Mechanisms and Patterns of Injury
4. Sacrococcygeal Spine
Pediatric Musuloskeletal Pediatric Radiology
(SALEKAN E-BOOK)
(James S. Meyer, MD)
2001
: ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﺷﺎﻣﻞ ﺍﻳﻦ ﻣﺒﺎﺣﺚ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ y Ultrasound in Padiatric Musculoskeletal Disease: Teachinques and Applications y Nuclear Medicnine Topics in Pediatric Musculoskeletal Disease: Teachinques and Applications y Imaging of Musculoskeletal Infections y Malignant and Benign Bone Tumors y Magnetic Rsonance Imaging of Musculoskeletal Soft Tissue Mass y Imaging of Pediatric Hip Disorder y Imaging of Pediatric Foot Disorder in Children y Imaging of Sports Injuries in Children and Adolescents y A Pragmatic Approach to the Radiologic Diagnosis of Pediatric Syndromes and Skeletal Dysplasias y The Orthopedists Perspective: Bone Tumors, Scoliosis, and Trauma y Imaging of Crowth Distubance in Children y Imaging of Child Abuse
57.1 THE RADIOLOGIC CLINICS OF NORTH AMERICA Update on Nuclear Medicine 58.1
ــــــ
THE RADIOLOGIC CLINICS OF NORTH AMERICA Update on Ultrasonography (FAYE C. LAING, MD) (W.B. SAUNDERS COMPABY)
ــــــ
: ﻣﻲﺑﺎﺷﺪ ﻭ ﺩﺍﺭﺍﻱ ﻣﺒﺎﺣﺚ ﻋﻤﺪﺓ ﺫﻳﻞ ﺩﺭ ﺧﺼﻮﺹ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺍﺳﺖThe Radiologic Clinics Of North America ﺍﺯ ﻣﺠﻤﻮﻋﻪ ﻛﺘﺎﺏﻫﺎﻱ٣٩ ﺑﺮﮔﺮﺩﺍﻥ ﺷﻤﺎﺭﻩ ﺳﻮﻡ ﺟﻠﺪCD ﺍﻳﻦ ﺗﻜﻨﻮﻟﻮﮊﻱ ﺭﻭﺯ-١ ﻣﻮﺍﺩ ﺣﺎﺟﺐ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﺪ-٢ ( ﺗﺤﺖ ﺭﺍﻫﻨﻤﺎﻳﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻲintervention) ﺍﻗﺪﺍﻣﺎﺕ ﻣﺪﺍﺧﻠﻪﺍﻱ-٣ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺭ ﺣﻴﻦ ﻋﻤﻞ ﺟﺮﺍﺣﻲ-٤ ﻭﺿﻌﻴﺖ ﻓﻌﻠﻲ ﺗﺸﺨﻴﺼﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺍﻧﺪﻭﺳﻜﻮﭘﻴﻚ-٥ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻣﻮﺳﻜﻮﻟﻮﺍﺳﻜﻠﺘﺎﻝ-٦ Breast ﺳﻮﻧﻮﮔﺮﺍﻓﻲ-٧ Gynecology ﻭObstetric ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺳﻪﺑﻌﺪﻱ ﺩﺭ-٨ Gynecologic ﺳﻮﻧﻮﮔﺮﺍﻓﻲ-٩ ﺍﺭﺯﻳﺎﺑﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﺍﺗﺴﺎﻉ ﺑﻄﻦﻫﺎﻱ ﺩﺍﺧﻞ ﻣﻐﺰﻱ ﺑﻪ ﺩﻧﺒﺎﻝ ﺧﻮﻧﺮﻳﺰﻱ-١٠ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻣﺤﻴﻄﻲ-١١ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻛﺎﺭﻭﺗﻴﺪ-١٢ 59.1
Ultrasound Atlas of Vascular Diseases
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(Carol A. Krebs, RT, RDMS, Vishan L. Giyanani, , Ronald L. Eisenberg) (APPLETON & LANGE Stamford, Connecticut) (SALEKAN E-Book)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
9
ــــــ ــــــ ــــــ
)Ultrasound Teaching Manual The basics of Performing and Interpreting Ultrasound Scans (Matthias Hofer) (With the collaboration of Tatjana Reihs) (Thieme )61.1 Uterosalpingography in Gynecology Hysterospingography (Salekan E-Book 62.1 VOXEL-MAN 3D-Navigator Brain and Skull (Regional, Functional, and Radiological Anatomy) (IMDM university Hospital Eppendorf, )Humburg )(Springer ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﺭ ﻗﺎﻟﺐ ﻳﻚ ﺍﻃﻠﺲ ﺳﻪﺑﻌﺪﻱ Interactiveﺍﺯ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺩﺍﺧﻠﻲ ﺗﻨﻪ ﺩﺭ ﺳﻪ ﻋﺪﺩ CDﺟﻬﺖ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻜﻲ ،ﻃﺮﺍﺣﻲ ﺷﻴﻮﺓ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﻭ ﺁﻣﻮﺯﺵ ﺩﺭﻭﺱ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳـﺖ .ﻓﺼـﻮﻝ ﻣﺨﺘﻠـﻒ ﺍﻳﻦ CDﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﺍﺳﺖ: ﺑﺨﺶ ﺍﻭﻝ( ﺁﻧﺎﺗﻮﻣﻲ :١-١ :ﺗﺸﺮﻳﺢ ﺳﻪﺑﻌﺪﻱ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺩﺍﺧﻞ ﺗﻨﻪ :ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺁﻧﺎﺗﻮﻣﻲ ﺳﻪﺑﻌﺪﻱ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﺑﺎ ﻗﺎﺑﻠﻴﺖ ﭼﺮﺧﺶ Ventricolﻭ ﭼﺮﺧﺶ horizontalﻭ ﺁﻧﺎﺗﻮﻣﻲ ﺷﻜﻢ ﺑﺎ ﻗﺎﺑﻠﻴﺖ ﭼﺮﺧﺶ ﺍﻓﻘﻲ ﻭ ﻋﻤﻮﺩﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ : ٢-١ﺗﺸﺮﻳﺢ ﺩﺳﺘﮕﺎﻩﻫﺎ ﻛﻪ ﺩﺭ ٩ﺑﺨﺶ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ )ﺍﺳﻜﻠﺖ ﺍﺳﺘﺨﻮﺍﻧﻲ ،ﺳﻴﺴﺘﻢ ﻗﻠﺒﻲ ﻋﺮﻭﻗﻲ ،ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ،ﻛﺒـﺪ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﻗﺎﺑﻠﻴﺖ ﺣﺬﻑ ﻭ ﺍﺿﺎﻓﻪﻧﻤﻮﺩﻥ ﻫﺮ ﻳﻚ ﺍﺯ ﺑﺨﺶﻫﺎﻱ ﺗﺼﺎﻭﻳﺮ ﻭ ﭼﺮﺧﺶ ١٨٠oﺁﻧﻬﺎ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. : ٣-١ﺁﻧﺎﺗﻮﻣﻲ ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ :ﺷﺎﻣﻞ ٢ﻗﺴﻤﺖ ﺁﻧﺎﺗﻮﻣﻲ ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ ﺳﻄﻮﺡ Coronalﻭ Sagittalﻣﻲﺑﺎﺷﺪ. ﻭ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺟﺎﻧﺒﻲ ،ﺷﺒﻴﻪﺳﺎﺯﻱ ﮔﺎﺳﺘﺮﻭﺳﻜﻮﭘﻲ ﺑﺎ ﻗﺎﺑﻠﻴﺖ ﺣﺮﻛﺖ ﺩﺭ ﻓﻀﺎﻱ ﻣﺮﻱ ﻭ ﻣﻌﺪﻩ( 60.1
ﺗﻮﻣﻮﮔﺮﺍﻓﻲﺑﺨﺶ ﺩﻭﻡ( ﺭﺍﺩﻳﻮﻟﻮﮊﻱ: -١-١ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ CT -٢-١ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ )ﺑﺎ ﻗﺎﺑﻠﻴﺖ ﺣﺮﻛﺖﺩﺍﺩﻥ ﺳﻄﺢ ﻣﻘﻄﻊ ﻭ ﻣﺸﺎﻫﺪﻩ ﺗﺼﻮﻳﺮ ﻫﺮ ﻗﺴﻤﺖ( -٤-١ﺷﺒﻴﻪﺳﺎﺯﻱ ﻗﺴﻤﺖ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻴﻚ ﻛﺒﺪ -٣-١ﻣﻘﺎﻳﺴﻪ ﺑﻴﻦ ﺗﺼﺎﻭﻳﺮ CTﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺳﻪﺑﻌﺪﻱ ﻭ ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ -ﺗﺼﺎﻭﻳﺮ X-ray
ــــــ ــــــ
-٤-٢ﺗﺼﺎﻭﻳﺮ X-rayﺍﺯ ﻛﻠﻴﺔ ﺍﻧﺪﺍﻡﻫﺎ -٣-٢ﺗﺼﺎﻭﻳﺮ X-rayﺍﺯ ﺍﻧﺪﺍﻡﻫﺎﻱ ﻣﻨﻔﺮﺩ -٢-٢ﺗﺼﺎﻭﻳﺮ X-rayﺍﺯ ﺷﻜﻢ -١-٢ﺗﺼﺎﻭﻳﺮ X-rayﺍﺯ ﻗﻔﺴﺔ ﺳﻴﻨﻪ ﻣﺎﺭﻙﺩﺍﺭﻧﻤﻮﺩﻥ ﻫﺮ ﺑﺨﺶ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﻭ ﻣﻘﺎﻃﻊ ﺗﺸﺮﻳﺤﻲ ﻗﺪﺭﺕ ﺍﻓﺰﺍﻳﺶ Zoomﺗﺼﺎﻭﻳﺮ ﺍﺭﺍﺋﻪ ﺗﺼﺎﻭﻳﺮ ﺑﺎﺯﺳﺎﺯﻱﺷﺪﻩ ﻛﺎﻣ ﹰ ﻼ ﻭﺍﻗﻌﻲ ﻛﻪ ﺍﺭﺍﺋﻪ ﻓﻬﺮﺳﺖ ﻛﺎﻣﻞ ﻣﻨﺪﺭﺟﺎﺕ ﺗﺼﺎﻭﻳﺮ ﺑـﻪ ﺳـﻪ ﺯﺑـﺎﻥ ﺍﻧﮕﻠﻴﺴـﻲ ،ﺁﻟﻤـﺎﻧﻲ ﻭ ﻧﺎﻣﮕــﺬﺍﺭﻱ ﺑﺨــﺶﻫــﺎﻱ ﻣﺨﺘﻠــﻒ ﺗﺼــﺎﺋﻴﺮ ﺑﺼــﻮﺭﺕ ﻛﺎﺭﺑﺮﺩ ﺁﻣﻮﺯﺷﻲ ﺟﺬﺍﺑﻲ ﺭﺍ ﺑﻪ ﻫﻤﺮﺍﻩ ﺩﺍﺭﺩ. ﻻﺗﻴﻦ Intractive
)VOXEL-MAN 3D-Navigator Inner Organs (Regional, Systemic and Radiological Anatomy) (IMDM university Hospital Eppendorf, Hamburg )64.1 Whole Body Computed Tomography (Second Edition) (Otto H. Wegener) (Blackwell Science ﺩﺭ ﺍﻳﻦ CDﺩﺭ ﻃﻲ ٢٨ﻓﺼﻞ ﺑﻪ ﺷﺮﺡ ﺁﻧﺎﺗﻮﻣﻲ ،ﺗﻜﻨﻴﻚ ﻭ ﻓﻴﺰﻳﻚ ﻣﺮﺑﻮﻁ ﺑﻪ CT Scanﻫﻤﺮﺍﻩ ﺑﺎ ﺑﺮﺭﺳﻲ ﺟﺰﺀ ﺑﻪ ﺟﺰﺀ ﻣﺴﺎﺋﻞ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﻧﻮﺍﺣﻲ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﮔﻮﻳﺎﻱ CT Scanﭘﺮﺩﺍﺧﺘﻪ ﺷﺪﻩ ﺍﺳـﺖ .ﻓﻬﺮﺳـﺖ ﻛﻠـﻲ ﻓﺼﻮﻝ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻜﻨﻴﻜﻬﺎﻱ CT Scan ﻣﻮﺍﺩ ﺣﺎﺟﺐ ﺗﺤﻠﻴﻞ ﺗﺼﻮﻳﺮ ﺩﺭ CT Scanﺁﻧﺎﺗﻮﻣﻲ ﺩﺭ CT Scan ﻛﻠﻴﻪ ﺍﺭﮔﺎﻧﻬﺎﻱ ﺗﻨﺎﺳﻠﻲ ﺯﻥ ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻧﻲ ﻣﺪﻳﺎﺳﺘﻦ ﺭﻭﺵ ﻭ ﺍﺳﺘﺮﺍﺗﮋﻱ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭ ﻗﻠﺐ ﺭﻳﻪﻫﺎ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺣﻔﺮﺓ ﺭﺗﺮﻭﭘﺮﻳﺘﻮﺋﻦ ﻏﺪﺩ ﻓﻮﻕ ﻛﻠﻴﻮﻱ ﺟﻨﺐ )ﭘﻠﻮﺭ( ﺩﻳﻮﺍﺭﺓ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﻛﺒﺪ ﻟﮕﻦ ﺍﺳﺘﺨﻮﺍﻧﻲ ﺳﻴﺴﺘﻢ ﺻﻔﺮﺍﻭﻱ ﻋﻀﻼﺕ ﻣﺜﺎﻧﻪ ﺗﺮﻣﻴﻨﻮﻟﻮﮊﻱ CT ﭘﺎﻧﻜﺮﺍﺱ ﺩﺳﺘﮕﺎﻩ ﮔﻮﺍﺭﺵ ﺣﻔﺮﺓ ﭘﺮﻳﺘﻮﺋﻦ ﻃﺤﺎﻝ ﭘﺮﻭﺳﺘﺎﺕ ﻭ ﺳﻤﻴﻨﺎﻝ ﻭﺯﻳﻜﻮﻝﻫﺎ ﺗﻮﻣﻮﺭﻫﺎﻱ ﻧﺴﺞ ﻧﺮﻡ 63.1
-٢ﮔﻮﺵ ،ﺣﻠﻖ ﻭ ﺑﻴﻨﻲ
ﻋﻨﻮﺍﻥ CD )Advanced Rhinoplasty Techniques Cosmetic Rhinoplasty (Rollin K. Daniel, M.D. Analysis, Marking & Anesthesia, Closed/Open Approach, Septum Exposure, Exposure & Dorsal Reduction,
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــــ
1.2
& Caudal Septum Resection, Ideal Profile Line, Open Approach, Tip Analysis, Septoplasty Septal Harvest, Grafts, Spreaser Grafts, Grural Strut, Tip Suture Technique, Closure, Nostril Sill Alar Wedge, Composite Graft, Lateral Osteotomy, Final Steps, Acknowledgments
2004 ــــــ
Advanced Therapy of OTITIS MEDIA )Atlas D'ORL Realise avec la collaboration des (Dr Michel Boucherat, Dr Jean-Robert Blondeau -Anatomie de l’oreille normale - Images pathologiques - Cas cliniques -Anatomie naso-sinusienne normale -Images pathologiques - Cas cliniques - Rappels des principes de la TDM et de l’IRM
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
2.2 3.2
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
10 ــــــ
)Atlas of Rhinoplasty Open and Endonasal Approaches (Gilbert Aiach, M.D
4.2
ــــــ
)Atlas of Head & Neck Surgery Otolaryngology (TEXTBOOK) (Byron J. Bailey, Karen H. Calhoun, Amy R. Coffey, J. Gail Neely
5.2
1- Atlas :
ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ٢٥ﺭﻭﺵ ﺟﺮﺍﺣﻲ ﺍﻧﺘﺨﺎﺑﻲ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻗﺴﻤﺖ ﺩﺍﺭﺍﻱ ٢٥ﻓﺼﻞ ﺩﺭ ﭼﻬﺎﺭ ﺑﺨﺶ ﺍﺻﻠﻲ ﺍﺳﺖ:
- Head & Neck Surgery :
ﺷﺎﻣﻞ ٦ﻋﻨﻮﺍﻥ ﺍﺻﻠﻲ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﺍﻃﻼﻋﺎﺕ ﺍﺳﺎﺳﻲ ﺭﺍﺟﻊ ﺑﻪ ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﺗﻤﻬﻴﺪﺍﺕ ﻗﺒﻞ ﺍﺯ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ،ﻭﺳﺎﻳﻞ ﻭ ﺭﻭﺵﻫﺎﻱ ﺑﻴﻬﻮﺷﻲ ﻭ ....ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ٦ .ﻋﻨﻮﺍﻥ ﺍﺻﻠﻲ ﺷﺎﻣﻞ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺳﺖ: • Thyroid & Parathyroid
• Neck & Larynx
• Ear
• Nose & maxilla
• Oral Clarity
: • Congenital Aural Base • Excision of skin Lesions
• Tran temporal Skull Base
- Otologic procedures
• Middle Ear and Ossicular Chain
- Plastic & Reconstructive Surgery : • Larygoplasty, Rhytidectomy, Rhinoplasty
• Mandibular Surgery, Local & Regional Flaps,
: • Ton Sillectomy
• Salivary Gland
- Pediatric and General Otolaryngology
• Nasal Polypectomy
ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺑﺮ ﺍﺳﺎﺱ ﻣﻮﺿﻮﻉ ،ﻛﻠﻤﺎﺕ ﻭ ﻭﺍﮊﻫﺎﻱ ﺗﺨﺼﺼﻲ ،ﻧﺎﻡ ﻧﻮﻳﺴﻨﺪﻩ ،ﺷﻤﺎﺭﺓ ﻣﺠﻠﻪ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻣﺒﺎﺣﺚ ﻣﻮﺭﺩ ﻧﻈﺮﺗﺎﻥ ﺭﺍ ﺟﺴﺘﺠﻮ ﻭ ﻣﻄﺎﻟﻌﻪ ﻧﻤﺎﺋﻴﺪ
• Frontal Sinus
2- Bilbo Med Medline :.
3- Head & Neck Surgery: - Textbook - Drug Reference - Textbook : ﺍﻳﻦ ﺑﺨﺶ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻧﻮﺷﺘﺔ ﺩﻛﺘﺮ Bailey
ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﻣﺘﻌﺪﺩ ﮔﻮﻳﺎ ﻭ ﻧﻤﻮﺩﺍﺭﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﺍﺳﺖ ﻛﻪ ﺷﺎﻣﻞ ١٨٠ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ. 1- Basic Science / General Medicine
٤ﺑﺨﺶ ﺍﺻﻠﻲ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﺍﻳﻦ ﺷﺮﺡ ﺍﺳﺖ:
)ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﮔﻮﻧﺎﮔﻮﻥ ﻭ ﺗﺨﺼﺼﻲ ﺭﺍﺟﻊ ﺑﻪ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﮔﻮﺵ ،ﺳﺮ ،ﮔﺮﺩﻥ(
2- Head & Neck :
3- Otology 4- Facial Plastic Reconstructive Surgery - Drug Reference :
ــــــ
ــــــ
ﺩﺍﺭﻭﻫﺎﻱ ﺍﺻﻠﻲ ﻭ ﮊﻧﻮﺗﻴﻚ ﺑﻪ ﺷﻜﻞ ﺍﻟﻔﺒﺎﻳﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺍﻃﻼﻋﺎﺕ ﻛﺎﻣﻞ ) ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ،ﺭﺩﺓ ﺩﺍﺭﻭﻳﻲ ،ﺍﺳﺎﻣﻲ ﺷﻴﻤﻴﺎﻳﻲ ﻭ ﺗﺠﺎﺭﺗﻲ ،ﻣﻘﺪﺍﺭ ﻣﺼﺮﻑ ﺍﺛﺮﺍﺕ ﺟﺎﻧﺒﻲ ،ﻓﺎﺭﻣﺎﻛﻮﻛﺴﻴﻚ ﺩﺍﺭﻭ ﻭ(..... )6.2 Causes of FAILURE in STAPES SURGERY (VCD I) (Howard P. House, TED N. Steffen )PITFALLS in STAPES SURGERY (VCD II )STAPEDECTOMY (Prefabricated Wire-Loop and Gelfoam Technique) (VCD III )7.2 Chirurgia Endoscopica Dei Seni Paranasali (A Cura di E. Pasquini G. Farneti 3. Aspetti radiologici
)(EIJI YANAGISAWA, MD
ــــــ 2002
1. Principi di anatomia endoscopica
2. Tecnica chirurgica
8.2 Color Atlas of Diagnostic Endoscopy in Otorhinolaryngolgy 9.2 Color Atlas of Ear Disease
)(Salekan E-book) (Richard A. Chole, MD, PhL, James W. Forsen )10.2 Cobblation Assisted Tonsillectomy (CAT) __ Cobblation Assisted Procedures (VCD) (CD I , II
ــــــ
ﺩﺭ CDﺷﻤﺎﺭﺓ ١ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺭﻭﻱ ﺗﻮﻧﺴﻴﻞﻫﺎ ﺑﺎ ﻛﻤﻚ ﺩﺳﺘﮕﺎﻩ Coblationﺑﻪ ﺷﻤﺎ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﺍﻳﻦ VCDﺷﺎﻣﻞ ﻣﻮﺍﺭﺩ ﺁﻣﻮﺯﺷﻲ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: 3- Coblation Assisted tonsilectomg
2- Lop – off "CAT" technique
1- Subtotal Cololation Assisted tonsillectomy
ﺩﺭ CDﺷﻤﺎﺭﺓ ٢ﺷﻤﺎ ﺑﺎ ﺩﺳﺘﮕﺎﻩ Coblationﻛﻪ ﺗﺤﻮﻟﻲ ﻋﻈﻴﻢ ﺩﺭ ﺣﻴﻄﻪ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ENTﺍﻳﺠﺎﺩ ﻛﺮﺩﻩ ﺍﺳﺖ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪ .ﻧﺤﻮﺓ ﻋﻤﻠﻜﺮﺩ ﺩﺳﺘﮕﺎﻩ ﺑﺮ ﺍﺳﺎﺱ ﺍﻣﻮﺍﺝ ﺭﺍﺩﻳﻮﻓﺮﻛﻮﺋﻨﺴﻲ ﺑﺎ ﻭﺍﺳﻄﻪ ﭘﻼﺳـﻤﺎ ﻣـﺎﻳﻊ ﻣـﻲﺑﺎﺷـﺪ ﻭ ﻣﺰﺍﻳـﺎﻱ ﻓﺮﺍﻭﺍﻧـﻲ ﺑـﺮ ﺩﺳـﺘﮕﺎﻫﻬﺎﻱ ﻟﻴـﺰﺭ ﻭ ﺭﺍﺩﻳﻮﻓﺮﻛﻮﺋﻨﺴﻲ ﻗﺪﻳﻤﻲ ﺩﺍﺭﺩ .ﻋﺪﻡ ﻧﻴﺎﺯ ﺑﻪ ﺑﻲﻫﻮﺷﻲ ﻋﻤﻮﻣﻲ ﻭ ﺍﻣﻜﺎﻥ ﺍﻧﺠﺎﻡ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺑﻪ ﺻﻮﺭﺕ ﺳﺮﭘﺎﻳﻲ ،ﺩﻭﺭﺍﻥ recoveryﻛﻮﺗﺎﻩ ،ﺗﺤﻤﻞ ﺑﺎﻻﻱ ﺑﻴﻤﺎﺭﺍﻥ ،ﻭﺟﻮﺩ ﺩﺭﺩ ﺑﺴﻴﺎﺭ ﻣﺨﺘﺼﺮ ﻳﺎ ﺣﺘﻲ ﻋﺪﻡ ﻭﺟﻮﺩ ﺩﺭﺩ ﭘﺲ ﺍﺯ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ،ﻇﺮﺍﻓﺖ ﻭ ﺗﻤﻴﺰﻱ ﺍﻋﻤﺎﻝ ،ﻫﻤﻮﺳـﺘﺎﺯ ﻋﺎﻟﻲ ،ﺣﺼﻮﻝ ﺳﺮﻳﻊ ﻧﺘﺎﻳﺞ ،ﺳﺮﻋﺖ ﺑﺎﻻﻱ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ﻭ ﺭﺍﺣﺘﻲ ﻓﻮﻕﺍﻟﻌﺎﺩﻩ ﺟﺮﺍﺡ ﺑﺮﺧﻲ ﺍﺯ ﻣﺰﺍﻳﺎﻱ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﺩﺳﺘﮕﺎﻩ ﻣﻲﺑﺎﺷﺪ .ﺍﺯ ﺍﻳﻦ ﺩﺳﺘﮕﺎﻩ ﺩﺭ ﺣﻴﻄﺔ ENTﺩﺭ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩ: 1- Coblation channeling of the inferior turbinate
ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﺩﺳﺘﮕﺎﻩ ﻭ ﺗﺤﺖ ﺑﻲﺣﺴﻲ ﻟﻮﻛﺎﻝ ،ﺍﻧﺴﺪﺍﺩ ﺑﻴﻨﻲ ﻧﺎﺷﻲ ﺍﺯ ﻫﻴﭙﺮﺗﺮﻭﻓﻲ ﺗﻮﺭﺑﻴﻨﻪ ﺗﺤﺘﺎﻧﻲ ﺑﻪ ﻛﻤﻚ Channelingﺗﻮﺭﺑﻴﻨﻪ ﺩﺭﻣﺎﻥ ﻣﻲﺷﻮﺩ .ﻧﺘﻴﺠﻪ ﻋﻤﻞ ﺑﻪ ﺻﻮﺭﺕ ﺭﻳﺪﺍﻛﺸﻦ ﺳﺮﻳﻊ ﺗﻮﺭﺑﻴﻨﻪ ﺑﻼﻓﺎﺻﻠﻪ ﻗﺎﺑﻞ ﻣﺸﺎﻫﺪﻩ ﺍﺳﺖ :ﺍﻳﻦ ﻋﻤﻞ ﺗﻘﺮﻳﺒﹰﺎ ﺑﻲﺩﺭﺩ ﺧﻮﺍﻫﺪ ﺑﻮﺩ. 2- Coblation channeling of the Soft palate
ﺩﺭ ﺍﻳﻦ ﻋﻤﻞ ،ﺑﺎ Channelingﻛﺎﻡ ﻧﺮﻡ ﺍﺯ ﺣﺠﻢ ﺁﻥ ﻛﺎﺳﺘﻪ ﺷﺪﻩ ﻭ ﺑﺎﻋﺚ ﺭﻓﻊ ﺧﺮﺧﺮ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﻣﻲﺷﻮﺩ .ﺍﻳﻦ ﻋﻤﻞ ﺳﺮﭘﺎﻳﻲ ﻭ ﺗﺤﺖ ﺑﻲﺣﺴﻲ ﻟﻮﻛﺎﻥ ﻭ ﺗﻘﺮﻳﺒﹰﺎ ﻓﺎﻗﺪ ﺩﺭﺩ ﺍﺳﺖ .ﻧﺘﻴﺠﺔ ﻋﻤﻞ ﻧﻴﺰ ﺑﻪ ﺳﺮﻋﺖ ﺣﺎﺩﺙ ﻣﻲﺷﻮﺩ. 3- Coblation channeling of the tonsil
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
11 . ﻧﺘﻴﺠﻪ ﺑﻪ ﺳﺮﻋﺖ ﺣﺎﺩﺙ ﺷﺪﻩ ﻭ ﻋﻤﻞ ﺗﻘﺮﻳﺒﹰﺎ ﻓﺎﻗﺪ ﺩﺭﺩ ﺍﺳﺖ. ﺑﺴﺘﻪ ﺑﻪ ﺷﺮﺍﻳﻂ ﺍﻳﻦ ﻋﻤﻞ ﻣﻲﺗﻮﺍﻧﺪ ﺳﺮﭘﺎﻳﻲ ﻳﺎ ﺗﺤﺖ ﺑﻲﻫﻮﺷﻲ ﻋﻤﻮﻣﻲ ﺑﺎﺷﺪ. ﺗﻮﻧﺴﻴﻞ ﻛﺎﺳﺘﻪ ﻣﻲﺷﻮﺩbulk ﻫﻴﭙﺮﺗﺮﻭﻧﻲ ﺗﻮﻧﺴﻴﻠﺮ ﺑﺮﻃﺮﻑ ﺷﺪﻩ ﻭ ﺍﺯ،ﺑﺎ ﺍﻳﻦ ﺭﻭﺵ 4- Coblation Assisted Tonsillectomy(CAT)
11.2 DALLAS RHINOPLASTY
. ﻭ ﺩﻭﺭﺍﻥ ﺑﻬﺒﻮﺩﻱ ﺳﺮﻳﻊ ﻣﻲﺑﺎﺷﺪ.ﻻ ﺑﺴﻴﺎﺭ ﻣﺨﺘﺼﺮ ﺍﺳﺖ ﺩﺭﺩ ﭘﺲ ﺍﺯ ﻋﻤﻞ ﻣﻌﻤﻮ ﹰ.ﺩﺭ ﺻﻮﺭﺕ ﻭﺟﻮﺩ ﺗﻮﻧﺴﻴﻞﻫﺎﻱ ﺑﺰﺭﮒ ﻳﺎ ﺗﻮﻧﺴﻴﻠﻴﺖ ﻓﺮﺽ ﺍﺯ ﺍﻳﻦ ﺭﻭﺵ ﺟﻬﺖ ﺍﻧﺠﺎﻡ ﺗﻮﻧﺴﻴﻠﻜﺘﻮﻣﻲ ﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩ
Nasal Surgery by the Masters (Reducing Tip Projection and Nostrill Show Via the Open Approach) (CD I , II)
VCD: 1 1) Cadaveric Rhinoplasty Dissection Technique 2) Role of Component Dorsal Reduction: Spreader Grafts in the Deviated Nose
2002
VCD: 2 Reducing Tip Projection and Nostril Show Via the Open Approach
: ﺑﻪ ﺷﻤﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺑﺮ ﺭﻭﻱ ﻛﺎﺭﺁﻭﺭ ﺍﺯ ﺍﺑﺘﺪﺍ ﻭ ﺩﺭ ﻏﺎﻟﺐ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﺑﻪ ﺗﺮﺗﻴﺐ ﺁﻣﻮﺯﺷﻲ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ، ﻛﻪ ﺩﺭ ﺳﭙﻮﺯﻳﻮﻡ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺩﺍﻻﺱ ﺗﻬﻴﻪ ﺷﺪﻩ ﺍﺳﺖ١ ﺷﻤﺎﺭﺓVCD ﺩﺭ 1)
Exposure/Nasal incisions A. Closed endonasal approach - Intracartilaginous (IC) incision B. Cartilage delivery technique - Infracartilaginous incision - Intercartilaginous incision C. Open Rhinoplasty approach - Transcolumellar incision
2) Tip Alteration 3) Sptal reconstraction 4) Osteotmies 5) Adjuctive techniques/Closure A. Columellar Stat placement A. Septal reconstraction A. Medial Osteotomy A. Alare base resection - Intercarural suture stabilization - Inferior tarbinate resection B. Lateral Osteotomy - Correction of alalr flaring B. Controlling dome angalation (Submacosal) C. External Osteotomy - Diminishing nostril shape and tip defining points - Septal reconstruction B. Closare - Interdomal sutures B. Modification of the dorsum C. Splints - Transdomal Satares - Component dorsum C. Correction of alar reduction pinching/notching - Spreader graft placement - lateral crural strut grafts - Alar contour grafts D. Tip grafts - Infratip graft - Onlay tip graft ﺑـﻪGunter ﺍﺯ ﻣﺼﺎﺣﺒﻪ ﺑﺎ ﺑﻴﻤﺎﺭ ﺁﻏﺎﺯ ﺷـﺪﻩ ﻭ ﺳـﭙﺲ ﺩﻛﺘـﺮVCD ﺁﻣﻮﺯﺵ ﺩﺭ ﺍﻳﻦ. ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩOpen ﺗﺤﺖ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺑﺎ ﺍﭘﺮﻭﭺGunter ﺯﻳﺎﺩ ﺗﻮﺳﻂ ﺁﻗﺎﻱ ﺩﻛﺘﺮnostril show , Projected tip ﺧﺎﻧﻢ ﺟﻮﺍﻧﻲ ﺑﺎ ﺷﻜﻞ٢ ﺷﻤﺎﺭﺓVCD ﺩﺭ
. ﺳﭙﺲ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﺑﺎ ﻇﺮﺍﻓﺖ ﻋﺎﻟﻲ ﺩﺭ ﻏﺎﻟﺐ ﻣﺮﺍﺣﻞ ﺯﻳﺮ ﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩ.ﺁﻧﺎﻟﻴﺰ ﻧﺎﺯﻭﻧﺎﺷﻴﺎﻝ ﻭﻱ ﻣﻲﭘﺮﺩﺍﺯﺩ 4) Transaction of lat Crura
3) Underminig tip Skin
2) Infracartilaginous and trans columellar incisions
1)Complete transfixion incision
8) Reduction of dorsal septum (DS) and upper lateral cartilage (ULC)
7) reduction of bony darsum (BD)
6) Preparing submucosal tunnels
5) Resection of feet of medial crura
12) Cephalic resection of lateral Crura (LC)
11) Spreader grafts
10) Medial asteomius
9) Harvesting Septal cartilages for grafting
16) Final adjustment of dorsal height
15) Lateral asteotomy Cinternal
14) Aligning the dorsum
13) Preparation for lateral crural grafts (LCSG)
19) Closure
18) Placement of lateral crural strut grafts
17) Columellar strt placemend
!! ﺗﻮﺟﻪ ﺷﻤﺎ ﺭﺍ ﺑﻪ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻭﺳﻴﻠﻪ ﺭﻳﺪﺍﻛﺸﻦ ﺩﻭﺭ ﺳﻮﻡ ﺍﺳﺘﺨﻮﺍﻧﻲ ﻧﻴﺰ ﺟﻠﺐ ﻣﻲﻛﻨﻴﻢVCD ﺩﺭ ﺍﻳﻦ.ﺩﺭ ﻧﻬﺎﻳﺖ ﺷﻤﺎ ﻧﺘﺎﻳﺞ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ ﺑﻴﻤﺎﺭ ﺩﺭ ﻓﻮﺍﺻﻞ ﻣﺨﺘﻠﻒ ﻣﺸﺎﻫﺪﻩ ﻣﻲﻛﻨﻴﺪ 12.2 EENT Welch Allyn Institute of Interactive Learning
ــــــ
13.2 Endoscopic Assisted Procedures used in Astatic Facial Plastic Surgery
(VCD) (CD I , II)
ــــــ
ﺁﻣﻮﺯﺷﻲ ﺑﻪ ﺻـﻮﺭﺕ ﻗـﺪﻡ. ﺳﭙﺲ ﺑﻪ ﺷﻤﺎ ﺗﻜﻨﻴﻚ ﺟﺮﺍﺣﻲ ﺍﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﻣﺎﻻﺭﻭﻓﺮﻭﻧﺘﺎﻝ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﻫﻨﺮﻱ ﺩﻟﻤﺎﺭ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. ﺷﺮﻛﺖ ﻛﺎﺭﻝ ﺍﺷﺘﻮﺭﺗﺰ ﭘﻴﺸﺮﻭ ﺩﺭ ﺍﺭﺍﺋﻪ ﺗﺠﻬﻴﺰﺍﺕ ﺍﻧﺪﻭﺳﻜﻮﭘﻲ ﻭ ﻣﺤﺼﻮﻻﺕ ﺁﻥ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪ، ﺍﻭﻝ ﺷﻤﺎ ﺩﺭ ﺍﺑﺘﺪﺍVCD ﺩﺭ ﺍﻳﻦ . ﺭﺍ ﺑﻪ ﻧﻤﺎﻳﺶ ﻣﻲﮔﺬﺍﺭﺩEndoscopic forehead rhytidectomy and brow elevation ﺗﻜﻨﻴﻚ ﺟﺮﺍﺣﻲGrlecory S. Keller ﺩﺭ ﻣﺮﺣﻠﺔ ﺑﻌﺪ ﺩﻛﺘﺮ.( ﺍﺩﺍﻣﻪ ﻣﻲﻳﺎﺑﺪclosure) ﺑﻪ ﻗﺪﻡ ﺍﺯ ﻧﺸﺎﻧﻪﮔﺬﺍﺭﻱ ﺭﻭﻱ ﭘﺮﺕ ﻭ ﺗﺰﺭﻳﻖ ﻭ ﺑﺮﺵﻫﺎ ﺷﺮﻭﻉ ﺷﺪﻩ ﻭ ﺗﺎ ﭘﺎﻳﺎﻥ ﻋﻤﻞ Extended Composite face Lift
Endoscopic midface Lift
Endoscopic forehead Lift
: ﺷﻤﺎ ﺑﺎ ﺍﻳﻦ ﻣﻮﺍﺭﺩEndoscopic assisted forehead and face lifting ﺩﻭﻡ ﺗﺤﺖ ﻋﻨﻮﺍﻥVCD ﺩﺭ
ﺍﺑﺰﺍﺭﺁﻻﺕ ﻻﺯﻡ ﺩﺭ ﻋﻤﻞ، ﺩﺭ ﭘﺎﻳﺎﻥ ﻧﺤﻮﺓ ﺛﺒﺖ ﺳﻪﺑﻌﺪﻱ ﺗﻐﻴﻴﺮﺍﺕ. ﻣﺎﻩ ﺑﻌﺪ( ﻫﻢ ﺑﻪ ﺷﻤﺎ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ٢) ﺩﺭ ﻫﺮ ﻣﻮﺭﺩ ﺑﺮﺍﻱ ﺷﻤﺎ ﻳﻚ ﺑﻴﻤﺎﺭ ﻣﻮﺭﺩ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﺗﻮﺳﻂ ﺁﻥ ﺗﻜﻨﻴﻚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﻧﺘﺎﻳﺞ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ.ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ ﻭ ﻓﻮﺍﻳﺪ ﻫﺮ ﺭﻭﺵ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪ .ﺟﺮﺍﺣﻲ ﻫﻢ ﺑﻪ ﺷﻤﺎ ﻣﻌﺮﻓﻲ ﻣﻲﺷﻮﺩ 14.2 Diseases of the Sinuses Diagnosis and Management (Darid W. Kennedy, MD, FRCSI, William E. Bolger, MD, FACS, S. James Zinreich, MD) . ﺍﻳﻦ ﻛﺘﺎﺏ ﺗﻘﺮﻳﺒﹰﺎ ﻣﻌﺘﺒﺮﺗﺮﻳﻦ ﺭﻓﺮﺍﻧﺲ ﺳﻴﻨﻮﻧﺎﺯﻭﻟﻮﮊﻱ ﺩﺭ ﺩﻧﻴﺎ ﻣﻲﺑﺎﺷﺪ. ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ2001 ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺳﻴﻨﻮﺱ ﺑﻪ ﺗﺎﻟﻴﻒ ﺁﻗﺎﻱ ﺩﻛﺘﺮ ﺩﻳﻮﻳﺪﻛﻨﺪﻱ ﻣﺤﺼﻮﻝ ﺳﺎﻝtext book ، CD ﺩﺭ ﺍﻳﻦ 15.2 Endoscopic Sinus Surgery (SALEKAN-eBook) ﺁﺷﻨﺎﻳﻲ ﺷﻤﺎ ﺷﺎﻣﻞ ﺍﺑﺘﺪﺍﻳﻲﺗﺮﻳﻦ ﻣﺴﺎﺋﻞ ﻣﻦﺟﻤﻠﻪ ﺍﺑﺰﺍﺭﺁﻻﺕ ﺑﻜﺎﺭ ﺭﻓﺘﻪ ﺩﺭ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺁﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﺳﻴﻨﻮﺱ ﻭ ﺣﺘﻲ ﻧﺤﻮﺓ ﺍﻳﺴﺘﺎﺩﻥ ﻳﺎ. ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﻃﺒﻘﻪﺑﻨﺪﻱ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﺷﻤﺎ ﺑﺎ ﻓﻴﻠﺪ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺁﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺳﻴﻨﻮﺳﻲ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪCD ﺩﺭ ﺍﻳﻦ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــــ ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
12 ( ﺑـﻪAtlas and textbook) ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﺟﺮﺍﺣﻲ ﺁﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﺳﻴﻨﻮﺱﻫﺎﻱ ﭘﺎﺭﺍﻧﺎﺯﺍﻝ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺮﺗﺒﻂ ﺑﺎ ﺍﻧﻬﺎ ﺑﻪ ﺻﻮﺭﺕ ﻣﺘﻦ ﻭ ﮔـﺮﺍﻑ. ﻣﺒﺎﻧﻲ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻭ ﺩﺍﻳﺴﻜﺸﻦ ﺑﺮﺍﻱ ﺷﻤﺎ ﺗﺸﺮﻳﺢ ﻣﻲﺷﻮﺩ.ﻧﺸﺴﺘﻦ ﻫﻨﮕﺎﻡ ﻋﻤﻞ ﻭ ﮔﺮﻓﺘﻦ ﺍﺑﺰﺍﺭ ﺩﺭ ﺩﺳﺖ ﻫﻢ ﻣﻲﺷﻮﺩ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﻓﺼﻮﻝ ﺍﻳﻦ.ﺷﻤﺎ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ 1- Consistent and Relible Anatomical Landmarks in Endoscopic Sinus Surgery
2- Surgical Instrumentation
3- Setup and patient positioning
4- Basic Dissection
5- Advanced Dissection
16.2 ENDONASAL SINUSECTOMY WITH CORRECTION OF THE NASAL CAVITY (Rikio Ashikawe, Takashi Ohmae, Toshio Ohnisshi, Yutaka Uchida)
ــــــ
The Endonasal sinusectomy with correction of the nasal cavity (Takahash's methodn) is carried out in seven steps. 17.2 Endoscopic Sinus Surgery NEW HORIZONS (Nikhil J. Bhatt, M.D.)
ــــــ
18.2 EVIDENCE-BASED OTITIS MEDIA (Richard M. Rosenfeld, MD, MPH, Charles D. Bluestone, MD)
ــــــ
ﺩﺭﻣـﺎﻥﻫـﺎﻱ ﺩﺍﺭﻭﻳـﻲ ﻭ ﺟﺮﺍﺣـﻲ ﺁﻥ، ﺗﺸﺨﻴﺺ، ﻋﻼﺋﻢ ﻭ ﻣﺴﻴﺮ ﺑﺎﻟﻴﻨﻲ، ﺁﺷﻨﺎﻳﻲ ﺍﺯ ﻣﺴﺎﺋﻞ ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻳﻚ ﻭ ﺗﺤﻘﻴﻘﺎﺕ ﺍﻧﺠﺎﻡ ﺷﺪﻩ ﺁﻏﺎﺯ ﺷﺪﻩ ﻭ ﺩﺭ ﺍﺩﺍﻣﻪ ﺑﻪ ﻣﻮﺷﻜﺎﻓﻲ ﺩﺭ ﻣﻮﺭﺩ ﺍﻧﻮﺍﻉ ﺍﺗﻴﻮﻟﻮﮊﻱ. ﺷﻤﺎ ﺑﺎ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻭﺗﻴﺖ ﻣﺪﻳﺎ ﺑﻪ ﺻﻮﺭﺗﻲ ﺍﺻﻮﻟﻲ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪCD ﺩﺭ ﺍﻳﻦ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﻓﺼﻮﻝ ﺍﻳﻦ. ﺩﺭ ﺿﻤﻦ ﺍﺛﺮﺍﺕ ﺍﻳﻦ ﺑﻴﻤﺎﺭﻱ ﺭﻭﻱ ﺗﻜﺎﻣﻞ ﻛﻮﺩﻙ ﻭ ﻛﻴﻔﻴﺖ ﺯﻧﺪﮔﻲ ﺍﻭ ﻧﻴﺰ ﺗﺸﺮﻳﺢ ﻣﻲﮔﺮﺩﺩ. ﺩﺭ ﺍﻧﺘﻬﺎ ﻧﺘﺎﻳﺞ ﺩﺭﻣﺎﻥ ﺑﺮﺭﺳﻲ ﻣﻲﺷﻮﺩ.ﻣﻲﭘﺮﺩﺍﺯﺩ 1- Methodology
2- Clinical Management
19.2 Facial Plastic & Reconstructive Surgery 20.2 Facial Nerve Surgery (Jack L. Pulec, M.D.)
3- Consequences and Sequelae
(Terence M. Davidson, MD) (VCD I , II)
ــــــ
Otologic Medical Group, Inc. Los Angeies
ــــــ
21.2 Head and Neck Surgery (Jatin P Shah, MD, MS (Surg), FACS) (Mosby)
ــــــ
22.2 Introduction to Ear Acupuncture (Martin Franke)
2001
ﺁﻣﻮﺯﺵ ﺍﺯ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻧﻮﺍﺣﻲ ﻣﺨﺘﻠﻒ ﻣﻮﺭﺩﻧﻈﺮ ﺩﺭ ﻃﺐ ﺳﻮﺯﻧﻲ ﮔﻮﺵ ﺁﻏﺎﺯ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺑﺎ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻃـﺐ. ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﺷﻤﺎ ﺑﺎ ﺍﺻﻮﻝ ﻛﻠﻲ ﻃﺐ ﺳﻮﺯﻧﻲ ﮔﻮﺵ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪThieme ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﻣﺎﺭﺗﻴﻦ ﻓﺮﺍﻧﻚ ﺗﻬﻴﻪ ﻭ ﺗﻮﺳﻂ ﺍﻧﺘﺸﺎﺭﺍﺕ ﻣﻌﺘﺒﺮCD ﺩﺭ ﺍﻳﻦ . ﺍﺩﺍﻣﻪ ﻣﻲﻳﺎﺑﺪ ﺳﭙﺲ ﺷﻤﺎ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻧﮕﺎﻫﻲ ﺑﻪ ﻧﺘﺎﻳﺞ ﺍﻳﻦ ﺍﻋﻤﺎﻝ ﻫﻢ ﺩﺍﺷﺘﻪ ﺑﺎﺷﻴﺪ ﻭ ﺁﻧﻬﺎ ﺭﺍ ﺍﺭﺯﻳﺎﺑﻲ ﻧﻤﺎﺋﻴﺪ... ﺍﻋﺘﻴﺎﺩ ﺑﻪ ﺳﻴﮕﺎﺭ ﻭ، ﺳﺮﮔﻴﺠﻪ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺧﻮﺍﺏ،ﺳﻮﺯﻧﻲ ﺩﺭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺨﺘﻠﻒ ﻫﻤﭽﻮﻥ ﻣﻴﮕﺮﻥ 1- Localization Assignment
2- Localization Determination
3- Treatment
4- Evaluation
23.2 La Rhinoplastica Ragionata (Valerio Micheli-Pellegrini, Roberto Polselli)
ــــــ
24.2 Nasal Aesthetics and Anatomy: A Cadaver Study (Rollin K. Daniel, M.D.)
ــــــ
25.2 Open Tip Graft in Twin Patient (Rollin K. Daniel, M.D.)
ــــــ
26.2 OPEN RHINOPLASTY Cadaver Dissection Program (Dean M. Toriumi, MD.) (Vol I , II) (College of Medicine at Chicago)
ــــــ
Analysis, Operative Planning, Twins Pre and Post, Anesthesia, Transfixion Incision, Septal Harvest, Open Approach, Exposure, Tip Anatomy, Tim Strips, Graft Preparation, Radix Graft, Crural Strut, Domal Excision, Graft, Shaping, Graft, Insertion, Closure, Post Op Result, Credits 1- Access to nasal Septum - Hemitrans Fixatu incision - Havvestiong Septal Cartilage
3- Open Rhinoplasty approach - Incisions - Flap Elevation
5- Management of Middle Nasal Vault - Division of apper Lateral Cartilages from septum - Application of Spreader grafts
2- Havvestiog of Conchal Cartilage - Anterior approach for harvestiog Cartilage - Flap elevention - Cartilage excision - Closure and dressing
4- Stractural grafts used in Secondary - loteral Crural grafts - Alar Batten grafts
6- Major septal reconstruction - Reconstraction of L-Shaped Septal Strat
7- Management of Lower third of the nose - Cephalic trimming of lateral Crura - Satured – in – place Collamellar Strut - Transdomal Sutur - Sutured – in – place tip 8- Chin augmentation - Preparation of the implant - Incision and dissection - placement of Implant
27.2 Open Structure Rhinoplasty (A Case Oriented Approach)
2005
28.2 Otorhinolaryngology Head and Neck Surgery
2003
Otology and Neurotology
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(SIXTEENTH EDITION) (James B, Snow Jr, MD, John Jacob Ballenger, MD,)
Facial Plastic and Reconstructive Surgery
Pediatric Otolaryngology
Rhinology
Bronchoesphagology
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
Laryngology
Head and Neck Surgery
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
13 ــــــ
)29.2 Plastic Surgery (Fifth Edition) (Grabb and Smith's) (Salekan E-Book
ــــــ
ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻣﺸﺘﻤﻞ ﺑﺮ ٩٢ﻓﺼﻞ ﺩﺭ ٧ﻗﺴﻤﺖ ،ﻛﺘﺎﺑﻲ ﻛﺎﻣﻞ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﺩﺭ ﺗﻤﺎﻡ ﻣﺒﺎﺣﺚ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﻣﻨﻈﻮﺭ ﻋﻼﻗﻤﻨﺪﻱ ﺑﻪ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺩﺭ ﺗﻤﺎﻡ ﺳﻄﻮﺡ ﺁﻣﻮﺯﺵ ﻭ ﺩﺭﻣﺎﻥ ﭘﺰﺷﻜﻲ ﻣﻲﺑﺎﺷﺪ ﻭ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﻣﻲﺑﺎﺷﺪ .ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ﺍﻳﻦ ﻛﺘﺎﺏ ﻫﻤﭽﻨﻴﻦ ﺑﺮﺍﻱ ﺍﻣﺘﺤﺎﻧﺎﺕ ﻭ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺑﻮﺭﺩ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺁﻣﺮﻳﻜﺎ ﺳﻮﺩﻣﻨﺪ ﺍﺳﺖ. ﺑﺨﺶ ﺍﻭﻝ General Reconstruction :ﺑﻮﺩﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﺗﺮﻣﻴﻢ ﺯﺧﻢ ،ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﻭﻟﻴﺔ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺁﻧﺸﺮﻱ ، implants ،ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ flapﻭ graftﻭ ...ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ ﺩﻭﻡ :ﺑﻪ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺩﺭ ﭘﻮﺳﺖ ﻣﻲﭘﺮﺩﺍﺯﺩ ﻛﻪ ﺷﺎﻣﻞ ﭼﮕﻮﻧﮕﻲ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺗﻮﻣﻮﺭﻫﺎﻱ ﭘﻮﺳﺖ ،ﺧﺎﻝﻫﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ،ﺟﺮﺍﺣﻲ ﺑﺎ Mothsﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﺩﺭ ﭘﻮﺳﺖ ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ ﺳﻮﻡ :ﺑﻪ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﺳﺮ ﻭ ﮔﺮﺩﻥ ﻣﻲﭘﺮﺩﺍﺯﺩ ﻣﺎﻧﻨﺪ )ﺍﺻﻼﺡ ﺩﻓﺮﻳﺘﻤﻲﻫﺎﻱ ﺳﺮ ﻭ ﺻﻮﺭﺕ ،ﺍﺗﻮﭘﻼﺳﻤﻲ Reconstruction ،ﺑﻴﻨﻲ ،ﮔﻮﺵ ﻭ ﮔﻮﻧﻪ ﻭ ﻟﺐ ﻭ (...ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ ﭼﻬﺎﺭﻡ :ﺟﺮﺍﺣﻲﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ ، dermabrasion, peeling) :ﺗﺰﺭﻳﻖ ﻛﻼﮊﻥ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ،ﻟﻴﭙﻮﺳﺎﻛﺸﻦ (...endoscopic plastic surgery ،ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ ﭘﻨﺠﻢ :ﺟﺮﺍﺣﻲﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﻭ ﺗﺮﻣﻴﻤﻲ breastﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﻛﻪ ﺷﺎﻣﻞ :ﻣﺎﻣﻮﭘﻼﺳﺘﻲ ،ﻛﻤﭙﻠﻴﻜﺎﺳﻴﻮﻥ ،ﺗﺼﻴﺤﻴﺤﻲ ﮊﻳﻨﻜﻮﻣﺎﺳﺘﻲ ﻭ ...ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ. ﺑﺨﺶ ﺷﺸﻢ :ﺍﻳﻦ ﻗﺴﻤﺖ ﺑﻪ ﺟﺮﺍﺣﻲ ﺗﺮﻣﻴﻤﻲ ﺩﺳﺖ ﺍﺧﺘﺼﺎﺹ ﺩﺍﺭﺩ. ﺑﺨﺶ ﻫﻔﺘﻢ :ﻣﺮﺑﻮﻁ ﺑﻪ ﻧﺎﺣﻴﺔ ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻨﻲ ﻭ ﺗﻨﻪ ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ :ﺩﺭﻣﺎﻥ ﺯﺧﻢ ﺑﺴﺘﺮ Reconstruction ،ﺩﻳﻮﺍﺭﺓ ﺷﻜﻢ ﻭ ..... ﺑﺨﺶ ﻫﺸﺘﻢ :ﺑﺤﺚ ﻧﺎﺣﻴﺔ ﮊﻧﻴﺘﺎﻟﻴﺎ ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ :ﺩﺭﻣﺎﻥ ﻫﻴﭙﻮﺳﭙﺎﺩﻳﺎﺱ ﻭ Reconstruction of peniﻭ.... ﻣﺆﻟﻔﻴﻦ ﻛﺘﺎﺏ ﺍﺯ ﺑﺮﺟﺴﺘﻪ ﺗﺮﻳﻦ ﭘﻴﺸﮕﺎﻣﺎﻥ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﺩﺭ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﻣﻲﺑﺎﺷﻨﺪ Fitzpatrickﻭ Goldmanﻫﻤﺮﺍﻩ ﺑﺎ Alsterﺳﻪ ﺗﻦ ﺍﺯ ﻣﻄﺮﺡﺗﺮﻳﻦ ﺍﺷﺨﺎﺹ ﺩﺭ ﻣﺒﺎﺣﺚ ﻟﻴﺰﺭﻱ ﻣﻲﺑﺎﺷﻨﺪ .ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ :ﻣﺎ ﺳﻌﻲ ﻛﺮﺩﻩ ﺍﻳﻢ ﻳﻜﺒﺎﺭ ﺩﻳﮕﺮ ﺍﻛﺜﺮ ﺗﺤﻘﻴﻘـﺎﺕ ﻭ ﺩﺍﻧﺶ ﻛﺎﺭﺑﺮﺩ ﻟﻴﺰﺭ ﺩﺭ ﭘﻮﺳﺖ ﺭﺍ ﺩ ﺍﺧﻞ ﻳﻚ ﻛﺘﺎﺏ ﮔﺮﺩﺁﻭﺭﻱ ﻛﻨﻴﻢ .ﻣﺒﺎﺣﺚ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﻃﻮﺭ ﺗﺨﺼﺼﻲ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﺓ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖ ﻫﺎ ﻭ ﺟﺮﺍﺣﺎﻧﻲ ﻛﻪ ﺩﺭ ﺯﻣﻴﻨﺔ rejuvenationﭘﻮﺳﺖ ﺻﻮﺭﺕ ﻓﻌﺎﻟﻴﺖ ﺩﺍﺭﻧﺪ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺳﺖ. )30.2 Primary Rhinoplasty (Bahman Guyuron, MD, FACS, Cleveland, Ohio) (VCD ﺩﺭ ﺍﻳﻦ VCDﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﻳﻜﻲ ﺍﺯ ﺑﺰﺭﮔﺘﺮﻳﻦ ﺟﺮﺍﺣﺎﻥ ﺻﺎﺣﺐ ﻧﺎﻡ ﺩﻧﻴﺎ ،ﺍﺯ ﻛﺸﻮﺭ ﻋﺰﻳﺰﻣﺎﻥ ﺍﻳﺮﺍﻥ ،ﺑﻪ ﻧﺎﻡ ﺁﻗﺎﻱ ﺩﻛﺘﺮ ﺑﻬﻤﻦ ﻏﻴﻮﺭﺍﻥ ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩ Ohioﺗﻬﻴﻪ ﺷﺪﻩ ﺍﺳﺖ ،ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻳﻚ ﻋﻤﻞ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺍﻭﻟﻴﻪ ﺑﺎ ﺍﭘﺮﻭﺝ Openﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﻣﻮﺭﺩ ﻋﻤﻞ ﺩﺧﺘﺮ ﺟﻮﺍﻧﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ Caseﻓﻮﻕﺍﻟﻌﺎﺩﻩ ﻣﺸﻜﻠﻲ ﺩﺭ ﺯﻣﻴﻨﻪ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﻣﺤﺴﻮﺏ ﺷﺪﻩ ﻭ ﺁﻗﺎﻱ ﺩﻛﺘﺮ ﻏﻴﻮﺭﺍﻥ ﭘﺲ ﺍﺯ ﺁﻧﺎﻟﻴﺰ ﻛﺎﻣﻞ ﻧﺎﺯﻭﻓﺎﺷﻴﺎﻝ ﺟﺮﺍﺣﻲ ﺭﺍ ﺑﺎ ﻇﺮﺍﻓﺖ ﻫﺮ ﭼﻪ ﺗﻤﺎﻣﺘﺮ ﺍﺯ ﺍﺑﺘﺪﺍﻱ ﺍﻣﺮ )ﺗﺰﺭﻳﻖ ﻭ ﺑﻲﺣﺴﻲ ﺗﻮﭘﻴﻜﺎﻝ( ﺗﺎ ﺍﻧﺘﻬﺎ )ﭘﺎﻧﺴﻤﺎﻥ( ﺍﺟﺮﺍ ﻣـﻲﻛﻨﻨـﺪ .ﺩﻳـﺪﻥ ﺍﻳـﻦ VCDﺭﺍ ﺍﻛﻴﺪﹰﺍ ﺑﻪ ﻛﻠﻴﻪ ﻣﺘﺨﺼﺼﻴﻦ ﺗﻮﺻﻴﻪ ﻣﻲﻛﻨﻴﻢ. )A Practical Guide to functional and asthetic surgery of the nose (G. J. Nolst
ــــــ
31.2 RHINOPLASTY
ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﻧﻮﻟﺴﺖ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ .ﺭﺍﻫﻨﻤﺎﻳﻲ ﻋﻤﻠﻲ ﺟﻬﺖ ﺟﺮﺍﺣﻲ ﻓﺎﻧﻜﺸﻨﺎﻝ ﻭ ﺍﺳﺘﺎﺗﻴﻚ ﺑﻴﻨﻲ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺍﻳﻦ ﻓﻴﻠﻢ ﺍﺻﻮﻝ ﭘﺎﻳﻪ ﺯﻳﺒﺎﻳﻲﺷﻨﺎﺳﻲ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ ،ﺍﺯ ﻣﺮﺍﺣﻞ ﭘﺎﻳﻪ )ﺍﺯ ﺗﻜﻨﻴﻚ ﺗﺎ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ( )ﺗﺤﺖ ﺑﻲﻫﻮﺷﻲ ﻋﻤﻮﻣﻲ( ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. ﺩﺭ ﺍﻳﻦ ﻓﻴﻠﻢ ﺗﻮﺟﻪ ﺷﻤﺎ ﺭﺍ ﺑﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﺍﺳﺘﺌﻮﺗﻮﻣﻲ ﺍﺯ ﺭﺍﻩ ﭘﻮﺳﺖ ﻭ ﻧﻴﺰ ﺣﻔﻆ ﺳﺎﭘﻮﺭﺕ tipﺟﻠﺐ ﻣﻲﻛﻨﻴﻢ .ﺩﺭ ﺍﻧﺘﻬﺎ ﺍﺯ ﻏﻀﺮﻭﻑ ﻛﻮﻧﻜﺎﻱ ﮔﻮﺵ ﺑﻴﻤﺎﺭ ،ﮔﺮﺍﻓﺖ )ﺷﻴﻠﺪ ﻳﺎ ﺍﺳﺘﺮﺍﺕ ﻛﻠﻮﻣﻼ( ﺗﻬﻴﻪ ﻣﻲﺷﻮﺩ ﻭ ﺑﺮﺍﻱ ﻗﺮﺍﺭﺩﺍﺩﻥ ﺁﻥ ﺍﺯ ﺍﭘﺮﻭﭺ openﻛﻤﻚ ﮔﺮﻓﺘﻪ ﻣﻲﺷﻮﺩ. ﺩﺭ ﻫﺮ ﻓﺼﻞ ﺍﺑﺘﺪﺍ ﺑﻪ ﺻﻮﺭﺕ textﺗﻮﺿﻴﺤﺎﺗﻲ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﻭ ﻓﻴﻠﻢ ﻣﺮﺑﻮﻁ ﺑﻪ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺁﻥ ﺑﺨﺶ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻮﻝ ﺍﻳﻦ CDﺷﺎﻣﻞ: : Basic Knowledgeﺷﺎﻣﻞ ﺁﻧﺎﺗﻮﻣﻲ ،ﺯﻳﺒﺎﺋﻲﺷﻨﺎﺧﺘﻲ Pre-opﻭ Post-opﻭ ﻛﻤﭙﻠﻴﻜﺎﺳﻴﻮﻥﻫﺎ ﻭ ﻧﺤﻮﺓ ﺑﻲﺣﺴﻲ ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢ ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ. : Operative techniquesﺑـﻪ ﺷـﻴﻮﻩﻫـﺎﻱ ﻋﻤـﻞ ﺳـﭙﺘﻮﭘﻼﺳـﺘﻲ ﻭ turbinate surgeryﮔﺮﺍﻓـﺖﻫـﺎ ،Spreadergrafs modified zplasty-Nasalvalve surgery ،ﺟﺮﺍﺣـﻲ osseocartileginousﺭﻳﻨﻮﭘﻼﺳـﺘﻲ ، external rhinoplasty ، Open Wedgeresection in alar base surgeryﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ. : Capita selectaﻓﺼﻞ ﺁﺧﺮ ﺑﻪ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺳﺎﺧﺘﻤﺎﻧﻲ ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ ﻣﺎﻧﻨﺪ ﺗﺼﺤﻴﺢ ﺷﻜﺎﻑ ﻟﺐ ﻭ ﺑﻴﻨﻲ rhinosurgery ، augmentation rhinoplasty ،ﺩﺭ ﻛﻮﺩﻛﺎﻥ Revision surgery ،ﺗﺼﺤﻴﺢ Pverprojected nasel tip. Saddle noseﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ.ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ CDﺁﺳﺎﻥ ﺑﻮﺩﻩ ﻭ ﺩﺍﺭﺍﻱ Video galleryﺷﺎﻣﻞ :ﻧﺸﺎﻥ ﺩﺍﺩﻥ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﻛﻮﺩﻛﺎﻥ ﻭ ﺍﭘﺮﻭﭺﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﺮﺍﻱ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ )ﺍﻛﺴﺘﺮﻧﺎﻝ ﻭ ( ...ﻣﻴﻜﺮﻭﺍﺳﺘﺌﻮﺗﻮﻣﻲ ﻭ Conchal Cartilage harvestingﻣﻲﺑﺎﺷﺪ. ــــــ
)(ROBERT L. SIMONS, MD., NORTH MIAMI BEACH, FLORIDA) (VCD) (CD I , II
GOLDMAN TECHNIQUE
32.2 RHINOPLASTY
ﺩﺭ ﺍﻳﻦ VCDﺁﻣﻮﺯﺷﻲ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻋﻤﻞ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﺳﻴﻤﻮﻥ ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩ ﻣﻴﺎﻣﻲ ﺗﺸﺮﻳﺢ ﻣﻲﺷﻮﺩ .ﻋﻤﺪﻩ ﻫﺪﻑ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﺼﺤﻴﺢ tipﺑﻴﻤﺎﺭ ) (tip plastyﺑﺎ ﻛﻤﻚ ﺗﻜﻨﻴﻚ ﮔﻠﺪﻣﻦ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻓﻮﻕ ﺑﺮﺍﻱ ﺗﺸﺮﻳﺢ ﺗﻜﻨﻴﻚ ﻳـﻚ Caseﻛﻪ ﺧﺎﻧﻢ ٢٧ﺳﺎﻟﻪﺍﻱ ﻣﻲﺑﺎﺷﺪ ﺗﺤﺖ ﻋﻤﻞ ﺑﺎ ﺑﻲﻫﻮﺷﻲ Stand byﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩ .ﺑﻴﻨﻲ ﺑﻴﻤﺎﺭ ﺍﺯ ﻧﻮﻉ projected tipﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺍﺑﺘﺪﺍ ﻳﻚ ﺁﻧﺎﻟﻴﺰ ﻛﺎﻣﻞ ﺍﺳﺘﺎﺗﻴﻚ ﻧﺎﺯﻭﻓﺎﺷﻴﺎﻝ ﺍﺯ ﺑﻴﻤﺎﺭ ﺑﻪ ﻋﻤﻞ ﻣﻲﺁﻳﺪ. ــــــ
)33.2 Rhinoplasty The American Academy of Facial Plastic and Reconstructive Surgery (CD I, II) (E. Gaylon McCollough, M.D.) (the St. Louis Aging Face Symposium
ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﺔ ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ) (E. Gaglon McCollough M.D.ﺩﺭ ﺳﻤﭙﻮﺯﻳﻮﻡ Aging Faceﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ،ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻳﻚ ﻋﻤﻞ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺑﺮ ﺭﻭﻱ ﺑﻴﻤﺎﺭ ﻣﻴﺎﻧﺴﺎﻝ ﺗﺤﺖ ﺑﻲﻫﻮﺷﻲ Stand byﺑﻪ ﺗﻔﻜﻴﻚ ﺑﻴﺎﻥ ﻭ ﺍﺟﺮﺍ ﻣﻲﺷـﻮﺩ .ﺩﺭ ﺍﻳـﻦ ﻋﻤـﻞ ﺍﺯ ﺍﭘﺮﻭﭺ Closedﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺑﻴﺸﺘﺮﻳﻦ ﺗﻮﺟﻪ ﺭﻭﻱ tip plastyﻣﻲﺑﺎﺷﺪ .ﺑﺮ ﺭﻭﻱ tipﺑﻴﻨﻲ ﺍﻳﻦ ﺑﻴﻤﺎﺭ ،ﺍﻓﺰﺍﻳﺶ rotationﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﺍﺯ ﺭﻭﺵ deliveryﺟﻬﺖ ﺗﺮﻣﻴﻢﻛﺮﺩﻥ ﻗﺴﻤﺖ ﺳﻔﺎﻟﻴﻚ ﻏﻀﺮﻭﻑﻫﺎﻱ LLCﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩ. ﺩﺭ ﻧﻬﺎﻳﺖ ﺑﺮﺍﻱ ﺑﻴﻤﺎﺭ Alar base resectionﺍﻧﺠﺎﻡ ﺷﺪﻩ ﻭ ﭘﺎﻧﺴﻤﺎﻥ ﻣﺨﺼﻮﺹ ﻭ ﺟﺎﻟﺐ ﻣﻮﻟﻒ ﺑﺮ ﺭﻭﻱ ﺻﻮﺭﺕ ﺑﻴﻤﺎﺭ ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. )34.2 RHINOPLASTY DOUBLE DOME UNIT (CD I , II) (E. Gaylon McCollough MD, Birmingham, Albama
ــــــ
ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﺔ ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ E. Gaglon MC Collouchﺍﺯ ﺩﺍﻧﺸﮕﺎﻩ ﺑﻴﺮﻣﻨﮕﺎﻡ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ .ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻋﻤﻞ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺑﺮ ﺭﻭﻱ ﺧﺎﻧﻤﻲ ﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩ ﻛﻪ ﻣﺸﻜﻞ ﺁﻥ ﻋﻤﺪﺗﹰﺎ ﺩﺭ ﻧﺎﺣﻴﻪ tipﺑﻮﺩﻩ ﻭ ﻫﺪﻑ ﻋﻤﺪﻩ ﺟﻤﻊ ﻛﺮﺩﻥ ﺁﻥ ﺍﺳﺖ .ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻧﮕﺮﺷﻲ ﺑﻪ Double Dome Unitﻭ ﻧﺤﻮﺓ managementﺁﻥ ﺍﺳﺖ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
14 35.2 Rhinoplasty The Overly Projected Nasal Tip
(Trent W. Smith, M.D.F.A.C.S.)
ــــــ
، ﺑﻴﻨـﻲtip ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﺑﻠﻨﺪﺑﻮﺩﻥ ﻃﻮﻝ ﻣﻮﻳﺎﻝ ﻛﺮﻭﺭﺍﻫﺎ ﺑﻪ ﻋﻨﻮﺍﻥ ﻋﻠﺖ ﺑﺮﭼﺴﺘﻪ ﺑـﻮﺩﻥ. ﺑﺮﺟﺴﺘﻪ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻋﻤﻞ ﺑﺮ ﺭﻭﻱ ﻳﻚ ﺑﻴﻤﺎﺭ ﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩtip ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﺔ ﺁﻣﻮﺯﺷﻲ ﻣﺘﺮﻭﻟﻮﮊﻱ ﻭ ﻧﺘﺎﻳﺞ ﻛﻠﻴﻨﻴﻜﻲ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺩﺭ ﺑﻴﻨﻲﻫﺎﻱ ﺑﺎ . ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﻮﺳﻂ ﺁﻗﺎﻱ ﺩﻛﺘﺮ ﺍﺳﻤﻴﺖ ﺍﺳﺘﺎﺩ ﻭ ﻣﺪﻳﺮ ﮔﺮﻭﻩ ﺑﺨﺶ ﮔﻮﺵ ﻭ ﺣﻠﻖ ﻭ ﺑﻴﻨﻲ ﻭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺩﺍﻧﺸﮕﺎﻩ ﺍﻭﻫﺎﻳﻮ ﺍﺭﺍﺋﻪ ﺷﻮﺩ.ﺗﻼﺵ ﺩﺭ ﺟﻬﺖ ﻛﻮﺗﺎﻩ ﺑﻮﺩﻥ ﻃﻮﻝ ﺁﻧﻬﺎ ﺩﺭ ﺟﻬﺖ ﺍﺻﻼﺡ ﺍﻳﻦ ﺑﺮﺟﺴﺘﮕﻲ ﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩ 36.2 SURGERY of the EAR
2003
(Fifth Edition) (Glasscock-Shambaugh) (Michael E. Glasscock III, MD, FACS, Aina Julianna Gulya, MD)
: ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ. ﻛﺘﺎﺏ ﺷﺎﻣﭙﻮ ﻳﻜﻲ ﺍﺯ ﻣﻌﺘﺒﺮﺗﺮﻳﻦ ﺭﻓﺮﺍﻧﺲﻫﺎﻱ ﺟﺮﺍﺣﻲ ﮔﻮﺵ ﺩﺭ ﺩﻧﻴﺎ ﻣﻲﺑﺎﺷﺪ.( ﺑﻪ ﺷﻤﺎ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ2003) ﺍﻭﻳﺸﻦ ﭘﻨﺠﻢ، ﺟﺮﺍﺣﻲ ﮔﻮﺵ ﺷﺎﻣﭙﻮـ ﮔﻼﺳﻜﻮtextbook . CD ﺩﺭ ﺍﻳﻦ
37.2
1- Scientific Foundations
3- Clinical Evaluation
5- Fundametals of Otologic/Neurotologic Surgery
7- Surgery of the External Ear
2- Surgery of the Tympanomastoid Compartment
4- Surgery of the Inner Ear
6- Surgery of the IAC/CPA/Petrous Apex
8- Surgery of the Skull Base
The MEDPOR Lower Eyelid Spacer (James Patrinely, M.D.F.A.C.S., and Charles N.S. Soparkar, M.D., Ph.D.) (VCD)
ــــــ
. ﺍﻳﻦ ﺁﺷﻨﺎﻳﻲ ﺩﺭ ﻏﺎﻟﺐ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ. ﺷﻤﺎ ﺑﺎ ﭘﺮﻭﺗﺰﻫﺎﻱ ﻣﺪﭘﻮﺭ ﭘﻠﻚ ﺗﺤﺘﺎﻧﻲ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪ، ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﭘﺎﺗﺮﻳﻨﻠﻲ ﻭ ﺩﻛﺘﺮ ﺳﻮﭘﺎﺭﻛﺎﺭ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩVCD ﺩﺭ ﺍﻳﻦ 3) Medpore biomaterial
2) Addressing and management potential Complications - managing winging are edge flare - managing ridging - managing under correction - managing overcorrection - managing implant exposure - managing entropion - managing entropion - Implant exchange
1) Introduction and Surgical technique - Cartilage grafts - Non-rigid spacer grafts (hard Patale/Sclera,dermis) - Medpore Lower Lid Advantages
38.2 The MEDPOR Nasal Shell Implant (Paul O'Keefe, M.B, B.S., (SYD), F.R.C.S., F.R.A.C.S.) (VCD)
ــــــ
39.2 VCD Journal of ENT APPROACH VESTIBULAR NEURECTOMY-TRANSTEMPORAL SUPRALABYRINTHINE APPROACH
ــــــ
MICROSURGERY OF THE SKULL BASE TRANSOTIC APPROACH ACOUSTIC NEUROMA (Prof. U. Fisch Zurich) (VCD#2) 40.2 VCD Journal of ENT INFRATEMPORAL FOSSA APPROACH TYPE C
(Prof. U. Fisch Zurich) (VCD#4)
ــــــ
41.2 VCD Journal of ENT INFRATFMPORAL FOSSA APPROACH GLOMUS TEMPORALE TUMOR (Prof. U. Fisch Zurich) (VCD#1)
ــــــ
42.2 VCD Journal of ENT MICROSURGERY OF THE SKULL BASE TRANSOTIC APPROACH ACOUSTIC NEUROMA-INFRATEMPORAL FOSSA APRROACH TYPE C (Prof. U. Fisch Zurich) (VCD#3)
ــــــ
43.2 VJGS Invited Presentation: Thyroidectomy (Jon A. van Heerden, ND)
ــــــ
44.2 San Diego Classics in Soft Tissue & Cosmetic Surgery Rhinoplasty (Part 1-6) (Richard C. Webster, MD, Terence M. Davidson, Alan M. Nahum)
ﺯﻧﺎﻥ ﻭ ﻣﺎﻣﺎﺋﻲ-٣
CD ﻋﻨﻮﺍﻥ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــــ
1.3
Abdominal Colposacropexy and Vaginal Sacropinus Suspension (Harold P. Drutz MD FRCS (C) (VCD)
2.3
Adapted form Physical Examination and Health Assessment, 2/e (Carolyn Jarvis, RN, C, MSN, FNP) (W.B. Saunders Company) (VCD)
ــــــ
3.3
Advanced Colposcopy: Understanding Vessel Patterns (Dorothy M. Babo, MD) (VCD)
ــــــ
: ﺗﻐﻴﻴﺮ ﻛﻮﻟﭙﻮﺳﻜﻮﭘﻲ ﺑﻪ ﺩﻭ ﻓﺎﻛﺘﻮﺭ ﻣﻬﻢ ﻧﻴﺎﺯ ﺩﺍﺭﺩ: ﺩﺭ ﻣﻮﺭﺩVJOG ﺍﺯ ﺳﺮﻱCD ﺍﻳﻦ ﻭﻳﺪﺋﻮ . ﺩﺍﻧﺶ ﺍﻟﮕﻮﻫﺎﻱ ﻧﺮﻣﺎﻝ ﻳﺎ ﺍﺑﻨﺮﻣﺎﻝ ﺳﺮﻭﻳﻜﺲ-٢ ﻧﮕﺮﺵ ﺩﻗﻴﻖ-١ ( ﻭ ﺍﻓﺘﺮﺍﻕ ﺁﻧﻬﺎ ﺍﺯ ﻳﻜﺪﻳﮕﺮ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺿﺎﻳﻌﺎﺕ ﻫﻤﺮﺍﻩ ﺑﺎ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲ ﻭ ﺍﺳﻼﻳﺪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖ ﺩﺭ ﻗﺴـﻤﺖ ﺁﺧـﺮ..... ﻛﺮﺍﺗﻴﻦ ﻭ،ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﻓﻴﺰﻳﻚ ﺩﺳﺘﮕﺎﻩ ﻭ ﺳﭙﺲ ﻋﻮﺍﻣﻠﻲ ﻛﻪ ﺩﺭ ﻣﺸﺎﻫﺪﻩ ﺿﺎﻳﻌﺎﺕ ﻣﻮﺛﺮ ﺍﺳﺖ )ﻣﺎﻧﻨﺪ ﺑﺎﺯﺗﺎﺏ ﻧﻮﺭ ﺗﻮﺳﻂ ﻣﻮﻛﻮﺱ .ﺭﻭﺵ ﻛﺎﺭﻛﺮﺩﻥ ﺻﺤﻴﺢ ﺑﺎ ﻛﻮﻟﭙﻮﺳﻜﻮﭖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
15 Advanced Therapy of BRAST DISEASE (S. Eva Singletry, MD, Geoffrey L. Robb, MD) 5.3 American Cancer Society Atlas of Clinical Oncology (Cancer of the Female Lowe Genital Tract) (Patricia J. Eifel, M.D. Charles Levenback, M.D.)
2000
4.3
(SALEKAN E-BOOK)
2001
Cervix ﺁﺧﺮﻳﻦ ﺗﻐﻴﻴﺮﺍﺕ ﺩﺭ ﺩﺭﻣﺎﻥﻫﺎﻱ ﭘﺬﻳﺮﻓﺘﻪﺷﺪﻩ ﺑﺮﺍﻱ ﻛﺎﻧﺴﺮ ﻣﻬﺎﺟﻢ. ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺩﺭﻣﺎﻥ ﻛﺎﻧﺴﺮﻫﺎ ﺩﺳﺘﮕﺎﻩ ﺗﻨﺎﺳﻠﻲ ﺗﺤﺘﺎﻧﻲ ﺯﻧﺎﻥ ﻣﻲﺑﺎﺷﺪ، ﺗﺸﺨﻴﺺ،ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ﺑﻪ ﻣﻨﻈﻮﺭ ﻓﺮﺍﻫﻢﻛﺮﺩﻥ ﻣﺮﻭﺭ ﻭ ﺁﻧﺎﻟﻴﺰ ﺑﻴﻮﻟﻮﮊﻱ
.ﻭ ﻳﻚ ﺑﺎﺯﻧﮕﺮﻱ ﻛﻠﻲ ﺩﺭ ﻫﻤﻪ ﻣﺒﺎﺣﺚ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺷﺪﻩ ﺍﺳﺖ 17- Chemotherapy in Curative Management
13- Surgery for Vulvar Cancer
18- Post-treatment Surveillance
14- Radiation Therapy for Vulvar Cancer
19- Palliative Care
15- Acute Effects of Radiation Therapy 16- Late Complications of Pelvic Radiation Therapy
6.3
9- Surgical Treatment of Invasive Cervical Cancer 10- Radiation Therapy for Invasive Cervical Cancer 11-Radical Management of Recurrent Cervical Cancer
5- Diagnostic Imaging
1- Epidemiology
6- Screening for Neoplasms
2- Pathology
7-Treatment of Squamous Intraepithelial Lesions
3- Molecular Biology
12- Management of Vaginal Cancer
8- Invasive Carcinoma of the Cervix
4- Anatomy and Natural History
Atlas of Clinical oncology Breast Cancer (American Cancer Society ) (David J Winchester, MD, David P Winchester, MD)
2000 : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ
yGenetics, Natural History, and DNA-Based Genetic Counseling in Hereditary Brast Cancer
y Breast Cancer Risk and Management: Chemoprevention, Surgery, and Surveillance
y Screening and Diagnostic Imaging yImaging-Directed y Breast Biopsy yHistophathology of Malignant Breast Disease yUnusual Breast Pathology y Prognostic and Predictive Markers in Breast Cancer y Surgical Management of Ductal Carcinoma In Situ yEvaluation and Surgical Management of Stage I and II Breast Cancer y Locally Advanced Breast Cancer y Breast Reconstruction
7.3
ATLAS OF ENDOSCOPIC TECHNIQUES IN GYNECOLOGY (First Edition) (Jeffrey M. Goldberg, MD, Tommaso Falcone, MD) (©W.B. Saunders, Philadelphia)
2001
:ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ 1234-
8.3 9.3
Instrumentation and Pelvic Anatomy Surgery for Pelvic Support Ovarian Surgery Hysteroscopic Surgery
5- Patient Preparation 6- Surgery for Endometriosis and Pelvic Pain 7- Complications
8- Tubal Surgery 9- New Procedures 10- Uterine Surgery
Atlas of Gynecologic Surgery (3rd edition) (H.A. Hirsch, M.D., O. Käser, M.D., F.A. Iklé, M.D.) (Thieme) Atlas of Transvaginal Surgery (Second Edition) (©W.B. Saunders, Philadelphia) (VCD) - Prolene sling in the treatment of stress incontinence - Transvaginal repair of enterocele and vault prolapse - Excision of urethral diverticula
10.3 COLPOSCOPY
an Interactive
CD-ROM
- Fibro-fatty labial flap (Martius Flat) for vaginal reconstruction - Transvaginal repair of vesico-vaginal fistula using a peritoneal flap - Transvaginal repair of posterior vaginal wall prolapse
(SALEKAN E-BOOK)
- Transvaginal hysterectomy for severe prolapse - Transvaginal repair of grade IV cystocele
(Thomas V. Sedlacek, MD, Charles J. Dunton, MD)
ــــــ 2001
ــــــ
11.3 Core Curriculum in Primary Care Patient Evaluation for Non-Cardiac Surgery and Gynecology and Urology (Michael K. Rees, MD, MPH)
ــــــ
ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳـﻦ. ﺯﻧﺎﻥ ﻭ ﺍﻭﺭﻭﮊﻱ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖ، ﺣﺎﺿﺮ ﺩﺭ ﻣﻮﺭﺩ ﺟﺮﺍﺣﻲCD . ﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖHarvard ﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻧﮓ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲCD ﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯCCC ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻـﻮﺭﺕ ﻳـﻚ ﻣﻘﺎﻟـﻪ ﭼـﺎﭘﻲ ﺩﺭ. ﺳﺆﺍﻻﺕ ﻣﺮﺑﻮﻃﻪ ﺑﻪ ﺻﻮﺭﺕ ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ، ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜﻲ.ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛﺎﺭﺑﺮ ﻣﻲﺑﺎﺷﺪ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ.ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﭼﮕﻮﻧﻪ ﻳﻚ ﺑﻴﻤﺎﺭ ﺭﺍ ﺑﺮﺍﻱ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ )ﺑﺠﺰ ﺟﺮﺍﺣﻲ ﻗﻠﺐ( ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺁﻣﺎﺩﻩ ﻛﻨﻴﻢ؟-١ Male impotence ﻋﻘﻴﻤﻲ ﻣﺮﺩﺍﻥ-٣ .(AUB) ﺍﺭﺯﻳﺎﺑﻲ ﺧﻮﻧﺮﻳﺰﻱﻫﺎﻱ ﺍﺑﻨﺮﻣﺎﻝ ﺭﺣﻢ-٢ 12.3 Core Curriculum in Primary Care Gynecology
(Michael, Isaac Schiff, Keith, Thomas, Annekathryn)
13.3 Danforth's Obstetrics and Gynecology
ــــــ
(James R. Scott) (9 Edition) (SALEKAN E-BOOK) Diagnosis of Benign Breast Disease (Dorothy M. Barbo, MD) (VCD) Submitted Subject The Limits of Laparoscopy: Diapharbmatic Endometriosis (David B. Redwine, MD) 14.3 .( ﻣﻲﺑﺎﺷﺪVideo Journal ob/Gyn) VJOG ﺍﺯ ﺳﺮﻱCD ﺍﻳﻦ ﻭﻳﺪﺋﻮ ﺍﺑﺘﺪﺍ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﺳﭙﺲ ﻃﺮﺯ ﻣﻌﺎﻳﻨﻪ ﻭ ﺍﻓﺘﺮﺍﻕ ﺿﺎﻳﻌﺎﺕ ﺧﻮﺵﺧﻴﻢ ﺍﺯ ﺑﺪﺧﻴﻢ ﺍﺯ ﻃﺮﻳﻖ ﺷﺮﺡ ﺣﺎﻝ ﺑﺎﻟﻴﻨﻲ ﻭ ﻣﺎﻣﻮﮔﺮﺍﻓﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺳﭙﺲ ﺷﻜﺎﻳﺎﺕ ﺷﺎﻳﻊ ﺑﻴﻤﺎﺭﺍﻥ ﺑﻴﺎﻥ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺑﺼﻮﺭﺕ ﺍﻟﮕﻮﺭﻳﺘﻢ ﻃﺮﺯ ﺑﺮﺧﻮﺭﺩ ﻭ ﺍﻧﺠﺎﻡ ﺁﺯﻣﺎﻳﺸﺎﺕ ﻣﺮﺑﻮﻃﻪ ﺩﺭ ﻣﻮﺭﺩCD ﺍﻳﻦ ﻭﻳﺪﺋﻮ.١ . ﺑﻴﻤﺎﺭ ﺑﺎ ﺍﻧﺪﻭﻣﺘﺮﻳﻮﺯ ﻧﺎﺣﻴﻪ ﺩﻳﺎﻓﺮﺍﮔﻢ ﺑﺤﺚ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ٢ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ. ﺩﺭ ﻣﻮﺭﺩ ﻣﺤﺪﻭﺩﻳﺖﻫﺎﻱ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖCD ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ.٢ . ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖSolid ﻭ ﻳﻚ ﺗﻮﺩﻩCyst ﻭnipple discharge ، Mastodynia ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2003 ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
16 )(Suttond & diamond) (second Edition
ــــــ
)(Michael Dixon, Richarc Sainsbury) (Salekan E-book
ــــــ
15.3 Endoscopic Surgery for Gynecologists
)16.3 Handbook of disease of the breast (Second Edition
)17.3 INTERACTIVE COLOR GUIDES Obstetrics Gynecology Neonatology (David James, Mary Pillai, Janice Rymer, Andrew N. J. Fish, Warren Hye
ــــــ ﻋﻨﺎﻭﻳﻦ ﻣﻮﺟﻮﺩ ﺩﺭ
ﺍﻳﻦ CD
ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ:
9. Skin Disorders 10. Low-Birth-Weight Infants
7. Iatrogenic Lesions 8. Surgical Problems
)(Dr G. F. Stohs, MD & Dr. L. P. Johonson, MD
ــــــ
3. Birth Trauma 4. Syndromes
5. Deformations 6. Infection
1. Normal Infant 2. Congennital Abnormalities
?18.3 LAVM: Our First one Hundred Cases; What have We Learned
ﺍﻣﺮﻭﺯﻩ ﻫﻴﺴﺘﺮﻛﺘﻮﻣﻲ ﺑﻪ ﻃﺮﻳﻘﻪ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﻓﺮﺍﮔﻴﺮ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ CDﻣﻮﺭﺑﻴﺪﻳﺘﻲ ﻭ ﻣﻮﺭﺗﺎﻟﻴﺘﻲ ﻭ ﻋﻮﺍﺭﺽ ﺍﻳﺠﺎﺩ ﺷﺪﻩ ﺑﺎ ﺍﻳﻦ ﺭﻭﺵ ﺣﻴﻦ ﻋﻤﻞ ﺩﺭ ١٠٠ﺑﻴﻤﺎﺭ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ.
)Nine Month Miracle (A.D.A.M. Software, Inc.
ــــــ
3. A Child's View of Pregnancy
2. The Family Album
1. Anatomy
19.3
20.3 Obstetric Ultrasound Principles and Techniques
ــــــ
ﺩﺭ ﺍﻳﻦ CDﻣﻄﺎﻟﺐ ﺟﺎﻣﻊ ﻭ ﺍﺭﺯﻧﺪﻩﺍﻱ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﻬﺎﺭﺕﻫﺎﻱ ﻻﺯﻣﻪ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻣﺎﻣﺎﺋﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﻛﻪ ﻋﻨﺎﻭﻳﻦ ﺁﻥ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﻴﻴﻦ ﺳﻦ ﺣﺎﻣﻠﮕﻲ ﺑﺮ ﺍﺳﺎﺱ ﻣﻌﻴﺎﺭﻫﺎﻱ FL . BPDﻭ ACﻭ HCﻭ ﺟﺪﺍﻭﻝ ﺁﻧﻬﺎ ﺑﺮﺭﺳﻲ ﺁﻧﺎﺗﻮﻣﻲ ﺟﻨﻴﻦ ﻭ ﺁﻧﻮﻣﺎﻟﻲﻫﺎﻱ CNSﻭ Body ﺁﻧﺎﺗﻮﻣﻲ ﺭﺣﻢ ﻭ ﺁﺩﻧﻜﺲﻫﺎ ﻭ ﺍﻣﺒﺮﻳﻮ ﻭ ﻛﻴﺴﻪ ﺯﺭﺩﻩ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺑﺮ ﺍﺳﺎﺱ Gsﻭ CRLﻭ ﻧﺤﻮﺓ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻧﻬﺎ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ ﺑﺮ ﺍﺳﺎﺱ ﺩﻭﺭ ﺳﺮ ﻭ ﻧﺤﻮﻩ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻥ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ ﺑﺮ ﺍﺳﺎﺱ FLﻭ ACﻭ ﻧﺤﻮﻩ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻧﻬﺎ ﺗﻌﻴﻴﻦ ﻣﺤﻞ ﺟﻔﺖ ﻭ ﺣﺠﻢ ﻣﺎﻳﻊ ﺁﻣﻨﻴﻮﺗﻴﻚ ﻣﻄﺎﻟﺐ ﺟﺎﻟﺒﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺁﻧﺎﺗﻮﻣﻲ ﺟﻨﻴﻦ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ )ﻣﻌﺪﻩ -ﻛﻠﻴﻪ (........ ﺗﻌﻴﻴﻦ ﻣﺤﻞ ﻻﻧﻪﮔﺰﻳﻨﻲ ﺟﻔﺖ ﻭ ﺑﺮﺭﺳﻲ ﺭﻛﻮﻟﻤﺎﻥ ﻭ ﭘﻼﻧﺘﺎﭘﺮﻭﻳﺎ ﺍﻧﻔﺎﺭﻛﺘﻮﺱ ﻭ ﻭﺍﺭﻳﺎﺳﻴﻮﻥ ﻣﺤﻞ ﺧﺮﻭﺝ ﺑﻨﺪ ﻧﺎﻑ )(Cord Insertion ﺑﺮﺭﺳﻲ ﻟﻜﻴﻨﻴﻜﺎﻝ ﻭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ Case Studyﻭ ﻣﻄﺮﺡﻛﺮﺩﻥ ﺳﺆﺍﻻﺕ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺁﻧﻬﺎ ﻭ ﭘﺎﺳﺦ ﻣﺮﺑﻮﻃﻪ ﺗﻮﺿﻴﺤﺎﺗﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ) BPPﺑﻴﻮﻓﻴﺰﻳﻜﺎﻝ ﭘﺮﻭﻓﺎﻳﻞ(21.3 Operative Obstetrics
)(Larry C. Gilstrap III) (2nd Edition) (SALEKAN E-BOOK )22.3 Safety principles for surgical techniques in minimally invasive gynecologic surgery (Dr. Samir Sawalhe) (CD I , II )(Equipment, preparation, positioning, approach alternatives, safe entry, nots on application
ــــــ ــــــ
5. Electrical morcellation
4. Approach alternatives
3. Disinfection/preparation
2. Positioning
1. Instruments/equipment
)23.3 Single Puncture Laparoscopic Technique (Marco Pelosi, MD) (VCD
ــــــ
ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ CDﺭﻭﺵ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺑﻪ ﺻﻮﺭﺕ Single punctureﺗﻮﺻﻴﻒ ﮔﺮﺩﻳﺪﻩ ﻭ ﺷﺮﺍﻳﻂ ﺍﻃﺎﻕ ﻋﻤﻞ ،ﻃﺮﻳﻘﻪ ﻭ ﻭﺳﺎﺋﻞ ﻋﻤﻞ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﻭ ﺳﭙﺲ ﻣﺰﺍﻳﺎ ﺍﻳﻦ ﺭﻭﺵ ﺑﻪ ﻧﻮﻉ multiple punctureﺑﻴﺎﻥ ﻣﻲﮔﺮﺩﺩ. )(Frances R. Batzer, MD
ــــــ
24.3 Submitted Subject: Transvaginal Sonographic Assessment of Pelvic Pathology: Preoperative Evaluation
ﺍﻳﻦ ﻭﻳﺪﺋﻮ CDﺍﺯ ٣ﺑﺨﺶ ﺯﻳﺮ ﺗﺸﻜﻴﻞ ﺷﺪﻩ ﺍﺳﺖ: )ﻓﻴﻠﻢ ﺍﻭﻝ( :ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺑﺤﺚ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺷﺮﺡ ﺣﺎﻝ ٦ﺑﻴﻤﺎﺭ ﺑﻴﺎﻥ ﺷﺪﻩ ﻭ ﺑﺎ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺗﺸﺨﻴﺺ ﻭ ﻣﺤﻞ ﺩﻗﻴﻖ ﺿﺎﻳﻌﺎﺕ ﻟﮕﻦ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺳﭙﺲ ﺑﺎ ﻫﻴﺴﺘﺮﺳﻜﻮﭘﻲ ﻭ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺿﺎﻳﻌﺎﺕ ﺟﺮﺍﺣﻲ ﻣﻲﮔﺮﺩﺩ Case .ﻫﺎﻱ ﺳﻄﺮ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ:
ﺧﺎﻧﻢ ٤٢ﺳﺎﻟﻪﺍﻱ ﺑﻪ ﻣﻨﻮﻣﺘﺮﻭﺭﺍﮊﻱ ﺑﻪ ﻣﺪﺕ ٢ﺳﺎﻝ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ﺳﺎﺏ ﻣﻮﻛﻮﺱ ﻓﻴﺒﺮﻭﻥ ← -١ﺧﺎﻧﻢ ٢٤ﺳﺎﻟﻪﺍﻱ ﺑﺎ ﺗﺎﺭﻳﺨﭽﻪ ﺧﺘﻢ ﺣﺎﻣﻠﮕﻲ ﻣﻜﺮﺭ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ← Septate uterusﺩﺭﻣﺎﻥHysteroscopic Resection : ﺩﺭﻣﺎﻥ
-٢ -٣ -٤ -٥ -٦
←
ﻫﻴﺴﺘﺮﻭﺳﻜﻮﭘﻴﻚ resection
ﺧﺎﻧﻢ ٣٦ﺳﺎﻟﻪ ﺑﺎ ﺗﺎﺭﻳﺨﭽﻪ ﺍﻧﺪﻭﻣﺘﺮﻳﻮﺯ ﻭ ﺩﺭﺩ ﻧﺎﮔﻬﺎﻧﻲ ﻭ ﺵ ﺩﻳﺪ ﻧﺎﺣﻴﻪ ﻟﮕﻦ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ﺍﻧﺪﻭﻣﺘﺮﻳﻮﻣﺎ ← ﺩﺭﻣﺎﻥ :ﺑﺮﺩﺍﺷﺘﻦ ﻛﻴﺴﺖ ﺑﺎ ﻻﭘﺎﺭﺍﺳﻜﻮﭖ ﺑﺎ ﻟﻴﺰﺭﻱ YA ﺧﺎﻧﻢ ٤١ﺳﺎﻟﻪ ﺑﺎ ﺩﺭﺩ ﻧﺎﺣﻴﻪ ﻟﮕﻦ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ﺩﺭﻣﻮﺋﻴﺪ ← Cystﺩﺭﻣﺎﻥ :ﺑﺮﺩﺍﺷﺘﻦ ﺩﺭﻣﻮﺋﻴﺪ ﻛﻴﺴﺖ ﺑﺎ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺧﺎﻧﻢ ٤٣ﺳﺎﻟﻪ ﺑﻄﻮﺭ ﺍﺗﻔﺎﻗﻲ ﻣﺘﻮﺟﻪ ﺑﺰﺭﮔﻲ ﺗﺨﻤﺪﺍﻥ ﻳﻜﻄﺮﻑ ﻣﻲﺷﻮﺩ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ﻓﻮﻟﻴﻜﻮﻝ ﺩﺭ ← Cystﺩﺭﻣﺎﻥ :ﺑﺮﺩﺍﺷﺘﻦ ﺿﺎﻳﻌﻪ ﺑﺎ ﻻﭘﺎﺭﺍﺳﻜﻮﭖ
ﺧﺎﻧﻢ ٢١ﺳﺎﻟﻪﺍﻱ ﺑﺎ ﺧﻮﻧﺮﻳﺰﻱ ﻣﺪﺍﻭﻡ ﻭ ٣ LMPﻫﻔﺘﻪ ﻗﺒﻞ ﺗﺸﺨﻴﺺ ←
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ectopicpregnancy
← ﺩﺭﻣﺎﻥ:
Left Salpingectomy
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
17 :()ﻓﻴﻠﻢ ﺩﻭﻡ Limiting Physician Exposure to Hepatitis B and HIV : Ob / Gyns
(R.Viscarello.MD)
. ﺩﺭ ﺗﻤﺎﺱ ﻣﻲﺑﺎﺷﺪ ﮔﻔﺘﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺭﺍﻫﻬﺎﻱ ﺻﺤﻴﺢ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻭ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﻭ ﺭﻭﺵﻫﺎﻱ ﭘﻴﺸﮕﻴﺮﻱ ﺩﺭ ﻣﻄﺐ ﻣﺘﺨﺼﺼﻴﻦ ﺯﻧﺎﻥ ﻭ ﺯﺍﻳﻤﺎﻥ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖHIV ﻳﺎHBV ﺭﺍﻩﻫﺎﻱ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﺩﺭﻣﺎﻥ ﻓﺮﺩﻱ ﻛﻪ ﺑﺎCD ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ :()ﻓﻴﻠﻢ ﺳﻮﻡ Laparoscopic Retropubic Colposuspension For Stress urinary incontinence
(Gordon. D. Davis, MD. & R.W.Lobel,MD
. ﺑﻄﺮﻳﻘﻪ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖStress incontinence ﻃﺮﻳﻘﻪ ﺍﺻﻼﺡCD ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ :()ﻓﻴﻠﻢ ﭼﻬﺎﺭﻡ Bi-polar Desiccation of Vascular Tissue: Laparoscopic Hysterectomy
(Paul, D. Indman,MD)
. ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖbi-polar desiccation ﺩﺭ ﺍﻳﻦ ﻓﻴﻠﻢ ﻃﺮﻳﻘﻪ ﺑﺮﺩﺍﺷﺘﻦ ﭘﺎﻳﻪﻫﺎﻱ ﻋﺮﻭﻗﻲ ﻛﻮﭼﻚ ﻭ ﻣﺘﻮﺳﻂ ﺩﺭ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺗﻮﺳﻂ 1999
25.3 TEXT AND ATLAS OF Female in Fertility Surgery (ROBERT B. HUNT) (Third Edition) (Mosby) (SALEKAN E-BOOK)
:ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ BASIC SCIENCE
ENERGY SOURCES
RADIOLOGIC PROCEDURES
HYSTEROSCOPY
LAPAROSCOPY
LAPAROTOMY
ENDOMETRIOSIS
ADDITIONAL CONSIDERATIONS
2002
26.3 Triplet Pregnancies and their Consequences (Louis G. Keith, MD, Isaac Blickstein, MD) (SALEKAN E-BOOK) Epidemiology and biology
Antepartum considerations
Delivery/birth considerations
The Matria database
Short-term outcomes
Prenatal diagnosis
Long-term outcomes
Preventive measures
Miscellaneous
Future dicections
Sources of information on multiple births
27.3 TVT Tension-free Vaginal – Tape
ــــــ : ﺍﺯ ﺑﺨﺶ ﺯﻳﺮ ﺗﺸﻜﻴﻞ ﺷﺪﻩ ﺍﺳﺖCD ﺍﻳﻦ
Stress Incontinence
Anatomy&Terminology
Tension-free Vaginal Tape
Indication&Patient Selection
TVT Procedure
Clinical Information
Sales Support
28.3 Urogynecology: Evaluation and Treatment of Urinary Incontinence (Bruce Rosenzweig, MD, Jeffrey S. Levy, MD, Donald R. Ostergard, MD)
ــــــ
. ﻭﺟﻮﺩ ﺩﺍﺭﺩCD ﻼ ﺭﻧﮕﻲ ﺑﻮﺩﻩ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﺑﻪ ﺻﻮﺭﺕ ﻧﻮﺷﺘﺎﺭﻱ ﻭ ﻓﺎﻳﻞ ﺻﻮﺗﻲ ﻛﻪ ﺑﺮ ﺭﻭﻱ ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﺍﻳﻦ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﺗﺼﺎﻭﻳﺮ ﻛﺎﻣ ﹰCD ﺍﻳﻦ : ﻗﺴﻤﺖ ﻣﺠﺰﺍ ﺩﺍﺭﺩ ﺷﺎﻣﻞ٤ Urogynechology Consideration for the OB/GYN Generalist
-
won surgical & surgical Management
-
Evaluation -
:ﺍﻳﻦ ﻗﺴﻤﺖ ﺧﻮﺩ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ Types of incontinernce y
incontinence awareness y
Patient misconceptions y
Introduction Definigg Incontinence
-
:Introduction & Defining Incontince (١ affected women y
incontince ﺗﺸﺨﻴﺺy
:incontinency ( ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺎ٢ Cystoscopy y uroflowmetry y Postvoid residual y Cystometrogram y Pad test y ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲy ﺗﺎﺭﻳﺨﭽﻪy Voiding diary y un , u/s y Pessary test y Multi-Channel urodynamics y
: Stress urinary incontinence ( ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﺟﺮﺍﺣﻲ ﻭ ﻏﻴﺮ ﺟﺮﺍﺣﻲ ﺩﺭ٣ .( ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ.... ﻭfunetional electrieal Stimalation ﻭ ﺩﺭﻣﺎﻥﻫﺎﻱ ﺩﺍﺭﻭﺋﻲbiofeedback, Beharioral modification)) ﺍﻳﻦ ﻗﺴﻤﺖ ﺷﺎﻣﻞ ﺍﻟﮕﻮﺭﻳﺘﻢ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻣﻲﺑﺎﺷﺪ ﻭ ﺳﭙﺲ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻏﻴﺮﺟﺮﺍﺣﻲ . ﺍﻳﻦ ﺭﻭﺵﻫﺎ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖComplication ﺩﺭ ﻗﺴﻤﺖﻫﺎﻱ ﺑﻌﺪﻱ ﻣﻘﺎﻳﺴﻪ ﺩﺭﺻﺪ ﻣﻮﻓﻘﻴﺖ ﺭﻭﺵﻫﺎ ﺫﻛﺮ ﺷﺪﻩ ﻭ ﺩﺭ ﺁﺧﺮ. ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖProcedure ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵﻫﺎﻱ ﺍﻧﺠﺎﻡ ﺟﺮﺍﺣﻲ ﺑﺤﺚ ﺷﺪﻩ ﻭ ﺳﭙﺲ:ﺭﻭﺵﻫﺎﻱ ﺟﺮﺍﺣﻲ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
18 : Consideration for the OB/Gyn Generalist (٤ ﺩﺭ ﺍﻳﻦ ﻓﺼﻞ: urogynechology as a subdiscipline y eystometry y
professional consideration y
Non surgical therapy y
Urodynamics y
incontinrence management to private patients y
Set-up requirement y
equipment cost y
Allied Staff y
ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ.
ــــــ
)29.3 Video Journal of Gynecology (Vaginal Hysterectomy Wedge morcellization Technique for the Large Uterus) (The Infertile Couple) (David Olive, MD, George W. Morley MD,
ــــــ
)30.3 WOMEN'S HEALTH (MOSBY'S PRIMARY CARE
2003
ﺍﻳﻦ CDﺷﺎﻣﻞ Procedureﻫﺎﻱ ﺳﺮﭘﺎﺋﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺯﻧﺎﻥ ﻭ ﺩﺳﺘﮕﺎﻩ ﮊﻧﻴﺘﺎﻟﻬﺎﻱ ﺯﻧﺎﻥ ) (Female Genitaliaﻭ ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ Female Genitiourinary Tractﻣﻲﺑﺎﺷﺪ. ﺩﺭ ﻫﺮ ﻓﺼﻞ ﻋﻼﻭﻩ ﺑﺮ ﺭﻭﺵ ، Lﺁﻧﺎﺗﻮﻣﻲ ،ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ Lﻭ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ﻭ ﻋﻮﺍﺭﺽ ﻭ ﺗﺴﺖﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﻭ ﻏﻴﺮﻩ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ. ﺧﺼﻮﺻﻴﺖ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮﺩ ﺍﻳﻦ CDﺷﺎﻣﻞ :ﻧﺸﺎﻥ ﺩﺍﺩﻥ ﺗﻤﺎﻡ ﺭﻭﺵﻫﺎ ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢﻫﺎﻱ ﻭﻳﺪﺋﻮﺋﻲ ﺩﺭ CDﻭ ﺩﻳﮕﺮ CNGﻳﺎ ﺗﺴﺖﻫﺎﻱ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺑﺨﺶ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ: ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ : Breast examination -١ﺷﺎﻣﻞ :ﺁﻧﺎﺗﻮﻣﻲ ،ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ،ﺗﺠﻬﻴﺰﺍﺕ ،ﺁﻣﻮﺯﺵ ﺑﻪ ﺑﻴﻤﺎﺭ ،ﻓﺮﻡ ﺭﺿﺎﻳﺖ ﻧﺎﻣﻪ Pojition ،ﺑﻴﻤﺎﺭ ﺗﻜﻨﻴﻚ ﻭ ﺛﺒﺖ ﻳﺎﻓﺘﻪﻫﺎ ﻭ ﭘﺮﻭﻧﺪﻩ ﻭ ﺍﺷﻜﺎﻻﺕ ﺗﻜﻨﻴﻜﻲ ،ﺗﺸـﺨﻴﺺ ﺍﻓﺘﺮﺍﻗـﻲ ﻭ quizﺍﻧﺘﻬـﺎﻱ ﺑﺨـﺶ ﻣﻲﺑﺎﺷﺪ ﺗﻤﺎﻡ ﻣﺮﺍﺣﻞ ﺑﺎﻳﺪ ﺑﻪ ﺻﻮﺭﺕ ﺗﻤﺎﺱﻫﺎﻱ ﺭﻧﮕﻲ ﻭ ﻓﺎﻳﻞﻫﺎﻱ ﻭﻳﺪﻳﻮﺋﻲ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﺍﺳﺖ : Colposcopy -٢ﺍﺑﺘﺪﺍ ﺁﻧﺎﺗﻮﻣﻲ cervixﺑﺎ ﺷﻜﻠﻬﺎﻱ ﺗﻤﺎﻡ ﺭﻧﮕﻲ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﻻﺯﻡ ﺩﺭ ﻣﺘﻦ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺳﭙﺲ ﺩﺭ ﻣﻮﺭﺩ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻧﺎﺣﻴﻪ ﺳﺮﻭﻛﻴﻞ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﺑﺎ ﺁﻣﻮﺯﺵ ﺑﻪ ﺑﻴﻤﺎﺭ ﺗﺠﻬﻴﺰﺍﺕ ﻻﺯﻡ ، Positioning ،ﺁﻣﺎﺩﻩ ﻛﺮﺩﻥ ﻣﺤﻞ ،ﺁﻧﺴﺘﺰﻱ ،ﺗﻜﻨﻴﻚ ﺍﻧﺠﺎﻡ Procedneﻭ ﻛﻤﭙﻴﻜﺎﺳﻴﻮﻥ ،ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻭ ﺗﻐﻴﻴﺮ ﻧﺘﺎﻳﺞ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺩﺭ ﺁﺧﺮ ﻓﺼﻞ Quizﻭﺟﻮﺩ ﺩﺍﺭﺩ ٧ .ﻓﻴﻠﻢ ﺩﺭ ﻣﻮﺭﺩ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺠﺎﻡ ﺭﻭﺵ ﻛﻮﭘﻴﻮﺳﻜﻮﭘﻲ ﺩﺭ ﺍﻳﻦ ﻓﺼﻞ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. -٣ﺍﻧﺪﻭﻣﺘﺮﻳﺎﻝ ﺑﻴﻮﭘﺴﻲ :ﺍﺑﺘﺪﺍ ﻭ ﻣﻘﺪﻣﻪ ﺗﺎﺭﻳﺨﭽﻪﺍﻱ ﺍﺯ D&Cﻭ ﺑﻴﻮﭘﺴﻲ ﺁﻧﺪﻭﻣﺘﺮﻳﺎﻝ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﻗﺪﻳﻤﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﺳﭙﺲ ﺁﻧﺎﺗﻮﻣﻲ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺁﻥ ﺑـﻪ ﺗﺼـﺎﻭﻳﺮ ﺭﻧﮕـﻲ ﺷـﺮﺡ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖ.ﺳـﭙﺲ ﻣﺎﻧﻨـﺪ ﺩﻳﮕـﺮ Procedureﻫـﺎ ﺍﻧﺪﻳﻜﺎﺳـﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﻭ ﺗﻜﻨﻴﻚ ،ﺁﻣﺎﺩﮔﻲ ﺑﻴﻤﺎﺭ Position ،ﺑﻴﻤﺎﺭ ،ﺁﻧﺴﺘﺰﻱ ﻭ ....ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺁﺧﺮ ﻓﺼﻞ ﻓﻴﻠﻢﻫﺎﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﺗﺠﻬﻴﺰﺍﺕ ﻭ ﺭﻭﺵﻫﺎﻱ ﺍﻧﺠﺎﻡ ﺑﻴﻮﭘﺴﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺁﺧﺮ ﻓﺼﻞ Quizﻗﺮﺍﺭ ﺩﺍﺭﺩ. : Pelvic Examination -٤ﺑﻌﺪ ﺍﺯ ﻣﻘﺪﻣﻪ ﺩﺭ ﻣﻮﺭﺩ ﺁﻧﺎﺗﻮﻣﻲ ﻧﺎﺣﻴﻪ ﮊﻧﺘﻴﻜﻲ ) (utenes , carivx , vagina , valveﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺠﺎﻡ ﻣﻌﺎﻳﻨﻪ Position،ﺑﻴﻤﺎﺭ ،ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ،ﻛﻨﺘﺮﺍﻳﻜﺎﺳﻴﻮﻥ ﻭ ﺗﻐﻴﻴﺮ ﻳﺎﻓﺘﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻭ ﺳﭙﺲ ٦ﻓﻴﻠﻢ ﻣﻌﺎﻳﻨﻪ ﻟﮕﻨﻲ ﻛﺎﻣﻞ ،ﻣﻌﺎﻳﻨﻪ exetrnalgenifalicnﺑﺎ ﭘﺎﭖ ﺁﺳﻤﻴﺮ ،ﻣﻌﺎﻳﻨﻪ rectovaginal , bimanualﻭ ﭼﮕﻮﻧﮕﻲ ﮔﺬﺍﺷﺘﻦ ﺍﺳﭙﻜﻮﻟﻮﻡ ﻭ ﺗﺠﻬﻴﺰﺍﺕ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺁﺧﺮ Quizﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. : Pap Smear -٥ﺍﺑﺘﺪﺍ ﺑﻌﺪ ﺍﺯ ﻣﻘﺪﻣﻪﺍﻱ ﻛﻮﺗﺎﻩ ﺩﺭ ﻣﻮﺭﺩ ﺁﻧﺎﺗﻮﻣﻲ ﻣﻨﻘﻄﻊ ﻭ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﻪ ﻣﻲﺷﻮﺩ ﺑﺎ ﭘﺎﭖ ﺁﺳﻤﻴﺮ ﺑﺮﺭﺳﻲ ﻛﺮﺩ .ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ،ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ Position ،ﺭﻭﺵ ﺍﻧﺠﺎﻡ ،ﺍﺷﻜﺎﻻﺕ ﺗﻜﻨﻴﻜﻲ ،ﺗﺠﻬﻴﺰﺍﺕ ﻭ ....ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ٥ .ﻓـﻴﻠﻢ ﺍﺯ ﭼﮕﻮﻧﮕﻲ ﻣﻌﺎﻳﻨﻪ ،ﮔﺬﺍﺷﺘﻦ ﺍﺳﻴﻜﻮﻟﻮﻡ ﻭ ﺍﻧﺠﺎﻡ ﭘﺎﭖ ﺍﺳﻤﻴﺮ ﻭ ﺗﺠﻬﻴﺰﺍﺕ ﺁﻥ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ) Vaginal Secretion -٦ﺗﺮﺷﺢ ﻭﺍﮊﻳﻨﺎﻝ( :ﺩﺭ ﺍﻳﻦ ﻣﺒﺤﺚ ﺍﺑﺘﺪﺍ ﻋﻠﻞ ﺗﺮﺷﺢ ﻭﺍﮊﻳﻨﺎﻝ ﻭ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﺁﻥ ﭘﺮﺩﺍﺧﺘﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺳﭙﺲ ﺗﺠﻬﻴﺰﺍﺕ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ،ﭼﮕﻮﻧﮕﻲ ﮔﺮﻓﺘﻦ ﻛﺸﺖ ،ﺍﻧﺠﺎﻡ ﺗﺴﺖ ، KOHﻗﺮﺍﺭ ﺩﺍﺩﻥ ﺗﺮﺷﺤﺎﺕ ﺑﺮ ﺭﻭﻱ slideﻭ ﻣﺸﺎﻫﺪﻩ ﺁﻥ ﺑﺎ ﻣﻴﻜﺮﻭﺳﻜﻮﭖ ﺑﺎ ﻓﻴﻠﻢ ﻭ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ Quizﻧﻴﺰ ﺩﺭ ﺁﺧﺮ ﻓﺼﻞ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. 31.3 UTEROSALPINGOGRAPHY IN GYNECOLOGY (Hysterosalpingography) It's Application in Physiological And Pathological Conditions )(SALEKAN E-BOOK ﺍﻳﻦ CDﺣﺎﻭﻱ ﻣﻄﺎﻟﺐ ﺫﻳﻞ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ Utero Salpingographyﻣﻲﺑﺎﺷﺪ: ﺍﺻﻮﻝ ﻛﻠﻲ ﺩﺭ Uterosalpingography
-ﺳﻘﻂ ﻣﻜﺮﺭ ﻭ ﻗﺎﻋﺪﮔﻲ ﺩﺭﺩﻧﺎﻙ )ﺩﻳﺲ ﻣﻨﻮﺭﻩ(
ﻋﻤﻠﻜﺮﺩ ﺭﺣﻢ ﻭ ﻟﻮﻟﻪﻫﺎﻱ ﻓﺎﻟﻮﭖ -ﺳﻞ ﺗﻨﺎﺳﻠﻲ ﻭ ﻓﻴﺴﺘﻮﻝ ﮊﻧﻴﺘﺎﻝ
ﺁﻧﻮﻣﺎﻟﻲﻫﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ﺭﺣﻢ ﻭ ﻟﻮﻟﻪﻫﺎﻱ ﻓﺎﻟﻮﭖ -ﭘﺎﺗﻮﻟﻮﮊﻱ ﻟﻮﻟﻪﻫﺎﻱ ﻓﺎﻟﻮﭖ ،ﭘﺮﻳﺘﻮﺋﻦ ﻭ ﺗﺨﻤﺪﺍﻥﻫﺎ
-ﺗﻐﻴﻴﺮﺍﺕ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﺭﺣﻢ
ﺩﺭ CDﻓﻮﻕﺍﻟﺬﻛﺮ ﺗﺼﺎﻭﻳﺮ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﻣﺘﻌﺪﺩ ﻭﺍﺿﺤﻲ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ USGﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ. 32.3 Your Pregnancy, Your Newborn The Complete Guide for Expectant and New Mothers
ــــــ
-٤ﻋﻠﻮﻡ ﺁﺯﻣﺎﻳﺸﮕﺎﻫﻲ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــــ
ﻋﻨﻮﺍﻥ CD )(Sixth Edition) (SALEKAN E-BOOK
)(Frances Fischbach
A Manual of Laboratory & Diagnostic Tests
1.4
ﺍﻳﻦ CDﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺪﻩ ﺍﺳﺖ ﻣﺸﺘﻤﻞ ﺑﺮ ١٦ﻓﺼﻞ ﺍﺳﺖ ﻭ ﺷﺎﻣﻞ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: Stool Studies
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
Urine Studies
Blood Studies
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
Diagnostic Testing
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
19 Cbemistry Studies Cytology, Histology, and Genetic Studies Prenatal Diagnosis and Tests of Fetal Well-Being
2.4
Microbiologic Studies Endoscopic Studies Cerebrespinal Fluid Studies
Immunodiagnostic Studies Ultrasound Studies X-ray Studies
Nuclear Medicine Studies Pulmonary Functio and Blood Gas Studies Special Systems, Organ Functions, and Post Mortem Studies
2002
A Slide Atlas of ATHEROSCLEROSIS (Progression and Regression) (Herbert C. Stary) ﻣﻄﺎﻟﻌﻪ ﺍﻳﻦ ﻧﺮﻡ ﺍﻓﺰﺍﺭ ﺑﻪ ﻣﺘﺨﺼﺼﻴﻦ ﭘﺎﺗﻮﻟﻮﮊﻱ. ﺍﺳﻼﻳﺪ ﺗﺨﺼﺼﻲ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﭘﻴﺸﺮﻓﺖ ﻭ ﭘﺴﺮﻓﺖ ﺑﻴﻤﺎﺭﻱ ﺁﺗﺮﻭﺍﺳﻜﻠﺮﻭﺯﻳﺲ ﺩﺭ ﺳﻨﻴﻦ ﻣﺨﺘﻠﻒ ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺭﺍ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﻭ ﺍﻟﻜﺘﺮﻭﻧﻲ ﺑﻪ ﺯﻳﺒﺎﻳﻲ ﺑﻪ ﺗﺼﻮﻳﺮ ﻛﺸﻴﺪﻩ ﺍﺳﺖ۹۴ ﺍﻳﻦ ﻧﺮﻡ ﺍﻓﺰﺍﺭ ﺑﺎ .ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﺗﻮﺻﻴﻪ ﻣﻴﺸﻮﺩ
3.4
2002
th
American Sodiety of Hematology (CD 1-5) (44 Annual Meeting) CD-1: ALL -AML -ASH/ASCO Joint Symposium -Atypical Cellular Disorders CD-2: CLL -CML -CNS Lymphoma -Cutaneous Lymphoma -E. Donnall Thomas Lecture CD-3: Enhancing Physician/Patient Communication Regarding Hematologic Disorders -Ham-Wasserman Lecture -Hematology Grants Workshop -Hypercoagulability: Too Many Tests, Too Much Conflicting Data -Malaria and the Red Cell -Marrow Failure CD-4: Multi[ple Myeloma -Myelodysplastic Syndromes Non-Myeloablative Transplantation -Platelets: Thrombotic Thrombocytopenic -Purpura Plenary Policy Frum CD-5: Presidential Symposium Long-Term Complications
4.4
-Red Cell Antigens as Functional Molecules and Obstacles to Transfusion
-Sickle Cell Disease
-Stem Cell Transplantation: Supportive Care and
-Stem Cells: Hype and Reality Update on Epidemiology and Therapeutics for Non-Hodgkin’s Lymphoma
An Electronic Companion to Microbiology for MajorsTM (Mark L. Wheelis)
ــــــ
Reviw , Test yourself
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ What Are Microorganisms? Classification
5.4
Methods of Microbiology Prokaryotic Cell Struture
Eukaryotic Cell Struture Growth & Reproduction
Metabolism & Energy Microbial Genetics
Gene Regulation Viruses
Microbial Ecology Defenses Againses Infection
Disease
Atlas of HEMATOLOGY
ــــــ : ﺣﺎﻭﻱ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ
1. Examination of Blood Cells
2. Normal Hematopoiesis and Blood Cells
3.Dynamic Cell Morphology
4. Hematolopathology
5. Cluster of differentiation Archive
6. Self-Assessment
6.4
Atlas of Surgical Pathology (Johns Hopkins) (Jonathan I. Epstein, Neera P. Agarwal-Antal, David B. Danner, Kim M. Ruska)
7.4
Atlas of Medical Parasitology (Dr. K. Ghazvini) ﻧﺎﻗﻞ اﻧﮕﻞ و ﺳﯿﮑﻞ زﻧﺪﮔﯽ و ﺗﮑﺜﯿﺮ اﻧﮕﻞ اﺳﺖ ﮐﻪ ﺟﻬﺖ اﺳﺘﻔﺎده ﮔﺮوهﻫﺎی ﻣﺨﺘﻠﻒ رﺷﺘﻪﻫﺎی ﭘﺰﺷـﮑﯽ ﺧﺼﻮﺻـﺎً رﺷـﺘﻪ ﻋﻠـﻮم، ﺿﺎﯾﻌﺎت اﯾﺠﺎدﺷﺪه، ﺗﺼﻮﯾﺮ رﻧﮕﯽ از اﻧﻮاع اﻧﮕﻞﻫﺎی ﺑﯿﻤﺎرﯾﺰای اﻧﺴﺎﻧﯽ ﺷﺎﻣﻞ ﺗﺼﻮﯾﺮ اﻧﮕﻞ2000 ﻧﺮماﻓﺰار ﻓﻮق ﺣﺎوی ﺣﺪود ﻣﺒﺎﺣﺚ ﻣﻄﺮحﺷﺪه در اﯾﻦ ﻧﺮماﻓـﺰار. ﺑﺴﯿﺎری از ﺗﺼﺎوﯾﺮ ﻣﻮﺟﻮد در اﯾﻦ ﻣﺠﻤﻮﻋﻪ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮد ﻣﯽﺑﺎﺷﺪ. ﺗﺼﺎوﯾﺮ ﻣﺠﻤﻮﻋﻪ ﻣﺰﺑﻮر از ﻣﻨﺎﺑﻊ ﻣﺨﺘﻠﻒ ﺟﻤﻊآوری ﮔﺮدﯾﺪه اﺳﺖ ﮐﻪ ﺗﻮﺳﻂ دﮐﺘﺮ ﻗﺰوﯾﻨﯽ ﺑﺎزﻧﮕﺮی و وﯾﺮاﯾﺶ ﮔﺮدﯾﺪه اﺳﺖ.آزﻣﺎﯾﺸﮕﺎﻫﯽ ﻣﻔﯿﺪ اﺳﺖ :ﻋﺒﺎرﺗﻨﺪ از * Heart and Muscles Parasites * Lung Parasites
8.4
* Eye Parasites * Skin Parasites
Basic histology: TEXT & ATLAS IMAGE LIBRARY (Tenth Edition)
* Central Nervous System (CNS) Parasites * Liver and Biliary Tree Parasites
* Gnito-Urinary Parasites * Intestinal Parasites (Helminths)
* Intestinal Parasites (Protozoa)
(Luiz Carlos, Juhqueira, Jose CARNEIRO) (A Division of The McGraw-Hill Companies)
2000
2 - Jose CARNEIRO
1- Luiz Carlos JUNQUEIRA 9.4
* Case reports and updates in parasitology * Blood, Bone Marrow, Spleen Parasites
2003
Biochemical Interactions An electronic companion to: FUNDAMENTALS OF BIOCHEMISTRY (Donald voet, Judith G. voet, charlotte W. Pratt)
(Version 1.02)
1999
: ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﺍﻳﻦ NUCLEOTIDES AND NUCLEIC ACIDS
PROTEINS: PRIMARY STRUCTURE
PROTEIN FUNCTION
LIPIDS
BIOLOGICAL MEMBRANES
MAMMALIAN FUEL METABOLOSM: INTEGRATION AND REGULATION
GLUCOSE CATABOLISM
GLYCOGEN METABOLISM AND GLUCONEOGENESIS
DNA REPLICATION REPAIR, AND RECOMBINATION
PHOTOSYNTHESIS
LIPID METABOLISM
AMINO ACID METABOLISM
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
20 NUCLEOTIDE METABOLISM
NUCLEIC ACID STRUCTURE
CITRIC ACID CYCLE
TRANSLATION
REGULATION OF GENE EXPRESSION
ENZYME KINETICS, INHIBITION, AND REGULATION
INTROCUCTION TO METABOLISM
ELECTRON TRANSPORT AND OXIDATIVE PHOSPORYLATION
PROTEINS: THREE-DIMENSIONAL STRUCTURE
TRANSCRIPTION AND RNA PROCESSING
10.4 BIOLOGY CONCEPTS & CONNECTIONS
(Second Edition) (Richard M. Liebaert) (CAMPBELL.MITCHELL.REECE)
ــــــ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﺍﻳﻦ
1. Introduction: The Sclentific Sindy of Life
3. The Life of the Cell
2. The Evolution of Biological Diversity
4. Animals: Form & Function
11.4 BLOOD PRINCIPLES AND PRACTICE OF HEMATOLOGY
5. Cellular Repoduction & Genetics
7. Concepls of Evolution
6. Plants: Form & Function
8. Ecology
(SECOND EDITION) (ROBERT I. HANDIN SAMUEL E. LUX THOMAS P. STOSSEL)
Part I: Fundamentals of Hmatology: Tools of the trade
Part II: The Hematopoietic System
Part III: Stem Cell Disorders
Part IV: White Blood Cells
Part V: Hemostasis
Part VII: Systemic Disease
Part VIII: Hematologic Therapies
Part VIIII: Appendices
Part VI: Red Blood Cells
12.4 BRS Cell Biology CELL BIOLOGY AND HISTOLOGY (4th edition) (Leslie P. Gartner, James L. Hiatt, Judy M. Strum) (LIPPINCOTT WILLIAMS & WILKINS)
2003
2003
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ Plasma Membrane Connective Tissue Circulatory System The Urinary System Epithelia and Glands
Nucleus Cartilage and Bone Lymphoid Tissue Female Reproductive System Blood and Hemopoiesis
13.4 Cellular & Molecular Neurobiology
Cytoplasm Muscle Endocrine System Digestive System: Oral Cavity and Alimentary Tract Digestive System: Glands
Extracellular Matrix Nervous Tissue Skin Special Senses Comprehensive Exam
(Second Edition)
ــــــ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﺍﻳﻦ
1- Lonotropic and Metabotropic Receptors in Synaptic Transmission and Sensory Transduction
3- Neurons: Excitable and Secretory Cells that Establish Synapses
2- Somato-Dendritic Processing and Plasticity of Postsynaptic Potentials
4- Activity and Developmen of Networks: The Hippocampus as an Example
14.4 Clinical Hematology (A Victor Hoffbrand , John E Pettit) (Mosby) Normal Hemopoiesis and
Blood Cells
Anaemias Blood Transfusion
ــــــ
Leucocyte Abnormialities
Hemostasis and Bleeding Disorders
Bone Marrow Transplantation
Hematological Malignancies Further Reading
Coagulation Disorders Acknowledgements
Bone Marrow in Non-hemopoietic Disease
Parasitic Infections Diagnosed in Blood
15.4 Clinical Immunology
ــــــ
16.4 COMMON PROBLEMS IN CLINICAL LABORATORY MANAGEMENT (Judith A. O'brien, M.S. CLSup (NCA)) (Salekan E-Book)
ــــــ
COMPLYING WITH CLIA '88 MEETING TUBERCULOSIS CONTROL REGULATIONS WRITING MANUALS: THE STANDARD OPERATING PROCEDURE MANUAL (SOPM)
OVERCOMING OSHA'S OBST ACLES THE EXPOSURE CONTROL PLAN PROVIDING AND USING PERSONAL PROTECTIVE EQUIPMENT PASSING PROFICEINCY TEST
OVERCOMING OSHA'S OBSTACLES THE CHEMICAL HYGIENE PLAN WRITING MANUALS: THE GENERAL OPERATING PROCEDURE MANUAL ( GOPM) FULFILING QUALITY CONTROL GUIDELINES
ESTABLISHING A QUALITY ASSURANCE PROGRAM
SURVIVING INSPECTIONS AND ATTAINING ACCREDIANCE
PURSUING PERSONNEL PERSPECTIVES
ENCOURAGING EDUCATION
THE ACQUISTION AND MAINTENANCE OF LABORATORY INSTRUMENTATION
MASTERING FINANCES: BILLING AND CODING
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
TAMING TECHNOLOGY: LABORATORY INFORMATION SYSTEM (LIS) RE-ENGINEERING FOR THE FUTURE: THE CORE LABORATORY, AUTOMATION, OUTREACH NETWORKING, AND THE MILLENNIUM BUG GENERATING LABORATORY NUMBERS: STATISTICS LINEARITY, CALIBRATION, REFERENCE, AND CRITICAL VALUES: CALCULATIONS MANAGING THE PHYSICIAN OFFICE LABORATORY (POL) TAMING TECHNOLOGY: POINT OF CARE TESTING (POCT)
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
21 (A data of multiple choice question in microscopic) (Bloom & Fawcett's) (Second Edition)
17.4 Concise Histology
ــــــ
18.4 Dianostic Hematology
ــــــ
This textbook, 'Diagnostic Hematology: A pattern approach', is accompanied by a CD-ROM with three knowledge-based systems applied to 237 case studies. The 3 knowledge-based systems are: 1. Professor Petrushka for peripheral blood analysis
2. Professor Fidelio for flow cytometry immunophenotyping
3. Professor Belmonte for bone marrow interpretation
19.4 Discover Biology
ــــــ
20.4 Electronic Atlas of Parasitology
(John T. Sullivan)
2000
university of the Incarnate Word
21.4 EMBRYO (CD Color Atlas for Developmental Biology) (Gary C. Schoenwolf) Chapter 1: Frog Embryos
Chapter 2: Chick Embryos
Chapter 3: Pig Embryos
ــــــ Chapter 4: Gametogenesis
22.4 Essential Cell Biology (with the voice of Julie Theriot designed and programmed by Christopher Thorpe)
ــــــ
23.4 Fields Virology (Forth Edition) (Volume 1) (Lippincott Williams & Wilkins)
2001
Section One: General Virology
Chapter 1-22
Section Two: Specific Virus Families Chapter 23-90
24.4 Functional HISTOLOGY WHEATER'S (FOURTH EDITION) (BARBARA YOUNG, JOHN W. HEATH) (ALAN STEVENS JAMES S. LOWE) (PHILIP J. DEAKIN)
ــــــ
25.4 Genetics From Genes to Genomes (Ann Reynolds, Ph.D.) (University of Washington)
2000
5- Gen RegVlation
(... ﺳﻴﮕﻨﺎﻝ ﺗﺮﻧﺴﻼﻛﺸﻦ ﻭ،)ﻛﻨﺘﺮﻝ ﺍﻭﭘﺮﻭﻥ ﻻﻛﺘﻮﺯ 6- Poplations & Evolvtion (... )ﻣﺒﺎﺣﺚ ﺟﻤﻌﻴﺖ ﻭ ﺗﻜﺎﻣﻞ ﻭ ﻓﺮﻛﺎﺵ ﺍﻟﻜﻞﻫﺎ ﻭ ﺩﺭ ﭘﺎﻳﺎﻥ ﻫـﺮ. ﺍﺟﺮﺍ ﮔﺮﺩﺩQuick
3- Molecular Genetice
4- Chromosomes FISH
1- Transmission Genetics
( ﺗﻜﻨﻴﻚ ﻧﻘﺸﻪ ﮊﻥ،)ﻣﺒﺎﺣﺚ ﻛﺎﺭﻳﻮﺗﺎﻳﭗ
2- Gentral Dogma
time
ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﺤﺖ ﺑﺮﻧﺎﻣﺔ... ﻫﻴﭙﺮﻳﺪﺍﺳﻴﻮﻥ ﻛﻠﺮﻧﻴﻨﮓ ﻭ،DVA ﻣﻮﺗﺎﺳﻴﻮﻥ ﻭ ﺗﺮﻣﻴﻢ، ﺍﻟﻜﺘﺮﻭﻓﻮﺭﺯ،PCR، ﻣﻴﺘﻮﺯﻭ ﻣﻴﻮﺯ... ﺗﻮﺟﻪ، ﻣﻜﺎﻧﻴﺴﻢ ﺭﻭﻧﻮﻳﺲ: ﻋﺪﺩ ﻭﻳﺪﺋﻮ ﻛﻠﻴﭗ ﺑﺼﻮﺭﺕ ﺍﻧﻴﻤﻴﺸﻦ ﺍﺯ ﻣﺒﺎﺣﺜﻲ ﻫﻤﭽﻮﻥ٢٧ ﺷﺎﻣﻞCD ﺍﻳﻦ .( ﻣﻲﺑﺎﺷﺪIn teractive) ﻫﻤﭽﻨﻴﻦ ﺩﺍﺭﺍﻱ ﺗﻤﺮﻳﻨﺎﺕ ﺑﺼﻮﺭﺕ ﺩﻭ ﺟﺎﻧﺒﻪ ﻭ ﻓﻌﺎﻝ. ﺩﺍﺭﺍﻱ ﻳﻚ ﻓﺼﻞ ﻣﺮﺑﻮﻁ ﺑﻪ ﺗﻌﺮﻳﻒ ﻭ ﺗﺮﺷﺢ ﻟﻔﺎﺕ ﻣﺸﻜﻞ ﻭ ﺗﺨﺼﺼﻲ ﺍﺳﺖ.ﻓﺼﻞ ﺧﻼﺻﺔ ﻣﺒﺎﺣﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ . ﻣﻮﺟﻮﺩ ﺍﺳﺖ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩCD ﻛﻪ ﺩﺭ ﺧﻮﺩQ.t. ( ﻭ ﻧﺼﺐ ﺑﺮﻧﺎﻣﺔSetup . exe ﻻﺯﻡ ﺍﺳﺖ ﺑﻌﺪ ﺍﺯ ﻧﺼﺐ ﺁﻥ )ﺑﺎ ﺩﻭ ﺑﺎﺭ ﻛﻠﻴﻚ ﻛﺮﺩﻥ ﺑﺮ ﺭﻭﻱCD ﺑﻜﺎﺭ ﺭﻓﺘﻪ ﺍﺳﺖ ﻭ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯCD ﺁﺑﺸﻦﻫﺎﻱ ﻣﺘﻨﻮﻉ ﻭ ﺯﻳﺒﺎﻳﻲ ﺩﺭ ﺍﻳﻦ
26.4 Gram Stain TUTOR
(ANINTERACTIVE TUTORIAL THAT TEACHES THE MICROSCOPIC EXAMINATION OF URINARY SEDIMENT)
ــــــ
(Brad Cookson, MD, PHD, Ajit Limaye, MD, Lydia Matheson, BA) 1. Introduction
2. Morphology
3. Specimen Sites
4. Case Studies 5. Exam
6. Image Atlas
1999
27.4 HISTOLOGY EXPLORER
: ﺩﺭ ﻣﻮﺭﺩ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺑﺤﺚ ﻣﻲﻛﻨﺪCD ﺍﻳﻦ Microscope 3D The Cell Epithelium
Connective Tissue Proper Blood and Bone Marrow The Sketetal Tissues
Nervous Tissue The Circulatory System The Lymphoid Organs
The Digestive System The Respiratory System The Urinary System
The Reproductive System The Mammary Giands The Eye
Glands Muscular Tissue The Skin
The Endocrine Glands The Ear
28.4 HUMAN HISTOLOGY CD-ROM (Alan Stevens. James Lowe)
ــــــ
29.4 Images of Disease An image database for the teaching of Pathology (Nick Hawkins, Mark Dziegielewski)
ــــــ
ﻣـﻮﺭﺩ ﻧﻈـﺮ ﺑـﻪ ﺗﻮﺻـﻴﻒ ﻣﺎﻛﺮﻭﺳـﻜﻮﭘﻲ ﻭ ﻣﻴﻜﺮﻭﺳـﻜﻮﭘﻲ ﺿـﺎﻳﻌﻪcase ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺗﻚ ﺗﻚ ﺑﻴﻤﺎﺭﻳﻬﺎ ﻧﻤﻮﻧﻪﻫﺎﻱ ﺑﺎﻓﺘﻲ ﺍﺭﮔﺎﻥ ﺩﺭﮔﻴﺮ ﺑﻴﻤﺎﺭﻱ ﺑﺼﻮﺭﺕ ﻣﺎﻛﺮﻭﺳﻜﻮﭘﻲ ﻭ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﻭﺍﺿﺢ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﻭ ﺿﻤﻦ ﺍﺭﺍﺋﻪ ﺷﺮﺡ ﺣﺎﻝCD ﺩﺭ ﺍﻳﻦ . ﺑﺨﺼﻮﺹ ﺑﻪ ﺩﺳﺘﻴﺎﺭﺍﻥ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻳﺴﺖ ﺩﻣﺎ ﺩﺭ ﺟﻬﺖ ﺗﺸﺨﻴﺺ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﺑﻴﻤﺎﺭﻳﻬﺎ ﻛﻤﻚ ﺷﺎﻳﺎﻥ ﻣﻲﻛﻨﺪ ﻭ ﻧﻤﺎﺩﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻣﻴﻜﺮﻭﺳﻜﻮﺑﻴﻚ ﺑﻴﻤﺎﺭﻳﻬﺎ ﺭﺍ ﺑﺼﻮﺭﺕ ﺟﺪﺍﮔﺎﻧﻪ ﻣﻮﺭﺩ ﺗﻮﺟﻪ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪCD ﺍﻳﻦ،ﻣﻲﭘﺮﺩﺍﺯﺩ 30.4 Immunology (Blackwell Science)
2000
31.4 Interactive Color Atlas of Histology (Version 1.0) (Leslie P. Gartner James L. Hiatt) (LIPPINCOTT WILLIAMS & WILKINS)
2000
32.4 Interactive Embryology The Human Embryo Program (Jay Lash Ph.D.) 33.4 Laboratory Medicine: URINALYSIS (Chemical and microscopic examination of urine Atlas of Microscopic Analysis Procedures for Urinalsis) (Pesce Kaplan Pubishers Inc.)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2000
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
22 Extensive atlas of microscopic analysis: over 50 microphotographs of urine sediment, including cells, casts, and artifacts
Method write-up for 15 chemical urinalysis procedures
Complete Specimen collection section
Interpretation of urine findings in common renal and lower urinary tract diseases
Tables reviewing results of chemical urinalyses
2000
34.4 Media Supplement for Biochemistry (FOURH EDITION) (Roy Tasker Carl Rhodes) 1. Reaction mechanisms
2. Metabolic Pathways
3. Membrane Processes
4. Protein Synthesis
5. Molecular Representations
35.4 Microbes in Motion III (Dr. Gloria Delisle and Dr. Lewis Tomalty Queen's University)
ﻭﻳﺮﻭﺱﺷﻨﺎﺳﻲ ﺍﭘﻴﺪﻭﻣﻴﻮﻟﻮﮊﻱ ﺑﺎﻛﺘﺮﻳﻮﻟﻮﮊﻱ ﻭﺍﻛﺴﻦﻫﺎ
ﺭﺍﻫﻬﺎ ﻭ ﺭﻭﺵﻫﺎﻱ ﻛﻨﺘﺮﻝ ﻭ ﻣﻬﺎﺭ ﺭﺷﺪ ﺑﺎﻛﺘﺮﻳﻬﺎ ﺍﻧﮕﻞﺷﻨﺎﺳﻲ (... ﺗﺮﺍﻧﺴﭙﻮﺯﻭﺭﻫﺎ ﻭ، DNA ﺳﺎﺧﺘﺎﺭ،ﮊﻧﺘﻴﻚ )ﺑﻴﻮﺗﻜﻨﻮﻟﻮﮊﻱ ﺑﺎﻛﺘﺮﻳﻬﺎﻱ ﮔﺮﻡ ﻣﺜﺒﺖ
ﻣﻴﻜﺮﻭﺑﻬﺎﻱ ﺑﻲﻫﻮﺍﺯﻱ ﻣﺤﻴﻄﻲ ﻣﻴﻜﺮﻭﺑﻴﻮﻟﻮﮊﻱ ﻣﺤﻴﻄﻲ ﺑﺎﻛﺘﺮﻳﻬﺎﻱ ﮔﺮﻡ ﻣﻨﻔﻲ
: ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ١٨ ﺩﺍﺭﺍﻱ ﻳﻚ ﻛﺘﺎﺑﺨﺎﻧﻪ ﺷﺎﻣﻞCD ﺍﻳﻦ ﭘﺎﺗﻮﮊﻧﺰ ﻣﺘﺎﺑﻮﻟﻴﺴﻢ ﻣﻴﻜﺮﻭﺑﻲ ﻗﺎﺭﭺﺷﻨﺎﺳﻲ
ﻋﻤﻠﻜﺮﺩ ﺿﺪ ﻣﻴﻜﺮﻭﺑﻬﺎ ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻱ ﻣﻘﺎﻭﻣﺖ ﺿﺪ ﻣﻴﻜﺮﻭﺑﻲ
Miscellaneous
2002
36.4 MICROBIOLOGY AND IMMUNOLOGY (KEN S. ROSENTHAL) (Mosby) 1.
TUTORIAL: I. Topics
II. Systems
ــــــ
2. TEST
III. Random
37.4 MICROBIOLOGY AND MICROBIAL INFECTIONS (Topley & Wilson's) (Albert Balows, Max sussman)
(NINTH EDITION)
ــــــ 1999
38.4 MODERN GENETIC ANALYSIS (Anthony J. F. Griffiths, William M. Gelbart, Jffrey H. Miller, Richard C. Lewontin)
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ Introduction
System Requirements
Getting Started
Reference
Freeman Genetics Web Site
39.4 MOLECULAR CELL BIOLOGY 4.0 (Paul Matusdaru, Amold Berk, S. lawence Zipufsky, David Baltimore, James Damell, Harey lodish) 40.4 NCCL INFOBASE Serving the World's Medical Science Community Through Voluntary Consensus
2000 2002
41.4 PATHOLOGIC BASIS OF DISESE Interactive Case Study Companion to ROBBIMS
ــــــ
Inflammation and Repair Infectious Disease Genitouinary, Breast, and Pregnancy Disorders
Fluid and Hemodynamic Disorders Cardiovascular Diseases Endocrine Diseases
Genetic Disorders Hematopatholory Disorders Skeletal Disorders
(W. B. Saunders Company) (Sixth Edition)
Diseases of Immunity Gastrointestinal Diseases Neuropathology
Neoplasia Diseases of Liver, Galbladder, and Pancreas
Systemic Pathology Diseases of Kidney
42.4 PATHOLOGY (Alan Stevens. James Lowe) 43.4 Peripheral Blood TUTOR
ــــــ
(ANINTERACTIVE TUTORIAL THAT TEACHES THE MICROSCOPIC EXAMINATION OF URINARY SEDIMENT)
ــــــ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﺍﻳﻦ
Introduction
Cell Morphologies
Disease Associations
Atlas
Overview, Smear Preparation Stain Procedure, Smear Evaluation
Cell Structure, Read Blood Cells, White Blood Cells, Platelets, Artifacts, Quiz
Red Blood Cells, White Blood Cells, Neoplastic Disorder
Cell Morphology Disease Association
44.4 PRINCIPLES OF Molecular Virology • Contents Introduciton Particles Genomes
Final Exam
2000
(THIRD EDITION) Replication
Expression
Infection
Pathogenesis
Novel Infectious Agents
• Appendices Glossary, Abbreviations and Pronounciations
Classification of Sub-Cellular Infections Agents
The History of Virology
45.4 RAPID REVIEW HISTOLOGY AND CELL BIOLOGY (E. ROBERT BURNS, M. DONALD CAVE) (MOSBY) 46.4 Samter's Immunologic Diseases (SIXTH EDITION) (K. Frank Austen, M.D, Michael M. Frank, M.D., John P. Atkinson, M.D., Harvey Cantor, M.D.)
2002 ــــ
: ﻗﺴﻤﺖ ﺍﺻﻠﻲ ﺍﺳﺖ ﻛﻪ ﻫﺮ ﻗﺴﻤﺖ ﺩﺍﺭﺍﻱ ﭼﻨﺪﻳﻦ ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ١٠ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺍﺭﺍﻱ. ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩFlash ﻭInternet explorer ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺍﺳﺖ ﻛﻪ ﺗﺤﺖ ﺑﺮﻧﺎﻣﺔCD ﺍﻳﻦ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
23 ( ﺗﺸﺨﻴﺺ ﻭ ﺷﻨﺎﺳﺎﻳﻲ )ﺍﻳﻤﻨﻲ ﺫﺍﺗﻲ ﻭ ﺍﻛﺘﺴﺎﺑﻲ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺧﺘﺼﺎﺻﻲ ﺍﻧﺪﺍﻡ-
ﻣﻜﺎﻧﻴﺰﻡﻫﺎﻱ ﻣﺆﺛﺮ ﺍﻳﻤﻨﻲ ﺩﺭ ﺍﻳﻤﻨﻲ ﺫﺍﺗﻲ ﻭ ﺍﻛﺘﺴﺎﺑﻲ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺁﻟﺮﮊﻳﻜﻲ-
ﺑﻴﻤﺎﺭﻱ ﻧﻘﺺ ﺍﻳﻤﻨﻲ ﺍﻭﻟﻴﻪ ﺳﻴﺴﺘﻢ ﺍﻳﻤﻨﻲ ﻓﻌﺎﻝ ﻭ ﻏﻴﺮ ﻣﺆﺛﺮ-
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺯﺩﻳﺎﺩ ﻭ ﺗﻜﺜﻴﺮ ﺳﻠﻮﻟﻬﺎﻱ ﺍﻳﻤﻨﻲ ﭘﻴﻮﻧﺪ ﺍﻋﻀﺎﺀ-
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺳﻴﺴﺘﻤﻴﻚ ﺍﻳﻤﻨﻲ ﺷﻨﺎﺳﻲ ﺩﺭﻣﺎﻧﻲ-
ﻗﺪﺭﺕ ﺑﺰﺭﮔﻨﻤﺎﻳﻲ ﺗﺼﺎﻭﻳﺮ ﻭ ﻧﻤﺎﻳﺶ ﻣﻨـﺎﺑﻊ. ﺗﻮﺍﻧﺎﻳﻲ ﺟﺴﺘﺠﻮ ﻭﺍﮊﻩﻫﺎ ﻭ ﻟﻐﺎﺕ ﺗﺨﺼﺼﻲ ﻭ ﭼﺎﭖ ﻣﺘﻮﻥ ﻛﺘﺎﺏ ﺭﺍ ﺩﺍﺭﺩ. ﺩﺍﺭﺍﻱ ﻳﻚ ﻛﺘﺎﺑﺨﺎﻧﻪ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ ﻓﺼﻞ ﻭ ﻫﺮ ﻣﻮﺿﻮﻉ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺟﺪﺍﻭﻝ ﻭ ﻃﺮﺡﻭﺍﺭﻩﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﺭﺍ ﺑﻪ ﻧﻤﺎﻳﺶ ﻣﻲﮔﺬﺍﺭﺩCD ﺍﻳﻦ .ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﻛﺘﺎﺏ ﺍﺯ ﻭﻳﮋﮔﻴﻬﺎﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﻲﺑﺎﺷﺪ 47.4 The American Society of Hematology (41st Annual Meeting and Exposition)
1999
48.4 The Cell 1.0 A Molecular Approach (Many Animations, Movies, Photos, and drawn images) (Geoffrey M. Cooper)
ــــــ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ
Cell Overview Organelles & Energy Metabolism
Humman Genetic Diseases The Cytoskeleto
Floww of Information The Plasma Membrane
The Nucleus The Extracellular Machine
The Cell Cycle Cancer-A Family od Diseases
Protein Sorting and Transport The Meiotic Divisions
49.4 THE HUMAN GENOME PROJECT
2003
50.4 The Metabolic and Molecular Bases of Inherited Disease
____
General Themes, Amino Acids, Prophyrins and Heme, Hormones: Synthesis and Action, Defense and Immune Mechanisms, Skin, Cancer and Genetics, Organic Acids, Metals, Vitamins, Connective Tissues, Intesine, Chromosomes and Autosomes, Peroxisomes, Blood and Blood Forming Tissue, Muscle, Neurogenetics, Carbohydrates, Lipoprotein and Lipid Metabolism disorders, Lysosomal Transport, Eye, Signiflcant Developments in Progress, Cancer and NEW Geneticx Update
2000
51.4 UNDERSTAND! Biochemistry (3/e Version) (Lehninger Principles of Biochemistry) 1. THE BACKGROUND 2. THE MOLECULES OF LIFE 3. PROTEINS IN ACTION
4. BIOENERGETICS 5. BIOSYNTHESIS 6. NUCLEIC ACIDS AND THEIR EXPRESSION
7. CELLULAR ARCHITECTURE AND TRAFFIC 8. THE DIVIDING CELL 9. SOME IMPORTANT TECHNIQUES
1999
52.4 UNDERSTAND! Biochemistry (VERSION 1.0)
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ - QUIZE
- INDEX
- Web links
-Minicourses:
53.4 UNDERSTAND! Biology: Biochemistry (Molecules, Cell & Genes)
ــــــ : ﻣﺸﺘﻤﻞ ﺑﺮ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ، ﻓﻮﻕCD
Basic Chemistry
Macromolecular assembly and modification
Bioenegetics
Signal transduction
Enzymology
The flow of genetic information
54.4 Urinalysis TUTOR (ANINTERACTIVE TUTORIAL THAT TEACHES THE MICROSCOPIC EXAMINATION OF URINARY SEDIMENT) (Caria M. Phillips, MLM, MT(ASCP),
Metabolism
Molecular biology techniques
Paul J. Henderson, MS, MT(ASCP), Claudia Bein, BS, MT(ASCP))
ــــــ
. ﻓﺼﻞ ﺭﻭﺵ ﺁﺯﻣﺎﻳﺸﺎﺕ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﻧﻤﻮﻧﻪﻫﺎﻱ ﺍﺩﺭﺍﺭﻱ ﺭﺍ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﺪ٥ ﺩﺭinteractive ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ( ﻋﻔﻮﻧﺖ ﻟﻮﻟﺔ ﺍﺩﺭﺍﺭﻱ، ﻓﻴﻠﻮﻧﻔﺮﻳﺖ، ﺳﻨﺪﺭﻡ ﻧﻔﺮﻭﺗﻴﻚ. ﺑﻴﻤﺎﺭﻳﻬﺎ )ﺳﻨﺪﺭﻡ ﮔﻠﻮﻣﺮﻭﻟﻮﻧﻔﺮﻳﺖ.٥ ( ﺁﺭﺗﻴﻔﻜﺖﻫﺎ، ﺍﺭﮔﺎﻧﻴﺰﻣﻬﺎ، ﻛﺮﻳﺴﺘﺎﻟﻬﺎ، ﺳﺎﺧﺘﺎﺭ ﻭ ﻣﺎﻫﻴﺖ ﺭﺳﻮﺑﺎﺕ ﺍﺩﺭﺍﺭ )ﺑﺮﺭﺳﻲ ﺳﻠﻮﻟﻬﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ ﺍﺩﺭﺍﺭ.٣
.( ﻫﺮ ﺳﺆﺍﻝ ﺑﻪ ﺷﻜﻞ ﻧﻤﺎﻳﺶ ﻳﻚ ﺗﺼﻮﻳﺮ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻣﻮﺭﺩ ﺳﺆﺍﻝ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ. ﺳﺆﺍﻻﺗﻲ ﺑﺼﻮﺭﺕ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ، ﺍﺯ ﻫﺮ ﺑﺨﺶ. ﻣﻲﺑﺎﺷﺪB ﻭA ﺍﻣﺘﺤﺎﻥ ﭘﺎﻳﺎﻧﻲ )ﺷﺎﻣﻞ ﺩﻭﺳﺮﻱ ﺍﻣﺘﺤﺎﻥ.٤
( ﻣﻜﺎﻧﻴﺴﻢ ﻋﻤﻠﻜﺮﺩ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﻭ ﻧﻤﻮﻧﻪﻫﺎﻱ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ، ﺗﻔﺴﻴﺮ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﻧﺘﺎﻳﺞ، ﻣﻘﺪﻣﻪ )ﻋﻤﻠﻜﺮﺩ ﻛﻠﻴﻪ.١ ( ﻓﻬﺮﺳﺖ ﺗﺼﺎﻭﻳﺮ )ﺗﺼﺎﻭﻳﺮ ﻓﺼﻞ ﺩﻭﻡ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺑﺼﻮﺭﺕ ﻣﺠﺰﺍ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﻣﻲﺁﻳﺪ.٢
ﻗﻠﺐ-٥
CD ﻋﻨﻮﺍﻥ 2.4
A Slide Atlas of ATHEROSCLEROSIS Progression and Regression (Herbert C. Stary, MD)
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ 2002
ﻣﻄﺎﻟﻌﻪ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﻪ. ﺍﺳﻼﻳﺪ ﺗﺨﺼﺼﻲ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﭘﻴﺸﺮﻓﺖ ﻭ ﭘﺴﺮﻓﺖ ﺑﻴﻤﺎﺭﻱ ﺁﺗﺮﻭﺍﺳﻜﻠﺮﻭﺯﻳﺲ ﺩﺭ ﺳﻨﻴﻦ ﻣﺨﺘﻠﻒ ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺭﺍ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﻭ ﺍﻟﻜﺘﺮﻭﻧﻲ ﺑﻪ ﺯﻳﺒﺎﻳﻲ ﺑﻪ ﺗﺼﻮﻳﺮ ﻛﺸﻴﺪﻩ ﺍﺳﺖ٩٤ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺎ .ﻣﺘﺨﺼﺼﻴﻦ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﺗﻮﺻﻴﻪ ﻣﻲﺷﻮﺩ 1.5
A visible improvement in angina treatment (VCD) Post-EECP stress perfusion image, Markedly improved anterior, septal, and inferior wall perfusion.
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
2.5 3.5 4.5
24 ACCSAP (Adult Clinical Cardiology Self-Assessment Program) (C. Richard Donti, MD, Richard P. Lewis, MD) (AMERICAN COLLEGE of CARDIOLOGY) Acute Heart Failure (THE CLEVELAND CLINIC FOUNDATION) (W. Frank Peacock, MD) (The Emergency Department and the Economics of Care) American Heart Associations fighting Heart Disease and Stroke Abstracts from Scientific Sessions (Augustus O. Grant, Raymond J. Gibbons)
2000 2004 2002
: ﺑﺤﺚ ﻣﻲﻛﻨﺪ ﺷﺎﻣﻞCD ﻣﺒﺎﺣﺜﻲ ﻛﻪ ﺍﻳﻦ 5.5
6.5
-Basic Science -Clinical Science -Population Science Atlas of Transesophageal Echocardiography (Navin C. Nanda, MD, Michael J. Domanski)
(Williams & Wilkins)
1. Normal Anatomy 2. Prosthetic Valves and Rings
7. Tricuspid and Pulmonary Valves 8. Congenital Heart Disease
3. Mitral Valve 4. Ischemic Heart Disease
5. Aortic Valve and Aorta 6. Cardiomyopathy
ــــــ
BEYOND HEART SOUNDS The Interactive Cardic Exam (John Michael Criley, MD) (VOL 1)
ــــــ
Introduction to anscultation Frontal Chest Anatomy The Cardinal areas of anscultation Using the stethoscope
7.5
Hemodynamics tutorial The cardiac cycle Pulse Tutorial Mitral and aortic valve flow Introduction Hemodynamic changes in disease Carotid Pulses Mitral Stenosis Jugular Venous Pulses Aortic stenosis Cardiac Catheterization, Angiography, and Intervention (SIXTH EDITION) (LIPPINCOTT WILLIAMS & WILKINS)
2000
. ﺩﻗﻴﻘﻪ ﻓﻴﻠﻢ ﺑﻮﺩﻩ ﻭ ﻛﻠﻴﻪ ﺗﺼﺎﻭﻳﺮ ﺑﻪ ﺻﻮﺭﺕ ﺭﻧﮕﻲ ﻣﻲﺑﺎﺷﺪ٣٥ ﻭGrossmam's Cadiac Cathetrization ....... ﺷﺸﻢ ﻛﺘﺎﺏedition ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞCD ﺍﻳﻦ . ﻣﻲﺑﺎﺷﺪProcerdue- related Findinig ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺒﻲ ﻭ ﻧﺮﻣﺎﻝ ﻫﻤﺮﺍﻩ ﺑﺎCase50 ﻭﺟﻪ ﻣﺸﺨﺼﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻓﻴﻠﻢ ﻭﻳﺪﺋﻮﻳﻲ ﺷﺎﻣﻞ . ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ٨ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ (.... ﻗﻠﺐ ﻭ ﻣﻘﺎﻭﻣﺖ ﻋﺮﻭﻕ ﻭoutput ﻭblood flow ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ- ﻣﻮﺍﺭﺩ ﻫﻤﻮﺩﻳﻨﺎﻣﻴﻚ )ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﻓﺸﺎﺭ-٣ ( ﻛﺎﺗﺘﺮﺍﺯﻳﺴﻮﻥ ﺗﺸﺨﻴﺼﻲ ﺩﺭ ﻛﻮﺩﻛﺎﻥ ﻭ ﻧﻮﺯﺍﺩﺍﻥ-Brachiel Cutdown – Percutaneous approuch) Basic ﺗﻜﻨﻴﻚﻫﺎﻱ-٢ ﻣﻼﺣﻈﺎﺕ ﻛﻠﻲ ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ-١ (... ﻭﻇﻴﻔﻪ ﺩﻳﺎﺳﺘﻮﻟﻲ ﻭ ﺳﻴﺴﺘﻮﻟﻲ ﺑﻄﻨﻲﻫﺎ ﻭ،Ejection Fraction ﻃﻲ ﻛﺎﺗﺘﺮﺍﺯﻳﺴﻴﻮﻥ ﻗﻠﺒﻲ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺣﺠﻢ ﺑﻄﻦﻫﺎTest ﺍﺭﺯﻳﺎﺑﻲ ﻓﺎﻧﻜﺸﻨﺎﻝ ﻗﻠﺒﻲ )ﺍﺳﺘﺮﺱ-٥ ( ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺁﺋﻮﺭﺕ ﻭ ﺷﺮﻳﺎﻧﻬﺎﻱ ﻣﺤﻴﻄﻲ- ﺗﻜﻨﻴﻚﻫﺎﻱ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ) ﺁﻧﮋﻳﻮﻛﺮﻭﻧﺮﻱ – ﻭﻧﺘﺮﻳﻜﻮﻟﻮﮔﺮﺍﻓﻲ ﻗﻠﺒﻲ – ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﻭﭘﻮﻟﻤﻮﻧﺮﻱ-٤ ﺗﻜﻨﻴـﻚﻫـﺎﻱ ﻣﺪﺍﺧﻠـﻪﺍﻱ )ﺁﻧﺘﮋﻳﻮﭘﻼﺳـﺘﻲ ﻋـﺮﻭﻕ-٧ (... ﻭintrathoracic balloon Counter Pulsation - ﺑﺮﺍﻱ ﺩﺭﻣـﺎﻥ ﺁﺭﻳﺘﻴﻤـﻲﻫـﺎdeivce ﻗﺮﺍﺭ ﺩﺍﺩﻥ- ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ- )ﺍﻛﻮﻛﺎﺭﺩﻳﺎﻝ ﺑﻴﻮﭘﺴﻲ: Special Catheter Techniquse -٦ – )ﻃـﺮﺯ ﺷﻨﺎﺳـﺎﻳﻲ ﻭ ﻛﺎﺗﺘﺮﻳﺰﺍﺳـﻴﻮﻥ ﻭ ﺁﻧﮋﻳـﻮﮔﺮﺍﻓﻲ ﺑﻴﻤـﺎﺭﻱﻫـﺎﻱ ﺩﺭﻳﭽـﻪﺍﻱ ﻗﻠـﺐ: ﺩﺭ ﺍﺧـﺘﻼﻻﺕ ﺍﺧﺘﺼﺎﺻـﻲProfile -٨ (ﮔﺬﺍﺭﻱ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮ – ﻣﺪﺍﺧﻠﻪ ﺩﺭ ﻋﺮﻭﻕ ﻣﺤﻴﻄﻲ ﻭ ﻋﺮﻭﻕ ﻛﻮﺩﻛﺎﻥStent- ﺁﺗﺮﻭﻛﺘﻮﻣﻲ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮﻱ ﻭ ﺗﺮﻭﻣﺒﻜﺘﻮﻣﻲ-ﻛﺮﻭﻧﺮﻱ :( ﻓﻴﻠﻢﻫﺎﻱ ﻭﻳﺪﺋﻮﻳﻲ ﺷﺎﻣﻞ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ ﻭ ﺍﻗﺪﺍﻣﺎﺕ ﺩﺭﻣﺎﻧﻲ... ﺑﻴﻤﺎﺭﻱ ﺍﻣﺒﻮﻟﻲ ﺭﻳﻪ ﻭ-ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺮﺍﺋﻴﻦ ﻛﺮﻭﻧﺮﻱ ﺍﺧﺘﻼﻻﺕ ﻭﻧﺘﺮﻳﻜﻮﻟﻮﮔﺮﺍﻓﻲ ﺑﻄﻦ ﭼﭗ ﻏﻴﺮ ﺁﺗﺮﻭﺳﻜﺮﻭﺗﻴﻚCAD ﺁﻧﻮﻣﺎﻟﻴﻬﺎ ﻭBasic ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ ﺍﺧﺘﻼﻻﺕ ﺁﺋﻮﺭﺕ ﻭ ﻋﺮﻭﻕ ﻣﺤﻴﻄﻲ.( ﻣﻲﺑﺎﺷﺪ.... ﻭRotabalator ﺑﺎﻟﻮﻥﮔﺬﺍﺭﻱ ﻭ ﻭﺍﻟﻮﭘﻼﺳﺘﻲ- ﻋﻮﺍﺭﺽ- ﮔﺬﺍﺭﻱStent) ﻣﺪﺍﺧﻼﺕ ﺩﺭﻣﺎﻧﻲ ﺷﺎﻣﻞ8.5
Cardiovascular Surgery (VCD) (CD I, II, III) Excerpted from "Medical & Surgical Controversies in CV disease: The Aorta and Peripheral Vessels" Course Directors: Thoralf M. Sundt III, MD and Peter C. Spittell, MD
2004
9.5
CathSAP Cardiac Catheterization and Interventional Cardiology Self-Assessment Program (Carl J. Pepine, MD, Steven E. Nissen, MD)
ــــــ
10.5 Challenging established treatment patterns in chronic heart failure
A Satellite Symposium held during the ESC Heart Failure meeting
11.5 Clinical TRANSESOPHAGEAL ECHOCARDIOGRAPHY (A PROBLEM- ORIENTED APPROACH) (Second Edition)
(Steven N. Konstadt)
2003 2003
12.5 Clinical Utility of Contrast Echocardiography
2001
13.5 Congestive Heart Failure
ــــــ
Sonovue: An ideal contrast agent for Low MI myocardial Perfusion (Dr. Daniela Bokor, Bracco sa, Milano) What's new in cardic echography (Dr. Luciano Agati, University "La Sapienza Roma" Ischemic coronary artery disease (Dr. Harld Becher, John Radcliffe Hospital, Oxford)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(NOVARTIS) (CD I , II)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
25 ﺍﺑﺘﺪﺍ ﭘﺰﺷﻚ ﺳﺆﺍﻻﺗﻲ ﺍﺯ ﺑﻴﻤﺎﺭ ﻣﻲﻛﻨﺪ ﻭ ﺑﻴﻤﺎﺭCase report ﺩﺭ. ﻓﻴﻠﻢ ﻭﻳﺪﺋﻮﻳﻲ ﻭ ﻓﺎﻳﻞ ﺻﻮﺗﻲ ﻣﻲﺑﺎﺷﺪ،Case report ، ﺷﺎﻣﻞ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲCD ﺍﻳﻦ. ﻣﻲﺑﺎﺷﺪFrank .H.Netter ﻣﺆﻟﻒ ﻛﺘﺎﺏ. ﺩﺭ ﻣﻮﺭﺩ ﻗﻠﺐ ﻣﻲﺑﺎﺷﺪCiba ﺷﺎﻣﻞ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲCD ﺍﻳﻦ ﺩﻭ . ﻣﻲﺑﺎﺷﺪCHF ﻭ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺑﻴﻤﺎﺭﻱmultiple choice test ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ. ﺳﭙﺲ ﻣﻌﺎﻳﻨﻪ ﻓﻴﺰﻳﻜﻲ ﺑﻴﻤﺎﺭ ﺗﻮﺳﻂ ﻓﻴﻠﻢ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺍﻃﻼﻋﺎﺕ ﺑﻴﺸﺘﺮ ﺗﻮﺳﻂ ﻛﺎﺭﺑﺮ ﺑﺎ ﻛﻠﻴﻚ ﻛﺮﺩﻥ ﺑﺮ ﺭﻭﻱ ﺩﻛﻤﻪﻫﺎ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺩﺳﺖ ﺁﻭﺭﺩ.ﺑﻪ ﺳﻮﺍﻻﺕ ﺟﻮﺍﺏ ﻣﻲﺩﻫﺪ . ﻣﻲﺑﺎﺷﺪCHF ﻭ ﺩﺭﻣﺎﻥmanagement ، ﺗﺸﺨﻴﺺ.٤
CHF ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ.٣
CHF ﺍﺗﻴﻮﻟﻮﮊﻱ ﻭ ﺗﻌﺮﻳﻒ ﺑﻴﻤﺎﺭﻱ.٢
ﻋﻤﻠﻜﺮﺩ ﻧﺮﻣﺎﻝ ﻗﻠﺐ ﻭ ﺳﻴﺴﺘﻢ ﻋﺮﻭﻗﻲ.١ : ﻓﺼﻮﻝ ﻛﺘﺎﺏ ﺷﺎﻣﻞ
14.5 Coronary Heart Disease (J. Hurley Myers, Ph.D., Frank H. Netter, M.D.)
ﺁﻣﻮﺯﺵ ﺑﺎﻟﻴﻨﻲ ﻭ ﺑﻴﻤﺎﺭﻱ-٢ ﺁﻣﻮﺯﺵ ﭘﺰﺷﻜﻲ-١ :ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ﺩﻭ ﺑﺨﺶ ﻣﻲﺑﺎﺷﺪ ﺗﺸﺨﻴﺺ ﻭ ﻣﺪﻳﺮﻳﺖ ﺩﺭﻣﺎﻥ-٤ ﺍﻧﻔﺎﺭﻛﺘﻮﺱ ﻣﻴﻮﻛﺎﺭﺩ-٣ ﺁﺗﺮﻭﺍﺳﻜﻠﺮﻭﺯﻳﺲ-٢ ﺁﻧﺎﺗﻮﻣﻲ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮﻱ-١ :ﺑﺨﺶ ﺍﻭﻝ ﺷﺎﻣﻞ . ﻛﺎﺭﺑﺮ ﻣﻲﺗﻮﺍﻧﺪ ﻳﺎﺩﺩﺍﺷﺖ ﺷﺨﺼﻲ ﺧﻮﺩ ﺭﺍ ﺍﺿﺎﻓﻪ ﻭ ﺫﺧﻴﺮﻩ ﻧﻤﺎﻳﺪ، ﺩﺭ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﻣﻮﺿﻮﻋﺎﺕ.ﻫﺮ ﻳﻚ ﺍﺯ ﭼﻬﺎﺭﻓﺼﻞ ﻓﻮﻕ ﺩﺍﺭﺍﻱ ﭼﻨﺪﻳﻦ ﺯﻳﺮﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺼﻮﺭﺕ ﺗﺼﺎﻭﻳﺮ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ ﻣﺘﻨﻲ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ﻭ-٩ ﺩﺍﺭﻭ ﺩﺭﻣﺎﻧﻲ-٨ ﺭﻭﺷﻬﺎﻱ ﺗﺸﺨﻴﺼﻲ-٧ ﺍﻧﻔﺎﺭﻛﺘﻮﺱ ﻣﻴﻮﻛﺎﺭﺩ-٦ ﺁﻧﮋﻳﻦ ﺻﺪﺭﻱ-٥ ﭘﻴﮕﻴﺮﻱ ﺍﺯ ﺑﻴﻤﺎﺭﻱ ﺍﻧﺴﺪﺍﺩ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮ-٤ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺴﺪﺍﺩ ﺳﺮﺧﺮﮔﻬﺎﻱ ﺍﻛﻠﻴﻠﻲ-٣ ﻋﺮﻭﻕ ﺧﻮﻧﻲ ﻗﻠﺐ-٢ ﻣﻘﺪﻣﻪ-١ ﻣﺒﺎﺣﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺷﺎﻣﻞ:ﺩﺭ ﺑﺨﺶ ﺩﻭﻡ .ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﻋﻨﺎﻭﻳﻦ ﻓﻮﻕ ﺗﻮﺳﻂ ﮔﻮﻳﻨﺪﻩ )ﺑﺎ ﭘﺨﺶ ﺻﺪﺍ( ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ (ﻋﻤﻞ ﺟﺮﺍﺣﻲ )ﺍﻳﻦ ﺑﺨﺶ ﺩﺍﺭﺍﻱ ﻓﻴﻠﻤﻬﺎﻱ ﻛﻮﺗﺎﻩ ﺍﺯ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﻗﻠﺐ ﻣﻲﺑﺎﺷﺪ
ــــــ
15.5 Dynamic Practical Electrodiography (Lippincott Williams & Wilkins)
ــــــ
16.5 ECG (Jay W. Mason, MD)
ــــــ
17.5 ECG DIAGNOSIS MADE EASY ROMEO VEGHT ﻓﺼﻞ ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﻣـﻮﺍﺭﺩ٩ . ﺗﻮﺍﻧﺎﻳﻲ ﺟﺴﺘﺠﻮﻱ ﻧﻤﻮﺩﺍﺭﻫﺎﻱ ﻭ ﭼﺎﭖ ﻭ ﺫﺧﻴﺮﺓ ﺁﻧﻬﺎ ﻧﻴﺰ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. ﮔﻮﻧﺎﮔﻮﻥ ﺍﺳﺖECG ﻋﺪﺩ ﻧﻤﻮﺩﺍﺭ٣٥٠ ﺩﺍﺭﺍﻱ. ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩInternet explorer ﻓﺼﻞ ﺍﺳﺖ ﻭ ﺗﺤﺖ ﺑﺮﻧﺎﻣﺔ٩ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻣﺸﺘﻤﻞ ﺑﺮ :ﺯﻳﺮ ﺍﺳﺖ 1. Basic Priciples ( ﻫﺪﺍﻳﺖ ﺟﺮﻳﺎﻥ ﺍﻟﻜﺘﺮﻳﻜﻲ، ﺩﭘﻮﻻﺭﻳﺰﺍﺳﻴﻮﻥ ﻋﻀﻠﻪ، ﻣﻮﻗﻌﻴﺖ ﺍﻟﻜﺘﺮﻭﺩﻫﺎ،ﻧﺮﻣﺎﻝ 3. ECG ﻭ ﻧﺤﻮﺓ ﺿﺒﻂ....) Ischaemic (Coronary) heart disease 5. Conductin impairment 7. Rhythm disturbances 2. Hypertrophy
6. Chardiomyopathies and autoimmune disorders
4. Pericarditis, myocarditis and metabolic disorders
6. Pacemakers, ICDs and cardioversion Mixed ECG quizzes
ﺭﺍ ﻣﻲﺯﻧﻴﻢ ﻣﺴﻴﺮ ﻧﺼﺐ ﭘﺮﺳﻴﺪﻩ ﻣﻲﺷﻮﺩ ﺩﺭ ﺻﻮﺭﺕ ﺗﻮﺍﻓـﻖNext ﺳﭙﺲ. ﺭﺍ ﺍﺟﺮﺍ ﻣﻲﻛﻨﻴﻢSetup ﻓﺎﻳﻞ. ﻣﻲﺷﻮﻳﻢSetup ﺷﺪﻩ ﻭ ﺍﺯ ﺁﻧﺠﺎ ﻭﺍﺭﺩ ﺷﺎﺧﻪCD ﺑﻌﺪ ﻭﺍﺭﺩ ﺩﺭﺍﻳﻮ. ﻣﻲﺷﻮﻳﻢmy 18.5 ECG-SAP III (Jay W. Mason, MD, FACC) -Using ECG-SAP III -Standard Tracings -Syndromes 19.5
ــــــ
computer ﺭﺍ ﺩﺭﻭﻥ ﺩﺭﺍﻳﻮ ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﻭ ﺳﭙﺲ ﻭﺍﺭﺩCD ﺍﺑﺘﺪﺍ:( ﻃﺮﻳﻘﺔ ﻧﺼﺐ . ﺭﺍ ﻓﺸﺎﺭ ﻣﻲﺩﻫﻴﻢFinish ﺭﺍ ﻣﻲﺯﻧﻴﻢ ﺑﺮﻧﺎﻣﻪ ﻧﺼﺐ ﻣﻲﺷﻮﺩ ﺩﺭ ﭘﺎﻳﺎﻥNext
ــــــ -Computer Overreads
-Serial Tracings
-Stress Testing
-ECG of the Month
-Guidelines
-Utilities
Echo Lecture (VIDEO SERIES) (7CD) (Mayo) : ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢ ﻣﻲﺑﺎﺷﺪ ﺷﺮﺡ ﻋﻨﺎﻭﻳﻦ ﺁﻥ ﺑﻪ ﺻﻮﺭﺕ ﺯﻳﺮ ﺍﺳﺖCD ﺳﺮﻱ٧ ﺍﻳﻦ ﻣﺠﻤﻮﻋﻪ ﻛﻪ ﺷﺎﻣﻞ
ــــــ
1. TEE in the Operating Room (Bijoy K. Khandheria, MD) Intraoperative echocardiography has become an essential component to the surgical approach to valvular disease. Dr. Bijoy Khandheria discusses the utility of intraoperative echocardiography and its impact on the surgical management of cardiovascular disease.
2. TEE in Adult Congenital Heart Disease (James B. Seward, M.D.)
Dr. James Seward Presents Adult Congenital Heart Disease. A generation of Children Have Grown into adulthood and Present with postoperative congenital heart disease. Transesophageal echocardiography is extremely helpful but may not always be necessary in the assessment of adult congenital heart disease. Learn from the expert regarding appropriate use of transesophageal echocardiography and assessment of residua and sequela of adult congenital heart disease.
3. Understanding Operative Procedures for Patients with Univentricular Heart from Palliation to Fontan (James B. Seward, M.D.) Dr. Seward gives a detailed overview of complex anomalies and their applicable corrections. Topics included are Blalock, Mustard, Glen and Fontan corrections. Graphic depictions of each corrective procedure, possible complications and echocardiographic example are included.
4. Mitral Valve Regurgitation: Essential Measurements. Pitfalls and Limitations. (Fletcher A. Miller, Jr., MD)
Dr. Fletcher Miller discusses and presents the current approach to the quantitative evaluation of mitral valve regurgitation. This is an excellent review of current quantitative assessment of mitral valve regurgitation including pitfalls and limitations.
5. Mitral Vale Regurgitation: Evidence-Based Practice (A. Jamil Tajik, MD) A Classic presentation by Dr. A. Jamil Tajik on a change in clinical practice with regard to the quantitation of regurgitation and then a change in medical management with early surgery and repair of the mitral valve.
6. Evaluating the Patient with Prothetic Valve (Fletcher A. Miller, Jr., MD) Dr. Fletcher Miller, an expert on the echocardiographic assessment of prosthetic valves, presents a detailed in-depth review of the quantitative echo Doppler approach to the prosthetic valve. It is important to understand the hemodynamic pitfalls and limitations of the echocardiographic assessment of cardiac prosthetic valves.
7. Stress Echocardiography and Contrast (Patricia A. Pellikka, M.D.) ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
26 Stress Echocardiography and Contrast Using illustrative cases, Dr. Pellikka gives an expert presentation and discussion on the role of contrast in stress echocardiography. Pitfalls and limitations of contrast stress echocardiography are also discussed. New Horizons in Stress Echocardiography Dr. Pellikka, an expert in Stress echocardiography, discusses Dobutamine stress echocardiography and its role in preoperative risk stratification. Also discussed are new advances in stress echocardiography such as color kinesis and acoustic quantification, color Doppler imaging, and strain and strain rate imaging.
ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (UPDATE NO. 1) (TRANSESOPHAGEAL- ECHOCARDIOGRAPHY) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 1) (VCD) (ECHOCARDIOGRAPHY Normal 2-D And M-MODE EXAM)) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 10) (VCD) (CARDIAC MASSES) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 11-A,B) (VCD CD I, ii) (ECHOCARDIOGRAPHIC ASSESSMENT OF PROSTHETIC HEART VALVES) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 12) (VCD) (INTERVENTIONAL ECHOCARDIOGRAPHY) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 2) (VCD) (DOPPLER AND COLOR FLOW IMAGING: PHYSICS, INSTRUMENTATIONS AND THE NORMAL EXAM) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 4) (VCD) (ECHOCARDIOGRAPHY IN AORTIC VAL VE DISEASE) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 5) (VCD) (ECHOCARDIOGRAPHY IN CORONARY HEART DISEASE) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 6) (VCD) (ECHOCARDIOGRAPHY IN CONGENITAL HEART DISEASE IN THE ADULT) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 7) (VCD) (ECHOCARDIOGRAPHY IN CARDIOMYOPATHIES: DILATED, RESTRICTIVE AND HYPERTROPHIC) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 8) (VCD) (ECHOCARDIOGRAPHY IN PERICARDIAL DISEASE) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 9) (VCD) (ECHOCARDIOGRAPHY IN TRICUSPID AND PULMONIC VALVE DISEASE AND DESEASES OF THE AORTA) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME3) (VCD) (ECHOCARDIOGRAPHY IN MITRAL VALVE DISEASE) EchoSAP III (Echocardiography Self-Assessment Program)(Echocardiography Overview: Technique and Applications) (Volume 1) 33.5 (Jemes D. Thomas, MD, Ellen Mayer-Sabik, MD)
20.5 21.5 22.5 23.5 24.5 25.5 26.5 27.5 28.5 29.5 30.5 31.5 32.5
-Introduction and Overview -Examinations -Applications -Self-Assessment Questions -Evidence-Based Medicine -Conclusions 34.5 Electronic Image Collection of Comprehensive Vascular and Endovascular Surgery (John W. Hallet, Joseph L. Mills, Jonothan J. Eamsbaw, Jim A Reekers) 1. Background 3. claudication 2. Mesenteric Syndromes 4. Renovascular disease
5. Chronic Lower Extremity Ischemia 6. Aneurysmal Disease
7. Acute Limb Ischemia 8. Cerebrovascular Disease
ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ 2000
2004
9. Upper Extremity Problems 10. Venous Disease
35.5 ENDOVASCULAR TECHNIQUES (Abdominal Aortic Aneurysms) (Workshop) (l. Flessenkämper) (15th Endovascular Symposium Berlin)
ــــــ
36.5 ESC Congress
2004
37.5 EVOLVING ISSUES IN THE MANAGEMENT CHD SECTION 1
(National Lipid Education Council
SECTION II
TM
2002
)
SECTION III
SECTION IV
SECTION V
Emerging Evidence-Based Data From Clinical Trials PAD Lipids and Risk Inflammatory Markers: Anovel Approach Use of Genomics to discover new targets for therapy Case study: Diabetes NON-HDL-Case Secondary Targert of Therapy Lipid Management Though combination Therapy Case Study: Novel Risk Markers Examining the nonlipid effects of statins What is it's Role in clinical practice? Case Study:Combination Therapy Case Study: NON-HDL-C
38.5 HEART DISEASE (FIFTH EDITION)
A Textbook of Cardiovascular Medicine (W.B. SAUNDERS COMPANY)
. ﻛﺘﺎﺏ ﻣﺠﺰﺍ ﺗﺸﻜﻴﻞ ﺷﺪﻩ ﺍﺳﺖ٤ ( ﺍﺯe-book) ﺩﺭ ﻭﺍﻗﻊ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ (Mendelsohn) Reviwe and Assessment Book -٤ (Hennekens) Clinical Trials in Cardiovascular Disease -٣ (chien) Molecular Basis of Heart Disase -٢ (Braunwald) Heart Disease -١ )ﺟﺴﺘﺠﻮ( ﺑﺨﺼﻮﺹ ﺑﺮﺍﻱ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎﻱ ﺭﺷﺘﻪﻫﺎﻱ ﻗﻠﺐ ﻭSearch ﻗﺎﺑﻠﻴﺖCD ﺧﺼﻮﺻﻴﺖ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮﺩ ﺍﻳﻦ. ﺳﻮﺍﻝ ﻭ ﺟﻮﺍﺏ ﻣﻲﺑﺎﺷﺪ٧٠٦ ﺩﺭ ﺁﺧﺮ ﻫﺮ ﻓﺼﻞ ﺳﻮﺍﻻﺕ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﺑﺎ ﺟﻮﺍﺏ ﺗﺸﺮﻳﺤﻲ ﻭ ﺭﻓﺮﺍﻧﺲ ﻛﺘﺎﺏ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻛﻪ ﻣﺸﺘﻤﻞ ﺑﺮ ( ﻫﻤﮕﻲe-book) ﺷﻜﻞ ﻭ ﻧﻤﻮﺩﺍﺭﻫﺎﻱ ﺍﻳﻦ. ﻣﻲﺗﻮﺍﻧﺪ ﺩﺭ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺍﺭﺗﻘﺎﺀ ﻭ ﺑﻮﺭﺩ ﻭ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺩﺭﻭﻥ ﺑﺨﺸﻲ ﻛﻤﻚ ﻗﺎﺑﻞ ﺗﻮﺟﻬﻲ ﻧﻤﺎﻳﺪCD ﺳﺮﻳﻊ ﻭ ﻭﺳﻴﻊ ﺍﻳﻦSearch ﻫﻢﭼﻨﻴﻦ ﻗﺎﺑﻠﻴﺖ.ﺩﺍﺧﻠﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﭘﻴﺪﺍ ﻛﺮﺩﻥ ﻣﻮﺿﻮﻋﻲ ﻳﺎ ﺣﺘﻲ ﻛﻠﻤﺎﺕ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﻣﻲﻧﻤﺎﻳﺪ . ﺷﻮﺩCCU ﻫﺎ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺳﺎﺗﻴﺪ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎ ﻭ ﻛﺎﺭﻛﻨﺎ ﻥ ﺑﺨﺶﻫﺎﻱ ﻗﻠﺐ ﻭclub ﺭﻧﮕﻲ ﺍﺳﺖ ﻭ ﻣﻲﺗﻮﺍﻧﺪ ﺑﺮﺍﻱ ﺗﺪﺭﻳﺲ ﻭ ﻳﺎ ﻛﻨﻔﺮﺍﻧﺲ ﻭ
39.5 HEART SOUNDS
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ــــــ
ــــــ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
27 40.5 HEART SOUNDS Basic Cardiac Auscultation Version 3.0 (Leonard Werner, M.D., Brian Pitts, David Gilsdorf)
2003
41.5 Heart Sounds Basic Cardiac Auscultation CD-ROM to Accompany (M.D., F.A/C.P., Brian Pitts, M.D., David Gilsdorf) (Lippincott Williams & Wilkins)
2003
42.5 Highlights
2004
ESC Congress
43.5 HURST'S THE HEART (R. Wayne Alexander, Robert C. Schlant, Valentin Fuster)
ــــــ
. ﺩﺍﺭﺩCD ﻓﺼﻠﻲ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺮﺍﻱ ﺷﻜﻞﻫﺎ ﻭ ﻧﻤﻮﺩﺍﺭﻫﺎﻱ ﻛﺘﺎﺏ ﻭ ﻫﻢ ﭼﻨﻴﻦ ﻓﺼﻠﻲ ﺩﻳﮕﺮ ﺑﺮﺍﻱ ﺻﺪﺍﻫﺎﻱ ﻗﻠﺒﻲ ﺑﻪ ﺻﻮﺭﺕ ﻓﺎﻳﻞ ﺻﻮﺗﻲ، ﻓﺼﻞ١٦ ﻣﺸﺘﻤﻞ ﺑﺮHurst ﻛﺘﺎﺏText ﻧﻬﻢ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻋﻼﻭﻩ ﺑﺮEdition ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺣﺎﺿﺮ . ﺍﺳﺘﻔﺎﺩﻩ ﻛﺮﺩ،( ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺨﺼﻲ ﻣﻲﺗﻮﺍﻥ ﺑﺮﺍﻱ ﺗﺪﺭﻳﺲ )ﺑﺨﺼﻮﺹ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺷﻜﻞﻫﺎﻱ ﺗﻤﺎﻡ ﺭﻧﮕﻲ ﺁﻥCD ﺍﺯ ﺍﻳﻦ. ﺗﺴﺖﻫﺎﻱ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ ﻓﺼﻞ ﻫﻤﺮﺍ ﺑﺎ ﺟﻮﺍﺏ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖCDﺩﺭ ﺁﺧﺮﺍﻳﻦ 44.5 Interactive Echocardiography: A Clinical Atlas
(Th. Binder, M.D., G. Rehak,G. Porenta. M.D., Ph.D., M. Zengeneh, M.D., G. Maurer, M.D., H. Baumgartner, M.D.)
University of Vienna, Austria
45.5 Interventional Cardiology Clinical Resource (Disc 1 & 2) (Evidence . Analysis . Recommendations . Consensus Reports) 46.5 Intra-Aortic Balloon Catheter Insertion and Removal Technique 1. INTRODUCTION
2. LAB SELECTION
3. LAB PREPARATION
4. LAB INSERTION
(ARROW) 5. LAB CATHETER
PREPARATION
6. LAB CATHETER INSERTION
7. LAB REMOVAL : ﺷﺎﻣﻞCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ
47.5 Mastering Auscultation An Audio Tour to Cardiac Diagnosis Clinical Findings Diagnosis Treatment Tutorial Text Reference (Dr. Anthony Don Michael's) 48.5 MVP Video Journal of Cardilogy (Maria-Teresa Olivari, M.D., Antonio M. Gotto, M.D., D. Phill.) ﺍﻳـﻦ. ﻳﻚ ﻣﻮﺿﻮﻉ ﺑﻪ ﺷﻜﻞ ﻣﺼﺎﺣﺒﺔ ﻋﻠﻤﻲ ﺑﺎ ﻳﻚ ﻣﺘﺨﺼﺺ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤـﺎﻳﺶ ﺍﺳـﻼﻳﺪ ﻭ ﻧﻤـﻮﺩﺍﺭ ﺑﺤـﺚ ﺷـﺪﻩ ﺍﺳـﺖ، ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ. ﺩﻗﻴﻘﻪ ﺩﺭ ﺳﻪ ﻗﺴﻤﺖ ﻣﺠﺰﺍ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ٤٥ ( ﺑﻪﻣﺪﺕVCD ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ )ﺩﺭ ﻗﺎﻟﺐMVP ﻫﺎﻱ ﺁﻣﻮﺯﺷﻲCD ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺯ ﺳﺮﻱ :ﻣﻮﺿﻮﻋﺎﺕ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ
ــــــ 2003 2002 ــــــ ــــــ
1-Determination of Rejection in the Cardiac transplant Recipient
Maria-Teresa Olivari ﺩﻛﺘﺮ: ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ . ﺭﻭﺷﻬﺎﻱ ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻳﻜﻲ )ﺁﻧﺘﻲ ﻣﻴﻮﺯﻳﻦ( ﻭ ﺩﻳﮕﺮ ﺭﻭﺷﻬﺎﻱ ﻏﻴﺮﺗﻬﺎﺟﻤﻲ ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ،MRI ، ﺍﻛﻮﺩﺍﭘﻠﺮ،ﭘﻴﮕﻴﺮﻱ ﻭ ﺗﺸﺨﻴﺺ ﺭﺩ ﭘﻴﻮﻧﺪ ﻗﻠﺐ ﺑﻪ ﻛﻤﻚ ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ Antonio Gotto ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ 2- Triglycerides, HDL and coronary Heat Disease . ﻭ ﺭﻋﺎﻳﺖ ﺍﺻﻮﻝ ﺑﻬﺪﺍﺷﺘﻲ ﺩﺭ ﺯﻣﻴﻨﺔ ﻋﺎﺭﺿﺔ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ، ﺑﻴﻤﺎﺭﻱ ﺩﻳﺎﺑﺖ ﻭ ﺭﻭﺷﻬﺎﻱ ﺩﺍﺭﻭﺩﺭﻣﺎﻧﻲ.ﻛﻠﻴﺔ ﺭﻳﺴﻚ ﻓﺎﻛﺘﻮﺭﻫﺎ ﻭ ﻋﻮﺍﻣﻞ ﻣﺆﺛﺮ ﺑﺮ ﺁﻧﻬﺎ ﺩﺭ ﻋﺎﺭﺿﺔ ﺭﮔﻬﺎﻱ ﻛﺮﻭﻧﺮﻱ ﻗﻠﺐ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ 3- Management of Cardiac Disease in Pregnancy Carl E. Orringer ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ ﺍﻓﺰﺍﻳﺶ، ﻛﺎﺭﺩﻳﻮﻣﻴﻮﭘﺎﺗﻲ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ، ﺩﺭﻣﺎﻥ ﺩﺍﺭﻭﻳﻲ ﺑﻴﻤﺎﺭﺍﻥ ﻗﻠﺒﻲ ﺑﺎﺭﺩﺍﺭ،... ﻭMRI ، ﺗﺸﺨﻴﺺ ﺑﻪ ﻛﻤﻚ ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ، ﺳﻤﻊ ﻗﻠﺐ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﻗﻠﺒﻲ ﺑﺎﺭﺩﺍﺭ، ﺗﻨﻔﺴﻲ- ﻋﻼﺋﻢ ﻗﻠﺒﻲ،(... ﺍﻳﺴﺖ ﻗﻠﺒﻲ ﻭ، ﺣﺠﻢ ﺿﺮﺑﻪﺍﻱ، ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻗﻠﺐ ﺩﺭ ﺯﻣﺎﻥ ﺑﺎﺭﺩﺍﺭﻱ )ﺑﺮﻭﻥﺩﻩ ﻗﻠﺒﻲ،ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ . ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﻭ ﻧﻤﻮﺩﺍﺭ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺷﺪﻩ ﺍﺳﺖ... ﻓﺸﺎﺭ ﺧﻮﻥ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ ﻭ
49.5 MVP Video Journal of Cardiology (Anthony C. Pearson, M.D., Charles B. Higgins, M.D., William W. O'Neill, M.D.) (VCD)
ــــــ
: ﺍﻳﻦ ﻣﻮﺿﻮﻋﺎﺕ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ. ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﻳﻚ ﻣﻮﺿﻮﻉ ﺑﻪ ﺷﻜﻞ ﻣﺼﺎﺣﺒﺔ ﻋﻠﻤﻲ ﺑﺎ ﻳﻚ ﻣﺘﺨﺼﺺ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﻪ ﻭ ﻓﻴﻠﻢ ﻭ ﻧﻤﻮﺩﺍﺭ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺷﺪﻩ ﺍﺳﺖ. ﺩﻗﻴﻘﻪ ﺩﺭ ﺳﻪ ﻗﺴﻤﺖ ﺍﺭﺍﺋﻪ ﺷﺪﻩﺍﻧﺪ40 ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻣﺪﺕMVP ﻫﺎﻱ ﺁﻣﻮﺯﺷﻲCD ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺯ ﺳﺮﻱ 1- The stately Art of MR in Cardiovascuvlar Disease Charles P. Higgins ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ . ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ.... ﻭMRI ﺩﺭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻗﻠﺒﻲ ﻋﺮﻭﻗﻲ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﻭ ﺗﺼﺎﻭﻳﺮMRI ﻛﺎﺭﺑﺮﺩ، ﺭﻭﺵﻫﺎﻱ ﻣﺘﻌﺪﺩ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺩﺭ ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ، MRI ﺗﺎﺭﻳﺨﭽﺔ،ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ 2. Arguing for Angioplasy in Acute Myocardial infction William w. ONeill ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ ﺑﺮﺁﻭﺭﺩ ﺩﻳﺴﻚ ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ﻭ ﺑﻪ ﻛﻤﻚ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﻭ ﻓﻴﻠﻢ، ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﺍﻧﮋﻳﻮﭘﻼﺳﺘﻲ، Lone PTCA ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ،ﺗﺎﺭﻳﺨﭽﻪ ﺍﻧﮋﻳﻮﭘﻼﺳﺘﻲ Anthony C. Pearson : ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ 3- Improved understanding of cardioembolic Stroke prorided by Transesophageal Echoecardiography . ﻣﺨﺘﻠﻒ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺷﺪﻩ ﺍﺳﺖCase ﺍﺯ ﭼﻨﺪﻳﻦTEE ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﻭ ﺗﻮﺿﻴﺢ ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻡ،TEE ﻭTEE ﻣﻘﺎﻳﺴﻪ ﺭﻭﺵ،TEE ﺗﺎﺭﻳﺨﭽﻪ ﺗﻜﻨﻴﻚ،ﺗﺎﺭﻳﺨﭽﺔ ﺩﺭﻣﺎﻥ ﺁﻣﭙﻮﻟﻲﻫﺎ 50.5 MVP VIDEO JOURNAL OF CARDIOTHORACIC SURGERY (VIDEO SEGMENT I & II) Thromboexclusion for Treatment of Descending Aortic Dissection (John A. Elefteriades, MD)
ــــــ
51.5 Perioperative Transesophageal Echocardiography
2003
1. Basics of Echocardiography
(Patricia M. Applegate, Richard L. Applegate, I)
2. Clinical TEE Examination
3. Clinical Uses of Perioperative TEE
4. Unknowns
5. Perioperative
52.5 PLUMER'S PRINCIPLES & PRACTICE OF INTERAVENOUS THERAPY (SEVEN EDITION) (Sharon M. Weinstein)
ــــــ
53.5 TEE An Intractive Exam Review on CD-ROM (CD I , II) (Lippincott Williams & Wilkins)
2002
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
28 nd )54.5 TEXTBOOK OF CARDIOVASCULAR MEDICINE (2 Edition) (ERIC J. TOPOL
ــــــ
CDﺣﺎﺿﺮ ﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﻛﺘﺎﺏﻫﺎﻱ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺍﺳﺖ ﻛﻪ ﻋﻼﻭﻩ ﺑﺮ Textﺩﺍﺭﺍﻱ ﻗﺎﺑﻠﻴﺖﻫﺎﻱ ﻓﻴﻠﻢ ،ﻋﻜﺲ ﻭ ﻓﺎﻳﻞﻫﺎﻱ ﺻﻮﺗﻲ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺐ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ CDﺷﺎﻣﻞ ﻛﺘﺎﺏ ﺩﻭ ﺟﻠـﺪﻱ Text book of Cardiovascular Medicineﺍﺳـﺖ ﻛـﻪ ﻭﺟﻮﺩ ﺻﺪﻫﺎ ﻋﻜﺲ ﻭ ﻛﻠﻴﭗ ﻭﻳﺪﺋﻮﺋﻲ ﻛﺘﺎﺏ ﺭﺍ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﺠﻤﻮﻋﺔ ﺯﻧﺪﻩ ﺩﺭ ﺁﻭﺭﺩﻩ ﺍﺳﺖ) .ﺑﻪ ﻋﻨﻮﺍﻥ ﻣﺜﺎﻝ ﺩﺭ ﻣﻮﺭﺩ ﺗﻨﮕﻲ ﺩﺭﻳﭽﻪ ﻣﻴﺘﺮﺍﻝ ﺩﺭ ﺑﺨﺶ ﻣﺮﺑﻮﻃﻪ ﻋﻼﻭﻩ ﺑﺮ ﻣﺘﻦ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲ ﺩﺭ ﺿﺎﻳﻌﻪ ،ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱﻫﺎ )ﺍﻛﻮ (...ﻭ ﻓﺎﻳﻞﻫﺎﻱ ﺻﻮﺗﻲ ،ﺻﺪﺍﻱ ECG,M.Sﻭ ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ ﺁﻥ ﺑﻪ ﺻﻮﺭﺕ ﻭﻳﺪﺋﻮﻛﻠﻴﭗ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻣﺒﺎﺣﺚ ﻛﺘﺎﺏ ﺷﺎﻣﻞ : -١ﺗﺎﺭﻳﺨﭽﻪ ﻋﻠﻢ ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ -٢ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ ﭘﻴﺸﮕﻴﺮﻱ )ﺷﺎﻣﻞ :ﺑﻴﻮﻟﻮﮊﻱ ﺍﺗﺮﻭﺳﻜﻠﺮﻭﺯ ،ﺭﮊﻳﻢ ﻏﺬﺍﻳﻲ ﻭ ﭼﺎﻗﻲ ﻭ ﺍﺧﺘﻼﻻﺕ ﭼﺮﺑﻲ ،ﻭﺭﺯﺵ ،ﻓﺸﺎﺭ ﺧﻮﻥ ﻭ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺁﻥ ،ﺳﻴﮕﺎﺭ ﻛﺸﻴﺪﻥ ،ﺩﻳﺎﺑﺖ ،ﺍﺳﺘﺮﻭﮊﻥ ،ﺟﻨﺲ ﺯﻥ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺒﻲ ،ﺍﺗﺎﻧﻮﻝ ﻭ ﻗﻠﺐ ،ﺭﻓﺘﺎﺭ ﻭ ﺷﺨﺼﻴﺖ ﺑﻴﻤﺎﺭﺍﻥ ﻗﻠﺒﻲ ،ﻧﻮﺗﻮﺍﻧﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺒﻲ( -٣ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ ﺑﺎﻟﻴﻨﻲ) :ﺷﺎﻣﻞ ﺗﺎﺭﻳﺨﭽﻪ ،ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ ،ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻳﺴﻜﻤﻲ ،ﺩﺭﻳﭽﻪﺍﻱ ،ﻋﻔﻮﻧﻲ ،ﻣﺎﺩﺭﺯﺍﺩﻱ ،ﺗﻮﻣﻮﺭﺍﻝ ﻗﻠﺐ ﻭ ﭘﺮﺩﻩﻫﺎﻱ ﺁﻥ ﻣﻲﺑﺎﺷﺪ ﻫﻢ ﭼﻨﻴﻦ ﺷﺎﻣﻞ ﻗﻠﺐ ﻭ ﺣﺎﻣﻠﮕﻲ ،ﭘﻴﺮﻱ ،ﻛﻠﻴﻪ ،ﻭﺭﺯﺵ ﻭ ﺗﺮﻭﻣـﺎ ﻣـﻲﺑﺎﺷـﺪ-(. ﻣﺸﺎﻭﺭﻩ ﻧﻮﻳﺴﻲ -ﺩﺍﺭﻭﻫﺎﻱ ﻗﻠﺒﻲ -ﺍﺷﺘﺒﺎﻫﺎﺕ ﭘﺰﺷﻜﻲ -٤ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻗﻠﺒﻲ :ﺷﺎﻣﻞ ﻋﻜﺲ ﻭ ﻓﺎﻳﻞ ﺻﻮﺗﻲ ﻭ ﻭﻳﺪﺋﻮ ﻛﻠﻴﭗ) :ﺗﻔﺴـﻴﺮ ﻋﻜـﺲ ﺳـﺎﺩﻩ ﺭﻳـﻪ – ECGﺩﺭ ﺣـﻴﻦ ﻭﺭﺯﺵ – ﺍﻛﻮﻛـﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ – transthoracicﺍﺳـﺘﺮﺱ ﺍﻛﻮﻛـﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ – ﺍﺭﺯﻳـﺎﺑﻲ ﺑـﺎ ﺩﺍﭘﻠـﺮ - ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ -transesophagealﺗﻜﻨﻴﻚﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻫﺴﺘﻪﺍﻱ – CT, PET , MRIﻗﻠﺐ – ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ -٥ .( intraoperativeﺍﻟﻜﺘﺮﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ Pacingﺷﺎﻣﻞ ) :ﻣﻜﺎﻧﻴﺴﻢ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺁﺭﻳﺘﻤـﻲﻫـﺎ ،ﺗﺴـﺖﻫـﺎﻱ ﺍﻟﻜﺘﺮﻭﻓﻴﺰﻭﻟـﻮﮊﻱECG
ﺿﺎﻳﻌﺎﺕ ﻗﻠﺒﻲ ﺍﻳﺴﻜﻤﻴﻚ ﻭ ﻏﻴﺮﺍﻳﺴﻜﻤﻴﻚ ،ﻃﺮﺯ ﮔﺬﺍﺷﺘﻦ Pacemakerﻭ ﻓﻴﺒﺮﻳﻠﻴﺘﻮﺭﻫﺎ( -٦ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ invasiveﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ :ﺷﺎﻣﻞ ﻋﻜـﺲ ﻭ ﻓـﻴﻠﻢ )ﺁﻧﮋﻳـﻮﮔﺮﺍﻓﻲ ﻛﺮﻭﻧـﺮﻱ -ﻛﺎﺗﺘﺮﻳﺰﺍﺳـﻴﻮﻥ ﻗﻠﺒـﻲ Procedures ،Percutaneos ،ﺑـﺎﻱﭘـﺲ ﻗﻠـﺐ– -٨ﻛـﺎﺭﺩﻳﻮﻟﻮﮊﻱ ﻣﻠﻜـﻮﻟﻲ ﻼ ﺑﺎﻱﭘﺲ ﺷﺪﻩﺍﻧﺪ – ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ ﻭ ﺁﻧﮋﻳﻮﺳﻜﻮﭘﻲ ﻭ ﺍﻟﻮﻟﻮﭘﻼﺳﺘﻲ ،ﻃﺮﺯ ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ ﺩﺭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ﻗﻠﺒﻲ( -٧ﻧﺎﺭﺳﺎﻳﻲ ﻗﻠﺐ ﻭ ﭘﻴﻮﻧﺪ ﻗﻠﺐ Restenosisﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ﻭ ﺩﺭﻣﺎﻥ– approachﺑﻪ ﺑﻴﻤﺎﺭﺍﻥ ﻛﻪ ﻗﺒ ﹰ -٩ﻭﺍﺳﻜﻮﻟﺮ ﺑﻴﻮﻟﻮﮊﻱ :Multimedia -١٠ﺷﺎﻣﻞ ﻋﻜﺲ ﻭ ﺻﺪﺍﻫﺎﻱ ﻗﻠﺒﻲ )ﻧﺮﻣﺎﻝ ﻭ ﺍﺑﻨﺮﻣﺎﻝ( ﻭ ﻛﻠﻴﭗﻫﺎﻱ ﻭﻳﺪﻳﻮﺋﻲ. ﻋﻜﺲ :ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ – - CT/MRIﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ – - ECGﺍﻭﻟﺘﺮﺍﺳﻮﻧﻮﮔﺮﺍﻓﻲ – intravascularﻧﻮﻛﻠﺌﺎﺭ – ﭘﺎﺗﻮﻟﻮﮊﻱ – ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ – ﺟﺮﺍﺣﻲ -ﭼﺸﻢ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺒﻲ ﻋﺮﻭﻗﻲ. ﻭﻳﺪﺋﻮﻛﻠﻴﭗ :ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ – – CT/MRIﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ – ﺍﻟﻜﺘﺮﻭﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ Pacingﻭ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ – ﺗﺼﺎﻭﻳﺮ ﻫﺴﺘﻪﺍﻱ – ﺟﺮﺍﺣﻲ. •
،Endof-Life Careﻗﻠﺐ ﻭﺭﺯﺷﻜﺎﺭﺍﻥ ،ﺍﺭﺯﻳﺎﺑﻲ ﺑﺎﻟﻴﻨﻲ ،ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﺍﺗﻮﻧﻮﻡ،
.
ﺻﺪﺍﻫﺎﻱ ﻗﻠﺒﻲ :ﻧﺮﻣﺎﻝ ﻭ ﺍﺑﻨﺮﻣﺎﻝ
ﻓﺼﻞﻫﺎﻱ ﺟﺪﻳﺪ ﻛﺘﺎﺏ ﻧﺴﺒﺖ ﺑﻪ ﻭﻳﺮﺍﻳﺶ ﻗﺒﻠﻲ ﻛﺘﺎﺏ ﻭ CD
ﺷﺎﻣﻞ:
، Percutaneous Coronaryintervantionﻣﻼﺣﻈﺎﺕ ﺟﺮﺍﺣﻲ ﺩﺭ ﺩﺭﻣﺎﻥ ﻧﺎﺭﺳﺎﺋﻲ ﻗﻠﺐ ،ﮊﻥﺗﺮﺍﭘﻲ ﻭ ﭘﻴﺸﺮﻓﺖﻫﺎﻱ ﻣﻠﻜﻮﻟﻲ ﺩﺭ ﻣﻮﺭﺩ ﻗﻠﺐ
( ﻃﺮﻳﻘﻪ ﻧﺼﺐ : TEXTBOOK OF CARDIOVASCULAR MEDICINEﺑﺮﺍﻱ ﻧﺼﺐ ﺑﺮﻧﺎﻣﺔ Cardiovascular Medicineﺍﺑﺘﺪﺍ CDﺭﺍ ﺩﺭﻭﻥ ﺩﺭﺍﻳﻮ ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﻭ ﺩﺭ ﭘﻨﺠﺮﻩ ﺍﻱ ﻛﻪ ﺑﺎ ﻋﻨﻮﺍﻥ Flashﺑﺎﺯ ﺷﺪﻩ ﺑﺮ ﺭﻭﻱ ﻛـﺎﺩﺭ ﺳـﻤﺖ ﭼـﭗ ﺗﺼـﻮﻳﺮ، ﮔﺰﻳﻨﺔ Install TOPOLﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﺮﺩﻩ ﺳﭙﺲ ﭘﻨﺠﺮﺓ ﻣﺤﺎﻭﺭﻩﺍﻱ ﺩﻳﮕﺮﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ )ﺣﺪﻭﺩﹰﺍ ٣٠-٤٠ﺛﺎﻧﻴﻪ ﺑﻌﺪ( ﻭ ﻣﺴﻴﺮ ﻧﺼﺐ ﺑﺮﻧﺎﻣﻪ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﻛﻨﺪ .ﺍﻳﻦ ﻣﺴﻴﺮ ﺑﺼﻮﺭﺕ ﭘﻴﺶ ﻓﺮﺽ C:\Program files\CardioVascularMedicineﺍﺳﺖ ﺩﺭ ﻗﺴـﻤﺖ ﭘـﺎﻳﻴﻦ ﺑﺮﺭﻭﻱ ﺩﻛﻤﺔ Installﻛﻠﻴﻚ ﻛﻨﻴﺪ )ﺍﮔﺮ ﺧﻮﺍﺳﺘﻴﺪ ﻣﺴﻴﺮ ﻓﻮﻕ ﺭﺍ ﺑﻪ ﺩﻟﺨﻮﺍﻩ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺗﻐﻴﻴﺮ ﺩﻫﻴﺪ( ﭘﺲ ﺍﺯ ﻛﻠﻴﻚ ﺑﺮﺭﻭﻱ Installﭘﻨﺠﺮﺓ ﺩﻳﮕﺮﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ ﻭ ﺑﺮﻧﺎﻣﻪ ﺧﻮﺩﺑﺨﻮﺩ ﻧﺼﺐ ﻣﻲ ﺷﻮﺩ ﭘﺲ ﺍﺯ ﺣﺪﻭﺩ ٢٠ﺛﺎﻧﻴﻪ ﭘﻨﺠﺮﺓ ﺁﺧﺮ ﺑﻨـﺎﻡ Install completeﻣـﻲ ﺁﻳـﺪ ﺑـﺮﺭﻭﻱ ﺩﻛﻤﺔ Doneﺩﺭ ﺍﻧﺘﻬﺎ ﻛﻠﻴﻚ ﻛﻨﻴﺪ .ﭘﺲ ﺍﺯ ﺁﻧﻜﻪ ﻣﺮﺍﺣﻞ ﻓﻮﻕ ﺍﻧﺠﺎﻡ ﭘﺬﻳﺮﻓﺖ ﺑﺮﻧﺎﻣﻪ ﻧﺼﺐ ﺷﺪﻩ ﺍﺳﺖ ﻭﻟﻲ ﺑﺮﺍﻱ ﺍﺟﺮﺍﻱ ﺁﻥ ﻧﻴﺎﺯ ﺍﺳﺖ ﺩﻭ ﺑﺮﻧﺎﻣﺔ ﻛﻤﻜﻲ ﺩﻳﮕﺮ ﻧﻴﺰ ﺑﺮ ﺭﻭﻱ ﺳﻴﺴﺘﻢ ﻋﺎﻣﻞ ﻧﺼﺐ ﺷﻮﺩ ﻛﻪ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ .Quick Time, Internet Explorer :ﺑﺮﺍﻱ ﻧﺼـﺐ ﺍﻳـﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺯ ﺍﻳﻨﺘﺮﻧﺖ ﺍﻛﺴﭙﻠﻮﺭﺭ ﺑﺎﻭﺭﮊﻥ 5.5ﺑﻪ ﺑﺎﻻ ﻣﻲﺗﻮﺍﻥ ﺍﺳﺘﻔﺎﺩﻩ ﻛﺮﺩ .ﺿﻤﻨﹰﺎ ﺳﻴﺴﺘﻢ ﻋﺎﻣﻠﻬﺎﻱ ﭘﻴﺸﻨﻬﺎﺩﻱ ﺑﺮﺍﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻭﻳﻨﺪﻭﺯﻫﺎﻱ 2000, NT, ME, 98, 95ﺍﺳﺖ ﻳﺎ 200 MHZﭘﺮﺩﺍﺯﺷﮕﺮ ﻭ ﺣﺪﺍﻗﻞ 32ﻣﮕﺎﺑﺎﻳﺖ ﺣﺎﻓﻈﻪ. ﺩﺭ ﭘﻨﺠﺮﻩ ﺍﻱ ﻛﻪ ﭘﻴﺶ ﺭﻭﺩﺍﺭﻳﺪ )ﺍﻭﻟﻴﻦ ﭘﻨﺠﺮﻩ ﻫﻨﮕﺎﻡ ﻗﺮﺍﺭﺩﺍﺩﻥ (CDﮔﺰﻳﻨﺔ Internet Explore 5.5ﺭﺍ ﻛﻠﻴﻚ ﻛﻨﻴﺪ .ﺩﺭ ﭘﻨﺠﺮﻩ ﺍﻱ ﻛﻪ ﭘﻴﺶ ﺭﻭﻱ ﺷﻤﺎ ﺑﺎﺯ ﻣﻲ ﺷﻮﺩ ﺩﺭ ﻗﺴﻤﺖ I accept the agreementﻛﻠﻴﻚ ﻛﻨﻴﺪ ﻭ ﺩﻛﻤﺔ Nextﺍﺯ ﭘﺎﺋﻴﻦ ﺭﺍ ﻓﺸﺎﺭ ﺩﻫﻴﺪ. ﺑﺮﻧﺎﻣﻪ ﻣﺸﻐﻮﻝ ﭼﻚ ﻛﺮﺩﻥ ﺳﻴﺴﺘﻢ ﻭ ﻣﺤﺘﻮﺍﻱ ﻓﺎﻳﻞﻫﺎ ﻣﻲﺷﻮﺩ .ﺳﭙﺲ ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ ﻛﻪ ﺑﺼﻮﺭﺕ ﭘﻴﺶ ﻓﺮﺽ ﺩﻛﻤﺔ ﺑﺎﻻﻳﻲ ﻓﻌﺎﻝ ﺍﺳﺖ ﻭ ﺷﻤﺎ ﺑﺎﻳﺪ ﺩﻛﻤﺔ Nextﺭﺍ ﻓﺸﺎﺭ ﺩﻫﻴﺪ .ﺣﺎﻝ ﺑﺎﻳﺪ ﻣﻨﺘﻈﺮ ﺑﻤﺎﻧﻴﺪ ﺗﺎ ﺑﺮﻧﺎﻣﻪ ﺑﺼـﻮﺭﺕ ﻛﺎﻣـﻞ ﻧﺼـﺐ ﮔـﺮﺩﺩ ﺳـﭙﺲ ﭘﻨﺠـﺮﺓ ﺩﻳﮕﺮﻱ ﺑﺎﺯ ﺷﺪﻩ ﺩﻭﺑﺎﺭﻩ Nextﺭﺍ ﻓﺸﺎﺭ ﺩﺍﺩﻩ ﻭ ﺩﻛﻤﺔ finishﺩﺭ ﺍﻧﺘﻬﺎ ﺯﺩﻩ ﺷﻮﺩ .ﺩﺭ ﺍﻳﻦ ﻣﻮﻗﻊ ﻭﻳﻨﺪﻭﺯ ﺧﻮﺩﺑﺨﻮﺩ restartﻣﻲﺷﻮﺩ .ﺩﻭﺑﺎﺭﻩ CDﺭﺍ ﺍﺟﺮﺍ ﻛﻨﻴﺪ )ﺍﻳﻦ ﻛﺎﺭ ﺭﺍ ﻣﻲ ﺗﻮﺍﻧﻴﺪ ﺑﺎ ﺯﺩﻥ ﺩﻛﻤﺔ Ejectﺩﺭﺍﻳﻮ CDﻭ ﻓﺸﺮﺩﻥ ﻣﺠﺪﺩ CDﺑﻪ ﺩﺭﻭﻥ ﺩﺭﺍﻳﻮ ﻭ ﻳﺎ ﺑـﺎﺯ ﻛـﺮﺩﻥ CDﻭ ﺍﺟﺮﺍﻱ ﺁﻥ ﺍﻧﺠﺎﻡ ﺩﻫﻴﺪ( ﺣﺎﻝ ﺑﻪ ﻗﺴﻤﺖ ﺳﻮﻡ ﻧﺼﺐ ﻣﻲﺭﺳﻴﻢ .ﺑﺎﻳﺪ ﺍﺯ ﭘﻨﺠﺮﺓ ﺑﺎﺯﺷﺪﻩ )ﭘﻨﺠﺮﺓ ﺍﻭﻝ ﻫﻨﮕﺎﻡ ﻗﺮﺍﺭﺩﺍﺩﻥ ( CDﺑﺮ ﺭﻭﻱ ﮔﺰﻳﻨﺔ Quick time 5ﻛﻠﻴﻚ ﻛﻨﻴﻢ .ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪﻱ ﻣﻲﺁﻳﺪ ﺩﻛﻤﺔ Nextﺭﺍ ﻓﺸﺎﺭ ﻣﻲ ﺩﻫﻴﻢ .ﭘﻨﺠﺮﺓ ﺑﻌﺪﻱ ﻫﻢ ﺑﺎﻳﺪ Nextﺭﺍ ﺑﺰﻧﻴﺪ ﺗﺎ ﭘﻨﺠﺮﺓ ﺩﻳﮕﺮﻱ ﺑﺎﺯ ﺷﻮﺩ ﺣﺎﻝ ﺩﻛﻤﺔ Agreeﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ ﻣﺴﻴﺮﻱ ﺭﺍ ﻣﻲ ﺑﻴﻨﻴﻢ ﺍﮔﺮ ﻣﻮﺍﻓﻖ ﺑﻮﺩﻳﺪ Nextﺭﺍ ﺑﺰﻧﻴﺪ ﻭ ﺩﺭ ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪ ﺑﺼﻮﺭﺕ ﭘﻴﺶ ﻓﺮﺽ ﺩﻛﻤﺔ ﺩﻭﻡ ﺍﺯ ﺑﻴﻦ ﺳﻪ ﺩﻛﻤﻪ ﺩﺭ ﺑﺎﻻﻱ ﻛﺎﺩﺭ ﻓﻌﺎﻝ ﺍﺳﺖ ﻣﺠﺪﺩﹰﺍ Nextﺭﺍ ﺑﺰﻧﻴﺪ ﻭ ﺑﺎﺯ ﻧﻴﺰ Nextﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ ﺩﺭ ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪ ﻧﻴﺰ Nextﺭﺍ ﻓﺸﺎﺭ ﺩﻫﻴﺪ ﭘﻨﺠﺮﺓ ﺑﻌﺪﻱ ﺳﺮﻳﺎﻝ ﻭ ﻧﺎﻡ ﺷﺮﻛﺖ ﺭﺍ ﻣﻲﭘﺮﺳﺪ ﻧﻴﺎﺯﻱ ﺑﻪ ﭘﺮﻛﺮﺩﻥ ﺁﻥ ﻧﻴﺴﺖ Nextﺭﺍ ﺯﺩﻩ ﺗﺎ ﺑﺮﻧﺎﻣﻪ ﻧﺼﺐ ﺷﻮﺩ ﺑﺮ ﺭﻭﻱ ﭘﻨﺠﺮﺓ ﻓﻌﺎﻝ ﻣﺎ ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ ﺁﻥ ﺭﺍ ﻧﻴﺰ Nextﺑﺰﻧﻴﺪ ﺩﻭ ﺑﺎﺭﻛﻪ Nextﻛﺮﺩﻳﺪ ﺍﻳﻦ ﭘﻨﺠﺮﻩ ﺭﺍ finishﻛﻨﻴﺪ ﺗﺎ ﺑﻪ ﭘﺎﻳﺎﻥ ﻛﺎﺭ ﺑﺮﺳﻴﻢ ﺁﺧﺮﻳﻦ ﭘﻨﺠﺮﻩ ﺭﺍ ﺑﺎ ﺑﺮﺩﺍﺷﺘﻦ ﺗﻴﻚﻫﺎﻱ ﺩﻭ ﻛﺎﺩﺭ ﺑﺎﻻ Closeﻛﻨﻴﺪ .ﺗﻤﺎﻡ ﭘﻨﺠﺮﻩ ﻫﺎ ﺭﺍ ﺑﺮﺭﻭﻱ ﺻـﻔﺤﺔ Desktopﺑﺒﻨﺪﻳـﺪ ﺑـﺮﺭﻭﻱ ﺩﻛﻤـﺔ Startﻛﻠﻴـﻚ ﻛـﺮﺩﻩ ﻭﺍﺭﺩ Programsﺷـﻮﻳﺪ ﻭ ﺍﺯ ﻣﻨـﻮﻱ Cardio Vascular Medicineﺑﺮﻧﺎﻣـﺔ Cardio Vascular CDﺭﺍ ﺍﺟﺮﺍ ﻛﻨﻴﺪ ﻭ ﺳﭙﺲ ﺑﺮﻧﺎﻣﺔ internet explorerﺭﺍ ﺑﺎﺯ ﻛﺮﺩﻩ ﻭ ﺩﺭ ﻗﺴﻤﺖ Addressﺧﻂ ﺯﻳﺮ ﺭﺍ ﺗﺎﻳﭗ ﻛﻨﻴﺪ .ﺑﺮﻧﺎﻣﻪ ﺩﺭ ﻣﺤﻴﻂ internet explorerﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ. http://127.0.0.1:83/PCIndex.htm.
2003 ــــــ
)Images from the Netter Collection (NOVARTIS )(John Michael Criley, M.D., Conrad Zalace, David Creley Catalog of Lesions yNormal yValvar Lesions yPericardial Disease
Timing of Murmurs ySystolic Murmurs yDiastolic Murmurs yContinuous Murmurs vs. “To and Fro” Murmurs
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
The Netter Presenter Cardiovascular and Renal Edition
55.5
56.5 The Physiological Orgins of HEART SOUNDS and MURMUS
Timing of Heart Sounds yValve Closure Sounds and Splitting of Sounds yOpening Sounds yThird Sounds
General Tutorials: yInspection and Palpation yIntriduction to Auscultation yEffect of Maneuvers and Perturbations
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
29 yCongenital Heart Disease yCardiomyopathies yMyxoma
ــــــ
ــــــ
yFriction Rubs
yFourth sounds yEjection Sounds yMid-Systolic Clicks
)(LAWRENCE S. COHEN, M.D, JOHN ELEFTERIADES, M.D.) (VCD
yHemoduction to Cardiac Imaging Modalities
57.5 VJC Video Journal of Cardiology
1. From a new perspective: mitral valve prolapse aortic dissections and aneurysms 2. Surgical and medical management of ascending and descending aortic dissections liporoten (A): a cardiovascular risk factor )58.5 VJC Video Journal of Cardiology (Christopher White, M.D, Michael E. Cain, M.D., Bruce D. Lindsay, M.D., Herbert Geschwind, M.D.) (VCD ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺯ ﺳﺮﻱ CDﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ VJCﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺩﺭ ﻗﺎﻟﺐ VCDﺑﻪ ﻣﺪﺕ 50ﺩﻗﻴﻘﻪ ﺩﺭ ﺳﻪ ﺑﺨﺶ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻳﻚ ﻣﻮﺿﻮﻉ ﺑﻪ ﺷﻜﻞ ﻣﺼﺎﺣﺒﺔ ﻋﻠﻤﻲ ﺑﺎ ﻳﻚ ﻣﺘﺨﺼﺺ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﻭ ﻓـﻴﻠﻢ ﻭ ﻧﻤﻮﺩﺍﺭﻫـﺎﻱ ﻣﺘﻌﺪﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺷﺪﻩ ﺍﺳﺖ .ﻣﻮﺿﻮﻋﺎﺕ ﻫﺮ ﺑﺨﺶ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ: ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ :ﺩﻛﺘﺮchristoher white : 1-Cold lege : The Approach to Acvte and progressive Peripheral Vascular Disease ﻋﻮﺍﺭﺽ ﻣﺮﺑﻮﻁ ﺑﻪ ﻋﺮﻭﻕ ﻣﺤﻴﻄﻲ ﻭ ﺭﻭﺷﻬﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺁﻧﻬﺎ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ .ﻣﺮﺍﺣﻞ ﺍﻧﺠﺎﻡ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﺗﺼﺎﻭﻳﺮ ﺁﻧﮋﻳﻮﺳﻜﻮﭘﻴﻚ ﻭ ﺁﻧﮋﻳﻮﮔﺮﺍﻡ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﻣﺼﺎﺣﻴﻪ ﺷﻮﻧﺪﻩ :ﺩﻛﺘﺮ Michael E. Cain :
Urokinase
،ﺍﺳﺘﺮﭘﺘﻮﻛﻴﻨﺎﺯ ،ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ﻟﻴﺰﺭﻱ ﻭ ....ﻧﻴﺰ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ.
2- RADiofrgvency ablation : Ablation of AVNode reentry tachycardias
ﺍﻟﻜﺘﺮﻭﻛﺎﺭﺩﻭﻳﻮﮔﺮﺍﻡ ﺑﺎﻟﻴﺪﮔﺬﺍﺭﻱﻫﺎﻱ ﻣﺨﺘﻠﻒECG ،ﻫﺎﻱ ﺩﺭ ﻓﻴﺒﺮﻳﻼﺳﻴﻮﻥ ﻭ ﺑﻠﻮﻙ AVﻭ ...ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪﻫﺎ ﻭ ﺭﺍﺩﻳﻮﮔﺮﺍﻡﻫﺎﻱ ﻣﺘﻌﺪﺩ ﺑﺮﺭﺳﻲ ﻭ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ :ﺩﻛﺘﺮHerbert Geschwind :
3- Laser Angioplasty for coronary Atherosclerotic Disease
ﻣﻜﺎﻧﻴﺰﻡ ﻋﻤﻞ ﺳﻴﺴﺘﻢ ﻟﻴﺰﺭ ﺩﺭ ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ،ﻛﺎﺭﺑﺮﺩ Pulserﻃﻮﻝ ﺑﺮﺝ ﺑﻬﻤﻴﻨﻪ ) ﻣﺎﻭﺭﺍﺀ ﻣﺎﺩﻭﻥ ﻗﺮﻣﺰ( ﺍﻫﺪﺍﻑ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ﻟﻴﺰﺭﻱ ﻭ ﻋﻮﺍﺭﺽ ﺁﻥ ﻣﺰﻳﺖ ﻫﺎ ﻭ ﻣﺤﺪﻭﺩﻳﺖﻫﺎ ﺍﻳﻦ ﺭﻭﺵ ﻭ ﻣﻘﺎﻳﺴﻪ ﺁﻥ ﺑﺎ PTCAﻭ ....ﻣﻮﺭﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. -٦ﭘﻮﺳﺖ ﻭ ﻣﻮ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ 2001
ﻋﻨﻮﺍﻥ CD )American Cancer Society Atlas of Clinical Oncology Skin Cancer (Arthur J. Sober, MD, Frank G. Haluka, MD, phD) (Bc Decker Inc
1.6
ﻫﻤﭽﻨﺎﻧﻜﻪ ﻭﺍﺭﺩ ﻗﺮﻥ ٢١ﻣﻲﺷﻮﻳﻢ ﺷﺎﻳﻊﺗﺮﻳﻦ ﺷﻜﻞ ﺳﺮﻃﺎﻥﻫﺎ ،ﻛﺎﻧﺴﺮﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻣﻲﺑﺎﺷﺪ ﻭ ﺑﻪ ﻋﻠﺖ ﺍﻳﻨﻜﻪ ﺑﺮ ﺧﻼﻑ ﻛﺎﻧﺴﺮﻫﺎﻱ ﺩﻳﮕﺮ ،ﻛﺎﻧﺴﺮﻫﺎﻱ ﭘﻮﺳﺖ ﺩﺭ ﻣﻌﺮﺽ ﺩﻳﺪ ﻣﻲﺑﺎﺷﺪ ﺳﺮﻳﻌﺘﺮ ﻭ ﺭﺍﺣﺖﺗﺮ ﻗﺎﺑـﻞ ﺗﺸـﺨﻴﺺ ﺍﺳـﺖ .ﺩﺭ ﻧﺘﻴﺠـﻪ ﺩﺍﻧـﺶ ﺗﺸـﺨﻴﺺ ﻭ ﺩﺭﻣـﺎﻥ ﻭ ﺟﻠﻮﮔﻴﺮﻱ ﺍﺯ ﺳﺮﻃﺎﻥﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻣﻮﺟﺐ ﻧﮕﺎﺭﺵ ﺍﻳﻦ ﻛﺘﺎﺏ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﻣﺸﺨﺼﺔ ﺍﻳﻦ ﻛﺘﺎﺏ ﺗﺄﻛﻴﺪ ﺑﺮ ﻧﻤﺎﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ Skin cancerﻣﻲﺑﺎﺷﺪ ﭼﻮﻥ ﻋﻠﻢ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﺮ ﭘﺎﻳﺔ ﻣﺸﺎﻫﺪﻩ ﺑﻨﺎ ﺷﺪﻩ ﺍﺳﺖ ،ﺑﻨﺎﺑﺮﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺍﺭﺍﻱ ﺗﺼﺎﻭﻳﺮ ﺯﻳﺎﺩ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺴﻴﺎﺭ ﺑﺎﻻﺳﺖ ﻭ ﻫﺮ ﺟﺎ ﻛﻪ ﻋﻜﺲﻫﺎ ﺩﺭ ﺍﺭﺍﺋﻪ ﻣﻄﻠﺐ ﻛﻤﻚﻛﻨﻨﺪﻩ ﻧﺒﻮﺩﻩ textﺍﺿﺎﻓﻪ ﺷﺪﻩ ﺍﺳﺖ .ﻭ ﻋﻼﻭﻩ ﺑﺮ ﺍﻳﻦ ﻧﻜﺎﺕ ﺗﺸﺨﻴﺼﻲ ،ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ،ﺩﺭﻣﺎﻧﻲ ﻭ ﭘﻴﺸﮕﻴﺮﻱ ﺩﺭ ﻛﺘﺎﺏ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ٤ﻗﺴﻤﺖ ﺗﻘﺴﻴﻢ ﺷﺪﻩ ﺍﺳﺖ: ﺑﺨﺶ Basic Concept :١ﺷﺎﻣﻞ ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ،ﮊﻧﺘﻴﻚ ﻛﺎﻧﺴﺮﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻭ ﻋﻮﺍﻣﻞ ﺧﻄﺮﺯﺍ ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ :٢ﺗﻈﺎﻫﺮﺍﺕ ﺑﺎﻟﻴﻨﻲ :ﺩﺭ ﻫﺮ ﻓﺼﻞ ﺟﺪﺍﮔﺎﻧﻪ ﻧﻤﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ (٤ﻭ ) BCEﻓﺼﻞ (٥ﻭ ) Sccﻓﺼﻞ (٦ﻟﻤﻔﻮﻡﻫﺎﻱ ﭘﻮﺳﺘﻲ )ﻓﺼﻞ (٧ﻭ ﻣﺎﻟﻴﻨﮕﻨﺎﻧﺴﻲﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻧﺎﺷﺎﻳﻊ )ﻓﺼﻞ ) Merckle cell Carcinoma (٨:١ﻓﺼﻞ ( ٨:٢ﻭ ﻛﺎﭘﻮﺳﻲ ﺳﺎﺭﻛﻮﻡ )ﻓﺼﻞ (٨:٣ﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺑﺨﺶ Management : ٣ﻛﻪ ﺷﺎﻣﻞ :ﺗﻜﻨﻴﻚ ﺑﻴﻮﭘﺴﻲ ﺍﺯ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ ، (٩ﺗﺪﺍﺑﻴﺮ ﺟﺮﺍﺣﻲ ﻣﻼﻧﻮﻡ ﭘﻮﺳﺘﻲ )ﻓﺼﻞ ،(١١ﺍﺭﺯﻳﺎﺑﻲ ﻟﻤﻒﻧﻮﺩﻫﺎ ﻭ ﺑﻴﻮﭘﺴﻲ ﺍﺯ ﻟﻤﻒﻧﻮﺩ ﺩﺭ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ adjuvant therapy ،(١١ﺩﺭ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ ،(١٢ﺍﻳﻤﻮﻧـﻮﺗﺮﺍﭘﻲ ﺩﺭ ﻣﻼﻧـﻮﻡ )ﻓﺼـﻞ (١٣ﻭ ﻛﻤـﻮﺗﺮﺍﭘﻲ ،ﺳـﻴﺘﻮﻛﻴﻦ ﺗﺮﺍﭘﻲ ﻭ ﺑﻴﻮﻛﻤﻮﺗﺮﺍﭘﻲ ﺩﺭ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ (١٤ﻣﻲﺑﺎﺷﺪ .ﻫﻤﭽﻨﻴﻦ ﺩﺭﻣﺎﻥ ﻟﻤﻔﻮﻡ ﭘﻮﺳﺘﻲ ﺍﻭﻟﻴﻪ ]) [MFﻓﺼﻞ (١٧ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ : ٤ﺩﺭ ﻣﻮﺭﺩ ﭘﻴﺸﮕﻴﺮﻱ ﺍﺯ ﻛﺎﻧﺴﺮﻫﺎﻱ ﭘﻮﺳﺘﻲ ﺑﺤﺚ ﻛﺮﺩﻩ ﺍﺳﺖ. )AQUAMIDE; Poly Acryl Amide Ged (an injectable gel for correction of soft Tissue Deficiencies
ــــــ
2.6
ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ CDﺩﺭ ﻣﻮﺭﺩ ﻳﻜﻲ ﺍﺯ ﻣﻮﺍﺩ fillerﺑﻪ ﻛﺎﺭ ﺭﻓﺘﻪ ﺩﺭ Cosmetic Surgeryﺗﻮﺿﻴﺤﺎﺗﻲ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﺑﺘﺪﺍ ﺧﻮﺍﺹ ﮊﻝ Aquamideﻭ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺁﻥ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﺳﭙﺲ ﻃﺮﻳﻘﻪ ﺗﺰﺭﻳﻖ ﺍﻳﻦ ﮊﻝ ﺩﺭ ﺍﺻﻼﺡ ﭼﻴﻦ ﻧﺎﺯﻭﺑﻴﺎﻝ ،ﺗﻐﻴﻴﺮ ﺷﻜﻞ ﻧﺎﻫﻨﺠﺎﺭﻱﻫﺎﻱ ﺑﻴﻨﻲ ،ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﭼﻴﻦﻫﺎﻱ ﭘﻴﺸﺎﻧﻲ ﻭ ﺍﻃﺮﺍﻑ ﻟﺐ ،ﭘﺮﻛﺮﺩﻥ ﻭ ﺍﺻﻼﺡ ﺿﺎﻳﻌﺎﺕ ﺁﺗﺮﻭﻓﻴﻚ ﻧﺎﺷﻲ ﺍﺯ ﺍﺳﻜﺎﺭ ﺁﺑﻠﻪﻣﺮﻏﺎﻥ ﻳﺎ ﺗﺮﻭﻣﺎﻫﺎ ،ﮔﻮﻧﻪﮔﺬﺍﺭﻱ ﻭ ﺧﻂ ﻟﺐ ﺑﻪ ﺻﻮﺭﺕ ﻧﻮﺍﺭ ﻭﻳﺪﺋﻮﺋﻲ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. 2002
)ATLAS OF COSMETIC SURGERY (MICHAEL S. KAMINER, MD, JEFFREY S. DOVER, MD, FRCPC, KENNETH A. ARNDT, MD) (W.B. SAUNDERS COMPANY) (Salekan E-Book ﺍﻃﻠﺲ ﺣﺎﺿﺮ ﺗﺄﻟﻴﻒ ﺩﻳﮕﺮﻱ ﺍﺯ Dr. Kenneth. Arndtﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻣﻘﺪﻣﻪ ﻛﺘﺎﺏ ) Dr. Leffellﺍﺳﺘﺎﺩ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺩﺍﻧﺸﮕﺎﻩ (Yaleﻣﻲﻧﻮﻳﺴﺪ"' :ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻓﻮﻕﺍﻟﻌﺎﺩﻩ ﺟﻤﻊﺁﻭﺭﻱ ﺗﺠﺎﺭﺏ ﻣﺆﻟﻔﻴﻦ ﺑﻮﺩﻩ ﻭ ﺑﻴﺸﺘﺮ ﺑﻪ ﻣـﻮﺍﺭﺩ ﻛـﺎﺭﺑﺮﺩﻱ ﺍﺷـﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ ﺑﻪ ﻃﻮﺭﻳﻜﻪ ﺑﻪ ﺷﻤﺎ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ﭼﮕﻮﻧﻪ ﺑﺎ ﻣﻮﻓﻘﻴﺖ ﻳﻚ ﻋﻤﻞ Cosmeticﺭﺍ ﺑﺮ ﺭﻭﻱ ﺑﻴﻤﺎﺭ ﺧﻮﺩ ﺍﻧﺠﺎﻡ ﺩﻫﻴﺪ Dr. Arndt .ﺳﺮﺩﺑﻴﺮ ﻣﺠﻠﻪ Archives of Dermatologyﺗﻘﺮﻳﺒﹰﺎ ﺑﻪ ﻣﺪﺕ ٢٠ﺳـﺎﻝ ﺍﺣﺎﻃـﺔ ﻭﺳـﻴﻌﻲ ﺩﺭ ﺟﺮﺍﺣـﻲﻫـﺎﻱ Cosmeticﺩﺍﺷـﺘﻪ ﻭ ﺩﺭ
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
3.6
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
30 ﺷﻜﻴﻞﺑﻮﺩﻥ ﻛﺘﺎﺏ ﺳﻬﻢ ﺑﺴﺰﺍﻳﻲ ﺩﺍﺭﺩ" ﻭﻳﮋﮔﻲ ﺍﻳﻦ ﻛﺘﺎﺏ ﻧﺴﺒﺖ ﺑﻪ ﻣﻮﺍﺭﺩ ﻣﺸﺎﺑﻪ ،ﺗﺠﺮﺑﻴﺎﺕ ﻣﺆﻟﻔﻴﻦ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻫﻤﮕﻲ ﺑﻪ ﻋﻨﻮﺍﻥ ﺭﻓﺮﺍﻧﺲ ﺩﻳﮕﺮ ﻛﺘﺐ ﻭ ﻣﺠﻼﺕ ﭘﺰﺷﻜﻲ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﺩ )ﺑﺮﺍﻱ ﻣﺜﺎﻝ ﭼﮕﻮﻧﮕﻲ ﺗﺰﺭﻳﻖ Botoxﻭ ﺩﺭﻣﺎﻥ ﺍﺳـﻜﺎﺭﻫﺎﻱ ﺁﻛﻨـﻪ ﻛـﻪ ﺩﺭ ﻣﺠـﻼﺕ ﻼ ﻣﺠﻬﺰ( ﺑﻴﺎﻥ ﻧﻤﻮﺩﻩﺍﻧﺪ .ﺑﺮﺍﻱ ﻣﺜﺎﻝ ﻣﺒﺎﺣﺚ ﺗﺰﺭﻳﻖ ، Botoxﻟﻴﺰﺭﺩﺭﻣـﺎﻧﻲ Archiveﻭ 2001 AADﻭ 2002ﭼﺎﭖ ﺷﺪﻩ ﺍﺳﺖ( ﻣﺆﻟﻔﻴﻦ ﻫﺪﻑ ﺍﺯ ﺗﺄﻟﻴﻒ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﺑﻴﺎﻥ ﺗﺠﺮﺑﻴﺎﺕ ﻛﺎﺭﺑﺮﺩﻱ ﺧﻮﺩ ﺩﺭ ﺑﻴﻤﺎﺭﺳﺘﺎﻥ ) Harvardﺑﺎ ١٣ﻟﻴﺰﺭ ﭘﻮﺳﺖ ﻭ ١٢ﺍﻃﺎﻕ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﻛﺎﻣ ﹰ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﻭ Scar managementﻭ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﺍﻳﻦ ﻛﺘﺎﺏ ﻛﺎﺭﺑﺮﺩﻱﺗﺮﻳﻦ ﻭ ﺑﻪ ﺍﺫﻋﺎﻥ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺩﺳﺘﻴﺎﺭﺍﻥ ﭘﻮﺳﺖ ﺑﻬﺘﺮﻳﻦ ﻛﺘﺎﺏ ﭼﺎﭖ ﺷﺪﻩ ﺩﺭ ﺍﻳﻦ ﻣﻮﺭﺩ ﻣﻲﺑﺎﺷﺪ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺷﻜﻞﻫﺎﻱ ﺳﺎﺩﻩ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻭ ﺑﻌﻀﹰﺎ ﺭﻧﮕﻲ ﺑﻪ ﻛﻴﻔﻴﺖ ﻭ ﺭﺍﺣﺘﻲ ﺁﻣﻮﺯﺵ ﺗﻜﻨﻴﻚﻫﺎ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ﻛﺮﺩﻩ ﺍﺳﺖ .ﻛﺘﺎﺏ Laser in Dermatologyﻣﺆﻟﻒ " "Kenneth, Arndtﺑﺰﻭﺩﻱ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ .ﺍﻳﻦ ﻛﺘﺎﺏ ﻣﻨﺤﺼﺮﺑﻪ ﻓﺮﺩ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: PART III COSMETIC SURGERY PROCEDURES AND TECHNIQUES 10 Topical Skin Care 11 Lasers in the Treatment of Vascular Lesions 12 Lasers in the Treatment of Pigmented Lesions 13 Laser Hair Removal 14 Liposuction 15 Hair Transplantation 16 Soft Tissue Augmentation 17 Botulinum A Exotoxin Injections for Photoaging and Hyperhidrosis, 18 Chemical Peels 19 Lasers in Skin Resurfacing 20 Blepharoplasty 21 Surgical Rhytidectomy: Face Lifts and the Endoscopic Forehead Lift 22 Leg Vein Management: Sclerotherapy, Ambulatory Phlebectomy, and Laser Surgery 23 Scar Management: Keloid, Hypertrophic, Atrophic, and Acne Scars
PART I EVALUATION OF THE COSMETIC SURGERY PATIENT 1 The History of Cosmetic Surgery 2 The History of Cosmetic Dermatologic Surgery 3 Evaluation of the Aging Face, 4 Photoaging: Mechanisms, Consequences, and Prevention 5 Beauty and Society 6 Psychosocial Issues and Their Relevance to the Cosmetic Surgery Patient PART II ANESTHESIA 7 Regional Anesthesia for Aesthetic Surgery 8 Office-Based Sedation and Monitoring 9 Postoperative Pain and Nausea Management
)(CD I , II
ــــــ
)(SALEKAN E-BOOK
)Atlas of Dermatology (Jhon's Hopkins
4.6
ﻼ ﺟﺎﻟﺐ ﺑﺎ ﺭﺯﻭﻟﻮﺷﻦ ﺑﺎﻻ ﺩﺭ ﺧﺼﻮﺹ ﺍﻧﻮﺍﻉ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮ ﻃﺒﻖ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎ Sortﮔﺮﺩﻳﺪﻩ ﻭ ﻣﺤﺼﻮﻝ ﺳﺎﻝ ٢٠٠٣ﺩﺍﻧﺸﮕﺎﻩ Jhon's Hopkinsﻣﻲﺑﺎﺷﺪ. ﺍﻃﻠﺲ ﻓﻮﻕ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ٢٥٠٠ﺗﺼﻮﻳﺮ ﻛﺎﻣ ﹰ 1999
)Atlas of Dermatology (T.L.Diepgen, M. Simon, A. Bittorf, M. Fartasch, G. Schuler) (with the DOIA team G. Eysenbach, J. Bauer, A. Sager) (springer
5.6
ــــــ
ﺗﺎﺭﻳﺨﭽﺔ ﺍﻃﻠﺲ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﺮﻣﻲﮔﺮﺩﺩ ﺑﻪ ﺳﺎﻝ ، ١٩٩٤ﻛﻪ ﺷﺒﻜﺔ ﺳﺮﺍﺳﺮﻱ ﺟﻬﺎﻧﻲ ﺍﻧﻴﺘﺮﻧﺖ ) (wwwﺍﻳﺠﺎﺩ ﺷﺪ .ﺍﺯ ﺁﻥ ﺳﺎﻝ ﺑﻪ ﺑﻌﺪ ﺍﺯ ﺳﺮﺍﺳﺮ ﺟﻬﺎﻥ ﺗﺼﺎﻭﻳﺮ ﺿﺎﻳﻌﺎﺕ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺩﺭ ﺍﻳﻦ ﺷﺒﻜﻪ ﺩﺭ ﻣﺤﻞ (DOIA) Dermatology online Atlasﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ﺳﺎﻳﺖ ﺍﻳﻨﺘﺮﻧﺘﻲ ﻋﻼﻭﻩ ﺑﺮ ٣٠٠٠ﺗﺼﺮﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺴﻴﺎﺭ ﺑﺎﻻﻱ ﺑﻴﺶ ﺍﺯ 600 DPIﺗﺸﺨﻴﺺ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ،ﺍﺭﺍﺋﻪ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ Case report ،ﺻﻮﺗﻲ ﻭ ...ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻨﺎﺑﺮﺍﻳﻦ ﺍﻃﻠﺲ ﻓﻮﻕ ﺑﻪ ﺻـﻮﺭﺕ Offlineﺍﺯ DOIAﺗﻬﻴـﻪ ﺷـﺪﻩ ﻛـﻪ ﻗﺎﺑﻠﻴـﺖ ﺍﺗﺼﺎﻝ ﺩﺭ ﻫﺮ ﺯﻣﺎﻥ ﺑﻪ ﺻﻮﺭﺕ onlineﺭﺍ ﺩﺍﺭﺩ. )Atlas of Differential Diagnosis in DERMATOLOGY (Klaus F. Helm, M.D., James G. Marks, Jr., M.D.
6.6
2003 ــــــ
ﺍﻳﻦ CDﺑﺮ ﺧﻼﻑ ﺍﻃﻠﺲﻫﺎﻱ ﺩﻳﮕﺮ ﻛﻪ ﺑﻴﻤﺎﺭﻱﻫﺎ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎﻳﻲ ﻳﺎ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﻛﺮﺩﻩ ﺗﺄﻛﻴﺪ ﺑﻴﺸﺘﺮ ﺑﻪ ﺗﺸﺨﻴﺺ ﺑﺎﻟﻴﻨﻲ ﻭ ﺍﻓﺘﺮﺍﻕ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﺯ ﻳﻜﺪﻳﮕﺮ ﺑﻪ ﺻﻮﺭﺕ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﺩﺍﺭﺩ .ﺑﻪ ﻃﺮﻳﻜﻪ ﺩﺭ ﻣﻮﺭﺩ ﺗﺸﺨﻴﺺ ﻳـﻚ ﺑﻴﻤﺎﺭ ﺗﺼﺎﻭﻳﺮ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺩﻳﮕﺮ ﻛﻪ ﺑﺎ ﺁﻥ ﺑﻴﻤﺎﺭﻳﻴﻲ ﺍﺷﺘﺒﺎﻩ ﻣﻲﺷﻮﺩ ﮔﺮﺩﺁﻭﺭﻱ ﺷﺪﻩ ﻭ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﺍﻃﻠﺲ Problem-orientedﺗﻨﻈﻴﻢ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ CDﺭﺍﺵﻫﺎ ﻭ ﻧﺌﻮﭘﻼﺳﻢﻫﺎ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﺷﻜﻞ ﻭ ﻣﺤﻞ ﺑﻪ ١٦ﻓﺼﻞ ﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﺷﺪﻩ ﺩﺭ ﺍﻭﻝ ﻫﺮ ﻓﺼـﻞ ﺍﺑﺘـﺮﺍ ﺍﻟﮕﻮﺭﻳﺘﻢ ﺭﺳﻴﺪﻥ ﺑﻪ ﺗﺸﺨﻴﺺ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪ ﻭ ﺳﭙﺲ ﺩﺭ ﺟﺪﺍﻭﻝ ﻣﻘﺎﻳﺴﻪﺍﺱ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻴﻬﺎﻱ ﺍﻳﻦ ﺿﺎﻳﻌﺎﺕ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺳﭙﺲ ﺗﺼﺎﻭﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺑﻪ ﺻﻮﺭﺕ ﻣﻘﺎﻳﺴﻪﺍﻱ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﺩﺭ ﺁﺧﺮ ﻫﺮ ﻓﺼﻞ ﻧﻴﺰ ﺍﺗﻴﻮﻟﻮﮊﻱ ،ﻧﻜﺎﺕ ﻣﻬﻢ ﺑﺎﻟﻴﻨﻲ ﻭ ﺩﺭﻣـﺎﻥ ﺑﺮﺍﻱ ﻫﺮ ﺑﻴﻤﺎﺭﻱ ﺑﻪ ﺻﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ CDﺩﺭ ﺑﺮﻧﺎﻣﻪ Acrobat readerﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﺑﺘﺪﺍ ﻳﻚ ﺑﺮﻧﺎﻣﻪ ﻣﺎﻟﺘﻲ ﻣﺪﻳﺎ ) ﺑﻪ ﺻﻮﺭﺕ (animationﺑﺮﺍﻱ ﺁﺷﻨﺎﻳﻲ ﺑﺎ ﻣﺤﺘﻮﻳﺎﺕ CDﻭ ﭼﮕﻮﻧﮕﻲ ﻛﺎﺭ ﺍﺭﺍﺋﻪ ﺷـﺪﻩ ﺍﺳـﺖ .ﺩﺭ ﺍﻳـﻦ image gallery .CDﻭﺟـﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﺗﺼﺎﻭﻳﺮ ﺑﺪﻭﻥ ﺗﻮﺿﻴﺢ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﻭ ﺍﺯ ﺁﻥ ﺑﻪ ﻋﻨﻮﺍﻥ quizﻭ ﺍﺭﺯﻳﺎﺑﻲ ﺷﺨﺼﻲ ﻣﻲﺗﻮﺍﻥ ﺍﺳﺘﻔﺎﺩﻩ ﻛﺮﺩ .ﺍﺯ index inconﻛﻪ ﺑﺮ ﺍﺳﺎﺱ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎﻱ ﺍﻧﮕﻠﻴﺴﻲ ﺑﻨﺎ ﺷﺪﻩ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺭﺍﺣﺘﻲ ﺑﺮﺍﻱ ﺟﺴﺘﺠﻮﻱ ﻣﻮﺿﻮﻉ ﺑﻴﻤﺎﺭﻱ ﻛﻤﻚ ﮔﺮﻓﺖ. )Botulinum Toxin Aesthetic Indications (Mauricio de Maio, Segio Talarico, Benjamin Ascher, Nam Ho Kim South )Color Atlas and synopsis of Clinical Dermatology Common and Serious Diseases Thomas B. (Fitzpatrick, M.D. Richard Allen Johnson, M.D. Dick Suurmond, M.D
7.6 8.6
ﺍﻳﻦ ﺍﻃﻠﺲ ﺑﺎ ٦٨٠ﺗﺼﻮﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﻣﻮﺟﺐ ﻛﻤﻚ ﺩﺭ ﺗﺸﺨﻴﺺ ﺑﻪ ﻭﺳﻴﻠﺔ ﻓﺮﺍﻫﻢ ﻛﺮﺩﻥ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﺑﺰﺭﮒ ﻭ ﻛﻴﻔﻴﺖ ﻋﺎﻟﻲ ﻣﻲﺑﺎﺷﺪ .ﻫﻤﭽﻨﻴﻦ ﺧﻼﺻﻪﺍﻱ ﺍﺯ ﺗﻈﺎﻫﺮﺍﺕ ﺍﺻﻠﻲ ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ﻭ ﺍﻧﺘﻴﻮﻟﻮﮊﻱ ﻭ ﺑﻴﻤﺎﺭﻱ ﺩﺭ ﻛﻨﺎﺭ ﺗﺼﺎﻭﻳﺮ ﺩﺭﺝ ﺷﺪﻩ ﺍﺳﺖ. ــــــ
)COLOR ATLAS OF CLINICAL DERMATOLOGY COMMON AND SERIOUS DISEASES (Salekan E-Book
9.6
)(Thomas B. Fitzpatrick, MD, Richard Allen Johnson, MD, Klaus Wolff, MD, Dick Suurmond, MD
2001
)10.6 Color Atlas of Dermatoxcopy 2nd, enlarged and completely revised edition (Wilhelm Stolz. Otto Braun-Falco) (Salekan E-Book
ــــــ
11.6 Correction of Wrinkles & Augmentation of lip and cheek with Restylane & Perlane
)(Natural beauty for as long as you like
ﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ Skin fillerﻫﺎ ﺑﺮﺍﻱ ﺭﻓﻊ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎﻱ ﺻﻮﺭﺕ ﻛﻪ ﺳﺎﺯﮔﺎﺭﻱ ﺁﻥ ﺑﺎ ﺑﺎﻓﺖ ﺍﻧﺴﺎﻥ %١٠٠ﺍﺳﺖ .ﻫﻴﺎﻧﻮﺭﻭﺗﻴﻚ ﺍﺳﻴﺪ ﺗﻮﻟﻴﺪ ﺷﺪﻩ ﺗﻮﺳﻂ ﺗﻜﻨﻴﻚ recombinantﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻣﺎﺩﻩ ﺗﻮﺳﻂ ﻛﺸﻮﺭ ﺳﻮﺋﺪ ﺩﺭ ﺳﻪ ﻏﻠﻈﺖ ﺑﻪ ﻧﺎﻡﻫﺎﻱ Restyalne , Restyane fineﻭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
31 ﻼ ﻭﺍﺿﺢ ﻧﺸﺎﻥ perlaneﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮ ﺣﺴﺐ ﻧﻮﻉ ﺧﻄﻮﻁ ﺻﻮﺭﺕ )ﻇﺮﻳﻒ ﻳﺎ ﻋﻤﻴﻖ( ﺩﺭ ﺳﻄﻮﺡ ﻣﺨﺘﻠﻒ ﺩﺭﻡ ﺗﺰﺭﻳﻖ ﻣﻲﺷﻮﺩ .ﺩﺭ ﺍﻳﻦ : VCDﺍﺑﺘﺪﺍ ﻣﺮﻭﺭﻱ ﺑﺮ ﭼﮕﻮﻧﮕﻲ ﺳﺎﺧﺖ ﺍﻳﻦ ﺳﻪ ﻣﺎﺩﻩ ﺩﺍﺭﺩ ﻭ ﺳﭙﺲ ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻭ ﭼﮕﻮﻧﮕﻲ ﺗﺰﺭﻳﻖ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺗﺰﺭﻳﻖ ﺭﺍ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﻛﺎﻣ ﹰ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .٢ .ﺩﺭ ﻗﺴﻤﺖ ﺑﻌﺪﻱ ﺑﻪ ﺻﻮﺭﺕ animationﻋﻤﻖ ﻭ ﻣﺤﻞ ﺗﺰﺭﻳﻖ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﺳﻪ ﻣﺤﺼﻮﻝ ﺭﺍ ﺩﺭ ﺩﺭﻡ ﻧﺸﺎﻥ ﻣﻲﺩﻫﺪ .٣ .ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﻃﺮﻳﻘﺔ ﺑﻲﺣﺴﻲ ﻣﻮﺿﻌﻲ ﺑﻪ ﻧﻤﺎﻳﺶ ﮔﺬﺍﺷﺘﻪ ﻣﻲﺷﻮﺩ .٣ .ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺗﻜﻨﻴﻚ ﺗﺰﺭﻳﻖ Reslane fineﻭ ﻣﺤﻞ ﺗﺰﺭﻳﻖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .٤ .ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺗﻜﻨﻴﻚ ﺗﺰﺭﻳﻖ Restylanaﻭ ﻣﺤﻞ ﺗﺰﺭﻳﻖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .٥ .ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺗﻜﻨﻴﻚ ﺗﺰﺭﻳﻖ Perlaneﺑﺮﺍﻱ ﺭﻓﻊ ﭼﻴﻦﻫـﺎﻱ ﻋﻤﻘـﻲ )ﻣﺎﻧﻨـﺪ ﻧﺎﺯﻭﺷـﻴﺎﻝ( ﻭ fonciel contouringﻣﺎﻧﻨـﺪ ) Lip enhan cemenlﻭ (cheek enhancmeatﻭ ﺩﺭﻣﺎﻥ oral Commisureﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .٦ .ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺗﺮﻛﻴﺒﻲ ﺍﺯ ﺗﺰﺭﻳﻘﺎﺕ ﺑﺎﻻ ﺭﺍ ﺩﺭ ﻳﻚ ﺑﻴﻤﺎﺭ ﻧﺸﺎﻥ ﻣﻲﺩﻫﺪ .٧ .ﺩﺭ ﺑﺨﺶ ﺍﻧﺘﻬﺎ followupﺑﻴﻤﺎﺭ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .٨ .ﺩﺭ ﺍﻧﺘﻬﺎﻱ ﻫﺮ ﻗﺴﻤﺖ ﺗﺼﺎﻭﻳﺮ ﻗﺒﻞ ﻭ ﺑﻌﺪ ﺍﺯ ﺗﺰﺭﻳﻖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺍﺳﺖ. ــــــ
12.6 Cosmetic Surgery for FACE and BODY
2000
13.6 COSMETIC LASER SURGERY
2001
)PERFECT THE TECHIQUES, REDUCE THE RISKS, AND ENJOY THE RESULTS WHEN PERFORMING COSMETIC LASER SURGERY (Richard E. Fitzpatrick Mitchel P. Goldman
)(ALAN R. SHALITA, M.D., DAVID A. NORRIS, M.D
BASIC AND CLINICAL DERMATOLOGY
An Interdisciplinory Approach
14.6 Cosmetic Surgery
ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻒ ﻛﺘﺎﺏ ﻛﻤﺘﺮ ﻛﺘﺎﺑﻲ ﺍﺳﺖ ﻛﻪ ﺗﻠﻔﻴﻘﻲ ﺍﺯ ﺩﺍﻧﺶ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ،ﻣﺎﮔﺰﻳﻠﻮﻓﺎﺷﻴﺎﻝ ﻭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺭﺍ ﺩﺭ ﺧﻮﺩ ﮔﻨﺠﺎﻧﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺣﺪﻭﺩ ١٠٠٠ﺻﻔﺤﻪﺍﻱ ،ﺁﺧـﺮﻳﻦ ﺗﻜﻨﻴـﻚﻫـﺎﻱ ﺩﺭ ﺩﺳﺘﺮﺱ ﺩﺭ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻧﻤﻮﺩﻩ ﺗﺎ ﺑﺮﺍﻱ ﻫﺮ ﺑﻴﻤﺎﺭ ﺑﻪ ﺻﻮﺭﺕ ﺍﻧﻔﺮﺍﺩﻱ ﺗﻜﻨﻴﻚ ﻣﻨﺎﺳﺐ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﻭ ﺑﻪ ﻛﺎﺭ ﺭﻭﺩ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺍﺭﺍﻱ ﻓﺼﻮﻟﻲ ﺍﺳﺖ ﻛﻪ ﺗﻮﺳﻂ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﺟﺮﺍﺣﺎﻥ ﭘﻼﺳﺘﻴﻚ ﻭ ﺟﺮﺍﺣﺎﻥ ﻓﻚ ﻭ ﺻﻮﺭﺕ ﻧﻮﺷﺘﻪ ﺷﺪﻩ ﺍﺳﺖ. ﺍﻳﻦ ﻛﺘﺎﺏ Procedureﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺭﺍ ﻗﺪﻡ ﺑﻪ ﻗﺪﻡ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﻭ ﺗﻤﺎﻡ ﺟﻨﺒﻪﻫﺎﻱ ﺗﻜﻨﻴﻚﻫـﺎﻱ ﺟﺮﺍﺣـﻲ ﺭﺍ ﺗﻮﺿـﻴﺢ ﺩﺍﺩﻩ ﺍﺳـﺖ .ﺍﻃﻼﻋـﺎﺕ Pre-opﻭ Post-opﻭ ﻓـﺮﻡ ﺭﺿـﺎﻳﺖﻧﺎﻣـﻪ ﺩﺭ ﻫـﺮ ﻓﺼـﻞ ﺁﻭﺭﺩﻩ ﺷـﺪﻩ .ﺩﺭ ﻫـﺮ ﻓﺼـﻞ ﺍﻧﺪﻳﻜﺎﺳـﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎﻱ ﻫﺮ ﺗﻜﻨﻴﻚ ﺟﺮﺍﺣﻲ ﻭ ﻣﺤﺪﻭﺩﻳﺖﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﻭ ﻋﻮﺍﺭﺽ ﻭ ﺩﺭﻣﺎﻥ ﻋﻮﺍﺭﺽ ﻭ ﺩﺭﻣﺎﻥ ﻋﻮﺍﺭﺽ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻒ ﻛﺘﺎﺏ ﭼﻮﻥ ﻫﺮ ﻓﺼﻞ ﻛﺘﺎﺏ ﺗﻮﺳﻂ ﻣﺠﺮﺏﺗﺮﻥ ﺍﻓﺮﺍﺩ ﺩﺭ ﺯﻣﻴﻨﻪ ﻛﺎﺭﻱ ﺧﻮﺩ ﻧﮕﺎﺭﺵ ﻳﺎﻓﺘﻪ ﺍﺳﺖ ﻧﻜﺎﺕ ﻛﻠﻴﺪﻱ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﺧﺘﺼﺎﺻﻲ ﻭ ﺍﻃﻼﻋﺎﺕ ﻛﻮﭼﻚ ﻭﻟﻲ ﺑﺎﺍﺭﺯﺵ ﺩﺭ ﻣﻮﺭﺩ ﺗﻜﻨﻴﻚﻫﺎ ﻭ ﺭﻭﺵ ﻋﻤﻞ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ -١ﻃﺮﺍﺣﻲ ﻣﻨﺎﺳﺐ ﺑﺮﺍﻱ ﻳﻚ ﺟﺮﺍﺣﻲ ﺑﺤﺚ ﺷﺪﻩ .ﻓﺼﻞ -٢ﺁﻧﺎﻟﻴﺰ ﺯﻳﺒﺎﻳﻲ ﺷﻨﺎﺧﺘﻲ ﺩﺭ ﻣﻮﺭﺩ ﺩﺭﻣﺎﻥ ﺻﻮﺭﺕﻫﺎﻱ ﭘﻴﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ .ﻓﺼﻞ ٣ﺗﺎ Peel ٦ﺳﻄﺤﻲ ﻭ ﻋﻤﻘﻲ ﻭ ﺗﺮﻛﻴﺐ Peelﻫﺎ ﻭ ﻋﻼﻭﻩ ﺑﺮ ﺁﻥ ) total body peelﮔﺮﺩﻥ Chest .ﻭ ﺩﺳﺖﻫﺎ ﻭ ﻣﻨﺎﻃﻖ ﺩﻳﮕﺮ( ﻧﻴﺰ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ٦ﻛﻤﭙﻠﻴﻜﺎﺳﻴﻮﻥ ﻭ ﺩﺭﻣﺎﻥ ﺑﻪ ﻃﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳـﺖ .ﺩﺭ ﻓﺼـﻮﻝ ٧ﻭ ٨ﻭ ٩ﻭ ٢٢ﻭ ٢٤ﻭ ٣٧ﺩﺭ ﻣﻮﺭﺩ ﺍﻧﻮﺍﻉ ﺩﺭﻣﺎﻥﻫﺎ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻟﻴﺰﺭ ) Er: YAG, Co2ﺿﺎﻳﻌﺎﺕ ﻋﺮﻭﻗﻲ tattooﻭ ﺿﺎﻳﻌﺎﺕ ﭘﻴﮕﻤﺎﻧﺘﻪ ( hair removalﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ٩ﺩﺭ ﻣﻮﺭﺩ ﻣﺆﺛﺮ ﺑﻮﺩﻥ ﻟﻴﺰﺭﻫﺎﻱ Resurfacingﺻـﺤﺒﺖ ﻧﻤـﻮﺩﻩ ﺍﺳـﺖ. ﻓﺼﻞ ١٠ﺑﻪ Dermabrasionﺍﺧﺘﺼﺎﺹ ﺩﺍﺩﻩ ﺍﺳﺖ .ﻓﺼﻞ ١١ﺍﻟﻲ ١٦ﺩﺭ ﻣﻮﺭﺩ ﺩﻓﻊ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎ ﺗﻮﺳﻂ Skin fillerﻫﺎ ) Restiylansﻭ ، inerrall , Perlaneﻛـﻼﮊﻥ ﻭ (....ﻭ ﺗﺰﺭﻳـﻖ ﭼﺮﺑـﻲ ﻭ ﺩﺭ ﻓﺼـﻞ ١٥ﺍﺧﺘﺼﺎﺻـﹰﺎ ﺑـﻪ ﭼﮕـﻮﻧﮕﻲ ﺍﺳـﺘﻔﺎﺩﻩ ﺍﺯ Gortexﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻞ ١٧ﺑﻪ BotulinumsToxinﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١٨ﭼﮕﻮﻧﮕﻲ ﺟﺮﺍﺣﻲ ﺧﺎﻝﻫﺎ Cyst ،ﺍﺳﻜﺎﺭ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻞ ١٩ﺍﺧﺘﺼﺎﺹ ﺑﻪ ﺍﻧـﻮﺍﻉ flapﻭ Graftﻫـﺎ ﺩﺍﺭﺩ .ﻓﺼـﻮﻝ ١٢ﻭ ١٣ﻭ ٢٥ﺑـﻪ ﻟﻴﭙﻮﺳﺎﻛﺸـﻦ ﻭ ﻟﻴﭙﻮﺍﻧﻔﻮﺯﻳﻮﻥ ﻭ tumescentﺍﺧﺘﺼﺎﺹ ﺩﺍﺭﺩ .ﺩﺭ ﻓﺼﻮﻝ ٣٣ﺗﺮﻛﻴﺐ procedureﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻮﻝ fac, Neck ٢٩-٣٢ﻭ liflingﺑﺤﺚ ﺷﺪﻩ ﻭ ﺭﻭﺵﻫﺎﻱ ﺩﺭ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ Brow Reyirvenationﺁﺭﺭﺩﻩ ﺷﺪﻩ ﺍﺳـﺖ ﻭ ﺩﺭ ﻓﺼﻞ ٣١ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﭘﻠﻚ ﺑﺎﻻ ﻭ ﭘﺎﻳﻴﻦ ﺍﺯ ﺩﻳﺪ ﺍﻓﺘﺎﻟﻤﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ٢٧ﻛﺘﺎﺏ ﺭﻭﺵ ﺍﺧﺘﺼﺎﺻﻲ D. Cookﺑﻪ ﻧﺎﻡ The cook weekend Altrnative to face liftﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻞ ٣٤ﺑﻪ ﻛﺎﺷﺖ ﻣـﻮ ﻭ Alopecia Redechionﺍﺧﺘﺼﺎﺹ ﺩﺍﺭﺩ .ﻓﺼﻞ ٣٨ﻛﺘﺎﺏ ﺑﻪ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻋﻜﺎﺳﻲ ﺩﺭ ﻣﻄﺐ ﺑﺮﺍﻱ ﻛﺎﺭﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﺍﺷﺎﺭﻩ ﺩﺍﺭﺩ .ﻓﺼﻞ ٣٩ﺑﻪ ﭼﮕﻮﻧﮕﻲ ﺑﺮﺧﻮﺭﺩ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺸﻜﻞﺁﻓﺮﻳﻦ ﻭ ﻧﺎﺭﺍﺿـﻲ ﺍﺧﺘﺼـﺎﺹ ﺩﺍﺭﺩ .ﻓﺼـﻞ ٤٠ﻭ ٤١ﺍﺧﺘﺼـﺎﺹ ﺑـﻪ ﺍﻳﻤﭙﻼﻧﺖﻫﺎﻱ ﺻﻮﺭﺕ ﻭ ﻛﺎﺭﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﺟﺮﺍﺣﻲﻫﺎﻱ ﻣﺎﮔﺰﻳﻠﻮﻓﺎﺳﻴﺎﻝ ﻭ ﺩﻫﺎﻥ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. ــــــ
15.6 COSMETIC LASER SURGERY For Face and Body
ــــــ
)16.6 Cutaneous Laser Surgery (Second edition) The Art and Science of Selective Photothermolysis (Goldman, Fitzpartick Cutaneous Laser Surgeryﭼﺎﭖ ﻫﻤﻴﻦ ﻣﺆﻟﻔﻴﻦ ﻣﻲﺑﺎﺷﺪ .ﻛﺘﺎﺏ Cutaneus Laser
ﻳﻚ ﻛﺘﺎﺏ textﺩﺭ ﺯﻣﻴﻨﺔ ﻟﻴﺰﺭ ﻣﻲﺑﺎﺷﺪ ﻭ ﻫﺮ ﻧﻮﻉ ﺍﺯ ﺗﻜﻨﻮﻟﻮﮊﻱ ﻟﻴـﺰﺭ ﺑـﺮﺍﻱ
ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﻣﻜﻤﻞ ﺑﺮ ﻛﺘﺎﺏ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﺭﺍ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺍﺳﺖ ﻭﻟﻲ ﻛﺘﺎﺏ Cosmetic Laser Surgeryﻛﻤﻜﻲ ﺍﺳﺖ ﺑﺮﺍﻱ ﭘﺰﺷﻜﺎﻥ ﺑﺎ ﺗﺄﻛﻴﺪ ﺑﻴﺸﺘﺮ ﺑﺮ ﺑﺮﺧﻮﺭﺩ ﺩﺭﻣﺎﻧﻲ ﺑﺎ ﺑﻴﻤﺎﺭ. ﻓﺼﻞ ﺍﻭﻝ ﻛﺘﺎﺏ ﻣﺮﻭﺭﻱ ﺑﺮ Laser tissue interactionﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻣﻲ ﺗﻮﺍﻥ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ mini text bookﺍﺯ ﺁﻥ ﺍﺳﺘﻔﺎﺩﻩ ﻛﺮﺩ .ﻓﺼﻞ ﺩﺭﺧﺸﺎﻥ ﻛﺘﺎﺏ ﻓﺼﻞ Wuond healingﻣﻲﺑﺎﺷﺪ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﻟﻴﺰﺭﻫﺎ ﻭ ﺑﻬﺘﺮﻳﻦ ﺗﻜﻨﻴﻚ ﻫﺎ ﺑﺪﻭﻥ ﺗﻮﺟﻪ ﺑـﻪ Post procedural wound healingﻣﻨﺠﺮ ﺑﻪ ﻛﻤﺘﺮﻳﻦ ﻧﺘﻴﺠﻪ ﻣﻲﺷﻮﺩ .ﻓﺼﻞ ٣ﻭ ٤ﻭ ٥ﻭ ٦ﻭ ﺩﺭ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻭ ﺗﻮﺿﻴﺢ ﻛﻤﭙﻠﻴﻜﺎﺳﻴﻮﻥ ﺍﺯ ﻟﻴﺰﺭﻫﺎﻱ co2ﻭ Erbium:Yagﺩﺭ resurfacingﻭ Er:yagﺻﻮﺭﺕ ﻭ ﮔﺮﺩﻥ ﻭ chestﻣـﻲﺑﺎﺷـﺪ ﻭ ﻫﻤﭽﻨـﻴﻦ ﺩﺭ ﻣـﻮﺭﺩ ﺍﺳـﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴـﺰﺭ carbon Dioxide ultrapulseﻭ Er:yagﺩﺭ ﺍﻃﺮﺍﻑ ﭼﺸﻢ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻳﻜﻲ ﺍﺯ ﻓﺼﻮﻝ ﺗﺎﺯﻩ ﻛﺘﺎﺏ ﺍﺳﺘﻔﺎﺩﻩ Nonablative Laserﺩﺭ ﻣﻮﺭﺩ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙ ﻫﺎﻱ ﺻﻮﺭﺕ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻣﻘﺒﻮﻟﻴﺖ ﺭﻭﺯﺍﻓﺮﻭﻥ ﭘﻴﺪﺍ ﻛﺮﺩﻩ ﺍﺳﺖ ﻭ ﺩﺭ ﻓﺼﻞ incisional laser Surgery ٩ﺑﺮﺍﻱ ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﻭ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١٠ﻛﺘﺎﺏ Tinas.Alsterﻣﺆﻟﻒ ﻛﺘﺎﺏ manual of cutaneous laser techniquesﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﺩﺭ Scar revisionﺭﺍ ﺷﺮﺡ ﺩﺍﺩﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١١ﺟﺪﻳﺪﺗﺮﻳﻦ ﺗﻜﻨﻴﻜﻬﺎﻱ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺭ hair ] removalﻣﻘﺎﻳﺴﻪ ﺁﻧﻬﺎ ﻭ ﻃﺮﺯ ﻛﺎﺭ ﻭ ﻣﻌﺮﻓﻲ ﻟﻴﺰﺭﻫﺎﻱ ﻣﻌﺘﺒﺮ ﺍﺯ ﻛﺎﺭﺧﺎﻧﻪ ﻫﺎﻱ ﻣﻌﺘﺒﺮ[ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ ﻭﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ mtense light sourceﺩﺭ hair transplantﺻﺤﺒﺖ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١٢ﺍﺳﺘﻔﺎﺩﻩ ﺟﺪﻳﺪ ﺍﺯ ﻟﻴﺰﺭ Co2ﻭ Er:yagﺩﺭ ) hair transplantﻛﺎﺷﺖ ﻣـﻮ( ﺑﺤﺚ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١٣ﻛﺘﺎﺏ ﺩﺭﻣﺎﻥ Leg veinﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺁﺧﺮ ،ﻣﺆﻟﻔﻴﻦ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﺑﻪ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﻟﻴﺰﺭ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺭﺍﻫﻨﻤﺎ ﺩﺭ ﺍﻧﺘﺨﺎﺏ ﻣﻨﺎﺳﺒﺘﺮﻳﻦ ﺗﻜﻨﻴﻚﻫﺎ ﺗﻮﺻﻴﻪ ﻣﻲﻧﻤﺎﻳﻨﺪ. 2001
)17.6 Cutaneous Medicine Cutaneous Manifestations of Systemic Disease (THOMAS T. PROVOST, MD, JOHN A.FLYNN, MD) (Johns Hopkins Medical Institutions Baltimore, Maryland
ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ،ﺍﻳﻦ ﻛﺘﺎﺏ ،ﺁﺭﻡ ﻭ ﻣﺸﺨﺼﻪ ﺩﭘﺎﺭﺗﻤﺎﻥ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ﺟﺎﻥ ﻫﺎﭘﻜﻴﻨﺰ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﻋﻠﻢ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻳﻚ ﻧﻈﺮ ﻛﻠﻲ ﻧﻪ ﻓﻘﻂ ﺑﻪ ﻋﻨﻮﺍﻥ ﭘﻮﺳﺖ ﻭ ﺿﻤﺎﺋﻢ ﺑﻠﻜﻪ ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﺗﻈﺎﻫﺮﺍﺕ ﺩﻳﮕﺮ ﺑﻴﻤﺎﺭﻱ ﺩﺭ ﺑﺪﻥ ﺍﺷﺎﺭﻩ ﺩﺍﺭﺩ .ﺍﻳﻦ ٧٨٢ﺻﻔﺤﻪﺍﻱ ﺑﺎ ٧٣ ﻓﺼﻞ ﺑﺎ ﻋﻜﺲﻫﺎﻱ ﺑﺎ ﻛﻴﻔﻴﺖ ﻋﺎﻟﻲ ﺑﻪ ﺭﺍﻫﻨﻤﺎﻳﻲ ﺑﺮﺍﻱ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺩﺍﺧﻠﻲ ﻣﻲﺑﺎﺷﺪ .ﻧﻜﺘﺔ ﺑﺎﺭﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺁﻭﺭﺩﻥ ﻧﻜﺎﺕ ﻣﻬﻢ ﻛﺘﺎﺏ ﺩﺭ ﺣﺎﺷﻴﻪ ﺻﻔﺤﺎﺕ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺩﺍﺧﻠﻲ ﻛﻪ ﺗﻈﺎﻫﺮﺍﺕ ﭘﻮﺳﺘﻲ ﺩﺍﺭﻧﺪ ﻭ ﺑﻴﻤﺎﺭﻱﻫـﺎﻱ ﭘﻮﺳـﺘﻲ ﻛـﻪ ﻣﻲﺗﻮﺍﻧﺪ ﻋﻼﺋﻢ ﻋﻤﻮﻣﻲ ﭘﻴﺪﺍ ﻛﻨﺪ ﺭﺍ ﺗﻮﺻﻴﻒ ﻛﺮﺩﻩ ﺍﺳﺖ .ﺗﻜﻴﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﻣﻮﺍﺭﺩ ﻛﻠﻴﺪ ﻛﻪ ﺩﺭ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ،ﻣﻲﺑﺎﺷﺪ ﻭ ﺍﺯ ﻣﺒﺎﺣﺚ ﻏﻴﺮﺿﺮﻭﺭﻱ ﺍﺟﺘﻨﺎﺏ ﻛﺮﺩﻩ ﺍﺳﺖ. Dr. Richard Dobsonﺩﺭ ﻣﺠﻠﺔ (AAD) American etcademy of Dermatologyﺩﺭ ﻣﻮﺭﺩ ﺍﻳﻦ ﻛﺘﺎﺏ ﮔﻔﺘﻪ ﺍﺳﺖ :ﺩﺭ ﮔﺬﺷﺘﺔ ﺍﻛﺜﺮ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﺑﻪ ﻋﻠﺖ ﺷﻴﻮﻉ ﺳﻴﻔﻴﻤﻴﺲ ﺑﺎ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺩﺍﺧﻠﻲ ﺁﺷﻨﺎ ﺑﻮﺗﺪﻩﺍﻧـﺪ ﺯﻳـﺮ ﺑـﻪ ﻗـﻮﻝ Sir Willamosler ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
32 ﺩﺍﻧﺴﺘﻦ ﺳﻴﻔﻴﻤﻴﺲ ﺩﺍﻧﺴﺘﻦ ﻋﻠﻢ ﭘﺰﺷﻜﻲ ﺍﺳﺖ .ﺑﺎ ﻭﺟﻮﺩ ﺍﻳﻨﺘﺮﻧﺖ Procedureﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺩﺭ ﻋﻠﻢ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﻪ ﻧﻈﺮ ﻣﻦ medical Dermatologistﺩﺭ ﺁﻳﻨﺪﻩ ﺍﺯ ﺟﺎﻳﮕﺎﻩ ﻭﻳﮋﻩﺍﻱ ﺑﺮﺧﻮﺭﺩﺍﺭ ﺧﻮﺍﻫﻨﺪ ﺑﻮﺩ ﺯﻳﺮ ﺍﺑﺎ ﻭﺟﻮﺩ ﺗﻈـﺎﻫﺮﺍﺕ ﭘﻮﺳـﺘﻲ ﺑﻴﻤـﺎﺭﻱ AIDS
ﻭ ﭘﻴﺸـﺮﻓﺖ
ﺩﺍﻧﺶ ﭘﺰﺷﻜﻲ ﺩﺭ ﻛﺎﺭﺑﺮﺩ ﺳﻴﺘﻮﻛﺴﻴﻦﻫﺎ ،ﺁﻧﺘﻲﺑﻴﻮﺗﻴﻚ ،ﻛﻤﻮﺗﺮﺍﭘﻲ ﻭ ﺍﻳﻤﻮﻧﻮﺳﺎﭘﺮﺳﻴﻮﻫﺎ ﻋﻠﻢ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﺎﻟﻴﻨﻲ ﺑﻪ ﺍﻓﺮﺍﺩﻱ ﺑﺮﺍﻱ ﭘﺮ ﻛﺮﺩﻥ ﺧﺎﻟﻲ ﺩﺭ ﻣﺮﺍﻛﺰ ﻋﻠﻤﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﺍﺣﺘﻴﺎﺝ ﺩﺍﺭﺩ. ــــــ
)18.6 Dermatology: A Multi-Media Teaching File (Disc 1,2) (Gross & Microscopic Symposium) (Mosby
2002
)19.6 EVIDENCE-BASED DERMATOLOGY (Howard I. Maibach, MD, Sagib J. Bashir, BSc (Hons), MB, ChB, Ann McKibbon, BSc, MLS ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺑﺮ ﺍﺳﺎﺱ ﻋﻠﻢ (Evidence- Based Heatlth Care) EBMCﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ EBHC .ﭼﻬﺎﺭﭼﻮﺑﻲ ﺑﺮﺍﻱ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺩﺭ ﺑﺎﻟﻴﻨﻲ ﻭ ﺗﺤﻘﻴﻘﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ .ﻭ ٥ﻣﺮﺣﻠﻪ ﺩﺍﺭﺩ:
ﺍﻳﻦ ﻛﺘﺎﺏ
-١ﺍﻳﺠﺎﺩ ﺳﺆﺍﻝ -٢ﭘﻴﺪﺍ ﻛﺮﺩﻥ ﻣﺪﺍﺭﻙ ﻣﻌﺘﺒﺮ ﺑﺮﺍﻱ ﺟﻮﺍﺏ ﺑﻪ ﺁﻥ ﺳﺆﺍﻝ -٣ﺍﺭﺯﻳﺎﺑﻲ ﺍﻳﻨﻜﻪ ﺍﻳﻦ ﻣﻨﺎﺑﻊ ﻭ ﻣﺪﺍﺭﻙ ﺁﻳﺎ ﻣﻌﺘﺒﺮﻧﺪ ﻳﺎ ﺧﻴﺮ -٤ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻣﺪﺍﺭﻙ ﺑﺮﺍﻱ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺩﺭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭ. ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﻭﺷﻲ ﻣﻨﻄﻘﻲ ﺑﺮﺍﻱ ﭘﻴﺪﺍﻛﺮﺩﻥ ﺳﺆﺍﻻﺕ ﺑﻪ ﻭﺟﻮﺩ ﺁﻣﺪﻩ ﺩﺭ ﺣﻴﻦ ﻛﺎﺭ ﺑﺎﻟﻴﻨﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ .ﺩﺭ ﻓﺼﻞ ﺍﻭﻝ ﻛﺘﺎﺏ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﻣﺮﺣﻠﻪ ﺑﻪ ﺗﻔﻀﻴﻞ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﭼﻄﻮﺭ ﻣﻲﺗﻮﺍﻥ ﻣﺘﻮﺟﻪ ﻣﻌﺘﺒﺮ ﺑﻮﺩﻥ ﻳﻚ ﻓﺮﺿﻴﻪ ﻳﺎ ﻣﻘﺎﻟﻪ ﮔﺮﺩﻳﺪ ﻭ... ﺩﺭ ﻓﺼﻞ ﺩﻭﻡ ﻛﺎﺭﺑﺮﺩ ﺍﻳﻦ ﻋﻠﻢ EBMEﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖ .ﻭ ﺩﺭ ﻓﺼﻠﻲ ﺟﺪﺍ ﻣﻨﺎﺑﻊ ﻣﻌﺘﺒﺮ ﻭ ﻗﺎﺑﻞ ﺗﻮﺟﻬﻲ ﺁﺩﺭﺱ ﺍﻳﻨﺘﺮﻧﺘﻲ ﺑﺎ ﻣﺸﺨﺼﺎﺕ ﻛﺎﻣﻞ ﺑﺮﺍﻱ ﺑﻪ ﺭﻭﺯﺑﻮﺩﻥ ﺍﻃﻼﻋﺎﺕ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻛﻪ ﺩﺭ ﻧﺸﺮ ﻛﺘﺎﺑﻲ ﺍﻳﻦ ﻣﻨﺎﺑﻊ ﺑﺎﺍﺭﺯﺵ ﻣﺸﺎﻫﺪﻩ ﻣﻲﺷﻮﺩ. ــــــ
20.6 Facial Lifting by "APTOS" threads Clinic of Plastic and Aesthetic Surgery
ــــــ
)21.6 Hair Removal with Intense Pulsed Laser (IPL
)ﻃﺮﻳﻘﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ -ﻣﺤﻞﻫﺎﻳﻲ ﻛﻪ ﺑﺮﺍﻱ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﺩ -ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ( +ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺍﻣﺮﻭﺯﻩ ﺭﻭﺵﻫﺎﻱ ﻭﻗﺖﮔﻴﺮ ﻭ ﺑﻌﻀﹰﺎ ﺑﺎ ﻋﺎﺭﺿﻪ ﺑﺮﺍﻱ ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﻣﺎﻧﻨﺪ ،sharingﻣﻮﺑﺮﻫﺎ ،ﺍﻟﻜﺘﺮﻭﻟﻴﺰ ﻭ ...ﻛﻤﺘﺮ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ .ﻟﻴﺰﺭﻫﺎﻱ ﺍﺯ ﺑﻴﻦﺑﺮﻧﺪﻩ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﺎ ﻭﻗﺖ ﻛﻤﺘﺮ ،ﻛﺎﺭﺍﺋﻲ ﺑﻴﺸﺘﺮ ﻭ ﻋﻮﺍﺭﺽ ﻣﺨﺘﺼﺮ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﺩﺭ ﻳﻚ ﺯﻧﺪﮔﻲ ﺑﺎ ﻛﻴﻔﻴﺖ ﻣﻄﻠﻮﺏ ﺑﺮﺍﻱ ﻣﺮﺍﺟﻌﻴﻦ ﺑﻪ ﭘﺰﺷﻜﺎﻥ ﺑﺨﺼﻮﺹ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﻛﻠﻴﻨﻴﻚﻫﺎﻱ ﺯﻳﺒﺎﺋﻲ ﺩﺍﺭﺩ .ﺍﺯ ﺟﻤﻠﻪ ﺟﺪﻳﺪﺗﺮﻳﻦ ﻟﻴﺰﺭﻫﺎﻱ ﺑﻜﺎﺭﺭﻓﺘﻪ ﻟﻴﺰﺭ IPLﻣﻲﺑﺎﺷﺪ .ﻓﻮﺍﺋﺪ ﺍﻳﻦ ﻟﻴﺰﺩ ﺩﺭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﻳﻦ ﻟﻴﺰﺭ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺎ Skin typeﺑﺎﻻ Spot size ،ﺑﺰﺭﮔﺘﺮ ﻭ ﺩﺭ ﻧﺘﻴﺠﻪ ﻃﻮﻝ ﻣﺪﺕ ﻛﻤﺘﺮ ﺩﺭﻣﺎﻥ Therapeatic window ،ﺑﺰﺭﮔﺘﺮ ﻛﻪ ﻣﻮﺟﺐ ﻋﺎﺭﺿﻪ ﻛﻤﺘﺮ ﻭ ﻛﺎﺭﻣﺪﻱ ﺑﻴﺸﺘﺮ ﻣﻲﺷﻮﺩ .ﺩﺭ ﺍﻳﻦ CDﻛﻪ ﺑﻪ ﺳﻔﺎﺭﺵ ﻛﻤﭙﺎﻧﻲ Ellipseﺗﻮﻟﻴﺪ ﺷﺪﻩ ﺍﺳﺖ .ﻣﻌﺮﻓﻲ ﻟﻴﺰﺭ ،IPLﭼﮕﻮﻧﮕﻲ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ،ﻓﻮﺍﺋﺪ ﻟﻴﺰﺭ ،IPLﻣﻨﺎﻃﻘﻲ ﻛﻪ ﺩﺭ ﺁﻥ ﺍﺯ ﻟﻴﺰﺭ IPLﺑﺮﺍﻱ
ﺭﻓﻊ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻛﻠﻴﭗ ﻭﻳﺪﺋﻮﺋﻲ ﺍﺯ ﺑﻴﻤﺎﺭﻳﺎﻥ ﻭ ﻧﺤﻮﻩ ﺩﺭﻣﺎﻥ ﻭ ﻧﺘﺎﻳﺞ ﺩﺭﻣﺎﻥ ﺑﺎ ﻋﻜﺲ ﻭ clipﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. )(The Art of Micrografting and Minigrafting) (Salekan E-Book
2002 ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ: TECHNIQUE
22.6 HAIR TRANSPLANTATION
PLANING AND PATIENT INSTRUCTUIONS
PATIENT EVALUATION
ANATOMY AND PHYSILOGY OF HAIR
SPECIAL APPLICATIONS
REOPERATIVE SURGERY
COMBINED FACE LIFT AND HAIR TRANSPLAYTATION
1999
)23.6 HANDBOOK OF ORAL DISEASE DIAGNOSIS AND MANAGEMENT Cripian Scully (MARTIN DUNITZ ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺷﺎﻣﻞ ٤٢٠ﺻﻔﺤﻪ ﻣﺘﻦ ﺑﻪ ﻫﻤﺮﺍﻩ ﺑﻴﺶ ﺍﺯ ٤٠٠ﺗﺼﻮﻳﺮ ﺭﻧﮕﻲ ﺍﺯ ﺿﺎﻳﻌﺎﺕ ﺩﻫﺎﻧﻲ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺭﻣﺎﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﺩﻧﺪﺍﻧﭙﺰﺷﻜﺎﻥ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﻳﻪ ﺗﻨﻬﺎ ﺑﻪ ﻋﻨـﻮﺍﻥ ﺍﻃﻠـﺲ ﺑﻠﻜـﻪ ﺍﺯ ﺟﻨﺒﺔ ﺍﺗﻴﻮﻟﻮﮊﻱ ،ﻛﻠﻴﺪﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺩﺭﻣﺎﻥ ﻭ ﺩﺭ ﺻﻮﺭﺕ ﺍﻣﻜﺎﻥ ﭘﻴﺸﮕﻴﺮﻱ ﻧﻴﺰ ﺑﻪ ﺿﺎﻳﻌﺎﺕ ﺩﻫﺎﻧﻲ ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ .ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺎﻳﻊ ﻭ ﻣﻬﻢ ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﺩﻫﺎﻧﻲ ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ ﻋﻼﻭﻩ ﺑﺮ ﺍﻳﻦ ﺗﻌﺪﺍﺩﻱ ﻣﻮﺍﺭﺩ ﻧﺎﺩﺭ ﻛﻪ ﺩﺭ ﺳﻄﺢ ﺟﻬﺎﻥ ﺭﻭ ﺑﻪ ﺍﻓﺰﺍﻳﺶ ﺍﺳﺖ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ .ﻓﺼﻞ ﺍﻭﻝ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﺑﺮﺭﺳﻲ symptom, signﺿﺎﻳﻌﺎﺕ ﺩﻫﺎﻧﻲ ﻣﻲﺑﺎﺷﺪ .ﻓﺼﻮﻝ ﺑﻌﺪﻱ ﺷﺎﻣﻞ ﺩﺭﺩﻫﺎﻱ ﻧﺎﺣﻴﺔ ﺩﻫﺎﻥ ﺑﺎ ﻣﻨﺸﺎﺀ ﻋﺮﻭﻗﻲ ﻳﺎ ﻋﺼﺒﻲ ،ﺷﻜﺎﻳﺎﺕ ﺩﻫﺎﻧﻲ ﺑﺎ ﻣﻨﺸﺎﺀ ﺭﻭﺍﻧﻲ ،ﺿﺎﻳﻌﺎﺕ ﻣﺨﺎﻃﻲ ،ﺑﺰﺍﻗﻲ ،ﺿﺎﻳﻌﺎﺕ ﻟﺜﻪﻫﺎ ،ﺿﺎﻳﻌﺎﺕ ﻟﺐ ﻭ ﻛـﺎﻡ ﻭ ﺿـﺎﻳﻌﺎﺕ ﺩﻫﺎﻧﻲ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻫﺮ ﻓﺼﻞ ﺍﺑﺘﺪﺍ ﺿﺎﻳﻌﺎﺕ ﺑﺮ ﺍﺳﺎﺱ ﺍﻟﻔﺒﺎﻱ ﺍﻧﮕﻠﻴﺴﻲ ﺗﻨﻈﻴﻢ ﻭ ﺳﭙﺲ ﺑﺮ ﺍﺳﺎﺱ management ،Diagnosis ،Clinical feature ،Aetiology ،Sexmainly affected ،Agemainly affected ،incidence ،Defintionﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﺷﺪﻩ ﺍﺳﺖ.
2000
24.6 Laser Hair Removal
)(David J. Goldman) (Martin Dunits ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﻣﺮﻭﺭﻱ ﺑﺮ ﻟﻴﺰﺭﻫﺎﻱ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺑﺮﺍﻱ ﺑﺮﺩﺍﺷﺖ ﻣﻮﻫﺎ ) (hair removalﻣﻲﺑﺎﺷﺪ .ﻧﺨﺴﺘﻴﻦ ﻓﺼﻞ ﻛﺘﺎﺏ ﺍﺧﺘﺼﺎﺹ ﺑﻪ ﺑﻴﻮﻟﻮﮊﻱ ﻣﻮ ﺩﺍﺭﺩ .ﻓﺼﻞ ﺑﻌﺪﻱ ﻛﺘﺎﺏ ﻣﺮﻭﺭﻱ ﮔﺬﺭﺍ ﺑﻪ ﻓﻴﺰﻳﻚ ﻟﻴﺰﺭ ﻭ ﻛﺎﺭﺑﺮﺩ ﺁﻥ ﺩﺭ hair removalﻣﻲﺑﺎﺷﺪ .ﻓﺼﻞ ﺑﻌﺪﻱ ﻛﺘﺎﺏ ،ﺑﻪ ﭼﮕﻮﻧﮕﻲ ﺁﻧﺠﺎﻡ ﺍﻟﻜﺘﺮﻭﻟﻴﺰ ﺩﺭ ﺭﻓﻊ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﻭ ﻣﻘﺎﻳﺴﺔ ﺁﻥ ﺑﺎ ﻟﻴﺰﺭ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺩﺭ ﻓﺼﻮﻝ ﺩﻳﮕﺮ ﻛﺘﺎﺏ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﻟﻴﺰﺭﻫﺎ ﻛﻪ ﺑﺮﺍﻱ ﺭﻓﻊ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﻧﺪ ﺑﺮﺭﺳﻲ ﻣﻲﮔﺮﺩﺩ: 5- Intense pulsed light
ND: YAG laser
4-
3- Diode laser
2- Normal mode alexandrite laser
1- Normal mode Ruby laser
ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻣﻘﺎﻻﺕ ﺗﺤﻘﻴﻘﻲ ﻭ ﻃﺮﻕ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻫﺮ ﻳﻚ ﺍﺯ ﺩﺳﺘﮕﺎﻫﻬﺎﻱ ﺍﻳﺰﺭ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﺩﺭ ﺁﺧﺮ ﻫﺮ ﻓﺼﻞ ﻧﻈﺮ ﻣﺆﻟﻒ ﺩﺭ ﺧﺼﻮﺹ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﺳﻴﺴﺘﻢﻫﺎ ﻣﻄﺮﺡ ﺷﺪﻩ ﺍﺳﺖ. ﻳﻜﻲ ﺍﺯ ﻧﻜﺎﺕ ﻣﻨﺤﺼﺮ ﺑﻪﻓﺮﺩ ﻛﺘﺎﺏ ﻣﻌﺮﻓﻲ ﻟﻴﺰﺭﻫﺎﻱ ﻣﻌﺘﺒﺮ ﺍﺯ ﺷﺮﻛﺖﻫﺎﻱ ﻣﻌﺘﺒﺮ ﻭ ﻣﻘﺎﻳﺴﺔ ﺁﻧﻬﺎ ﺑﺎ ﻳﻜﺪﻳﮕﺮ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﭘﺰﺷﻚ ﺭﺍ ﺩﺭ ﺍﻧﺘﺨﺎﺏ ﺩﺳﺘﮕﺎﻩ ﻟﻴﺰﺭ ﻣﻨﺎﺳﺐ ﻳﺎﺭﻱ ﻣﻲﻛﻨﺪ ﻛﻪ ﺩﺭ ﻧﻬﺎﻳﺖ ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﺻﺤﻴﺢ ﺑﻪ ﺣﺼﻮﻝ ﻧﺘﻴﺠﺔ ﺧﻮﺏ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﻣﻲﻧﻤﺎﻳﺪ. ــــــ
)25.6 MANAGEMENT OF FACIAL LINES AND WRINKLES (ANDREW BLITZER, WILLIAM J. BINDER, J. BRIAN BOYD ALASTAIR CARRUTHERS) (SALEKAN E-BOOK
ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺷﺎﻣﻞ ٢٢ﻓﺼﻞ ﺍﻃﻼﻋﺎﺕ ﺟﺎﻟﺒﻲ ﺩﺭ ﻣﻮﺭﺩ ﺩﺭﻣﺎﻥ ﻭ ﻧﻮﻉ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎ ) (Line 8 Wrinkleﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﺳﭙﺲ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻓﺼﻮﻝ ﻣﺠﺰﺍ exfoliantsﻳﺎ Superfical peelﻣﺮﻃﻮﺏﻛﻨﻨﺪﺓ ﺁﻧﺎﻟﻮﮒﻫﺎﻱ Chemical ، Vitaminsﺑﺎﻓﻨﻮﻝ ﻭ ، TCAﻣﻘﺎﻳﺴﻪ Peelﺷﻴﻤﻴﺎﻳﻲ ﻭ ﻟﻴﺰﺭ Dermabrasion ،ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻧﻮﺍﻉ implantﻫﺎﻱ ﺻﻮﺭﺕ ،ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ Dermal Allograftﻃﺮﻳﻘـﺔ ﮔﺬﺍﺷـﺘﻦ GORTEXﺗـﺰﺭﻱ ﻛـﻼﮊﻥ ﻭ ﭼﺮﺑﻲ Directexcision ،ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎ ﺗﺼﺤﻴﺢ ﺟﺮﺍﺣﻲ facelifting, endoscopic Browloft Skeletal frameﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ .ﻳﻚ ﻓﺼﻞ ﺍﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺧﺘﺼﺎﺹ ﺑﻪ ﻣﺮﻭﺭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ ﻛﺎﺭﺑﺮﺩ ﺩﺭﻣﺎﻥ ﺗﻮﻛﺴﻴﻦ ﺑﻮﺗﻮﻟﻴﻨﻴﻮﻡ ﺩﺭ ﭘﺰﺷﻜﻲ ﻭ ﻓﺼﻞ ﺩﻳﮕـﺮ ﺑـﻪ ﻃﺮﻳﻘـﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺗﺰﺭﻳﻖ Botulinium Toxinﺑﺮﺍﻱ ﺩﺭﻣﺎﻥ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎ ﺑﺤﺚ ﻣﻲﻧﻤﺎﻳﺪ .ﺳﭙﺲ ﺩﺭ ﻓﺼﻞ ٢٠ﻃﺮﻳﻘﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﻭ Botulinumtoxinﺩﺭ ﺭﻓﻊ ﺧﻄﻮﻁ ﺩﺭ ﭼﺸﻢ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ٢١ﻃﺮﻳﻘﺔ ﻋﻜﺲ ﮔـﺮﻓﺘﻦ ﺍﺯ ﺑﻴﻤـﺎﺭ ﺑـﻪ ﻋﻨـﻮﺍﻥ ﻳـﻚ ﺳـﻨﺪ ﭘﺰﺷﻜﻲ ﻭ Computer imagingﺑﺎ ﺩﻭﺭﺑﻴﻦﻫﺎﻱ ﺩﻳﺠﻴﺘﺎﻟﻲ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
33 )26.6 MANUAL OF CUTANEOUS LASER TECHNIQUES (Second Edition) (Tinal S. Alster, M.D.) (SALEKAN E-BOOK
2000
ــــــ
ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺷﺎﻣﻞ ١٢ﻓﺼﻞ ﺍﺳﺖ ﻛﻪ ﻳﻜﻲ ﺍﺯ ﻛﺎﺭﺑﺮﺩﻱﺗﺮﻳﻦ ﻛﺘﺎﺏﻫﺎ ﺩﺭ ﺯﻣﻴﻨﺔ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﺑﺎ ﻟﻴﺰﺭ ﻣﻲﺑﺎﺷﺪ .ﻧﮕﺎﻩ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻴﺸﺘﺮ ﺑﺮ ﻧﻜﺎﺕ ﻋﻤﻠﻲ ﻟﻴﺰﺭ ﻭ ﺗﻜﻨﻴﻚﻫﺎ ﻭ ﻣﺸﻜﻼﺗﻲ ﺍﺳﺖ ﻛﻪ ﺣﻴﻦ ﻭ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ ﺍﻳﺠﺎﺩ ﻣﻲﺷﻮﺩ ،ﻣﺘﻤﺮﻛﺰ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ﺗﻮﺿﻴﺤﺎﺗﻲ ﻛﻪ ﺑﻪ ﺑﻴﻤﺎﺭ ﻗﺒﻞ ﺍﺯ ﻋﻤﻞ ﻭ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ ﺑﺎﻳﺪ ﺩﺍﺩﻩ ﺷﻮﺩ ﻭ ﻫﻤﭽﻨﻴﻦ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺘﺨﺎﺏ ﺑﻴﻤﺎﺭ ﻣﻨﺎﺳﺐ ) (Patient selectionﺑﻪ ﻃﻮﺭ ﻛﺎﻣﻞ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺑﻌﻀﻲ ﺍﺯ ﻓﺼﻮﻝ ،ﻛﺘﺎﺏ ﺑﻪ ﻣﻌﺮﻓﻲ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺑﻪ ﻛﺎﺭﮔﻴﺮﻱ ﻟﻴﺰﺭﻫﺎ ﻭ ﻣﻌﺮﻓﻲ ﺩﺳﺘﮕﺎﻩﻫﺎﻱ ﻟﻴﺰﺭﻱ ﻣﻌﺘﺒﺮ ﻭ ﻣﻘﺎﻳﺴﺔ ﺩﺳﺘﮕﺎﻫﻬﺎﻱ ﻟﻴﺰﺭ ﻭ ﺭﻭﺵ ﺍﻧﺠﺎﻡ ﻛﺎﺭ ﺑﻪ ﻃﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺮﺍﻱ ﻟﻴﺰﺭﻫﺎﻱ ﺍﺧﺘﺼﺎﺻﻲ ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻮﻝ ﺟﺪﻳﺪ ﻛﺘﺎﺏ ﻧﺴﺒﺖ ﺑﻪ editionﻗﺒﻞ ﺷـﺎﻣﻞ erbium :YAG laserﻭ Resurfacingﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﺑﺎ ﻟﻴﺰﺭ ﻭ ﻟﻴﻔﺘﮓ ﭘﻴﺸﺎﻧﻲ ﻫﻤﺰﻣﺎﻥ ﺑﺎ ﻟﻴﺰﺭ ﻭ ﻟﻴﺰﺭﻫﺎﻱ hair removalﺍﺿﺎﻓﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺩﺭ ﻓﺼﻮﻝ ﺁﺧﺮ ﻛﺘﺎﺏ ﻋﻮﺍﺭﺽ ﻟﻴﺰﺭ ﻭ ﭼﮕﻮﻧﮕﻲ ﺩﺭﻣﺎﻥ ﺁﻧﻬﺎ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻟﻴﺰﺭ ﺑﻪ ﻃﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ. ﻣﻲﺗﻮﺍﻥ ﮔﻔﺖ ﻛﺘﺎﺏ ﺣﺎﺿﺮ ﻫﻤﺮﺍﻩ ﺑﺎ Cutaneous Laser in Medicineﻧﻮﺷﺘﺔ Fitzpatricﻭ Goldmanﻛﺎﻣﻞﺗﺮﻳﻦ ﻛﺘﺎﺏﻫﺎﻱ ﭘﺎﻳﻪ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﺩﺭ ﻋﻠﻢ ﻟﻴﺰﺭ ﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﻮﺩﻩ ﻭ ﺍﺻﻠﻲﺗﺮﻳﻦ ﻛﺘﺎﺑﻲ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫـﺎ ﻭ ﺟﺮﺍﺣـﺎﻥ ﺑـﺎ ﮔـﺮﺍﻳﺶ facial rejuvenationﺑﻪ ﺁﻥ ﻧﻴﺎﺯ ﺩﺍﺭﻧﺪ. )Clifford M Lawrence Neil H Cox (Joseph L Jorizzo) (SALEKAN E-BOOK )27.6 PHYSICAL SIGNS IN DERMATOLOGY (SECOND EDITION ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ٧٠٠ﺗﺼﻮﻳﺮ ﺗﻤﺎﻡ ﺭﻧﮕﺲ ﺍﺯ ﺿﺎﻳﻌﺎﺕ ﻣﺨﺘﻠﻒ ﭘﻮﺳﺘﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮ ﺍﺳﺎﺱ ﺷﻜﻞ ﻭ ﺭﻧﮓ ﻭ ﻣﺤﻞ ﺿﺎﻳﻌﺎﺕ ﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﺷﺪﻩ ﻭ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻓﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﺧﻮﺍﻧﻨﺪﻩ ﺍﻳﻦ ﺍﻣﻜﺎﻥ ﺭﺍ ﻣﻲﺩﻫﺪ ﻛﻪ ﺑﺎ ﺁﻧﺎﻟﻴﺰ ﺩﺭ ﻣﺸﺎﻫﺪﺓ ﺑﺎﻟﻴﻨﻲ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻌﻠﻮﻣﺎﺕ ﺑﻪ ﺗﺸﺨﻴﺺ ﺻﺤﻴﺢ ﺿﺎﻳﻌﺎﺕ ﺑﺮﺳﺪ. ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻴﻤﺎﺭﻱﻫﺎ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﻓﻴﺰﻳﻮﭘﺎﺗﻮﻟﻮﮊﻱ )ﻋﻔﻮﻧﻲ ،ﺍﺗﻮﺍﻳﻤﻮﻥ ﻭ ( ...ﺗﻘﺴﻴﻢ ﺑﻨﺪﻱ ﻧﻜﺮﺩﻩ ﺑﻠﻜﻪ ﺑﺮ ﺍﺳﺎﺱ ﺷﻜﻞ ﻭ ﻣﺤﻞ ﺿﺎﻳﻌﺎﺕ ﻓﺼﻞ ﺑﻨﺪﻱ ﺷﺪﻩ ﺍﺳﺖ .ﻛﻪ ﺑﺮﺍﻱ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻳﻚ approachﻋﻤﻠﻲ ﺑﺮﺍﻱ ﺭﺳﻴﺪﻥ ﺑﻪ ﺗﺸﺨﻴﺺ ﺿﺎﻳﻌﺎﺕ ﺭﺍ ﻓﺮﺍﻫﻢ ﻣﻲﻛﻨﺪ. ﺍﻳﻦ ﻛﺘﺎﺏ ﻫﺮ ﭼﻨﺪ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﻛﺘﺎﺏ testﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻧﻤﻲﺑﺎﺷﺪ ﻭﻟﻲ ﺗﻤﺎﻡ ﻣﺒﺎﺣﺚ ﻣﻬﻢ ﻭ ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﻣﻮﺍﺭﺩ ﻧﺎﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺩﺭ ﺁﻥ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻳﻜﻲ ﺍﺯ ﻧﻜﺎﺕ ﻣﻤﺘﺎﺯ ﺩﺭ ﻭﻳﺮﺍﻳﺶ ﺟﺪﻳﺪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺁﻭﺭﺩﻥ ﺟﺪﺍﻭﻟﻲ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺁﻧﻬﺎ ﻧﻜﺎﺕ ﻛﻠﻴﺪﻱ ﺩﺭ ﺗﺸﺨﻴﺺ ﻭ pitfallsﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺑﻴﺎﻥ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺣﻘﻴﻘﺖ ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﺍﻃﻠﺲ ﺭﻧﮕﻲ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﻭ ﺷﺮﺡ ﻭ ﺁﻧﺎﻟﻴﺰ ﺭﺳﻴﺪﻥ ﺑﻪ ﺗﺸﺨﻴﺺ ﺿﺎﻳﻌﺎﺕ ﻭ ﺟﺪﺍﻭﻝ ﻛﻤﻚ ﻛﻨﻨﺪﻩ ﺩﺭ ﺗﺸﺨﻴﺺ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻣﻮﺟﺐ ﺷﺪﻩ ﻳﻚ ﻛﺘﺎﺏ ﺑﺎﺍﺭﺯﺵ ﻧﻪ ﺗﻨﻬﺎ ﺑﺮﺍﻱ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﺑﻠﻜﻪ ﺑﺮﺍﻱ ﺳﺎﻳﺮ ﭘﺰﺷﻜﺎﻥ ﻛﻪ ﺑﺎ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻛﻤﺘﺮ ﺁﺷﻨﺎﻳﻲ ﺩﺍﺭﻧﺪ ﺑﻪ ﻛﺎﺭ ﺭﻭﺩ .ﺑﻪ ﮔﻔﺘﺔ Dr. Joav Merickﺗﺼﺎﻭﻳﺮ ﺁﻥ ﭼﻨﺎﻥ ﻛﻴﻔﻴﺘﻲ ﺩﺍﺭﻧﺪﻛﻪ ﮔﻮﻳﺎ ﺑﻴﻤﺎﺭ ﺩﺭ ﻣﻘﺎﺑﻞ ﺷﻤﺎ ﺍﻳﺴﺘﺎﺩﻩ ﺍﺳﺖ .ﺑﻪ ﻋﻠﺖ ﺍﻫﻤﻴﺖ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺎﻳﺪ ﻫﺮ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺘﻲ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﻫﻤﺮﺍﻩ ﺩﺍﺷﺘﻪ ﺑﺎﺷﺪ ﻭ ﺳﺎﻳﺮ ﺧﺎﻧﻮﺍﺩﻩﻫﺎﻱ ﭘﺮﺷﻜﻲ ،ﻣﺘﺨﺼﻴﺼﻴﻦ ﺍﻃﻔﺎﻝ ﻭ ﺩﺍﺧﻠﻲ ﺩﺭ ﻓﻌﺎﻟﻴﺖ ﺑﺎﻟﻴﻨﻲ ﺑﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺣﺘﻴﺎﺝ ﭘﻴﺪﺍ ﺧﻮﺍﻫﻨﺪ ﻛﺮﺩ .ﻫﺮ ﻛﺘﺎﺑﺨﺎﻧﺔ ﭘﺰﺷﻜﻲ ﺑﺎﻳﺪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﺩﺭ ﻗﻔﺴﻪﻫﺎﻱ ﺧﻮﺩ ﺟﺎﻱ ﺩﻫﺪ... 28.6 Practical MINOR SURGERY
ــــ 2002
)(Third Edition) (Antoinette F. Hood, Thedore H. Kwan, Martin C. Mihm, Jr., Thomas D. Horn, Bruce R. Smoller 7. Bonus Quizzes 6. Panniculus
4. Reticular Dermis 5. Appendages
29.6 Primer of Dermatopathology
3. Basement Membrane Zone, Oaoillary Dermis, and Superficial Vascular Plexus
1. Introduction 2. Epidermis
ــــــ
)Radiosurgical Treatment of Superficial Skin Lesions (S. Randolph Waldman, M.D.
30.6
ــــــ
)Radiosurgical Vaporization of Dermatologic Lesions (Dr. Stephen Chiarello
31.6
)6. Basal Cell Carcinoma (Nasal Bridge
)5. Scar Revision (Nose
)4. Basel Cell Carcinoma (Nasal Tip
)3. Scar Revision (Back
11. Tonsillectomy
10. Rhinoplasty
9. Turbinate Shrinkage
8. Radiosurgery in ENT
12. Tympanoplasty
ــــــ
)(SALEKAN E-BOOK
2- Keratosis Removal
1- Rhinophyma
)7. Scar Revision (Lower Forehead
Reconstructive Facial Plastic Surgery
32.6
)ﻃﺮﻳﻘﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ -ﻣﺤﻞﻫﺎﻳﻲ ﻛﻪ ﺑﺮﺍﻱ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﺩ -ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ( +ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺍﻣﺮﻭﺯﻩ ﺭﻭﺵﻫﺎﻱ ﻭﻗﺖﮔﻴﺮ ﻭ ﺑﻌﻀﹰﺎ ﺑﺎ ﻋﺎﺭﺿﻪ ﺑﺮﺍﻱ ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﻣﺎﻧﻨﺪ ،sharingﻣﻮﺑﺮﻫﺎ ،ﺍﻟﻜﺘﺮﻭﻟﻴﺰ ﻭ ...ﻛﻤﺘﺮ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ. ﻟﻴﺰﺭﻫﺎﻱ ﺍﺯ ﺑﻴﻦﺑﺮﻧﺪﻩ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﺎ ﻭﻗﺖ ﻛﻤﺘﺮ ،ﻛﺎﺭﺍﺋﻲ ﺑﻴﺸﺘﺮ ﻭ ﻋﻮﺍﺭﺽ ﻣﺨﺘﺼﺮ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﺩﺭ ﻳﻚ ﺯﻧﺪﮔﻲ ﺑﺎ ﻛﻴﻔﻴﺖ ﻣﻄﻠﻮﺏ ﺑﺮﺍﻱ ﻣﺮﺍﺟﻌﻴﻦ ﺑﻪ ﭘﺰﺷﻜﺎﻥ ﺑﺨﺼﻮﺹ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﻛﻠﻴﻨﻴﻚﻫﺎﻱ ﺯﻳﺒﺎﺋﻲ ﺩﺍﺭﺩ. ﺍﺯ ﺟﻤﻠﻪ ﺟﺪﻳﺪﺗﺮﻳﻦ ﻟﻴﺰﺭﻫﺎﻱ ﺑﻜﺎﺭﺭﻓﺘﻪ ﻟﻴﺰﺭ IPLﻣﻲﺑﺎﺷﺪ .ﻓﻮﺍﺋﺪ ﺍﻳﻦ ﻟﻴﺰﺩ ﺩﺭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﻳﻦ ﻟﻴﺰﺭ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺎ Skin typeﺑﺎﻻ Spot size ،ﺑﺰﺭﮔﺘﺮ ﻭ ﺩﺭ ﻧﺘﻴﺠﻪ ﻃﻮﻝ ﻣﺪﺕ ﻛﻤﺘﺮ ﺩﺭﻣﺎﻥ Therapeatic window ،ﺑﺰﺭﮔﺘﺮ ﻛﻪ ﻣﻮﺟﺐ ﻋﺎﺭﺿﻪ ﻛﻤﺘﺮ ﻭ ﻛﺎﺭﻣﺪﻱ ﺑﻴﺸﺘﺮ ﻣﻲﺷﻮﺩ. ﺩﺭ ﺍﻳﻦ CDﻛﻪ ﺑﻪ ﺳﻔﺎﺭﺵ ﻛﻤﭙﺎﻧﻲ Ellipseﺗﻮﻟﻴﺪ ﺷﺪﻩ ﺍﺳﺖ .ﻣﻌﺮﻓﻲ ﻟﻴﺰﺭ ،IPLﭼﮕﻮﻧﮕﻲ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ،ﻓﻮﺍﺋﺪ ﻟﻴﺰﺭ ،IPLﻣﻨﺎﻃﻘﻲ ﻛﻪ ﺩﺭ ﺁﻥ ﺍﺯ ﻟﻴﺰﺭ IPLﺑﺮﺍﻱ ﺭﻓﻊ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻛﻠﻴﭗ ﻭﻳـﺪﺋﻮﺋﻲ ﺍﺯ ﺑﻴﻤﺎﺭﻳـﺎﻥ ﻭ ﻧﺤـﻮﻩ ﺩﺭﻣـﺎﻥ ﻭ ﻧﺘﺎﻳﺞ ﺩﺭﻣﺎﻥ ﺑﺎ ﻋﻜﺲ ﻭ clipﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. 2002
)33.6 REFINEMENT IN HAIR TRANSPLANTATION: Micro and minigraft Megasession (Alfonso Barrera, M.D.
ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺩﺭ ﻣﻮﺭﺩ ﭘﻴﻮﻧﺪ ﻣﻮ ﺑﻪ ﺭﻭﺵ ﻣﻴﻜﺮﻭﮔﺮﺍﻓﺖ )ﮔﺮﺍﻓﺖ ١-٢ﻣﻮ( ﻭ ﻣﻴﻨﻲﮔﺮﺍﻓﺖ )ﮔﺮﺍﻓﺖ ٣-٤ﻣﻮ( ﺑﺮﺍﻱ ﻃﺎﺳﻲ ﻣﺮﺩﺍﻧﻪ ﻭ ﺩﻳﮕﺮ ﺍﺧﺘﻼﻻﺕ ﺭﻳﺰﺵ ﻣﻮ ﻣﻲﺑﺎﺷﺪ .ﻋﻼﻭﻩ ﺑﺮ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ،ﺗﺼﺎﻭﻳﺮ ﮔﺮﺍﻓﻴﻜﻲ ﺑﺮﺍﻱ ﻓﻬﻢ ﻣﻄﺎﻟﺐ ﺑﻪ ﻛﺎﺭ ﺭﻓﺘﻪ ﺍﺳﺖ. ﻓﺼﻞ -١ﺩﺭ ﻣﻮﺭﺩ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻣﻮ ﻣﻲﺑﺎﺷﺪ ﺗﺎ ﺍﻃﻼﻋﺎﺕ ﭘﺎﻳﻪﺍﻱ ﻗﺒﻞ ﺍﺯ ﺍﻧﺠﺎﻡ ﺍﻋﻤﺎﻝ ﭘﻴﻮﻧﺪ ﺑﻪ ﻧﻮﺁﻣﻮﺯﺍﻥ ﺑﺪﻫﺪ. ﻓﺼﻞ -٢ﺍﻃﻼﻋﺎﺕ ﺳﻮﺩﻣﻨﺪﻱ ﺩﺭ ﻣﻮﺭﺩ ﺍﻟﮕﻮﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺭﻳﺰﺵ ﻣﻮ ﻭ ﺟﺮﺍﺣﻲ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﻣﺸﻜﻼﺕ ﻓﺮﺩﻱ ﺑﻴﻤﺎﺭ ﻭ ﺑﻬﺘﺮﻳﻦ ﺭﻭﺵ ﺑﺮﺍﻱ ﺑﺮﻃﺮﻑﻛﺮﺩﻥ ﺭﻳﺰ ﻣﻮ ﻛﻤﻚ ﻣﻲﻛﻨﺪ. ﻓﺼﻞ -٣ﺩﺭ ﻣﻮﺭﺩ ﺗﺠﻬﻴﺰﺍﺕ ﻻﺯﻡ ﺑﺮﺍﻱ ﺍﻧﺠﺎﻡ ﭘﻴﻮﻧﺪ ﻣﻮ ﻭ ﻫﻤﭽﻨﻴﻦ ﺍﻃﻼﻋﺎﺗﻲ ﻛﻪ ﺑﺎﻳﺪ ﺑﻪ ﺑﻴﻤﺎﺭ ﻗﺒﻞ ﺍﺯ ﺍﻧﺠﺎﻡ ﺟﺮﺍﺣﻲ ﺩﺍﺩﻩ ﺷﻮﺩ. ﻓﺼﻞ -٤ﺗﻮﺿﻴﺢ ﻗﺪﻡ ﺑﻪ ﻗﺪﻡ ﺗﻮﺳﻂ ﺗﺼﺎﻭﻳﺮ ﻭﺍﻗﻌﻲ ﻭ ﮔﺮﺍﻓﻴﻜﻲ ﺍﻧﺠﺎﻡ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﭘﻴﻮﻧﺪ ﻣﻮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺗﺼﺎﻭﻳﺮ Caseﻫﺎﻱ ﺟﺮﺍﺣﻲﺷﺪﻩ ﺍﺯ ﺍﺑﺘﺪﺍ ﺗﺎ ﺍﻧﺘﻬﺎﻱ ﻋﻤﻞ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻧﺘﺎﻳﺞ ﻫﺮ ﻳﻚ ﺑﺤﺚ ﻣﻲﺷﻮﺩ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
34 ﻼ ﺗﻮﺳﻂ ﺭﻭﺵﻫﺎﻱ ﺩﻳﮕﺮ ﺑﺮﺍﻱ ﻃﺎﺳﻲ ﺳﺮ ﺟﺮﺍﺣﻲ ﺷﺪﻩﺍﻧﺪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺗﺮﻣﻴﻢ ﺁﻧﻬﺎ ﺑﻪ ﺭﻭﺵ ﻣﻴﻨﻲ ﻭ ﻣﻴﻜﺮﻭﮔﺮﺍﻓﺖ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻓﺼﻞ -٥ﺗﺮﻛﻴﺐ ﺟﺮﺍﺣﻲ ﭘﻴﻮﻧﺪ ﻣﻮ ﺑﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺩﻳﮕﺮ ﻣﺎﻧﻨﺪ face liftingﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺍﻳﻦ ﻓﺼﻞ Caseﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻛﻪ ﻗﺒ ﹰ ﻓﺼﻞ -٦ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺩﻳﮕﺮ ﻣﻴﻜﺮﻭﮔﺮﺍﻓﺖ ﻭ ﻣﻴﻨﻲﮔﺮﺍﻓﺖ ﺩﺭ ﻛﺎﺭﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﻭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻓﺼﻞ -٧ﻛﺘﺎﺏ ﻛﺎﺭﺑﺮﺩ ﻣﻴﻜﺮﻭﮔﺮﺍﻓﺖ ﻭ ﻣﻴﻨﻲﮔﺮﺍﻓﺖ ﺩﺭ ﭘﻨﻬﺎﻥﻛﺮﺩﻥ ﺍﺳﻜﺎﺭﻫﺎﻱ ،Scafpﺍﺻﻼﺡ ﺧﻂ ﺭﻳﺶ ﺑﺨﺼﻮﺹ ﺑﻌﺪ ﺍﺯ ،face liftﻛﺎﺷﺖ ﺍﺑﺮﻭ ،ﺳﺒﻴﻞ ،ﺭﻳﺶ ،ﺩﺭﻣﺎﻥ ﺁﻟﭙﻮﺳﭙﻲ ﺑﻪ ﻋﻠﺖ ﺳﻮﺧﺘﮕﻲ ﻭ ﻛﺎﺷﺖ ﻣﮋﻩ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻞ ٧ﺑﺮﺟﺴﺘﻪﺗـﺮﻳﻦ ﻓﺼـﻞ ﻛﺘـﺎﺏ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍﺯ ﻛﺘﺐ ﻣﺸﺎﺑﻪ ﭘﻴﻮﻧﺪ ﻣﻮ ﺭﺍ ﻣﺘﻤﺎﻳﺰ ﻣﻲﻛﻨﺪ. ــــــ
)34.6 Skin Rejuvenation with skin filler (E.E.A. Derm
1998
35.6 Textbook of Dermatology (Sixth Editions) (R.H. CHAMPION, J.L. BURTON, D.A.BURNS, S.M.BREATHNACH) (ROOK) (Software c Gention I.T. Consuliants Ltd.,) Version 1.2.0 ﻭﻳﺮﺍﻳﺶ ﺷﺸﻢ ﻛﺘﺎﺏ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ Rookﺷﺎﻣﻞ ٤ﺟﻠﺪ ﻭ ٣٦٨٣ﺻﻔﺤﻪ ﻣﻲﺑﺎﺷﺪ ﺩﺭ ﺍﻳﻦ ﻭﻳﺮﺍﻳﺶ ﺗﻤﺎﻡ ﻓﺼﻞﻫﺎ ﻣﺮﻭﺭ ﺷﺪﻩ ﻭ ﺁﺧﺮﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺍﺿﺎﻓﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﻓﺼﻞﻫﺎ ﺑﺎﺯﻧﻮﻳﺴﻲ ﺷﺪﻩ ﻭ ﺩﺭ ﺣﺪﻭﺩ % ٢٥ -٣٠ﺭﻓﺮﺍﻧﺲﻫﺎ ﺟﺪﻳﺪ ﻣﻲﺑﺎﺷﻨﺪ.
CDﺣﺎﺿﺮ ،ﺭﻭﺵ ﺍﻧﺘﺨﺎﺏ ،ﺁﻧﺴﺘﺰﻱ ﻭ ﺗﺰﺭﻳﻖ Juvedermﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ ،CDﻧﺤﻮﺓ ﺁﻧﺴﺘﺰﻱ ﺑﺪﻭﻥ ﺍﻳﻨﻜﻪ ﺁﻧﺎﺗﻮﻣﻲ ﻣﺤﻴﻂ ﻧﺎﺣﻴﻪ ﺗﺰﺭﻳﻖ ﺍﺯ ﺑﻴﻦ ﺑﺮﻭﺩ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺳﭙﺲ ﭘﺮﻛﺮﺩﻥ ﭼﻴﻦ ﻧﺎﺯﻭﺑﻴﺎﻝ ﺑﺎ Juvederm30ﻭ ﺳﭙﺲ ﺍﻓﺰﺍﻳﺶ ﺣﺠﻢ ﻟﺐ ﺑﺎ Juvederm24ﻭ ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﭼﺮﻭﻙﻫﺎﻱ ﻇﺮﻳﻒ ﺑﺎ Juvederm18ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ.
ﺩﺭ ﻫﺮ ﻓﺼﻞ ﺗﺼﺎﻭﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺳﺘﻔﺎﺩﻩﻛﻨﻨﺪﮔﺎﻥ ﺍﺯ CDﺍﻳﻦ ﻛﺘﺎﺏ ﻣﻲﺗﻮﺍﻧﻨﺪ ﺍﺯ ﻋﻜﺲﻫﺎﻱ ﻛﺘﺎﺏ ﺑﻪ ﻋﻨﻮﺍﻥ Slide Conferenceﺍﺳﺘﻔﺎﺩﻩ ﻧﻤﺎﻳﻨﺪ .ﻛﺘﺎﺏ ﺣﺎﺿﺮ ﺭﻓﺮﺍﻧﺲ ﺩﺳﺘﻴﺎﺭﻳﺎﻥ ﭘﻮﺳﺖ ﻭ Board certificationﻣﻲﺑﺎﺷﺪ. 2004 2000
2002
)36.6 Textbook of Dermatology (Rook's
)(Seven Edition) (Volume 1-4) (E-Book )37.6 Textbook of Pediatric Dermatology (JOHN HARPER ARNOLD ORANJE NEIL PROSE) (VOLUME 1 , 2 ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺩﺭ ﺧﺼﻮﺹ Pediatric dermatologyﺍﺳﺖ ﻛﻪ ﺩﺭ ﺍﻛﺜﺮ ﻛﺸﻮﺭﻫﺎ ﻳﻚ Subspecialityﺟﺪﺍﮔﺎﻧﻪ ﻣﻲﺑﺎﺷﺪ .ﻣﺆﻟﻔﻴﻦ ﺍﻳﻦ ﻛﺘﺎﺏ ﻳﻚ encyclopedic textﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻼ ﻣﺸﺎﺑﻪ ﺑﻪ ﺭﻭﺵ ﻧﮕﺎﺭﺵ ﻛﺘﺎﺏ (RooK) text book of general dermatologyﻣﻲﺑﺎﺷﺪ. ﺍﻃﻔﺎﻝ ﺑﻪ ﻛﻤﻚ 185ﻣﺤﻘﻖ ﺍﺯ ﺳﺮﺍﺳﺮ ﺟﻬﺎﻥ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩﺍﻧﺪ ﻛﻪ ﺑﻪ ﻋﻨﻮﺍﻥ board cerificaitionﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺍﻃﻔﺎﻝ ﭘﺬﻳﺮﻓﺘﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺭﻭﺵ ﻧﮕﺎﺭﺵ ﻛﺘﺎﺏ ﻛﺎﻣ ﹰ ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ ﺑﺮ ﮔﻴﺮﻧﺪﺓ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺍﺯ ﺩﻭﺭﺓ ﭘﺮﻩﻧﺎﺗﺎﻝ ﺗﺎ adolescentﻣﻲﺑﺎﺷﺪ .ﻛﺘﺎﺏ ﻣﺸﺘﻤﻞ ﺑﺮ ٢٩ﻓﺼﻞ ﺑﻮﺩﻩ ﻛﻪ ﺷﺎﻣﻞ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺷﺎﻳﻊ ﻣﺎﻧﻨﺪ Psoriasisﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻧﺎﺩﺭ ﻣﻲﺑﺎﺷﺪ .ﻫﻤﭽﻨﻴﻦ ﺁﺧﺮﻳﻦ ﭘﻴﺸﺮﻓﺖ ﺩﺭ ﮊﻧﺘﻴﻚ ﻣﻠﻜﻮﻟﻲ ﻭ ﺭﻭﺵﻫـﺎﻱ ﺩﺭﻣـﺎﻧﻲ ﺩﺭ ﺍﻳـﻦ ﻛﺘﺎﺏ ﮔﻨﭽﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺑﺨﺶ ﻋﻔﻮﻧﻲ ﻛﺘﺎﺏ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﻧﺪﻣﻴﻚ ﻣﺎﻧﻨﺪ ﻟﭙﺮﻭﺯﻱ ﻭ ﻟﻴﺸﻤﺎﻧﻴﻮﺯ ﻭ ﺍﻧﺪﻣﻴﻚ ﺗﺮﭘﻮﻧﻮﻣﺎﺗﻮﺯ ﻭ ...ﻛﻪ ﺩﺭ ﻛﺘﺎﺏﻫﺎﻱ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺩﻳﮕﺮ ﺑﻪ ﺍﺧﺘﺼﺎﺭ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ ﺗﻮﺳﻂ ﺍﻓﺮﺍﺩ ftrsthand knowledgeﺗﺤﺮﻳﺮ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺑﺨـﺶ ﻟﻴـﺰﺭ ﻛﺘﺎﺏ ﺍﺳﺘﻔﺎﺩﻩ ﻟﻴﺰﺭ ﺑﺮﺍﻱ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﭘﻴﮕﻤﺎﻧﺘﻪ ﻭ ﻋﺮﻭﻗﻲ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺭﻭﺵﻫﺎﻱ Sedationﻭ ﺑﻴﻬﻮﺷﻲ ﺩﺭ ﺍﻃﻔﺎﻝ ﺩﺭ ﻓﺼﻞ Surgeryﻛﺘﺎﺏ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ Surgeryﺗﻜﻨﻴﻚﻫﺎﻱ ﺳﺎﺩﻩ ﻭ ﭘﻴﭽﻴﺪﺓ ﺟﺮﺍﺣـﻲ ﻣﺸـﺘﻤﻞ ﺑـﺮ tissue expansionﻭ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ،graftﻛﺸﺖ ﻛﺮﺍﺗﻴﻨﻮﺳﻴﺖﻫﺎ ،ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﻛﻠﻮﺋﻴﺪ ،ﺍﺳﻜﺎﺭ ﻭ ﺳﻮﺧﺘﮕﻲ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻣﺸﺨﺼﺔ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮﺩ ﻛﺘﺎﺏ ﻋﻜﺲﻫﺎﻱ ﻣﺘﻨﺎﺑﻪ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺑﻮﺩﻩ ﻛﻪ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺍﻃﻠﺲ ﭘﻮﺳﺖ ﺩﺭ Pediatric dermatologyﻛﺎﺭﺑﺮﺩ ﺩﺍﺭﺩ .ﻭ ﺑﻪ ﮔﻔﺘـﺔ ﻣﺆﻟﻔﻴﻦ ﺗﻼﺵ ﺯﻳﺎﺩ ﺷﺪﻩ ﻛﻪ ﺗﻈﺎﻫﺮﺍﺕ ﻣﺨﺘﻠﻒ ﭘﻮﺳﺘﻲ ﺩﺭ ﻧﮋﺍﺩﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺣﺪﺍﻗﻞ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺎﻳﻊ ﺟﻤﻊﺁﻭﺭﻱ ﮔﺮﺩﺩ. )(CD I , II A Systematic Approach The Aging Face (Calvin M. Johnson, Jr., Ramsey )Alsarraf 38.6 5. Closure 9. Closure -Closure
2002
4. The Procerus and frontalis 7. Fat Removal 8. The Skin Pinch
-Resuspension
-The Submental Region
CD I: y The Coronal Browlift: 1. Introduction 2. The Incision 3. The Corrugator Muscles y Blepharoplasty: 1. Uooer Lids 3. Marking and Incision 5. Skin and Muscle 2. Lower Lids 4. The Incision 6. Fant Removal CD II: -The Deep Plane Facelift -Marking and Incision -Skin Elevation -The Deep Plane
)39.6 Treatment of Skin Disease Comprehensive therapeutic Strategies (Mark G Lebwohl Warren R Heymann, John Berth-Jones, Ian Coulson) (SALEKAN E-BOOK) (MOSBY ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺣﺎﺿﺮ ﺷﺎﻣﻞ ﺍﻃﻠﺲ +ﺍﺳﺘﺮﺍﺗﮋﻱ ﺩﺭﻣﺎﻧﻲ +ﺩﺍﺭﻭﺩﺭﻣﺎﻧﻲ ﺑﻴﻤﺎﺭﻱ ﭘﻮﺳﺖ ﻣﻲﺑﺎﺷﺪ( ﻣﺸﻜﻞ ﺍﺻﻠﻲ ﭘﺰﺷﻜﺎﻥ ﺩﺭ ﻣﻮﺍﺟﻬﻪ ﺑﻪ ﻳﻚ ﺑﻴﻤﺎﺭﻱ ﺑﻌﺪ ﺍﺯ ﺗﺸﺨﻴﺺ managementﺑﻴﻤﺎﺭﻱ ﻣﻲﺑﺎﺷﺪ .ﭼﻪ ﺳﺆﺍﻻﺗﻲ ﺑﺎﻳﺪ ﺍﺯ ﺑﻴﻤﺎﺭ ﭘﺮﺳﻴﺪﻩ ﺷﻮﺩ ﻭ ﭼﻪ ﺁﺯﻣﺎﻳﺸﺎﺗﻲ ﺑﺎﻳﺪ ﺩﺭﺧﻮﺍﺳﺖ ﮔﺮﺩﺩ .ﻫﺮ ﻓﺼﻞ ﺍﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﻳﻚ ﺑﻴﻤﺎﺭﻱ )ﺑﻪ ﺗﺮﺗﻴﺐ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎ ﺑﺮﺍﻱ ﺩﺳﺘﻴﺎﺑﻲ ﺑﻪ ﺁﺳﺎﻥ ﺑﻪ ﺑﻴﻤﺎﺭﻱ( ﺑﻮﺩﻩ ﻭ ﻫﺮ ﻓﺼﻞ ﻭ ﺷﺎﻣﻞ: -٣ﺟﺪﻭﻝ ﺑﺮﺍﻱ ﺍﻳﻨﻜﻪ ﭘﺰﺷﻚ ﭼﻪ ﺁﺯﻣﺎﻳﺸﺎﺕ ﭘﺎﺭﺍﻛﻠﻴﻨﻴﻜﻲ ﺭﺍ ﺩﺭﺧﻮﺍﺳﺖ ﻛﻨﺪ )(specific investigations
-٢ﺍﺳﺘﺮﺍﮊﻱ ﺩﺭﻣﺎﻧﻲ) management strategyﺩﺭ ﺑﺎﻟﻴﻦ ﻭ ﻣﻌﺎﻳﻨﻪ ﻭ ﺷﺮﺡ ﺣﺎﻝ ﺑﺎﻳﺪ ﭼﻪ ﻧﻜﺎﺗﻲ ﺟﺴﺘﺠﻮ ﺷﻮﺩ( -١ﺧﻼﺻﻪﺍﻱ ﺍﺯ ﺑﻴﻤﺎﺭﻱ -٤ﺩﺭﻣﺎﻥ )ﺑﻪ ﺗﺮﺗﻴﺐ ﺧﻂ ﺍﻭﻝ ،ﺧﻂ ﺩﻭﻡ ،ﺧﻂ ﺳﻮﻡ ﺩﺭﻣﺎﻥ( ﻧﻜﺘﺔ ﻣﺘﻤﺎﻳﺰﻛﻨﻨﺪﻩ ﺍﻳﻦ ﻛﺘﺎﺏ ﻧﺴﺒﺖ ﺑﻪ ﻛﺘﺎﺏﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺩﻳﮕﺮ ﭘﻮﺳﺖ ﺍﻟﻮﻳﺖﺑﻨﺪﻱ ﺩﺭﻣﺎﻥ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﺍﻟﻮﻳﺖﺑﻨﺪﻱ ﺑﺮ ﺍﺳﺎﺱ evidence-Basedﻣﻲﺑﺎﺷﺪ ﻭ ﺍﻟﻮﻳﺖ ﺑﺮ ﺍﺳﺎﺱ ﻧﻮﻉ ﻣﻄﺎﻟﻌﺎﺕ ﺍﻧﺠﺎﻡﺷـﺪﻩ ﺩﺭ ﻣﻘﺎﻻﺕ ﺍﺯ A-Eﻧﺎﻡﮔﺬﺍﺭﻱ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻪ ﻋﻨﻮﺍﻥ ﻣﺜﺎﻝ ﺩﺭ ﺩﺭﻣﺎﻥ ﺁﻛﻨﻪ ﺍﺗﺮﻭﮊﺳﻦﻫﺎﻱ ﺧﻮﺭﺍﻛﻲ ) (Aﻭ ﺍﺳﭙﻴﺮﻭﻧﻮﺍﺭﻛﺘﻮﻥ ) (Bﻧﺎﻡﮔﺬﺍﺭﻱ ﺷﺪﻩ ﻛﻪ ) (Aﻣﺸﺨﺼﻪ ) (double blind studyﺑﻮﺩﻩ ﻭ ) (Bﻣﺸﺨﺼﻪ ) (Clinical trialﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﭘﺰﺷﻚ ﻛﻤـﻚ ﻣـﻲﻛﻨـﺪ ﺗـﺎ ﺑﺘﻮﺍﻧﺪ ﺍﺭﺯﺵ ﺩﺍﺭﻭﺩﺭﻣﺎﻧﻲ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﻧﻮﻉ ﻣﻄﺎﻟﻌﻪ ﺑﻴﺎﻥ ﻛﻨﺪ .ﺳﭙﺲ ﺧﻼﺻﻪ ﻣﻘﺎﻻﺕ ﺩﺭ ﺍﺩﺍﻣﻪ ﺩﺭﻣﺎﻥ ﺫﻛﺮ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ٢١٣ﺑﻴﻤﺎﺭﻱ ﻫﻤﺮﺍﻩ ﺑﺎ ﻋﻜﺲﻫﺎﻱ ﻛﺎﻣ ﹰ ﻼ ﺭﻧﮕﻲ ﻣﻲﺑﺎﺷﺪ. )(Jean Carruthers, Alastair Carruthers
2003 ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ:
40.6 USING BOTULINUM TOXINS COSMETICALLY
MID and Lower Face Perioal Rhytides
Periorbitalarea Infraorbital Orbicularis Oculi
Horizontal Forehead Lines
Introduction
MID and Lower Face Nasalis
MID and Lower Face Perioral Rhytides
Periorbitalarea Lateral Orbital Wrinkles
Brow Injections Brow Lift
Cervical Injections Horizontal Necklace Lines
MID and Lower Face Mouthe Frown and Mentalis
Acknowledgemetns
Cervical Injections Vertical Platysmal Bands
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
35 ﺍﺭﺗﻮﭘﺪﻱ-٧
CD ﻋﻨﻮﺍﻥ 1.7
A New Generation in Cemented Hip Design (VCD) (Part I , II) (David S. Hungerford, Clayton R. Perry) Segment I: Core Decomtpression
2.7 3.7
Segment II: Trauma Case Studies: Retrograde Femoral Nailing
LCP system Description Implants and instruments Application Indications Operating techniques
LCP cases Humerus Forearm Pelvis and acetabulum Femur Tibia Periprosthetic
AO Principles of Fracture Management (Thomas P. Ruedi, William M. Murphy) (CD I , II)
5.7
Atlas of Orthopaedics Surgery (Disk 1-6)
1- AO philosophy and Its basis
2- Decision making and planning
2002
Literature and studies Related Literature Study results
4.7
7.7
2001
AO Image Collection AO Principles of fracture Management (T.P. Ruedi, W.M. Murphy) AO International AO Teaching Series-LCP (Thomas P. Ruedi, Prof. Michael Wagner) Foreword-Basics Methods of osteosynthesis AO Principles Biomechanical Principles Surgical techniques
6.7
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــــ
3- Reduction and fixation techniques
2001 4- Specific fractures
5- General topics
6- Complications
Disk 1: Condylar Plate Fixation in the Distal Femur, Malleolar Fracture Fixation, Malleolar Fracture Type B, Malleolar Fracture Type C, Tension Band Wiring on the Elbow Femoral Neck Rfacture Large Cannulated System, Fracture of the Radius Shaft 3.5 LC-DCP, Screw Fixation and Plating Disk 2: Techniques of Absolute Stability, Proximal Humerus Fracture, Reduction with Clamps, Posterior Wall Fracture, Posteror + Transverse Wall Fracture, Undeamed Tibial Nail (UTN), Intraaticular Fracture of the Distal Humerus Disk 3: Fracture of the Tibiaplateau, Tibia Fracture in Foarm LEG UTN, Reduction Techniq, The Undeamed Femoral Nail System, Dynamic Condylar Screw (DCS), Dynamic Hip Screw (DHS), Pilon Tibial Fractures (Foamed Foot) Disk 4: Application of Large Distractor, AO Asif External Fixator, PC-FIX Point Contact Fixator an Internal Biologicl, The Proximal Femoral Nail (PFN), Bicondylar Fracture of Tibia Plateau, Minimal Invasive Plating of the Tibia Disk 5: Direct and Indirect Reduction Techniques, Short Oblique Radius Fracture, Small External Fixator, Intraarticular Fracture Distal Radius, Distal Radius, Open Reduction & Fractures of the Calcaneus, Postoperative Treatment, Internal Fixation of a Humeral Shaft Fracture Disk 6: High Cinematography of a Butterfly Fracture, Posterior, Pelvic Fixations Symphysis Pubis & Pubic Rami, Pelvic Fixations, Anterior Plate Fixation 53028, The Pelvic C-Clamp, Liss Less Invasive Stabilization System, LCP Locking Compression Plate
Body in Motion (Susan K. Hillman) -Anatomy -Content -Everything -Anatomy Text
2003
-Surface Anatomy Videos -Muscle Aciton Videos
CCC (Core Curriculum in Primary Care) Orthopedics/Sport Medicine Section 1- Introduction
2- Orthopedic Procedures: A Rheumatology's Perspective
3- Xercise and Aging A Prescripton for life
ــــــ
4- Foot and Ankle Problems Part Two
ــــــ
8.7
Click'X VenttoFix SynCage (J. Webb, O. Schwarzenbach J. Thalgott) (VCD) (AO ASIF OFFICIAL TAPE)
ــــــ
9.7
FRACTURES IN ADULTS (ROCKWOOD AND GREEN'S)
ــــــ
1- General Principles
2- Upper Extremity
3- Spine
4- Lower Extremity
10.7 FRACTURES IN CHILDREN General Principlse Upper Extremity Spine Lower Extremity (ROCKWOOD AND WILKINS) (James H. Beaty, James R. Kasser)
ــــــ
11.7 FRACTURES OF THE PELVIS AND ACETABULUM (G.F. Zinghi, A. Briccoli, P.Bungaro)
ــــــ
(Salekan E-Book)
12.7 Gait Analysis an introduction (Third Edition) An interactive multi-media presentation produced using polygon software (Micheal W. Whittle)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
36 ___
33.1 Imaging of Spinal Trauma in Children (Lawrence R. Kuhns, M.D.) (University of Michigan Medical Center) Principles AND TECHNIQUES Normal Spine Variants and Anatomy Mechanisms and Patterns of Injury Thoracic Spine Injuries
13.7
Interactive orthopaedics and Sport Medicine
Epidemiology Measurements Occipitocervical Injuries
ATLAS OF SPINAL INJURIES IN CHILDREN Cervcal Spine Lumbar Spine Thoracic Spine Sacrococcygeal Spine Lumbar
Special Views and Techniques Experimental and Necropsy Data Sacral Injuries
1. Interactive Spine 2. Interactive Hand 3. Interactive hand therapy 4. Interactive Hip 5. Interactive Shoulder 6. Interactive Knee 7. Sports Injuries The Knee 8. Interactive Food and Ankle 9. Interactve Skeleton
ــــــ
14.7 Internal Fixation of a Humeral Shaft Fracture with the UHN -Technical Information
-Operation
-Postoperative Concept
ــــــ
(P.M.Rommens, J. Blum)
-Poat-op –X-ray control
- Poat-op treatment
15.7 MASTER TECHNIQUES IN ORTHOPAEDIC SURGERY RECONSTRUCTIVE KNEE SURGERY Southern California Center for Sports Medicine Long Beach, California (DOUGLAS W. JACKSON, M.D.)
ــــــ
: ﺷﺎﻣﻞCD ﻣﺒﺎﺣﺚ ﺍﻳﻦ. ﻣﻄﺎﻟﺐ ﺩﺭ ﺁﻥ ﻣﻲﺑﺎﺷﺪserch ﺑﻮﺩﻩ ﻭ ﻗﺎﺑﻠﻴﺖTEXT ﮔﺮﺩﻳﺪﻩ ﻭ ﺷﺎﻣﻞ ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﻛﺘﺎﺏ ﺑﻪ ﺻﻮﺭﺕebook ﻛﻪ ﺷﺎﻣﻞ ﻛﻞ ﻣﺘﻦ ﻛﺘﺎﺏ ﻓﻮﻕﺍﻟﺬﻛﺮ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪCD ﺍﻳﻦ PART IV INTRAARTICULAR FRACTURES OF THE TIBIA AND PATELLA
Operating Room Environment
Arthroscopic Management of Intraarticular Tibial Fractures Arthroscopically-Assisted Fixation of Patella Fractures Open Reduction Internal Fixation of Intraarticular Fractures of the Tibia
PART I EXTENSOR MECHANISM PATELLOFEMORAL PROBLEMS
Arthroscopic Lateral Release of the Patella with Electrocautery Anteromedial Tibial Tubercle Transfer Patellectomy PART II MENISCUS SURGERY
PART V ARTICULAR CARTILAGE AND SYNOVIUM
Meniscus Repair: The Outside-In Technique Meniscus Repair: The Inside-Out Technique Meniscus Repair: The All-Inside Arthroscopic Technique
Arthroscopic Chondroplasty Osteochondritis Dissecans Arthroscopic Synovectomy
PART III LIGAMENT INJURIES AND INSTABILITY
Anterior Cruciate Ligament Reconstruction Arthroscope-Assisted Posterior Cruciate Ligament Repair/Reconstruction Posterolateral Corner Collateral Ligament Reconstruction Surgical Technique for Knee Dislocations High Tibial Osteotomy in Knees with Associated Chronic Ligament Deficiencies
35.1 Magnetic Resonance Imaging in Orthopedics and Sport Medicine (David W. Stoller) MRI ﺗﻬﻴﺔ ﺗﺼﺎﻭﻳﺮ-١ ﺟﻬﺖ ﺳﻴﺴﺘﻢ ﻣﻮﺳﻜﻮﻟﻮﺍﺳﻜﻠﺘﺎﻝEcho-Planar ﺍﺻﻮﻝ ﺗﺼﻮﻳﺮﺳﺎﺯﻱ-٢ ﺯﺍﻧﻮ-٣ ﺁﺭﻧﺞ-٤ Kinematic MRI -٥
MRI ﺍﺛﺮﺍﺕ ﺑﻴﻮﻟﻮﮊﻳﻚ ﻭ ﺍﻳﻤﻨﻲ ﺩﺭ-٦ ﻋﻀﺮﻭﻑ ﻣﻔﺼﻠﻲ ﻭ ﺩﮊﻧﺮﺍﺳﻴﻮﻥ ﻋﻀﺮﻭﻓﻲMRI -٧ ﻣﭻ ﭘﺎ ﻭ ﭘﺎ-٨ ﻣﭻ ﺩﺳﺖ ﻭ ﺩﺳﺖ-٩ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ-١٠
: ﺩﺭ ﺍﺭﺗﻮﭘﺪﻱ ﻭ ﻃﺐ ﻭﺭﺯﺵ ﻣﻲﺑﺎﺷﺪ ﻭ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖMRI ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻛﺎﺭﺑﺮﺩ ﺳﻪﺑﻌﺪﻱMRI ﺗﻜﻨﻴﻚ ﺑﺎﺯﺳﺎﺯﻱ ﺟﻬﺖ-١١ (Hip) ﻣﻔﺼﻞ ﺭﺍﻥ-١٢ ﺷﺎﻧﻪ-١٣ (TMJ) ﻣﻔﺼﻞ ﻛﻤﭙﻮﺭﻭﻣﺎﻧﺪﻳﺒﻮﻻﺭ-١٤ ﺍﺯ ﻣﻐﺰ ﺍﺳﺘﺨﻮﺍﻥMRI ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ-١٥
(VCD) (Video-Atelier Othmar Keel AG) -CCA - Straight Shaft -CCE -Vault Pan -CCB -Socket -CBC Stem -RM Cup
ــــــ
ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻥ ﻭ ﺑﺎﻓﺖ ﻧﺮﻡ-١٦ ﺁﺳﻴﺒﻬﺎﻱ ﻋﻀﻼﻧﻲMRI -١٧
16.7 MATHYS ORTHOPAEDICS
ــــــ
17.7 MATHYS-ORTHOPAEDICS HIP PROSTHESES (VCD)
ــــــ
1. Cemented Stem-CCA
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
2. Cemented Cup-CCB
3. Cementless Steam-CBC
4. Cementless Cup-RM Cup
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
37 (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins)
18.7 Operative Arthroscopy
2003
Shoulder: Arthroscopic Cuff Repair: -Mssive U-Shaped Tear: Subscapulais, Infraspinatus and Biceps (Stephen S. Burkhar, MD San Antonio, Texas) -Partial: Repair of Oartial Articular Sufrace Rotator Cuff Tear (Stephen S. Burkhar, MD San Antonio, Texas), San Antonio, Texas Slap Lesions: -Arthroscopic Repair of the Slap Lesion (Stephen S. Burkhar, MD San Antonio, Texas) 19.7 Operative Arthroscopy (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins)
2003
Hip: Southern Sport Medicine & Orthopaedic Center Operative Hip Arthroscopy: -Dense Soft Tissue Envelope -Constrained Ball and Socket Anatomy 20.7 Operative Arthroscopy (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins)
2003
-Thick Capsule, Limited Compliance
Ankle: Ankle Arthroscopy (James Tasto M.D.) - Ankle & Subtalar Arthroscopy Operative Arthroscopy (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins) 21.7
2003
Wrist: Wrist Arthroscopy (Robert Richards MD FRCSC) -Portal Markings -Establishing the 3/4 Portal -Radiocarpal Arthroscopy Carpal Tunnel Release 22.7 Operative Arthroscopy (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins)
2003
Knee (CD-1): Arthroscopic meniscal repair: -suture repair -implantable fixation Knee (CD-2): -ACL -Complex articular surface injuries -Fractures -Patellofemoral 23.7 Operative Arthroscopy (SECOND EDITION) (John B. McGinty)
ــــــ
1- Basic Principles
2- The Knee
24.7 Operative Orthopaedics
3- The Shoulder
4- The Elbow
5- The Wrist
6- The Foot and Ankle
7- The Temporomandibular Joint
8- The Spine
9- The Hip
1999
(Ninth Edition) (CAMPBELL'S) (S. TERRY CANALE) . ﭼﺎﭖ ﺑﺎ ﺗﻤﺎﻣﻲ ﺗﺼﺎﻭﻳﺮ ﻣﺮﺗﺒﻂ ﺑﺎ ﻛﺘﺎﺏ ﻣﻲﺑﺎﺷﺪSerch ﻛﺎﻣﻞ ﻛﺘﺎﺏ ﻛﻤﭙﻞ ﺍﺭﺗﻮﭘﺪﻱ ﻣﻲﺑﺎﺷﺪ ﻭ ﻗﺎﺑﻠﻴﺖTEXT ﺷﺎﻣﻞCD ﺍﻳﻦ
2003
25.7 OPERATIVE ORTHOPAEDICS (CAMPBELL'S)
: ﺷﺎﻣﻞCD ﻛﺘﺎﺏ ﻛﻤﭙﻞ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻓﻴﻠﻢﻫﺎﻱ ﺍﻳﻦTEXT ﺷﺎﻣﻞ ﻋﻤﻞﻫﺎﻱ ﺟﺮﺍﺣﻲ ﻣﺮﺗﺒﻂ ﺑﺎCD ﺍﻳﻦ Trochanteric osteotomy-hip revision Reconstruction nailing femoral fracture Anterior Cervical discectomy & fusion
Arthroscopic assisted ACL reconstruction Chevron osteotomy hallux valgus
Screw fixation SCFE Ligament balancing Knee arthroplasty
Intramedullary nailing forearm fracture ORIF calconeal fracture
2002
26.7 ORTHOPAEDIC SURGERY (Third Edition) (CHAPMAN) - Surgical Principles and Techniques - Sport Medicine - Skeletal Disorders
- Fractures, Dislocations, Nonunions and Malunions - Neoplastic, Infectious - The Spine
- The Hand - Neurologic and Other - Pediatric Disorders
- The Foot - Joint Reconstruction, Arthritis, and Arthroplasty
27.7 OPERATIVE ORTHOPAEDICS
(CAMPBELL'S) (Tenth Edition) (Volume 1-4) (E-Book) (S. Terry Canale, MD) 28.7 PEDIATRIC ORTHOPAEDICS (Lovell and Winter's) (Fifth edition) (Salekan E-Book) (Volume II) KYPHOSIS
THE UPPER LIMB
SPONDYLOLYSIS AND SPONDYLOLISTHESIS
DEVELOPMENTAL HIP DYSPLASIA AND DISLOCATION
THE CERVICAL SPINE
LEGG-CALVE-PERTHES SYNDROME
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
2003 2001
SLIPPED CAPITAL FEMORAL EPIPHYSIS DEVELOPMENTAL COXA VARA, TRANSIENT SYNOVITIS, AND IDIOPATHIC CHONDROLYSIS OF THE HIP THE LOWER EXTREMITY
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
38 LEG LENGTH DISCREPANCY SPORTS MEDICINE IN CHILDREN AND ADOLESCENTS
THE FOOT MANAGEMENT OF FRACTURES
THE LIMB-DEFICIENT CHILD THE ROLE OF THE ORTHOPAEDICS IN CHILD ABUSE
29.7 Photographic manual of Regional Orthopaedic and Neurological Tests
ــــ
. ﻓﺼﻮﻝ ﺑﺮ ﺍﺳﺎﺱ ﻣﺤﻞ ﻣﻮﺭﺩ ﻣﻌﺎﻳﻨﻪ ﻃﺮﺍﺣﻲ ﻭ ﻗﺴﻤﺖﺑﻨﺪﻱ ﺷﺪﻩﺍﻧـﺪ. ﺩﺭ ﻣﻮﺍﻗﻊ ﻟﺰﻭﻡ ﺗﺼﺎﻭﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻚ ﺿﺮﻭﺭﻱ ﻧﻴﺰ ﺍﺿﺎﻓﻪ ﺷﺪﻩﺍﻧﺪ. ﺗﺼﻮﻳﺮ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﺗﻤﺎﻡ ﻣﻌﺎﻳﻨﺎﺕ ﻧﻮﺭﻭﻟﻮﮊﻳﻚ ﻭ ﺍﺭﺗﻮﭘﺪﻳﻚ ﺭﺍ ﺑﺎ ﺟﺰﺋﻴﺎﺕ ﺗﻤﺎﻡ ﺭﻭﺷﻦ ﻣﻲﺳﺎﺯﺩ٨٥٠ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯCD ﺍﻳﻦ ﺩﺭ ﺿـﻤﻦ ﻳـﻚ. ﺩﺭ ﻳﻚ ﺻﻔﺤﻪ ﻳﺎ ﺩﻭ ﺻﻔﺤﻪ ﻣﻘﺎﺑﻞ ﻫﻢ ﺑﺎ ﻋﻜﺲﻫﺎﻳﻲ ﻛﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻣﻌﺎﻳﻨـﻪ ﺭﺍ ﺑﻮﺿـﻮﺡ ﻧﺸـﺎﻥ ﻣـﻲﺩﻫﻨـﺪ ﺗﻮﺿـﻴﺢ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖTest ﻫﺮ.ﻣﻌﺎﻳﻨﺎﺕ ﺍﺯ ﻓﻘﺮﺍﺕ ﮔﺮﺩﻧﻲ ﻭ ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ ﺷﺮﻭﻉ ﻭ ﺑﻪ ﻓﻘﺮﺍﺕ ﻛﻤﺮﻱ ﻭ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺗﺤﺘﺎﻧﻲ ﺧﺘﻢ ﻣﻲﺷﻮﻧﺪ . ﺍﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺩﺭ ﺑﻜﺎﺭﮔﻴﺮﻱ ﺗﺴﺖﻫﺎﻱ ﺣﺴﺎﺳﺘﺮ ﻭ ﺍﺧﺘﺼﺎﺹﺗﺮ ﻛﻤﻚ ﻓﺮﺍﻭﺍﻥ ﺑﻪ ﭘﺰﺷﻚ ﻣﻲﻧﻤﺎﻳﺪ. ﻧﻴﺰ ﺑﺮﺍﻱ ﻫﺮ ﻣﻌﺎﻳﻨﻪ ﺗﻌﺮﻳﻒ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻣﻴﺰﺍﻥ ﺣﺴﺎﺳﻴﺖ ﻭ ﻗﺎﺑﻠﻴﺖ ﺍﻋﺘﻤﺎﺩ ﺑﻪ ﺁﻥ ﻣﻌﺎﻳﻨﻪ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﺳﺎﺯﺩSensitivity/Relialility Scale 45.1 Radiology imaging Bank:
1. Section
2. History
Orthopeadic 3. Findings 4. Diagnosis
5. Images
6. Classification
30.7
Range of Motion-AO Neutral-O Method
31.7
SPINE (VCD 1-A) (J. o' Dowd, P. Moulin, E. Morscher P. Moutin, J. Webb, M. Aebi)
7. Imagenumber ــــــ ــــــ
Pedicie Identification (Conultant: J. O'Dowd)
Cervical Spine Locking Plate: Corporectomy C6 (P. Moulin)
CS-Titanium Locking Plate (E. Morscher P.Moutin)
Cervical Spine Locking Plate (P. Moulin)
Cervical Spine Locking Plate Vertebrectomy C6 (J. Webb, M. Aebi) Posterior Cervical Plate Fixation ( C2-T1) ( j.wEBB, M.Aebi)
Posterior Plating Technique C6 to T1 (J. Webb, M.Aebi)
32.7 SPINE (VCD 1-B) (M. Aebi, J. Webb, Ghr. Ulrich, J. Nothwang, B. Jeanneret, M. Aebi J. Webb, J. Webb, M. Aebi P. Bryne) AnteriorFixation of the Dens with Cannulated Screws ( M. Aebi, J. Webb Ghr. Ulrich, J. Nothwang) Cervix: Fixation C3-C7 in Presenceb of a Laminectomy ( B. Jeanneret) U.S.S: Lumbar Degenrrative Scotiosis Side-Opening Pedicte Screws (M.Aebi J.Webb)
U.S.S: Lumbosacral Stabilisation: Back-Opening Pedicte Screws (M. Aebi J. Webb) USS: Lumbosacral Fusion Sacral Implants (J. Webb M.Aebi P.Bryne)
33.7 SPINE (VCD 1-C) (J. Webb, M. Aebi, G.Wisner, J. Webb M. Aebi, J. Webb M. Aebi, J. O'Dowd) USS: Lumbosacral Stabilisation Side Opening Pedicle Screws (J.Webb, M.Aebi, G. Winsner)
Universal Spine System Thoraco - Lumbar Fractures (J. Webb M. Aebi)
ــــــ Universal Spine System:
Right Thoracic Scoliosis: Side Opening hooks & Screws (J.Webb, M.Aebi, J.O'Dowd)
34.7 SPINE (VCD 1-D) (J. Webb, O. Schwarzenbach, J. Thalgott & J. Webb, J. Webb) Click'X (J.Webb)
ــــــ
The Snterior Rod System (J.Thalgott & J.Webb)
35.7 SPINE implants
ــــــ
Contact Fusion Cage (J.Webb)
(CD I , II)
ــــ . ﻧﺤﻮﺓ ﺟﺮﺍﺣﻲ ﻭ ﺑﻪﻛﺎﺭﮔﺬﺍﺷﺘﻦ ﭘﺮﻭﺗﺰﻫﺎﻱ ﻣﻬﺮﻩ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺍﻃﻼﻋﺎﺕ ﻛﺎﻣﻠﻲ ﺭﺍﺟﻊ ﺑﻪ ﭘﺮﻭﺗﺰﻫﺎﻱ ﺟﺎﻧﺸﻴﻦ ﺟﺴﻢ ﻣﻬﺮﻩ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩCD ﺩﺭ ﺍﻳﻦ: CD I . ﺑﺮ ﺭﻭﻱ ﻣﻬﺮﻩﻫﺎﻱ ﻛﻤﺮﻱ ﺩﺭ ﺩﺭﻣﺎﻥ ﻣﻮﺍﺭﺩ ﺗﺮﻭﻣﺎﺗﻴﻚ ﻭ ﺍﺳﻜﻮﺍﻧﻴﻮﺭ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩDiapasone-hook ﻧﺤﻮﻩ ﺟﺮﺍﺣﻲ ﻭ ﺑﻜﺎﺭﮔﺬﺍﺷﺘﻦ ﺩﺳﺘﮕﺎﻩCD ﺩﺭ ﺍﻳﻦ: CD II 1999
36.7 Surgery of the Foot and Ankle (Michael J. Coughlin, Roger A. Mann) Volume One: 1. General Considerations
2. The forefoot
Volume Two: 1. Miscellaneous Disorders
2. Sports Medicine
37.7 Surgery of the Knee
3. Postural Disorders 3. Pediatrics
4. Neurologic Disorders
5. Arthritic Conditions
4. Trauma
2001
(Third Edition) (John N. Insall, W. Norman Scott)
1- VIDEO
2- PHOTOS
3- ILLUSTRATIONS
- Anatomy
-Anatomical Aberrations
4- 3D KNEE
-Biomechanics
-Imaging
5-IMAGING -Surgical Approaches
38.7 The Adult Hip On CD
ــــــ
39.7 The Shoulder (2
ــــــ
nd
Edition) (Rockwood and Matsen)
1- Disorders of the Acromiocavicular Joint
40.7 The Unreamed Femoral Nail System
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
2- Disorders of the Sternoclavicular Joint
3- Glenohumeral Instability
(N. Sudkamp P. Duwelius)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
4- Glenohumeral Arthritis and Its Management
ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
41.7 Video Collection Labor for Experimental Orthopaedics Surgery
VCD 1-A
( R Texhammar,
ــــــ
P Holzach)
AO/ASIF Instrumentation Care and Maintenance
VCD 1-B
39 AO/ASIF VCD (CD 1-10)
PreOperative Preparation of the Patient
Approaches to the Femur, Pelvis Knee and Elbow
(P Matter M.D., S.M. Perren, B Noesberger)
Approach to the Proximal Femur and Elbow
After-Care Following Lower Leg Surgery
Dynamic Compression Unit
Approaches to the Upper Limb
Reduction Techniques
DCP 4.5 Compression Tibial Shaft
VCD 1-C (B Noesberger, J.Stadler, P. Holzach, Th. Ruedi) DCP 4.5 Butterss Tibial Plateau
LC-DCP 4.5 for the Distal Tbia
DCP 3.5 Radius Shaft 3.5 LC-DCP
DCP 4.5 Neutralization Plate of a Spiral Fracture
Fracture of the Radius Shaft 3.5 LC-DCP with Shaft screws
VCD 2-A (S.M. Perren, K.M. Pfeiffer M.D.)
. Correctional Osteotomy (dist. Radius)
. Basic Lag Screw Techniques . Internal Fixation of a Closed Butterfly Fracture of Right Tibia (Operation Video)
VCD 2-B (Th. Ruedi, J. Mast M.D., P.E Ochsner) Fracture of the Lateral Tibiaplateau Pilon Fracture
Indirect Reduction and Plate Fixation of a Pilon Fracture Malleolar fracture Type A
Malleolar Fracture Type B Malleolar Fracture Type C
VCD 2-C (T.Ruedi, P.Holzach, Th. Ruedi M. Schuler, P. Hozach, P Regazzoni, Th. Ruedi M.D.) Proximal Humerus Fracture Distal Humerus Fracture Type C 1.3
VCD 3-A
Tension Band Wiring of the Elbow Dynamic Hip Screw
Intaarticular Type C Fracture of the Distal Humerus Dynamic Condylar Screw (DCS) Proximal Femur
Condylar Plate Fixation in the Distal Femur
(R. Ganz R.P. Jakob P.Koch, Th Ruedi M.D., P.Regazzoni)
Condylar Plate Proximal Femur
Large Cannulated Screw System
AO/ASIF External Fixator
VCD 3-B Small External Fixator Distractor Handling Consultant Seija Pearson
VCD 3-C
Using the Small Air Drill Compact Air Drive Basic Operating Procedure & Working with attachments Intramedullary Nailing with the AO/ASIF Universal Femoral Nail
(R. Frigg, D. Hontzsch, Th. Ruedi)
The Interlocking of the Universal Femoral Intramedullary Nail Opening Procedure of the Tibial Cavity for Intramedullary Nailing The Universal Tibial Nail
VCD4
AO Universal Femoral Nail With Distractor
Intramedullary Nailing of the Tibia Intramedullary Nailing of the Tibia with a Pseudarthrosis Mid-Shaft Tibial Fracture Locked Universal Nail
(R. Frigg, Ch. Krettek)
UTN Unreamed Tibial Nail
Distal Aiming Device for UTN
ﭼﺸﻢﭘﺰﺷﻜﻲ-٨
CD ﻋﻨﻮﺍﻥ 1.8
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
Atlas of Clinical Oncology Tumors of the Eye and Ocular Adnexa (American Cancer Society) (Devron H. Char, MD)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2001
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
40
ﺍﻳﻦ CDﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: 4- ORBITAL TUMORS
3- RETINAL AND OPTIC NERVEHEAD TUMORS
2- UVEAL AND INTRAOCULAR TUMORS
1- LID AND CONJUNCTIVAL TUMORS
ــــ
)ATLAS OF OPHTALMOLOGY (RICHARD K. PARRISG II) (CD I , II) (Mosby
2.8
ــــ
)ATLAS OF OPHTHALOMOLGY (SUE FORDRONALD MARSH) (Mosby ﻼ ﻣﻌﻠﻮﻡ ﻭ ﻣﺸﺨﺺ ﺑﻮﺩﻩ ،ﻣﻄﺎﻟﻌﺔ ﻛﺘﺐ textﺑﺪﻭﻥ ﻫﻤﺮﺍﻫﻲ ﺍﻃﻠﺲﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﺗﺄﺛﻴﺮ ﻭ ﻛﺎﺭﺁﺋﻲ ﻻﺯﻡ ﺭﺍ ﻧﺨﻮﺍﻫﺪ ﺩﺍﺷﺖCD .ﻫﺎﻱ ﺫﻳﻞ ﻛﻪ ﺣﺎﻭﻱ ﻣﻌﺘﺒﺮﺗـﺮﻳﻦ ﻭ ﺷـﻨﺎﺧﺘﻪﺷـﺪﻩﺗـﺮﻳﻦ ﺍﺭﺯﺵ ﻳﻚ ﺍﻃﻠﺲ ﺧﻮﺏ ﺩﺭ ﺗﻤﺎﻣﻲ ﺷﺎﺧﻪﻫﺎﻱ ﻋﻠﻢ ﭘﺰﺷﻜﻲ ﺧﺼﻮﺻﹰﺎ ﭼﺸﻢﭘﺰﺷﻜﻲ ﻛﺎﻣ ﹰ ﺍﻃﻠﺲﻫﺎﻱ ﭼﺸﻢﭘﺰﺷﻜﻲ ﻣﻲﺑﺎﺷﻨﺪ ،ﻋﻼﻭﻩ ﺑﺮ ﺗﻮﺍﻧﺎﺋﻲ ﺑﺰﺭﮔﻨﻤﺎﻳﻲ ﺗﺼﺎﻭﻳﺮ ﺗﺎ ﭼﻨﺪﻳﻦ ﺑﺮﺍﺑﺮ ﺑﺪﻭﻥ ﻛﺎﺳﺘﻪﺷﺪﻥ ﺍﺯ ﻛﻴﻔﻴﺖ ﺑﻲﻧﻈﻴﺮ ﺁﻥ ﺩﺍﺭﺍﻱ ﻗﺎﺑﻠﻴﺖ Searchﻭ ﺟﺴﺘﺠﻮﻱ Caseﻣﻮﺭﺩ ﻧﻈﺮ ﺩﺭ ﻛﻤﺘﺮﻳﻦ ﺯﻣﺎﻥ ﻣﻤﻜﻦ ﻣﻲﺑﺎﺷﻨﺪ .ﺩﺭ ﻛﻨﺎﺭﺩﺍﺷﺘﻦ ﺍﻳـﻦ ﺍﻃﻠـﺲﻫـﺎ ﭼـﻪ ﺑـﻪ ﻫﻨﮕـﺎﻡ ﺁﻣﻮﺯﺵ ﻭ ﻳﺎﺩﮔﻴﺮﻱ ﺩﺭ ﺩﻭﺭﺓ ﺩﺳﺘﻴﺎﺭﻱ ﻭ ﭼﻪ ﺑﻪ ﻫﻨﮕﺎﻡ Practiceﻭ ﻣﻮﺍﺟﻪ ﺑﻪ Caseﻫﺎﻱ ﻧﺴﺒﺘﹰﺎ ﻧﺎﺩﺭ ﺩﺭ ﻛﻠﻴﻨﻴﻚ ﺑﺴﻴﺎﺭ ﻣﻔﻴﺪ ﻭ ﻛﻤﻚﻛﻨﻨﺪﻩ ﺧﻮﺍﻫﺪ ﺑﻮﺩ.
3.8
)Basic and Clinical Science Course Retina and Vitreous (Section 12) (American Academy of Ophthalmology
4.8
ــــ
Basic Ophthalmology Physiology of the Eye )OPHTHALMOLOGY (Myron Yanoff.Jay S. Duker) (Mosby ﺍﻳﻦ CD ٣ﺑﻪ ﺗﻮﺿﻴﺢ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﭼﺸﻢ ﻭ ﺭﺍﻫﻬﺎﻱ ﺑﻴﻨﺎﺋﻲ ،ﻣﻜﺎﻧﻴﺴﻢ ﻋﻴﻮﺏ ﺍﻧﻜﺴﺎﺭﻱ ﻭ ﻧﻴﺰ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭼﺸﻢ ﺩﺭ ﺳﻄﺢ ﻧﻴﺎﺯ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﭘﺰﺷﻜﻲ ،ﭘﺰﺷﻜﺎﻥ ﻋﻤﻮﻣﻲ ﻭ ﭘﺰﺷﻜﺎﻥ ﻣﺘﺨﺼﺺ ﺩﺭ ﺳﺎﻳﺮ ﺭﺷﺘﻪﻫﺎﻱ ﭘﺰﺷﻜﻲ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺩﻳﺪﻥ ﺍﺷﻜﺎﻝ ﺷﻤﺎﺗﻴﻚ ﺯﻳﺒﺎ ﻭ ﻧﻴﺰ ﺗﺼﺎﻭﻳﺮ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﺨﺘﻠﻒ ﭼﺸﻤﻲ ﻣﻮﺟﻮﺩ ﺩﺭ ﺍﻳﻦ CDﻫﺎ ﺑﺮﺍﻱ ﻣﺘﺨﺼﺼﻴﻦ ﻣﺤﺘﺮﻡ ﭼﺸﻢﭘﺰﺷﻜﻲ ﻧﻴﺰ ﺧﺎﻟﻲ ﺍﺯ ﻟﻄﻒ ﻧﺨﻮﺍﻫﺪ ﺑﻮﺩ
5.8
ــــ
Clinical update course on Retina
2003
)(SALEKAN E-BOOK
6.8 7.8 8.8
CDﻓﻮﻕ ﺍﺯ ﺳﺮﻱ CDﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ (Lifelong education for the ophthalmologist) LEOﻣﺘﻌﻠﻖ ﺑﻪ ﺁﻛﺎﺩﻣﻲ ﭼﺸﻢﭘﺰﺷﻜﻲ ﺁﻣﺮﻳﻜﺎ ) (AAOﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ Lecture ١٥ﻭ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ،ﻣﺮﻭﺭﻱ ﺩﺍﺭﺩ ﺑﺮ ﺟﺪﻳﺪﺗﺮﻳﻦ ﻣﺘﺪﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺩﺭ ﻓﻴﻠـﺪ ﻭ ﺗﻴـﺮﻩ ﻭ ﺭﺗﻴﻦ .ﺍﺯ ﺟﻤﻠﻪ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ CDﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺷﻴﻮﻩﻫﺎﻱ ﺩﺭﻣﺎﻥ endophthalmitis ،macular hole ،BRVO ،DR ،AMDﻭ ...ﺍﺷﺎﺭﻩ ﻧﻤﻮﺩ. ــــ
)Clinical Update Course on Neuro-ophthalmology (Peter J. Savino, MD, Steven E. Feldon. MD, Barrett Katz, MD, Thmas L. Slamovits, MD ﺍﻳﻦ CDﺑﻪ ﻣﻌﺮﻓﻲ ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﮔﻠﻮﻛﻮﻡ ﻭ ﺁﺧﺮﻳﻦ ﭘﻴﺸﺮﻓﺖﻫﺎﻱ ﺣﺎﺻﻠﻪ ﺩﺭ ﺁﻧﻬﺎ ﻣﻲﭘﺮﺩﺍﺯﺩ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ Lecture ٩ﺍﺯ ﺍﺳﺘﺎﺩﺍﻥ ﺻﺎﺣﺐﻧﺎﻡ ﺍﻳﻦ ﺭﺷﺘﻪ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺯ ﺟﻤﻠﻪ ﻣﺒﺎﺣـﺚ ﻣﻬـﻢ ﺁﻣـﻮﺯﺵ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺩﺭ ﺍﻳـﻦ CDﻣـﻲﺗـﻮﺍﻥ ﺑـﻪ LTP ،Perimetryﻭ CPCﺍﺷﺎﺭﻩ ﻧﻤﻮﺩ.
ــــ
1999
)(SALEKAN E-BOOK
9.8
10.8 Complications in Phacoemulsification
ﺑﻪ ﻗﻠﻢ ﺑﺮﺟﺴﺘﻪﺗﺮﻳﻦ phacosurgenﻫﺎﻱ ﺣﺎﻝ ﺣﺎﺿﺮ ﺩﺭ ﺩﻧﻴﺎ ﻣﻦﺟﻤﻠﻪ … , H. Gimbel ، H. Fineﺗﻤﺎﻣﹰﺎ ﺑﻪ ﺗﻮﺿﻴﺢ ﺗﻜﻨﻴﻜﻬﺎﻱ ﻣﺨﺘﻠﻒ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ، Phacoﻋﻮﺍﺭﺽ ﺍﺣﺘﻤﺎﻟﻲ ،ﺷﻴﻮﺓ ﺗﺸﺨﻴﺺ ﺑﻪ ﻣﻮﻗﻊ ﻭ ﭼﮕﻮﻧﮕﻲ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺁﻧﻬﺎ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺍﺷﻜﺎﻝ ﺷـﻤﺎﺗﻴﻚ ﻭ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﺁﻥ ﺩﺭ ﺩﺭﻙ ﻣﻜﺎﻧﺴﻢ ﻭ ﻋﻠﺖ ﺑﺮﻭﺯ ﻋﻮﺍﺭﺽ ﻭ ﭼﮕﻮﻧﮕﻲ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﻧﻴﺰ managementﺁﻥﻫﺎ ﺑﺴﻴﺎﺭ ﻛﻤﻚﻛﻨﻨﺪﻩ ﻭ ﺩﺭ ﻧﻮﻉ ﺧﻮﺩ ﺑﻲﻧﻈﻴﺮ ﺍﺳﺖ. )11.8 CONTACT LENS COMPLICATIONS Efron Grading Morphs For the clinical assessment of contact lens complications (NATHAN EFRON, PHILIP MORGAN ﺍﻳﻦ CDﻋﻮﺍﺭﺽ ﻣﺨﺘﻠﻒ ﻧﺎﺷﻲ ﺍﺯ ﻛﺎﺭﺑﺮﺩ ﻟﻨﺰﻫﺎﻱ ﺗﻤﺎﺳﻲ ﻭ ﭼﮕﻮﻧﮕﻲ ﭘﻴﺸﺮﻓﺖ ﻭ ﺳﻴﺮ ﺁﻧﻬﺎ ﺭﺍ ﺑﻪ ﺻﻮﺭﺗﻲ ﺑﺴﻴﺎﺭ ﺯﻳﺒـﺎ ﻭ ﺑﻴﺎﺩﻣﺎﻧـﺪﻧﻲ ﻧﻤـﺎﻳﺶ ﻣـﻲﺩﻫـﺪ ﺑﻄﻮﺭﻳﻜـﻪ ﺗﺸـﺨﻴﺺ ﻭ Gradingﻋﻮﺍﺭﺿـﻲ ﭼـﻮﻥ microcystes ،epithelial polymegethism
، epithelial
papillary conjunctivitisﻭ ...ﻣﻴﺴﺮ ﻣﻲﮔﺮﺩﺩ. )12.8 Dodick Laser Photolysis (Ultra Small Incision Cataract Surgery) (Jack M. Dodik
ــــ
Journal of Cataract & Refractive Surgery Surgical Cases Provided by Photolysis System Manufacturer
2000
Department of Clinical Ophthalmology Institute of Ophthalmology University College London
)(Hamish MA Towler, Julian A Patterson, Susan Lightman
13.8 Diabetes And The Eye
ﺍﻳﻦ CDﺁﻣﻮﺯﺵ ﺟﺎﻣﻌﻲ ﺍﺯ ﻣﻘﻮﻟﺔ diabetic retinopathyﺍﺭﺍﺋﻪ ﻣﻲﻧﻤﺎﻳﺪ .ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﻣﻦﺟﻤﻠﻪ Fluorescein angiographyﻭ ﺑﺎﻻﺧﺮﻩ ﻟﻴﺰﺭﺗﺮﺍﭘﻲ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻣﻬـﻢ ﺑـﻪ ﻛﻤـﻚ ﻋﻜـﺲ ﻭ textﺁﻣـﻮﺯﺵ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖ. ﻫﻤﭽﻨﻴﻦ CDﻣﺬﻛﻮﺭ ﺩﺍﺭﺍﻱ ﻗﺎﺑﻠﻴﺖ Seff-testﺍﺯ ﻣﻄﺎﻟﺐ ﻣﻮﺟﻮﺩ ﺩﺭ ﺁﻥ ﻣﻲﺑﺎﺷﺪ. 2000
)14.8 DICTIONARY OF VISUAL SCIENCE AND RELATED CLINICAL TERMS (Henry W. Hofstetter, John R. Griffin, Morris S. Berman, Ronald W. Everson
2004
)15.8 Duane’s Ophthalmology (Foundations of clinical Ophthalmology) (LIPPINCOTT-RAVEN
ــــ
)(CD I , II
ــــ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
)(David I. Silbert, MD FAAP
16.8 Endoscopic Dacryocystorhinostomy (DCR) Advantages and Indications
Welch Allyn Institute of Interactive Learning ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
17.8 EENT
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
41 18.8 Endoscopic Laser Assisted Lacrimal Surgery (Russel S. Gonnering, MD) (VCD)
ــــ
. ﻓﻮﺍﻳﺪ ﺁﻥ ﺭﺍ ﺑﺮﺭﺳﻲ ﻣﻲﻧﻤﺎﻳﺪ، ﺑﻪ ﺁﻣﻮﺯﺵ ﺍﻳﻦ ﺷﻴﻮﻩ ﻛﻤﺘﺮ ﺗﻬﺎﺟﻤﻲ ﺩﺭ ﺟﺮﺍﺣﻲ ﻣﺠﺎﺭﻱ ﺍﺷﻜﻲ ﭘﺮﺩﺍﺧﺘﻪVCD ﺍﻳﻦ. ﺑﺤﺚﻫﺎﻱ ﺯﻳﺎﺩﻱ ﺑﺮﺍﻧﮕﻴﺨﺘﻪ ﻭ ﻣﺨﺎﻟﻔﺎﻥ ﻭ ﻣﻮﺍﻓﻘﺎﻥ ﺯﻳﺎﺩﻱ ﺩﺍﺭﺩendoscopic laser ﺟﺮﺍﺣﻲ ﺳﻴﺴﺘﻢ ﻻﻛﺮﻳﻤﺎﻝ ﺑﻪ ﻛﻤﻚ ﺗﻜﻨﻴﻚ ﻧﺴﺒﺘﹰﺎ ﺟﺪﻳﺪ Enucleation Techniques With MEDPOR Orbital Implant MCP Placement in a Vascularized MEDPOR Implant (VCD) (Charles N. S. Soparker, Peter A. D.) 19.8 Natural Movement For Artificial Eyes With MEDPOR Biomaterial Orbit Implants ans the MEDPOR MPC Motility Coupling Post (VCD) (POREX) 20.8 Orbital Floor reconstruction using MEDPOR surgical implants 21.8 ﺁﻥ ﻭ ﻗـﺮﺍﺭﺩﺍﺩﻥ ﭘﺮﻭﺗـﺰdrilling ﻭ ﺩﺭ ﺍﻧﺘﻬﺎﺏ ﺑﻪMEDPOR ﺳﭙﺲ ﺑﻪ ﻃﺮﻳﻘﺔ ﻛﺎﺷﺖ ﺍﻳﻤﭙﻼﻧﺖ،enucleation ﺍﻭﻝ ﺍﺑﺘﺪﺍ ﺑﻪ ﺭﻭﺵﻫﺎﻱCD ٢ . ﺭﺍ ﺩﺭ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺗﺮﻣﻴﻤﻲ ﺍﺭﺑﻴﺖ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﻨﺪMEDPOR ﻓﻮﻕ ﻣﺠﻤﻮﻋﹰﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻛﺎﺷﺖ ﺍﻳﻤﭙﻼﻧﺘﻬﺎﻱVCD
ــــ
٣
. ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩMEDPOR Surgical implant ﺳﻮﻡ ﭼﮕﻮﻧﮕﻲ ﺗﺮﻣﻴﻢ ﻭ ﺑﺎﺯﺳﺎﺯﻱ ﺩﻓﻜﺖﻫﺎﻱ ﻛﻒ ﺍﺭﺑﻴﺖ ﺑﻪ ﻛﻤﻚCD ﻗﺎﺑﻞ ﻗﺒﻮﻝ ﺁﻥ ﺭﺍ ﻧﻤﺎﻳﺶ ﻣﻲﺩﻫﺪ ﺩﺭMotility ﻣﻲﭘﺮﺩﺍﺯﺩ ﻭMCP ﻭimplant ﻣﺮﺑﻮﻃﻪ ﺭﻭﻱ ﻣﺠﻤﻮﻋﺔ 16.2 Facial Plastic & Reconstructive Surgery
(Terence M. Davidson, MD) (VCD I , II) FUNDAMENTALS OF CORMEAL TOPOGRAPHY 22.8 ﻫﺎﻱ ﺍﺣﺘﻤﺎﻟﻲ ﻭ ﻧﻴﺰ ﺳﻴﺮ ﺗﻐﻴﻴﺮﺍﺕ ﺗﻮﭘﻮﮔﺮﺍﻓﻲ ﻭ ﺣﺎﻻﺕ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﺨﺘﻠـﻒ ﻗﺮﻧﻴـﻪartefact ، ﺍﻧﻮﺍﻉ ﻣﻮﺍﺭﺩ ﻃﺒﻴﻌﻲ ﻭ ﻏﻴﺮﻃﺒﻴﻌﻲ، ﻧﺤﻮﺓ ﺗﻔﺴﻴﺮ ﺗﻮﭘﻮﮔﺮﺍﻓﻲ ﻗﺮﻧﻴﻪ، ﻣﻜﺎﻧﻴﺴﻢ ﻭ ﭼﮕﻮﻧﮕﻲ ﻋﻤﻠﻜﺮﺩ ﺩﺳﺘﮕﺎﻩ. ﺟﻤﻌﹰﺎ ﺁﻣﻮﺯﺵ ﻛﺎﻣﻠﻲ ﺍﺯ ﺗﻮﭘﻮﮔﺮﺍﻓﻲ ﻗﺮﻧﻴﻪ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﻨﺪCD ﺍﻳﻦ ﺩﻭ . ﺗﻮﺻﻴﻪ ﻣﻲﺷﻮﺩOSCE ﻋﻼﻭﻩ ﺑﺮ ﻛﺎﺭﺑﺮﺩ ﻛﻠﻴﻨﻴﻜﻲ ﺁﻥ ﺟﻬﺖ ﺷﺮﻛﺖ ﺩﺭ ﺍﻣﺘﺤﺎﻧﺎﺕCD ﺑﻬﺮﻩﮔﻴﺮﻱ ﺍﺯ ﺍﻳﻦ ﺩﻭ.ﺑﻄﻮﺭ ﺟﺎﻣﻊ ﻭ ﻗﺎﺑﻞ ﺍﺳﺘﻔﺎﺩﻩﺍﻱ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ
ــــــ ــــ
23.8 Glaucoma Basic and Clinical Science Course (Section 10)
2003
(Salekan E-Book)
2000
25.8 26.8 27.8 28.8 29.8 30.8 31.8 32.8
Cataract & Refractive Sugery
24.8 Hereditary Retinal Dystrophies (Ulrich Kellner, Markus Ladewing, Christoph Heinrich)
Highlights Highlights Highlights Highlights Highlights Highlights Highlights Highlights
of of of of of of of of
the the the the the the the the
ASCRS ASCRS ASCRS ASCRS ASCRS ASCRS ASCRS ASCRS
1995 1996 1997 1998 1999 2000 2001 2003
Annual Annual Annual Annual Annual Annual Annual Annual
Meeting Meeting Meeting Meeting Meeting Meeting Meeting Meeting
، I.Howard Fine ﺍﺯ ﺑﺮﺟﺴـــﺘﻪﺗـــﺮﻳﻦ ﺍﺳـــﺎﺗﻴﺪ ﻣﺎﻧﻨـــﺪCataract & refractive Surgury ﺩﺭ ﺑـــﺎﺏLecture ﻫــﺎﻱ ﻣﻘﺎﺑـــﻞ ﺣـــﺎﻭﻱ ﺩﻫﻬـــﺎCD ﺁﺧـﺮﻳﻦ، ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻛﻤﻚ ﻓـﻴﻠﻢ ﺟﺮﺍﺣـﻲﻫـﺎﻱ ﺍﻧﺠـﺎﻡﺷـﺪﻩ ﺗﻮﺳـﻂ ﺍﻳـﻦ ﺍﺳـﺘﺎﺩﺍﻥ... ﻭRobert J. Cionni ، Roger F. Steinert، Douglas D. Koch ﻫـﺎﻱCD ﻣﺠﻤﻮﻋـﻪ. ﺭﺍ ﺁﻣـﻮﺯﺵ ﻣـﻲﺩﻫـﺪPRK ﻭLASIK ﻭ ﻧﻴﺰ ﺟﺮﺍﺣﻲ ﻛﺮﺍﺗﻮﺭﻓﺮﺍﻛﺘﻴﻮ ﺷـﺎﻣﻞPhacoemulsification ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺑﺮﻭﺵ . ﻭ ﭼﻪ ﺟﻬﺖ ﺑﻪ ﺭﻭﺯﺩﺭﺁﻭﺭﺩﻥ ﺍﻃﻼﻋﺎﺕ ﻭ ﻣﻬﺎﺭﺕﻫﺎﻱ ﻗﺒﻠﻲ ﻣﻲﺑﺎﺷﺪLASIK ﻭPhaco ﭼﻪ ﺑﻪ ﻣﻨﻈﻮﺭ ﺁﻣﻮﺯﺵ ﺍﻭﻟﻴﺔ،ﻣﺬﻛﻮﺭ ﺑﻪ ﻣﻨﺰﻟﺔ ﻛﺎﺭﮔﺎﻩ ﺁﻣﻮﺯﺷﻲ ﺍﺭﺯﺷﻤﻨﺪﻱ
33.8 Highlights of the XVIIth Congress of the ESCRS VIENNA'99
(EUROPEAN SOCIETY OF CATARACT & REFRACTIVE SURGEONS)
ــــ
34.8 Highlights of the XVIIth Congress of the ESCRS VIENNA'99
(EUROPEAN SOCIETY OF CATARACT & REFRACTIVE SURGEONS)
ــــ
1. Intrastromal Corneal Rings
2. Multifocal IOLs
3. Cataract Technidues
35.8 Illustrated Tutorials Clinical Ophthalmology
4. LASIK: Muopia & Mixed Astigmatism
5. Phakic IOLs
(Jack J Kansski, Anne Bolton)
ــــ
36.8 Implantation of AcryFlex Foldable Lens (Surgery Performed by Dr. Jagdeep M Kakadla) (VCD)
ــــ
37.8 IMPLANTE MEDPOR MANDIBULAR (VCD), (AJL OPHTHALMIC, S.A.)
ــــ
38.8 IMPROVING SUCCESS IN FILTRATION SURGERY American Academy of Ophthalmology (BRADFORD J. SHINGLETON)
ــــ
ﻫﻤﭽﻨﻴﻦ ﺑﻪ ﻣﻌﺮﻓﻲ ﺩﻭ ﺷﻴﻮﺓ ﺟﺪﻳـﺪ ﺩﺭﻣـﺎﻥ ﺟﺮﺍﺣـﻲCD ﺍﻳﻦ. ﻣﻲﺑﺎﺷﺪ ﻭ ﺟﺰﺋﻴﺎﺕ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺭﻭﺵﻫﺎ ﺭﺍ ﺑﺎ ﻛﻤﻚ ﻓﻴﻠﻢﻫﺎﻱ ﺗﻬﻴﻪﺷﺪﻩ ﺍﺯ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﻣﺮﺑﻮﻃﻪ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﺪFilstratioh Surgery ﻳﻚ ﺩﻭﺭﺓ ﻛﺎﻣﻞ ﺁﻣﻮﺯﺷﻲ ﺩﺭ ﻣﻮﺭﺩ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺨﺘﻠﻒCD ﺍﻳﻦ . ﻣﻲﭘﺮﺩﺍﺯﺩViscocanalostomy ﻭDeep Sclerectomy ﺑﻴﻤﺎﺭﺍﻥ ﮔﻠﻮﻛﻮﻣﻲ ﻳﻌﻨﻲ 2000
th 39.8 Incomitant Deviatons (4 edition) a supplement chapter 17 of Pickwell's Binocular Vision Anomalies
ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻋﻼﻭﻩ ﺑﺮ ﺗﻮﺿﻴﺢ ﻭ ﺗﺸﺮﻳﺢ... ﻭBrown's ، Duane's ﻭ ﻧﻴﺰ ﺳﻨﺪﺭﻡﻫﺎﻱrectus ﻭ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
oblique ﻛﻢﻛﺎﺭﻱ ﻭ ﻓﻠﺞ ﻋﻀﻼﺕ، ﻣﻦﺟﻤﻠﻪ ﭘﺮﻛﺎﺭﻱComitant ﻣﺠﻤﻮﻋﻪﺍﻱ ﻛﻢﻧﻈﻴﺮ ﺟﻬﺖ ﻛﻤﻚ ﺑﻪ ﺩﺭﻙ ﺑﻬﺘﺮ ﻭ ﻋﻤﻴﻖﺗﺮ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﺍﻧﺤﺮﺍﻓﺎﺕ ﭼﺸﻤﻲCD
ﺍﻳﻦ . ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢ ﺑﺮﺍﻱ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺁﻧﻬﺎ ﻣﻲﭘﺮﺩﺍﺯﺩCase ﻃﺒﻘﻪﺑﻨﺪﻱ ﻭ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﻫﺮ ﻧﻮﻉ ﺍﻧﺤﺮﺍﻑ ﺑﻪ ﻣﻌﺮﻓﻲ ﭼﻨﺪﻳﻦ، ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ،ﻣﻜﺎﻧﻴﺴﻢ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
42 40.8 Intraocular Inflammation and Uveitis
(Section 9)
2003
(SALEKAN E-BOOK)
41.8 LEO Clinical Update Course on Retina (H. Michael Lambert, Charles. Arr, J. Paul Diechert, Mark W. Johnson, James S. Tiedeman)
ــــ
42.8 LEO Clinical Update Course on Cataract (Stephen S. Lane, MD, Alan S. Candall, MD, Douglas D. Koch, MD, Roger F. Steinert, MD)
ــــ
43.8 LEO Clinical Update Course on Pediatric Ophthalmology and Strabismus THE AMERICAN ACADEMY OF OPHTHALMOLOGY (American Academy of Ophthalmology)
ﻫﻤﺮﺍﻩ ﺑﺎ ﺍﺳﻼﻳﺪ ﻭ ﻓﻴﻢ ﺁﻣﻮﺯﺷـﻲ ﺍﺯ ﺍﺳـﺘﺎﺩﺍﻥ ﻣﻌﺮﻭﻓـﻲ ﻫﻤﭽـﻮﻥLecture ١٣ ( ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺷﺎﻣﻞAAO) ( ﻣﺘﻌﻠﻖ ﺑﻪ ﺁﻛﺎﺩﻣﻲ ﭼﺸﻢﭘﺰﺷﻜﻲ ﺁﻣﺮﻳﻜﺎLifelong education for the ophthalmologist)LEO ﻫﺎﻱ ﺍﺭﺯﺷﻤﻨﺪ ﻭ ﻣﻌﺘﺒﺮCD ﻓﻮﻕ ﺍﺯ ﺳﺮﻱCD . ﺍﻧﺴﺪﺍﺩ ﻣﺠﺮﺍﻱ ﺍﺷﻜﻲ ﻣﺎﺩﺭﺯﺍﺩﻱ ﻭ ﻫﻤﭽﻨﻴﻦ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﺍﻧﺤﺮﺍﻓﺎﺕ ﭼﺸﻤﻲ ﻭ ﺭﻭﺵﻫﺎﻱ ﺩﺭﻣﺎﻥ ﺁﻧﻬﺎ ﺍﺷﺎﺭﻩ ﻛﺮﺩ،ROP ، ﮔﻠﻮﻛﻮﻡ ﻭ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺍﻃﻔﺎﻝ، ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺁﻣﺒﻠﻴﻮﭘﻲCD ﺍﺯ ﺳﺮﻱ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ. ﺍﺳﺖM.X.Repka ﻭK.W.Wright Loeil Prental Endoscopie du Vitre Phaco Chop (VIDEO Media) (Roussat B. Choukroun J, Boscher C, Lebuisson DA, Amar R, Escalas P) 44.8 : ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ - Reconnaissance des structures oculaires - Lors des echographies prenatales - Possibilites et limites actuelles Roussat B, Choukroun J (Paris)
- Anatomie endoscopique normale et Pathologique de la base du vitre anterieur Boscher C, Lebuisson DA, Amar R (paris)
2000
2003
- Le Phaco Chop: Pour que les noyaux durs deviennet un plaisir Escalas P (Nantes)
45.8 MOVIMIENTQ NATURAL PARA EL OJO ARTIFICIAL (VCD), (AJL OPHTHALMIC, S.A.)
ــــ
46.8 MVP VIDEO JOURNAL OF OPHTHALMOLOGY
ــــ
47.8 New England Eye Center Imaging in Glaucoma
ــــ
. ﻭ ﻧﻴﺰ ﺑﻴﻮﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﺪ ﺍﺷﺎﺭﻩ ﻛﺮﺩOCT ،SLO ﺍﺯ ﺟﻤﻠﺔ ﺍﻳﻦ ﺭﻭﺵﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﻲﺗﻮﺍﻥ ﺑﻪ. ﺑﺎ ﺗﻮﺟﻪ ﻭﻳﮋﻩ ﺑﻪ ﻛﺎﺭﺑﺮﺩ ﺁﻧﻬﺎ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﮔﻠﻮﻛﻮﻣﻲ ﻣﻲﭘﺮﺩﺍﺯﺩOptic nerve ﻓﻮﻕ ﺑﻪ ﻣﻌﺮﻓﻲ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺭﺗﻴﻦ ﻭCD 48.8 New England Eye Center Photorefractive Keratectomy (PRK) Course (Helen K. WU, MD, Roger F. Steinert, MD, Michael B. Raizman, MD)
ﺍﺯ ﻣﺸﺨﺼﺎﺕ ﻟﻴﺰﺭ ﺑﻪ ﻛﺎﺭPRK ﻣﻲﺑﺎﺷﺪ ﻛﻠﻴﺔ ﻣﺴﺎﺋﻞ ﻭ ﻣﺒﺎﺣﺚRoger F. Steinert ﻛﻪ ﻋﻤﺪﺗﹰﺎ ﺍﺯ ﺩﻛﺘﺮLecture ١٥ ﺑﻪ ﺷﻤﺎﺭ ﻣﻲﺭﻭﺩ ﻛﻪ ﺍﺯ ﻃﺮﻳﻖPRK ﺗﻬﻴﻪ ﻭ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﺩﺭ ﻭﺍﻗﻊ ﻳﻚ ﻛﺎﺭﮔﺎﻩ ﺁﻣﻮﺯﺷﻲNew England ﻓﻮﻕ ﻛﻪ ﺗﻮﺳﻂ ﻣﺮﻛﺰ ﭼﺸﻢﭘﺰﺷﻜﻲCD . ﺗﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻋﻤﻞ ﻭ ﺑﺎﻻﺧﺮﻩ ﻋﻮﺍﺭﺽ ﺍﺣﺘﻤﺎﻟﻲ ﻭ ﺭﺍﻩﻫﺎﻱ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﺩﺭﻣﺎﻥ ﺁﻧﻬﺎ ﺭﺍ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﺍﺳﺖPatient sclection ﺭﻓﺘﻪ 49.8 OCULAR PATHOLOGY (FIFTH EDITION) (MYRON YANOFF, MD AND BEN S. FINE, MD) (Mosby) (SALEKAN E-BOOK) Basic Principles of Pathology Congenital Anomalies Cornea and Sclera Neural (Sensory) Retina Orbit Ocular Melanotic Tumors
Surgical and Nonsurgical Trauma Nongranulomatous Inflammation: Uveltis, Endophthalmitis, Panophthalmitis, and Sequelae Granulomatous Inflammation. Uvea Vitreous Diabetes Mellitus Retinoblastoma and Pseudoglioma
50.8 Ophthalmic Lenses & Dispensing
ــــ
2002
Skin and Lacrimal Drainage System Conjunctive Lens Optid Nerve Glaucoma
(Mo JALIE)
ــــ
. ﺟﺰﺋﻴﺎﺕ ﻭ ﻧﻜﺎﺕ ﻣﺮﺑﻮﻁ ﺑﻪ ﺗﺠﻮﻳﺰ ﻟﻨﺰ ﻭ ﭘﺮﻳﺴﻢ ﺟﻬﺖ ﺍﺻﻼﺡ ﻋﻴﻮﺏ ﺍﻧﻜﺴﺎﺭﻱ ﻭ ﺍﻧﺤﺮﺍﻓﺎﺕ ﭼﺸﻤﻲ ﺭﺍ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ، ﭘﺮﺩﺍﺧﺘﻪRefraction ﻭOptic ﻓﻮﻕ ﺍﺯ ﻃﺮﻳﻖ ﺗﺼﺎﻭﻳﺮ ﺷﻤﺎﺗﻴﻚ ﺑﻪ ﺁﻣﻮﺯﺵ ﻣﻔﺎﻫﻴﻢ ﭘﺎﻳﻪ ﻭ ﻛﺎﺭﺑﺮﺩﻱCD 51.8 Ophthalmic Surgery: principles and Techniques (BLACKWELL SCIENCE) (SALEKAN E-BOOK)
ــــ
52.8 Ophthalmology A multimedia tutorial for Primary care physicians and medical students (Robert Johnston FRCOpth, Jonathan Boulton MA MRCP FRCOpth)
ــــ
53.8 Orbital Floor Reconstruction Using Medpor Surgical Implant
ــــ
(Joseph M. Serletti, MD, Paul Manson, MD) (VCD)
54.8 PHACO TODAY
(The Latest Development in Phacomulsification and Small Incision Cataract Surgery) (HOWARD FINE, MD) ﺍﺷـﻜﺎﻝ. ﺭﺍ ﺁﻣﻮﺯﺵ ﻣـﻲﺩﻫـﺪphacoemulsfication ﻭIncisions ،Anesthesin ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺪﻳﺪ، ﺍﻳﺮﺍﺩﺷﺪﻩ ﺍﺳﺖ ﺳﻴﺮ ﺟﺮﺍﺣﻲ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺑﻪ ﺭﻭﺵ ﻓﻴﻜﻮ ﺭﺍ ﻣﺮﻭﺭ ﻛﺮﺩﻩI. Howard Fine ﻭ ﺍﺳﻼﻳﺪ ﻛﻪ ﻋﻤﺪﺗﹰﺎ ﺗﻮﺳﻂLecture ١٤ ﺩﺭ ﻗﺎﻟﺐCD ﺍﻳﻦ ﺗﻚ .ﺷﻤﺎﺗﻴﻚ ﻭ ﺗﺼﺎﻭﻳﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺩﺭ ﺁﻥ ﺑﻪ ﺩﺭﻙ ﺑﻬﺘﺮ ﻣﻜﺎﻧﻴﺴﻢﻫﺎ ﻭ ﺗﻜﻨﻴﻜﻬﺎﻱ ﺟﺮﺍﺣﻲ ﺩﺭ ﻓﻴﻜﻮ ﻛﻤﻚ ﺯﻳﺎﺩﻱ ﻣﻲﻧﻤﺎﻳﺪ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
43 55.8 PhcoChop (Mastering Techniques, Optimizing Technology, and Avoiding Complications) David F. Chang CD-1: Hydrodissection Pearls CD-2: Learning Phacochop CD-3: Phacodynamic Principles for PhacoChop, Vertical Chop and Cold Phaco for Brunescent Nuclel CD-4: Strategles for PC Rupture with Nucleus Present, Bimanual Chop for Cataracts with Large Zonular Defects
2004
56.8 Phacoemyulsification Cataract Surgery (Multimedia Oculosurgical Module) (Robert M. Schertzer, David X. Pang, MSE, Luanna R. Bartholomew, PhD) (Mosby) "Scleral tunnel"
ــــ
ﺑـﻪ ﻣﺜﺎﺑـﺔ ﻛﺎﺭﮔـﺎﻩ ﺁﻣﻮﺯﺷـﻲ ﻛـﻢﻧﻈﻴـﺮﻱ ﺩﺭ ﺯﻣﻴﻨـﺔ ﺟﺮﺍﺣـﻲ ﻛﺎﺗﺎﺭﺍﻛـﺖ ﺑـﺮﻭﺵCD ﺍﻳـﻦ. ﻣـﻲﺑﺎﺷـﺪMosby ( ﻣﺘﻌﻠـﻖ ﺑـﻪ ﺍﻧﺘﺸـﺎﺭﺍﺕMultimedia Oulosurgical Module) MOM ﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﻌـﺮﻭﻑ ﻭ ﻣﻌﺘﺒـﺮCD ﻓﻮﻕ ﺍﺯ ﺳﺮﻱCD
. ﻛﻠﻴﻪ ﻣﺮﺍﺣﻞ ﻋﻤﻞ ﺭﺍ ﺑﻪ ﺻﻮﺭﺗﻲ ﻛﺎﻣ ﹰﻼ ﻛﺎﺭﺑﺮﺩﻱ ﻭ ﻗﺎﺑﻞ ﺍﺳﺘﻔﺎﺩﻩ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﺪtext ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ ﻓﻴﻠﻢ ﻭphacoemulsification 57.8 Physiology of the Eye
Anatomy of the Eye 3-D Tour of the Eye Development of Vision Physics of Light & Color Illusions & Your Vision 58.8 Practical Viewing of the Optic Disc (KATHLEEN B. DIGRE, M.D., JAMES J. CORBETT, M.D. Getting Ready-Preparing to View the Opic Disc
What Should I Look for in the Normal Fundus?
Is the Disc Swollen?
Common Eye Conditions 2003
: ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ Is the Disc Pale?
Amaurosis Fugax and Not So Fugax-Vaxcular Disorders of the Eye
White Spots-What Are They?
Hemorrhage
Pigment
What is That in the Retina?
Macula
Practical Viewing in Children
What to Look for in the Aging
Viewing the Disc in Pregnancy
Practical Viewing of the Optic Disc and Retina in the Emergency Department
59.8 PROVISION INTERACTIVE: Clinical Case Studies (AAO) (Thomas A. Weingeist, MD., ph, D)
ــــ
60.8 RECONSTRUCCIÓN DE BASE ORBITAL CON IMPLANTE MEDPOR (VCD), (AJL OPHTHALMIC, S.A.)
ــــ
61.8 Refractive Surgery First interactive Symposium (Marguerite B. McDonald, MD)
ــــ
(American Academy of Ophthalmology)
Roger F. Steinert ،،Jack T. Holladay : ﺍﺯ ﺍﺳﺘﺎﺩﺍﻥ ﺻﺎﺣﺐﻧﺎﻡ ﺍﻳﻦ ﺭﺷﺘﻪ ﻣﻦﺟﻤﻠﻪLecture ﺍﺳﺖ ﻛﻪ ﺩﺭﺑﺮﮔﻴﺮﻧﺪﺓ ﺩﻫﻬﺎManus C. Kraff ﺑﻪ ﺳﺮﭘﺮﺳﺘﻲ ﺩﻛﺘﺮASCRS ﺗﻬﻴﻪ ﺷﺪﻩ ﺍﺯ ﺍﻭﻟﻴﻦ ﺳﻤﭙﻮﺯﻳﻮﻡ ﺟﺮﺍﺣﻲ ﺭﻓﺮﺍﻛﺘﻴﻮ ﺍﻧﺠﻤﻦCD
.PRK ﻭLASIK ،phacoemulsification
ﻓﻮﻕ ﻳﻜﻲ ﺍﺯ ﻣﺠﻤﻮﻋﺔ ﺩﻭCD ﻣﺠﻤﻮﻋﺔ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﺑﻪ ﻫﻤﺮﺍﻩ ﻓﻴﻠﻢ ﻭ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺍﻳﻦ ﻣﺠﻤﻮﻋﻪ ﻣﺮﻭﺭﻱ ﺩﺍﺭﺩ ﺑﺮ ﺍﺧﺮﻳﻦ ﻭ ﺟﺪﻳﺪﺗﺮﻳﻦ ﭘﻴﺸﺮﻓﺖﻫﺎ ﺩﺭ ﺯﻣﻴﻨﺔ ﺟﺮﺍﺣﻲ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺑﻪ ﺭﻭﺵ. ﻣﻲﺑﺎﺷﺪ... ﻭ ــــ
62.8 Refractive Surgery in the new millennium. 63.8 Evolution in LASIK 64.8
LASIK: Customized Ablations and Quality of Vision ﺗﺎ ﺗﻜﻨﻴﻚPatient Selection ﺑﻪ ﺷﻤﺎﺭ ﻣﻲﺭﻭﺩ ﻭ ﺷﺎﻣﻞ ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﺍﺯ ﻣﻌﺎﻳﻨﺎﺕ ﻣﻘﺪﻣﺎﺗﻲLASIK ﺩﻭﺭﺓ ﺟﺎﻣﻊ ﺁﻣﻮﺯﺵ،( ﻣﻲﺑﺎﺷﺪAAO) ( ﻣﺘﻌﻠﻖ ﺑﻪ ﺁﻛﺎﺩﻣﻲ ﭼﺸﻢﭘﺰﺷﻜﻲ ﺁﻣﺮﻳﻜﺎOphthalmology Interactive) ﻫﺎﻱ ﻣﻌﺘﺒﺮCD ﻛﻪ ﺍﺯ ﺳﺮﻱCD ٣ ﻣﺠﻤﻮﻋﺔ ﺍﻳﻦ ﺍﻧﺠﺎﻡ ﺁﻥ ﻭ ﺑﺎﻻﺧﺮﻩ ﻋﻮﺍﺭﺽ ﺍﺣﺘﻤﺎﻟﻲ ﻭ ﻃﺮﻕ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﺩﺭﻣﺎﻥ ﺁﻧﻬﺎ ﺍﺳﺖ
ــــ 2000
65.8 RETINA (Stephen J. Ryan, M.D., Thomas E. Ogden, M.D.,)
ــــ
66.8 RETINA LIBRARY
ــــ
67.8 Retina & Vitneous
ــــ
68.8 Stereoscopic Atlas of Macular Diseases: diagnosis and treatment (Fourth Edition) (J. Donald M. Gass, M.D.) (Mosby)
ــــ
69.8 Subjective Refraction: Cross Cylider Technique
ــــ
70.8 SURGICAL TECHNIQUES WITH MEDPORIMPLANTS AND THE MCP (VCD), (AJL OPHTHALMIC, S.A.)
ــــ
Hereditary retinal dystrophies ﺑـﻪCD ﺩﺍﺷﺘﻦ ﺍﻳﻦ. ﺗﺼﻮﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺘﻲ ﻛﻢﻧﻈﻴﺮ ﻣﻮﺭﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪﺍﻧﺪ١٧٠٠ ﻭ ﺑﺎﻟﻎ ﺑﺮCase ٤٦٧ ﺗﻤﺎﻣﻲ ﺍﻧﻮﺍﻉ ﺩﻳﺴﺘﺮﻭﻓﻲﻫﺎﻱ ﺭﺗﻴﻦ ﺍﺯ ﺷﺎﻳﻊﺗﺮﻳﻦ ﺗﺎ ﻧﺎﺩﺭﺗﺮﻳﻦ ﺁﻧﻬﺎ ﺩﺭ ﻗﺎﻟﺐ. ﻓﻮﻕ ﻳﻜﻲ ﺍﺯ ﺟﺎﻣﻊﺗﺮﻳﻦ ﻣﺮﺍﺟﻊ ﻣﻌﺘﺒﺮ ﺩﺭ ﺑﺎﺏ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﺩﻳﺴﺘﺮﻭﻓﻲﻫﺎﻱ ﺭﺗﻴﻦ ﺍﺳﺖCD .ﻋﻨﻮﺍﻥ ﺭﻓﺮﺍﻧﺴﻲ ﻣﺼﻮﺭ ﺩﺭ ﻣﻮﺍﺟﻪ ﺑﺎ ﻣﻮﺍﺭﺩ ﮔﻮﻧﺎﮔﻮﻥ ﺩﻳﺴﺘﺮﻭﻓﻲﻫﺎﻱ ﺭﺗﻴﻦ ﺩﺭ ﻛﻠﻴﻨﻴﻚ ﺿﺮﻭﺭﻱ ﻣﻲﻧﻤﺎﻳﺪ
71.8 ADVANCED CONCEPTS IN CATARACT SURGERY The American Society of Cataract and Refractive Surgery (ASCRS)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
44 ــــ
)71.8 Clinical Update Course on Glaucoma (Mark B. Sherwood, MD, James D. Brandt, MD, Neil T. Choplin, MD, Joel S. Schuman, MD )72.8 Techniques in CLEAR CORNEAL CATARACT SURGERY OPHTHALMOLOGY Interactive 73.8
ﺗﻤﺎﻣﻲ ﻣﺮﺍﺣﻞ ﺟﺮﺍﺣﻲ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺑﺮﻭﺵ "Clear cornea" Phacoemulsificationﺷﺎﻣﻞ ﺍﻧﺘﺨﺎﺏ ﺑﻴﻤﺎﺭ ،ﺑﻲﺣﺴـﻲ ﺗﺎﭘﻴﻜـﺎﻝ ﻭ ،Prep & drape ، intracameralﺍﻧﺴـﺰﻳﻮﻥ capsulorrhexis ،Clear corneaﻭ ﻇﺮﺍﻳـﻒ ﻣﺮﺑﻮﻃـﻪsetting ،hydrodissection ،
ﻓﻴﻜـﻮ ﺩﺭ ﺍﻧـﻮﺍﻉ ﻣﺨﺘﻠـﻒ
ﻛﺎﺗﺎﺭﺍﻛﺖ ،ﻛﺎﺷﺖ Foldable IOLﻭ ﺑﺎﻻﺧﺮﻩ ﻋﻮﺍﺭﺽ ﺍﺣﺘﻤﺎﻟﻲ ﻭ ﻃﺮﻳﻘﺔ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺁﻧﻬﺎ ﺩﺭ ﻣﺠﻤﻮﻋﺔ CD٣ﻓﻮﻕ ﺍﺯ ﻃﺮﻳﻖ ،Lectureﺗﺼﺎﻭﻳﺮ ﺷﻤﺎﺗﻴﻚ ﻭ ﻓﻴﻠﻢ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺍﻧﺠﺎﻡﺷﺪﻩ ﺗﻮﺳﻂ ﺍﺳﺘﺎﺩﺍﻥ ﺑﻨﺎﻡ ﺍﻳﻦ ﺭﺷﺘﻪ ﺑﻄﻮﺭ ﻛﺎﻣﻞ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. )74.8 TEXBOOK OF OPHTHALMOLOGY (KENNETH W.WRIGHT )REVIEW QUESTIONS IN OPHTHALMOLOGY (KENNETHC. CHERN.KENNETH W. WRIGHT
ــــ
ــــ
ﺩﺭ ﺩﺳﺘﺮﺱ ﺑﻮﺩﻥ ﻛﺘﺐ ﻣﺮﺟﻊ ﺑﺼﻮﺭﺕ ﻟﻮﺡ ﻓﺸﺮﺩﻩ ) (CDﺍﺭﺯﺵ ﺁﻧﻬﺎ ﺭﺍ ﺩﻭ ﭼﻨﺪﺍﻥ ﻣﻲﻛﻨﺪ ﺯﻳﺮﺍ ﻋﻼﻭﻩ ﺑﺮ ﺍﺷﻐﺎﻝ ﻓﻀﺎﻱ ﻛﻤﺘﺮ ﻭ ﺣﻤﻞ ﻭ ﻧﻘﻞ ﺭﺍﺣﺘﺘﺮ ،ﺍﻣﻜﺎﻥ ﺟﺴﺘﺠﻮﻱ ﺳﺮﻳﻊ ﻣﻄﻠﺐ ﻣﻮﺭﺩ ﻧﻈﺮ ﻭ ﺍﺣﻴﺎﻧﹰﺎ ﺗﻬﻴﺔ Printﺍﺯ ﺁﻥ ﻧﻴﺰ ﻓﺮﺍﻫﻢ ﺍﺳﺖ .ﺍﺯ ﺳﻮﻱ ﺩﻳﮕﺮ ،ﺑﻬﺎﻱ CDﺣﺘﻲ ﺑﺎ ﻼ ﺑﺼﻮﺭﺕ CDﻣﻌﺮﻓﻲ ﻣﻲﮔﺮﺩﺩ ،ﺍﻧﺤﺼﺎﺭﹰﺍ ﺗﻮﺳﻂ ﺷﺮﻛﺖ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺑﺎ ﺩﻗﺘﻲ ﻭﺳﻮﺍﺱ ﮔﻮﻧﻪ ﺍﺯ ﺭﻭﻱ ﺁﺧﺮﻳﻦ ﺗﺠﺪﻳﺪﻧﻈﺮ ﻛﺘـﺐ textﺗﻬﻴـﻪ ﺷـﺪﻩ ﻛﺘﺐ textﻣﻌﺎﺩﻝ ﺁﻥ ﻛﻪ ﺩﺭ ﺩﺍﺧﻞ ﻛﺸﻮﺭ ﺍﹸﻓﺴﺖ ﺷﺪﻩ ﻗﺎﺑﻞ ﻣﻘﺎﻳﺴﻪ ﻧﻤﻲﺑﺎﺷﺪ .ﺩﻭ ﻧﻤﻮﻧﻪ ﺍﺯ ﻛﺘﺐ ﻣﺮﺟﻌﻲ ﻛﻪ ﺫﻳ ﹰ ﺍﺳﺖ ،ﺑﻄﻮﺭﻳﻜﻪ ﺗﺼﺎﻭﻳﺮ ﻭ ﻋﻜﺲﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ ﺁﻧﻬﺎ ﺩﺍﺭﺍﻱ ﻗﺎﺑﻠﻴﺖ ﺑﺰﺭﮔﻨﻤﺎﺋﻲ ﺑﻮﺩﻩ ،ﺍﺯ ﻧﻈﺮ ﻛﻴﻔﻲ ﺑﻬﻴﭻ ﻋﻨﻮﺍﻥ ﺑﺎ ﻛﺘﺐ ﺍﻓﺴﺖ ﻣﻮﺟﻮﺩ ﺩﺭ ﺩﺍﺧﻞ ﻛﺸﻮﺭ ﻗﺎﺑﻞ ﻣﻘﺎﻳﺴﻪ ﻧﻴﺴﺖ. )75.8 THE FAILING GLAUCOMA FILTER: EARLY IDENTIFICATION & TREATMENT (Bradford J. Shingleton, MD CDﻓﻮﻕ ﺗﻤﺎﻣﹰﺎ ﺑﻪ ﻣﻘﻮﻟﺔ Failing Filtration Surgeryﭘﺮﺩﺍﺧﺘﻪ ﻭ ﻋﻠﻞ ،ﻋﻮﺍﻣﻞ ﻣﺴﺘﻌﺪﻛﻨﻨﺪﻩ ،ﺭﺍﻩﻫﺎﻱ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﺑﺎﻻﺧﺮﻩ ﺩﺭﻣﺎﻥﻫﺎﻱ ﻃﺒﻲ ﻭ ﺟﺮﺍﺣﻲ ﺁﻥ ﺭﺍ ﺍﺯ ﻃﺮﻳﻖ ﭼﻨﺪﻳﻦ Lectureﻭ ﻓﻴﻠﻢﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺮﺑﻮﻃﻪ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ .ﺩﺭ ﺍﻳﻦ CDﺗﻜﻨﻴﻚﻫﺎﻳﻲ ﻣﺎﻧﻨﺪ Choroidal tapﻭ ﻼ ﺿﺮﻭﺭﻱ ﻣﻲﺑﺎﺷﺪ ﺑﺨﻮﺑﻲ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. bleb revisionﻛﻪ ﺩﺍﻧﺴﺘﻦ ﺁﻧﻬﺎ ﺑﺮﺍﻱ ﻫﺮ ﺟﺮﺍﺡ ﮔﻠﻮﻛﻮﻣﻲ ﻛﺎﻣ ﹰ
ــــ
)(MICHAEL K. SMOLEK, PH. D.
76.8 The Multimedia Atlas of Videokeratography Basics of Map Interpretation
ــــ
)77.8 The Retina ATLAS ( Yannuzzi,Green) (Mosby
)(S.LBosniak
ــــ
)78.8 THE VIDEO ATLAS OF COSMETIC BLEPHAROPLASTY (8 CDs
ﻣﺠﻤﻮﻋﺔ VCD ٨ﻓﻮﻕ ﻳﻚ ﺩﻭﺭﺓ ﻛﺎﻣﻞ ﺁﻣﻮﺯﺵ ﺟﺮﺍﺣﻲ ﭘﻠﻚ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﻮﺳﻂ ﺍﺳﺘﺎﺩ ﺑﺮﺟﺴﺘﻪ S.LBosniakﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺷﺎﻣﻞ ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﺍﺯ ﺁﻧﺎﺗﻮﻣﻲ ﭘﻠﻚ ﻭ ﺭﻭﺵﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﻲﺣﺴﻲ ﺗﺎ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺩﺭ ﺍﺻـﻼﺡ ﻭ ﺗـﺮﻣﻴﻢ ﻛﻠﻴـﺔ ﻣﺴﺎﺋﻞ ﻭ ﻣﺸﻜﻼﺕ ﭘﻠﻜﻲ ﻣﻦﺟﻤﻠﻪ ،ﺁﻧﺘﺮﻭﭘﻴﻮﻥ ،ﺍﻛﺘﺮﻭﭘﻴﻮﻥ ،ﭘﺘﻮﺯ ،ﺩﺭﻣﺎﺗﻮﺷﺎﻻﺯﻳﺲ ﻭ ...ﻣﻲﺑﺎﺷﺪ .ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻣﺠﻤﻮﻋﻪ ﺭﺍ ﺑﺎﻳﺪ ﺑﻪ ﻣﻨﺰﻟﺔ ﮔﺬﺭﺍﻧﺪﻥ ﻳﻚ ﺩﻭﺭﻩ ﻛﺎﺭﮔﺎﻩ ﺁﻣﻮﺯﺷﻲ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﺩﺍﻧﺴﺖ. ــــ
)Vitreoretinal Course Bascom Palmer Eye Institute's (William E. Smiddy, Philip Rosenfeld, Patrick E. Rubsamen, Janet L.
79.8
CDﻓﻮﻕ ﺍﺯ ﺳﺮﻱ CDﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ (Ophthalmology interactive) OIﻣﺘﻌﻠﻖ ﺑﻪ ﺁﻛﺎﺩﻣﻲ ﭼﺸﻢﭘﺰﺷﻜﻲ ﺁﻣﺮﻳﻜﺎ ) ،(AAOﺣﺎﻭﻱ Lecture ١٦ﺑﻪ ﻫﻤﺮﺍﻩ ﺍﺳﻼﻳﺪ ﻭ ﻓﻴﻢ ﺍﺯ ﺍﺳﺘﺎﺩﺍﻥ ﺑﺮﺟﺴﺘﻪﺍﻱ ﭼﻮﻥ W.E.Smiddyﻭ H.W.Flynnﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻣﺮﻭﺭ ﻭ ﻣﻌﺮﻓﻲ ﺁﺧﺮﻳﻦ ﺩﺳﺘﺎﻭﺭﺩﻫﺎ ﺩﺭ ﻣﻮﺭﺩ ﻣﺒﺎﺣﺚ ﻣﺨﺘﻠﻒ ﺟﺮﺍﺣﻲ ﺳﮕﻤﺎﻥ ﺧﻠﻔﻲ ﭼﺸﻢ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺍﺯ ﺟﻤﻠﻪ ﻣﻮﺿﻮﻋﺎﺕ ﻣﻮﺭﺩ ﺑﺤﺚ ﺩﺭ ﺍﻳﻦ CDﻣﻲﺗﻮﺍﻥ Macular hole ،Giant retinal tear،Dislocated IOLs ،AMD , ROP ،Endophthalmitis :ﻭ ...ﺭﺍ ﻧﺎﻡ ﺑﺮﺩ. ــــ
)80.8 VJO Ophthalmology (I, I , III ,) (VCD) (Charles, H. Cozean, James S. Lewis, Richard J. Mackool
-٩ﻣﻐﺰ ﻭ ﺍﻋﺼﺎﺏ
ﻋﻨﻮﺍﻥ CD
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ 2004
)5 Minute Neurology Consult (SALEKAN E-BOOK) (D. Joanne Lynn
1.9
ﺍﻳﻦ CDﻛﻪ ﺑﺮﺍﻱ ﺍﺳﺘﻔﺎﺩﻩ ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎ ،ﺭﺯﻳﺪﻧﺖﻫﺎ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺩﺍﺧﻠﻲ ﺍﺳﺖ .ﺑﻪ ﻋﻨﻮﺍﻥ ﺭﻓﺮﺍﻧﺲ ﺳﺮﻳﻌﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ ﺳﺮﻱ 5-Minuteﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﻓﺮﻣﺖ ﺩﻭﺻﻔﺤﻪﺍﻱ ﺍﺳـﺘﻔﺎﺩﻩ ﺑﻼﻓﺎﺻـﻠﻪ ﻭ ﺳـﺮﻳﻊ ﺍﺯ ﺁﻥ ﺭﺍ ﺭﺍﺣـﺖ ﻛﺮﺩﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ٢٠٠ﺑﻴﻤﺎﺭﻱ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻛﺎﺭ ﺑﺎﻟﻴﻨﻲ ﺑﻪ ﻃﻮﺭ ﺷﺎﻳﻌﻲ ﺑﺎ ﺁﻧﻬﺎ ﻣﻮﺍﺟﻪ ﻣﻲﺷﻮﻳﻢ .ﻫﺮ ﻣﺒﺤﺚ ﺷﺎﻣﻞ Follow up ، Medications ، Management ، Diagnosis ،Basicsﻭ MiscellaneousﻣـﻲﺑﺎﺷـﺪCD . ﺷﺎﻣﻞ ﻓﺼﻮﻝ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ. -Short Topics 2003
-Neurologic Symptoms and Signs -Neurologic Diagnostic Tests -Neurologic Diseases and Disorders th )55 Annual Meeting March 29-Aprill 5, American Academy of Neurology (HAWAII
2.9
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺷﺎﻣﻞ Full textﺗﻤﺎﻡ ﻣﻘﺎﻻﺕ ﻭ Presentationﻫﺎﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺩﺭ ﻛﻨﮕﺮﻩ ﺁﻛﺎﺩﻣﻲ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺍﻣﺮﻳﻜﺎ ﺩﺭ ﺁﻭﺭﻳﻞ 2003ﺩﺭ ﻫﺎﻭﺍﻳﻲ ﻣﻲﺑﺎﺷﺪ. 2000 ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
)(Barlow/Durand's, Durand/Barlow's, Trull/Pharcs
3.9 Abnormal Psychology LIVE and interactive tutorial
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
45 2004
4.9 American Academy of Neurology 2004 Syllabi
ﺍﻳﻦ CDﻛﻪ ﺣﺎﺻﻞ ﻣﻘﺎﻻﺕ ﺁﺧﺮﻳﻦ ﻛﻨﮕﺮﻩ ﺁﻛﺎﺩﻣﻲ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺍﻣﺮﻳﻜﺎ ﺩﺭ ﺳﺎﻝ ٢٠٠٤ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ١٦٠ﻣﻮﺿﻮﻉ ﺩﺭ ﺯﻣﻴﻨﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻃﺒﺎﺑﺖ ﺑﺎﻟﻴﻨﻲ ﻧﻮﺭﻭﻟﻮﮊﻱ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻫﺮ ﻣﻮﺿﻮﻉ ﺷﺎﻣﻞ ﭼﻨﺪ ﻣﻘﺎﻟﻪ ﻭ ﻣﺒﺤﺚ ﻣﻲﮔﺮﺩﺩ .ﺑﻌﻀﻲ ﺍﺯ ﻣﻘﺎﻻﺕ ﺍﺭﺍﺋﻪﺷﺪﻩ ﻫﻤﺮﺍﻩ ﺑﺎ ﻓﺎﻳﻞﻫﺎ ﻭ ﺍﺳﻼﻳﺪﻫﺎﻱ Presentationﻧﻴﺰ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻛﺎﺭﺑﺮﺩ ﺁﻥ ﺭﺍ ﺑﺮﺍﻱ ﺗﺪﺭﻳﺲ ﻭ ﺍﺭﺍﺋﺔ ﻣﺠﺪﺩ ﺩﻭﭼﻨﺪﺍﻥ ﻣﻲﺳﺎﺯﺩ .ﻓﺎﻳﻞﻫﺎ ﺍﺯ ﻃﺮﻳﻖ Javaﻭ ﺑﻪ ﺻﻮﺭﺕ Autorunﺍﺟﺮﺍ ﻣﻲﮔﺮﺩﻧﺪ ﻗﺎﺑﻠﻴﺖ Searchﺑﺮ ﺍﺳﺎﺱ ﻣﻮﺿﻮﻉ ﻭ ﻧﻮﻳﺴﻨﺪﻩ ﺍﺯ ﻣﺰﺍﻳﺎﻱ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺍﺳﺖ. ﻣﺒﺎﺣﺚ ﻣﻬﻢ ﻣﻄﺮﺡﺷﺪﻩ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: Stroke Demyelinating dyorden
ــــ
Botutinum Toxin Injection Movement disorders
Balance and gaif disorder Clinical EMG
)Advanced Therapy of HEADACHE CONQUERING HEADACHE (SECOND REVIED EDITION) An Illustrated Guide to Understanding The Treatment and Control of Headache (Alan M. Rapoport, Fred D. Sheftell
(١ (٢ (٣
)6.9 Atlas of Functional Neuroanatomy (Dr. Walter J. Hendelman
)(Phoenix, Arizona
2003
7.9 Boehringer Ingelheim Satellite Symposium Interanational Stroke Conference
)(An interactive digital atlas designed to assist in learning human neuroanatomy
1996 ــــ
5.9
ﺍﻳﻦ CDﺷﺎﻣﻞ ﺳﻪ ﻗﺴﻤﺖ ﻣﻲﺑﺎﺷﺪ. ﻣﺘﻦ ﻓﺎﻳﻞ PDFﻛﺘﺎﺏ ) Advanced Therapy of headache (1999ﺗﻮﺳﻂ ) Alan rappaportﺍﺳﺘﺎﺩ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ) Fred sheftell ( Yaleﺍﺳﺘﺎﺩ ﺑﺨﺶ ﺭﻭﺍﻧﭙﺰﺷﻜﻲ ﺩﺍﻧﺸـﮕﺎﻩ ( Newyorkﻧﻮﺷـﺘﻪ ﺷـﺪﻩ ﺍﺳـﺖ .ﺷـﺎﻣﻞ 48ﻣﺒﺤـﺚ ﭘﺎﻳـﻪ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﺍﺻﻮﻝ ﺗﺌﻮﺭﻱ ﻭ ﻋﻤﻠﻲ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﺳﺮﺩﺭﺩ ﺍﺯ ﺟﻤﻠﻪ ﺗﺸﺨﻴﺺﻫﺎﻱ ﭘﻴﭽﻴﺪﻩ ،ﺩﺭﻣﺎﻥ ﺷﺎﻣﻞ ﺩﺭﻣﺎﻧﻬﺎﻱ ﺟﺪﻳﺪ ﻭ ﻧﻴﺰ managementﺑﻴﻤﺎﺭﺍﻥ ﻣﻲﺑﺎﺷﺪ. ﻣﺘﻦ ﻓﺎﻳﻞ PDFﻛﺘﺎﺏ Conquering headache 1998 2nd editionﺍﺯ ﻧﻮﻳﺴﻨﺪﮔﺎﻥ ﻓﻮﻕ ﻛﻪ ﺍﻃﻼﻋﺎﺗﻲ ﺩﺭ ﺁﻥ ﺟﻬﺖ ﻣﻘﺎﺑﻠﻪ ﺑﺎ ﺳﺮﺩﺭﺩ ﻭ ﺑﻬﺒﻮﺩ ﻧﺤﻮﺓ ﺯﻧﺪﮔﻲ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻫﻤﺮﺍﻩ ﺑﺎ ﺁﺧﺮﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺭﺍﺟﻊ ﺑﻪ ﺗﻘﺴﻴﻢ ﺑﻨﺪﻱ ﺳﺮﺩﺭﺩﻫﺎ -ﺩﺭﻣﺎﻧﻬـﺎﻱ ﺩﺍﺭﻭﻳـﻲ ﺗﺌﻮﺭﻱﻫﺎﻱ ﺟﺪﻳﺪ -ﺍﺻﻮﻝ ﺗﻐﺬﻳﻪﺍﻱ ﻭﺭﺯﺷﻲ -ﺧﻮﺍﺏ -ﺭﻭﺵﻫﺎﻱ ﻏﻴﺮ ﺩﺍﺭﻭﻳﻲ ﺩﻳﮕﺮ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ.ﻣﺘﻦ PDFﺟﻤﻠﺔ Seminars in Headache mamagementﻛﻪ ﺗﻮﺳﻂ James W.Lanceﺍﺩﺍﺭﻩ ﻣﻲﮔﺮﺩﺩ ﻭ ﺷﺎﻣﻞ ﺳﻪ ﺳﺎﻝ ﺍﺯ ﺳﺎﻝ 1996- 1998ﻣﻲﺑﺎﺷﺪ .ﻣﺒﺎﺣﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ :ﺗﺸﺨﻴﺺ -ﺩﺭﻣﺎﻥ ﺣﺎﺩ ﻣﻴﮕﺮﻥ ﻭ ﺩﺭﻣﺎﻥ ﭘﺮﻭﻓﻴﻼﻛﺘﻴﻚ ﻣﺒﺎﺣﺚ ﺳﺮﺩﺭﺩﻫﺎﻱ ﻛﻼﺳﺘﺮ – Post traumatic -ﺍﻳﺴﻜﻤﻲ ﻣﻐﺰﻱ ﻧﺎﺷﻲ ﺍﺯ ﻣﻴﮕﺮﻥ -ﻣﻴﮕﺮﻥ ﻭ ﻫﻮﺭﻣﻮﻧﻬﺎﻱ ﺟﻨﺴﻲ.
2000 ــــ
Bedside Neurology Clinical EEG
Seizure and antiepilep drugs Child Neurology
)(Version 1.52
Medical Multimedia Systems Presents
TM
!8.9 Brainiac
)Clinical Neurology (G David Perkin Fred H Hochberg Douglas C Miller
9.9
)10.9 Comprehensive Textbook of PSYCHIATRY (Seventh Edition CD-ROM) (Benjamin J. Sadock, MD – Virginia A. Sadock, MD) ( LIPPINCOTT WILLIAMS & WILKINS
ﻼ ﺍﺯ ﻭﺿﻮﺡ ﺑﺎﻻﻳﻲ ﺑﺮﺧﻮﺭﺩﺍﺭﻧﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻳﻚ ﻛﺘﺎﺏ ﺟﺎﻣﻊ ﻭ ﻣﺮﺟﻊ ﺩﺭ ﺯﻣﻴﻨﺔ ﺭﻭﺍﻥ ﭘﺰﺷﻜﻲ ﺍﺳـﺖ .ﺗﺼـﺎﻭﻳﺮ ﻣﺘﻌـﺪﺩ ﺁﻣﻮﺯﺷـﻲ،MRI ، ﺍﻳﻦ CDﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻚ ﻣﺸﺘﻤﻞ ﺑﺮ ٥٥ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ .ﻫﻤﭽﻨﻴﻦ ﺣﺎﻭﻱ ٦٥٠ﺗﺼﻮﻳﺮ ﺁﻣﻮﺯﺷﻲ ﻭ ﻧﻴﺰ ﺟﺪﺍﻭﻝ ﻣﺘﻌﺪﺩﻱ ﺍﺳﺖ ﻛﻪ ﻛﺎﻣ ﹰ ﻃﺮﺡﻭﺍﺭﻩﻫﺎ ﻭ ﺗﺼﺎﻭﻳﺮ ﺑﺮﺧﻲ ﺍﺯ ﺩﺍﻧﺸﻤﻨﺪﺍﻥ ﺍﻳﻦ ﺭﺷﺘﻪ ،ﺍﺭﺍﺋﻪ ﻛﺎﻣﻞ ﻣﻨﺎﺑﻊ ﺩﺭ ﭘﺎﻳﺎﻥ ﻫﺮ ﻓﺼﻞ ،ﻓﻬﺮﺳﺖ ﻛﺎﻣﻞ ﻣﻮﺿﻮﻋﺎﺕ ،ﺍﺭﺍﺋﻪ ﺩﺍﺭﻭﻫﺎﻱ ﺭﻭﺍﻧﭙﺰﺷﻜﻲ ﻭ ﺍﺷﻜﺎﻝ ﺩﺍﺭﻭﺋﻲ ﻣﺨﺘﻠﻒ ﺑﻪ ﻫﻤﺮﺍﻩ ﺗﺼﻮﻳﺮ ﺁﻧﻬﺎ ﺍﺯ ﻭﻳﮋﮔﻲﻫﺎﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﻲﺑﺎﺷﺪ .ﺑﺮﺧﻲ ﺍﺯ ﻓﺼﻮﻝ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ. -١ﺭﻭﺍﻧﭙﺰﺷﻜﻲ ﺍﻋﺼﺎﺏ ﻭ ﺭﻓﺘﺎﺭ -٢ﻋﻠﻮﻡ ﺍﻋﺼﺎﺏ -٣ﺗﺌﻮﺭﻳﻬﺎﻱ ﺷﺨﺼﻴﺖ ﻭ ﺁﺳﻴﺐﺷﻨﺎﺳﻲ ﺁﻧﻬﺎ -٤ﺭﻭﺷﻬﺎﻱ ﺗﺸﺨﻴﺺ ﺩﺭ ﺭﻭﺍﻥﭘﺰﺷﻜﻲ -٥ﻃﺒﻘﻪﺑﻨﺪﻱ ﺑﻴﻤﺎﺭﻫﺎﻱ ﻣﻐﺰﻱ -٦ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺷﻨﺎﺧﺘﻲ … -٧ ((Delirium Dementin,ﺍﺳﻜﻴﺰﻭﻓﺮﻧﻲ -٨ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺿﻄﺮﺍﺏ -٩ﺑﻴﻤﺎﺭﻳﻬﺎﻱ -١٠ Moodﺑﻴﻤﺎﺭﻫﺎﻱ ﺭﻭﺍﻧﻲ ﺧﻮﺍﺏ -١١ﺑﻴﻤﺎﺭﻳﻬﺎﻱ -١٢ Dissociativeﺧﻮﺩﻛﺸﻲﻫﺎ -١٣ﺭﻭﺍﻥ ﭘﺰﺷﻜﻲ ﺍﻃﻔﺎﻝ -١٤ﺑﻴﻤﺎﺭﻫﺎﻱ ﻳﺎﺩﮔﻴﺮﻱ -١٥ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺭﺗﺒﺎﻃﻲ -١٦ﺑﻴﻤﺎﺭﻱﻫﺎﻱ Ticﻋﺼﺒﻲ -١٧ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺿﻄﺮﺍﺏ ﺩﺭ ﻛﻮﺩﻛﺎﻥ -١٩ Adoption -١٨ﺭﻭﺍﻧﭙﺰﺷﻜﻲ )ﮔﺬﺷﺘﻪ ﺩﺭ ﺁﻳﻨﺪﻩ( ﻭ ...ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﻮﺍﻧﺎﻳﻲ ﺟﺴﺘﺠﻮ ﺑﺮ ﺍﺳﺎﺱ ﻭﺍﮊﻩﻫﺎﻱ ﺗﺨﺼﺼﻲ ﻭ ﺍﺳﺎﻣﻲ ﺩﺍﺭﻭﻫﺎ ﺭﺍ ﺩﺍﺭﺍﺳﺖ .ﺟﺴﺘﺠﻮﻱ ﺗﺼﺎﻭﻳﺮ ،ﺗﻮﺍﻧﺎﻳﻲ ﭼﺎﭖ ﻣﺘﻦ ﻭ ﺗﺼﺎﻭﻳﺮ ،ﺍﺿﺎﻓﻪ ﻧﻤﻮﺩﻥ ﻳﺎﺩﺩﺍﺷﺖﻫﺎﻱ ﺷﺨﺼﻲ ﺍﺯ ﻭﻳﮋﮔﻴﻬﺎﻱ ﺩﻳﮕﺮ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺳﺖ. 2001
)11.9 Computational Neuroscience Realistic Modeling for Experimentalists (Erik De Schutter Introduction to Equation Solving and Parameter Fitting Modeling Networks of Signalling Pathways Modeling Local and Global Calcium Signals Using Reaction-Diffusion Equations Monte Carlo Methods for Simulating Realistic Synaptic Microphysiology Using Mcell Which Formalism to Use for Modeling voltage-Dependent Conductances? Accuate Reconstruction of Neunal Morphology Modeling Dendritic Geometry and the Development of Nerve Connections Passive Cable Modeling-A practical Introduction Modeling Simple and Complex Active Neurons Realistic Modeling of Small Neuronal Circuits Modeling of Interactions Between Neural Networks and Musculoskeletal System
2001
)12.9 CONTEMPORARY NEUROSURGERY A BIWEEKLY PUBLICATION FOR CLINICAL NEUROSURGICAL CONTINUING MEDICAL EDUCATION (Ali F. Krisht, MD
ــــ
)(Micheal K. Rees, MD, MPH, Robert Birnbaum, MD, PHD, James A.D. Otis
13.9 Core Curriculum in Primary Care Psychiatry and Pain Management Section
ﺍﻳﻦ CDﺍﺯ ﺳﺮﻱ CCCﻋﻤﺪﺗﺎﹰ ﺟﻬﺖ ﭘﺎﺳﺨﮕﻮﻳﻲ ﺑﻪ ﻧﻴﺎﺯ ﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﭘﺰﺷﻜﺎﻥ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻋﻤﺪﺓ ﻓﻌﺎﻟﻴﺘﺸﺎﻥ ﺩﺭ ﺯﻣﻴﻨﻪ ﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻭ ﺑﻴﻤﺎﺭﺍﻥ ﺳﺮﭘﺎﻳﻲ ﺍﺳﺖ ﺑﻪ ﻃﻮﺭﻳﻜﻪ ﺗﻤﺎﻡ ﻣﺒﺎﺣﺚ ﻭ ﻣﻔﺎﻫﻴﻢ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺑﺮﺍﻱ ﺍﺟﺮﺍﻱ ﻋﻤﻠﻲ ﺩﺭ ﻛﻠﻴﻨﻴﻚ ﺟﻬـﺖﺩﻫـﻲ ﺷﺪﻩﺍﻧﺪ ﻭ ﺁﺧﺮﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺑﺎﻟﻴﻨﻲ ﺭﺍ ﺑﺎ ﺷﻌﺎﺭ" "Current best Standard of therapyﺍﺭﺍﺋﻪ ﻣﻲﻧﻤﺎﻳﻨﺪ .ﺷﺎﻣﻞ ﺩﻭ ﻣﺒﺤﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
46 : ﺍﺭﺍﺋﻪ ﻣﻲﮔﺮﺩﺩ ﻭ ﺷﺎﻣﻞ ﺳﺮ ﻓﺼﻞﻫﺎﻱ ﺯﻳﺮ ﺍﺳﺖHarvard Medical School ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩRobert Birnbaum ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ: Psychopharmacology for primay Care Medicine -١ Anxiety disorder- Panic disorder- Social phobia- Specific phobia- Obcessive & Compulsire disorder- PTSD- Generalized Anxiety disorder- Depression-Dysthymia
. ﺟﺮﺍﺣﻲ( ﻣﻮﺭﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ- ﺭﻭﺍﻧﺪﺭﻣﺎﻧﻲ- ﻣﺨﺪﺭ- ﺍﻧﻮﺍﻉ ﺩﺭﻣﺎﻧﻬﺎﻱ ﺩﺭﺩ )ﺩﺍﺭﻭﻳﻲ- ﺗﺸﺨﻴﺺ ﺩﺳﺘﻪﺑﻨﺪﻱ- ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﻭ ﺍﺭﺯﻳﺎﺑﻲBoston ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩJames A.D. otis ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ: Pain Management -٢ . ﻗﺎﺑﻠﻴﺖ ﺍﻧﺘﺨﺎﺏ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺩﻟﺨﻮﺍﻩ ﺟﻬﺖ ﺍﺭﺍﺋﻪ ﻭ ﻛﻨﻔﺮﺍﻧﺲ ﺟﺪﺍﮔﺎﻧﻪ ﻧﻴﺰ ﻣﻲﺑﺎﺷﺪCD ﻧﺮﻡﺍﻓﺰﺍﺭ ﺍﻳﻦ. ﺗﻌﺪﺍﺩﻱ ﺳﻮﺍﻝ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﺒﺤﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﻣﻄﺮﺡ ﻭ ﭘﺎﺳﺦ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﻲﺑﺎﺷﺪprint ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﺩﺭ ﻓﺎﻳﻞ ﺟﺪﺍﮔﺎﻧﻪﺍﻱ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﻗﺎﺑﻞ 14.9 Corel Medical Series Epilepsy (Alan Guberman MD, FRCP (C)) (Professor of Neurology University of Ottawa
ــــ
ﻛﺎﻣـﻞQuiz ﺍﻧﻴﻤﻴﺸﻦ ﻭ ﻗﻄﻌـﺎﺕ ﻭﻳـﺪﺋﻮﻳﻲ ﻭ- ﺳﺮ ﻓﺼﻞﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﺁﻧﺎﻟﻴﺰ ﮔﺮﺩﺩ ﻭ ﺑﺎ ﺗﺼﺎﻭﻳﺮ: ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺳﻌﻲ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻳﻜﺴﺮﻱ ﺍﺯ ﻣﺸﻜﻼﺕ ﺷﺎﻳﻊ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ ﺻﺮﻉ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﻮﺩ. ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩ ﺍﺗﺎﻭﺍ ﻃﺮﺍﺣﻲ ﻭ ﺍﺟﺮﺍ ﺷﺪﻩ ﺍﺳﺖAllan Guberman ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﺷﺎﻣﻞ ﺳﺮ ﻓﺼﻞﻫﺎﻱ ﺯﻳﺮ ﺍﺳﺖ. ﺑﻮﺩﻩ ﺍﺳﺖproblem based interactive ﺑﻪ ﺻﻮﺭﺕreview ﺳﻌﻲ ﺩﺭ ﺁﻣﻮﺯﺵ ﻭ. ﺗﻤﺎﻣﻲ ﻣﻄﺎﻟﺐ ﺍﺯ ﻧﻘﺎﻁ ﻗﻮﺕ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩPrint ﺍﻃﻼﻋﺎﺕ ﺑﻴﻤﺎﺭﺍﻥ ﻭ ﺗﻮﺍﻧﺎﻳﻲ ﺑﺎﺯﮔﺸﺖ ﻣﻄﺎﻟﺐ ﻭ ﻗﺎﺑﻠﻴﺖ- ﻗﻮﻱSearch .ﮔﺮﺩﺩ Definitions
Topic index
15.9 CRANIAL NERVES
Epilepsy Notes
Patient & Family information
Epilepsy Case Study
Video
Reference list
Epilepsy Facts
What is Epilepsy
Learning Objectives
2002
in health and disease (Second Edition)
ﺷﺎﻣﻞ ﺗﺼﺎﻭﻳﺮ ﻋﺎﻟﻲ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻭ ﻃﺮﺍﺣﻲﻫﺎﻱ ﺭﻧﮕﻲ ﺍﺯ ﻣﺴﻴﺮﻫﺎﻱ ﺍﻋﺼﺎﺏ ﻛﺮﺍﻧﻴﺎﻝ ﺍﺯ ﺍﻃﺮﺍﻑ ﺑﻪ ﻣﻐﺰ ﻭ ﺍﺯ ﻣﻐﺰ ﺑﻪ. ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﻮﺳﻂ ﺟﻤﻌﻲ ﺍﺯ ﺍﺳﺎﺗﻴﺪ ﺟﺮﺍﺡ ﻭ ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖ ﺩﺍﻧﺸﮕﺎﻩﻫﺎﻱ ﻛﺎﻧﺎﺩﺍ ﻧﻮﺷﺘﻪ ﺷﺪﻩ ﺍﺳﺖ2002 ﻛﺘﺎﺏ ﻓﻮﻕ ﭼﺎﭖPDF ﺷﺎﻣﻞ ﻣﺘﻦCD ﺍﻳﻦ ﻣﻄﺮﺡ ﺷﺪﻩ ﻭ ﻟـﺬﺍ ﺑـﺮﺍﻱProblem-oriented ﺍﺻﻮﻝ ﺑﺤﺚ ﺑﺮ ﻣﺒﻨﺎﻱ. ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩﺍﻧﺪCD ﺟﻬﺖ ﺩﺭﻙ ﺑﻬﺘﺮ ﺭﻭﺍﺑﻂ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻭ ﺍﺛﺮﺍﺕ ﻓﻴﺰﻳﻮﻟﻮﮊﻳﻚ ﺩﺭanimation ﭼﻨﺪ ﺗﺼﻮﻳﺮ. ﺳﻨﺎﺭﻳﻮﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻭ ﺗﺴﺖﻫﺎﻱ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ،ﺍﻃﺮﺍﻑ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ ﻣﺘﻦ . ﺩﺭ ﻗﺴﻤﺖ ﺩﻳﮕﺮ ﻓﻴﻠﻢ ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻋﺼﺎﺏ ﺑﺼﻮﺭﺕ ﺗﻚ ﺗﻚ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻭ ﭼﺸﻢ ﭘﺰﺷﻜﻲ ﺑﺴﻴﺎﺭ ﻣﻔﻴﺪ ﻭ ﺿﺮﻭﺭﻱ ﺑﻪ ﻧﻈﺮ ﻣﻲﺭﺳﺪENT ، ﺟﺮﺍﺣﻲ ﻓﻚ ﻭ ﺻﻮﺭﺕ،ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺭﺷﺘﻪﻫﺎﻱ ﻧﻮﺭﻭﻟﻮﮊﻱ 2005
16.9 Textbook of CRITICAL CARE (Salekan E-book) SECTION I RESUSCITATION AND MEDICAL EMERGENCIES SECTION II TRAUMA SECTION III IMAGING SECTION IV CELL INJURY AND CELL DEATH SECTION V INFECTIONS DISEASE SECTION VI ENDOCTINOLOGY, METABOLISM, NUTRITION, PHARMACOLOGY SECTION VII CARDIOVASCULAR SECTION VIII PULMONARY 17.9 Critical Decisions in Headache Management
(Giammarco. Edmeads. Dodick)
ــــ
(SALEKAN E-BOOK)
2002
18.9 CURRENT MANAGEMENT IN CHILD NEUROLOGY (SECOND EDITION) (Bernrd L. Maria, MD, MBA) Section 1: Clinical Practice Trends Section 2: The Office Visit Section 3: The Hospitalized Child
ــــ
19.9 DICTIONARY OF MULTIPLE SCLEROSIS (Lance D Blumgardt) (Martin Dunitz) 20.9 DISORDERS OF COGNITIVE FUNCTION
(VCD-I)
Severe Amnesic Syndrome: Anterograde and Retrograde Amnesia Left Spatial Neglect Broca's Aphasia
21.9 DISORDERS OF COGNITIVE FUNCTION Wernicke's Aphasia Negative Signs of Executive Dysfunction
Basic Mental Status Examination
Perseverative Verbal Behavior in Amnesia Eye Movements in Severe Left Spatial Neglect Lewy Bodies
Semantic Memory Loss Anosognosia for Hemiparesis Impaired Verbatim Repetition
Fluctuativng Sensorium in Dementia With Paraphasias
2002
(VCD-II) (AMERICAN ACADEMY OF NEUROLOGY) (CONTINUUM)
Dysexecutive Syndrome Prosopognosia and Visual Agnosia
22.9 DISORDERS OF COGNITIVE FUNCTION
2002
(AMERICAN ACADEMY OF NEUROLOGY) (CONTINUUM)
Disinhibited Behavior Simultanagnosia
Grasp Response and Imitation Behavior Optic Ataxia
Positive Signs of Executive Dysfunction Ocular Apraxia
Progressive Apraxia
2002
(VCD-III) (AMERICAN ACADEMY OF NEUROLOGY) (CONTINUUM)
Token Test for Auditory Comprehension
Confrontation Naming
Finger Constructions
Luria 3-Step Test
Line Cancellation
Gestural Praxis
23.9 EMG Training (Kenneth Ricker, M.D.)
ــــ
ﻣﺘﻦ ﻫﻤﺮﺍﻩ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﺩﺭ ﻣﻮﺭﺩ ﻧﺤﻮﺓ ﻛﺎﺭ. ﺑﻴﻤﺎﺭ ﻣﺨﺘﻠﻒ ﺭﺍ ﻫﻤﺎﻧﮕﻮﻧﻪ ﻛﻪ ﻣﺎﻧﻴﺘﻮﺭ ﻣﺸﺎﻫﺪﻩ ﻣﻲﮔﺮﺩﺩ ﺑﻪ ﺗﺼﻮﻳﺮ ﻛﺸﻴﺪﻩ ﻭ ﺻﺪﺍﻱ ﺁﻥ ﺭﺍ ﭘﺨﺶ ﻣﻲﻛﻨﺪ٢٧ ﺍﺯEMG ﻣﻮﺭﺩ٧٥ . ﺗﻬﻴﻪ ﺷﺪﻩ ﺍﺳﺖTOENNIES ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻛﻪ ﺟﻬﺖ ﺁﻣﻮﺯﺵ ﺍﻟﻜﺘﺮﻭﻣﻴﻮﮔﺮﺍﻓﻲ ﺗﻮﺳﻂ ﺷﺮﻛﺖ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
47 . ﺑﺮﺍﻱ ﻣﺒﺘﺪﻳﺎﻥ ﻭ ﻧﻴﺰ ﺍﻓﺮﺍﺩ ﻣﺠﺮﺏ ﺩﺭ ﺍﻳﻦ ﺯﻣﻴﻨﻪ ﺟﺎﻟﺐ ﺗﻮﺟﻪ ﺧﻮﺍﻫﺪ ﺑﻮﺩCD ﻓﺎﻳﻞﻫﺎ ﺭﺍ ﻓﺮﺍﻫﻢ ﻣﻲﺁﻭﺭﺩ ﺍﻳﻦSearch ﺍﻣﻜﺎﻥEMG glossary . ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻓﺎﻳﻞ ﻣﺴﺘﻘﻞ ﺍﺭﺍﺋﻪ ﻣﻲﮔﺮﺩﺩCase ﻫﺮ.ﺭﺍ ﺍﺭﺍﺋﻪ ﻛﺮﺩﻩ ﺍﺳﺖ ﻭ ﺳﺆﺍﻻﺗﻲ ﺭﺍ ﻣﻄﺮﺡ ﻧﻤﻮﺩﻩ ﻭ ﭘﺎﺳﺦ ﺩﺍﺩﻩ ﺍﺳﺖ 24.9 ENS Teaching Course
ــــ
ﻋﻤﺪﺓ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡﺷﺪﻩ ﺗﺤﺖ ﻋﻨﺎﻭﻳﻦ. ﻣﻲﺑﺎﺷﺪ ﺍﻃﻼﻋﺎﺕ ﺑﻪﺭﻭﺯ ﺭﺍ ﺩﺭ ﻣﻮﺭﺩ ﻣﺒﺎﺣﺚ ﻋﻤﺪﻩ ﻭ ﺑﺤﺚﺍﻧﮕﻴﺰ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺟﺪﻳﺪ ﻭ ﻧﻴﺰ ﺩﻳﺪﮔﺎﻩ ﺟﺪﻳﺪ ﻧﺴﺒﺖ ﺑﻪ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺎﻳﻊ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺭﺍ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ٢٠٠٣ ﺩﺭ ﺳﺎﻝENS ﻛﻪ ﺷﺎﻣﻞ ﻣﻘﺎﻻﺕ ﺩﻭﺭﺓ ﺁﻣﻮﺯﺷﻲ ﻛﻨﮕﺮﻩCD ﺍﻳﻦ . ﻣﺨﺘﻠﻒ ﻧﻴﺰ ﻣﻲﺑﺎﺷﺪTitle ﺯﻳﺮ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﻧﺪ ﻛﻪ ﻫﺮ ﻛﺪﺍﻡ ﺷﺎﻣﻞ ﭼﻨﺪ Dizziness and vesthg Neurogenetics for Clinicians Neuroimaging ICU in Neurology
25.9 EPILEPSY
Clinical Neurophysiology NeuroSurgery for Neurologist Neurology of Systemic disease Movement discords
The Comprehensive CD-ROM
Clinical Neuropathology Epilepsy Parkinson's diseane Neuroplathies
Sleep Disorder Multiple Sclerosis Ultrasound in Neurology Current Treatments Neurology
(Jerome Engel, Jr., M.D., Ph.D., Timothy A. Pedley, M.D.)
Stroke Muscle disorders Dementia
1999
Lippincott Williams & Wilkins
ﺗﻮﺍﻧـﺎﻳﻲ. ﮔﻨﺠﺎﻧـﺪﻩ ﺷـﺪﻩ ﺍﺳـﺖCD ﺩﺭimaging ﻋﻜـﺲ ﻭ٨٠٠ ﻫﻤﭽﻨـﻴﻦ. ﺳﺮﻓﺼـﻞ ﻣـﻲﺑﺎﺷـﺪ٢٨٩ ﻛﺘﺎﺏ ﺭﺍ ﺩﺭ ﺑﺮﻣﻲﮔﻴﺮﺩ ﻛﻪ ﻣﺸـﺘﻤﻞ ﺑـﺮFull text . ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖEpilepsy: A comprehensive textBook ﻛﻪ ﺑﺮﺍﺳﺎﺱ ﻛﺘﺎﺏCD ﺍﻳﻦ . ﺭﻓﺮﺍﻧﺲ ﻛﻪ ﺗﻮﺳﻂ ﻧﻮﻳﺴﻨﺪﻩ ﺟﻤﻊﺁﻭﺭﻱ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﺍﺯ ﻧﻘﺎﻁ ﻗﻮﺕ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩ٥٠٠ ﻭ ﺧﻼﺻﻪ ﻣﻘﺎﻻﺕ ﺑﻴﺶ ﺍﺯWeblink- Seasch 26.9 Essentials of Clinical Neurophysiology
2002
(Karl E. Misulis MD. PhD, Thomas C. Head MD)
27.9 Foundations of NEUROBIOLOGY
ــــ
28.9 Foundations of Behavioural Neuroscience
ــــ
. ﻗﺴﻤﺖ ﺯﻳﺮ ﺍﺳﺖ٥ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺷﺎﻣﻞ، ﻭ ﺗﻜﻤﻴﻞ ﺍﻃﻼﻋﺎﺕ ﺍﻓﺮﺍﺩﻱ ﻛﻪ ﺑﺎ ﻋﻠﻮﻡ ﻣﺮﺑﻮﻁ ﺑﻪ ﺍﻋﺼﺎﺏ ﻭ ﺑﻴﻮﻟﻮﮊﻱ ﺳﺮﻭﻛﺎﺭ ﺩﺍﺭﻧﺪSelf evaluattion ﺑﻪ ﻣﻨﻈﻮﺭCD ﺍﻳﻦ . ﺧﻮﺩﺁﺯﻣﺎﻳﻲﻫﺎ ﻛﻪ ﻓﻬﺮﺳﺖﺑﻨﺪﻱ ﺷﺪﻩ ﻭ ﺟﻬﺖ ﺩﺍﺭﻧﺪ-١ ﺁﻣﺎﺩﮔﻲ ﺳﺨﻨﺮﺍﻧﻲ ﻛﻪ ﺑﻪ ﻣﺎ ﺍﻣﻜﺎﻥ ﻣﻲﺩﻫـﺪ ﺑـﺎ-٤ Expansion Module -٣ . ﺍﻧﻴﻤﻴﺸﻦﻫﺎ ﻭ ﻓﻴﻠﻢﻫﺎﻱ ﻭﻳﺪﺋﻮﻳﻲ ﺁﻣﻮﺯﻧﺪﻩ ﻭ ﺑﻴﺎﺩﻣﺎﻧﺪﻧﻲ ﺑﻪ ﻫﻤﺮﺍﻩ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺘﺒﻲ ﺭﺍﺟﻊ ﺑﻪ ﻫﺮ ﻗﻄﻌﻪ ﻓﻴﻠﻢ-٢ . ﻣﻌﺮﻓﻲ ﺷﺪﻩﺍﻧﺪ ﻭ ﻟﻴﻨﻚﻫﺎﻱ ﻣﺘﻌﺪﺩ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩﺍﻧﺪNeurobiology ﺳﺎﻳﺖﻫﺎﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﻋﻠﻮﻡ، CD ﺩﺭ ﺑﺨﺶ ﺩﻳﮕﺮﻱ ﺍﺯ. ﻣﺨﺼﻮﺹ ﺑﻪ ﺧﻮﺩ ﺭﺍ ﺳﺎﺧﺘﻪ ﻭ ﺟﻬﺖ ﺍﺭﺍﺋﻪ ﺩﺭ ﻛﻨﻔﺮﺍﻧﺲﻫﺎ ﻳﺎ ﺗﺪﺭﻳﺲ ﺍﺯ ﺁﻧﻬﺎ ﺑﻬﺮﻩ ﺑﺒﺮﻳﻢplay list ، CD ﺍﺷﻜﺎﻝ ﻭ ﻓﻴﻠﻢﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ
-Neural Communication -
. ﺑﺨﺶ ﻋﻤﺪﻩ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ٥ ﺷﺎﻣﻞCD ﺍﻳﻦ
Central Nervous system
-Research methods
-Visual System
- Control of movements
Quiz ﺩﺭ ﭼﻨﺪ ﻓﺼﻞ ﺳـﻮﺍﻻﺗﻲ ﺑـﻪ ﻋﻨـﻮﺍﻥ. ﻓﻬﺮﺳﺖ ﺩﺭﺧﺘﭽﻪﺍﻱ ﻣﻄﺎﻟﺐ ﻛﻤﻚ ﻣﻬﻤﻲ ﺑﻪ ﻳﺎﺩﮔﻴﺮﻱ ﻋﻠﻮﻡ ﭘﺎﻳﻪ ﺍﻋﺼﺎﺏ ﻣﻲﻧﻤﺎﻳﺪ. ﻛﺎﻣﻞ ﻣﻲﺑﺎﺷﺪglossary , Search ﻫﻤﺮﺍﻩ ﺑﺎ ﻣﻮﺗﻮﺭ.ﺣﺎﻭﻱ ﺗﺼﺎﻭﻳﺮﻱ ﺑﺎ ﻃﺮﺍﺣﻲ ﻋﺎﻟﻲ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺭﺍﺣﺖ ﺟﻬﺖ ﻓﻬﻢ ﺟﺰﺋﻴﺎﺕ ﭘﻴﭽﻴﺪﻩ ﻭ ﺭﻳﺰ ﺳﺎﺧﺘﻤﺎﻥﻫﺎﻱ ﻧﻮﺭﻭﻧﻲ ﻣﻲﺑﺎﺷﺪ
.ﻣﻄﺮﺡ ﺷﺪﻩﺍﻧﺪ ﻛﻪ ﺟﻬﺖ ﺗﻜﻤﻴﻞ ﺁﻣﻮﺧﺘﻪﻫﺎ ﻭ ﻳﺎﺩﮔﻴﺮﻱ ﻣﻨﺎﺳﺐ ﺍﺳﺖ 29.9 FUNDAMENTALS OF HUMAN NEURAL STRUCTURE (S. Mark Williams) (Sylvius 30.9 General depression and its pharmacological treatment (Professor Brain Leonard)
TM
ــــ
2.0)
(VCD)
31.9 Guidelines (American Academy of Neurology) (SALEKAN E-BOOK) . ﺑﺎ ﺩﺳﺘﺮﺳﻲ ﺁﺳﺎﻥ ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻛﺎﺭﺑﺮ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪOffline ﺩﺭ ﺁﻣﺪﻩ ﺍﺳﺖ ﻛﻪ ﻛﻠﻴﻪ ﻣﻘﺎﻻﺕ ﺭﺍ ﺑﻪ ﺻﻮﺭﺕSalekan E-Book ﺩﺭ ﻗﺎﻟﺐSearch ﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺩﺭﻣﺎﻧﻲ ﺁﻛﺎﺩﻣﻲ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺁﻣﺮﻳﻜﺎ ﻣﻲﺑﺎﺷﺪ ﺑﻪ ﺻﻮﺭﺕ ﻓﺎﻳﻞ ﻗﺎﺑﻞGuidline ﻛﻪ ﺷﺎﻣﻞ ﺁﺧﺮﻳﻦCD ﺍﻳﻦ - Brain Injury & Brain Death - Child Neurology
- Dementia
- Epilepsy
32.9 Human Brain Cancer: Diagnostic Decisions 33.9 Interactive Guide to Human Neuroanatomy Atlas: -Surface Anatomy of Brain Exam:I -Surface Anatomy of the Brain
- Headache - Movement Disorders - Multiple Sclerosis
(Lauren A. Langford, MD, Dr. med,)
- Neuroimaging
- Neuromuscular
- Stroke and Vascular Neurology
-Technology Assessment
American Medical Association
ــــ 2002
(Mark F. Bear, Barry W. Connors, Michael A. Paradiso)
-Cross-Sectional Anatomy of Brain -Cross-Sectional Anatomy of the Brain
2004
-The Spinal Cord -The Anatomy Nervous System -Comprehensive Exam
-The Cranial Nerves -The Blood Supply to the Brain
34.9 ICU Syllabus
ــــ
٢٠٠٤ ﺍﺯ ﻣﻨـﺎﺑﻊ ﻭ ﻣﺠـﻼﺕ ﻣﺨﺘﻠـﻒ ﺗـﺎ ﺳـﺎﻝICU Patient Care ﺁﺧﺮﻳﻦ ﻣﻘﺎﻻﺕ ﻣﻨﺘﺸﺮﻩ ﻭ ﻧﻴﺰ ﻣﻘﺎﻻﺕ ﻣﻬﻢ ﻗﺒﻠﻲ ﺩﺭ ﺯﻣﻴﻨﻪﻫﺎﻱ ﻣﺨﺘﻠـﻒ، ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ، ﺳﺮﻭﻛﺎﺭ ﺩﺍﺭﻧﺪICU ﻛﻪ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﭘﺰﺷﻜﺎﻧﻲ ﻛﻪ ﺑﺎ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺪﺣﺎﻝ ﻭ ﺑﺴﺘﺮﻱ ﺩﺭCD ﺩﺭ ﺍﻳﻦ : ﺳﺮﻓﺼﻞﻫﺎﻱ ﻋﻤﺪﻩ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ. ﻗﻮﻱ ﺍﺟﺮﺍ ﺷﺪﻩ ﺍﺳﺖSearch ﺑﺎ ﻗﺎﺑﻠﻴﺖPDF ﺟﻤﻊﺁﻭﺭﻱ ﻭ ﺑﻪ ﺻﻮﺭﺕ ﻓﺎﻳﻞ Anemia and blood Transfusion Hyperghycemia and Ihsulia Non invasive Ventilation
ARDS Hypothermia for cardiac arrest Nutritions
35.9 InterBRAIN (Martin C. hirsh) (Springer) 1. Gross Anatomy
2. Vessels and Meninges
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
3. Brain Slices
Ethics Impaired cognition Pneumonia
Fever Wokup Liver disease Pulmonary Embolism
Hemodynamics Mechanical Vetitation Renal failure
RARS Sedation Sepsis
Weaning From Mechanical Vetitation
ــــ 4. Microscopical Sections
5. Functional Systems
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
48 2003
36.9 International Symposium ON 10 Years Betaferon
CDﻓﻮﻕ ﻛﻪ ﻣﺎﺣﺼﻞ ﺳﻤﭙﻮﺯﻳﻮﻡ ﭘﺮﺍﮒ ﺩﺭ ﺳﺎﻝ ٢٠٠٣ﺩﺭ ﻣﻮﺭﺩ ﺗﺠﺮﺑﻪ ﺩﻩﺳﺎﻟﺔ ﻣﺼﺮﻑ ﺑﺘﺎﻓﺮﻭﻥﻫﺎ ﺩﺭ ﺩﺭﻣﺎﻥ MSﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ ﺗﻤﺎﻡ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ ﻛﻨﮕﺮﻩ ﺍﺳﺖ .ﻋﻨﺎﻭﻳﻦ ﻣﺒﺎﺣﺚ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺗﺰ: ﺩﺭﻣﺎﻥ ﺳﻤﭙﺘﻮﻣﺎﺗﻴﻚ ﻭ ﺗﻮﺍﻧﺒﺨﺸﻲ ﺩﺭ MS
ﺍﻓﻖﻫﺎﻱ ﺟﺪﻳﺪ
Geomics and Proteomics
ﺁﻣﻮﺧﺘﻪﻫﺎﻱ ﻣﺎﻟﻮﺯ ﻣﻄﺎﻟﻌﺎﺕ ﺑﺎﻟﻴﻨﻲ ﺩﺭﺑﺎﺭﺓ ﻓﺎﻛﺘﻮﺭﻫﺎﻱ ﭘﺮﻭﮔﻨﻮﺳﺘﻴﻚ ﺍﻳﻨﺘﺮﻓﺮﻭﻥ ﺩﻭﺯ ﺑﺎﻻ ﻳﺎ ﭘﺎﻳﻴﻦ؟
ﻧﺘﺎﻳﺞ ﻣﻄﺎﻟﻌﺎﺕ BENEFITﻭ BEYOND
ﺍﻫﻤﻴﺖ ﺑﺎﻟﻴﻨﻲ ﻳﺎﻓﺘﻪﻫﺎﻱ ﻧﺮﻭﭘﺎﺗﻮﻟﻮﮊﻳﻚ MS
ﺗﺎﺭﻳﺨﭽﺔ ﺩﺭﻣﺎﻥ ﻣﺪﺭﻥ MS
ﻧﻘﺶ Stem Cell Transplantﺩﺭ ﺩﺭﻣﺎﻥ Aggressive MS
ﺑﺘﺎﻓﺮﻭﻥ ﺩﺭ ﺩﺭﻣﺎﻥ Primary Progressive MS
37.9 MANAGING STRESS
2002 ــــ
)38.9 Manual of Pain Management (Carol A. Warfield, Hilary J. Fausett
)(Second Edition) (SALEKAN E-BOOK ﺍﻳﻦ CDﺑﺎ ﻓﺮﻣﺖ ﺧﺎﺹ ﺧﻮﺩ ﻛﻪ ﻧﺤﻮﺓ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﻥ ﺭﺍ ﺭﺍﺣﺖ ﻧﻤﻮﺩﻩ ﺍﺳﺖ .ﺯﻣﻨﻴﺔ ﻛﺎﻣﻠﻲ ﺑﺮﺍﻱ ﻣﻄﺎﻟﻌﻪ ﻧﺤﻮﺓ ﺍﺩﺍﺭﻩ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ ﺩﺭﺩﻫﺎﻱ ﻗﺴﻤﺖﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺭﺍ ﻓﺮﺍﻫﻢ ﻣﻲﺁﻭﺭﺩ .ﺩﺭ ﻓﺼﻞ ﺍﻭﻝ ﻧﻈﺮﻳﻪﻫﺎﻱ ﻋﻤﺪﺓ ﻓﻴﺰﻭﻟﻮﮊﻱ ﺩﺭﺩ ﻣﻄﺮﺡ ﺷﺪﻩ ﺍﺳﺖ. ﻋﻤﺪﻩ ﺍﻳﻦ CDﺗﻮﺻﻴﻔﻲ ﺍﺯ ﺳﻨﺪﺭﻡﻫﺎﻱ ﺷﺎﻳﻊ ﺩﺭﺩ ﺍﺳﺖ ﻛﻪ ﺑﺮ ﺍﺳﺎﺱ ﺁﻧﺎﺗﻮﻣﻲ ﺑﺎﻟﻴﻨﻲ ﻛﻼﺳﻪﺑﻨﺪﻱ ﺷﺪﻩﺍﻧﺪ .ﻓﺼﻞ ﺑﻌﺪﻱ ﺑﺮ ﺭﻭﻱ ﺩﺭﻣﺎﻥﻫﺎ ﻭ Procedureﻫﺎﻳﻲ ﻛﻪ ﺑﺮ ﺭﻭﻱ ﺑﻴﻤﺎﺭﻳﺎﻥ ﺩﺭﺩﻣﻨﺪ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﻧﺪ ،ﻣﺘﻤﺮﻛﺰ ﻛﺮﺩﻩ ﺍﺳـﺖ .ﺩﺭﻣـﺎﻥ ﺩﺭﺩ ﻛﻮﺩﻛـﺎﻥ ،ﺳـﺎﻟﻤﻨﺪﺍﻥ ﻭ ﻧﻴـﺰ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ HIVﻧﻴﺰ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. -Pain Management
ــــ
-Common Painful Syndromes
)(CD I, II , III , IV
-Understanding pain
-Pain by Anatomic Location
)39.9 Microneurosurgery (M. G. Yasargil) Cassette 1 Aneurysms (VCD) (Thieme AV
2001
)40.9 Migraine Current Approaches To Treatment (Dr. Andrew Dowson
2002
)41.9 Movement Disorders Society Official Journal of The Movement Disorder Society Published by John Wiley & Sons, Ins VCD (I, II
2002
)42.9 Needle Electromyography (Daniel Dumitru, M.D., PhD. ﺍﻳﻦ CDﻛﻪ ﺑﺮ ﺍﺳﺎﺱ ﻛﺘﺎﺏ Needle EMGﻧﻮﺷﺘﺔ Daniel Dumitruﺩﺭ ﺳﺎﻝ ٢٠٠٢ﻃﺮﺍﺣﻲ ﻭ ﺍﺟﺮﺍ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ﻣﺘﻦ ﻛﺘﺎﺏ ﺑﻌﻼﻭﺓ EMG Video Libraryﺍﺳﺖ ٣٣ .ﻓﺎﻳﻞ ﻣﺨﺘﻠﻒ ﺷﺎﻣﻞ ﺍﻣﻮﺍﺝ ﻧﺮﻣﺎﻝ ﻭ ﻏﻴﺮﻧﺮﻣﺎﻝ ﻣﺨﺘﻠﻒ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ. ﺗﺼﺎﻭﻳﺮ ﺍﺭﺍﺋﻪﺷﺪﻩ ﺍﻃﻼﻋﺎﺕ ﻛﺎﻓﻲ ﺩﺭ ﻣﻮﺭﺩ ﻧﺤﻮﺓ ﺍﺟﺮﺍﻱ EMGﻭ Pitfullﻫﺎﻱ ﺁﻥ ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻗﺮﺍﺭ ﻣﻲﺩﻫﻨﺪ .ﻗﺎﺑﻠﻴﺖ Glossary , Searchﻗﻮﻱ ﻧﻴﺰ ﺍﺯ ﻣﺰﺍﻳﺎﻱ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻓﻮﻕ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩ.
1999
)43.9 NEUROANATOMY-3D-Stereoscopic Atlas of the Human Brain (Martin C. Hirsch, Thomas Kramer) (Springer ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺗﺼﺎﻭﻳﺮ ﺳﻪ ﺑﻌﺪﻱ ﻭ ﺑﺴﻴﺎﺭ ﺩﻗﻴﻘﻲ ﺍﺯ ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﻣﺮﻛﺰﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﻗﺪﺭﺕ ﺑﺎﻻﻱ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻗﺎﺩﺭﻳﻢ ﺍﺯ ﻫﺮ ﺟﻬﺖ ﺩﻟﺨﻮﺍﻩ ﺑﻪ ﺗﺼﻮﻳﺮ Grossﻣﻐﺰ ﺑﻨﮕﺮﻳﻢ .ﺑﺎ ﺩﺭﻧﻈﺮﮔﺮﻓﺘﻦ ﺍﻳﻨﻜﻪ ﺗﻚ ﺗﻚ ﺍﺟﺰﺍﻱ ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﺭﺍ ﻣﺮﺣﻠﻪ ﺑﻪ ﻣﺮﺣﻠﻪ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺗﺼﻮﻳﺮ ﻗﺒﻠﻲ ﺍﺿﺎﻓﻪ ﻭ
ﻳﺎ ﻛﻢ ﻛﺮﺩ ،ﺟﺰﺋﻴﺎﺕ ﺍﺭﺗﺒﺎﻃﺎﺕ ﺳﻴﺴﺘﻢﻫﺎﻱ ﻋﻤﻠﻜﺮﺩﻱ ﻣﺨﺘﻠﻒ ﺑﻪ ﻭﺿﻮﺡ ﻣﺸﺨﺺ ﻣﻲﺷﻮﺩ .ﺗﺼﺎﻭﻳﺮ ﻭ ﺑﺮﺵﻫﺎ ﺑﺴﻴﺎﺭ ﻫﻮﺷﻤﻨﺪﺍﻧﻪ ﻭ ﻫﻨﺮﻣﻨﺪﺍﻧﻪ ﻃﺮﺍﺣﻲ ﮔﺸﺘﻪﺍﻧﺪ ﻭ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ،ﭘﺰﺷﻜﺎﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺩﺭﮔﻴﺮ ﺑﺎ ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﺁﻧﺮﺍ ﺗﺠﺮﺑﺔ ﺟﺪﻳﺪﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺮﺩﻩﺍﻧﺪ. ــــ
44.9 Neurofunctional Systems 3D
ــــ
)45.9 Neurological surgery (julian R. Youmans , MD Editor-in-Chief) (Fourth Edition) (Y.O.U.M.A.N.S
2001
)46.9 Neurology (Baker's clinical on CD-ROM
2002
47.9 New Analgesic Options: Overcoming Obstacles to Pain Relief -References
-Trauma
-Post Op Pain
-OA Pain
-Back Pain -Fibromyalgia
-Pharmacist Answer Sheet
- MD, NP, PA, RN Answer Sheet
25.7 Photographic manual of Regional Orthopaedic and Neurological Tests
ــــ
ﺍﻳﻦ CDﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ٨٥٠ﺗﺼﻮﻳﺮ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﺗﻤﺎﻡ ﻣﻌﺎﻳﻨﺎﺕ ﻧﻮﺭﻭﻟﻮﮊﻳﻚ ﻭ ﺍﺭﺗﻮﭘﺪﻳﻚ ﺭﺍ ﺑﺎ ﺟﺰﺋﻴﺎﺕ ﺗﻤﺎﻡ ﺭﻭﺷﻦ ﻣﻲﺳﺎﺯﺩ .ﺩﺭ ﻣﻮﺍﻗﻊ ﻟﺰﻭﻡ ﺗﺼﺎﻭﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻚ ﺿﺮﻭﺭﻱ ﻧﻴﺰ ﺍﺿﺎﻓﻪ ﺷﺪﻩﺍﻧﺪ .ﻓﺼﻮﻝ ﺑﺮ ﺍﺳﺎﺱ ﻣﺤﻞ ﻣﻮﺭﺩ ﻣﻌﺎﻳﻨﻪ ﻃﺮﺍﺣﻲ ﻭ ﻗﺴﻤﺖﺑﻨﺪﻱ ﺷﺪﻩﺍﻧـﺪ. ﻣﻌﺎﻳﻨﺎﺕ ﺍﺯ ﻓﻘﺮﺍﺕ ﮔﺮﺩﻧﻲ ﻭ ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ ﺷﺮﻭﻉ ﻭ ﺑﻪ ﻓﻘﺮﺍﺕ ﻛﻤﺮﻱ ﻭ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺗﺤﺘﺎﻧﻲ ﺧﺘﻢ ﻣﻲﺷﻮﻧﺪ .ﻫﺮ Testﺩﺭ ﻳﻚ ﺻﻔﺤﻪ ﻳﺎ ﺩﻭ ﺻﻔﺤﻪ ﻣﻘﺎﺑﻞ ﻫﻢ ﺑﺎ ﻋﻜﺲﻫﺎﻳﻲ ﻛﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻣﻌﺎﻳﻨـﻪ ﺭﺍ ﺑﻮﺿـﻮﺡ ﻧﺸـﺎﻥ ﻣـﻲﺩﻫﻨـﺪ ﺗﻮﺿـﻴﺢ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖ .ﺩﺭ ﺿـﻤﻦ ﻳـﻚ Sensitivity/Relialility Scaleﻧﻴﺰ ﺑﺮﺍﻱ ﻫﺮ ﻣﻌﺎﻳﻨﻪ ﺗﻌﺮﻳﻒ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻣﻴﺰﺍﻥ ﺣﺴﺎﺳﻴﺖ ﻭ ﻗﺎﺑﻠﻴﺖ ﺍﻋﺘﻤﺎﺩ ﺑﻪ ﺁﻥ ﻣﻌﺎﻳﻨﻪ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﺳﺎﺯﺩ .ﺍﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺩﺭ ﺑﻜﺎﺭﮔﻴﺮﻱ ﺗﺴﺖﻫﺎﻱ ﺣﺴﺎﺳﺘﺮ ﻭ ﺍﺧﺘﺼﺎﺹﺗﺮ ﻛﻤﻚ ﻓﺮﺍﻭﺍﻥ ﺑﻪ ﭘﺰﺷﻚ ﻣﻲﻧﻤﺎﻳﺪ. 1998
)48.9 Principles of Neurology (6th Edition) (Raymond D. Adams, M.A., M.D. 49.9 PROFESS
ــــ
ﺍﻳﻦ CDﻛﻪ ﻣﺎﺣﺼﻞ ﺳﻤﭙﻮﺯﻳﻮﻡ ﭘﻴﺸﮕﻴﺮﻱ ﺍﺯ ﺳﻜﺘﻪﻫﺎﻱ ﻣﻐﺰﻱ ﺩﺭ International Stroke Conferenceﺩﺭﺁﺭﻳﺰﻭﻧﺎﻱ ﺍﻣﺮﻳﻜﺎ ﺩﺭ ﺳﺎﻝ ٢٠٠٣ﻣﻲﺑﺎﺷﺪ ﭼﺎﻟﺶﻫﺎﻱ ﭘﻴﺶﺭﻭ ﺩﺭ ﺩﺭﻣﺎﻥ ﻭ ﭘﻴﺸﮕﻴﺮﻱ ﺍﺯ ﺳﻜﺘﻪﻫﺎﻱ ﻣﺠﺪﺩ ﻣﻐﺰﻱ ﺭﺍ ﻣﻄﺮﺡ ﻛﺮﺩﻩ ﻭ ﺁﺧﺮﻳﻦ ﺭﮊﻳﻢﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﻭﻳﺮﻭﺗﺮﻛﻞﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺭﺍ ﺩﺭ ﻗﺎﻟﺐ Lectureﻫﺎ ،ﺳﺆﺍﻝ ﻭ ﺟﻮﺍﺏ ﻭ ﺧﻼﺻﻪ ﻣﻘﺎﻻﺕ ﺍﺭﺍﺋﻪ ﻛﺮﺩﻩ ﺍﺳﺖ .ﻓﻬﺮﺳﺖ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: ﺍﻃﻼﻋﺎﺗﻲ ﻛﻪ ﺩﺭﺑﺎﺭﺓ ﺩﻳﭙﺮﻳﺪﺍﻣﻮﻝ ﻭﺟﻮﺩ ﺩﺍﺭﺩ - .ﭼﺮﺍ ﺑﺮﺧﻮﺭﺩ ﺑﺎ CVAﻣﺘﻔﺎﻭﺕ ﺍﺯ MIﺍﺳﺖ - .ﺁﻳﺎ ﺩﺭﻣﺎﻥ ﻣﺮﻛﺐ ﺁﻧﺘﻲﭘﻜﺪﺗﻲ ﺧﻄﺮﻧﺎﻙ ﺍﺳﺖ ﻳﺎ ﻣﻔﻴﺪ؟ -ﺁﻳﺎ ﺁﻧﮋﻳﻮﺗﺎﻧﻴﻦ IIﺩﻳﺴﻜﺎﻓﺎﻛﺘﻮﺭ ﻣﺴﺘﻘﻠﻲ ﺑﺮﺍﻱ ﺳﻜﺘﻪ ﺍﺳﺖ؟ -ﺭﮊﻳﻢ ﺩﺭﻣﺎﻧﻲ ﭘﻴﺸﮕﻴﺮﻱ ﺍﺯ ﺳﻜﺘﻪ ﺩﻭﻡ.ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
49 2000
50.9 Psychotropics
2001
)51.9 Recognizing Extrapyramidal Symptoms (VCD
ﺩﺍﻳﺮõﺍﻟﻤﻌﺎﺭﻑ ﻛﺎﻣﻠﻲ ﺍﺯ ﺗﻤﺎﻡ ﻣﻮﺍﺩ ﻭ ﺩﺍﺭﻭﻫﺎﻱ ﻣﻮﺛﺮ ﺑﺮ ﺳﻴﺴﺘﻢ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺷﺎﻣﻞ ﺑﺨﺸﻬﺎﻱ ﺯﻳﺮ ﻣﻲﺷﻮﺩ :ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﺭﻭﻳﻲ -ﻋﻮﺍﺭﺽ ﺟﺎﻧﺒﻲ -ﺗﺪﺍﺧﻼﺕ ﺩﺍﺭﻭﻳﻲ -ﻓﻬﺮﺳﺖ ﺍﺳﺎﻣﻲ ﺭﺍﻳﺞ ﺧﻴﺎﺑﺎﻧﻲ ﺩﺍﺭﻭﻫﺎ -ﺍﺻﻮﻝ ﺗﺮﻙ ﺩﺍﺭﻭ ،ﻣﻨﺤﻨﻲﻫﺎﻱ ﻧﻴﻤﻪ ﻋﻤﺮ ﺩﺍﺭﻭﻳﻲ -ﺍﻳﻨﺪﻛﺲ ﺑﺎ ﻣﺮﺍﺟﻌﻪ ﺑﻪ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﻣﻨﻮﮔﺮﺍﻑﻫﺎ ﻣﻲﺗﻮﺍﻥ ﺍﺯ ﺳﺎﺧﺘﻤﺎﻥ ﺷﻴﻤﻴﺎﻳﻲ -ﻓﺮﻣﻮﻝ ﺷﻴﻤﻴﺎﻳﻲ -ﻣﻮﺍﺭﺩ ﻭ ﻧﺤﻮﺓ ﺍﺳﺘﻔﺎﺩﺓ ﺑﺎﻟﻴﻨﻲ ﺷﺮﻛﺖﻫﺎﻱ ﺳﺎﺯﻧﺪﻩ ﻭ ﻧﺎﻡﻫﺎﻱ ﺗﺠﺎﺭﻱ ﻭ ﻧﻴﺰ ﺭﻓﺮﻧﺲﻫﺎﻱ ﻣﻄﺎﻟﻌﺎﺗﻲ ﻫﺮ ﻣﺎﺩﺓ ﺳﺎﻳﻜﻮﺗﺮﻭﭖ ﺍﻃﻼﻉ ﭘﻴﺪﺍ ﻛﺮﺩ. - and Tardive- Dyskinesia
ﻣﺒﺎﺣﺚ ﺍﻳﻦ CDﺷﺎﻣﻞ:
- Parkinsonism
- Akathisia
2001
- Clinical Examples of Acute Dystonia
52.9 Rune Aaslid TCD Simulator Version 2.1
ﺍﻳﻦ ﻧﺮﻡ ﺍﻓﺰﺍﺭ ﻳﻚ ﺷﺒﻴﻪ ﺳﺎﺯ ﺑﺮﺭﺳﻲﻫﺎﻱ ﺩﺍﭘﻠﺮ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻭﺍﻛﺴﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﻮﺳﻂ ﻣﺨﺘﺮﻉ ، TCDﺁﻗﺎﻱ Rune Aaslidﺩﺭ ﺍﻳﻦ CDﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ﻣﺘﻨﻲ ﺍﺳﺖ ﻛﻪ ﻧﺤﻮﺓ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ CDﺭﺍ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﺪ .ﺍﺻﻮﻝ ﺩﺍﭘﻠﺮ ﺳـﻮﻧﻮﮔﺮﺍﻓﻲ- ﺁﻧﺎﺗﻮﻣﻲ -ﻫﻤﻮﺩﻳﻨﺎﻣﻴﻚ ﻭ ﻣﻮﺍﺭﺩ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻋﺮﻭﻕ ﻣﻐﺰﻱ ﺭﺍ ﺗﻮﺿﻴﺢ ﻣﻲﺩﻫﺪ .ﻗﺎﺑﻠﻴﺖﻫﺎﻱ ﻓﺮﺍﻭﺍﻧﻲ ﺍﺯ ﺟﻤﻠﻪ ﺍﻳﻦ ﻣﻮﺍﺭﺩ ﺭﺍ ﺩﺍﺭﺍ ﺍﺳﺖ :ﻧﻤﺎﻳﺶ ﺍﺳﭙﻜﺘﺮﻭﻡ ﺩﺍﭘﻠﺮ -ﻧﻤﺎﻳﺶ ﻣﺤﻞ ﺗﺎﺑﺶ ﻭ ﺯﺍﻭﻳﻪ ﺗﺎﺑﺶ ﺍﻣﻮﺍﺝ -ﻣﻮﻧﻴﺘﻮﺭﻳﻨﮓ -ﺗﺼﻮﻳﺮ – CBFﺁﻧـﺎﺗﻮﻣﻲ ﻭ ﭘـﺎﺗﻮﻟﻮﮊﻱﻫـﺎﻱ ﻣﺨﺘﻠـﻒ، ﻛﻨﺘﺮﻝ ﻛﺎﺭﺩﻳﻮ ﻭﺍﺳﻜﻮﻻﺭ -ﺗﺄﺛﻴﺮ ﺗﻐﻴﻴﺮ ﺿﺮﺑﺎﻥ ﻗﻠﺐ -ﺗﺄﺛﻴﺮ ﺗﻐﻴﻴﺮ ﺗﻨﻔﺲ HITS -ﻭ ﺑﺎﻻﺧﺮﻩ ﺩﻳﺪ ﺳﻪ ﺑﻌﺪﻱ ﻛﻪ ﺗﺠﺴﻢ ﻣﻮﻗﻌﻴﺖ ﻓﻀﺎﻳﻲ ﻋﺮﻭﻕ ﺩﺭ ﺩﺍﺧﻞ ﺟﻤﺠﻤﻪ ﺭﺍ ﺳﻬﻞ ﻣﻲﻧﻤﺎﻳﺪ .ﺍﻳﻦ CDﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﻭ ﻣﺆﺛﺮﺗﺮﻳﻦ ﺍﺑﺰﺍﺭﻫﺎﻱ ﺁﻣﻮﺯﺵ TCDﺍﺳﺖ ﻛﻪ ﺗﻮﺳـﻂ ﺍﺳـﺎﺗﻴﺪ ﻭ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ .ﻣﻔﺎﻫﻴﻢ ﭘﻴﭽﻴﺪﻩ ﺩﺍﭘﻠﺮ ﻋﺮﻭﻕ ﻣﻐﺰﻱ ﺭﺍ ﺑﺼﻮﺭﺕ ﻣﻠﻤﻮﺱ ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻋﻼﻗﻪﻣﻨﺪﺍﻥ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ. ــــ
ــــ
53.9 Stroke Overview of Stroke: 1. Stroke in Perspective 2. Pathogenesis & Pathophysiology 3. Evaluation & Diagnosis 4. Interventions 5. Thrombolytic Therapy Studies IV Tissue Plasminogen Activator(t-PA) Studies: 1. Recent Multicenter, IV Streptokinase (SK) Studies Ultra Rapid Response: 1. Increasing Public/Professional Awareness 2. Modifying Care Patterns 3. Stroke Care Systems 4. Assessing Critical Resources Case Studies 31.7 SPINE implants )(CD I , II
: CD Iﺩﺭ ﺍﻳﻦ CDﻧﺤﻮﺓ ﺟﺮﺍﺣﻲ ﻭ ﺑﻪﻛﺎﺭﮔﺬﺍﺷﺘﻦ ﭘﺮﻭﺗﺰﻫﺎﻱ ﻣﻬﺮﻩ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺍﻃﻼﻋﺎﺕ ﻛﺎﻣﻠﻲ ﺭﺍﺟﻊ ﺑﻪ ﭘﺮﻭﺗﺰﻫﺎﻱ ﺟﺎﻧﺸﻴﻦ ﺟﺴﻢ ﻣﻬﺮﻩ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. : CD IIﺩﺭ ﺍﻳﻦ CDﻧﺤﻮﻩ ﺟﺮﺍﺣﻲ ﻭ ﺑﻜﺎﺭﮔﺬﺍﺷﺘﻦ ﺩﺳﺘﮕﺎﻩ Diapasone-hookﺑﺮ ﺭﻭﻱ ﻣﻬﺮﻩﻫﺎﻱ ﻛﻤﺮﻱ ﺩﺭ ﺩﺭﻣﺎﻥ ﻣﻮﺍﺭﺩ ﺗﺮﻭﻣﺎﺗﻴﻚ ﻭ ﺍﺳﻜﻮﺍﻧﻴﻮﺭ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. 1999 ــــ
)54.9 TEXTBOOK of CLINICAL NEUROLOGY (Christopher G. Goetz, MD, Eric J. Pappert, MD) (W.B. Saunders Company
)Atlas of Brain Anatomy An interactive tool for students, teachers, and researchers (Wieslaw L. Nowinski, A. Thirunavuukarasuu, R. Nick Bryan ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺗﺼﺎﻭﻳﺮ MRIﺩﺭ ﺳﻪ ﺟﻬﺖ ،ﻃﺮﺍﺣﻲﻫﺎﻱ ﺭﻧﮕﻲ ﻭ ﺳﻴﺴﺘﻢ ﻧﺎﻣﮕﺬﺍﺭﻱ ﻣﺎ ﺭﺍ ﻗﺎﺩﺭ ﻣﻲﺳﺎﺯﺩ ﺑﺮﺍﺣﺘﻲ ﻫﺮ ﺳﺎﺧﺘﻤﺎﻥ ﺩﺍﺧﻠﻲ ﻣﻐﺰﻱ ﺭﺍ ﺩﺭ ٣ﺟﻬﺖ ﺑﻄﻮﺭ ﻫﻤﺰﻣﺎﻥ ﻣﺸﺎﻫﺪﻩ ﻧﻤﺎﻳﻴﻢ .ﺟﻬﺖ ﺗﺠﺴﻢ ﻓﻀﺎﻳﻲ ﺑﻬﺘﺮ ﻭ ﻋﻤﻠﻴﺎﺕ ﺍﺳﺘﺮﺗﻮﺗﺎﻛﺴﻲ ﻣـﻲﺗـﻮﺍﻥ Gridﺧﺎﺻﻲ ﺭﺍ ﺑﺮ ﺭﻭﻱ ﺗﺼﻮﻳﺮ ﻗﺮﺍﺭ ﺩﺍﺩ ﻭ ﻓﺎﺻﻠﻪﻫﺎﻱ ﺩﻟﺨﻮﺍﻩ ﺭﺍ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﻧﻤﻮﺩ .ﺩﺭ ﻗﺴﻤﺖ ﺗﺴﺖ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ interactiveﻭ ﺑﺴﻴﺎﺭ ﺟﺬﺍﺏ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﺍﺭﺯﻳﺎﺑﻲ ﻣﻔﺎﻫﻴﻢ ﻭ ﺁﻣﻮﺧﺘﻪﻫﺎ ﻣﻘﺪﻭﺭ ﻣﻲﮔﺮﺩﺩ .ﺩﺭ ﻗﺴﻤﺖ Glossoryﺗﻮﺿﻴﺢ ﻛﺎﻣﻠﻲ ﺭﺍﺟﻊ ﺑﻪ ﻫﺮ ﻛﺪﺍﻡ TM
55.9 The Cerefy
ﺍﺯ ﻣﻨﺎﻃﻖ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻣﻮﺭﺩ ﺍﺷﺎﺭﻩ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ CDﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺍﻓﺮﺍﺩﻳﻜﻪ ﻧﻮﺭﻭﺁﻧﺎﺗﻮﻣﻲ ،ﻧﺮﻭﻟﻮﮊﻱ -ﺟﺮﺍﺣﻲ ﺍﻋﺼﺎﺏ -ﻧﺮﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ -ﻋﻠﻮﻡ ﻧﺮﻭﺳﺎﻳﻨﺲ ﻭ ﺭﻭﺍﻧﭙﺰﺷﻜﻲ ﻣﻲﺁﻣﻮﺯﻧﺪ ﻳﺎ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﻨﺪ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ. )56.9 The Clinical Diagnosis of Alzheimer's Disease (An Interactive Guide for Family Physician
ــــ
ﺗﻮﺳﻂ ﮔﺮﻭﻩ Alzheimer disease groupﺑﻴﻤﺎﺭﺳﺘﺎﻥ RiverViewﻛﺎﻧﺎﺩﺍ ﺗﻬﻴﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﭼﻨﺪﻳﻦ ﻗﻄﻌﻪ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺭﺍﺟﻊ ﺑﻪ ﻧﺤﻮﺓ ﻣﺼﺎﺣﺒﻪ ﺑﺎ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ ﺁﻟﺰﺍﻳﻤﺮ ﻭ Flowchart
ﺗﺸﺨﻴﺺ ﺑﺎﻟﻴﻨﻲ
ﺑﺮﺭﺳﻲ ﺁﺯﻣﺎﻳﺸﮕﺎﻫﻲ
ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ
ﻣﻌﺮﻓﻲ
ﺗﺸﺨﻴﺼﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﭼﻨﺪﻱ ﻣﻲﺑﺎﺷﺪ .ﺷﺎﻣﻞ ٨ﻣﺒﺤﺚ ﻋﻤﺪﺓ ﺯﻳﺮ ﺍﺳﺖ:
Case Studies
ﺑﺮﺭﺳﻲ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ
)(Marion Hall David Robinson
ــــ
ﺑﺮﺭﺳﻲ ﺷﻨﺎﺧﺘﻲ
ﺷﺮﺡ ﺣﺎﻝ
57.9 THE HUMAN BRAIN
ــــ
)58.9 THE HUMAN NERVOUS SYSTEM (Springer
ــــ
)59.9 The Massachusetts General Hospital Handbook of Pain Management (Second Edition
)(Jane Ballantyne, Scott M. Fishman, Salahadin Abdi) (SALEKAN-E-book II. Diagnosis of Pain III. Therapeutic Options: Pharmacologic Approaches IV. Therapeutic Options: Nonpharmacologic Approaches I. General Considerations V. Acute Pain VI. Chronic Pain VII. Pain Due to Cancer VIII. Special Situations - Apendices - Subject Index
2002
60.9 The Movement Disorder Society's Guide to Botulinum Toxin Injections
CDﺍﻭﻝ :ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺵ ﻧﺤﻮﺓ ﺗﺰﺭﻳﻖ ﺑﻮﺗﻮﻟﻴﻨﻮﻡ ﺗﻮﻛﺴﻴﻦ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻛﺎﺩﺭ ﺍﻭﻝ ﺗﺼﻮﻳﺮ ﻛﻠﻲ ﺑﺪﻥ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﻛﻪ ﻗﺴﻤﺖ ﻣﻮﺭﺩ ﻧﻈﺮ ﺟﻬﺖ ﺗﺰﺭﻳﻖ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻣﻲﻧﻤﺎﻳﻲ .ﻋﻀﻼﺕ ﻭ ﺳﻨﺪﺭﻡﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻥ ﻗﺴﻤﺖ ﻓﻌﺎﻝ ﻣﻲﺷﻮﻧﺪ .ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﺳﻨﺪﺭﻡ ﺑﺎﻟﻴﻨﻲ ﻳـﺎ ﻋﻀـﻠﺔ ﺩﻟﺨـﻮﺍﻩ ﺍﺯ ﻟﻴﺴﺖ ،ﻓﻴﻠﻢ ﻧﺤﻮﺓ ﺗﺰﺭﻳﻖ ﺑﻬﻤﺮﺍﻩ ﺩﻳﺎﮔﺮﺍﻡ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﻣﻲﺷﻮﻧﺪ .ﺟﺰﺋﻴﺎﺕ ﺗﻜﻨﻴﻚ ﺗﺰﺭﻳﻖ ﻣﺎﻧﻨﺪ ﻧﺤﻮﺓ ﻧﺸﺴﺘﻦ ﺑﻴﻤﺎﺭ -ﻧﺤﻮﺓ ﻳﺎﻓﺘﻦ ﻋﻀﻠﻪ -ﻣﺸﺨﺼﺎﺕ ﺳﻮﺯﻥ ﻭ ﻧﺤﻮﺓ ﻓﻌﺎﻝﻛﺮﺩﻥ ﻋﻀﻠﻪ -ﻧﺤﻮﺓ ﻭﺭﻭﺩ ﺳﻮﺯﻥ -ﺗﻌﺪﺍﺩ ﺗﺰﺭﻳﻘﺎﺕ ﻭ ﺍﺣﺘﻴﺎﻃﺎﺕ ﻻﺯﻡ ﻧﻴﺰ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩﺍﻧﺪ. CDﺩﻭﻡ :ﻧﺮﻡﺍﻓﺰﺍﺭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺑﻮﺗﻮﻟﻴﻨﻮﻡ ﺗﻮﻛﺴﻴﻦ ﺩﺭ ﻛﻠﻴﻨﻴﻚ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺎﻧﻚ ﺍﻃﻼﻋﺎﺗﻲ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﺑﻴﻤﺎﺭ ﺭﺍ ﺗﺸﻜﻴﻞ ﺩﺍﺩﻩ ﻭ ﺑﺎ ﻗﺎﺑﻠﻴﺖ Searchﺑﺮ ﺣﺴﺐ ﺍﻟﻔﺒﺎ ﺩﺳﺘﻴﺎﺑﻲ ﺑﻪ ﺳﻮﺍﺑﻖ ﺑﻴﻤﺎﺭ ﺭﺍ ﻣﻤﻜﻦ ﻣﻲﺳﺎﺯﺩ .ﺩﺭ ﭼﺎﺭﺕﻫﺎﻱ ﺭﻧﮕﻲ ﻣﺮﺑﻮﻁ ﺑـﻪ ﻫـﺮ ﺑﻴﻤـﺎﺭ ﻣﺤـﻞ ﻭ ﻣﻘـﺪﺍﺭ ﺗﺰﺭﻳﻖ ﻣﺸﺨﺺ ﺷﺪﻩ ﻭ ﺩﺭ ﺣﺎﻓﻈﻪ ﺫﺧﻴﺮﻩ ﻣﻲﮔﺮﺩﻧﺪ .ﻓﺎﻳﻞ PDFﺁﻣﻮﺯﺷﻲ ﺟﻬﺖ ﺭﺍﻫﻨﻤﺎﻳﻲ ﺑﻴﻤﺎﺭﺍﻥ ﻭ ﺍﻃﻼﻋﺎﺕ ﺑﻴﺸﺘﺮ ﺩﺭ CDﻣﻮﺟﻮﺩ ﺍﺳﺖ .ﺍﻳﻦ CDﺑﻪ ﭘﺰﺷﻜﺎﻥ ﺩﺭ ﺟﻤﻊﺁﻭﺭﻱ ﻳﺎﻓﺘﻪﻫﺎ ﻭ ﻛﻼﺳﻪﺑﻨﺪﻱ ﺁﻧﻬﺎ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﺑﻌﺪﻱ ﻭ ﺗﺤﻘﻴﻘﺎﺕ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﻣﻲﻛﻨﺪ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
50 2001
61.9 Thinking a head (Critical question in ms therapy) 62.9 Understanding and Diagnosing Restless Legs Syndrome
ــــ
. ﺩﺭ ﺩﺳﺘﺮﺱ ﻣﻲﺑﺎﺷﺪPDF ﺁﺧﺮﻳﻦ ﺍﻃﻼﻋﺎﺕ ﻭ ﻳﺎﻓﺘﻪﻫﺎ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱ ﺳﻨﺪﺭﻡ ﭘﺎﻫﺎﻱ ﺑﻲﻗﺮﺍﺭ ﻭ ﺭﻭﺵﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﻣﺨﺘﻠﻒ ﺍﻥ ﺑﺤﺚ ﺷﺪﻩ ﻭ ﺑﻪ ﺻﻮﺭﺕ ﻓﺎﻳﻞﻫﺎﻱ. ﻃﺮﺍﺣﻲ ﻭ ﺍﺟﺮﺍ ﺷﺪﻩ ﺍﺳﺖRLS Foundation ﻛﻪ ﺗﻮﺳﻂ ﻫﻴﺌﺖ ﻋﻠﻤﻲCD ﺩﺭ ﺍﻳﻦ . ﻳﺎﻓﺖ ﻣﻲﺷﻮﺩCD ﻫﻤﭽﻨﻴﻦ ﻳﻚ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺩﺭﺑﺎﺭﺓ ﺍﻳﻦ ﺳﻨﺪﺭﻡ ﻭ ﺗﻈﺎﻫﺮﺍﺕ ﺑﺎﻟﻴﻨﻲ ﺁﻥ ﻭ ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﻣﺨﺘﻠﻒ ﻧﻴﺰ ﺩﺭ ﺍﻳﻦ ﺩﺍﺧﻠﻲ-١٠
CD ﻋﻨﻮﺍﻥ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ 2003
1.10 (AGA Postgraduate Course) A Day and Night in the Life of a Gastroenterologist
Esophagus and Stomach Liver Pancreas and Biliary Tract 3DClinic (Version 1.0) Seeing is Understanding 2.10
Nutrition
GI Malignancy
Small Bowel and Colon
Clinical Challenge Sessions ___
ﺷﻤﺎDesktop ( ﺑﺮ ﺭﻭﻱ2D Clinic) Icon . ﻛﻨﻴﺪRestart ﺳﭙﺲ ﺳﻴﺴﺘﻢ ﺭﺍ.( ﺭﺍ ﺑﻬﻤﺮﺍﻩ ﺍﺳﻢ ﺧﻮﺩ ﻭﺍﺭﺩ ﻧﻤﺎﻳﻴﺪSN: BI-B25600000-131) ﻣﻮﺟﻮﺩ ﺍﺳﺖ ﻧﺼﺐ ﻧﻤﻮﺩﻩ ﻭ ﺳﭙﺲ ﺩﺭ ﻗﺴﻤﺖ ﺩﻭﻡCD ﺭﺍ ﻛﻪ ﺩﺭQTS ﺍﺑﺘﺪﺍAutorun ﺟﻬﺖ ﻧﺼﺐ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﻌﺪ ﺍﺯ ﺷﺮﻭﻉ ﺑﺮﻧﺎﻣﻪ ﺑﻪ ﺻﻮﺭﺕ - ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻋﻜﺲﻫﺎ ﻭ ﻓﻴﻠﻢﻫﺎﻱ ﺳﻪﺑﻌﺪﻱ ﺟﺬﺍﺏ ﻣﻔﺎﻫﻴﻢ ﻣﺨﺘﻠﻒ ﻣﺮﺑﻮﻁ ﺑﻪ ﺳﻴﺴﺘﻢﻫﺎﻱ ﻣﺨﺘﻠـﻒ ﺑـﺪﻥ ﺍﺯ ﺟﻤﻠـﻪ. ﺑﻌﺪ ﺍﺯ ﻧﺼﺐ ﺑﺮﻧﺎﻣﻪ ﺑﻪ ﻃﻮﺭ ﻛﺎﻣﻞ ﺩﺭ ﻛﺎﻣﭙﻴﻮﺗﺮ ﺣﻔﻆ ﺧﻮﺍﻫﺪ ﺷﺪ. ﻛﻪ ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﻭ ﺍﺟﺮﺍﻱ ﺁﻥ ﻣﻨﻮﻱ ﺍﺻﻠﻲ ﻇﺎﻫﺮ ﻣﻲﺷﻮﺩ.ﻇﺎﻫﺮ ﺧﻮﺍﻫﺪ ﺷﺪ ﻛﻪ ﺑﻪ ﺍﻧﺘﺨﺎﺏ ﺷﻤﺎ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ3D ﻓﻴﻠﻢﻫﺎﻱ. ﻧﺸﺎﻥ ﻣﻲﺩﻫﺪDisorder ﻭHealthy ﺭﺍ ﺩﺭ ﺩﻭ ﺣﺎﻟﺖGastrointestinal -Musculoskeletal -Respiratory -Nervous -Urinary -Sensory -Endocrine -Lymphatic -Skin ﺍﺿﺎﻓﻪﻛﺮﺩﻥ ﻧﻜﺎﺕ ﻣﻬﻢ ﺑﺎ ﻣﺎﺭﻛﺮ ﻭ ﻧﻴﺰ ﺗﺎﻳﭗ ﺑﺮ ﺭﻭﻱ ﻋﻜﺲﻫﺎ ﺍﺯ ﻗﺎﺑﻠﻴﺖﻫﺎﻱ ﺟﺎﻟﺐ ﺍﻳـﻦ، ﻗﺎﺑﻠﻴﺖ ﻧﮕﻬﺪﺍﺷﺘﻦ ﻓﻴﻠﻢ ﺩﺭ ﻟﺤﻈﻪ ﺩﻟﺨﻮﺍﻩ.ﻣﻲﺷﻮﻧﺪ ﻗﺴﻤﺖﻫﺎﻱ ﺑﺴﻴﺎﺭ ﺟﺎﻟﺐ ﻭ ﺁﻣﻮﺯﻧﺪﻩﺍﻱ ﺍﺯ ﺳﻴﺴﺘﻢﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺩﺭ ﺣﺎﻟﺖ ﻧﺮﻣﺎﻝ ﻭ ﺑﻴﻤﺎﺭﻱ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ ﻛﻪ ﺑﻪ ﺩﺭﻙ ﺑﻬﺘﺮ ﻣﻮﺿﻮﻉ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﻣﻲﻧﻤﺎﻳﺪ . ﺷﻤﺎ ﺩﺭ ﺻﻮﺭﺕ ﺗﻤﺎﻳﻞ ﻣﻲﺗﻮﺍﻧﻴﺪ ﭘﺮﻳﻨﺖ ﻭ ﺍﺳﻼﻳﺪ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺗﻬﻴﻪ ﻓﺮﻣﺎﺋﻴﺪ.ﻧﺮﻡﺍﻓﺰﺍﺭ ﻣﻲﺑﺎﺷﺪ
-Cardiovascular
3.10 Adult Airway Management Principles & Techniques American Association
ــــ
(afael A. Ortega, M.D., Harold Arkoff, M.D.)
4.10 Advanced Therapy of INFLAMMATORY BOWEL DISEASE (Theodore M. Bayless, MD, Stephen B. Hanauer, MD) 5.10 AGA Postgraduate Course CONTROVERSIES And CLINICAL CHALLENGES in Pancreatic Diseases
2001 ــــ
(An Intensive Two-Day Course Covering A Diversity of Topics Related to the Pancreas)
6.10
-Expanded Content -Includes Results of the Q&A -Section Challenge Sessions Atlas of GASTROINTESTINAL in Health and Disease (Marvin M. Schuster, Michael D. Crowell, Kenneth L. Koch) Part 1: Physiologic Basis of Gastrointestinal Motility
Part 2: Motility Test for the Gastrointestinal Tract 2002
7.10 Atlas of GASTROINTESTINAL MOTILITY in Health and Disease (Second Edition) (Marvin M. Schuster, MD, FACP, FAPA, FACG, Michael D. Crowell, PhD, FACG, Kenneth L. Koch, MD)
Part I: Physiologic Basic of Gastrointestinal Motility Part II: Motility Tests for The Gastrointestinal Tract 8.10 Atlas of Clinical Oncology Soft Tissue Sarcomas American Cancer Sosiety (Raphael E. Pollock, MD, Phd) 9.10 Atlas of Clinical Oncology Cancer of the Lower Gastrointestinal Tract (Christopher G. Willett, MD) nd 10.10 Atlas of Clinical Rheumatology (2 Edition) (David J. Nashel, Chief, Rheumatology Section Va Medical Center, Washington, Professor of Medicine Georgetown University)
2002 2001
11.10 CANCER Principles & Practice of Oncology
ــــــ
1. Clinical Atlas of Rheumatic Diseases 2. Radiograph Intrerpretation Instructional Module
3. Physical Examination 4. Procures
5. Physical Findings Instructional Module Radiography 6. Aspiration/Injection Instructional Module
(6th Edition) (Vincent T. DeVita, Jr., Samuel Hellman, Steven A. Rosenberg)
ــــــ
12.10 Case Studies in GASTROENTEROLOGY (Second Edition) (Ingram Roberts, MD)
ــــــ
13.10 CD-ATLAS OF DIAGNOSTIC ONCOLOGY
ــــــ
14.10 Clinical Endocarinology Adrenals
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(G. Michael Besser MD, DSc, FRCP, Michael O. Thorner MB BS, DSc, FRCP) Gonads
Growth
Hormone Assay
ــــــ
Imaging Techniques
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
Pancreas
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
51 Ectopic Humoral Syndromes Gastrointestinal Tract Lipids and Lipoproteins Thyroid & Parathyroide Pituitary and Hypothalamus 15.10 Clinical Immunology PRINCIPLES AND PRACTICE (Second Edition) (Robert R Rich, Thomas A Fleisher, William T Shearer, Brain L Kotzin, Harry W Schroeder)
: ﺑﺨﺶ ﻣﻲﺑﺎﺷﺪ١١ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ. ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖRich ﻧﻮﺷﺘﺔ ﺩﻛﺘﺮClinical Immunology ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺮﺍﺳﺎﺱ ﻛﺘﺎﺏ ﺭﻭﺷﻬﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺩﺭ ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻱ-٧ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻳﻜﻲ-٦ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺁﻟﺮﮊﻳﻜﻲ-٥ ﺳﻴﺴﺘﻢ ﺩﻓﺎﻋﻲ ﺫﺍﺗﻲ ﻭ ﺍﻛﺘﺴﺎﺑﻲ-٤ ﻋﻔﻮﻧﺖ ﻭ ﺳﻴﺴﺘﻢ ﺍﻳﻤﻨﻲ-٣ ﻣﻜﺎﻧﻴﺴﻢﻫﺎﻱ ﺩﻓﺎﻋﻲ ﻣﻴﺰﺑﺎﻥ ﻭ ﺍﻟﺘﻬﺎﺏ- ٢ ﺍﺻﻮﻝ ﺗﺸﺨﻴﺼﻲ ﺍﻳﻤﻨﻲ-١ Slide ﻫﺮ ﺍﺳﻼﻳﺪ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﺩﺭ ﻳﻚ ﻓﺎﻳﻞ )ﺗﺤﺖ ﺑﺮﻧﺎﻣﺔdrag & drop ﺑﺎ ﺭﻭﺵ. ﻭﺍﮊﻩ ﻭ ﻟﻐﺎﺕ ﺭﺍ ﺩﺍﺭﺳﺖ ﻭ ﻧﻴﺰ ﺗﺼﺎﻭﻳﺮ ﻭ ﺍﺳﻼﻳﺪﻫﺎ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﭼﺎﭖ ﻧﻤﻮﺩSearch ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻗﺎﺑﻠﻴﺖ. ﺍﺳﻼﻳﺪﻫﺎﻱ ﻣﺘﻌﺪﺩﻱ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺢ ﺍﺭﺍﺋﻪ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ،ﺩﺭ ﻫﺮﺑﺨﺶ . ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩSlide vision ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ ﻭ ﺗﺤﺖAutorun ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ. ﻫﻤﭽﻨﻴﻦ ﻣﻲﺗﻮﺍﻥ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺩﻳﮕﺮﻱ ﺭﺍ ﺑﻪ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺿﺎﻓﻪ ﻳﺎ ﺣﺬﻑ ﻛﺮﺩ. ( ﺫﺧﻴﺮﻩ ﻭ ﻧﮕﻬﺪﺍﺭﻱ ﻧﻤﻮﺩvision
ــــــ
16.10 CLINICAL ONCOLOGY (Raymond E. Lenhard, J. MD, Robert T. Osteen, MD, Ted Gansler, MD)
2001
17.10 Comprehensive Clinical Endocrinology G. Michael Besser MD, DSc, FRCP, Michael O. Thorner
2000
Hypothalamus and Pituitary, Thyroid, Adrenal, Control of Blood glucose and its disturbance, gonad and growth, General conditions-basic, General conditionsclinical, Imaging, Patient Perspectives on endocrine Diseases 18.10 COMPREHENSIVE MANAGEMENT OF Chronic Obstructive Pulmonary Disease (Jean Bourbeau, MD, MSc, FRCPC, Diane Nault, RN, MSc, Elizabet Borycki)
2002
19.10 Core Curriculum in Primary Care Metabolic Diseases Section
ــــــ
20.10 Digestive Diseases
ــــــ
. ﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖHarvard ﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲCD ﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯCCC ﺳـﺆﺍﻻﺕ ﻣﺮﺑﻮﻃـﻪ ﺑـﻪ ﺻـﻮﺭﺕ، ﺩﺭ ﺁﺧـﺮ ﻫـﺮ ﺳـﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜـﻲ. ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛـﺎﺭﺑﺮ ﻣـﻲﺑﺎﺷـﺪ. ﺣﺎﺿﺮ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱ ﺩﺍﺧﻠﻲ ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖCD . ﺑﻪ ﺻﻮﺭﺕ ﺩﺭﺳﻨﺎﻣﻪ ﺁﻣﻮﺯﺷﻲ ﻣﻮﺟﻮﺩ ﺍﺳﺖCD ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺩﺭ. ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﻘﺎﻟﻪ ﭼﺎﭘﻲ ﺩﺭ ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ.ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻣﺘﺎﺑﻮﻟﻴﺴﻢ ﺁﻫﻦ-٤ ( ﻧﮕﺮﺷﻲ ﻋﻤﻠﻲ )ﻗﺴﻤﺖ ﺩﻭﻡ: ﺩﻳﺎﺑﺖ ﻣﻠﻴﺘﻮﺱ-٣ ( ﻧﮕﺮﺷﻲ ﻋﻤﻠﻲ )ﻗﺴﻤﺖ ﺍﻭﻝ: ﺩﻳﺎﺑﺖ ﻣﻠﻴﺘﻮﺱ-٢ ﻫﺎ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕLipid -١ Self-Education Program
21.10 Diseases of the Liver
(A Core Curriculum and Self-Assessment in Gastroenterology and Hepatology)
(8th Edition) (Lippincott Williams & Wilkins)
General Considerations Autoimmune Liver Disease The Liver in Pregnancy and Childhood
The Consequences of Liver Disease Alcohol and Drug-Luduced Disease Infections and Granulomatous Disorders
ــــــ The Cholestasis Disorders Genetic and Metabolic Disease Transplantation
Viral Hepatitis Vascular Disease and Trauma Benign and Malignant Tumors
Immunology of Liver
26.1 EBUS
Endo Bronchial Ultrasound (Heinrich D. Becher, MD. Fccp) - Basic Introduction -Bronchial Anatomy -Interactive Sonography -Product Information
22.10 ESAP
(Endocrinology Self-Assessment Program)
ــــــ
(Clark T. Sawin, MD, Kathryn A. Martin, MD) (The Endocrine Society)
23.10 Evidence-Based Asthma Management PATHOPHYSIOLOGY/DIAGNOSIS/MANAGEMENT (7
TH
edition)
2003 2001
ﺁﺳﻢ ﻳﻚ ﺑﻴﻤﺎﺭﻱ ﺷﺎﻳﻊ ﭘﺰﺷﻜﻲ ﺍﺳﺖ ﻛﻪ ﺷـﻴﻮﻉ ﺭﻭ. ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻣﺘﺨﺼﺼﻴﻦ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ﺗﺎ ﺑﻬﺘﺮﻳﻦ ﺩﺭﻣﺎﻥ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﺩﺭﻳﺎﻓﺖ ﺷﺨﺼﻲ ﺧﻮﺩ ﺍﺯ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺩﺭﻣﺎﻥﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ ﻣﻘﺎﻻﺕ ﻭ ﻛﺘﺎﺏﻫﺎ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﺮﺩﻩ ﻭ ﺑﻪ ﻛﺎﺭ ﺑﺮﺩEvidence-Based in medicin ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺯ ﺳﺮﻱ ﻛﺘﺎﺏﻫﺎﻱ . ﺁﻣﺎﺭﮔﻴﺮﻱﻫﺎ ﻭ ﻣﻄﺎﻟﻌﺎﺕ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻛﻪ ﺍﻓﺰﺍﻳﺶ ﺷﻴﻮﻉ ﺁﺳﻢ ﻭﺍﻗﻌﻲ ﺑﻮﺩﻩ ﻭ ﺑﺎ ﺍﺯ ﻛﺎﺭﺍﻓﺘﺎﺩﮔﻲ ﺑﻴﻤﺎﺭ ﻫﻤﺮﺍﻩ ﺑﻮﺩﻩ ﻛﻪ ﻧﺸﺎﻥﺩﻫﻨﺪﻩ ﺩﺭﻣﺎﻥ ﺗﺎ ﻛﺎﻣﻞ ﺍﻳﻦ ﺑﻴﻤﺎﺭﺍﻥ ﺍﺳﺖ.ﺑﻪ ﺍﻓﺰﺍﻳﺶ ﺩﺍﺭﺩ : ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺣﺎﺿﺮ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ.ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺎ ﺁﻭﺭﺩﻥ ﻣﻘﺎﻻﺕ ﺑﺮ ﺍﺳﺎﺱ ﻣﻌﺘﺒﺮﺑﻮﺩﻥ ﻭ ﺩﺭﺟﻪﺑﻨﺪﻱ ﺍﻋﺘﺒﺎﺭ ﻣﻘﺎﻻﺕ ﭘﺰﺷﻚ ﻣﺘﺨﺼﺺ ﺭﺍ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ﺗﺎ ﺩﺭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱ ﺁﺳﻢ ﺑﻬﺘﺮﻳﻦ ﻭ ﻛﻢﻋﺎﺭﺿﻪﺗﺮﻳﻦ ﺩﺭﻣﺎﻥ ﺭﺍ ﺑﺮﺍﻱ ﻫﺮ ﺑﻴﻤﺎﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﺪ 1. Natural History and Epidemiology 2. Diagnosis 3. Role of Childhood Infection 4. Management of Persistent Asthma in Childhood 5. Use of Theophylline and Anticholinergic Therapy 6. Leukotriene Modifiers 7. Acute Life-Threatening Asthma 8. Role of Asthma Education
9. Genetics of Asthma 10. Role of the Outdoor Environment 11. Diagnosis and Management of Occupational Asthma 12. Mechanisms of Action of 2-Agonists and Short-Acting 2 Therapy 13. Environmental Control and Immunotherapy 14. Alternative Anti-inflammatory Therapies 15. Management of Asthma in the Intensive Care Unit 16. Asthma Unresponsive to Usual Therapy
17. Cellular and Pathologic Characteristics 18. Role of Indoor Aeroallergens 19. Principles of Asthma Management in Adults 20. Role of Long-Acting 2-Adrenergic Agents 21. Role of Inhaled Corticosteroids 22. Exercise-Induced Bronchoconstriction 23. Severe Acute Asthma in Children 24. Measures of Outcome
24.10 EVIDENCE-BASED DIABETES CARE (Hertzel C. Gerstein, MD, R. Brain Haynes, MD,) 1- EVIDENCE 2- DEFINITION AND IMPORTANCE OF DIABETES MELLITUS 3- ETIOLOGIC CLASSIFICATION OF DIABETES
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2001
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
52 4- PREVENTION AND SCREENING FOR DIABETES MELLITUS
5- LONG-TERM CONSEQUENCES OF DIABETES
6- DELIVERY OF CARE
2001
25.10 EVIDENCE-BASED Diagnosis: A Handbook of Clinical Prediction Rules (Mark Ebell, MD, MS) (Springer-Verlag)
-Cardiovascular Diseases -Endocrinology -Gastroenterology -Gynecology and Obstetrics -Hematology/Oncology -Musculoskeletal -Neurology -Pulmonary Diseas -Renal Disease -Surgery and Trauma
-Infectious Disease 2000
26.10 Gastric Cancer Diagnosis and Treatment (An interactive Training Program) (J.R. Siewert, D.Kelsen, K. Maruyama) (Springer) 27.10 Gastroenterology
ــــ
Endoscopy (2nd Edition)
2002
th 28.10 Gastrointestinal and Liver Disease Pathophysiology/Diagnosis/Management (7 edition) (Sleisenger & Fordtran's)
Esophagus Pancreas
Liver Biliary tract
Nutrition in gastroenterology Approach to patients with symptoms and signs
Topics involving multiple organs Small and Large Intestine
Biology of the Gastrointestinal Tract and Liver Vasculature and Supporting Structures
Stomach and duodenum Psychosocial
29.10 HARRISON'S 15 McGraw-Hill presents
ــــ 1998
32.1 Imaging of Diffuse Lung Disease (David A. Lynch, MB, John D. Newell Jr, MD, FCCP, Jin Seong Lee, MD)
: ﺑﻌﻀﻲ ﻓﺼﻮﻝ ﻛﺘﺎﺏ ﺷﺎﻣﻞ.( ﺩﺭ ﺍﻃﻔﺎﻝ ﻭ ﺑﺎﻟﻐﻴﻦ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﻨﺘﺸﺮ ﺭﻳﻪ ﻣﻲﺑﺎﺷﺪ.... ﻭMRI,CT-Xray) ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ ﺗﻔﺴﻴﺮ ﻋﻜﺲﺑﺮﺩﺍﺭﻱ، ﺷﺮﺡ ﺣﺎﻝ، ﻛﻪ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﺷﺎﻣﻞ ﺗﻠﻔﻴﻘﻲ ﺍﺯ ﻣﻌﺎﻳﻨﻪ.( ﻣﻲﺑﺎﺷﺪDLN) ﻓﺼﻞ ﺍﺯ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﻨﺘﺸﺮ ﺭﻳﻪ١١ ﺣﺎﺿﺮ ﺷﺎﻣﻞCD ﺍﺭﺯﻳﺎﺑﻲ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺑﻴﻤﺎﺭﻫﺎﻱ ﺭﻳﻪ ﺁﻧﻬﺎ ﺑﻪ ﻃﻮﺭ ﻣﺠﺰﺍ ﻣﻲﺑﺎﺷﺪX-Ray,CT ﻭ ﻣﻘﺎﻳﺴﻪDLD ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ
DLDﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﻐﻠﻲ ﻭ ﻣﺤﻴﻄﻲ ﻭ
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺭﺍﻫﻬﺎﻱ ﻫﻮﺍﺋﻲ
ﭘﻴﻮﻧﺪ ﺭﻳﻪ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺁﻣﻔﻴﺰﻡ
ﺗﺼﻮﻳﺮ ﺑﺮﺩﺍﺭﻱ ﻋﺮﻭﻕ ﺭﻳﻮﻱ ﻛﻮﺩﻛﺎﻥDLD ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻧﻔﻴﻠﺘﺮﺍﺗﻴﻮ ﺭﻳﻪ
. ﻗﻠﺐ ﻭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻣﻲﺩﻫﺪ، ﺭﻳﻪ، ﺑﻮﺩﻩ ﻭ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﻧﮕﺎﻫﻲ ﺟﺪﻳﺪ ﺑﻪ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎﻱ ﺩﺍﺧﻠﻲAcrobat Reader ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ ﺑﺮﻧﺎﻣﻪ 30.10 INFECTIOUS DISEASES
(W Edmund Farrar, Martin J Wood, John A Innes, Hugh Tubbs)
The Head and Neck The Urinary Tract Vira, Fungal and Ectoparasitic Infections
Lower Respiratory Tract The Genital Tract The Eye
The Nervous System Bones and Joints Systemic Infections
ــــ
The Gastrointestinal Tract The Cardiovascular System HIV Infection and Aids
The liver and Biliary Tract Bacterial Infections Acknowledgements
31.10 Menopausal Osteoporosis (Neill Musselwhlte, M.D., Herman Rose, M.D.)
ﺳﺆﺍﻻﺕ ﺟﺪﻳﺪ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ ﺯﻣﻴﻨﻪ-٦
ﺍﺳﺘﺌﻮﭘﺮﻭﺯ-٥
ــــــ : ﻣﻄﺎﻟﺐ ﺟﺎﻟﺒﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﻨﻮﭘﻮﺯ ﻭ ﺍﺳﺘﺌﻮﭘﺮﻭﺯ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻋﻨﺎﻭﻳﻦ ﺁﻥ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺩﺭ ﺍﻳﻦ ﻧﮕﺮﺍﻧﻲﻫﺎﻱ ﺑﻴﻤﺎﺭﻳﺎﻥ-٣ ﺭﻭﺵ ﺟﻠﻮﮔﻴﺮﻱ ﺍﺯ ﻋﻮﺍﺭﺽ ﺁﻥ-٢ ﻣﻨﻮﭘﻮﺯ ﻭ ﻧﺤﻮﺓ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺁﻥ-١
Impact of osteobrosis -٤
2001
32.10 MKSAP® 12 (American College of Physiciance-American Sosiety Internal Medicine)
: ﺷﺎﻣﻞCD ﻋﻨﺎﻭﻳﻦ ﻣﻮﺭﺩ ﺑﺤﺚ ﺍﻳﻦ -Gastroenterology and Hepatology - Endocrinology and Metabolism -Infectious Disease Medicine - Rheumatology -Neurology
- Dermatology - Nephrology -Hospital-Based Medicine and Critical Care
- Oncology
- Hematology
- Cardiovascular Medicine
- Pulmonary Medicine
- Ambulatory Medicine
33.10 Oxford Textbook of Medicine (OTM) (Weatherall, Ledingham, Weatherall) ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻳﻚ ﻣﻨﺒﻊ ﻭ ﻣﺮﺟﻊ ﻗﻮﻱ ﺑﻪ ﻣﻨﻈﻮﺭ ﻣﺸﺎﻭﺭﻩ ﺩﺭ ﻣﻌﺎﻳﻨـﺎﺕ ﺭﻭﺯﻣـﺮﻩ ﻭ ﭘﺎﺳـﺦ. ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﻋﻠﻮﻡ ﭘﺎﻳﻪ ﻭ ﻣﻬﺎﺭﺗﻬﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﻃﺐ ﺩﺍﺧﻠﻲ ﻭ ﺗﺨﺼﺺﻫﺎﻱ ﻭﺍﺑﺴﺘﻪ ﺭﺍ ﺩﺭﺑﺮ ﻣﻲﮔﻴﺮﺩCD ﺍﻳﻦ. ﺗﺼﻮﻳﺮ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ٢٥٠٠ ﺻﻔﺤﻪ ﻭ٥٠٠ ﻓﺼﻞ ﺩﺭ٣٣ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻣﺸﺘﻤﻞ ﺑﺮ : ﺍﺯ ﻣﺰﻳﺖﻫﺎﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺷﺎﺭﻩ ﻛﺮﺩ. ﻣﻘﺎﻟﻪﻧﻮﻳﺲ ﻭ ﻣﺤﻘﻖ ﻣﻌﺘﺒﺮ ﺩﺭ ﺳﺮﺗﺎﺳﺮ ﺟﻬﺎﻥ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ٥٨٠ ﺩﺭ ﻧﻮﺷﺘﻦ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺍﺯ. ﻣﻲﺑﺎﺷﺪ،ﺳﺆﺍﻻﺗﻲ ﻛﻪ ﺧﺎﺭﺝ ﺗﺨﺼﺺ ﭘﺰﺷﻜﺎﻥ ﻣﻄﺮﺡ ﻣﻲﺷﻮﺩ ﺩﺭ. ﺑﻴﻤﺎﺭﻳﻬـﺎﻱ ﻣﻘـﺎﺭﺑﺘﻲ، ﻣﻌﺎﻟﺠﺎﺕ ﺩﻭﺭﻩﺍﻱ، ﭘﺰﺷﻜﻲ ﭘﻴﺮﻱ، ﭘﺰﺷﻜﻲ ﻗﺎﻧﻮﻧﻲ، ﭘﺰﺷﻜﻲ ﻭﺭﺯﺷﻲ. ﺑﻴﺸﺘﺮ ﻣﻔﺎﻫﻴﻢ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻋﻔﻮﻧﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﺩﺭﺳﻨﺎﻣﻪ ﭘﺰﺷﻜﻲ ﺭﺍ ﭘﻮﺷﺶ ﻣﻲﺩﻫﺪ. ﺩﺍﻣﻨﺔ ﻣﺒﺎﺣﺚ ﻭ ﻣﻮﺿﻮﻋﺎﺕ ﺍﺯ ﻗﺒﻞ ﻭﺳﻴﻊﺗﺮ ﺷﺪﻩ ﺍﺳﺖ.ﮔﺮﺩﺁﻭﺭﻱ ﻏﻴﺮﺗﻜﺮﺍﺭﻱ ﻣﺒﺎﺣﺚ ﻋﻠﻮﻡ ﭘﺎﻳﻪ ﻭ ﻋﻠﻮﻡ ﺑﺎﻟﻴﻨﻲ . ﻣﻮﺭﺩ ﺑﺤﺚ ﺩﻗﻴﻖ ﻭ ﻣﻮﺷﻜﺎﻓﺎﻧﻪ ﻗﺮﺍﺭ ﻧﮕﺮﻓﺘﻪ ﺍﺳﺖ، ﺍﺧﺘﻼﻻﺕ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﻋﺘﻴﺎﺩ ﻭ ﺭﻭﺍﻥﭘﺰﺷﻜﻲ ﺩﺭ ﻣﻌﺎﻳﻨﺎﺕ ﻋﻤﻮﻣﻲ، ﺗﻐﺬﻳﻪ، ﺑﻬﺪﺍﺷﺖ ﻣﺤﻴﻂ ﻭ ﻣﺸﺎﻏﻞ. ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺑﺎﺭﺩﺍﺭﻱ،CD ﺍﻳﻦ ﻗﺪﺭﺕ ﺗﻐﻴﻴﺮ ﺍﻧﺪﺍﺯﺓ ﻗﻠﻤﻬﺎﻱ ﻣﺘﻮﻥ ﻭ ﭼﺎﭘﮕﺮ ﻭ ﻧﻴﺰ ﻗﺪﺭﺕ ﭼﺎﭖ ﻣﺘﻦ ﻭ ﺟﺴﺘﺠﻮﻱ ﻛﻠﻤـﺎﺕ ﻭ ﻭﺍﮊﻩﻫـﺎﻱ ﺗﺨﺼﺼـﻲ ﻭ ﺩﺳﺘﺮﺳـﻲ ﺁﺳـﺎﻥ ﺑـﻪ. ﺭﺍ ﻧﻴﺰ ﺟﺪﺍﮔﺎﻧﻪ ﻣﺸﺎﻫﺪﻩ ﻧﻤﻮﺩCD ﻛﻪ ﻣﻲﺗﻮﺍﻥ ﺗﻤﺎﻣﻲ ﺗﺼﺎﻭﻳﺮ، ﻫﺮ ﻓﺼﻞ ﺩﺍﺭﺍﻱ ﺗﺼﺎﻭﻳﺮﻱ ﻣﻲﺑﺎﺷﺪ. ﻣﻨﺎﺑﻊ ﺁﻥ ﻗﻴﺪ ﺷﺪﻩ ﺍﺳﺖ،ﺩﺭ ﭘﺎﻳﺎﻥ ﻫﺮ ﻓﺼﻞ ﻛﺘﺎﺏ . ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖCD ﺳﺆﺍﻻﺕ ﭼﻨﺪﮔﺰﻳﻨﻪﺍﻱ )ﻛﻪ ﺑﺼﻮﺭﺕ ﺟﺪﺍﮔﺎﻧﻪ ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ( ﻭ ﻓﻬﺮﺳﺖ ﺗﻔﺼﻴﻠﻲ ﺍﺯ ﻣﻨﺪﺭﺟﺎﺕ ﻛﺘﺎﺏ ﻧﻴﺰ ﺩﺭ ﺍﻳﻦ.ﺟﺪﺍﻭﻝ ﻭ ﺗﺼﺎﻭﻳﺮ ﺍﺯ ﻭﻳﮋﮔﻲﻫﺎﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺳﺖ
ــــ
34.10 Pre-Colonoscopy Education Program (Dr. Michael Shaw, Dr. Oliver cass Dr. James Reynolds Patricia Tomshine, Rn)
ــــ
- Reason for Colonoscopy
- The Colon and The Colonoscope
35.10 Principles & Practice of Infectious Diseases
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
- Preparations - Day of the Procedure
- About the Procedure -After the Procedur - Minor Complicaions
A Harcourt Health Sciences Company
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
- Major Complications
2000 ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
53 : ﺷﺎﻣﻞ ﺳﻪ ﺑﺨﺶ ﺍﺻﻠﻲ ﺍﺳﺖCD ﺍﻳﻦ. ﻭ ﺷﺎﻣﻞ ﺗﻤﺎﻣﻲ ﻣﻔﺎﻫﻴﻢ ﺍﺳﺎﺳﻲ ﻭ ﺟﺎﺭﻱ ﺩﺭ ﻣﻴﻜﺮﻭﺑﻴﻮﻟﻮﮊﻱ ﻭ ﺩﺭﻣﺎﻥ ﻋﻮﺍﺭﺽ ﻋﻔﻮﻧﻲ ﺍﺳﺖ. ﺗﺼﻮﻳﺮ ﻣﻲﺑﺎﺷﺪ٨٠٠ ﺟﺪﻭﻝ ﻭ٨٠٠ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻫﻤﺮﺍﻩ ﺑﺎ ﺑﻴﺶ ﺍﺯCD ﺍﻳﻦ 1- Browse Mandell, Douglas & Bennett s .ﻛﻪ ﻣﺘﻦ ﺍﺻﻠﻲ ﻛﺘﺎﺏ ﺭﺍ ﺷﺎﻣﻞ ﻣﻲﺷﻮﺩ 2- Subject index Search: .ﺑﺮ ﺍﺳﺎﺱ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎ ﻭﺍﮊﻩﻫﺎﻱ ﺗﺨﺼﺼﻲ ﺭﺍ ﭘﻴﺪﺍ ﻧﻤﻮﺩ ﻭ ﺑﻪ ﻓﺼﻞ ﻭ ﻣﺒﺎﺣﺚ ﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻥ ﺩﺭ ﻛﺘﺎﺏ ﻣﻨﺘﻘﻞ ﺷﺪ 3- Help ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖCD ﻃﺮﻳﻘﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ، ﻋﺮﻭﻗﻲ- ﻋﻔﻮﻧﺖﻫﺎﻱ ﺩﺳﺘﮕﺎﻩ ﻗﻠﺒﻲ، ﻋﻔﻮﻧﺘﻬﺎﻱ ﺑﺮﻭﻧﺸﻴﻮﻟﻬﺎ، ﻋﻔﻮﻧﺘﻬﺎﻱ ﻓﻮﻗﺎﻧﻲ ﺗﻨﻔﺴﻲ،( ﻋﻼﺋﻢ ﻭ ﻧﺸﺎﻧﻪﻫﺎﻱ ﻛﻠﻴﻨﻴﻜﻲ )ﺗﺐ٢ ( ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ﺭﻭﺷﻬﺎﻱ ﺩﺭﻣﺎﻧﻲ، ﻣﻜﺎﻧﻴﺰﻡﻫﺎﻱ ﺩﻓﺎﻋﻲ ﻣﻴﺰﺑﺎﻥ،( ﺍﺻﻮﻝ ﺍﻭﻟﻴﻪ ﺩﺭ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻋﻔﻮﻧﻲ )ﻋﻮﺍﻣﻞ ﻣﻴﻜﺮﻭﺑﻲ١ (... ﺟﺮﺍﺣﻲ ﻭ ﻋﻔﻮﻧﺘﻬﺎﻱ ﺗﺮﻭﻣﺎ ﻭ، ﻋﻔﻮﻧﺘﻬﺎﻱ ﻣﻴﺰﺑﺎﻧﻬﺎﻱ ﺧﺎﺹ، )ﻋﻔﻮﻧﺘﻬﺎﻱ ﺑﻴﻤﺎﺭﺳﺘﺎﻧﻲ،Special problems (٤ (.... ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﻴﻮﭘﻼﺳﻢﻫﺎ ﻭ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﭘﺮﻳﻮﻥﻫﺎ،( ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻋﻔﻮﻧﻲ ﻭ ﻋﻮﺍﻣﻞ ﻭ ﻋﻠﻞ ﺁﻧﻬﺎ )ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻭﻳﺮﻭﺳﻲ٣ (....... ﻋﻔﻮﻧﺘﻬﺎﻱ ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﻭ .( ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﻧﺪCD ﻗﺎﺑﻞ ﺍﺟﺮﺍ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻫﻨﮕﺎﻡ ﻧﺼﺐ ﺁﻥ ﺑﺮ ﺭﻭﻱ ﻛﺎﻣﭙﻴﻮﺗﺮ ﺷﻤﺎ )ﺍﺯ ﻃﺮﻳﻖJava VM ﻭinternet explver ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﺤﺖ 36.10 Rheumatology (John H. Klippel.Paul A Dieppe)
-Rheumatic Diseases -Regional Pain Problems
-Signs and Symptoms -Connective Tissue Disorders
37.10 TEXTBOOK OF Gastroenterology (Third Edition)
-Rheumatoid Arthritis and Spondylopathy -Disorders of Bone, Cartilage
ــــ
-Infection and Arthritis -Management of Rheumatic Disease
ــــ
ATLAS OF Gastroenterology (Second Edition) (David H. Alpers, MD, Loren Laine, MD)
2001
38.10 Textbook of Rheumatology (Kelley's) (W.B. Saunders Company) Section I BIOLOGY OF THE NORMAL JOINT Section III EVALUATION OF THE PATIENT Section V DIAGNOSTIC TESTS AND PROCEDURES Section VII CLINICAL PHARMACOLOGY Section IX SPONDYLOARTHROPATHIES Section XI VASCULITIC SYNDROMES Section XIII STRUCTURE, FUNCTION, AND DISEASE OF MUSCLE Section XV CRYSTAL-ASSOCIATED SYNOVITIS Section XVII ARTHRITIS RELATED TO INFECTION Section XIX DISORDERS OF BONE AND STRUCTURAL PROTEIN Section XXI RECONSTRUCTIVE SURGERY FOR RHEUMATIC DISEASE
Section II IMMUNE AND INFLAMMATORY RESPONSES Section IV MUSCULOSKELETAL PAIN AND EVALUATION Section VI SPECIAL ISSUES Section VIII RHEUMATOID ARTHRITIS Section X SYSTEMIC LUPUS ERYTHEMATOSUS AND RELATED SYNDROMES Section XII SCLERODERMA AND MIXED CONNECTIVE TISSUE DISEASES Section XIV RHEUMATIC DISEASES OF CHILDHOOD Section XVI OSTEOARTHRITIS, POLYCHONDRITIS, AND HERITABLE DISORDERS Section XVIII ARTHRITIS ACCOMPANYING SYSTEMIC DISORDERS Section XX TUMORS INVOLVING JOINTS
39.10 Textbook of TRAVEL MEDICINE and HEALTH (Herbert L. Dupont, M.D., Robert Steffen, M.D.) (B.C.DECKER INC)
57.9
ــــ
ﺩﺭ ﺯﻣﺎﻥ ﻣﺴﺎﻓﺮﺕ ﺑﻪ ﻣﻨﺎﻃﻖ ﻣﺨﺘﻠﻒ ﺍﻣﻜﺎﻥ ﺍﺑﺘﻼ ﺑﻪ ﺑﺮﺧﻲ ﺑﻴﻤﺎﺭﻳﻬﺎ ﺑﺎ ﺗﻮﺟﻪ ﺑـﻪ ﺷـﺮﺍﻳﻂ ﺍﭘﻴـﺪﻣﻴﻜﻲ ﻭ. ﻧﻮﺷﺘﻪ ﺷﺪﻩ ﺍﺳﺖSteffen ﻭ ﺩﻛﺘﺮDupont ﻭ ﺗﻮﺳﻂ ﺩﻛﺘﺮ. ﺻﻔﺤﻪ ﻣﻲﺑﺎﺷﺪ٣٧٠ ﻓﺼﻞ ﺩﺭ٣٤ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺍﺳﺖ ﻛﻪ ﺷﺎﻣﻞ ﺩﺭ ﻣﺴﺎﻓﺮﺍﻥ ﻣﺨﺘﻠﻒ ﺩﺭ ﻛﺸﻮﺭﻫﺎﻱ ﮔﻮﻧﺎﮔﻮﻥ ﻣﻮﺭﺩ ﺑﺤﺚ. . . ﺍﺛﺮﺍﺕ ﻭﺍﻛﺴﻴﻨﺎﺳﻴﻮﻥ ﻭ ﺁﻣﺎﺭ ﻣﺮﮒ ﻭ ﻣﻴﺮ ﻭ، ﺷﻴﻮﻩﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻧﺎﺷﻲ ﺍﺯ ﺣﻮﺍﺩﺙ. ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﻘﺎﺭﺑﺘﻲ ﺍﺯ ﺍﻳﻦ ﺟﻤﻠﻪ ﻫﺴﺘﻨﺪ، ﻭﺑﺎ، ﺍﻳﺪﺯ، ﺗﻴﻔﻮﺋﻴﺪ، ﻫﭙﺎﺗﻴﺖ، ﺑﻴﻤﺎﺭﻳﻬﺎﻳﻲ ﻣﺜﻞ ﻣﺎﻻﺭﻳﺎ.ﺍﻧﺪﻣﻴﻚ ﺑﻴﺸﺘﺮ ﻣﻲﺷﻮﺩ . ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖCD ﻭ ﺑﺮﺭﺳﻲ ﺩﺭ ﺍﻳﻦ
The Massachusetts General Hospital Handbook of Pain Management
(Second Edition)
(Jane Ballantyne, Scott M. Fishman, Salahadin Abdi) (SALEKAN-E-book)
ــــ
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﻗﺴﻤﺖﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺍﻳﻦ I. General Considerations II. Diagnosis of Pain III. Therapeutic Options: Pharmacologic Approaches IV. Therapeutic Options: Nonpharmacologic Approaches V. Acute Pain VI. Chronic Pain VII. Pain Due to Cancer VIII. Special Situations - Apendices - Subject Index
ــــ
40.10 UEGW Gastroenterology Week 10th United European (Geneva, Switzerland)
2003
41.10 UEGW IBS: Management not myth 1. IBS: the clinician's view
2. IBS: care, cost and consequences
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ 3. Diagnosis: identigy, Probe, eliminate
42.10 Upper GI Endoscopy An Interactive Aducasional Program
4. Tegaserod: a world of experience
Video Segments of Common Pathologics of the Upper Gl tract (Iencludes Educational text)
43.10 UpToDate CLINICAL REFERENCE LIBRARY 13.1 (CD I , II) (Burton D. Rose, MD, Joseph M. Rush, MD)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
5. Chairman's summary
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــ 2005
: ﺷﺎﻣﻞCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
54 Adult Primary Care Allwrgy and Immonology Cardiology Critical Care Drug Information Enodcrinoology Family Medicine Rheumatology Women's Health Gastroenterology Gynecology Hematology Infections Disease Nephrology Oncology Pediatrics Pulmonology
44.10 YEAR BOOK of RHEUMATOLOGY, ARTHRITI, AND MUSCULOSKELETAL DISEASE
TM
(Richrd S. Panush, MD) (SALEKAN E-BOOK)
Health Sciences, Epidemiology, Economics, & Arthritis Care
Systemic Lupus Erythematosus and Related Disorders
Rheumatoid Arthritis
Vasculitis and Systemic Rheumatic Diseases and Other Related Disorders
Systemic Selerosis and Related Disorders
Osteoarthritis, Crystal-Related Arthropathies, Osteoporosis, Infectious Arthritides, and Spondyloarthropathies
Regional Pain Syndromes, Non-Articular Musculoskeletal Disorders, and Fibromyalgia
Miscellaneous Topics
2003
ﺍﻃﻔﺎﻝ-١١
CD ﻋﻨﻮﺍﻥ 1.11 A Major Contributor to Neonatal Infant Morbidity and Mortality (SURVANTA) (Part I , II) (Alan J. Gold, MD, J. Harry Gunkel, Arvin M. Overbach) 2.11 Atlas of Pediatric Gastrointestinal Disease 3.11 Basic Mechanisms of Pediatric Respiratory Disease (Second Edition) (Gabriel G. Haddad,MD, Steven H. Abman, MD) Genetic and Developmental Biology of the Respiratory System Developmental Physiology of the Respiratory System 4.11 Child Development, 9/e (John W. Santrock) 18.9 CURRENT MANAGEMENT IN CHILD NEUROLOGY
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــ ــــ 2002
Structure-Function Relations of the Respiratory System During Development Inflammation and Pulmonary Defense Mechanisms (SECOND EDITION) (Bernrd L. Maria, MD, MBA)
Section 1: Clinical Practice Trends Section 2: The Office Visit Section 3: The Hospitalized Child 5.11 EVIDENCE-BASED PEDIATRICS (William Feldmam, MD, FRCPC) (B.C. Decker Inc.) 6.11 PEDIATRIC GASTROINTESTINAL DISEASE Pathophysiology . Diagnosis . Management (Third Edition) 7.11 TEXTBOOK OF NEONATAL RESUSCITATION (4TH EDITION MULTIMEDIA CD-ROM)
2001 2002 2000 ــــ ــــ
ﻋﻤﻮﻣﻲ:١٢
CD ﻋﻨﻮﺍﻥ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
1.12 1. Review for USMLE NMS® (Step 1) 2. Review for USMLE NMS® (Step 2) 3. Review for USMLE NMS® (Step 3)
ــــ
2.12 A.D.A.M. PracticePractical Review Anatomy – Create New Test – Open Existing Test
ــــ
ﺳﺆﺍﻝ ﺍﻣﺘﺤﺎﻧﻲ ﺑﻮﺩﻩ ﻛﻪ ﺑﻪﻣﻨﻈﻮﺭ ﻳﺎﺩﺁﻭﺭﻱ ﻭ ﻣﺮﻭﺭ١٥٠٠٠ ﺩﺍﺭﺍﻱ ﺑﻴﺶ ﺍﺯ.( ﻣﻲﺑﺎﺷﺪX-ray ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﻭ، ﺗﺼﻮﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ )ﺗﺼﺎﻭﻳﺮ ﻭﺍﻗﻌﻲ٥٠٠ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ.ﻫﺪﻑ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﺮﻭﺭ ﻣﺒﺎﺣﺚ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻣﺤﻚ ﺯﺩﻥ ﺍﻃﻼﻋﺎﺕ ﻛﺎﺭﺑﺮ ﺩﺭ ﺍﻳﻦ ﺯﻣﻴﻨﻪ ﺍﺳﺖ ﺏ( ﻣﺒﺎﺣﺚ ﻣﺮﺑﻮﻁ ﺑﻪ ﺩﺳﺘﮕﺎﻩﻫﺎﻱ ﺑﺪﻥ ﺍﻟﻒ( ﻣﺒﺎﺣﺚ ﻣﺮﺑﻮﻁ ﺑﻪ ﻧﻮﺍﺣﻲ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ : ﻗﺴﻤﺖ ﻣﺒﺎﺣﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩﺍﻧﺪ٢ ﺩﺭ،CD ﺩﺭ ﺍﻳﻦReview Anatomy ﺩﺭ ﭘﻨﺠﺮﺓ ﺍﺻﻠﻲ.ﻣﻄﺎﻟﺐ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ : ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡ ﺷﺪﻩ ﺩﺭ ﺑﺨﺶ ﻧﻮﺍﺣﻲ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﺷﺎﻣﻞ.ﻫﺮ ﻗﺴﻤﺖ ﺭﺍ ﻛﻪ ﻣﺸﺨﺺ ﻧﻤﺎﻳﻴﺪ ﺗﺼﺎﻭﻳﺮ ﻭ ﺳﺆﺍﻻﺕ ﺍﻣﺘﺤﺎﻧﻲ ﺁﻥ ﺑﺨﺶ ﺍﺭﺍﺋﻪ ﺧﻮﺍﻫﺪ ﺷﺪ . ﺁﻧﺎﺗﻮﻣﻲ ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻲ-٧ ﺁﻧﺎﺗﻮﻣﻲ ﻟﮕﻦ ﺧﺎﺻﺮﻩ-٦ ﺁﻧﺎﺗﻮﻣﻲ ﺷﻜﻢ-٥ ﺁﻧﺎﺗﻮﻣﻲ ﻗﻔﺴﻪ ﺳﻴﻨﻪ-٤ ﺁﻧﺎﺗﻮﻣﻲ ﺗﻨﻪ-٣ ﺁﻧﺎﺗﻮﻣﻲ ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ-٢ ﺁﻧﺎﺗﻮﻣﻲ ﺳﺮ ﻭ ﮔﺮﺩﻥ-١ ﻗﺪﺭﺕ ﺑﺰﺭﮔﻨﻤﺎﻳﻲ ﺗﺼﺎﻭﻳﺮ ﻭ ﻧﻴﺰ ﺣﺬﻑ ﻭ ﺍﺿﺎﻓﻪ ﻧﻤﻮﺩﻥ ﺗﺼﺎﻭﻳﺮ ﻣﻮﺭﺩ ﺩﻟﺨـﻮﺍﻩ ﻭ ﻧﻤـﺎﻳﺶ. ﺷﻤﺎ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻧﻮﻉ ﻣﻘﻄﻊ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﺭﺍ ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﻣﺸﺨﺺ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﻴﺪ. ﺑﻄﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩRelated images ﺗﺼﺎﻭﻳﺮ ﻭﺍﺑﺴﺘﻪ ﺑﻪ ﻫﺮ ﺑﺤﺚ ﺍﺯ ﻃﺮﻳﻖ ﺩﻛﻤﺔ ﭘﺎﺳﺦ ﺳﺆﺍﻻﺕ ﺑﻪShow Results ﺑﺎ ﺯﺩﻥ ﻛﻠﻴﺪ، ﻳﻚ ﺗﺼﻮﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﻣﻲﺁﻳﺪ ﻭ ﻧﺎﻡ ﺑﺨﺸﻲ ﺍﺯ ﺁﻥ ﻣﻮﺭﺩ ﺳﺆﺍﻝ ﺍﺳﺖtext ﺩﺭ ﭘﻨﺠﺮﺓStart test ﻧﺤﻮﺓ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺑﺪﻳﻦ ﺻﻮﺭﺕ ﺍﺳﺖ ﻛﻪ ﺑﺎ ﻓﻌﺎﻝ ﻧﻤﻮﺩﻥ. ﺗﺼﻮﻳﺮ ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻭﺟﻮﺩ ﺩﺍﺭﺩ٤ ﻭ٢ ،١ ﻫﻤﺰﻣﺎﻥ ﺍﺑﺘﺪﺍ ﺷﻤﺎ ﺩﺳﺘﮕﺎﻩ ﻳﺎ ﻧﺎﺣﻴﺔ، ﺩﺭ ﻧﻮﻉ ﺩﻳﮕﺮﻱ ﺍﺯ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ. ﺭﺍ ﺧﻮﺩ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺑﻪ ﺩﻟﺨﻮﺍﻩ ﺗﻨﻈﻴﻢ ﻧﻤﺎﻳﻴﺪCD ﺯﻣﺎﻥ ﭘﺎﺳﺦ ﺑﻪ ﻫﺮ ﺳﺆﺍﻝ ﺩﺭ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺍﻳﻦ. ﻗﺎﺑﻠﻴﺖ ﺍﺿﺎﻓﻪ ﻧﻤﻮﺩﻥ ﻳﺎﺩﺩﺍﺷﺖﻫﺎﻱ ﺷﺨﺼﻲ ﺑﻪ ﻫﺮ ﺗﺼﻮﻳﺮ ﻧﻴﺰ ﻭﺟﻮﺩ ﺩﺍﺭﺩ.ﻫﻤﺮﺍﻩ ﻧﻤﺮﺓ ﻧﻬﺎﻳﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
55 ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﻣﻮﺭﺩﻧﻈﺮ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻣﻲﻧﻤﺎﻳﻴﺪ )ﻭ ﻧﻴﺰ ﺯﻣﺎﻥ ﭘﺎﺳﺦ ﻫﺮ ﺳﺆﺍﻝ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﻛﻨﻴﺪ( ﺑﺎ ﺯﺩﻥ ﻛﻠﻴﺪ Startﺍﻣﺘﺤﺎﻥ ﺷﺮﻭﻉ ﻣﻲﺷﻮﺩ .ﺩﺭ ﻫﺮ ﺳﺆﺍﻝ ﻧﺎﻡ ﺑﺨﺸﻲ ﺍﺯ ﻳﻚ ﺗﺼﻮﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﻣﻮﺭﺩﻧﻈﺮ ﺍﺳﺖ .ﺯﻣﺎﻥ ﺑﺎﻗﻴﻤﺎﻧﺪﻩ ﺑﺮﺍﻱ ﻫﺮ ﺳﺆﺍﻝ ﺩﺭ ﺣﻴﻦ ﺍﻣﺘﺤﺎﻥ ﺩﺭ ﺣﺎﻝ ﻧﻤﺎﻳﺶ ﺍﺳﺖ .ﺍﻳﻦ CDﻧﻮﺷﺘﺔ ﺩﻛﺘﺮ Pawlinaﻭ ﺩﻛﺘﺮ Olsonﻣﻲﺑﺎﺷﺪ ﻭ ﺑﺼﻮﺭﺕ Autorunﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ. Atlas of Clinical Medicine
3.12
Infection Cardiovascular Renal Joints and Bones Respiratory Endocrine, Metabolic and Nutritional )CECIL TEXTBOOK of MEDICINE (21st Edition
4.12
)(Version 2.0) (Forbes. Jackson
ــــ Blood Nerve and Muscle 2001
Gastrointestinal Liver and Pancreas
II SOCIAL AND ETHICAL ISSUES IN MEDICINE IV PREVENTIVE HEALTH CARE VI PRINCIPLES OF HUMAN GENETICS VIII RESPIRATORY DISEASES X RENAL AND GENITOURINARY DISEASES Part XI GASTROINTESTINAL DISEASES
Part Part Part Part Part
Part XIV ONCOLOGY Part XVI NUTRITIONAL DISEASES Part XVIII WOMEN'S HEALTH Part XX DISEASES OF THE IMMUNE SYSTEM Part XXII INFECTIOUS DISEASES Part XXIV DISEASES OF PROTOZOA AND METAZOA Part XXVI EYE, EAR, NOSE, AND THROAT DISEASES Part XXVIII LABORATORY REFERENCE INTERVALS AND VALUES
Part I MEDICINE AS A LEARNED AND HUMANE PROFESSION Part III AGING AND GERIATRIC MEDICINE Part V PRINCIPLES OF EVALUATION AND MANAGEMENT Part VII CARDIOVASCULAR DISEASES Part IX CRITICAL CARE MEDICINE Part XII DISEASES OF THE LIVER, GALLBLADDER, AND BILE DUCTS Part XIII HEMATOLOGIC DISEASES Part XV METABOLIC DISEASES Part XVII ENDOCRINE DISEASES Part XIX DISEASES OF BONE AND BONE MINERAL METABOLISM Part XXI MUSCULOSKELETAL AND CONNECTIVE TISSUE DISEASES Part XXIII HIV AND THE ACQUIRED IMMUNODEFICIENCY SYNDROME Part XXV NEUROLOGY Part XXVII SKIN DISEASES
BEST MEDICAL COLLECTION
2003
5.12
ﺍﻳﻦ CDﺩﺍﺭﺍﻱ ٧ﺑﺮﻧﺎﻣﺔ ﻣﺨﺘﻠﻒ ﻣﻲﺑﺎﺷﺪ ،ﻛﻪ ﻫﺮ ﻳﻚ ﺭﺍ ﺑﺎﻳﺪ ﺑﻄﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺍﺯ ﻓﺎﻳﻞ ﻣﺮﺑﻮﻁ ﺍﻧﺘﺨﺎﺏ ،ﻧﺼﺐ ﻭ ﺍﺟﺮﺍ ﻧﻤﻮﺩ .ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪﻫﺎ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ : -٧ﻧﺮﻡﺍﻓﺰﺍﺭ ﺳﻼﻣﺖ Health soft
-١ﺩﻳﻜﺸﻨﺮﻱ ﭘﺰﺷﻜﻲ -٢ ،ﻃﺐ ﺳﻮﺯﻧﻲ -٥ ،Health manger -٤ ،Multimedia workout -٣ ،ﺩﺍﺭﻭﻫﺎﻱ ﻧﺴﺨﻪﺍﻱ )) medical Drug Reference -٦ ،(Prescription Drugsﻣﺮﺟﻊ ﭘﺰﺷﻜﻲ ﺩﺍﺭﻭﻳﻲ( -١ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﻳﻜﺸﻨﺮﻱ ﭘﺰﺷﻜﻲ :ﻣﻔﺎﻫﻴﻢ ﻭﺍﮊﻩﻫﺎ ﻭ ﺍﺻﻄﻼﻋﺎﺕ ﭘﺰﺷﻜﻲ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﺗﻮﺳﻂ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺟﺴﺘﺠﻮ ﻧﻤﻮﺩ .ﻫﻤﭽﻨﻴﻦ ﺩﻭ ﻓﺼﻞ ﺑﺼﻮﺭﺕ :ﺍﻟﻒ( ﺳﻼﻣﺖ ﺧﺎﻧﻮﺍﺩﻩ ﺏ( ﺳﻼﻣﺖ ﻛﻮﺩﻛﺎﻥ ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﻫﺮ ﻗﺴﻤﺖ ﺩﺍﺭﺍﻱ ﻋﻨﺎﻭﻳﻦ ﻭ ﻣﻄـﺎﻟﺒﻲ ﺑﺼﻮﺭﺕ textﻣﻲﺑﺎﺷﺪ. -٢ﻃــﺐ ﺳــﻮﺯﻧﻲ :ﺷــﺎﻣﻞ ٩ﻓﺼــﻞ ﻣــﻲﺑﺎﺷــﺪ ﻛــﻪ ﺭﻭﺵ ﻛــﺎﺭ ﺑــﺎ ﻭﺳــﺎﻳﻞ ﻭ ﻧﺤــﻮﺓ ﺩﺭﻣــﺎﻥ ﺑﻴﻤﺎﺭﻳﻬــﺎ ،ﺑﺼــﻮﺭﺕ ﺗﻮﺿــﻴﺤﺎﺕ ﻣﺘﻨــﻲ ﺍﺭﺍﺋــﻪ ﺷــﺪﻩ ﺍﺳــﺖ .ﻳــﻚ ﻓــﻴﻠﻢ ﺭﺍﺟــﻊ ﺑــﻪ ﻃــﺐ ﺳــﻮﺯﻧﻲ ﻧﻴــﺰ ﻟﺤــﺎﻅ ﺷــﺪﻩ ﺍﺳــﺖ .ﺍﻳــﻦ ﺑﺮﻧﺎﻣــﻪ ﻣﺤﺼــﻮﻝ ﺷــﺮﻛﺖ Hopkins technologyﺳﺎﻝ ١٩٩٧ﻣﻲﺑﺎﺷﺪ. -٣ﺑﺮﻧﺎﻣﺔ workoutﻧﺴﺨﺔ :١ﺑﺎ ﻭﺍﺭﺩ ﻧﻤﻮﺩﻥ ﻣﺸﺨﺼﺎﺕ ﻓﺮﺩﻱ )ﺳﻦ ،ﻗﺪ ،ﻭﺯﻥ ،ﺟﻨﺴﻴﺖ ،ﻣﻴﺰﺍﻥ ﺍﻧﺮﮊﻱ ﭘﺎﻳﺔ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﻭ (...ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺭﮊﻳﻢ ﻏﺬﺍﻳﻲ ﻣﻨﺎﺳﺐ ،ﻧﻮﻉ ﻧﺮﻣﺶ ﺍﻭ ﻣﻮﺭﺩﻧﻈﺮ ﺭﺍ ﺑﻪ ﺷﻤﺎ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ .ﺍﻳـﻦ ﺑﺮﻧﺎﻣـﻪ ﻣﺤﺼـﻮﻝ ﺳـﺎﻝ ١٩٩٤ﺍﺳـﺖ ﻭ ﺩﺍﺭﺍﻱ ﭼﻨﺪﻳﻦ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺍﺯ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻧﺮﻣﺶﻫﺎ ﻧﻴﺰ ﻣﻲﺑﺎﺷﺪ. :Health manager -٤ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺭ ﺣﻘﻴﻘﺖ ﺍﻃﻼﻋﺎﺕ ﺑﻴﻤﺎﺭﻱ ﻭ ﺳﻼﻣﺘﻲ ﺷﻐﻠﻲ ﺍﻓﺮﺍﺩ ﺭﺍ ﻣﺪﻳﺮﻳﺖ ﻣﻲﻛﻨﺪ .ﺑﺮﻧﺎﻣﻪﺍﻱ ﺍﺳﺖ ﺟﻬﺖ ﺿﺒﻂ ﻭ ﻧﮕﻬﺪﺍﺭﻱ ﻭﻗﺎﻳﻊ ﭘﺰﺷﻜﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﺷﺨﺼﻲ ،ﻟﻴﺴﺖ ﺩﺍﺭﻭﻫﺎﻱ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﺓ ﻓﺮﺩ ،ﺩﺍﺭﻭﻫـﺎﻱ ﺁﻟـﺮﮊﻱ ﻭ ﻳـﻚ ﻛﺘـﺎﺏ ﺁﺩﺭﺱ ﺍﺯ ﻣﺮﺍﻛﺰ ﻣﻬﻢ ﺑﻬﺪﺍﺷﺘﻲ ﻭ ﺩﺭﻣﺎﻧﻲ .ﺯﻣﺎﻥ ﺗﺠﺪﻳﺪ ﻭ ﺗﻌﻮﻳﺾ ﻧﺴﺨﺔ ﭘﺰﺷﻜﻲ ﻭ ﻣﺮﺍﺟﻌﻪ ﺑﻪ ﺩﻧﺪﺍﻧﭙﺰﺷﻚ ﺩﺭ ﺟﺪﺍﻭﻟﻲ ﻣﺸﺨﺺ ﻣﻲﺷﻮﺩ. -٥ﺩﺍﺭﻭﻫﺎﻱ ﻧﺴﺨﻪﺍﻱ :ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﻮﺿﻴﺤﺎﺕ ﻣﺨﺘﺼﺮﻱ ﺭﺍﺟﻊ ﺑﻪ ﺩﺍﺭﻭﻫﺎ ﻭ ﺍﻃﻼﻋﺎﺕ ﻓﺎﺭﻣﺎﻛﻮﻟﻮﮊﻳﻜﻲ ﻣﺮﺑﻮﻃﻪ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ .ﻣﺤﺼﻮﻝ ﺷﺮﻛﺖ Quanta Pressﺳﺎﻝ ١٩٩٢ﻣﻲﺑﺎﺷﺪ. -٦ﻣﺮﺟﻊ ﭘﺰﺷﻜﻲ ﺩﺍﺭﻭﻳﻲ ﻧﺴﺨﺔ :٢ﺍﺯ ﺳﻪ ﺭﺍﻩ ﻣﻲﺗﻮﺍﻥ ﻭﺍﺭﺩ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺪ ﻭ ﺍﺯ ﺁﻥ ﺍﺳﺘﻔﺎﺩﻩ ﻧﻤﻮﺩ: ﺏ( ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻴﻠﺔ ﺟﺴﺘﺠﻮ ،ﻧﺎﻡ ﺩﺍﺭﻭ ﺭﺍ ﺗﺎﻳﭗ ﻧﻤﻮﺩﻩ ﻭ ﺁﻧﺮﺍ ﺑﻴﺎﺑﻴﺪ ﺝ( ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻛﻠﻴﻪ ،Classﮔﺮﻭﻫﻬﺎﻱ ﺩﺍﺭﻭﻳﻲ ﻣﺨﺘﻠﻒ ﻣﻌﺮﻓﻲ ﻣﻲﮔﺮﺩﻧﺪ. ﺍﻟﻒ( ﻟﻴﺴﺖ ﺩﺍﺭﻭﻫﺎ :ﺩﺍﺭﻭﻱ ﻣﻮﺭﺩﻧﻈﺮ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﻴﺪ ﻭ ﺍﻃﻼﻋﺎﺕ ﻻﺯﻡ ﺭﺍ ﺩﺭﻳﺎﻓﺖ ﻛﻨﻴﺪ. ﺩﺭﻣﻮﺭﺩ ﻫﺮ ﺩﺍﺭﻭ ،ﻣﻘﺪﺍﺭ ﻣﺼﺮﻑ ﺭﻭﺯﺍﻧﻪ ،ﺍﺛﺮﺍﺕ ﺟﺎﻧﺒﻲ ،ﺍﺷﻜﺎﻝ ﻣﺨﺘﻠﻒ ﺩﺍﺭﻭ ﻭ ﻫﺸﺪﺍﺭﻫﺎﻱ ﻻﺯﻡ ﺩﺭﻣﻮﺭﺩ ﺍﺛﺮﺍﺕ ﺳﻮﺀ ﺁﻥ ،ﺭﻭﺷﻬﺎﻱ ﻧﮕﻬﺪﺍﺭﻱ ﺩﺍﺭﻭ ﻭ . . .ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﺤﺼﻮﻝ ﺷﺮﻛﺖ Parsons Technologyﺳﺎﻝ ١٩٩٥ﻣﻲﺑﺎﺷﺪ. -٧ﻧﺮﻡﺍﻓﺰﺍﺭ ﺳﻼﻣﺖ ) : (Healthsoftﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺷﺎﻣﻞ ﺳﻪﺑﺨﺶ )ﺳﻪ ﺑﺮﻧﺎﻣﻪ( ﻣﺴﺘﻘﻞ ﻣﻲﺑﺎﺷﺪ: ﺍﻟﻒ( ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ﺗﻮﺿﻴﺤﺎﺗﻲ ﺭﺍﺟﻊ ﺑﻪ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ،ﻣﺮﺍﻗﺒﺖﻫﺎﻱ ﭘﺲ ﺍﺯ ﻋﻤﻞ ،ﺍﻋﻤﺎﻟﻲ ﻛﻪ ﺩﺭ ﺯﻣﺎﻥ ﺍﻭﺭﮊﺍﻧﺲ ﺑﺎﻳﺪ ﺍﻧﺠﺎﻡ ﺩﺍﺩ ﻭ . . .ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺍﺭﺍﻱ ﺗﺼﺎﻭﻳﺮ ﻣﺘﻌﺪﺩ ﻭ ﻧﻴﺰ ﺗﻠﻔﻆ ﺻﺤﻴﺢ ﺍﺻﻄﻼﺣﺎﺕ ﭘﺰﺷﻜﻲ ﻧﺎﺁﺷﻨﺎ ﻧﻴﺰ ﻣـﻲﺑﺎﺷـﺪ ،ﺑـﺎ ﺍﺳـﺘﻔﺎﺩﻩ ﺍﺯ ﻓﻬﺮﺳـﺖ ﺍﻟﻔﺒﺎﻳﻲ ﻣﻲﺗﻮﺍﻥ ﺍﻃﻼﻋﺎﺗﻲ ﺭﺍﺟﻊ ﺑﻪ ﻫﺮ ﻭﺍﮊﻩ ﺭﺍ ﭘﻴﺪﺍ ﻧﻤﻮﺩ. ﺏ( ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ،ﻋﻠﺖ ﺑﻴﻤﺎﺭﻳﻬﺎ ،ﻋﻼﺋﻢ ﻭ ﻧﺸﺎﻧﻪﻫﺎﻱ ﺑﻴﻤﺎﺭﻳﻬﺎ ،ﭘﻴﺸﮕﻴﺮﻱ ،ﻣﺮﺍﻗﺒﺖﻫﺎﻱ ﺑﻬﺪﺍﺷﺘﻲ ،ﺭﻭﺷﻬﺎﻱ ﺻﺤﻴﺢ ﻣﻌﺎﻟﺠﻪ ﻭ ﻧﻴﺰ ﺯﻣﺎﻥ ﻻﺯﻡ ﺑﺮﺍﻱ ﻣﺮﺍﺟﻌﻪ ﺑﻪ ﭘﺰﺷﻚ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
56 ﺝ( ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﻃﻼﻋﺎﺗﻲ ﺭﺍﺟﻊ ﺑﻪ ﺩﺍﺭﻭﻫﺎﻱ ﮊﻧﺘﻴﻚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺛﺮﺍﺕ ﺟﺎﻧﺒﻲ ﺩﺍﺭﻭﻫﺎ ،ﻭﺍﻛﻨﺶ ﻧﺎﺳﺎﺯﮔﺎﺭﻱ ﺗﺪﺍﺧﻞ ﺩﺍﺭﻭﻳﻲ ﻭ . . .ﺩﺭ ﺍﻳﻦ CDﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻟﺒﺘﻪ ﺍﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺗﻨﻬﺎ ﺟﻨﺒﺔ ﺁﮔﺎﻫﻲ ﺩﺍﺩﻥ ﺑﻪ ﻛﺎﺭﺑﺮ ﺭﺍ ﺩﺍﺷﺘﻪ ﻭ ﻧﻮﻳﺴﻨﺪﻩ ﻭ ﺷﺮﻛﺖ ﺗﻮﻟﻴﺪ ﻛﻨﻨﺪﺓ CDﻫﻴﭻ ﺗﻮﺻﻴﻪﺍﻱ ﺩﺭ ﺍﻳﻦ ﺧﺼﻮﺹ ﺍﺭﺍﺋﻪ ﻧﻤﻲﺩﻫﻨﺪ .ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻋﻼﻭﻩ ﺑﺮ ﺍﺭﺍﺋﺔ ﻧﺎﻣﻬﺎﻱ ﮊﻧﺘﻴﻚ ﻭ ﺗﺠﺎﺭﻱ ،ﮔﺮﻭﻫﻬﺎﻱ ﺩﺍﺭﻭﺋﻲ ﻭ ﻣﻮﺍﺭﺩ ﻛﺎﺭﺑﺮﺩﻱ ﺁﻧﻬﺎ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﻣﻘﺪﺍﺭ ﻣﺼﺮﻑ ﺩﺍﺭﻭ ،ﻋﻼﺋﻢ ﻭ ﻧﺸﺎﻧﻪﻫﺎﻱ Dverdoseﺩﺍﺭﻭﻫﺎ ،ﻣﻮﺍﺭﺩ ﻣﻨﻊ ﻣﺼـﺮﻑ ﺁﻧﻬـﺎ ﻭ ﺗﻠﻔﻆ ﺻﺤﻴﺢ ﻧﺎﻡ ﺩﺍﺭﻭ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. Clinical Examination
ــــــ Nervous system
Male genitalia
Heart & cardiovascular system
Respiratory system
Skin, nails & hair
Infants & children
Bones, joints & muscle
Abdomen
Femal breast & genittalia
Ear, nose & throah
CMDT CURREAT Medical Diagnosis & Treatment
7.12
Endoscopic Assessment of Esophagitis According to the Los Angeles Classification System
8.12
ــــــ ــــــ
6.12
ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ :ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: y Viewing Area 1 :Slide Viewer 2: Slide Gallery 3:Video Gallery
3: Complicatins
2: Los Angeles Classification
2: On Endoscopic Assessment of Esophagitis
2002
1: Mucosal Break
y Definitions
1: International Working Group
y Quiz
GRIFFITH'S 5-MINUTE CLINICAL CONSULT
9.12
ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ،ﺍﻳﻦ CDﺑﺮﺍﻱ ﭘﺰﺷﻜﺎﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺩﺳﺘﻲ`ﺍﺭﺍﻥ ﺑﺮﺍﻱ ﻣﺮﻭﺭ ﺳﺮﻳﻊ ﻭﻟﻲ ﺟﺎﻣﻊ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻋﻤﺪﻩ ﺩﺍﺧﻠﻲ ،ﺯﻧﺎﻥ ،ﭘﻮﺳﺖ ،ﺟﺮﺍﺣﻲ ،ﭼﺸﻢ ﻭ ENTﻭ ....ﮔﺮﺩﺁﻭﺭﻱ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻴﺶ ﺍﺯ ﻫﺰﺍﺭ ﻋﻨﻮﺍﻥ ﺑﻴﻤﺎﺭﻱ ﺑﻪ ﺗﺮﺗﻴﺐ ﺍﻟﻔﺒﺎ ﺗﺮﺗﻴﺐ ﻳﺎﻓﺘـﻪ ﺍﺳـﺖ ﻛﻪ ﺩﺭ ﻫﺮ ﻋﻨﻮﺍﻥ ﺟﺰﺋﻴﺎﺕ ﻛﺎﻓﻲ ﺑﺮﺍﻱ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﻭ ﭘﻴﮕﻴﺮﻱ ﺑﻴﻤﺎﺭﻱ ﻭﺟﻮﺩ ﺩﺍﺭﺩ .ﺑﻴﺶ ﺍﺯ ٣٣٠ﻧﻔﺮ ﻣﺘﺨﺼﺼﻴﻦ ﻣﺠﺮﺏ ﺩﺭ ﮔﺮﺩﺁﻭﺭﻱ ﺍﻳﻦ ﻣﺠﻤﻮﻋﻪ ﻫﻤﻜﺎﺭﻱ ﺩﺍﺷﺘﻪﺍﻧﺪ .ﺍﻳﻦ CDﺷﺎﻣﻞ ﺗﻮﺿﻴﺢ ﺑﻴﻤﺎﺭﻱﻫﺎ )ﺩﺭ ﺯﻳﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ( ﻭ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲ ،ﻧﻤﻮﺩﺍﺭ ﻭ ﺟﺪﻭﻝ ﻣﻲﺑﺎﺷﺪ. ﻋﻨﻮﺍﻥ ﻫﺮ ﺑﻴﻤﺎﺭﻱ ﺩﺭ ٦ﻗﺴﻤﺖ ﺍﺻﻠﻲ ﻭ ٣٦ﻗﺴﻤﺖ ﻓﺮﻋﻲ ﺑﻪ ﺗﻔﻀﻴﻞ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻣﺸﺮﻭﺡ ﻋﻨﺎﻭﻳﻦ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: 1- BASICS • Description • Genetics • Prevalence • Age • Signs and symptoms • Causes • Risk factors
2002
2000
2- DIAGNOSIS • Differential • Laboratory • Pathological findings • Special tests • Imaging
3- TREATMENT • Genral measures • Surgical measures • Activity • Diet • Patient education
4- MEDICATION • Drugs of choice • Contraindications • Precautions • Interactions • Alternate drugs
5- FOLLOW-UP • Monitoring • Prevention • Complications • Prognosis
6- MISCELLANEOUS • Associated conditions • Age-related factors • Pregnancy • Synonyms • ICD-9-CM • See also • Other notes • Abbreviations • References
)10.12 HEALTH ASSESSMENT (Gaylene Bouska Altman, RN, Ph.D., Karrin Johnson, RN, Robert W. Wallach, MD ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ٤ﺑﺨﺶ ﺭﺍﺟﻊ ﺑﻪ ﺍﺭﺯﻳﺎﺑﻲ ﺳﻼﻣﺖ ﻭ ﺁﺯﻣﺎﻳﺸﺎﺕ ﻭ ﻣﻌﺎﻳﻨﺎﺕ ﻓﻴﺰﻳﻜﻲ ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ :١ﻣﺮﻭﺭﻱ ﺑﺮ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ :ﺷﺎﻣﻞ ١٧٥ﻗﺴﻤﺖ ﻫﻤﺮﺍﻩ ﺑﺎ ٥٩ﺗﺼﻮﻳﺮ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺯ ﺩﺳﺘﮕﺎﻫﻬﺎ ﻭ ﺍﻧﺪﺍﻣﻬﺎﻱ ﺑﺪﻥ ﺑﻪ ﻫﻤﺮﺍﻩ ﺍﻃﻼﻋﺎﺕ ﻣﺘﻨﻲ ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺗﻤﺎﻣﻲ ﻣﻄﺎﻟﺐ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻣﺮﻭﺭ ﺷﺪﻩ ﺍﺳﺖ. ﺑﺨﺶ :٢ﺻﺪﺍﻫﺎﻱ ﻗﻠﺐ ﻭ ﺭﻳﻪ :ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺻﺪﺍﻫﺎﻱ ﻗﻠﺐ ﻭ ﺭﻳﻪ )ﺩﺭ ﺣﺎﻟﺖ ﺳﻼﻣﺘﻲ ﻭ ﺑﻴﻤﺎﺭﻱ( ﺩﺭ ﻫﻨﮕﺎﻡ ﻣﻌﺎﻳﻨﺔ ﻣﺮﻳﺾ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﻫﻤﭽﻨﻴﻦ ﻋﻤﻠﻜﺮﺩ ﻭ ﺳﺎﺧﺘﺎﺭﻫﺎﻱ ﻗﻠﺐ ﻧﻴﺰ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ. ﺑﺨﺶ :٣ﻣﻬﺎﺭﺗﻬﺎﻱ ﺣﻴﺎﺗﻲ ﺩﺭ ﺍﺭﺯﻳﺎﺑﻲ ﺳﻼﻣﺘﻲ ﻭ ﻣﻌﺎﻳﻨﺎﺕ ﻓﻴﺰﻳﻜﻲ :ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺑﺼﻮﺭﺕ »ﺑﺮﺭﺳﻲ ﻭ ﻣﻄﺎﻟﻌﺔ ﻣﻮﺭﺩﻱ« ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ Case ٢٠ .ﻣﺨﺘﻠﻒ ﭘﺲ ﺍﺯ ﺍﺭﺍﺋﻪ ﺷﺮﺡ ﺣﺎﻝ ،ﻭﺿﻌﻴﺖ ﺑﻴﻤﺎﺭﻱ ﺁﻧﻬﺎ )ﺑﺼﻮﺭﺕ ﺳﺆﺍﻝ ﻭ ﺟﻮﺍﺏ( ﺗﻮﺳﻂ ﻛـﺎﺭﺑﺮ ﻣﺸـﺨﺺ ﻣـﻲﺷـﻮﺩ. ﻫﺪﻑ ﺍﺯ ﺍﻳﻦ ﺑﺨﺶ ﺍﻓﺰﺍﻳﺶ ﻗﺪﺭﺕ ﻭ ﻣﻬﺎﺭﺕ ﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﺩﺭ ﺗﺸﺨﻴﺺ ﺑﻴﻤﺎﺭﻳﻬﺎﺳﺖ. ﺑﺨﺶ :٤ﺁﺷﻨﺎﻳﻲ ﺑﺼﺮﻱ ﺑﺎ ﻣﻌﺎﻳﻨﺎﺕ ﻓﻴﺰﻳﻜﻲ؛ ﻛﻪ ﺩﺍﺭﺍﻱ ٢Cﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ ،ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﻳﻚ ﺑﺮﻧﺎﻣﺔ ﺁﻣﻮﺯﺷﻲ ﻣﺼﻮﺭ ﻫﻤﺮﺍﻩ ﺑﺎ ﺍﺭﺍﺋﻪ ﺗﻌﺎﺭﻳﻒ ﻭ ﺍﺻﻄﻼﺣﺎﺕ ﻣﺮﺑﻮﻁ ﺑﻪ ﻣﻌﺎﻳﻨﺎﺕ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺭ ﻫﺮ ﭼﻬﺎﺭ ﺑﺨﺶ ﺍﻣﺘﺤﺎﻥ ﺑﺼﻮﺭﺕ ﺳﺆﺍﻻﺕ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﻧﻴﺰ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. (11.12 MCCQE Review Nots and Lecture Series (Marcus Law & Brain Rotengberg Section Menu: Anesthesia, Cardiology, Color Atlas, Community Med, Dermatololgy, Diagnostic Imaging, Emergency, Endocrinology, Family Medicinne, Gastroenterology, General Surgery, Geriatrics, Gynecology, Hematology, Infectious Disease, Nephrology, Neurology, Neurosurgery, Obstetrics, Ophthalmology, Orthopedics, Otolaryngology, Pediatrics, Plastic Surgery, Psychiatry, Respirology, Rheumatology, Urology
2000 ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
)12.12 Medical Dictionary (Dorland's) (by W. B. Saunders ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
57 )13.12 MEDICAL Encyclopedia For Health Consumers (With Atlas TM )(The Best Internal Medicine Board Review 14.12 MedStudy
ــــ 2000
3. The Most Effective
4. The Most Talked About
2. The Most Powerful
1. The Most Board Specific
2002
)15.12 Natural Medicine Instructions for Patients (Lara U. Pizzorno, Joseph E. Pizzorno, Jr, Michael T. Murray
2002
16.12 Patient Teaching Aids ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺵ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﺑﻴﻤﺎﺭﺍﻥ ﻭ ﭘﺰﺷﻜﺎﻥ ﺩﺭ ﺭﺷﺘﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﺁﻣﻮﺯﺵﻫﺎﻱ ﻻﺯﻡ ﺭﺍ ﺩﺭ ﺑﺎﺑﺖ ﺍﻗﺪﺍﻣﺎﺕ ﺣﻤﺎﻳﺘﻲ ،ﺍﻗﺪﺍﻣﺎﺕ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻧﻲ ﺩﺭﺑﺮ ﺩﺍﺭﺩ .ﻣﻄﺎﻟﺐ ﺑﺮ ﺍﺳﺎﺱ ﻣﻮﺿﻮﻉ ﻭ ﺑﻴﻤﺎﺭﻱ ﺩﺳﺘﻪﺑﻨﺪﻱ ﺷﺪﻩﺍﻧﺪ ﻭ ﻫﺮ ﻣﻄﻠﺐ ﺣـﺪﻭﺩ ﻳـﻚ ﺻﻔﺤﻪ ﻣﻲﺑﺎﺷﺪ .ﺻﻔﺤﺎﺕ ﻗﺎﺑﻞ Printﻭ ﺍﺭﺍﺋﻪ ﺑﻪ ﺑﻴﻤﺎﺭﺍﻥ ﻫﺴﺘﻨﺪ .ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻧﻘﺶ ﺑﻴﻤﺎﺭ ﺭﺍ ﺩﺭ ﻓﺮﺁﻳﻨﺪ ﺩﺭﻣﺎﻥ ﺗﻘﻮﻳﺖ ﻛﺮﺩﻩ ﻭ ﺩﻳﺪﮔﺎﻩ ﻋﻠﻤﻲ ﻭ ﻣﻨﺎﺳﺒﻲ ﺑﻪ ﻭﻱ ﻣﻲﺩﻫﺪ ﻛﻪ ﺑﻪ ﺭﻭﻧﺪ ﻛﻠﻲ ﺳﻼﻣﺖ ﻭ ﺑﻬﺒﻮﺩ ﻛﻤﻚ ﺑﺴﺰﺍﻳﻲ ﺩﺍﺭﺩ .ﻗﺎﺑﻠﻴﺖ Searchﻗـﻮﻱ ﻭ ﻧﻴـﺰ ﺍﺿﺎﻓﻪﻛﺮﺩﻥ ﻧﻮﺷﺘﻪ ﺑﻪ ﻣﺘﻦ ﺍﺯ ﻣﺰﺍﻳﺎﻱ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩ .ﺣﺪﻭﺩ ٤٠٠ﺳﺮﻓﺼﻞ ﻛﻪ ﻫﺮ ﻛﺪﺍﻡ ﺷﺎﻣﻞ ﭼﻨﺪ Tapicﻋﻤﺪﻩ ﻭ ﺷﺎﻳﻊ ﻣﻲﺑﺎﺷﺪ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﺑﺮﺍﺣﺘﻲ ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻳﺎﻓﺖ. )(Third Edition
ــــ
)17.12 Practical General Practice (Guidelines for effective clinical management) (Alex Khot, Andrew Polmear
2002
)18.12 RAPID REVIEW FOR USMLE STEP 1 (Mosby y Anatomy y Behavioral Science y Biochemistry y Histology/Cell Biology y Microbiology/Immunology y Neuroscience y Pathology y Pharmocology y Physiology y Randomize All
Sciences:
2003
19.12 SPSS 12.0 for Windows
2002
)20.12 Textbook of Physical Diagnosis HISTORY AND EXAMINATION (Fourth Edition) (Mark H. Swartz, M.D.) (W.B. SAUNDERS COMPANY 21.12 The Basics for Interns
ــــ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ٦ﻓﺼﻞ ﺍﺻﻠﻲ ﺍﺳﺖ: -١ -٢ -٣ -٤ -٥ -٦
) airway Managementﺍﺭﺯﻳﺎﺑﻲ ﻣﺴﻴﺮ ﺭﺍﻫﻬﺎﻱ ﻫﻮﺍﻳﻲ ،ﻛﻨﺘﺮﻝ ﻣﺴﻴﺮ ﺭﺍﻫﻬﺎﻱ ﻫﻮﺍﻳﻲ ﺩﺭ Apneaﻭ hypoxiaﻭ ، . . .ﺍﺑﺰﺍﺭﻫﺎﻱ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺭ ﻣﺴﻴﺮﻫﺎﻱ ﻫﻮﺍﻳﻲ ﺑﻴﻨﻲ ﻭ ﺩﻫﺎﻥ ،ﺭﻭﺷﻬﺎﻱ ﺑﻴﻬﻮﺷﻲ ،ﻭ ﻧﻴﺘﻼﺳﻴﻮﻥ ﻣﺎﺳﻚ ﻛﻴﺴﻪﺍﻱ ،ﻟﻮﻟﻪﮔﺬﺍﺭﻱ ﻧﺎﻱ ﺗﺮﺍﻛﻨﻮﺗﻮﻣﻲ( ﺗﻔﺴﻴﺮ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﺍﻭﻟﻴﺔ ﺗﺼﻮﻳﺮ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ )ﺷﺎﻣﻞ ﺗﺼﺎﻭﻳﺮ – Chest x-rayﺗﺼﺎﻭﻳﺮ Abdominal x-rayﻭ (CT-scan ﻣﺪﻳﺮﻳﺖ ﺟﺮﺍﺣﻲ ﺯﺧﻢﻫﺎ )ﺷﺎﻣﻞ ﻧﺦﻫﺎﻱ ﺟﺮﺍﺣﻲ – ﻣﻌﺮﻓﻲ ﺍﺑﺰﺍﺭ ﻭ ﻭﺳﺎﻳﻞ ﺟﺮﺍﺣﻲ – ﻧﻤﺎﻳﺶ ﻧﺤﻮﺓ ﺍﻧﻮﺍﻉ ﺑﺨﻴﻪ ﺯﺩﻥﻫﺎ ،ﺭﻭﺵ ﭘﺎﻧﺴﻤﺎﻥ ﺯﺧﻢﻫﺎ ( . . . ﺩﺳﺘﺮﺳﻲ ﺑﻪ ﺷﺮﻳﺎﻥﻫﺎ )ﺷﺎﻣﻞ ﺷﺮﻳﺎﻥ ﺭﺍﺩﻳﺎﻝ – ﺷﺮﻳﺎﻥ ﻓﻤﻮﺭﺍﻝ( ﺩﺳﺘﺮﺳﻲ ﻭ ﺑﻜﺎﺭﮔﻴﺮﻱ ﺳﻴﺎﻫﺮﮒﻫﺎ )ﻣﻌﺮﻓﻲ ﻭﺳﺎﻳﻞ ﺟﻬﺖ ﺩﺳﺘﺮﺳﻲ ﻃﻮﻻﻧﻲ ﻣﺪﺕ ﺑﻪ ﺳﻴﺎﻫﺮﮒﻫﺎ -ﺍﺭﺯﻳﺎﺑﻲ ﭘﻴﺶ ﺍﺯ ﻋﻤﻞ ﻭ ﺗﺪﺍﺭﻛﺎﺕ ﻻﺯﻡ – ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺑﺮﺷﻲ ﺳﻴﺎﻫﺮﮒﻫﺎ ﻭ ﺍﻳﻤﭙﻠﻨﺖﻫﺎﻱ ﺯﻳﺮﭘﻮﺳﺘﻲ ﻭ ( . . . ﺩﺭ ﻧﺎﮊ ﻭ ﺗﺨﻠﻴﻪ ﭘﻠﻮﺭﺍﻝ ) :ﻣﻮﺍﺭﺩ ﺍﺳﺘﻌﻤﺎﻝ ،ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ،ﺗﻜﻨﻴﻚ ﺗﻮﺭﺍﺳﻨﺘﺰ ،ﺗﻜﻨﻴﻚ ﺗﻴﻮﺏ ﺗﻮﺭﺍﻛﻮﺳﺘﻮﻣﻲ (
-٧
ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﻋﻨﻮﺍﻥ ﺷﺪﻩ ﺩﺭ ﺑﺎﻻ ﺑﺼﻮﺭﺕ ﻓﻴﻠﻤﻐﻬﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻭ ﺗﺼﺎﻭﻳﺮ ﻣﺘﻌﺪﺩ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ ﮔﻮﻳﻨﺪﻩ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻓﻴﻠﻤﻐﻬﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻳﺎ ﺑﺼﻮﺭﺕ ﻭﺍﻗﻌﻲ ﺍﺳﺖ ﻭ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ﺑﺮﺭﻭﻱ ﻣﺮﻳﺾ ﺩﻗﻴﻘﹰﺎ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﻳﺎ ﺑﺼﻮﺭﺕ ﺍﻧﻴﻤﻴﺸﻦ ﺍﺳﺖ.
ــــ
)22.12 Understanding Lung Sounds (Audio CD
ــــ
)23.12 UNDERSTANDING PATHOPHYSIOLOGY (Second Edition) (Sue E. Huether, Kathryn L. McCance
ــــ
)(W.B. Saunders Company
th )24.12 Virtual Medical Office CHALLENGE (to accompany Bonewit-West Clinical Procedures for Medical Assistants, 5 Edition
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ CaseStudyﻫﺎﻱ ﻣﺘﻌﺪﺩ ﻣﻄﺮﺡﺷﺪﻩ ﻛﺎﺭﺑﺮ ﺭﺍ ﺑﻪ ﺍﺳﺘﻔﺎﺩﻩ ﺑﺎﻟﻴﻨﻲ ﺍﺯ ﺍﻃﻼﻋﺎﺕ ﺍﺭﺍﺋﻪﺷﺪﻩ ﺩﺭ ﻛﺘﺐ ﺭﻓﺮﺍﻧﺲ ﻋﺎﺩﺕ ﻣﻲﺩﻫﺪ .ﺩﺭ ﻋﻴﻦ ﺣﺎﻝ ﺷﻴﻮﺓ ﺣﻞ ﻣﺸﻜﻼﺕ ،ﻗﺪﺭﺕ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺑﻪ ﺿﺮﺍﻓﺖﻫﺎﻱ Criticalﻭ Triage ﻛﻪ ﺍﺯ ﻣﻬﻤﺘﺮﻳﻦ ﻣﻬﺎﺭﺕﻫﺎ ﺑﺎﻟﻴﻨﻲ ﭘﺰﺷﻜﺎﻥ ﻭ ﻛﺎﺩﺭ ﭘﺰﺷﻜﻲ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩ ،ﺩﺭ ﻃﻲ ﻣﺮﺍﺣﻞ ﻣﺘﻌﺪﺩ ﻭ ﺑﻪ ﺻﻮﺭﺕ ﻋﻤﻠﻲ ﻭ ﺳﻤﻌﻲ ﺑﺼﺮﻱ ﺁﻣﻮﺯﺵ ﻭ ﺗﻤﺮﻳﻦ ﻣﻲﮔﺮﺩﻧﺪ .ﺍﻳﻦ CDﺷﺎﻣﻞ ﭼﻬﺎﺭ ﺳﺮﻓﺼﻞ ﻋﻤﺪﻩ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﺍﺳﺖ: -Help
- Challenge Status
- Clinical Skills
- Case Study
ﺗﻐﺬﻳﻪ 2002 ___ 2002 ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
)25.12 Contemporary Nutrition Food Wise (Food Wise, Weight Manager )26.12 Food Works (College Edition )27.12 INTRODUCTION TO NUTRIOTION AND METABOLISM (Third Edition) (DAVID A Bender ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
58 28.12 Multimedia Workout
(Jeffrey S. Smith, Joseph D. Cook)
ــــ
29.12 NUTRIENTS IN FOOD (Elizabet S. Hands)
2002
30.12 THE FOOD LOVER'S ENCYCLOPEDIA Culinary Techniques Recipes Nutrition Foods
ــــ
ﺩﺍﺭﻭﺋﻲ-١٣
CD ﻋﻨﻮﺍﻥ 1.13
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
American DRUG INDEX (FACTS AND COMPARISONS)
2.13 Appleton and Lange's Quick Review PHARMACY -Parmaceutics/Pharmokinetics
-Pharmacology
2001 ___
(Twelfth Edition) (Joyce A. Generali, Christine A. Berger)
: ﺩﺭ ﻣﻮﺭﺩ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺑﺤﺚ ﻣﻲﻛﻨﺪCD ﺍﻳﻦ
-Microbiology and Public Health
-Chemistry and Biochemistry
-Physiology/Pathology
-Clinical Pharmacy
3.13 British Pharmacopoeia (version 6.0) Vol 1: -Notices -Preface -British Pharmacopoeia Commision -Introduction -General Notices -Monographs: Meidicinal and Pharmaceutical Substances Vol 2: -Notices -General Notices -Monographs -Infrared Reference Spectra -Appendices -Supplementary Chapters British Pharmacopoeia (Veterinary): -Preface -British Pharmacopoeia Commission -Introduction -General Notices -Monographs -Infrared Reference Spectra -Appendics th 4.13 CLINICAL DRUG THERAPY Rationnales for Nursing Practice (7 Edition) (ANNE COLLINS ABRAMS) (Lippincott Williams & Wilkins) -Dosage Calc Challenge!
-Animations
-NCLEX Questions
-Monographs of 100 Most Commonly Prescribed Drug
-Preventing Medication Errors Video
2002
___
-Patient Teaching Sheets
5.13
Chem Office (Renate Buergin Schaller)
___
6.13
DERIVATIZATION REACTIONS FOR HPLC (Georgelunn, Louise C. Hellwic)
___ 2000
7.13 Dosages and Solutions CD Conpanion (Virginia Daugherty, RN, MSN, Diana Romans, RN, BSN) (Harcourt Health Sciences)
8.13
-Mathematics Review -Introducing Drug Measures -How to Read a Drug Label -Calculatin Dosages DRU ERUPTION REFERENCE MANUAL (The Parthenon Publishing Group) (Jerome Z. Litt, MD) Search by:
- Drug Name
-Reactions
9.13
DRUG CONSULT (Mosby)
10.13
Drug Identifier Find Products by: -Drug name
-Interactions
-Categories
-Company
-Multiple Search
: ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ
-Comprehensive Posttest 2004 -Printing
-Common
-Reaciton ___ 2003
-Imprint
-NDC code
-Manufacturer name
11.13 GoodMan and Gilmans's CD-ROM
___
12.13 HERBAL MEDICINE Expanded Commission E Monographs (INTEGRATIVMEDICINE)
___
13.13 Herbal Remedy FINDER
___
14.13 HPLC and CE METHODS for Pharmaceutical Analysis
(Version 2.0)
(George Lunn) (John Wiley and ons)
15.13 Patient Education Guide to Oncology Drugs Name Search – Categories – Comparisons
2000 ___
(Gail M. Wilkes, RNC, MS, AOCN, Terri B. Ades, RN, MS, AOCN)
16.13 PDQ PHARMACOLOGY (GORDON E. JOHNSON, PHD)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2002 ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
59 PDR® Electronic Library™ PHYSICIANS DESK REFERENCE (Thomson Medical Economics).
2004
ﺍﺭﺍﺋـﻪ ﺷـﺪﻩﺍﻧـﺪ ﺍﺯ ﻣﻌﺘﺒﺮﺗـﺮﻳﻦ ﻭ ﺟﺪﻳـﺪﺗﺮﻳﻦCD ( ﻓﺎﺭﻣﺎﻛﻮﻟﻮﮊﻱ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕPDR, PDQ) ﺩﻭ ﺭﻓﺮﺍﻧﺲ. ﻭﺟﻮﺩ ﻳﻚ ﺭﻓﺮﺍﻧﺲ ﺟﺎﻣﻊ ﻭ ﻣﻌﺘﺒﺮ ﺍﻃﻼﻋﺎﺕ ﺩﺍﺭﻭﺋﻲ ﺿﺮﻭﺭﻱ ﻣﻲﻧﻤﺎﻳﺪ، ﺻﺮﻓﻨﻈﺮ ﺍﺯ ﻧﻮﻉ ﺗﺨﺼﺺ،ﺩﺭ ﻣﻄﺐ ﺭﻭﻱ ﻣﻴﺰ ﻛﺎﺭ ﻫﺮ ﭘﺰﺷﻚ . ﺭﺍ ﺑﻪ ﺩﺳﺖ ﺁﻭﺭﺩ... ﻋﻮﺍﺭﺽ ﺟﺎﻧﺒﻲ ﻭ، ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ، ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ،ﻣﺮﺍﺟﻊ ﺩﺍﺭﻭﺷﻨﺎﺳﻲ ﻣﻲﺑﺎﺷﻨﺪ ﻛﻪ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﻧﻬﺎ ﻣﻲﺗﻮﺍﻥ ﺩﺭ ﻛﻤﺘﺮﻳﻦ ﺯﻣﺎﻥ ﻣﻤﻜﻦ ﻛﻠﻴﺔ ﺍﻃﻼﻋﺎﺕ ﻻﺯﻡ ﺩﺭ ﻣﻮﺭﺩ ﺩﺍﺭﻭﻱ ﻣﻮﺭﺩ ﻧﻈﺮ ﻣﻦﺟﻤﻠﻪ ﺩﻭﺯﺍﮊ PDQ Pharmacology ( ﻃﺮﻳﻘﺔ ﻧﺼﺐ . ﻛﻨﻴﺪNext ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ. ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ١ ﺑﻨﺎﺑﺮﺍﻳﻦ ﮔﺰﻳﻨﺔ. ﺭﺍ ﻧﺼﺐ ﻛﻨﻴﻢAcroba Reader ﭘﻨﺠﺮﻩﺍﻱ ﻇﺎﻫﺮ ﻣﻲﺷﻮﺩ ﺑﺮﺍﻱ ﺷﺮﻭﻉ ﻣﻲﺑﺎﻳﺴﺘﻲ ﺑﺮﻧﺎﻣﺔ. ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ﺍﺗﻮﻣﺎﺗﻴﻚ ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ، ﺭﺍ ﺩﺭﻭﻥ ﺩﺭﺍﻳﻮ ﻗﺮﺍﺭ ﻣﻲﺩﻫﻴﻢCD ﺍﺑﺘﺪﺍ Adobe ( ﺍﻳـﻦ ﺑﺮﻧﺎﻣـﻪ ﺗﺤـﺖ ﺑﺮﻧﺎﻣـﺔStart) ﺭﺍ ﺍﺯ ﺍﻭﻟـﻴﻦ ﭘﻨﺠـﺮﻩ ﺍﻧﺘﺨـﺎﺏ ﻛﻨﻴـﺪ٢ ﺑﺮﺍﻱ ﺍﺟﺮﺍﻱ ﺑﺮﻧﺎﻣﺔ ﺍﺻﻠﻲ ﮔﺰﻳﻨﺔ. ﺭﺍ ﻓﺸﺎﺭ ﺩﻫﻴﺪOK ﺩﺭ ﻧﻬﺎﻳﺖ. ﻛﻨﻴﺪNext ﭘﻨﺠﺮﺓ ﻓﻌﻠﻲ ﻣﺴﻴﺮ ﻧﺼﺐ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﻛﻨﺪ ﺩﺭ ﺻﻮﺭﺕ ﺗﻮﺍﻓﻖ ﺑﺎ ﺁﻥ . ﻗﺎﺑﻞ ﺍﺟﺮﺍ ﺍﺳﺖAerobat Reader 17.13 PHARMACOLOGY (Thomas L. Pazderink, Laszlo Kerecsen, Mrugshkumar K. Shah) (Mosby) 18.13 PHYSICANAS' CANCER CHEMOTHERAPHY DRUG MANUAL - Principles of Cancer Chemotheraphy - Common Chemotherapy Regimens in Clinical Practice
19.13 The Herbalist
-Basic Principles
(David L. Hoffman) -Human Systems
2003 2004
(Jones & Bartlett)
:ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﺭ ﻣﻮﺭﺩ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﺑﺤﺚ ﻣﻲﻛﻨﺪ
- Physician's Cancer Chemotherapy Drug Manual 2004 - Guidelines for Chemotherapy and Dosing Modifications - Antimetic Agents for the Treatment of Chemotherapy-Induced Nausea and Vomiting
___ -Actions
-Herbal Materia Medica
20.13 THE MERCK INDEX on CD-ROM (Version 12:3)
2000
21.13 USP 26-NF 21 Through Supplement Two (U.S. PHARMACOPEIA) (The standard of Quality)
(The United States Phamocopeial Convention, Inc)
2003
ﺯﺑﺎﻥ:١٤
CD ﻋﻨﻮﺍﻥ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
1.14
BUILDING A MEDICAL VOCABULARY (FIFTH EDITION) (FEGGY C. LEONARD) (W.B. Saunders Company)
2001
2.14
ELECTRONIC MEDICAL DICTIONARY (STEDMAN'S) (LIPPINCOTT WILLIAMS & WILKINS)
2001
3.14
English Family (Merriam-Webster)
ــــ
4.14
Entertainment Collection
ــــ
5.14
How to Prepare for TOEFL
ــــ
6.14
Learn To Speak English Dictionary & Grammer
7.14
Mad About English Spelling (Interactive Learning)
(CD1-4)
ــــ ــــ
8.14 Medical Information on the Internet (A Guide for Health Professionals) (Second Edition) Why use the Internet? Internetive Learning The future Appendix D: Configuring TCP/IP
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
Getting Wired E-mail, discussion lists and newsgroups Appendix A: Finding more information information Appendix E: Glossary
(Robert Kiley)
ــــ
Finding what you want The quality issue Appendix B: Netscape Navigator and Internet
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
The top ten medical resources Consumer health information Appendix C: Optimising your computer
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
60 9.14
Preparation For the TOEFL (Dictionary Crossword Puzzle Matching Game)
ــــ
10.14 Preparing for the GRE Writing Assessment
ــــ
What does the GRE General Test measure? The GRE General Test is designed to measuregeneral knowledge and reasoning skills in three areas that are important for a academic achievement: Verbal Ability Quantitative Ability Analytical Ability 11.14 Speak Fluent Series
ــــ
12.14 Studying a Study Texting a Test (Fourth Edition) (Richard K. Riegelman)
ــــ
Accreditation Statement Designation Statement
Instructions to Users Target Audience
Lippincott Williams & Wilkins Test-CME Needs Assessment
Continuing Medical Education Glossary
CME User assessment Learning Objectives
Faculty Credentials/Disclosure
13.14 The AMERICAN HERITAGE® TALKING DICTIONARY (Daniel Finkel) 14.14 THE LANGUAGE OF MEDICINE (6
TH
1. Word Ports
(Chapters 1-4)
ــــ 2000
EDITION) (W.B. Saunders Company)
2.Body Systems
(Chapter 5-18)
3. Specialties
(Chapter 19-22)
15.14 TriplePlayPlus! ENGLISH (Syracuse Languag Systems)
ــــ
16.14 Users' Guides To The Medical Literature (A manual for Evidence-Based Clinical Practice) (Gordon Guyatt, MD, Drummond Rennie, MD, Robert Hayward, MD)
2002
ﺟﺮﺍﺣﻲ-١٥
CD ﻋﻨﻮﺍﻥ 1.15
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
1. Reflux Disease and Nissen Fundoplication (Philip E. Donahue, MD) (VCD)
ــــ
2. Supraceliac Aortic-Celiac Axix-Superior Mesenteric Artery Bypass (Gregorio A. Sicard, Charles B. Anderson) 2.15
Advanced Therapy in THORACIC SURGERY (Kenneth L. Franco, MD, Joe B. Putnam Jr., MD)
ــــ
3.15
Aesthetic Department
ــــ
ARTECOLL: Injectable micro-Implant, for long lasting levelling of facial wrinkles and folds M-Implants By Rofil THE BEAUTY PHILOSOPHY: M-Implantans by Rofil you and your patients with the highest quality mammary implants in every option possible. 4.15
American Collage of Surgeons ACS Surgery Principles & Practice (CDI , II)
ــــ
5.15
Aspects of Electrosurgery (Dr. Anthony C. Easty, PhD PEng CCE) Department Medical Engineering
6.15
Atlas of Liposuction (Tolbert s. Wilkinson, MD)
ــــ ــــ
7.15
Atlas of RENAL TRANSPLANTATION
8.15
-Histopathology -surgery -clinical section -imaging -immunology Basic Surgical Skills (David A. Sherris. M.D., Eugene B. Kern, M.D.) (Mayo Clinic)
9.15
Breast-Augmentation with NovagoldTM
(Prof. Legndre, Martin, Helenon, Lebranchu, Halloran, Nochy) -immunosupperssive
The PVP-Hydrogel Filled Implant
10.15 Case Presentations In Plastic Surgery (Christopher Stone, Consultant Plastic Surgeon)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ــــــ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــ ــــ 2004
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
61 11.15 Cholecystectomy by Laparoscopy (Department of Surgery Hospitalor Saint-Avold France) (VCD)
ــــ
12.15 Clinical Surgery (Second Edition) (Michael M. Henry, Jeremy N. Thompson)
ــــ
13.15 Core Curriculum in Primary Care Patient Evaluation for Non-Cardiac Surgery and Gynecology and Urology (Michael K. Rees, MD, MPH)
ــــ
1. Appendicectomy
2. Highly Selective Vagotomy
3. Taylor's Operation
. ﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖHarvard ﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲCD ﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯCCC ﺳـﺆﺍﻻﺕ ﻣﺮﺑﻮﻃـﻪ ﺑـﻪ، ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜﻲ. ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛﺎﺭﺑﺮ ﻣﻲﺑﺎﺷﺪ. ﺯﻧﺎﻥ ﻭ ﺍﻭﺭﻭﮊﻱ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖ، ﺣﺎﺿﺮ ﺩﺭ ﻣﻮﺭﺩ ﺟﺮﺍﺣﻲCD : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ. ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﻘﺎﻟﻪ ﭼﺎﭘﻲ ﺩﺭ ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ.ﺻﻮﺭﺕ ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ Male impotence
ﻋﻘﻴﻤﻲ ﻣﺮﺩﺍﻥ-٣
.(AUB) ﺍﺭﺯﻳﺎﺑﻲ ﺧﻮﻧﺮﻳﺰﻱﻫﺎﻱ ﺍﺑﻨﺮﻣﺎﻝ ﺭﺣﻢ
-٢
ﭼﮕﻮﻧﻪ ﻳﻚ ﺑﻴﻤﺎﺭ ﺭﺍ ﺑﺮﺍﻱ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ )ﺑﺠﺰ ﺟﺮﺍﺣﻲ ﻗﻠﺐ( ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺁﻣﺎﺩﻩ ﻛﻨﻴﻢ؟-١ . ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖtext ﺳﺆﺍﻻﺕ ﺷﻨﻮﻧﺪﮔﺎﻥ ﻭ ﺟﻮﺍﺏ ﺳﺨﻨﺮﺍﻥ ﻧﻴﺰ ﺑﻪ ﺻﻮﺭﺕ،ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ
12.3
Core Curriculum in Primary Care Gynecology (Michael, Isaac Schiff, Keith, Thomas, Annekathryn)
14.15 Core Curriculum in Primary Care Gynecology 15.15
19.15 20.15 21.15 22.15 23.15 24.15 25.15
management of the aging face)
18.15
(A practical and systematic guide to surgical
17.15
ــــــ
(Michael, Isaac Schiff, Keith, Thomas, Annekathryn)
VCD 1: Rhinophyma (9:52) - Alloderm Lip Augmentation (14:04) - Collagen Injection Sequence COMPREHENSIVE FACIAL REJUVENATION
16.15
ــــــ
VCD 2: Full-Face Jessner’s/35% Trichloroacetic Acid Pell (31:21)
ــــ
VCD 3: Combined Resurfacing Technique for Aone Scarring (10:18) Botox Reconstitution and Injection Sequence (20:53) - Carbon Dioxide Laser Resurfacing (8:10)
ــــ 2000
VCD 4: Postoperative Care of the Chemical Peel Patient (31:21) VCD 5: Transconjunctival Lower-Lid Blepharoplasty (9:05) Skin-Muscle Flap Lower-Lid Blepharoplasty with Midface Extension (16:20)
ــــ
VCD 6: Follicular Transfer Hair Transplantation Session (30:20)
ــــ
VCD 7: Upper-Lid Blepharoplasty (11:25) - Chin Augmentation with Gore-Tex Alloplast (13:21)
ــــ
VCD 8: Minimal Incision Brow and Midface Lift (31:02)
ــــ
VCD 9: Primary Facelift (37:17)
ــــ
VCD 10: Secondary Facelift with Gore-Tex Sling (30:21)
ــــ ــــ
VCD 11: Scalp Reduction Sessions (31:47)
26.15 LAPAROTOMY (Royal Society of Medicine in association with Royal College of Surgeons of England) (VCD)
ــــ
27.15 Lipostructure (Sydncy Coleman, M.D.) (byron) (VCD)
ــــ
28.15 Lower Body Lift (Abdominoplasty) (Lockwood, M. d., Kansas Gity) (VCD) (CD I , II)
ــــ
29.15 MALAR AUGMINTATION (CLINICAL MIRASIERRA MADRID)
ــــ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(Ulrich T. Hinderer Dr. Juan L. Del Rio) (VCD)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
62 30.15 Mammary augmention by High-Cohesive Silicon Gel Implant
ــــ
(Igar Nicchajev, Goran Jurell)
31.15 Mastery of Endoscopic & Laparoscopic Surgery (Second Edition)
2005
32.15 NMS Surgery Tutor
2000
(Dereck Mooney, T. Mack Brown, Cristian Jansenson, Denise Riedlinger)
ــــ
33.15 Open Repair of Abdominal Wall Hernias Using Prosthetic materials (Arthur I. Gilbert, M.D.)
-Small Bowel Obstrution Immediately Following Laparoscopic Herniorraphy (Karl A. Zucher, MD) -VJGS Case Study: Laparoscopic Loop Ilestomy for Temporary Fecal Diversion (Steven D. Wexner, Petachia Reissman) -VJGS Consultants Corner: Managed Care Update, Pt, III (Michael A. Wood) 34.15 Plastic and Reconstructive Breast Surgery (Second Edition) (Volume 1 , 2)
ــــ
35.15 Plug Repair for Inguinal Hernias 1- First Case: Inguinal Hernia type "Direct" 25.6 Practical MINOR SURGERY
ــــ 2- Second Case: Injuinal Hernia type "Indirect"
ــــ 2005
36.15 Principles of Surgery (Eight Edition) (Schwartz's) (E-Book) (CD I , II) Part1: Basic Considerations Part II: Specific Considerations 37.15 Single Puncture Laparoscopic Technique (Marco Pelosi, MD) (VCD)
ــــ 2004
38.15 Structural Fat Grafting (Sydney R. Caleman) (E-book & Film) 39.15 Submitted Subject: Transvaginal Sonographic Assessment of Pelvic Pathology: Preoperative Evaluation 40.15 SURGERY (John D Corson, Robin CN Willimson) -Surgical Principles and Critical Care
-Trauma
(Frances R. Batzer, MD)
(Launching Slide Vision) (Mosby)
-Gastrointestinal surgery
-Vascular Surgery
-Brast and Endoceine Surgery
-Transplantation Surgery
41.15 Surgery of the Liver & Biliary Tract 3e: Selected Operative Procedures (L.H. BLUMGART, Y. FONG)
-Allied Surgical Specialties
(W.B. Saunders)
-Hepatic Procedures -Biliary Procedures -Special Procedures The Distal Splenorenal Shunt: Effective or Obsolete? (VIDEO JOURNAL OF GENERAL SURGERY) (Layton Fredrick Rikkers, M.D.) (VCD) 42.15 - Options for Treating Portal Hypertension -HIPS Advantages
-Ideal Candidates for Distal Splenorenal Shunt -HIPS Disadvantages
ــــ ــــ 2000 ــــ
-Components of Distal Splenorenal Shunt Procedure -Distal Splenorenal Shunt Patency
43.15 The Ileana Pull-through Operative Prpcedure of Ulcerative Colitis: Eliminating the Permanent Ileostomy (Eric W. Fonkalseud, M.D.) (VCD)
ــــ
44.15 The Massachusetts General Hospital Handbook of Pain Management (Second Edition)
ــــ
- General Considerations - Acute Pain
- Diagnosis of Pain - Chronic Pain
- Therapeutic Options: Pharmacologic Approaches - Pain Due to Cancer
(Jane Ballantyne, Scott M. Fishman, Salahadin Abdi) (SALEKAN-E-book)
- Therapeutic Options: Nonpharmacologic Approaches - Special Situations - Apendices - Subject Index
45.15 TISSUE ADHESIVES In Wound Care (James V. Quinn, M.D., FACEP)
ــــ 2004
46.15 Tissue Glues in Cosmetic Surgery (RENATO SALTZ, M.D., DEAN M. TORIUMI, M.D.) 47.15 Tolaryngology Surgery for Fronatal Sinus Disease 48.15
Video Journal General Surgery
(Professor & Chairman, Bobby R. Alford, M.D.) (VCD)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ــــ
(VCD)
1. Reflux Disease and Nissen Fundoplication (Philip E. Donahue, MD) 2. Supraceliac Aortic-Celiac Axis-Superior Mesenteric Artery Bypass
ــــ
(Gregorio, Leonardo, Brent, Charles)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
63 ــــ
)(VCD
Video Journal General Surgery
)Open Repair of Abdominal Wall Hernias Using Prosthetic materials (Arthur I. Gilbert, M.D. )Small Bowel Obstrution Immediately Following Lapatoscopic Herniorraphy (Karl A. Zucker, MD )Laparoscopic Loop Ileostomy For Temporary Fecal Diversion (Steven D. Wxner, MD, Petachia Reissman, MD )Consultants Corner: Managed Care Update, Pt, III (Michael A. Wood
49.15
1. 2. 3. 4.
-١٦ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ
ﻋﻨﻮﺍﻥ CD
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
Burkect's Oral Medicine Diagnosis and Treatment
ــــ ــــ ــــ
ﭼﮕﻮﻧﮕﻲ ﺗﺸﺨﻴﺺ ﻭ Mangeﻛﺮﺩﻥ ﺑﻴﻤﺎﺭﺍﻥ -ﺍﺧﺘﻼﻻﺕ ﺗﻤﭙﻮﺭﻭﻣﻨﺪﻣﺒﻮﻻﺭ ﻭ Manageﺁﻧﻬﺎ -ﻣﻼﺣﻈﺎﺕ ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ ﺩﺭ ﺑﻴﻤﺎﺭﺍﺕ ﺩﺍﺭﺍﻱ ﺑﻴﻤﺎﺭﻱ ﺳﻴﺴﺘﻤﻴﻚth Caratera's Clinical PERIODONTOLOGY 9 Edition Textbookﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ ﻭ ﭘﺮﻳﻮﺩﻭﻧﺘﻮﻟﻮﮊﻱ -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﻟﺜﻪ ﻧﺮﻣﺎ -ﻃﺒﻘﻪﺑﻨﺪﻱ ﺑﻴﻤﺎﺭﻱ ﻟﺜﻪ ﻭ PPLﻭ – ...ﻧﺤﻮﻩ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻟﺜﻪ ﻭ PDL)COLOR ATLAS OF Dental Medicine Aesthetic Dentistry (Josef Schnidsedes
3.16
Color Atlas of Endodontics
4.16
ﻋﻨﺎﻭﻳﻦ ﻣﻬﻢ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: ﺍﻃﻠﺲ ﺭﻧﮕﻲ ﺩﺭﻣﺎﻥﻫﺎﻱ ﺩﻧﺪﺍﻧﻲ -ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ ﺯﻳﺒﺎﻳﻲ -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﻣﺘﺎﻝ ﻛﺮﺍﻭﻧﻬﺎ ﻭ ﺭﻭﺵﻫﺎﻱ ﻛﺮﺍﻭﻥﻛﺮﺩﻥ -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﺳﺮﺍﻣﻴﻚ ﻛﺮﺍﻭﻥﻫﺎ -ﺩﺭﻣﺎﻥﻫﺎﻱ ﻗﺒﻞ ﺍﺯ ﺗﺮﻣﻴﻢ -ﻛﺎﻣﭙﺎﺯﻳﺖ ﺍﻓﻴﻠﻪ )ﻣﺰﺍﻳﺎ ﻭ ﻣﻌﺎﻳﺐ( – (PFM) -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﻭﻧﻴﺮﻭ ﺭﻭﺵﻫﺎ ﻭ ﺍﺻﻮﻝ ﻭﻧﻴﺮﻛﺮﺍﻭﻥ
ــــ
1.16
-ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺺ -ﺭﻭﺵﻫﺎﻱ - Acsessﺗﺸﺨﻴﺺ ﻭ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﻃﻮﻝ ﻛﺎﻧﺎﻝ ﺭﻳﺸﻪ
ــــ -ﺍﺭﺗﻮﺩﻭﻧﺴﻲ ﻧﻮﻳﻦ Textbook -ﺍﺭﺗﻮﺩﻭﻧﺴﻲ ﺩﺭ ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ -ﻣﺸﻜﻼﺕ ﺍﺭﺗﻮﺩﻭﻧﺴﻲ
)(William T. Johnson DDS.MS ﺁﻣﺎﺩﻩﻛﺮﺩﻥ ﻛﺎﻧﺎﻝ ﻭ – ...ﺩﺭﻣﺎﻥ ﻣﺠﺪﺩ )(RetreatmentContemporary Orthodontics PROFFIT -ﻧﺤﻮﻩ ﺗﻜﺎﻣﻞ ﺍﻳﺮﺍﺩﺍﺕ ﺍﺭﺗﻮﺩﻭﻧﺴﻲ -ﺗﺸﺨﻴﺺ ﻭ ﻃﺮﺡ ﺩﺭﻣﺎﻥ
2.16
5.16
ﻣﻜﺎﻧﻴﺴﻢﻫﺎ ﻭ ﺑﻴﻮﻣﻜﺎﻧﻴﺴﻢﻫﺎ -ﺍﺧﺘﻼﻻﺕ TMJﻭ ..Craniofacial Development
6.16
Critical Decisious in Periodoutology
7.16
ــــ
Dental Assisting ﺁﻣﻮﺯﺵ ﺑﻪ ﺻﻮﺭﺕ ﺗﺼﻮﻳﺮﻱ -ﻛﻠﻴﻪ ﺭﻭﺵﻫﺎﻱ ﻛﻨﺘﺮﻝ ﻋﻔﻮﻧﺖ ﺩﺭ ﻣﻄﺐ -ﺭﻭﺵﻫﺎﻱ ﻓﻠﻮﺭﺍﻳﺪﺗﺮﺍﭘﻲ -ﺭﻭﺵﻫﺎﻱ ﻣﻌﺎﻳﻨﻪ ﻭ Positionﺑﻴﻤﺎﺭ ﻭ ﺩﻧﺪﺍﻧﭙﺰﺷﻚ -ﺭﻭﺵ ﺻﺤﻴﺢ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ) Instromentﻗﻠﻢﻫﺎ( -ﺭﻭﺵ ﻧﺼﺐ ﺭﺍﺑﺮﺩﻡ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺻﺤﻴﺢ ﺍﺯ ﺁﻥ ﺭﻭﺵﻫﺎﻱ ﺻﺤﻴﺢ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻲ ﮔﺮﻓﺘﻦ ﻭ ﻧﺤﻮﻩ ﻇﻬﻮﺭ ﺁﻧﻬﺎ ﻭ ﻛﻨﺘﺮﻝ ﻋﻔﻮﻧﺖ ﺗﺎﺭﻳﻜﺨﺎﻧﻪ -ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ Dessingﻭ ﻧﺤﻮﻩ ﺑﺮﺩﺍﺷﺘﻦ ﺁﻥDental Implant System -ﺍﻳﻨﺘﺮﻭﻣﻨﺖ -ﺁﻧﺎﻟﻴﺰ ﻭ ﺑﺮﺭﺳﻲ ﺭﻭﺵ ﻛﺎﺭ -ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ -ﺗﺮﻣﻴﻢ ﻭ ﺁﻣﻮﺯﺵ ﺑﻴﻤﺎﺭ
8.16
ــــ
)Dental Implant System Fixed Implant Restorations (ITI Dental Implant System) (VCD
10.16
ــــ
Endodontics
11.16
ــــ
)Endodontics 5 Edition (John I. Ingle, DDS, MSD, Leif K. Bakland, DDS
12.16
ــــ
)ESSENTIAL OF ORAL MEDICINE (Silverman, Roy Eversole, Truelove ﺑﺮﺭﺳﻲ ﺩﺭ ﺩﻫﺎﻥ ﺳﺮ ﻭ ﺻﻮﺭﺕ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺁﻣﻮﺯﺷﻲ ﻫﻤﺮﺍﻩ ﺑﺎ Caseﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻭ ﭘﺮﺳﺶ ﻭ ﭘﺎﺳﺦ ﻧﻜﺎﺕ ﺿﺮﻭﺭﻱ ﻓﺎﺭﻣﺎﻛﻮﻣﻮﺭﻋﻲ .aﺑﺮﺭﺳﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺳﻴﺴﺘﻤﻴﻚ ﻭ ﺗﻈﺎﻫﺮﺍﺕ ﺩﻫﺎﻧﻲ ﺁﻧﻬﺎ )ESTHETIC DENTISTRY 2th Edition (Dennet W. Aschheim, Barry G. Dale ﺍﺻﻮﻝ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ-١ :ﺗﺮﻣﻴﻢﻫﺎﻱ ﻛﺎﻣﭙﺎﺯﻳﺖ -٢ﺳﺮﺍﻣﻴﻚ -ﻣﺘﺎﻝ -٣ﭼﻴﻨﻲ ﻓﻮﻝﻛﺮﺍﻭﻥ -٤ﻭﻳﻨﻴﺮ ) -٥ (PFMﺭﺯﻳﻨﺖﻫﺎﻱ ﭼﺴﺒﻨﺪﻩ -٦ﺑﻠﻴﭽﻴﻨﮓ )ﺳﻔﻴﺪﻛﺮﺩﻥ ﺩﻧﺪﺍﻥﻫﺎ( -٧ﺍﻳﻤﭙﻠﻨﺖ ﻭ ﺟﺮﺍﺣﻲ ﺩﻫﺎﻥ ﻭ ﺻﻮﺭﺕ
13.16
ــــ ﺳﻴﻨﻮﺱﻫﺎﻱ ﭘﺎﺭﺍﻧﺎﺯﺍﻝ -ﻣﻨﺪﻳﺒﻮﻝ ﻭ ...ــــ -ﺑﺮﺭﺳﻲﻫﺎﻱ ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ -ﺳﺎﺑﻘﻪ ﺑﻴﻤﺎﺭ -ﻧﺤﻮﻩ ﺷﻨﺎﺳﺎﻳﻲ ﺿﺎﻳﻌﺎﺕ
ــــ
ــــ
-ﻃﺮﺡ ﺩﺭﻣﺎﻥﻫﺎﻱ ﻣﻮﺭﺩ ﻧﻴﺎﺯ
)(Walte R.B.HALL -ﺩﺭﻣﺎﻥﻫﺎﻱ ﺟﺮﺍﺣﻲ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﺩﺭ ﭘﺮﻳﻮﺩﻭﻧﺘﻴﻜﺲ ﻭ ﺯﻳﺒﺎﻳﻲ
ﺍﻳﻨﺘﺪﻭﻣﻨﺖﻫﺎﻱ ﺟﺪﻳﺪ – Shaping - Cleaningﻭ ﺁﺩﺍﭘﺘﻪﻛﺮﺩﻥ ﺭﻭﺕﻛﺎﻧﺎﻝ ﻭ ...th
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
9.16
14.16
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
64 ــــ ــــ
-١ﺟﺎﻳﮕﺰﻳﻨﻲ ﺗﻚﺩﻧﺪﺍﻧﻲ ﺑﺎ ﺍﻳﻤﭙﻠﻨﺖ ITI
)Esthetic Implant Dentistry (Daniel Buser, Hans Peter Hirt) (VCD
15.16
)ESTHETIC IMPLANT DENTISTRY (Daniel A. Bases, Urs.E.Belses
16.16
-٢ﺍﻳﻤﭙﻠﻨﺖ ﺩﻧﺪﺍﻧﻲ ﺗﻴﺘﺎﻧﻴﻮﻡ ﺑﺎ ﭘﻮﺷﺶ TPS
ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻣﻞ ﻭ ﻧﺤﻮﺓ ﺟﺎﻳﮕﺬﺍﺭﻱ ﺍﻳﻤﭙﻠﻨﺖ – ﻣﺰﺍﻳﺎ ﻭ ﻣﻌﺎﻳﺐ ﺍﻧﻮﺍﻉ ﺍﻳﻤﭙﻠﻨﺖﻫﺎ -ﺑﺮﺭﺳﻲ ﺑﺎﻓﺖ ﻧﺮﻡ ﻗﺒﻞ ﺍﺯ ﺍﻧﺠﺎﻡ ﺍﻳﻤﭙﻠﻨﺖ ﻭ ﺑﺮﺭﺳﻲ ﺩﺭﺻﺪ ﻣﻮﻓﻘﻴﺖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. )Esthetic in Dentistry (Vol 1- Vol 2
17.16
)ESTHETICS IN DENTISTRY (Second Edition
18.16
Glossary of Orthodontic Terms
19.16
)Guide to Physical Examination (Mosby
20.16
Implant Medpor Mandibular A method to Restore Skeletal Support to the Lower Face
21.16
ITI Dental Implant
22.16
)ITI TE Solution ITI TE Implant (DENTAL IMPLANT SYSTEM) (Daniel Buser) (Disk 1-3
23.16
Journal of Esthetic & Restorative Dentistry -٦ﺑﺮﺭﺳﻲ ﺭﻭﺵﻫﺎ -٧ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ -٨ﺑﻠﻴﭽﻴﻨﮓ
24.16
)LINGUAL ORTHODONTICS (Rafi Romano) (TO EXPLORE THE CD-ROM
25.16
)Local Anesthesia in Dentistry (VCD -ﺑﺮﺭﺳﻲ ﺭﻭﺵﻫﺎﻱ ﺻﺤﻴﺢ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﺎﻭﻳﺮﻱ ﮔﻮﻳﺎ ﺑﻪ ﺻﻮﺭﺕ ﻋﻤﻠﻲ -ﺧﻄﺮﺍﺕ ﻣﻮﺟﻮﺩ ﻭ ﺍﻳﺮﺍﺩﺍﺕ
26.16
)Local Anesthesia in Dentistry (Dr. Markus D. W. Lipp Wolfgang Kelm) (VCD
27.16
My Orthodontics
28.16
Oral Disease Diagnosis & Treatment
29.16
Oral Pathology 4th edition
30.16
Orthodontics & Paediatric Dentistry
31.16
Orthodontics Priociples & Techniques 3th Edition
32.16
)Pathways of the PMP (8th Edition
33.16
)PERIODONTAL MEDICINE (L.F. Rose, R.J.Genco, B.L. Mealey, D.W. Cohen
34.16
Periodontal Surgery
35.16
ــــ -ﻣﺎﻝ ﺍﻛﻠﻮﮊﻱ
ﻣﺸﻜﻼﺕ ﺯﻳﺒﺎﻳﻲ ﺗﻚﺩﻧﺪﺍﻧﻲ -ﺍﺯ ﺩﺳﺖﺩﺍﺩﻥ ﺩﻧﺪﺍﻥ1998
PRINCIPLES COMMUNICATIONS TREATMENT METHODS
)(John Daskalogiannakis
ــــ ــــ
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺮﺭﺳﻲ ﺑﻬﺪﺍﺷﺖ ﺩﻫﺎﻧﻲ ﻭ ﺑﺮﺭﺳﻲ ﭼﻨﺪﻳﻦ Caseﻫﻤﺮﺍﻩ ﺑﺎ ﻋﻜﺲﻫﺎ ﻭ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻲﻫﺎﻱ ﺩﻫﺎﻧﻲ ﺭﺍ ﺗﻮﺿﻴﺢ ﻣﻲﺩﻫﺪ. )(Oscar M. Ramirez M.D., F.A.C.S.) (POREX) (VCD
ــــ
)(CD I , II , III
ــــ -ﻛﻠﻴﻪ ﻣﺮﺍﺣﻞ ﺁﻣﺎﺩﻩﺳﺎﺯﻱ
-ﻭﺳﺎﻳﻞ ﻣﻮﺭﺩ ﻧﻴﺎﺯ
-ﻧﺤﻮﻩ ﺟﺮﺍﺣﻲ ﻟﺜﻪ ﻭ ﻓﻚ ﻭ ﺁﻣﺎﺩﻩﺳﺎﺯﻱ ﻣﺤﻞ
2004 ــــ -١ﺑﺮﺭﺳﻲ ﻛﺎﻣﻞ ﺍﻧﻮﺍﻉ ﺍﻧﻮﺍﻉ ﺗﺮﻳﺲﻫﺎ -٢ﮊﻭﺭﻧﺎﻝ ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ ﺗﺮﻣﻴﻤﻲ ﻭ ﺯﻳﺒﺎﻳﻲ -٩ﻋﻜﺲﻫﺎﻱ ﻛﺎﻣﻞ ﺍﺯ ﻣﺮﺍﺣﻞ ﺗﺮﻣﻴﻢ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ
-٣ﺳﺮﺍﻣﻴﻚ ﺍﻳﻨﻠﻪ ﻭ ﺍﻧﻠﻪ -٤ﻛﺎﻣﭙﺎﺯﻳﺖ ﺭﺯﻳﻦ -٥ﻛﺎﻣﭙﺎﺯﻳﺖ ﺭﺯﻳﻦ Packable Crown -١١ﺗﻤﺎﻡ ﺳﺮﺍﻣﻴﻚ Post -١٠
1998 ــــ ﺭﻭﺵﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺗﺰﺭﻳﻖ ﺑﺎ ﺍﻫﺪﺍﻑ ﻣﺘﻔﺎﻭﺕ ﺑﺮﺍﻱ ﺑﻲﺣﺴﻲ ﻧﻮﺍﺣﻲ ﻣﺨﺘﻠﻒ ﺩﻧﺪﺍﻥﻫﺎ ﻭ ﻟﺜﻪ ﻭ ﺑﺎﻓﺖ ﻧﺮﻡــــ ــــ -ﺑﺮﺭﺳﻲ ﻣﺮﺍﺣﻞ ﻣﻌﺎﻳﻨﻪ -ﻗﺒﻞ ﺍﺯ ﺩﺭﻣﺎﻥ ،ﻃﻲ ﺩﺭﻣﺎﻥ ،ﺑﻌﺪ ﺍﺯ ﺩﺭﻣﺎﻥ
-ﻧﺘﺎﻳﺞ ﺣﺎﺻﻠﻪ ﺍﺯ ﺩﺭﻣﺎﻥ ،ﻣﺮﺍﻗﺒﺖﻫﺎﻱ ﺣﻴﻦ ﺩﺭﻣﺎﻥ -ﺩﺍﺭﺍﻱ ﻟﻴﻨﻚﻫﺎﻱ ﻣﺘﻌﺪﺩ ﻭ ﺁﺩﺭﺱﻫﺎﻱ ﺟﺎﻟﺐ ﺳﺎﻳﺖﻫﺎﻱ ﺍﺭﺗﻮﺩﻭﻧﺴﻲ
ــــ ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﺿﺎﻳﻌﺎﺕ ﺩﻫﺎﻥ -ﺿﺎﻳﻌﺎﺕ ﺳﻔﻴﺪ ﺁﺑﻲ ﻗﺮﻣﺰــــ ــــ
-ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻭﺯﻳﻜﻮﻟﻮﺑﻮﻟﻮﺯ
ﺑﺮﺭﺳﻲ ﺑﻴﺶ ﺍﺯ Case ٥٠ﻣﺘﻔﺎﻭﺕ -ﺑﺮﺭﺳﻲ ﺑﻪ ﺻﻮﺭﺕ ﺁﺯﻣﻮﻥ ﻫﻤﺮﺍﻩ ﺑﺎ ﺟﻮﺍﺏ ﺻﺤﻴﺢ -ﻣﺎﻝ ﺍﻛﻠﻮﮊﻥ Mixed dentition-
-ﺷﺮﺍﻳﻂ ﺯﺧﻢﻫﺎ
-ﺍﺧﺘﻼﻻﺕ ﺭﻧﮕﺪﺍﻧﻪﺍﻱ
-ﺿﺎﻳﻌﺎﺕ ﺑﺎﻓﺖ ﻫﻤﺒﻨﺪ
-ﻣﻄﺎﻟﻌﺔ ﺟﺰﺋﻴﺎﺕ ﻭ ﻣﻼﺣﻈﺎﺕ ﻭ ﻣﺸﺨﺼﺎﺕ ﺑﻴﻤﺎﺭ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﻮﻳﺮ
-ﻣﺎﻝ ﺍﻛﻠﻮﮊﻥ ﻭ ﺍﺧﺘﻼﻻﺕ TMJ
ــــ -ﺗﺸﺨﻴﺺ ﻭ ﻃﺮﺡ ﺩﺭﻣﺎﻥ ﺩﺭ ﺍﺭﺗﻮﺩﻭﻧﺴﻲ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺩﺭﻣﺎﻥ
-ﻭﺍﻛﻨﺶﻫﺎﻱ ﺑﺎﻓﺖﻫﺎ
-ﻛﻴﺴﺖﻫﺎ ﻭ ﺗﻮﻣﻮﺭﻫﺎ
-ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺍﺳﺘﺨﻮﺍﻥ -ﺍﺧﺘﻼﻻﺕ TMJﻭ ﺑﻴﻮﻣﻜﺎﻧﻴﺴﻢﻫﺎ
ــــ Part III: Related Clinical Topics
2000
Part II: The Science of Endodoutics
ــــ ﺟﺮﺍﺣﻲ ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ -ﺣﺬﻑ ﭘﺎﻛﺖ ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ -ﺑﺮﺭﺳﻲ ﺗﺤﻠﻴﻞ ﻟﺜﻪ ﺩﺭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ ﻛﻮﺭﺗﺎﮊ -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺮﻳﻮﺩﻭﻧﺸﻴﻢ -ﺩﺭﻣﺎﻥﻫﺎ ﻭ ﺁﻣﻮﺯﺵ ﺑﻬﺪﺍﺷﺖ ﭘﺲ ﺍﺯ ﺩﺭﻣﺎﻥﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
Part I: The Art of Endodoutics
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
65 ــــ
36.16
Periodontal Surgery Clinical Atlas
37.16
Removal Orthodontics Apliances
38.16
Saunders Dental Assisting (Multimedia Resource) (Second Edition) (Doni L. Bird , Debbie S. Robinson)
39.16
Strauman Dental Implant System (VCD)
40.16
The Center of Education, Teaching and Research for Oral Implant Reconstruction (Prof. Dr. Hns L. Grafelmann) (CD I , II) - Vertical Load -Pitt-Easy BIO OSS -Phase TPS Cylinder Implant
ــــ
41.16
The Entegra Dental Implant System Entegra Surgical Videos (Robert Schroering)
ــــ
42.16
The IMZ Implant System (VCD) (Dr. Karl-Ludwing Ackermann, Dr. Axel Kirsch)
ــــ
43.16
Toothcolored Restoratives
44.16
TOOTH-COLORED RESTORATIVES Ninth Edition (Principles and Techniques)
45.16
Treatment Planning in Dentistry
46.16
Treatment Planning in Dentistry (Stephen Stefanac, D.D.S., M.S.Sam Nesbit, D.D.S., M.S.)
ــــ
47.16
UCD Implant
ــــ
. ﻫﻤﺮﺍﻩ ﺑﺎ ﻣﺮﺍﺣﻞ ﻻﺑﺮﺍﺗﻮﺍﺭﻱ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻣﻞ ﻭ ﺗﺼﻮﻳﺮﻫﺎﻱ ﻛﺎﻣﻞ ﺍﺯ ﺗﻤﺎﻡ ﻣﺮﺍﺣﻞIII ﻭII ﻭI ﻣﺨﺘﻠﻒ ﺍﻋﻢ ﺍﺯ ﻛﻼﺱCase ﺑﺮﺭﺳﻲ ﺩﻫﻬﺎ
ــــ 2003 ــــ
ﺍﻳﻤﭙﻠﻨﺖ ﭼﻨﺪ ﺩﻧﺪﺍﻧﻲ ﻣﺎﮔﺰﻳﻠﺪ- ﭘﻴﻦﮔﺬﺍﺭﻱ ﺩﺭ ﺍﺳﺘﺨﻮﺍﻥ ﺍﻟﻮﺋﻞ- ﻧﺤﻮﻩ ﺁﻣﺎﺩﻩﺳﺎﺯﻱ ﻧﺴﺞ ﻧﺮﻡ ﻭ ﺳﺨﺖ ﺑﺮﺍﻱ ﺍﺳﺘﻘﺮﺍﺭ ﺍﻳﻤﭙﻠﻨﺖ-
(CD I , II)
ــــ
ﻭ ﺩﻧﺪﺍﻥ ﻧﻴﺎﺯﻣﻨﺪ ﺑﻪ ﺗﺮﻣﻴﻢCase ﻧﺤﻮﻩ ﺗﺸﺨﻴﺺ ﻭ ﺍﻧﺘﺨﺎﺏ-
ﺍﺻﻮﻝ ﻭ ﺗﻜﻨﻴﻚﻫﺎ-
ﺑﺮﺭﺳﻲ ﻣﻮﺍﺩ ﻣﺨﺘﻠﻒ ﺩﺭ ﺗﺮﻣﻴﻢ ﻫﻤﺮﻧﮓ ﻣﺰﺍﻳﺎ ﻭ ﻣﻌﺎﻳﺐ2002
(Harry F. Albers, DDS) ﺩﺍﺭﺍﻱ ﺁﺯﻣﻮﻥﻫﺎﻱ ﺟﺎﻟﺐ ﻭ ﻛﺎﻣﻞ-
ﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻫﻤﺮﺍﻩ ﺑﺎ ﭘﺮﻭﻧﺪﻩﻫﺎﻱ ﻛﺎﻣﻞCase ﺑﺮﺭﺳﻲ-
ــــ
... ﻧﺤﻮﻩ ﺟﺎﻳﮕﺬﺍﺭﻱ ﭘﻴﻦﻫﺎ ﻭ- ﺁﻣﺎﺩﻩﺳﺎﺯﻱ ﻧﺴﺞ ﻧﺮﻡ ﻭ ﻧﺤﻮﻩ ﺍﻳﺠﺎﺩ ﻓﻠﭗ ﻭ ﻧﺤﻮﻩ ﺁﻣﺎﺩﻩﺳﺎﺯﻱ ﻧﺴﺞ ﺍﺳﺘﺨﻮﺍﻥ- ﺭﻭﺵﻫﺎﻱ ﺑﻲﺣﺴﻲ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ:١٧
1.17 ANATOMY & PHYSIOLOGY (5 Edition) th
(Gary A. Thibodeau, Kevin T. Patton) 2.17 BODY WORKS 6.0 A 3D Journey Through The Human Anatomy 3.17 Interactive Guide to Human Neuroanatomy (Mark F. Bear, Barry W. Connors, Michael A. Paradiso) Atlas: -Surface Anatomy of Brain Exam:I -Surface Anatomy of the Brain
4.17
6.17
-The Spinal Cord -The Anatomy Nervous System -Comprehensive Exam
-The Cranial Nerves -The Blood Supply to the Brain
Interactive Physilogy MUSCULAR SYSTEM (A. D. A. M. Benjamin/Cummings) (Marvin J. Branstrom, Ph.D.) -Anatomy Review: Skeletal Muscle Tissue
5.17
-Cross-Sectional Anatomy of Brain -Cross-Sectional Anatomy of the Brain
ــــ ــــ 2002
-The Neuromuscular Junction
-Sliding Filament Theory
-Muscle Metabolism
-Contraction of Motor Units
ــــ -Contraction of Whole Musle
InterActive PHYSIOLOGY Cardiovascular System
ــــ
The Heart
Blood Vessels
Anatomy Review: The Heart Intrinsic Conduction System Cardiac Action Potential Cardiac Cycle Cardiac Output
Anatomy Review: Blood Vessel Structure and Function Measuring Blood Pressure Factors that Affect Blood Pressure
Interactive PHYSIOLOGY for Windows Urinary System
Blood Pressure Regulation Autoregulation and Capillary Dynamics
ــــ
Version 1.0
ﺏ( ﻋﺮﻭﻕ ﺧﻮﻧﻲ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ﺍﻟﻒ( ﻗﻠﺐ.ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺍﺭﺍﻱ ﺩﻭ ﻣﺒﺤﺚ ﻣﺠﺰﺍ ﻣﻲﺑﺎﺷﺪ ﻭ ﺍﻫﺪﺍﻑ ﺁﻣﻮﺯﺷﻲ ﺩﺭ ﺍﺑﺘﺪﺍﻱ ﻫﺮ ﻓﺼﻞ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
66 ﺧـﻮﺩﺗﻨﻈﻴﻤﻲ ﻭ ﺩﻳﻨﺎﻣﻴـﻚ، ﺗﻨﻈـﻴﻢ ﻓﺸـﺎﺭ ﺧـﻮﻥ، ﻓﺎﻛﺘﻮﺭﻫﺎﻱ ﻣـﺆﺛﺮ ﺑـﺮﺭﻭﻱ ﻓﺸـﺎﺭ ﺧـﻮﻥ، ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﻓﺸﺎﺭ ﺧﻮﻥ، ﺳﺎﺧﺘﺎﺭ ﻭ ﻋﻤﻠﻜﺮﺩ ﻋﺮﻭﻕ ﺧﻮﻧﻲ: ﺏ( ﻋﺮﻭﻕ ﺧﻮﻧﻲ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ. ﭼﺮﺧﺔ ﻗﻠﺒﻲ ﻭ ﺑﺮﻭﻥﺩﻩ ﻗﻠﺒﻲ، ﭘﺘﺎﻧﺴﻴﻞ ﻋﻤﻞ ﻗﻠﺒﻲ، ﺳﻴﺴﺘﻢ ﻫﺪﺍﻳﺘﻲ ﻗﻠﺐ، ﺁﻧﺎﺗﻮﻣﻲ ﻗﻠﺐ:ﺍﻟﻒ( ﻗﻠﺐ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ . ﺩﺍﺭﺍﻱ ﻳﻚ ﻓﻬﺮﺳﺘﻲ ﺍﺯ ﺍﺻﻄﻼﺣﺎﺕ ﺍﺳﺖ ﻭ ﻫﺮ ﻭﺍﮊﻩ ﺭﺍ ﻣﺨﺘﺼﺮﹰﺍ ﺗﻮﺿﻴﺢ ﻣﻲﺩﻫﺪCD ﺍﻳﻦ. ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺭﺋﻮﺱ ﻣﻄﺎﻟﺐ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﮔﻮﻳﻨﺪﻩ ﺁﻧﻬﺎ ﺭﺍ ﺑﻴﺎﻥ ﻣﻲﻛﻨﺪ.ﻣﻮﻳﺮﮒﻫﺎ . ﺳﺆﺍﻻﺕ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﭘﺎﺳﺦﻫﺎﻱ ﻧﺎﺻﺤﻴﺢ ﺑﺎ ﺭﻧﮓ ﻗﺮﻣﺰ ﻣﺸﺨﺺ ﻣﻲﺷﻮﻧﺪ،( ﺩﺭ ﻫﺮ ﻳﻚ ﺍﺯ ﻣﺒﺎﺣﺚ ﻓﻮﻕQuiz) ﺩﺭ ﺑﺨﺶ ﺍﻣﺘﺤﺎﻥ 7.17
Interactive Physiology RESPIRATORY SYSTEM (A. D. A. M. Benjamin/Cummings)
-Anatomy Reviw: Respiratory Structures 8.17 MedWorks Anatomy & Physilogy Anatomy Y Physiology: Overview The Endocrine System The Sensory Organs
-Pulmonary Ventilation
(Andrea K. Salmi)
-Gas Exchange
ــــ
-Gas Transport
-Control of Respiration ــــ
Cells and Tissues
The Integumentary System
Body Chemistry
The Skeletal System
The Muscula System
Cardiovascular System: The Blood Somatic and Autonomic Systems
Cardiovascular System, The Heart The Peripheral Nervous Systems
Lymphatic and Immune System
The Respiratory System The Digestive System
Inheritance
The central Nervous System
The Nervous System Organization The Urinary System
The Reproductive System
. ﺍﻧﺘﺨﺎﺏ ﻭ ﺍﺟﺮﺍ ﻛﻨﻴﺪMedwork ﺭﺍ ﺍﺯ ﻣﺴﻴﺮ ﺩﺍﻳﺮﻛﺘﻮﺭﻱSetup.exe ﻓﺎﻳﻞ،ﺑﺮﺍﻱ ﺍﺟﺮﺍ Panorama of Anatomy & Physiology Structure & Function of the Body (Eleven Edition) (Gary A. Thibodeau, Kevin T. Patton) (Time) 10.17 Range of Motion-AO Neutral-0 Method Measurement and Documentation
ــــ ــــ
9.17
2002
11.17 Sobotta (Atlas of Human Anatomy) (Urban & Schwarzenbery) 1. General Anatomy
2. Head and neck
3. Upper Limb
4. Brain and Spine Cord
Past ( ﺍﺟـﺮﺍ ﺷـﺪﻩSetup )ﻫﻤﺎﻥ ﻣﺴﻴﺮﻱ ﻛـﻪC:\Urban ﺭﺍ ﻛﭙﻲ ﻛﺮﺩﻩ ﻭ ﺩﺭSobotta 1.5Crack
5. Eye
6. Ear
7. Thoracic and Abdominal Wall
8. Thoracic Oegans
9. Lower Limb
ﻭ ﺳﭙﺲCrack ﻭﺍﺭﺩ ﺩﺍﻳﺮﻛﺘﻮﺭﻱ، ﭘﺲ ﺍﺯ ﺍﺗﻤﺎﻡ. ﺁﺑﻲﺭﻧﮓ ﺭﺍ ﺍﺟﺮﺍ ﻣﻲﻛﻨﻴﻢSetup ، English ﺟﻬﺖ ﻧﺼﺐ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺍﺑﺘﺪﺍ ﺍﺯ ﺩﺍﻳﺮﻛﺘﻮﺭﻱ:( ﻃﺮﻳﻘﺔ ﻧﺼﺐ . ﺣﺎﻝ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻓﻮﻕ ﻗﺎﺑﻞ ﺧﻮﺍﻧﺪﻥ ﻭ ﺍﺟﺮﺍﺳﺖ.ﻣﻲﻛﻨﻴﻢ 2003 ــــــ
12.17 Student Companion CD-ROM for Principles of Anatomy & Physiology (Tenth Edition) (John Willey & Sons, INC.) 13.17 The Interactive Skeleton Tutorial 1. Head
2. Spine
3. Ribs
(Dr. peter Abrahams of cambridger University, UK.) 4. Upper Limb
5. Lower Limb
14.17 World of SPORT examined
ــــ ﭘﺮﺳﺘﺎﺭﻱ:١٨
1.18 2.18 3.18 4.18 5.18 6.18
The Oncology Nursing Society presents THE ADVANCED PRACTICE ONCOLOGY NURSING REVIEW Textbook of MEDICAL SURGUCAL NURSING (Ninth Edition) (Katherine H. Dimmock) Student Self Study Disk to Accompany BRUNNER & SUDDARTH'S Focus on Nursing Pharmacology (Lippincott Williams & Wilkins) Wongs ESSENTIALS OF Pediatric Nursing (Mosby) A Harcoun Health Sciences Company Maternal, Neonatal and Women's Health Nursing By Delmar, a division of Thomson Learning Nursing Care of Infants and Children (Seven Edition)
ــــ ــــ 2000 2001 2002 2003
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ - Childre, Their Families, and the Nurse
- Family-Centered Care of the Newborn
- Family-Centered Care of the Infant
- Family-Centered Care of the Young Child - Family-Centered Care of the School-Age Child
- Family-Centered Care of the Adolescent
- Family-Centered Care of the Child with Special Needs
- The Child who is Hospitalized
- The Child with Problems Related to Transfer of Oxygen and Nutrients
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
- Assessment of the Child and Family - The Child with Disturbance of Fluid and Electrolytes
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
67 - The Child with Problems Related to Production & Circulation of Blood
- The Child with Disturbance of Regulatory Mechanisms
- The Child With a Problem that Interfers with Physical Mobility
McMinn's Interactive Clinical Anatomy 8.18 INRERACTIVE ATLAS OF CLINICAL ANATOMY (Illustrations by Frank H. Netter, M.D.) 7.18
ــــ ــــ
ﻓﻴﺰﻳﻮﺗﺮﺍﭘﻲ-١٩ 1.19 2.19 3.19
Clinical Tests for the Musculoskeletal System (Klaus Buckup, KlinikumDortmund Orthopaedic Hospital Dortmund Germany) (Salekan E-Book) DIET & FITNESS DIGITAL SHIATSU
2004 ــــ ــــ
: ﻗﺴﻤﺖ ﻣﻲ ﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ٦ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺍﺭﺍﻱ ﺭﺍﻫﻨﻤﺎ-
ﺍﺳﺎﺱ ﻭ ﻣﺒﺎﻧﻲ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ-
ﺟﺴﺘﺠﻮ-
(therapies) ﻣﻮﺍﺭﺩ ﻛﺎﺭﺑﺮﺩ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ-
(total body) ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﺗﻤﺎﻣﻲ ﺑﺪﻥ-
(self- shiatsu) ﺧﻮﺩ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ-
. ﺩﺭ ﺗﺼﺎﻭﻳﺮ ﻃﺮﺡﻭﺍﺭﻫﺎﻱ ﻧﻘﺎﻁ ﺣﺴﺎﺱ ﻛﻪ ﺩﺭ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﻣﻮﺭﺩ ﺗﻮﺟﻪ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺭﻭﺵ ﻣﺎﺳﺎﮊ ﺻﺤﻴﺢ ﻭ ﻋﻤﻠﻲ ﺗﻤﺎﻣﻲ ﺑﺪﻥ ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﻓﻴﻠﻢ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﮔﻮﻳﻨﺪﻩ ﻭ ﻣﺘﻦ ﭼﺎﭘﻲ ﺍﺭﺍﺋﻪ ﻣﻲ ﺷﻮﺩ-١ . ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﻓﻴﻠﻢ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﮔﻮﻳﻨﺪﻩ ﺩﺭ ﺩﻭ ﻗﺴﻤﺖ ﺭﻭﺵ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ-٢ (... ﮔﺮﻓﺘﮕﻲ ﻭ ﻛﺮﺍﻣﭗ ﭘﺎ ﻭ، ﻗﺎﻋﺪﮔﻲ، ﺍﺳﻬﺎﻝ، ﻳﺎﺋﺴﮕﻲ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﻠﻴﻮﻱ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﺒﺪﻱ، ﺧﻮﻥ ﺩﻣﺎﻍ، ﺳﻴﻨﻮﺯﻳﺖ، ﺩﺭﺩ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﻓﻠﺞ ﺻﻮﺭﺕ، ﺁﺭﺗﺮﻳﻮﺍﺳﻜﻠﺮﻭﺯ: ) ﺷﺎﻣﻞ. ﻣﻮﺭﺩ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ٢٢ ﻣﻮﺍﺭﺩ ﻛﺎﺭﺑﺮﺩ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﺩﺭ-٣ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖNamikoshi ﺍﺻﻮﻝ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﻭ ﺭﻭﺷﻬﺎﻱ ﻛﻼﺳﻴﻚ ﺁﻥ ﻭ ﻧﻴﺰ ﺗﺎﺭﻳﺨﭽﻪ ﻣﺘﺪ-٤ . ﺑﺮ ﺍﺳﺎﺱ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎﻳﻲ ﻣﻲ ﺗﻮﺍﻥ ﻭﺍﮊﻩﻫﺎﻱ ﺗﺨﺼﺼﻲ ﻣﻮﺭﺩ ﻧﻈﺮ ﺧﻮﺩ ﺭﺍ ﭘﻴﺪﺍ ﻧﻤﻮﺩ ﻭ ﺑﺎ ﻛﻠﻴﻚ ﻧﻤﻮﺩﻥ ﺑﺮ ﺭﻭﻱ ﺁﻥ ﺑﻪ ﺁﻥ ﻣﺒﺎﺣﺚ ﻣﻨﺘﻘﻞ ﺷﺪ-٥ . ﺍﺟﺮﺍ ﻣﻲ ﺷﻮﺩAutorun ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﻪ ﺻﻮﺭﺕ . ﻧﺼﺐ ﻣﻲ ﺷﻮﺩprogram ﺩﺭ ﮔﺰﻳﻨﻪLifestyle softuare Group ﺩﺭ ﻧﻬﺎﻳﺖ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﻪ ﻧﺎﻡ، ﺩﻭ ﺑﺎﺭ ﻛﻠﻴﻚ ﻧﻤﺎﺋﻴﺪ ﻭ ﻣﺮﺍﺣﻞ ﻧﺼﺐ ﺭﺍ ﭘﻴﮕﻴﺮﻱ ﻛﻨﻴﺪSetup.exe ﺟﻬﺖ ﻧﺼﺐ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻻﺯﻡ ﺍﺳﺖ ﺑﺮ ﺭﻭﻱ ﺁﻳﻜﻮﻥ:( ﻃﺮﻳﻘﺔ ﻧﺼﺐ
. ﻛﻠﻴﻚ ﻧﻤﺎﺋﻴﺪinstall.exe ﺑﺮﺍﻱ ﻧﺼﺐ ﺁﻳﻜﻮﻥ. ﻛﺎﻣﭙﻴﻮﺗﺮ ﺷﻤﺎ ﺑﻪ ﻛﺎﺭ ﻣﻲ ﺭﻭﺩDesktop ﻧﻴﺰ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﺑﺮﺍﻱ ﺳﻔﺎﺭﺷﻲ ﻧﻤﻮﺩﻥ ﺻﻔﺤﻪJurassic Park Entertainment ﻳﻚ ﺑﺮﻧﺎﻣﻪ ﺟﺎﻧﺒﻲ ﺑﻪ ﻧﺎﻡCD ﺩﺭ ﺍﻳﻦ 4.19
EXERCISE THERAPY PREVENTION AND TREATMENT OF DISEASE ( John Gormley and Juliette Hussey)
5.19
Fibromyalgia Syndrome Bodywork Management Strategies ٥ ﺳﭙﺲ ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺩﺭﻣﺎﻥ ﻓﻴﺒﺮﻭﻣﻴﺎﻟﮋﻳﺎ ﺑﺮ ﺍﺳﺎﺱ ﭘﺮﻭﺳﻪ ﺩﺭﻣﺎﻧﻲ ﭘﻴﺸﻨﻬﺎﺩ ﺷﺪﻩ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﺑﺪﻳﻦﺻﻮﺭﺕ ﻛﻪ ﺩﺭ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﺍﺭﺯﻳﺎﺑﻲ ﻛﻪ ﺷـﺎﻣﻞ. ﻛﻪ ﺩﺭ ﺯﻣﻴﻨﺔ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺩﺳﺘﻲ ﺍﺳﺖ ﻣﻌﺮﻓﻲ ﺷﺪﻩ ﺍﺳﺖLeon Chitow ﺍﺑﺘﺪﺍ ﺗﻌﺪﺍﺩﻱ ﺍﺯ ﻛﺘﺐCD ﺩﺭ ﺍﻳﻦ .ﺑﺨﺶ ﻣﻲﺑﺎﺷﺪ ﺑﺎ ﺗﺄﻛﻴﺪ ﺑﺮ ﻣﻬﺎﺭﺕﻫﺎﻱ ﻟﻤﺲ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ Assessment Methodes
6.19
Fundamentale of Sensation ad Perception (3rd Edition) (M.W. Levine)
(
- Manual Thermal Diagnosis
- Skin on Fascia Adherence
- Hyperalgesic Skin Zones reduced Skin elasticity
- Drag palpation for increased hydrosis
2005 ___
- Neuro muscular Technique Evaluation (NMT)
ــــ : ﻋﻨﻮﺍﻥ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ١٦ ﺷﺎﻣﻞCD ﻣﺤﺘﻮﺍﻱ ﺍﻳﻦ
Introduction and instructions Afterimages Depth from motion of random dots Traveling waves on the basilar membrane Gnglion Cells responding to light
Threshold experiment or Signal Detection Brain anatomy, Blink Suppression, or Cortical Cell responses Optical IIIusions and Constancies
Motion demonstrations
Retinal Cells responding to light Demonstratuins of Fourier components Color mixing or Opponent cells
Pitch and Loudness of tones
Speech sounds of Mystery phrase
Muscle spindle feedback
Motions from form of Impossible figures
Mechanics of the middle and inner ear
Taste-influenced by vision
7.19 Health & Fitness (DataSel Software, Inc) 1. Getting Started
2. The Exercise Demonstration Screen
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
3. Strength
4. Stretch
Specializations of the Vertebrate eye Cortical columns or Equiluminant demos
5. Equipment
6. Muscles
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
7. Workouts
8. Setup
9. Technical Support
ــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
68 8.19 Interactive Atlas of Human Anatomy
ــــ 2005 ــــــ
9.19 Introduction to Massage Therapy (Mary Beth Braum, Steplianic Simonsoon) (Salekan E-Book) 10.19 MANIPULATION OF THE SPINE, THORAX AND PELVIS An Osteopatic Perspective (Peter Gibbons, Philip Tehan)
ﺍﻳﻦ ﻓﻴﻠﻢﻫﺎ ﺩﺭ ﺩﻭ ﺑﺨﺶ ﻛﻠﻲ ﺑﻪ ﺷﺮﺡ ﺫﻳـﻞ. ﻓﻘﺴﺔ ﺳﻴﻨﻪ ﻭ ﻟﮕﻦ ﺧﺎﺻﺮﻩ ﻣﻲﺑﺎﺷﺪ، ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻧﻲ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕmanipulation ﻗﻄﻌﻪ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﻛﻮﺗﺎﻩ ﺩﺭ ﺧﺼﻮﺹ ﺗﻜﻨﻴﻚﻫﺎ ﻭ ﻧﺤﻮﺓ ﻣﻌﺎﻳﻨﺔ ﻓﻴﺰﻳﻜﻲ ﻭ٣٤ ﺑﺼﻮﺭﺕ ﻧﻤﺎﻳﺶCD ﺍﻳﻦ :ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﺑﺨﺶ ﺍﻭﻝ: HVLA thrust techniques-spine and thorax
- Cervical and cervicothoracie spine
-Thoracic spine and rib cage
-Lumbar and thora Columbar spine
ﺑﺨﺶ ﺩﻭﻡ: HVLA thrust techniques-pelvis . ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩAutorun ﺑﻪ ﺻﻮﺭﺕCD ﺍﻳﻦ. ﺭﺍ ﺑﺮ ﺭﻭﻱ ﺑﻴﻤﺎﺭ ﻧﻤﺎﻳﺶ ﻣﻲﺩﻫﺪmanipulafion ﭘﺰﺷﻚ ﻣﺘﺨﺼﺺ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻣﻌﺎﻳﻨﻪ ﻭ،ﺩﺭ ﻫﺮ ﻗﻄﻌﻪ ﻓﻴﻠﻢ 11.19 Massage Therapy Review
(interactive Edition) (Mosby)
ـــــ
12.19 Men's Health GET RID OF THAT GUT
STAGE 1: BEGINNERS LEVEL
STAGE 2: INTERMEDIATE LEVEL
13.19 MUSCLE ENERGY TECHNIQUES
STAGE 3: ADVANCED LEVEL 2001
ADVANCED SOFT TISSUE TECHNIQUES (Second Edition)
. ﺗﺼﻮﻳﺮ ﻭﻳﺪﺋﻮﺋﻲ ﻭﺟﻮﺩ ﺩﺍﺭﺩ٣٠ ﻓﺼﻞ ﺑﻪ ﻫﻤﺮﺍﻩ٨ ﻟﺌﻮﻥ ﭼﻴﺘﻮ ﻣﺸﺘﻤﻞ ﺑﺮMuscle Energy Techniques ﻣﺘﻦ ﻛﺎﻣﻞ ﻛﺘﺎﺏCD ﺩﺭ ﺍﻳﻦ ﺩﺭ ﺍﻳﻦ ﺗﻜﻨﻴﻚ ﺑﻴﻤﺎﺭ ﻧﻘﺶ ﻓﻌﺎﻟﻲ ﺩﺭ ﺍﺻﻼﺡ ﺍﺧﺘﻼﻻﺕ ﻋﻤﻠﻜﺮﺩﻱ ﺑﺮ ﻋﻬـﺪﻩ ﺩﺍﺭﺩ ﻭ. ﻳﻜﻲ ﺍﺯ ﺭﻭﺵﻫﺎﻱ ﺩﺭﻣﺎﻥ ﺩﺳﺘﻲ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺁﻥ ﺍﺯ ﺍﻧﻘﺒﺎﺽ ﺍﺭﺍﺩﻱ ﻋﻀﻠﻪ ﺩﺭ ﻳﻚ ﺟﻬﺖ ﻛﻨﺘﺮﻝ ﺷﺪﻩ ﻭ ﺩﻗﻴﻖ ﺑﺎ ﺷﺪﺕﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻭ ﺩﺭ ﺑﺮﺍﺑﺮ ﻧﻴﺮﻭﻱ ﺩﺭﻣﺎﻧﮕﺮ ﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩMET : ﺍﻳﻦ ﺗﻜﻨﻴﻚ ﻛﺎﺭﺑﺮﺩ ﺑﺎﻟﻴﻨﻲ ﺯﻳﺎﺩﻱ ﺩﺍﺭﺩ ﻛﻪ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺷﺎﺭﻩ ﻛﺮﺩ. ﺑﺎﻋﺚ ﻛﺎﻫﺶ ﺗﻮﻥ ﻳﺎ ﻣﻬﺎﺭ ﻋﻀﻼﺕ ﻛﻮﺗﺎﻩﺷﺪﻩ ﻭ ﺗﻘﻮﻳﺖ ﻋﻀﻼﺕ ﺿﻌﻴﻒ ﻣﻲﺷﻮﺩReciprocal inhibtion ﻳﺎPost isometric Relaxation ﺗﺮﺍﭘﻴﺴﺖ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﮔﻴﺮﺍﻓﺘﺎﺩﮔﻲ ﻣﻨﻴﺴﻚ ﻭ ﻋﺪﻡ ﺗﻄﺎﺑﻖ ﻛﺎﻣﻞ ﺳﻄﻮﺡ، ﺍﺻﻼﺡ ﻣﻮﺍﻧﻊ ﻣﻜﺎﻧﻴﻜﻲ ﺩﺍﺧﻞ ﻣﻔﺼﻞ ﻣﺜﻞ ﺁﺭﺗﺮﻳﺖ، ﻛﺎﻫﺶ ﺍﺩﻡ ﻣﻮﺿﻌﻲ، ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﭼﺴﺒﻨﺪﮔﻲ ﻣﺘﻌﺎﻗﺐ ﺍﺣﺘﻘﺎﻥ ﻭﺭﻳﺪﻱ، ﺭﻓﻊ ﺍﺣﺘﻘﺎﻥﻫﺎﻱ ﻭﺭﻳﺪﻱ، ﺗﻘﻮﻳﺖ ﻋﻀﻼﺕ ﺿﻌﻴﻒ،ﻛﺸﺶ ﻋﻀﻼﺕ ﻛﻮﺗﺎﻩ ﻭ ﺍﺳﭙﺎﺳﺘﻴﻚ ﻣﻔﺼﻠﻲ ﻭ ﻫﻤﭽﻨﻴﻦ ﻣﺘﺤﺮﻙﻧﻤﻮﺩﻥ ﻣﻔﺎﺻﻞ ﻣﺤﺪﻭﺩ 14.19 Myofascial Release Techniques
(John F. Barnes, PT) (VCD I , II) 15.19 Orthopaedics for Nurses (John Ebnezar) (Salekan E-Book) 16.19 Orthopedic Massage Theory and Technique (Whitney Lowe Leon Chaitow) 17.19 Palpation Skills for Muscles and Joints
ــــــ ــــ 2003 ــــــ
18.19 Physical Education and the Study of Sport (Bob Davis, Ros Bull, Jan Roscoe, Dennis Roscoe) (Mosby)
ــــــ
1- Physical Education and the Study of Sport
2- Synoptic Questions Harcourt Health Sciences
rd 19.19 Physical Rehabilitatioon of the Injured Athlete 3 Edition
20.19 Positional Release Techniques
3- The Project Personal Performance Profile
(James R. Andrews, Gary I., Harrison, Kevin) (Salekan E-Book)
ADVANCED SOFT TISSUE TECHNIQUES (Leon Chaitow) (Harcourt) (Second Edition)
2004 ــــــ
. ﺗﺼﻮﻳﺮ ﻭﻳﺪﺋﻮﺋﻲ ﺍﺯ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﻋﻤﺎﻝﺷﺪﻩ ﻭﺟﻮﺩ ﺩﺍﺭﺩ٣١ ﻓﺼﻞ ﻫﻤﺮﺍﻩ ﺑﺎ١٢ ﻟﺌﻮﻥ ﭼﻴﺘﻮ ﻣﺸﺘﻤﻞ ﺑﺮPositional Release ﻣﺘﻦ ﻛﺎﻣﻞ ﻛﺘﺎﺏCD ﺩﺭ ﺍﻳﻦ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻜﻲ ﺍﺯ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺆﺛﺮ ﺩﺭ ﺩﺭﻣﺎﻥ ﺑﺎﻓﺖ ﻫﻤﺒﻨﺪ ﻣﻨﺎﻃﻘﻲ ﻛﻪ ﺩﺭ ﻟﻤﺲ ﻫﺎﻳﭙﺮﺗﻮﻥ ﻳﺎ ﻛﻮﺗﺎﻩ ﺷﺪﻩﺍﻧﺪ ﺑﻜﺒﺎﺭ ﻣﻲﺭﻭﺩ ﻭ ﭼﻮﻥ ﺍﺳﺎﺱ ﺁﻥ ﻗﺮﺍﺭﺩﺍﺩﻥ ﺑﺎﻓﺖ ﻫﻤﺒﻨﺪ ﻳﺎ ﻋﻀﻠﻪ ﺩﺭ ﺭﺍﺣﺖﺗﺮﻥ ﻭﺿﻌﻴﺖ ﻣﻲﺑﺎﺷﺪ ﺑﻪﻛﺎﺭﺑﺮﺩﻥ ﺁﻥ ﺩﺭ ﻣﻮﺍﺭﺩﻳﻜﻪ ﺑﻪ ﻋﻠـﺖ ﺍﺳﭙﺎﺳـﻢ ﻳـﺎ ﺍﻟﺘﻬـﺎﺏPositional Release . ﻟﺬﺍ ﺩﺭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ ﻣﺸﻜﻼﺕ ﻣﺎﺳﻜﻠﻮﺍﺳﻜﻠﺘﺎﻝ ﺑﺴﻴﺎﺭ ﻣﺆﺛﺮ ﺍﺳﺖ.ﺑﺎﻓﺖ ﻫﻤﺒﻨﺪ ﺑﺴﻴﺎﺭ ﺩﺭﺩﻧﺎﻙ ﺍﺳﺖ ﺑﺮﺍﻱ ﺑﻴﻤﺎﺭ ﻗﺎﺑﻞ ﺗﺤﻤﻞ ﻣﻲﺑﺎﺷﺪ Spontaneous Positional relese variations
The evolution of dysfunction
Unloading and Proprioceptive taping
Modified strain/counterstrain technique
Learning SCS
SCS for muscle pain (plus INTT and self-treatment)
Goodheart and Morrison's Positional release variations and lift techniques
SCS (and SCS variations) in hospital settings
The Mulligan concept: NAGs, SNAGs, MWMs, etc.
Functional technique
Facilitated Positional release (FPR)
Cranial and TMJ Positional release methods
21.19 Power Touch
ــــــ
22.19 Principles of Manual Therapy (A Manual Therapy Approach to Musculoskeletal Dyslimction) (Salekan E-Book)
2005
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
69 23.19 Surface and Living Anatomy
2002
(Gordon Joslin SOtJ)
. ﺩﺭ ﻛﻨﺎﺭ ﻫﺮ ﻳﻚ ﺍﺯ ﻣﺘﻦﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﺑﻪ ﻭﺳﻴﻠﺔ ﻣﺎﺭﻛﺮﻫﺎﻳﻲ ﻣﻨﺎﻃﻖ ﻣﺮﺑﻮﻃﻪ ﺭﺍ ﻧﺸﺎﻥ ﻣﻲﺩﻫﻨﺪ. ﻣﻨﻄﻘﻪ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﺭﺍ ﻣﺮﺣﻠﻪ ﺑﻪ ﻣﺮﺣﻠﻪ ﺗﻮﺿﻴﺢ ﻣﻲﺩﻫﺪ٢٢٦ ﻣﺘﻦ ﻛﺎﻣﻞ ﺁﻧﺎﺗﻮﻣﻲ ﺳﻄﺤﻲ ﻗﺴﻤﺖﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻭ ﭘﻴﺪﺍﻛﺮﺩﻥCD ﺩﺭ ﺍﻳﻦ 24.19 The Complete Acupuncture
ــــ
25.19 The Principles of Harmonic Techniques
(Eyal Lederman)
(VCD)
ــــــ
ﺑﺮ ﺍﻳﻦ ﺍﺳﺎﺱ ﻛﻪ ﻫﺮ ﺳﻴﺴﺘﻤﻲ ﻳﻚ ﻓﺮﻛﺎﻧﺲ ﻧﻮﺳﺎﻥ ﻃﺒﻴﻌﻲ ﺩﺍﺭﺩ ﭼﻨﺎﻧﭽﻪ ﺍﻳﻦ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺩﺭ ﻣﺤﺪﻭﺩﺓ ﻓﺮﻛﺎﻧﺲ ﺑﺎﻓﺖﻫﺎ. ﻣﻌﺮﻓﻲ ﺷﺪEyal Lederman ﻫﺎﺭﻣﻮﻧﻴﻚ ﺗﻜﻨﻴﻚ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺗﻜﻨﻴﻚ ﺩﺭﻣﺎﻧﻲ ﻣﺆﺛﺮ ﺩﺭ ﺯﻣﻴﻨﻪ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺎﻧﻮﺍﻝ )ﺩﺳﺘﻲ( ﺑﻪ ﻭﺳﻴﻠﺔ : ﺑﺨﺶ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ٤ ﺍﺻﻮﻝ ﻭ ﺭﻭﺵ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﺗﻜﻨﻴﻚ ﺩﺭ ﻣﻔﺎﺻﻞ ﻣﺨﺘﻠﻒ ﺩﺭCD ﺩﺭ ﺍﻳﻦ.ﻭ ﺗﻮﺩﻩﻫﺎﻱ ﺑﺪﻥ ﺍﻋﻤﺎﻝ ﺷﻮﻧﺪ ﺑﺎﻋﺚ ﺍﻳﺠﺎﺩ ﺭﺯﻭﻧﺎﻧﺲ ﺷﺪﻩ ﺑﺎ ﺻﺮﻑ ﺍﻧﺮﮊﻱ ﻛﻤﺘﺮ ﺗﻮﺳﻂ ﺩﺭﻣﺎﻧﮕﺮ ﺩﺍﻣﻨﻪ ﺣﺮﻛﺘﻲ ﻣﻨﺎﺳﺐ ﺩﺭ ﺑﻴﻤﺎﺭ ﺍﻳﺠﺎﺩ ﻣﻲﺷﻮﺩ 1- The Principles of Harmonic Technique 2- The Principles of Harmonic Technique Using Thoracic Mass Oscillations
3- The Principles of Harmonic Technique Using Pelvic Mass Oscillations 4- The Principles of harmonic Technique Using Appendicular Oscillations
26.19 YOGA for YOU (Anatomy)
ــــ ﺍﻭﺭﮊﺍﻧﺲ ﻭ ﺑﻴﻬﻮﺷﻲ:٢٠
1.20 2.20
American College of Surgons ACS Surgery Principles & Pracitce (CD I , II) (E-Book) Advanced Pediatric Life Support: The Critical First Hour CPR and ACLS Review (David G. Nichols, MD)
2004 : ﺭﻳﻮﻱ ﭘﻴﺸﺮﻓﺘﻪ ﺩﺭ ﻛﻮﺩﻛﺎﻥ ﻭ ﺑﺎﻟﻐﻴﻦ ﺷﺮﺡ ﻣﻲﺩﻫﺪ- ﺩﺭ ﻣﻮﺭﺩ ﺍﺣﻴﺎﺀ ﻗﻠﺒﻲCD ﺍﻳﻦ
ــــــ
1: Initial Evaluation, 2: Airway Management, 3: Epiglottitis and Gidup, 4: Respiratory Failure, 5: Advanced Pediatric CPR, 6: Resuscitative Drugs 3.20
ANESTHESIA (Ronald D. Miller, MD) (Fifth Edition)
Anesthesiology (The Journal of the American Society of Anesthesiologists, Inc) Abstracts of Scientific Papers 5.20 Anesthesiology (The Journal of the American Society of Anesthesiologists, Inc) Abstracts of Scientific Papers 4.20 6.20 7.20
Clinical Procedures in EMERGENCY MEDICINE (4th Edition) (James R. Roberts, MD, Jerris R. Hedges, MD, MS) (E-Book) (CD I, II) Emergency Medical Training (MedEMT) Victory Technology, Inc. Presents (DISC ONE, TWO) MedEMT Overview
Emergency Medical Services (EMS)
The Well-Being of the EMT-Basic
Anatomy and Physiology-Part 1
Medical Terminology
Vital Signs and SAMPLE History
Lifting and Moving Patients
Airway Management
Patient Assessment
Medical and Behaval Care I
Medical and Behavioral Care II
Obstetric and Gynecological Care
Trauma
Infants and Children
Operations
Appendix A: Video/Animation List
Appendix B: Victory Products
1. Anatomical Fundamentals 2. Peripheral Neve Stimulation 3. Regional Anaesthesia 4. Upper, Lower Extremity 5. Peripheral Neve Blocks 11.20 The American Academy of Pediatric (David G. Nichols, MD Associate Professor of Anesthesiology and Clinical Care Medicine)
-Ventilating the Infant
-Chest Compressions
12.20 The Lipponcott-Raven Interactive Anesthesia Library on CD-ROM 13.20 The Massachusetts General Hospital Handbook of Pain Management
، ﺳﺮﻭﻛﺎﺭ ﺩﺍﺭﻧـﺪ، ﺑﻪ ﻋﻠﺖ ﺩﺳﺘﻴﺎﺑﻲ ﺭﺍﺣﺖ ﭘﺰﺷﻜﺎﻧﻲ ﻛﻪ ﺑﺎ ﺑﻴﻤﺎﺭﺍﻥ ﺩﺭﺩﻣﻨﺪPoacet
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ــــــ
Anatomy and Physology-Part 2
8.20 EMERGENCY MEDICINE A COMPREHENSIVE STUDY GUIDE (Rosen's ) (Volume 1-3) (Sixth Edition) (Judith E. Tintinall, MD, MS) 9.20 EMT-Basic Slide Set Slide Program Guide (John A. Stouffer, EMT-P, Richard S. Bennett, RN, EMT-P, BSN) (Mosby) 10.20 Peripheral Regional Anaesthesia Tutorial in the Ulm Rehabilitation hospital (Prof. Dr. Med. H. Mehrkens) (VCD) (CD I , II)
-Intitial Steps in Resuscitation
2000 2002 2000 2004
2004 1999 ـــــ
6. Peripheral Neve Blocks
-Endotracheal Intubaion
(Version 2.0) (Paul G. Barash, MD) (Salekan E-Book)
ــــــ ـــــ ـــــ
guide ﺍﺯEdition ﺍﻳﻦ. ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻛﺎﺭﺑﺮ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ، ﺍﺟﺮﺍ ﻣﻲﮔﺮﺩﻧﺪMass.Gen
ﺩﻳﺪﮔﺎﻩ ﻛﺎﻣﻞ ﻭ ﻣﻔﻴﺪﻱ ﺍﺯ ﺍﻃﻼﻋﺎﺗﻲ ﻛﻪ ﺩﺭ ﺩﺭﻣﺎﻥ ﻣﺆﺛﺮ ﺩﺭﺩ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﻣﻲﺑﺎﺷﻨﺪ ﻭ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥCD ﺍﻳﻦ . ﻣﺰﻣﻦ ﻭ ﺩﺭﺩ ﻛﺎﻧﺴﺮ ﺭﺍ ﭘﻮﺷﺶ ﻣﻲﺩﻫﺪ، ﻣﻮﺍﻟﻴﺘﻪﺍﻱ ﺩﺭﻣﺎﻧﻲ ﻣﺨﺘﻠﻒ ﺭﺍ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ ﻭ ﺟﻨﺒﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺩﺭﺩ ﺍﻋﻢ ﺍﺯ ﺣﺎﺩCD ﺍﻳﻦ، ﺑﺎ ﻣﺮﻭﺭ ﻣﺒﺎﺣﺚ ﻋﻤﺪﺓ ﺩﺭﺩ.ﻣﺸﻬﻮﺭ ﻣﻲﺑﺎﺷﺪ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
. ﺍﻃﻼﻋﺎﺕ ﺩﺍﺭﻭﻳﻲ ﻛﺎﻣﻞ ﻣﻲﺑﺎﺷﺪ48.9
70 ﺩﺭﺩ ﺻﻮﺭﺕ-
ﻣﺪﺍﺧﻼﺕ ﺭﺍﺩﻳﻮﺗﺮﺍﭘﻲ ﻭ ﺭﺍﺩﻳﻮﻓﺎﺭﻣﺎﺳﻲ ﺑﺮﺍﻱ ﺩﺭﺩﻫﺎﻱ ﻛﺎﻧﺴﺮ-
ﻣﺪﺍﺧﻼﺕ ﺟﺮﺍﺣﻲ ﻭ ﺟﺮﺍﺣﻲ ﺍﻋﺼﺎﺏ-
:ﺷﺎﻣﻞ 2002
New Analgesic Options: Overcoming Obstacles to Pain Relief - MD, NP, PA, RN Answer Sheet
-Pharmacist Answer Sheet
-Back Pain
-Fibromyalgia
-OA Pain
-Post Op Pain
-Trauma
-References
2005
11.20 Textbook of CRITICAL CARE (Salekan E-book) SECTION I RESUSCITATION AND MEDICAL EMERGENCIES SECTION II TRAUMA SECTION III IMAGING SECTION IV CELL INJURY AND CELL DEATH SECTION V INFECTIONS DISEASE SECTION VI ENDOCTINOLOGY, METABOLISM, NUTRITION, PHARMACOLOGY SECTION VII CARDIOVASCULAR SECTION VIII PULMONARY 12.20 Miller's Anesthesia (Vol I & II) (Salekan E-book)
2005
SECTION I: INTRODUCTION SECTION II: SCIENTIFIC PRINCIPLES SECTION III: ANESTHESIA VOLUME 2 SECTION IV: SUB SPECIAL TV SECTION V: CRITICAL CARE MEDICINE SECTION VI: ANCILLARY RESPONSIBILITIES AND PROBLEMS COMPANION VIDEO CD-ROM Video 1 Patient Positioning in Anesthesia Video 2 Code Blue Simulation
2004
13.20 NEW YORK SCHOOL OF REGIONAL ANESTHESIA PERIPHERAL NERVE BLOCKS PRINCIPLES AND PRACTICE -TRAINING IN PERIPHERAL NERVE BLOCKS - ESSENTIAL REGIONAL ANESTHESIA ANATOMY -EQUIPMENT AND PATIENT MONITORING IN REGIONAL ANESTHESIA -PERIPHERAL NERVE STIMULATORS AND NERVE STIMULATION -CLINICAL PHARMACOLOGY OF LOCAL ANESTHETICS -NEUROLOGIC COMPLICATIONS OF PERIPHERAL NERVE BLOCKS -KEYS TO SUCCESS WITH PERIPHERAL NERVE BLOCKS -CERVICAL PLEXUS BLOCK -INTERSCALENE BRACHIAL PLEXUS BLOCK -INFRACLAVICULAR BRACHIAL PLEXUS BLOCK -AXILLARY BRACHIAL PLEXUS BLOCK -INTRAVENOUS REGIONAL BLOCK OF THE UPPER EXTREMITY -CUTANEOUS NERVE BLOCKS OF THE UPPER EXTREMITY -THORACIC PARAVERTEBRAL BLOCK -THORACOLUMBAR PARAVERTEBRAL BLOCK -LUMBAR PLEXUS BLOCK - SCIATIC BLOCK: POSTERIOR APPROACH 234 -SCIATIC BLOCK: ANTERIOR APPROACH 252 -FEMORAL NERVE BLOCK -POPLITEAL BLOCK: INTERTENDINOUS APPROACH -POPLITEAL BLOCK: LATERAL APPROACH -ANKLE BLOCK - WRIST BLOCK -CUTANEOUS NERVE BLOCKS OF THE LOWER EXTERMITY -DIGITAL BLOCK
14.20 Interactive Regional Anesthesia
ــــــ
؛ ﺍﻭﺭﻭﻟﻮﮊﻱ٢١ 1.21
Adult and Pediatric Urology
2.21
Adult Urology Adult Urology Continued Pediatric Urology Video Library Advanced Therapy of Prostate Disease (Martin I. Resnick, MD, Ian M. Thompson, MD)
(Jay Y. Gillenwater, john T. Grayhack, Stuart S. Howards, Michael E. Mitchell)
2002 2000
. ﺭﻓﺮﺍﻧﺲﻫﺎ ﺩﺭ ﻣﻮﺭﺩ ﭼﮕﻮﻧﮕﻲ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺮﻭﺳﺘﺎﺕ ﻣﻲﺑﺎﺷﺪ. ﺑﻮﺩﻩ ﻭ ﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﺭﻓﺮﺍﻧﺲﻫﺎ ﺩﺭ ﻣﻮﺭﺩ ﭼﮕﻮﻧﮕﻲ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺮﻭﺳﺘﺎﺕ ﻣﻲﺑﺎﺷﺪAcrobat reader ﺻﻔﺤﻪﺍﻱ ﺩﺭ ﻣﺤﻴﻂ٦٤٨ ﺍﻳﻦ ﻛﺘﺎﺏ . ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ٧١ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ ، ﻏﺮﺑــﺎﻟﮕﺮﻱ ﻛﺎﻧﺴــﺮ ﭘﺮﻭﺳــﺘﺎﺕ-٩ ﻭ١١ ﻭ١٢ ﻓﺼـﻮﻝ. ﻓﺎﻛﺘﻮﺭﻫــﺎﻱ ﻣﻠﻜـﻮﻟﻲ ﺩﺭ ﺍﺭﺯﻳــﺎﺑﻲ ﻛﺎﻧﺴــﺮ ﭘﺮﻭﺳـﺘﺎﺕ-٨ ﻓﺼــﻞ. ﺍﻟﮕــﻮﺭﻳﺘﻢ ﺍﺭﺯﻳـﺎﺑﻲ ﺧﻄــﺮ ﭘﺮﻭﺳــﺘﺎﺕ ﻛﺎﻧﺴـﺮ ﺷــﺮﺡ ﺩﺍﺩﻩ ﺷــﺪﻩ ﺍﺳـﺖ-٧ ﻓﺼــﻞ. ﺍﭘﻴــﺪﻣﻴﻮﻟﻮﮊﻱ ﻛﺎﻧﺴــﺮ ﭘﺮﻭﺳـﺘﺎﺕ ﺷــﺮﺡ ﺩﺍﺩﻩ ﺷــﺪﻩ ﺍﺳـﺖ٦-١ ﻓﺼـﻮﻝ . ﺭﺍﺩﻳﻜﺎﻝ ﭘﺮﻭﺳﺘﺎﺗﻜﺘﻮﻣﻲ:ﺁﻣﺎﺩﮔﻲ ﺑﻴﻤﺎﺭ ﺑﺮﺍﻱ-١٩ ﻓﺼﻞ، ﻛﺎﻧﺴﺮ ﭘﺮﻭﺳﺘﺎﺕstaging ﺗﺸﺨﻴﺺ ﻭ-١٧-١٨ ﻓﺼﻞ. ﺗﺎﺭﻳﺨﭽﺔ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﭘﺮﻭﺳﺘﺎﺕ ﻭ ﺗﺎﺭﻳﺨﭽﺔ ﭘﺎﺗﻮﺑﻴﻮﻟﻮﮊﻱ ﻛﺎﻧﺴﺮ ﭘﺮﻭﺳﺘﺎﺕ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖ-١٣-١٦ ﻓﺼﻮﻝ. ﺍﺑﺰﺍﺭﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ-١٠ ﻓﺼﻞ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
71 ٢٠ﻭ ٢١ﻭ Stage -٢٢ﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺩﺭ ﺭﻭﺵﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺁﻧﻬﺎ -٢٩-٢٤ .Radical Perianal Prostatectomy -٢٣ .ﺭﺍﺩﻳﻮﺗﺮﺍﭘﻲ Brachy therapy ،ﻭ ﻫﻮﺭﻣﻮﻧﺎﻝﺗﺮﺍﭘـﻲ ﻭ ﻛﺮﺍﻳﺮﺗﺮﺍﭘـﻲ ﻛﺎﻧﺴـﺮﻫﺎﻱ ﻣﺨﺘﻠـﻒ ﭘﺮﻭﺳـﺘﺎﺕ -٣٩-٣٠ﺩﺭ ﻫـﺮ ﻓﺼـﻞ (TNM) Staging
ﺟﺪﺍﮔﺎﻧﻪ ﺷﺮﺡ ﻭ ﺭﻭﺵ ﺩﺭﻣﺎﻥ ﺁﻥ ﻧﻴﺰ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ -٤٠-٤٣ﭼﮕﻮﻧﮕﻲ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﺍﻥ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ ﭘﺮﻭﺳﺘﺎﺗﻜﺘﻮﻣﻲ ﺑﺎ PSAﻭ ﻫﻮﺭﻣﻮﻥﺗﺮﺍﭘﻲ ﻭ -٤٤ ...ﺍﺳﻔﻨﻜﺘﺮ genitourinaryﺁﺭﺗﻴﻔﻴﺸﺘﺎﻝ -٤٥ﻛﻼﮊﻥﺗﺮﺍﭘﻲ ﺑﺮﺍﻱ ﺑﻲﺍﺧﺘﻴﺎﺭﻱ ﺑﻌﺪ ﺍﺯ ﻋﻤـﻞ ﺟﺮﺍﺣـﻲ ﭘﺮﻭﺳـﺘﺎﺕ -٤٧ -٤٦ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﺑﺮﺍﻱ ﻋﻮﺍﺭﺽ erctionﻭ ﺍﻧﻮﺭﻛﺘﺎﻝ -٥٠-٤٨ﺟﻠﻮﮔﻴﺮﻱ ﺍﺯ ﻋﻮﺩ ﻛﺎﻧﺴﺮ ﺑﺎ ﺷﻴﻤﻲﺩﺭﻣﺎﻧﻲ ﻭ ﺭﺍﺩﻳﻮﺗﺮﺍﭘﻲ -٥١ﻧﮕﺮﺵ ﺳﻠﻮﻟﻲ ﻭ ﻫﻮﺭﻣﻮﻧﻲ ﺑﻪ -٥٢-٥٣ . BPHﻧﺴﺒﺖ ﺍﻭﺭﻭﺩﻳﻨﺎﻣﻴﻚ ﻭ ﺍﺑﻨﺮﻣﺎﻟﻲﻫﺎﻱ ﺩﻳﮕـﺮ -٥٤ .ﭘـﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺍﻧﺴـﺪﺍﺩ ﻣﺠـﺮﺍﻱ ﺧﺮﻭﺟـﻲ ﻣﺜﺎﻧـﻪ ﻭ ﺍﺧﺘﻼﻝ ﺩﺭ -٥٥ Vodingﺟﻠﻮﮔﻴﺮﻱ ﺍﺯ ﭘﻴﺸﺮﻓﺖ ﻭ ﻋﻮﺍﺭﺽ ﺑﻠﻨﺪﻣﺪﺕ :BPH -٥٦ BPHﻛﻲ ﺑﺎﻳﺪ ﻣﺪﺍﺧﻠﻪ ﻛﺮﺩ؟ -٥٧-٥٨ﺭﻭﺵﻫﺎﻱ ﺍﺭﺯﻳﺎﺑﻲ /ﺁﻣﺎﺩﮔﻲ ﻭ ﺍﻧﺘﺨﺎﺏ ﺩﺭﻣﺎﻥ ﻣﻨﺎﺳﺐ ﺑﺮﺍﻱ -٥٩ BPHﻣﻬﺎﺭﻛﻨﻨﺪﻩﻫﺎﻱ 5αﺭﺩﻭﻛﺘﺎﺯ -٦٠-٦٦ﺭﻭﺵﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺟﺮﺍﺣـﻲ ﺩﺭ BPH ﺷﺎﻣﻞ )ﺗﺮﺍﻧﺲ ﺍﻭﺭﺗﺮﺍﻝ ،needle Ablationﻟﻴﺰﺗﺮﺍﭘﻲ TUIP ،TUFP ،ﻭ ﻓﻴﺘﻮﺗﺮﺍﭘﻲ ﻭ openﭘﺮﻭﺳﺘﺎﺗﻜﺘﻮﻣﻲ( -٦٧-٧١ .ﭘﺮﻭﺳﺘﺎﺕ :ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ،ﻓﺎﻛﺘﻮﺭﻫﺎﻱ ﻣﺆﺛﺮ ﺩﺭ ﭘﺮﻭﮔﻨﻮﺯ ﻭ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺩﺭﻣﺎﻥﻫﺎ ﺩﺭ ﭘﺮﻭﺳﺘﺎﺕ. Atlas of RENAL TRANSPLANTATION
5.15
-Histopathology -surgery -clinical section -imaging -immunology AUA Vide Digest The American Urogical association (AUA) Impotence and Infertility
3.21
)(Prof. Legndre, Martin, Helenon, Lebranchu, Halloran, Nochy
ــــــ
-immunosupperssive ـــــ
ﺍﻳﻦ CDﺷﺎﻣﻞ ﻳﻜﻲ ﺍﺯ ﺳﺮﻱ ﻓﻴﻠﻢﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﺍﻧﺠﻤﻦ ﺍﻭﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎﻱ ﺁﻣﺮﻳﻜﺎ ) (AUA video digestﻣﻲﺑﺎﺷﺪ .ﻛﻪ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ Impotenceﻭ Infertiliteyﻣﻲﺑﺎﺷﺪ. ﻗﺴﻤﺖ ﺍﻭﻝ :Impotenceﺍﻟﻒ( ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﻭ ﺳﭙﺲ ﺍﻧﺘﺨﺎﺏ ﺩﺭﻣﺎﻥ ﻣﻨﺎﺳﺐ ﺁﻥ ﺑﻴﺎﻥ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺩﺭ ﺣﻴﻦ ﻧﺸﺎﻥﺩﺍﺩﻥ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺵ ﺗﻮﺳﻂ ﺍﺳﺎﺗﻴﺪ ﻣﺮﺑﻮﻃﻪ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ(Diagnosis8 treatment option) .
ﺏ( :Penile Venous Ligationﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﺑﺎ ﺗﻮﺿﻴﺢ ﺣﻴﻦ ﻋﻤﻞ ﺑﺎ ﻓﻴﻠﻢ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻗﺴﻤﺖ ﺩﻭﻡ :Rectal Probe Electroejaculation :Infertiliryﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ejaculationﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﺳﭙﺲ ﺗﺠﻬﻴﺰﺍﺕ ﻭ ﺩﺳﺘﮕﺎﻩﻫﺎﻱ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﻭ ﻃﺮﺯ ﻛﺎﺭ ﺁﻧﻬﺎ ﺑﺎ ﻓﻴﻠﻢ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﻃﺮﻳﻘﻪ ﺍﻧﺠﺎﻡ ﭘﺮﻭﺏﮔﺬﺍﺭﻱ ﻭ ﺍﻳﺠﺎﺩ ejaculationﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﺍﺳﺖ. 2004
)BLADDER BIOPSY INTERPRETATIONS (Jonathan I. Epstein, M.D., Mahul B. Amin, M.D., Victor E. Reuter, M.D.) (CD I, II) (SALEKAN E-BOOK
4.21
ﺍﻳﻦ ﻛﺘﺎﺏ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: Papillary Urothelial Neoplasms with Inverted Growth Patterns
Flat Urothelial Lesions
Normal Blodder Anatomy and Variants of Normal histology
Conventional Morphologic, Prognostic, and Predictive Factors and Reporting of Bladder Cancer Cystitis Second ary Tumors of the Bladder
Glandular Lesions Mesenchymal Tumors and Tumor-Like Lesions
Invasive Urothelial Carcinoma Squamous Lesions Miscellaneous Nontumors and Tumors
)Bristol Urological Institute (Computer Aided Learning Program
ــــــ
5.21
ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ﺍﻳﻦ CDﺑﺮﺍﻱ ﺍﻓﺰﺍﻳﺶ ﻣﻌﻠﻮﻣﺎﺕ ﺣﻔﻈﻲ ﻧﻴﺴﺖ ﺑﻠﻜﻪ ﻫﺪﻑ ﺍﻳﻦ CDﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﻧﺶ ﺍﻭﺭﻭﻟﻮﮊﻱ ﻫﺮ ﺷﺨﺺ ﻭ ﭼﮕﻮﻧﮕﻲ ﻓﻬﻢ ﻣﻄﺎﻟﺐ ﻭ ﻛﻢ ﺑﻪ ﺑﻬﺘﺮﻓﻬﻤﻴﺪﻥ ﻭ ﺗﺼﻤﻴﻢ ﮔﺮﻓﺘﻦ ﺩﺭ ﻣﻮﺭﺩ ﻣﺒﺎﺣﺚ ﺍﻭﺭﻭﻟﻮﮊﻱ ﺍﺳﺖ. ﺍﻳﻦ CDﺷﺎﻣﻞ ﺗﺴﺖﻫﺎﻱ ٤ﮔﺰﻳﻨﻪﺍﻱ ﺍﺳﺖ ﻭ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ: -١ﻣﻌﺎﻳﻨﻪ ﺑﻴﻤﺎﺭﺍﻥ ﺍﻭﺭﻭﻟﻮﮊﻱ
impotence -٢
-٣ﺗﺮﻭﻣﺎﻱ ﻛﻠﻴﻪ
-٤ﻋﻼﺋﻢ ﺩﺳﺘﮕﺎﻩ ﺍﺩﺭﺍﺭﻱ ﺗﺤﺘﺎﻧﻲ
-٥ﻫﻤﺎﺗﻮﺭﻱ
-٦ﻋﻘﻴﻤﻲ ﻣﺮﺩﺍﻥ -٧ﺳﻨﮓﻫﺎﻱ ﻛﻠﻴﻮﻱ
-٨ﺑﻲﺍﺧﺘﻴﺎﺭﻱ ﺍﺩﺭﺍﺭ
-٩ﺍﺧﺘﻼﻻﺕ ﺍﺳﻜﺮﻭﺗﻮﻡ
-١٠ﻛﺎﻧﺴﺮ ﭘﺮﻭﺳﺘﺎﺕ
-١ﺩﺭ ﻫﺮ ﻋﻨﻮﺍﻥ ﺍﺑﺘﺪﺍ ﻣﻘﺪﻣﻪﺍﻱ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱ ﻭ ﺍﺧﺘﻼﻻﺕ ﻣﺮﺑﻮﻃﻪ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ -٢ .ﺳﭙﺲ ﺍﻫﺪﺍﻓﻲ ﻛﻪ ﺑﺎ ﻣﻄﺎﻟﻌﻪ ﺍﻳﻦ ﻗﺴﻤﺖ ﺍﺯ ﺑﻴﻤﺎﺭﻱ ﺑﺎﻳﺪ ﺑﻪ ﺩﺳﺖ ﺁﻭﺭﺩ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖ -٣ .ﺩﺭ ﻗﺴﻤﺖ ﺳﻮﻡ ﺍﺑﺘﺪﺍ ﺷﺮﺡ ﺣﺎﻝ ﺑﻴﻤـﺎﺭﻱ ﻭ ﺳـﭙﺲ ﺗﺼـﺎﻭﻳﺮ ﺭﻧﮕـﻲ ،ﺭﺍﺩﻳـﻮﮔﺮﺍﻓﻲ، ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ،ﭘﺎﺗﻮﻟﻮﮊﻱ ﻫﺮ ﺍﺧﺘﻼﻝ ﺩﺭ ﺻﻔﺤﻪﺍﻱ ﺟﺪﺍﮔﺎﻧﻪ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﺳﺆﺍﻻﺕ ٤ﺟﻮﺍﺑﻲ ﺑﺮ ﺁﻥ ﻓﺮﺍﻫﻢ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺁﺧﺮ ﻧﻴﺰ ﺑﻪ ﻣﻌﻠﻮﻣﺎﺕ ﺷﺨﺺ Scoreﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. CAMPBELL'S UROLOGY
2003 & Voiding Function Dysfunction
Infections and Inflammations of the Genitourinary Tract
Physiology, Pathology, and Management of Upper Urinary Tract Diseases
Oncology
Pediatric Urology
Sexual Function and Dysfunction
Urologic Examination and Diagnostic Techniques Reproductive Function and Dysfunction
Radiology Atlas
Pathology Atlas
Urologic Surgery
Urinary Lithiasis and Endourology Additional Media
ــــــ
)Non-Cardiac Surgery and Gynecology and Urology (Michael K. Rees, MD, MPH
Patient Evaluation for
6.21
Anatomy Benign Prostatic Hyperplasia Carcinoma of the Prostate Study Guide
Core Curriculum in Primary Care
7.21
CCCﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯ CDﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲ Harvardﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
72 CDﺣﺎﺿﺮ ﺩﺭ ﻣﻮﺭﺩ ﺟﺮﺍﺣﻲ ،ﺯﻧﺎﻥ ﻭ ﺍﻭﺭﻭﮊﻱ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖ .ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛﺎﺭﺑﺮ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜﻲ ،ﺳﺆﺍﻻﺕ ﻣﺮﺑﻮﻃﻪ ﺑﻪ ﺻﻮﺭﺕ ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑـﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﻘﺎﻟﻪ ﭼﺎﭘﻲ ﺩﺭ ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: -١ﭼﮕﻮﻧﻪ ﻳﻚ ﺑﻴﻤﺎﺭ ﺭﺍ ﺑﺮﺍﻱ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ )ﺑﺠﺰ ﺟﺮﺍﺣﻲ ﻗﻠﺐ( ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺁﻣﺎﺩﻩ ﻛﻨﻴﻢ؟ ــــــ
Male impotence
-٣ﻋﻘﻴﻤﻲ ﻣﺮﺩﺍﻥ -٢ﺍﺭﺯﻳﺎﺑﻲ ﺧﻮﻧﺮﻳﺰﻱﻫﺎﻱ ﺍﺑﻨﺮﻣﺎﻝ ﺭﺣﻢ ).(AUB )8.21 Core Curriculum in Primary Care Nephrology (Michael K. Rees, MD, MPH
CCCﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯ CDﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲ Harvardﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. CDﺣﺎﺿﺮ ﻣﻄﺎﻟﺒﻲ ﺍﺯ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺑﻪ ﺻﻮﺭﺕ ﺍﺳﻼﻳﺪ ،ﺳﺨﻨﺮﺍﻧﻲ ،ﻧﻤﻮﺩﺍﺭ ﻭ ﺍﻟﮕﻮﺭﻳﺘﻢﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖ. ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛﺎﺭﺑﺮ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜﻲ ،ﺳﺆﺍﻻﺕ ﻣﺮﺑﻮﻃﻪ ﺑﻪ ﺻﻮﺭﺕ ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﻘﺎﻟﻪ ﭼﺎﭘﻲ ﺩﺭ ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺩﺭ ﺍﻭﺭﻭﻟﻮﮊﻱ ﺩﺭ ﺍﻳﻦ CDﻣﻮﺟﻮﺩ ﺍﺳﺖ. 4-Clinical Application of Renal Physiology
2- Drugs vs Diet in Modifying Renal failure
3- Treatment of Mypertension-Special Case
1- How to erahcate Renal mass/Tumor
ــــــ
)Core Curriculum in Primary Care Gynecology (Michael, Isaac Schiff, Keith, Thomas, Annekathryn
12.3
ــــــ
Cystectomy and Construction an Ileocecal Neobladder for Urethral Voiding
9.21
)(John A. Libertino MD, FACS
2004
)(Roger S Kirby, Michael P O'Leary) (SALEKAN E-BOOK Erectile dysfunction and cardiovascular disease
New developments for the treatment of erectile dysfunction: Present and Future
Apoptosis in the prostate
ــــ
10.21 Hot Topics in UROLOGY Premature ejaculation Michael P O'Leary
Angiogenesis as a diagnostic and therapeutic tool in urological malignancy Chemoprevention of prostate cancer Robotic surgery and nanotechnology
Adjuvant therapy for prostate cancer
Marginally worse? Positive resection limits after radical prostatectomy
What,s hot and whats not - the medical management of BPH
I mmunotherapy for prostate
Bisphosphonates: a potential new treatment strategy in prostate cancer
Urethral stricture surgery: the state of the art
Future prospects for .. nephron conservation in renalcel I carcinoma
Three-dimensional imaging of the upper urinary tract
Laparoscopic radical prostatectomy
Management of female sexual dysfunction
Reducing medical errors in urology
Organ preserving therapies for penile carcinomas
The overactive bladder
Antisense therapy in oncology: current
)11.21 PRIMER ON KIDNEY DISEASES (Second Edition) (NATINAL KINDEY FOUNDATION SCIENTIFIC ADVISORY BOARD
ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻚ ﺩﺭ ﻣﺤﻴﻂ ﺍﻛﺮﻭﺑﺎﺕ ﺍﺟﺮﺍ ﺷﺪﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ١١ﻓﺼﻞ ﻭ ﻣﺸﺘﻤﻞ ﺑﺮ ٥١٧ﺻﻔﺤﻪ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -١ﺳﺎﺧﺘﻤﺎﻥ ﻭﻓﺎﻧﻜﺸﻦ ﻛﻠﻴﻪ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﺑﺎﻟﻴﻨﻲ ﻛﻠﻴﻪ ﺷﺎﻣﻞ :ﺁﻧﺎﺗﻮﻣﻲ ،ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﺍﺭﺯﻳﺎﺑﻲ ﻓﺎﻧﻜﺸﻦ ﻛﻠﻴﻪ ،U/A ،ﻫﻤﺎﺗﻮﺭﻱ ،ﭘﺮﻭﺗﺌﻴﻦ ﺍﺩﺭﺍﺭﻱ ،ﺗﻜﻨﻴﻚ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺍﺯ ﻛﻠﻴﻪ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -٢ﺍﺧﺘﻼﻻﺕ ﺍﺳﻴﺪ ﻭ ﺑﺎﺯ ﻭ ﺍﻟﻜﺘﺮﻭﻧﻴﻚ ﺷﺎﻣﻞ :ﻫﻴﭙﻮﻭﻫﻴﺒﺮﻧﺎﺗﻮﻣﻲ ،ﺍﺳﻴﺪﻭﺯ ،ﺍﻟﻜﺎﻟﻮﺯﻣﺘﺎﺑﻮﻟﻴﻚ ،ﺍﺧﺘﻼﻻﺕ ﻣﺘﺎﺑﻮﻟﻴﺴﻢ ﭘﺘﺎﺳﻴﻢ ﻭ ﻛﻠﻴﺴﻴﻢ ،ﻣﻨﻴﺰﻳﻮﻡ ﻭ ﺩﻳﻮﺭﺗﻴﻚ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ Glomerular Diseuse -٣ﺷﺎﻣﻞ :ﺍﻳﻤﻮﻧﻮﭘﺎﺗﻮﮊﻧﺰ ﺑﻴﻤﺎﺭﻱ ﺍﻱ ﮔﻠﻮﻣﺮﻭﻱ MGN ،FSGN ،MPGN ،MCD ،ﻭ ﺳﻨﺪﺭﻭﻡ ﮔﻮﺩﭘﺎﺳﭽﺮ ﻭ IGAﻧﻔﺮﻭﭘﺎﺗﺎ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -٤ﻛﻠﻴﻪ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺳﻴﺴﺘﻤﻴﻚ ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ :ﻛﻠﻴﻪ ﺩﺭ CHFﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﺒﺪﻱ PSGN ،ﻭ ﺍﺳﻜﻮﻟﻴﺖﻫﺎ ﻭ ﻛﻠﻴﻪ SLE ،ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺭﻭﻣﺎﺗﻴﺴﻤﻲ ﻭ ﻛﻠﻴﻪ ،ﺩﻳﺎﺑﺘﻴﻚ ﻧﻔﺮﻭﭘﺎﺗﻲ ﻭ HIVﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﻠﻴﻪ ﻭ ....ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -٥ﻧﺎﺭﺳﺎﺋﻲ ﺣﺎﺩ ﻛﻠﻴﻪ ﺷﺎﻣﻞ :ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﻋﻠﻞ approach ،ﻭ ﺩﺭﻣﺎﻥ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -٦ﺩﺍﺭﻭﻫﺎﻱ ﻭ ﻛﻠﻴﻪ :ﺷﺎﻣﻞ NSAIDﻭ ﻛﻠﻴﻪ ﻭ ﻣﻮﺍﺭﺩ ﺩﺍﺭﻭﻱ ﺩﺭﻣﺎﻧﻲ ﺩﺭ ﻧﺎﺭﺳﺎﺋﻲ ﻛﻠﻴﻪ ﻓﺼﻞ -٧ﺍﺧﺘﻼﻻﺕ ﺍﺭﺛﻲ ﻛﻠﻴﻪ :ﻧﻔﺮﻭﭘﺎﺗﻲ ،Sickle cellﺑﻴﻤﺎﺭﻱﻫﺎﻱ Cysticﻛﻠﻴﻪ ،ﺳﻨﺪﺭﻭﻡ Alportﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﺴﻴﺘﻴﻚ ﻛﻠﻴﻪ ﻓﺼﻞ -٨ﻧﻔﺮﻭﭘﺎﺗﻲ ﺗﻮﺑﻮﻟﻮﺍﻳﻨﺘﺮﺳﺘﻴﺸﻴﻞ ﻭ ﺍﺧﺘﻼﻻﺕ ﻣﺠﺎﺭﻱ ﺍﺩﺍﺭﻱ ﺷﺎﻣﻞ :ﺑﻴﻤﺎﺭﻱ ﻛﻠﻴﻪ ﻭ ﻟﻴﺘﻴﻮﻡ ﺳﺮﺏ ،ﺍﮔﺰﺍﻻﺕ ﺳﻨﮓﻫﺎﻱ ﻛﻠﻴﻮﻱ ،ﻋﻔﻮﻧﺖﻫﺎﻱ ﻛﻠﻴﻮﻱ ،ﻋﻔﻮﻧﺖﻫﺎﻱ ﻛﻠﻴﻮﻱ ﺍﻧﺴﺪﺍﺩ ﻣﺠﺎﺭﻱ ﻭ ﺳﺮﻃﺎﻥﻫﺎﻱ ﻛﻠﻴﻪ ﻭ ﻣﺠﺎﺭﻱ ﺁﻥ. ﻓﺼﻞ -٩ﻛﻠﻴﻪ ﻭ ﻣﻮﺍﺭﺩ ﺧﺎﺹ ﺷﺎﻣﻞ‚ ﻛﻠﻴﻪ ﺩﺭ ﻧﻮﺯﺍﺩﺍﻥ ﻭ ﻛﻮﺩﻛﺎﻥ ،ﻛﻠﻴﻪ ﺩﺭ ﺣﺎﻣﻠﮕﻲ ،ﻛﻠﻴﻪ ﺩﺭ ﭘﻴﺮﻱ. ﻓﺼﻞ -١٠ﻧﺎﺭﺳﺎﺋﻲ ﻣﺰﻣﻦ ﻛﻠﻴﻪ ﻭ ﺩﺭﻣﺎﻥ ﺷﺎﻣﻞ :ﺳﻨﺪﺭﻭﻡ ﺍﻭﺭﻣﻲ ،ﻫﻤﻮﺩﻳﺎﻟﻴﺰ ﻭ ﻫﻤﻮﻓﻴﻠﺘﺮﺍﺳﻴﻮﻥ ﺩﻳﺎﻟﻴﺰ ﺻﻔﺎﺗﻲ ،ﭘﻴﺶﺁﮔﻬﻲ ﻭ ﺗﻐﺬﻳﻪ ،CRFﺗﻈﺎﻫﺮﺍﺕ ﻗﻠﺒﻲ ،ﻋﺼﺒﻲ ،ﻫﻤﺎﺗﻮﻟﻮﮊﻱ ،ﻏﺪﺩﻱ CRFﻭ ﭘﻴﻮﻧﺪ ﻛﻠﻴﻪ ﻭ ﭼﮕﻮﻧﮕﻲ ﺩﺍﺭﻭﺩﻣﺎﻧﻲ ﺩﺭ ﺁﻧﻬﺎ. ﻓﺼﻞ -١١ﻓﺸﺎﺭ ﺧﻮﻥ ﺷﺎﻣﻞ :ﭘﺎﻧﻮﮊﻧﺰ ،ﻓﺸﺎﺭ ﺧﻮﻥ ﺍﺳﺎﺳﻲ ،ﻓﺸﺎﺭ ﺧﻮﻥ Renovascularﻭ ﺩﺭﻣﺎﻥ ﻓﺸﺎﺭ ﺧﻮﻥ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
73 )(Official Journal of the American Urological Association
2003
-CME Participant Assessment Test and Course Evaluation
)(CD I, II
)(Spring & Summer
12.21 The Journal of UROLOGY
-Urological Survey
-Investigative Urology
-Pediatric Urology
- Clinical Urology
CD I:
-Urological Survey
-Investigative Urology
-Pediatric Urology
- Clinical Urology
CD II:
)13.21 Urogynecology: Evaluation and Treatment of Urinary Incontinence (Bruce Rosenzweig, MD, Jeffrey S. Levy, MD, Donald R. Ostergard, MD
ــــــ
ﻼ ﺭﻧﮕﻲ ﺑﻮﺩﻩ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﺑﻪ ﺻﻮﺭﺕ ﻧﻮﺷﺘﺎﺭﻱ ﻭ ﻓﺎﻳﻞ ﺻﻮﺗﻲ ﻛﻪ ﺑﺮ ﺭﻭﻱ ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﺍﻳﻦ CDﻭﺟﻮﺩ ﺩﺍﺭﺩ. ﺍﻳﻦ CDﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﺗﺼﺎﻭﻳﺮ ﻛﺎﻣ ﹰ ٤ Urogynechologyﻗﺴﻤﺖ ﻣﺠﺰﺍ ﺩﺍﺭﺩ ﺷﺎﻣﻞ:
-١
Introduction Definigg Incontinence
Evaluation -٢
:Introduction & Defining Incontince (١
-٣
won surgical & surgical Management
ﺍﻳﻦ ﻗﺴﻤﺖ ﺧﻮﺩ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ:
yﺗﺸﺨﻴﺺ incontince
-٤
Consideration for the OB/GYN Generalist
affected women y
Patient misconceptions y
Types of incontinernce y incontinence awareness y (٢ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺎ :incontinency
y Voiding diary yﺗﺎﺭﻳﺨﭽﻪ yﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ
un , u/s y Multi-Channel urodynamics y
Cystoscopy y uroflowmetry y Postvoid residual y Cystometrogram y Pad test y
Pessary test y
(٣ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﺟﺮﺍﺣﻲ ﻭ ﻏﻴﺮ ﺟﺮﺍﺣﻲ ﺩﺭ : Stress urinary incontinence ﺍﻳﻦ ﻗﺴﻤﺖ ﺷﺎﻣﻞ ﺍﻟﮕﻮﺭﻳﺘﻢ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻣﻲﺑﺎﺷﺪ ﻭ ﺳﭙﺲ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻏﻴﺮﺟﺮﺍﺣﻲ )) biofeedback, Beharioral modificationﻭ ﺩﺭﻣﺎﻥﻫﺎﻱ ﺩﺍﺭﻭﺋﻲ funetional electrieal Stimalationﻭ (....ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ. ﺭﻭﺵﻫﺎﻱ ﺟﺮﺍﺣﻲ :ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵﻫﺎﻱ ﺍﻧﺠﺎﻡ ﺟﺮﺍﺣﻲ ﺑﺤﺚ ﺷﺪﻩ ﻭ ﺳﭙﺲ Procedureﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻗﺴﻤﺖﻫﺎﻱ ﺑﻌﺪﻱ ﻣﻘﺎﻳﺴﻪ ﺩﺭﺻﺪ ﻣﻮﻓﻘﻴﺖ ﺭﻭﺵﻫﺎ ﺫﻛـﺮ ﺷـﺪﻩ ﻭ ﺩﺭ ﺁﺧـﺮ Complicationﺍﻳـﻦ ﺭﻭﺵﻫـﺎ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. : Consideration for the OB/Gyn Generalist (٤ ﺩﺭ ﺍﻳﻦ ﻓﺼﻞ: urogynechology as a subdiscipline y professional consideration y
Non surgical therapy y Urodynamics y
incontinrence management to private patients y equipment cost ySet-up requirement y
eystometry y Allied Staff y
)Seven Edition (Barry M. Brenner) (E-Book
ــــ
ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. )(Volume 1-2
14.21 The Kidney
ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ ﺩﻭ ﺟﻠﺪ ﺍﺳﺖ . ﺩﺭ ﺍﻧﺘﻬﺎﻱ ﻫﺮ ﺑﺨﺶ ﻛﺘﺎﺏ ،ﺗﺼﺎﻭﻳﺮ ﻣﺮﺑﻮﻃﻪ ﺑﺎ ﻭﺿﻮﺡ ﺑﺎﻻ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻛﻴﻔﻴﺖ ﺑﺎﻻﻱ ﺗﺼﺎﻭﻳﺮ ،ﺍﻳﻦ ﺍﻣﻜﺎﻥ ﺭﺍ ﻓﺮﺍﻫﻤﻲ ﻣﻲﺳﺎﺯﺩ ﺗﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﻧﻬﺎ ﺩﺭ ﺳﻤﻴﻨﺎﺭﻫﺎ ﻭ ﻫﻤﻴﻨﻄﻮﺭ ﺟﻬﺖ ﺁﻣﻮﺯﺵ ﻣﻨﺎﺳﺐ ﺑﺎﺷﺪ .ﺍﻳﻦ ﺟﻠﺪ ﺩﺍﺭﺍﻱ ﺩﻭ ﺑﺨﺶ ﺍﺳﺖ:
-١ﻗﺴﻤﺖﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻛﻠﻴﻪ ﻃﺒﻴﻌﻲ ﻭ ﻋﻤﻠﻜﺮﺩ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﺑﺨﺶﻫﺎ ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﻣﺒﺎﺣﺜﻲ ﻫﻤﭽﻮﻥ ﺁﻧﺎﺗﻮﻣﻲ ﻛﻠﻴﻪ ،ﺭﺷﺪ ﻭ ﺑﻠﻮﻍ ﻛﻠﻴﻪ ،ﺍﺻﻮﻝ ﻣﺘﺎﺑﻮﻟﻴﻚ ﺍﻧﺘﻘﺎﻝ ﻳﻮﻥ ،ﺟﺮﻳﺎﻥ ﺧﻮﻥ ﻛﻠﻴﻪ ،ﺍﻧﺘﻘﺎﻝ ﻛﻠﻴﻮﻱ ﮔﻠﻮﻛﺰ ،ﺍﺳﻴﺪ ﺁﻣﻴﻨﻪ ،ﺳﺪﻳﻢ ،....ﻛﻨﺘﺮﻝ ﺗﺮﺷﺢ ﻛﻠﻴﻮﻱ ﭘﺘﺎﺳﻴﻢ ﻭ ....ﺩﻫﻬﺎ ﻋﻨﻮﺍﻥ ﺩﻳﮕﺮ ﻣﻄﺮﺡ ﺷﺪﻩﺍﻧﺪ. -٢ﺍﺧﺘﻼﻝ ﺩﺭ ﻛﻨﺘﺮﻝ ﺣﺠﻢ ﻣﺎﻳﻊ ﺑﺪﻥ :ﻛﻨﺘﺮﻝ ﺣﺠﻢ ﺧﺎﺭﺝ ﺳﻠﻮﻟﻲ ﻭ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺍﺩﻡ ،ﻋﻮﺍﻣﻞ ﻣﺆﺛﺮ ﺑﺮ ﻫﻤﻮﺳﺘﺎﺯ ﻣﺎﻳﻊ ،ﻓﺎﻛﺘﻮﺭﻫﺎﻱ ﻣﺆﺛﺮ ﺑﺮ ﺗﻮﺑﺮﻝ ﻛﻠﻴﻪ ،AVP ،ﭘﺮﻭﺳﺘﺎﮔﻼﻧﺪﻳﻦﻫﺎ ،ﺍﺩﻡ ﺩﺭ ﺳﻴﺮﻭﺯ ،ﺍﺩﻡ ﺩﺭ ،CHFﺩﻳﺎﺑﺖ ﺑﻲﻣﺰﻩ ﻭ ﺍﻧـﻮﺍﻉ ﺁﻥ ،ﻫﻴﭙﻮﻧـﺎﺗﺮﻣﻲ ﻭ ﺍﻳﺘﻮﻟـﻮﮊﻱﻫـﺎﻱ ﻣﺨﺘﻠﻒ ﺁﻥ ،ﺍﺧﺘﻼﻻﺕ ﺍﺳﻴﺪ ﻭ ﺑﺎﺯ ،ﺍﺧﺘﻼﻻﺕ ﺗﻮﺍﺯﻥ ﭘﺘﺎﺳﻴﻢ ،ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺑﻴﻤﺎﺭ ﻣﺒﺘﻼ ﺑﻪ ﻫﻴﭙﻮﻭﻫﻴﭙﺮﻛﺎﺳﻤﻲ ،ﺍﺧﺘﻼﻻﺕ ﻛﻠﺴﻴﻢ ﻭ ﻓﺴﻔﺮ ﻭ ....ﺩﻫﻬﺎ ﻣﻄﻠﺐ ﺩﻳﮕﺮ ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ،ﺩﺭ ﺩﺳﺘﺮﺱ ﻣﻲﺑﺎﺷﻨﺪ. ﺟﻠﺪ ٢ﻛﺘﺎﺏ ﺷﺎﻣﻞ ٣ﻗﺴﻤﺖ ﺍﺳﺖ:
ﺍﻟﻒ( ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﻠﻴﻪ :ﻣﺒﺎﺣﺜﻲ ﭼﻮﻥ :ﺍﺭﺯﻳﺎﺑﻲ ﺑﺎﻟﻴﻨﻲ ﺩﺭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﻠﻴﻪ ،ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﮔﻠﻮﻣﺮﻭﻟﻲ ﺍﻭﻟﻴﻪ ﻭ ﺛﺎﻧﻮﻳﻪ ،ﻋﻔﻮﻧﺖﻫﺎﻱ ﺍﺩﺭﺍﺭﻱ ،ﻧﻔﺮﻭﭘﺎﺗﻲ ﺗﻮﻛﺴﻴﻚ ﻭ ....ﺩﻫﻬﺎ ﻣﻄﻠﺐ ﺩﻳﮕﺮ. ﺏ( ﭘﺎﺗﻮﮊﻧﺰ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﻠﻴﻪ :ﻧﺌﻮﭘﻼﺯﻱ ﻛﻠﻴﻪ ،ﻫﻴﭙﺮﺗﺎﻧﺴﻴﻮﻥ )ﺍﻭﻟﻴﻪ (renovascularﺍﻭﺭﻱ ،ﺍﺳﺘﺌﻮﺩﺳﻴﺘﺮﻭﻓﻲ ﺭﻧﺎﻝ ﻭ ...ﺍﺯ ﺟﻤﻠﻪ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡ ﺷﺪﻩ ﻣﻲﺑﺎﺷﻨﺪ. ﺝ( ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺑﻴﻤﺎﺭ ﻣﺒﺘﻼ ﺑﻪ ﻧﺎﺭﺳﺎﻳﻲ ﻛﻠﻴﻮﻱ :ﺍﻧﻮﺍﻉ ﺩﻳﺎﻟﻴﺰ ،ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻱ ﭘﻴﻮﻧﺪ ،ﺍﻧﻮﺍﻉ ﺩﺍﺭﻭﻫﺎﻱ ﺩﻳﻮﺭﺗﻴﻚ ﻭ ....ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺑﺤﺚ ﺷﺪﻫﺎﻧﺪ. 2005
)15.21 SCHWARTZ'S PRINCIPLES OF SURGERY (8th Edition) (F. Charles Brunicardi, Dana K. Andersen, Timothy R. Billiar) (Salekan e-book) (CD I, II
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
74
ﻃﺮﻳﻘﺔ ﻣﺸﺎﻫﺪﻩ ﻓﻴﻠﻢﻫﺎﻱ VCDﺗﻮﺳﻂ ﻛﺎﻣﭙﻴﻮﺗﺮ :
ﺍﺑﺘﺪﺍ ﺑﻪ my computerﺭﻓﺘﻪ ﻭ ﻭﺍﺭﺩ ﺩﺭﺍﻳﻮ CD-ROMﺩﺳﺘﮕﺎﻩ ﺷﻮﻳﺪ ﺳﭙﺲ ﺑﺎ ﺩﻭﺑﺎﺭ ﻛﻠﻴﻚ ﺑﺮ ﺭﻭﻱ Xing playerﺑﺮﻧﺎﻣﻪ Xingﺭﺍ ﻧﺼﺐ ﻛﻨﻴـﺪ .ﺍﺯ ﺭﻭﻱ Xing Mpeg Player ، desktopﺭﺍ ﺑـﺎﺯ ﻛـﺮﺩﻩ ، ﺳﭙﺲ ﺍﺯ ﺭﻭﻱ ﻣﻨﻮﻱ Open ، Fileﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ .ﺩﺭ ﻗﺴﻤﺖ Look inﺩﺭﺍﻳﻮ CD-Romﺩﺳﺘﮕﺎﻩ ﺧﻮﺩ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﺮﺩﻩ ﻭ ﺩﺭ ﻗﺴﻤﺖ Video CD ( *.dat) . Files of typeﺭﺍ ﺍﻧﺘﺨـﺎﺏ ﻛﻨﻴـﺪ ،ﺳـﭙﺲ ﺑـﻪ ﺩﺍﻳﺮﻛﺘﻮﺭﻱ Mpegavﺭﻓﺘﻪ ﻭ Avseq01ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﺮﺩﻩ ﻭ Openﺭﺍ ﺑﺰﻧﻴﺪ.
ﻃﺮﻳﻘﻪ ﻧﺼﺐ ﻧﺮﻡ ﺍﻓﺰﺍﺭﻫﺎﻱ : E-book
-١ -٢ -٣ -٤ -٥ -٦
ﺑﺎ ﺍﺯ ﻗﺮﺍﺭ ﺩﺍﺩﻥ ﺳﻲ ﺩﻱ E-bookﺩﺭ ﺩﺭﺍﻳﻮ CD-Romﺻﻔﺤﻪ PCA pdf book setupﺑﻪ ﺻﻮﺭﺕ Autorunﺑﺎﺯ ﻣﻲﺷﻮﺩ . ﺩﺭ ﺻﻮﺭﺗﻲ ﻛﻪ ﺍﻭﻟﻴﻦ ﺑﺎﺭ ﺍﺳﺖ ﻛﻪ CDﻫﺎﻱ E-bookﺍﻳﻦ ﺷﺮﻛﺖ ﺭﺍ ﺩﺭ ﺩﺳﺘﮕﺎﻩ ﻣﻲﮔﺬﺍﺭﻳـﺪ “ ﺑـﺎ ﺍﻧﺘﺨـﺎﺏ ﮔﺰﻳﻨـﻪ Acrobat Reader Installationﺑﺮﻧﺎﻣـﻪ Acrobatﺭﺍ ﻧﺼـﺐ ﻭ ﻣﺮﺍﺣﻞ ﺁﻥ ﺭﺍ ﺗﺎ ﺍﻧﺘﻬﺎ ﻃﻲ ﻛﻨﻴﺪ“ ﺩﺭ ﻏﻴﺮ ﺍﻳﻨﺼﻮﺭﺕ ﺑﻪ ﻣﺮﺣﻠﻪ ٣ﺑﺮﻭﻳﺪ . ﻣﻨﻮﻱ Execute The Programﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ. ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﻧﺎﻡ ﻛﺘﺎﺏ ،ﮔﺰﻳﻨﻪ Viewﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ. ﺑﺮﻧﺎﻣﻪ Acrobatﺑﺎﺯ ﻣﻲﺷﻮﺩ ﻭ ﻛﺘﺎﺏ ﺭﺍ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻣﻄﺎﻟﻌﻪ ﺑﻔﺮﻣﺎﺋﻴﺪ. ﺑﺮﺍﻱ ﺍﺟﺮﺍﻱ ﺑﺮﻧﺎﻣﻪ ﻻﺯﻡ ﺍﺳﺖ ﻛﻪ ﺩﺭﺍﻳﻮ \ C:ﺩﺳﺘﮕﺎﻫﺘﺎﻥ ﺣﺪﺍﻗﻞ 500ﻣﮕﺎﺑﺎﻳﺖ ﻓﻀﺎﻱ ﺧﺎﻟﻲ ﺩﺍﺷﺘﻪ ﺑﺎﺷﺪ ﺩﺭ ﻏﻴﺮ ﺍﻳﻨﺼﻮﺭﺕ ﺑﻌﺪ ﺍﺯ ﺯﺩﻥ Viewﺩﺳﺘﮕﺎﻩ Error 110ﺭﺍ ﻣﻲﺩﻫﺪ.
ﺍﺳﺎﻣﻲ ﻛﺘﺎﺏ/ﻧﻮﻳﺴﻨﺪﻩ
ﻗﻴﻤﺖ )ﺭﻳﺎﻝ( ﺗﻌﺪﺍﺩ ﻣﺠﻠﺪﺍﺕ
RADIOLOGY 200,000
ﺗﻚ ﺟﻠﺪﻱ
)Pediatric Radiology (The Requestions) (Hans Blickman
1.
240,000
ﺗﻚ ﺟﻠﺪﻱ
)Differential Diagnosis in Conventioanl Gastrointestinal Readiology (Francis A. Burgener, Marti Konnano
2.
500,000
ﺗﻚ ﺟﻠﺪﻱ
)Dynamic Radiology of the Abdomen: Normal and Pathologic Anatomy (Morton A. Meyers, 5 Edition Springer Verla
3.
250,000
ﺗﻚ ﺟﻠﺪﻱ
)Primary Care Radiology (Mettker, Guibert EAU. VO.SS', URBINA
4.
400,000
ﺗﻚ ﺟﻠﺪﻱ
)Textbook of Uroradiology (N. Reed Dunnick, MD, Carl M. Sandler, Md, Jeffrey H. Newhouse, MD, Estephen Amis', JR., MD
5.
400,000
ﺗﻚ ﺟﻠﺪﻱ
)Head and Neck Radiology a Teaching File (Anthony a Mancusd, Hiroya Ojiri, Ronald G. Quisling)(Lippincottt Williams & Wilkins
6.
700,000
ﺩﻭ ﺟﻠﺪﻱ
)Essentials of Skeletal Radiology (Terry R. Yochum; Lindsay J. Rowe
7.
th
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
75
)Textbook of Radiology & Imaging (David Stutton) (2003
8.
)Radiology Reviw Manual (Fourth Edition) (Wolfgang Dahnert) (2003
9.
1,400,000
ﺩﻭ ﺟﻠﺪﻱ )ﺍﻭﺭﮊﻳﻨﺎﻝ(
400,000
ﺗﻚ ﺟﻠﺪﻱ
300,000
ﺗﻚ ﺟﻠﺪﻱ
)10. Forensic Radiology (B. G. Brogdon MD
400,000
ﺗﻚ ﺟﻠﺪﻱ
)11. The Core Curriculum Neuroradiology (Mauricio Castillo) (Lippincott Williams & Wilkins
500,000
ﺗﻚ ﺟﻠﺪﻱ
)12. Diagnostic Neuroradiology (Anne G. Osborn) (Mosby
300,000
ﺗﻚ ﺟﻠﺪﻱ
)13. Bone and Joint Disorders (Conventional Radiologic Differentioal Diagnosis) (Francis A. Burgener Marti Kormano
400,000
ﺗﻚ ﺟﻠﺪﻱ
)14. Atlas of Radiologic Measurement (Theodore E. Keats, Christopher Sistrom) (Mosby
400,000
ﺗﻚ ﺟﻠﺪﻱ
)15. Radiobiology for the Radiologist (Fifthe Edition
470,000
ﺗﻚ ﺟﻠﺪﻱ
)16. Anatomy Positioning & Procedures Workbook (Steven G. Hayes
700,000
ﺗﻚ ﺟﻠﺪﻱ
)17. Atlas of Normal Roentgen Variants That May Simulate disease (Seven Edition) (Theodere E. Keats & Mark W. Anderson) (Mosby
50,000
ﺗﻚ ﺟﻠﺪﻱ
ﻣﺒﺎﻧﻲ ﺍﺳﺎﺳﻲ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﻭ ﺗﺠﻬﻴﺰﺍﺕ ﺁﻥ )ﺗﺮﺟﻤﻪ ﻭ ﮔﺮﺩﺁﻭﺭﻱ :ﺩﻛﺘﺮ ﭘﺮﻭﻳﻦ ﻋﻠﻲﭘﻮﺭ( 18.
180,000
ﺗﻚ ﺟﻠﺪﻱ
ﺍﺻﻮﻝ ﺗﺸﺨﻴﺼﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺴﺘﺎﻥ )ﺩﻛﺘﺮ ﻣﻌﺼﻮﻣﻪ ﮔﻴﺘﻲ ،ﺩﻛﺘﺮ ﺍﻟﻬﺎﻡ ﺭﺣﻴﻤﻴﺎﻥ ،ﺩﻛﺘﺮ ﻋﻠﻲ ﻋﺮﺏ ﺧﺮﺩﻣﻨﺪ( 19.
50,000
ﺗﻚ ﺟﻠﺪﻱ
ﺷﺎﻳﻌﺘﺮﻳﻦﻫﺎ ،ﻧﺎﺩﺭﺗﺮﻳﻦﻫﺎ ،ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ،ﺑﻬﺘﺮﻳﻦ ﺭﻭﺵ ﺗﺸﺨﻴﺺ ﺑﻴﻤﺎﺭﻱﻫﺎ )ﺗﺄﻟﻴﻒ :ﺩﻛﺘﺮ ﺍﺣﻤﺪ ﻋﻠﻴﺰﺍﺩﻩ( 20.
380,000
ﺩﻭ ﺟﻠﺪﻱ
)21. Radiographic Anatomy Positioning and Procedures Workbook (Second Edition) (volume I , II) (Steven G. Hayes, Sr.
600,000
ﺗﻚ ﺟﻠﺪﻱ
250,000
ﺗﻚ ﺟﻠﺪﻱ
)23. Imaging Atlas of Human Anatomy (Third Edition) (Jamie Weir, Peter H. Abrahams) (2003
600,000
ﺗﻚ ﺟﻠﺪﻱ
)24. Pediatric Sonography (Third Edition) (Thieme) (Francis A. Burgener, Steven P. Meyers) (2004
500,000
ﺗﻚ ﺟﻠﺪﻱ
)25. Musculoskeletal Imaging Companion (Thomas H. Berquist) (2002
ﺗﻚ ﺟﻠﺪﻱ
)26. Practical Guide to Abdominal & Pelvic MRI (John R. Leyendecker, Jeffrey J. Brown
در اﯾﻦ ﮐﺘﺎب ،ﻗﺴﻤﺖ اﻋﻈﻢ ﺟﺪاول و ﻧﻤﻮدارﻫﺎی ﻣﻌﻢ ﮐﺎرﺑﺮدی ﻣﺮﺗﺒﻂ ﺑﺎ اﻧﺪازهﮔﯿﺮیﻫﺎی رادﯾﻮﻟﻮژی و ﺗﺼﻮﯾﺮﺑﺮداری در 14ﻣﺒﺤﺚ و در 630ﺻﻔﺤﻪ ﮔﺮدآوری ﮔﺮدﯾﺪه و ﻣﯽﺗﻮاﻧﺪ ﺑﻪ ﻋﻨﻮان ﯾﮏ اﺑﺰار ﺑﺴﯿﺎر ﻣﻬﻢ در ﺗﻔﺴﯿﺮ ﻧﻮاﺣﯽﻫﺎی ﻣﺨﺘﻠﻒ ﻣﻮرد اﺳﺘﻔﺎده ﻗﺮار ﮔﯿﺮد .ﻓﺼﻮل اﯾﻦ ﮐﺘﺎب ﺑﻪ ﻗﺮار ذﯾﻞ ﻣﯽﺑﺎﺷﻨﺪ: ﻣﺤﺘﻮﯾﺎت اﯾﻨﺘﺮاﮐﺮاﻧﯿﺎل -ﺟﻤﺠﻤﻪ ﺣﻔﺮه ادرﺑﯿﺖ و ﺳﯿﻨﻮسﻫﺎی ﭘﺎراﻧﺎﻣﺎل -ﻣﺤﺘﯿﺎت ادرﺑﯿﺖ ﺻﻮرت و ﮔﺮدن -ﺳﺘﻮن ﻓﻘﺮات و ﻣﺤﺘﻮﯾﺎت آن -اﻧﺪام ﻓﻮﻗﺎﻧﯽ -ﻟﮕﻦ و ﻣﻔﺎﺻﻞ - Hipاﻧﺪام ﺗﺤﺘﺎﻧﯽ ﺑﯿﻮﻣﺘﺮی و ﭘﻠﻮﺳﯿﺘﺮی در ﺟﺮﯾﺎن ﺣﺎﻣﻠﮕﯽ -ﺳﯿﺴﺘﻢ ﻋﺮوﻗﯽ و ﻟﻨﻔﺎوی ﺗﻮراﮐﺲ ،رﯾﻪﻫﺎ ،ﻣﺪﯾﺎﺳﺘﻦ و ﺟﻨﺐ -دﺳﺘﮕﺎه ﮔﻮارش -دﺳﺘﮕﺎه ادراری -ﺗﻨﺎﺳﻠﯽ ﻗﻠﺐ و ﻋﺮوق ﺑﺰرگ -ﺑﻠﻮغ اﺳﮑﻠﺘﯽ
)(Lippincott Williams & Wilkins) (2003
)(Ronald L. Eisenberg
)22. Gastrointestinal Radiology A Pattern Approach (4th Edition
اﯾﻦ ﮐﺘﺎب ﻣﺠﻤﻮﻋﮥ ﮐﺎﻣﻠﯽ از ﻣﺒﺎﺣﺚ ﻣﺨﺘﻠﻒ ﻣﺮﺗﺒﻂ ﺑﺎ ﺗﺼﻮﯾﺮﺑﺮداری دﺳﺘﮕﺎه ﮔﻮارش ﻣﯽﺑﺎﺷﺪ .ﻣﻄﺎﻟﺐ اﯾﻦ ﮐﺘﺎب در 80ﻣﺒﺤﺚ 10 ،ﻓﺼﻞ ﺗﺪوﯾﻦ ﮔﺮدﯾﺪه و ﺣﺪود 1200ﺻﻔﺤﻪ ﺣﺠﻢ دارد روش اراﺋﻪ ﻣﻄﺎﻟﺐ در اﯾﻦ ﮐﺘﺎب ﺑﻪ ﺻﻮرت Pattern Approachﺑﻮده و ﺧﻮاﻧﻨﺪه را ﻗﺎدر ﻣﯽﺳﺎزد ﺗﺎ اﻟﮕﻮﻫﺎی ﺗﺼﻮﯾﺮﺑﺮداری ﻣﺨﺘﻠﻒ دﺳﺘﮕﺎه ﮔﻮارش را دﺳﺘﻪﺑﻨﺪی ﻧﻤﻮده و ﺗﺸﺨﯿﺺﻫﺎی اﻓﺘﺮاﻗﯽ ﻫﺮ ﮐﺪام را ﺑﻪ ﺧﻮﺑﯽ از دﯾﮕﺮ اﻟﮕﻮﻫﺎ ﺗﻤﯿﺰ دﻫﺪ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
76
SONOGRAPHY 350,000
ﺗﻚ ﺟﻠﺪﻱ
)27. Ultrasonography in Urology A Practical Approach to Clinical Problems (Edward I. Bluth-Peter H.
70,000
ﺗﻚ ﺟﻠﺪﻱ
28. Seminars in Ultrasound CT and MR
1,400,000
ﺩﻭ ﺟﻠﺪﻱ
)29. Diagnostic Ultrasound (Rumack, Wilson, Charboneau) (2005 ﭼﺎپ اول اﯾﻦ ﮐﺘﺎب ﮐﻪ در ﺳﺎل 1991ﺑﻪ ﭘﺎﯾﺎن رﺳﯿﺪ و ﺑﻪ ﻋﻨﻮان راﯾﺞﺗﺮﯾﻦ ﻣﺮﺟﻊ ﺳﻮﻧﻮﮔﺮاﻓﯽ در ﺟﻬﺎن ﻣﯽﺑﺎﺷﺪ .از آﻧﺠﺎ ﮐﻪ داﻧﺶ ﺳﻮﻧﻮﮔﺮاﻓﯽ در ﻃﻮل 6ﺳﺎل ﮔﺬﺷﺘﻪ ﭘﯿﺸﺮﻓﺖﻫﺎی ﺑﺴﯿﺎری داﺷﺘﻪ اﺳﺖ ﻧﯿـﺎز ﺑـﻪ ﺑـﺎزﻧﮕﺮی در اﯾﻦ ﮐﺘﺎب اﺣﺴﺎس ﻣﯽﺷﺪ. در اﯾﻦ ﮐﺘﺎب ﺑﯿﺶ از ﯾﮑﺼﺪ ﻧﻮﯾﺴﻨﺪه ﻣﺘﺨﺼﺺ درﺳﻮﻧﻮﮔﺮاﻓﯽ ﺗﻼش ﮐﺮدهاﻧﺪ ﺗﺎ آﺧﺮﯾﻦ دﺳﺘﺎوردﻫﺎی داﻧﺶ ﺳﻮﻧﻮﮔﺮاﻓﯽ در زﻣﯿﻨﻪ ﺗﺼﻮﯾﺮﺑﺮداری ،ﺗﺸﺨﯿﺺ و ﮐﺎرﺑﺮد آﻧﻬﺎ را ﺑﻪ رﺷـﺘﻪ ﺗﺤﺮﯾـﺮ درآوردهاﻧـﺪ .ﻓﺼـﻮل ﮐﺘـﺎب ﺷـﺎﻣﻞ ﻫﯿﺴﺘﺮوﺳﻮﻧﻮﮔﺮاﻓﯽ ﻻﭘﺎروﺳﮑﻮﭘﯿﮏ ﺳﻮﻧﻮﮔﺮاﻓﯽ و ﺗﮑﻨﯿﮏﻫﺎی ﺑﯿﻮﭘﯽ ﺗﺤﺖ ﻫﺪاﯾﺖ ﺳﻮﻧﻮﮔﺮاﻓﯽ ﻧﯿﺰ ﻣﯽﺑﺎﺷﺪ .در ﮐﻠﯽ %25ﺑﻪ ﺣﺠﻢ ﮐﻠﯽ ﮐﺘﺎب اﻓﺰوده ﺷﺪه اﺳﺖ ﺑﺤﺚ ﻋﻤﺪه اﻓﺰاﯾﺶ ﺣﺠﻢ ﻣﺮﺑﻮط ﺑﻪ ﺳﻮﻧﻮﮔﺮاﻓﯽ زﻧﺎن و زاﯾﻤﺎن ﻣﯽﺑﺎﺷﺪ. ﺗﻌﺪاد زﯾﺎدی از ﺗﺼﺎوﯾﺮ ﺟﺎﯾﮕﺰﯾﻦ ﺷﺪهاﻧﺪ و ﺑﯿﺶ از 450ﺗﺼﻮﯾﺮ ﺗﻤﺎم رﻧﮕﯽ در وﯾﺮاﯾﺶ ﺟﺪﯾﺪ وﺟﻮد دارد .ﺗﻐﯿﯿﺮات ﺟﺪﯾﺪی ﺑﺮای ﺳﻬﻮﻟﺖ ﺧﻮاﻧﺪن و درک ﻣﻄﻠﺐ در ﺳﺎﺧﺘﺎر وﯾﺮاﯾﺶ اﻧﺠﺎم ﺷـﺪه اﺳـﺖ .ﮐﺪﺑﻨـﺪیﻫـﺎی رﻧﮕـﯽ ﻣﻄﺎﻟـﺐ و ﺟﺪاول highlightﺷﺪه ﺑﺮای ﻧﮑﺎت ﮐﻠﯿﺪی ﺗﺸﺨﯿﺼﯽ اﻧﺠﺎم ﺷﺪه اﺳﺖ .ﻣﻄﺎﻟﺐ ﻣﻬﻢﺗﺮ درﺷﺖﺗﺮ ﻧﻮﺷﺘﻪ ﺷﺪهاﻧﺪ و ﻣﺮاﺟﻊ اﺳﺘﻔﺎده ﺷﺪه ﺑﻪ ﺻﻮرت دﻗﯿﻖﺗﺮی ﺑﺎزﻧﻮﯾﺴﯽ ﺷﺪهاﻧﺪ .اﯾﻦ ﮐﺘﺎب در دو ﺟﻠﺪ ﻧﻮﺷﺘﻪ ﺷﺪه اﺳـﺖ .ﺟﻠـﺪ اول ﺷـﺎﻣﻞ ﭘﻨﺞ ﻓﺼﻞ ﻣﯽﺑﺎﺷﺪ ﻓﺼﻞ اول ﺷﺎﻣﻞ ﻓﯿﺰﯾﮏ و اﺛﺮات ﺑﯿﻮﻟﻮژﯾﮏ ﺳﻮﻧﻮﮔﺮاﻓﯽ و ﻣﻮاد ﺣﺎﺟﺐ در ﺳﻮﻧﻮﮔﺮاﻓﯽ ﻣﯽﺑﺎﺷﺪ .ﻓﺼﻞ دوم ﺷﺎﻣﻞ ﺳﻮﻧﻮﮔﺮاﻓﯽ ﺳﻮﻧﻮﮔﺮاﻓﯽ ﺷﮑﻢ و ﻟﮕﻦ ،ﺗﻮراﮐﺲ و روشﻫﺎی ﻣﺪاﺧﻠﻪای ) (interrcntionalﻣﯽﺑﺎﺷـﺪ. ﻓﺼﻞ ﺳﻮم ﺳﻮﻧﻮﮔﺮاﻓﯽ Intraoperativeو ﻻﭘﺎراﺳﮑﻮﭘﯿﮏ را ﺷﺮح ﻣﯽدﻫﺪ ﻓﺼﻞ ﭼﻬﺎرم ﺗﺼﻮﯾﺮﺑﺮداری اﻋﻀﺎء ﮐﻮﭼﮏ ) (small partرا اراﺋﻪ ﻣﯽﮐﻨﺪ .ﮐﻪ ﺷﺎﻣﻞ ﮐﺎروﺗﯿﺪ ،ﺷﺮﯾﺎنﻫﺎ و ورﯾﺪﻫﺎی ﻣﺤﯿﻄﯽ اﺳﺖ .ﺟﻠـﺪ دوم ﮐﺘـﺎب ﺷـﺎﻣﻞ ﻓﺼﻞ ﭘﻨﺠﻢ ﮐﻪ ﺑﺤﺚ ﮐﺎﻣﻞ ﺳﻮﻧﻮﮔﺮاﻓﯽ زﻧﺎن و ﻣﺎﻣﺎﯾﯽ اﺳﺖ و ﻧﻬﺎﯾﺘﺎً ﻓﺼﻞ ﺷﺸﻢ ﺳﻮﻧﻮﮔﺮاﻓﯽ اﻃﻔﺎل اﺳﺖ .ﺑﺨﺶ ﺟﺪﯾﺪ در ﻣﻮرد ﺳﻮﻧﻮﮔﺮاﻓﯽ داﭘﻠﺮ اﻃﻔﺎل و ﺳﻮﻧﻮﮔﺮاﻓﯽ ﻣﺪاﺧﻠﻪای در اﻃﻔﺎل ﺑﻪ اﯾﻦ ﻓﺼﻞ اﻓﺰوده ﺷﺪه اﺳﺖ .ﺧﻮاﻧﺪن اﯾـﻦ ﮐﺘﺎب ﻣﺘﺨﺼﺼﯿﻦ و دﺳﺘﯿﺎران رادﯾﻮﻟﻮژی داﻧﺸﺠﻮﯾﺎن ﭘﺰﺷﮑﯽ و ﺳﻮﻧﻮﮔﺮاﻓﻬﺎ ﺗﻮﺻﯿﻪ ﻣﯽﮔﺮدد.
ﺯﻳﺮ ﭼﺎﭖ
ﺗﻚ ﺟﻠﺪﻱ
)30. Diagnostic Ultrasound (John P. McBany Gorgon, B. Gorgon, MD) (2005
500,000
ﺗﻚ ﺟﻠﺪﻱ
)31. Ultrasound A Practical Approach to Clinical Problems (Edward Bluth, Peter H. Arger Carol B. Benson, Philip W. Rails, Marilyan) (Thieme
800,000
ﺗﻚ ﺟﻠﺪﻱ
)32. Breast Ultrasound (A. Thomas Stavros, MD, FACR) (2004
500,000
ﺗﻚ ﺟﻠﺪﻱ
)33. Musculosceletal Ultrasound (Thomas R. Nelson, Donal B. downey, Dolores H. Pretorius, A aron Fenster
400,000
ﺗﻚ ﺟﻠﺪﻱ
)34. The Core Curriculum Ultrasound (William E. Brant) (Lippincott Williams & Wilkins
800,000
ﺗﻚ ﺟﻠﺪﻱ
2005
35. Ultrasound in Obstetrics and Gynecology (Eberhard Merz) (Thieme) (Vol.1: Obstetrics )36. Color Atlas of Ultrasound Anatomy (B. Block) (Thieme) (2004
450,000 CT 250,000
ﺗﻚ ﺟﻠﺪﻱ
)37. Fundamentals of Body CT (Second Edition) (Webb & Brant & Helms
240,000
ﺗﻚ ﺟﻠﺪﻱ
38. Body CT A Practical Approach
280,000
ﺗﻚ ﺟﻠﺪﻱ
)39. High Resolution CT of the Lung (W. Richard Webb
320,000
ﺗﻚ ﺟﻠﺪﻱ
)40. High Resolution CT of the Chest Comprehensive Atlas (Second Edition) (Eric J. ster, Stephen J. Swensen)(Lippincott Williams&Wilkins
320,000
ﺗﻚ ﺟﻠﺪﻱ
)41. Pediatric Body CT (Marilyn J. Siegel
250,000
ﺗﻚ ﺟﻠﺪﻱ
)42. CT Teaching Manual (Marthias Hofer) (Thieme) (2000
550,000
ﺗﻚ ﺟﻠﺪﻱ
)43. CT Teaching Manual (A Systematic Approach to CT Reading) (Second Edition) (Thieme) (2005
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
77
44. Spiral CT (Eliot K Fishman & R. Brocke Jeffrey)
ﺗﻚ ﺟﻠﺪﻱ
400,000
45. Helical (Spiral) computed Tomography (A Practical Approach to Clinical Protocols) (Paul M. Silverman)
ﺗﻚ ﺟﻠﺪﻱ
250,000
46. Norma findings in CT and MRI (Torsten B. Moeller, EmilReif) (Thieme)
ﺗﻚ ﺟﻠﺪﻱ
300,000
47. CT and MR Imaging of the Whole Body (John R. Haaga, MD) (2003)
ﺩﻭ ﺟﻠﺪﻱ
1,000,000
48. Multidetector CT (Principles, Techniques, & Clinical Applications) (Elliot K. Fissman, R. Brooke Jeffrey, JR.)
ﺗﻚ ﺟﻠﺪﻱ
550,000
49. Spiral and Multislice Computed Tomography of the Body (Aart J. Van der Molen Cornelia M. Schaefer-Prokop) (Thieme) (2003)
ﺗﻚ ﺟﻠﺪﻱ
800,000
50. MRI of the Musculoskeletal System (Thomas H. Berquist)
ﺗﻚ ﺟﻠﺪﻱ
600,000
51. MRI of the Musculoskeletal System MRI Teaching file Series (Karence K Cahn, Mini Pathria)
ﺗﻚ ﺟﻠﺪﻱ
240,000
52. MRI of the Head and Neck MRI Teaching file Series (Jrffrey S. Ross)
ﺗﻚ ﺟﻠﺪﻱ
240,000
53. MRI of the Spine MRI Teaching file Series (Jeffrey S. Ross)
ﺗﻚ ﺟﻠﺪﻱ
240,000
54. MRI of the Brain I & II MRI Teaching file Series (Michel Brant, Zawadzki and…)
ﺩﻭ ﺟﻠﺪﻱ
480,000
55. MRI the basics fray h. Hashemi and William g. bradley, Jr.) (Williams & Wilkins)
ﺗﻚ ﺟﻠﺪﻱ
35,000
56. MRI Principles (Donald G. Mitcell, MD)
ﺗﻚ ﺟﻠﺪﻱ
190,000
57. Clinical Pelvic Imaging CT, Ultrasound, and MRI (Arnold C. Friedman, MD)
ﺗﻚ ﺟﻠﺪﻱ
300,000
58. Magnetic Resonance in Medicine The Basic Textbook of the European Magnetic Resonance Forum (Peter A. Rinck)
ﺗﻚ ﺟﻠﺪﻱ
105,000
59. Magnetic Resonance in diagnosis of C.N.S. disorders (vaso antunavic, gradimir dragutinovic, zvonimir lec) (Thieme)
ﺗﻚ ﺟﻠﺪﻱ
450,000
60. Section and MRI anatomy of the human body (slobodan marinkovic, milan milisavljevic, dieter sehellinger, vaso antunovic) (Thieme)
ﺗﻚ ﺟﻠﺪﻱ
450,000
61. PRACTICAL GUIDE TO ABDOMINAL & PELVIC MRI (JOHN R. LEYENDECHER, JEFFERY J. BROWN)
ﺗﻚ ﺟﻠﺪﻱ
450,000
62. Vascular diagnosis with Ultrasound Clinical References With Case Studies (Hennerici, Neuerburg-Heusler)(Thieme)
ﺗﻚ ﺟﻠﺪﻱ
600,000
63. Introduction to Vascular Ultrasonography (Fourth Edition) (Zwiebel) (James Saunders)
ﺗﻚ ﺟﻠﺪﻱ
600,000
MRI
Doppler
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺭﺍ ﺍﺯ ﻧﻈﺮ ﺩﻭﺭ ﻧﺪﺍﺷﺘﻪ ﻭ ﺍﻳﻦ ﺭﻭﺵ ﺭﺍ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺷﻴﻮﻩ ﺁﻟﺘﺮﻧﺎﺗﻴﻮ ﻏﻴﺮﺗﻬﺎﺟﻤﻲ ﻛﺎﺭﺁﻣﺪ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻋﺮﻭﻕ ﺑﺪﻥ ﺩﺭ ﻛﻨـﺎﺭ ﺁﻧﮋﻳـﻮﮔﺮﺍﻓﻲ، ﭘﻴﺸﺮﻓﺖﻫﺎﻱ ﺍﺧﻴﺮ ﺩﺭ ﻋﺮﺻﻪ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺷـﺎﻣﻞ ﺳﺮﻓﺼـﻞﻫـﺎﻱ. ﻣﺒﺤﺚ ﺟﺰﺋﻲﺗﺮ( ﺑﻪ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺁﺧﺮﻳﻦ ﺩﺳﺘﺎﻭﺭﺩﻫﺎﻱ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺩﺭ ﺗﺸﺨﻴﺺ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﺍﺭﮔﺎﻥﻫﺎﻱ ﺑﺪﻥ ﻣﻲﭘﺮﺩﺍﺯﺩ٣١ ﺑﺨﺶ ﺍﺻﻠﻲ )ﻣﺸﺘﻤﻞ ﺑﺮ٥ ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ.ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﺍﺳﺖ :ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ ﻭ ﺗﺠﻬﻴﺰﺍﺕ ﻻﺯﻡB-mode ﻓﻴﺰﻳﻚ ﺩﺍﭘﻠﺮ ﻭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ.٢ ﻧﻜﺎﺕ ﻗﺎﺑﻞ ﺗﻮﺟﻪ ﻫﻤﻮﺩﻳﻨﺎﻣﻴﻚ ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻋﺮﻭﻕ ﻣﺤﻴﻄﻲ.١ : ﺍﺻﻮﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ-ﺍﻟﻒ ﻣﻮﺍﺩ ﺣﺎﺟﺐ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ.٥ ﻧﻘﺶ ﺩﺍﭘﻠﺮ ﺭﻧﮕﻲ ﺩﺭ ﺗﺸﺨﻴﺺ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻋﺮﻭﻗﻲ.٤ ﺁﻧﺎﻟﻴﺰ ﻃﻴﻒ )ﻣﻮﺝ( ﻓﺮﻛﺎﻧﺲ ﺩﺍﭘﻠﺮ.٣ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
78
ﺍﺭﺯﻳﺎﺑﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﭘﻼﻙ ﻛﺎﺭﻭﺗﻴﺪ.٩ ﺷﺮﺍﺋﻴﻦ ﻛﺎﺭﻭﺗﻴﺪ ﻧﺮﻣﺎﻝ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﭘﻠﺮ ﻛﺎﺭﻭﺗﻴﺪ.٨ ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ﻋﺮﻭﻕ ﻣﻐﺰﻱ.٧ ﻣﻘﻴﺎﺱ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﻋﺮﻭﻕ ﻣﻐﺰﻱ.٦ : ﻋﺮﻭﻕ ﻣﻐﺰﻱ-ﺏ (TCD) ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺗﺮﺍﻧﺲ ﻛﺮﺍﻧﻴﺎﻝ.١٣ ﺍﺭﺯﻳﺎﺑﻲ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻴﻚ ﻋﺮﻭﻕ ﻭ ﺭﺗﺒﺮﺍﻝ.١٢ ( ﺩﻳﺴﻜﻨﺴﻴﻮﻥ- ﻣﻮﺿﻮﻋﺎﺕ ﻣﺘﻔﺮﻗﻪ ﺑﺎ ﻛﺎﺭﻭﺗﻴﺪ )ﺷﺎﻣﻞ ﺍﺳﺪﺍﺩ.١١ ﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﭘﻠﺮ ﺗﻨﮕﻲ ﻛﺎﺭﻭﺗﻴﺪ.١٠ ﻧﻘﺶﻫﺎﻱ ﻓﻴﺰﻳﻮﻟﻮﮊﻳﻚ ﺟﻬﺖ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺮﻳﺎﻧﻲ ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻲ.١٦ ﺁﻧﺎﺗﻮﻣﻲ ﺷﺮﻳﺎﻧﻲ ﺍﻧﺪﺍﻡﻫﺎ.١٥ ﻧﻘﺶ ﺭﻭﺵﻫﺎﻱ ﻏﻴﺮﺗﻬﺎﺟﻤﻲ ﺩﺭ ﭘﻲﮔﻴﺮﻱ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺮﻳﺎﻧﻲ ﺍﻧﺪﺍﻡﻫﺎ.١٤ : ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ-ﺝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻲ.١٨ ﺍﺭﺯﻳﺎﺑﻲ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ.١٧ ( ﺍﺭﺯﻳﺎﺑﻲ ﻭﺭﻳﺪﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ )ﺟﻨﺒﻪﻫﺎﻱ ﺗﻜﻨﻴﻜﻲ.٢٢ ﺗﺮﻣﻴﻨﻮﻟﻮﮊﻱ ﻭ ﻛﺎﺭﺍﻛﺘﺮﻫﺎﻱ ﻧﺮﻣﺎﻝ.٢١ ﺁﻧﺎﺗﻮﻣﻲ ﻭﺭﻳﺪﻱ ﺍﻧﺪﺍﻡﻫﺎ.٢٠ ﻣﻘﻴﺎﺱ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺩﺭ ﺍﺭﺯﻳﺎﺑﻲ ﻭﺭﻳﺪﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ.١٩ : ﻭﺭﻳﺪﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ-ﺩ ( ﻭ ﭘﺎﻣﻮﻟﻮﮊﻱ ﻏﻴﺮﻭﺭﻳﺪﻱ ﺍﻧﺪﺍﻡAVF) ﻓﻴﺴﺘﻮﻝ ﺷﺮﻳﺎﻧﻲ ﻭﺭﻳﺪﻱ.٢٤ ﺗﺮﻭﻣﺒﻮﺯ ﻭﺭﻳﺪﻱ.٢٣ ﺍﺧﺘﻼﻻﺕ ﻋﺮﻭﻗﻲ ﻛﺒﺪ.٢٩ ﺍﺭﺯﻳﺎﺑﻲ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻴﻚ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﺣﺸﺎﺋﻲ.٢٨ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻳﻠﻴﺎﻙ، ﺁﺋﻮﺭﺕ.٢٧ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻧﻤﺎﻫﺎﻱ ﻧﺮﻣﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﺩﺍﭘﻠﺮ ﻋﺮﻭﻕ ﺷﻜﻤﻲ.٢٦ : ﻋﺮﻭﻕ ﺷﻜﻤﻲ-ه Penis ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻣﻌﻤﻮﻟﻲ ﻭ ﺩﺍﭘﻠﺮ.٣١ ( ﻭ ﻛﻠﻴﺔ ﭘﻴﻮﻧﺪﻱNative ﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﭘﻠﺮ ﻋﺮﻭﻕ ﻛﻠﻴﻮﻱ )ﻣﺮﺑﻮﻁ ﺑﻪ ﻛﻠﻴﺔ.٣٠ 64. Teaching Manual of Color Duplex Sonography A Wokbook in color duplex ultrasound and echocardiographer (Matthias Hofer) (Thieme) (2005)
ﺗﻚ ﺟﻠﺪﻱ
550,000
65. Vascular Ultrasound of the Neck an Interpretive atlas (Antonio Alayon)(Lippincott Williams & Wilkins)
ﺗﻚ ﺟﻠﺪﻱ
400,000
66. Duplex Scanning in Vascular Disorders (Third Edition) (D. Eugene Strandness, Jr.)
ﺗﻚ ﺟﻠﺪﻱ
600,000
67. Doppler Ultrasound in Gynecology and Obstetrics (Christof Sohn, Hans-Joachim Voigt, Klaus Vetter) (2004)
ﺗﻚ ﺟﻠﺪﻱ
500,000
ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ
500,000
ﺗﻚ ﺟﻠﺪﻱ ﺩﻭ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ
4 00,000
Imaging 68. Skeletal Imaging Atlas of the Spine and Extremities (John A. M. Donald Resnick, MD) 69. Imaging for Surgeons 70. Imaging of the Newborn, Infant and Young Child (Fourth Edition) (Leonard E. Swischuk) (2004) 71. Thoracic Imaging A Practical Approach (Richard H. slone Fernando R. Gutier) 72. Gastrointestinal Imaging, Case Review (Peter J. Feczko, Obert d. Halperi) 73. Imaging in Hepatobiliary and Pancreatic Disease A Practical Clinical Approach (Dirk Van Leeuwen, Jacques Reeders, Joe Ariyama) 74. Aids Imaging A Practical Clinical Approach (J WA J. Reeders, J. R. Mathieson) 75. Special Procedures in diagnostic Imaging (C'lark's)(A. Stewart Whitley, Chrissie W. Alsop Adrin D. Moore) 76. Breast Imaging (Second Edition) (David B. Kopans) 77. The Core curriculum Breast Imaging (Gilda Cardenosa) 78. Neuroimaging I & II (William It. On'ison, jr) 79. Fundamentals of Neuroimaging (William w. Woodruff.M.D.) 80. Magnetic Resonance Imaging computed Tomography of the Head and Spine (C. Barrie Grossman) 81. Atlas of Musculoskeletal Imaging (Thomas Lee Pope, Jr. Stephen Loehr)(Thieme) 82. Atlas of Head and Neck Imaging (The Extracranial Head and Neck) (Suresh K. Mukherji, Vincent chong) 83. Magnetic Resonance Imaging of Orthopeadic Trauma (Stephen J. Eustace)(Lippincott Williams & Wilkins) ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
90,000 600,000 250,000 250,000 500,000 420,000 350,000 500,000 900,000 360,000 400,000 420,000 500,000 250,000
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
79
)84. Pediatric Gastrointestinal Imaging and Intervention (David A. Stringer-Paul S. Babyn MDCM
500,000
ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ
87. Clinical Imaging
1,100 ,000
ﺗﻚ ﺟﻠﺪﻱ
)88. Diagnostic Imaging Brain (Osborn) (2004
900,000
ﺗﻚ ﺟﻠﺪﻱ
1,000 ,000
ﺗﻚ ﺟﻠﺪﻱ
)90. Diagnostic Imaging Head and Neck (Harnsberger) (2004
1,350 ,000
ﺗﻚ ﺟﻠﺪﻱ
)91. Cranial Neuroimaging and Clinical Neuroanatomy Atlas of MR Imaging and Computed Tomography (Hans-Joachim Kretschmann
450,000
ﺗﻚ ﺟﻠﺪﻱ
)92. DIAGNOSTIC MUSCULOSKELETAL IMAGING (THEODORE T. MILLER, MARK E. SCHWEITZER) (2005
700,000
ﺗﻚ ﺟﻠﺪﻱ
)93. Orthopedic IMAGING (A Pracitcal Approach) (ADAM GREENSPAN) (Michael W. Chapman) (2004
250,000
ﺗﻚ ﺟﻠﺪﻱ
)94. Aids to RADIOLOCIAL DIFFERENTIAL DIAGNOSIS (Forth Edition) (Stephen Chapman and Richard Nakielny) (2003
260,000 500,000 580,000
)85. Modern Head and Neck Imaging Medical Radiology, Diolopy, Nostic Imaging (S. K. Mukhetji, J. A. castelijins)(Springer )86. Variants and Pitfalls in Body Imaging (Ali Shirkhoda)(Lippincot Williams & Wilkin's
ﻣﺪﺕ ﻃﻮﻻﻧﻲ ﺑﻮﺩ ﻛﻪ ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎ ،ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻳﺴﺖﻫﺎ ،ﻧﻮﺭﻭﭘﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﺟﺮﺍﺣﺎﻥ ﺍﻋﺼﺎﺏ ﻣﻨﺘﻈﺮ ﻛﺘﺎﺏ ﺟﺪﻳﺪﻱ ﺍﺯ ﺩﻛﺘﺮ " "Ann Osbornﺑﻮﺩﻧﺪ .ﺍﻳﻦ ﻛﺎﺭ ﺟﺪﻳﺪ ﻧﻤﺎﻳﺎﻧﮕﺮﻱ ﺍﺯ ﻛﺘﺐ ﻣﺮﺟﻊ ﺩﺭ ﻗﺮﻥ ٢١ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﻳﮕﺮ ﻣﺎﻧﻨﺪ ﻛﺘﺎﺏﻫﺎﻱ ﻗﺪﻳﻤﻲﺗﺮ ﺍﻃﻼﻋﺎﺕ ﺑﺴﻴﺎﺭ ﺯﻳﺎﺩ ﺭﺍ ﺑﻪ ﺻﻮﺭﺕ ﻓﺸﺮﺩﻩ ﻭ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺍﻧﺪﻙ ﺍﺭﺍﺋﻪ ﻧﻤﻲﺩﻫﺪ ﺑﻠﻜﻪ ﺑﺎ formatﻣﺪﺭﻥ ﻭ ﭘﻴﺸﺮﻓﺘﻪ ﺧﻮﺩ ﺩﻭ ﺑﺮﺍﺑﺮ ﺍﻃﻼﻋﺎﺕ ﻭ ﭼﻬﺎﺭ ﺑﺮﺍﺑﺮ ﺗﺼﺎﻭﻳﺮ ﺑﻴﺸﺘﺮﻱ ﺑﺮﺍﻱ ﻫﺮ ﺗﺸﺨﻴﺺ ﺩﺍﺭﺩ .ﻛﻴﻔﻴﺖ ﺗﺼﺎﻭﻳﺮ ﻭ ﮔﺮﺍﻓﻴـﻚﻫـﺎ ﻭﺍﻗﻌـﹰﺎ ﻋﺎﻟﻴﺴـﺖ ﻭ ﺟﻬﺖ ﺑﻬﺘﺮﻧﺸﺎﻥﺩﺍﺩﻥ ﺗﺼﺎﻭﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﺍﺳﺘﻔﺎﺩﺓ ﺯﻳﺎﺩﻱ ﺍﺯ ﺭﻧﮓﻫﺎ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺑﺘﻜﺎﺭ ﺩﻳﮕﺮ ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻳﻦ ﺍﺳﺖ ﻛﻪ ﻣﻮﺍﺭﺩ ﻭ ﺗﺼﺎﻭﻳﺮ ﻣﺸﺎﺑﻪ ﻭ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻕ ﺭﺍ ﺩﺭ ﻫﻤﺎﻥ ﻓﺼﻞ ﺟﻬﺖ ﺑﺮﺭﺳﻲ ﺑﻴﺸﺘﺮ ﺍﺭﺍﺋﻪ ﻧﻤﻮﺩﻩ ﺍﺳﺖ .ﺷﺎﻳﺪ ﺑﺘـﻮﺍﻥ ﮔﻔﺖ ﻛﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﻳﻚﺟﻠﺪﻱ "ﺍﻳﻨﺘﺮﻧﺖ" ﻧﻮﺭﻭﻟﻮﮊﻱ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ CNSﻣﻲﺑﺎﺷﺪ :ﻛﺎﻣﻞ ،ﻣﻮﺟﺮ ﻭ ﺑﺮﻭﺯ ﺑﻄﻮﺭﻳﻜﻪ ﺣﺘﻲ ﻛﻠﻤﻪﺍﻱ ﺭﺍ ﻧﻤﻲﺗﻮﺍﻥ ﻳﺎﻓﺖ ﻛﻪ ﺍﺿﺎﻓﻲ ﻧﮕﺎﺷﺘﻪ ﺷﺪﻩ ﺑﺎﺷﺪ. PART I (Pathology-based diagnoses): Congenital malformations-Trauma Sulianachnoid hemorrhage and Aneurisms-Stroke-Vascular Malformations Neoplasm's and Tumor in lesions-Primary Non-neoplastic cystsInfection and Demyelinating Disease-Metabolic/Degenerative Disorders, Inhenited-Toxic/Metabolic/Degenesative Disorders, Acquired PART II (Anatomy-based Diagnoses): Ventricles and Cysterns-Sella and Pitutary-CPA-IAC-Skull, Scalp and Meninges
ﺗﻮﺿﻴﺤﺎﺕ ﺍﺭﺍﺋﻪﺷﺪﻩ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﺑﻴﻤﺎﺭﻱ ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: Terminology-Imaging Findings-Differentioal Diagnosis-Pathology Clinical Issues-Selected references-Imaging Gallery-Key Facts
ﻫﺮ ﺟﺎﻳﻲ ﻛﻪ ﻻﺯﻡ ﺑﻮﺩﻩ ﺍﺳﺖ ﺗﻮﺿﻴﺤﺎﺕ ﺿﺮﻭﺭﻱ ﺍﺯ ﺁﻧﺎﺗﻮﻣﻲ ،ﺟﻨﻴﻦﺷﻨﺎﺳﻲ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺗﺎ ﺑﻪ ﺧﻮﺍﻧﻨﺪﻩ ﺩﺭﻙ ﺗﺸﺨﻴﺺ ﻭ ﻣﻮﻗﻌﻴﺖ ﻛﻤﻚ ﻧﻤﺎﻳﺪ .ﻗﺴﻤﺖ Key Factsﺧﻼﺻﻪﺍﻱ ﺟﺎﻣﻊ ﺑﺮﺍﻱ ﻣﺮﻭﺭ ﺳﺮﻳﻊ ﻭ ﺁﺳﺎﻥ ﻣﻲﺑﺎﺷﺪ. ﺑﻪ ﻧﻈﺮ ﻣﻲﺭﺳﺪ ﻛﻪ ﻛﺘﺎﺏ " "Diagnostic Imaging Brain Osborn 2004ﻣﻨﺒﻊ ﺑﺴﻴﺎﺭ ﻏﻨﻲ ﻭ ﻣﺆﺛﺮ ﺍﺯ ﻣﻄﺎﻟﺐ ﻋﻠﻤﻲ ﺟﺪﻳﺪ ﺑـﺮﺍﻱ ﺩﺍﻧﺸـﺠﻮﻳﺎﻥ- ﺭﺯﻳﺪﻧﺖﻫﺎ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺭﺷﺘﻪﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﺍﻋﻢ ﺍﺯ ﻧﻮﺭﻭﻟﻮﮊﻱ ،ﺟﺮﺍﺣﻲ ﺍﻋﺼﺎﺏ ،ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺑﺎﺷﺪ.
)(Stoller.Tirman Bredella) (2004
89. Diagnostic Imaging Orthopaedics
ﺍﻳﻦ ﻛﺘﺎﺏ ﭼﺎﭖ ﺳﻮﻡ ﻛﺘﺎﺏ Cranial Neuroimaging and Clinical Neuroanatomyﺩﺭ ﺳﺎﻝ 2004ﻣﻲﺑﺎﺷﺪ .ﺗﻤﺎﻣﻲ ﻓﺼﻮﻝ ﻛﺘﺎﺏ ﺗﻐﻴﻴﺮ ﻭ ﺑﺎﺯﻧﻮﻳﺴﻲ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻲﮔﻤﺎﻥ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﻣﻨﺎﺑﻊ ﺑﺮﺍﻱ ﻓﻬـﻢ ﻭ ﺩﺭﻙ ﺁﻧـﺎﺗﻮﻣﻲ ﻣﺴـﻴﺮﻫﺎﻱ ﻋﺼﺒﻲ ﻭ ﺳﺎﺧﺘﻤﺎﻥﻫﺎﻱ ﻋﺮﻭﻗﻲ ﻣﻲﺑﺎﺷﺪ .ﺗﺼﺎﻭﻳﺮ ﺑﺰﺭﮒ ﻭ ﺻﻔﺤﻪﺁﺭﺍﻳﻲ ﺧﻮﺏ ﺁﻥ ﺍﺟﺎﺯﻩ ﺍﺳﺘﻔﺎﺩﻩ ﺁﺳﺎﻥ ﻭ ﺩﺳﺘﺮﺳﻲ ﺳﺮﻳﻊ ﺭﺍ ﻣﻴﺴﺮ ﻣﻲﺳﺎﺯﺩ. ﻣﻘﺪﻣﻪ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﺑﺤﺚ ﮔﺴﺘﺮﺩﻩﺍﻱ ﺩﺭ ﻣﻮﺭﺩ ﺁﺯﻣﻮﻥﻫﺎﻱ ﻧﻮﺭﻭﻟﻮﮊﻱ ﻭ ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎﻱ ﺁﻧﻬﺎﺳﺖ .ﻭ ﺭﺍﻫﻨﻤﺎﻱ ﺧﻮﺑﻲ ﺑﺮﺍﻱ ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﺻﺤﻴﺢ ﻭ ﺑﺠﺎ ﺍﺯ ﺁﺯﻣﻮﻥﻫﺎﻱ ﻋﺼﺒﻲ ﻣﻲﺑﺎﺷﺪ. ﭼﺎﭖ ﺟﺪﻳﺪ ﻛﺘﺎﺏ ﺣﺎﻭﻱ ﺗﺼﺎﻭﻳﺮ ﺟﺪﻳﺪ ﺩﺭ ﻣﻮﺭﺩ ﺳﺎﺧﺘﻤﺎﻥﻫﺎﻱ ﻋﺮﻭﻗﻲ ﺣﻔﺮﻩ ﺣﻠﻘﻲ ﺍﺳﺖ .ﮔﺴﺘﺮﺵ ﺳﺮﻳﻊ MRIﻭ ﺗﺼﺎﻭﻳﺮ NeuroFunctionalﻧﻴﺎﺯ ﺑﻴﺸﺘﺮ ﺑﻪ ﺍﻳﻦ ﻧﻮﻉ ﺑﺤﺚﻫﺎﻱ ﻛﺎﺭﺑﺮﺩﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺭﺍ ﺩﺍﺭﺩ ﺑـﺎ ﻣﺮﺍﺟﻌـﻪ ﺑـﻪ ﺍﻳـﻦ ﻛﺘـﺎﺏ ﻣـﻲﺗـﻮﺍﻥ ﺍﺯ ﺳﺎﺧﺘﻤﺎﻥﻫﺎﻱ ﺩﻗﻴﻖ ﻋﺮﻭﻕ ﺗﺮ ﻣﺴﻴﺮﻫﺎﻱ ﺍﻟﻴﺎﻑ ﻋﺼﺒﻲ ﻭ ﻣﺴﻴﺮ ﺍﻋﺼﺎﺏ ﻛﺮﺍﻧﻴﺎﻝ ﺁﮔﺎﻫﻲ ﻳﺎﻓﺖ ﻭ ﻋﻼﻳﻢ ﺑﺎﻟﻴﻨﻲ ﺑﺴﻴﺎﺭﻱ ﺭﺍ ﺑﺎ ﻳﺎﻓﺘﻪﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﻄﺎﺑﻘﺖ ﺩﺍﺩ .ﺗﺼﺎﻭﻳﺮ ﺳﻲﺗﻲﺍﺳﻜﻦ ﻭ MRIﺩﺭ ﻣﻘﺎﻃﻊ ﻛﺮﻭﻧﺎﻝ ،ﺍﮔﺰﻳﺎﻝ ،ﺳﺎﮊﻳﺘﺎﻝ ﺑﻪ ﻧﻤﺎﻳﺶ ﮔﺬﺍﺷﺘﻪ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﺑﺎ ﻛﺪﺑﻨﺪﻱ ﺭﻧﮕﻲ ﻭ ﺩﻳﺎﮔﺮﺍﻡﻫﺎﻱ ﺷﻤﺎﺗﻴﻚ ﻣﻄﺎﺑﻘﺖ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺗﻤﺎﻣﻲ ﻣﺘﺨﺼﺼﻴﻦ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ،ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﺟﺮﺍﺣﺎﻥ ﺍﻋﺼﺎﺏ ﺗﻮﺻﻴﻪ ﻣﻲﮔﺮﺩﺩ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
80
95. Teaching Atlas of Brain Imaging (Nancy J. Fischbein, William P. Dillon, A. James Barkovich)
ﺗﻚ ﺟﻠﺪﻱ
500,000
96. The Radiologic Clinics of North America Imaging of Obstructive Pulmonary Disease (W. Richard Webb.M.D.)
ﺗﻚ ﺟﻠﺪﻱ
150,000
97. The Radiologic Clinics of North America Neonatal Imaging (Janet L. ST. Rife, M.D.)
ﺗﻚ ﺟﻠﺪﻱ
115,000
98. The Radiologic Clinics of North America Lung Cancer (Claudia I. Henschke. Phil, M.D.)
ﺗﻚ ﺟﻠﺪﻱ
140,000
99. The Radiologic Clinics of North America Interventional Procedures in Musculoskeletal Radio I Interventional Techniques (Jamshid Tehranzadeh, MD)
ﺗﻚ ﺟﻠﺪﻱ
100,000
100. The Radiologic Clinics of North America Interventional Procedures in Musculoskeletal Radio II Advanced Arthrography (Jamshid Tehranzadeh)
ﺗﻚ ﺟﻠﺪﻱ
200,000
101. The Radiologic Clinics of North America Advances in Emergency Radiology I & II (Robert A. Novell)
ﺩﻭ ﺟﻠﺪﻱ
120,000
102. The Radiologic Clinics of North America Cardiac Radiology (Lawrence M. Boxt. MD)
ﺗﻚ ﺟﻠﺪﻱ
150,000
103. The Radiologic Clinics of North America Interventional Chest Radiology (Jeffrey S. Klein, M.D.)
ﺗﻚ ﺟﻠﺪﻱ
150,000
The Radiologic Clinics of North America
Imaging of the newborn, infant, and young child
(LEONARD E. SWISCHUK, M. D.) (FIFTH EDITION)
Borderlands of Normal and Early Pathological Finding in Skeletal Radiography (Juergen Freyschmidt, Joachim Brossmann, Juergen Wiens, Andreas Sternberg)
Clinical Imaging
(Ronald L. Eisenberg, Amelda County
(Fifth revised edition)
(Thieme)
)ﺭﺋﻴﺲ ﺩﭘﺎﺭﺗﻤﺎﻥ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻛﻠﻴﻨﻴﻜﺎﻝ
(an atlas of differential diagnosis) (Lippincott Williums & Wilkins)
(2004)
(Forth Edition)
ﺭﻳﺎﻝ600,000 :ﻗﻴﻤﺖ
(2003)
ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﻻﺯﻡ ﻭ ﺩﺭ ﻋﻴﻦ ﺣﺎﻝ ﻛﺎﻣﻞ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﻧﻤﺎﻫﺎﻱ ﮔﻮﻧﺎﮔﻮﻥ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﻲﺑﺎﺷﺪ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻣﺨﺘﻠﻒ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ ﻧﻤﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴـﻚ )ﺑﻌﻨـﻮﺍﻥ ﺍﻳـﻦ ﻛﺘـﺎﺏ ﺗﻘﺮﻳﺒـﹰﺎ ﺷـﺎﻣﻞ.( ﺗﺼﺎﻭﻳﺮ ﻣﺮﺗﺒﻂ ﺑﻪ ﻫﺮ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺭﺍ ﺑﻄﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻛﺪﺍﻡ ﻧﻴﺰ ﺗﻮﺿﻴﺤﺎﺕ ﻻﺯﻡ ﺑﺎ ﻧﮕﺎﺭﺷﻲ ﺑﺴـﻴﺎﺭ ﻗﺎﺑـﻞ ﻓﻬـﻢ ﺫﻛـﺮ ﮔﺮﺩﻳـﺪﻩ ﺍﺳـﺖmultiple Pulmonary nodules ﻼ ﻣﺜ ﹰ .( ﺩﺭ ﺁﻥ ﻟﺤﺎﻅ ﺷﺪﻩ ﺍﺳﺖ... ﻭMRI ، CTScan ، ﺳﻮﻧﻮﮔﺮﺍﻓﻲ، ﻣﻄﺎﻟﻌﺎﺕ ﺑﺎ ﻛﻨﺘﺮﺍﺳﺖ، Plain film )ﺍﺯ ﻗﺒﻴﻞImaging ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻛﻞ ﺑﺪﻥ ﺑﻮﺩﻩ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺨﺘﻠﻒ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
81
ﻓﻬﺮﺳﺖ ﻛﻠﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﻓﺼﻮﻝ ﻣﺨﺘﻠﻒ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ: -١ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ Chest
-٦ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
-٢ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ
-٧ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺟﻤﺠﻤﻪ
-٣ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ -٨ Gastrointestinalﺑﻴﻤﺎﺭﻱﻫﺎﻱ Breastﻭ ﻣﺎﻣﻮﮔﺮﺍﻓﻲ -٤ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ Genitourinary
-٩ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺟﻨﻴﻦ
-٥ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺍﺳﻜﺘﺎﻝ
ﺿﻤﻨﹰﺎ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﻓﺼﻞﻫﺎﻱ ﻓﻮﻕﺍﻟﺬﻛﺮ ،ﺩﺭ ﺍﺑﺘﺪﺍﻱ ﻫﺮ ﻓﺼﻞ ،ﻓﻬﺮﺳﺖ ﻛﺪﺩﺍﺭ ﻭﻳﮋﻩﺍﻱ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻧﺸﺎﻧﻪﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﻣﺮﺑﻮﻁ ﺑﻪ ﻣﺒﺤﺚ ﻣﺬﻛﻮﺭ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺗﺴﻬﻴﻞ ﻭ ﺗﺴﺮﻳﻊ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺴـﻴﺎﺭ ﻣـﺆﺛﺮ ﺧﻮﺍﻫـﺪ ﺑـﻮﺩ. ﻣﻄﺎﻟﻌﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺭﺯﺷﻤﻨﺪ ﺑﺮﺍﻱ ﺷﺮﻛﺖ ﺩﺭ ﺍﻣﺘﺤﺎﻧﺎﻥ ﺑﺮﺩ ﺗﺨﺼﺺ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﻫﻤﭽﻨﻴﻦ ﻛﺎﺭ ﻋﻤﻠﻲ ﺩﺭ ﻣﺆﺳﺴﺎﺕ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺑﺴﻴﺎﺭ ﻣﻔﻴﺪ ﺧﻮﺍﻫﺪ ﺑﻮﺩ. ﺗﻌﺪﺍﺩ ﺻﻔﺤﺎﺕ
1307
)(Seventh Edition
)(Mosby Inc.) (2001 ﻗﻴﻤﺖ 700,000 :ﺭﻳﺎﻝ
Atlas Of Normal Roentgen Variants that may Simulate Disease )ﺩﺍﻧﺸﻴﺎﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ﻭﻳﺮﺟﻴﻨﻴﺎ , Mark W. Anderson M.d.ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ﻭﻳﺮﺟﻴﻨﻴﺎ
(Theodore E. Keats M.D.
ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ،ﺑﺎ ﻛﻤﻚ ﺗﺼﺎﻭﻳﺮ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﻣﺘﻌﺪﺩ ،ﺑﺎ ﻧﻤﺎﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻭﺍﺭﻳﺎﺳﻴﻮﻥﻫﺎﻱ ﻧﺮﻣﺎﻝ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﻢ ﻭ ﺑﺪﻳﻦ ﻃﺮﻳﻖ ﺍﺯ ﻣﻴﺰﺍﻥ Over diagnosisﻛﻪ ﻣﻤﻜﻦ ﺍﺳﺖ ﺩﺭ ﺟﺮﻳﺎﻥ ﮔﺰﺍﺭﺷﺎﺕ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﺍﺗﻔﺎﻕ ﺑﻴﺎﻓﺘﺪ ،ﻛﺎﺳـﺘﻪ ﺧﻮﺍﻫـﺪ ﺷﺪ. ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﺩﻭ ﺑﺨﺶ ﺍﺻﻠﻲ ﻣﻲﺑﺎﺷﺪ .ﺑﺨﺶ ﺍﻭﻝ ﻣﺮﺑﻮﻁ ﺑﻪ ﻭﺍﺭﻳﺎﺳﻴﻨﻮﺱﻫﺎﻱ ﻧﺮﻣﺎﻝ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺍﺳﺘﺨﻮﺍﻥﻫﺎ ﻭ ﺑﺨﺶ ﺩﻭﻡ ﻣﺮﺑﻮﻁ ﺑﻪ ﻭﺍﺭﻳﺎﺳﻴﻨﻮﺱﻫﺎﻱ ﻧﺮﻣﺎﻝ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﻣﻲﺑﺎﺷﺪ .ﺑﺨـﺶ ﺍﻭﻝ ﻭ ﺩﻭﻡ ﺷـﺎﻣﻞ ﻓﺼـﻮﻝ ﺫﻳـﻞ ﻣﻲﺑﺎﺷﻨﺪ: ﺑﺨﺶ ﺍﻭﻝ ﻓﺼﻞ -١ﺟﻤﺠﻤﻪ ﻓﺼﻞ -٢ﺍﺳﺘﺨﻮﺍﻥﻫﺎﻱ ﺻﻮﺭﺕ ﻓﺼﻞ -٣ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻓﺼﻞ -٤ﻛﻤﺮﺑﻨﺪ ﻟﮕﻨﻲ
ﺑﺨﺶ ﺩﻭﻡ
ﻓﺼﻞ -٥ﻛﻤﺮﺑﻨﺪ ﺷﺎﻧﻪﺍﻱ ﻭ ﻗﻔﺴﺔ ﺻﺪﺭﻱ ﻓﺼﻞ -٦ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ ﻓﺼﻞ -٧ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻲ
ﻗﻴﻤﺖ 500,000 :ﺭﻳﺎﻝ
ﻓﺼﻞ -٨ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﮔﺮﺩﻥ ﻓﺼﻞ -٩ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﻗﻔﺴﺔ ﺳﻴﻨﻪ ﻓﺼﻞ -١٠ﺩﻳﺎﻓﺮﺍﮔﻢ
ﺗﻌﺪﺍﺩ ﺻﻔﺤﺎﺕ:
478
)ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ Leuvenﺑﻠﮋﻳﻚ
ﻓﺼﻞ -١١ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﺷﻜﻢ ﻓﺼﻞ -١٢ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﻟﮕﻦ ﻓﺼﻞ -١٣ﺳﻴﺴﺘﻢ ﺍﺩﺭﺍﺭﻱ ﺗﻨﺎﺳﻠﻲ
)(Springer) (2003
Magnetic Resonance Angiography
, Guy Marchal, PhD, M.D.ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ﺍﺷﺘﺮﺕ ﮔﺎﺭﺩ ﺁﻟﻤﺎﻥ (Ingolf P. Arlart, Phd, M.D.
ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﮔﺮﺍﻳﺶ ﺭﻭﺯﺍﻓﺰﻭﻥ ﺑﻪ ﻏﻴﺮﺗﻬﺎﺟﻤﻲﺷﺪﻥ ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﭘﺰﺷﻜﻲ ﻧﻴﺎﺯ ﺑﻪ ﺩﺍﻧﺴﺘﻦ ﺗﻜﻨﻴﻚﻫﺎ ﻭ ﻫﻤﭽﻨﻴﻦ ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺑﺎ ﻛﻤﻚ ﺭﺯﻭﻧﺎﻧﺲ ﻣﻐﻨﺎﻃﻴﺴﻲ ) (MRAﺑﻴﺶ ﺍﺯ ﭘﻴﺶ ﺍﺣﺴﺎﺱ ﻣﻲﺷﻮﺩ ﻭ ﻫﺪﻑ ﺍﺻﻠﻲ ﺍﻳﻦ ﻛﺘـﺎﺏ ﻧﻴـﺰ ﺁﺷﻨﺎﻳﻲ ﺑﺎ ﺍﺻﻮﻝ ﻭ ﻣﻼﺣﻈﺎﺕ ﺗﻜﻨﻴﻜﻲ MRAﻭ ﻫﻤﭽﻨﻴﻦ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﺍﻳﻦ ﺭﻭﺵ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺗﺸﺨﻴﺼﻲ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻮﻝ ﻋﻤﺪﺓ ﺍﻳﻦ ﻛﺘﺎﺏ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
82 -١ﺳﻴﺴﺘﻢ ﻋﺮﻭﻗﻲ :ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱﻫﺎﻱ ﻋﺮﻭﻗﻲ ﻭ ﺍﺻﻮﻝ ﻫﻤﻮﺩﻳﻨﺎﻣﻴﻚ
-٩ﺗﻜﻨﻴﻚﻫﺎﻱ ﻧﻤﺎﻳﺶ ﺗﺼﻮﻳﺮ
-١٧ﻋﺮﻭﻕ ﺭﻳﻮﻱ
-٢ﺗﻌﺮﻳﻒ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺭﺯﻭﻧﺎﻧﺲ ﻣﻐﻨﺎﻃﻴﺴﻲ )(MRA
-١٠ﻛﻤﻴﺖ ﺟﺮﻳﺎﻥ ﺧﻮﻥ
-١٨ﺁﺋﻮﺭﺕ ﺷﻜﻤﻲ ﻭ ﺷﺎﺧﻪﻫﺎﻱ ﺁﻥ
-٣ﺍﺻﻮﻝ ﭘﺎﻳﻪ ﺭﺯﻭﻧﺎﻧﺲ ﻣﻐﻨﺎﻃﻴﺴﻲ ﻫﺴﺘﻪﺍﻱ ) (NMRﺟﻬﺖ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﭘﺰﺷﻜﻲ
-١١ﺗﺸﺮﻳﺢ ﻧﻤﺎﻳﺸﻲ ﺳﺨﺖﺍﻓﺰﺍﺭ
-١٩ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ
-٤ﻓﻀﺎﻱ Kﻭ Resolution
-١٢ﺁﺭﺗﻴﻔﻜﺖﻫﺎ ﻭ ﻣﺤﺪﻭﺩﻳﺖﻫﺎ
-٢٠ﻭﺭﻳﺪﻫﺎﻱ ﺑﺰﺭﮒ ﺑﺪﻥ ﻭ ﺍﻧﺪﺍﻡﻫﺎ
-٥ﺗﻜﻨﻴﻚﻫﺎﻱ Acquistionﻭﺍﺑﺴﺘﻪ ﺑﻪ ﺟﺮﻳﺎﻥ
-١٣ﻋﺮﻭﻕ ﺩﺍﺧﻞ ﺟﻤﺠﻤﻪ
-٢١ﺳﻴﺴﺘﻢ ﻭﺭﻳﺪﻱ ﺍﺳﭙﻠﻨﻮﭘﻮﺭﺗﺎﻝ
-٦ﺗﻜﻨﻴﻚﻫﺎﻱ Acquistionﻣﺴﺘﻘﻞ ﺍﺯ ﺟﺮﻳﺎﻥ
-١٤ﺷﺮﻳﺎﻥﻫﺎﻱ ﻛﺎﺭﻭﺗﻴﺪ ﻭ ﻭﺭﺗﺒﺮﺍﻝ
-٢٢ﺍﺭﺍﺋﺔ ﺭﺍﻫﻨﻤﺎ ) (Guideﺟﻬﺖ ﺭﻭﺵﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ
Resolution -٧ﻓﻀﺎﻳﻲ ﺩﺭ ﻣﻘﺎﺑﻞ Resolutionﺯﻣﺎﻧﻲ ﺩﺭ MRAﺑﺎ ﺗﺸﺪﻳﺪ ﻛﻨﺘﺮﺍﺳﺖ
-١٥ﺁﺋﻮﺭﺕ ﺷﻜﻤﻲ ﻭ ﺷﺎﺧﻪﻫﺎﻱ ﺁﻥ
Implant -٢٣ﻫﺎﻱ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ :ﺍﻳﻤﻨﻲ ﻭ ﺁﺭﺗﻴﻔﻜﺖﻫﺎ
-٨ﻣﺎﺩﻩ ﺣﺎﺟﺐ ﺩﺭ MRA
-١٦ﺷﺮﻳﺎﻥﻫﺎﻱ ﻛﻮﺭﻭﻧﺎﺭﻱ
)ﺗﻌﺪﺍﺩ ﺻﻔﺤﺎﺕ] 2272 :ﺩﻭﺟﻠﺪﻱ[ (
)CT and MR Imaging of the Whole Body (Mosby) (2003
ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺟﺮﺍﺣﻲ ﺍﻋﺼﺎﺏ ﺩﺍﻧﺸﮕﺎﻩ Clevelandﺍﻭﻫﺎﻳﻮ )(Charles F. Lanzieri, MD, FACR
ﺭﻳﺎﺳﺖ ﺩﭘﺎﺭﺗﻤﺎﻥ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ Clevelandﺍﻭﻫﺎﻳﻮ )(John R. Haaga, MD , FACR
ﺍﺳﺘﺎﺩ ﺑﺨﺶﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Thoracic , Headﺩﺍﻧﺸﮕﺎﻩ Case Western Reserveﺷﻬﺮ Clevelandﺍﻭﻫﺎﻳﻮ )(Robert C. Gilkeson, MD
ﻗﻴﻤﺖ 1000,000 :ﺭﻳﺎﻝ
ﺍﻳﻦ ﻛﺘﺎﺏ ﻳﻜﻲ ﺍﺯ ﻛﺎﻣﻠﺘﺮﻳﻦ ﻣﺮﺍﺟﻊ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ MRI ,CT Scanﺑﻮﺩﻩ ﻭ ﺩﺭ ﺁﻥ ﺿﻤﻦ ﺑﺤﺚ ﻛﺎﻣﻞ ﻭ ﺩﻗﻴﻖ ﺩﺭ ﻣﻮﺭﺩ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﻫﻤﭽﻨﻴﻦ ﻳﺎﻓﺘﻪﻫﺎﻱ Imagingﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺨﺘﻠﻒ ،ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﮔﻮﻳـﺎ ﻭ ﺗﻴﭙﻴـﻚ ﻣﺘﻌـﺪﺩ ﻫﻤـﺮﺍﻩ ﺑـﺎ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﺑﺮﺍﻱ ﻓﻬﻢ ﻣﻄﺎﻟﺐ ﺍﺳﺘﻔﺎﺩﻩ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﻭ ﺍﺯ ﺗﻜﻨﻴﻜﻬﺎ ﻭ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺭﻭﺷﻬﺎﻱ MRI, CT Scanﺑﻘﺪﺭ ﻛﻔﺎﻳﺖ ﺻﺤﺒﺖ ﺻﺤﺒﺖ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ ﺩﻭ ﺟﻠﺪ ﺗﺪﻭﻳﻦ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺟﻠﺪ ﺍﻭﻝ ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﭘﻨﺞ ﺑﺨـﺶ ﻋﻤـﺪﻩ ﻣﻲﺑﺎﺷﺪ ﻭ ﻓﻬﺮﺳﺖ ﻓﺼﻮﻝ ﺁﻥ ﺩﺭ ﺫﻳﻞ ﺁﻭﺭﺩﻩ ﺷﺪﻩﺍﻧﺪ: ﺑﺨﺶ ﺍﻭﻝ -ﺍﺻﻮﻝ MRI, CT Scan
ﺑﺨﺶ ﺩﻭﻡ -ﻣﻐﺰ ﻭ ﻣﻨﻨﮋﻫﺎ
ﺑﺨﺶ ﺳﻮﻡ -ﺗﺼﻮﻳﺮ ﺑﺮﺩﺍﺭﻱ ﺳﺮ ﻭ ﮔﺮﺩﻥ
ﺍﺻﻮﻝ ﺗﺼﻮﻳﺮ ﺑﺮﺩﺍﺭﻱ ﺩﺭ CT Scan
ﻓﺼﻞ -٤ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ MRI, CT Scanﻣﻐﺰ ﻭ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻓﺼﻞ -٥ﻧﺌﻮﭘﻼﺳﻢﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻓﺼﻞ -٦ﻋﻔﻮﻧﺘﻬﺎ ﻭ ﺍﻟﺘﻬﺎﺑﺎﺕ ﻣﻐﺰ ﻓﺼﻞ -٧ﺳﻜﺘﻪ ﻣﻐﺰﻱ ﻓﺼﻞ -٨ﻣﺎﻟﻔﻮﺭﻣﺎﺳﻴﻮﻧﻬﺎﻱ ﻋﺮﻭﻗﻲ ﻭ ﺁﻧﻮﺭﻳﺴﻤﻬﺎﻱ ﻣﻐﺰﻱ ﻓﺼﻞ -٩ﺗﺮﻭﻣﺎﻱ ﺳﻴﺴﺘﻢ ﺍﻋﺼﺎﺏ ﻣﺮﻛﺰﻱ ﻓﺼﻞ -١٠ﺍﺧﺘﻼﻻﺕ ﻧﻮﺭﻭﺩﮊﻧﺮﺍﺗﻴﻮ ﻓﺼﻞ Magnetic Resonance Spectroscopy -١١ﻣﻐﺰ ﻓﺼﻞ -١٢ﻓﺮﺁﻳﻨﺪﻫﺎﻱ ﻣﻨﻨﮋﻳﺎﻝ ﻓﺼﻞ -١٣ﻟﻮﻛﻮﺍﻧﺴﻔﺎﻟﻮﭘﺎﺗﻲﻫﺎ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺩﻣﻴﻠﻴﻨﻴﺰﺍﻥ
ﻓﺼﻞ -١٤ﺍﻭﺭﺑﻴﺖ ﻓﺼﻞ -١٥ﺍﺳﺘﺨﻮﺍﻥ ﺗﻤﭙﻮﺭﺍﻝ ﻓﺼﻞ -١٦ﻛﺎﻭﻳﺘﻲ ﺳﻴﻨﻮﻧﺎﺯﺍﻝ ﻓﺼﻞ -١٧ﺗﻮﺩﻩﻫﺎﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﮔﺮﺩﻥ ﻭ ﺁﺩﻧﻮﭘﺎﺗﻲ ﮔﺮﺩﻧﻲ ﻓﺼﻞ -١٨ﺣﻨﺠﺮﻩ ﻓﺼﻞ -١٩ﻧﺎﺯﻭﻓﺎﺭﻧﻜﺲ ﻭ ﺍﻭﺭﻓﺎﺭﻧﻜﺲ ﻓﺼﻞ -٢٠ﻏﺪﺩ ﺗﻴﺮﻭﺋﻴﺪ ﻭ ﭘﺎﺭﺍﺗﻴﺮﻭﺋﻴﺪ ﻓﺼﻞ -٢١ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺳﺮ ﻭ ﮔﺮﺩﻥ ﺍﻃﻔﺎﻝ
ﻓﺼﻞ -١ ﻓﺼﻞ -٢ ﻓﺼﻞ -٣ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺭﺯﻭﻧﺎﻧﺲ ﻣﻐﻨﺎﻃﻴﺲ ) :(MRIﺍﺻﻮﻝ ﻭ ﺗﻜﻨﻴﻜﻬﺎ ﻓﻴﺰﻳﻚ MRI
ﺑﺨﺶ ﭘﻨﺠﻢ -ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻗﻔﺴﺔ ﺳﻴﻨﻪ ﻓﺼﻞ -٢٧ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻏﻴﺮ ﻧﺌﻮﭘﻼﺳﺘﻴﻚ ﭘﺎﺭﺍﻧﺸﻴﻤﺎﻝ ﺭﻳﻪ ﻓﺼﻞ MRI, CT Scan -٣١ﺁﺋﻮﺭﺕ ﺗﻮﺭﺍﺳﻴﻚ
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻓﺼﻞ -٢٨ﻧﺌﻮﭘﻼﺳﻢﻫﺎﻱ ﺍﻭﻟﻴﺔ ﺭﻳﻮﻱ ﻓﺼﻞ CT Scan -٣٢ﻗﻠﺐ ﻭ ﭘﺮﻳﻜﺎﺭﺩ
ﻓﺼﻞ -٢٩ﻣﺪﻳﺎﺳﺘﻦ
ﻓﺼﻞ -٣٠ﺟﻨﺐ )ﭘﻠﻮﺭ( ﻭ ﺩﻳﻮﺍﺭﺓ ﻓﻘﺴﺔ ﺻﺪﺭﻱ ﻓﺼﻞ MRI -٣٣ﻗﻠﺐ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
83
: ﺑﺨﺶ ﻋﻤﺪﻩ ﺑﻮﺩﻩ ﻭ ﻓﻬﺮﺳﺖ ﻓﺼﻮﻝ ﺁﻥ ﺑﻪ ﺗﺮﺗﻴﺐ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ٤ ﺟﻠﺪ ﺩﻭﻡ ﻛﺘﺎﺏ ﻫﺎﮔﺎ ﺷﺎﻣﻞ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺍﻃﻔﺎﻝ-ﺑﺨﺶ ﻫﺸﺘﻢ ﻣﻼﺣﻈﺎﺕ ﻭﻳﮋﻩ: ﺩﺭ ﻛﻮﺩﻛﺎﻥMRI, CT Scan -٥١ ﻓﺼﻞ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﺑﺰﺭﮒ-٥٢ ﻓﺼﻞ ﻗﻔﺴﻪ ﺳﻴﻨﻪ-٥٣ ﻓﺼﻞ ﺳﻴﺴﺘﻢ ﻛﺒﺪﻱ ﺻﻔﺮﺍﻭﻱ-٥٤ ﻓﺼﻞ ﻃﺤﺎﻝ ﺍﻃﻔﺎﻝ-٥٥ ﻓﺼﻞ ﭘﺎﻧﻜﺮﺍﺱ-٥٦ ﻓﺼﻞ ﻛﻠﻴﻪﻫﺎ ﻭ ﻏﺪﺩ ﻓﻮﻕ ﻛﻠﻴﻮﻱ-٥٧ ﻓﺼﻞ ﺣﻔﺮﺓ ﭘﺮﻳﺘﻮﺋﻦ ﻭ ﻣﺰﺍﻧﺘﺮ، ﺩﺳﺘﮕﺎﻩ ﮔﻮﺍﺭﺵ-٥٨ ﻓﺼﻞ ﻟﮕﻦ ﻛﻮﺩﻛﺎﻥ ﻭ ﻧﻮﺟﻮﺍﻧﺎﻥ-٥٩ ﻓﺼﻞ ﺳﻴﺴﺘﻢ ﻋﻀﻼﻧﻲ ﻭ ﺍﺳﻜﻠﺘﻲ-٦٠ ﻓﺼﻞ
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺳﻴﺴﺘﻢ ﻋﻀﻼﻧﻲ ﻭ ﺍﺳﻜﻠﺘﻲ-ﺑﺨﺶ ﻫﻔﺘﻢ ﺗﻮﻣﻮﺭﻫﺎﻱ ﻣﻮﺳﻜﻮﻟﻮﺍﺳﻜﻠﺘﺎﻝ-٤٦ ﻓﺼﻞ ﭘﺎ ﻭ ﻣﭻ ﭘﺎMRI, CT Scan -٤٧ ﻓﺼﻞ ﺯﺍﻧﻮ-٤٨ ﻓﺼﻞ (Hip) ﻣﻔﺼﻞ ﺭﺍﻥ-٤٩ ﻓﺼﻞ ﺷﺎﻧﻪ-٥٠ ﻓﺼﻞ
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺷﻜﻢ ﻭ ﻟﮕﻦ-ﺑﺨﺶ ﺷﺸﻢ ﺩﺳﺘﮕﺎﻩ ﮔﻮﺍﺭﺵ-٣٤ ﻓﺼﻞ ﺿﺎﻳﻌﺎﺕ ﺗﻮﺩﻩﺍﻱ ﻛﺒﺪ-٣٥ ﻓﺼﻞ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﻨﺘﺸﺮ، ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ: ﻛﺒﺪ-٣٦ ﻓﺼﻞ ﻛﻴﺴﻪ ﺻﻔﺮﺍ ﻭ ﺳﻴﺴﺘﻢ ﺻﻔﺮﺍﻭﻱ-٣٧ ﻓﺼﻞ ﭘﺎﻧﻜﺮﺍﺱ-٣٨ ﻓﺼﻞ ﻃﺤﺎﻝ-٣٩ ﻓﺼﻞ ﻏﺪﺩ ﻓﻮﻕ ﻛﻠﻴﻮﻱ-٤٠ ﻓﺼﻞ ﻛﻠﻴﻪ-٤١ ﻓﺼﻞ ﭘﺮﻳﺘﻮﺋﻦ ﻭ ﻣﺰﺍﻧﺘﺮ-٤٢ ﻓﺼﻞ ( ﺭﺗﺮﻭﭘﺮﻳﺘﻮﺋﻦ )ﺧﻠﻒ ﺻﻔﺎﻕ-٤٣ ﻓﺼﻞ ﻟﮕﻦCT Scan -٤٤ ﻓﺼﻞ ﻟﮕﻦMRI -٤٥ ﻓﺼﻞ
Looking for the number key to the diagrams? Just fold out this page… A didactically brilliant and unprecedented approach to understanding CT imaging (Matthias Hofer, MD) Institute fo Diagnostic Radiology, MNR Clinic, Duesseldorf, Germany
Ideal for radiology residents, students and technicians, this concise manual is the perfect introduction to the practice and interpretation of computed tomography. Designed as a systematic learning tool, it introduces the use of CT scanners for all organs. Finally, self-assessment quizzes –including answers-ath the end of each chapter help the reader monitor progress and evaluate knowledge gained. Special Feature Includes detachable, pocket-sized cards containing checklists and tables of normal measurements –perfect for study or quick reference when on rounds. Contents: -Technical Aspects -Basic Rules of CT Reading -Preparing the patient -Administration of Contrast Media -Atlas of Normal and Common Pathological Findings in:the Cranium, Neck, Thorax, Abdomen, Retroperitoneum, Bones, and Lower Extremity -Interventional CT -CT-Angiography -Dose reduction -New protocols for 1-, 4-, and 16-row multislice scanners
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
84
MRI and CT Scan of Head and Spine
ﻗﻴﻤﺖ 500,000 :ﺭﻳﺎﻝ
)ﺗﻌﺪﺍﺩ ﺻﻔﺤﺎﺕ
( 810 :
)(Williams & Wilkins
)ﻓﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻳﺴﺖ ﻭ ﻣﺘﺪﻭﻟﻮﮊﻳﺴﺖ ﺩﺍﻧﺸﮕﺎﻩ (C. Barrie Grossman, M.D. Indiana
ﻛﺘﺎﺏ ﻓﻮﻕﺍﻟﺬﻛﺮ ﺩﺭ ﻣﻮﺭﺩ CT Scanﻭ MRIﺩﺭ ﺯﻣﻴﻨﺔ ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺑﻪ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻣﻲﭘﺮﺩﺍﺯﺩ ﻭ ﺷﺎﻣﻞ ٤ﺑﺨﺶ ﺍﺻﻠﻲ ﺍﺳﺖ: ﺑﺨﺶ ﺍﻭﻝ :ﻣﻼﺣﻈﺎﺕ ﺗﻜﻨﻴﻜﻲ ﭘﺎﻳﻪ ﻓﺼﻞ -١
ﺑﺨﺶ ﺩﻭﻡ :ﻣﻐﺰ
ﺍﺻﻮﻝ ﻓﻴﺰﻳﻜﻲ ﻣﺮﺑﻮﻁ ﺑﻪ CT Scanﻭ MRI
ﻓﺼﻞ -٢ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺑﺎﻟﻴﻨﻲ CT Scan ﻓﺼﻞ -٣ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺑﺎﻟﻴﻨﻲ MRI
ﺑﺨﺶ ﺳﻮﻡ :ﻛﻒ ﺟﻤﺠﻤﻪ ،ﺟﻤﺠﻤﻪ ﻭ ﺻﻮﺭﺕ ﻓﺼﻞ -١١ﻧﺎﺣﻴﺔ ﺯﻳﻦ )(Sella
ﻓﺼﻞ -٤ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ﻣﻐﺰ ﺩﺭ CT Scanﻭ MRI
ﻓﺼﻞ -٥ﻧﺌﻮﭘﻼﺳﻢﻫﺎ ﻭ ﻛﻴﺴﺖﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻓﺼﻞ -٦ﺍﺧﺘﻼﻻﺕ ﻋﺮﻭﻗﻲ ﻣﻐﺰ ﻓﺼﻞ -٧ﺁﺳﻴﺐﻫﺎ ﻛﺮﺍﻧﻴﺎﻝ ﻭ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ
ﻓﺼﻞ -٨ﻋﻔﻮﻧﺖﻫﺎ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻟﺘﻬﺎﺑﻲ ﻓﺼﻞ -٩ﻣﺎﻟﻔﻮﺭﻣﺎﺳﻴﻮﻥﻫﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ﻣﻐﺰ ﻭ ﺍﺧﺘﻼﻻﺕ ﻧﻮﺯﺍﺩﻱ ﻓﺼﻞ -١٠ﻫﻴﺪﺭﻭﺳﻔﺎﻟﻲ ﻭ ﺍﺧﺘﻼﻻﺕ ﺩﮊﻧﺮﺍﺗﻴﻮ ﻭ ﺁﺗﺮﻭﻓﻴﻚ ﻣﻐﺰ
ﺑﺨﺶ ﭼﻬﺎﺭﻡ :ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
ﻓﺼﻞ -١٢ﻧﺎﺣﻴﻪ ﺗﻤﭙﻮﺭﺍﻝ ﻓﺼﻞ -١٣ﺟﻤﺠﻤﻪ ،ﺻﻮﺭﺕ ،ﺳﻴﻨﻮﺱﻫﺎﻱ ﭘﺎﺭﺍﻧﺎﺯﺍﻝ ﻭ ﻧﺎﺯﻭﻓﺎﺭﻧﻜﺲ ﻓﺼﻞ -١٤ﺍﻭﺭﺑﻴﺖ
ﻓﺼﻞ -١٥ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻧﺮﻣﺎﻝ ،ﺗﻜﻨﻴﮓﻫﺎﻱ ﺗﺼﻮﻳﺮ ﻓﺼﻞ -١٦ﻭﺿﻌﻴﺖﻫﺎﻱ ﺩﮊﻧﺮﺍﺗﻴﻮ ﻭ ﺗﺮﻭﻣﺎﺗﻴﻚ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻓﺼﻞ -١٧ﺳﺎﻳﺮ ﭘﺎﺗﻮﻟﻮﮊﻱﻫﺎﻱ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
ﻻﺯﻡ ﺑﻪ ﺫﻛﺮ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻛﺘﺎﺏ ﻓﻮﻕ ،ﺑﺮﺍﻱ ﻓﻬﻢ ﺑﻬﺘﺮ ﻣﻄﺎﻟﺐ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﮔﻮﻳﺎ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﺍﺳﺘﻔﺎﺩﻩ ﮔﺮﺩﻳﺪﻩ ﻭ ﺑﺮﺍﻱ ﻃﺒﻘﻪﺑﻨﺪﻱ ﻧﻜﺎﺕ ﺍﺳﺎﺳﻲ ﺍﺯ ﺟﺪﺍﻭﻝ ﻣﺘﻌﺪﺩ ﺑﻬﺮﻩﮔﻴﺮﻱ ﺷﺪﻩ ﺍﺳﺖ.
HIGHLIGHTS OF OPHTHALMOLOGY INTERNATIONAL
WAVEFRONT ANALYSIS, ABERROMETERS and CORNEAL TOPOGRAPHY 1100,000R
)(2003
A. AGARWAL
B. BYOD,
ﮔﺮﭼــﻪ ﻫﻨــﻮﺯ ﻫــﻢ ﺩﺭ ﺑﺴــﻴﺎﺭﻱ ﺍﺯ ﻧﻘــﺎﻁ ﻛﺸــﻮﺭﻣﺎﻥ ﺍﻣﻜــﺎﻥ ﻋﻤــﻞ ﺟﺮﺍﺣــﻲ ﻛﺎﺗﺎﺭﺍﻛــﺖ ﺣﺘــﻲ ﺑــﻪ ﺭﻭﺵﻫــﺎﻱ ﻧﺴــﺒﺘﹰﺎ ﻗــﺪﻳﻤﻲ ﻧﻴــﺰ ﻭﺟــﻮﺩ ﻧﺪﺍﺷــﺘﻪ ،ﻋﺪﺳــﻲﻫــﺎﻱ ﺯﻳــﺎﺩﻱ ﺑــﻪ ﭘــﺎﺱ ﺧــﺪﻣﺎﺕ ﺩﺍﻧﺸــﻤﻨﺪ ﺑــﺰﺭﮒ ،ﻣﻮﺭﮔــﺎﻧﻲ ﻧــﺎﻡ ﻣــﻲﮔﻴﺮﻧــﺪ ) (!!) (Morgagnian Cataractﻟﻴﻜﻦ ﭘﻴﺸﺮﻓﺖ ﻋﻠﻢ ﻭ ﻓﻨﺎﻭﺭﻱ ﺧﺼﻮﺻﹰﺎ ﺩﺭ ﺩﻭ ﺩﻫﻪ ﺍﺧﻴﺮ ﭼﻨﺎﻥ ﺑﻮﺩﻩ ﻛﻪ ﺩﻳﮕﺮ ﺣﺪﺕ ﺑﻴﻨﺎﻳﻲ ٢٠/٢٠ﻫﺪﻑ ﻧﻬﺎﻳﻲ ﭘﺰﺷﻚ ﻭ ﺑﻴﻤﺎﺭ ﻧﺒﻮﺩﻩ ،ﻛﻴﻔﻴﺖ ﺑﻴﻨﺎﻳﻲ ﺑﺎ ﻫﻤﻪ ﺍﺑﻌﺎﺩ ﮔﺴﺘﺮﺩﻩﺍﺵ ﻣﺪ ﻧﻈﺮ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. ﺩﺭ ﺳﺎﻝﻫﺎﻱ ﺍﺧﻴﺮ ﺑﺎ ﻭﺭﻭﺩ ﺗﻜﻨﻴﻚ Wavefront Analysisﺍﺯ ﻋﺮﺻﻪ ﻋﻠﻢ ﻧﺠﻮﻡ ﺑﻪ ﺣﻴﻄﻪ ﺟﺮﺍﺣﻲ ﻛﺮﺍﺗﻮﺭﻓﺮﺍﻛﺘﻴﻮ ﻭ ﻣﻄﺮﺡﺷﺪﻥ ، Customized LASIKﺍﻓﻖ ﺗﺎﺯﻩﺍﻱ ﺑﻪ ﻧﺎﻡ " "Super Visionﺩﺭ ﺑﺮﺍﺑﺮ ﺩﻳﺪﮔﺎﻥ ﺟﻬﺎﻧﻴﺎﻥ ﭘﺪﻳﺪﺍﺭ ﮔﺸـﺘﻪ ﺍﺳـﺖ .ﺳـﻴﺮ ﺑﺴـﻴﺎﺭ ﺳـﺮﻳﻊ ﺍﻳـﻦ ﭘﻴﺸﺮﻓﺖ ﺑﺎﻋﺚ ﺷﺪﻩ ﻛﻪ ﻛﺘﺐ Textﻣﻮﺟﻮﺩ ﻭ ﻗﺎﺑﻞ ﺩﺳﺘﺮﺳﻲ ﺩﺭ ﻛﺸﻮﺭ ﺍﺯ ﺁﻥ ﺟﺎ ﺑﻤﺎﻧﻨﺪ ﻭ ﻻﺟﺮﻡ ﺩﺍﻧﺴﺘﻪﻫﺎﻱ ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﭼﺸﻢﭘﺰﺷﻜﺎﻥ ﻋﺰﻳﺰ ﻫﻢ ﺑﻪ ﺭﻭﺯ ﻧﺒﻮﺩﻩ ،ﻭ ﻳﺎ ﻣﺤﺪﻭﺩ ﺑﻪ ﺍﻃﻼﻋﺎﺕ ﭘﺮﺍﻛﻨﺪﻩ ﺑﻪ ﺩﺳﺖ ﺁﻣﺪﻩ ﺍﺯ ﻣﻘﺎﻻﺕ ﺑﺎﺷﺪ. ﻛﺘﺎﺏ ﺣﺎﺿﺮ ﻛﻪ ﺑﻪ ﻫﻤﺖ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺩﺭ ﻛﻮﺗﺎﻫﺘﺮﻳﻦ ﺯﻣﺎﻥ ﻣﻤﻜﻦ ﺍﺯ ﺍﻧﺘﺸﺎﺭ ﺁﻥ ﺩﺭ ﺧﺎﺭﺝ ﺍﺯ ﻛﺸﻮﺭ ﺗﻬﻴﻪ ﺑﻪ ﺻﻮﺭﺕ ﺗﻤﺎﻡ ﺭﻧﮕﻲ ﺑﺮ ﺭﻭﻱ ﻛﺎﻏﺬ ﮔﻼﺳﺔ ﻣﺎﺕ ﻭ ﺑﺎ ﻛﻴﻔﻴﺘﻲ ﻛﻢ ﻧﻈﻴﺮ ﺑﻪ ﺯﻳﻮﺭ ﭼـﺎﭖ ﺁﺭﺍﺳـﺘﻪ ﮔﺮﺩﻳـﺪﻩ ،ﭘﺎﺳـﺨﻲ ﺍﺳـﺖ ﺩﺭ ﺟﻬﺖ ﻓﺮﻭﻧﺸﺎﻧﺪﻥ ﻋﻄﺶ ﻋﻠﻤﻲ ﻣﻮﺟﻮﺩ ﺩﺭ ﺍﻳﻦ ﺯﻣﻴﻨﻪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺎ ﻋﻨﻮﺍﻥ WAVEFRONT ANALYSIS, ABERROMETERS and CORNEAL TOPOGRAPHYﺍﺯ ﺳﺮﻱ ﻛﺘﺎﺏﻫﺎﻱ ، Highlights Of Ophthalmologyﺍﺯ ﻣﻌﺪﻭﺩ ﻛﺘﺐ ﺗﻜﺴﺖ ﻣﻨﺘﺸـﺮ ﺷﺪﻩ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﻤﺎﻣﹰﺎ ﺑﻪ ﻣﻘﻮﻟﻪ Wavefront Analysis, Orbscan, Topographyﻭ ﺍﺯ ﻫﻤﻪ ﻣﻬﻤﺘﺮ ﻛﺎﺭﺑﺮﺩ ﺁﻧﻬﺎ ﺩﺭ Cataract Surgery, Customized LASIK, Standard LASIKﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ. ﻼ ﻣﻮﺟﺰ ﻭ ﻗﺎﺑﻞ ﺩﺭﻙ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﺑﻪ ﺟﺎﻣﻌﺔ ﺟﻬﺎﻧﻲ ﭼﺸﻢﭘﺰﺷﻜﺎﻥ ﺍﺭﺍﺋﻪ ﻛﺮﺩﻩﺍﻧﺪ ﻧﻮﻳﺴﻨﺪﮔﺎﻥ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺳﺘﺎﺩﺍﻥ ﺑﺮﺟﺴﺘﻪﺍﻱ ﺍﺯ ﻛﺸﻮﺭﻫﺎﻱ ﺁﻣﺮﻳﻜﺎ ،ﺍﺳﭙﺎﻧﻴﺎ ،ﮊﺍﭘﻦ ﻭ ﻫﻨﺪ ﻣﻲﺑﺎﺷﻨﺪ ﻛﻪ ﺑﻪ ﺳﺮﭘﺮﺳﺘﻲ Benjamin F. Boyd, M.D., FACSﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﺑﻪ ﺻﻮﺭﺗﻲ ﻛﺎﻣ ﹰ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
85
AMERICAN ACADEMY OF OPHTHALMOLOGY
1 2 3 4 5 6 7 8 9 10 11 12 13
BASIC AND CLINICAL SCIENCE COURSE
ﻋﻨﻮﺍﻥ ﻛﺘﺎﺏ Section 1: Section 2: Section 3: Section 4: Section 5: Section 6: Section 7: Section 8: Section 9: Section 10: Section 11: Section 12: Section 13:
Update on General Medicine Fundamentals and Principles of Ophthalmology Optics, Refraction, and Contact Lenses Ophthalmic Pathology and Intraocular Tumors Neuro-Ophthalmolog Pediatric Ophthalmology and Strabismus Orbit, Eyelids, and Lacrimal System External Disease and Cornea Intraocular Inflammation and Uveitis Glaucoma Lens and Cataract Retina and Vitreous International Ophthalmology
ﻋﻨﻮﺍﻥ ﻛﺘﺎﺏ 14 15 16 17 18 19 20 21 22
WAVEFRONT ANALYSIS, ABERROMETERS and CORNEAL TOPOGRAPHY OPHTHALMOLOGY MONOGRAPHS Cataract Surgery and Intraocular Lenses COSMETIC OCULOPLASTIC SURGERY Eyelid, Forehead, and Facial Techniques Glaucoma THE REQUISITES IN OPHTHALMOLOGY LASIK Principles and Techniques THE GLAUCOMAS THE WILLS EYE MANUAL Office and emergency Room Deagnosis and Treatment of Eye Disease Complications in Phacoemulsification (Avoidance, Recognition, and Management) Retina and Optic Nerve Imaging (Thomas A. Ciulla, Carl D. Regillo, Alon Harris)
ﺳﺎﻝ ﻧﺸﺮ
(ﻗﻴﻤﺖ )ﺭﻳﺎﻝ
2002-2003
2002-2003
215,000 270,000 215,000 210,000 230,000 250,000 190,000 280,000 185,000 160,000 180,000 230,000 235,000
ﺳﺎﻝ ﻧﺸﺮ
(ﻗﻴﻤﺖ )ﺭﻳﺎﻝ
2003
1100,000
2001
200,000
1999
300,000
2000
200,000
1998
250,000
2000
180,000
1999
220,000
2002
400,000
2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003
.
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
Christopher M. Norris, MSc, MCSP Director, Norris Associates, Manchester, UK
Human Kinetics
Norris, Christopher M. Back stability I Christopher M. Norris. p.cm. Includes bibliographical references and index. ISBN 0-7360-008 I-X I. Backache--Treatment. 2. Backache--Prevention. 3. Backache--Exercise therapy. I. Title. RD771.158 N67 2000 617.5'64--dc21
99-089545
ISBN 0-7360-008 I-X
,
Copyright @ 2000 by Christopher M. Norris All rights reserved. Except for use in a review, the reproduction or utilization of this work in any form or by any electronic, mechanical, or other means, now known or hereafter invented, including xerography, photocopying, and recording, and in any information storage and retrieval system, is forbidden without the written permission of the publisher. Permission notices for material reprinted in this book from other sources can be found on page 263. Acquisitions Editor: Loam D. Robertson, PhD; Developmental Editor: Elaine Mustain; Writer: Brian Mustain; Assistant Editors: Derek Campbell, Melissa Feld, Maggie Schwarzentraub; Copyeditor: Lisa Morgan; Proofreader: Myla Smith; Indexer: Craig Brown; Permission Manager: Heather Munson; Graphic Designer: Fred Starbird; Graphic Artist: Yvonne Griffith; Cover Designer: Keith Blomberg; Photographer (cover): Tom Roberts; Art Manager: Craig Newsom; Illustrator: Kristin Mount; Printer: Edwards Brothers Printed in the United States of America
10 9
8 7
6
5 4
3
2
Human Kinetics Web site: www.humankinetics.com United States: Human Kinetics P.O. Box 5076 Champaign, IL 61825-5076 800-747-4457 e-mail: [email protected]
Australia: Human Kinetics 57A Price Avenue Lower Mitcham, South Australia 5062 08 8277 1555 e-mail: [email protected]
Canada: Human Kinetics 475 Devonshire Road, Unit 100 Windsor, ON N8Y 2L5 800-465-7301 (in Canada only) e-mail: [email protected]
New Zealand: Human Kinetics P.O. Box 105-231, Auckland Central 09-523-3462 e-mail: [email protected]
Europe: Human Kinetics Units C2IC3 Wira Business Park West Park Ring Road Leeds LSl6 6EB, United Kingdom +44 (0)113 2781708
e-mail: [email protected]
Contents Preface vi Acknowledgments
viii
·
Part I The Conce~tua1 Foundation
1
Chapter 1 What Is Back Stability? The Scope of the Problem A New Look at the Etiology and Treatment of Back Pain The Model Used in This Book: Lumbar Stabilization Summary
3 3 4 7 13
Chapter 2 Biomechanics of the Lumbar Spine Anatomy of the Vertebral Column Axial Compression Movements of the Lumbar Spine and Pelvis The Mechanics of Lifting Lifting Methods Summary
14 14 25 30 35 40 42
Chapter 3 Stabilization Mechanisms
43
in the Lumbar Spine
The Posterior Ligamentous System The Thoracolumbar Fascia Trunk Muscle Action Intra-Abdominal Pressure Mechanism Summary
·
Part II Exercises for Establishing Stabilitt Chapter 4 Teaching Your Clients the Basic Skills Teaching Your Clients to Control Pelvic Tilt Teaching Your Clients to Identify and Assume the Neutral Position
43 44 49 62 65
67 69 70 78
iii
iv
. Contents Teaching Your Clients to Use Abdominal Hollowing Teaching Your Clients to Contract the Multifidus Muscles at Will Summary
81 89 91
Chapter 5 Muscle Imbalance Basic Concepts Muscle Adaptation to Injury, Immobilization, and Training Training Specificity Changes in Muscle Length Principles of Muscle Stretching Stretching Target Muscles Summary
99 100 111 113 118
Chapter 6 Basic Abdominal Muscle Training Current Practice in Abdominal Training Modifications of Traditional Abdominal Exercises Ab Roller Exercises Summary
120 120 124 130 133
Chapter 7 Posture Optimal Postural Alignment Postural Stability and Body Sway Basic Postural Assessment Principles of Postural Correction Posture Types and How to Correct Them Summary
134 134 135 136 143 145 163
Part III. Building Back Fitness Chapter8 AdvancedStabilityTraining Superimposed Limb Movements and Balance Boards Stability Ball Exercises Proprioceptive Training Summary
92 92 96
165 167 168 186 197 201
Contents
Chapter 9 More Advanced Stability Training: Weight Training and Plyometrics Weight Training Using Plyometrics to Train for Power and Speed Summary
·
Part IV Putting It All Together
.
v
202 203 222 227
229
Chapter10 Buildinga BackStabilityProgram
231
for Your Client Preliminary Assessment of Your Client General Principles for Designing a Stability Program Parallel Tracks in Designing a Stability Program Designing an Advanced Stability Program Summary
231 234 235 237 246
Chapter 11 Preventing Back Injuries and Reinjuries Keep the Spine Vertical Principles of Lifting in the Home and on the Job Summary
247 247 248 254
Bibliography 255 Credits 263 Index 264 About the Author 272
Preface This book presents an approach to treating low back pain that is different from what you've seen before. I'd like to present a brief story to illustrate my point. One of the editorial staff who worked on this book had experienced severe back problems for over a quarter century. Only a few months before he saw this manuscript, he had completed a 12-week intensive weight-training program that he had hoped would help his back. It provided some relief, but not a great deal. After he had read the manuscript, this person began employing just a couple of the very elementary principles described in chapter 4 (specifically, hollowing his abdomen and intentionally tightening his multifidus muscles). He did not even do any of the exercises-he just practiced abdominal hollowing and multifidus tightening as he sat at his desk, or in his car, or as he walked through the supermarket. A month after he began this very minimal effort, he reported to me that his sharp sciatica pain had declined about 80% and that his periodic minor (but quite distressing) bowel incontinence, caused by impingement of vertebrae on a nerve, had declined from about a dozen episodes per week to about one every two weeks. While I certainly do not endorse this person's decision to do only the bare minimum in trying to alleviate his back problems, I note the story here to illustrate a single point: This approachworks! It works because it is based on sound anatomical, physiological, and neurological principles. While health professionals have long known that a large number of back problems arise because of muscle weakness, solving the problems simply by "doing strengthening exercises" is like telling a person with an infection to "take a lot of antibiotics" without targeting the medicine to the microbe. I have treated scores of "hunks" who had terrible problems with lower back pain. An individual can have unusually strong abdominal and back muscles while those unsung, unpublicized, invisible muscles that run alongside the spine-and that actually keep it stable-are. weak and stretched. This book shows you how to help your clients solve lower back problems by attending to the actual anatomical structures that control the problem-and these are not merely the gross, obvious muscles that make one look good at the beach. They are nearly invisible muscles such as the transversus abdominis and the multifidus; invisible tendons that have become inelastic; and hidden nerves carrying invisible impulses, all of
vi
Preface
.
vii
which can be trained surprisingly well (I'll teach you how) to stabilize the back even when your client isn't thinking about it. I have honed the techniques described in this book over many years, during which I have helped thousands of clients who for the most part had not been significantly helped with traditional approaches. If you ever treat, advise, coach, train, massage, or in any other way deal with people who have lower back pain, this book is for you. If you're a physical therapist, a massage therapist, a chiropractor, an athletic trainer, or a sports physician, this book may well prove vital to your professional practice. Even if you are a casual reader and are not able to understand the more technical aspects, you at least can benefit from learning the basic moves that stabilize the back, as in chapter 4. Because the body is a complex unit of closely interconnecting systems, any treatment must address the whole, even though it targets a single system. Thus, back stability is part of a holistic approach centering on muscle balance. Muscles affect the support of the spine, posture, and both our ability to move and the way that we move. If we examine the biomechanical factors at work in the back, we can see that there are three elements that combine to restore the muscle balance that is vital to back stability: correction of segmental control, shortening and strengthening lax muscles, and lengthening tight muscles. In Back Stability, I will explain these three elements to you, and I'll show you how to order them according to each client's symptoms, using them to construct a program uniquely tailored for that client. In part I ("The Conceptual Foundation"), I lead you through the anatomical, physiological, and neurological underpinnings of back pain, and of both traditional and newer approaches to treating it. I help you understand why traditional approaches so often don't work, and why the back stabilization method is so successful. Then, in part II ("Exercises for Establishing Stability"), I show you how to teach your clients the basic skills for back stabilization. In part III ("Building Back Fitness"), I teach you a wide range of exercises that will help your clients prevent recurrence of back pain and rehabilitate their backs (when appropriate) for strenuous on-the-job lifting or for challenging sports activities. Finally, in part IV ("Putting It All Together"), I discuss how you decide which assessments, exercises, etc., to prescribe for which clients. Be sure you don't begin applying the material herein to your clients till after you've studied chapter 10 since that's the roadmap that helps you navigate the exercises with a particular client in mind. Chapter 11,while short, is vital, as it briefly points out how you should coach your clients to avoid reinjuring their backs. Simple stick figures rather than lifelike line drawings have been used to represent human beings in the illustrations of those exercises in which the
viii
. Preface
position of the pelvic girdle might otherwise be difficult for a layperson to understand. This device makes it easier for your clients to see the required position of the pelvic girdle in those particular exercises. When more lifelike drawings were deemed clearer, we have used them. Therefore you, the practitioner, can use the book as a teaching tool, showing your clients the drawings as you explain the exercises to them, and they will be able to see clearly what the desired positions are. Christopher
M. Norris
Acknowledgments I
would like to thank Brian Mustain for translating British English into American English and for unraveling the "knotted ball of wool" that formed my thoughts, and Elaine Mustain for maintaining the book's momentum when all seemed lost. In addition to the references quoted in this book, I acknowledge the work of several individuals in the field of back stability-including Carolyn Richardson, Gwendolen Jull, Paul Hodges, and Julie Hides from the University of Queensland, Australia; Vladamir Janda and Karl Lewit from the University of Prague, Czech Republic; Shirley Sahrmann from the University of Washington, U.S.A.; and Mark Comerford from Kinetic Control, England. I would also like to thank the staff at Norris Associates, Manchester, England, for sharing their clinical experience in the field of back stability.
PART
II
The Concet!fttal Foundation Because the approach used in this book differs somewhat from what you have seen in the past, it is important that you understand the theoretical basis for what you read. I begin in chapter 1 ("What Is Back Stability?") with a general introduction to the problems of back pain and back instability. In one sense, the true "problem" is that some health professionals fail to understand that instability IS the problem for many instances of low back pain! People who suffer from back pain may be subjected to manipulation, instructed to perform exercises, told to "work out"; they may be given chemicals to relax their muscles and poked with electric needles-all intended to alleviate their pain. But surprisingly few professionals understand that a great deal of low back pain occurs for one simple reason: the spine is not supported by the tissues surrounding it and therefore "wobbles" in ways that impinge on nerves and in general do bad things to a person's quality of life. Traditional approaches are often quite helpful-but there are some clients for whom they simply do not address the root problem of back pain completely. The purpose of this book is to teach you how to deal with back pain by helping your clients stabilize their spines. From discussion of the basic etiology of pain in chapter 1, I proceed in chapter 2 ("Biomechanics of the Lumbar Spine") to an explanation of how the spine works: its anatomy, its movements, even the physics of lifting. Then, in chapter 3 ("Stabilization Mechanisms in the Lumbar Spine"), I show you how the anatomical lessons of the first two chapters lead logically to certain specific, but frequently ignored, treatments. I hope you will digest these three chapters thoroughly-without their conceptual foundation, the rest of the book will appear to be little more than one more listing of exercises. If you appreciate the anatomical and physiological underpinnings of the following chapters, however, you will see that the "how to" chapters will open for your clients a world of new possibilities that traditional programs cannot provide.
11
What Is Back Stabili!Yl Back pain is a universal problem, particularly important in the largely sedentary Western world. New information about this condition is stimulating new ways to manage it, focusing particularly on new approaches to exercise.
THE SCOPE OF THE PROBLEM As many as 80% of individuals in the Western world will suffer at least one disabling episode of low back pain during their lives; at any time, as many as 35% of the population suffers from some kind of back pain (Frymoyer and Cats-Baril 1991). The cost is tremendous, both financially and in terms of personal suffering. Most individuals with low back pain recover within six weeks, but 5-15% of subjects progress to permanent disability, accounting for up to 90% of total expenditures for this condition (Liebenson 1996). Unfortunately, recurrence of back pain after an acute episode is common. Over 60% of individuals suffering an acute episode of low back pain will experience another bout within a year, and 45% of these will have a second recurrence within the following four years (Liebenson 1996). As many as 15% of individuals with low back pain progress to permanent disability, and 60% suffer from a recurrence of pain within one year.
KEY POINT:
Back pain is universal. Sufferers in the United States spend $60 billion per year treating it (Frymoyer and Gordon 1989) and receive $27 billion for permanent disability. The rate of increase in back pain is 14 times greater than the population growth, and during a period when disability awards for all conditions rose by 347%, awards for back pain increased by 2,680% (Frymoyer and Cats-Baril 1991). 3
4
.
Back Stability
In the United Kingdom, 46.5 million working days were lost through back pain in 1989-representing a cost to the National Health Service of £0.5 billion ($840 million) per year and an even larger cost to industry of £5.1 billion ($8.59 billion) in lost production (CSP 1998; Tye and Brown 1990). In 1994-1995, 14 million people in the UK visited their doctors for back pain and lost 116 million working days.
A NEW LOOK AT THE ETIOLOGY AND TREATMENT
OF BACK PAIN
In spite of the tremendous increase in the number of back pain sufferers in the past two decades, popular understanding about the nature of back pain has remained somewhat static. It is commonly believed that back pain results from a structural injury or fault that must be corrected in order to reduce pain and restore full function. According to this viewpoint, normal function is impossible-or even dangerous-until the defective structure has changed (Zusman 1998). While it is true that many individuals with low back pain exhibit structural changes, CT (computerized tomography) scans reveal similar "positive findings" in up to 50% of normal, asymptomatic subjects (Boden et al. 1990; Jensel et al. 1994)! It is the same with radiographic changes in the lumbar spine: as many individuals without pain show evidence of disc degeneration as do those with pain (Nachemson 1992). Moreover, studies with cadavers have shown no correlation between structural changes in the lumbar spine and a history of low back pain (Videman et al. 1990), and large disc lesions with nerve compression may be totally asymptomatic (SaaI1995). .:f:a":.l'JI.'.~ Structural changes in the spine are as likely in asymptomatic individuals as in those with low back pain and loss of function.
Nonorganic Causes of Back Pain At least three sources of back pain do not originate in the sufferer's body: iatrogenic, forensic, and behavioral (compare Zusman 1998).
.
Iatrogenic factors (brought on by the practitioner) include labels of disability and the consequences of deconditioning through prolonged (bed) rest. For example, a label such as "prolapsed disc" is far more threatening to a patient than "simple back pain," even though the total amount of pain experienced by the patient may be the same in both cases. Labels that imply disease or disability such as "arthritis" also suggest
What Is Back Stability?
.
5
severe conditions even though a mild form of the pathology may be present. Alternatives such as "slight roughening" or "normal wear and tear" are less threatening. Although avoiding stressful activities on the back is important, and limited rest has its place, prolonged bed rest has been shown to be counterproductive. Deyo et a1. (1986) compared two days of bed rest with two weeks of bed rest. They found both periods to be equally effective in terms of pain reduction, but the two-week period led to significant "negative effects due to immobilization" (such as weakening and stiffness around the spine) that were not present in the two-day period. Forensic factors (associated with legal proceedings) contribute significantly to chronic back pain. In a study of 2,000 back pain patients (Long 1995), involvement in litigation was the only factor that accurately predicted that a person would not rapidly return to work. Two important behavioral factors are perceived disability and anticipation of pain. 1. Perceived disability. Patients often fail to take part in daily activities because they believethey are physically incapable of doing the taskalthough structural changes in their spines do not bear out this belief (Zusman 1998). Perceived disability is often associated with a mistaken fear of reinjury (Vlaeyen et a1. 1995). 2. Anticipation of pain. Often the anticipation of pain rather than pain itself is enough to limit activity and create protective behaviors (Zusman 1998). The physical changes brought about by the fear of pain can be measured on surface EMG (sEMG). Main and Watson (1996) applied experimental noxious stimuli to the upper trapezius on normal subjects and on those with back pain. Normal subjects showed the expected reflex increase in sEMG activity in the trapezius muscles. Those with back pain, however, showed the reaction not in the upper trapezius, but in the lumbar regionsuggesting that the subjects viewed any pain as an inherent part of their back condition even when the pain was in fact occurring in another part of their bodies.
.
.
Perceived disability and the anticipation of pain contribute significantly to loss of function.
KEY POINT:
A New Model for Low Back Pain Management Most people traditionally have perceived back pain as a structural condition that requires rest to recover. New information is challenging this approach, however, viewing back pain at least in part as a functional change .
6
.
BackStability
that requires functional management. Exercise is at the forefront of this new approach. The Traditional Model Rest is still the most common treatment for back pain, despite the fact that prolonged bed rest has been shown to be harmful. Controlled exercises restore function, reduce both distress and perceived disability, diminish pain, and promote a return to work (Waddell 1987). Rest has little effect on the natural history of back pain and may actually increase its severity (Twomey and Taylor 1994). For back pain without significant radiation, bed rest probably should be limited to a maximum of two days. Longer periods are almost certainly counterproductive due to the negative effects of whole-body immobilization (Spitzer et al. 1987). Surgery is effective in only a small group of low back pain patients. Waddell (1987) argued that surgical intervention can help only 1% of patients. Comparing surgically and conservatively treated patients suffering from disc prolapse, Weber (1983) found no difference in outcome after two years. Aggressive conservative management can successfully treat over 80% of patients with clinically diagnosed sciatica and radiological evidence of nerve root entrapment (Bush et al. 1992). According to Allan and Waddell (1989), "disc surgery. . . [has left] more tragic human wreckage in its wake than any other operation in history." The New Model In proposing a new model for the treatment of low back pain, Waddell (1987) recommended that the patient's role should change from one of resting and being a passive recipient of treatment to an active role of sharing responsibility for restoration of function. Rehabilitation professionals increasingly are adopting this philosophy, using exercise programs to enhance lumbar stabilization Oull and Richardson 1994b; Norris 1995a; O'Sullivan et al. 1997). Here are some examples:
·
For a herniated lumbar disc. A rehabilitation program that emphasized skill-basedexercisetherapy for the spine effectively treated herniated lumbar discs (Saal and Saa11989) and rehabilitated football players with back injury (SaaI1988). The program aimed to restore automatic control of muscular stabilization of the trunk by teaching subjects to maintain a correct lumbar pelvic position (Le., "neutral position"-see following discussion) while performing progressively more complex tasks. In a study by Skall et al. (1994), intensive exercise when pain was not a limiting factor was more effective than mild mobilizing exercise five weeks following disc surgery. A one-year follow-up showed a trend favoring the intensive exercise group. Even when the diagnosis is uncertain, progressive exercis~onsisting of strengthening, proprioceptive training, and aerobic training-may restore
What Is Back Stability?
.
7
pain-free function (Deutsch 1996). Pain, physical dysfunction, and psychosocial dysfunction improved following a 1D-week exercise program for chronic low back pain patients studied by Risch et al. (1993), whereas all three factors worsened for those who remained inactive.
.
100 90 80 70 60 50 40 30 20 10
Control Exercise
.q
",,
&
,,
Pain intensity
group group
----
I
,, " boo-.......0
0
0
o 35
Pain description
30 25 20 15
.
~~ ,
10
---''II> '0..........- -0
0
0
5
o 50 45 40 35 30 25 20 15 10 5
o
Pre
Post
3 mo. Functional measure
,
.,,
.
I
" '\:>-.-.-
0
0
For
spondylolysis
or
spondylolisthesis. A back stability program targeting the anterolateral abdomina Is and multifidus was more effective than conventional rehabilitation in patients with radiographic diagnosis of spondylolysis or spondylolisthesis (O'Sullivan et al. 1997). In this study, one group of patients underwent a 1D-week program of gym work (including trunk curl exercises), general exercises such as swimming, and pain-relieving modalities. A second group, which engaged only in back stability exercises, showed a statistically significant reduction in pain intensity, pain descriptor scale, and functional disability that was maintained at a 3D-month follow-up (figure 1.1). This trial provides the strongest evidence so far in the literature regarding the effectiveness of stabilization programs for the lumbar spine. I have expanded some of these techniques for use in this book.
0
THE MODEL 'I--r 6 mo. 30 mo.
Figure 1.1 A comparison of conventional exercise and stability exercise effects on spondylolys isl s pondylol isthes is. Adapted from O'Sullivanet al. 1997.
USED IN THIS BOOK: LUMBAR STABILIZATION
This book presents a program of back treatment based on the
8
.
Back Stability
new model of active patient participation. The most important concept underlying the program is that of lumbar back stability versus lumbar back instability. Instability of the lumbar spine is not the same as hypermobility. In both conditions the range of motion is greater than norma!. However, instability is present when there is "an excessive range of abnormal movement for which there is no protective muscular contro!." There is no instability in hypermobility, however, since the "excessive range of movement. . . has complete muscular control" (Maitland 1986). The essential feature of stability
is therefore
the ability of the body to control the whole range of motion
of a joint, in this case the lumbar spine.
~.
Stability of ajoint implies the body's ability to control the entire range of motion around that joint.
An unstable lumbar spine cannot maintain correct vertebral alignment. Because the unstable segment is less stiff (less resistant to movement), movement within the spinal column increases even under minor loadsthereby altering both the quality and quantity of motion. Unstable lumbar spines often reveal no clinical damage to the spinal cord or nerve roots and no incapacitating deformity. If untreated, however, an unstable spine may irritate or damage neural tissue, leading to positive neurological signs on clinical examination. Positive neurological examination therefore does not preclude prescription of stabilization exercise since instability may indeed be the cause of the positive findings. The excessive movement in an unstable spine may either stretch or compress pain-sensitive structures, leading to inflammation (Kirkaldy-Willis 1990; Panjabi 1992). A number of physical signs can suggest instability in a clinical assessment, as outlined in "Physical Signs of Instability," below. See also "Preliminary Assessment of Your Client," page 231. Physical
.
Signs of Instability
Step deformity (spondylolisthesis) or rotation deformity (spondylolisis)
on standing,
which reduces on lying
. Transverse band of muscle spasm, which reduces on lying
. Localized muscle twitching while shifting weight from one leg to the other . . Alteration to passive intervertebral motion testing, suggesting excessive mobility in the sagittal plane Juddering
or shaking during forward bending
Source; Paris 1985; Maitland 1986
What Is Back Stability?
.
9
Stable Movement and Position of the Lumbar Spine Both the gross and fine positions of the lumbar spine are vital to back stability and may be described in terms of "neutral zone" and "neutral position." Control of these positions requires an interplay among several body systems and forms the basis of the back stability program.
Movement in the Neutral Zone Lumbar instability may be defined as an excessive range of motion without muscular control. Another way to visualize instability is as a loss of stiffness (Pope and Panjabi 1985)-not the negative condition we refer to when we speak of "a stiff back:' but rather a positive factor referring to the amount of resistance a structure (in this case, the spine) provides in order to move against a force. (Imagine a bodybuilder arm wrestling a weakling, and consider whose arm would be more stiff/stable.) Less stiffness leads to more movement from application of the same force. If a back is not stiff enough, it will buckle and move under very little force, resulting in compression or stretching of sensitive structures. Pain is the consequence. Panjabi et al. (1989)proposed the concept of the neutral zone-the zone in which movement occurs at the beginning of the range of motion before any effective resistance is offered from either the muscular system or the spinal column. The neutral zone represents the range of motion that lacks effective restraint, either active or passive. It is the vertebral displacement that occurs before resistance is offered. A grossly unstable spinal segment has quite a large neutral zone (figure 1.2). Physiotherapists use this concept when they Vertebra in neutral position ~.~ anterior cc ~~movement 15 .(i) cn~ 1:J c:
+
posterior movement ~\!!.
~
~*
Q)
:J
£
llJ cc
Neutral zone-. Figure 1.2 The neutral zone.
10
. Back Stability
assess lumbar joint movements by palpation-they note the onset either of motion resistance or of pain as they move the joint. In the case of the lumbar spine in the prone position, movement of this type is usually in a posteroantero (PA) direction. Note that the resistance felt by physiotherapists is mainly passive and does not necessarily represent significant resistance offered by muscle contraction. The passive stability system (ligaments and bone contour) reduces motion toward the end of the neutral zone. Our strategy, however, is to reduce the size of the neutral zone by increasing muscle stability. Exercise that increases muscle stability may reduce motion within the neutral zone before the passive elements even come into play. Note that neutral zone motion is different from the total range of motion-€ven though stabilizing exercise increases muscle "stiffness," it does not correspondingly reduce the total range of motion. Panjabi (1992) investigated the relationship between total range to neutral zone range by studying the effect of external fixation on the cervical spine in cadavers-and noted that neutral zone motion declined over 70% in association with a decrease of only 40% in total range of motion. In reducing the size of the neutral zone, the back stability program decreases the amount of motion that occurs when minimal forces are imposed on the spine (Le., those same forces that, when experienced hour after hour, can produce the compression/ stretching that lead to back pain). A stable back is not constantly buffeted by minor stresses related to mere sitting, standing, etc., such as those that occur in individuals with unstable spines. Instability alters both the quality and quantity of lumbar motion.
KEY POINT:
Neutral Position of the Lumbar Spine The neutral position of the lumbar spine is different from the neutral zone. Lumbar neutral position refers to an overall movement of the lumbar spine rather than to individual movements between vertebrae. Lumbar neutral position is midway between full flexion and full extension as brought about by posterior and anterior tilting of the pelvis. Teaching patients to identify and maintain the neutral position of their lumbar spines is a key component of each stage of the back stability program, since the neutral position places minimal stress on body tissues. Also, because postural alignment is optimal, the neutral position is generally the most effective position from which trunk muscles can work. The neutral position of the lumbar spine is important in all stages of the back stability program because it minimizes stress.
KEY POINT:
What Is Back Stability?
.
11
Achieving and Maintaining Spinal Stability Three interrelated systems maintain spinal stability (figure 1.3). Inert tissues (in particular, ligaments) provide passive support; contractile tissues give active support; and neural control centers coordinate sensory feedback from both systems (Panjabi 1992). Since one or two systems may compensate for reduced stability in another, the active system may sometimes increase its contribution to stability in order to minimize stress on the passive system (Tropp et a!. 1993). When the goal of rehabilitation is healing of the spine, appropriate exercise-by enabling the active system to take more of the total load placed on the back-can permit the passive system to repair itself. The net result is decreased pain and increased function. Conversely, continually loading the passive system without proper support from the active system can increase the time to recovery and lead to further tissue damage. Simply developing muscle strength, however, is insufficient. To provide maximum relief to the passive system, one must augment both of the other systems (i.e., the active and neural control systems). Yetmany popular strength exercises for the trunk actually increase mobility in this region to dangerously high levels (Norris 1993, 1994a). Rather than improving stability, exercises of this type may reduce it and therefore exacerbate symptoms-€specially those associated with inflammation. An example is the bilateral straight-leg-raise movement where both legs are lifted simultaneously from a supine lying position. Although individuals performing this exercise may indeed strengthen their abdominal muscles, they often fail to maintain pelvic alignment. Anterior tilting of the pelvis leads to lumbar facet compression and overstretches the anterior spinal
Figure 1.3 The spinal stabilizing system consists of three interrelating subsystems. Reprinted, by permission, from M.M.Panjabi, 1992, "The stabilisation of the spine. Part 1. Function, dysfunction, adaptation, and enhancement," Journal of Spinal Disorders 5(4): 383-389.
12
.
Back Stability
tissues. In this case, the anterior longitudinal ligament of the spine may be overstretched, reducing the effect of an important passive stabilizing structure. Passive Support Passive support of the lumbar region is provided by the stretching (especially of ligaments) and compression of soft tissues. A compressed ligament is more relaxed and offers less support. In full lumbar extension, for example, as may occur when standing with an anteriorly tilted pelvis, the lumbar facet joints are loaded and compressed. The anterior structures, including the anterior longitudinal ligament, are stretched: stability is provided (passively) through elastic recoil of this ligament and because facet joints of the spine are forcibly closed. Developing Active Lumbar Stability Poor postural control can leave the spine vulnerable to injury by placing excessive stress on the body tissues (Kendall et al. 1993). In the lumbar spine, the trunk muscles protect spinal tissues from excessive motion. To do this, however, the muscles surrounding the trunk must be able to cocontract isometrically when appropriate (Richardson et al. 1990). The synergistic interaction between various trunk muscles is complex: some muscles act as prime movers to create the gross movements of the trunk, while others function as stabilizers (fixators) and neutralizers to support the spinal structures and control unwanted movements. Rehabilitation through active lumbar stabilization not only deals with the torqueproducing capacity of muscles, as is true of many traditional programs, but also seeks to enable a subject to unconsciously and consistently coordinate an optimal pattern of muscle activity Oull and Richardson 1994a). Developing the Neural System The neural system links the passive and active systems. Upon detecting movement within the neutral zone, the neural system relays information to the active system (muscles) about the position and direction of movement. The muscles' ability to contract and maintain stability (i.e., to increase stiffness and reduce the size of the neutral zone) depends on the speed and accuracy with which the information is relayed. The vital aspects of neural system development are therefore accuracy of movement and speed of reaction. Thus the stability program emphasizes accuracy of movement early on; speed comes later.
What Is Back Stability? . 1 3
SUMMARY
· · · . ·
Low back pain is a massive challenge to health-care professionals and a major financial drain on Western economies. Low back pain produces alterations in behavior patterns that can exacerbate the condition. The traditional structural approach to treating back pain must be balanced with restoration of function. New approaches to treating back pain emphasize the use of exercise ra ther than rest.
Back stability consists of three interrelating control systems: active, passive, and neural. . Although traditional exercise systems that work the trunk may strengthen muscle, they also may reduce total back stability. · Enhancing the active and neural systems can partially compensate for decrements in the passive system.
·
Enhanced movement accuracy and muscle reaction speed are vital to full rehabilitation of the back.
2 Biomechanics of the Lumbar Spine In order to explain how the back is stabilized, I must briefly review some important aspects of spinal anatomy. Chapter 1 describes the passive stability system-the "brakes" provided by inert tissues that will stretch only a certain amount (both individually and as systems of tissues) before they restrict further movement. In this chapter, I describe this passive system for each of the major physiological movements of the lumbar spine and then use the example of lifting to illustrate the importance of stability.
ANATOMY
OF THE VERTEBRAL
COLUMN
The gross anatomy of the lumbar spine includes vertebral bones, joints, and discs, plus the sacroiliac joints. Although none of these structures moves in isolation, it should prove helpful if I describe them individually.
The Bones and Their Joints The adult human vertebral column comprises 33 vertebrae. Five vertebrae are fused to form the sacrum and four are fused to form the coccyx. The remaining 24 movable vertebrae are divided among the cervical (7), thoracic (12) and lumbar (5) regions (figure 2.1). Any two neighboring vertebrae make up a spinal segment (figure 2.2). To understand how the vertebrae fit together in the spine, one must know the parts of the typical vertebra. The two vertebrae within a spinal segment are attached (articulated) by both joints and ligaments. There are three joints-the articulating triadconsisting of the disc, which forms the joint between the bodies of adjacent vertebrae, and the two facet joints (also called zygapophyseal or apophyseal joints), where the inferior articular processes on either side of the upper vertebra come together with the superior articular processes on either side of the lower vertebra. 14
Biomechanics of the Lumbar Spine
2.1 The vertebral column. Reprinted from Watkins 1999. Figure
.
15
Figure 2.2 A typical spinal segment. Reprinted
from
Watkins
1999.
A spinal segment comprises two adjacent vertebrae, articulating with each other through the intervertebral disc and two facet joints. The articulations form a triad.
KEY POINT: I
The disk and its associated facet joints are intimately linked both structurally and functionally. Degeneration of the intervertebral disc as a result of injury can lead to degeneration of the neighboring facet joints (Vernon-Roberts 1992); and as we shall see later, the ligamentous support to both structures is continuous. We can compare the spinal segment to a simple leverage system (Kapandji 1974), with the facet joints forming a fulcrum. The posterior tissues (ligamentous and muscular) and the anteriorly placed disc resist both compressive and tensile forces. The ligaments themselves may be categorized into three interrelating functional groups as shown in table 2.1.
Ligaments The neural arch ligaments consist mainly of the ligamentum flavum and the interspinous ligament, with the supraspinous and inter transverse
16
. Back Stability
Table 2.1
Ligaments
of the Spinal Segment
Neural arch Ligamentum flavum Interspinous ligament Supraspinous ligament Intertransverse ligament
. .. .
Capsular
.
Ventral
Facet joint capsule
(reinforced by the ligamentum flavum)
. .
Anterior longitudinal ligament Posterior longitudinal ligament
Adapted, by permission, from EH. Willard, 1997, The muscular, ligamentous and neural structure of the low back and its relation to back pain. In Movement stability and low back pain, edited by A. Vleeming, V. Mooney, T. Dorman, C. Snijders, and R. Stoeckart (Edinburgh: Churchill Livingstone).
a
Anterior longitudinal ligament
b
Left intertransverse ligament
Left ligamentum flavum
Figure 2.3 Ligaments of the spinal segment (a) side view, (b) superior view.
ligaments providing additional support (figure 2.3 a and b). Although these four ligaments are traditionally described as separate structures, they are actually merged at their edges and act functionally as a single unit. This is an extremely important point, as it bears significantly on the question of how one stabilizes the back. On dissection, when the bony components of the neural arch are removed, the neural arch ligaments can be seen to maintain their continuity (Willard 1997). The lateral fibers of the ligamentum f1avum are continuous with the facet joint capsule (YongHing et al. 1976) and form the rear wall of the spinal canal. The anterior border of the interspinous ligament is a continuation of the ligamentum f1avum, while the posterior border of this ligament is thickened into the supraspinous ligament. The supraspinous ligament merges with the thoracolumbar fascia (TLF) (figure 2.4), which in turn connects
TeymsYou .ShPEti(l$.now ~ articulate to join or connect loosely to allow motion between the connection, such as a joint caudal any tail-like structure contralateral fibers fibers originating in or affecting the opposite side of the body distraction force a force that separates a joint surface without injury or dislocation extension a movement that straightens a limb to a parallel or nearparallel position fascia a sheet of fibrous tissue under the skin that encloses muscles as well as separates and supports them; connects the skin with the tissue beneath it flexion bending or being bent; opposite of extension innominate bone the hip bone composed of the ilium, ischium, and pubis; forms the pelvis investing fascia fascia that surrounds rather than connects or separates ischemic deficiency of blood to a body part due to an obstruction in or a narrowing of the blood vessels lamina of vertebral arch the posterior portion of the arch that provides a base for the spine lateral flexion bending or being bent to the side lordosis inward curvature of the cervical and lumbar spines occiput the back part of the head vertebral pedicle the bony process that extends posteriorly from the body of a vertebra; one of the paired parts of the vertebral arch that connect the lamina to the vertebral body pelvic inlet the upper opening of the pelvis pelvic outlet the lower opening of the pelvis periosteum a thick, fibrous membrane covering all the bones of the body except at the joints prolapse downward displacement sagittal rotation turning from the front to the back sagittal plane a vertical plane through the body that divides it into the left and right side Schmorls node an irregular or hemispherical bone defect in the body of a vertebra, which a spinal disk herniates into trabecula fibrous cord of connective tissue that extends into an organ's wall to serve as support ventral front side of the body
17
18
.
Back Stability
Ligamentum
flavum
Superior articular process
Figure 2.4 Interspinous-supraspinous-thoracolumbar (1ST)ligamentous complex. The 1STcomplex supports the lumbar spine by anchoring the thoracolumbar fascia and multifidus sheath to the facet joint capsules
with the deep abdominal muscles (see page 57). The force generated by the deep abdominal muscles therefore can be transmitted through the TLF, via the supraspinous ligament, directly into the ligamentum flavum-preventing this ligament from buckling towards the spinal cord. This is one way the deep abdominals assist in spinal stabilization. Note that it is not only abdominal muscles that affect the spine. The interspinous ligament merges with the supraspinous ligament and then into the TLF, forming the interspinous-supra spinous-thoracolumbar (1ST) ligamentous complex (Willard 1997). The 1STcomplex attaches the fascia of the back to the lumbar spine. The importance of this system is that tension developed in the extremities is transmitted to the vertebral column, making the seemingly distant limb musculature essential to the rehabilitation of spinal function. The intertransverse ligament, although small, becomes more important caudally as it expands into the iliolumbar ligament, the importance of which I will discuss later. Force from the extremity muscles is transmitted to the spine via ligaments and fasciae, which ultimately attach to the vertebrae themselves. The deep abdominal muscles have
KEY POINT:
lth:. g~eate~tcapacityto stabilizethe spine. _
_
__ _
j
The capsule of the facet joint is reinforced posteriorly by the multifidus muscle and anteriorly by the ligamentum flavum. It is surrounded by fascia which is itself continuous with that covering the ligamentum flavum and the investing fascia of the vertebral body. The facet joint capsule there-
Biomechanics of the Lumbar Spine
.
19
fore can be seen as a "bridge" of connective tissue between the ligaments of the neural arch and those of the vertebral body (Willard 1997) (figure 2.5). The anterior longitudinal ligament (ALL) and posterior longitudinal ligament (PLL) lie ventrally within the spinal segment. The ALL is the stronger of the two and extends from the occiput to the sacrum where it merges with the sacroiliac joint capsule. The ALL has two sets of fibers (Bogduk and Twomey 1991). The superficial fibers span several vertebral segments, while the deep fibers attach loosely to the annulus of the spinal disc (figure 2.6). The PLL exists in the cervical spine as the tectorial membrane and extends caudally to the periosteum of the sacrum. It expands as it passes the intervertebral discs and narrows around the vertebral body. Because it is considerably weaker than the ALL, the main ligamentous restriction to flexion is not from the PLL but from the ligamentum flavum and the facet joint capsule into which it merges. The ligamentum flavum and facet joint capsules combine to offer 52% of the resistance to flexion in the lumbar spine (Bogduk and Twomey 1991). The structural pairing of the PLL and the ligamentum flavum is functionally obvious as well. Load-deformation (stress-strain) curves plotted for the two ligaments are similar (Panjabi and White 1990), suggesting in this case that the two ligaments may have a similar purpose.
Ligamentum
flavum
Multifidus muscle
Figure 2.5 Facet joint capsule. Reprinted from Watkins 1999.
Figure 2.6 Vertical section through pedicles in lumbar region: posterior aspect of vertebral bodies showing attachment of posterior longitudinal ligament to spinal discs. Reprinted from Watkins 1999.
20
. Back Stability
The longitudinal ligaments are viscoelastic, meaning that they stiffen when loaded rapidly. They do not store all the energy used to stretch them because they lose some as heat, a feature known as hysteresis. When loaded repeatedly, these ligaments become even stiffer, and the hysteresis is less marked, making them more prone to fatigue failure (Hukins 1987). The supraspinous and interspinous ligaments are farther from the flexion axis and therefore need to stretch more than the posterior longitudinalligament when they resist flexion. With age, all ligaments gradually lose their ability to absorb energy (Tkaczuk 1968). The stiffest ligament in the spine is the posterior longitudinalligament; the most flexible is the supraspinous (Panjabi et al. 1987). The ligamentum flavum in the lumbar spine is "pretensioned" (possesses tension at rest) when the spine is in its neutral position, a situation that compresses the spinal disc. This ligament has the highest percentage of elastic fibers of any tissue in the body (Nachemson and Evans 1968) and contains nearly twice as much elastin as collagen. The anterior longitudinalligament and joint capsules are among the strongest ligamentous tissues in the body, while the interspinous and posterior longitudinalligaments are the weakest (Panjabi et al. 1987). The ligamentum f1avum is the most elastic ligament in the body and the main ligament limiting flexion. It forms the anterior portion of the facet joint capsule.
KEY POINT:
Spinal Discs There are 24 intervertebral discs lying between successive vertebrae, making the spine an alternatively rigid then elastic column. The amount of flexibility in a particular spinal segment is determined by the size and shape of the disc and by the resistance to motion of the soft tissue that supports the spinal joints. The discs increase in size as they descend the column, the lumbar discs having an average thickness of 10 mm, twice that of the cervical discs. The disc shapes are accommodated to the curvatures of the spine and to the shapes of the vertebrae. The greater anterior widths of the discs in the cervical and lumbar regions reflect the curvatures of these areas. Each disc comprises three closely related components-the annulus fibrosis, nucleus pulposus, and cartilage end plates (figure 2.7). The annulus comprises layers of fibrous tissue arranged in concentric bands-about 20-like those in an onion. The fibers within each band are parallel, with the various bands angled at 45° to each other. The bands are more closely packed anteriorly and posteriorly than they are laterally, and those innermost are the thinnest. Fiber orientation, although partially determined at birth, is influenced by torsional stresses in the adult (Palastanga
Biomechanics of the Lumbar Spine
.
21
Anterior Nucleus
pulposus
Annulus fibrosus
Posterior Figure through
2.7 (a) Concentric a disc.
bands
of annular
fibers.
(b) Horizontal
section
Reprinted, by permission, from j. Watkins, 1999, Structure and function of the musculoskeletal system (Champaign, IL: Human Kinetics), 142.
et al. 1994). The posterolateral regions have a more irregular makeuppossibly one reason why they become weaker with aging and more predisposed to injury. KEY POINT: I
The spinal discs have fewer concentric bands
posterolaterally than in other regions, and these are irregularmaking this region of the disc more susceptible to injury.
The annular fibers pass over the edge of the cartilage end plate of the disc and are anchored to the bony rim of the vertebra and to its periosteum and body. The attaching fibers are actually interwoven with the fibers of the bony trabeculae of the vertebral body. The outer layer of fibers blend with the posterior longitudinal ligament; some authors claim that the anterior longitudinal ligament has no such attachment (Vernon-Roberts 1987). Resting on the surface of the vertebra, the hyaline cartilage end plate is approximately 1 mm thick at its outer edge and becomes thinner toward its center. The central portion of the end plate acts as a semipermeable membrane to facilitate fluid exchange into and out of the disc; it also protects the vertebral body from excessive pressure. In early life, canals from the vertebral body penetrate the end plate, but these disappear after the age of 20 to 30. The end plate then starts to ossify and become more brittle, while the central portion thins and, in some cases, is completely destroyed. The nucleus pulposus is a soft hydrophilic (water-attracting) substance taking up about 25% of the total disc area. It is continuous with the annulus, but the nuclear fibers are far less dense than those of the annulus. Mucopolysaccharides called proteoglycans fill the spaces between the collagen fibers of the nucleus, giving the nucleus its water-retaining capacity
. BackStability
22
and making it mechanically plastic. Metabolically very active, the area between the nucleus and annulus is sensitive both to physical force and to chemical/hormonal influence (Palastanga et al. 1994). Although the collagen volume of the nucleus remains unchanged, the proteoglycan content decreases with age-leading to a net reduction in water content. In early life, the water content may be as high as 80-90%, but this decreases to about 70% by middle age. The lumbar discs are the largest avascular structures in the body. The nucleus obtains fluids by passive diffusion from the margins of the vertebral body and across the cartilage end plate-particularly across the center of the end plate, which is more permeable than the periphery. Intense anaerobic activity within the nucleus (Holm et al. 1981) can lead to lactate buildup and low oxygen concentration, placing the nuclear cells at risk. Inadequate ATP levels may lead to cell death. Some researchers hypothesize that regular exercise involving movement of the spine may improve the nutrition of the disc-and over the years might not only improve the general health of discs, but even slow the loss of height due to water loss from discs. KEY POINT: The lurTihar spinal discs are avascular and depend on fluid exchange by passive diffusion. Regular movement/ activity is vital to this process.
:
Facet Joints The facet joints are synovial joints (cushioned by synovia, a viscous fluid) between the inferior articular process of one vertebra and the superior articular process of its neighbor. As with other typical synovial joints, they have articular cartilage, a synovial membrane to contain the fluid, and a joint capsule; but they also have a number of unique features (Bogduk and Twomey 1991). The facet joint capsule holds about 2 ml of synovial fluid. Its anterior wall is formed by the ligamentum flavum; posteriorly, the capsule is reinforced by the deep fibers of the multifidus muscle. At its superior and inferior poles, the joint leaves a small gap, creating the subscapular pockets. These are filled with fat, contained within the synovial membrane. Within the subscapular pocket lies a small foramen for passage of the fat in and out of the joint as the spine moves. Within the capsule, there are three structures of interest. The first is the connective tissue rim, a thickened wedge-shaped area that makes up for the curved shape of the articular cartilage in much the same way as the menisci of the knee do. The second structure is an adipose tissue pad, a 2-mm fold of synovium filled with fat and blood vessels. The third structure is the fibroadipose meniscoid, a 5-mm leaf-like fold that projects from the inner sur-
Biomechanics of the Lumbar Spine.
23
faces of the superior and inferior capsules. The last two structures have a protective function. Flexion leaves some of the articular facets' cartilage exposed-both the adipose tissue pad and the fibro-adipose meniscus cover the exposed regions (Bogduk and Engel 1984). With aging, cartilage of the facet joint can split parallel to the joint surface, pulling a portion of joint capsule with it. The split cartilage, with its attached piece of capsule, forms a false intra-articular meniscoid (Taylor and Twomey 1986). Flexion normally draws the fibro-adipose meniscus out from the joint, and it moves back in with extension. If the meniscus fails to move back, it will buckle and remain under the capsule, causing pain (Bogduk and Jull 1985). A mobilization or manipulation that combines flexion and rotation may relieve pain by allowing the meniscoid to move back into its original position.
The Sacroiliac Joint As with the lumbar spine, the sacroiliac joint (SIJ)-the rather large surface where the sacrum (the five fused bottom vertebrae of the spine) fits into the pelvis (figure 2.8)-is stabilized by several ligaments that connect to muscles within the region. The iliolumbar ligament attaches to the transverse process of 1.5, and in some subjects to those of L4 as well (Willard 1997), and passes anteromedially to the iliac crest and the surface of the a
Iliolumbar ligaments Anterior sacroiliac ligament
Right innominate bone (ilium,ischium, and pubis)
b
Sacrotuberous ligament
Iliolumbar ligaments
Pubic arch c Iliac crest Posterior sacroiliac ligament
Sacrospinous ligament Ischial tuberosity Sacrotuberous ligament Figure 2.8 The sacroiliac joint and its supporting ligaments: (a) anterior aspect; (b) posterior aspect; and (c) left aspect of medial section through the pelvis. Reprinted, by permission, from J. Watkins, 1999, Structure and function of the musculoskeletal system (Champaign, IL:Human Kinetics), 1972.
24
.
Back Stability
ilium. The iliolumbar ligament resists movement between the sacrum and lumbar spine, particularly that of lateral flexion. When the ligament is cut, movement of the lumbar spine (L5) on the sacrum increases significantly-lateral flexion by nearly 30%; and flexion, extension, and rotation by 18-23% (Yamamoto et al. 1990). The superior aspect of the SIJcapsule is an extension of the iliolumbar ligament, while the anterior portion of the capsule merges into the sacrotuberous ligament. The sacrotuberous ligament has a triangular shape extending between the posterior iliac spines, SIJ capsule, and coccyx (figure 2.8). Importantly, the tendon of biceps femoris (the large muscle at the back of the upper leg) extends over the ischial tuberosity to attach to the sacrotuberous ligament (Vleeming et al. 1989); the ligament also attaches into some of the deepest fibers of the multifidus muscle (the multifidus runs vertically down the entire length of the back, on either side of the spine) (Willard 1997). Movement at the sacroiliac joint is described as nutation and countemutation (table 2.2). The sacrotuberous ligament resists nutation of the sacrum, while the long dorsal sacroiliac ligament resists countemutation. Even though it is difficult to discern this from observing most anatomical diagrams, the sacrum is not fused with the pelvis-so when I speak of movement of the sacrum, I mean motion within the pelvis as opposed to motion of the pelvis, where the entire structure is moving on the hip. Greater movement ranges have been reported in nonweightbearing than weightbearing movements. Nonweightbearing movements have exhibited as much as 12° innominate rotation during flexion, together with 8 mm translation during extension (Lavignolle et a!. 1983); weightbearing movements were reduced to 2.5° rotation and 1.6 mm maximal translaTable 2.2
Movement
of the Sacroiliac
Nutation Anterior tilting of sacrum Sacral base moves down and forward, apex moves up Size of pelvic outlet increased, pelvic inlet decreased Occurs in standing
.. .
. . Increased as lumbar lordosis increased
.
Iliac bones pulled together,
impacted . Superior aspect of pubis compressed
SIJ
Joint (SIJ)
Counternutation Posterior tilting of sacrum Sacral base moves up and back, apex moves down Pelvic inlet increased, outlet red uced . Occurs in nonweightbearing position such as lying Increased as lumbar lordosis decreased (flatback posture) Iliac bones move apart, SIJdistracted
. .
. . .
. Inferioraspect of pubiscompressed
Biomechanics of the Lumbar Spine
.
25
tion (Sturesson et al. 1989).In a study of healthy individuals aged 20-50 years, Jacob and Kissling (1995) found average rotational motion at the SI] to be 2°, whereas symptomatic patients averaged 6°. Nutation of the SIJ is an anterior tilting of the sacrum on the fixed innominate bones. The sacral base moves down and forward, while the sacral apex moves up, increasing the pelvic outlet. Nutation occurs in standing and increases as lordosis deepens. By pulling the iliac bones together, nutation compresses the SI] as well as the superior portion of the pubic symphasis. Countemutation is the opposite movement, with the sacral base moving up and back and the apex moving downward. This movement occurs in nonweightbearing situations, such as lying prone, and increases as the lordosis is reduced and the low back is flattened. During countemutation, the iliac bones move apart, the pelvic inlet increases, and the pelvic outlet reduces (Kesson and Atkins 1998). A variety of movements occur about the SI] during trunk actions (Lee 1994). During forward bending of the trunk, the pelvis tilts anteriorly and the sacrum moves into extension (coccyx moving backward; i.e., nutation around an oblique axis), causing the iliac crests and posterior superior iliac spines (PSIS) to approximate (i.e., press toward each other) and the ischial tuberosities and the anterior superior iliac spines (ASIS) to separate. During side bending, the trunk laterally flexes and the pelvis shifts to the opposite direction to maintain balance. With left lateral flexion and right pelvic shift, the right innominate bone rotates posteriorly, and the left innominate rotates anteriorly. The sacrum rotates to the right. During trunk rotation, the pelvis rotates in the same direction; therefore, with left trunk rotation, the right innominate anteriorly rotates and the left posteriorly rotates. The sacrum is driven into left rotation.
AXIAL COMPRESSION Vertical loading of the lumbar spine (axial compression) occurs during upright (standing or sitting) postures, exacerbating certain forms of back pain. Knowledge of loading can help us to design safer exercise programs for the back pain sufferer.
Compression
of the Vertebral
Bodies
Within the vertebra itself, compressive force is transmitted by both the cancellous (spongy) bone of the vertebral body and its cortical bone shell. Until about the age of 40, the cancellous bone contributes about 25-55% of the vertebra's strength. As aging-related decreases in bone density lead to a decline in the proportion of cancellous bone, the cortical bone shell carries a greater proportion of load (Rockoff et al. 1969). As the vertebral body is compressed, a net flow of blood out of it (Crock and Yoshizawa
26
. BackStability
1976) reduces bone volume and dissipates energy (Roaf 1960). Blood returns slowly as the force is reduced-leaving a latent period after the initial compression and diminishing the shock-absorbing properties of the bone. Exercises that involve prolonged periods of repeated shock to the spine (e.g., jumping on a hard surface) are therefore more likely to damage vertebrae than those that load the spine for short periods and allow recovery of the vertebral blood flow before repeating a movement.
.
Blood flows-out of the vertebral body with loading, decreasing its shock-absorbing properties. Exercises I that repeatedly load the spine without allowing recovery can therefore lead to accumulated stress.
KEY POINT:
Compression of Intervertebral Discs During standing, 12-25% of axial compression forces are transmitted between adjacent vertebrae by the facet joints (see discussion on page 28); the intervertebral disc absorbs the rest of the force (Miller et al. 1983). The annulus fibrosis of a healthy disc resists buckling; even if a disc's nucleus pulposus has been removed, its annulus alone can exhibit a loadbearing
capacity similar to that of the fully intact discfor a brief period (Markolfand Morris 1974). When exposed to prolonged loading however, the collagen
lamellae of the annulus eventually buckle (see figure 2.7). Throughout the waking day, discalloading diminishes a person's height until the forces inside the disc equal the load forces (Twomey and Taylor 1994). By reducing axial loading, lying down permits restoration of the former spinal length. Lying in a flexed position speeds the regain of lost height as the lumbar discs are distracted (unloaded) during flexion (Tyrrell et al. 1985). Application of an axial load compresses the fluid nucleus of the disc, causing it to expand laterally. This lateral expansion stretches the annular fibers, preventing them from buckling. The degree of discal compression depends on the weight imposed and the rate of loading. A 100kg axial load can compress a disc by 1.4 mm and cause a lateral expansion of 0.75 mm (Hirsch and Nachemson 1954). The stretch in the annular fibers stores energy, which is released when the compression stress is removed. The stored energy gives the disc a certain springiness, which helps to offset any deformation that occurred in the nucleus. A force applied rapidly is not lessened by this mechanism, but its rate of application is slowed, giving the spinal tissues time to adapt. Deformation of the disc occurs more rapidly at the onset of axial load application, the majority of its deformation occurring within 10 minutes of onset. After this time, deformation continues but slows to a rate of about 1 mm per hour (Markolf and Morris 1974),leading to loss of height throughout the day. Under constant loading the discs exhibit "creep" (i.e., they
Biomechanics
of the
Lumbar
Spine
.
27
continue to deform even though the load is not increasing). Because compression causes a rise in fluid pressure, fluid is actually lost from both the nucleus and the annulus. About 10% of the water within the disc can be squeezed out by this method (Kraemer et al. 1985), the exact amount dependent on the size and duration of the applied force. When the compressive force is reduced, the fluid is absorbed back through pores in the cartilage end plates of the vertebra. Exercises that axially load the spine reduce a person's height through discal compression-squat exercises in weight training, for example, can create compression loads in the L3-L4 segment of 6-10 times bodyweight (Cappozzo et al. 1985). Researchers have observed average height losses of 5.4 mm over a 25-minute period of general weight training, and 3.25 mm after a 6-km run (Leatt et al. 1986) (figure 2.9). Static axial loading of the spine with a 40-kg barbell over a 20minute period can reduce a subject's height by as much as 11.2mm (Tyrrell et al. 1985). Clearly, exercises that involve this degree of spinal loading are unsuitable for individuals with discal pathology. The vertebral end plates of the discs are compressed centrally and are able to undergo less deformation than either the annulus or the cancellous bone. The end plates are therefore likely to fail (fracture) under high compression (Norkin and Levangie 1992). Discs subjected to very high compressive loads can show permanent deformation without herniation (Farfan et al. 1976; MarkoH and Morris 1974). However, such compression forces may lead to Schmorls node formation (Bernhardt et al. 1992): the disc end plate (which joins the disc to the vertebral body) ruptures, and nuclear material from the disc passes through to the vertebral body itself. Bending and torsional stresses on the spine, when combined with compression, are more damaging than compression alone, and degenerated discs are particularly at risk. Average failure torques for normal discs are
D D
15
E
.s
10
Weight
training 6-km run
.40-k9 ~static load
.E
C> 0ij; I
5
o
Activity
Figure 2.9 Discal compression
and height loss during exercise.
28
. Back Stability
25% higher than for degenerative discs (Farfan et al. 1976). Degenerative discs also demonstrate poorer viscoelastic properties and therefore a reduced ability to attenuate shock. The proteoglycan of the disc's nucleus makes it hydrophilic, and its ability to transmit load relies on high water content; yet proteoglycan content declines from about 65% in early life to about 30% by middle age (Bogduk and Twomey 1987). When the proteoglycan content of the disc is high (up to age 30 in most subjects), the nucleus pulposus is gelatinous, producing a uniform fluid pressure. After this age, the lower water content of the disc leaves the nucleus unable to build as much fluid pressure. Less central pressure is produced, and the load is distributed more peripherally, eventually causing the annular fibers to become fibrillated and to crack (Hirsch and Schajowicz 1952). The net result is that a disc's reaction to compressive stress declines with age (figure 2.10). The age-related changes in discs cause greater susceptibility to injury. This fact-<:ombined with a general reduction in fitness and changes in trunk movement patterns related to activities of daily living-greatly increases the risk of injury in older individuals. Encourage previously inactive persons over the age of 40 to engage in trunk exercises, under the supervision of a physiotherapist, before attending fitness classes.
Compression
of Facet Joints
The orientations of facet joints differ among various regions of the spine, thereby altering the available motion. In the mid- and lower cervical spine, for example, rotation and lateral flexion are limited but flexion and extension are possible. In the thoracic spine, flexion and extension are limited but lateral flexion and rotation are free. At the thoracolumbar junction (T12-Ll), rotation is the only movement that is limited; in the lumbar spine, both rotation and lateral flexion are limited. a
b
Figure 2.10 Age-related changes in lumbar discs. (a) Maximal disc height and end plate length of youth. (b) Reduced measurements through aging.
Biomechanics of the Lumbar Spine
.
29
The superior / inferior alignment of the facet joints in the lumbar spine means that, during axial loading in the neutral position, the joint surfaces slide past each other. Note, however, that anywhere between T9 and T12, the orientation of the facet joints may change from those characteristic of the thoracic spine to those of the lumbar spine. Therefore, the level at which particular movements will occur can vary considerably among subjects. During lumbar movements, displacement of the facet joint surfaces causes them to impact, or press together. Because the sacrum is inclined and the body and disc of L5 are wedge shaped, during axial loading L5 is subjected to a shearing force. This force is resisted by the more anterior orientation of the L5 inferior articular processes. As the lordosis increases, moreover, the anterior longitudinal ligament and the anterior portion of the annulus fibrosis are stretched, providing tension to resist the bending force. Additional stabilization is provided for the L5 vertebra by the iliolumbar ligament, attached to the L5 transverse process. This ligament, together with the facet joint capsules, stretches to resist the distraction force. Once the axial compression force stops, release of the stored elastic energy in the spinal ligaments re-establishes the neutral lordosis. With compression of the lordotic lumbar spine, or in cases where gross disc narrowing has occurred, the inferior articular processes may impact on the lamina of the vertebra below (see figure 2.11). In this case, the lower joints (L3/4, L4/5, L5/S1) may bear as much as 19% of the compression force, while the upper joints (Ll/2, L2/3) bear only 11% (Adams et al. 1980).
Figure 2.11 Results of compression on discs and facet joints. (a) Normal disc thickness and alignment of superior and inferior articular processes. (b) Reduced disc thickness resulting in increased compression load on facet joint. (c) Extra.articular impingement of facet joint. Reprinted, by permission, from J. Watkins, 1999, Structure and function of the musculoskeletal system (Champaign, IL:Human Kinetics), 146.
30
.
Back Stability
MOVEMENTS
OF THE LUMBAR
SPINE AND PELVIS
Much of the material for this section comes from Norris (1995a) and Norris (1998), to which I refer you for further reading.
Flexion and Extension Both disc height and the horizontal length of the vertebral end plate affect the range of motion attainable during sagittal plane movement of the lumbar spine. Greatest range of motion occurs with a combination of maximum disc height and maximum end plate length (figure 2.10). Since this alignment most often occurs in young females, it is they who possess the greatest ranges of motion at the lumbar spine. With aging, disc height and end plate length become more similar between the sexes, equalizing the available range of motion for males and females in old age (Twomey and Taylor 1994). Q) During flexion movements, the C> C anterior annulus of a lumbar disc co .J::. is compressed, whereas the posU Q) terior fibers are stretched. Simi:; larly, the nucleus pulposus of the disc is compressed anteriorly, c. Q) whereas pressure is relieved over .2: OJ its posterior surface. Since the a; c: total volume of the disc remains unchanged, however, its pressure a should not increase. The increases in pressure seen with posture Q) changes are due not to the bendC> C ing motion of the bones within co .J::. the vertebral joint itself but to the U !!? soft tissue tension created to con::> (/) (/) trol the bending. If the pressure Q) ~ at the L3 disc for a 70-kg standc. Q) ing subject is said to be 100%, su.2: OJ pine lying reduces the pressure to a; c: 25%. The pressure variations inb crease dramatically as soon as the Figure 2.12 Pressure changes in the lumbar spine is flexed and tissue third lumbar disc: (a) in different posi- tension increases (figure 2.12). The sitting posture increases intions; (b) in different muscle-strengthening exercises. tradiscal pressure to 140%, whereas sitting and leaning forFrom Norris 1998. (/) (/) Q)
Biomechanics of the Lumbar Spine
.
31
ward with a lO-kg weight in each hand increases pressure to 275% (Nachemson 1992). The selection of an appropriate starting position for trunk exercises is therefore of great importance. Spinal exercise from a slumped sitting posture, for example, places considerably more stress on spinal discs than the same movement beginning from crook lying (lying on the back with the knees and hips flexed, feet flat on the floor). The posterior annulus stretches during flexion, whereas the nucleus is compressed onto the posterior wall. Since the posterior portion of the annulus is the thinnest part, the combination of stretch and pressure to this area may result in discal bulging or herniation. Because layers of annular fibers alternate in direction, rotation movements stretch only half of the fibers at any given time. The disc is more easily injured during a combination of rotation and flexion, which stretches all the fibers at the same time. As the lumbar spine flexes, the lordosis flattens and then reverses at its upper levels. Reversal of lordosis does not occur at LS-S1 (Pearcy et al. 1984). Flexion of the lumbar spine involves a combination of anterior sagittal rotation and anterior translation. As sagittal rotation occurs, the articular facets move apart, permitting the translation movement to occur. Translation is limited by impaction of the inferior facet of one vertebra on the superior facet of the vertebra below. As flexion increases, or if the spine is angled forward on the hip, the surface (i.e., the top) of the vertebral body faces more vertically, increasing the shearing force due to gravity. The forces involved in facet impaction therefore increase to limit translation of the vertebra and stabilize the lumbar spine. Because the facet joint has a curved articular facet, the load is not concentrated evenly across the whole surface but is focused on the anteromedial portion of the facets (figure 2.13). The sagittal rotation movement of the facet joint causes the joint to open and is therefore limited by the stretch of the joint capsule. The posteriorly placed spinal ligaments are also tightened. Adams et al. (1980) used mathematical modeling to analyze the forces that limit sagittal rotation within the lumbar spine. They found that the disc contributes 29% of the limit to movement, the supraspinous and interspinous ligaments 19%, and the facet joint capsules 39%. In one experiment, the researchers cut (and thereby "released") various posterior tissues in cadavers in order to measure the effects of those tissues on flexion range. Range of motion increased about 40 when the posterior ligaments were released and 90 when the capsule was released. Releasing the pedicles increased the flexion range by 240 in young (14-22 years) subjects. Cutting all the posterior elements increased the flexion range by 100% in the young subjects but by only 60% in the elderly (61-78 years) subjects. During sustained flexion, tissue overstretch results in creep-gradually increasing the range of motion as tissues elongate over time. With aging, the amount of creep is greater, but recovery takes longer (Twomey and
32
. Back Stability Taylor 1994). Occupations that involve prolonged flexion with little recovery (e.g., bricklaying or sitting with poor posture) provide little chance for the overstretched tissue to recover, leading to chronic adaptation of both soft tissue and bone. Such individuals suffer from a high incidence of chronic postural back pain with many acute episodes (Twomey et al. 1988). Sustained flexion results in creep of the lumbar tissues (Le., a gradual increase in range of motion over time). Prolonged flexion with inadequate tissue recovery can lead to chronic adaptation and consequent pain.
KEY POINT:
During extension, anterior structures are under tension, whereas posterior structures are first taken off c stretch and then compressed (depending on the range of motion). Extension movements subject the vertebral bodies to posterior sagittal rotation. The inferior articular processes move downward, causing them to impact against the lamina of the vertebra below. Once the bony block has occurred, if further load is applied, the upper vertebra will axially rotate by pivoting on the impacted inferior articular process. The inferior articular process will move backward, overstretching and possibly damaging the joint capsule (Yang and King 1984). Repeated moveFigure 2.13 The lower lumbar spine and sacrum in (a) standing, ments of this type eventually can lead (b) extension, and (c) flexion. to erosion of the laminal periosteum Reprinted, by permission, from J. (Oliver and Middleditch 1991). At the Watkins, 1999, Structure and function site of impaction, the joint capsule may of the musculoskeletal system (Chamcatch between the opposing bones, crepaign, IL:Human Kinetics), 147.
Biomechanics of the Lumbar Spine.
33
ating another source of pain (Adams and Hutton 1983). Since structural abnormalities can alter a vertebra's axis of rotation, considerable variation exists among subjects (Klein and Hukins 1983).
Rotation and Lateral Flexion During rotation, torsional stiffness is provided by the outer layers of the annulus, by the orientation of the facet joints, and by the cortical bone shell of the vertebral bodies themselves. Moreover, the annular fibers of the disc are stretched as their orientation permits-since alternating layers of fibers are angled obliquely to each other, some fibers will be stretched while others relax. A maximum range of 3° of rotation can occur before the annular fibers will be microscopically damaged and a maximum of 12° before tissue failure (Bogduk and Twomey 1987). The spinous processes separate during rotation, stretching the supraspinous and interspinous ligaments. Impaction occurs between the opposing articular facets on one side, causing the articular cartilage to compress by 0.5 mm for each 1° of rotation and providing a substantial buffer mechanism (Bogduk and Twomey 1987). If rotation continues beyond this point, the vertebra pivots around the impacted facet joint, causing posterior and lateral movement. The combination of movements and forces stress the impacted facet joint by compression, the spinal disc by torsion and shear, and the capsule of the opposite facet joint by traction. The disc provides only 35% of the total resistance (Farfan et al. 1976). When the lumbar spine is laterally flexed, the annular fibers toward the concavity of the curve are compressed and begin to bulge, while those on the convexity of the curve are stretched. The contralateral fibers of the outer annulus and the contralateral intertransverse ligaments help to resist extremes of motion (Norkin and Levangie 1992). Lateral flexion and rotation occur as coupled movements. In the neutral position, rotation of the upper four lumbar segments is accompanied by lateral flexion to the opposite side; rotation of the L5-S1 joint, however, occurs with lateral flexion to the same side. The nature of the coupling varies with the degree of flexion and extension. In the neutral position, rotation and lateral flexion occur to the opposite side, called "type I movement" (i.e., right rotation is coupled with left lateral flexion). But when the lumbar spine is in flexion or extension, rotation and lateral flexion occur in the same direction, called "type II movement" (i.e., right rotation is coupled with right lateral flexion). In the concavity of lateral flexion, the inferior facet of the upper vertebra slides downward on the superior facet of the vertebra below, reducing the area of the intervertebral foramen on that side. On the convexity of the laterally flexed spine, the inferior facet slides upwards on the superior facet of the vertebra below, increasing the diameter of the intervertebral foramen.
34
.
Back Stability
Lumbar-Pelvic Rhythm When people bend forward as though to touch their toes, the movement comes from both the pelvis and the lumqar spine. The pelvis anteriorly tilts on the femur, while the lumbar spine flexes on the pelvis. The combined movement of both lumbar and pelvic motion is called "lumbarpelvic rhythm." With the lumbar spine held immobile and the knees locked, the pelvis can tilt only to roughly 90° hip flexion (hamstring tightness limits further movement). To touch the floor, one must also flex the lumbar spine. Similarly, with the pelvis held immobile, lumbar flexion is limited to about 30-40°, with most movement occurring at the lower lumbar segments. Therefore, to achieve full forward bending, one must move both body segments. When flexing to midrange levels during daily living, individuals can significantly reduce their lumbar flexion by using anterior pelvic tilt. Reduced ability to anteriorly tilt the pelvis increases the need to flex the lumbar spine, opening the possibility of postural pain through repetitive loading of the lumbar tissues. When a person bends forward from a standing position, the pelvis and lumbar spine rotate in the same direction. Lumbar flexion accompanies anterior tilt of the pelvis (figure 2.14a). In the upright posture, the feet and shoulders are static, and the pelvis and lumbar spine move in opposite directions (figure 2.14b)-lumbar extension compensates for an anteriorly tilted pelvis in order to maintain the head and shoulders in an upright orientation. Table 2.3 describes the relationship between various pelvic movements and the corresponding hip joint action. b
Figure 2.14 (a) Lumbar-pelvic rhythm in open chain formation occurs in the same direction. Anterior pelvic tilt accompanies lumbar flexion. (b) Lumbarpelvic rhythm in closed kinetic chain formation occurs in opposite directions. Anterior pelvic tilt is compensated by lumbar extension. From Norris 1998.
Biomechanics of the Lumbar Spine
.
35
Table 2.3 Relationship of Pelvis, Hip Joint, and Lumbar Spine During Right Lower-Extremity Weightbearing and Upright Posture Pelvic
motion
Anterior
pelvic
Posterior
Accompanying joint motion tilt
pelvic
tilt
hip
Compensatory lumbar motion
Hip flexion
Lumbar extension
Hip extension
Lateral drop)
pelvic
tilt (pelvic
Right hip adduction
Lumbar flexion Right lateral flexion
Lateral hitch)
pelvic
tilt (hip
Right hip abduction
Left lateral
Right hip MR
Rotation
to the left
Right hip LR
Rotation
to the right
Forward Backward
rotation
rotation
MR = medial rotation; LR = lateral rotation. Reprinted, by permission, from c.c. Norkin and P.K. Levangie, and function: A comprehensive analysis, 2d ed. (Philadelphia:
flexion
1992, joint structure Davis).
Controlling Spinal Range of Motion If the trunk is moving slowly, a subject feels tissue tension at the end range and is able to stop a movement short of the full end range-thereby protecting the spinal tissues from overstretching. However, rapid trunk movements can build up sufficient momentum to push the spine to the full end range, thereby stressing the spinal tissues. Many amateur and even professional sports directors, teachers, and coaches have their charges engage in rapid and ballistic warm-up exercises, performed with high numbers of repetitions. These activities can lead to excessive flexibility and a reduction in passive stability of the spine.
THE MECHANICS
OF LIFTING
Many individuals engage in some sort of lifting throughout the day. This section briefly describes the mechanical factors and the muscle work involved in lifting. See chapter 11 for proper lifting techniques.
Lifting As a Set of Torques Lifting an object from the ground actually represents a rather complex mechanical problem. One must create a set of torques (technically, torque = force x distance to axis of rotation), involving both the body and the object to be lifted, that will produce the desired outcome (figure 2.15). The forces created during flexion by leverage, body weight, and muscle force-plus those created by the weight being lifted-must be overcome
36
.
Back Stability
by an opposing extension force created by the hip extensor muscles as they contract upon the spine.
·
If the spine is not stable, posterior pelvic tilting brought about by the hip extensors (gluteus maximus and the hamstrings) merely increases the flexion of the spine.
Hip extension
·
Object lifted Figure lifting.
2.15
The mechanics
of
If the spine is stable, the power (cre-
ated when the hip extensors posteriorly tilt the pelvis) is transmitted by the erector spinae along the length of the spine to the upper limb, which then delivers the force to the object being lifted.
The hip extensor muscles are better suited than the erector spinae to initiate a lift from a flexed position. A ISO-pound athlete develops a torque of about 10,000 inch-pounds in lifting a 450-pound weight. Although the hip extensors can generate a torque of about 15,000 inch-pounds, the erector spinae can generate only 3,000, or 30% of that required to perform the lift (Farfan 1988). Note that the bulk of the muscles creating the force (gluteus maxim us) are some distance from the limb controlling the movement (compare this arrangement with the fingers: the muscles that flex and extend the fingers are located not right above the fingers, where they would be in the way, but in the forearm). When prescribing exercises within the back stability program to help re-educate a person in correct lifting habits, emphasize use of the hip extensors (spinal extensors are far less important in this case), working with a stable spine. The hip hinge action, which emphasizes the gluteals, is a good exercise to use (see page 72). Modeling the spine as a cantilever system according to standard mechanical principles, one can calculate the torques of various forces acting on the spine during lifting. Where the leverage is in equilibrium, the sum of the torques is zero, with flexion forces exactly balancing extension forces. It is possible to calculate both the force needed to lift an object and the resulting compression force on the lumbar spine (Sullivan 1997). In order to lift a weight, the muscles and connective tissues in the lumbar spine must counteract the flexion caused by the weight by providing an equal amount of extension (figure 2.15). However, since the weight is far from the fulcrum while the lower back muscles and tissues are very near to it, the muscles and tissues have much less leverage and must therefore exert much more force than just the weight of the object being lifted. Meanwhile, the vertebral joints experience a compression
Biomechanics of the Lumbar Spine
.
37
that is the sum of this force and the weight of the object. That sum is much greater than the weight alone and can be very large indeed! Yet, using postmortem measurements of actual vertebral strength, Perey (1957) estimated that lifting a weight heavier than 110 kg (242.5 lb.) would exceed the compressive strength of vertebrae. Such calculations clearly indicate that the spinal column alone cannot bear excessively large weights without undergoing severe damage. In order to reduce the compressive force acting on the spinal column when lifting large amounts of weight (as, for example, in Olympic weight lifting), an individual must substantially strengthen all the vertebral reinforcing mechanisms reviewed in chapter 3. The spinal column itself is not strong enough to bear the compression force from lifting heavy weights. The force created by the torque of lifting heavy weights can be many, many times the force of the weight itself-the muscles and connective tissues of the lumbar spine must bear the large majority of the forces involved. If these soft tissues are not sufficiently trained, severe injury can result.
KEY POINT:
The Flexion Relaxation Response
in Lifting
When a subject flexes the spine during a lift, the erector spinae are electrically silent just short of full flexion (Kippers and Parker 1984). This phenomenon, called the flexion relaxation responseor critical point, is the result of elastic recoil (rebound) of the posterior ligaments and musculature. This point does not occur in all individuals (see below) and occurs later in the range of motion when weights are carried (Bogduk and Twomey 1991). During the final stages of flexion and from 2-100extension (Sullivan 1997), movement occurs by recoil of the stretched tissues rather than by active muscle work. During bending, the erector spinae are electrically silent just short of full flexion. This phenomenon is the "flexion relaxation response."
KEY POINT:
If the erector spinae are in spasm, chronic low back pain often obliterates the flexion relaxation response. Failure of the muscles to relax prevents adequate perfusion with fresh blood and can lead to local ischemic muscle pain. Interestingly, during a squat lift with the back perfectly straight, the latissimus dorsi contracts powerfully at the beginning of the lift-perhaps to initiate extension by pulling on the thoracolumbar fascia (McGill and Norman 1986; Sullivan 1997). With extremely heavy lifts of any type, as subjects flex forward to the point of electrical silence, the
38
. Back Stability
positions of the vertebrae suggest that they do not reach the point at which the ligaments would be loaded (i.e., stretched or tensioned greater than at rest) (Cholewicki and McGill 1992). The electrical silence of the muscles and the anatomical alignment of the vertebral segments suggest that the final degrees of flexion as well as the first degrees of extension occur through elastic recoil of the spinal extensor muscles. The length/tension relationship in muscles (figure 2.16) shows that a muscle loses active tension as it is stretched-but even toward the end of the range of movement, there is little decrease in total tension since an increase in passive force (recoil, as happens with a stretched rubber band) largely makes up for the decrease in active contraction. As the spine returns from a fully flexed position, the ligaments may produce some 50 N . m of tension while the recoiling muscles produce 200 N . m. The combined extensor forces of the two passive systems represents the major component of the "posterior ligamentous system" supporting the spine (Bogduk and Twomey 1991).
Arch Model of the Spine Instead of representing the spine as a cantilever system as just described, one can use the model of an arch (Aspden 1987, 1989).The ends (abutments) of the arch are provided caudally by the sacrum and cranially by a combination ofbodyweight and muscular /ligamentous forces. The principle difference between a lever and an arch is that the lever is externally supported, whereas the arch is intrinsically stable. Any load positioned on the convex surface of the arch will create an internal thrust line that runs in a straight
......./
.Total
"
.'
,
,,
, ,,
,,
, ,,
,,
Muscle length
Figure 2.16 The length-tension From Norris 1998.
relationship
in muscles.
Active
Biomechanics ofrhe
Lumbar Spine.
39
line to the arch abutments (figure 2.17a). For the arch to remain stable, the thrust line must stay within the physical boundaries of the arch. The deeper within the arch the thrust line stays, the more stable the arch will be. In the case of the spine, the thrust line is positioned within the vertebral bodies. Because a lOO-kg weight lifted in a stooped position (lordosis lost) creates a thrust line outside the spine (figure 2.17b), the arch is unstable. By tensing the back extensor and abdominal muscles at the same time, however, one can create intra-abdominal pressure (lAP) that moves the thrust line back into the spine and increases spinal stability (figure 2.17c).
b
Figure 2.17 (a) General mechanics of an arch. A load on the convex surface of an arch creates an internal thrust line. For stability, the thrust line must stay within the depth of the arch ring. (b) Applying the arch model to the spine. Lifting a heavy weight in a stooped position creates a thrust line that moves outside the arch of the spine, making the spine unstable. (e) lAP acting on the anterior surface of the spine and adjustment of lordosis moves the thrust line back within the vertebral bodies. Reprinted, by permission, from C. Norris, 1995, "Spinal stabilisation," Physiotherapy journa/Bl(3):
4-12.
40
. Back Stability
Moreover, an individual can use the spinal muscles (which are intrinsic to the arch) to adjust the lordosis, so that the thrust line continually remains within the arch of the spine. The stiffness of the spine (resistance to bending) also is increased through the thoracolumbar fascia (TLF) and hydraulic amplifier mechanisms. Some writers believe the arch model of the spine seriously underestimates the compressive forces on the spine (Adams 1989). For further discussion of lAP and other stabilizing mechanisms, see chapter 3.
LIFTING
METHODS
There are two basic ways to lift something: in the squat lift, a person bends the knees and back; in the stoop lift, the legs remain straight and the back alone bends. Because the legs are apart and bent with the squat lift, an individual can hold the object closer to the body's line of gravity-thereby reducing the length of the lever arm from the body's line of gravity to the center of gravity of the object. The disadvantage of the squat lift is that individuals are lifting more of their bodies (the legs and trunk as opposed to the trunk alone) and therefore must expend more energy than with a stoop lift. The erector spinae are more active in positions where the lordosis is maintained (Delitto et al. 1987)-after they have attained a fully erect position when lifting a heavy weight, people tend to lean back in order to balance the weight and to use their hip flexor muscles to resist further spinal extension and to stabilize their spines. In a squat lift, a person can hold a weight closer to the body's center of gravity, thereby reducing the torque on the spine.
KEY POINT:
In addition to differentiating between the squat lift and stoop lift, we must also examine the difference between using a squat lift with the back lordotic (lumbar spine minimally extended) and with the back flat (lumbar spine minimally flexed). Lumbar curvature is calculated as the angle formed between the surface of the vertebral body of L1 and that of the sacrum (figure 2.18). The population mean value of this angle is 50°, although in children it is increased to 67° and in young males to as much as 74° (Bogduk and Twomey 1991) depending on posture type. The lordosis naturally results from the shapes of the vertebrae and disks of the lumbar spine. The L5-S1 vertebral disc is wedge shaped, its posterior height typically about 7 mm less than its anterior. The L5 vertebral body also is wedge shaped, its posterior height typically 3 mm less than its anterior. The remainder of the lordosis occurs because the discs themselves (not the vertebral bodies) are wedge shaped. The sacrum is angled at about 30° to the horizontal, and changes to this angle affect the sacroiliac joint.
Biomechanics
of the Lumbar
Spine
.
41
Because the orientation of the vertebrae differ between the squat and stoop L1 lifts, the load distribution is affected. The lengths of various trunk muscles also difL2 fer between the two lifts. Since the depth of the lumbar discs (6-12 mm) is considL3 erably smaller than the vertical height of the lumbar vertebrae (30-45 mm), even minimal changes in vertebral angles can L4 greatly deform the discs. A flexion angle of 10-12°, for example, stretches the posL5 terior annulus by more than 50% (Adams and Dolan 1997). Repeated loading in a lordotic posture can cause compressive stress within the posterior annulus of a disc and load the adjacent facet joints. Maximal flexion (up to the elastic limit) Sacrum can thin the posterior annulus and cause posterior prolapse. Minimal flexion (flatback), however, which brings the verteCoccyx~ bral bodies into vertical alignment, equalizes compressive stress across the Figure 2.18 The curvature of whole disc and unloads the facets the lumbar spine can be designated by the angle (Q) formed (Adams et al. 1994). At 60-80% of maxibetween lines through the surmum flexion, the posterior tissues exert face of L 1 and the sacrum. a substantial extensor torque--yet there Adapted, by permission, from J.K. is only a small compression effect on the Loudon, S.L. Bell, and J,M. Johnston, lumbar discs. Moreover, tension in the 1998, The clinical orthopedic assessment guide (Champaign, IL: Human thoracolumbar fascia helps to stabilize Kinetics), 54. the sacroiliac joint-and contraction of the gluteal muscles, the abdominals, and latissimus dorsi all increase the TLF tension in a flatback posture. To lift a heavy object, one optimally should use a squat lift while maintaining the neutral position of the spine. The spine is likely to flatten as the weight is taken, and this technique should prevent hyperflexion as long as the object is pulled toward the pelvis. KEY POINT: Have your client perform squat lifts when lifting an object, bringing the object in toward the pelvis. As your client begins to raise the weight, her lumbar spine flattens to minimally compress the lumbar discs and unload the facet joints. In this position, tissue recoil provides substantial extension power.
. BackStability
42
SUMMARY
· .
A spinal segment, comprising two adjacent vertebrae, is comparable to a simple leverage system, connected and held together by ligaments. Because spinal ligaments are interconnected with fasciae surrounding back muscles, which in turn eventually merge with ligaments and muscles as distant as the extremities of limbs, movements of most parts of the body can affect the stability of the spine. The deep abdominal muscles in particular are very important in keeping the spine stable (Le., keeping vertebrae in line even during heavy lifting). Spinal discs, between each pair of vertebrae, absorb stress through stretching of the elastic fibers in the outer annulus and through cushioning by the highly plastic, hydrophilic nucleus pulposus. With age, the nucleus loses water content and the fibers lose elasticity. The facet joints are synovial joints between the inferior articular process of one vertebra and the superior articular process of its neighbor. Their articular cartilage can become brittle with age. Within the vertebra itself, compressive force is transmitted by both the cancellous (spongy) bone of the vertebral body and its cortical bone shell. Cancellous tissue declines with age. The vertebrae themselves, however, can bear only a small fraction of the load placed on the spine by heavy weights without experiencing serious injury. In order to successfully bear heavy weight, the spine must be stabilized by muscles and ligaments.
. . . . .
~ Stabilization Mechanisms in the Lumbar S1!ine Devoid of its musculature, the human spine is inherently unstable. The spine of a fresh cadaver stripped of muscle can sustain a load of only 4-5 lb. before it buckles into flexion (Panjabi et al. 1989). Moreover, the center of gravity of the upper body (when standing upright) lies at stemallevel (Norkin and Levangie 1992). This combination of flexibility and weight distribution is approximately comparable to balancing a 75-pound weight at the end of a 14-inch flexible rod (Farfan 1988). From the strictly mechanical standpoint, discs don't contribute as much as one might think to the spine's strength: lifting heavy objects imposes on the lower lumbar spine a compressive force that greatly exceeds the failure load of the vertebral discs unless additional support is present (Bartelink 1957; Bradford and Spurling 1945; Morris et al. 1961). By reducing the compression forces on lumbar discs, several mechanisms help stabilize the spine (Norris 1995a). These mechanisms, on which this chapter focuses, include the posterior ligamentous system, several processes involving the thoracolumbar fascia, actions of trunk muscles, and intra-abdominal pressure.
THE POSTERIOR
LIGAMENTOUS
SYSTEM
The interspinous and supraspinous ligaments, facet joint capsules, and thoracolumbar fascia (TLF) together provide passive support for the spine sufficient to balance between 24% and 55% of imposed flexion stress (Adams et al. 1980). In the unstretched position, collagen fibers within the anterior and posterior longitudinal ligaments and the ligamentum flavum (see figure 2.3, page 16) are aligned haphazardly. When the ligaments are stretched as the spine flexes or extends, however, the collagen fibers become aligned and the ligament becomes stiffer (Hukins et al. 1990; Kirby et al. 1989). Prestressed by 10-13% at rest, the ligaments retract when cut (Hukins et al. 1990). The 43
44
. Back Stability
longitudinal ligaments therefore maintain a compressive force along the axis of the spine, causing it to act somewhat like a prestressed beam (Aspden 1992).The ligaments are viscoelastic (Le.,they stiffen when loaded rapidly). Rapid loading therefore increases the thrust within the spine and tends to approximate (bring closer together) the vertebrae, enhancing spinal stability. Power created by the hip extensors posteriorly tilts the pelvis and is transmitted through the spine to the thorax and upper limbs via the ligamentous system. Some authors have maintained that for this passive mechanism to work, the spine must remain flexed. They argued that if the spine extends, tightness of the posterior ligaments will decrease and their ability to stabilize the spine will be lost (McGill and Norman 1986). More recently, however, it has been shown that the spine need not become kyphotic before it can create tension by stretching the tissues (Gracovetsky et al. 1990). The posterior ligamentous system alone can sustain a maximum torque of only about 50 N . m (Bogduk and Twomey 1991), less than 25% of that of the contracting erector spinae. However, two passive systems are at work here (see page 38). In addition to the recoil from the posterior ligamentous sytem, the erector spinae are also recoiling. At the point of full flexion, these muscles no longer contract (they are electrically silent), but they do exert a force through recoil much like that of a giant elastic band. The force that the erector spinae create through recoil is about 200 N . m equal to their potential contractile force. The combined posterior musculoligamentous system therefore provides a substantial stabilizing mechanism in full flexion.
~
The posterior ligaments of the spine can sustain 50 N . m of torque and resist over 50% of the flexion stress imposed on the spine. The passive tension (elastic recoil) in the stretched erector spinae can create 200 N . m of torque, equal to their maximum contraction.
THE THORACOLUMBAR
FASCIA
The thoracolumbar fascia performs a number of important functions during back stability, which I briefly review here. Note that the fascia also acts to stabilize the sacroiliac joints.
Structure of the Thoracolumbar
Fascia
The thoracolumbar (lumbardorsal) fascia (TLF) has three layers that cover the muscles of the back (figure 3.1). The anterior layer derives from fascia covering the quadratus lumborum and attaches to the transverse processes
Stabilization Mechanisms in the Lumbar Spine.
45
-Terms YouSh'OUltI Kn-ow=: aponeurosis connective tissue that attaches muscle to bone approximate (verb) to move or bring objects closer together contralateral originating in or affecting the opposite side of the body fascicle a small bundle of nerve or muscle fibers hoop pressure the inward pressure exerted by the muscles surrounding the trunk ipsilateral on the same side (of the body) kyphotic convex curvature of the thoracic spine creating a hunchback lamina a thin flat layer or membrane raphe, lateral a ridge along the side of the erector spinae muscles formed by the connective tissue of the latissimus dorsi, internal obliques. and transversus abdominus
(Bogduk and Twomey 1991). The middle layer, behind the quadratus lumborum, attaches both to the transverse processes and to the intertransverse ligaments. Laterally, it extends to cover transversus abdominis. The posterior layer, which envelops the erector spinae, attaches from the spinous processes and wraps around the back muscles to blend with the rest of the TLF laterally to the iliocostalis. The point at which the layers blend is the lateral raphe. The superficial layer of the TLF is continuous with the latissimus dorsi and gluteus maximus. Sometimes a few fibers attach to parts of the external oblique and trapezius, and some cross the body midline (Vleeming et al. 1995). At L4-LS level, fibers from latissimus dorsi and gluteus maximus differ in orientation, giving the superficial layer of the TLF a crosshatched appearance. This appearance may even extend down to the LS-S2 level (Vleeming et al. 1997).The fibers of the deep layer are continuous with the sacrotuberous ligament (and through it to the biceps femoris muscle of the upper leg); and they attach to the posterior superior iliac spines, the iliac crests, and the sacroiliac ligaments (see figure 2.8, page 23). In the thoracic region, fibers of the serratus posterior inferior are continuous with the TLF (figure 3.2).
Thoracolumbar
Fascia Mechanism
In addition to its passive role, the TLF has two further capacities that involve muscle contraction. The transversus abdominis, through its attachment to the lateral raphe, pulls on the TLF. Although both attach to the lateral raphe (figure 3.3), the deep laminae of the TLF angle upward, while
Transversus
Psoas
CD Anterior @ Middle @ Posterior
Figure
3.1
abdominis
layer Erector
layer
spinae
layer Cross
section
of trunk
showing
thoracolumbar
fascia
(TLF).
Trapezius Serratus posterior inferior (beneath latissimus dorsi)
Latissimus
dorsi
Internal oblique and transversus abdominis
External oblique
Gluteus maximus
Figure
46
3.2 Muscle attachments
into the thoracolumbar
fascia (TLF).
Stabilization Mechanisms in the Lumbar Spine.
47
Superficial lamina ofTLF Lateral raphe
Figure 3.3 The thoracolumbar fascia mechanism. Through its attachment to the lateral raphe, the transversus abdominis pulls on the TLF.The angulation of both the deep and superficial layers of the TLF creates a net force that tends to approximate the vertebrae.
the superficial laminae angle downward. As the transversus abdominis contracts and pulls on the lateral raphe, the deep and superficial fibers of the TLF pull laterally for the most part, although some force is transmitted along the length of the TLF. Originally, this approximating force was calculated as 57% of the force applied to the lateral raphe (Macintosh and Bogduk 1987), an increase in force termed the "gain" of the TLF (Gracovetsky et al. 1985). However, more detailed anatomical investigation has revealed that the torque created by contraction of transversus abdominis onto the TLF is between 3.9 and 5.9 N . m-compared to that from the back extensors of 250-280 N . m (Macintosh et al. 1987). Rather than actively extending the spine through the approximating force represented by "gain," then, the primary importance of the TLF seems to be providing passive resistance to flexion.
Thoracolumbar
Fascia as Hydraulic Amplifier
The TLF exerts an even greater stabilizing effect through its role in the socalled hydraulic amplifier effect (Gracovetsky et al. 1977). The posterior layer of the TLF is retinacular tissue (i.e., very strong reinforcing connective tissue) that envelops the erector spinae. As the erector spinae contract, the TLF resists the expansion of the bellies of the shortening muscles by increasing tension in the fascia. Some believe that the predominant antiflexion effect of the TLF occurs via this hydraulic amplifier effect rather than by
48
.
Back Stability
its pull on the transversus abdominis (Macintosh et al. 1987). Restriction of the radial expansion of the erector spinae by the TLF has been shown to increase the stress generated by these muscles by as much as 30% (Hukins et al. 1990).
Thoracolumbar Fascia Coupling and the Sacroiliac Joint A combination of form closure and force closure stabilizes the sacroiliac joint (51])(Vleeming et al. 1990). Form closure arises from the anatomical alignment of the bones of the ilium and sacrum, where the sacrum forms a kind of keystone between the wings of the pelvis (Norris 1998). Force closure results from muscles pulling laterally onto fascia and ligaments that pass over the joint. The combination of form and force closure creates a very useful self-locking mechanism within the 51J. Any activity that weakens these forms of closure can create pathological symptoms in the 51J. Nutation (see table 2.2 on page 24) tensions the 51Jligaments, pulling the posterior parts of the iliac bones together and increasing 51Jcompression. Two ligaments are of special importance to self locking-the sacrotuberous ligament connecting the sacrum to the ischial tuberosity, and the long dorsal sacroiliacligament from the third and fourth sacral segments to the posterior superior iliac spines (PSIS). Both ligaments blend over the posterolateral aspect of the sacrum to form an expansion approximately 20 mm wide and 60 mm long. The ligaments attach to the posterior layer of the TLF and to the aponeurosis of the erector spinae. Nutation tensions the sacrotuberous ligament, while counternutation tensions the long dorsal sacroiliac (51)ligament. The 51 ligament is tensioned by contraction of the biceps femoris and of the gluteus maximus. Force closure of the 51] opens the possibility of treating 51Jlesions with exercise therapy either passively (automobilization) or actively through contraction of the biceps femoris, gluteus maxim us, latissimus dorsi, or erector spine. Clearly, if muscle affects the 51J, as has been shown by Vleeming's work (Vleeming et al. 1995a), training these muscles could improve 51Jfunctions. Moreover, any muscle that tensions the TLF should also affect force closure of the 51J. When the erector spinae contract, they pull the sacrum forwardinducing nutation of the 51]and tensing the interosseous and sacrotuberous ligaments. The iliac portion of the muscle tends to pull the cranial aspect of the 51Jtogether, whereas the action of nutation pulls the caudal aspect apart. The gluteus maxim us can compress the 51Jdirectly and indirectly through its attachment to the sacrotuberous ligament. This occurs particularly when the gluteus maximus contracts with the contralateral
Stabilization Mechanisms in the Lumbar Spine
.
49
latissimus dorsi and both muscles tension the TLF, whose fibers join the two muscles. Tension in the sacrotuberous ligament is increased by tensioning the long head of biceps femoris. This occurs most noticeably in a flexed trunk or stooped position, in which the sacrotuberous ligament is also tensioned by the sacral portion of the erector spinae and the gluteus maxim us. 51] pain frequently occurs during and after pregnancy, when laxness of the 51] ligaments reduces form closure of the joints. Female gymnasts experience similar problems: the inherent hyperflexibility of gymnastics generally increases the laxity of the pelvic ligaments, reducing the form closure that they produce. The increased muscular stability resulting from the muscular demands of the sport is compensated for by the laxness, as long as the women continue their activity. When their muscle strength declines after they stop practicing the sport, the 51] is left unstable and open to pathology. SI] pain of this type is often helped by using a pelvic belt; it may also be helped by improving force closure of the 51] by using stabilization techniques for the lumbar spine and enhancing gluteal muscle strength using the hip hinge action (see page 77). Specific exercise can improve stability of the sacroiliac joint by restoring the natural mechanisms of form closure and force closure.
KEY POINT:
TRUNK
MUSCLE ACTION
Facilitating co-contraction of the muscles surrounding the lumbar spineincluding the erector spinae, transversus abdominis, multifidus, and the oblique abdominals-may enhance spinal stability (Richardson et al. 1990).
Spinal Extensor Muscles The spinal extensors may be broadly categorized into superficial muscles (the erector spinae) that travel the length of the lumbar spine and attach to the sacrum and pelvis, and deep, or intersegmental (unisegmental) muscles (multifidi, interspinales, and intertransversarii) that span the spaces between the individual lumbar segments. The intersegmental muscles, being more deeply placed, are closer to the center of rotation of the spine and have a shorter lever arm than the superficial muscles. However, their closeness to the center of rotation means that the change in length of intersegmental muscles is less for any given change in the spine's angular position; and the muscles' shorter length gives them a faster reaction time, creating a smoother and more efficient stabilizing control system (Panjabi et al. 1989). The intersegmental nature
so
.
Back Stability
of these muscles also means that they are able to "fine tune" the spinal movements by acting on individual lumbar segments rather than the whole spine (Aspden 1992). Being larger in size and further from the center of rotation, the superficial muscles are better placed to create gross sagittal rotation movements, while the intersegmental muscles are of greater importance to spinal stability (Panjabi et al. 1989). Furthermore, because the smaller intersegmental muscles have about seven times the number of muscle spindles (Bastide et al. 1989) than the larger muscles have, they have a greater proprioceptive role (see following discussion). Deep (Intersegmental) Muscles Of the deeply placed intersegmental muscles, the multifidus is most important for lumbar stability. The fibers of multifidus are arranged segmentally, and each fascicle of a given vertebra has a separate innervation by the medial branch of the dorsal ramus of the vertebra below (Macintosh and L1 Bogduk 1986). The primary function of each multifidus fascicle may be to control L2 lordosis at its particular vertebral level and to independently counteract any imposed loading (Aspden 1992). The action of the L3 multifidus can be resolved into a small horizontal and very much larger vertical L4 component (figure 3.4), which (as is clear when viewed from the side) acts at 90° to L5 the spinous processes. This configuration enables multifidus to produce posterior sagittal rotation (rocking) of the lumbar vertebrae (Macintosh and Bogduk 1986). This action neutralizes spinal flexion caused as a secondary action when the Sacrum oblique abdominals produce spinal rotation. Because the line of action of the long fascicles of multifidus lies behind the lumCOCCyxL bar spine, the muscle also increases lumbar lordosis. Multifidus is active through Figure 3.4 Lateral view showthe whole range of flexion, during rotaing the line of action of multifidus, with its vertical alignment. tion in either direction, and during extenAdapted, by permission, from J.K. sion movements of the hip (Valencia and Loudon, 5.L. Bell,andJ,M.Johnston, Munro 1985). Posterior sagittal rotation J 998, The clinical orthopedic assessment guide (Champaign, IL: occurs during all flexion movements, in order to resist the anterior sagittal rotation Human Kinetics), 54.
Stabilization Mechanisms in the Lumbar Spine
.
51
that naturally accompanies flexion. The importance of multifidus in producing this action is therefore essential to stability of the lumbar spine in normal movements. Panjabi's (1992) description of instability (as a reduction in stiffness within the neutral zone of the lumbar spine) is particularly relevant to multifidus function. Multifidus is a muscle well positioned to enhance segmental stiffness in the neutral zone and contributes nearly 70% of the stiffness resulting from muscle contraction (Wilke et al. 1995). Real-time ultrasound imaging has revealed marked asymmetry of the multifidus in patients with low back pain (Hides et al. 1994). Crosssectional area (CSA) of the multifidus was markedly reduced on the ipsilateral side to symptoms, the site of reduction corresponding to the level of lumbar lesion as assessed by manual therapy palpation. The muscle also showed a rounder shape, suggesting muscle spasm. The suggested mechanism for the CSA reduction was by inhibition through perceived pain via a long loop reflex. The level of vertebral pathology may have been targeted to protect the damaged tissues from movement. The authors suggested that the rapid muscle wasting (less than 14 days in 20 of the 26 patients studied) may have resulted from spasm-induced reduction in circulation to the muscle. In addition to changes in muscle bulk, Biedermann et al. (1991) observed altered fiber types in the multifidus of low back pain (LBP) patients; patients who tended to decrease their physical and social activities as a result of LBP showed a reduced ratio of slow twitch to fast twitch muscle fibers. This could be the muscle's adaptive response to changes in functional demand placed on it, and/ or the injury may have caused a shift in recruitment patterns of motor units of the paraspinal muscles, with the fast twitch motor units being recruited before the slow twitch units. Pathologic changes in the multifidus following low back pain include a motheaten appearance of type I fibers (Hides et al. 1996) and an increase in fatty deposits (Parkkola et al. 1993). Recovery of multifidus function following low back pain does not occur automatically following the resolution of pain and resumption of normal daily activity. In a study comparing medical treatment alone (1-3 days' bed rest, analgesics, and anti-inflammatory medication) with medical treatment plus specific exercise therapy to the multifidus, Hides et al. (1996) showed that multifidus activity could be retrained. Subjects who had experienced first-episode acute low back pain showed an average of 24% reduction in CSA to the multifidus on the painful side. The difference between painful and painless sides changed from nearly 17% after 4 weeks to 14% after 10 weeks in those subjects receiving medical treatment alone. For those who received additional exercise therapy, however, the mean values were 0.7% at 4 weeks dropping
to 0.24% after 10 weeks (figure 3.5).
S2 . Back Stability
30
No exercise
therapy
25 % difference in cross-sectional area between sides
-----
20
Exercise
therapy
15
10 5 o o
Figure Reprinted
~
3.5 from
Ultrasound Hides
2 Weeks
imaging
results
3
4
of multifidus
muscle
recovery.
et al. 1996.
Low back pain leads to reduced cross-sectional area in the multifidus muscle. As the pain reduces, recovery not automatic-rehabilitation is required.
Superficial
Muscles
The lumbar
erector spinae
consists of two muscles:
is
the iliocostalis
and
the longissimus (figure 3.6). Each of these muscles has two components arising from both the thoracic and lumbar spine. Functionally, therefore, the erector spinae can be considered in four distinct groups: lumbar longissimus, lumbar iliocostalis, thoracic longissimus, and thoracic iliocostalis (Macintosh and Bogduk 1987). The force produced by the lumbar longissimus can be resolved into a large vertical vector and a smaller horizontal vector (figure 3.7). However, the fascicle attachments are closer to the axis of Iliocostalis thoracis sagittal rotation than those of multifidus, so Longissimus thoracis their effect on posteSerratus rior sagittal rotation is posterior inferior less. Because the horizontal vectors of lumIliocostalis lumborum bar longissimus are directed backward, Longissimus lumborum the muscle is able to Quadratus lumborum draw the vertebrae backward into posterior translation and Figure 3.6 Muscles of the back. restore the anterior
Stabilization Mechanisms in the Lumbar Spine.
53
translation that occurs with lumbar flexion. The upper lumbar fascicles are better equipped to facilitate posterior sagittal rol2 tation, whereas the lower levels are better suited to resist anterior translation. The lumbar iliocostalis has a similar l3 action to that of the lumbar longissimus. In addition, the muscle cooperates with l4 multifidus to neutralize flexion caused when the abdominals rotate the trunk. The thoracic longissimus can indirectly l5 increase lumbar lordosis via its effect on the aponeurosis of the erector spinae. It also indirectly laterally flexes the lumbar spine through its lateral flexion of the thoracic spine. Sacrum The thoracic iliocostalis attaches not to the lumbar vertebrae but to the iliac crest. On contraction, these fascicles increase lordosis; through their additional leverage Coccyx~ from the ribs, they indirectly laterally flex Figure 3.7 lateral view of the the lumbar spine. During contralateral lumbar spine, showing the line of the lumbar iliocostalis and rotation, the ribs separate, stretching the thoracic iliocostalis which can therefore act lumbar longissimus, and their more oblique orientation. Note as a limiting factor to this movement. On the greater horizontal force contraction, the thoracic iliocostalis will vector (H) and smaller verical de-rotate the rib cage and lumbar spine force vector (V) of the lower fifrom a position of contralateral rotation. bers of these muscles. It is probably the endurance rather than Adapted, by permission, from J.K. the strength of the erector spinae that is Loudon,S.L.Bell,andJ,M.Johnston, 199B, The clinical orthopedic as- important to LBP rehabilitation. Endursessment guide (Champaign, IL: ance has been used as a predictor for susHuman Kinetics), 54. ceptibility to LBP (Beiring-Sorensen 1984). Moreover, subjects with a history of LBP may have reduced endurance of the back extensors compared to normal subjects, but similar strength Gorgensen and Nicolaisen 1987). As fatigue increases, subjects with LBP show reduced precision and control of trunk movements. Loss of torque from the trunk muscles in these subjects is relatively less than the loss of control and precision (Pamianpour et al. 1988), indicating that a rehabilitation program should include restoration of endurance for the spinal extensors. Selective recruitment of the torque-producing superficial muscles from the stabilizing deep muscles is also important for rehabilitation of active lumbar stabilization (Ng and Richardson 1994). l1
54
.
Back Stability
The quadratus lumborum (figure 3.6) can be an important back stabilizer in certain circumstances (McGill et al. 1996). The muscle lies deeper than the erector spinae and has medial and lateral fibers. The medial fibers connect the lumbar transverse processes to the ilium and iliolumbar ligament or the 12th rib, while the lateral fibers directly connect the ilium and iliolumbar ligament and 12th rib (Bogduk and Twomey 1991). The quadratus lumborum has a small extensor torque and a larger lateral flexion torque and is able to stabilize the lumbar spine via its segmental attachments (McGill et al. 1996). EMG with fine wire electrodes has shown the muscle to be more active during lateral bending than during extension and especially active in upright standing and unilateral carrying (McGill et al. 1996). Side-support actions shift some of the loading of the muscles from the discs and facet joints of the lumbar spine to the side (McGill 1998). This role of the quadratus lumborum as a potential stabilizer of the lumbar spine expands the traditionally recognized role of the muscle as a prime mover of side flexion and as an auxiliary muscle of respiration.
The Iliopsoas The iliopsoas (figure 3.8) consists of the separate psoas and iliacus muscles. The psoas major arises from the vertebral bodies and discs of the lumbar and 12th thoracic vertebrae and from their transverse processes. The muscle passes downward and laterally, beneath the inguinalligament, to blend with the fibers of iliacus and then to Psoas attach onto the posterior aspect of the lesser trochanter of the femur. The iliacus is a large triangular muscle on the anterior Iliacus aspect of the pelvis. It arises primarily from the upper and posterior portions of the iliac fossa, but some fibers have been found on the sacrum and anterior sacroiliac ligament (Palastanga et al. 1994). The fibers from iliacus pass downward and medially to blend with those of psoas major and attach into the lesser trochanter, Figure 3.8 The iliopsoas muscle, compris- a few fibers merging with the ing the psoas and the iliacus, anterior view. joint capsule.
Stabilization Mechanisms in the Lumbar Spine.
55
The iliopsoas flexes the hip; with the hip fixed, it anteriorly tilts the pelvis and flexes the lumbar spine. Although these actions are minimal, the psoas major extends the upper lumbar spine and flexes the lower lumbar spine (Bogduk et al. 1992); far more important is its production of compression and shear forces over the lumbar spine. The individual fascicles of psoas spiral anteromedially and are all of similar lengths. The lines of action of these fascicles run very close to the axis of rotation of the lumbar spine, giving the muscle fascicles very small torque arms and reducing the muscle's ability to flex the trunk on the stationary hip. However, the compression and shear forces created by the psoas on the lumbar spine are considerable and may even equal full trunk weight. The shearing force exerted on 15-51 by maximum contraction of a single psoas muscle is nearly twice that exerted on this joint by trunk weight in normal upright standing (Bogduk et al. 1992). Because the two components of iliopsoas have a separate innervation (psoas from the anterior rami and Ll-3, and iliacus from the femoral nerve), they can be activated separately. In a study using fine wire electrodes guided by high-resolution ultrasound, Andersson et al. (1995) showed selective recruitment of iliacus during contralateral leg extension from single-leg standing. No postural activity was seen in either muscle during relaxed standing or with the whole trunk flexed to 30°. When the contralateral hand was loaded (34-kg weight), psoas was active but iliacus was electrically silent. During sitting with a straight back, psoas was active but iliacus relatively silent; while in relaxed sitting, both muscles were inactive. Both muscles showed moderate activity when subjects sat with an anteriorly tilted pelvis and an increased lordosis. During abdominal exercise, both muscles were active during straight-leg sit-ups-with even higher activity during sit-ups with the knees and hips flexed to 90° (crunch position). However, little activity was seen when subjects performed trunk curls from the crunch position. During straight-leg raising, both muscles were active when the ipsilateral leg was lifted; both were inactive when the contralateral leg lifted (table 3.1).
Abdominal Muscles The abdominal muscle group consists of four muscles, divided into two groups. The deep (anterolateral) abdominals are transversus abdominis and internal oblique; the superficial (front) abdominals are the rectus abdominis and external oblique.
Anatomy of the Superficial Abdominals The rectus abdominis (figure 3.9) is positioned vertically at the front of the abdomen. It attaches from the symphasis pubis and pubic crest and runs to the xiphoid process and 5/6/7th ribs, being broader superiorly. The lateral border (semilunaris) can be seen in lean subjects, as can the central separation between the two muscles, the linea alba. Of the three
~ ,.
56 .")f ck Stability
. f
"
.'0;
.!~
""15,,
.}''i
e 3.1
Psoas and Iliacus Activity Measured on EMG
s a Percentage
.
0 f Maximum
Starting position Single-leg standing Same. leg flexion (90") Opposite-leg extension (30") Same-leg abduction Standing Standing with trunk flexed to 300
Psoas %
Iliacus %
0 99
0 99
0
26
36 0
S6 0
0
0
Standing opposite hand loaded Sitting with straight back
11 9
0 4
Relaxed sitting Sitting, hyperlordosis and pelvic tilt
0 17
0 22
Sit-up, straight legs
52
42
Sit-up, legs 4S0 to floor
88
60
Trunk curl, legs straight
0
0
4 59
0 58
Trunk curl, legs 900 (end range) Straight-leg. raising (bilateral) Data from Andersson et al. 1995.
noticeable tendinous intersections of this muscle, one is level with the umbilicus, one is level with the xiphoid, and one is midway between the two. Each rectus muscle is enclosed within a fibrous sheath (the rectus sheath) formed from the aponeuroses of the internal and external oblique muscles and of the transversus abdominis. These aponeuroses join centrally to form the linea alba. The rectus sheath changes at a level midway between the pubic symphasis and the umbilicus. In the upper area of the muscle, above this point, the aponeurosis of internal oblique splits into two, one part passing behind the rectus and the other in front. The aponeurosis of transversus abdominis fuses with the posterior portion of the sheath, while the aponeurosis of external oblique fuses with the anterior sheath. In the lower portion of the muscle (below the midpoint between the pubis and umbilicus), the oblique abdominal and transversus abdominis aponeuroses pass in front of the rectus, and as a result the rectus is less visible in this region (Palastanga et al. 1994). The external oblique (figure 3.9) is positioned on the anterolateral aspect of the abdomen, with its fibers running downward and medially. It attaches from the outer borders of the lower eight ribs (and their costal cartilages) and then passes toward the midline. The muscle interdigitates
Stabilization Mechanisms in the Lumbar Spine'
Serratus muscle
Rectus
57
anterior
sheath
Linea alba
External oblique muscle (cut away)
Inguinal
Figure
ligament
3.9 Muscles of the abdomen
I (intermediate
dissection).
with the serratus anterior (above) and latissimus dorsi (below). The lateral fibers are almost vertical and attach to the iliac crest, while the medial fibers attach into the rectus sheath. The lower border of the muscle aponeurosis passes between the pubic tubercle and the anterior superior iliac spine to form the inguinal ligament. Anatomy of the Deep Abdominals The internal oblique (figure 3.9) is deep to the external oblique and attaches from the lateral two-thirds of the inguinal ligament and the anterior two-thirds of the iliac crest. It also takes attachment from the thoracolumbar fascia. The fibers fan outward and upward (the posterior fibers being almost vertical) to attach to the inferior borders of the lower four ribs. The anterior fibers pass medially to help form the rectus sheath (figure 3.10). The portion of the muscle that attaches to the inguinal ligament joins its neighboring fibers from transversus abdominis to form the conjoint tendon. The transversus abdominis (figure 3.10) is the deepest of the sheet-like abdominal muscles and attaches from the lateral third of the inguinalligament and the anterior two-thirds of the inner lip of the iliac crest (Palastanga et aI. 1994). In addition, it has an attachment from the thoracolumbar fascia (where it merges with internal oblique to form the lateral raphe) and
58
.
Back Stability
Anterior layer of rectus sheath
Transversus
abdominis muscle
(cut)
Transversalis
fascia
Figure
3.10
Muscles
of the abdomen
II (deep
dissection).
from the lower six ribs, where it interdigitates with the diaphragm. Its fibers pass horizontally to merge into the rectus sheath (figure 3.11), with the lower fibers attaching to the inguinal ligament and merging with the fibers of the internal oblique to form the conjoint tendon. The lower part of the transversus abdominis forms into the transversalis fascia in which lies the deep inguinal ring. Functions of the Abdominals The rectus abdominis and lateral fibers of external oblique are the prime movers of trunk flexion; the internal oblique and transversus abdominis are the major stabilizers (Miller and Medeiros 1987). The rectus and external oblique are superficial muscles that often dominate trunk actions. The transversus and internal oblique are more deeply placed, and patients often are unable to contract them voluntarily. The rectus abdominis flexes the trunk by approximating the pelvis and rib cage. EMG investigation has shown that trunk flexion emphasizes the supraumbilical portion, whereas posterior pelvic tilt shows greater activity in the infra umbilical portion (Guimaraes et a1.
Stabilization Mechanisms in the Lumbar Spine.
59
1991; Lipetz and Cutin 1970).Abdominal hollowing activates the internal oblique and transversus muscles (Richardson Transversalis fascia Rectus abdominis muscle et al. 1992), and the transversus acts at the Figure 3.11 Cross section of the rectus sheath. initiation of movement to stabilize the trunk in overhead and lower-limb actions (Hodges and Richardson 1996). In resisted actions such as sport or lifting, the abdominal muscles essentially function to stabilize the trunk and provide a firm base of support for the arms and legs to work against. If stability is poor (in relation to total power of the subject), some of the energy of the limb actions can displace the pelvis and trunk instead of providing the desired limb movement. Compare what would happen if a baseball batter wearing sneakers were standing on ice when he connected with the ball, rather than having his feet dug into firm ground-much of the energy of the swing would be lost, and his body would twist awkwardly. In the same way, if trunk stability is poor, limb power suffers and additional stress is placed on the spinal tissues if they move to full end range. Consider an overhead lifting action performed with an unstable spine (figure 3.12, a and b): if the pelvis tilts forward, lumbar lordosis increases and the abdominal muscles overstretch as the lumbar spine moves into full extension (see page 34). In this case, what trunk stability is present comes from facet joint approximation and elastic recoil of noncontractile tissues (passive stability) rather than from muscle action (active stability) (see
Skin
a
b
Figure 3.12 Trunk stability in overhead lifting: (a) active stability of the trunk through tight abdominals and level pelvis. re-
sulting in reduced stress on lumI I
~
L\
bar tissues; (b) passive stability of the trunk through lax abdominals and tilted pelvis, resulting in increased stress on lumbar tissues. From C. Norris, 199B, Diagnosis and management, 2d ed. (Oxford: Butterworth Heinemann), 175. Reprinted by permission of Butterworth Heinemann Publishers, a division of Reed Educational & Professional Publishing Ltd.
60
.
Back Stability
page 30). The fundamental key to safe and effective abdominal training in sport is to train for trunk stability before training for trunk muscle performance. In this way, the exercises are performed on a spine made stable by muscle rather than placing excessive stress on spinal joints before muscle stability has had time to build up. KEY POINT: -stability
forriiS1he -foundation o(ili"irunkexercise. Individuals should train for trunk stability before [ !,!:a,!!1ing for muscle perform~nce. _
Patterns of Coordination Among the Abdominals During Spinal Movement In terms of spinal stabilization, the contraction speed of the abdomina Is is more critical than their strength when they react to a force tending to displace the lumbar spine (Saal and SaaI1989). Moreover, the ability of a patient to dissociate deep abdominal function from that of the superficial abdominals is important, and the key to lumbar stabilization appears to be the ratio rather than the intensity of muscle activity. Abdominal hollowing (rather than a sit-up movement) works the transversus abdominis and internal oblique (not the rectus abdominis and the external oblique) (Richardson et aI. 1992). Patients with chronic low back pain (CLBP) are poorer at using the internal oblique than the rectus abdominis and external oblique, reflecting a shift in the pattern of motor activity (O'Sullivan et aI. 1997).As CLBP patients attempt an abdominal hollowing action, they tend to substitute the superficial muscles that override the deep abdominals. When expressed as a ratio of internal oblique over rectus abdominis (IO/RA), the value from the control group (non-LBP) was 8.74 while the CLBP group had a ratio of only 2.41-indicating a much larger proportional contribution to hollowing by the internal oblique in the control group (figure 3.13). Pain inhibition in
(!)
ero
.
0.9 0.8
o Internal
0.7
~ WI/)5- 0.6 Q) c:
0.5
m
0.4
g
'§!:
C/)~
Rectus abdominis oblique
0.3 0.2 0.1
o
Control
CLBP
Figure 3.13 Abdominal muscle activation in chronic low back pain (CLBP). Data from O'Sullivan et al. 1997.
Stabilization Mechanisms in the Lumbar Spine
.
61
the subjects with CLBPmay have led to altered muscle recruitment and compensatory strategies (O'Sullivan et al. 1997). EMG measurements of trunk muscles have shown that the muscles do not simply work as prime movers of the spine but show antagonistic activity during various movements. The oblique abdomina Is are more active than predicted, to help stabilize the trunk. In a study by Zetterberg et al. (1987), subjects' abdominal muscle activities during maximum trunk extension ranged from 32% to 68% of their longissimus activities. As would be expected, the ipsilateral muscles showed maximum activity in resisted lateral flexion-but the contralateral muscles were also active at about 1020% of the maximum values. The coordinated patterns among the abdominal muscles are taskspecific. But the only muscle that is active in all patterns is the transversus abdominis. During maximum voluntary isometric trunk extension, transversus abdominis is the only one of the abdominal muscles to show marked activity. It is also the muscle most consistently related to changes in intra-abdominal pressure (lAP) (Cresswell et al. 1992). The transversus abdominis not only contracts whenever the trunk moves in any direction-its activity always precedes the contraction of the other trunk muscles in the normal (non-LBP) subject (Cresswell et al. 1994). Transversus abdominis is the only abdominal muscle to be active in trunk movements in all directions. Its activity always precedes that of the other abdominal muscles in normal subjects.
KEY POINT:
When people engage in repeated movements, their bodies anticipate the predictable load and the muscles brace themselves accordingly. Using fine wire electrodes, Hodges and Richardson (1996) assessed abdominal muscle action during 10 repetitions of shoulder flexion, extension, and abduction. They found that transversus abdominis contracted before the shoulder muscles by as much as 38.9 milliseconds. The reaction time for the deltoid was on average 188 msec, with the abdominal muscles (except transversus) following the deltoid contraction by 9.84 msec. With subjects who had a history of low back pain, however, the contraction of the transversus failed to precede that of the deltoid, indicating that the subjects had lost the anticipatory nature of stability (figure 3.14). These highly significant data reveal a uniform dysfunction in the motor control of transversus abdominis in people with low back painthe problem is not simply one of muscle strength. It appears that the anticipatory nature of transversus may be lost in those with low back pain, leaving open the possibility that this mechanism may be redeveloped therapeutically.
62
.
Back Stability Controls
Subjects
with back pain
150
~
(!) en 100 ::E5LJ.J"' 50
~f,j ~ ~
~8.:.
0
-50
-100 -150
. D
o
Flexion Abduction Extension
Figure 3.14 Activity of transversus abdominis muscle during shoulder movements. Note that subjects with back pain had a longer transversus reaction time. Point 0 represents the onset of shoulder movement.
Patients With chronic low back pain exhibit a motor control deficit (alteration in muscle reaction timing and anticipatory bracing) in the transversus abdominis.
KEY POINT:
A number of authors have highlighted contraction of the abdominal muscles before the initiation of limb movement as an example of a feedforward postural reaction (Friedli et al. 1984; Aruin and Latach 1995). In these cases, as would be expected, the erector spinae and the external oblique contract before arm flexion, while the rectus abdominis contracts before arm extension. In each case, the trunk muscles act to limit the reactive body movement toward the moving limb. Contraction of the transversus before the other abdominal muscle has been described by Cresswell et al. (1994) in response to trunk movements, but anticipatory contraction during limb movements is a newer finding. The transversus abdominis seems to be contracting during posture not simply to bring the body back closer to the posture line but to increase the stiffness of the lumbar region and enhance stability (Hodges et al. 1996).
INTRA.ABDOMINAL
PRESSURE MECHANISM
Intra-abdominal pressure (lAP) is sometimes described as intratruncal pressure (Watkins 1999), although the latter term includes both intra-abdominal and intrathoracic pressure. Intrathoracic pressure is created during inspiration by expanding the lungs within the ribcage to coincide with a lift or other effort. Although intrathoracic pressure can be useful in competitive sport, I do not emphasize it within this text because the rather complex coordination between it and abdominal hollowing (described later) makes
Stabilization Mechanisms in the Lumbar Spine
.
63
it unsuitable for most rehabilitation programs. Timing inspiration with effort, moreover, can lead to use of the Valsalva maneuver where the breath is held to maintain increased intrathoracic pressure. If done during exercise, the Valsalva can raise blood pressure to dangerous levels (Linsenbardt et al. 1992), an inappropriate situation given the poor health status of many individuals with back pain. lAP involves synchronous contraction of the abdominal muscles, the diaphragm, and the muscles of the pelvic floor. The deep abdominals (transversus abdominis and internal oblique) are the more important of the abdominal muscle groups in this respect since they are visceral compressors rather than flexors. Although they have no name for it, most people experience lAP in everyday life-as, for example, when the muscles contract reflexively to defend the abdomen from a direct blow. The theoretical basis for the lAP mechanism is that pressure within the abdomen, acting against the pelvis and diaphragm, provides additional extensor torque to the spine (figure 3.15)-moreover, the "inflated balloon" acts on a torque arm that is as much as three times greater than that of the erector spinae. Intra-abdominal pressure is created by synchronous contraction of the abdominal muscles, the diaphragm, and th~_muscles of the pelvic floor.
KEY POINT:
j
Contraction of the transversus abdominis and the internal oblique increases lAP, providing the glottis is closed. Imagine the trunk as a cylinder. The top of the cylinder is formed by the diaphragm, the bottom the pelvic floor, and the walls the deep abdominals (transversus and internal oblique). As the abdominal wall is pulled in and up, the walls of the cylinder are effectively pulled in. If a deep breath is taken, the diaphragm is lowered, compressing the cylinder from the top. Providing the pelvic floor (the bottom of the cylinder) is intact, the cylinder is "pressurized" and made more solid. In this way, it is able to resist any bending stress applied to it. The lAP is greater if the breath is held following a deep inspiration (Valsalva maneuver) as the diaphragm is lower and the comparative size of the abdominal cavity (the cylinder) is reduced. During Figure 3.15 Intra-abdominal pressure mechanism. Pressure within the abdomen acting against the pelvis and diaphragm provides additional extensor torque to the spine.
64
.
Back Stability
lifting, the pelvic floor muscles (the floor of the cylinder) contract to maintain pelvic integrity and prevent urination. The Valsalva maneuver is therefore appropriate in heavy lifting as long as it occurs only briefly. It must be borne in mind, however, that the blood pressure changes may not be desirable in subjects with poor cardiopulmonary health. Heavy lifting for this group is, therefore, not recommended. Making the trunk into a more solid cylinder reduces axial compression and shear loads and transmits loads over a wider area (Twomey and Taylor 1987). lAP may also help to protect the spine from excessive indirect loads (those not acting directly on the spine but through limb loading), with the muscles acting to involuntarily fix the rib cage. lAP is greater when heavy lifts are performed and when the lift is rapid (Davis and Troup 1964). Abdominal muscle strength affects lAP-strong athletes can produce very large lAP values (Harman et al. 1988). Yet strengthening the abdominal muscles with movements such as sit-ups does not permanently increase lAP (Hemborg et al. 1983)since these exercises usually do not mimic the coordination among abdominal muscles that is inherent in the lAP mechanism (Oliver and Middleditch 1991). Investigating the effect of abdominal muscle training on lAp, Hemborg et al. (1985)used isometric trunk curl and twist exercises. Increased recruitment of motor units in the oblique abdominal muscles clearly demonstrated muscle strengtheningyet EMG activity of these muscles decreased during lifting, implying that the subjects did not make functional use of their increased ability to recruit more motor units. The differentiation between increased strength and functional ability is an important one. If an exercise is not specific to a task being carried out, the physiological adaptation of the musculoskeletal system may be inappropriate. See page 99 for more discussion of training specificity. KEY POINT: -sit-'up exercises 'Willnot permanentlyraise intra-
.
abdominal pressure. A number of important criticisms has been made against the lAP mechanism when it has been presented as the only stabilizing process for the spine (Bogduk and Twomey 1987). First, to fully stabilize the spine during the lifting of heavy weights, the lAP would have to exceed the systolic pressure within the aorta, effectively cutting off the blood flow to the viscera and lower limbs. Competitive weight lifters have been known to black out when lifting extremely heavy weight, perhaps because of very high lAP (McGill et al. 1990).At the onset of a lift, there is an initial rapid rise in lAP-known as the snatch pressure-that may last for less than 0.5 second. The pressure declines during the remainder of the lift. Hemborg et al. (1985) calculated that a peak lAP of 250 mm Hg would be required to
Stabilization Mechanisms in the Lumbar Spine.
65
lift a 100-kg weight. Second, the muscle force required to create a sufficiently high lAP is greater than the hoop pressure possible from the abdominal muscles (Gracovetsky et al. 1985). Third, if the rectus abdominis contracts to increase lAP, it produces a flexion torque that counteracts the antiflexion effect of lAP created as the diaphragm and pelvic floor spread apart. These criticisms of lAP have led to reexamination of its contribution to back stability. Originally, lAP was believed to reduce the compression acting on the lumbar spine by as much as 40% (Eie 1966), but more recent studies have shown this to be only 7% (McGill et al. 1990). Inira-abdominal pressure has been estimated to reduce the compression acting on the lumbar spine by only 7%.
KEY POINT:
Bogduk and Twomey (1991) have considered a further effect of lAP in controlling axial rotation while lifting. Most mathematical models describe lifting in the sagittal plane only. From the functional standpoint, however, lifting is a multi plane activity, requiring stability to rotation as well as flexion-extension. If the internal and external obliques contract to control rotation, lAP may increase as a secondary effect.
SUMMARY
· · ·
The human spine is inherently unstable without its musculature. The interspinous and supraspinous ligaments, facet joint capsules, and thoracolumbar fascia (TLF) together provide passive support for the spine sufficient to balance between 24% and 55% of imposed flexion stress.
·
The posterior ligamentous through elastic recoil.
the spine passively
and
The TLF stabilizes the spine through three primary mechanisms: (1) passive resistance through its connections with the transversus abdominis muscle; (2) hydraulic amplification, as it restricts expansion of the erector spinae; and (3) "form closure" and "force closure" of the sacroiliac joint.
· · .
system stabilizes
Of the deep intersegmental muscles, the for stabilizing the spine by helping neutralizing spinal flexion. Following therapy is required to restore multifidus
multifidus is most important to control lordosis and for lower-back injury, exercise function.
Of the superficial back muscles, the erector spinae are most significant for back stabilization. It is their endurance rather than their strength that is particularly important. Of the abdominal muscles, the internal oblique and transversus abdominis are the major back stabilizers rather than the more
. Back Stability
66
·
·
superficial external oblique and rectus abdominis. The ratio in which these muscles are used is more important that mere muscle strength. The key to effective abdominal training in sport is to train for trunk stability before training for trunk muscle performance. Individuals with low back pain tend to favor the more external abdominal muscles. Abdominal hollowing (rather than sit-ups), however, activates the internal oblique and transversus muscles-and since an important aim of rehabilitation is to help patients learn to dissociate use of the deeper muscles from use of the more superficial muscles, learning to practice abdominal hollowing is a vital part of rehabilitation.
PART
ITIT
Exercises for Establishing Stabititt Chapter 4 ("Teaching Your Clients the Basic Skills") is probably the most important chapter in this book. If you do no more than help your back pain clients to master all the movements in that chapter, you may well help them more than they would have been by a lifetime of standard weight training, exercises, massages, manipulations, etc. But teaching your clients pelvic tilt, abdominal hollowing, how to assume the neutral lumbar position, and how to contract the multifidus (the essence of chapter 4) is just the beginning. The skills described in chapter 4 get your clients to the point where you can proceed with the rest of their treatment plans. You will want to identify and correct muscle imbalance as it is the source of much back pain and instability. Chapter 5 ("Muscle Imbalance") tells you how to diagnose imbalance and how to correct it. Chapter 6 ("Basic Abdominal Muscle Training") shows you how to teach your clients to train the abdominal muscles that most strongly affect low back pain-and these are not just the muscles that some therapists target when they assign "ab workouts" in order to deal with back problems. Your clients can do abdominal crunches until they have the most beautiful "six pack" on Malibu Beach and still be wracked with back pain. I show you how to target all the important structures (and they are not all muscles-you need to help your clients train their neurological responses as well!). In chapter 7 ("Posture"), I show you how to determine if your clients have less-than-ideal posture and how to correct the different kinds of abnormal posture that can be a major factor in low back pain.
67
4 Teaching Your Clients the Basic SkiDs Before your clients can follow rigorously the programs and practices discussed later in this book, they must have certain fundamental abilities. This chapter will help you understand how to teach your clients these skills. Muscle action can stabilize the trunk effectively only if the trunk is a solid cylinder. In chapter 3, we saw that the deep (lateral) abdominal muscles (transversus abdominis and internal oblique) were the most important of the abdominal group for achieving this aim, whereas the multifidus is the most important of the back muscles. Our initial aim is to reeducate these muscles to gain voluntary control over their actions.
-
KEY POINT: The back stability program begins with muscle reeducation. Before proceeding to the exercises described in later chapters, your clients should be able to control pelvic tilt; to identify and assume the neutral position of the lumbar
spine; to perform abdominal hollowing; and to voluntarily I contract the multifidus muscle.
1 I
I
Once your clients have achieved voluntary control, they are more able to use the muscles with minimal effort-the aim in all these exercises is for contraction intensities of only 30-40% of maximum, which can be easily sustained. Your clients must then learn to build the endurance of the muscles, aiming to perform 10 repetitions and hold each for 10 seconds. They also must learn to recognize the neutral position of the lumbar spine, to detect when the lumbar spine has moved away from this neutral position, and to correct the position of the lumbar spine using a pelvic tilting action.
69
.
70
Back Stability
TEACHING YOUR CLIENTS TO CONTROL PELVIC TILT If you determine that your clients' lumbar-pelvic alignment is incorrect, you will need to teach them how to tilt and hold their pelvises in order to correct the misalignment. As you begin treatment, remember that for some, touching may be a sensitive issue. Be alert for words or body language that indicate tension in your client. Before you touch the client, explain clearly what you are going to do and be sure that she is comfortable with the proposed action. If not, try a different approach. With extra-sensitive clients, by proceeding gradually, you can usually establish the trust necessary to pursue the most helpful therapeutic course. Always bear in mind that therapist-client trust is an essential ingredient for successful treatment; do everything you can to establish and maintain that trust.
Segmental Control The ability to dissociate the movement of one body segment from that of a neighboring segment is dependent on stabilization ability and adequate muscle length. The central requirement of segmental control as it applies to back stability is that the pelvis be able to tilt independently of the lumbar spine in both frontal and sagittal planes. The combination of movements of the hip on the pelvis and of the lumbar spine on the pelvis increases the range of motion of this body area. The relationship between lumbar and pelvic movement is called lumbar-pelvic rhythm (see page 34). During forward flexion in standing, when the legs are straight, movement of the pelvis on the hip is limited to about 90° hip flexion. Any further movement, allowing the subject to touch the ground, must occur at the lumbar spine. For lumbar-pelvic rhythm to function correctly, movement of the pelvis on the hip should be equal to or greater than movement of the lumbar spine on the pelvis. In people with a history of back pain, however, the ability to perform pelvic tilting (pelvis moving on hip) is often lost-almost all the movement during forward bending comes from the lumbar spine, which shows excessive flexion laxity but limited, or often blocked, extension. In the lower trunk, the ability to dissociate lumbar movement from pelvic movement is therefore important, and correction of faulty lumbar-pelvic rhythm is vital. KEY POINT: ThecibTlitYto-dissociatemovementof'tnefumDar
't
spine from movement of the pelvis is essential for the healthy functioning of the back.
1
-----
Your Clients the Basic Skills.
Teaching
71
Assessing Lumbar.Pelvic Dissociation You can use a variety of exercises to assess lumbar-pelvic rhythm; you may subsequently use the same exercises as part of the rehabilitation process. There is no stated "goal" for each of the following exercises because they all have basically the same goal: to allow you to assess your clients' abilities to dissociate lumbar from pelvic movement.
Knee Raising in Standing The subject stands at a right angle to a wall bar for support, flexing his hip beyond 90° by raising his thigh to his chest and allowing his knee to bend. The movement should ideally occur in three phases. Initially there should be no pelvic or lumbar movement, with phase I consisting of hip flexion alone (a). During phase II, the pelvis should begin to posteriorly tilt as the hip approaches 90°. The lordosis should flatten, but the lumbar spine movement should not be excessive (b). In phase III, no further hip or pelvic movement is available, and the final position is obtained by lumbar flexion alone (c). When control of lumbar-pelvic rhythm is poor, lumbar flexion and pelvic rotation often occur early in phase I, with thoracic movement noticeable as the subject dips his chest downward toward the knee (d).
~
,. ,,
a
c
,
When lumbar flexion occurs early in the movement, the action of knee raising in standing can be used as a stability exercise in itself. Instruct your client to raise his knee initially by performing 10-20° hip flexion while maintaining stability of the lumbar-pelvic region and avoiding any pelvic tilt. To progress the overload of the exercise, increase the range of hip motion to 30-45° and slow the action so that the knee raise takes a total of 10seconds.
..-.
72
.
Back Stability
Passive
Assessment
of Pelvic
Tilt
While your client is standing, grip her below the waist with your forearm placed around the pelvic rim. Place your other hand flat on the sacrum, and use your shoulder to stabilize her thoracic spine. Move your client's pelvis into anterior and then into posterior tilt, assessing how far you can move it in either direction. If your client demonstrates a flatback posture, the amount of anterior tilt will be reduced; if she demonstrates a lordotic posture, the corresponding amount of posterior tilt will be limited.
Assessing
Lumbar-Pelvic
Rhythm
in Prone
Kneeling
The subject sits back toward his ankles. Again, the action should occur in three phases. In phase I, no lumbar or pelvic movement should occur (a); in phase II, posterior pelvic tilt and hip flexion occur (b); and in phase III, lumbar flexion and some thoracic flexion finish the action (c). Faulty lumbar-pelvic rhythm often shows up immediately when lumbar flexion and posterior pelvic tilt occur immediately (d). ._
o ~
~, .~ ~
o
t
...
'-:'" 0
a
The Hip Hinge Movement
.._ ,~ -- I. .
'..
~:
.-"..-,
t
Io I
C
~ .
d:
.._...... I0
I
I
in Standing
This activity permits you to observe your client's ability to isolate pelvic motion from that of the lumbar spine in the more functional position of standing. Your first aim is to assess the client's forward flexion since the relative contribution of anterior pelvic tilt to this movement is important. With normal lumbar-pelvic rhythm, unlocked knees and anterior pelvic tilt reduce the amount of lumbar flexion required to reach downward to below waist height, as when continued
Teaching Your Clients the Basic Skills.
73
The Hip Hinge Movement in Standing, continued standing and working at a low bench (a). Where pelvic tilt is limited, greater lumbar flexion is required. Throughout the day, the number of lumbar flexion movements is greatly increased, leading to accumulated stress on the body tissues in this area (b).
Assessing
Pelvic Motion Control
in the Frontal Plane: The Trendelenburg
Sign
When one leg supports all the body weight, the hip abLax ductors (mainly gluteus meabductor dius) of the supporting leg muscles....... work to prevent the pelvis Tight from dipping (a). When these adductor muscles muscles are unable to hold an inner-range contraction, a b the pelvis dips downward toward the lifted leg, effectively adducting the weightbearing limb (b). Persistent use of this action in the swayback posture can lead to an imbalance, combining lengthening of the hip abductors and shortening of the hip adductors.
Recognizing
False Hip Abduction
In a nonweightbearing situation, inactivity of the gluteus medius shows as a false hip abduction movement. Normally when the upper leg is lifted from side lying, the pelvis remains level and the hip moves on this stable base (a). When the hip abductors are weak, the subject is unable to abduct the leg correctly (b).
continued
74
.
Back Stability
Recognizing False Hip Abduction, continued
Instead, his pelvis tilts laterally on the spine using the trunk side flexors, which give the false appearance of hip abduction. Although the leg lifts, the relationship between the femur and pelvis remains unchanged, with close inspection showing the movement isolated to the lower spine.
Regaining Correct Lumbar.Pelvic Rhythm The restoration of correct lumbar-pelvic rhythm is essential for the correct functioning of this region. Rehabilitation of this mechanism begins with your client recognizing the action of pelvic tilt and being able to maintain the neutral lumbar spine. Control of lumbar-pelvic rhythm is used extensively during static loading of the stabilizing system covered in chapter 8 and during the rehabilitation of lifting in chapter 9. The following exercises will help your client gain the essential control of pelvic tilt that is necessary for basic back stability. The last two exercises use a gym ball and will prepare your client for the more advanced gym ball exercises described in chapter 9. The pelvic tilt mechanism-is an important key-to movements of the lumbar-pelvic region.
KEY POINT:
Assisted
Pelvic Tilting While Standing
.1'{t1~,.. For subjects
who are unable to initiate a pelvic tilt.
Promote passive movement while your clients are standing by gripping around their pelvic rim and supporting their sacrum with the flat of your opposite hand (as in "Passive Assessment of Pelvic Tilt," page 72). Push the pelvis into anterior tilt and then into posterior tilt, and have your clients attempt to return to the neutral position each time (i.e., to reproduce the passive motion) in order to enhance proprioceptive input to this area.
Teaching
Assisted .f['7~'.
Your Clients the Basic Skills.
75
Pelvic Tilt While Sitting
For subjects who are currently unable to perform a pelvic tilt while sitting. The action is especially useful for individuals whose flatback posture causes pain after prolonged sitting.
Stand in front of your client and place a webbing belt around her waist. Gripping the belt, place your hand over her sternum to prevent upper body sway. As you pull the belt, her lumbar lordosis increases and her pelvis tends to tilt anteriorly. This action is made easier if your client sits on a wedge-in this case, the ischial tuberosities are higher than the pubic bone, and the pelvis is forced into anterior tilt. Initially, most of the power comes from your pulling on the belt, but gradually the belt provides less and less assistance as the subject becomes able to perform the tilting action by herself.
Assisted .f['H.
Pelvic Tilt From Crook Lying Position
For subjects who are unable to perform a full active tilt by themselves in any position.
The subject begins in the crook lying position, as for the heel slide maneuver on page 106. Grip his pelvis over the pelvic rim on each side, and push the pelvis into anterior and then posterior tilt. Encourage your subject to visualize the effect of the tilt on the lumbar spine as the lordosis is increased and reduced. Have him attempt first to follow the action using his own musculature (abdominals and gluteals), then gradually reduce your force in tilting the pelvis until he is performing the action independently. Once your client can perform the action regularly in crook lying, he should attempt the same movements in the standing position. Begin with passive control (you provide the force for movement), then have your client gradually assume active control. Eventually have him perform pelvic tilting in a variety of starting positions including 4-point kneeling, 2-point kneeling, sitting, and supine lying. In each case the action of pelvic tilt is important, and the ability to reproduce the neutral lumbar position is essential.
continued
76
.
Back Stability
Assisted Pelvic Tilt From Crook Lying Position, continued
Hip Hinge Action in High (2-Point) Kneeling (Assisted) .1'Ie1~'. Uses a pelvic tilt action to move the spine forward and backward. Once your subject can perform pelvic tilting well, she should combine it with classic "hip hinge" actions-where the trunk moves on the hip in a hinge action, and the spine remains straight. With your client in the 2-point kneeling position, assist her in performing the pelvic tilt. Encourage her to follow this movement with her shoulders, keeping her spine stable and avoiding any increase or decrease in lumbar lordosis. She should gently draw her abdominal muscles in (hollowing, see page 85) and maintain this minimal contraction (a feeling of "tightness" only) throughout the movement. The essence of this action is to angle the spine forward and backward from the hip without flexing or extending the spine. The movement is made easier if the subject visualizes a rod tipping forward and backward from a single point (the hip) rather than a rope bending. You should provide gentle pressure on the back of your client's shoulders to initiate forward angulation of the spine and pressure over the front of the shoulder to initiate backward angulation. In each case, the spine remains straight, and the action comes from the spine (acting as a single unit) moving on the hip through pelvic tilting.
Teaching Your Clients the Basic Skills
.
77
Hip Hinge (Table Support) .f{"~,,, A progression on assisted hip hinge. The subject stands facing a couch or other object placed just below waist level, with his hands on the couch surface (a). With his knees unlocked to relax the hamstring muscles, he performs the hip hinge action described in the previous exercise, using pelvic tilt and a fully stable spine. As he leans forward, he supports some of his weight with his hands, thus reducing spinal loading. After your client has mastered this supported action, he should move to the free standing position (b).
Controlled .f{"~,,,
Forward Bending
Teaches segmental control of the lumbar-pelvic region as a precursor to lifting.
Once an individual has mastered the hip hinge actions, permit him a small degree of lumbar flexion-have him perform normal forward bend actions, with the pelvis initiating the action and both the pelvis and lumbar spine contributing equally throughout the first half of the range of motion.
Sitting Pelvic Tilt Using Gym Ball .f{"~'"
Teaches anterior-posterior
pelvic tilt control.
See chapter 9 for more thorough discussion of gym ball exercises and for more advanced exercises. The ball used is a standard 65-cm ball. Instruct your client to sit on the ball with her knees apart, feet flat on the floor. Both hips and knees should be flexed to about 90°. She should then tilt her pelvis alternately in both anterior and posterior directions, making sure that her shoulders and thoracic spine remain inactive. At first, she should attempt only small
continued
78
.
Back Stability
Sitting Pelvic Tilt Using Gym Ball. continued
ranges of movement; as she gradually works up to larger ranges, the ball should roll forward and backward slightly.
Sitting Lateral Tilt Using Gym Ball .1'111.'1. Teaches lateral pelvic tilt control.
Instruct your client to sit on the ball, as in the previous exercise, and to use lateral tilting to roll the ball from side to side, transferring the body weight from one ischial tuberosity to the other. Again, the shoulders should remain still throughout the action. The aim is to control the movement throughout the range using a smooth action and to avoid "falling into" the end-range position.
TEACHING YOUR CLIENTS TO IDENTIFY AND ASSUME THE NEUTRAL POSITION Teaching clients to identify and maintain the neutral position of their lumbar spines is important for each stage of the back stability program since the neutral position places minimal stress on body tissues. Lumbar neutral position is midway between full flexion and full extension as brought about by posterior and anterior tilting of the pelvis. The discs and facet joints are minimally loaded in this position, and the soft tissues surrounding the lumbar spine are in elastic equilibrium. Because postural alignment is optimal in this position, it is generally the most effective position from which trunk muscles can work. In the normal (nonpathological) person, the neutral position corresponds to lumbar alignment in an optimal posture. Individuals with suboptimal posture may increase or reduce their pelvic tilt, causing corresponding changes in the depth of lumbar lordosis. In either case, the neutral position remains midway between end-range flexion and end-range extension-in cases of postural malalignment, however, part of the treatment aim is to restore optimal posture by rebalancing the length of the surrounding soft tissueelements.Subjects can find neutral position passively (as you move the pelvis) or actively (subject moves her own pelvis through muscle action). Refer to "Optimal Posture Alignment" in chapter 7 (page 134) for more thorough treatment of the neutral position while standing. In kneeling,
Teaching
Your Clients the Basic Skills
.
79
your subject attempts similar lumbar alignment by slightly hollowing the lumbar spine. A flatback or excessive lordosis both mean that the subject has moved away from the neutral position and will need to reposition by tilting the pelvis. With time, your clients will be able to recognize the neutral position and maintain it as appropriate. In the early stages of the program, however, you will need to constantly remind them of their spinal alignment. Proprioceptive exercises will help your client learn to assume neutral position at will.
Proprioception-Basic
Concepts
Because proprioception is vital to the process of back stability during later stages of rehabilitation (Norris 1998), your clients should begin appropriate proprioceptive exercises at the start of their treatment programs. Lephart and Fu (1995) define proprioception as a specialized variation of touch encompassing the sensations of both joint movement and joint position. During acute injury, the reflexes initiated by displacement of mechanoreceptors and muscle spindles occurs far more rapidly than that brought about by pain (nociception) (Barrack and Skinner 1990). Effusion (escape of fluid) from joints contributes to a reduction in mechanoreceptor discharge, resulting in inhibition of muscular contraction. This inhibition commonly occurs in the vastus medialis (VMO) of the knee, for example, where just 60 ml of intra-articular effusion may result in 30-50% inhibition of quadriceps contraction (Kennedy et a1. 1982). Proprioceptive deficits parallel joint degeneration (Barrett et a1.1991),but it is unclear whether this is a cause or a result of degeneration (Lephart and Fu 1995). Proprioceptive exercise is useful from the early stages of rehabilitation to restore normal functioning of the proprioceptive control of the back. And it is nowhere more useful than in helping your clients master assuming neutral position. From a clinical standpoint, proprioception consists of three interrelating components (Beard et a1. 1994) that represent activity at spinal, brain stem, and higher centers (Tyldesley and Grieve 1989)(table 4.1). Individuals
Table 4.1
Components
of Proprioception
Level of neural system
Component
of proprioception
controlled
Spinal Brain stem Higher
Regulates muscle stiffness Controls static joint positioning Controls kinesthesia (movement sense)
80
.
Back Stability
beginning back stability training should focus on brain stem activities, characterized especially by static joint positioning, for they must cultivate this ability before proceeding to more advanced training.
Static Joint Positioning Static joint position sense helps to maintain posture and balance at the brain stem level. Input for these actions is from joint proprioception, from the vestibular centers in the ears, and from the eyes. Balance and postural exercise with the eyes open or closed can enhance static joint position sense. Reproduction of passive positioning (RPP) and reproduction of active positioning (RAP) are exercises in which an individual tries to place a joint back in its starting position after either active or passive movement.
Reproduction .1'I'l'1.
of Passive
Positioning
To teach individuals how to maintain neutral position improving the accuracy of body segment position.
by
Four-point kneeling is the best starting position for restoring RPP during back stability training. Have your client kneel, with the lumbar spine in neutral position. After you passively move the spine away from neutral, instruct your client to place the spine back into the neutral position. Initially, you should work with single movements from flexion back to neutral and then extension back to neutral; then progress to combinations of movements-flexion-extension and lateral flexion and then back to neutral, for example. The aim is to increase the precision of movements so that the individual is able to accurately reproduce the neutral position alignment after each movement away from this starting position. After your client has mastered RPP in the 4-point kneeling position, move to other positions-especially those common to daily activities, such as sitting and standing.
Reproduction .I'IIT~'.
of Active
Positioning
To teach individuals how to maintain neutral position improving the accuracy of movement.
by
After your client has become proficient in passive positioning, he should initiate his own movements. Instruct him to begin in neutral position, move away from this position using single movements, and then move back into the neutral starting position. It sometimes works best if he continued
Teaching Your Clients the Basic Skills
.
81
Reproduction of Active Positioning, continued
begins RAP with a sitting or standing position-that way he can practice in front of a mirror, with his hands flat over his lower abdomen and sacrum to monitor pelvic tilt. Eventually, he uses no mirror and performs the movement without monitoring the action with his hands. Again, use a variety of movements from several starting positions.
performing-exercises to'improVer~'pfoauc~':, ion of passive or active positioning (RPP/RAP),your client hould focu.s=, onpreci~io.n",,,-.,,,,,;,:;,,,,;'~'''Aof movelT)~nt. . ". ;_~; ,,;ill, ~I~c-;-"ii;;",~i_ ~'!I;>"'_'i,,::': '1<--'. -;'<;['" i''':,;u,"
KEY POINT:
"'.Wnen
'
TEACHING YOUR CLIENTS TO USE ABDOMINAL HOLLOWING Individuals with low back pain must re-educate their muscles by learning to isolate the deep (lateral) abdominals from the superficial abdominals. This requires a hollowing action of the abdomen, using the internal oblique and transversus abdominis muscles (Lacote et al. 1987) rather than the traditional lumbar flexion movements (e.g., sit-ups) that emphasize the upper rectus (O'Sullivan et al. 1998). Before they can proceed with the exercises described later in this book, your clients must be able to perform abdominal hollowing well and cons-istently. Because the concept of abdominal hollowing is probably less familiar than other major points in this chapter, I shall devote a disproportionately large portion of the chapter to this discussion.
Abdominal Hollowing--General
Considerations
The basic process of abdominal hollowing is in theory simple and the same in all positions: the subject pulls the belly in and up at the navel without moving the rib cage, the pelvis, or the spine. Everything else in this section merely elaborates on that basic action and on how you can best help your clients to learn it well. In comparison with mobilizer muscles (see page 92), stability muscles are better suited to endurance (postural holding) and better recruited at low resistance levels. Contraction intensities of 30-40% of the maximum voluntary contraction (MVC) work best for the deep (lateral) abdominal muscles. Your clients initially will have little control over the intensity of their contractioris. Often they will begin with minimal contractions, then build to high intensities (60-70% MVC). This is acceptable during the early stages of learning and enables your clients to "feel the muscles working."
82
.
BackStability
They eventually must gain accurate control, however, and you should instruct your clients to master changing the intensity of contraction in all hollowing exercises. An effective way to achieve this mastery is to ask for a maximal contraction, then tell your clients to relax by half, and then half again. Once they have achieved minimal contraction, they should then build up the intensity again, in steps, to the maximum. Only when they can control hollowing with minimal muscle intensity over a period of time (10 repetitions each of 30-40% MVC, held for 10 seconds) should they progress to more advanced exercises. The position in which the movements are performed is important. Have your clients assume the neutral position of the spine whenever possibleinitially, you will need to position your client correctly (you may want to read ahead to the section on "Optimal Postural Alignment" in chapter 7 [page 134] for the optimal position while standing). If your clients are kneeling, have them try to achieve proper alignment by slightly hollowing the lumbar spine-a flatback or excessive lordosis both mean that the subject has moved away from the neutral position and should appropriately reposition by tilting the pelvis. Eventually, your clients will be able to maintain the neutral position throughout their exercises. ~-Have yo'Ur"'dierits maintain-the "ii'e'i:itralpo'Sit1'On([' ;he spine throughout all the exercises in this ch.apter. :
Abdominal Hollowing-Starting
Positions
Different individuals require different starting positions, depending on their weight, degree of injury, flexibility, and so on. Standing (wall support) and 4-point kneeling are probably the easiest positions for most people. Four-point kneeling places the fibers of the transversus abdominis muscle vertically. It thereby initiates some stretching in the transversus, making contraction of this muscle easier. The 4-point kneeling position is usually more comfortable than the other positions for people with back pain. On the other hand, 4-point kneeling requires control of structures in the spine, shoulders, and hips, whereas lying positions require control over only spinal structures. Since controlling a single body segment is considerably easier than controlling three, many people (especially those with poor body control, and especially when unsupervised) find exercises in the lying position easier to perform. Moreover, because 4-point kneeling places compression on the patellae and the wrists, individuals with pathology in these joints (such as arthritis) may need to modify the kneeling position. Modifications include (a) placing the open fist on the ground rather than the flat of the hand to reduce the wrist extension stress, (b) placing extra padding beneath the shins and leaving the patellae free,
Teaching Your Clients the Basic Skills
.
83
(c) taking the body weight on the forearms rather than the wrists, and (d) supporting the upper body with the chest on a chair in order to reduce the upper body weight transmitted to the arms and wrists. Obese subjects often have trouble performing abdominal hollowing in a kneeling position-the sheer weight of their abdominal tissue presents too large an overload for their deep abdomina Is to work against. For obese individuals, the standing (wall support) position is better: although it is usually a progression from kneeling (standing provides no stretch facilitation of the deep abdominals), obese individuals can control the action more easily. They can use their hands to palpate the abdominal wall, and the action of "pulling the tummy in" is often rather familiar in the standing position. Prone lying is not suitable for obese individuals with poor abdominal muscle tone because of the compression of excess body tissue in this position. Lean people often like the prone position, however, since it provides many sensory cues-the act of hollowing to draw the abdominal wall away from the supporting surface gives useful tactile feedback (especially if a pressure biofeedback unit is used, as described later in this chapter). You must use your own judgment to select appropriate starting positions for clients, taking into account body size, body condition, age, and pathology. Be flexible-experiment with different starting positions until your client feels comfortable with the exercise.
Abdominal .I'("~'.
Hollowing: 4-Point Kneeling
To isolate the transversus abdominis and internal oblique.
Because the transversus fibers are aligned horizontally, 4-point kneeling allows the abdominal muscles to sag, facilitating stretch. Position your client with her lumbar spine in a neutral position, her head looking at the floor, not forward, and her ears horizontally aligned to her shoulder joint. Her hip should be directly above the knee, her shoulder directly above the hand. The hands and knees are shoulder-width apart. Instruct your client to focus her attention on her navel area, and to pull that region "in and up" while breathing normally. This action dissociates activity in the internal obliques and transversus from that of the rectus abdominis (Richardson et al. 1992). The exercise is thus useful for re-educating the stabilizing function of the abdominals when the rectus abdominis has become the dominant muscle of the group.
84
.
Back Stability
Abdominal
Hollowing: Standing
.f'['1~,..A progression from 4-point kneeling, or an initial position for obese individuals or others for whom 4-point kneeling is uncomfortable. Some subjects find 4-point kneeling difficult to control and tend to round their spines as they attempt abdominal hollowing. In this case, wall-supported standing is a more appropriate starting position. Your client should stand with his feet six inches from a wall and his back against the wall, while maintaining a neutral spinal position (a). An easy way to monitor neutral position is for your client to place one hand behind his back (over the sacrum) and the other in front of the abdomen, enabling him to monitor the position of his pelvis. He can also use his front hand to feel the contraction of the abdominal muscles as he initiates hollowing and a draws the abdominal wall away from his hand. In an obese or poorly toned subject, the weight of the digestive organs will pull the abdominal wall out and down (visceral ptosis). If this occurs, position a belt below his navel (b), instructing him to contract the lateral abdominals and to pull the abdominal wall "in and up," trying to create a space between the abdomen and the belt. Since motor programming links lateral abdominal action and pelvic floor action as part of the intraabdominal pressure mechanism, pelvic floor contracb tions are also useful to aid learning of abdominal hollowing. Instruct your client to pull in the pelvic floor as though trying to stop himself from urinating. In men, the action of "lifting the penis" is also useful imagery.
Linkingabdominai hollowing w'ithpelvic floor ; contractions is a useful way to enhance learning in both males L:.n~~ales._ __
KEY POINT:
It is important that your clients be able to differentiate the abdominal hollowing action from pelvic tilting. Be careful to ensure that your clients do not flatten their backs completely against the wall as that would indicate posterior pelvic tilting through action of the rectus abdominis. Once a client has performed wall-standing abdominal hollowing cor-
Teaching Your Clients the Basic Skills.
85
rectly to repetition, have him repeat the action without wall support. There should be no movement of the spine, pelvis, or rib cage.
Abdominal
.fI"~'.
Hollowing:
For subjects
2-Point Kneeling and Sitting
who are already
able to maintain
lumbar position and control body sway.
the neutral
Two-point kneeling and sitting (stool) can help lead up to free standing, as they require greater body segment control than either lying or 4-point kneeling. This is because in both 2-point kneeling and sitting, the upper part of the trunk is unsupported, while in 4-point kneeling, the arms support the upper trunk. Individuals must be more active in controlling the upper trunk when it is unsupported, paying attention to the hollowing action as well as to the position of the lumbar spine (maintaining neutral position) and the position of their shoulders (avoiding body sway). These positions are also the starting points for the hip hinge actions described later. Have your clients pay close attention to movement of the rib cage, as well as to shoulder position, pelvic tilt, and maintenance of a neutral lordosis. Instructing your client to "sit tall" or "kneel tall" can facilitate correct alignment; this concept is also helpful in correcting whole-body posture while standing.
Abdominal .fllm.
Hollowing:
Lying
Suitable for lean individuals perform hollowing.
and those already
able to
In prone lying, abdominal hollowing pulls the abdominal wall away from the floor-a practical cue for the beginning subject. Use of a pressure
continued
86
.
Back Stability
Abdominal Hollowing: Lying, continued
biofeedback unit can be very helpful (consult a medical supply catalog). Note that the pressure biofeedback unit is useful only for assessment and not for continuing exercises. Place the bladder of the feedback unit below the navel, its lower edge in line with the anterior superior iliac spines. As your client performs hollowing, the dial of the biofeedback unit will show a decline in his body's pressure on the bladder. Once your client has mastered this action, you can link it with hip extension movements, if you wish, to provide abdominal-gluteal co-contraction. Abdominal hollowing in supine lying permits an individual to feel the muscle activity and the pelvic position; again, pressure biofeedback may be useful. Have your client assume the crook lying position, with his fingers flat against the lateral abdominals below his navel. Explain that no pelvic tilt should occur during lateral abdominal contraction-you can check this by palpating the anterior superior iliac spine. You can use pressure biofeedback to monitor the depth of the lordosis: flattening of the back (posterior pelvic tilt) shows as increasing pressure on the dial and indicates activity of the rectus abdominis; excessive hollowing shows as reduced pressure and indicates loss of stability associated with anterior pelvic tilt. As your client performs abdominal hollowing, the pressure biofeedback unit should register no more than a 5-mm Hg increase in pressure-at this level of pressure the internal oblique, the transversus abdominis, and the diaphragm are all recruited together. Higher values (up to 15 mm Hg) will not increase the recruitment of the deep abdominals but will increase the activity of both the diaphragm and the rectus abdominis (Allison et al. 1998).
Tips for Teaching Abdominal Hollowing Multisensory cues can facilitate learning (Miller and Medeiros 1987). You can provide auditory cues by giving your clients frequent feedback about their performance; to create visual cues, encourage people to look at their muscles as they function and to place a mirror on the floor/couch below the abdomen; for kinesthetic cues, encourage subjects to "feel" the particular action-for example, ask them to "feel the stomach being pulled in." Muitlsensory cueing involves increased sensory input through auditory, visual, kinesthetic, and tactile stimuli, I i~o_nlunction with v~ualization of correct e~er:ise techni~~
KEY POINT:
:
J
Tactilecues for abdominal hollowing can come from you and/ or from a belt touching your client's abdomen. The first technique involves palpation. Place the heel of your hand over the client's anterior superior iliac spine and point your fingers toward the pubic bone (figure 4.1). Your
Teaching Your Clients the Basic Skills.
87
fingertips will then fall over the retroaponeurotic triangle, which is the most superficial position of transversus abdominis (Walters and Partridge 1957).At this point the external obliqje is aponeurotic and, so, not electrically active. This point may be used for siting the electrode of a surface EMG unit. Since the muscles are sheetlike, they will flatten rather than bulge when they contract. One way to facilitate the contraction is to instruct your clients to "stop me from pushing in" as you palpate the abdominal wall. A second way Figure 4.1 Palpation of the is have them cough (visceral compression) deep abdominals-the retro- and hold the muscle contraction they feel aponeurotic triangle-to teach beneath your fingers. This "cough and abdominal hollowing. hold" procedure is also useful in conjunction with surface EMG-as the muscle contraction shows on the EMG unit, encourage the subject to maintain the contraction while breathing normally. Continue with this exercise until your client can hold the contraction for a single 3D-second repetition or for 10 repetitions of 10 seconds each. Then encourage your client to reduce the contraction intensity of the muscle to the minimum required to maintain the hollow abdomen position. Another tip for tactile cues in the 4-point kneeling position: fasten a webbing belt around your client's abdomen below the navel, with the muscles relaxed and sagging (figure 4.2). The belt should be just tight enough to touch the skin but not to pull in the muscles. Have your client hollow the abdomen, pull the muscles away from the belt, and then relax them completely to fill the belt again. Figure 4.2 Using a belt to teach abSome people may be unable to dominal hollowing. draw the muscles away from the belt; others may contract their muscles too strongly, making the abdominal wall rigid and leading to aninability to relax the muscles again to fill the belt. Several days' practice will give your clients full muscle control over both actions. Once they can achieve the appropriate contraction, have them build up the holding time to 10-30 seconds while breathing normally.
88
. Back Stability
A final learning technique is visualization of correct exercise technique following your demonstration. For this "mental practice," your clients should relax and "see" themselves performing the exercise in their imagination. Such visualization has been shown to benefit development of both motor skills (Fansler et al. 1985) and strength (Cornwall et al. 1991). To help your "clients visualize the hollowing action, help them understand the workings of the transversus abdominis and internal oblique musclesyou can use simple diagrams of the muscles and then demonstrate their location using palpation. Analogies such as "personal muscle corset" or "cylinder of muscles" can be helpful. Abdominal Hollowing: Common Errors Be sure that your client's rib cage, shoulders, and pelvis remain still throughout the hollowing action (figure 4.3a). The contour of the abdomen will flatten if a person takes and holds a deep breath, but you will notice the chest expansion (figure 4.3b). If this occurs, instruct your client to exhale and then hold the resulting chest position while performing the exercise. Placing a belt around the lower chest provides helpful feedback about chestmovement (Richardson and Hodges 1996). If your client is using the external oblique to brace the abdomen, which is also an incorrect technique, the lower ribs will be depressed, and you may observe a horizontal skin crease across the upper abdomen (figure 4.3c). When this occurs, instruct your client to perform pelvic floor contraction at the same time as abdominal hollowing, but to avoid contracting the gluteus maximus (use of which leads in this case to inappropriate motor patterns for trunk stability during dynamic sports activity).
Lower ribs stay still a
Figure 4.3 Abdominal are incorrect.
Rib cage depressed
Rib cage lifted
c
b hollowing
in standing:
(a) is correct,
and (b) and (c)
Teaching Your Clients the Basic Skills
.
89
In kneeling, lying, and sitting positions, pressing onto the floor with the feet indicates a failure to isolate the deep abdominal action from that of the hip muscles. Placing your client's feet on a bathroom scale will provide clear feedback about hip extension pressure-ideally, the scales should show no increase in weight during the exercise. Your clients should maintain a neutral lumbar position during abdominal hollowing and refrain from significant movement of ribs, pelvis, or hips.
KEY POINT:
TEACHING YOUR CLIENTS TO CONTRACT THE MULTIFIDUS MUSCLES AT WILL Multifidus is the key stabilizer muscle within the spinal extensor group (page 50). Subjects with low back pain often lose the ability to contract this muscle (probably through pain inhibition), and they do not regain the ability spontaneously (Hides et al. 1996). Two kinds of exercises will help increase your client's basic back stability. The first focuses solely on the multifidus muscles, with an emphasis on helping your client learn to recognize what it feels like to tension/relax only those particular muscles. The second, using the techniques of proprioception, focuses not only on the multifidus but also on the lateral abdominals, which of course are also vital for basic stability.
The Basic Exercise for Multifidus Contraction Your help is essential for your client to learn adequate control of this muscle.
Multifidus Contraction .f{.1~'"
To learn to use the multifidus other muscles.
at will and separately
from
Your client begins in a prone lying position while you palpate his lower back medial to the longissimus at L4 and L5levels. Identify the spinous processes and slide your fingers laterally into the hollow between the spinous process and the longissimus bulk. Assess the difference in muscle consistency, and then determine your client's ability to isometrically contract the multifidus in a "setting" action. Once the individual can consciously contract the muscle, encourage him to use multifidus setting continued
90
. Back Stability
Multifidus Contraction, continued
in a sitting position with a neutral lumbar spine. He should become able to symmetrically contract the two multifidus muscles and sustain the contraction for 10-30 seconds.
Rhythmic Stabilization Rhythmic stabilization involves gross action of the multifidus in conjunction with the lateral abdominals. Rhythmic stabilization is a PNF (proprioceptive neuromuscular facilitation) technique that involves alternating isometric contractions of the agonist and antagonist muscles, building up to co-contraction (Sullivan et al. 1982). The general idea is simple: first, you apply a resistance in one direction and your client contracts her muscle against the resistance. Once you feel that the contraction has reached a maximum, instantaneously apply your resistance in the opposite direction-at which point she contracts the antagonist muscle, with no momentary relaxation between the two contractions. In this way, the muscle pairs are contracting to gradually higher levels. The following exercise uses this technique in teaching your client to contract the multifidus.
Rhythmic Stabilization of Multifidus and Lateral Abdominals in Side Lying Position .f{'7~'.
To encourage your client to contract lateral abdominals simultaneously.
the multifidus
and
With your client in the crook side lying position, palpate the intervertebral joints to ascertain the midpoint of the movement range at the spinal level where you have found pain/pathology (Maitland 1986). Remember that the multifidus muscle is unisegmental-that is, each fascicle stretches over only a single segment of the lumbar spine. Wasting of the muscle occurs at the same level as the segment of pathology (Hides et al. 1994). To place the relevant muscle fascicle at its optimum length, you must move the painful segment into its midrange. If you feel inadequate to do this, ask an experienced orthopedic physical therapist to work with you.
The exercise consists of you pushing forward on your client's pelvis and backward onto the shoulder while your client resists the action. Then reverse the action: while you push backward on the pelvis and forward onto the shoulder, she continues to resist the action, not allowing herself to relax even for a second. The action can be more localized by an orthopedic physical therapist who can palpate the specific spinal continued
Teaching
Your Clients the Basic Skills.
91
Rhythmic Stabilization of Multifidus and Lateral Abdominals in Side Lying Position, continued
level that requires resistance to rotation. General resisted rotation can be performed for the whole spine by having a partner help you use this exercise at home. The exercise is repeated 5-10 times at each of three treatment sessions.
Teaching Tips for Multifidus Contraction Initially, you will palpate with your thumb and the knuckle of your first finger placed on either side of the lumbar spinous process at any one level. Instruct your client to "feel the muscle swelling" without actively flexing the lumbar spine (figure 4.4). You may want to suggest that your client practice this action with his own thumbs so he'll have some feedback for home practice. While sitting, he should press into the extensor region with his thumbs at the side of the spinous processes. Figure 4.4 Palpating to The pressure should be steady but deep. The assist your client in detectaim is to feel the muscle swelling against his ing multifidus contraction. digital pressure without allowing his pelvis to From Norris 1998. tilt or his spine to arch. Angling the trunk forward at the hip (hip hinge action) will contract the longissimus and enable your client to distinguish between the longissimus fibers (more lateral) and the multifidus. Performing abdominal hollowing at the same time will improve the multifidus contraction.
.
SUMMARY Safely improving back stability requires that an individual learn to contract certain muscles voluntarily and independently-in particular, the deep abdominal muscles (transversus abdominis and internal oblique) and the multifidus muscles of the back.
.
Such independent muscle control enables an individual 1. to control pelvic tilt (i.e., to voluntarily move the pelvis independently of the spine); 2. to support the spine with contracted multifidus; 3. to support the spine with abdominal hollowing; and 4. to achieve the neutral position of the lumbar spine, from which position most exercises in this book should begin.
.
This chapter teaches you, the therapist,
these skills.
how to help your clients learn
S Muscle Imbalance Muscle imbalance occurs when a particular agonist is significantly stronger than its antagonist, or when one or the other is abnormally shortened or stretched. The body's attempts to compensate for imbalance generally exacerbate the problem and can lead to serious disability. This chapter first presents general theory about muscle balance and imbalance. It then shows you how to identify such problems and how to treat them. Much of the material for this section is modified from Norris (1998), to which you are referred for further reading.
BASIC CONCEPTS We can categorize muscles into two nondistinct groups Ganda and Schmid 1980; Richardson 1992): (1) Muscles that primarily stabilize a joint and approximate the joint surfaces are known as stabilizers or "postural muscles." (2) Muscles primarily responsible for movement (those which develop angular rotation more effectively than the stabilizers), are called mobilizers or "task muscles."
CTermsYOUShoulil1<now
~
diastasis separation of normally joined parts. pseudoparesis apparent weakness brought on by increased tone in a muscle antagonist.
Stabilizers (postural muscles) primarilyfix a joint'" and prevent movement. Mobilizers (task muscles) primarily create movement.
KEY POINT:
I
Stability muscles tend to be more deeply placed in the body and are usually monoarticular (one-joint) muscles, whereas mobilizers are on the whole superficial and are often biarticular (two-joint) muscles. For example, in the leg, the rectus femoris is classified as a mobilizer, while the other Chapter 5 exercise descriptions adapted from Norris 1998. 92
Muscle Imbalance.
93
quadriceps muscles are stabilizers. Stabilizer function is more slow-twitch (type I) or tonic in nature, whereas that of the mobilizers tends toward fast-twitch (type II) action. This physiology suits the functional requirements of the muscles-enabling mobilizers to contract and develop maximal tension rapidly but also to fatigue quickly. The stabilizer muscles build tension slowly and perform well at lower tensions over longer periods, being more fatigue-resistant. Stabilizers can be subdivided into primary and secondary types Gull 1994) (table 5.1). The primary stabilizers (e.g., multifidus, transversus abdominis, and vastus medialis oblique) have very deep attachments, lying close to the axis of rotation of the joint. In this position, they are unable to contribute any significant torque but will approximate the joint.
Table 5.1
Muscle Types
The following characteristics are not absolute but are only tendencies within these sometimes inexact categories of muscles. Stabilizers Mobilizers Primarily responsible for movement, Primarily responsible for stabilizing including angular rotation and approximating joints Examples: rectus femoris. hamExamples: multifidus, transversus strings abdominis, vastus medialis oblique
.
.
.
.
Primary stabilizers . Deep, close to joint . Slow twitch
.
Usuallymonoarticular (1 joint)
Secondary stabilizers
. . . .
Intermediate
depth Slow twitch Usually mono-
articular Primary source of torq ue ments multipinnate
. torque . . Build tension slowly, more fatigue resistant No significant Short fibers
. .
.
Better activated at low levels of resistance More effective in closed chain movement In muscle imbalance, tend to weaken and lengthen
. Superficial . Fast twitch
.Often biarticular (2 joints) .
.
Secondary
source of torque
Build tension rapidly, fatigue quickly . Better activated at high levels of resistance More effective in open chain movements In muscle imbalance, tend to tighten and shorten
.
.
94
. Back Stability
In addition, many of these smaller muscles have important proprioceptive functions (8astide et al. 1989). The secondary stabilizers (e.g., gluteals and oblique abdominals) are the main torque producers, being large monoarticular muscles attaching via extensive aponeurosis. Their multipinnate fiber arrangement makes them powerful and able to absorb large amounts of force through eccentric action. The mobilizers (e.g., rectus femoris and hamstrings) act as stabilizers only in conditions of extreme need. They are fusiform in shape-a less powerful fiber arrangement, but one able to produce large ranges of motion. Stabilizer muscles are better activated at low resistance levels-about 30-40% of the maximum voluntary contraction (MVC)-while mobilizer muscles are generally better activated above this level. Re-educating the muscles of back stability therefore calls for low-level contractions, not the extreme workouts well-meaning therapists sometimes prescribe for lower back pain. In addition, stabilizer muscles respond better to closed kinetic chain actions, where movement occurs proximally on a stabilized distal segment; in standing, this would be with the foot on the ground for the lower limb, or the hand on a wall for the upper limb. Mobilizer function is more effective in an open chain situation, where free movement occurs without distal fixation. In the lower limb, the swing phase of gait is open chain; in the upper limb, throwing is a prime example. The structure and functional characteristics of the two muscle categories makes the stabilizers better equipped for postural holding and antigravity function. The mobilizers are better designed for rapid ballistic movements. Two fundamental changes appear when there is muscle imbalance: (1) tightening of mobilizer (two-joint) muscles and (2) loss of endurance (holding) within the inner range of motion of the (single-joint) stabilizer muscles, which arises from their being abnormally stretched. These two changes are used as tests for the degree of muscle imbalance present. Since the changes in length and tension alter muscle pull around a joint, they may draw the joint out of alignment. Changes in body segment alignment and the degree of segmental control (the ability to move one body segment without moving any others) form the basis of the third type of test used when assessing muscle imbalance. The mixture of tightness and weakness in muscle imbalance alters body segment alignment and changes the equilibrium point of a joint. Normally, the equal resting tone of agonist and antagonist muscles allows the joint to assume a balanced resting position, with the joint surfaces evenly loaded and the joint's inert tissues not excessively stressed. However, if the muscles on one side of a joint are tight and the opposing muscles are lax, the joint will be pulled out of alignment toward the tight muscle (figure 5.1). This alteration in alignment throws weightbearing stress onto a smaller region of the joint surface, increasing pressure per unit area. Further, the inert tissues on the shortened (closed) side of the joint will contract over time.
.
Muscle Imbalance
95
Normal
a Joint
Joint
Figure 5.1 Posture and muscle imbalance. (a) Equal muscle tone gives correct joint alignment. (b) Unequal muscle tone pulls joint out of alignment, resulting in faulty posture. Reprinted from Griffin 1998.
a ()
b
c
I I I
I I I I
ID
:-;
I
.,
'.
I
I
I I I,
I I
:E)
()
Figure 5.2 Relative flexibility. When the attached tighter cord (A-B) moves less than the looser cord From Norris 1998.
cords (B-C).
I
are stretched,
the
Imbalance also leads to a lack of accurate segmental control. The combination of stiffness (hypoflexibility) in one body segment and laxity (hyperflexibility) in an adjacent segment leads to relative flexibility (White and Sahrmann 1994). In a chain of movement, the body seems to take the path of least resistance, with the more flexible segment always contributing more to the total movement range. Consider two pieces of rubber tubing of unequal strengths that are attached to one another (figure 5.2). If the movement begins at C and A is fixed, the more flexible area B-C moves more. This will still be the case if C is held immobile and A moves. Taking this example into the body, figure
5.3
shows
areas
a toe-touching
of interest
for relative
exercise.
flexibility
The
two
are the
a
Figure 5.3 Relative stiffness in the body. bine equal
pelvic
tilt and spinal flexion. stressing the more lax spinal tissues. (0) From Norris 1998.
(a) Forward flexion should com(b) Tight hamstrings limit pelvic tilt,
96
. BackStability
hamstrings and lumbar spine tissues. As we flex forward, movement should occur through a combination of anterior pelvic tilt and lumbar spinal flexion. Many people have tight hamstrings and excessively lax lumbar tissues due to excessive bending (lumbar flexion) during everyday activities. During this flexing action, greater movement (and therefore greater tissue strain) always occurs at the lumbar spine. Relative stiffness in this case makes the toe-touching exercise ineffective as a hamstring stretch unless the trunk muscles are tightened to stabilize the lumbar spine.
~
Muscle imbalance can iead to changes in-b-oth
functionand structure of the body tissues.
MUSCLE ADAPTATION TO INJURY, AND TRAINING
IMMOBILIZATION,
Different kinds of muscles react differently to injury and immobilization. Primary stabilizers such as multifidus and transversus abdominis, for example, react quickly (by inhibition) to pain and swelling (see table 5.2). Table 5.2 Stabilizer and Mobilizer That Affect the Lower Back
Muscles marked
with'
Muscles
can act as both stabilizers
and mobilizers,
situations. Stabilizers
Mobilizers
. Primary stabilizers Multifidus Transversus abdominis Internal oblique Gluteus medius Vastus medialis Serratus anterior Lower trapezius Deep neck flexors . Secondary stabilizers Gluteus maximus Quadriceps Iliopsoas' Subscapularis Infraspinatus Upper trapezius' Quadratus lumborum'
. Iliopsoas' . Hamstrings . Rectus femoris . Tensor fasciae Hip adductors Piriformis
. . . . . . . .
lata (TFL)
. Rectus abdominis External oblique Quadratus lumborum' Erector spinae Sternomastoid Upper trapezius' Levator scapulae . Rhomboids . Pectoralis minor . Pectoralis major . Scalenes
in different
Muscle Imbalance.
97
There are even more clear differences in reactions to reduced usage, which has been studied extensively using immobilized limbs. The greatest tissue changes occur within the first few days of disuse. Strength loss can be as much as 6% per day for the first eight days, with minimal loss after this period (Appell 1990). Type I and type II muscle fibers differ considerably in response to disuse, with type I fibers showing greater reduction in size and greater loss of total fiber numbers than type II. In fact, the number of type II fibers actually increases-demonstrating a process of selective atrophy of the type I fibers (Templeton et al. 1984). However, not all muscles show an equal amount of type I fiber atrophy. Atrophy is largely related to change in use relative to normal function, with the initial percentage of type I fibers that a muscle contains being a good indicator of likely atrophy pattern. Those muscles with a predominantly antigravity function, which cross one joint and have a large proportion of type I fibers (e.g., the soleus and vastus medialis muscles) show greatest selective atrophy. Predominantly slow twitch antigravity muscles that cross multiple joints are next in order of atrophy (e.g., erector spinae). Finally, the phasic, predominantly fast type II muscles (e.g., biceps) can be immobilized with less loss of strength than the other two groups (Lieber 1992). Training also causes selective changes in muscle. In the knee, rapid flexion-extension actions can selectively increase activity in the rectus femoris and hamstrings (biarticular mobilizers) but not in the vasti (monoarticular stabilizers). In a study by Richardson and Bullock (1986) comparing speeds of 75°/sec and 195°/sec, mean muscle activity for the rectus femoris increased from 23.0 f.I. V to 69.9 f.I. V. In contrast, muscle activity for the vastus medialis increased from 35.5 f.I. V to only 42.3 f.I.V (figure 5.4). The pattern of muscle activity was also noticeably different after training. The rectus femoris and hamstrings displayed phasic (on-and-off) activity at the fastest speeds, while the vastus medialis show~d a tonic (continuous) pattern. The graphs in figure 5.5 show an EMG trace of the electrical activity produced when a muscle contracts. The general trend of the graph shape is important, rather than each individual line. Note that there are clear groups of electrical spikes for the rectus femoris and the hamstrings, indicating that activity occurred in these muscles at specific points in the total movement. For the vastus medialis there are no clear groups, indicating that the activity occurred continually throughout the movement. Ng and Richardson (1990) found similar changes even in the more functional closed kinetic chain position. A four-week training period of rapid plantar flexion (in standing position) gave significant increases in jump height (gastrocnemius, biarticular) but also significant losses of static function of the soleus (monoarticular). Recruitment patterns of lower back muscles also change depending on the type of training used (O'Sullivan et al. 1998). Subjects followed a
98
. 8ack Stability 70-
o 75°/sec .1500/sec .195°/sec
60-
:~ (;
~50-
co Q)
40U ::> 30'" :2 20 10
n Vastus lateralis
Rectus femoris
Vastus medialis
Lateral hamstring
Figure 5.4 Muscle activity changes with increases in speed. Reprinted from Richardson and Bullock 1986.
Rectus femoris Hamstrings
Vastus medialis 0°
Knee angle
Figure 5.5 Muscle activity patterns during rapid alternating knee flexionextension. Note that biarticular muscles are phasic, while monoarticular muscles are tonic. Reprinted from Richardson and Bullock 1986.
lO-week training program involving either abdominal hollowing (15 minutes daily, progressed with limb loading) or gym exercise that included trunk curls. EMG activity of the internal oblique (more important for back stability) increased in the hollowing group, whereas that of the rectus abdominis remained relatively unchanged. Trunk curls (but
Muscle Imbalance
1000
1000
~~ 500
500
. 99
w~
o
Before
After
Before
o
After
.
After
Abdominal
Trunk curl
D
Before
Before
After
hollowing
Rectus abdominis Internal
oblique
Figure 5.6 Altered abdominal Data from O'Sullivan et al. 1998.
muscle
not hollowing) led to an increase duction in activity of the internal
TRAINING
recruitment
pattern
with
in rectus abdominis activity oblique (figure 5.6).
training.
and
a re-
SPECIFICITY
The aforementioned differences in responses of stabilizer and mobilizer muscles illustrate the importance of training specificity. Responses to training closely correspond to the type of exercise used. For example, if runners want to reduce their marathon running time, sprint training will not be effective. This is because sprinting is primarily an anaerobic activity (energy supplied from stores within the body), whereas marathon training is predominantly aerobic (energy supplied by using oxygen and food as fuel). We can say in this case that, although the sprint training caused an increase in fitness, the aspect of fitness that improved was not strictly relevant to the event that the training was designed for. The training was not specific to the event. In the same way, we have seen that high-speed muscle training leads to recruitment of mobilizer muscles. In the example from Richardson and Bullock (1986) described previously, the rectus femoris increased its activity markedly at high-speed (195°/sec) movements. If we used this highspeed training to try to improve the vastus medialis, it would not be very effective. Specificity can be remembered by a simple mnemonic, S.A.I.D., which stands for Specific Adaptation to Imposed Demand. The change occurring in the body (the adaptation) is specific to (exactly matches) the training used (the imposed demand). You can adequately address your clients'
100
.
Back Stability
muscle imbalances only by using quite specific exercises-which, of course, require equally accurate, specific assessments of which muscles need what kind of treatment. The tests described later in this chapter will help you make such appropriate assessments. '""Training specificity dictates that, when de5'i'Qriing an exercise program for a client, you must consider the
KEY POINT: I
functional requirements, contraction type, and speed of contraction of a muscle.
CHANGES IN MUSCLE
LENGTH
Changes in muscle length do not occur in a uniform manner throughout the body. An overly simplistic but useful description is that stabilizer muscles tend to "weaken" (sag), whereas mobilizers tend to "shorten" (tighten). Exercise therapy aimed at muscle must therefore be selective rather than general, seeking to lengthen (stretch) tight mobilizer muscles and shorten/build endurance of inactive stabilizer muscles.
Chronic Muscle Lengthening The weakening of stabilizer muscles has been termed stretch weakness (Kendall et al. 1993): the muscle remains in an elongated position, beyond its normal resting position but within its normal range. This is different from overstretch, in which the muscle is elongated beyond its normal range. The length-tension relationship of a muscle (page 38) dictates that a stretched muscle, where the actin and myosin filaments are pulled apart, can exert less force than a muscle at normal resting length. Where the stretch is maintained, however, this short-term response (reduced force output) becomes a long-term adaptation: the muscle adds more sarcomeres to its ends in an attempt to move its actin and myosin filaments closer together (figure 5.7). This adaptation, known as an increase in serial sarcomere number (SSN), can lengthen a muscle by up to 20% (Gossman et al. 1982). The length-tension curve of an adaptively lengthened muscle moves to the right (figure 5.8). The peak tension such a muscle can produce in the laboratory is up to 35% greater than that of a normal length muscle (Williams and Goldspink 1978). However, this peak tension occurs at approximately the position where the muscle has been immobilized (point a, figure 5.8). If the strength of the lengthened muscle is tested with the joint in midrange or inner range (point b, figure 5.8), as is common in clinical practice, the muscle cannot produce its peak tension and appears "weak." For this reason, manual muscle tests appear to be more accurate indicators of positional strength than measures of total strength (Sahrmann 1987).
-
Figure 5.7 Muscle length adaptation. (0) Normal muscle length. (b) In stretched muscle, the filaments move apart, resulting in loss of muscle tension. (c) Normal filament alignment is restored by increases in serial sarcomere number (SSN), resulting in chronic abnormal muscle length. From Norris 1998.
10
Shortened Control Lengthened
a ,.,---....
8
§ c: o 'w c: $
6
~
4
U
2
,.,~/ , ,
, ,,
,
, ,,
,
, ,,
,
, ,,
,
,,"
1 0
1 0
% muscle belly length of control
Figure 5.8 Effects of immobilizing positions (see text for explanation).
a muscle in shortened
and lengthened
From Norris 1998.
101
102
.
Back Stability
In the laboratory, a lengthened muscle returns to its optimal length within approximately one week if placed in a shortened position (Goldspink 1992). Clinically, restoration of optimal length may be achieved by immobilizing the muscle in its physiological rest position (Kendall et al. 1993) and/or by exercising it in its shortened (inner-range) position (Sahrmann 1990). Enhancement of strength is not the priority in this situation-indeed, the load on the muscle may need to be reduced to ensure correct alignment of the various body segments and correct performance of the relevant movement pattern. SSN may be partly responsible for changes in muscle strength without parallel changes in hypertrophy (Koh 1995). A number of factors influence SSN, which exhibits marked plasticity. For example, immobilization of rabbit plantarflexors in a lengthened position showed an 8% increase in SSN in only four days; applying electrical stimulation to increase muscle force led to an even greater increase (Williams et al. 1986). Stretching a muscle appears to affect SSN significantly more than does immobilization in a shortened position. Following immobilization in a shortened position for two weeks, the mouse soleus decreased SSN by almost 20% (Williams 1990). However, stretching for just one hour per day in this study not only eliminated the SSN reduction, but actually increased SSN by nearly 10%. Eccentric stimuli appear to cause a greater adaptation of SSN than concentric stimuli. Morgan and Lynn (1994) subjected rats to uphill or downhill running and found SSN in the vastus intermedius to be 12% greater in the eccentric-trained rats after one week. Koh (1995) has suggested that, if SSN adaptation occurs in humans, strength training may produce such a change if it is performed at a joint angle different from that at which the maximal force is produced during normal activity. The lengthened muscle is not weak-it merely lacks the ability to maintain full contraction within the inner range. This shows up clinically as a difference between the active and passive inner ranges. If the joint is passively placed in full anatomical inner range, the subject is unable to hold the position. Sometimes the position cannot be held at all, but more usually the contraction cannot be sustained, indicating a lack in slow twitch endurance capacity. Clinically, reduction of muscle length is seen as the enhanced ability to hold an inner-range contraction. This mayor may not represent a reduction in SSN but is a required functional improvement in postural control for muscles that are abnormally lengthened. Muscle shortening appears in the dorsiflexors of equestrians, who clearly do not hold the shortened position permanently, as with splinting, but rather show a training response. Following pregnancy, SSN increases in the rectus abdominis in combination with diastasis. Again, length of the muscle gradually reduces in the months following birth. Inner-range training, then, is likely to shorten a lengthened muscle (Goldspink 1996).
Muscle Imbalance
. 103
Assessing Stretched MusclesTesting Inner-Range Holding Ability We have seen from figure 5.8 that the length-tension curve of a lengthened muscle moves to the right, indicating that it is unable to produce significant power within the full inner range. This fact forms the basis of the assessment of stabilizer muscle length by inner-range holding tests. Tests for the most important stabilizing muscles are described below. Lower Back and Hip Muscles-inner-Range Hoiding Tests The ability of a stabilizer to maintain a low-load isometric contraction over a period of time is vital to its antigravity function and may be assessed using the standard muscle test position (Richardson 1992; Richardson and Sims 1991). In all the following assessments, ask your clients to maintain a contraction in full inner range, the key factor being the length of time they can maintain the static hold before developing jerky (phasic) movements. In each case, you will place the limb passively into the full inner range. If the limb drops upon release, the passive range of motion differs from the active range-an important indicator of poor stabilizer function. Full stabilizing function is present only when a subject can maintain the innerrange position for 10 repetitions of 10 seconds' duration Ou1l1994). In all the tests, it is important that your subjects attempt all 10 repetitions; often they will perform the first two or three normally, with the deficit becoming apparent only in later repetitions.
Assessing
Muscle
Balance
in the Iliopsoas
While sitting, your client flexes her hip while maintaining 90° knee flexion so that the foot is lifted clear of the ground. Have her hold this position as long as she can, while you record the time at which phasic movements begin. Note also the position of the pelvis and lumbar spine. Where the iliopsoas is lengthened, one of two things may happen: (1) If lumbar stability is poor, the pelvis will drop back into posterior tilt, flattening or even reversing the lumbar lordosis. (2) If lumbar stability is good, your client will be able to maintain the neutral position of the lumbar spine and pelvis-but the knee will simply drop, indicating that the hip flexor muscles have lengthened (but not necessarily weakened) and are unable to hold the full inner-range position.
104
. Back Stability
Assessing
Muscle
Balance
in the Gluteus
Maximus
,,----.. Have your client lie in a prone , -position with her knee flexed to 90°. Then she should lift her \/ , hip to the inner range of ex-----tension and hold it steady (right; b, below). Using palpation, note the order of muscle contraction during the hip extension. Normally, the hamstrings should contract first, followed by the gluteus maxim us, then the contralateral erector spinae, and finally the ipsilateral erector spinae (Lewit 1991). In many cases of imbalance, the gluteus is poorly recruited or even inhibited (pseudoparesis) by tightness in the opposing hip flexors (Janda 1986). Where this is the case, the order of muscle contraction changes. If the gluteals do not function adequately, the hamstrings dominate the movement-little gluteal activity is apparent, and the muscle mass remains flaccid. Note how long your client can hold the position steady before phasic movement begins. Performing the test with the knee bent reduces the contribution that the hamstrings make to the movement by shortening them. The contribution of the gluteus is therefore more apparent. Your ability to see and feel the subtle changes that indicate the order of muscle contraction, however, takes time to develop. Until you have gained experience in this area of examination, you can use dual-channel EMG to show the intensity and timing of muscle contraction. Note: watch carefully to see if your client performs a false hip extension movement; in this action, the pelvis anteriorly tilts due to powerful action of the erector spinae, and the relationship between the hip and pelvis remains the same (c). Thoroughly explain to your client which muscles she should be using to perform this activity and in which order. If she tends to make a false hip extension, hold her pelvis down while she raises her leg using only her gluteals, so that that she learns what the correct movement feels like.
a ,, ,
o c
/' \v "-.:. '7"
Muscle Imbalance
Assessing
Muscle
Balance
in the Gluteus
.
105
Medius
The action in this test is combined hip abduction, with slight lateral rotation to emphasize the posterior fibers of the muscle. Have your client lie on her side with her upper knee flexed. Instruct her to abduct and externally rotate her upper leg so that the femur is at a 45° angle to the ground and her knee is flexed about 45° (dotted lines in figure). Then have her rotate her chest toward the examination table while keeping her upper leg in place Oull1994). Deep Abdominal Muscles-inner-Range Holding Tests Rather than deal with specific abdominal muscles as I did with the hip muscles, I think it more useful in this section to focus on the entire system of deep abdominal muscles that affect lumbar stability and that often are abnormally stretched (and therefore weak in their inner ranges). You can test clients' ability to hold the inner range of the deep abdomina Is (1) by assessing their abilities to hollow the abdomen, and (2) by monitoring lumbar lordosis and pelvic tilt while overloading the stability system. You can assess both actions by accurate palpation and motion recording, but I recommend use of pressure biofeedback, which will make the assessment considerably easier. Note that the pressure biofeedback unit is more useful for assessment rather than for continuing exercises. To assess limb function relative to lumbar-pelvic stability, you can use a number of starting positions-two of which I will describe in detail.
Prone Abdominal
Hollowing Test
Using
Pressure
Biofeedback
.I'{"~'.
To asse.ss client's ahility to hold the inner range of the deep ahdomlnals.
With your subject lying prone, place the pressure biofeedback unit beneath his abdomen with the J upper edge of the device's bladder below his navel. Inflate the unit to ~70 mm Hg, and instruct your client to perform abdominal hollowing (see chapter 4). The aim is to reduce the pressure reading on the biofeedback unit by 6-10 mm Hg continued
~
106
. Back Stability
Prone Abdominal Hollowing Test Using Pressure Biofeedback. continued
and to be able to maintain this contraction for 10 repetitions of 10 seconds each while breathing normally (Richardson and Hodges 1996).
Heel Slide Maneuver Using Pressure
Biofeedback
.,{l1~'" Assess the deep abdominals' ability to maintain spinal stability. The subject begins in a crook lying position with the spine in a neutral position and the pressure biofeedback unit positioned beneath his lower spine. While you palpate the anterior superior iliac spine (ASIS), instruct him to gradually straighten one leg, sliding the heel along the ground to take the weight off the limb. During this action, the hip flexors are working eccentrically and pulling on the pelvis and lumbar spine. If the strong pull of these muscles is sufficient to displace the pelvis, you will be able to feel the pelvis tilt; moreover, the pressure shown on the dial of the biofeedback unit will change. If your client cannot complete the action without any alteration of pelvic tilt or depth of lordosis, palpate the abdominal muscle action. Often subjects will substitute their rectus abdominis and/ or external oblique in an attempt to fix the pelvis rather than using transversus abdominis and internal oblique. Where this is the case, these deeper abdominal muscles will need to be re-educated.
Assessing
Shortened Muscles
Mobilizer muscles have a tendency to tighten. TIghtness in the hamstrings (mobilizers), for example, is common, while tightness in the gluteals (stabilizers) is rare. In addition to reducing range of motion, muscle tightening may lead to development of trigger points (Travell and Simmons 1983)small hypersensitive regions within a muscle that stimulate afferent nerve fibers, causing pain. The sensation created is a deep tenderness with an overlying increase in tone, creating a palpably tender band of muscle. When palpated deeply, the trigger point creates a local muscle spasm, the "jump sign" Ganda 1993). Because tight muscles have a lowered irritability threshold, they are activated earlier than normal in a movement sequence-and they have less slack to take up before contraction begins. In addition, tight muscles have increased afferent input via the stretch receptors (Sahrmann 1990).
Muscle Imbalance
.
107
There are several important reasons why you should assess the tightness of your client's mobilizer muscles. First, since limited range of motion may not allow sufficient movement for correct body segment alignment, limbs may be pulled into positions that stress joint surfaces and collateral ligaments. Second, tightness in a muscle may, through reciprocal innervation, inhibit the opposing muscle through the process of pseudoparesis Oanda 1986). Third, stability must be relative to flexibility. Consider the straight-leg raise (SLR) exercise (see page 109): poor stability can lead the pelvis to tilt very early in the range of motion. Normally, the pelvis only tilts when the hamstring muscles reach the end of their stretch-they are fully 'wound up' -and this may not occur until 80-90° hip flexion. If pelvic tilt is seen before this (in a flexible individual), an imbalance exists. The individual's level of stability is not sufficient for her level of flexibility-she has lost active muscular control over a portion of her total range of motion, a fundamental feature in the difference between hypermobility and instability. If you find muscle tightness, you can use the test movements as starting positions for stretching. But before prescribing stretching exercises, be sure that they will not place excessive strain on adjacent body parts because of relative stiffness. Your clients often will require some stability work before beginning the stretches. The need for stability work is indicated if the subject's alignment is degraded (partially lost) as a stretch is applied. To assess tightness in those muscles that are most likely to exacerbate lower back problems, there are four principal tests--each of which in its own way will help you to assess restriction of pelvic motion: (1) the modified Thomas test, (2) the straight-leg raise (SLR) test, (3) the Ober test, and (4) the tripod test. Carefully note whether any of the movements in these tests reproduces the pain for which the patient has sought treatment; note also if the range is significantly less than the optimal position. (For the Thomas test, optimum is for the femur of the lower leg to drop down to the horizontal, and the tibia of the same leg to drop to the vertical. For the SLR, the optimal value is 70-80° from the horizontal; and for the Ober test, the upper leg should drop down to the level of the couch.) In either case, the muscle will require specific stretching.
The Thomas Test .fl:t1.,.
To assess/correct femoris.
tightness in the iliopsoas and rectus
The patient begins in crook lying at the end of the examination table. Instruct her to lift both knees up to her chest, keeping her back flattened continued
108 . Back Stability
The Thomas Test, continued
to a point where the sacrum just begins to lift away from the examination table surface, but not farther. You can monitor the movement of the pelvis and lumbar spine using a pressure biofeedback unit. As she holds one leg close to the chest to maintain the pelvic position, have her lower the other leg over the end of the table, maintaining a 90° angle at the knee (a). Optimal alignment occurs with the femur horizontal and aligned with the sagittal plane (no abduction) and with the subject's shoulder, hip, and knee more or less in line. The tibia should hang vertically (90° knee flexion) and be aligned with the sagittal plane (no hip rotation-see c). If the femur rests a above the horizontal and the knee is flexed less than 90°, tightness may be present in either the iliopsoas or rectus femoris. If the rectus is tight, straightening the knee will take the stretch off the muscle and the leg will drop down (b). If the knee is straightened and the leg stays in place, it indicates tightness in the iliopsoas. Use palpation to distinguish between the psoas and iliacus. Psoas can be palpated deep in the abdomen at the side of the lumbar spine. Iliacus is found on the inner side of the pelvis. Both muscles take experience to palpate, as they lie beneath the abdominal con- c tents (see figure 3.lOb, page 58).
The Ober Test .f'[t1~,..
To assess both the length of tensor fasciae lata muscle and the tightness of the iliotibial band.
The modified Ober test begins in side lying with the pelvis in a neutral position (a). Have your client bend her lower leg to improve overall body continued
Muscle Imbalance
.
109
The Ober Test, continued
stability while you stabilize the pelvis to avoid lateral pelvic dipping. The examination table should be low enough to allow you to place pressure through the subject's iliac crest in the direction of the lower shoulder. You may monitor the position of the spine and pelvis using pressure biofeedback. While she maintains the neutral pelvic position, have your client abduct the upper leg to 15° above the horizontal and then extend her hip about 15°. She should then adduct it while maintaining extension. For an athlete, optimal muscle length would be confirmed if she is able to lower the upper leg to the level of the table; the nonathlete should be able to lower the leg to the horizontal (b). A false reading is obtained if the pelvis is allowed to tip and the lumbar spine to laterally flex. You can still proceed with the test when hip extension is limited, but you should further assess the hip tightness to determine if it results from muscular, capsular, or osteological factors-an examination for which you should refer the subject to an orthopedic physical therapist.
The Straight-Leg .f{tH.
Raise (SLR) Test
To assess tightness
in hamstrings.
Have your client lie supine on the examination table, one leg slightly bent. Have her raise the other leg while keeping it completely straight. Palpate the anterior rim of the pelvis to note the point at which the pelvis begins to posteriorly tilt due to hamstring tightness-this is the point at which a stable base is no longer being provided for the hamstrings to stretch against. Two body segments are moving here; this is a prime example of relative flexibility, as mentioned on page 95. As the maximal continued
110
.
Back Stability
The Straighr-Leg Raise (SLR) Test, continued
range of hamstring flexibility is reached, the pelvis will begin to tilt posteriorly, bringing the ischial tuberosity of the pelvis forward in an attempt to reduce tension in the hamstrings. Look for pelvic tilt, which will occur before the hamstrings are fully stretched to their end range. For example, if your client can stretch the hamstrings to 90° hip flexion, does the pelvis move at 80-90° as it should because the tension in the hamstrings is maximal? Or does the pelvis begin to tilt at perhaps 4050°, when the tension in the hamstrings is only moderate? The latter case indicates a lack of muscular control over the pelvisthe individual is unable to create the stable pelvic base (using the trunk stabilizers) for the stretched hamstrings to pull against.
The Tripod Test .1'{'1~'. To assess/correct imbalanced hamstrings. Have your client sit on the examination table with his lumbar spine in the neutral position and his feet hanging off the edge. As he straightens one leg, note two measures: (1) the point at which posterior pelvic tilting occurs, and (2) the total range of combined motion at both hip and knee. For optimal performance, the lumbar spine should remain neutral and should allow the knee to straighten to within 10° of full extension while the femur remains horizontal. If you find muscle tightness, you can use the test movements as starting positions for stretching.
Muscle Imbalance
PRINCIPLES
OF MUSCLE
.
111
STRETCHING
Five methods of stretching are generally recognized: ballistic, static, active, and two PNF (proprioceptive neuromuscular facilitation) techniques (table 5.3). PNF stretching has been adopted by the sporting world from neurological physiotherapy treatments. By alternately contracting and relaxing muscles, these techniques capitalize on various muscle reflexes to achieve a greater level of relaxation during the stretch. The back stability program uses two PNF techniques: contract-relax (CR), and contractrelax-agonist-contract (CRAC). PNF stretching was believed at one time to be the most effective type of stretching (Etnyre and Abraham 1986; Holt and Smith 1983), with CRAC methods generally being better than CR. The data are not consistent, however. Moore and Kukulka (1991) found CRAC to cause more pain than either CR or static stretching; moreover, they found that static stretching appeared to be the most effective of all the techniques, leading to less pain and more range of motion. 1recommend that you select stretching techniques on a client-by-client basis. Test to see what works best for each individual. The advantage of static stretching, of course, is that it does not require your presence or that of anyone else. Table 5.3
Principal Stretching Techniques
Method
. .
Action Rapid jerking actions at end of range to force the tissues to stretch. Slowly and passively stretching the muscle to full range, and maintaining this stretched position for a set
.
Ballistic
.
Static
period-usually from 15 to 30
. Active .
Contract-relax
.
seconds.
. Contracting the agonist muscle to full inner range to impart a stretch (CR)
Contract-relax-agonist-contract (CRAC)
'
.
on the antagonist. Isometrically contracting the stretched muscle, then relaxing and passively stretching the muscle still farther. This action is usually performed by a partner. The same as CR. except that during the final stages of the stretching phase. the muscle opposite the one being stretched is contracted.
.
112
.
Back Stability
Here are the basic five stretching methods: 1. Ballistic stretching involves taking the limb to the end of its movement range and adding repetitive bouncing movements. This method is increasingly out of favor since it appears that it may cause injury and muscle soreness (Etnyre and Lee 1987). Although not recommended for regular training, ballistic stretching may have a place in the final stages of rehabilitation for athletes whose sport requiresballistic actions (e.g., high kicks in martial arts practice) (Norris 1998). 2. During static stretching, a muscle is stretched to the point of slight discomfort and held there for an extended period. A holding time of 30 seconds has been shown to be optimal, with 15 seconds being less effective and 60 seconds being not more effective (Bandy and Irion 1994). Repeating the stretch is important, with the greatest stretching effects occurring within the first four repetitions (Taylor et al. 1990). Easily remembered, basic guidelines for static stretching are 5 repetitions, holding each for 30 seconds, with a 3D-second rest period between each movement. 3. Active stretching involves pulling a limb into full inner range so that the antagonist muscle is stretched passively while the agonist is strengthened. This type of stretch can be important when correcting muscle imbalance. The inner-range contraction helps shorten a lengthened (lax) muscle, while the shortened muscle is stretched using a functionally relevant movement. Webright et al. (1997) found static and active stretching equally effective when used daily for a six-week period. Static stretching involves less coordination and fewer repetitions than active stretching, so it is more appropriate to early treatment stages. Active stretching involves more complex coordination and requires greater segmental control, making it more useful in later stages of rehabilitation. 4. The CR (contract-relax) PNF technique involves lengthening a muscle until a comfortable stretch is felt. From this position, the muscle is isometrically contracted and held for a set period. The muscle is relaxed again, then taken to a new lengthened position until the subject again feels the full stretch. The rationale behind the CR method is that the contracted muscle will relax as a result of autogenic inhibition, as the Golgi tendon organ (GTO) fires to inhibit tension. Some authors argue that a maximal isometric contraction is needed to initiate relaxation through the GTO mechanism Uanda 1992). Others recommend the use of minimal isometric contractions (Lewit 1991), which seem more appropriate in situations where pain is present. A window of opportunity exists after isometric muscle contraction-since the stretch reflex is suppressed for about 10 seconds following isometric contraction (Moore and Kukulka 1991), the stretch must be imposed during this time. 5. With the CRAC (contract-relax-agonist-contract) PNF technique, the muscle is stretched as just described-but in the final stages of the stretch,
Muscle Imbalance
.
113
the opposing muscle groups are isometrically contracted to make use of reciprocal inhibition of the agonist and to reduce its tension. To illustrate each of these procedures, consider stretching the hamstrings. 1.A ballisticstretch could involve keeping the leg straight while standing and vigorously reaching for the toes with a bouncing action. While the rapid action may actually tighten the muscle by increasing its tone, it may stretch other soft tissues-including the noncontractile muscle elements, muscle tendons, and ligaments surrounding the hip, knee, and spine. In this particular exercise, moreover, repeated spinal flexion may increase intradiscal pressure within the lumbar discs, potentially leading to discal migration (McKenzie 1981) or discal herniation. For this reason, ballistic stretching should only be performed in the presence of good lumbar stability and optimal segmental alignment. 2. An easy static stretch for the hamstrings involves lying supine on the floor in a doorway, with the hips just inside the door frame. With the leg farthest from the door frame flat on the ground and the back in neutral position, raise the other leg, keeping it straight, until it rests on the door frame. To increase/ decrease the stretch, move the body closer to or farther away from the door frame. The stretch is held for 30 seconds. 3.An active stretchcould be performed by standing, holding on to a wall bar for support, and lifting the straight leg upward using the force of the hip flexors. 4. An individual could perform the CR technique for the hamstrings while lying on his back. A training partner lifts his leg, keeping the knee straight. After holding the stretch for 10seconds, the athlete contracts his hamstrings by pulling the straight leg down toward the floor against his partner's resistance. He holds the tension for 10 to 20 seconds-sufficient time to allow the GTO to override the stretch reflex. He then releases the tension, and the training partner reapplies the stretch. 5. The CRAC technique takes this stretch even further: as the stretch is applied, the athlete tries to increase the stretch himself by pulling the straight leg up toward his head, tensing his hip flexors. In so doing, the hamstrings are relaxed still further through reciprocal inhibition, and the stretch becomes even more effective.
STRETCHING
TARGET
MUSCLES
Several mobilizer muscles within the lumbar-pelvic region are commonly tight and may require stretching. It is generally best to begin with passive static stretching, followed by contract-relax techniques. Finally, the opposing muscles are shortened to full inner range to stretch
the antagonist actively.
114
. Back Stability
Thomas
Test Stretch
.1'1".'. To stretch the hip flexors. This stretch is performed from the Thomas test position (see page 107). Any firm surface may be used at home, such as a sturdy coffee table. Your client should hold one knee tightly to her chest and allow the other leg to rest in a stretched position near the horizontal. To increase the emphasis on the rectus femorus muscle, the knee of the lower (horizontal) leg may be bent. Throughout the movement the back must remain flat on the table and the pelvis must not be allowed to move. She should hold the stretched position for 10-20 seconds, and then lower the leg slowly. Raising into the stretch position and recovering from it should be performed with control, taking 5 seconds in each direction. Reverse the legs and repeat the cycle two more times. Have her perform this stretch daily until she can perform the Thomas test satisfactorily.
Half Lunge .1'111.'. To stretch
the hip flexors.
Have your client take up the half-kneeling position, with one hand on a chair to aid balance and the other hand pressing into the lumbar spine on the side of the dependent leg (the one with the knee on the floor). Instruct him to keep his abdomen hollowed throughout the exercise in order to keep the lumbar spine in neutral position. Tell him to lunge his body forward, forcing the dependent hip into extension while avoiding increasing the lordosis. Hold this stretched position for 10 seconds. Instruct your client to perform this exercise three times a day, each session comprising 10 lunges on each side.
Muscle Imbalance
.
115
Hip Hitch .lIel~''- To work the trunk side flexors on the side of the weightbearing leg. This exercise is used in preparation for the Ober stretch, to enable the subject to control the pelvis with the trunk side flexors. Your client should stand with her hands on a tabletop for support at home, or a bar in the clinic. Instructing her to keep her legs straight throughout the movement, have her make one leg shorter than the other by laterally tilting her pelvis. It may help by suggesting that she imagine she is drawing the rim of her pelvis vertically upward on the side of the shortening leg, raising her heel slightly off the ground. To avoid simply coming up onto the toes, have your client dorsiflex (pull up) her foot-this way you can assess movement of the whole leg in one section. Tell her to keep her upper body from swaying and to relax her shoulders. Once she has mastered this action, have her practice it unsupported (hand off the tabletop), then lying supine, and finally while lying on her side. In each case, the knee must be kept straight throughout the movement, with the action coming from pelvic movement alone. When using the side lying position, she should place her upper hand on her upper hip to provide resistance (since there is no gravity to resist), and she should pull her upper leg up as she simultaneously pushes the leg that is against the floor down (as if she's trying to make that leg as long as possible). Instruct your client to perform this exercise three times a day, with five repetitions for each side from each of the three starting positions (standing, supine, side lying).
Ober
Test Stretch
.lIeN'-Stretch (TFL).
the iliotibial band (lTB) and tensor fasciae lata
The ITB and TFL can become overactive and tight to compensate for a weak or inactive gluteus medius muscle. When this occurs, tightness in the ITB-TFL can cause friction of this structure over the greater trochanter of the femur or the lateral epicondyle of the femur. Both of these areas continued
116
.
Back Stability
Ober Test Stretch, continued
are common sites for ITB friction syndrome-a common overuse condition, particularly among distance runners, that results from muscle imbalance. Beginning in a side-lying position, your client first performs the hip hitch as just described. Then he continues with the Ober test actions (see page 108): he abducts the upper leg to 15° above the horizontal, extends it to 15°, then lowers it into adduction (toward the floor or couch) while maintaining an immobilepelvis. The exercise is complex because it requires the control of two body parts simultaneously. Supervise your client closely, (1) watching the pelvic rim to note any unwanted pelvic movement and (2) noting if the hip extension is being maintained. When the hip extension is lost, the leg falls forward into flexion and the stretch is lost from the TFL. If your client is unable to maintain stability of his pelvis, assist him by holding the pelvis in place with your hands.
Active Knee Extension,
Holding Thigh
.1'[17.'. To stretch the hamstrings. Have your client lie supine, then raise one leg to 90° hip flexion, comfortably bent at the knee, and hold it with her hands beneath the thigh. Then instruct her to straighten the leg as much as possible. The sensation should be one of a deep stretching sensation rather than acute pain. The discomfort should reduce as the stretch is held. She should hold the stretch for 30 seconds. Instruct her to perform this stretch at home three times a day, with two repetitions for each leg at each session.
Active
.1'[.'.'.
Knee
Extension,
To strengthen
Pushing
Against
Thigh
hip flexors, hip
extensors, and hamstrings.
This action stretches the hamstrings while activating the quadriceps against a resistance. Increasing the quadriceps activity should reduce the hamstring tone through reciprocal innervation. continued
Muscle Imbalance
.
117
Active Knee Extension, Pushing Against Thigh, continued
Have your client lie supine and, with one knee comfortably bent, raise that leg until it is at a 600angle to the floor. Instruct him then to straighten the leg, and then slowly raise the straightened leg till it is vertical (900 hip flexion). He should keep the leg completely straight and use only his hip flexor muscles to raise the leg (no use of the hands this time!), without allowing the knee to bend. Once the leg is vertical (or as near vertical as your client can raise it), have him place his hand on the leg just above the knee and use it as a fulcrum to straighten the leg just a little bit more. This is especially helpful in stretching the hamstrings. He should hold this position for 30 seconds. Tell your client to do this exercise three times a day, using three repetitions for each leg per session.
Tripod Stretch .f{'7~'.
To stretch the hamstrings.
Have your client sit upright on the edge of a table, her lumbar spine in its neutral position, her feet hanging over the edge of the table. She should maintain abdominal hollowing throughout the exercise. Have her straighten one leg, to stretch the hamstrings against the stable base of the unmoving pelvis. She should hold the leg straight for 15 seconds, then slowly lower it. Instruct your client to perform this exercise three times a day, with three repetitions per leg per session.
Trunk Side Flexor Stretch .f{'H.
To stretch the quadratus the oblique abdominals.
lumborum
and lateral portion
of
These muscles are commonly tight after prolonged periods of sitting or bed rest. Have your client stand with his back against a wall, his feet shoulder-width apart, his hands clasped behind the head. He should keep his abdomen hollowed throughout the exercise. Instruct him to slowly bend his spine (and only his spine) to one side, being very careful to keep his pelvis level and his knees straight. Until he learns what the continued
. Back Stability
118
Trunk Side Flexor Stretch. continued
proper movement feels like, you should place your hands on his pelvis and let him know when it's bending. Tell him to reach his upper elbow as far toward the ceiling as he can, in an attempt to "lengthen his spine," and to hold this position for 30 seconds. Then he should repeat the exercise to the other side. The height of the upper elbow indicates the range of motion obtained, and the comparative range of each side will reveal your client's degree of symmetry. Instruct your client to do this stretch three times a day on each side.
J.'7:,\
~
':. ,
"'-'
r/
'
J
.
"
Four-Point Kneeling Stretch .fle,,-,.
To stretch the erector spinae.
,:-_... The erector spinae muscles also can tighten :~ during long periods of sitting or bed rest. Have your client assume a 4-point kneeling position. Emphasize that, throughout this exercise, she must move only her spine, with her shoulders remaining over her hands and her hips remaining over her knees at all times. Have her tilt her pelvis posteriorly and continue flexing her spine until her face points toward the groin. She should hold this position for 30 seconds, then slowly relax back toward the starting position. Instruct your client to perform this exercise three times a day, with six repetitions per session.
~~
.
SUMMARY Muscles can be divided roughly, although not unambiguously, into stabilizer or mobilizer muscles. Stabilizer muscles tend to be deep, to contain mainly slow-twitch fibers,
. .
to control only one joint, and primarily to prevent movement while stabilizing a joint. They are the primary postural muscles. Mobilizer muscles tend to be more superficial, to contain mainly fasttwitch fibers, to act over two joints, and primarily
to create movement.
Muscfe Imbalance
·
.
119
Disuse, long-term bed rest, and injury can cause muscle systems to become imbalanced-with an agonist shortened while its antagonist is stretched.
·
To train specific muscles, you must carefully target those muscles in your exercise prescriptions; exercises meant to improve back stability often fail to do so because they target the wrong muscles (especially the deep stabilizer muscles).
·
You can treat such imbalance by prescribing exercises that strengthen/ shorten the stretched muscle and stretch the shortened muscle; this chapter describes a number of such exercises.
~ Basic Abdominal Muscle Training Much of the back stability program involves working on the abdominal muscles. Especially for your clients who want to take abdominal training further (to enhance performance rather than merely to build stability), you must offer training that is both safe and effective. First I want to discuss currently popular abdominal exercises and assess their effects on the muscles and tissue. Then I will present modifications to improve the safety and effectiveness of such exercises.
CURRENT
PRACTICE
IN ABDOMINAL
TRAINING
Abdominal training can be dangerous, whether for competitive sport or for general fitness. In sport, athletes often adhere with almost religious fervor to traditional but potentially harmful training methods. In the general population, fashion often dictates which movements are in favoryet many popular exercises lack reliable scientific foundation. Before you can prescribe the most appropriate trunk exercises for your clients, you must understand what the traditional exercises actually achieve. To this end I will begin by briefly analyzing the two major categories of abdominal exercises: the sit-up and the leg raise.
The Sit-Up In the sit-up, an individual comes from a supine lying to a long sitting position using hip flexion, usually combined with trunk flexion. In a classic sit-up, the rectus abdominis shows activity as soon as the head lifts (Walters and Partridge 1957), and as a consequence the rib cage is depressed anteriorly. This initial period of flexion emphasizes the supra umbilical portion of the rectus; the infra umbilical portion contracts later, with the internal oblique (Kendall et al. 1993). As the internal oblique contracts, it pulls on the lower ribs, increasing the infrasternal angle by causing the ribs to flare out. 120
Basic Abdominal Muscle Training
.
121
Fixation of the pelvis is provided by the hip flexors, especially the iliacus through its attachment to the pelvic rim. The strong pull of the hip flexors is partially counteracted by the pull of the lateral fibers of external oblique and the infra umbilical portion of the rectus abdominis, which tend to tilt the pelvis posteriorly. Action of the external oblique, if powerful enough, compresses the ribs and reduces the infrasternal angle once more (Kendall et al. 1993). Problems Resulting From Poor Conditioning Initiation of the sit-up action sometimes leads to "bow stringing" in poorly toned individuals. For the superficial abdominals (rectus abdominis and external oblique) to pull flat, the deep abdominals (transversus abdominis and internal oblique) must be able to pull on the rectus sheath to hold the abdominal wall down. Many people, however, have lost the ability to coordinate action of both the superficial and deep abdominals, which this action requires-the two sets of abdominal muscles are imbalanced, with poorly recruited deep abdominals and dominant superficial abdominals. When this is the case, the abdominal wall appears to dome and the athlete may lift the trunk with the lumbar spine extended or flat rather than flexed (figure 6.1). Weak deep abdominal muscles cannot hold the rectus abdominis down as it contracts, leading to "doming" of the abdominal wall.
KEY POINT:
a
b Figure 6.1 Trunk alignment during a sit-up exercise. (a) Strong deep abdominals flatten abdominal wall. (b) Weakened deep abdominals allow abdominal wall "doming," while lengthened superficial abdominals allow anterior pelvic tilt and hollowing of the back. From Norris 1998.
122
.
BackStability
Poorly conditioned subjects also tend to use the hip extensors to momentarily tilt the pelvis posteriorly at the beginning of a sit-up, prestretching the hip flexors. This gives the hip flexors a mechanical advantage before hip flexion occurs and reduces both the work required of the abdomina Is and the conditioning effect of the exercise on the abdominals. During this phase, the abdominal muscles work eccentrically (Ricci et al. 1981). Effects of Foot Fixation If a person attempts a sit-up from the supine position without allowing trunk flexion, the legs tend to lift up from the supporting surface-this occurs because the legs constitute roughly one-third of total body weight whereas the trunk contributes two-thirds. The upper body's center of gravity moves toward the hip as the abdominal muscles flex the spine, reducing the lever arm of the trunk and enabling the subject to perform the sit-up without lifting the legs (figure 6.2). When the abdominal muscles are weak and lengthened, maximum spinal flexion does not occur because the muscles are unable to pull the lumbar spine into full inner range-the lever arm of the trunk remains long, and the legs lift. The point at which this occurs in the movement depends on a subject's weight and height. If the feet are fixed, however, the hip flexors can pull powerfully without causing the legs to lift. The act of foot fixation itself, in fact, may facilitate the iliopsoas Oanda and Schmid 1980). To pull against the fixation point, one must use active dorsiflexion-which simulates the gait pattern at heel contact, increasing activity in the tibialis anterior, quadriceps, and iliopsoas (a pattern known as flexor synergy during gait) (Atkinson 1986). , ...-......, I
,---_
I... \ " "',..-' ",
, ,-, , , ,, , ~r- , , ,.... , , ...'" , , , , "
,,
Figure 6.2 As the trunk flexes, the center of gravity of the upper body moves caudally. From Norris 1998.
Basic Abdominal Muscle Training.
The hip flexor muscles contract powerfully in a traditional sit-up. Fixing the foot causes the hip flexors to work even harder, without significantly increasing the work on the abdominal muscles.
KEY POINT:
123
1
The Straight-Leg Raise The bilateral straight-leg raise (SLR) creates only slight activity in the upper rectus, although the lower rectus contributes a greater proportion of the total abdominal work in this exercise than with the sit-up (Lipetz and Cutin 1970). The rectus works isometrically to fix the pelvis against the strong pull of iliopsoas (Silvermetz 1990). The iliopsoas contracts with maximum force when the lever arm of the leg is greatest (near the horizontal) and reduces as the leg is lifted toward the vertical. Problems Resulting From Poor Conditioning In subjects with weaker abdominals, the pelvis tilts and the lumbar spine hyperextends during the SLR. This forced hyperextension dramatically increases stress on the facet joints, especially those in the lumbar spine. The movement is likely to be limited by impaction of the inferior articular processes on the laminae of the vertebrae below (see chapter 2) or, in some cases, by contact between the spinous processes (Twomey and Taylor 1987). Rapid action of this kind can damage the facet joint structures. Once the facet and lamina are touching each other, further loading causes axial rotation of the superior vertebra (Yang and King 1984); the superior vertebra then pivots, causing the inferior articular process to move backward, overstretching the joint capsule. Effects of Arm Fixation When the legs are lifted in an SLR, the body position is less secure because its base of support is smaller. People tend to rock toward the side of the lifted leg (where one leg is lifted) or to struggle to keep their backs on the floor (where both legs are lifted). Fixing the arms by holding onto an overhead object (e.g., gym bench) with the arms, or by pressing down with the flats of the hands with the arms by the side, improves the security of the starting position. The disadvantage of fixing the arms, however, is that people can pull harder with their hip flexors without realizing they have lost their lumbar alignment. This is especially true of the bilateral leg raise action. At the beginning of this action the leverage from the legs is maximal, as they are horizontal. Without fixing their arms, poorly conditioned subjects may be unable to lift their legs at all-thereby self-limiting potential stress on the lumbar spine. With arms fixed, however, they may be able to lift their legs by rapidly pulling
124
. Back Stability
with their arms and "jerking" their legs up with a rapid contraction of the hip flexors. Once the legs move toward the vertical, their leverage is reduced and the movement can be continued-leading people to believe (wrongly) that, since they completed the action, they must have performed it correctly. The jerking action is extremely dangerous, however, due to the compression and shear forces it imposes on the lumbar spine. For SLRs, then, permit your clients to fix their arms only when they will perform the exercises in a slow and controlled fashion, and only after you have chosen the exercise most appropriate for their specific body condition. Straight-leg actions are inappropriate for poorly conditioned subjects or for those with a history of back pain.
MODIFICATIONS ABDOMINAL
OF TRADITIONAL EXERCISES
Your clients will find it easier to learn modifications of exercises they already know than to learn totally new procedures. Such modifications also may be more acceptable to "experienced trainers" than if you try to convince them to change their ways completely. Remember that in every case your clients should begin with their abdomens hollowed and their lumbar spines in neutral position. Except where otherwise noted, have your clients perform 8-10 reps of each exercise once a day, three days per week. Except where otherwise noted, the initial movement of each exercise should take about 2-3 seconds; your clients should hold the position for 1-3 seconds; then should perform the reverse movement in 2-3 seconds. Note, however, that these are mere guidelines. If at any time your clients are not working hard enough, increase the overload by slowing down the exercise or increasing the number of repetitions. If they are working too hard, reduce the overload. As your clients become more proficient at a given exercise, they can increase the number of repetitions, perform the movements more slowly, and/ or increase the time for the holding period. Remember to emphasize to your clients that, when moving slowly, they must breathe normally (no holding their breaths!). The limiting factor is not how many times individuals can superficially perform an exercise-but rather how well they can do it while stilI maintaining
Modifications
proper spinal alignment
and abdominal
hal/owing.
of the Sit-Up
Bending the knees and hips to alter the starting position of the sit-up affects both passive and active actions of the hip flexors, and the biomechanics of the lumbar spine. Supine lying stretches the iliopsoas, aligning it with the horizontal (figure 6.3). As the muscle contracts in this position,
Basic Abdominal Muscle Training.
125
trunk lifting is at a mechanical disadvantage and vertebral compression is at its greatest-the ratio of lifting to compression is approximately 1:10 (Watson 1983). Flexing the knees pulls the iliopsoas more vertically, reducing the ratio of trunk lifting to vertebral compression to 2:5 in crook lying and 1:1 in bench lying. If flexion historically has exacerbated clients' back pain (consult with their physical therapists on this), they can use fewer repetitions (2 or 3) while increasing the exercise timing (8-12 seconds in each direction). This schedule reduces the number of flexion movements but maintains the overload on the muscle. With 450 hip flexion, tension in the iliopsoas is 70-80% of its maximum; with the hips and knees flexed to 900,the figure reduces to 40-50% Gohnson and Reid 1991). Note, however, that the iliopsoas develop passive tension due to elastic recoil. Since the iliopsoas are not fully stretched when the hips are flexed, they cannot passively limit the posterior tilt of the pelvis. Instead, to fix the pelvis and provide a stable base for the abdominals to pull on when the hips are flexed, the hip flexors contract earlier in the situp action. This contraction has reduced intensity (Walters and Partridge 1957), however, due to the length-tension relationship of the muscle.
Pull of iliopsoas
Trunk
lifting 1:10
t~
.
Vertebral compression 2:5
1:1
Figure 6.3 Flexing the hip lengthens the moment arm of the iliopsoas, enabling the muscle to complete the sit-up action with less force. Thus, verte. bral compression is reduced. From Norris 1998.
126
. BackStability
With the legs straight in the traditional sit-up position, the iliopsoas are stretched and can passively limit posterior tilting of the pelvis. The stretched position also enables the iliopsoas to exert greater force during hip flexion-which means that, if the abdominal muscles are too weak to maintain the position of the pelvis, the stronger hip flexors will hyperextend the lumbar spine and cause the pelvis to tilt forward, thus lengthening the abdominals and hyperextending the lumbar spine. This type of action is therefore unsuitable for postural re-education if the aim is to shorten lengthened abdominal muscles.
Bent Knee Sit-Up .1I.m.
To strengthen the abdominals while reducing the action of the hip flexors.
Have your client begin with the crook lying position, knees flexed to 90° and hips flexed to 45°. He should lift his trunk, moving from the hip alone, and either at the same time or slightly later should flex his hips. Suggest that he imagine himself as a hinge pivoting on the hip joint. The action must be slow and controlled, without strain. A pure bent knee sit-up requires keeping the spine straight, moving it around the fixed hip, and reducing the action of the hip flexors. Tell your client that, if he feels his back muscles straining instead of his abdomina Is, he should stop the exercise and perform abdominal hollowing before resuming the exercise.
Trunk Curl .''117.'. To shorten and strengthen the rectus abdominis. In this exercise there is no hip flexion, the lumbar spine remaining in contact with the supporting surface. Have your client assume the crook lying position, knees flexed to 90° and hips flexed to 45°. continued
Basic Abdominal Muscle Training'
127
Trunk Curl, continued
Instruct him to "roll through the spine," performing cervical flexion until the chin comes toward the chest, followed by thoracic flexion, until only the lumbar spine remains on the supporting surface. He then should reverse these actions, first lowering the thoracic spine from bottom to top and finally releasing the cervical spine so that the head is gently lowered back onto the supporting surface.
Bench Curl .f{17.:.'" To strengthen the upper abdominals (supraumbilical portion of rectus abdominis with the lateral fibers of external oblique) while reducing the pull of the hip flexors and lessening the stresses on the lumbar spine. The bench curl is performed from a starting position of 90° flexion at both the hip and the knee, with the calves supported on a bench or chair. Since shortening the hip flexors in this way reduces their ability to contribute to the movement, hip flexor action does not obscure the action of the abdominals. Instruct your client to "roll through the spine" just as in the trunk curl.
Modifications
of the Straight-Leg Raise
As none of the abdominal muscles actually crosses the hip, these muscles are not prime movers for the SLR. The SLR is nevertheless important for abdominal training because it enhances the pelvic stabilizing function of the infra umbilical portion of the rectus abdominis and lateral external oblique. Several modifications of the bilateral straight-leg raise can help reduce stress on the lumbar spine.
128
.
Back Stability
Heel Slide (see also discussion of this action in chapter 8) .f'[,,~,.
To statically overload the abdominal muscles, increasing the emphasis on the deep abdominals.
Have your client assume a crook lying position, then straighten one leg while keeping the heel on the ground and sliding the leg into extension. Instruct her to place her hands over her lower abdomen on either side of the navel, her fingertips 5-6 inches apart. She should perform abdominal hollowing and keep the abdominal muscles tight beneath her hands as she slowly performs the leg action over a period of about 3-5 seconds (see page 170).
Leg Lowering .fI'l'1.
To increase the static overload on the abdominal while maintaining a neutral spine.
Instructyourclienttoliesu-
muscles
-
pine with hips flexed to 90° but with the knees extended so that the straightened legs are vertical. Tell him to slowly lower his legs until the pelvis begins to tilt. As soon as this occurs, he should raise the legs again to 90° hip flexion. Each cycle should take about 3-5 seconds. The advantage of this exercise over the standard straight-leg raise is one of changing leverage. With the standard leg raising action, the subject starts with maximum leverage on the leg, forcing the hip flexors and abdomina Is to work maximally from the very beginning. With leg lowering, the starting position provides minimum leverage. As the legs are lowered away from the vertical, leverage increases-but the subject is able to control the descent of the legs and avoid the position of maximal leverage that would cause the spine to hyperextend. Should a client find the leg lowering difficult to control, tell him to bend his knees in order to reduce leverage on the leg; or have him perform the exercise close to a wall, so he cannot fully lower the legs.
Basic Abdominal Muscle Training
.
129
Bench Lying Pelvic Raise .fI.1~'"
To strengthen the abdominal muscles, especially the lower (infraumbilical) portion of rectus abdominis.
Instruct your client to lie supine and flex both hips and knees 90o-a position she will main, tain throughout the movement. 5he should place her arms by her sides, hands flat on the table or floor. Have her lift her buttocks from the ground by flexing her lumbar spine, while keeping her legs relatively inactive. Although in this movement the lumbar spine is flexed as with the trunk curl, the movement occurs from "below upward" with the L551 joint moving first followed by flexion of each successively higher lumbar segment. The trunk curl provides the reverse movement (above downward) (McKenzie 1981).
i(........
~~~o /
Wall Bar Hanging Leg Raise .fll1~'" To strengthen the lower rectus, with increasing leg leverage, while providing traction for the lumbar spine. Performing leg raises while hanging from a wall bar considerably reduces the leverage forces on the lumbar spine and provides traction. Explain to your client that he must hold a neutral pelvic position throughout all versions of this exercise, preventing anterior tilt of the pelvis, and (except in the last variation) pressing the small of his back into the wall bars. There are three forms of the exercise: 1. Instruct your client to stand with his back against the wall bar, place his arms overhead, and hold onto a bar above head height. Then, avoiding any jerking action, he should slowly take his weight onto his arms and, keeping his legs straight, raise his feet slightly off the ground (a). Tell him to feel the stretch through the whole of his spine-and to tighten his abdominal muscles while pressing his lower back into the wall bar and breathing normally. Instruct him to hold this position for 2-3 seconds, and then release it slowly. continued
130
.
Back Stability
Wall Bar Hanging Leg Raise, continued
b
a
2. The action then progresses to include hip and knee flexion. For this exercise, instruct your client to bend his knees and raise them until he has achieved 90° hip flexion (Le., knees level with hips), while still keeping the lumbar spine in contact with the wall bars. Be sure that he doesn't jerk his knees up-the movement should be slow, lasting about 3-5 seconds. Suggest that he focus his attention on his abdominal muscles, pulling them in as he moves his legs. After holding the 90° flexed position for 2-3 seconds, he should slowly lower his legs to the starting position. 3. The final progression of this exercise requires flexing the lumbar spine to lift the back away from the support of the wall bars. This action, while working the abdominals hard, also strengthens and possibly shortens the hip flexors. Once your client has reached the 90° flexed position as in the previous exercise, instruct him to round his spine in order to slowly lift his tailbone away from the wall bar (b). Emphasize that, in the reverse movement, your client must not allow his body to "fall" and strike his tailbone hard onto the wall bar.
AB ROLLER
EXERCISES
The ab roller can help your clients re-educate their muscles for the trunk curl action (spinal flexion) as distinct from the sit-up movement (straight spine moving on a fixed femur). The frame allows only trunk flexion, while the subject's lumbar spine remains in contact with the ground.
Basic Abdominal Muscle Training
.
131
Basic Crunch .,{l7~'.
To work the abdominal muscles in general, with increased emphasis on inner-range activity of the upper abdominals.
Instruct your client to lie on her back with her knees bent and feet flat on the floor (crook lying), her head and neck on the neck rest of the machine. She should either grasp the centers of the curled handles at the sides of the device's arms or hold her arms straight with her wrists against the horizontal piece that connects the handles-whichever is more comfortable for her. Tell her to curl her trunk ("basic crunch"), keeping her head on the pad and gently assisting the movement by extending the shoulder. Her focus should be on pulling the abdominal wall in (hollowing). There is a tendency with this exercise for people to rapidly "pump" the movement-an error that adds considerable momentum to the spine and may forcibly overstretch the posterior tissues. Make sure that the exercise stays slow and controlled, following the earlier-stated principle that each movement should last 2-3 seconds. With time, your client will gain sufficient control to rest her elbows on the machine pads and press down with her elbows (shoulder extension), gripping only lightly with her open hand on the machine frame.
Reverse Crunch .f{t7~'.'ntense
strengthening
for the lower rectus abdominis.
This action emphasizes the lower portion of rectus abdominis. Instruct your client to raise her legs (one at a time) into a vertical position and maintain this position throughout the exercise. The exercise action is to vertically lift the leg as though trying to reach the toes to the ceiling, while keeping the upper body still. In so doing, she will lift her sacrum from the floor, a movement which combines posterior pelvic tilt with lower lumbar flexion. The movement must be slow and controlled with no lunging or bouncing.
132
.
Back Stability
Double
Crunch
.1'['7.:.'"To strengthen the upper and lower rectus abdom;n;s. The double crunch movement combines the actions of the trunk curl and the leg raise, working both the upper and lower portions of the rectus abdominis. Since two body areas work together for this exercise, it requires a greater degree of coordination than the other crunches. Starting position is the same as that of the basic crunch. Instruct your client to simultaneously (1) raise her knees toward her chest, posteriorly tilting the pelvis; and (2) raise her upper body (as in the basic crunch) to flex the spine. The lumbar spine remains on the floor, while the shoulders and sacrum both lift off the floor. She should perform the action slowly and precisely, avoiding the excess momentum on the spine that rapid "pumping" actions cause. Make sure that she neither holds her breath nor hyperventilates (breathes too rapidly). If she does hyperventilate, she should rest on her side and not attempt to stand up until the lightheadedness has passed.
Side Crunch .1'[.7.:.'" To strengthen the oblique abdom;nals the rectus abdom;n;s.
wh;le also working
Have your client begin in the basic crunch position, then lower her knees to one side; she should raise her arms up straight and cross them, her wrists resting on the horizontal bar as in one version of the basic crunch. Instruct her to perform, from this altered starting position, the same actions as in the basic crunch-to curl her trunk, keeping her head on the pad. Since asymmetry is common in this body region, your client may find that one side is stronger or more flexible than the other; as she continues with this exercise (assuming she uses correct form), the asymmetry should resolve and both sides should perform equally.
Basic Abdominal Muscle Training.
133
SUMMARY
· · · · ·
Popular abdominal exercises can be only moderately effective, or even dangerous, for some people with lower back injuries. Poorly conditioned individuals tend to place emphasis on the wrong muscles to perform straight-leg raises and sit-ups; modified versions of these exercises force them to use the correct muscles. Poorly conditioned subjects, or those with a history of back pain, should avoid straight-leg abdominal exercises altogether. It is generally more productive for you to introduce your clients to modifications of exercises they already know than to try to teach them totally new movements. This chapter introduces specific abdominal exercises that are both safe and maximally effective for functional abdominal training.
7 Posture Because postural alignment reflects changes in muscle length, it is the first form of assessment you will generally use to determine muscle imbalance. Before you can diagnose changes in alignment, however, you need a standard of optimal posture. The body moves continually around the optimal position in a process called body sway, and back stability is an essential component of this mechanism. In this chapter, I describe four principal types of posture.
OPTIMAL
POSTURAL
ALIGNMENT
Posture is the arrangement of body parts in a state of balance that protects the supporting structures of the body against injury or progressive deformity-a definition given in 1947 by the Posture Committee of the American Academy of Orthopaedic Surgeons (Cailliet 1983). A good posture is therefore effortless, nonfatiguing, and painless when the individual remains erect for reasonable periods (Cailliet 1981). Muscles function most efficiently in such an alignment, and the joints are optimally positioned (Bullock-Saxton 1988). Optimal posture combines both minimal muscle work and minimal joint loading. It is the combination of these two factors that is important-where optimal posture is lost (for example in "slouched standing"), the muscle activity is clearly reduced, but there is a significant increase in joint loadmg. Minimizing joint loading over time is important-articular cartilage gains its nutrition through intermittent loading (Norris 1998), and an even distribution of force is preferable to point pressure. Contact pressure is directly proportional to the transmitted force, but inversely proportional to area (McConnell 1993). Distributing force over a larger area by optimizing segmental alignment, therefore, reduces joint surface compression and lessens the risk of degenerative changes to a joint. The aim of any posture should be to reduce total energy expenditure and lessen stress on the supporting body structures. 134
Posture
.
135
_ Terms-You Shoultl Know ~ lateral malleolus the lower end of the fibula that forms the projection of the ankle tragus cartilaginous projection over the external opening of the ear
A good posture reduces total energy expenditure I and lessens the stress on the supporting body structures.
KEY POINT:
-
-
-
Any change in the alignment of one body segment automatically causes neighboring segments to move in an attempt to maintain stability. If one body segment moves forward, for example, another must move backward to keep the line of gravity of the body (LOG) within the base of support (figure 7.1). Over time, changes in force per unit area cause tissue adaptation (Norkin and Levangie 1992). Changes in serial sarcomere number within muscles (see chapter 5), for example, are adaptations to postural changes over time. Shortening ligaments lead to reduced range of motion, while lengthening ligaments reduce a joint's passive stability. Static posture-when the body is stationary-reflects the alignment of body segments and can reflect both changes in load distribution across joints and resting muscle length. Such postures include standing, sitting, and lying. Dynamic posture-body position during movement-can give information about body segment alignment, muscle actions, and motor skill. Typical dynamic postures are walking, running, jumping, and lifting. You can use both description of position (kinematic) and of force (kinetic) to assess posture.
POSTURAL
STABILITY
AND BODY SWAY
When standing erect, the human body has a small base of support due to its bipedal stance and comparatively high center of gravity (approximately
m m ctJ
-0
o ctJ-
Figure 7.1 When one body segment moves out of alignment, a neighboring segment moves in the opposite direction to maintain the line of gravity within the base of support.
136
.
Back Stability
at the second sacral segment). Humans are thus relatively unstable in comparison with quadrupeds with their larger base of support and lower center of gravity. Maintaining an erect posture takes surprisingly little energy, however, as a result of constant motion brought about by postural control. This motion (postural sway) depends on kinesthesis, or "motion sense" (Kent 1994), which enables us to detect the position of our body parts through organs of proprioception, vision, the vestibular apparatus in the inner ear, and skin receptors. Normal postural sway consists of a small continuous motion in the sagittal plane. This oscillation of the center of gravity results from alternating muscle activity-possibly a relief mechanism to reduce lower-limb fatigue and to aid blood flow (BullockSaxton et al. 1991). Excessive postural sway generally reveals poor balance and stability, a situation commonly seen in the elderly and inactive. Heavier people also may exhibit greater body sway (Sugano and Takeya 1970), as may taller individuals (Murray et al. 1975).Training usually can reduce postural sway. In the elderly, strength training may improve stability and limit postural sway (Hughes et al. 1996); following ankle injury, postural sway increases. By using balance and coordination training, body sway may be reduced to normal values once more (Bernier and Perrin 1998). Levels of postural sway can predict risk of recurrent falls among frail nursing home residents (Thapa et al. 1996). Lord and colleagues (1996) reduced fracture risk in women (ages 60-85) using a general aerobic exercise program whose effect was to improve postural sway rather than to change bone density.
BASIC POSTURAL ASSESSMENT You can assess static posture through comparisons to a standard reference line (Kendall et al. 1993), which represents the line of gravity. A weight board can help identify both the center of gravity (COG) and the vertical extension of this point to the ground (line of gravity). Find the horizontal distance from the edge of the board to the subject's line of gravity (d) by multiplying the combined weight of subject and board by the total length of the board (L) and dividing the result by the subject's body weight (W). See Luttgens and Wells (1982) for full details of this method. As the vertical extension of the COG, the LOG must pass within the body's base of support to maintain stability. The closer the body segments are to the LOG, the less torque there is around a joint. Where the LOG passes through the joint axis, no torque is created around that joint. If the LOG passes some distance from the joint axis, gravitational torque would tend to move the body segment toward the line of gravity were the segment not counterbalanced by elastic recoil of soft tissue and muscle action (Norkin and Levangie 1992). With the LOG anterior to the joint axis, the
Posture
.
137
proximal segment of the body connected to the joint tends to move anteriorly (figure 7.2); posterior motion tends to occur when the LOG is posterior to the joint axis. In the standard posture (viewed from the side), the subject is positioned with a plumb line representing the LOG, passing just in front of lateral malleolus (the bulge on the outside of the ankle). In an ideal posture, this line should pass just anterior to the midline of the knee and then through the greater trochanter, bodies of the lumbar vertebrae, shoulder joint, bodies of the cervical vertebrae, and the lobe of the ear (figure 7.3). Since the LOG is anterior to the ankle joint, gravity is continuously pulling the tibia anteriorly. This would result in enough dorsiflexion to unbalance the body were it not for constant opposing resistance provided by muscle action from the soleus (Nor kin and Levangie 1992). The LOG passes in front of the knee joint axis (but behind the patella), forcing the femur anteriorly and creating an extension torque resisted by the posterior knee structures. Table 7.1 shows the gravitational torques created by the position of the LOG and the opposing structures resisting these torques. When viewed from the front, with the feet 3-4 inches (10 cm) apart, the LOG should bisect the body into two equal halves. The anterior superior iliac spines (ASIS) should be approximately in the same horizontal plane, and the pubis and ASIS should be in the same vertical plane (Kendall et al. 1993). This alignment defines the neutral lumbar-pelvic alignment, which typically is about 5° to the horizontal. The joint axes of the hips, knees, and ankles should be equidistant from the LOG, and the LOG should transect the vertebral bodies (Nor kin and Levangie 1992). The gravitational torque imposed on one side of the body should equal that of the other side. Anatomical landmarks that provide comparisons for horizontal level on the right and left sides of the body include the knee creases, buttock
Gravity line Figure
7.2 When the gravity
line falls outside
segment tends to move toward the gravity line.
a joint,
the proximal
body
138
. BackStability
Figure 7.3 The standard reference line for posture. Reprinted, by permission, fromJ.C. Griffin, 1998, Client-centered exercise prescription (Champaign, Il: Human Kinetics), 66.
creases, pelvic rim, inferior angle of the scapulae, acromion processes, ears, and the external occipital protuberances. You also can observe alignment of the spinous processes and rib angles; minor scoliosis becomes more evident when assessed in Adam's position (forward flexion in standing). Unequal distances between arms and trunk (referred to as the keyhole), various skin creases, or unequal muscle bulk should prompt you to closer examination. You should also assess foot and ankle alignment. Figure 7.4 provides a simple checklist for postural assessment in the clinic. View the subject from behind and assess the symmetry of each of the body parts shown in the first column of figure 7.4 by comparing the right and left sides of the body. Record your observations in the section headed Notes (e.g., "head tilted to right," "left shoulder higher than right," or "left scapula lower"). These notes will highlight the region of the body that requires local testing of muscle length and joint movement by yourself or another therapist. Another way to assess static posture is to use a posture grid. The posture grid again uses a plumb line as a reference, but the subject stands behind a screen divided into 10-cm squares to aid inspection of body part alignment. To ensure reliability of the plumb line assessment for a given client, you must perform it at the same time of day to help remove diurnal variability (Tyrrell et al. 1985). Have subjects stand with their feet 10 em apart. They should walk on the spot (10
Posture
Table 7.1
Normal Alignment
in the Sagittal
Joints
Gravitational torque
forces
Passive opposing forces
Active opposing forces
Ligamentum nuchae; tectorial membrane
Posterior neck muscles
Cervical
Flexion Anterior Anterior to transverse axis for flexion and extension Extension Posterior
Thoracic
Anterior
Flexion
Posterior longitudinalligament; ligamentum flavum; supraspinous ligament
Lumbar
Posterior
Extension
Anterior longitudinalligament
Sacroiliac Anterior joint
Flexion type motion
Sacrotuberous ligament; sacrospinous ligament; sacroiliac ligament
Hip joint
Posterior
Extension
Knee joint
Anterior
Extension
Iliofemoral ligament Posterior joint capsule
Ankle joint
Anterior
Dorsiflexion
Atlantooccipital
13 9
Plane Opposing
Line of gravity
.
Anterior longitudinalligament Extensors
Iliopsoas
Soleus
Reprinted, by permission, from c.c. Norkin and P.K.Levangie, 1992, Joint structure and function: A comprehensive analysis, 2d ed. (Philadelphia: Davis). paces) and then come to rest, to aid general body relaxation. Instruct your clients to maintain their "normal" posture rather than to seek to modify or improve it. You can refine whole-body posture analysis by measuring alignment of individual body segments. You can assess pelvic tilt with a pelvic inclinometer, which measures the angle of pelvic tilt relative to the horizontal. The inclinometer consists of a protractor mounted on a base plate and attached to a pair of bone calipers. The inclinometer reads 0° when the caliper arms are horizontal. The end of the arms are positioned over the posterior superior iliac spine and the anterior superior iliac spine of one side of the body. The inclinometer dial shows the angle of pelvic tilt in the
Position
of body part
Head
Shoulder
Notes
position
level
Position of shoulder blade alignment
Skin creases at waist and spinal alignment
level
of bullock creases
level of knee creases
Calf muscle bulk and Achilles alignment
Flat foot or high arch
Figure
7.4
Assessing
standing
posture
from
From C. Norris, 199B, Diagnosis and management, Heinemann). Reprinted by permission of Butterworth of Reed Educational & Professional Publishing Ltd.
140
behind. 2d ed. Heinemann
(Oxford: Butterworth Publishers, a division
Posture
.
141
sagittal plane. This method of assessing pelvic tilt appears to be accurate to within::!: %0 (Toppenberg and Bullock 1986). Inclinometers are highly reliable and quite valid in comparison with lateral radiographs (Crowell et al. 1994). Pelvic tilt and lumbar lordosis are intimately linked, with changes in pelvic tilt causing significant alteration in the depth of the lordosis (Day et al. 1984). Bullock-Saxton (1993) demonstrated that inclinometer measurement is repeatable in both normal and symptomatic females: subjects were measured three times on a single day with three-minute intervals between consecutive tests, and then over three separate days with a four-day rest period between each test. You can use a flexible ruler to measure the depth of lordosis. Locate the spinous process of the second sacral segment (52), which lies between the posterior superior iliac spines. Palpate each spinous process from 52, counting back to the first lumbar vertebra (Ll) (figure 7.5). Record the length
L1
L2
L3
L4
L5
Figure 7.5 S2 lies between the posterior superior iliac spines. Palpate each spinous process cephalically from S2 up to L1. Use a flexible ruler to assess the depth of lumbar lordosis.
\
142
. Back Stability
(radius) of the traced curvature (L) of the lordosis from Ll to 52 and the depth of the lordosis (H) from the line joining Ll-52 to the deepest part of the lordotic curve, as shown on figure 7.5. Calculate the lordotic index (8) using the arctan formula, 8
=4 arctan(2H/L).
Arctan is a trigonometric term that can be calculated on most scientific calculators or computer spreadsheet programs. The flexible ruler method of assessing lordosis is highly reliable, as verified by lateral radiographs (Hart and Rose 1986; Lovell et a1. 1989). Lordosis measured in this manner showed average (mean) values of 50.9° in normal individuals and 40.4° in subjects who demonstrated lower abdominal weakness, confirmed as an inability to maintain alignment on supine leg lowering tasks (Levine et a1. 1997). Detect head position relative to trunk position with a stadiometer, an apparatus used to measure horizontal displacement of body segments relative to each other. The stadiometer consists of two or more sliding arms mounted on a vertical frame. The arms may be raised or lowered to the level of the body segments being measured, and then adjusted forward and backward (horizontally). A scale on the side of the horizontal arm shows the distance of each body segment from the vertical arm. Record the craniovertebral (CV) angle by measuring the degree of forward shift of the head, which pulls the suboccipital region into hyperextension (Watson 1994). The CV angle is that formed between a horizontal line through the C7 spinous process and the tragus (the prominence on the inner side of the ear) (figure 7.6). The average CV angle in asymptomatic subjects is 50° (range 48.6-52.0°); people who complain of cervical headaches have reduced angles (44.3°) (Watson 1994), indicating a head-heldforward posture as described by McKenzie (1990).
Figure 7.6 Using a stadiometer
to measure the craniovertebral
(CV) angle.
Posture.
143
Local "low-tech" measures of posture can be valid, reliable, and reproducible.
KEY POINT:
PRINCIPLES
OF POSTURAL
CORRECTION
Correcting posture requires a combination of several factors, embracing the approach to muscle imbalance described in chapter 5. Shortened muscles must be stretched, and lengthened muscle shortened. Static and PNF techniques can stretch muscles, while inner-range holding techniques can shorten lengthened muscles and build postural holding time. You must use principles of motor skill training (Norris 1998). Make use of the three stages of motor skill training to help your clients regain segmental control (table 7.2). In the cognitive stage, your client must learn objectively the requirements of a skill. In terms of postural reeducation, this often involves passive positioning of optimal postureyou place your clients passively into the optimal postural alignment by correcting pelvic tilt, for example, and instruct them to hold this position. This passive positioning is repeated several times until your clients are able to recreate the optimal position themselves. This signifies that they have progressed to the second stage of skill training (motor). During the second stage, the key factor is that individuals can identify their own mistakes. In the case of posture this means that they can consciously move into the optimal posture. Once they have achieved this ability, they are ready to perform a home-exercise program designed to build endurance Table 7.2
Stages of Motor Skill Learning
Cognitive
Motor
Automatic
.Movement "runs by movement . Stage of understanding .Effective itself' now obtained .tion Independent of atten. Movement more .Environmental cues important demands consistent . Action very fast . Use information from . Able to identify own past experiences . Poorly coordinated .mistakes Proprioception more important than visual . Unable to identify own mistakes
. .
Visual/verbal cues more important than proprioceptive Much coaching
needed
144
. Back Stability
of the postural muscles. Only after many thousands of repetitions of a movement will a person move into the third and final stage of motor training (automatic). Now, he is able to maintain an optimal postural alignment without conscious control because the action has become automatic. The process of learning to drive a car illustrates the three stages of motor learning. When we first learn to drive, the actions are difficult and we must concentrate on many separate activities. The actions become easier with repetition, as we begin to integrate the independent actions into a whole. Eventually, driving becomes largely automatic. Similarly, the separate components of postural control must be corrected individually and then pieced together to form a more complex single movement. By dividing the total movement into a number of component sequences, you can help your client learn the action more easily. Correcting a posture so that the correction becomes automatic is extremely difficult. If poor posture is held by shortened tissue, stretching can sufficiently lengthen tissue so that posture can change permanentlyassuming that the tissue is not allowed to shorten again through poor postural alignment. If poor posture is the result of muscle weakness brought on through injury (wasting or pain inhibition), muscle strengthening may successfully optimize posture. For many cases of poor stability, progressive exercises and proprioceptive training can effectively enhance stability and produce positive postural changes. When posture has been suboptimal for many years, however, full correction probably is not possible. Certainly improvements can be made, and these may be clinically significant (especially in relieving pain), but they will be limited. As an example of postural re-education, consider how you might treat common lordotic posture. This posture combines lack of active lumbar stability, lengthening of the rectus abdominis, and shortening of both hamstrings and hip flexors; moreover, the gluteus maximus often is poorly recruited. Re-education begins with stabilization training for the back, emphasizing use of the deep abdominals. Once your client has enhanced her basic stability, she should stretch her hamstrings. She could then combine the two separate activities, using a hamstring stretch in sitting position while maintaining spinal alignment. Following work to improve recruitment of the gluteals, stretch the hip flexors, and shorten the rectus abdominis, she should begin whole-body postural re-education using standing, walking, and sitting movements. Finally, she would begin proprioceptive training as described on page 197. Especially in the early stages of learning, you could use taping to give your client feedback. The taping performs two functions: First, structural taping or bracing can support a hypermobile segment of the body; second, functional taping can provide tactile feedback. In the latter case, skin
Posture.
145
drag will remind your client that her posture has moved away from the optimal alignment (place breathable undertaping under zinc oxide tape to protect the skin) (Norris 1994b).
POSTURE TYPES AND HOW TO CORRECT THEM There are four classic abnormal posture types (figure 7.7). In the lordotic posture, the main feature is excessive anterior pelvic tilt (a). Anterior displacement of the pelvis characterizes the swayback (b), while the flatback has slight posterior pelvic tilting and loss of lumbar lordosis (c). In the kyphotic posture the thoracic curve is excessive (d).
lordotic
Posture
In the classic lordotic or "hollow back" posture, the greater trochanter remains on the LOG, but the pelvis tilts anteriorly, moving the anterior superior iliac spine (ASIS) forward and downward in relation to the pubic bone. The abdominal muscles and gluteals are typically lengthened and have poor tone. Over time, the hip flexors may shorten, and pelvic tilt is limited by tightness in the overactive and tight hamstrings (Jull and Janda 1987). In an extreme lordotic posture seen in chronic obesity, the lumbar spine rests in extension with the lumbar facet joints impacted; the elastic recoil of the hamstrings allows the pelvis to hang. Janda and Schmid (1980) call this posture the pelvic crossed syndrome: high contact pressures occur in the facet joints, with the inferior articular processes impinging on the lamina
)
a Figure
7.7 Classic abnormal
(c) flatback;
and (d) kyphotic.
d
c
b
posture
types:
(a) lordotic;
(b) swayback;
146
.
Back Stability
below. Increased weightbearing of the facet joints in turn reduces the compression force on the lumbar discs (Adams et al. 1994). Lordotic posture is common in dancers and in young gymnasts, for whom it is a requirement of the sport. It is the posture most noticeable in women after childbirth, especially multiple births. In the case of childbirth, however, lengthening of the rectus abdominis through serial sarcomere adaptation is accompanied by diastasis, which mayor may not resolve spontaneously. Correction of lordotic posture requires shortening the abdominal muscles and lengthening the hip flexors. The rectus abdominis must be shortened by combining a posterior pelvic tilt with spinal flexion-but only after developing effective deep abdominal muscles to prevent bowstringing, where the abdominal muscles contract and bulge outward instead of pulling flat. This is different from the diastasis that occurs during pregnancy. With bowstringing there is no long-term structural change in the muscle, nor does the linea alba (the tendinous line between the two rectus abdominis muscles) split.
Modified Trunk Curl .f{t7~,. To shorten and strengthen the rectus abdominis muscle. The modified trunk curl action can help correct lordotic posture. Where full inner-range motion is lacking due to muscle lengthening, your client can perform the modified trunk curl in progressive stages. In stage 1, he lies supine with the knees bent and then posteriorly tilts his pelvis. Then have him curl up as far as he is able, combining spinal flexion with posterior pelvic tilt to fully shorten the rectus abdominis muscle. For stage 2, your client needs assistance either from you or from himself. You can gently pull your client into a slightly higher position, or he can pull himself higher by gripping his thighs. The extra lift should be no more than 1 or 2 inches (2.5-5.0 cm) and must be performed slowly and with care to avoid jolting the spine. Have your client hold the upper position with an isometric contraction for stage 4 (stage 3 is for those who can't perform stage 4), gradually building up the holding time from 1-2 seconds to 4-5 and finally to 10 seconds, at all times breathing normally. Individuals unable to hold the upper position should practice eccentric lowering, which represents stage 3: after they are lifted into the upper position and released, they should slow their descent back to the floor as much as possible. Initially they may almost fall back to the floor in less than 1 second. With practice, they should be able to lower themselves more slowly, taking 1-2 and then 4-5 and finally a full 10 seconds to lower continued
Posture
.
147
Modified Trunk Curl, continued
themselves. When they have achieved this level of strength, they can progress to holding the full upper position as for stage 4. How will you know if the abdominal muscles are lengthened and require shortening by this full inner-range holding method? In chapter 5, we saw that the length-tension curve moves to the right for lengthened muscles (see figure 5.8, page 101), indicating that they are unable to hold a joint at full inner range (i.e., to close the joint fully). When your clients perform the trunk curl, they are attempting full spinal flexion. If, in an attempt to pull the spine into full flexion, they fall back away from the inner-range position while performing the extra lift (with your help or by pulling on their thighs), you can safely conclude that the muscle is lengthened and requires this type of training to shorten it. Normally, full-range flexion of the spine is not recommended for general back care. Individuals with lordotic posture, however, have been maintaining the lumbar spine in extension. Full flexion is therefore a treatment of choice for such individuals and is widely used within physical therapy practice (McKenzie 1981).
Gluteus Maximus Inner-Range Exercise _fl,,,.,.
To contract and fully shorten the gluteus maximus.
The gluteus maxim us muscles must be tightened and shortened by working them in inner range (page 104). Have your client lie prone and flex one knee to 90°. She should then extend her hip, trying to emphasize the action of the gluteal muscles. If she is unable to lift the leg into full inner range, lift the leg for her. Then she should try either to hold this position (isometric) or to control the leg as it descends (eccentric). She eventually should attain full inner-range holding ability, with holding times built up from 3-5 seconds to 30-60 seconds. Take a gradual, progressive approach for those who are unable to lift the leg, always remembering to adapt the program to your client's individual level of progress. Begin with muscle re-education, encouraging your client simply to contract the gluteus in prone lying. Use of EMG feedback and manual muscle stimulation is helpful at this stage if the individual is completely unable to perform a static contraction. Tapping or brushing the gluteus with the fingers adds to multisensory cueing, making the task easier by increasing the amount of information that accompanies the movement. By making the contractions forceful, your client can increase the holding time until she can contract and hold the muscle for 10 seconds. Once she can do that, the next step is to lift the continued
J48
.
Back Stability
Gluteus Maximus Inner-Range Exercise, continued
femur into 10-150extension and place the knee on a block or cushion to maintain the extended hip position. She then contracts and holds the muscle as before, but in this new starting position. Eventually, she will develop sufficient strength so that you can remove the cushion and ask her to hold the extended position by herself. If your client is unable to hold this nonsupported position, have her use eccentric lowering. After you have raised her hip into 150extension, instruct her to hold it there as you release the leg. Encourage her to use the same intensity of muscle contraction as for the first two movements. If she is unable to hold the leg into extension (i.e., off the examination table), she should try to lower it in a controlled way rather than allowing it to drop. Have her gradually increase the time required to lower the leg to at least 10 seconds. The next stage is for your client to forcibly contract the gluteal muscles and simultaneously try to lift the leg off the table into extension. Suggest that she bend the knee to reduce the hamstrings' contribution to extension. Begin with 2-5 repetitions, lifting the leg as high as possible without allowing the pelvis to tilt. Try placing your hand just above your client's heel on the lifting leg and then encouraging her to lift the leg until her heel touches your hand. The final progression is first to lift the leg to full extension and hold this inner-range position for a full 10 seconds and then to perform 10 repetitions of this movement. If clients have both poor tone in the gluteals and poor control of hip extension in the prone position, have them begin a progression of exercises leading toward the goal of performing 10 repetitions, with each contraction held 10 seconds, at each exercise session. For the first week, they should perform the exercises only every other day to reduce the likelihood of muscle soreness. They should perform 2 sets of 10 repetitions, one in the morning and one in the evening, for the first two exercise days, then 3 sets (morning, late afternoon, and evening) on the next two exercise days. Instruct clients to work gradually on increasing reps and holding time-perhaps starting with 3 repetitions, held as long as possible, then alternating between adding to the number of reps and increasing the holding time. Once they can hold a full contraction in both prone position and in extension, they should do the exercises 10 times twice per day for two days followed by 10 reps three times per day for two days. They should take a full day's rest after each four-day cycle. They should follow the sequence of 2 sets/ day for two days, then 3 sets/day for two days, followed by one day of rest, for each progression until they can consistently perform 10 reps at each session, holding each rep for 10 seconds. continued
Posture
.
149
Gluteus Maximus Inner-Range Exercise, continued
Although this kind of inner-range exercise may shorten the previously lengthened rectus abdominis and gluteus maxim us, excessive pelvic tilt will be corrected only if the tight hip flexors are stretched to release the pull on the pelvis through the iliacus muscle. Tightness of the hip flexors (if due to increased muscle tone rather than to adaptive shortening of connective tissue) inhibits the activity of the hip extensors through a process called pseudoparesis Oanda 1986). When this is the case, an individual must reduce muscle tone in the hip flexors before engaging in exercises to strengthen the hip extensors. The Thomas test (page 114) can show if the hip flexors are tight and whether the rectus femoris or iliopsoas is the tighter muscle. You also can prescribe the Thomas test for initial stretching of the hip flexors, later using the half lunge to combine lumbar stability with hip flexor stretching.
Half Lunge (without chair-see .I{el".
To stretch
page 114)
the hip flexors while maintaining
back stability.
Instruct your clients to assume a half-kneeling position and to tighten their abdominal muscles (using a hollowing action) to stabilize the pelvis. From this position, they should press the pelvis forward to force the trailing hip into extension. Providing the pelvis is not allowed to anteriorly tilt, the hip flexors will be stretched. Prescribe twice-daily exercise for four days, 10 repetitions per session, holding the position 20-30 seconds for each repetition. Instruct your clients to rest for a day, then repeat the four-day cycle until they have gained the desired range of motion, or until range improvement has stopped. The long-term maintenance exercise schedule should be 10 repetitions, three times per week. A chair may be useful for the client to hold (page 114) if they find the balance of this exercise difficult.
Back Flattening .1{e7.:.'. Stretches hip flexors and strengthens/builds the abdominal muscles, while re-educating
endurance in posture control.
Once an individual has corrected the muscle imbalance of the lordotic posture, he should practice assuming optimal posture. A back flattening exercise can help. Have your client stand with his back flat against a wall and his feet 6 inches (15 cm) from the wall. He should then tighten continued
150
.
Back Stability
Back Flattening,
continued
the abdominal muscles and gluteals in order to posteriorly tilt the pelvis, while his legs remain fully extended. The posterior pelvic tilting will effectively stretch the hip flexors. He can gradually increase the holding time, starting at 3-5seconds and building to 30-60 seconds, breathing normally Tighten throughout the exercise. Prescribe exercises abdominals i .' twice daily for 10 repetitions, with each , repetition held 5 seconds, and a rest day Streichtight ~ hipflexors taken after every four exercise days. \, Strengthening the abdominal muscles is , , not sufficient to correct a lordotic posture. Unless a person modifies hip flexor tightness and corrects abnormal lengthening of abdominal muscles, abdominal strength changes will have little effect on pelvic tilt or lumbar lordosis. Walker et al. (1987) and Levine et al. (1997) both examined the effects of abdominal strengthening alone and found no changes in postural variables.
t
I
Swayback In the swayback or "slouched" posture, the pelvis remains level, but the hip joint is pushed forward, the greater trochanter lying anterior to the LOG. Whereas in normal posture the sternum is the most anterior structure, now the pelvis has shifted and become the more anterior body segment, with the LOG moving from the ankle to the midfoot and toes (see figure 7.7b, page 145). The hip is effectively extended, lengthening the hip flexors, and the body "hangs" on the hip ligaments and anterior hip structures. The lordosis now changes shape from an even curve to a deeper, shorter curve with a prominent crease normally at L3 level. The kyphosis is now longer and may extend into the lumbar spine. The lower lumbar region is flatter than normal, and the pelvis may be minimally posteriorly tilted. A person with this posture will often be able to point to the exact point of pain, which normally occurs after prolonged standing. Swayback is common in youth and is the most common posture in young (18-28 years) athletes (Norris and Berry 1998). The rectus abdominis remains relatively unchanged in the swayback posture because the pubic bone and lower ribs in general retain their anatomical relationship. However, due to the direction of the fibers of the oblique abdomina Is, the external oblique is lengthened and the internal oblique unchanged or shortened (figure 7.8); in the latter case, it is the upper fibers that are affected (Kendall et al. 1993).
Posture
. 151
The swayback posture may be combined with dominance of one leg in standing ("hanging on the hip"), especially in adolescents. In this case, weakness in the gluteus medius allows the pelvis to tip laterally, a situation partially compensated by increased tone in the tensor fasciae latae. Shortening is seen in the iliotibial band (ITB), with a prominent groove apparent on the lateral aspect of the thigh, as the tight fascial band pulls on the skin. You can assess tightness in the ITB using the Ober test (see page 108), which you may also use to Figure 7.8 Changing length of the stretch the tight muscle. Assess the oblique abdominals in swayback ability of the gluteus medius to mainposture. tain pelvic stability in single-leg standing by using the Trendelenburg sign test (see page 73). Page 105 shows the inner-range holding test position of this muscle in side lying. Correction of swayback relies on two essential points of the posture type: the pelvis is the most anteriorly placed structure instead of the sternum, and the posture results in height loss. To correct the posture, you must help your client change the relative alignment of chest and pelvis.
Correction of Swayback Posture .f{'1~'.
For re-education of body segment positioning.
Have your client stand with his pelvis against the top of a table; from this position he presses his chest forward, shifting it as a single segment and avoiding any spinal flexion. At the same time, he performs abdominal hollowing to reeducate the flat abdomen alignment. If you have observed single-leg dominance with the swayback posture, help your client correct it by stretching the adductor muscle group pn the tight side, and enhancing the endurance of the abductors (gluteus medius) on the lax side. Symmetry between the two legs is essential. Use the Ober test (page 108) on both legs to determine the length of the hip abductors. continued
152
. Back Stability
Correction of Swayback Posture, continued
Determine hip adductor length by passively stretching your client's straightened leg into an abducted position, with a total of 900 hip abduction (450 on each leg) being desirable. You can use the following two exercises both to assess the range of hip abduction and to develop it. The first assesses tightness in only the short adductors inserting above the knee (adductor longus, adductor brevis, adductor magnus) because the knee is allowed to bend. The second targets the long adductor inserting below the knee (gracilis) by keeping the knee straight throughout the stretch.
Sitting Bilateral Hip Adductor Stretch .f{t1~,.. To stretch the hip adductors, excluding the gracilis. Have your client sit on the floor on a folded towel (2 inches thick), her back supported against a wall. She should place the soles of her feet together, grip the feet, and press down on her knees using her elbows, holding the full stretch for 5-10 seconds while maintaining back alignment. A desirable range of motion is for the knees to fall to within 3-4 inches of the floor. Prescribe 10 repetitions daily.
Sitting .f'lt1~,..
Wide Splits To stretch all the hip adductor
muscles.
Have your client sit on the floor in an upright posture with her arms behind her, hands on the floor to stop her from leaning back too far, legs straight. The body should be as vertical as possible. Instruct her to abduct her legs as far as possible, allowing the pelvis to posteriorly tilt. This posterior tilt will take the stretch off the adductors slightly, enabling the subject to get into the position comfortably. Then, she can increase the stretch by maintaining the position of the feet and pressing the hands against the floor to lengthen the trunk (the instructor can use the instruction "grow taller" or "try to reach your head up to continued
Posture.
153
Sitting Wide Splits. continued
the ceiling"). As this occurs, the subject attempts to anteriorly tilt the pelvis which will move the pubic bone (the upper insertion of the adductor muscles) backwards and so increase the stretch. A desirable range of motion is a total of 90° hip abduction between both legs. She should hold the full stretch for 5-10 seconds. Prescribe 10 repetitions daily. Because swayback posture is common in youth, but not associated with marked muscle tightening or weakening, it is difficult to correct. The emphasis is on re-education, with postural awareness playing an important part in the process. You can increase postural awareness by the use of proprioception during the spinal lengthening exercise below.
Spinal Lengthening .f{l1~'.
To improve awareness of body position.
Your client needs a partner for this exercise. As your client stands in his normal resting posture, his partner places a hand 1-2 inches (2.5-5.0 cm) above the crown of the client's head. Instruct your client to lengthen his spine (the instruction is to" grow taller"), attempting to touch his partner's hand with the top of his head. He must not look up (cervical extension) in an attempt to lengthen his neck, and must not stand on his toes! Once he has mastered this action, he should attempt the same lengthening action without the help of a partner. The action is again to "grow taller." Placing a light book or beanbag on the head helps to give sensory feedback and can help him focus his attention on moving the top of his head upward. Initially he practices simple lengthening at whatever speed is comfortable, with the beanbag on the head. Eventually he should slow the lengthening action, attempting to hold the lengthened position for 5-10 seconds while breathing normally (some people take a deep breath and hold it-this must not be allowed, as it can lead to lightheadedness). The lengthened position should be relatively relaxed and not stiff-comparisons with a puppet rather than a wooden stick can illustrate the difference between stability (spine lengthened and continued
154
.
Back Stability
Spinal Lengthening, continued
aligned) and rigidity (spine fixed). When your client is able to perform the movement and hold the corrected body position, he can progress to walking while holding the lengthened position, and then to simple activities such as sitting/standing from a chair to increase the variety of movements. In order to provide sensory feedback when the swayback posture is incorrectly stretching the muscle, try applying nonelastictape on the skin over the external oblique, taking up any skin slack. Attach the tape to the lower lateral aspect of the abdomen, out toward the anterior rim of the pelvis. Pull the tape tight from this point up to the posterolateral aspect of the lower ribs. Although the tape is not strong enough to prevent the pelvis from moving forward in relation to the rib cage, it will remind your client when this is happening and encourage him to correct the posture. The more times he makes the correction, the more likely it is that optimal postural alignment will become automatic. Either a physical therapist or athletic trainer should apply the tape, and it should be done immediately following the spinal lengthening exercise above, to encourage maintaining correct alignment between exercise bouts. Another way to reinforce automatic alignment is to build correction into daily activities. Encourage your client to perform the pelvis-chest realignment exercise regularly throughout the day. Office workers, for example, can perform the exercise whenever the telephone rings, and students can perform it each time a bell rings to end class. If the iliopsoas is lengthened by the extended position of the hip (the Thomas test will reveal this; see chapter 5) its inner-range holding must be redeveloped.
Sitting, Hip Flexor Shortening .f{"~'.
To shorten the iliopsoas and rectus femoris muscles and build their endurance. While your client is sitting, you should passively flex the hip to the maximum degree possible without pain-or to approximately 110°, or to the point where the pelvis just begins to posteriorly rotate. Instruct your client to hold this position for 10 seconds, while maintaining a continued
Posture
.
155
Sitting, Hip Flexor Shortening, continued
neutral lordosis. Inability to hold at full inner range for 10 repetitions (10 seconds each) is a sign of postural lengthening. If the iliopsoas is lengthened, the leg may drop and/or the pelvis drop back into posterior tilt, moving the iliopsoas into its lengthened position. Your client can redevelop inner-range holding of the iliopsoas by using first eccentric and then isometric inner-range hip flexor exercises while maintaining a neutral lordosis. In the preceding exercise position, your client should try to lift her leg to full flexion. Then you should try to lift the leg farther (increasing hip flexion), without altering the position of the spine or pelvis. Remember that a lengthened muscle cannot contract powerfully to pull a limb into its fully closed (inner-range) position. If your client's hip flexors are lengthened, further passive movement will be possible because she will not have been able to pull her own leg into full inner range. Have her attempt to hold this new (passive) inner-range position. If she is able to do so, instruct her to build up holding time from 1-2 seconds to 10 seconds while performing the exercise daily for two weeks-her target is 10 repetitions of the 10-second hold. If your client is not able to hold the passive inner-range position, she should use controlled lowering (eccentric). From the passive inner-range position, she attempts to slow the descent of the leg after you release it from its fully flexed position. She should continue the controlled lowering until she can slow the descent sufficiently to hold the leg still. She then progresses to holding at reducing joint angles. For example, assume that the active inner-range position (with your client using her own muscles) is 90° hip flexion, and the passive inner-range position (as you lift the leg farther into flexion) is 120°. The target for active flexion! holding is about 110°.You lift her leg to 120° hip flexion and release the leg. She then controls the lowering back to the 90° starting position. Once she can do this consistently, you lift her leg to 90-100° and she attempts to hold it. Once she can hold this position, you repeat the exercise, beginning again with the 110-120° passive flexion. She should perform each holding or lowering exercise only five times before taking a rest period since the muscle fatigues quickly with this exercise and alignment will be lost. Prescribe 3 sets of 5 repetitions twice daily for four days (a family member can provide the passive flexion), followed by a single day of rest, then another five-day cycle, and so on. The goal is the ability to actively flex the leg to 110° and hold it for 10 seconds for each exercise set.
156
.
Back Stability
Flatback With the flatback posture, the main problem is lack of mobility in the lumbar spine and a flattening of the lordosis (lumbar flexion). This posture reflects the extension dysfunction described by McKenzie (1981) and is common in chronic low back pain after extended periods of inactivity. The pelvis may be posteriorly tilted in comparison to the reference line, and the lumbar tissues are often thickened and immobile. The flatback posture is also seen in subjects who practice a high number of sit-up type exercises (repeated lumbar flexion). In this case the lumbar spine may be mobile-but the rectus abdominis is strong and tight, and is by far the dominant member of the abdominal muscle group. Flatback is corrected by regaining appropriate mobility in the lumbar spine through passive and active extension movements.
Passive
.'{If.'.
Back Extension in Lying Position
To improve spine.
the passive
range of extension
in the lumbar
Performed in the lying position, extension exercises first mobilize the upper lumbar levels, a with proportionally less caudal movement (McKenzie 1981). Instruct your client to lie prone on the lab table (or floor), with his hands by his shoulders in a pushb up position (a). He should extend his arms while keeping his pelvis on the table, thereby forcing extension of the spine (b). Initially, some people may need to push up only with their forearms on the table, gradually building up to full arm extension. To emphasize the motion of the spine rather than the pelvis, try fixing the pelvis to the table with a webbing belt. If your client experiences any pain in the lumbar region during this exercise, refer him to a physical therapist (PT). Often, instead of the whole '. lumbar spine being stiff to extension, one or two vertebrae may be stiffer than others. These stiff units require a specific manual therapy techcontinued
Posture
.
157
Passive Back Extension in Lying Position, continued
nique of "joint mobilization" either before or during the exercise program. When a specific stiff area has started to move (the PT will assess this), you can move the webbing belt up or down within the lumbar region to form a fulcrum around which the movement occurs. In this way, the extension action is focused more exactly on a single lumbar joint. See that your clients practice the passive extension movement often, but for only a short time each session, to allow the movement to develop without causing too much reactionary pain. Suggest 10 repetitions every two hours throughout the waking day, with a full day's rest after every four days. The exercise should continue until the individual has achieved the desired movement range.
Pelvic Tilt Re-Education, Sitting .f{t7~,. To regain both range and quality of movement in the lumbar spine. If the lower lumbar spine has reduced extension, the pelvic tilting action may be effective in correcting it. Instruct your client to sit on a low stool with his feet on the ground. Keeping his shoulders still, he should try to tilt his pelvis forward and down. Tell him to think of his pelvis as a bowl full of water, and that by tilting the bowl he can pour the water onto the ground between his feet. He should try to bring the backside of the bowl up as he pushes the front of it down, always keeping his shoulders still and his sternum up. When the motion is especially poor, provide passive assistance. Wrap a webbing belt around your client's waist and, fixing the sternum, pull the lumbar spine into extension as he attempts to tilt his pelvis (see page 75, "Assisted Pelvic Tilting While Sitting"). Refer to chapter 4 for a fuller discussion of pelvic tilt.
Kyphotic
Back
In the kyphotic posture, the shoulder joint moves anteriorly to the posture line, increasing the thoracic kyphosis. In optimal upper body alignment
158
. Back Stability
(table 7.3), the scapulae should be approximately the width of three fingers from the spine, and the medial borders of the scapulae should be vertical. Assess optimal positioning of the shoulder by comparing the head of the humerus in relation to the acromion process. In optimal positioning, no more that one-third of the humeral head should be anterior to the point of the acromion. The humerus should be held with the cubital fossa (elbow crease) at 45° to the sagittal plane in relaxed standing. A smaller angle indicates excessive medial rotation, indicating tightness in the medial rotators (especially the pectoralis major) and lengthening of the lateral rotators. Visualizing how this would appear from above may be helpful. When the arm is held in medial rotation, the crease of the elbow is orientated more forward and inward; when lateral rotation is greater than normal, the elbow crease faces farther outward. Deviation from the ideal is often described as a "round-shouldered" posture, a blanket term that covers a number of scenarios. TIghtness in the anterior structures pulls the shoulder forward, away from the posture line. The weight of the arm moves farther from the upper body's center of gravity, dramatically increasing the leverage forces transmitted to the thorax. Eventually, thoracic kyphosis increases. Tightness in the pectoralis minor pulls on the coracoid process, tilting the scapula forward (figure 7.9a). Tightness in the pectoralis major causes both excessive medial rotation at the glenohumeral joint and anterior displacement of the humeral head (figure 7.9b). Lengthening of the lower trapezius and serratus anterior may cause excessive abduction (figure 7.9c) and downward rotation (figure 7.9d) of the scapula. Excessive elevation (figure 7.ge) and upward rotation may result from tightness in the upper fibers of the trapezius. Correction of kyphotic posture depends on flexibility of the thoracic spine. Where the kyphosis appears fixed and thoracic motion is grossly reduced, thoracic joint mobilization is required as a first step. Once some mobility has been gained passively by manual therapy, you can use exerTable 7.3
Correct Alignment of the Shoulder Girdle
From behind
. .
Medial border of scapula vertical
Medial border of scapula no more than three finger breadths from the spinous processes Spine of scapular T3/T4 level,
. inferior angle at T7
. Scapula flat against thoracic wall
From the side Line from ear canal to center of shoulder joint is perpendicular to floor No more than one-third of head of humerus anterior to acromion
. .
. Humerus held with elbow crease 45° to sagittal plane
Posture
I
I
I
I
I
I
I I
a
I
I
,I
.
159
,, , ,,, ,, ,, ,, ,
,, ,, ,, ' e Figure 7.9 Postural changes
around the shoulder.
cise therapy to maintain the newly gained motion. The stemallift action (page 162) is the exercise of choice. If the subject is younger and the thoracic spine is mobile, only scapular repositioning is required.
Thoracic Joint Mobilization 1Jf['1~'. To increase mobility of thoracic joints, using manual therapy, in preparation for exercise therapy. With your client in the prone lying position, work with a PT to use posterior-anterior vertebral pressures (PAVP) or gross extension pressures to isolate the thoracic spine. With your client sitting, you can combine mobilization with overpressure. Have her sit facing a treatment table, with her arms folded and placed on the table. As you press the thoracic spine into extension, instruct her to try to follow the action. If thoracic mobility is quite limited, at first you will simply press the spine passively into extension. As your client gains mobility, encourage her to follow your motion with her own active movement while you gradually reduce the pressure you apply. The first step in this active process is for the subject to be able to "feel" the movement. Many people with a kyphotic posture have a poor ability to control the quality of motion in the thoracic spine, and this type of guided exercise can help them improve their control. If your client is still unable to perform active thoracic extension even after regaining passive extension, suggest a visualization technique: encourage her to imagine herself performing the action. continued
160
. Back Stability
Thoracic Joint Mobilization, continued
Either you or a model should perform the action correctly. You can also use video to enable your client to see the action from behind, while a mirror provides a view from the front. Then have her repeat her attempt at active thoracic extension. She may need to cycle through a series of visualization sessions, passive extension, and attempts at active extension before she can finally sense what active extension feels like. Once that happens, she can proceed to daily exercises. The subject should perform the exercise daily for 10-15 repetitions. In the early stages as mobility is very poor, some soreness can be expected following the exercise, so a greater number of repetitions should not be performed.
Scapula Repositioning .fl:I1.'. To improve control of scapular retraction and depression. If the thoracic spine is mobile, you can correct kyphotic posture by repositioning the scapulae-shortening the shoulder retractors and enhancing the scapular stabilizers (especially lower trapezius and serratus anterior). The aim here is to improve control of movement rather than simply to increase strength. By improving strength, muscle endurance, and movement quality (coordination and timing), these exercises differ from many traditional weight-training programs whose primary aims are gains in strength and muscle size. With your client lying prone, passively place his scapula into optimal alignment-the medial borders vertical, three finger widths from the spine. The scapula should be firmly anchored to the thorax (by action of the serratus anterior and lower trapezius muscles) rather than being separated from the rib cage. Frequently this involves passively depressing and adducting the scapula, but the amount of passive movement of the scapula that is required depends on the postural alignment of the subject. More movement is needed in subjects who have grossly abducted scapulae (medial border of scapula 5-6 inches [13-15 em] from the spine) than for those with minimal abduction (medial border 3-4 inches [8-10 em] from the spine) (Mottram 1997; Norris 1998). Initially, encourage your client to hold the new position for 1-2 seconds. Often the tendency is for the subject to "brace" the shoulders back continued
Posture
.
161
Scapula Repositioning, continued
hard. Discourage this reaction since it requires maximal muscle activity. Encourage your client to "let go" until the scapula just begins to move away from the corrected position, and then to hold the muscles slightly tight. Progressively increase the amount of time that this position is held with minimal muscle work, from 1-2 to 3-4 and eventually 10 seconds. The aim is to build up to 10 reps, holding each for 10 seconds, with the minimal amount of scapular muscle work that is required to maintain good scapular alignment. Tight anterior structures must be stretched to allow the shoulders to retract fully. Check for tightness in the pectoralis major and pectoralis minor, and if necessary prescribe stretching exercises as detailed in the following sections.
Door Frame Stretch .flI1~'" Stretch pectoralis major muscles. Instruct your client to lean forward onto a doorframe, his arms horizontal, his forearms vertical against the frame. He then pushes his arms back into extension by leaning into the doorway opening, holding the position for 20 seconds. Have your client do this exercise 3 times a day, with 2 repetitions each time.
Weight .fllm..
Bag Passive Stretch pectoralis
Stretch minor muscles.
A tight pectoralis minor can pull the scapula down and forward. Have your client lie in a supine position. Place a 3- to 5-lb weight bag over the anterior aspect of her shoulder. She should relax and allow the bag to press the shoulder back into position for 30 seconds. The weight bag continued
162
.
Back Stability
Weight Bag Passive Stretch, continued
will help press the shoulder back into retraction, passively stretching the anterior structures. To use a contractrelax technique, the client presses the shoulder into protraction for 2 seconds, trying to lift the weight bag, and then relaxes for 5-10 seconds, allowing the weight bag to press the shoulder farther back. Astatic stretch may also be used with the client simply lying relaxed, allowing the weight bag to press her shoulders back.
Sternal Lift Exercise .I'!"~'.
Combines thoracic extension and scapular repositioning.
While sitting, your client should lift his sternum using thoracic extension (rather than simply taking a deep breath) (a). At the same time, he should draw the scapulae down and in toward their optimal alignment. He may prefer to perform the action against a wall, where the movement should be one of "rolling" the thoracic spine up the wall while keeping the lumbar spine stable and avoiding any increase in the depth of the lumbar lordosis (b). b a If the client's lumbar spine stability is particularly poor and he. is unable to avoid hyperflexion, modify the starting position by having him sit on a bench, with his feet on a chair to bring the femur above the horizontal. This position posteriorly tilts the pelvis and flattens or reverses the lumbar lordosis.
Posture
. 163
SUMMARY
· · ·· ·
Posture is the arrangement of body parts in a state of balance that protects the supporting structures of the body against injury or progressive deformity. Postural sway consists of a small continuous motion in the sagittal plane-an oscillation of the center of gravity that may reduce lowerlimb fatigue and aid blood flow.
·
Excessive postural sway generally reveals poor balance and stability. You can assess clients' postures by use of a plumb line or a posture grid. There are four basic types of abnormal posture: 1. Lordotic posture is characterized by excessive anterior pelvic tilt. 2. Swayback is characterized by anterior displacement of the pelvis. 3. Flatback is characterized by slight posterior pelvic tilting and loss of lumbar lordosis. 4. Kyphosis is characterized by excessive thoracic curve. This chapter describes how to assess different abnormal posture types and presents exercises that can help correct them.
PART
nnn
BuildinL Back Fitness If you bring a client all the way through the assessments and exercises in the previous chapters, he or she should have a basically stable back, with no pain. Some clients need more, however-namely, those whose demands in the workplace or in sport activities require extraordinary strength, speed, or accuracy of movement. Chapter 8 ("Advanced Stability Training") presents exercises that will build on the training already achieved, using body movements alone, using balance boards, using stability balls, or employing proprioceptive training to increase accuracy of muscle control. Chapter 9 ("More Advanced Stability Training: Weight Training and Plyometrics") is for those clients who need the most rigorous training possible for their backs because of extremely heavy sport/workplace demands. Please note: the approaches used in chapters 8 and 9 are specifically for people who have had lowerback problems and/ or who need to prevent such problems in the future. Study the chapters with that in mind-the material does NOT merely restate what you've read before about weight training, etc. Because these chapters approach advanced training from the viewpoint of increasing your client's back stability, and not simply with the idea of building pretty muscles or increasing overall strength, they will be invaluable to your clients who have major concerns about their backs.
165
~ Advanced Stabilig Training Atter your clients have used the procedures and exercises of previous chapters to achieve basic back stability, they are ready (if they wish) to build on that stability. By now they should have learned to control pelvic tilt; to automatically assume the neutral position; to maintain abdominal hollowing (at 30-40% of the maximum effort); and to contract the multifidus at will-or, in quantitative terms, to perform the basic procedures in chapter 4 with variable intensity for 10 repetitions, holding each repetition for 10 seconds. With your help, they should have begun correcting muscle imbalances using the approaches in chapter 5. They should have developed their abdominal strength using the exercises in chapter 6. They should be able to maintain proper posture as described in chapter 7. Many people-who are relatively sedentary and whose back stability is rarely challenged through workplace or leisure-time activities-may have little motivation to proceed with additional training. Others will want to go further, however, especially if they are involved in sports or if they face heavy physical demands on the job. In this chapter, I cover exercises for developing even greater back stability. Chapter 9 goes further still, but your clients should master the material in this chapter before moving to the very strenuous work in that chapter. The first class of exercises in this chapter simply adds layers of complexity onto movements your clients will already know from other chapters. But there is also an entire series of exercises using a stability ball (or "gym ball"), which was introduced briefly in chapter 4-many people find these exercises more "user friendly" for their home workouts. Finally, I cover a small core of proprioceptive exercises-training that is advanced beyond what your clients have seen thus far, and that provides a kind of transition between some of the later exercises in the first section and the plyometric exercises in chapter 9.
167
168
. Back Stability
Very important: for each of the exercises in this chapter, your clients should gently contract their deep abdominal muscles to perform abdominal hollowing and maintain this contraction throughout the exercise. By now, moreover, they should be able to voluntarily contract the multifidus muscles--especially if they began the program as sufferers from chronic low back pain. They should begin all exercises in the neutral position.
SUPERIMPOSED LIMB MOVEMENTS AND BALANCE BOARDS Each of the following exercises involves limb movements that are superimposed on a basically stable back that the exercises of chapter 4 can create (Le., in these exercises an individual tightens the back stability muscles and then moves the limbs upon the stable base). As your clients focus their attention on limb movements, they will become more able to control their back stability muscles without conscious thought. This kind of automatic response occurs only with long repetition of the exercises. You should find it surprisingly easy to observe the point at which your clients are exerting automatic control. If they perform a limb-loading exercise such as the standing single-leg raise or the crook lying heel slide, for example, movement of the pelvis will reveal lack of back stability. In this case, you would retreat a couple of steps and have your clients practice the hollowing actions to enhance their ability to stabilize the spine. Once they have built up endurance of these muscles and can hold the abdominal contraction for 10 repetitions of 10 seconds each, you would once again try adding limb movements to the basic exercises. If they can now successfully control limb movements while avoiding unwanted pelvic movement (maintaining the lumbar spine's neutral position throughout the action), you will know that they are gaining automatic control of the stabilizing muscles-they no longer have to focus their attention on these muscles and can now concentrate on accurate positioning of the limb. For each of the following exercises, your client should progress in a single session only to the point at which he can no longer maintain neutral position, correct pelvic tilt, or maintain abdominal hollowing. Have him do the exercise daily for four days, rest one day, then resume the pattern, gradually increasing the progression or the number of repetitions until he eventually can do the exercise in its most challenging form for 10 reps, holding (where appropriate) for 10 seconds each time. Obvi-
Advanced Stability Training
.
169
ously, all one-sided movements should be performed on both right and left sides, one being the mirror image of the other. Each exercise should be performed in a slow, controlled fashion, maintaining the neutral position of the spine throughout the exercise. Since limb leverage changes when arms/legs are bent and straightened, your clients will necessarily have to vary the amount of abdominal work they use to maintain the neutral position. It is this variation that makes the difference (in terms of skill) between the holding exercises, such as abdominal hollowing, and these more advanced exercises that involve limb movements upon the stable trunk base.
Determining the Starting Position An individual's starting position depends on his physical characteristics and abilities. You should always be open, moreover, to changing the starting position if you perceive that your first choice may not have been the best-which will be the case if your client is not succeeding with an exercise. Some exercises are easier than others because they involve less muscle work. For example, in the heel slide movement, the ground partially takes the weight of the leg, while in the single-leg raise, the subject lifts the whole of the leg weight. The former exercise is therefore easier in terms of pure muscle work. Some movements may be more comfortable for certain subjects. Since lying positions are more supported than kneeling, for example, many people feel more secure in lying. The program generally follows a neurodevelopmental progression (Le., the sequence that children go through when they learn to sit, stand, and walk). In the present case, we go from ground support, to apparatus support, and finally to increasingly complex free exercises.
Exercises in the Crook Lying Position The crook lying position, which was used to perform abdominal hollowing and pelvic tilting, is a good starting position for superimposed limb movements. As an individual straightens the leg or lowers it to the ground, the overload placed on the trunk becomes progressively greater-the individual must therefore vary the intensity of muscular stabilization to maintain the neutral position. This variation in muscle contraction intensity increases the person's cOlltrolrather than simply strength or endurance capacity.
170
. Back Stability
Heel Slide-the
Basic Movement
.1'{17.'. To place minimal, but progressive,
limb loading on the trunk.
Instruct your client to slowly straighten one leg, with the heel resting on the ground. This movement is easier if the heel is on a slippery surface (a cloth if on a polished floor, or a piece of shiny paper if on carpet). The moment the pelvis anteriorly tilts and the lordosis increases, the movement must stop and the leg be drawn back into flexion once more.
Leg Lowering .1'{17.'. Limb loading as a progression from the heel slide. Instruct your client to flex both her hips to 90° so that her thighs are vertical to the ground, while keeping her knees relaxed. She should then slowly extend one hip until her foot touches the ground. Have her gradually extend the knee farther in subsequent repetitions, so that the foot touches the ground farther from the buttock, increasing the limb leverage and therefore progressing the resistance. The exercise is performed daily for four days and then a single day's rest is taken. She should continue this sequence until she can perform the exercise with the leg almost straight. Once she can perform the exercise with the leg almost straight, she can progress to single-leg raises.
Advanced Stability Training.
171
Single Bent-Leg Raises .f{"~'.
Progression from leg lowering.
Beginning in the crook lying position, your client should lift one leg-still bent at the knee-while the other rests on the floor. He brings the knee up as far as he can without moving out of neutral position, then lowers it. Then he repeats with the other leg. As a progression on this action, have him begin lifting one leg just before the other limb has touched the ground so that momentarily they are both off the floor at the same time. Finally, he should lift and lower both legs together, initially with minimal limb leverage (Le., with knees well bent) and finally with increasing leverage (legs increasingly straightened). The maximum leverage will vary with each individual. For most well-conditioned individuals, 90-120"knee extension is appropriate. At no time should the pelvis anteriorly tilt, and at no time should the abdominal muscles be allowed to bowstring (bulge outward rather than maintain a flat or hollow contour). I do not recommend progressing all the way to bilateral straight-leg raises-the compression and shear forces imposed by the psoas muscle upon the lumbar spine make this unsuitable for use in rehabilitation following low back pain.
. maintained
The neutral position of the lumbar spine must be throughout the exercises. If the pelvis tilts and neutral position is lost, the exercise must be stopped, and the client should revert to an earlier stage of the exercise in which the pelvic tilt was accurately controlled. Be certain also that your clients keep their abdomens hollowed throughout the exercises.
KEY POINT: I
Prone Lying Gluteal Brace .1'['7~'. Co-contraction of trunk stabilizers with gluteals. Instruct your client to lie prone, then to dorsiflex one foot, with the toes bent up toward the knee. She should then slightly flex both her knee (about 10°) and her hip (also about 10°). She then contracts her gluteal muscles to lift the femur into extension to the horizontal position (with the foot remaining on the ground), straightening the knee.
~~
172
.
Back Stability
Prone
Bent-Leg
Lift
.I'{,,~,. Active movement of an unsupported leg on the stable trunk. In the prone lying position, your client should flex one leg to 90° at the knee. Instruct your client to set her abdominal muscles and contract the gluteals to lift the leg from the floor. To prevent passive anterior pelvic tilt, the maximum hip extension should be only 15°. This position places the hamstring muscles at a mechanical disadvantage, reducing the tension they can create and therefore throwing greater stress onto the gluteals. To increase the isolation of the gluteals from the hamstrings, have your client slowly flex her knee while maintaining hip extensionthis causes the gluteals to act isometrically as hip stabilizers while the hamstrings acts isotonically as prime knee flexors.
Bridge
From
.I'{"~'. Using
Crook
Lying
leg power to lift the trunk while maintaining
neutral lumbar position.
a
In a crook lying position, your client should tighten his gluteal muscles and then lift his pelvis from the ground, aiming to form a straight line from shoulders to hips and then to the knees. This exercise tends to induce movement in the sagittal plane (anterior-posterior pelvic tilt, and/ or lumbar flexion-extension). Lifting one leg (see next exercise) imposes an additional rotary stress, tending to cause movement within the transverse plane.
Advanced Stability Training
.
173
Bridge With Leg Lift .I'{IJ~'. A progression from bridge from crook lying. Instruct your client to assume the bridge position, starting from lying. Then he lifts one leg, avoiding the tendency for the pelvis toward the unsupported side. Placing a stick across the anterior rior iliac spines of the pelvis gives useful feedback for keeping the level.
crook to fall supepelvis
Exercises in 4.Point Kneeling Position The 4-point kneeling position is initially stable since four symmetrical points (both hands and both knees) bear the weight. As one arm or one leg is lifted to reduce support to three points, the body is less stable and the stability muscles must now work harder to maintain trunk alignment and stop the body from tipping.
Four-Point
Body Sway
.I'{IJ.,. Learning to maintain neutral position as the limbs are moved. Instruct your client, who begins in the standard 4-point position, to sway the body forward and back, moving at the shoulders and hips only. As she passes the critical point of 90° hip flexion, be sure that her lumbar spine remains in its neutral position. As soon as she begins to lose the neutral lumbar position, she should reverse the movement back into full 4-point kneeling. The aim is to gradually work farther and farther back (increasing hip flexion) while maintaining a neutral spine.
174
.
Back Stability
Four-Point Pelvic Shift .f'[11.'. Learning to unload the limbs prior to lifting them. After assuming the 4-point position, your client should shift to the side to take the weight of the far leg. She then barely lifts the leg on this side from the supporting surface, leaving only one knee in contact with the ground. Be sure that she lifts the leg a maximum of 1-2 inches (2.5-5.0em). Some people find the subtlety of this movement difficult and tend to lift the leg by 6-8 inches (15-20cm)-but this imposes an unwanted rotation on the spine and must be discouraged. Placing a stick across the upper pelvis (level with the posterior superior iliac spines) is helpful. With the required subtle movement, the stick will stay in place. If the leg is lifted too far, however, pelvic rotation will cause the stick to fall.
Four-Point Leg Flexion/Extension .f'[I1.,. Controlling back stability in the presence of limb movement. Your client should begin as for the previous exercise, shifting weight to one leg. Instruct him to move the unloaded leg into flexion! extension and abduction! adduction, while maintaining a neutral lumbar spine and keeping the lower leg parallel to the floor. He should use only small movements, the knee moving forward/backward and side to side by only 2-3 inches (5-8 em). Larger movements will require greater changes in pelvic tilt and are more difficult to control. The movements should be slow to avoid excessive limb momentum-no more than 1 or 2 complete limb movements per second.
Four-Point Kneeling Leg Lift .1'111.'. Maintainingstability movement.
during increasing
complexities
of leg
From the basic 4-point kneeling position, your client should extend one leg completely, keeping the foot on the ground (a). The next step is to lift the leg until it is parallel to the floor (b). Finally, instruct him to alternately flex and extend the raised leg at the knee, keeping the raised thigh continued
Advanced Stability Training.
175
Four-PointKneeling Leg Lift. continued
parallel to the floor. The foot should remain in a middle (neutral) position, toes and foot neither fully pointed (plantarflexed) nor fully pulled up (dorsiflexed)-holding the shin or calf muscles tight can cause muscle cramping. a Several alignment faults are common in this final movement. First, while your client is focusing on the limb movement, he may forget to maintain contraction of the trunk stabilizing muscles-leading b the abdominal wall to bulge because the hollowing action is lost. As this happens, the pelvis may anteriorly tilt, pulling the lumbar spine into excessive extension (back hollowing). Finally, if the gluteals have poor endurance, the client may start to rely on his hamstrings to maintain the extended hip position: as the hamstrings begin to flex the knee, he loses the hip extension position and the leg drops below the horizontal. In each case, you should stop the procedure and return to the previous exercise.
Four-Point Kneeling Arm and Leg Lift .fI.H.'ncreasing taining
back
the complexity stability.
of limb
movements
while
main-
Have your client begin as with the kneeling leg lift above. But this time, once the leg reaches the horizontal, he should also lift the diagonally opposite arm. Watch to see that his shoulder does not sag or drop down on this side; the scapula should not move as the elbow bends to unload the arm. Once your client's hand has cleared the ground, he should lift the arm forward toward the horizontal.
Exercises in the Side Lying Position We saw in chapter 7 that, in the frontal plane, the gluteus medius may lack endurance and inner-range holding ability, leading both the tensor fasciae lata/iliotibial band (TFL/ITB) and the hip adductors to tighten. In the side lying position, we are attempting to work the gluteus medius and to stretch the adductors, while maintaining stability of the pelvis and lumbar spine
176
.
Back Stability
in the frontal plane. The stability is achieved by contraction of the lateral abdominals and the quadratus lumborum acting together.Where lateral abdominal function is poor, the quadratus lumborum can become overactive and tight. Each of the following exercises overloads the quadratus lumborum and the oblique abdominal muscles on the upper side of the body. The movements must be reversed to provide a symmetrical overload.
Side Lying Knee Lift .f'll7~'" Maintaining trunk stability in the frontal (side flexion) plane during limb movement. Have your client begin the exercise in side lying, and align her pelvis so that the line joining the two anterior superior iliac spines is vertical. She must maintain this alignment throughout the exercise. Do not allow lateral movement of the pelvis. Instruct her to place the foot of her top leg on the floor in front of the shin of her lower leg. Then she should lift the top knee by abducting and externally rotating her hip, keeping the foot in place on the ground. Palpate the posterior fibers of gluteus medius above and behind the greater trochanter to make sure they are contracting. Give your client feedback until she is able to tell when she is contracting these fibers as she lifts her knee. Once she is able to feel the appropriate contraction, have her attempt to lift to full inner range, but stop her immediately if the pelvis begins to move out of alignment.
Side Lying Leg Rotation .f{e7~'" Maintaining trunk stability hip rotation. The second exer-
cise combines abduction and
trunk
ability stab il-
~
\ ~
and isolating pelvic control from
-
-
ii' ~
ity, while isolating hip movement from that of the pelvis. From the stabilized side lying position, your client should hold her upper leg straight and abduct it to the horizontal. continued
Advanced Stability Training
.
177
Side Lying Leg Rotation, continued
Tell her to then externally rotate the entire leg from the hip, turning the foot toward the ceiling and then back to pointing forward. Have your client perform 3-5 rotations before lowering the leg, unless she loses alignment of the pelvis-in which case she should lower her leg immediately.
Side Lying Leg Abduction .fl:IH.
Controlling hip abduction on a stable trunk.
The third exercise represents true abduction upon a stable base. Have your client assume the stable side lying position, then lift his upper leg into abduction while avoiding flexion and external rotation. Encourage him to "lengthen his leg" to avoid lateral pelvic movement, and then to abduct his leg as high as he can without experiencing discomfort, up to a maximum of 45° from the horizontal. All the movement should be in the hip-tell him to avoid lumbar-pelvic movement. He may have to work up gradually to the 45-degree target.
Side Lying Spine Lengthening .fl:lm.
Controlling the quadratus the oblique abdominals.
lumborum
and lateral fibers of
Side lying is also a useful starting position for strong co-contraction of the abdominal muscles with minimal compressive and shear forces on the lumbar spine (McGill 1997). Have your client lie on his left side, his thighs in line with his body but his knees flexed 90°, with his upper body supported on his left elbow to side flex the spine. He should then straighten his spine against the force of gravity, leaving the body supported on the forearm of the underneath arm and hip.
178
.
Back Stability
Side Lying Hip Lift .1{'1~'" Progression from side lying spine lengthening_ Have your client assume the position for the side lying spine lengthening. Then have him lift his hips, leaving the body supported on the forearm of the underneath arm and the knees.
Side Lying
Body Lift
.1{11~'. Final progression for developing control of quadratus lumborum and lateral fibers of oblique abdominals. Again, have your client assume the position for the side lying spine lengthening. Instruct him to straighten his knees and cross the upper leg in front of the lower leg. Then he should lift his body to the full side support position, leaving the body supported on the forearm of the underneath arm and the feet. Encourage him to "lengthen his body" and to "broaden his shoulders" to avoid their "falling" into scapular adduction-the aim being to form a straight line from the feet, through the pelvis, to the shoulders.
Exercises in the Standing Position The standing position is clearly important for the activities of daily living. The aim of the following exercises is to add limb and thoracic movements to the stable lumbar spine and to add whole spinal movements to the stable hip. You can monitor changes in the depth of lordosis by having your client lean against a wall-feet 4-6 inches (10-15 cm) forward of the
Advanced Stability Training
.
179
wall, his buttocks and scapulae on the wall-while you place the bladder of a pressure biofeedback unit between his lumbar spine and the wall.
Standing Sternal Lift .lIe1.:.'" To help correct excessive thoracic kyphosis by extending the thoracic spine in isolation. The idea of this first sequence of exercises is to teach your client to move the thoracic spine independently from the nonmoving, stable lumbar spine. Instruct your client to stand facing a table, his thighs pressed against the edge to prevent anterior shift of the pelvis into a swayback position. Have him lift the sternum up and forward, while drawing the scapulae down. Suggest that he place one hand in front of his sternum to monitor the sternal lift action. The anterior upward movement and posterior downward movement work like two guide wires pulling a wheel with its axle in the chest. The action is to flatten the thoracic curve rather than simply expand the chest or extend the lumbar spine. If your client finds it difficult to isolate the thoracic from the lumbar movement, have him try the same action while sitting-he should place his feet on a low stool to bring his knees above the level of the hips, thereby flexing the lumbar spine and reversing the lumbar lordosis. This action reduces the available extension in the lumbar spine and focuses the action to the thoracic area. After he has mastered the action in a sitting position, have him work on it while standing (see "Sternal Lift Exercise," page 162).
Pelvic Shift With Unloading .lIe1.:.'" To build isolation of leg movements on a stable base-a precursor to standing leg lifting in the frontal plane. Initially your client should stand with his side to a wall for support (gripping wall bars is also OK). As he develops skill in the movement, he should do it in a freestanding position. Instruct him to "lengthen his spine" ("grow taller"); to shift his pelvis to the left while maintaining alignment (a); then to unload the right leg by slightly flexing the knee and lifting the heel, while keeping the toe on the floor (b).
a Pelvic shift to unload leg
b Leg lift
180
.
Back Stability
Pelvic Shift With Leg Lift .r{'1~'"
To teach pelvic control and stability in single-leg standing.
Ask your client to shift her pelvis to the left, so that her body weight is over the left leg only, then slowly lift her right leg no more than 4-6 inches (10-15 em) while maintaining alignment in all three planes-there should be no posterior tilt of the pelvis, no hip drop, and no spinal rotation. Figure b (a) in "Pelvic Shift With Unloading" shows the a Lateral Anterior correct form; here, figure (a) shows lateral pelvic pelvicdip pelvic dip tilt (incorrect!); figure (b) illustrates anterior pelvic tilt (incorrect!). The action is one of pure hip flexion upon a stable back: the supporting leg supports the pelvis, and the pelvis supports the back. The knee should be raised no more than 45° from the horizontal. If your client finds the movement difficult to control, let her practice at first with her back supported by a wall. The sequence of pelvic shift, leg unloading, and knee lift are the same, but the back remains against the wall throughout the movement.
Standing Hip Abduction .r{'1~'"
Learning performing
to maintain stability
in the frontal
plane
while
hip abduction.
Your client begins by standing with her back 2-4 inches (5-10 em) from a wall. If your client loses pure abduction as the movement progresses (i.e., if she uses any flexion or extension), she will know immediately because the leg
will move closer to or farther
a
b
away from the wall. Instruct her to shift her pelvis to the right, unloading the left leg (a). Then, maintaining alignment, she should abduct the left leg by 10-20° (b). Be sure that she does not laterally tilt her pelvis or spine (c). She should gradually increase the abduction range to a maximum of 45°. Reduce the range or stop the exercise as soon as alignment is lost.
Advanced Stability Training.
Standing
181
Hip Hinge
.f{e1~'. Learning to move the spine and pelvis as a single unit on the hip. Have your client stand about 4 inches (10 cm) from a table. She may place her hands on the table only to help guide her movement, not to bear weight. Instruct her to bend from the hip, keeping her spine straight, until the spine is angled 30-45° from the vertical. It is often easier if your client focuses attention on her sacrum and imagines it moving from a b near vertical to near horizontal-tell her to "push her tail away." Once she has mastered this movement, she should do it without table support. Two kinds of feedback may be helpful. First, she can monitor pelvic tilt by placing the flat of one hand over the lower (infra umbilical) abdomen and the back of the other hand over the sacrum (a). The action is to tilt the pelvis while maintaining the relationship of the lumbar spine to the pelvis-the palm of the back hand should end up facing toward the ceiling. The second feedback method uses a long, straight stick. As your client places one hand over her sacrum and the other between her shoulder blades, she should grip the stick with both hands. She must keep her spine on the stick as she performs the hip hinge action (b). Rounding the spine (a typical error) increases pressure of the spinous processes on the stick; hollowing the spine increases the gap between the spine and the stick.
Exercises in the Sitting Position Incorrect sitting positions often cause low back pain, especially that of postural origin. But, while sitting at home or work, one can also conveniently practice the following exercises throughout the day. The first exercise uses the process of relative flexibility to overload the stabilizing system. The sitting position used in these exercises must reflect the optimal alignment of body segments. The hips should be at 70° flexion; the knees should be below the hips and slightly wider than shoulder-width apart (bringing the knees together posteriorly tilts the pelvis through soft tissue tension). About 70% of the body's weight should rest on the ischial tuberosities, 30% on the pubis. The gravity line for the upper body should pass from
182
. Back Stability
the center of the hip joint to the shoulder joint and ear canal, with the spine evenly distributed along the gravity line. Your instructions to hollow the abdomen and "lengthen the spine" will help bring about the correct alignment. If you wish, you can monitor the depth of the lumbar lordosis with pressure biofeedback, placing the bladder of the unit between the lumbar spine and the chair back. (Note that the sitting position used in this case is not what most people use in everyday activities; they can have their backs against the chair for use with a pressure bladder by slightly straddling the seat with their legs, which, as you recall, are to be somewhat spread, with knees lower than hips.)
Sitting Hamstring Stretch .l1:tJ.,. Maintaining pelvic position against the pull of the hamstrings. For the first exercise, instruct your client to straighten one leg to stretch the hamstrings, while maintaining lumbar-pelvic alignment. As soon as the pelvis posteriorly tilts (to bring the ischial tuberosity forward and take the stretch off the hamstrings), stop the exercise because alignment has been lost. Progress the exercise by gradually straightening the leg further (while maintaining alignment) until the knee can be locked fully with the hip at 70° flexion (see "Tripod Stretch," page 117).
Sitting _It.,.,.
Sternal
Lift
Performing active thoracic extension lumbar extension.
and isolating
it from
Instruct your client to raise her sternum while drawing the scapulae down, as in the standing sternal lift on page 179. The movement is one of thoracic spine extension rather than deep inspiration. To assist the learning process, place the flat of your hand on your client's sternum and "draw it up," while placing the thumb and forefingers of your opposite hand on the inferior angles of the scapulae and "draw it down." If breathing control proves to be problematic, encourage your client to breathe out as she begins the sternal lift. Many people mistakenly extend the lumbar spine rather than the thoracic spine. If this occurs with your client, let her practice the exercise with her feet on a small stool to bring her knees above hip level-this position reverses the lumbar lordosis and throws the extension force high up the spine to the thoracic continued
Advanced Stability Training
.
183
Sitting Sternal Lift. continued
region. Once she has mastered the movement in this position, try the standard position again (see "Sternal Lift Exercise," [a], page 162).
Sitting Knee Raise Maintaining pelvic position I!imIpull of the hip flexors.
against the
In this third exercise, we overload the stability muscles by using the pull of the iliopsoas to displace the lumbar spine. Instruct your client to raise one knee, in stages, to about 3 inches above the horizontal, while maintaining lumbar-pelvic alignment. Be sure that he avoids posterior pelvic tilt. Initially, he should gradually unload the limb by lifting just the heel. If he is able to maintain good alignment, have him proceed to lift the entire leg.
Sitting Knee and Arm Raise .1'{'1~''''ncreasing
the complexity to challenge coordination.
Have your client flex one arm to 90°. Holding a small (7.5-10 lb., or 3-5 kg) dumbbell in the hand increases the overload; he should keep the dumbbell moving rather than holding it still. Combining alternate arm and leg movements is a useful progression-the right arm is lifted at the same time as the left knee to provide a diagonal stress on the body; this is then reversed with the left arm and right knee being raised.
Repeated Pelvic Tilting Exercises Using Balance Boards Moving the pelvis beneath an immobile trunk is an excellent teaching method to improve control of the neutral position, to reduce muscle reaction speed, and to enhance general stability. Using a "rocker board" (moves like a see-saw), and progressing to a "wobble board" (mounted on a hemisphere-moves in any direction), is an effective (and rather fun) way to perform such exercises.
184
. BackStability
Simple Pelvic Tilt, Progressing to Use of Balance Boards
Em
For advanced control of pelvic tilt.
At first, have your client sit in the optimal position (see page 181)on a wooden bench or stool with his feet on the floor. Instruct him to tilt his pelvis alternately in the anterior and then posterior direction, while maintaining the position of his shoulders and thoracic spine. The aim is to isolate the pelvis and lower lumbar spine from the thoracic spine, and the shoulders from the upper lumbar spine. Progress the exercise by having your client perform it while sitting first on a rocker board (like a see-saw, moves in only one plane-shown in the next exercise section), and then on a wobble board (mounted on a sphere, moves in any direction-see page 185, "Neutral Position Maintenance").
Pelvic Rock on Rocker Board .f{I1~'. Progression from simple pelvic tilt. Initially place the rocker in the frontal plane to facilitate anterior and posterior tilting of the pelvis. Changing the rocker orientation of the board to the sagittal plane will facilitate lateral tilting. In each case, the lumbarpelvic movement must be isolated from that of the upper body. To begin working for muscle reaction speed, apply pressure on the shoulders to push your client off balance while he tries to stay upright on the rocker board. Alternate the orientation of the board, between frontal and sagittal planes. You'll know when to stop any given session when your client is no longer able to maintain neutral position or maintain abdominal hollowing. Build up to 2 minutes in both planes before progressing to the wobble board.
Advanced Stability Training.
185
Pelvic Rock on Wobble Board IIm%i!!IMultiplane (sagittal. frontal. and transverse) stability in sitting_ Initially, have your client merely sit on the wobble board and attempt to maintain the optimal sitting position. Have him progress to single plane actions (flexion/extension and lateral flexion). Once he has mastered these actions, instruct him to "tip the board around a clock face" (i.e., to tilt to 1 o'clock and then back to neutral, to 2 o'clock and back to neutral, to 3 o'clock and back to neutral, etc.). Encourage him to use slow, deliberate movements, taking perhaps 2-5 seconds to reach each position of the clock, holding that position for 2 seconds, taking 2-5 seconds to return to neutral, holding neutral position for 2 seconds, and then beginning the next phase.
Neutral Position Maintenance IIm%i!!I Building stability reaction speed in sitting_ Finally, you should try to knock your client off balance while he maintains the neutral position on a wobble board. Initially use slow-onset pressure, working gradually up to rapid pressure from a variety of directions. Have your client close his eyes to faci!itate anticipatory muscle action and muscle contraction speed. The progression here is one of time. Initially, try to prolong the movement for 30 seconds, then 60 seconds, stopping each time when alignment is lost or the client loses his balance.
Sitting
Hip Hinge
IIm%i!!I Moving spine and pelvis
as a single
unit on the hip_
The final exercise is the hip hinge (compare "Standing Hip Hinge," page 181). As in all these sitting exercises, be sure your client begins continued
186
.
Back Stability
Sitting Hip Hinge, continued
in the optimal sitting position, with the knees astride to facilitate pelvic tilt (see description under "Exercises in the Sitting Position," page 181). Have him tip the whole of his upper body forward as a single unit, moving the pelvis and spine on the fixed femU[ He should initiate the action by leaning his whole body forward to change the sitting weight distribution. In optimal sitting, approximately 30% of the body weight is taken on the pubic bones and 70% on the ischial tuberosities, provided that the knees are aligned below the hip and the femurs are angled below the horizontal. As your client leans forward, he takes weight from the ischial tuberosities and places it onto the pubic bone, ending with 70-80% of his weight on the pubic bone. To lean back, he reverses the weight transference. To facilitate the action, suggest that he perform it while sitting on a rocker board. In each case the pelvis and spine should move as one unit, avoiding any change in lordosis.
STABILITY
BALL EXERCISES
In addition to or even instead of the exercises in the previous section, your clients can obtain advanced levels of stability by exercises with stability balls (also called gym balls). These exercises require quite complex movements and will help increase the stability already obtained through previous exercises in this book. They also can strengthen stability muscles that otherwise might not be exercised. At first your clients should use the ball under your supervision, but later they can use it at home-it is an inexpensive and effective apparatus for back stability. Several authors have described general exercises on the gym ball, and these publications make useful follow-up material (Hyman and Liebenson 1996; Lester and Posner-Mayer 1993; Norris 1995a).
Advanced Stability Training.
187
A 26-inch (65-cm) gym ball facilitates the optimal sitting position for most people. Your clients should be able to sit on the ball with their femurs horizontal and their hips and knees both at approximately 900 flexion. Feet should be shoulder-width apart and flat on the floor to enable free pelvic tilting and provide a wide base of support. The ball should be inflated so that it feels firm but will give slightly when a person sits on it. Use higher inflation pressures for heavier clients. Deflating the ball slightly will increase the base of support. You can reduce the ball's tendency to roll by setting it on a "collar"-a plastic ring on the floor. When you need to increase your clients' confidence or provide support, place the ball between two chairs: either position the chair backs toward the ball so that your clients can lightly touch the chair with arms outstretched at shoulder level; or, for even more support, position the seats toward the ball so your clients can place the flats of their hands on the seat surface. As with all exercises, your clients should warm up and stretch before engaging in these activities. During all exercises they should maintain the neutral position of their spines and keep their abdomens hollowed. They should perform mirror images of anyone-sided exercises, so the body is worked symmetrically. The progression with stability ball exercises is similar to that for previous exercises: begin with 8-10 repetitions, for example, then increase to 12-15. Note that the gym ball introduces balance as an additional variable. Even if your clients are not fatigued, if they lose alignment or lose their balance and become unstable (and therefore likely to slip off the ball), they must stop, rest, and start again using a lower number of repetitions. If gym ball exercises are the only ones your clients are doing, they should perform all of the following exercises during each session. I suggest at least three but no more than five sessions per week, for at least 1016 weeks. At first have your clients use a slow count of 4 or 5 to move into the holding position; hold the designated position for a count of 5; then use a count of 4 or 5 to move back into the starting position. They can progress by adding reps and/or by adding to the holding time. Determine the limits for a given exercise by observing the point at which your clients just begin to lose spinal alignment or abdominal hollowing, or to lose their balance-then instruct them to stay just below that level of timing or rep number for at least a week before trying to add holding time or reps. They should always stay just a little bit within their maximum capacity, as determined by their ability to maintain alignment and abdominal hollowing.
J88
. Back Stability
Sitting Knee Raise .fI.m.
Maintaining stability in the presence of hip movement on a reduced base of support.
While sitting upright on the gym ball, your client should lift a single knee from 90° hip flexion to 120° hip flexion. She must make the action slow and deliberate, maintaining her body position throughout, and avoiding the temptation to "fall toward" the lifting leg.
Abdominal Slide .fllT,:.'. Controlling moving.
the action of the rectus abdominis
while
Instruct your client to tilt her pelvis backward from a sitting position on the ball, then to roll back until her spine rests on the ball. The action is to roll through the spine-the ischial tuberosities begin on the ball, but the weight is transferred to the coccyx and sacrum and eventually to the lumbar spine. The final holding position is with the trunk slightly flexed and the abdominal muscles contracted in a half-sitting position.
Half-Sitting Arm and Leg Movements .fI'N.
Maintaining stability unstable position.
while moving arms and legs in an continued
Advanced Stability Training
.
189
Half-Sitting Arm and Leg Movements, continued
Have your client perform the abdominal slide action just described, but maintain the position when his trunk is at 45° to the horizontaL Then he should raise one arm while lowering the other. Once he can do this in a controlled fashion, with the trunk remaining in alignment, have him rest his arms, then lift one leg while lowering the other. He should try to keep the thigh of the leg being raised parallel to the ground (i.e., only the lower leg should move). Finally, he should perform arm and leg movements together-the right arm and left leg lifting together, and vice versa. To make the exercise even more challenging, suggest that your client hold small dumbbells in his hands as he does the movements.
Lying Trunk Curl Over Ball .f[,,~,.
Strengthens upper rectus abdominis muscles.
Instruct your client to begin with his thoracolumbar spine supported on the ball, his arms at his side. He should move from this sligh tl y flexed position to spinal extension, relaxing over the balL He then performs a curling movement while performing abdominal hollowing and pressing his lumbar spine onto the ball surface. Once he can perform the basic exercise well, increase the difficulty by having him hold his arms by the side of his head or even completely overhead.
190
. Back Stability
Lying Trunk Curl With Leg Lift .I'{t:r..,. Strengthens upper and lower abdominals. From the "lying trunk curl over ball" position, your client should lift one leg while maintaining the stable position, trying to keep the thigh parallel to the other thigh. The movement is easier if the ball rests closer to the shoulders with the waist at the ball's edge rather than at the ball's center. Lying over the ball, in fact, is an excellent way to stretch the whole spine into extension as part of postural correction of a flatback posture.
Basic Superman .1'{t7~,. Strengthens the spinal and hip extensors. Have your client lie prone with his abdomen on the ball, and his feet astride and flat against a wall. He should tighten his abdominal muscles to form a firm surface pressing against the ball and retract his head (tuck the chin in without looking down). He should retract and depress his shoulders in order to draw his arms downward and back, then extend his thoracic spine to bring his chest off the ball. Have him hold the innerrange position for 5-10 seconds.
Superman With Arms .1'{t1~,. Strengthens spinal extensors; helps shoulder retractors contribute more to movement. From the basic superman movement, instruct your client to extend first one and then both arms overhead to increase the overload for both trunk and shoulders. Holding a light ball or balloon between his hands can help give him the feeling of lengthening his body. Observe carefully to make sure that your client doesn't lose alignment and hyperextend his spine. There should be a straight line through the heels, knees, hips, shoulders, and hands. continued
Advanced Stability Training.
191
Superman With Arms, continued
Bridge .I'[IJ~'.
To simultaneously extensors.
strengthen
both hip extensors
and spinal
Have your client lie with her shoulders and back on the ball and her feet flat on the floor, knees apart. At first, place a small stool under her buttocks and instruct her to raise and lower her body from the stool using hip extension force. Once she is able to hold the raised position, remove the stool. Instruct her to hold the position, making sure that her lumbar spine is in its optimal position; she should gradually build up the holding time to 30 seconds.
Bridge With Pelvic Tilt .1'['1.'1. Strengthens back and hip extensors of pelvic tilt.
while improving
control
While your client holds the bridge position, have her perform a pelvic tilt. She can intensify the bridge movement by combining anterior tilt with lowering her buttocks onto the floor, and a posterior tilt with lifting herself back into the bridge position. This exercise helps teach the subtleties of muscle control involved in minor adjustments in pelvic tilt. It is especially helpful to clients who can only perform a tilt as an "all-or-nothing" movement using maximal force to bring about a full tilt.
192
. Back Stability
Bridge With Leg Lift .f{"~'.'ncreases bridge.
overload-especially
of lower abdominals-during
Have your client perform the standard bridge exercise-but once he is in the high position, he should lift one knee to bring the foot off the ground. Be sure that he maintains spinal alignment, avoiding the temptation to tip the pelvis toward the lifted leg. If he finds it difficult to keep his pelvis level, place a stick across the front of the pelvis just below the level of the anterior superior iliac spines. If the pelvis tilts too far, the stick will fall off!
Bridge .f{'1~'.
With
Leg Lift and Extension
Strengthens lower abdominals
while increasing
leg control.
Have your client perform the standard bridge and lift the right knee so that the right foot clears the floor, avoiding the tendency to allow the pelvis to tilt to the right. At the high position, he should gradually straighten the right leg until it is completely in line with the spine. After maintaining this position for 2-3 seconds, he slowly bends the leg and lowers it till his foot is back on the ground.
Bridge .f{'1~'.
With Therapist Strengthens
Pressure
hip and trunk stability
stability with continuously directions.
variable
muscles by challenging overload
from
multiple
While your client performs the standard bridge, you should kneel at his side. Push against his pelvis from above/below and side/side. Rapid pushes will decrease muscle reaction time, training the muscles to contract more quickly without loss of intensity.
Advanced Stability Training.
Reverse
193
Bridge
.f!I7~'" Strengthens back and hip muscles while increasing leg motion control. Your client's feet and calves should rest on the ball, with her trunk on the floor. Instruct her to abduct her arms to about 30. to aid balance. Then she should lift her hips to make a straight line from the shoulders to the hips and feet.
Reverse Bridge and Roll .f!'1~'"
Strengthens trunk and hip muscles, while increasing leg motion control.
Once your client is in the high position of the reverse bridge movement, she should roll the ball toward herself by flexing her knees and hips; then roll it away by extending the legs again.
Heel Bridge .f!I7~'" Increases overload in the bridge position. Instruct your clien t to assume the high position of the reverse bridge, with this difference: only her heels should be on the ball. Instruct her to push each heel alternately into the ball-this entails pushing down with the whole leg to activate the hamstrings and gluteals, rather than simply flexing the knee to work the hamstrings alone.
194
. BackStability
Single-Leg .f{'N.
Heel
Bridge
Provides maximal overload in the bridge position.
Your client's trunk should be on the floor, and only her heels should be on the ball. Have her lift one leg and hold it away from the ball. Then have her perform a single-leg heel bridge by pushing her heel into the ball and lifting her buttocks off the floor. She should hold the position for 5-10 seconds, then lower her body under control to the starting position.
Heel
Bridge
With
Leg Raise,
Ball Rolling
.f{I1~'. Provides maximal overload in the bridge position, while increasing leg movement control. Instruct your client to begin as with the previous exercise, up through the point of raising one leg. At this point, she should roll the ball toward herself by flexing her knee and hip; then roll it away by extending her leg again.
Prone
Fall
.f{'1~'.
Provides co-contraction
for the hip and trunk muscles.
Have your client place his thighs on the ball, with his legs together and his hands on the floor. He should lengthen his body to achieve a neutral spine, and retract his head to maintain cervical alignment. He should begin with the ball close to his pelvis, and then walk his hands forward so that the ball moves down his legs toward the knees. By shifting the body's center of gravity farther from the center of the ball, this movement increases the leverage effect.
Advanced Stability Training.
195
Prone Fall With Arm Lift ."tN.'ncreases
overload in prone fall.
Have your client begin with the prone fall movement. Then he should lift one hand about 0.5 inches (1.3 em) from the floor without allowing the shoulder girdle to dip down. He then lifts the arm first to the side and eventually forward, pointing the hand and lengthening the whole body.
Prone Fall With Single-Leg Lift ."t7.:.'.'ncreases overload (especially for gluteals) in prone fall, while training for abdominal-gluteal co-contraction. Have your client begin with the prone fall movement, then lift one leg to 15° hip extension, keeping the knee locked. Instruct him to perform alternate single-leg lifts; to train for speed as well as strength, have him gradually increase the speed of the lifts. Eventually he should do them as fast as he can without losing correct alignment.
Wall Sit ."t7.:.'.
To prepare the body for lifting, while strengthening to provide power for the lift.
the legs
Your client performs the following exercise with the ball sandwiched between his back and a wall. This has two main advantages over simply leaning against the wall. First, vertical movement is easier because the rolling of the ball removes the friction between the individual's back continued
196
. Back Stability
Wall Sit, continued
and the wall. Second, these exercises require more control since the subject is leaning on a mobile object rather than a fixed wall. The greater degree of control builds more automatic stability (i.e., the individual need not focus so much on the stability muscles in order to keep them stable). While your client stands with his back toward the wall, his feet about 2.5 feet (0.75 m) from the wall, place the gym ball between the wall and the lumbar region of his back. Instruct him to lower his body to the sitting position while rolling the ball down the wall. Once he achieves 90° hip and knee flexion (a), he should hold the position for 5-10 seconds and then roll back up to the starting position. He can then progress to the single-leg wall sit (b).
Free Squat .flaB.
Teaches whole-body
control during vertical movement.
Place the gym ball on a collar to stop it from rolling. Have your client stand in front of the ball, feet astride. She should slowly squat, keeping her back aligned, until she sits on the ball, then slowly stand up again.
Arm Lift in 4-Point Kneeling .fle7.:.,.'ncreases
overall stability during shoulder movements.
Decrease the ball pressure for kneeling actions so that it will fit comfortably under your client's abdomen in 4-point kneeling. Once your client is kneeling over the ball, instruct him to lift first one (a) and then both continued
Advanced Stability Training
.
197
Arm Lift in 4.Point Kneeling, continued
arms to the horizontaL Tell him to "lengthen his body" through the arms and hold the fully extended position for 5-10 seconds. The next progression is for the client to extend his spine and lift his arms behind himself to the horizontal (b).
b
Double-Leg
Raise
.f'('7.'.'ncreases strength of hip and spine extensors, while promot. ing trunk stability. Your client begins as with the previous exercise, but with the ball lower down the body toward the hips. Have him first lift one leg to the horizontal, maintaining good body alignment throughout the action. He can then progress to lifting both legs. If your client's legs are especially heavy, his arms may lift from the floor during this exercise. To prevent this, he should hold onto a low object such as the legs of a heavy gym bench. He should hold the fully extended position for 5-10 seconds.
PROPRIOCEPTIVE The aim of most of the to move/position their become stable, and (2) second goal is virtually
TRAINING
training in this book is for your clients (1) to learn muscles in such a way that their lower backs will to keep their backs in the stable position. And the unattainable unless your clients' bodies learn to
198
. BackStability
do what is necessary without conscious thought. The movements, the postures, and the balance must be more automatic. This is the goal of proprioceptive training.
Theory of Proprioception Because I believe it is important that you know the underlying mechanisms behind the activities you prescribe for your clients, the next few paragraphs provide a brief overview of proprioception. Movement Sense Kinesthetic awareness, or "movement sense," includes the detection of both joint displacement and change in velocity (Le.,acceleration). It is commonly assessed by measuring the threshold to detection of passive motion (TIDPM): individuals simply state when they feel movement has begun. One cannot act to correct imbalance until one is aware that there is an imbalance. The awareness can be conscious or unconscious, however, and the corrective action likewise can be intentional or automatic. The purpose of proprioceptive training is to help individuals learn both to detect and to correct imbalances without conscious awareness that they are doing so. Consciously performed joint-positioning activities, especially at end range, will enhance the development of automatic control and cognitive awareness (Lephart and Fu 1995). Regulation of Muscle Stiffness Dynamic joint stability (Le., the body's ability to constantly make unconscious "microcorrections" to keep a joint stable) occurs via reflexes at the spinal level. And reflexes by definition are not conscious or intentional movements. A common illustration is the body's response when your finger touches a hot skillet. The incoming nerve stimulus (afferent, Le., going "toward" the central nervous system) doesn't even make it to the brain-rather, it gets only as far as the spinal cord before it is processed and an appropriate outgoing (efferent, i.e., going "away from" the central nervous system) signal is sent to the muscles: "Move your hand!" In fact, you end up moving your hand without thinking about it because your brain had nothing to do with the reaction-it all occurred in a "closed loop" of signals between your hand and your spinal cord. The ideal situation as far as back stability is concerned is that you have such "closed loop" efferent signals constantly going out to your stability muscles: the receptor nerves detect a slight increase in instability, they send messages to the spinal cord, and instantaneously outgoing "efferent" signals are sent out to tweak a multifidus muscle, to slightly increase tension in your left internal oblique muscle, etc. It
Advanced Stability Training
.
199
all happens dozens of times a second without your even thinking about it. Such is the goal of proprioceptive exercises. It is possible to "train" your nervous system to be more sensitive to incoming messages that say "stability is weakening" and to provide more automatic outgoing signals that instruct which muscles to change in which way. If such a fine-tuned system seems unimaginable, try this experiment: open a water faucet at least halfway, place a drinking glass under it, and keep the glass as perfectly level as you can. You'll find that you can keep it quite still. Now consider the complexity of the nerve signals involved in the task you just completed. Thousands of times a second, afferent signals left your hand with the message, "The cup has just gotten heavier." And thousands of times a second, efferent signals returned from your central nervous system: "OK, tighten such-and-such muscles a teensy bit more." But it all happens so fast, and the microadjustments are so smooth, that for the most part your hand is able to hold the drinking glass stable. This is a closed loop system. Your brain isn't significantly involved. The signals go to your spinal cord, they are processed, and the return messages head immediately back to your hand. Proprioceptive exercises involve sudden alterations in joint position in order to train the body's reflexes. Chapter 7 provided exercises to help your clients learn simply to reproduce passive positioning of body segments. The training in this section is similar to those activities, but on a very fast track! In order to thoroughly follow an individual's progress, you theoretically can measure the precise onset of muscle contraction in relation to joint displacement-unfortunately, however, you most likely would need to refer your client to a physical therapy department or specialist biomechanics lab to make accurate measurements. Yet, with experience, you can assess onset of muscle contraction to some degree by palpating the muscle during a passive movement test. This type of examination, while not exact, can be useful for muscle re-education. The aim is simply to note if the muscles are able to limit joint displacement and effectively stabilize the joint.
Benefits of Training Using TIDPM and reproduction of passive positioning (RPP), Barrack et al. (1983) found decreased kinesthesia with increasing age (Le., the closed loop system for stability works less well). Injury further reduces proprioceptive input due to prolonged inactivity and damage to proprioceptive nerve endings within the injured tissues. A number of authors have stressed the importance of proprioceptive training in rehabilitation following injury to the knee (Barrack et al. 1983; Beard et al. 1994), ankle (Freeman et al. 1965; Konradsen and Ravn 1990; Lentell et al. 1990), and shoulder
200
. Back Stability
(Lephart et al. 1994; Smith and Brunolli 1990). The functional importance of proprioceptive training has also been emphasized during rehabilitation of the spine (Irion 1992; Lewit 1991; Norris 1995a), although its use in spinal rehabilitation is less common than for other areas of the body. Proprioception and accompanying reflexes may indeed be enhanced with training. Barrack et al. (1983) found enhanced kinesthesia in trained dancers, and Lephart and Fu (1995) demonstrated the same in intercollegiate gymnasts. Both types of athletes practice free exercise using body weight as resistance and using complex multijoint activities. This type of training appears appropriate for proprioceptive rehabilitation. Proprioception and stabilizing reflexes may be enhanced by using training that involves complex multijoint activities.
KEY POINT:
The basis of proprioceptive training for the back is maintenance of stability against
a rapidly
applied force tending
to displace
the spine. In most cases,
you can instruct your clients to practice one or more of the following exercises for at least five minutes a day, four or five days per week. The limiting factor is whether or not your clients can keep their spines stable (they should stop before they lose stability). They should do the most advanced exercise(s) of which they are capable, as quickly as they are able-remember, the idea is to train their reflexes to act with such extreme speed that maintaining spinal stability will be as smooth an operation as your holding the glass motionless as it fills under a tap.
Rapid Displacement
in Sitting
.1"111.01.Develop muscle reaction speed for back stability. Have your client sit on a stool with her spine optimally aligned. A training partner stands behind her and presses against her shoulders from multiple directions to flex, extend, and laterally flex the spine. Initially the pressure should be even, but gradually it should become varied in both direction and force. The aim is for your client to be able to rapidly stabilize the spine before the spine moves away from its neutral position. Instruct her to relax her trunk muscles between repetitions (which should last about a minute each), rather than hold them rigidly braced throughout the whole exercise. If you have it available, you may want to use surface EMG to monitor changing muscle tone. As your client's reactions become more proficient, the movements should become fasterbut she must always maintain good alignment.
Advanced Stability Training.
201
Muscle Reaction Speed Using a Mobile Platform .1'1:11.'. Further develop
muscle reaction
speed for back stability.
Instruct your client to assume a 2-point kneeling position on a balance board and to align his lumbar spine into its neutral position. Then a training partner should push him off balance so that the platform tilts. The aim is to maintain lumbar stability as the board tilts, while keeping the edges of the board off the ground. Start with a rocker board (allows single-plane motion), advancing later to a domed balance board (wobble board) that allows trip lane motion. You may also want to use other mobile platforms such as the Fitter ski trainer (Fitter International Inc., Calgary, Alberta, Canada), the slide trainer (Forza Fitness Equipment, London, England), or a mini trampette (available in most large sports stores). Again, increase the speed of the movements as your client becomes more proficient.
Throw-Catch Activities
on a Mobile Surface
.1'1:11.'. Develop rapid-onset back stability. Throw-catch activities using a basketball or medicine ball will increase the challenge to the stabilizing system. The aim is to align the lumbar spine optimally while balancing on the mobile surface. As your client catches the ball, she must maintain spinal alignment in spite of the platform's motion. Instruct your client to increase the speed of the exercises as she becomes more proficient.
SUMMARY
· · · ·
Once individuals
have achieved
basic back stability
through
the
exercises in previous chapters, they can begin building greater stability and training their backs for sports or on-the-job lifting by using the advanced exercises in this chapter. Advanced stability exercises, with movement of limbs on the stable trunk, will greatly increase an individual's ability to maintain stability automatically, without conscious thought.
back
Exercises with gym balls also help develop automatic stability and help develop muscles that previous, more basic, exercises may not affect. Proprioceptive exercises can be very useful in training your clients' reflexes to automatically (unconsciously) keep the spine stable.
9 More Advanced
Stabilig Training! Weight Training and Plyometrics If one's
goal is merely to develop adequate back stability, special equipment is unnecessary. People with sport and occupational injuries, however, require limb strength in addition to back stability in order to complete their rehabilitation-especially if they are to resume on-the-job lifting tasks or sports activities in which the body works against resistance. Weight training has several important advantages for those with lower back problems. First, it can increase the limb strength that some people need. Second, it can further enhance trunk muscle strength/stability to the level often required in sports-especially contact sports where abdominal strength can have a protective function for the internal organs. Finally, weight training can help to guard against further back injury. When we use weight training for back stability, we are strengthening muscles upon an already stable base-weight training is appropriate only for individuals who have already re-educated and built up endurance within the stabilizing muscles. Weight training takes the process further, adding greater resistance both to strengthen muscle and to challenge the stability system itself. The target muscles are those of the trunk, the limb muscles attaching to the trunk, and the limb muscles that provide the power for lifting. Plyometric exercises also can enhance strength and stability, with the added benefit of training for very fast reaction times. Your clients can use plyometrics in place of weight training if they wish, although I suggest a combination of both if they can afford the time. They need good stability before beginning either kind of training-but since the speed of movement in plyometrics is far greater than that in basic weight training, your clients will need better stability to begin plyometrics than to begin using machine weights.
202
Weight Training and Plyometrics
.
203
Weight training or plyometric exercise for greater back stability is appropriate only for those who have already developed good back stability using exercises described earlier in this book.
KEY POINT:
WEIGHT TRAINING Emphasize to your clients that the weight training you are giving them is specifically part of a back stability program, and therefore the activities will be somewhat different from those they may see other people doing in the weight rooms. Make sure they understand that they must follow your instructions, resisting the temptation to emulate the practices of other exercisers.
Before You Start Before introducing any of these weight-training exercises, give your clients the following instructions: (1) They must keep the whole spine correctly aligned and the lumbar spine in neutral position. (2) They should perform abdominal hollowing to tighten the stabilizing muscles and provide a stable base upon which the limbs can move. (3) They should exhale when lifting a weight, rather than holding their breaths, and be careful that deep breathing does not lead to hyperventilation and associated dizziness. Weight training involves three types of muscle work. The weight is lifted through concentric muscle action, held steady by isometric action, and lowered under control by eccentric action. Your clients should use all three phases. Remind them that the common practice of lifting the weight rapidly and then dropping it minimizes eccentric and isometric action, both of which are vital to stability work. A ratio of lifting for a count of 3, holding for a count of 2, and lowering for a count of 4 will emphasize each type of muscle work. Your clients should feel comfortably challenged during these exercises rather than excessively strained. Their breathing rates will increase, but they should be able to talk normally at all times-if they are fighting for breath, the exercise intensity is too great for rehabilitation and you should stop the exercise. Individuals may sweat lightly and experience mild reddening/ darkening of the skin; but excessive red coloration and bulging of veins in the face and neck are indications that the exercise intensity is too great, and the exercise should be stopped. See that a therapist or trainer supervises your clients during the initial stages of weight training, until both parties are confident that the exercise techniques are correct.
204
. Back Stability
Safety Check All exercise equipment has risks that must be minimized (see "Safety Checklist for Weight Training," below). The risks fall broadly into two categories: those associated with moving machinery, and those associated with the lifting action itself. Here are the rules you should present to your clients, and the explanations you should give them for why the rules are important:
·
Control the weights. Moving weights carry considerable momentum. Unless the weights are kept under control throughout the full range of motion, there is considerable risk to joints and body tissues. When a limb reaches the end of its motion range, the ligaments and muscles surrounding it become tight and limit further movement. Movements that are too rapid lead to loss of control-the joint stops moving at the end of the motion range, but the inertia of the weight forces the joint further against the tightening support tissues, causing severe trauma or overuse injury. With a traumatic injury, tissues are suddenly tom and function is lost-the athlete sometimes feels the body part "tear" or "give." Bleeding and swelling result. Overuse injuries are more insidious. The tissues undergo microtrauma as they are continually pulled further than their normal range allows. The resulting low-grade inflammation in some cases gives rise to formation of scar tissue, and in others may actually pull a tendon attachment away from the bone. When this happens the bone membrane (periosteum) may be lifted and the area may calcify, giving a cloudy appearance on X ray. In either case, the message is clear: when using Safety Checklist
for Weight Training
.. .. . Remove jewelry.
Always warm up before training. Check machinery before use. Set up machinery to suit your height and weight. Tie back long hair and be careful with loose clothing.
..
Wearserviceable footwear-no flip-flops! Use correct exercise techniques and keep the weight under control. Watch your body alignment-keep a neutral, stable spine.
. .. Keep abdomen hollowed during exercises. Practice good back care-lift correctly.
..
Train within your own limitations.
Never train through an injury-see
a physical therapist.
Adapted, by permission, from eM. Norris, 1995, Weight training: Principles and practice (London: A & C Black).
Weight Training and Plyometrics
.
205
weight-training apparatus, your clients must always move the weights in a controlled fashion. When using weight-training equipment, your clients must move the weights in a controlled, slow manner. Tell them, "Make sure you control the weight; don't let it control you'"
KEY POINT:
·
Wear appropriate clothing. Even though most machines have guards, fingers and especially hair and clothing can be trapped in the moving weight stack with severe results. Instruct your clients to tie back long hair when they use machine weights and to keep loose clothing well away from the machines. They should remove watches, large rings, and dangling jewelry. Good sports shoes will help protect their feet-the weight gym is no place for beach shoes or flip-flops! Toes can be stubbed and free weights dropped onto feet. As well as giving your lower limbs better alignment, sports shoes offer the first line of defense against foot injuries. Adjust the equipment. Most good weight-training machines allow users to adjust the unit for the shape and size of their bodies. Make sure that the machine is set up beforeit is used, and that the user knows exactly how the machine works before beginning the exercise. Know your limits. Remind your clients to train well within their limits. An old adage says, "Never sacrifice technique for weight." Lifting a weight that is too heavy can impair both technique and body alignment and increase the risk of injury.
· ·
·
Listen to your body. Your clients must not train with an injury unless they are following a structured rehabilitation program. The key is to listen to the body, especially pain. Never allow an individual to exercise through increasing pain. If a movement hurts and is continued slowly, the pain may diminish-in which case the person is probably suffering from stiffness that is working loose. If pain increases, however, the movement must stop. Caution: remember that some rapid, repeated actions may "reduce" pain simply because the exercise hurts more than the injury! Alert your clients to this possibility, and remind them to stop such movements immediately if they even suspect a masking effect. KEY POINT:
Never exercise through increasing pain.
Machine Exercises A major advantage of machine exercises is that they usually allow only singleplane motions and are therefore easy to coordinate (pulleys are an exception-
206
.
Back Stability
because they allow motion in three planes, they require more complex coordination). Have your clients use "pyramid training," with light resistance for the first sets to prepare the muscles for higher overload. They generally should employ slow repetitions to make the movement exact, and light resistances in order to build endurance. Obviously, they should do all exercises using both left and right sides of their bodies-they should simply follow mirror-image instructions for anyone-sided exercises described in the next section. Once your clients have mastered the basic movements for any of these exercises, using fairly light weights, prescribe a progressive program similar to the following, taking your clients' individual needs into account: for each machine, determine the weight with which the clients can perform 15 full repetitions and still have enough energy left to do 3 or 4 more before reaching exhaustion. Prescribe 12-15 reps per exercise session, three sessions per week, skipping at least one day between sessions. After two weeks, they can increase the weight, again according to how much they can lift using 15 full reps and not quite be at the point of exhaustion. Let them follow this program-12-15 reps / session, three sessions / week, for a period of at least 16 weeks, never increasing the weights past the point where they can do 15 reps and still feel they can do several more. Remember, this is not a program of building photogenic bodies-it is a program designed to further increase back stability and help prevent future back problems. You can prescribe higher numbers of repetitions (20-25) to enhance muscle endurance rather than strength. Although 12-15 repetitions will produce some increase in both muscle strength and muscle endurance, higher numbers of reps are required for muscle endurance with minimal joint loading. This is relevant for clients whose clinical conditions preclude their handling larger weights. Those with high blood pressure or severe osteoporosis, for example, may require higher numbers of repetitions with very little resistance. This type of workout will help your clients learn the proper movement without overloading the joints. The weight your clients lift should always feel comfortable and lightly challenging to them. If a weight feels too heavy, it will lead to poor exercise technique-and body alignment will suffer. If you see this happening, reduce the weight.
Lateral Pulldown .1'(t1~,.. To strengthen the latissimus dorsi (which tensions the thoracolumbar fascia, an essential component of stabilization). For the lat pulldown, one may lower the bar either behind the shoulders or to sternal level on the chest. Either position can be used, and both have continued
Weight Training and Plyometrics
.
207
Lateral Pulldown, continued
advantages and disadvantages. Pulling the bar behind the neck will increase your client's shoulder mobility, as that position requires a higher degree of external rotation at the shoulder than pulling the bar to the chest. Since external rotation is often limited, this is a desirable form of mobility training. Remember, however, that the seventh cervical vertebra has a very prominent spinous process (the point of bone pressing out through the skin), and your clients must take care not to strike this point with the bar. To lessen the likelihood of this happening, they should pass the bar behind the head by 2-3 inches (5-8 cm) rather than letting it brush the hair. In this way, the bar will miss the cervical spine and come to rest across the shoulders. Individuals unable to adopt this position should pull the bar to the upper chest. The action is a smooth pull downward, placing the bar (in the first case) behind the neck and across the shoulders. The head should be tilted forward slightly, and the bar must not strike the cervical vertebrae but rest across the middle fibers of the trapezius. The lowering action of the weight pulls the bar up again. Instruct your clients not to permit the weights to rest together at the end of the movement, so that useful traction will be maintained in the latissimus dorsi and the thoracolumbar fascia. Bringing the bar in front of the body to the top of the sternum reduces the range of external rotation and extension at the shoulder and is especially useful for less flexible individuals and those with a history of shoulder subluxation or dislocation. Although you may permit your clients to use whatever grip seems most comfortablewide, narrow, pronated, supinated, or midposition-keep the following in mind: using a narrow grip either on a standard wide bar or a box frame (with elbows in pronated or mid position) will allow the elbows to pass close to the sides of the body as the bar is pulled down; and, according to Weider (1989), keeping the elbows in will thicken the latissimus dorsi rather than broaden it. Using a supinated grip reduces the emphasis on the latissimus dorsi and emphasizes the biceps brachii.
208
. Back Stability
Cable Crossover .I{"~,,,
To strengthen the latissimus dorsi and pectoralis major.
The movement begins with both arms abducted. The feet are apart, slightly wider than shoulder width. The action is to exhale and pull both arms into adduction to the sides of the body. An alternate approach is to pull the arms forward across the chestthis technique increases the adduction range and emphasizes the pectoralis major. The elbows should be slightly bent throughout the movement, to reduce stress on the elbow joint.
Back Extension
(Machine)
.1{11~'" Strengthens
the erector
spinae (full range).
The back extension machine can help rehabilitate and strengthen the back extensors but can cause problems if faulty technique is used. It requires close supervision. Permit clients to use this machine only after they have mastered the hip hinge action and pelvic tilt movements (both in chapter 4). Have your client adjust the machine so that knees and hips are bent to 70-80° and the pivot point of the machine is aligned with the hip joint axis. The movement begins with a posterior tilt of the pelvis, moving the seat contact point from the ischial tuberosities back onto the sacrum. The action is movement of the pelvis on the stationary femur, with the back stabilized and immobile throughout the early part of the movement. Only when the second half of the movement range begins should the spine move into extension.
Weight Training and Plyometrics
.
209
Back Extension (Frame) .1'[t1~,.. Strengthens the erector spinae (limited range). The back hyperextension frame is useful in both the early and advanced stages of training but can be dangerous if used incorrectly. The exercise position is similar to the superman (pages 190-191). Quality supervision is vital. Be doubly sure that your client maintains the neutral position at all times during this exercise and is performing abdominal hollowing. Place a bench or stool in front of the machine, level with your client's shoulders. He should place his hands on the stool in a push-up position, with his legs locked onto the machine pads. He lifts first one hand and then both hands from the stool, placing his arms by his sides. Have him perform this action 10 times, resting his arms on the stool between each movement. Once he can perform this action in a controlled manner, add spinal extension. He should begin in the neutral position (with or without stool support), move into extension, lifting the shoulders about 2-3 inches (5-8 em) above the hip only, then back to neutral, and finally down into flexion. Avoid full inner-range extension, to reduce loading on the lumbar facet joints. Note that this action can injure an individual with poor back stability. At the beginning of the movement, if the abdominal muscles are relaxed, the pelvis will anteriorly tilt and the lumbar spine hyperextend, compressing the lumbar facet joints without sufficient intra-abdominal pressure to reduce the loading. Back stability and good alignment control are essential prerequisites for performing this exercise.
Seated Rowing .,{l7~'"
To strengthen scapular retractors (middle trapezius, lower trapezius, serratus anterior) and glenohumeral extensors (triceps)-bilateral.
Instruct your client to perform this exercise with her knees bent, in order to relax the hamstrings and allow the pelvis to anteriorly tilt sufficiently for her lumbar spine to remain in neutral position. The action is upper arm extension, keeping the elbows in to the sides of the body. The scapulae should adduct, and the thoracic spine extend in the stemallift action (chapter 7). When lowering the weight, she should not allow it to pull the thoracic spine into flexion.
210
. Back Stability
Single Arm Pulley Row .,{t1~'" Strengthens scapular retractors and shoulder extensors (as in seated rowing~unilateral. Because this exercise combines back extension and rotation with shoulder extension, it offers a significant challenge to the stabilizing system of the back. Have your client stand in a lunge position to the left of the pulley, with the left foot forward and the 0 handle of the low pulley gripped in the right hand. He should place his left hand on the left knee for support and angle his body forward (trunk on hip) at 45°. He then pulls the right arm into extension at the shoulder-and, as the pulley hand approaches his chest, he slightly rotates his trunk to the right and extends the thoracic spine (a) (stemallift action, see chapter 7). Using a low pulley position (pulley at mid-shin level) requires the exerciser to lean over slightly, increasing the workload on the spinal extensors (b). This is suitable only where alignment is good and the individual can keep his spine straight throughout the action. Placing the pulley at waist height negates the requirement to lean forward, taking the workload off the spinal extensors and reducing leverage on the spine. Use the waist-high position if your client's alignment is poor.
n
a
b
low Pulley Spinal Rotation .f['1~'"
Strengthens
oblique abdominals.
One can perform spinal rotation exercises in lying, sitting, or standing positions. For the lying exercise (a), have your client assume a half-crook lying position perpendicular to the direction of pull, flexing the leg closer to the pulley. Attach the cable of the pulley to
a continued
Weight Training and Plyometrics
Low Pulley
Spinal
Rotation,
.
211
continued
the flexed knee with a leather or webbing strap. The action is to rotate the spine so that the bent knee passes over the straight leg and onto the floor. In the sitting position (b), your client sits on a stool, facing perpendicular to the pulley, with .. her left side about 18 inches (0.5 m) from the pulley. She should flex her right arm 90° at the elbow, holding it across her body. After adjusting the level of the lower pulley so that it is level with her elbow, she should grip the D handle of the pulley with her right hand. The action is to b rotate her trunk to the right, keeping her hips, legs, and arm immobile so the weight of the pulley unit is lifted by the trunk action alone. The standing exercise is similar to the sitting. She again adjusts the pulley to elbow level and folds the outer arm across her body, her feet apart to maintain a wide base of support.
Rotary Torso Machine .1'(t1~,. To strengthen oblique abdominals while avoiding end-range movements.
Position the rotation lock to allow full rotation range but not to overstretch the spine. If rotation is painful or the range is limited, set the lock of the machine to avoid the painful end-range position. The action is a smooth rotation into full muscular inner range. Have your client hold the position and then slowly release it, avoiding the temptation to drop the weights rapidly and spin the machine. Reset the machine for the opposite rotation, remembering that range and strength are not necessarily symmetrical. Remember also that the full inner-range position into which an individual's muscles can pull (physiologicalinner range) is generally less than the full inner range into which he can be taken passively (anatomical inner range). As long as the motion is smooth and not too fast, your client is in no danger of overly stressing the facet joints of the spine during this exercise. If the motion is too rapid, however, the momentum of the machine can take the spine past physiological inner range and into anatomical inner range, loading the facet joints unnecessarily.
212
.
Back Stability
Abdominal
Machine
.f'(I1.". Strengthens the rectus abdom;n;s. Several abdominal machines are available on the market, but most provide resistance to trunk flexion, emphasizing the supraurnbilical portion of the rectus abdominis. Some provide additional resistance for the hip flexors working the infraumbilical portion of rectus abdominis as well. If possible, align the pivot of the machine with the center or lower portion of the lumbar spine rather than the hips. It is important that the rectus abdorninis does not bulge outward or "bowstring" during the action, but abdominal hollowing (practiced in all these exercises) will alleviate this potential problem. Have your client grip the machine arms, holding his elbows in throughout the action. Instruct him to "roll into flexion," keeping his back on the backrest and avoiding the tendency to lean forward. The movement begins by pulling the sternum down rather than forward. The eccentric component of the movement is important, so lowering the weight has to be slow and controlled.
Trunk Flexion With High Pulley (Pulley Crunch) .IIIH.
Strengthens
the rectus abdom;n;s.
Instruct your client either to kneel (2-point kneeling) or to sit, with his back to the machine, holding the 0 handle of the machine in both hands behind or in front of the neck (either is correctthe client should choose the most comfortable position). He should shuffle forward until he has taken up the slack in the machine cable. The action is to flex the trunk alone rather than the trunk on the hip (hip hinging), with the movement pointing the head downward toward the knees rather than forward in front of the knees. The action must be slow and controlled. Very little movement is available, so it is essential that the machine cable is tight before the action begins.
Weight Training and Plyometrics
.
21 3
Free Weight Exercises In the context of a back stability program, free weights are only for people whose bodies have heavy demands for strength and speed-generally, individuals who perform either medium or heavy manual handling on their jobs, or who are involved in strenuous sports. Free weights are also helpful in late-stage rehabilitation because of the complexity of skills they require (as compared with machine weights). It is best if, before beginning this stage, your clients have mastered the machine weight exercises just described, as those exercises help build the strength needed in these more complex free weight movements. They must do the exercises in this section only under strict supervision until they have perfected the actions. Give special consideration to clients younger than 18 or older than 60 years of age because their skeletons and joint structures are generally more prone to injury that those of other people. These individuals should exercise only under the supervision of a physical therapist or trainer who is specially trained to teach these groups.
~I
Individuals must demonstrate
good stability,
segmental control, and whole-body alignment before beginning late-stage rehabilitation exercises.
Special Concerns Regarding Free Weights Because free weight exercises combine both speed and weight, they expose the body to high levels of momentum (the product of mass X velocity). It's easy to stop a fast-moving arm if you have a pencil in your hand; but an arm moving at the same speed with a 20-pound weight in the hand can end up with torn tissues if the movement is not controlled. It is important that your sports-oriented clients-whether they swing objects such as racquets, or move their bodies quickly-learn to control momentum forces. The same is true for clients involved in moving or lifting heavy objects on the job. Before allowing individuals to begin free weight exercises, establish the following prerequisites and ground rules:
·
Your clients must have good stability and alignment. They must be able to maintain a neutral spinal position against limb resistance, as illustrated by good performance on the heel slide action (chapter 8, page 170). They must be able to maintain good alignment throughout the free weight-training program, keeping their lumbar spines in or near the neutral position at all times-the thoracic spine should be at its optimal position for each client, with shoulders held back comfortably (but not rigidly braced) and the chin held in.
214
.
Back Stability
· · ·
They must have good stability endurance. They should be able to perform 10 repetitions of each of the exercises in chapter 4, holding each rep for 10 seconds. They should have mastered all the machine weight exercises in the previous section of this chapter. They must warm up and stretch thoroughly before each weight session. First, they should lightly exercise (treadmill, stationary bike, etc.) till they just begin to sweat. Second, they should perform comprehensive stretching exercises that will take every major joint (hip, knee, shoulder, and spine) through its full range of motion. Third, they should rehearse each exercise by performing the first set at a light weight before adding further resistance. · They must stretch adequately after each weight-lifting session.
· At the beginning, a qualified trainer should supervise all free weight exercises, until both client and trainer are satisfied that the exercise technique is good.
·
Within the context of a back stability program, your clients should perform all free weight exercises progressively-first using light weights, then taking a rest period, then progressing to medium weights, another rest period, and finally heavy weights.
·
Free weight exercises as part of a stability program are not competitive; they are intended to progressively develop your clients' abilities to perform work against a resistance at speed. Clients should not compete with each other to see who can lift the most weight. Basic Free Weight Exercises For best results, have your clients go through all the following exercises in a single session. These exercises are appropriate for most individuals who fulfill the preliminary requirements just described. All the movements should be slow and well controlled. In the next section, I will describe more advanced exercises for people who need a great deal of "explosive power." Remember that the exercises are designed to build adequate strength, not bulk. Refer to Baechle (1994)for more detailed descriptions of the teaching points for these exercises. Because free weight exercises require more balance and coordination than do machine exercises, less weight should be used. Prescribe about 10-12 repetitions for each exercise, using a final weight that is comfortable for that number of reps (i.e., if the individual can perform 20 repetitions, the weight is too light; if he/she can perform only 5 reps, it is too heavy). For each exercise, your client should perform 2 or 3 sets of 10-12 repetitions: use a moderate weight (perhaps half the final weight) for the first set, three-fourths the final weight for the second,
.
Weight Training
and Pfyometrics
.
21 5
and the full weight only during the third set. In this way, the muscles gradually become accustomed to handling the weight. Your clients should rest after each set until their breathing rates and heart rates return to normalnever let them start a fresh set while their hearts are pounding or they are out of breath. Explain to your more impatient clients that this type of training is designed to "encourage" strength adaptation, not to "force" it. Training should be slow and controlled rather than fast and furious. Prescribe 2 or 3 sets for each exercise, three sessions per week, skipping at least one day between sessions. After two weeks, they may increase the target weight, again according to how much they can lift comfortably. Let them follow this program-2 or 3 sets of 10-12 reps, three sessions/weekfor a period of at least 16 weeks, never increasing the weights to the point where they feel exhausted. Remember that exercises described for just one side should be done on both sides, and that the instructions for the side not described are, of course, the mirror image of the instructions given.
Lying Barbell Row .flt1~'"
To strengthen shoulder retractors and increase thoracic spine extension (correct kyphotic posture).
Instruct your client to lie prone on top of a gym bench, with a light barbell (about 22.5-32.5 lb., or 10-15 kg) beneath the bench. She should grip the barbell at arm's length and lift it until it touches the underside of the ! bench. She may hold her elbows either close to the sides of her chest or with arms abducted to 90°-the narrow position places greater work on the latissimus dorsi, while the wider grip emphasizes the posterior deltoids and scapular stabilizers.
Dumbbell .fltH..
Row
Helps correct asymmetry between the shoulder retractors (middle and lower trapezius, serratus anterior).
You can recognize asymmetry by your client's inability to lift the same amount of weight, or to perform the same number of repetitions, with each arm. Have your client assume the half-kneeling position on a gym bench, his right arm and right knee on the bench and his left leg straight continued
216
.
Back Stability
Dumbbell Row, continued
with his left foot on the ground. He should grip a dumbbell (whatever weight feels comfortable to him) with his left hand, then pull (lift) it toward him, brushing the side of his body with his elbow. He should stop the movement when the dumbbell approaches his chest. As he pulls the upper arm into extension, the scapula is adducted; he should hold the inner-range position for 2-3 seconds before lowering the weight.
Good Morning .1'('1:.'" Works the spinal extensors statically and the hip extensors dynamically. This is basically a hip hinge action (several variations are in chapter 4) performed with a weight. Instruct your client to stand with her feet just wider than shoulder-width apart. Her knees should be unlocked to relax the hamstrings slightly and allow free pelvic tilt. With a light barbell (about 22.5 lb., or 10 kg) across her shoulders, she should tilt her pelvis anteriorly (always maintaining the alignment of the spine to the pelvis) so that her trunk angles forward to 45°. Watch carefully to be sure she does not allow her spine to flex, moving the axis of rotation from the hip joint to the mid lumbar spine-this stresses the spine considerably and can increase intradiscal pressure sufficiently to cause severe injury.
Squat .1'('1:.'" Teaches correct spinal alignment and strengthens quadriceps, hamstrings, and gluteals.
the
Have your client practice the correct form and movement using a light wooden pole (e.g., broom handle) until she has perfected the technique. The beginning weight should be 10-30% of body weight, depending on body build-stronger clients can use the larger value. Instruct your clicontinued
Weight Training and Plyometrics
.
217
Squat, continued
ent always to use a squat rack, so she can take the bar in the standing position. Her feet should be shoulder-width apart, toes turned out slightly. She should step under the bar, her hips directly under her shoulders, and, gripping the bar with hands slightly wider than shoulder width, place it across the back of her shoulders (over the posterior deltoids and trapezius). She should perform a sternal lift action and straighten both legs to lift the bar off the rack-then take a small step backward to clear the bar from the rack. Throughout the movement, your client should look up and keep her spine nearly vertical. The action is to flex hips and knees simultaneously, keeping the weight of the bar over the center of the foot rather than the toes. Instruct her to lower the bar under control until her thighs are parallel to the ground. After a momentary pause in this lower position to assist balance (but no bounce!), she reverses her actions to lift the bar. Watch to be sure her upward movement is controlled (no increase in speed toward the end of the action) and her knees stay over the foot rather than moving apart or together. Table 9.1 lists common errors associated with the squat. Table 9.1
Common Errors When Performing a Squat
Technique modification Error Knees come inward ("knock-kneed" Foot may be hyperpronating; conposition). sider more supportive footwear.
Knees stay behind feet throughout movement.
Practice a knee-bend position onto a bench in front of a mirror. Check if dorsiflexion range is limited in the ankle, and use a wooden block beneath the heels. Practice sitting onto a bench, pressing the knee forward onto the instructor's hand. continued
218
. Back Stability
Squat, continued
Table 9.1
(continued)
Error
Technique
Back angles
too far forward.
Spine flexes in thoracic
region.
modification
Press the knee forward, and aim to keep the spine more vertically aligned. Practice the basic squat motion sideon to a mirror. Ensure that adequate thoracic extension range is available, and practice the sternal lift motion in isolation. Strengthen the shoulder retractors and stretch the shoulder protractors (page 161).
Anterior pelvic tilt is exaggerated and lumbar lordosis increases.
Strengthen the abdominal muscles, and check for tightness in the hip flexors (chapter 7, pages 144-1 SO). Practice back flattening (chapter 7, page 149) against a wall.
Heel lifts.
Ensure that the weight of the bar is taken through the center of the foot, not through the toes. Check for adequate dorsiflexion range in the ankle, and use a wooden block beneath the heel.
Bar dips to one side.
Practice the squat in front of a mirror, and use a horizontal line drawn on the mirror to line up the reflection of the barbell.
Bouncing
Practice squatting onto a bench or
in the low position.
stool, lowering final position.
Barbell
gradually
into the
Lunge
.f{t1~,.. Helps improve spinal alignment and leg power, but with less spinal compression than in a squat. The start position is with the bar across the shoulders as for the squat. Because only one leg leads the movement, less weight (less than half) is used than in a squat-and so less spinal compression is created. Have your client stand with feet shoulder-width apart, the feet marking the end of an imaginary rectangle on the floor in front of him (shoulderwidth wide and twice shoulder-width long). As in the squat, he should perform a stemallift action while maintaining spinal alignment. Instruct him to step directly forward with the right leg (as though placing his continued
Weight Training and Plyometrics
.
219
Barbell Lunge, continued
foot along the long edge of the rectangle), then bend his knees so that the knee of the leading leg obscures the foot and that of the trailing leg moves toward the ground, stopping when it is 2-4 inches (5-10 cm) above the floor. The side of the trailing knee should be 6-14 inches (15-35 cm) from the inner edge of the heel of the leading foot. To stand up again, he pushes off the leading leg, bringing the leading foot back to its shoulder-width start position. The movement must not involve "falling" into the lower position or "jumping" into the upright position. Throughout the movement, your client should look up and forward, and the bar should remain horizontal.
Free Weight Exercises for Explosive Power Because of unusually heavy demands at work or in strenuous sport activities, some individuals require a high degree of explosive strength (Le., movement against a resistance [the weight] performed at speed [rapid resisted movements]). A variety of free weight exercises can help develop explosive power in the late stages of a sport-specific or workplace-specific back stability program. In order to perform these exercises, your clients must have progressed through the full back stability program and have good segmental control and spinal alignment. They should have mastered the machine exercises and basic free weight exercises in the previous section of this chapter. Have them rehearse all of the power movements using a wooden pole. Although you should still prescribe 2 or 3 sets of 10-12 reps, the first set should be with an empty bar to be doubly sure that the technique is correct and to train the muscles in the correct movements. Your primary guide for subsequent
sets must be spinal alignment
rather than the amount
of weight
the client can comfortably lift. If alignment is degraded, stop the exercise and reduce the weight, even if the client feels the resulting weight is "too light." Remember: the aim here is rehabilitation, not competitive weight lifting or body sculpting. For advanced free weight exercises, determine the amount of weight not according to how much your client can lift-rather, by how much your client can lift and still maintain correct alignment of the spine.
KEY POINT:
220
. Back Stability
Hang Clean .f["~,,,
Stage I power training.
Have your client begin with the barbell (held with hands pronated) resting on the middle of the thighs. For this exercise you should hand the bar to your client, who is already in the basic position illustrated by (a). Her body should be angled forward (30-45°) at the hips, and her spine straight. Knees and hips should be flexed, ankles dorsiflexed. The action is divided into two phases: the upward movement and the catch. During the upward movement, have your client hold her trunk erect and lift the bar explosively in a single "jump" action, extending the hips and knees and plantarflexing the ankles, without allowing her feet to come off the ground. Her shoulders should stay directly over the bar, and the path of the bar should be as close to the body as possible. At the point of maximum plantarflexion of the ankle, her shoulders will begin to shrug to continue the upward path of the bar (b). During the catch phase, which follows the shoulder shrug as a continuous motion, the client maintains the upward movement by flexing her arms. The elbows drop under the bar, forcing the wrists into extension to allow the bar to rest on the now horizontal palms (c). The elbows point directly forward, and the bar rests over the anterior aspect of the shoulders. As the bar touches the shoulders, your client should slightly flex her knees and hips to absorb shock and prevent a sudden jolt of the bar as she catches it on her shoulders. Instruct your client to lower the bar all the way to the ground, at first simply by reversing her earlier actions-she dips beneath the bar by bending her knees slightly, then allows her elbows to drop, with the bar staying close to the body as it is lowered. Her knees should bend so her body is not pulled into spinal flexion as the bar approaches the ground.
a
b
Weight Training
and Plyometrics
.
221
Power Clean .I'{IJ~'. Stage" power training. The power clean is a progression from the hang clean, with your client now lifting the weight from the floor rather than from the thighs. The barbell rests either on the floor or on two racks about 10-20 inches (25-50 cm) high. Instruct your client to stand with feet shoulder-width apart and knees inside the arms, feet flat and turned out slightly. It is important with this exercise that your client wears supportive training shoes-preferably a weight-lifting boot or high-cut cross-training shoes with broad, stable heels. Your client should grasp the bar with hands slightly wider than shoulderwidth apart, arms straight. She should squat down so that her shins are almost in contact with the bar, her knees over the center of her feet, her shoulders over or slightly in front of the bar (a). A common error with this movement is to get closer to the bar by flexing the spine, using only limited knee and hip flexion. This markedly increases the stress on the spine and must be avoided. The lift consists of three uninterrupted phases: (1) Instruct your client to extend her knees and move her hips forward as she raises her shoulders. Her shins should stay back (a common error with novices is to hit the knees with the bar), always maintaining the alignment of her back. The line of the bar's movement should be vertical, with her heels staying on the ground and the bar passing close to her body (b). Her shoulders should stay back, either over or slightly in front of the bar, and she should position her head to look straight ahead or slightly up. (2) For the "scoop," she drives her hips forward, keeping her shoulders over the bar and her elbows fully extended. The trunk is nearly vertical at this stage (c). This movement brings the bar to the midpoint of the thighs. (3) The exercise continues here as if it were the hang clean, through the upward movement and catch phases of that exercise (see illustrations for hang clean, previous page). The action is one of continuous movement, with no significant pauses between sections. Although the bar maintains its momentum, your client should never lose control of the movement. She should lower the bar in a vertical path, bending her knees to prevent her spine from being pulled into flexion.
222
.
Back Stability
Dead Lift .f{lN.
To improve back and hip strength, and add power for lifting.
The exercise begins with the bar on the floor (novices may use low racks at first, until they gain control through the full range of the exercise). Your client should stand with feet flat on the floor (heels must not lift) and shoulder-width apart, knees inside the arms, gripping the bar with hands pronated and slightly wider than shoulder-width apart, elbows pointing out to the sides. (Some athletes use an alternate grip, with one forearm pronated and the other supinated, i.e., knuckles down. If your client finds this grip more comfortable, by all means let him use itonly suggest that he alternate which hand is pronated and which supinated.) Have him position the bar over the balls of his feet, almost touching the shins, with his shoulders over or slightly ahead of the bar and his spine aligned in its neutral position (a). The movement begins by extending the knees and driving the hips forward. At the same time, your client raises his shoulders so that the alignment of his back remains unchanged. The path of the bar is initially vertical, and it is held close to the body at all times (b). The elbows must not bend, as that will cause a loss of power, and the shoulders should stay over or slightly in front of the bar. The head should be placed so that your client looks forward. Feet should remain flat. As the knees approach full extension, the back begins to move on the hip, maintaining spinal alignment (c). Have your client lower the bar with a squat motion, still maintaining the spine erect, keeping the bar close to the shins.
c
USING PLYOMETRICS TO TRAIN FOR POWER AND SPEED For most recreational athletes, almost any kind of training with more rapid movements (such as those in the free weight exercises) will suffice to im-
Weight Training and Plyometrics
.
223
prove speed. For clients who participate in higher levels of sports competition, however, or who simply want greater fitness gains than they have obtained after mastering everything in this book through chapter 8, proceed to the following plyometric exercises. These exercises can boost both reaction time and response time to high levels. There is no simplistic formula to help you decide, in consultation with your clients, whether they should do the exercises in this section in addition to the weight-training work just described, or instead of the weighttraining exercises. Together, you must weigh your clients' precise needs and goals. The main considerations will probably center around your clients' needs either for especially quick, strong reactions (e.g., hockey goalies or rodeo athletes), or for simple strength that must be explosive, but not necessarily blinding in its speed (e.g., football players or iron workers). If your client has the time and inclination, prescribe both kinds of exercise; if he has neither, but still wants to do more advanced work, choose either the weight training or the plyometrics. In order for you to understand the physiology behind the exercises, I need to present a bit of theoretical background. First, a few definitions: Power is the rate at which work is performed (work/time). Within the context of sports, Kent (1994) defined power as the ability to transform physical energy into force at a fast rate. Speed is simply the rate of movement. Reaction time is the time from the presentation of a stimulus to the initiation of a response. In terms of muscle work for stabilization, muscle reaction time is the time between the onset of a passive movement that disrupts stability and the initiation of muscle contraction to restabilize the joint. Response time combines both reaction time and movement time, the latter dependent on a variety of factors such as energy availability, nerve conduction, and actin/ myosin coupling. Good muscle reactiontime is vital to improving joint stability. Following ligamentous injury, for example, it is the reaction time of the supporting peroneus muscles that is the deciding factor for the return of full functionnot just the strength of the muscles (Freeman et al. 1965; Konradsen and Ravn 1990). And following knee injury, the important factor for rehabilitation is the reaction time of the hamstring muscles to resist anterior displacement of the tibia-not the strength of those muscles (Beard et al. 1994). The stretch-shorten cycle is important for anyone who trains for power and speed. Normally, the muscle supplies force through purely chemical means as actin and myosin filaments bond to cause the muscle to shorten. When an eccentric contraction (controlled lengthening) precedes a concentric action, however, force increases dramatically. Observe how a batter always swings his arms back immediately before swinging at a baseball. Or compare a squat jump (jumping from a static squatting position) with a countermovement jump (standing, dropping into a squat position, and then jumping). The height gained with the latter is greater than that from the former. Enoka (1988) measured average heights of 32.4 cm for
224
.
Back Stability
squat jumps, but 36.4 cm for countermovement jumps-more than 12% greater. The increased height comes from two sources: release of stored elastic energy, and additional chemical energy through a preload effect. In a countermovement, the extra energy gained relative to a standard movement comes from the release of stored elastic energy within the muscle, and from the preload effect.
KEY POINT:
Elastic energy results from passive stretching of the elastic components of the muscle. The muscle membranes (endomysium, epimysium, etc.) are noncontractile, but they are elastic and will recoil when released from a stretch, as will muscle tendons. The combined recoil of membranes and tendons provides a significant amount of energy. It takes time for actin and myosin coupling to occur. Chemical energy increases in a countermovement because, when the muscle is contracted eccentrically before it is contracted concentrically, the additional time permits more coupling-which leads to release of more chemical energy. Providing extra time to allow chemical reactions to occur creates the preload effect. Think of elastic energy as the muscle's springing back or recoiling like an elastic band-it is passive, and physical; whereas preload is like giving the muscle a running start on the chemical processes that lead to earlier contraction-it is active, and chemical. Three factors are important to energy release during concentric-eccentric coupling (Enoka 1988): 1. Time. If there is a delay between stretching the muscle and concentric contraction, some of the stored energy is dissipated. During the delay, actin and myosin filaments become detached and reattach farther along the muscle fiber under less stretch. 2. Magnitude. If the stretch magnitude is too great, fewer crossbridges are able to remain attached, and less elastic energy is available. 3. Velocity. A more rapid stretch (greater velocity) creates more elastic energy. To create maximum power with concentric-eccentric coupling, an individual must be warmed up; and a rapid eccentric movement must be followed immediately by a rapid concentric movement with no rest between the two phases. Any standard exercise can be performed in this way, and the exercises created are known as plyometrics. Yet not all exercises should be included in a plyometric workout since leverage forces and momentum acting on the spine can be dangerous: beware especially of rapid endrange motion on the spine and long lever movements.
Weight Training and Plyometrics
.
225
Before You Start Before progressing to the following plyometric exercises, your clients must
· ·
demonstrate good basic stability-able to perform the heel slide exercise (chapter 8, page 170) 10 times, and in general to perform adequately the exercises in chapter 4;
·
demonstrate good power and control in the trunk-able to perform gym ball exercises, including the superman (chapter 8, page 190) and bridge (chapter 8, page 191); and have good overall general fitness-demonstrated by regular, moderateto-intense exercise over the previous six to eight weeks. The exercise intensity should have been sufficient to raise the heart rate above 100 beats per minute. Each exercise session should have lasted for a minimum of 20 continuous minutes, with three periods of exercise per week.
Plyometric Exercises A number of exercises are useful. Be certain that your clients are supervised during all of them until both subjects and trainers are satisfied that your clients have learned the proper technique. Have your clients perform each exercise (for both right and left sides if it is asymmetrical) a maximum of 20 times per session, stopping earlier if they lose alignment or abdominal hollowing. They should try from one to three sessions per week for at least eight weeks, gradually increasing the speed of their movements as they are able. After the eight-week period, your clients may stop using plyometrics unless they are competitive athletes who require explosive strength to aid performance-in which case their strength coaches should prescribe the advanced plyometric exercises, tailoring them to the athletes' particular sports or events.
Plyometric Side Bend Using a Punching Bag .1'111.-'. Develops power and speed of the trunk side flexors while maintaining back stability. Instruct your client to stand with his left side toward a punching bag, feet shoulder-width apart, with his left arm abducted to 90°. He should flex his trunk to the left and push (not hit) the bag with his straight left arm. As the bag swings back, he takes its weight with his straight arm, then side flexes to the right to decelerate the swing of the bag (stopping short of full range!). The left side flexion begins the motion again. The action is reversed with the subject standing with his right side toward the bag.
226
. Back Stability
Plyometric
Flexion
and Extension Using a Punching Bag .1'{11~'" Develops power and speed in the trunk flexors and extensors while maintaining back stability. Have your client stand facing the punching bag, then push the bag with one or both hands. He should follow the movement through, using trunk flexion only, to 45°. He remains in this flexed position, and, as the bag swings back, he takes the bag with his arms straight (but unlocked) and flexes the arms, extending his trunk minimally and transferring his body weight to his back foot to cushion the momentum of the moving bag.
Twist and Throw With Medicine Ball .l'{lm.. Develops power and speed of the trunk rotators while maintaining back stability. Your client should stand in an aligned posture, with stabilized trunk and minimal abdominal hollowing. A training partner, facing in the same direction as your client, stands about three feet to her right, holding a medicine ball. While your client rotates her trunk to the right, her partner throws the medicine ball to her. As she catches the ball, she should rotate to the left, prestretching the oblique abdominals. She stops the movement short of full range, rotates back to the right, and throws the ball back to her partner.
Medicine .I'{IH..
Ball Trunk
Curl
Develops power and speed in the trunk flexors while maintaining back stability.
This exercise is a modification of the trunk curl (chapter 6, page 126). Instruct both your client and his training partner to lie on a mat with continued
Weight Training and Plyometrics
.
227
Medicine Ball Trunk Curl, continued
their knees bent (crook lying), such that their ankles are almost touching. They should then raise their trunks (without significantly moving their legs) to a stable upright position. The training partner throws a medicine ball to your client, who catches it while in the upright position, holding it close to his chest, but then moves back into the lower trunk curl position. He should stop the movement short of full range (his back should not touch the ground), then "bounce" back with a concentric trunk curl and throw the ball back to his partner. Increase the range of the curling action by having your client lie over a cushion-this allows the trunk to move into extension before moving into flexion. Be sure that movement stops short of full range in each direction in order to reduce joint loading.
Leg Raise .1'(.1.'1.
Throw
To develop
power and speed in the lower abdominals.
Make sure your client can easily perform the wall bar hanging leg raise (page 129) before attempting this movement. Your client should hang from a gymnasium beam with a ball beneath him. ,, Instruct him to grip the ball between both feet, then flex his hips and spine to throw the ball forward to a waiting partner. The partner places the ball back between your client's feet while the hips are still flexed to 90°. Your client then lowers his legs to prestretch the lower abdominals before repeating the movement.
SUMMARY
·
It is imperative that individuals be able to consistently hollow their abdomens, contract their multifidus muscles at will, and maintain neutral position before they attempt these exercises.
.
228
·
· · ·
Back Stability
After (and only after) your client has attained basic back stability using exercises presented earlier in this book, he/she can progress to using (1) machine exercises and/ or (2) plyometric exercises, each of which can further stabilize the back and help prevent future injury. Basic free weight exercises are useful for people whose jobs or sport activities demand greater back stability than that created by the earlier exercises. Advanced free weight exercises are appropriate for those whose jobs or sport activities are extremely demanding and require "explosive strength." Plyometric exercises are particularly useful for individuals who need
veryfast reaction times along with strength in their movements.
·
Because the material in this chapter is specifically designed for individuals with a history of low back pain, the exercises may differ from those you might prescribe for other individuals.
PART
ITW
Putting It All Together Although chapters 1 through 9 provide everything you really need to know in order to prescribe a very effective back stability program for virtually any client, I have summarized some ideas in chapter 10 ("Building a Back Stability Program for Your Client") that should help you synthesize the theoretical and practical material more easily. In chapter 10, you'll learn more about how to deal with pain since you generally will need to take care of that before even attempting to prescribe exercises. And I provide general tips about how to decide which exercises to prescribe for whom. Possibly the most helpful part of this chapter is the four case histories, which help you understand how to deal with four different kinds of client, from your first meeting until you discharge them. Chapter 11, "Preventing Back Injuries and Reinjuries," advocates a more proactive approach to dealing with your clients' daily activities. It is very common for people to reinjure themselves by lifting objects they had no business lifting, or by lifting them in the wrong way. Some therapists merely hand clients a pamphlet that describes proper lifting procedures, but most clients do not take written material alone very seriously. Chapter 11shows you how to teach your clients to avoid reinjury, with the suggestion that you actually do a bit of role-playing in order to help your clients internalize the theoretical principles.
229
1l((D
Building a Back Stabili!I Prog!am for Your Client We have corne full circle from the preface and seen how the three components of muscle imbalance-correction of segmental control, shortening and strengthening lax muscles, and lengthening tight muscles--combine to produce back stability. Although there is a great deal of highly varied material in previous chapters, you should nevertheless find it rather easy to tailor a unique back stability program to each client, taking these three components into account as they are needed for each individual. It is largely a question of (1) assessing where the problems lie and (2) prescribing appropriate exercises to correct the problems. Yet before you even think about a back stability program for a given individual, make sure that you should be treating the individual in the first place.
PRELIMINARY
ASSESSMENT OF YOUR
CLIENT
Especially for individuals who have experienced serious cardiovascular illness, you must decide whether exercise is appropriate at all. It is rare, but occasionally you may see someone whose general health is in such a state that the slightest additional stress could be catastrophic. If you have any doubts about an individual, be sure to have him or her obtain clearance through a medical doctor before proceeding with therapy. Note also that, although a back stability program is generally suitable for even the very unfit, it is contraindicated in some cases where people are not able to practice it correctly. If hypertensive individuals cannot be taught to hollow without holding their breath, for example, then hollowing is clearly contraindicated. And advanced exercises using weights are contraindicated in cases of reduced bone density.
Pain If clients are in pain when they first corne to you, manage the pain before proceeding with any muscle training. If you are qualified to treat the pain, 231
232
.
Back Stability
then apply whatever treatments you deem appropriate. If you are not qualified, refer clients to someone who is and work jointly with that therapist. Pain can inhibit muscle contraction and can affect alignment by making people take up positions that are less painful, but that reinforce poor alignment. It is certainly true that back stability exercise can lead to significant pain relief (e.g., multifidus training can release back spasms), but such activities work best when used as an adjunct to pain-relieving treatments. Where pain is extreme, elimination of the pain may become the primary aim of treatment. Pain that occurs through muscle spasm, or through trigger points in tight muscles, may be relieved by treatments that reduce muscle tone-various physical therapy treatments, manual therapy, and/or stretching. See Norris (1999) for details of these types of treatment. Where pain is the result of persistent overstress on a hypermobile segment, focus initial treatments on segmental control and stability. You may have to create stability passively at first (through taping or splinting), until your client has gained sufficient control of the muscular stabilizing system.
Diagnostic
Triage
Diagnostic triage categorizes low back pain into three types: simple back ache; nerve root pain (the nerve root is the "T" junction of the nerve as it joins to the spinal cord-pain from this area indicates compression of the nerve by a spinal disc or other structure); or possibly serious pathology requiring referral to a specialist (Waddell et al. 1997). See "Diagnostic Triage," page 233. I do not generally recommend referral to a specialist for simple back ache, and clients with nerve root compression do not usually require referral
if their
pain resolves within four weeks of its on-
set. Clients with possibly serious pathology require prompt referral, while those with likely cauda equina syndrome (involving a group of fine nerves at the base of the spinal cord) require immediate referral. For individuals with simple back ache or nerve root compression, you generally can begin back stability exercises immediately (with or without other physical therapy treatment). Those with serious pathology, however, may require surgical intervention before you begin back stability exercise, but please note the discussion in chapter 1, page 6, concerning the appropriateness of surgery on low back pain. Back stability exercise is a necessity as follow-up therapy for those with a previous history of back pain but no current pain, and as a preventive therapy for clients with no history of back pain (table 10.1).
Diagnostic
Triage
Diagnostic triage is the differential diagnosis between 1. Simple back pain (nonspecific low back pain-Le., pain with no specific cause) 2. Nerve root compression 3. Possibly serious spinal pathology (such as bone damage, infection, carcinoma, or pain traveling/referred from the abdomen or gastro/ urinary systems) 1. Simple
back ache: specialist referral not required
Patient aged 20-55 years Pain restricted to lumbosacral region, buttocks, or thighs Pain is "mechanical" (Le., pain changes with and can be relieved by movement) Patient otherwise in good health (no temperature, nausea/dizziness, weight loss, etc.)
2. Nerve root pain: specialist
referral not generally first four weeks, if the pain is resolving
required
within
Unilateral (one side of the body) leg pain that is worse than low back pain Pain radiates into the foot or toes Numbness and paresthesia (altered feeling) in the same area as pain Localized neurological signs (such as reduced tendon jerk and positive nerve tests) 3. Red flags (caution) promptly to specialist
for possibly
serious
spinal
pathology:
refer
Patient under 20 or over 55 years of age Nonmechanical pain (Le., pain does not improve with movement) Thoracic pain Past history of carcinoma, steroid drugs, or HIV Patient unwell or has lost weight Widespread neurological signs Obvious structural deformity (such as bone displacement after an accident, or a lump which has appeared recently) Sphincter disturbance (unable to pass water or incontinent) Gait disturbance (unable to walk correctly) Saddle anesthesia (no feeling in crotch area between the legs) Cauda equina syndrome (refer to specialist immediately-i.e., same da0 If in doubt, always refer the patient to an orthopedic physical therapist. Adapted, by permission, from G. Waddell, G. Feder, and M. Lewis, 1997, "Systematic reviews of bed rest and advice to stay active for acute low back pain:' British Journal of General Practice 47: 647-652. 233
.
234
Back Stability
Table 10.1
Use of Back Stability
Exercises
Type of back pain
Back stability
Simple
Begin immediately; fully functional.
Nerve
Serious
root compression
No history
continue
until
Begin as pain allows; refer to specialist if no marked progress within four weeks.
pathology
Previous
exercise
Use back stability surgical/medical
back pain now resolved of back pain
exercise after intervention.
Use back stability full function.
exercise
to restore
Use back stability risk of developing
exercise to reduce back pain.
Reprinted, by permission, from G. Waddell, G. Feder, and M. Lewis, 1997, "Systematic reviews of bed rest and advice to stay active for acute low back pain," British journal of General Practice 47: 647-652.
GENERAL
PRINCIPLES FOR DESIGNING A STABILITY PROGRAM
There are a few basic principles that apply in every situation:
· .
If you are not trained to properly diagnose back ailments, proceed no further until you've referred your client to a trained therapist-then work as closely with that therapist as you can, prescribing exercises appropriate to the therapist's diagnoses. Remember the general principle that bed rest is counterproductive
(see
chapter 1). Except in unusual circumstances, get your clients up and performing controlled activities as quickly as possible after an injury. Start back stability work as soon as possible after you have determined
·
· ·
that such a program is appropriate for an individual. The longer people are unstable, the more likely they are to develop compensatory postures that will need to be retrained. Always pay close attention to pain-it can be a very reliable guide. In
a careful series of assessments, it can tell you where the problems lie; throughout an individual's program, it can tell you when to stop a given exercise. Remember
the principle of specificity: prescribe
specific activities
for
specific problems/goals. This is why careful assessment is so important. Many therapists have a one-size-fits-all program. I have heard about many unhappy individuals, especially in the United States, who have visited physicians because of back pain-and the way the
Building a Back Stability Program for Your Client.
235
doctor "treated" them was to hand them a "back care pamphlet" and instruct them to do all the exercises in it! After reading part I of this book, you know that you must deal with each individual according to his or her precise symptoms. Remember the principle of overload: if the overload is not great enough, there will be no training effect; your client will merely be engaging in physical activity rather than training. Too great an overload, however, will break down tissue; and since the body cannot adapt sufficiently to match the imposed stress, overuse injury results. Carefully following the exercise programs presented in this book will enable you to achieve a training effect with your clients and to avoid overtraining injuriesa particular danger with those who have experienced low back pain or back injury.
.
Be sure that you always have a clear vision of your goal for each individual, and of the best path to reach that goal. That path should consider all systems-muscle tightness/laxness, posture, strength, flexibility,reaction speed, skill, and even emotional factors. Be careful that you do not fall into the common trap of overemphasizing a single aspect of fitness or rehabilitation. This is especially easy to do when strong-willed, generally knowledgeable clients make it clear that they have a certain problem and they want it fixed in a certain way ("I hurt my back at work, and I need to do some weight training so I can lift boxes again. . ."). Working one system in isolation can do more harm than good. Excessive flexibility in relation to strength, for example, may lead to instability of a joint. Individuals with increased strength, but without parallel improvement in muscle reaction speed, may be unable to use their extra strength in functional situations (Konradsen and Ravn 1990). Increases in either strength or flexibility that fail to improve skill may make injury more likely (Tropp et al. 1993). PARALLEL
TRACKS
A STABILITY
IN DESIGNING PROGRAM
Because the body is a complex unit of closely interconnecting systems, any approach to treatment must be holistic, even if it targets a single system. In training clients for back stability, we constantly intertwine our focuses on correcting segmental control, shortening and strengthening lax muscles, and lengthening tight muscles. The order in which you use these exercises, of course, will depend on your clients' symptoms. You ideally want to pay attention to all these areas at all times. When time constraints require that you teach only one or two exercises, stretches, etc., at a time, simply focus first on the most problematic area. In the accompanying case histories, note how I generally started with just one or two exercises, aiming to solve the most acute problem first.
236
.
Back Stability
The following sections provide suggestions for parallel exerciseprogressions. Don't (for example) just look at basic stability, proceed to correct it, and finally go on to other items only after your client can do a great hip hinge. Assess basic stability, deep abdominal control, muscle imbalance, and posture when you first see a client. At first, you may need to deal only with the most glaring deficiency, as the case histories illustrate. By your third or fourth treatment session, you generally will want to prescribe appropriate measures to correcteachdeficiency at the same time, working on each "track" during each session, and prescribing home exercises for each area. This is not as time consuming as it sounds, as many of the exercises in this book address several aims at the same time.
Assess
Back Stability
Your first task upon seeing a new client is to learn how stable her back is-and, to the degree it is not stable, to determine wherein lies the instability and to begin creating stability through appropriate activities described in chapter 4. Almost all prescriptive journeys begin in chapter 4. Your clients should not advance to actual strengthening or even stretching exercises until they have mastered the movements in that chapter. The best way to begin assessment is with the heel slide (page 170): if the pelvis tilts, your client has an unstable back and you should begin by teaching her abdominal hollowing (chapter 4, page 83). If her pelvis does not move during the heel slide, indicating a degree of stability, begin by teaching your client to control pelvic tilt (chapter 4, page 74) and to assume/ maintain the neutral position (chapter 4, page 78), without ignoring abdominal hollowing, of course. She should progress through pelvic tilt actions, to supported hip hinge exercises, and finally to free hip hinge exercises (all in chapter 4). Once your client demonstrates adequate segmental control by being able to independently control her pelvis and spine, let her progress to the good morning exercise, first without and finally with light barbell weights (chapter 9, page 216).
Assess the Degree of Deep Abdominal Control Can your client perform abdominal hollowing in the prone kneeling position? If not, follow the instructions under "Teaching Your Clients to Use Abdominal Hollowing" in chapter 4 (page 81), especially the subsection on teaching tips (page 86). Once he has mastered abdominal hollowing in all positions, help him gradually build up his strength and endurance till he can perform the movement for 10 reps, 10 seconds each, in the kneeling position. For more advanced abdominal control, he can progress to limb-loading exercises in chapter 8--€specially the heel slide (page 170) and leg lowering (page 170).
Building
Assess
a Back Stability Program for Your Client.
237
Muscle Imbalance
For each client, go through all the assessments in chapter 5 under" Assessing Stretched Muscles" (page 103) and under" Assessing Shortened Muscles" (page 106).Then proceed to correct whatever deficiency you find. For stretched or weakened abdominal muscles, for example, prescribe appropriate exercises (look at the "goal" statements) from chapter 6 under "Modifications of Traditional Abdominal Exercises" (page 124) and" Ab Roller Exercises" (page 130). For tightened muscles, refer to "Stretching Target Muscles" in chapter 5 (page 113). If clients have both tight muscles and an unstable back, I suggest that you begin with stretching exercisesyour clients first must learn tofind the neutral position before they take the second step in doing exercises to help them maintain neutral position. Some clients, especially the elderly, will have chronic muscle tightness that is virtually impossible to cure completely. Yetyou are unlikely to meet someone whom you can't help at all-€ven if you cannot help people achieve optimal posture, you probably can help them move more freely, increase their range of motion, and experience less discomfort.
Assess Posture Assessing posture goes hand-in-hand with checking muscle balance and can often give the first indication of which muscles may need to be tested for imbalance. Select the procedures under "Basic Postural Assessment" (chapter 7, page 136) that you find most useful given your availability of equipment, and thoroughly assess your client's posture. If you suspect a muscle is lengthened, test its inner-range holding ability (e.g., test the gluteals for lordotic posture); if you think it is tight, use specific tests of muscle length (e.g., for lordotic posture use the Thomas test for tight hip flexors). Then train the muscle accordingly, using inner-range holding for lengthened muscles and static or PNF stretching for tight muscles. See "Principles of Postural Correction" (page 143) and "Posture Types and How to Correct Them" (page 145).
DESIGNING AN ADVANCED STABILITY PROGRAM After clients have achieved basic back stability, they may wish to press on with more intense work because of heavy physical demands from work or from athletic activities. Chapters 8 and 9 are for such individuals.
In General, Be Specific The single most important concept is to determine, in close consultation with clients, precisely what their needs/ goals are. Does she have to lift 50pound grain bags all day at work? Is he a tennis player whose body is
238
.
Back Stability
constantly twisted and exposed to very rapid loads? Is your client a doorman who spends eight hours each day standing up and moving relatively little? Is she a caregiver who must bend over and lift bedridden patients many times a day? Every individual's specific needs will call for specific exercises to strengthen, stretch, increase reaction speed, increase accuracy of movement, or whatever. And there is no way I can suggest sequences of exercises to cover all possibilities. That is why each exercise is preceded by a "goal" statement. Once you have determined specific goals for a client, select the exercises in chapters 8 and 9 that match those goals. Choosing the exercises is relatively straightforward. Where you must be very careful is in your exercise prescriptions. I have provided basic guidelines for the exercises in each chapter, either with introductory remarks or with the exercises themselves. But these are no more than guidelines. Carefully monitor your clients as they first perform any exercise, not only to be sure they are performing the exercises correctly, but also to be sure they are performing enough reps and using sufficient load to challenge their muscles, but not to excessively load them.
Tips for Designing
Weight-Training Programs
In addition to the rather specific instructions I provide for the weighttraining exercises, here are a few more strategies you can use to guide your prescriptions of exercises. The order in which weight-training exercises are performed in a single exercise session is important. In general, have your clients work large muscle groups first with multijoint exercises, and smaller groups second using isolation movements. A multijoint exercise is one that works a number of muscles, including those with a large muscle mass. For example, the bench press works the pectoral muscles and the triceps. Because the triceps are far smaller than the pectorals, they fatigue first and so are the limiting factor in the exercise. If the triceps are worked first, fewer bench press movements are possible and the pectoral muscles will not be sufficiently challenged. Another method of combining exercises is to use a superset (i.e., to work the muscles on one side of a limb, and then immediately [without a rest] work those on the opposing side). This type of training keeps the blood within a body part, while the individual muscles themselves have some rest. A typical superset routine would involve biceps-triceps-biceps. One way to provide maximum challenge to muscles is to use pyramid training. Have your client perform 12 repetitions with an average weight for the first set, 10 reps with a heavier weight for the second set, and finally 8 reps with the heaviest weight he can manage for the final set. In this way, the muscle is worked maximally, but only when it is thoroughly warmed up. See Norris (1995b) for further details of weight-training programs.
Building a Back Stability Program for Your Client.
CASE
239
HISTORY
The Overweight
Client
A 42-year-old man with a history of persistent back pain, AH worked on a production line. He was about 56 pounds overweight, with marked lordotic posture. The goal of my treatment was first to reduce pain and then to restore postural balance. In the first treatment session, I instructed AH to perform supine lying lumbar flexion, bringing the knees to the chest with overpressure to encourage flexion of the lumbar spine. The principle here was that AH's lordotic posture was placing an excessive extension stress on his low back. The flexion exercise that I used was designed to neutralize this. With repetition (15-25 reps), his low back pain eased. I showed him how to get onto and off the floor without bending and advised him to practice this exercise every two hours of the waking day for two days. I gave AH general advice concerning back care and resting, used standard physical therapy modalities to reduce local pain, and referred him to a dietician to begin a weight-loss program. By the second treatment session two days later, AH's pain was markedly reduced. I started him on a general aerobic exercise session with his back supported-he used static cycling (seat and handlebar adjusted to minimize back str~ss) and a ski trainer to perform heart-rate-controlled exercise for 15-20 minutes every other day. At the second session, I also started AH on stability training, beginning with abdominal hollowing in the 4-point kneeling position and using a webbing belt around his abdomen. Since AH was unable to perform abdominal hollowing correctly, I provided a surface EMG unit to give feedback. It took 40 minutes to re-educate deep abdominal contraction using surface EMG, palpation, and voice encouragement. But since AH was still unable to perform the exercise unaided, I did not yet prescribe abdominal hollowing as a home exercise. AH continued with his back care and aerobic training for two more days. During his third treatment session, AH was able to perform abdominal hollowing with a 5- to 7-second hold for 3 repetitions. We had to work hard to help him refrain from holding his breath-I encouraged him to count out loud as he performed abdominal hollowing, to show that he was breathing normally. AH progressed in hollowing his abdomen but found it difficult to control the neutral position of his spine without my feedback. I taught him abdominal hollowing in wall-support standing to allow him to practice at home without having to think about his spine. He used a belt, focusing on pulling his abdomina Is in and up from the belt. He particularly liked this exercise, as it began to give his abdominal wall a flatter appearance-and, combined with weight loss, AH's physical appearance began to be leaner. continued
I'
240
I
.
Back Stability
Case History, continued We repeatedly set goals: goals for weight loss, numbers of repetitions performed, holding time of exercises, and heart-rate-monitored exercise. AH's low back pain had now gone, and he progressed from abdominal hollowing in standing to standing posterior pelvic tilt. Since his cardiopulmonary fitness (measured as heart-rate recovery) had improved with a decline in percent body fat (38% to 30%), I had him increase his aerobic activity. He still used nonweightbearing or partial weightbearing activities in the gymnasium to reduce joint loading, but now he began walking (on grass/gravel with shock absorbing sports shoes) for 15-20 minutes daily. In an attempt to shorten AH's rectus abdominis, to his standing posterior pelvic tilt I added posterior tilt in the lying position, held for 20-30 seconds (breathing normally). AH had short hip flexors and hamstrings, and he stretched them using the half-kneeling hip flexor stretch and active knee extension. AH built up his stability work with kneeling activities (knee raise, 10 repetitions on each leg, holding for 10 seconds) and began hollowing his abdomen regularly during his walking. I discharged AH from physical therapy to a personal trainer at a local gymnasium, where he incorporated stability work into a general fitness and weight-loss program. Points to Note V' AH had mechanical back pain brought on by his lordotic posture. V' Posture correction began with weight loss. V' Because AH was initially unable to perform correct abdominal hollowing, I did not give this as a home exercise. V' Surface EMG proved useful in initially teaching abdominal hollowing. V' We repeatedly used goal setting. V' Since AH liked the standing abdominal intensely.
hollowing exercise, I used it
V' AH used aerobic training to aid general fitness as well as specific back stability. V' The back stability program formed a focus for more general lifestyle changes. V' When discharged from physical therapy care, AH continued stability program in another setting. CASE
Poor Stability
the back
HISTORY
in an Athlete
Twenty-six-year-old HC trains daily in a gymnasium, using either weighttraining apparatus (40 minutes) plus cardiopulmonary apparatus (20 mincontinued
Building
a Back Stability Program for Your Client.
241
Case History, continued utes), or step aerobics (60 minutes). One day she complained of low back pain the morning after training. X-ray examination of the low back and pelvic joints showed no abnormality, and blood tests were normal. She was referred to me for physical therapy three months after the onset of pain. Her lumbar spine and sacroiliac joints were unremarkable upon examination, but repeated lumbar extension-especially anterior pelvic tilt-caused pain. Kinesiological examination (movement analysis) showed poor lumbar stability with overhead movements and with hip extension actions in standing. HC stated that two exercises in particular gave rise to her pain following workouts: standing hip extension on a "multihip" unit that targets the gluteals and repeated overhead pressing actions in standing with an aerobics bar. Examination of these moves showed that her pelvis moved rapidly into anterior tilt and remained in that position throughout the exercises. In assessing He's abdominal musculature, I found high tone in the superficial abdomina Is, with marked muscular definition of the rectus abdominis (the "six pack"). Yet she performed poorly on stability tests, being unable to perform abdominal hollowing in 4-point kneeling while maintaining a neutral lumbar spine. In the heel slide action monitored by a pressure biofeedback unit, HC was unable to perform more than 3 repetitions before her pelvis tilted anteriorly. In 4-point kneeling, leg lifting actions caused marked muscle quivering, demonstrating poor performance. He's gross segmental control was also poor-she was unable to perform a controlled hip hinge action. She moved not into spinal flexion (like most people) but into extension, anteriorly tilting her pelvis and hyperextending her lumbar spine. In her first treatment session, I had her perform supine knee and hip flexion, to press the lumbar spine into flexion. I told her to do these movements at the end of each workout period. I temporarily removed the overhead press and hip extension exercises from her gym program. Following her first two workout periods after the first session, HC noted reduced pain in the mornings. I used video feedback to show HC her performance in the hip extension and overhead exercises. She was surprised, having been unaware of her lack of alignment. I had HC try to perform abdominal hollowing in 4-point kneeling, and she was able to perform the exercise within 2-3 minutes of being shown the movement. She then used abdominal hollowing in wallsupport standing, progressing to free standing after 2 sets of 10 repetitions. She used abdominal hollowing in free standing and free (stool) sitting during her gym workouts, performing a single set with a 3D-second hold, breathing normally. HC progressed quickly (within two weeks) to supine lying heel slide and finally to supine lying foot drop (2 sets, 10 reps, 3D-second hold). I prescribed 4-point kneeling knee movements to improve stability control. continued
242
.
Back Stability
Case History, continued By the third treatment session (10 days after beginning treatment), noting that HC was able to perform abdominal hollowing for 10 reps, holding each for 30 seconds, I prescribed the hip hinge action. Initially I had her use controlled pelvic tilt in crook lying. In that same session, she progressed to pelvic tilt in wall-support standing, and finally in free standing. She performed the hip hinge with a stick held along the length of the spine to give feedback about spinal position. Initially she performed the exercise next to a mirror, then without a mirror, then without a stick, and finally with her eyes closed (to overload proprioception). HC had mastered the hip hinge action by her fourth treatment session-at which point I had her perform overhead pressing actions with a stick, and perform hip extensions on the multihip unit with minimal weight. Her goal was to maintain abdominal hollowing and a neutral lumbar alignment throughout the exercise. I incorporated stability principles of abdominal hollowing (30% max contraction) and neutral lumbar alignment into all of He's exercise activities. PoiniS to' Note V' HC had excellent cosmetic appearance of her abdominal region (superficial abdominals), but poor deep abdominal control. V' She was unable to maintain neutral lumbar alignment, she had high muscle tone.
even though
V' I used extensive movement analysis and made a point of observing the exercises that HC practiced in her gym. V' She had poor segmental control, moving into extension rather than flexion as is more common. V' Video feedback permitted HC to see her alignment. use of a stick increased feedback.
Mirrors and the
V' HC was a regular exerciser and had good body visualization. able to pick up new exercise techniques very quickly. V' Deep abdominal training and segmental formed the basis of her program.
She was
control (hip hinge action)
V' I waited until after HC was pain free to begin the basic stability program.
CASE
HISTORY
Acute
Pain
DB, 34 years old, came to me with acute simple low back pain that was localized to the lower lumbar region and minimally referred into the right buttock. The pain was mechanical in nature, made worse by lumbar flexion continued
Building
a Back Stability Program for Your Client.
243
Case History. continued
and better by lumbar extension. Initially I treated the pain, using physical therapy and lumbar manipulation. Then I had her begin multifidus contractions in left side lying, while I palpated the right multifidus and encouraged her to attempt to "swell" the muscle beneath my fingers. Although unable to perform this action at first, by the end of the second treatment session she was minimally able to contract the multifidus. I had her perform rhythmic stabilizations in left side lying-I placed pressure over her pelvis and shoulder to encourage spinal rotation and instructed DB to resist this motion with slight muscle contraction. As contraction built in intensity, I changed my hand position to resist spinal rotation in the opposite direction. The combination of rhythmic stabilization and isolated multifidus contractions gave substantial pain relief, with pain reducing from 8 to 3 on a subjective scale (10 = most intense pain, 1 = least intense). In the second treatment session, I introduced abdominal hollowing. As DB lay prone, I instructed her to draw her abdomen in, in an attempt to pull her tummy away from the surface of the treatment table. Since DB was at first unable to perform this action, I used pressure biofeedback, placing the bladder of the biofeedback unit beneath her abdomen just above the top of her pelvis and inflating the bladder sufficiently for DB to feel pressure over the abdomen. I instructed her to draw in her abdomen in an attempt to pull away from the biofeedback unit, thereby reducing the pressure on the bag. I wanted DB to perform the exercise at home, but since she was unable to identify when she was performing abdominal hollowing correctly, I brought her husband into the treatment session and showed him how to assist her. At home, DB placed a folded towel beneath her abdomen in the same position that the biofeedback bladder had occupied. I instructed DB's husband to gently try to slide the towel out from beneath DB's abdomen, while his wife drew in her abdomen sufficiently to take her weight from the towel and permit it to be pulled away. I instructed her to repeat this exercise 3 times daily, performing 10 reps each time. Once DB was able to perform the hollowing action unaided in the prone lying position, I had her progress to abdominal hollowing in kneeling and sitting positions. While aiding DB in her back stability training, I also instructed her on general back care, with emphasis on correct sitting and resting postures. I also taught her basic lifting techniques for use in the home. She progressed through the early stages of the back stability program using the heel slide, kneeling leg lift, and hip hinge actions. I then referred her to an exercise instructor at a local health club, to perform a general exercise program incorporating back stability principles. Points fo Note Because DB was in intense pain, I used physical therapy for pain relief at the beginning of her first session, before introducing her to stability exercises later in the session. continued
244
. Back Stability
Case History, cOl1til1ued
V On the first day, I began teaching her to control the multifidus, helped in pain relief. V I used pressure biofeedback and palpation.
which
v I showed a family member how to assist with DB's abdominal hollowing exercises at home. v DB continued her back stability training at a health club, along with general fitness activities.
CASE
Patient
HISTORY
Unwilling
to Exercise
SD was a 53-year-old manual worker in a food company. About 42 pounds overweight, he had marked abdominal sagging and chronic back pain that was localized to the lower lumbar region. His erector spinae muscles were tight and thickened. When standing, SD had a flattened lumbar curve, showing a typical "flatback" posture. Examination of range of movement revealed a lack of lumbar extension, and grossly limited pelvic tilt during I forward flexion movements. The pelvis contributed little to forward bending since most forward movement came from the upper lumbar and lower thoracic spine. Examination of SD's lifting techniques showed repeated bending actions with his legs straight, and adoption of poor resting positions with marked spinal flexion. SD had attended his company's manual handling course and even a refresher course, but his line manager confirmed SD's unwillingness to practice correct handling procedures on a regular basis. My initial physical therapy treatment targeted pain relief, but I also wanted to make SD contribute to his own treatment by taking part in exercise. It required considerable persuasion to convince SD to begin exercising! I taught him passive extension procedures that involved his lying on the floor and pressing with his arms to encourage restoration of a normal lumbar curve. During this exercise, his pain reduced in intensity, and localized to the lumbar region, shrinking in size. To encourage correct bending, I placed 15-inch-long strips of nonelastic tape on either side of his spine, from the pelvic region to the mid thoracic area. As SD bent forward, the I tape tightened on the skin, restricting spinal flexion and encouraging him to bend from the knees. I taught SD pelvic tilting, first passively and then actively, during the first treatment session. Although I instructed him to continue practicing at home, he showed little willingness to do so. I therefore instructed him to visit the company medical center daily, to practice his exercises under supervision of a physical therapy assistant or nurse. He did this each working day for two weeks.
cOl1til1ued
Building
a Back Stability Program for Your Client.
245
Case History, continued In his second treatment session, I started SO on a single abdominal hollowing exercise, choosing hollowing in wall-supported standing (with a webbing belt) since it was easiest for him to perform. With the use of a mirror, palpation, and surface EMG feedback, he was able to perform consistent hollowing by his third treatment session. I then encouraged him to practice hollowing without aids in wall-support standing, instructing him to draw his abdominal wall away from the waistband of his trousers (without holding his breath) and to hold the contraction for 5-10 seconds. I told him to repeat the exercise 3 times daily for 10 repetitions. By our third session, the combination of increased flexibility to pelvic tilt and back taping made SO bend more correctly. I assigned hamstring stretching exercises (active knee extension) in a lying position-lO reps, holding each for 10 seconds, during his treatment sessions on alternate working days. I also referred him to the company occupational health nurse for advice on diet and monitored weight loss. Video feedback helped SO learn correct bending techniques; and he practiced the hip hinge action (with a stick placed along the length of the spine) first with and then without video feedback. After four treatment sessions and 10 days of supervised exercise, SO was pain free. (But I also discovered that SO stopped practicing his exercise program two weeks after treatment began!) I encouraged him to perform the hollowing procedure when walking to his tea break (morning and afternoon) and his lunch break. The action was to contract the muscles to pull away from the waistband, hold the contraction while taking 10 steps, relax for 10 steps, and begin over againa technique known as "postural walking." I told him to continue this contraction-and-rest procedure for the full length of the walk (about 5 minutes). Because this action was easy to perform and was built into SO's daily activity, he received it well. Three months after his first appointment, SO was still practicing the postural walking procedure daily. He reported a feeling of "strength" in his abdomen, with the added advantage of increased tone and a flatter stomach. Points to Note If' SO had a flatback posture and chronic back pain. If' Previous to my seeing him, SO had received only medication and passive physical treatments. If' He had taken no active part in the care of his own back condition. If' Back taping encouraged him to move more correctly. If' Because SO was unwilling to exercise on his own, I arranged for him to do his exercises at work under supervision of a PT assistant. If' Although he did not continue abdominal hollowing exercises at home, he liked the "postural walking" approach-which we therefore built into his daily activities.
.
246
· · · ·
Back Stability
SUMMARY When you first see a client, assess him or her for basic stability, posture, alignment, segmental control, and muscle imbalance.
Treat pain before proceeding with stability exercises. In many cases, your first several sessions will address only the most severe deficiency. By the third or fourth session, if not earlier, you generally will want to focus on all aspects of stability, prescribing exercises for any area where there is a deficit.
·
Prescribe specific exercises for specific goals; there is no such thing as a "general" prescription for back stability.
·
The principle of specificity applies also to advanced
·
stability exercises.
When prescribing procedures from chapters 8 or 9, target them to your clients' specific goals and needs, whether they are related to the workplace or to the playing field. Four case histories provide step-by-step examples of treatment programs for individuals with varying kinds of problems.
1l1l Preventing Back Injuries and Reinjuries It is surprising how many people go to a great deal of effort to follow a rehabilitation program after a back injury, only to reinjure the back by doing something foolish at home or at work. I strongly urge you to take a few minutes to go over the information in this chapter with your clients so that they will have an increased probability of maintaining the progress you've helped them achieve. In the large majority of cases, according to my experience, you will meet with mild resistance or even boredom, because most people will say (at least to themselves if not to you), "Yes, yes, I know all that, use your legs and not your back, don't bend over. . . ." Yet a significant number of these same people will end up doing something outrageously silly because they haven't internalized proper safety procedures. I suggest that you actually role play these ideas with your clients. After leading them through the information in this chapter, take just 5 or 10 minutes to point to various objects and say, "All right, let's say you have to carry that chair into the next room and set it against the wall. Plan it out for me, explain to me the proper lifting/carrying procedure, then show me how you would position yourself for the lift." (I don't suggest letting anyone do a heavy or awkward lift, for reasons of liability.)
KEEP THE SPINE VERTICAL Merely reaching over a table can tremendously leverage the stress on the spine. Picking up a mug of coffee from the opposite side of a table, for example, can produce more force against the intervertebral disks than lifting a 20-pound weight next to one's body. Remember, torque = force x the length of the lever arm. If the spine remains vertical, leverage is minimal. If the spine is allowed to move toward the horizontal, higher leverage forces increase the tendency for the spine to flex, loading the spinal tissues. An analogy: when a flexible fishing rod is held vertically, it remains 247
248
.
Back Stability
straight; if you tilt it, it bends under its own weight. In order to keep the rod straight in a tilted or horizontal position, you must support its weight. The same principle applies to the back. If you want to move your back away from the vertical, you should support it by placing your hand onto a nearby tabletop or chair or whatever, or onto your knee if nothing else is available. The additional support greatly reduces the stress on the spine and enables you to maintain correct alignment. Repeated flexion also adds to spinal stress, greatly increasing discal pressure and continually stretching the posterior spinal tissues. Over time, repeated flexion can lead to tissue breakdown. Microtrauma of this type gives rise to classical postural pain syndromes (McKenzie 1981). Instruct your clients to reduce their total amount of bending in anyone day by using more effective movements and by improving general back care. Figure 11.1 shows examples of poor general back care, along with alternatives for reducing stress on the spine.
~
Support the spine whenever it is not vertical, and reduce the total amount of bending.
PRINCIPLES
OF LIFTING IN THE AND ON THE JOB
HOME
Both at home and at work, your clients should follow the principles of good back stability in any lifting or other manual tasks. Most simply stated, they must plan their actions carefully and minimize the forces of the lift.
Planning Planning prevents surprises. One of the most common reasons for lifting injuries is failure to assess the entire situation before trying to move an object. Tell your clients they must evaluate three areas: 1. Assess the environment. Note the floor surface. Is it uneven? Is it wet? Are there potential trip hazards? They should plan the entire path over which they will carry the object. Does the path involve going through a doorway? If so, is it accessible and open? Is it wide enough? (It is amazing how often people will carry a couch or desk up to a doorway, only to discover the opening is too small!) Where is the object to be placed? If it is to go on a table, is there room for it or do other items need to be moved first? 2. Assess the object. The distribution of the object's weight can be even more important than the absolute weight. The heaviest part of the object should be held close to the body to reduce the leverage effect, and
Correct
/'
Incorrect
X
Vacuuming
Removing clothes from the dryer
Reaching for object on a high shelf
Lifting (or even talking with) a small child
Figure 11.1
Proper
and improper
back care in the home. 249
250
. BackStability
individuals must feel comfortable with the weight lifted in relation to their own health status, training, and capability. They should consider the size and shape of the object: a light object that is very bulky or that may shift (e.g., a container of powder or fluid) offers a greater potential for injury. They must also consider any possible danger from the contents-if a container holds acid, or a scalding liquid, what would happen in the event of an unforeseen accident? 3. Assess themselves. Do they feel confident that a lift is within their capability? Individuals with a knee injury, for example, may not be able to bend their knees sufficiently to lift the object in a correct manner. Are there any relevant medical conditions? Pregnant women should severely restrict their lifting; and individuals with heart disease, low back pain, or hip pathology will have reduced capacities. Many people injure their backs by trying to lift objects they suspected were too heavy for them. I often hear something like "I was afraid I couldn't lift it, but it had to be moved and I didn't have time to find help" when I examine people following back injuries. Especially in men, "machismo" is a very common and very dangerous attitude. Emphasize to your clients that it is in no way "wimpy" to admit they should not lift a given item. Such a statement in fact shows great wisdom and maturity. If special training is generally needed before a certain kind of lift, and if a person has not received that training, he certainly must not attempt it. In general, aspect of a lift, they should not attempt it. KEY POINT: the slightest safely.
if individuals
are unsure
about
any
individuals should not attempt any lift if they have doubts about their abilities to perform the lift
Minimizing the Stress of a Lift There are several ways to reduce the physical stress of a lift. The Safe Zone The center of gravity of the human body typically lies at the 52/53 level. Pulling an object near to this "safe zone" reduces the leverage forces acting on the body; allowing the object to move farther away from this point increases the leverage and therefore the stress. If holding an object within the safe zone next to the pelvis represents 100% lifting capacity, this capacity is reduced by 20% when the object is held a forearm's length from the body, and by 75% when the object is lifted at arm's length. Teach your clients to pull objects they are lifting toward the body's center of gravity at the sacrum-to pull them into the safe zone as soon as possible and keep them there as long as possible. When lifting something
Preventing
Back Injuries
and Reinjuries
.
251
from the floor, they should pull it in toward the body early in the lift by sliding the object along the floor. Only when the object is pulled close to the safe zone should the lift begin. Although it may not be possible to keep the object within the safe zone during the entire lift, the longer it is held there, the better. If a lift takes a total of 15 seconds to complete, it will be performed far more safely if the object is within the safe zone for 12 of the 15 seconds than if it is there for only 5 seconds. Since the lift takes the same total time in each case, lifting safely will not slow a person down. KEY POINT: I
Pull an object into the "safe zone" (near the
sacrum) as soon as possible during a lift, and keep it there for as long as possible.
Appropriate Stance and Grip Instruct your clients to use two hands when lifting a heavy object from the floor. They should stand at the comer of the object, with the feet at 90° to each other (figure 11.2). With this foot position, the knees pass to the
Figure 11.2 Double-handed
lift.
252
.
Back Stability
sides of the object as they are bent. At least one foot must stay flat on the floor, to aid stability. The hands should grip under the object ("hook grip") rather than merely at its sides, to avoid their slipping-elbows in to aid power; knees bent; the back aligned and near vertical for the majority of the lift (only when the object is approaching the floor, when the individual is setting it down, is the back allowed to flex slightly). Individuals should look up as they lift, to aid the general feeling of back extension; and their hips should remain below the shoulders at all times. For certain heavy, large objects such as a sack of grain or a bag of concrete (figure 11.3), suggest a modification of the double-handed lift called
@ Figure 11.3 (1) Bend knees to get close to the sack, gripping it at the top; (2) rapidly straighten the legs and pull the sack up high; (3) dip down beneath the sack as its momentum continues to carry it upward; (4) straighten the legs to stand up, holding the sack high against the chest.
Preventing Back Injuries and Reinjuries
.
253
a snatch lift. The snatch lift uses speed and momentum to reduce the strength needed for the lift, but is only possible for objects that can be grasped at the top. It is highly effective, but requires great skill and therefore practice. Since it is performed rapidly, there is little margin for error. The person lifting uses a position similar to that used for the double-handed lift, except the squat is not as deep. Gripping the object at its top, the individual keeps his back straight and his legs somewhat bent. The action is to rapidly straighten the legs and raise onto the toes (as with the power clean exercise, page 221) while pulling the object upward. Most of the power for the lift comes from the legs, the arm pull being used mostly to transmit the power and guide the path of the object. The object's momentum carries it upward-and at the height of its movement (when its weight feels minimal), the individual changes his grip to place his hands under the object and pull it firmly into the safe zone. Single-handed lifts are appropriate for lighter objects (figure 11.4). The individual should assume a lunge position, with feet shoulder-width apart and one foot forward of the other. If the right hand is used to lift, the left foot leads the movement and the left hand may be placed on the left knee for support. The back remains in its neutral position and is kept near the vertical throughout the lift. The knee of the forward leg should pass just over the foot, but no farther, so that the tibia of the leading leg is nearly vertical-this way the individual will be pressing her hand down on a more stable lower leg. If the leading foot is dorsiflexed too far, the hand pressing down on the knee will increase the range of dorsiflexion and make it more difficult to raise the body from the ground. Pushing and pulling activities can also place considerable stress on the back if they are performed incorrectly. It is essential that back alignment is maintained, and that the power for the movement comes from the legs rather than from the spine. Instruct your clients to begin a push either facing forward with their hands on the object and their arms straight, or facing backward with their backs flat against the object. In either case, they should keep their pelvises in neutral position and produce most of the power for pushing/pulling in the legs-power that is directed through the straight, stable spine to the object being moved. Make sure your clients know to take only small steps during the push/pull-overly large steps will overstretch the body and pull the spine out of alignment.
Figure 11.4 Single-handed
lift.
.
254
Back Stability
SUMMARY
· ·
Individuals should keep their spines vertical, or as near vertical as possible, during a lift. Repeated spinal flexion during lifting can lead to serious breakdown of tissues. Whenever the spine is not vertical, it should be supported by placing a hand either on a stable object or on the bent knee. Before lifting any object, individuals should plan the move: they should assess the environment, the object, and their own capabilities.
· ·
· ·
. .
If there is any doubt in individuals'
minds that they can safely lift/
carry an object, they should refrain from doing so. The "safe zone" is near the sacrum, since the average person's center of gravity is at approximately the S2/S3level. Lifted objects should be brought to the safe zone as quickly as possible, and remain there as long as possible. Individuals should use two hands to lift heavy objects. When lifting lighter objects with only one hand, they should place the free hand on a bent knee to provide support for the spine. The "snatch lift" is useful for lifting heavy objects that can be grasped at the top, but the movement is difficult and should be practiced before it is used.
Bibliography Adams, M. 1989. Letter to the editor. Spine 14:1272. Adams, M.A., and Dolan, P. 1997. The combined function of the spine, pelvis, and legs when lifting with a straight back. In Movement, stability and low back pain, ed. A. Vleeming. V. Mooney, T. Dorman, e. Snijders, and R Stoeckart. New York: Churchill Livingstone. Adams, M.A, and Hutton, W.e. 1983. The mechanical function of the lumbar apophyseal joints Spine 8:327-30. Adams, M.A.; Hutton, w.e.; and Stott,J.R.R. 1980. The resistance to flexion of the lumbar intervertebral joint. Spine 5:245-53. Adams, M.A.; McNally, D.5.; Chinn, H.; and Dolan, P. 1994. Posture and the compressive strength of the lumbar spine. Clinical Biomechanics 9:5-14. Allan, D.B., and Waddell, G. 1989. An historical perspective on tow back pain and disability. Acta Orthop Scand (Suppl) 60:1-5. Allison, G.; Kendle, K.; Roll, S.; Schupelius, J.; Scott, Q.; and Panizza, J. 1998. The role of the diaphragm during abdominal hollowing exercises. Australian Journal of Physiotherapy 44:95-102. Andersson, E.; Oddsson, L.; Grundstrom, H.; and Thorstensson, A 1995. The role of the psoas and iliacus muscles for stability and movement of the lumbar spine, pelvis and hip. Scandinawln Journal of Medicine and Science in Sports 5:1()'16. Appell, H.J. 1990. Muscular atrophy following immobilisation: a review. Sports Medicine 10:42-58. Aruin, AS., and Latach, M.L. 1995. Directional specificity of postural muscles in feed-forward postural reactions during fast voluntary ann movements. Experimental Brain Research 103:323-32. Aspden, R.M. 1987. Intra-abdominal pressure and its role in spinal mechanics. Clinical Biomechanics 2:168-74. Aspden, RM. 1989. The spine as an arch. A new mathematical model. Spine 14:266-74. Aspden, R.M. 1992. Review of the functional anatomy of the spinal ligaments and the lumbar erector spinae muscles. Clinical Anatomy 5:372-87. Atkinson, H.W. 1986. Principles of treatment. In Cash's textbaok of neurology for physiotherapists, 4th edition, ed. P.A Downie. London: Faber and Faber. Baechle, T.R 1994. Essentials of strength training and conditioning. Champaign, II.: Human Kinetics. Bandy, W.D., and Irion, J.M. 1994. The effect of time on static stretch of the flexibility of the hamstring muscles. Physical Therapy 74:845-52. Barrack, R.L., and Skinner, H.B. 1990. The sensory function of knee ligaments. In Knee ligaments: structure, function, and injury, ed. D. Daniel. New York: Raven Press. Barrack, RL.; Skinner, H.B.; and Brunet, G. 1983. Joint kinesthesia in the highly trained knee. Journal of Sports Medicine and Physical Fitness 24:18-20. Barrett, D.5.; Cobb, AG.; and Bentley, G. 1991. Joint proprioception in normal, osteoarthritic, and replaced knees. Journal of Bone and Joint Surgery 73B:53-56. Bartelink, D.L. 1957.The role of abdominal pressure in relieving the pressure on the lumbar intervertebral discs. Journal of Bone and Joint Surgery 398:718-25. Bastide, G.; Zadeh, J.; and Lefebre, D. 1989. Are the little muscles what we think they are? Surgical aud Radiological Anatomy 11:255-56. Beard, D.J.; Kyberd, P.J.; O'Connor, J.J.; Fergusson, e.M.; and Dodd, C.A.F. 1994. Reflex hamstring contraction latency in anterior cruciate ligament deficiency. JournalofOrthopaedicResearch12:219-28. Beiring-Sorensen, R. 1984. Physical measurement as risk indicators for low back trouble over a one year period. Spine 9:106-19. Bernhardt, M.; White, A.A.; Panjabi, M.M. 1992. Lumbar spine instability. In The lumbar spine and back pain. 4th ed., ed. M.l.V. Jayson. Edinburgh: Churchill Livingstone. Bernier, J.N., and Perrin, D.H. 1998. Effect of coordination training on proprioception of the functionally unstable ankle. Journal of Orthopedic and Sports Physical Therapy 27:264-75. Biedermann, H.J.; Shanks, G.L.; Forrest, W.J.; and Inglis, J. 1991. Power spectrum analyses of electromyographic activity. Spine 16:1179-84. Boden, S.D.; Davis, D.O.; and Dina, T.S. 1990. Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects. Journal of Bone and Joint Surgery [Ami 72:403. Bogduk, N.; and Engel. R 1984. The menisci of the lumbar zygapophyseal joints. A review of their anatomy and clinical significance. Spine 9:454-60. Bogduk, N.; and Jull, G. 1985. The theoretical pathology of acute locked back: a basis for manipulative therapy. Manual Medicine 1:78-82. 255
256
.
Bibliography
Bogduk,
N.; Pearcy, M.; and Hadfield, G. 1992. Anatomy and biomechanics of psoas major. Clinical 7:109-19. Bogduk, N., and Twomey, L.T. 1987. Clinical anatomy of the lumbar spine. Edinburgh: Churchill Livingstone. Bogduk, N., and Twomey, L.T. 1991. Clinical anatomy of the lumbar spine. 2d ed. Edinburgh: Churchill Biomec1umics
Livingstone.
Bradford,
F.K., and Spurling,
Bullock-Saxton,
RG. 1945. The intervertebral
J. 1988. Normal
and
abnormal
postures
disc. Springfield, in the sagittal
low back pain. Physiotherapy Practice 4:94-104. Bullock-Saxton,). 1993. Postural alignment in standing: a repeatability iotherapy 39:25-29. Bullock-Saxton, J.E.; Bullock, M.I.; Tod, C; Riley, D.R; and Morgan, young adult men and women. New Zealand journal of Physiotherapy Bush, K.; Cowan, N.; and Katz, D.E. 1992. The natural history of sciatica
IL: Charles C Thomas.
plane
and
their
study. Australian
relationship journal
to
of Phys-
A.E. 1991. Postural stability in 3:7-10. associated with disc pathology: a prospective study with clinical and independent radiographic follow up. Spine 17:1205-12. Cailliet, R 1981. Low back pain syndrome. 3d ed. Philadelphia: Davis. Cailliet, R 1983. Soft tissue pain and disability. Philadelphia: Davis. Chartered Society of Physiotherapy (CSP). 1998. Low backpain. Information for sufferers. [Online]. Available: http:.I'www.csp.org.uk [October 15, 1999]. Cappozzo, A.; Felici, F.; Figura, F.; and Gazzani, F. 1985. Lumbar spine loading during half-squat exercises. Medicine and Science in Sports and Exercise 17(5):613-20. Cholewicki, J., and McGill, S.M. 1992. Lumbar posterior ligament involvement during extremely heavy lifts estimated from fluoroscopic measurements. journal of Biomechanics 25(1):17-28. Comerford, M. 1995. Muscle imbalance. Course notes. Nottingham School of Physiotherapy. Comerford, M. 1998. Dynamic stability. Physiotools compatible computer programme. Physiotools development office. Pihapolku F. 02420. Jorvas. Finland. Cornwall, M.W.; Melinda, P.B.; and Barry, S. 1991. Effect of mental practice on isometric muscular strength. journal of Orthopedic and Sparts Physical Therapy 13:217-23. Cresswell, A.G.; Grundstrom, H.; and Thorstensson, A. 1992. Observations on intra-abdominal pressure and patterns of abdominal intra-muscular activity in man. Acta Physiol Scand 144:409-18. Cresswell, A.G.; Oddsson, L.; and Thorstensson, A. 1994. The influence of sudden perturbations on trunk muscle activity and intra-abdominal pressure whiJe standing. Experimental Brain Research 98:336-41. Crock, H.V., and Yoshizawa, H. 1976. The blood supply of the lumbar vertebral column. Clinical Orthopaedics 115:6-21. Crowell, RD.; Cummings, G.5.; Walker,J.R; and TIllman, L.J. 1994. Intra tester and intertester reliability and validity of measures on innominate bone inclination. Journal of Orthopedic and Sports Physical Therapy Davis,
20:88-97.
P.R., and
Troup,
JD.G.
1964. Pressures
Ergonomics 7:465-74. Day, J.W.; Smidt, G.L.; and Lehmann, 64:510-16. Delitto, R.S.; Rose,
S.J.; and
lifting. Physical Therapy Deutsch,
F.E. 1996. Isolated
of Manipulative Deyo, RA.; Diehl, New
England
in the trunk
cavities
T. 1984. Effect of pelvic
pulling.
tilt on standing
pushing,
posture.
and
Physical
lifting. Therapy
Apts, D.W. 1987. Electromyographic analysis of two techniques for squat 67:1329-34. lumbar strengthening in the rehabilitation of chronic low back pain. Journal
and Physiological Therapeutics 19:124-33. A.K.; and Rosenthal, M. 1986. How many Journal
when
of Medicine
days
of bed
rest for acute
low back
pain.
315:1064.
Eie, N. 1966. Load capacity of the low back. Journal of Oslo City Hospitals 16:73-98. Enoka, R.M. 1988. Neuromechanical basis of kinesiology. Champaign, IL: Human Kinetics. Etnyre, B.R., and Abraham, L.D. 1986. H-reflex changes during static stretching and two variations proprioceptive 010gy63:174-79. Etnyre, B.R., and
neuromuscular Lee,
E.J. 1987.
facilitation Comments
techniques.
Electroencephalography
on proprioceptive
Research Quarterly for Exercise and Sport 58:184-88. Fansler, CL.; Poff, CL.; and Shepard, K.F. 1985. Effects of mental Physical T.herapy 65:1332-38. Farfan, H.F. 1988. Biomechanics of the lumbar spine. In Managing Willis. London: Churchill Livingstone.
neuromuscular practice
and Clinical
Neurophysi-
facilitation
stretching.
on balance
in elderly
of
women.
low back pain. 2d ed., ed. W.H. Kirkaldy-
Farfan, H.F.; Osteria, V.; and Lamy, C 1976. The mechanical etiology of spondylolysis and spondylolisthesis. Clinical Orthopedics and Related Research 117:40-55. Freeman, M.A.R.; Dean, M.R.E.; and Hanham, I.W.F. 1965. The etiology and prevention of functional instability of the foot. Journal of Bone and joint Surgery 478(4):678-85.
.
Bibliography
257
Friedli, WG.; Hallet, M.; and Simon, S.R. 1984. Postural adjustments associated with rapid voluntary arm movements. Electromyographic data. Journal of Neurology, Neurosurgery and Psychiatry47:611-22. Frymoyer, J.W., and Cats-Baril, W.L. 1991. An overview of the incidences and costs of low back pain. Orthopedic Clinics of North America 22:263. Frymoyer, J.W., and Gordon, S.L. 1989. Symposium on new perspectives on low back pain. Park Ridge, IL: American Academy of Orthopedic Surgeons. Goldspink, G. 1992. Cellular and molecular aspects of adaptation in skeletal muscle. In Strength and power in sport, ed. P.V. Komi. Oxford: Blackwell. Goldspink, G. 1996. Personal communication. Gossman, M.R.; Sahrmann, S.A; and Rose, S.J. 1982. Review of length associated changes in muscle. Physical Th£rapy 62: 1799-808. Gracovetsky, S.; Farfan, H.E; and Helleur, C 1985. The abdominal mechanism. Spine 10:317-24. Gracovetsky, S.; Kary, M.; Levy, S.; Ben Said, R.; Pitchen, I.; and Helie, J. 1990. Analysis of spinal and muscular activity during flexion/extension and free lifts. Spine 15:1333-39. Gracovetsky, S.; Farfan, H.E; and Lamy, C. 1977. A mathematical model of the lumbar spine using an optimal system to control muscles and ligaments. Orthopaedic Clinics of North America 8:135-53. Guimaraes, ACS.; Vaz, M.A.; De Campos, M.LA.; and Marantes, R. 1991. The contribution of the rectus abdominis and rectus femoris in twelve selected abdominal exercises. Journal of Sports Medicine and Physical Fitness 31:222-30. Harman E.; Frykman, P.; Clagett, B.; and Kraemer, W 1988. Intra-abdominal and intra-thoracic pressures during lifting and jumping. Medicine and Science in Sports and Exercise 20:195-201. Hart, D.L, and Rose, S.J. 1986. Reliability of a non-invasive method for measuring the lumbar curve. Journal of Orthopedic and Sports Physical Therapy 8:180-84. Hemborg, B.; Moritz, U.; and Hamberg, J. 1983. Intra-abdominal pressure and trunk muscle activity during lifting---
165-72. Hirsch,
C and Schajowicz,
Orthopaedica Scandinavica Hirsch, C., and Nachemson,
F. 1952. Studies 22:184-89. A. 1954. New
Orthopaedica Scandinavica 23:254-83 Hodges, P.W., and Richardson, CA. 1996.
on structural
changes
in the lumbar
annulus
fibrosis.
observations
on mechanical
behaviour
of lumbar
Contraction
of transversus
abdominis
invariably
Acta
discs.
Acta
precedes
movement of the upper and lower limb. In Proceedings of the 6th Illternational Conference of the International Federation of Orthopaedic Manipulative Therapists. Lillehammer, Norway. Hodges, P.; Richardson, C; and Jull, G. 1996. Evaluation of the relationship between laboratory and clinical tests of transversus Holm, S.; Maroudas, A.; Urban,
abdominis function. Physiotherapy J.PG.; Selstam, G.; and Nachemson,
Research International 1:30-40. A. 1981. Nutrition of the intervertebral
disc: solute transport and metabolism. Cotlnect Tissue Res 8:101-19. Holt, L.E., and Smith, R. 1983. The effect of selected stretching programs on active and passive flexibility. Mar, CA: Research Center for Sport. Hughes, M.A.; Duncan, r.W; Rose, OK; Chandler, J.M.; and Studenski, S.A. 1996. The relationship postural
sway
to sensorimotor
function,
functional
performance,
and
disability
in the elderly
Del of Ar-
chives of Physical Medicine and Rehabilitation 77:567-72. Hukins, D.W.L. 1987. Properties of spinal materials. In The lumbar spine and back pain, ed. M.I.V. Jayson. Edinburgh: Churchill Livingstone. Hukins, D.W.L.; Aspden, R.M.; and Hickey, D.5. 1990. Thoracolumbar fascia can increase the efficiency of the erector spinae muscles. Clinical Biomechanics Hyman, J., and Liebenson, C. 1996. Spinal stabilization
5:30-34. exercise
ed. C Liebenson. Baltimore: Williams & Wilkins. Irion, J .M. 1992. Use of the gym ball in rehabilitation of spinal
program.
dysfunction.
In Rehabilitation In Orthopaedic
of the spine,
physical
therapy
clinics of North America. Oxford: Churchill Livingstone. Jacob, H.A.C, and Kissling, R.O. 1995. The mobility of the sacroiliac joints in healthy volunteers between 20 and 50 years of age. Clinical Biomechanics 10:352-61. Janda, V. 1986. Muscle weakI1l.'Ss and inhibition pseudoparcsis in back pain syndromes. In Modern manual therapy, ed. G. Grieve. Edinburgh: Churchill Livingstone.
258
. Bibliography
Janda, V. 1992. Muscle imbalance and musculoskeletal pain. Course notes. University of Oxford. UK. Janda, V. 1993. Muscle strength in relation to muscle length, pain and muscle imbalance. In Muscle strength. International perspectives in physical therapy, ed. K. Harms-Ringdahl. Edinburgh: Churchill Livingstone. Janda v., and Schmid, H.J.A. 1980. Muscles as a pathogenic factor in back pain. Proceedings of the International Federation of Orthopaedic Manipulative Therapists, 4th Conference, 17-18. New Zealand. Jensel, M.C.; Brant-Zawadzki, M,N.; and Obuchowki, N. 1994. Magnetic resonance imaging of the lumbar spine in people without back pain. New England Journal of Medicine 2:69. Johnson, C., and Reid, J.G. 1991. Lumbar compressive and shear forces during various curl up exercises. Clinical Biomechanics 6:97-104. Jorgensen, K., and Nicolaisen, T. 1987. Trunk extensor endurance: determination and relation to lowback trouble. Ergonomics 30:259-67. Jull, G.A. 1994. Headaches of cervical origin. In Physical therapy of the cervical and thoracic spine, ed. R. Grant. New York: Churchill Livingstone. Jull, G.A., and Janda, V. 1987. Muscles and motor control in low back pain: assessment and management. In Physical therapy of the low back, ed. L.T. Twomey. New York: Churchill Livingstone. Jull, G., and Richardson, CA. 1994a. Active stabilisation of the trunk. Course notes. University of Edinburgh. Jull, G.A., and Richardson, CA. 1994b. Rehabilitation of active stabilization of the lumbar spine. In Physical therapy of the low back. 2d ed., ed. L.T. Twomey and L.T. Taylor. Edinburgh: Churchill Livingstone. Kapandji, I. 1974. The physiology of joints, vol. 3. The spine. London: Churchill Livingstone. Kendall, EP.; McCreary, E.K.; and Provance, P.G. 1993. Muscles. Testing and function. 4th ed. Baltimore: Williams & Wilkins. Kennedy, J.C; Alexander, I.J.; and Hayes, K.C 1982. Nerve supply of the human knee and its functional importance. American Journal of Sports Medicine 10:329. Kent, M. 1994. The Oxford dictionary of sports science and medicine. Oxford: Oxford University Press. Kesson, M., and Atkins, E. 1998. Orthopaedic medicine. A practical approach. Oxford: Butterworth Heinemann. Kippers, V., and Parker, A.W. 1984. Posture related to myoelectric silence of erectores spinae during trunk flexion. Spine 9:74045. Kirby, M.C; Sikoryn, T.A.; Hukins, D.W.L.; and Aspden, R.M. 1989. Structure and mechanical properties of the longitudinal ligaments and ligamentum flavum of the spine. Journal of Biomedical Engineering 11:192-96. Kirkaldy-Willis, W.H. 1990. The lumbar spine. New York: Saunders. Klein, J .A., and Hukins, D. w.L. 1983. Relocation of the bending axis during flexion-extension of the lumbar intervertebral discs and its implications for prolapse. Spine 8: 659-64. Koh, T.J. 1995. Do adaptations in serial sarcomere number occur with strength training? Human Movement Science 14:61-77. Konradsen, L., and Ravn, J.B.1990. Ankle instability cause by prolonged peroneal reaction time. Acta Orthop Scand 61:388-90. Kraemer, J.; Kolditz, D.; and Gowin, R. 1985. Water and electrolyte content of human intervertebral discs under variabJe load. Spine 10:69-71. Lacote, M.; Chevalier, A.M.; Miranda, A.; Sleton, J.P.; and Stevenin, P. 1987. Clinical evaluation of muscle function. Edinburgh: Churchill Livingstone. Lavignolle, B.; Vital, J.M.; and Senegas, J. 1983. An approach to the functionaJ anatomy of the sacroiliac joints in vivo. Anatomia Clinica 5:169-76. Leatt. P.; Reilly, T.; and Troup, J.G.D. 1986. Spinal loading during circuit weight-training and running. British Journal ofSparts Medicine 20(3):119-24. Lee, D.G. 1994. Kinematics of the pelvic joints. In Grieves modern manual therapy, ed. J.D. Boyling and N. Palastanga. Edinburgh: Churchill Livingstone. LenteJl, G.L.; Katzman, L.L.; and Walters, M.R. 1990. The relationship between muscle function and ankle stability. Journal of Orthopedic and Sports Physical Therapy 11:605-11. !.ephart, S.M., and Fu, EH. 1995. The role of proprioception in the treatment of sports injuries. Sparts Exerciseand Injury 1:96-102. !.ephart, S.M.; Warner, J.P.; Borsa, P.A.; and Fu, EH. 1994. Proprioception of the shoulder in normal, unstable, and surgical individuals. Journal of Shoulder and Elbow Surgery 3:224-28. Lester, M.N., and Posner-Mayer, J. 1993. Spinal stabilisatio,,: utilizing the Swiss ball video. Denver: Ball Dynamics. Levine, D.; Walker, J.R.; and TIllman, L.J. 1997. The effect of abdominal muscle strengthening on pelvic tilt and lumbar lordosis. Physiotherapy Theory and Practice 13:217-26.
Bibliography.
259
Lewit, K. 1991. Manipulative therapy in rehabilitation of the locomotor system. 2d ed. Oxford: Butterworth Heinemann. Liebenson, C. 1996. Rehabilitation of the spine. Baltimore: Williams & Wilkins. Lieber, R.L. 1992. Skeletal muscle structure and function. Baltimore: Williams & Wilkins. Linsenbardt, S.T.; Thomas, TR.; and Madsen, R.w. 1992. Effect of breathing techniques on blood pressure response
to resistance
exercise.
British
/ouma1
of Sports
Medicine
26:97-100.
Lipetz, S., and Gutin, B. 1970. An electromyographic study of four abdominal exercises. Medicine and Science in Sports and Exercise 2:35-38. Long, D.M. 1995. Effectiveness of therapies currently employed for persistent low back and leg pain. Pain Forum 4:122-25. Lord,S.R.;Ward,J.A.; Williams, P.;and Zivanovic, E. 1996. The effects of a community exercise program on fracture risk factors in older women. Osteoporosis International 6:361-67. Lovell, F.W.; Rothstein, j.M.; and Personius, w.j. 1989. Reliability of clinical measurements of lumbar lordosis taken with a nexible rule. Physical TIIerapy 69:96-105. Luttgens, K.; and Wells, K. 1982. Kinesiology. Scientific basis alld human motion. 7th ed. Philadelphia: Saunders College Publishing. Macintosh,j.E., and Bogduk, N. 1986. The biomechanics of the lumbar multifidus. Clinical Biomechanics 1:205-13. Macintosh, j.E., and Bogduk, N. 1987. The anatomy and function of the lumbar back muscles and their fascia. In Physical therapy of the low back, ed. L.T Twomey. New York: Churchill Livingstone. Macintosh, j.E.; Bogduk, N.; and Gracovetsky, S. 1987. The biomechanics of the thoracolumbar fascia. Clillical Biomechallics 2:78-83. Main, c.j., and Watson, P.j. 1996. Guarded movements: development of chronicity. Journal ofMusculoskeletal Pain 4:163-70. Maitland, G.D. 1986. Vertebral manipulatioll. 5th ed. London: Butterworths. Markolf, K.L., and Morris, j.M. 1974. The structural components of the intervertebral disc. Journal of Balle alld Joint Surgery 56A:675-87. McConnell, J. 1993. Promoting effective segmental alignment. In Kry issues ill musculoskeletal physiotherapy, ed. J. Crosbie and j. McConnell. Oxford: Butterworth Heinemann. McGill, S.M. 1997. Distribution of tissue loads in the low back during a variety of daily and rehabilitation tasks. Journal of Rehabilitatioll Researcll alld Development 34:448-58. McGill, S.M. 1998. Low back exercises: evidence for improving exercise regimens. Physical TIIerapy 78:7546S. McGill, S.M., and Norman, R.W. 1986. Partitioning of the L4-LS dynamic moment into disc, ligamentous, and muscular components during lifting. Spine 11:666-78. McGill, S.M.; Norman, R.W.; and Sharratt, M.T 1990. The effect of an abdominal belt on trunk muscles activity and intra-abdominal pressure during squat lifts. Ergonomics 33:147-60. McGill, S.M.; Juker, D.; and Kropf. P. 1996. Quantitative intramuscular myoelectric activity of quadratus lumborum during a wide variety of tasks. Clinical Biomechanics 11:170-72. McKenzie, R.A. 1981. The lumbar spille. Mechanical diagnosis and therapy. Lower Hutt, New Zealand: Spinal Publications. McKenzie, R.A. 1990. TIle ceroical and tlJOraricspine. Mechanical diagnosis and therapy. Lower Hutt, New Zealand: Spinal Publications. Miller, j.A.A.; Haderspeck, K.A.; and Schultz, A.B. 1983. Posterior element loads in lumbar motion segments. Spine 8:331-37. Miller, M.L, and Medeiros, j.M. 1987. Recruitment of internal oblique and transversus abdominis muscles during the eccentric phase of the curl-up exercise. Physical Therapy 67:1213-17. Moore, M.A., and Kukulka, CG. 1991. Depression of Hoffman reflexes following voluntary contraction and implications for proprioceptive neuromuscular facilitation therapy. Physical Therapy 71:321-33. Morgan, D.L., and Lynn, R. 1994. Decline running produces more sarcomeres in rat vastus intermedius muscle fibers than does incline running. Journal of Applied Physiology 77:1439-44. Morris, j.M.; Lucas, 0.8.; and Bresler, B. 1961. Role of the trunk in stability of the spine. Journal of Balle alld Joint Surgery (Am) 43A:327-51. Mottram, S.L. 1997. Dynamic stability of the scapula. Mallual Therapy 2:123-31. Murray, M.P.; Seireg, A.; and Sepic, S.B. 1975. Normal postural stability and steadiness: quantitative assessment. Journal of Balle alld Joint Surgery S7 A:S10-16. Nachemson, A.L. 1992. Newest knowledge of low back pain. Clinical Orthopaedics 279:8. Nachemson, A., and Evans, j. 1968. Some mechanical properties of the third lumbar laminar ligament (ligamentum flavum). Journal of Biomechanics 1:211. Ng, G., and Richardson, CA. 1990. The effects of training triceps surae using progressive speed loading. Physiotherapy Practice 6:77-84.
260
.
Bibliography
Ng, G., and extension Norkin, CC, delphia: Norris, CM. Norris, CM.
Richardson, C 1994. EMG study of erector spinae and multifidus in two isometric back exercises. Australian Journal of Physiotherapy 40:115-21. and Levangie, P.K. 1992. Joint structure and function. A comprehensive analysis. 2d ed. PhilaDavis. 1993. Abdominal muscle training in sport. British Journal of Sports Medicine 27:19-27. 1994b. Abdominal training. Dangers and exercise modifications. Physiotherapy in Sport
14:10-14. Norris, CM. 1994c. Taping: components, applications and mechanisms. Sports Exercise and Injury 1:14-17. Norris, CM. 1995a. Spinal stabilisation 2. Limiting factors to end-range motion in the lumbar spine. Physiotherapy 81 :4-12. Norris, CM. 1995b. Weight training. Principles and practice. London: A&C Black. Norris, CM. 1997. Abdominal training. London: A&C Black. Norris, CM. 1998. Sports Injuries. Diagnosis and management. 2d ed. Oxford: Butterworth Heinemann. Norris, CM. 1999. Functional load abdominal training: part 1. Journal of Bodywork and Movement Therapies 3(3):150-58. Norris, CM., and Berry, S. 1998. Occurrence of common lumbar posture types in the student sporting population: an initial evaluation. Sports, Exercise, and Injury 4:15-18. O'Sullivan, P.B.; Twomey, L.T.; and Allison, G.T. 1997. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine 22:2959-67. O'Sullivan, P.B.; Twomey, L.; and Allison, G.T. 1998. Altered abdominal muscle recruitment in patients with chronic back pain following a specific exercise intervention. Journal of Orthopedic and Sports Physical Therapy 27:114-24. Oliver, J., and Middleditch, A. 1991. Functional anatomy of the spine. Oxford: Butterworth Heinemann. Palastanga, N.; Field, D.; and Soames, R 1994. Anatomy and human movement. 2d ed. Oxford: Butterworth Heinemann. Panjabi, M.M. 1992. The stabilizing system of the spine. Part 1. Function, dysfunction, adaptation, and enhancement. Journal of Spinal Disorders 5:383-89. Panjabi, M.M.; Abumi, K.; Duranceau, J.; and Oxland, T. 1989. Spinal stability and intersegmental muscle forces. A biomechanical model. Spine 14:194-200. Panjabi, M.M.; Hult, J.E.; and White, A.A. 1987. Biomechanics studies in cadaveric spines. In The lumbar spine and back pain, ed. M.l.V.Jayson. Edinburgh: Churchill Livingstone. Panjabi, M.M., and White, A.A. 1990. Physical properties and functional biomechanics of the spine. In Clinical biomechanics of the spine, ed. A.A. White and M.M. Panjabi. Philadelphia: Lippincott. Paris, S.V. 1985. Physical signs of instability. Spine 10:277-79. Parkkola, R; Rytokoski, U.; and Kormano, M. 1993. Magnetic resonance imaging of the discs and trunk muscles in patients with chronic low back pain and healthy control subjects. Spine 18:830-36. Pamianpour, M.; Nordin, M.; Kahanovitz, N.; and Frankel, V. 1988. The triaxial coupling of torque generation of trunk muscles during isometric exertions and the effect of fatiguing isoinertial movements on the motor output and movement patterns. Spine 13:982-92. Pearcy, p.; Portek, I.; and Shepherd, J. 1984. Three dimensional X ray analysis of normal movement in the lumbar spine. Spine 9:294-97. Perey, 0.1957. Fracture of the vertebral end plate in the lumbar spine. Acta Orthap Scand (Suppl) 25:1-101. Pope, M.H., and Panjabi, M.M. 1985. Biomechanical definitions of instability. Spine 10:255-56. Ricci, B.; Marchetti, M.; and Figura, F. 1981. Biomechanics of sit up exercises. Medicine and Science in Sports and Exercise 13:54-59. Richardson, CA. 1992. Muscle imbalance: principles of treatment and assessment. Proceedings of the New Zealand Society of Physiotherapists Challenges Conference. Christchurch, New Zealand. Richardson, CA., and Bullock, M.1. 1986. Changes in muscle activity during fast, alternating flexionextension movements of the knee. Scandinavian Journal of Rehabilitation Medicine 18:51-58. Richardson, CA., and Hodges, P. 1996. New advances in exercise to rehabilitate spinal stabilisation. Course notes. University of Edinburgh. Richardson, C; Jull, G.; Toppenburg, R; and Comerford, M. 1992. Techniques for active lumbar stabilisation for spinal protection: a pilot study. Australian Journal of Physiotherapy 38:105-12. Richardson, CA., and Sims, K. 1991. An inner range holding contraction: an objective measure of stabilising function of an antigravity muscle. Proceedings of the World Confederation for Physical Therapy, 11th International Congress. London. Richardson, C; Toppenberg, R.; and Jull, G. 1990. An initial evaluation of eight abdominal exercises for their ability to provide stabilisation for the lumbar spine. Australian Journal of Physiotherapy 36:6-11. Risch, 5.V.; Norvell, N.K.; Pollock, M.L.; Risch, E.D.; Langer, H.; Fulton, M.; Graves, J.E.; and Leggett, S.H. 1993. Lumbar strengthening in chronic low back pain patients. Physical and psychological
benefits. Spine 18:232-38.
Bibliography.
261
Roaf, R. 1960. A study of the mechanics of spinal injuries. Journal of Bone and Joint Surgery 42B:810-23. Rock~ff, S.F.i Sweet, E.; and Bleustein, J. 1969. The relative contribution of trabecular and cortical bone to the strength of human lumbar vertebrae. Calcified Tissue Research 3:163-75. SaaI. J.A. 1988. Rehabilitation of football players with lumbar spine injury. Physician and Sports medicine 16:61-67. Saal, J.A. 1995. The pathophysiology of painful lumbar disorder. Spine 20:180-83. Saal, J.A., and Saal, JS. 1989. Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. Spine 14:431-37. Sahrmann, S.A. 1987. Posture and muscle imbalance: faulty lumbar-pelvic alignment and associated musculoskeletal pain syndromes. In Postgraduate advances in physical therapy. Berryvill, VA: Forum Medicum. Sahrmann, S.A. 1990. Diagnosis and treatment of movement related pain syndromes associated with muscle and movement imbalances. Course notes. Washington University. Silvermetz, M.A. 1990. Pathokinesiology of supine double leg lifts as an abdominal strengthener and suggested alternative exercises. Athletic Trianing 25:17-22. Skall, F.H.; Manniche, C; and Nielsen, CJ. 1994. Intensive back exercises 5 weeks after surgery of lumbar disk prolapse. A prospective randomized multicenter trial with a historical control group. Ugeskr Laeger 156:643-46. Smith, R.L., and Brunolli, J. 1990. Shoulder kinesthesia after anterior glenohumeral joint dislocation. Physical Therapy 69: I 06-12. Spitzer, W.O.; Le Blanc, F.E.; and Dupuis, M. 1987. Scientific approach to the assessment and management of activity related spinal disorders: a monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine 12 (Suppl 7). Sturesson, 8.; Selvik, G.; and Uden, A. 1989. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine 14:162-65. Sugano, H., and Takeya, T. 1970. Measurement of body movement and its clinical application. Japanese Journal of Physiology 20:296-308. Sullivan, MS. 1997. Lifting and back pain. In Physical therapy of the low back,ed. L.T. Twomey and J.R Taylor. Edinburgh: Churchill Livingstone. Sullivan, P.E.; Markos, P.O.; and Minor, M.A.D. 1982. An integrated approach to therapeutic exercise. Reston, VA: Reston Publishing. Swanepoel, M.W.; Adams, L.M.; and Smeathers, J.E. 1995. Human lumbar apophyseal joint damage and intervertebral disc degeneration. Annals of the Rheumatic Diseases 54:182-88. Taylor, D.C; Dalton, j.; 5oaber, A.V.; and Garrett, W.E. 1990. The viscoelastic properties of muscle-tendon units. American Journal of Sports Medicine 18:300-09. Taylor, J.R, and Twomey, L.T. 1986. Age changes in lumbar zygapophyseal joints. Spine 11:739-45. Templeton, G.H.; Padalino, M.; and Manton, J. 1984. Influence of suspension hypokinesia on rat soleus muscle. Journal of Applied Physiology 56:278-86. Thapa, P.B.; Gideon, P.; Brockman, K.G.; Fought, RL.; measures
of balance
as fall predictors
in ambulatory
and
Ray, W.A.
nursing
home
1996. Clinical residents.
and Journal
biomechanical of Gerontology
51:239-46. Tkaczuk, H. 1968. Tensile properties of human lumbar longitudinal ligaments. Acta Orthop Scand 115 (Suppl). Toppenburg, R.M., and Bullock, M.l. 1986. The interrelation of spinal curves, pelvic tilt and muscle lengths in the adolescent female. Australian Journal of Physiotherapy 32:6-12. Travell, J.G., and Simmons, D.G. 1983. Myofascial pain and dysfunction. Baltimore: Williams & Wilkins. Tropp, H.; Alaranta, H.; and Renstrom, P.A.F.H. 1993. Proprioception and coordination training in injury prevention. In Sports injuries: basicprinciples of prevention and care. IOC Medical Commission publication, ed. P.A.F.H. Renstrom. London: Blackwell Scientific. Twomey, L.T., and Taylor, 1.R. 1987. Lumbar posture, movement and mechanics. In Physical therapy of the low back, ed. LT. Twomey. New York: Churchill Livingstone. Twomey, L.T., and Taylor, 1.R. 1994. Factors influencing ranges of movement in the spine. In Physical therapy of the low back. 2d ed., ed. L.T.Twomey and J.R Taylor. Edinburgh: Churchill Livingstone. Twomey, L.T.; Taylor, J.R.; and Oliver, M. 1988. Sustained flexion loading, rapid extension loading of the lumbar spine and the physical therapy of related injuries. Physiotherapy Practice 4:129-38. Tye, J., and Brown, V. 1990. Back pain-the ignored epidemic. London: British Safety Council. Tyldesley, B., and Grieve, 1.1. 1989. Muscles, nerves and movement: kinesiology in daily living. Oxford: Blackwell Scientific. Tyrrell, A.R; Reilly, T.; and Troup, JD.G. 1985. Circadian variation in stature and the effects of spinal loading. Spine 10:161-64. Valencia, P.P.,and Munro, R.R. 1985. An electromyographic study of the lumbar multifidus in man. Electromyography and Clinical Neurophysiology 25:205-21.
262
. Bibliography
Vernon-Roberts, B. 1987. Pathology of intervertebral discs and apophyseal joints. In Tile lumbar spine and back pain. ed. M.I. V. Jayson. Edinburgh: Churchill Livingstone. Vernon-Roberts, B. 1992. Age related and degenerative pathology of intervertebral discs and apophyseal joints. In The lumbar spine and back pain, ed. M.I.V. Jayson. Edinburgh: Churchill Livingstone. Videman, T.; Nurminen, M.; and Troup, j.D.G. 1990. Lumbar spine pathology in cadaveric material in relation to history of back pain, occupation, and physical loading. Spine 15:728-40. Vlaeyen, J.W.S.; Kole-Snijders, AM.J.; Boeren, RG.B.; and van Eek, H. 1995. Fear of movement/reinjury in chronic low back Vleeming, A; Mooney,
and its relation to behavioural performance. Pain 62:363-72. v.; Snijders, CJ.; Dorman, T.A; and Stoeckart, R. 1997. Movement pain
low back pain. New York: Churchill Livingstone. Vleeming. A; Pool-Goudzwaanl, A.L.; and Stoeckart, fascia: Vleeming.
its function in load A; Pool-Goudzwaanl,
transfer from spine AL.; Stoeckart,
rior layer of the thoracolumbar Vleeming. A; Stoeckart, R; and
to its dynamic Vleeming.
fascia: Snijders,
role in stabilizing
A.; Stoeckart,
R 1995a.
its function in load transfer C 1989. The sacrotuberous
A.CW.;
and
Snijders,
tion in the sacroiliac joint. Spine 15:130-32. Waddell, G. 1987. A new clinical model for the treatment Waddell, G.; Feder, G.; and Lewis, M. 1997. Systematic
acute low back pain. British ,ournal Walker,
M.L.;
Rothstein,
J.M.; Finucane,
dosis, pelvic tilt, and abdominal Walters,
C,
and
Partridge,
M. 1957.
Watson,
D.H.
flexor
1994.
Cervical
headache:
performance.
muscle
CJ.
from spine ligament:
Biomechanics 1990. Relation
and
of the thoracolumbar CJ.
1995. The poste-
to legs. Spine 20:753-58. a conceptual approach
4:201-03. between
form
and
func-
of low-back pain. Spine 12:632-44. reviews oibed rest and advice to stay active
of General Practice S.D.; and Lamb,
47:647-52. RL. 1987. Relationships between Physical Therapy 67:512-16.
muscle performance.
during exercise. American ,ournal Watkins, J. 1999. Structure and function
layer
to legs. Spine 20:753-58. R; Wingerden, J.P.; and Snijders,
the sacroiliac joint. Clinical
R; Volkers,
The posterior
stability
Electromyographic study of the differential of Physical Medicine 36:259-68. system.
an investigation
of natural
head
lumbar
abdominal
Champaign,
of the musculoskeletal
and
Kinetics.
upper
cervical
In Grieve's modern manual therapy. 2d ed., ed. J.D. Boyline
Palastanga. Edinburgh: Churchill Livingstone. Watson, J. 1983. An introduction for mechanics of human movement. Weber, H. 1983. Lumbar disc herniation: a controlled prospective
lor-
muscles
1L: Human
posture
for
and
N.
Lancaster, UK: MTP Press. study with ten years of observation.
Spine 8:131-38. Webright,
w.G.;
Randolph,
B.J.; and
Perrin,
D.H.
1997. Comparison
of nonballistic
active
knee
exten-
sion in neural slump position and static techniques on hamstring flexibility. Sparts Physical Therapy 26:7-13. Weider, J. 1989. Ultimate badybuilding. Chicago: Contemporary Books.
Journal of Orthopedic
White,
to management
S.G., and Sahrmann,
culoskeletal
Livingstone. Wilke, H.J.; Wolf, S.; Claes, with Willard,
S.A. 1994. A movement
pain. In Physical therapy of the cervical L.E.; Arand,
different muscle groups: F.H. 1997. The muscular,
system
balance
and thoracic
M.; and Weisend,
approach
and
of mus-
spine, ed. R Grant. New York: Churchill
A. 1995. Stability
increase
of the lumbar
spine
a biomechanical in vitro study. Spine 20:192-98. ligamentous and neural structure of the low back and its relation
to
back pain. In Movement stability and low back pain, ed. A. Vleeming. V. Mooney, T. Dorman, C Snijders, and R Stoeckart. Edinburgh: Churchill Livingstone. Williams, P.; Watt, P.; Bicik, V.; and Goldspink, G. 1986. Effect of stretch
combined
with electrical
tion on the type of sarcomeres produced at the ends of muscle Williams, P.E. 1990. Use of intennittent stretch in the prevention
fibers. Experimental of serial sarcomere
muscle. Annals of the Rheumatic Diseases 49:3]6-]7. Williams, P.E., and Goldspink, G. 1978. Changes in sarcomere
length
immobilised Yamamoto,
muscle.,ournal
I.; Panjabi,
M.M.;
of Anatomy 127:459-68. Oxland, T.R.; and Crisco,
the lumbosacral junction. Spine 15:1138-41. Yang, K.H., and King, A.1. 1984. Mechanism pain.
Spine
Yong-Hing, Zetterberg.
of facet load
and physiological
The role of the iliolumbar
transmission
as a hypothesis
properties
in
ligament
in
for low
back
9:557-65.
K.; Reilly, J.; and Kirkaldy-Willis, C; Andersson,
G.B.J.;
44:13-20.
W.H. 1976. The ligamentum
Schultz, A.B. 1987. The activity Spine 12:1035-40.
ing heavy physical loading. Zusman, M. 1998. Structure-oriented iotherapy
J.J. ]990.
stimula-
Neurology 93:500-09. loss in immobilised
and
beliefs and disability
flavum. Spine 1:226-34.
of individual
due to back pain. Australian
trunk
muscles ,ournal
dur-
of Phys-
Credits From J.e. Griffin, 1998, Client-centered exercise prescription (Champaign, ics): Figure 5.1 (page 95) reprinted, by permission, from p. 176.
IL: Human Kinet-
From J.A. Hides, e.A. Richardson, and G.A. Jull, 1996, "Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain," Spine 21 (23): Figure 3.5 (page 52) reprinted, by permission, from pp. 2763-2769. From National Strength and Conditioning Association, 1994, Essentials of strength conditioning and training (Champaign, IL:Human Kinetics): Exercise figure, a-c, "Hang Clean" (Page 220) adapted, by permission, from p. 394; Exercise figure, a.c, "Power Clean" (page 221) adapted, by permission, from p. 392; Exercise figure, a-c, "Dead Lift" (page 222) adapted, by permission, from p. 380. From e. Norris, 1995, "Spinal stabilisation," Physiotherapy Journal 81 (3): Exercise figure, a. c, "Assessing Muscle Balance in the Gluteus Maximus" (page 104) reprinted, by permission, from p. 26. From e. Norris, 1998, Diagnosis and management, 2d ed. (Oxford: 8utterworth Heinemann): Figure 2.12, a and b (page30); Figure 2.14, a and b (page 34); Figure 2.16 (page 3B) reprinted from p. 18; Exercise figure, a-d, "Knee Raising in Standing" (page 71); Exe,.. cise figure, a.d, "Assessing Lumba,..Pelvic Rhythm in Prone Kneeling" (page 72); Exercise figure, a and b, ''The Hip Hinge Movement in Standing" (page 72); Exercise figure, a and b, "Recognizing False Hip Abduction" (Page 73) reprinted from p. 167; Figure Figure 4.4 (page 91) reprinted from p_ 155; Chapter 5 exercise descriptions; 5.2 (page 95) and Figure 5.3 a (page 95) reprinted from p. 145; Figure 5.7 (page 101) and Figure 5.8 (page 101); Exercise figure, "Assessing Muscle Balance in the IliopMuscle Balance in the Glu. soas" (page 103); Exercise figure, top right, "Assessing teus Maximus" (page 104); Exercise figure, "Assessing Muscle Balance in the Glu. teus Medius" (page 105); Exercise figure, "Half Lunge" (page 114), Exercise figure, "Hip Hitch" (page 115), Exercise figure, "Active Knee Extension, Holding Thigh" (Page 116), Exercise figure, "Active Knee Extension, Pushing Against Thigh" (Page 116) and Exercise figure, ''Tripod Stretch" (page 117) reprinted from p. 175; Figure 6.1, a and b (page 121) reprinted from p. 176; Figure 6.2 (page 122) and Figure 6.3 (page 125) reprinted from p. 177; Exercise figure, "Leg Lowering" (page 128); Exe,.. cise figure, "Bench Lying Pelvic Raise" (page 129) and Exercise figure, a, "Wail Bar Hanging Leg Raise" (page 130) reprinted from p. 177; Exercise figure, "Plyometrlc Flexion and Extension Using a Punching Bag" (page 226) and Exercise figure, "Leg Raise Throw (Page 227) reprinted from p. 129. All reprinted by permission of Butterworth Heinemann Publishers, a division of Reed Educational & Professional Publishing Ltd. From CM. Norris, 1997. Abdominal Training (london: A & C Black): Exercise figure, "Correction of Swayback Posture" (page 151) and Exercise figure, a and b, "Passive Back Extension in Lying Position" (page 156) adapted, by permission, from p. 38. Illustrations by Jean Ashley. From P.B. O'Sullivan, l.T. Twomey, and G.T. Allison, 1997, "Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiological diagnosis of spondylolysis or spondylolisthesis," Spine 22 (24): Figure 1.1 (page 7) adapted, by permission, from pp.2959-2967. From e.A. Richardson and M.I. Bullock, 1986, "Changes in muscle activity during fast, alternating flexion-extension movements of the knee," Scandinavian Journal of Rehabilitation Medicine 18: Figure 5.4 (page98) and Figure 5.5 (page98), reprinted, by permission, from pp. 51-58. From J. Watkins, 1999, Structure and function of the musculoskeletal system (Champaign, IL: Human Kinetics): Figure 2.1 (page 15) reprinted from p. 61; Figure 2.2 (page 15) reprinted from p. 63; Figure 2.5 (page 19) reprinted from p. 145; Figure 2.6 (page 19) reprinted from p. 150. 263
Index Figures and tables are indicated by the italicized assessments have italicized page numbers.
letters
A abdominal hollowing: about 60; assessing 236; basic process 81; common errors 88-89; correct and incorrect positions 88; fourpoint kneeling 83; general considerations 81-82; importance 168; lying 85-86; with pelvic floor contractions 84; prone test using pressure biofeedback 105-106; standing 84; starting positions 82-86; teaching clients 81-89; teaching tips 86; two-point kneeling and sitting 85; with webbing belt 87f; in weight training 203 abdominal machine 212 abdominal muscles: activation in chronic low back pain 6Of; coordination during spinal movement 60-62; deep abdominals anatomy 57-58; deep dissection illustration 58f; "doming" of abdominal wall 121; functions 58-60; intermediate dissection illustration 57£; in resisted actions 59; superficial abdominals anatomy 55-57 abdominal slide 188 abdominal training: current practice 120-124; modifications of traditional exercises 124-130 abdominal wall "doming" 121 ab roller exercises 130-132 active knee extension: holding thigh 116; pushing against thigh 116-117 active lumbar stability 12 active positioning reproduction 80-81 active stretching 111!, 112, 113 acute pain case history 242-244 Adams, M. 31 Adam's position 138 adipose tissue pad 22-23 advanced training qualifications 167-168 aerobic exercise 99 aging: chronic muscle tightness 237; compression of vertebral bodies 25; disc changes 28; facet joint cartilage 23; and ligaments 20; lumbar disc changes 28f; and posture 136; proteoglycan content 22; tissue overstretch 31 Allan, D.B. 6 American Academy of Orthopaedic Surgeons
134 anaerobic exercise 99 Andersson, E. 55 annulus fibrosis 20-21,21f anterior pelvic tilt 34f anterolateral muscles 7 aponeurosis 45 approximate (verb), defined arch mechanics 39f
264
45
t and f follCJWing the page number.
Exercises
and
arctan formula 142 arm fixation 123-124 arm lift in four-point kneeling 196-197 articulate, defined 17 articulating triad 14 assessments: heel slide maneuver using pressure biofeedback 106; hip hinge movement in standing 72-73; knee raising in standing 71; lumbar-pelvic rhythm in prone kneeling 72; muscle balance in gluteus maximus 104; muscle balance in gluteus medius 105; muscle balance in iliopsoas 103; Ober test 108-109; passive assessment of pelvic tilt 72; pelvic motion control in frontal plane 73; prone abdominal hoUowing test using pressure biofeedback 105-106; recognizing false hip abduction 73-74; straight-leg raise test 109-110; Thomas test 107-108; tripod test 110 assisted
pelvic
tilt: from
crook
lying
position
75-
76; while sitting 75; while standing 74 atrophy 97 axial compression: of facet joints 28-29; of intervertebral discs 26-28; verterbal bodies 25-26
B back back back back back back
care, in home 249f extension (frame) 209 extension (machine) 208 flattening 149-150 muscles 52f pain: back stability exercises 234t; diagnostic triage 233; nonorganic causes 4-5; recurrence 3; scope of problem 3--4 back pain management: about 5-6; lumbar stabilization model 7-12; new model 6-7; traditional model 6 back stability assessment 236 back stability exercises 234t Baechle, T.R. 214 balance boards 168-169,183-186 ballistic stretching 1111, 112, 113 barbell lunge 218-219 Barrack, R.L. 199-200 basic crunch, ab roller 131 basic superman 190 bed rest 5, 234 behavioral factors 5 bench curl 127 bench lying pelvic raise 129 bending: erector spinae 37; sacroiliac joint 25; torsional stresses 27 bent knee sit-up 126 Biedermann, H.j. 51 blood flow, out of vertebral body 26
Index.
blood pressure, and Valsalva maneuver 63 body, listening to 205 body sway, and postural stability 135-136 Bogduk, M. 65 bones, vertebral column anatomy 14-15 brain stem activities 80 breathing, in weight training 203 bridge: from crook lying 172; with gym ball 191; with leg lift 173,192; with leg lift and extension 192; with pelvic tilt 191; with therapist pressure 192 Bullock, M.l. 97,99 Bullock-Saxton, J. 141
C cable crossover 208 capsular ligaments 16t, 18 cartilage end plates 20,22 case histories: acute pain 242-244; obese client 239-240; poor stability 240-242; unwillingness to exercise 244-245 cauda equina syndrome 232
caudal, defined 17 center of gravity, in postural assessment 136 chronic low back pain: and abdominal hollowing 60-61; abdominal muscle activation 6Of; motor control deficit in transversus abdominis 62 chronic muscle lengthening 100-102 clients (see also teaching clients): advanced training qualifications 167-168; postural re-education 144; preliminary assessment 231-234; training progression 168169,206,214; working with 71 closed loop system 198-199 clothing, for weight training 205 common beliefs 4 compressed ligament 12 concentric-eccentric coupling 224 conditioning: and traditional sit-up 121-122; and traditional straight-leg raise 123 connective tissue rim 22 contractile tissues 11 contract-relax-agonist-contract stretching 111t, 112, 113 contract-relax stretching 11It, 112, 113 contralateral, defined 45 contralateral fibers 17 controlled forward bending 77 correction of swayback posture 151-152 costs, of treatment 3-4 countermovement 224 countemutation, of sacroiliac joint 24t, 25 coupled movements 33 CRAC stretching lilt, 112, 113 craniovertebral angle 142, 142f creep: of discs 26-27; of lumbar tissues 31-32 Cresswell, A.G. 62 critical point 37.38 crook lying position exercises 169-173 CR stretching lilt, 112, 113
o dancers: and lordotic posture tive training 200
146; propriocep-
265
dead lift 222 deep abdominal muscles 57-58: inner-range holding tests 105-106 deep (intersegmental) muscles 50-52 deformation of disc 26-27 degenerative discs 28 Deyo, R.H. 5 diagnostic triage 232-234 disability; labels of 4-5; permanent 3 disc, defined 14 discal compression 26-28, 27f. 29f disc surgery 6 distraction force 17 door frame stretch 161 double crunch, ab roller 132 double-handed lift 251f double-leg raise 197 dumbbell row 215-216 dynamic posture 135
E elastic energy 224 electrical silence, of muscles 37-38 Enoka, R.M. 223-224 equipment, for weight training 205 erector spinae 37, 40 exercise: with axial loading 27; compression of vertebral bodies 26; controlled 6; disc compression and height losses 27f; lifting habit education 36; and sacroiliac joint stability 49; from sitting posture 31; and spinal stability 11-12; starting positions 31,82-86,169; training specificity 99 exercises: abdominal hollowing: four-point kneeling 83; abdominal hollowing: lying 85-86; abdominal hollowing: standing 84; abdominal hollowing: two-point kneeling and sitting 85; abdominal machine 212; abdominal slide 188; active knee extension, holding thigh 116; active
knee
extension,
pushing against
thigh 116-117; arm lift in four-point kneeling 196-197; assisted pelvic tilt from crook lying position 75-76; assisted pelvic tilt while sitting 75; assisted pelvic tilt while standing 74; back extension (frame) 209; back extension (machine) 208; back flattening 149-150; barbell lunge 218-219; basic crunch, ab roller 131; basic superman 190; bench curl 127; bench lying pelvic raise 129; bent knee sit-up 126; bridge from crook lying 172; bridge with gym ball 191; bridge with leg lift 173, 192; bridge with leg lift and extension 192; bridge with pelvic tilt 191; bridge with therapist pressure 192; cable crossover 208; controlled forward bending 77; correction of swayback posture 151-152; dead lift 222; door frame stretch 161; double crunch, ab roller 132; double-leg raise 197; dumbbell row 215-216; four-point body sway 173; four-point kneeling arm and leg lift 175; four-point kneeling leg lift 174-175; four-point kneeling stretch 118;
266 . Index
exercises (continued): four-point leg flexion/ extension 174; lour-point pelvic shilt 174; lree squat 196; gluteus maximus inner-range exercise 147-149; good morning 216; hall lunge 114; hall lunge (without chair) 149; hall-sitting arm and leg movements 188-189; hang clean 220; heel bridge 193; heel bridge with leg raise, ball rolling 194; heel slide 128; heel slide basic movement 170; hip hinge action in high kneeling 76; hip hinge with table support 77; hip hitch 115; lateral puUdown 206-207; leg lowering 128,170; leg raise throw 227; low pulley spinal rotation 210-211; lying barbell row 215; lying trunk curl over baU 189; lying trunk curl with leg lilt 190; medicine ball trunk curl 226-227; modified trunk curl 146-147; multiludus contraction 89-90; muscle reaction speed using mobile platform 201; neutral position maintenance 185; Dber test stretch 115-116; passive back extension in lying position 156-157; pelvic rock on rocker board 184; pelvic rock on wobble board 185; pelvic shilt with leg lilt 180; pelvic shilt with unloading 179; pelvic tilt re-education, sitting 157; plyometric lIexion and extension using punching bag 226; plyometric side bend using punching bag 225; power clean 221; prone bent-leg lilt 172; prone laU 194; prone laU with arm lilt 195; prone lall with single-leg lilt 195; prone lying gluteal brace 171; pulley crunch 212; rapid displacement in sitting 200; reproduction of active positioning 80-81; reproduction of passive positioning 80; reverse bridge 193; reverse bridge and roll 193; reverse crunch, ab roller 131; rhythmic stabilization 01 multifudus and lateral abdomina Is in side lying position 90-91; rotary torso machine 211; scapula repositioning 160161; seated rowing 209; side crunch, ab roller 132; side lying body lilt 178; side lying hip lilt 178; side lying knee lilt 176; side lying leg abduction 177; side lying leg rotation 176-177; side lying spine lengthening 177; simple pelvic tilt, progressing to balance boards 184; single arm pulley row 210; single-bent leg raises 171; single-leg heel bridge 194; sitting, hip lIexor shortening 154-155; sitting bilateral hip adductor stretch 152; sitting hamstring stretch 182; sitting hip hinge 185-186; sitting knee and arm raise 183; sitting knee raise 183, 188; sitting lateral tilt using gym baU 78; sitting pelvic tilt using gym ball 77-78; sitting sternal lilt 182-183; sitting wide splits 152-153; spinal lengthening 153-154; squat 216-218; standing hip abduction 180; standing hip hinge 181; standing sternal lilt 179; sternalliEt exercise 162;
superman, basic 190; superman with arms 190-191; Thomas test stretch 114; thoracic joint mobilization 159-160; throw-catch activities on mobile surface 201; tripod stretch 117; trunk curl 126127; trunk lIexion with high pulley 212; trunk side lIexor stretch 117-118; twist and throw with medicine ball 226; wall bar hanging leg raise 129-130; wall sit 195-196; weight bag passive stretch 161162 explosive power 219-222 extension 17,32-33 external oblique muscle 56-57,57f
F lacet joint capsule 19f lacet joints: about 14; axial compression 28-29; compression results 29f; 01 vertebral column 22-23 lalse hip abduction, recognizing 73-74 lascia 17 lascicle, delined 45 fast-twitch muscles 93 !ibro-adipose meniscoid 22-23 lIatback 145[ 156-157 lIexion 17,30-32 flexion relaxation response 37-38 flexor synergy during gait 122 lIuid loss 27 foot fixation 122 force closure 48 forensic back pain factors 5 form closure 48 lour-point body sway 173 lour-point kneeling 82: arm and leg lilt 175; exercises 173-175; leg lilt 174-175; stretch 118 four-point leg flexion/extension 174 four-point pelvic shift 174 lree squat 196 free weight concerns 213-214 exercises: about 213;basic 214-219; for explosive power 219-222
free weight
Fu, EH. 79,200 lunctional taping
144-145
G gender, and range of motion 30 gluteus maximus inner-range exercise 147-149 gluteus maximus muscle balance assessment 104 gluteus medius muscle balance assessment 105 good morning 216 gym ball exercises 186-197 gymnasts: and lordotic posture 146; proprioceptive training 200; and sacroiliac joint pain 49
H hall lunge 114 hall lunge (without chair) 149 half-sitting arm and leg movements hamstrings, stretching 113
hang clean 220
188-189
Index. heel bridge 193 heel bridge with leg raise, ball rolling 194 heel slide 128: basic movement 170; using pressure biofeedback 106 height losses 26,27, 27f Hemborg. B. 64-65 herniated lumbar disc 6-7 Hides, J.A. 51 hip extensor muscles 36, 122 hip flexor muscles 123 hip hinge 36; in high kneeling 76; in standing 72-73; with table support 77 hip hitch 115 hip joint, motion relationships with pelvis and lumbar spine 351 hip muscles, inner-range holding tests 103-105 Hodges, P. 61 holding 94 holistic treatment 235-236 hollow back 145. (set!also lordotic posture home back care 249f hoop pressure 45 hydraulic amplifier effect 47-48 hyperflexibility 95-96 hypoflexibility 95-96 hysteresis 20
I iatrogenic back pain factors 4-5 iliacus 54f 561 iliopsoas muscle: about 54-55; illustrated 54J; muscle balance assessment 103 immobilization: effects on muscles 101f; muscle adaptation 96-99 impaction 33 inclinometer 139,141 inert tissues 11 inguinal ligament 57f injury, muscle adaptation 96-99 injury prevention 247-253 inner-range holding ability 103-106 innominate bone 17 internal oblique muscle 57,57f interspinous-supraspinous-thoracolumbar complex 18f intervertebral discs, axial compression 26-28 intra-abdominal pressure mechanism 62-65,631 intradiscal pressure 301 intrathoracic pressure 62-63 intra truncal pressure 62 investing fascia 17 ipsilateral, defined 45 ischemic, defined 17
J Jacob, H.A.e. 25 Janda, V. 145-146 joint degeneration 79 joint loading, minimizing 134 joints, vertebral column anatomy joint stability 8
K Kent, M. 223 keyhole 138
14-15
267
kinesthesis 136, 198 Kissling. R.O. 25 knee raising in standing 71 Koh, T.J. 102 Kukulka, e.G. 111 kyphotic back 45, 145f 157-162
L lamina, lamina lateral lateral lateral lateral
defined 45 of vertebral arch 17 flexion 17,33 malleolus 135 pulldown 206-207 raphe 45 laxity 95-96 lean clients, and abdominal hollowing 83 leg lowering 128,170 leg raise throw 227 Lephart, S.M. 79, 200 Lifting: appropriate stance and grip 251-253; arch model of spine 38-40; flexion relaxation response 37-38; large objects 37, 252J; mechanics 35-40,36J; methods 40-41; minimizing stress 250-253; planning 248, 250; principles 248-253; safe zone 250-251; as set of torques 3537; with unstable spine 59; and Valsalva maneuver 64 Ligaments: elasticity 20; self locking 48; of spinal segment 16f 161; and spinal stability 11; of vertebral column 15-16, 18-20 limb strength 202 limits,
in weight
training
205
linea alba 57f line of gravity: gravitational torques maintaining 135fi in postural
137, 139t; assessment
136-137 long dorsal sacroiliac ligament 48 Lord, S.R. 136 Lordosis: defined 17; depth measurement 141142,141f lordotic index 142 lordotic posture 145-150, 145f low back pain: anticipatory nature of stability 61; incorrect sitting positions 181; and multifudus muscle 51-52; and superficial muscles 53 tower back muscles, inner-range holding tests
103-105 low-level contractions 94 low pulley spinal rotation 210-211 lumbar curvature 40,41f lumbar erector spinae 52 lumbar hypermobility 8 lumbar iliocostalis muscle 53 lumbar instability 8-10 lumbar longissumus muscle 52-53 lumbar neutral position 10, 78-79 lumbar-pelvic dissociation 71-74 lumbar-pelvic rhythm: about 34-35; assessing in prone kneeling 72; in closed kinetic chain 34f; correct function 70; in open chain 34J; regaining correct 74-78
268
.
Index
lumbar region 191 lumbar spine: biomechanics 14; flexion and extension 30-33; lateral view 53f; lumbar-pelvic rhythm 34-35; motion relationships with pelvis and hip joint 351; rotation and lateral flexion 33; stabilization mechanisms 43; stable movement and position 9-10; in standin~ extension, and flexion 321 lumbar stabilization model: about 7-8; spinal stability 11-12; stable movement and position 9-10 Luttgens, K. 136 lying, lost height restoration 26 lying abdominal hollowing 85-86 lying barbell row 215 lying trunk curl over ball 189 lying trunk curl with leg lift 190 Lynn, R. 102
M machine exercises 205-212 machismo, and lifting 250 McKenzie, R.A. 142,156 Main, Cj. 5 medicine balls 226-227 medicine ball trunk curl 226-227 men, range of motion 30 mobile surfaces 201 mobilizer muscles: about 92,94; affecting lower back 96/; characteristics 93/ modified trunk curl 146-147 momentum, and free weights 213 Moore, M.A. 111 Morgan, D.L. 102 motion sense 136 motor skiIlleaming stages 143/ motor skiU training 143-144 movement sense 198 multifudus contraction 89-90 multifudus muscle: contraction 89-91; exercise effects 51; exercises for contraction 8990; function 50-51; lateral view SOft medical treatment effects 51; targeting 7 multisensory cues 86 muscle activity: changes with speed increase 98f; patterns during rapid knee flexionextension 98f; in weight training 203 muscle balance assessment: in gluteus maximus 104; in gluteus medius 105; in iliopsoas 103 muscle imbalance: about 92; assessment 237; characteristics 94-96; and posture 95f muscle length: about 100; adaptation 101f; chronic muscle lengthening 100-102; shortened muscle assessment 106-110; stretched muscle assessment 103-106 muscle reaction speed using mobile platform
201 muscles:
of abdomen 57f; adaptation to injury, immobilization, and training 96-99; of back 52f; basic concepts 92-96; electrical silence 37-38; endurance vs. strength 206; immobilization effects 101f; lengthtension relationship 38f; in optimal
posture alignment 134; proprioceptive functions 94; re-ed uca tion 69; stretching principles 111-113; target stretching 113118; thoracolumbar fascia attachments 46f; transmission of force 18; types 93/; voluntary control 69; working large groups first 238 muscle stiffness regulation 198-199
N nerve root entrapment 6 nerve root pain 232,233 nervous system training 198-199 neural arch ligaments 15-16, 16t, 18 neural control centers 11 neural system, developing 12 neutral position: and abdominal hollowing 82; in crook lying position exercises 171; of lumbar spine 10,78-79; teaching clients 78-81; in weight training 203 neutral position maintenance 185 neutral zone 9-1O,9f Ng, G. 97 Norris, CM. 30,92, 232, 238 nucleus pulposus 20,21-22,211 nutation, of sacroiliac joint 24t, 25, 48
a Ober test 108-109, 151 Ober test stretch 115-116 obese clients 83,239-240 occiput 17 occupational considerations 32 overemphasis of single aspect 235 overhead lifting 59,59f overload principle 235 overstretch 100 overuse injury 204
p pain (see also back pain; chronic low back pain; low back pain): acute pain case history 242-244; anticipation of 5; assessing 231232; nerve root pain 232, 233; not exercising through 205; as reliable guide 234 palpation 86-87, 87j. 91f Panjabi, M.M. 9,10,51 parallel exercise progressions 236 passive back extension in lying position 156-157 passive positioning reproduction 80, 199-200 passive stability system 10 passive support, of lumbar region 12 pelvic crossed syndrome 145-146 pelvic inclinometer 139,141 pelvic inlet 17 pelvic motion control, assessing in frontal plane 73 pelvic rock on rocker board 184 pelvic rock on wobble board 185 pelvic shift with leg lift 180 pelvic shift with unloading 179 pelvic tilt: inclinometer assessment 139,141; passive assessment 72; repeated pelvic tilting exercises 183-186 pelvic tilt control: about 70; lumbar-pelvic dissociation 71-74; segmental control 70
Index.
pelvic tilt re-education, sitting 157 pelvis, motion relationships with hip joint and lumbar spine 351 Perey, O. 37 periosteum 17 permanent disability 3 physiology 238 plumb line, in postural assessment 137, 137f, 138139 plyometric exercises 225-227 plyometric flexion and extension using punching bag 226 plyometrics: about 202; for power and speed 222-225; preparation 225 plyometric side bend using punching bag 225 PNF stretching 111-113 poor conditioning: in traditional sit-up 121-122; in traditional straight-leg raise 123 poor stability, case history 240-242 posterior ligamentous system 43-44 postural muscles 92. (see also stabilizer muscles postural stability, and body sway 135-136 posture: anatomical landmarks 137-138; assessing 237; basic assessment 136-142; correction principles 143-145; dynamic posture 135; energy expenditure reduction 135; home-exercise programs 143-144; "low-tech" measurement 143; and muscle imbalance 95f; optimal alignment 134-135; re-education 144; standard reference 138J; standing posture assessment 140f; static posture
135 Posture Committee, American Academy of Orthopaedic Surgeons 134 posture grid 138-139 posture types: about 145; flatback 145f, 156-157; kyphotic back 45, 145f, 157-162; lordotic posture 145-150,1451; swayback 1451, 150-155 power: defined 223; in free-weight exercises 219-222; with plyometrics 222-227 power clean 221 preload effect 224 pressure biofeedback 105-106 primary mobilizer muscles 93t primary stabilizer muscles 93t principle of overload 235 principle of specificity 234-235 prolapse, defined 17 prone abdominal hollowing test using pressure biofeedback 105-106 prone bent-leg lift 172 prone fall 194: with arm lift 195; with single-leg lift 195 prone lying 83 prone lying gluteal brace 171 proprioception: basic concepts 79-80; components 79t; defined 79; kinesthesis 198; movement sense 198; regulation of muscle stiffness 198-199; theory 198-199; training benefits 199-200 proprioceptive neuromuscular facilitation 111113. (see also PNF stretching) proprioceptive training 197-201
269
proteoglycans 21-22,28 psoas 54f, 561 pulley crunch 212 punching bags 225-226 pyramid training 206, 238
Q quadratus
lumborum
muscle
54
R range of motion 30, 35 raphe, lateral 45 rapid displacement in sitting 200 reaction time 223 rectus abdominis muscle 55-56, 57f, 591 rectus sheath 57f, 58f, 591 reinjury prevention 247-253 relative flexibility 951 relative stiffness 951 repeated pelvic tilting exercises 183~186 repetitions, in weight training 206 reproduction of active positioning 80-81 reproduction of passive positioning 80, 199-200 response time 223 rest, as most common treatment 6 reverse bridge 193 reverse bridge and roll 193 reverse crunch, ab roller 131 rhythmic stabilization 90-91: of multifudus and lateral abdominals in side lying position
90-91 Richardson, C. 61 Richardson, C.A. 97, 99 Risch, S.V. 7 rocker boards 183, 184 rotary torso machine 211 rotation, of lumbar spine 33
round-shouldered posture 158 S joint: about 23-25; gymnasts' pain 49; illustrated 23J; movement 241; and thoracolumbar fascia coupling 48-49 sacrotuberous ligament 48 sacrum, in standing, extension, and flexion 32/ safety checklist, weight training 204 sagittal plane 17, 139/ sagittal rotation 17,31 S.A.I.D. (specific adaptation to imposed demand) 99-100 scapula repositioning 160-161 Schmid, H.j.A. 145-146 Schmorls node 17, 27 sciatica 6 seated rowing 209 segmental control 70, 94, 95 self-assessment in lifting 250 serial sarcomere number 100-102 serious spinal pathology 233 serratus anterior muscle 57! shortened muscle assessment 106-110 shoulder, postural changes around 159/ shoulder girdle alignment 158/ side crunch, ab roller 132 side lying body lift 178 side lying hip lift 178
sacroiliac
270
.
Index
side lying knee lift 176 side lying leg abduction 177 side lying leg rotation 176-177 side lying position exercises 175-178 side lying spine lengthening 177 simple pelvic tilt, progressing to balance boards 184 single arm pulley row 210 single aspect overemphasis 235 single-bent leg raises 171 single-handed lift 253f single-leg heel bridge 194 sitting, hip flexor shortening 154-155 sitting, intradiscal pressure 30-31 sitting bilateral hip adductor stretch 152 sitting hamstring stretch 182 sitting hip hinge 185-186 sitting knee and arm raise 183 sitting knee raise 183,188 sitting lateral tilt using gym ball 78 sitting pelvic tilt using gym ball 77-78 sitting position exercises 181-183 sitting sternal lift 182-183 sitting wide splits 152-153 sit-up: exercises 64; modified 124-127; traditional 120-122 Skall, EH. 6 skill-based exercise therapy 6-7 slouched posture 150. (see also swayback slow-twitch muscles 93 snatch lift 253 specific adaptation to imposed demand 99-100 specificity principle 234-235 speed: defined 223; with plyometrics 222-227 spinal discs: avascular nature 22; concentric bands 21; of vertebral column 20-22 spinal extensor muscles: about 49-50; deep (intersegmental) muscles 50-52; superficial muscles 52-54 spinal lengthening 153-154 spinal pathology 233 spinal range of motion 35 spinal segment 14,15/ spinal segment ligaments 16f, 16t spinal stability: achieving and maintaining 1112; and lifting 36; system 11/ spine: arch model 38-40; as cantilever system 36-37; keeping vertical 247-248; structural changes 4 spondylolisthesis 7, 7f spondylolysis 7,7/ squat 216-218 squat lift 40-41 stability ball exercises 186-197 stability program: advanced design 237-238; design principles 234-235; parallel tracks 235-237 stabilizer muscles: about 92-96; affecting lower back 96/; characteristics 93t stadiometer 142,142f standing: abdominal hollowing 82; axial compression 26 standing abdominal hollowing 84
standing assisted pelvic tilt 74 standing hip abduction 180 standing hip hinge 181 standing hip hinge movement 72-73 standing knee raising 71 standing position exercises 178-181 standing posture assessment 140f standing sternal lift 179 starting positions 31,82-86,169 static joint positioning 8D-81 static posture 135 static stretching I11t, 112, 113 sternal lift exercise 162 stiffness 95-96,198-199 stoop lift 40-41 straight-leg raise: modified 127-130; traditional 123-124 straight-leg raise test 109-110 stretched muscle assessment 103-106 stretching: principles 111-113; target muscles 113-118; techniques I11t stretch-shorten cycle 223-224 stretch weakness 100 structural injury 4 structural taping 144 superficial abdominal muscles 55-57 superficial spinal extensor muscles 52-54 superimposed limb movements 168-169 superman, basic 190 superman with arms 190-191 superset 238 surgery 6 sustained flexion 31-32 swayback 145f, 150-155, 151f symmetry, in postural assessment 138 synovia 22
T tactile cues 86-87 taping 144-145,244-245 task muscles 92. (see also mobilizer muscles) teaching clients: abdominal hollowing 81-89; advance preparation 69; modifications of exercises 124; multifudus contraction 89-91; multisensory cues 86; neutral position 78-81; pelvic tilt control 70-78; rhythmic stabilization 90-91; tactile cues 86-87; visualization 88 terminology 17,45,135 therapist referrals 234 Thomas test 107-108,237 Thomas test stretch 114 thoracic iliocostalis muscle 53 thoracic joint mobilization 159-160 thoracic longissimus muscle 53 thoracolumbar fascia: coupling and sacroiliac joint 48-49; cross section 46f; as hydraulic amplifier 47-48; muscle attachments to 46f; structure 44-45 thoracolumbar fascia mechanism 45,47,47/ threshold to detection of passive motion 198,199200 throw-catch activities on mobile surface201
Index' tightening 94 tightness, assessing 107 tissue microtrauma 204,248 tissue overstretch 31 torque: defined 35; lifting as set of 35-37; in posterior ligamentous system 44 trabecula 17 tragus 135 trainer qualifications 214,234 . . . training: abdominaUsee abdommal trammg); abdominal muscle recruitment 99J; advanced training qualifications 167-168; motor skill training 143-144; muscle adaptation 97-99; nervous system 198199; postural sway reduction 136; . progression 168-169,206,214; prop noceptive training 197-201; pyramid training 206, 238 training specificity 99-100 transversalis fascia 58! 59! transversus abdominis muscle 57-58, 58!, 61-62, 62f traumatic injury 204 treatment costs 3-4 Trendelenburg sign 73, 151 trigger points 106 tripod stretch 117 tripod test 110 trunk alignment, in traditional sit-up 121! trunk curl 126-127 trunk flexion, in traditional sit-up 132! trunk flexion with high pulley 212 trunk muscle action: abdominal muscles 55-60; coordination of abdominals during spinal movement 60-62; iliopsoas 54-55; spinal extensor muscles 49-54 trunk side flexor stretch 117-118 trunk stability, in overhead lifting 59-60, 59! TTDPM (threshold to detection of passive motion) 198,199-200 twist and throw with medicine ball 226 Twomey, L.T. 65
type type
II movement I movement
271
33 33
U unwillingness
to exercise
244-245
V Valsalva maneuver 63-64 ventral, defined 17 ventral ligaments 16/, 18-20 vertebral column IS! vertebral column anatomy: bones and joints 1415; facet joints 22-23; ligaments 15-16, 18-20; sacroiliac joint 23-25; spinal discs 20-22 vertebral compression 125/ vertebral pedicle 17 vertical spine 247-248 video feedback 241,245 visualization 88 Vleeming, A. 48 voluntary muscle control 69
W Waddell, G. 6 wall bar hanging leg raise 129-130 wall sit 195-196 Watson, P.). 5 webbing belt 87,87! Weber, H. 6 Webright, WG. 112 Weider,). 207 weight bag passive stretch 161-162 . weight training: about 202; free weight exercises 213-222; machine exercises 205-212; preparation 203; program design 238; safety 204 Wells, K. 136 wobble boards 183, 185 women, range of motion 30
Z Zetterberg,
C. 61
About the Author Christopher M. Norris, MSc, MCSp, has more than twenty years of experience as a physiotherapist and sport scientist. His specialty is exercise therapy. He is currently the director of Norris Associates in Manchester, UK. An expert on back stability, Norris is the author of four books. One of his books on sports injuries is in its second edition and has been adopted by most physiotherapy schools in the United Kingdom. He has taught for the British Association of Sports Medicine on flexibility training and back rehabilitation. In addition to serving as a consultant to major companies, Norris also published the first-ever review of back stability in a series of articles in Physiotherapy Journal. Norris is a member of the Chartered Society of Physiotherapy and the Society of Orthopaedic Medicine. He holds a certificate in occupational health physiotherapy, an advanced certificate in acupuncture, and a certificate in business administration. He and his wife Hildegard live in the Peak District National Park. He enjoys hill walking and ju jitsu.
272
1
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺍﺭﺍﺋﻪﻛﻨﻨﺪﻩ ﻛﺘﺎﺏ ﻭ ﻧﺮﻡﺍﻓﺰﺍﺭﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﺎﻥ ﻫﻤﮕﺎﻡ ﺑﺎ ﺗﻮﺳﻌﻪ ﻋﻠﻤﻲ ﻭ ﻓﺮﻫﻨﮕﻲ ﺟﻬﺎﻥ ﻣﻌﺎﺻﺮ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺭﻭﺯﺍﻓﺰﻭﻥ ﻛﺎﻣﭙﻴﻮﺗﺮ ﺩﺭ ﺑﻴﻦ ﺟﻮﺍﻣﻊ ﺑﺸﺮﻱ ﺧﺼﻮﺻ ًﹰﺎ ﺭﺷﺘﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻋﻠﻮﻡ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺑﻬﻴﻨﻪ ﺍﺯ ﺁﺧﺮﻳﻦ ﻳﺎﻓﺘﻪﻫﺎﻱ ﭘﺰﺷﻜﻲ ﺩﻧﻴﺎ ﻭ ﺍﺭﺍﺋﻪ ﺍﻳﻦ ﻳﺎﻓﺘﻪﻫـﺎ ﺩﺭ ﻗﺎﻟـﺐ ﻧـﺮﻡﺍﻓﺰﺍﺭﻫـﺎﻱ ﭘﺰﺷﻜﻲ ) VHS ، DVD ، VCD ، ebookﻭ (...ﻣﺎ ﺭﺍ ﺑﺮ ﺁﻥ ﺩﺍﺷﺖ ﻛﻪ ﺑﺎ ﮔﺮﺩﺁﻭﺭﻱ ﻭ ﺍﺭﺍﺋﺔ ﺍﻳﻦ ﻳﺎﻓﺘﻪﻫﺎ ﮔﺎﻣﻲ ﻛﻮﭼﻚ ﺩﺭ ﺭﺍﻩ ﺍﺭﺗﻘﺎﺀ ﺳﻄﺢ ﻋﻠﻤﻲ ﻣﺘﺨﺼﺼﻴﻦ ﻛﻠﻴﻪ ﺭﺷﺘﻪﻫﺎﻱ ﭘﺰﺷﻜﻲ ﻛﺸﻮﺭ ﺑﻪ ﺻﻮﺭﺕ ﺳﻤﻌﻲ ﻭ ﺑﺼﺮﻱ ﺑﺮﺩﺍﺭﻳﻢ .ﺍﻣﻴﺪ ﺍﺳﺖ ﻣﺸﻮﻕ ﻣﺎ ﺩﺭ ﺍﻳﻦ ﺭﺍﻩ ﺑﺎﺷﻴﺪ. ﻟﺬﺍ ﻋﻼﻗﻤﻨﺪﺍﻥ ﻣﻲﺗﻮﺍﻧﻨﺪ ﺑﺮﺍﻱ ﺩﺭﻳﺎﻓﺖ ﻫﺮ ﻳﻚ ﺍﺯ ﻣﺤﺼﻮﻻﺕ ﺍﺭﺍﺋﻪﺷﺪﻩ ﺑﻪ ﺍﺯﺍﺀ ﻫﺮ CDﻣﺒﻠﻎ ٥٠٠٠ﺗﻮﻣﺎﻥ ﺑﻪ ﺣﺴﺎﺏ ﺟﺎﺭﻱ ١٣٢٤٣٦ﺑﺎﻧﻚ ﺭﻓﺎﻩ ﻛﺎﺭﮔﺮﺍﻥ ﺷﻌﺒﻪ ﻣﻴﺪﺍﻥ ﺍﻧﻘﻼﺏ ﻛﺪ ﺷﻌﺒﻪ ١١٢ﺑﻪ ﻧﺎﻡ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﻭﺍﺭﻳﺰ ﻭ ﭘـﺲ ﺍﺯ ﻓﺎﻛﺲ ﻓﻴﺶ ﻓﻮﻕ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﺸﺎﻧﻲ ﺩﻗﻴﻖ ﻧﺴﺒﺖ ﺑﻪ ﺧﺮﻳﺪ ﺍﻗﻼﻡ ﻭ ﺩﺭﻳﺎﻓﺖ ﻛﺎﻻﻱ ﻣﻮﺭﺩ ﻧﻈﺮ ﺧﻮﺩ ﺍﻗﺪﺍﻡ ﻧﻤﺎﻳﻨﺪ .ﻻﺯﻡ ﺑﻪ ﺫﻛﺮ ﺍﺳﺖ ﻓﻘﻂ ﺑﻪ ﺳﻔﺎﺭﺷﺎﺗﻲ ﻛﻪ ﻭﺟﻪ ﻣﻮﺭﺩ ﺳﻔﺎﺭﺵ ﺑﻪ ﺣﺴﺎﺏ ﻓﻮﻕ ﺫﻛﺮ ﻭﺍﺭﻳﺰ ﺷﺪﻩ ﺗﺮﺗﻴﺐ ﺍﺛﺮ ﺩﺍﺩﻩ ﺧﻮﺍﻫﺪ ﺷﺪ ،ﻟـﺬﺍ ﺧﻮﺍﻫﺸﻤﻨﺪ ﺍﺳﺖ ﺍﺯ ﻭﺍﺭﻳﺰ ﻭﺟﻪ ﺑﻪ ﻫﺮ ﮔﻮﻧﻪ ﺣﺴﺎﺏ ﺩﻳﮕﺮﻱ ﺍﻛﻴﺪﺍ ﺧﻮﺩﺩﺍﺭﻱ ﻓﺮﻣﺎﺋﻴﺪ. ﻻﺯﻡ ﺑﻪ ﺫﻛﺮ ﺍﺳﺖ ﺩﺭ ﺻﻮﺭﺕ ﻧﻴﺎﺯ ﺑﻪ ﻫﺮﮔﻮﻧﻪ ﺍﻃﻼﻋﺎﺕ ﺗﻜﻤﻴﻠﻲ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺑﻪ ﻧﺸﺎﻧﻲ ﻣﺮﻛﺰ ﻣﺮﺍﺟﻌﻪ ﻭ ﻳﺎ ﺑﺎ ﺗﻠﻔﻦ ٦٩٣٦٦٩٦ﺗﻤﺎﺱ ﺣﺎﺻﻞ ﻧﻤﺎﻳﻴﺪ.
-١ﺭﺍﺩﻳﻮﻟﻮﮊﻱ
ﻋﻨﻮﺍﻥ CD
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
)3D Conformal Radiation Therapy A multimedia introduction to methods and techniques (Springer
ــــــ
1.1
)2.1 Abdominal and pelvic Ultrasound with CT and MR correlation (R. Brooke Jeffrey, Jr., M.D.
ــــــ
ﺍﻳﻦ ﻳﻚ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺷﻲ ﻗﻮﻱ ﺑﻤﻨﻈﻮﺭ Self teachingﻭ Self evaluationﺗﺸﺨﻴﺺﻫﺎﻱ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺷﻜﻢ ﻭ ﻟﮕﻦ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻛﻨﺎﺭ ﺗﺼﺎﻭﻳﺮ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ ﺑﻴﻤﺎﺭﻱ ،ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﻫﻤﺰﻣﺎﻥ CT Scanﻭ MRIﺑﺮﺍﻱ ﻓﻬﻢ ﻭ ﺩﺭﻙ ﺑﻬﺘـﺮ ﻣﻄﺎﻟـﺐ ﺍﺳـﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ، CDﻣﺒﺎﺣﺚ ﻣﺨﺘﻠﻒ ﺑﻪ ﺻﻮﺭﺕ Caseﻣﻄﺮﺡ ﮔﺮﺩﻳﺪﻩ ﻭ ﺿﻤﻦ ﺑﻴﺎﻥ ﺷﺮﺡ ﺣﺎﻝ ﺑﻴﻤﺎﺭ ،ﺗﺼﺎﻭﻳﺮ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ )ﻭ ﺩﺭ ﺻﻮﺭﺕ ﻟﺰﻭﻡ MRIﻭ (CT Scanﺑﻪ ﻧﻤﺎﻳﺶ ﮔﺬﺍﺷﺘﻪ ﺷﺪﻩ ﻭ ﺑﺎ Clickﺁﺭﺍﻳﺔ ،Textﻣﻄﺎﻟﺐ ﺗﺌﻮﺭﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ Caseﺑﺎ ﺑﻴﺎﻧﻲ ﺳـﺎﺩﻩ ﻭ ﺩﺭ ﻋﻴﻦ ﺣﺎﻝ ﻛﺎﻣﻞ ،ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻛﺎﺭﺑﺮ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ. ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ ﺍﻳﻦ CDﺑﺮ ﺣﺴﺐ ﻣﻮﺿﻮﻉ ﺑﻪ ﻗﺮﺍﺭ ﺟﺪﻭﻝ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﺪﺍﺩ Case
٧٨
ﻣﻮﺿﻮﻉ ﺳﻴﺴﺘﻢ ﮔﻮﺍﺭﺷﻲ
ﺗﻌﺪﺍﺩ Case
٣٥
ﻣﻮﺿﻮﻉ ﻛﻠﻴﻪ ﻭ ﻏﺪﻩ ﺁﺩﺭﻧﺎﻝ
ﺗﻌﺪﺍﺩ Case
٣٧
ﻣﻮﺿﻮﻉ ﭘﺎﻧﻜﺮﺍﺱ
ﺗﻌﺪﺍﺩ Case
١٢ ٧
ﻣﻮﺿﻮﻉ ﻃﺤﺎﻝ ﺭﺗﺮﻭﭘﺮﻳﺘﻮﺋﻦ
ﺗﻌﺪﺍﺩ Case
٤٠ ٤٦
ﻣﻮﺿﻮﻉ ﻛﻴﺴﺔ ﺻﻔﺮﺍ ﻭﻣﺠﺎﺭﻱ ﺻﻔﺮﺍﻭﻱ ﻟﮕﻦ
ﺗﻌﺪﺍﺩ Case
٦٧ ١٠
ﻣﻮﺿﻮﻉ ﻛﺒﺪ ﺣﺎﻣﻠﮕﻲ
)ACR - Chest (Learning file) (American college of Radiology ﺍﻳﻦ CDﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ:
2001 4- Airway Disease 8-Pediatric Chest 12- Immunocompromised Host
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
3- Vascular Disease 7- Chest Wall and Diaphragm 11- Pulmonary Infection
2- Cardiac Disease 6- Pleural Disease 10- Neoplasma and Tumors
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
3.1
1- chest Trauma 5- Mediastinal Masses 9- Normal Disease 13- Diffuse Disease
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
2 ACR - Gastrointestinal (Learning file) (American college of Radiology) (Igor Laufer, M.D., James M. Messmer, M.D.) (Learning file) (American college of Radiology) 5.1 ACR - Genitourinary ( ﺑﻮﺩﻩ ﻭ ﺩﺭﺻﻮﺭﺕ... ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻭ، CT Scan ، ﻣﻄﺎﻟﻌﺎﺕ ﺑﺎ ﻣﻮﺍﺩ ﺣﺎﺟﺐ، ﺗﺼﺎﻭﻳﺮ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ )ﻋﻜﺲﻫﺎﻱ ﺳﺎﺩﻩ، ﺩﺍﺭﺍﻱ ﺗﺎﺭﻳﺨﭽﻪ ﺑﺎﻟﻴﻨﻲCase ﻫﺮ. ﻣﻄﺮﺡ ﮔﺮﺩﻳﺪﻩﺍﻧﺪCase ﺗﻌﺪﺍﺩﻱ، ﺷﺎﻣﻞ ﻓﺼﻮﻝ ﻣﺘﻌﺪﺩﻱ ﺩﺭ ﺧﺼﻮﺹ ﺍﻭﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻣﻲﺑﺎﺷﺪ ﻭ ﺩﺭ ﻫﺮﻓﺼﻞCD ﺍﻳﻦ . ﺗﺸﺨﻴﺺ ﻧﻬﺎﻳﻲ ﻭ ﻫﻤﭽﻨﻴﻦ ﺗﻮﺿﻴﺤﺎﺕ ﻋﻠﻤﻲ ﺍﺿﺎﻓﻪ ﻣﺮﺗﺒﻂ ﺑﺎ ﺗﺸﺨﻴﺺ ﺑﺎ ﺍﻃﻼﻉ ﺷﺪ، ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﺭﺍﻳﻪﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﻣﻲﺗﻮﺍﻥ ﺍﺯ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ، ﺩﺭﻧﻬﺎﻳﺖ. ﻣﻄﻠﻊ ﮔﺮﺩﺩFinding ﻧﻤﻮﺩﻥ ﺑﺮﺭﻭﻱ ﺁﻳﻜﻮﻥClick ﺑﺎImaging ﻓﺮﺩ ﻣﻲﺗﻮﺍﻧﺪ ﺍﺯ ﻳﺎﻓﺘﻪﻫﺎﻱ،ﻧﻴﺎﺯ : ﻫﺎﻱ ﻣﻄﺮﺡ ﺷﺪﻩ ﺑﺮ ﺣﺴﺐ ﻫﺮ ﻓﺼﻞ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCase ﺗﻌﺪﺍﺩ 4.1
ﻣﻮﺿﻮﻉ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﻠﻴﻪ ﺑﺎﻟﻐﻴﻦ
ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case
١١٨
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﻠﻴﻪ ﺍﻃﻔﺎﻝ
ﺗﻌﺪﺍﺩ Case
٢٦
ﻣﻮﺿﻮﻉ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺣﺎﻟﺐ
ﺗﻌﺪﺍﺩ
ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case
Case
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﮊﻧﻴﻜﻮﻟﻮﮊﻳﻚ
١٧
ﻣﻮﺿﻮﻉ ﻏﺪﺩ ﺁﺩﺭﻧﺎﻝ
١٥
ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case
ﺳﻴﺴﺘﻢ ﺍﺩﺭﺍﺭﻱ ﺗﺤﺘﺎﻧﻲ ﺍﻃﻔﺎﻝ
١١
ﺗﻌﺪﺍﺩ
ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case
١٨
Case
ﺭﺗﺮﻭﭘﺮﻳﺘﻮﺋﻦ
١٠
ﻣﻮﺿﻮﻉ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺜﺎﻧﻪ
ﺗﻌﺪﺍﺩ Case
١٧
ﻣﻮﺿﻮﻉ
ﺗﻌﺪﺍﺩ Case
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﭘﺮﻭﺳﺘﺎﺕ
١٠
ﻣﻮﺿﻮﻉ ﺩﺳﺘﮕﺎﻩ ﺗﻨﺎﺳﻠﻲ ﺧﺎﺭﺟﻲ ﻣﺬﻛﺮ
1998 1998
ﺗﻌﺪﺍﺩ Case
١٦
6.1
ACR - Head & Neck (Learning file) (American college of Radiology)
1998
7.1
ACR - Neuroradiology (Learning file) (American college of Radiology)
1998 ــــــ
ACR - Nuclear medicine (Learning file) (American college of Radiology) (Paul Shreve, M.D. and James Corbett, M.D.) 9.1 ACR - Pediatric (Learning file) (American college of Radiology) (Beverly P. Wood, M.D., David C. Kushner, M.D.) : ﻣﺮﺗﺒﻂ ﺑﺎ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺍﻃﻔﺎﻝ ﺑﻮﺩﻩ ﻭ ﺩﺍﺭﺍﻱ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪTeaching File ﻓﻮﻕ ﻳﻚCD
8.1
ﻋﻨﻮﺍﻥ
Case ﺗﻌﺪﺍﺩ
Chest
٢٠٢ ٣١
ﺳﺮ ﻭ ﮔﺮﺩﻥ
ﻋﻨﻮﺍﻥ ﻗﻠﺐ ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ
Case ﺗﻌﺪﺍﺩ
٧٨ ٩٠
Case ﺗﻌﺪﺍﺩ
ﻋﻨﻮﺍﻥ ﮔﻮﺍﺭﺵ Skeletal
١٦٣ ٩٧
ﻋﻨﻮﺍﻥ ﭘﺎﻧﻜﺮﺍﺱ، ﻃﺤﺎﻝ،ﻛﺒﺪ
Case ﺗﻌﺪﺍﺩ
ﻋﻨﻮﺍﻥ
Case ﺗﻌﺪﺍﺩ
٧١
Genitourimary
١٠٩
10.1 ACR - Skeletal (B.J Manaster, M.D., Ph.D.) (Learning file) 1. Tumolrs 2. Arthritis 3. Trauma 4. Metabolic Congeaital 11.1 ACR
1998
ــــــ
- Ultrasound (Learning file) (American college of Radiology)
1998
12.1 Anatomy and MRI of the JOINTS (A Multiplanar Atlas) (William D. Middleton, Thomas L. Lawson)
(Department of Radiology Medical College of Wisconsin Milwaukee, Wisconsin) The Tmporomandibular
The Shoulder
The Wrist
The Finger
The Vertebral Column
The Hip
The Knee
The Ankle
TM
Brainiac! Medical Multimedia Systems Presents (Version 1.52) (An interactive digital atlas designed to assist in learning human neuroanatomy) Breast Implant Imaging (SALEKAN E-BOOK) (MICHAEL S. MIDDLETON, PH,D., M.D, MICHAEL P.MCNAMARA JR., M.D.) 13.1 9.9
(Serial # 316.34427)
:ﺍﻳﻦ ﻛﺘﺎﺏ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ A History and Overview of Breast Augmentation and Implant Imaging Basic Principles of Breast Implant Imaging Classification of Breast Implants Evaluation of Silicone Fluid Injecitons
Clinical Presentation Principles of Imaging Breast Implant Rupture and Soft-Tissue Silicone Practical Consideration in the Evaluaion of Implant Integrity Breast Cancer Imaging
14.1 Carotid Duplex Ultrasonography Extracranial and Intracranial
2000 2003
Methods of Imaging Artifacts of MR and Ultrasound Imaging of Breast Implants and Soft-Tissue Silicone Evaluation of Soft-Tissue Silicone from Ruptured Implants Surgical and Other Considerations
(Michael Jaff DO, Serge Kownator MD, Alain Voorons Audlovlsuel)
ــــــ
ﺣﻠﻘﺔ ﻭﻳﻠﻴﺲ ﺗﻨﻪ ﺑﺮﺍﻛﻴﻮﺳﻔﺎﻟﻴﻚ ﻭ ﻗﻮﺱ ﺁﺋﻮﺭﺕ ﻣﻮﺭﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ ﻭ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺛﺎﺑﺖ ﻭ ﻣﺘﺤﺮﻙ ﮔﻮﻳـﺎ )ﺑـﻪ ﺯﺑـﺎﻥ ﺍﻧﮕﻠﻴﺴـﻲ( ﺟﻬـﺖ ﻧﻤـﺎﻳﺶ ﺗﻜﻨﻴـﻚﻫـﺎﻱ، ﻭﺭﺗﺒﺮﺍﻝ، ﺳﺎﺏ ﻛﻼﻭﻳﻦ، ﻛﻠﻴﺎﺕ ﺍﻧﺠﺎﻡ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻛﺎﺭﻭﺗﻴﺪ، CD ﺩﺭ ﺍﻳﻦ : ﺭﺋﻮﺱ ﻣﻄﺎﻟﺐ ﻣﻮﺭﺩ ﺑﺤﺚ ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺪﻳﻦ ﻗﺮﺍﺭ ﺍﺳﺖ. ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ،ﺳﻮﻧﻮﮔﺮﺍﻓﻲﻫﺎﻱ ﻓﻮﻕ ﻭ ﻫﻤﭽﻨﻴﻦ ﭼﮕﻮﻧﮕﻲ ﺗﻔﺴﻴﺮ ﻧﺘﺎﻳﺞ ﺣﺎﺻﻞ ﺍﺯ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻓﻮﻕ ﻭ ﻫﻤﭽﻨﻴﻦ ﭼﮕﻮﻧﮕﻲ ﺗﻔﺴﻴﺮ ﻧﺘﺎﻳﺞ ﺣﺎﺻﻞ ﺍﺯ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻓﻮﻕﺍﻟﺬﻛﺮ ﺁﺷﻨﺎﻳﻲ ﺑﺎ ﺩﺳﺘﮕﺎﻩ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺳﺎﺏ ﻛﻼﻭﻳﻦ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﺳﻮﺑﺮﺍﻝ ﻭ ﺣﻠﻘﺔ ﻭﻳﻠﻴﺲ
ﺩﺳﺘﮕﺎﻩSetting ﭼﮕﻮﻧﮕﻲ ﺍﺳﻜﻦﻛﺮﺩﻥ ﻋﺮﻭﻕ ﻓﻮﻕﺍﻟﺬﻛﺮ ﻭ ﻧﺤﻮﺓ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻭﺭﺗﺒﺮﺍﻝ ﺿﺎﻳﻌﺎﺕ ﻣﺠﺎﻭﺭ
ﺷﺮﻳﺎﻥﻫﺎﻱ ﻛﺎﺭﻭﺗﻴﺪ ﺍﻛﺴﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻗﻮﺱ ﺁﺋﻮﺭﺕ ﻭ ﺗﻨﺔ ﺑﺮﺍﻛﻴﻮ ﺳﻔﺎﻟﻴﻚ Revaseularization ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﭘﺲ ﺍﺯ
. ﻣﻲﺑﺎﺷﺪPost-Test ﻭPre-Test ﺟﻬﺖ ﺍﺭﺯﻳﺎﺑﻲ ﻓﺮﺩ ﺍﺯ ﺧﻮﺩ ﺩﺍﺭﺍﻱCD ﺿﻤﻨﹰﺎ ﺍﻳﻦ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
3 ــــــ
)(Pamela T. Johnson, Alfred B. Kurtz
WITH CROSS-REFERENCES TO THE REQUISITES SERIES
15.1 CASE REVIEW Obstetric and Gynecologic Ultrasound
ﺍﻳﻦ CDﻣﺤﺘﻮﻱ Case ١٢٧ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺯﻧﺎﻥ ﻭ ﺯﺍﻳﻤﺎﻥ )ﺑﺼﻮﺭﺕ ﭘﺮﺳﺶ ﻭ ﭘﺎﺳﺦ( ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻫﻤﺮﺍﻩ ﺗﻮﺿﻴﺤﺎﺕ ﻭ ﺗﺼﺎﻭﻳﺮ ﻣﺮﺑﻮﻃﻪ ﺑﻮﺩﻩ ﻭ ﺩﺭ ﻓﻬﻢ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ Gynecologyﻭ Obstetricﺑﺴﻴﺎﺭ ﻣﻔﻴﺪ ﺧﻮﺍﻫﺪ ﺑﻮﺩ. ــــــ
)16.1 CD Roentgen (Michael McDermott, M.D., Thorsten Krebs, M.D.) (Williams & Wilkins
2000 ــــــ
17.1 Cerebral and Spinal Computerized Tomography )18.1 Cerebral MR Perfusion Imaging CD-ROM to complement the book (A. Gregory Sorensen, Peter Reimer) (Thieme
ﺍﻳﻦ CDﺩﺭ ﺯﻣﻴﻨﺔ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﭘﺮﻓﻮﺯﻳﻮﻥ ﻣﻐﺰﻱ ﺑﻮﺳﻴﻠﺔ MRIﺑﻪ ﺷﺮﺡ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﻭ ﻫﻤﭽﻨﻴﻦ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﺁﻧﻬﺎ ﭘﺮﺩﺍﺧﺘﻪ ﻭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺛﺎﺑﺖ ﻭ ﻣﺘﺤﺮﺕ ﺑﻪ ﺷﺮﺡ ﻣﻔﺎﻫﻴﻢ ﻣﺮﺗﺒﻂ ﺑﺎ ﺍﻳﻦ ﺭﻭﺵ ﺗﺸﺨﻴﺼﻲ ﻣﻲﭘﺮﺩﺍﺯﺩ. 19.1 CHEST X-RAY INTERPRETATION
2002
CDﺣﺎﺿﺮ ﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﺑﺮﻧﺎﻣﻪﻫﺎ )ﭼﻪ ﻛﺘﺎﺏ ﻭ ﭼﻪ (CDﺩﺭ ﻣﻮﺭﺩ ﭼﮕﻮﻧﮕﻲ ﺗﻔﺴﻴﺮ CXRﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ CDﺷﺎﻣﻞ ٣ﺑﺨﺶ Clinic -٣ seminar -٢ Library -١ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻋﻜﺲ ﺳﺎﻟﻢ ﺭﻳﻪ ﻫﻤـﺮﺍﻩ ﺑـﺎ ﺗﻮﺿـﻴﺤﺎﺕ ﻭ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻭ ﺑﺮﺍﻱ ﻓﻬﻢ ﻣﻄﻠﺐ ﻓﻴﻠﻢﻫﺎﻱ ٣ﺑﻌﺪﻱ animatoryﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺑﺨﺶ ﺍﻭﻝ Library :ﻳﺎ ﻛﺘﺎﺑﺨﺎﻧﻪ : ﺍﻟﻒ( ﺑﻴﻤﺎﺭﻱﻫﺎ ﺑﻪ ﺗﺮﺗﻴﺐ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﺳﭙﺲ CXRﻭ ﻣﺘﻦ ﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻥ ﺑﻴﻤﺎﺭﻱ ﻭ ﺗﻔﺴﻴﺮ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺏ :ﺍﺑﺘﺪﺍ ﻳﻚ ﻋﻜﺲ ﺭﻳﻪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺳﭙﺲ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺁﻥ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﺝ : Sings, clue :ﻋﻼﺋﻢ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﺗﻌﺮﻳﻒ ﻭ ﺩﺭ CXRﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻣﺎﻧﻨﺪ(…,westermark Sing, Sign) : ﺩ : Anatomy World :ﺁﻧﺎﺗﻮﻣﻲ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﺑﺎ ﻣﻘﺎﻃﻊ ﻃﻮﻟﻲ ﻭ ﻋﺮﺿﻲ ﻭ ﻫﻮﺭﻳﺰﻧﺘﺎﻝ ﺑﻪ ﺻﻮﺭﺕ 3Dﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻫ :ﺩﻳﻜﺸﻨﺮﻱ :ﺗﻌﺎﺭﻳﻒ ﻋﻼﺋﻢ ﻭ ﻧﺸﺎﻧﻪﻫﺎﻱ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻭ :CME Quiz :ﻋﻜﺲ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻲ ﻭ ﺷﺮﺡ ﺣﺎﻝ ﺑﻴﻤﺎﺭ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪ .ﺳﭙﺲ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﻳﺎﻓﺘﻪﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺭﺍ ﻣﺸﺨﺺ ﻧﻤﺎﻳﺪ. ﺑﺨﺶ ﺩﻭﻡ ﻳﺎ :Seminarﺑﻪ ٥ﺑﺨﺶ: -٢ Soft tissue -١ﺍﺳﺘﺨﻮﺍﻧﻬﺎ -٣ﭘﻠﻮﺭﻭﺩﻳﺎﻓﺮﺍﮔﻢ -٤ﺭﻳﻪ ﻭ -٥ﻣﺪﻳﺸﺎﻥ ﺗﻘﺴﻴﻢ ﺷﺪﻩ. ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﺍﺑﺘﺪﺍ ﻋﻜﺴﻲ ﺍﺯ ﺭﻳﻪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺷﺨﺺ ﺑﺎﻳﺪ ﻣﺤﻞ ﺿﺎﻳﻌﻪ ﻭ ﺗﺸﺨﻴﺺ ﺑﻴﻤﺎﺭﻱ ﺭﺍ ﻣﺸﺨﺺ ﺳﺎﺯﺩ .ﺩﺭ ﻣﻮﺭﺩ ﻗﺴﻤﺖ ﺭﻳﻪ ﺧﻮﺩ ﺑﻪ ٤ﺑﺨﺶ Searchﻭ Localizeﻭ describeﻭ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺗﻘﺴﻴﻢ ﺷﺪﻩ ﺍﺳﺖ. : Searchﻋﻜﺲ ﺭﻳﻪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﻣﺤﻞ ﺿﺎﻳﻌﻪ ﺭﺍ ﻧﺸﺎﻥ ﺩﻫﺪ ) ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻮﺱ( :Localizeﺍﺑﺘﺪﺍ ﻋﻼﻣﺖ ﻳﺎ ﻧﺸﺎﻧﻪ ﺑﻴﻤﺎﺭﻱ ﺩﺭ CXRﺷﺮﺡ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﻣﺤﻞ ﺁﻧﺮﺍ ﻧﺸﺎﻥ ﺩﻫﺪ. ﻼ ﺗﻮﺩﻩﺍﻱ ﺩﺭ CXRﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﺑﺘﻮﺍﻧﺪ ﺗﻌﻴﻴﻦ ﻛﻨﺪ ﺧﻮﺵ ﺧﻴﻢ ﺍﺳﺖ ﻳﺎ ﺑﺪ ﺧﻴﻢ. :Describeﺍﺑﺘﺪﺍ CXRﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﺍﺯ ﺑﻴﻦ ٢ﮔﺰﻳﻨﻪ ﻳﻜﻲ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﺪ ﻣﺜ ﹰ CXR :Differential diagnosisﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭﺳﭙﺲ ﺑﻴﻤﺎﺭﻳﻬﺎpattern ،ﻫﺎﻱ ﺑﻴﻤﺎﺭﻱ ﺑﻪ ﺻﻮﺭﺕ ﺗﺴﺖ ﭼﻨﺪ ﺟﻮﺍﺑﻲ ﺁﻭﺭﺩ ﺷﺪﻩ ﺍﺳﺖ. ﺑﺨﺶ ﺳﻮﻡ :Clinicﺍﻳﻦ ﺑﺨﺶ ﺭﺍ ﺑﺮﺍﻱ ﻛﻤﻚ ﺑﻪ ﺗﻘﺴﻴﻢ ﻗﺪﻡ ﺑﻪ ﻗﺪﻡ ﻭ ﻳﺎ ﻧﻮﺷﺘﻦ ﻳﻚ ﺗﻔﺴﻴﺮ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺍﺳﺖ. ﺑﻴﻤﺎﺭ ﺑﻪ ﻫﻤﺮﺍﻩ ﺷﺮﺡ ﺣﺎﻝ ،ﻣﻌﺎﻳﻨﻪ ﻓﻴﺰﻳﻜﻲ ﻭ CXRﻭ ﺩﺭ ﺻﻮﺭﺕ ﻟﺰﻭﻡ CT/MRIﺑﺮﻭﻧﻜﻮﺳﻜﻮﻳﻲ ﻭ ﺑﻴﻮﭘﺴﻲ ﻭ ﻧﻮﻛﺌﺎﺭﺩﺍﺳﻜﻦ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ. ﻛﺎﺭﺑﺮ ﺑﺎﻳﺪ ﺑﺮ ﺍﺳﺎﺱ ﻓﻮﺭﻳﺖ ﺗﻌﻴﻴﻦ ﺷﺪﻩ ﺍﺑﺘﺪﺍ ← Softtissueﺍﺳﺘﺨﻮﺍﻥ ← ﭘﻠﻮﺭﻭﺩﻳﺎﻓﺮﺍﮔﻢ ← ﺭﻳﻪ ← ﻣﺪﻳﺴﺘﺎﻥ ← ﻧﺎﻑ ﺭﻳﻪ ﻋﻜﺲ ﺭﺍ ﻣﻄﺎﻟﻌﻪ ﻧﻤﺎﻳﺪ ﺑﺮﺍﻱ ﻛﻤﻚ ﺑﻪ ﺗﻔﺴﻴﺮ ،ﺧﻮﺩ ﺑﺮﻧﺎﻣﻪ ﺑﺎ ﺗﻌﻴﻴﻦ ﺧﺼﻮﺻﻴﺎﺕ ﻣﻨﻄﻘﻪ ﺑﻪ ﻛـﺎﺭﺑﺮ ﺩﺭ ﺗﻔﺴـﻴﺮ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ﺑﺮﺍﻱ ﻣﺜﺎﻝ :ﺩﺭ ﻣﻮﺭﺩ ...... Softtissueﺑﺎﻓﺖ ﻧﺮﻡ ﺟﺪﺍﺭ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﺍﻓﺰﺍﻳﺶ ،ﻛﺎﻫﺶ ،ﻧﺮﻣﺎﻝ ﻭ ﻛﻠﻴﺴﻔﻴﻜﺎﺳﻴﻮﻥ ﻭ ﺍﺑﻨﺮﻣﺎﻝ airﻭ ....ﻣﻲﺑﺎﺷﺪ. )(Mosby
ــــــ
20.1 Comprehensive Reviw of Radiography
ﺍﻳﻦ CDﺑﻤﻨﻈﻮﺭ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ) (Self evaluationﺍﻓﺮﺍﺩ ﻣﺮﺗﺒﻂ ﺑﺎ ﺣﺮﻓﺔ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺗﺸﺨﻴﺼﻲ ﺩﺭ ﺯﻣﻴﻨﻪﻫﺎﻱ ﺯﻳﺮ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ: ﺗﻬﻴﻪ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﮔﺮﺍﻓﻲﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻛﺎﺭﻛﺮﺩ ﻭ ﻧﮕﻬﺪﺍﺭﻱ ﺍﺯ ﺩﺳﺘﮕﺎﻩﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺣﻔﺎﻇﺖ ﺍﺯ ﺍﺷﻌﻪ ﻧﮕﻬﺪﺍﺭﻱ ﻭ ﻣﺪﻳﺮﻳﺖ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺑﻴﻤﺎﺭﺍﻥ ﺭﻭﺵﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﭘﺲ ﺍﺯ ﻧﺼﺐ CDﻓﻮﻕ ،ﺩﺭ ﺷﺮﻭﻉ ،ﺷﺨﺺ ﺑﺎﻳﺴﺘﻲ ﻳﻜﻲ ﺍﺯ ﻣﺒﺎﺣﺚ ﭘﻨﺞﮔﺎﻧﻪ ﻓﻮﻕ ﺭﺍ ﺟﻬﺖ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﺪ ﻭ ﺑﻪ ﺩﻧﺒﺎﻝ ﺁﻥ ،ﺳﺆﺍﻻﺕ ﻫﺮ ﻣﺒﺤﺚ ﺑﺼﻮﺭﺕ ﭼﻨﺪﮔﺰﻳﻨﻪﺍﻱ ﻣﻮﺭﺩ ﺁﺯﻣﻮﻥ ﻗﺮﺍﺭ ﺧﻮﺍﻫﻨﺪ ﮔﺮﻓﺖ ﻭ ﺑﻪ ﺩﻧﺒﺎﻝ ﻫﺮ ﭘﺎﺳﺦ ،ﺗﻮﺿﻴﺤﺎﺕ ﻋﻠﻤﻲ ﻣﺮﺑﻮﻁ ﺟﻬـﺖ ﺍﺭﺗﻘﺎﺀ ﻋﻠﻤﻲ ﻓﺮﺩ ،ﺑﻪ ﻭﻱ ﺍﺭﺍﺋﻪ ﺧﻮﺍﻫﺪ ﮔﺮﺩﻳﺪ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
4 ــــــ
)21.1 Computed Body Tomography with MRI Correlation (Joseph K. T. Lee, Stuart S. Sagel, Robert J. Stanley, Jay P. Heiken) (3rd Edition) (LIPPINCOTT WILLIAMS & WILKINS
ــــــ 2000
)(Salekan E-Book
)(Matthias Hofer) (Thieme
22.1 CT Teaching Manual
)23.1 Diagnostic Imaging Expert (A CD-ROM Reference & Review) (Ralph Weissleder, Jack Witterberg, Mark J. Rieumont, Genevieve Bennett
ﺍﻳﻦ ﻳﻚ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺷﻲ ﺍﺯ ﻣﻄﺎﻟﺐ ﻣﺨﺘﻠﻒ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﺤﺴﻮﺏ ﻣﻲﺷﻮﺩ ﻭ ﺩﺭ ﺯﻣﻴﻨﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ،ﺑﻪ ﺑﺤﺚ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎ ﻭ ﺭﻭﺵﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ Imagingﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻧﻬﺎ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺍﻳـﻦ CDﺩﺍﺭﺍﻱ ﺁﺭﺍﻳـﻪﻫـﺎﻱ ﺫﻳـﻞ ﻣﻲﺑﺎﺷﺪ: 1- Chest 2- Breast
3- Cardiac 4- Obstetric
5- Gastrointestinal 6- Pediatric
7- Genitourinary 8- Nuclear Imaging
9- Musculoskeletal 10- Contrast agent
11- Neurologic
14- Vascular 13- Head and Neck 12- Imaging Physics
)24.1 DIAGNOSTIC ULTRASOUND A LOGICAL APPROACH (JOHN P. McGAHAN, BARRY B. GOLDBERG
ــــــ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ٣ﻗﺴﻤﺖ ﺍﺳﺖ:
-١ﻛﺘﺎﺏ Diagnostic Ultrasoundﻋﻼﻭﻩ ﺑﺮ ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﻭ ﺟﺰﺀ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮﺩ ﺩﻳﮕﺮ ﺷﺎﻣﻞ ﺩﻭ ﻓﻴﻠﻢ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻭ ﺩﺍﭘﻠﺮ ﻫﺮ ﺑﺨﺶ ﺑﻪ ﺻﻮﺭﺕ ﺯﻧﺪﻩ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. Selp-assessment -٢ﺑﻪ ﺻﻮﺭﺕ CMPﻭ ﺗﺴﺖﻫﺎﻱ ﭼﻨﺪﮔﺰﻳﻨﻪﺍﻱ ﻣﻲﺑﺎﺷﺪ. ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺣﺎﺿﺮ ﺷﺎﻣﻞ ٤١ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺷﺎﻣﻞ: -١ﻓﻴﺰﻳــــﻚ -٢ bioeffectsﺁﺭﺗﻔﻜــــﺖ ٣ﻭ -٤ﺭﻭﺵﻫــــﺎﻱ ﺗﻬــــﺎﺟﻤﻲ ﺑــــﺎ ﺳــــﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺭ )ﺑﻴﻮﭘﺴــــﻲ ،ﺁﺳﭙﻴﺮﺍﺳــــﻴﻮﻥ ﻭ ﺩﺭﻧــــﺎﮊ( ﻭ ﺩﺭ ﺑﻴﻤــــﺎﺭﻱﻫــــﺎﻱ ﺯﻧــــﺎﻥ ﻭ ﺯﺍﻳﻤــــﺎﻥ -٥ﺭﻭﺵﻫــــﺎﻱ ﺍﻭﻟﺘﺮﺍﺳــــﻮﻧﻮﮔﺮﺍﻓﻲ ﺣــــﻴﻦ ﻋﻤــــﻞ ﺟﺮﺍﺣــــﻲ :٦-١٨ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺣﺎﻣﻠﮕﻲ ،ﭘﻼﺳﻨﺘﺎ ﻭ Cervixﻭ ﺑﻨﺪ ﻧﺎﻑ ﻭ ﭘﺮﺩﻩ ﺁﻣﻨﻴﻮﺗﻴﻚ ،ﺳﺮ ﻭ ﺻﻮﺭﺕ ﻭ ﮔﺮﺩﻥ ﻭ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﺷﻜﻢ ﻭ ﻟﮕﻦ ﻭ ﺿﺮﺑﺎﻥ ﻗﻠﺐ ﻭ ﺍﻧﺪﺍﺯﻩﻫﺎﻱ ﺟﻨﻴﻦ ﻭ ﺣﺎﻣﻠﮕﻲ ﺩﻭﻗﻠﻮﺋﻲ ﻭ Small-for-date , large-for-dataﻭ .... ﺩﺭ ﺑﺨﺶﻫﺎﻱ ﺩﻳﮕﺮ ﻫﺮ ﺳﻴﺴﺘﻢ ﺑﺪﻥ ﺍﺯ ﻟﺤﺎﺽ ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ،ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ،ﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﻳﺎﻓﺘﻪﻫﺎ ﺑﻪ ﻧﺮﻣﺎﻝ ﻭ ﻏﻴﺮﻧﺮﻣﺎﻝ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ،ﺗﺸﺨﻴﺺ ﻳﺎﻓﺘﻪ ﻭ ﺭﺳﻴﺪﻥ ﺑﻪ ﻳﻚ ﺗﺸﺨﻴﺺ ﺑﺎﻟﻴﻨﻲ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ -١٩ﺩﺳﺘﮕﺎﻩ ﮔﻮﺍﺭﺵ )ﺣﻔـﺮﻩ ﭘﺮﻳﺘﻮﺍﻥ( -٢٠ﺍﺭﺯﻳﺎﺑﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺍﻋﻀﺎﺀ ﭘﻴﻮﻧﺪ ﺯﺩﻩ ﺷﺪﻩ )ﻛﺒﺪ – ﻛﻠﻴﻪ -ﭘﺎﻧﻜﺮﺍﺱ( -٢١ﻛﺒﺪ -٢٢ﻛﻴﺴﻪ ﺻﻔﺮﺍ ﻭ ﻣﺠـﺎﺭﻱ ﺻـﻔﺮﺍﻭﻱ -٢٣ﺭﺗﺮﻭﭘﺮﺗﻴـﻮﺍﻥ ﻭ ﭘـﺎﻧﻜﺮﺍﺱ ،ﻃﺤـﺎﻝ ،ﻟﻤـﻒ ﻧـﻮﺩ -٢٤ﺩﺳـﺘﮕﺎﻩ ﺍﺩﺭﺍﺭﻱ -٢٥ﭘﺮﻭﺳـﺘﺎﺕ -٢٧ Penis -٢٦ﺍﺳـﻜﺮﻭﺗﻮﻡ ﻭ testes -٣٠ Post meno Pausal Pelvis -٢٩ Female Pelvis -٢٨ﺳﻴﺴــﺘﻢ ﻋــﺮﻭﻕ ﻣﺤﻴﻄــﻲ -٣١ﻛﺎﺭﻭﺗﻴــﺪ -٣٥ Chest -٣٤ Brest -٣٣ trans cranial -٣٢ﺗﻴﺮﻭﺋﻴــﺪ ،ﭘﺎﺭﺍﺗﻴﺮﻭﺋﻴــﺪ ﻭ ﻏــﺪﺩ ﺩﻳﮕــﺮ -٣٦ﺳﻴﺴــﺘﻢ Skeletalﻭ Pediactric Head -٣٧ Softtissue -٤١ ultrasound-Guided Percutaneous tissue Ablation -٤٠ Three dimensional ultrasound -٣٩ Ultrasoud Contrast agent -٣٨ﺍﻭﻟﺘﺮﺍﺳﻮﻧﺪﺍﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﻻﺯﻡ ﺑﻪ ﺫﻛﺮ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻫﻨﮕﺎﻡ ﻧﺼﺐ ﺍﻳﻦ CDﺑﺎﻳﺴﺘﻲ ﺍﺯ ﻛﺪ ﻋﺒﻮﺭ RUSR 2335ﺍﺳﺘﻔﺎﺩﻩ ﺷﻮﺩ. )25.1 Diagnostic Ultrasound of Fetal Anomalies: Principles and Techniques (CD I,II
1999
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺷﻲ ﺩﺍﺭﺍﻱ ٢ﻋﺪﺩ CDﻣﻲﺑﺎﺷﺪ .ﺩﺭ CDﺷﻤﺎﺭﻩ ١ﺑﺎ ﺑﻬﺮﻩﮔﻴﺮﻱ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺛﺎﺑﺖ ﻭ ﻣﺘﺤﺮﻙ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺟﻨﻴﻦ ﻛﻪ ﺩﺍﺭﺍﻱ ﻛﻴﻔﻴﺖ ﻓﻮﻕﺍﻟﻌﺎﺩﻩ ﻋﺎﻟﻲ ﻣﻲﺑﺎﺷﻨﺪ ،ﺁﻧﻮﻣﺎﻟﻲﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻣﺎﺩﺭﺯﺍﺩﻱ ﺑﺼﻮﺭﺕ ﺗﻴﭙﻴﻚ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻳﻚ ،ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ CDﺷﻤﺎﺭﻩ ، ٢ﺍﻣﻜﺎﻥ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﺷﺨﺺ ﺑﻪ ﺻﻮﺭﺕ Caseﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻭ ﺑﻪ ﻃﺮﻳﻘﺔ Multiple Choice questionﻓﺮﺍﻫﻢ ﮔﺮﺩﻳﺪﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ، Caseﺗﻮﺿﻴﺤﺎﺕ ﻻﺯﻡ ﺩﺍﺩﻩ ﺷﺪﻩﺍﻧﺪ .ﻣﺒﺎﺣﺚ ﻭ ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ ٢ﻋﺪﺩ CDﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﻣﻲﺑﺎﺷﻨﺪ: ﻣﺒﺤﺚ ﻣﺒﺤﺚ ﻣﺒﺤﺚ ﻣﺒﺤﺚ ﻣﺒﺤﺚ ﺗﻌﺪﺍﺩ Case ﺗﻌﺪﺍﺩ Case ﺗﻌﺪﺍﺩ Case ﺗﻌﺪﺍﺩ Case ﺗﻌﺪﺍﺩ Case Headﺟﻨﻴﻦ ٣٦ ١٩ ٢ ﺟﻨﺴﻴﺖ ٤ ﺟﻨﻴﻦ ﺍﺳﻜﺘﺎﻝ ﺳﻴﺴﺘﻢ ١٦ Neural tube Amniotic Fluid ٢٠ ٣ ﻣﻮﺍﺭﺩ ﻣﺘﻔﺮﻗﻪ ٢ ﺩﺳﺘﮕﺎﻩ ﺍﺩﺭﺍﺭﻱ ﺟﻨﻴﻦ ١٢ Body wall Umblical Cord ﻗﻠﺐ ﺟﻨﻴﻦ ١٤ ﺻﻮﺭﺕ ﺟﻨﻴﻦ ٦ Chestﺟﻨﻴﻦ ١٢ ﺳﻴﺴﺘﻢ ﮔﻮﺍﺭﺷﻲ ﺟﻨﻴﻦ ٤ ــــــ
)26.1 EBUS (Endo Bronchial Ultrasound
2004
)27.1 Endoscopy and Gastrointestinal Radiology (Gregory G. Ginsberg, Michael L. Kochman Colonoscopy
Upper endoscopy
Percutaneous Management of Biliary Obstruction
Clinical Application of Magnetic Resonance Imaging in the Abdomen
Contrast Radiology
Endoscopiy Endoscopic Ultrasound
Computed Tomography and Ultrasound of the Abdomen and Gastrointestinal Tract
Endoscopic Retrograte Cholagiopancreatography
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
5 28.1 Essentials of Radiology
ــــــ
ﺩﺭ CDﻓﻮﻕ ،ﺿﺮﻭﺭﻳﺎﺕ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺗﺸﺨﻴﺼﻲ ﺑﺼﻮﺭﺕ Caseﻣﻄﺮﺡ ﮔﺮﺩﻳﺪﻩﺍﻧﺪ ﻭ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺗﻴﭙﻴﻚ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﻭ ﺗﻮﺻﻴﻒ ﺩﻗﻴﻖ ﻧﻤﺎﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ CDﺑﺮ ﺣﺴﺐ ﻣﻮﺿﻮﻉ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﺪﺍﺩ Case
ﻣﻮﺿﻮﻉ
ﺗﻌﺪﺍﺩ Case
ﻣﻮﺿﻮﻉ
٢٠ ١٦ ١ ١٣ ٢٨ ١٢
ﻣﺮﺍﻗﺒﺖ ﺑﺤﺮﺍﻧﻲ ﻛﻮﻟﻮﻥ ﻭ ﻧﺎﺣﻴﻪ LLQﺷﻜﻢ ﻣﻄﺎﻟﻌﺎﺕ ﻓﻠﻮﺭﻭﺳﻜﻮﭘﻴﻚ ﺷﻜﻢ ﺳﻴﺴﺘﻢ ﺍﺩﺭﺍﺭﻱ ﺗﻨﺎﺳﻠﻲ ﺳﻴﺴﺘﻢ ﺍﺳﻜﻠﺘﺎﻝ ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻣﻐﺰ
١٥ ٧ ٧ ٧ ٥ ٣
ﻧﺎﺣﻴﻪ RLQﺷﻜﻢ ﺭﻭﺓ ﺑﺎﺭﻳﻚ ﻗﻠﺐ ﮊﻧﻴﻜﻮﻟﻮﮊﻱ ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
TB
ﺗﻌﺪﺍﺩ Case
ﻣﻮﺿﻮﻉ
ﺗﻌﺪﺍﺩ Case
٨ ١٢ ٦ ١٢ ١٧ ١٨
ﺍﻧﺴﺪﺍﺩ ﻭ ﭘﺮﻓﻮﺭﺍﺳﻴﻮﻥ ﻧﺎﺣﻴﻪ RUQﺷﻜﻢ ﻣﻌﺪﻩ
٣٠ ١٢ ٦ ٩ ١٨ ١٦ ١٣
AIDS
ﺗﺮﻭﻣﺎ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ Breast
ﻣﻮﺿﻮﻉ
ﭘﻨﻮﻣﻮﻧﻲ ﻛﺎﻧﺴﺮ ﺭﻳﻪ ﻣﺮﻱ ﭘﻨﻮﻣﻮﻛﻮﻧﻴﻮﺯ ﺍﻃﻔﺎﻝ obstetrics
ﭘﺰﺷﻜﻲ ﻫﺴﺘﻪﺍﻱ
ــــــ
)29.1 Exam Preparation for Diagnostic Ultrasound Abdomen and OB/GYN (RogerC. Sanders, Jann D. Dolk, Nancy Smith Miner
ــــــ
)30.1 Image Data Bank RADIOGRAPHIC ANATOMY & POSITIONING (APPLETON & LANGE
1998
31.1 Imaging Atlas of Human Anatomy
)(Mosby
)(version 2.0
ﺑﺎ ﻛﻤﻚ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻗﺎﺩﺭ ﺧﻮﺍﻫﻴﺪ ﺑﻮﺩ ﻛﻪ ﺩﺭ ﻣﺪﺕ ﺑﺴﻴﺎﺭ ﻛﻮﺗﺎﻫﻲ ﺑﺎ ﺁﻧﺎﺗﻮﻣﻲ ﺑﺪﻥ ﺩﺭ ﺗﺼﺎﻭﻳﺮ ﻣﺨﺘﻠﻒ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ )ﻓﻴﻠﻢﻫﺎﻱ ﺳﺎﺩﻩ ،ﺗﺼﺎﻭﻳﺮ ﺑﺎ ﻛﻨﺘﺮﺍﺳـﺖ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴـﻚ MRI ، CT Scan ،ﻭ ﺳـﻮﻧﻮﮔﺮﺍﻓﻲ( ﺁﺷـﻨﺎ ﺷـﻮﻳﺪ .ﺭﻭﺵ ﻳـﺎﺩﮔﻴﺮﻱ ﺁﻧـﺎﺗﻨﻮﻣﻲ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ CDﺑﺴﻴﺎﺭ ﺁﺳﺎﻥ ﺑﻮﺩﻩ ﻭ ﺍﻣﻜﺎﻧﺎﺕ ﻣﺨﺘﻠﻔﻲ ﺍﺯ ﻗﺒﻴﻞ ﺑﺰﺭﮒﻧﻤﺎﻳﻲ ﺗﺼﻮﻳﺮ negative ،ﻛﺮﺩﻥ ﺗﺼﻮﻳﺮ ،ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﻭ ...ﺟﻬﺖ ﺍﻳﺠﺎﺩ ﻋﻼﻗﻤﻨﺪﺍﻥ ﺑﻴﺸﺘﺮ ﺩﺭ ﺍﻣﺮ ﻳﺎﺩﮔﻴﺮﻱ ﺩﺭ ﻧﻈﺮ ﮔﺮﻓﺘﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺿﻤﻨﹰﺎ ﺑﺎ ﺍﺳـﺘﻔﺎﺩﻩ ﺍﺯ ﺁﺭﺍﻳـﺔ ، noteﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺍﻃﻼﻋﺎﺕ ﻋﻠﻤﻲ ﺍﺿﺎﻓﻲ ﻣﺮﺗﺒﻂ ﺑﺎ ﺗﺼﻮﻳﺮ ﻣﻮﺭﺩ ﻣﻄﺎﻟﻌﻪ ﺩﺳﺘﻴﺎﺑﻲ ﭘﻴﺪﺍ ﻧﻤﻮﺩ. 1998
)32.1 Imaging of Diffuse Lung Disease (David A. Lynch, MB, John D. Newell Jr, MD, FCCP, Jin Seong Lee, MD
CDﺣﺎﺿﺮ ﺷﺎﻣﻞ ١١ﻓﺼﻞ ﺍﺯ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﻨﺘﺸﺮ ﺭﻳﻪ ) (DLNﻣﻲﺑﺎﺷﺪ .ﻛﻪ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﺷﺎﻣﻞ ﺗﻠﻔﻴﻘﻲ ﺍﺯ ﻣﻌﺎﻳﻨﻪ ،ﺷﺮﺡ ﺣﺎﻝ ،ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ ﺗﻔﺴﻴﺮ ﻋﻜﺲﺑﺮﺩﺍﺭﻱ ) MRI,CT-Xrayﻭ (....ﺩﺭ ﺍﻃﻔﺎﻝ ﻭ ﺑﺎﻟﻐﻴﻦ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫـﺎﻱ ﻣﻨﺘﺸـﺮ ﺭﻳﻪ ﻣﻲﺑﺎﺷﺪ. ﺑﻌﻀﻲ ﻓﺼﻮﻝ ﻛﺘﺎﺏ ﺷﺎﻣﻞ : ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ DLDﻛﻮﺩﻛﺎﻥ ﺗﺼﻮﻳﺮ ﺑﺮﺩﺍﺭﻱ ﻋﺮﻭﻕ ﺭﻳﻮﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻧﻔﻴﻠﺘﺮﺍﺗﻴﻮ ﺭﻳﻪ
ﭘﻴﻮﻧﺪ ﺭﻳﻪ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺁﻣﻔﻴﺰﻡ
ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﻐﻠﻲ ﻭ ﻣﺤﻴﻄﻲ ﻭDLD
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺭﺍﻫﻬﺎﻱ ﻫﻮﺍﺋﻲ
ﺍﺭﺯﻳﺎﺑﻲ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺑﻴﻤﺎﺭﻫﺎﻱ ﺭﻳﻪ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ DLDﻭ ﻣﻘﺎﻳﺴﻪ X-Ray,CTﺁﻧﻬﺎ ﺑﻪ ﻃﻮﺭ ﻣﺠﺰﺍ ﻣﻲﺑﺎﺷﺪ
ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ ﺑﺮﻧﺎﻣﻪ Acrobat Readerﺑﻮﺩﻩ ﻭ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﻧﮕﺎﻫﻲ ﺟﺪﻳﺪ ﺑﻪ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎﻱ ﺩﺍﺧﻠﻲ ،ﺭﻳﻪ ،ﻗﻠﺐ ﻭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻣﻲﺩﻫﺪ. ___
)33.1 Imaging of Spinal Trauma in Children (Lawrence R. Kuhns, M.D.) (University of Michigan Medical Center
ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ:
ATLAS OF SPINAL INJURIES IN CHILDREN Cervcal Spine Lumbar Spine Thoracic Spine Sacrococcygeal Spine Lumbar
ــــــ
Special Views and Techniques Experimental and Necropsy Data Sacral Injuries
Principles AND TECHNIQUES Normal Spine Variants and Anatomy Mechanisms and Patterns of Injury Thoracic Spine Injuries
Epidemiology Measurements Occipitocervical Injuries
)34.1 MAGNETIC RESONANCE IMAGING (Third Edition) (Dauld Stark, William Bradley
ﺳﻪ ﺟﻠﺪ ﻛﺘﺎﺏ David Starkﺩﺭ ﺍﻳﻦ CDﻣﻮﺟﻮﺩ ﻣﻴﺒﺎﺷﺪ.
2. Magnetic Resonance: Bioeffects and Safety
1. Generation and Manipulation of Magnetic Resonance Images
4. Principles of Echo Planar Imaging: Implications for Musculoskeletal System
3. Three-Dimensional Magnetic Resonance Rendering Technique
6. The Hip
5. MR Imaging of Articular Cartilage and of Cartilage Degneration
12. The Temporomandibular Joint
9. The Shoulder
8. The Ankle and Foot 13. Kinematic Magnetic Resonance Imaging 14. The Spine
7. The Knee
11. The Wrist and hand
10. The Elbow
15. Marrow Imaging 16. Bone and Soft-Tissue Tumors 17. Magnetic Resonance Imaging of Muscle Injuries
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
6 )35.1 Magnetic Resonance Imaging in Orthopedics and Sport Medicine (David W. Stoller
ــــــ
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻛﺎﺭﺑﺮﺩ MRIﺩﺭ ﺍﺭﺗﻮﭘﺪﻱ ﻭ ﻃﺐ ﻭﺭﺯﺵ ﻣﻲﺑﺎﺷﺪ ﻭ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖ: -١٦ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻥ ﻭ ﺑﺎﻓﺖ ﻧﺮﻡ MRI -١٧ﺁﺳﻴﺒﻬﺎﻱ ﻋﻀﻼﻧﻲ
-١١ﺗﻜﻨﻴﻚ ﺑﺎﺯﺳﺎﺯﻱ ﺟﻬﺖ MRIﺳﻪﺑﻌﺪﻱ -١٢ﻣﻔﺼﻞ ﺭﺍﻥ )(Hip -١٣ﺷﺎﻧﻪ -١٤ﻣﻔﺼﻞ ﻛﻤﭙﻮﺭﻭﻣﺎﻧﺪﻳﺒﻮﻻﺭ )(TMJ -١٥ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ MRIﺍﺯ ﻣﻐﺰ ﺍﺳﺘﺨﻮﺍﻥ
-٦ﺍﺛﺮﺍﺕ ﺑﻴﻮﻟﻮﮊﻳﻚ ﻭ ﺍﻳﻤﻨﻲ ﺩﺭ MRI
-١ﺗﻬﻴﺔ ﺗﺼﺎﻭﻳﺮ MRI
MRI -٧ﻋﻀﺮﻭﻑ ﻣﻔﺼﻠﻲ ﻭ ﺩﮊﻧﺮﺍﺳﻴﻮﻥ ﻋﻀﺮﻭﻓﻲ -٨ﻣﭻ ﭘﺎ ﻭ ﭘﺎ -٩ﻣﭻ ﺩﺳﺖ ﻭ ﺩﺳﺖ -١٠ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
-٢ﺍﺻﻮﻝ ﺗﺼﻮﻳﺮﺳﺎﺯﻱ Echo-Planarﺟﻬﺖ ﺳﻴﺴﺘﻢ ﻣﻮﺳﻜﻮﻟﻮﺍﺳﻜﻠﺘﺎﻝ -٣ﺯﺍﻧﻮ -٤ﺁﺭﻧﺞ Kinematic MRI -٥
2000
)(Ralphl. Smathers, M.D.
ﺩﺭ ﺍﻳﻦ CDﻣﻄﺎﻟﺒﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﺎﻣﻮﮔﺮﺍﻓﻲ ﺑﺎ ﻋﻨﺎﻭﻳﻦ ﺫﻳﻞ ﻣﻄﺮﺡ ﺷﺪﻩ ﺍﺳﺖ: ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ﭘﺴﺘﺎﻥ ﺗﻐﻴﻴﺮﺍﺕ ﺯﻣﺎﻥ ﻭ ﺁﺭﺗﻔﻜﺖﻫﺎ -ﺭﻭﺵﻫﺎﻱ ﺍﻧﺠﺎﻡ ﻣﺎﻣﻮﮔﺮﺍﻓﻲ )ﺑﻪ ﺻﻮﺭﺕ ﻟﻮﻛﺎﻟﻴﺰﻩ ﺑﺎ Needleﻭ ﻳﺎ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ(
ﺗﻐﻴﻴﺮﺍﺕ ﻓﻴﺒﺮﻭﻛﻴﺴﺘﻴﻚ ﻭ ﺗﻮﺩﻩﻫﺎﻳﻲ ﺑﺎ ﺣﺪﻭﺩ ﻣﺸﺨﺺ ﻭ ﺧﻮﺵﺧﻴﻢ -ﺑﺮﺭﺳﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﻴﺸﺮﻓﺘﻪ ﻭ ﻣﺘﺎﺳﺘﺎﺯ ﻭ ﻫﻤﭽﻨﻴﻦ ﺩﺭ ﻣﻮﺭﺩ ﺭﺍﺩﻳﻮﺗﺮﺍﭘﻲ
2001 Aortic Coarcation Miscellaneous
2001 ــــــ
Aortic Arch Anomalies Congenital venous anomalies
Aortic Arch Anomalies Aequised venous diseases
36.1 Mammography Diagnosis and Intervention
-ﺗﻮﺩﻩﻫﺎﻳﻲ ﺑﺎ ﺣﺪﻭﺩ ﻧﺎﻣﺸﺨﺺ ﻭ ﺗﻮﻣﻮﺭﻫﺎﻱ ﺑﺪﺧﻴﻢ ﻭ Aggressive
)37.1 MR Angiography Thoracic Vessels (O. Ratib & D. Didier Methods & Techniques Aortic Aneurysms Aortitis Pulmonary astesies diseases )38.1 MR Imagin Expert (Geir Torhim, Peter A. Rinck
4th Edition "This version is a special adaptation for "Magnetic Resonance in Medicine The Basic Textbook of the European Magnetic Redonance Forum )39.1 MRI of the BRAIN & SPINE (SCOT W. ATLAS) (LIPPINCOTT-ROVEN ﺍﻳﻦ CDﻳﻚ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺷﻲ ﭼﻨﺪﻣﻨﻈﻮﺭﻩ ﺑﻪ ﺣﺴﺎﺏ ﻣﻲﺁﻳﺪ ﺯﻳﺮﺍ ﺩﺭ ﺁﻥ ،ﻋﻼﻭﻩ ﺑﺮ ﺗﻮﺿﻴﺤﺎﺕ ﻻﺯﻡ ﻭ ﺩﺭ ﻋﻴﻦ ﺣﺎﻝ ﻣﺨﺘﺼﺮ ﺩﺭ ﻣﻮﺭﺩ ﻓﻴﺰﻳﻚ ﻭ ﺍﺻﻮﻝ MRIﻭ ﻫﻤﭽﻨﻴﻦ ﺗﻜﻨﻴﻜﻬﺎﻱ ﻣﺮﺑﻮﻃﻪ ،ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻣﺒﺤﺚ ﺑﺎﻟﻴﻨﻲ ﻧﻴﺰ ﺩﺭ ﻃﻲ ٣٢ﻓﺼﻞ ﺑﻪ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻳﺎﻓﺘﻪﻫﺎﻱ Imagingﭘﺮﺩﺍﺧﺘﻪ ﺷﺪﻩ ﻭ ﺑﻴﺶ ﺍﺯ ٤٠٠٠ﺗﺼﻮﻳﺮ MRIﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺑﺮﺣﺴﺐ ﻣﻮﺭﺩ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﺍﺳﺖ .ﺿﻤﻨﹰﺎ ﺑﺮﺍﻱ ﻓﻬﻢ ﺑﻬﺘﺮ ﻣﻄﺎﻟﺐ ،ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻫﺮ ﻣﻮﺿﻮﻉ ﺑﺎﻟﻴﻨﻲ ﻭ ﻳﺎ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺍﺯ ﺟﺪﺍﻭﻝ ﻣﻔﻴﺪ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻗﺴﻤﺖ ﺁﻧﺎﺗﻮﻣﻲ ﻧﻴﺰ ،ﻧﻮﺭﻭﺁﻧﺎﺗﻮﻣﻲ ﺑﻪ ﺻﻮﺭﺕ Sectionalﻭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺳﻪ ﺭﻭﺵ )ﺗﺼﺎﻭﻳﺮ ﺷﻤﺎﺗﻴﻚ +ﺗﺼﺎﻭﻳﺮ ﻃﺒﻴﻌﻲ +ﺗﺼﺎﻭﻳﺮ (MRIﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻧﻜﺘﺔ ﺑﺴﻴﺎﺭ ﺟﺎﻟﺐ ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ،ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﻣﻄﺎﻟﺐ ﻣﻄﺎﻟﻌﻪ ﺷﺪﻩ ﺑﻮﺳﻴﻠﻪ Caseﻫﺎﻱ ﻣﺘﻌﺪﺩ ﺍﺳﺖ ﻛﻪ ﺑﺮﺣﺴﺐ ﻣﻮﺿﻮﻉ ،ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡ ﺷﺪﻩ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡ ﺷﺪﻩ ٥ ٦ ٦ ٦ ٦ ٥ ٣ ٥ ٤ ٥
ﻣﻮﺿﻮﻉ ﺧﻮﻧﺮﻳﺰﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﻳﻨﺎﻝ ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﻛﺴﺘﺮﺍﺁﮔﺰﻳﺎﻝ ﻣﻐﺰ ﺍﻳﺴﻜﻤﻲ ﻭ ﺁﻧﻔﺎﺭﻛﺘﻮﺱ ﻣﻐﺰﻱ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺎﺩﺓ ﺳﻔﻴﺪ ﺗﻈﺎﻫﺮﺍﺕ ﺳﻴﺴﺘﻢ ﺍﻋﺼﺎﺏ ﻣﺮﻛﺰﻱ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻓﺎﻛﻮﻣﺎﺗﻮﺭﻫﺎ ﺳﻼﺗﻮﺭﺳﻴﻜﺎ ﻭ ﻧﺎﺣﻴﻪ ﭘﺎﺭﺍﺳﻼﺭ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻥ ﻛﻤﭙﻮﺭﺍﻝ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﮊﻧﺮﺍﻳﺘﻮ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻋﻔﻮﻧﻲ ﻭ ﺍﻟﺘﻬﺎﺑﻲ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻧﺌﻮﭘﻼﺳﺘﻴﻚ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻭ ﻧﺨﺎﻉ
ﺗﻌﺪﺍﺩ Caseﻫﺎﻱ ﻣﻄﺮﺡ ﺷﺪﻩ ٧ ٦ ٦ ٥ ٥ ٤ ٥ ٦ ٣ ٣ ٢
ﻣﻮﺿﻮﻉ ﺍﺧﺘﻼﻻﺕ ﺗﻜﺎﻣﻠﻲ ﻣﻐﺰ ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﺁﮔﺰﻳﺎﻝ ﻣﻐﺰ ﻣﺎﻟﻔﻮﺭﻣﺎﺳﻴﻮﻧﻬﺎﻱ ﻋﺮﻭﻗﻲ ﻭ ﺁﻧﻮﺭﻳﺴﻢﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻳﻨﺎﻝ ﺗﺮﻭﻣﺎﻱ ﺳﺮ ﻋﻔﻮﻧﺖﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻳﻨﺎﻝ Agingﻣﻐﺰ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻧﻮﺭﻭﺩﮊﻧﺮﺍﻳﺘﻮ ﻗﺎﻋﺪﺓ ﺟﻤﺠﻤﻪ ﺍﻭﺭﺑﻴﺖ ﻭ ﺳﻴﺴﺘﻢ ﺑﻴﻨﺎﻳﻲ ﺗﺮﻭﻣﺎﻱ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺁﻧﺎﻣﺎﻟﻴﻬﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻭ ﻧﺨﺎﻉ ﺍﺧﺘﻼﻻﺕ ﻋﺮﻭﻕ ﻧﺨﺎﻋﻲ
ــــــ
40.1 MRI der Extremitaten
2000
)41.1 Normal Findings in CT and MRI (Torsten B Moeller, Emil Reif) (Thieme
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
7 20.3 Obstetric Ultrasound Principles and Techniques
ــــــ
ﺩﺭ ﺍﻳﻦ CDﻣﻄﺎﻟﺐ ﺟﺎﻣﻊ ﻭ ﺍﺭﺯﻧﺪﻩﺍﻱ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﻬﺎﺭﺕﻫﺎﻱ ﻻﺯﻣﻪ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻣﺎﻣﺎﺋﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﻛﻪ ﻋﻨﺎﻭﻳﻦ ﺁﻥ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﻴﻴﻦ ﺳﻦ ﺣﺎﻣﻠﮕﻲ ﺑﺮ ﺍﺳﺎﺱ ﻣﻌﻴﺎﺭﻫﺎﻱ FL . BPDﻭ ACﻭ HCﻭ ﺟﺪﺍﻭﻝ ﺁﻧﻬﺎ ﺑﺮﺭﺳﻲ ﺁﻧﺎﺗﻮﻣﻲ ﺟﻨﻴﻦ ﻭ ﺁﻧﻮﻣﺎﻟﻲﻫﺎﻱ CNSﻭ Body ﺁﻧﺎﺗﻮﻣﻲ ﺭﺣﻢ ﻭ ﺁﺩﻧﻜﺲﻫﺎ ﻭ ﺍﻣﺒﺮﻳﻮ ﻭ ﻛﻴﺴﻪ ﺯﺭﺩﻩ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺑﺮ ﺍﺳﺎﺱ Gsﻭ CRLﻭ ﻧﺤﻮﺓ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻧﻬﺎ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ ﺑﺮ ﺍﺳﺎﺱ ﺩﻭﺭ ﺳﺮ ﻭ ﻧﺤﻮﻩ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻥ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ ﺑﺮ ﺍﺳﺎﺱ FLﻭ ACﻭ ﻧﺤﻮﻩ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻧﻬﺎ ﺗﻌﻴﻴﻦ ﻣﺤﻞ ﺟﻔﺖ ﻭ ﺣﺠﻢ ﻣﺎﻳﻊ ﺁﻣﻨﻴﻮﺗﻴﻚ ﻣﻄﺎﻟﺐ ﺟﺎﻟﺒﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺁﻧﺎﺗﻮﻣﻲ ﺟﻨﻴﻦ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ )ﻣﻌﺪﻩ -ﻛﻠﻴﻪ (........ ﺗﻌﻴﻴﻦ ﻣﺤﻞ ﻻﻧﻪﮔﺰﻳﻨﻲ ﺟﻔﺖ ﻭ ﺑﺮﺭﺳﻲ ﺭﻛﻮﻟﻤﺎﻥ ﻭ ﭘﻼﻧﺘﺎﭘﺮﻭﻳﺎ ﺍﻧﻔﺎﺭﻛﺘﻮﺱ ﻭ ﻭﺍﺭﻳﺎﺳﻴﻮﻥ ﻣﺤﻞ ﺧﺮﻭﺝ ﺑﻨﺪ ﻧﺎﻑ )(Cord Insertion ﺑﺮﺭﺳﻲ ﻟﻜﻴﻨﻴﻜﺎﻝ ﻭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ Case Studyﻭ ﻣﻄﺮﺡﻛﺮﺩﻥ ﺳﺆﺍﻻﺕ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺁﻧﻬﺎ ﻭ ﭘﺎﺳﺦ ﻣﺮﺑﻮﻃﻪ ﺗﻮﺿﻴﺤﺎﺗﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ) BPPﺑﻴﻮﻓﻴﺰﻳﻜﺎﻝ ﭘﺮﻭﻓﺎﻳﻞ(ــــــ
)(DAVID A. STRINGER, PAUL S. BABYN, MDCM
)(Second Edition
42.1 PEDIATRIC GASTROINTESTINAL IMAGING AND INTERVENTION
)43.1 Peripheral Musculoskeletal Ultrasound Interactive Atlas A CD-ROM (J. E. Cabay, B. Daenen) (R. F. Dondelinger
ــــــ
ﺁﻣﻮﺯﺵ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ MusculoSkeletalﻣﺤﺴﻮﺏ ﻧﻤﻮﺩ ﭼﺮﺍ ﻛﻪ ﺑﺎ ﻛﻤﻚ ﺗﺼﺎﻭﻳﺮ ﺛﺎﺑﺖ ﻭ ﻣﺘﺤﺮﻙ ﻣﺘﻌﺪﺩ ﻭ ﺗﻴﭙﻴﻚ ،ﺷﻤﺎ ﺭﺍ ﺑﻪ ﺧﻮﺑﻲ ﺑﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻻﺯﻡ ﺟﻬﺖ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻧﺴﻮﺝ ﻧﺮﻡ ﺳﻄﺤﻲ ﻭ ﺗﺼﺎﻭﻳﺮ ﻧﺮﻣﺎﻝ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱﻫﺎﻱ ﺍﻳﻦ ﺳﻴﺴﺘﻢ ﺁﺷﻨﺎ ﻣﻲﺳﺎﺯﺩ ﻭ ﺿـﻤﻨﹰﺎ ﺍﻣﻜـﺎﻥ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ) (Quizﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻓﺮﺍﻫﻢ ﺍﺳﺖ .ﺩﺭ ﻣﻨﻮﻱ ﺍﻳﻦ CDﺷﻤﺎ ﺑﺮﺍﻱ ﺑﺮﺭﺳﻲ ﺗﺼﺎﻭﻳﺮ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﻧﺮﻣﺎﻝ ﻭ ﻳﺎ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﺩﺭ ﺳﻴﺴﺘﻢ ﻣﻮﺳﻜﻮﻟﻮ ﺍﺳﻜﻠﺘﺎﻝ ﺍﺯ ﺩﻭ ﺷﻴﻮﺓ ﻣﺨﺘﻠﻒ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺑﻬﺮﻩﻣﻨﺪ ﺷﻮﻳﺪ: ﺍﻟﻒ -ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻨﻮﻱ :Generalﻛﻪ ﺩﺭ ﺍﻳﻦ ﺻﻮﺭﺕ ﺷﻤﺎ ﻳﻜﻲ ﺍﺯ itemﻫﺎﻱ ﺯﻳﺮ ﺭﺍ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﺋﻴﺪ: -١٠ﭘﻮﺳﺖ
-٩ﻋﺼﺐ
-٨ﻋﺮﻭﻕ
-٧ﻏﻀﺮﻭﻑ ﻓﻴﺒﺮﻭ
-٦ﻏﻀﺮﻭﻑ ﻫﻴﺎﻟﻴﻦ
-٥ﻛﭙﺴﻮﻝ ﻣﻔﺼﻠﻲ ﻭ ﺑﻮﺭﺱ
-٣ﻟﻴﮕﺎﻣﺎﻥ
-٤ﺍﺳﺘﺨﻮﺍﻥ ﻭ ﭘﺮﻳﻮﺳﺖ
-٢ﺗﺎﻧﺪﻭﻥ
-١ﻋﻀﻠﻪ
ﺏ -ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻨﻮﻱ :Regionﻛﻪ ﺩﺭ ﺍﻳﻦ ﺻﻮﺭﺕ ﺷﻤﺎ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻳﻜﻲ ﺍﺯ itemﻫﺎﻱ ﺯﻳﺮ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﺋﻴﺪ: 1- Ankle
2- Elbow
3- Foot
4- Hand
5- Hip
6- Knee
7- Shoulder
ــــــ 2002 ــــــ
8- Wrist
44.1 Principles of MRI
)(Jeery Papp) (Mosby )(UNIVERSITY OF FLORIDA COLLEGE OF MEDICINE DEPARTMENT OF RADIOLOGY
45.1 Quality Management in the Imaging sciences
Interactive Tutorial on Normal Radiology
46.1 RADIOLOGIC ANATOMY
ﻼ ﺍﮔﺮ ﻣﻲﺧﻮﺍﻫﻴﻢ ﺩﺭ ﻣﻮﺭﺩ (Lower Extremityﺍﻃﻼﻋﺎﺕ ﺁﻧﺎﺗﻮﻣﻴﻚ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺑﺪﺳﺖ ﺁﻭﺭﻳﻢ ﺑﺮ ﺭﻭﻱ ﺍﻧـﺪﺍﻡ ﺗﺤﺘـﺎﻧﻲ ﺷـﻜﻞ ﻣـﺬﻛﻮﺭ ﺑﺮﺍﻱ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ، CDﺍﺑﺘﺪﺍ ﺑﺎﻳﺪ ﺑﺮ ﺭﻭﻱ ﻗﺴﻤﺖ ﻣﻮﺭﺩ ﻧﻈﺮ ﺑﺮ ﺭﻭﻱ ﺷﻜﻞ ﺍﻧﺴﺎﻥ )ﺩﺭ ﻛﺎﺩﺭ ﺳﻤﺖ ﺭﺍﺳﺖ( Clickﺷﻮﺩ )ﻣﺜ ﹰ Clickﻣﻲﻛﻨﻴﻢ( ،ﺳﭙﺲ ﺩﺭ ﻛﺎﺩﺭ ﺳﻤﺖ ﭼﭗ ﻟﻴﺴﺖ ﻗﺴﻤﺖﻫﺎﻱ ﻛﻠﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﻧﺎﺣﻴﻪ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻣﻮﺭﺩ ﻣﻄﺎﻟﻌﻪ ﻇﺎﻫﺮ ﻣﻲﺷﻮﺩ ﻭ ﻣﺎ ﻣﻲﺗﻮﺍﻧﻴﻢ ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﻗﺴﻤﺖﻫﺎﻱ ﻛﻠﻲ ،ﻭﺍﺭﺩ ﺟﺰﺋﻴﺎﺕ ﺑﻴﺸﺘﺮ ﺁﻥ ﺷﻮﻳﻢ .ﺿﻤﻨﹰﺎ ﺩﺭ ﻗﺴﻤﺖ ﭘﺎﻳﻴﻦ ﻛﺎﺩﺭﻫـﺎﻱ ﻓـﻮﻕ ،ﺳـﻪ ﻋـﺪﺩ Iconﻛﺎﺭﺑﺮﺩﻱ ﺩﺭ ﻗﺴﻤﺖ ﻭﺳﻂ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﺑﺎ ﻛﻤﻚ ﺁﻧﻬﺎ ﻣﻲﺗﻮﺍﻥ ﺑﺘﺮﺗﻴﺐ ﺍﺯ ﺗﻜﻨﻴﻚ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﻗﺴﻤﺖ ﻣﻮﺭﺩ ﻧﻈﺮ ،ﺁﻧﺎﺗﻮﻣﻲ ﻃﺒﻴﻌﻲ ﻗﺴﻤﺖ ﻣﺬﻛﻮﺭ ﻭ ﻫﻤﭽﻨﻴﻦ ﻣﺴﺎﺋﻞ ﻛﻠﻴﻨﻴﻜﻲ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﻋﻀـﻮ ﻣـﻮﺭﺩ ﻣﻄﺎﻟﻌـﻪ ﺁﮔـﺎﻫﻲ ﻛﺎﻣـﻞ ﻳﺎﻓـﺖ .ﺿـﻤﻨﹰﺎ ﺍﻣﻜـﺎﻥ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ) (Self evaluationﺑﺮ ﺍﺳﺎﺱ ﻣﺒﺎﺣﺚ ﻣﻮﺭﺩ ﻧﻈﺮ ﻭﺟﻮﺩ ﺩﺍﺭﺩ .ﻧﻜﺘﺔ ﻗﺎﺑﻞ ﺗﻮﺟﻪ ﺩﺭ ﺍﻳﻦ ، CDﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻛﻠﻴﺔ ﺭﻭﺵﻫﺎﻱ ) Imagingﺍﺯ ﻗﺒﻴﻞ ، Plain Filmﻣﻄﺎﻟﻌﺎﺕ ﺑﺎ ﻣﻮﺍﺩ ﺣﺎﺟﺐ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴـﻚ MRI ، CTScan ،ﻭ (...ﺑـﺮﺍﻱ ﻧﺸـﺎﻥﺩﺍﺩﻥ ﺗﻜﻨﻴـﻚﻫـﺎﻱ ﻣﺨﺘﻠﻒ ﻣﺮﺑﻮﻁ ﺑﻪ Imagingﻫﺮ ﻋﻀﻮ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ( ﻃﺮﻳﻘﺔ ﻧﺼﺐ : hCDﺑﻌﺪ ﺍﺯ ﻗﺮﺍﺭﺩﺍﺩﻥ CDﺩﺭ CD-ROMﺩﺳﺘﮕﺎﻫﺘﺎﻥ ﺻﻔﺤﺔ Autoplay menuﺭﺍ ﺑﺒﻨﺪﻳﺪ ﺳﭙﺲ ﺑﻪ my computerﺭﻓﺘﻪ ﻭ ﺭﻭﻱ ﺩﺭﺍﻳﻮ CD-ROMﺩﺳﺘﮕﺎﻩ ﺧﻮﺩ ﺭﺍﺳـﺖﻛﻠﻴـﻚ ﻛﻨﻴـﺪ ﻭ ﮔﺰﻳﻨـﺔ Openﺭﺍ ﺍﻧﺨـﺎﺏ ﻛﻨﻴـﺪ ﺳﭙﺲ ﺭﻭﻱ * ، Setupﺩﺍﺑﻞ ﻛﻠﻴﻚ ﻛﻨﻴﺪ ﺻﻔﺤﻪﺍﻱ ﺑﺎ ﻧﺎﻡ radiologic Anatomy installationﻇﺎﻫﺮ ﻣﻲﺷﻮﺩ ﻣﺴﻴﺮ ﻧﺼﺐ ﺭﺍ ﻭﺍﺭﺩ ﻛﺮﺩﻩ ﻭ ﻳﺎ ﭘﻴﺶﻓﺮﺽ ﺭﺍ ﺑﺎ ﻛﻠﻴﻚ ﺑﺮ ﺭﻭﻱ OKﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ .ﺑﻌﺪ ﺍﺯ ﻧﺼﺐ ﭘﻴﻐـﺎﻣﻲ ﻣﺒﻨـﻲ ﺑـﺮ ﻧﺼـﺐ ﻛﺎﻣـﻞ CD ﻣﻲﺁﻳﺪ ﻛﻪ ﺁﻥ ﺭﺍ OKﻛﻨﻴﺪ ،ﺳﭙﺲ ﺍﺯ ﻣﻨﻮﻱ Startﺑﻪ Programﺭﻓﺘﻪ ﻭ ﺩﺭ radilogic Anatomyﻋﻨﻮﺍﻥ ﻣﺮﺑﻮﻃﻪ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ. * iconﻫﺎﻱ ﺩﻳﮕﺮﻱ ﺑﺎ ﻋﻨﺎﻭﻳﻦ ) (ssetup.apm ، setup.cfg ، ssetup ، Setup.ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﻣﺮﺑﻮﻁ ﺑﻪ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻧﻴﺴﺖ ﻟﻄﻔﹰﺎ ﻓﻘﻂ setup.exeﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ. )(International Medical Multimedia
ــــــ
47.1 Radiology Image Bank: Orthopedic Radiology
)48.1 Radiology on CD-ROM Diagnosis, Imaging, Intervention (Juan M. Taveras, MD, Joseph T. Ferrucci, MD
ــــــ ﺍﻳﻦ ، CDﻣﺠﻤﻮﻋﻪ ﻛﺎﻣﻠﻲ ﺍﺯ ﻛﺘﺎﺏ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Tavers
)ﻛﻪ ﻳﻜﻲ ﺍﺯ ﻣﻌﺘﺒﺮﺗﺮﻳﻦ ﻭ ﻛﺎﻣﻞﺗﺮﻳﻦ ﻣﺮﺍﺟﻊ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺭ ﺟﻬﺎﻥ ﻣﻲﺑﺎﺷﺪ( ﻫﻤﺮﺍﻩ ﺑﺎ ﺁﺧﺮﻳﻦ ﺗﻐﻴﻴﺮﺍﺕ ﺩﺍﺩﻩﺷﺪﻩ ﺗﺎ ﺳﺎﻝ 2001ﻣﻴﻼﺩﻱ ﺑﻮﺩﻩ ﻭ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﻋﻤﺪﺓ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: -٤ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Gastrointestinal
-٣ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Vascular
-٨ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Cardiac
Breast Imaging -٧ -١١ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Skeletal
2002 ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
-٢ﺳﻴﺎﺳﺖ ﺑﻬﺪﺍﺷﺘﻲ ﻭ ﻣﺪﻳﺮﻳﺖ ﺩﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ -٦ﻓﻴﺰﻳﻚ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ -١٠ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Adbomen
-١ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Pulmonary -٥ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Genitourinary
-٩ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺳﺮ ﻭ ﮔﺮﺩﻥ
)49.1 REVIEW FOR THE Radiography Examination (A & LERT) (McGrow-Hill's
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
8 50.1 Teaching Atlas of Mammography (Laszlo Tabar, Peter B. Dean) 51.1 The Basics of MRI of NMR
(Thieme)
ــــــ
(Joseph P. Hornak, Ph.D.)
ــــــ
52.1 The Encyclopaedia of Medical Imaging from NICER
ــــــ
53.1 THE MRI TEACHING FILE (Robert B. Lufkin, William G. Bradley, Jr., Michael Brant-Zawadzki)
2001
ﺗﻌـﺪﺍﺩ. ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﺷﺮﺡ ﺣﺎﻝ ﻭ ﻳﺎﻓﺘﻪﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺩﺍﺭﺍﻱ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻭ ﺗﺸﺨﻴﺺ ﻧﻬﺎﻳﻲ ﺑﻮﺩﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﺗﺸﺨﻴﺺ ﻧﻜﺎﺕ ﻣﻬﻢ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳـﺖCase ﻣﻲﺑﺎﺷﺪ ﻭ ﻫﺮMRI ﻫﺎﻱ ﻣﺘﻌﺪﺩ ﻣﺮﺑﻮﻁ ﺑﻪ ﻣﺒﺎﺣﺚ ﻣﺨﺘﻠﻒ ﺩﺭ ﺯﻣﻴﻨﺔCase ﻓﻮﻕ ﺩﺍﺭﺍﻱCD : ﺑﺼﻮﺭﺕ ﺟﺪﻭﻝ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪCD ﻫﺎﻱ ﻣﻄﺮﺡﺷﺪﻩ ﺑﺮ ﺣﺴﺐ ﻫﺮ ﻣﻮﺿﻮﻉ ﺩﺭ ﺍﻳﻦCase ﻣﻮﺿﻮﻉ
Case ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case ﺗﻌﺪﺍﺩ
ﻣﻮﺿﻮﻉ
Case ﺗﻌﺪﺍﺩ
ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻏﻴﺮﻧﺌﻮﭘﻼﺳﺘﻴﻚ ﻣﻐﺰ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺍﻃﻔﺎﻝ
٢٠١ ١٠٠ ١٠٠
ﻧﺌﻮﭘﻼﺳﻢﻫﺎﻱ ﻣﻐﺰﻱ ﺳﻴﺴﺘﻢ ﻋﻀﻼﻧﻲ ﺍﺳﻜﻠﺘﻲ ﺍﺻﻮﻝ ﻭ ﺁﺭﺗﻴﻔﻜﺖﻫﺎ
١٠٢ ١٠٠ ١٠٠
ﻣﻐﺰMRA ﺗﻨﻪ
١٠ ١٠٢
ﺳﺮ ﻭ ﮔﺮﺩﻥ ﺳﻴﺴﺘﻢ ﻗﻠﺒﻲﻋﺮﻭﻗﻲ
١٠٠ ١٠٤
54.1 THE RADIOLOGIC CLINICS OF NORTH AMERICA High-Resolution CT of the Lung II (DAVID A. LYNCH, MD)
(NUMBER 1 VOLUME 40)
ــــــ
: ﺭﻳﻪ ﺍﺳﺖHRCT ﻣﻲﺑﺎﺷﺪ ﻭ ﺩﺍﺭﺍﻱ ﻣﺒﺎﺣﺚ ﻋﻤﺪﺓ ﺫﻳﻞ ﺩﺭﺧﺼﻮﺹThe Radiologic clinics of North America ﺑﺮﮔﺮﺩﺍﻥ ﺷﻤﺎﺭﻩ ﺍﻭﻝ ﺟﻠﺪ ﭼﻬﻠﻢ ﺍﺯ ﻣﺠﻤﻮﻋﺔ ﻛﺘﺎﺑﻬﺎﻱCD ﺍﻳﻦ ﻭ ﺑﺮﻭﻧﺸﻜﺘﺎﺯﻱAir Way ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱCT Scan ﺩﺭ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺷﻐﻠﻲ ﻭ ﻣﺤﻴﻄﻲ ﺭﻳﻪHRCT ﻧﻘﺶ( ﺭﻳﻪquantitative) ﻛﻤﻴﺘﻲCT -
Peripheral Airways ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱHRCT Drug-Induced ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺭﻳﻮﻱHRCT -
ﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻣﻔﻴﺰﻡCT Scan Non-TB ﻭTB ﻣﺮﺑﻮﻁ ﺑﻪ ﻋﻔﻮﻧﺘﻬﺎﻱ ﻣﺎﻳﻜﻮﺑﺎﻛﺘﺮﻳﺎﻳﻲCT Scan -
ﺩﺭ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺭﻳﻮﻱ ﺍﻃﻔﺎﻝHRCT ﻧﻘﺶ ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺗﺮﻭﻣﺒﻮﺁﻣﺒﻮﻟﻴﻚ ﺭﻳﻮﻱCT Scan -
ﻧﺪﻭﻝ ﻣﻨﻔﺮﺩ ﺭﻳﻮﻱ-
55.1 THE RADIOLOGIC CLINICS OF NORTH AMERICA Imaging of Musculoskeletal and Spinal Infections • PRINCIPLES AND TECHNIQUES 1. Epidemiology 3. Normal Spine Variants and Anatomy 2. Thoracic Spine Injuries 4. Experimental and Necropsy Data • ATLAS OF SPINE INJURIES IN CHILDREN 1. Cervcal Spine 2. Thoracic Spine 3. Lumbar Spine
56.1 THE RADIOLOGIC CLINICS OF NORTH AMERICA
5. Measurements 6. Special Views and Techniwques
1999 7. Sacral Injuries 8. Occipitocervical Injuries
9- Mechanisms and Patterns of Injury
4. Sacrococcygeal Spine
Pediatric Musuloskeletal Pediatric Radiology
(SALEKAN E-BOOK)
(James S. Meyer, MD)
2001
: ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﺷﺎﻣﻞ ﺍﻳﻦ ﻣﺒﺎﺣﺚ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ y Ultrasound in Padiatric Musculoskeletal Disease: Teachinques and Applications y Nuclear Medicnine Topics in Pediatric Musculoskeletal Disease: Teachinques and Applications y Imaging of Musculoskeletal Infections y Malignant and Benign Bone Tumors y Magnetic Rsonance Imaging of Musculoskeletal Soft Tissue Mass y Imaging of Pediatric Hip Disorder y Imaging of Pediatric Foot Disorder in Children y Imaging of Sports Injuries in Children and Adolescents y A Pragmatic Approach to the Radiologic Diagnosis of Pediatric Syndromes and Skeletal Dysplasias y The Orthopedists Perspective: Bone Tumors, Scoliosis, and Trauma y Imaging of Crowth Distubance in Children y Imaging of Child Abuse
57.1 THE RADIOLOGIC CLINICS OF NORTH AMERICA Update on Nuclear Medicine 58.1
ــــــ
THE RADIOLOGIC CLINICS OF NORTH AMERICA Update on Ultrasonography (FAYE C. LAING, MD) (W.B. SAUNDERS COMPABY)
ــــــ
: ﻣﻲﺑﺎﺷﺪ ﻭ ﺩﺍﺭﺍﻱ ﻣﺒﺎﺣﺚ ﻋﻤﺪﺓ ﺫﻳﻞ ﺩﺭ ﺧﺼﻮﺹ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺍﺳﺖThe Radiologic Clinics Of North America ﺍﺯ ﻣﺠﻤﻮﻋﻪ ﻛﺘﺎﺏﻫﺎﻱ٣٩ ﺑﺮﮔﺮﺩﺍﻥ ﺷﻤﺎﺭﻩ ﺳﻮﻡ ﺟﻠﺪCD ﺍﻳﻦ ﺗﻜﻨﻮﻟﻮﮊﻱ ﺭﻭﺯ-١ ﻣﻮﺍﺩ ﺣﺎﺟﺐ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﺪ-٢ ( ﺗﺤﺖ ﺭﺍﻫﻨﻤﺎﻳﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻲintervention) ﺍﻗﺪﺍﻣﺎﺕ ﻣﺪﺍﺧﻠﻪﺍﻱ-٣ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺭ ﺣﻴﻦ ﻋﻤﻞ ﺟﺮﺍﺣﻲ-٤ ﻭﺿﻌﻴﺖ ﻓﻌﻠﻲ ﺗﺸﺨﻴﺼﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺍﻧﺪﻭﺳﻜﻮﭘﻴﻚ-٥ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻣﻮﺳﻜﻮﻟﻮﺍﺳﻜﻠﺘﺎﻝ-٦ Breast ﺳﻮﻧﻮﮔﺮﺍﻓﻲ-٧ Gynecology ﻭObstetric ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺳﻪﺑﻌﺪﻱ ﺩﺭ-٨ Gynecologic ﺳﻮﻧﻮﮔﺮﺍﻓﻲ-٩ ﺍﺭﺯﻳﺎﺑﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﺍﺗﺴﺎﻉ ﺑﻄﻦﻫﺎﻱ ﺩﺍﺧﻞ ﻣﻐﺰﻱ ﺑﻪ ﺩﻧﺒﺎﻝ ﺧﻮﻧﺮﻳﺰﻱ-١٠ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺷﺮﻳﺎﻥﻫﺎﻱ ﻣﺤﻴﻄﻲ-١١ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻛﺎﺭﻭﺗﻴﺪ-١٢ 59.1
Ultrasound Atlas of Vascular Diseases
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(Carol A. Krebs, RT, RDMS, Vishan L. Giyanani, , Ronald L. Eisenberg) (APPLETON & LANGE Stamford, Connecticut) (SALEKAN E-Book)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
9
ــــــ ــــــ ــــــ
)Ultrasound Teaching Manual The basics of Performing and Interpreting Ultrasound Scans (Matthias Hofer) (With the collaboration of Tatjana Reihs) (Thieme )61.1 Uterosalpingography in Gynecology Hysterospingography (Salekan E-Book 62.1 VOXEL-MAN 3D-Navigator Brain and Skull (Regional, Functional, and Radiological Anatomy) (IMDM university Hospital Eppendorf, )Humburg )(Springer ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﺭ ﻗﺎﻟﺐ ﻳﻚ ﺍﻃﻠﺲ ﺳﻪﺑﻌﺪﻱ Interactiveﺍﺯ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺩﺍﺧﻠﻲ ﺗﻨﻪ ﺩﺭ ﺳﻪ ﻋﺪﺩ CDﺟﻬﺖ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻜﻲ ،ﻃﺮﺍﺣﻲ ﺷﻴﻮﺓ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﻭ ﺁﻣﻮﺯﺵ ﺩﺭﻭﺱ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳـﺖ .ﻓﺼـﻮﻝ ﻣﺨﺘﻠـﻒ ﺍﻳﻦ CDﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﺍﺳﺖ: ﺑﺨﺶ ﺍﻭﻝ( ﺁﻧﺎﺗﻮﻣﻲ :١-١ :ﺗﺸﺮﻳﺢ ﺳﻪﺑﻌﺪﻱ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺩﺍﺧﻞ ﺗﻨﻪ :ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺁﻧﺎﺗﻮﻣﻲ ﺳﻪﺑﻌﺪﻱ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﺑﺎ ﻗﺎﺑﻠﻴﺖ ﭼﺮﺧﺶ Ventricolﻭ ﭼﺮﺧﺶ horizontalﻭ ﺁﻧﺎﺗﻮﻣﻲ ﺷﻜﻢ ﺑﺎ ﻗﺎﺑﻠﻴﺖ ﭼﺮﺧﺶ ﺍﻓﻘﻲ ﻭ ﻋﻤﻮﺩﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ : ٢-١ﺗﺸﺮﻳﺢ ﺩﺳﺘﮕﺎﻩﻫﺎ ﻛﻪ ﺩﺭ ٩ﺑﺨﺶ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ )ﺍﺳﻜﻠﺖ ﺍﺳﺘﺨﻮﺍﻧﻲ ،ﺳﻴﺴﺘﻢ ﻗﻠﺒﻲ ﻋﺮﻭﻗﻲ ،ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ،ﻛﺒـﺪ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﻗﺎﺑﻠﻴﺖ ﺣﺬﻑ ﻭ ﺍﺿﺎﻓﻪﻧﻤﻮﺩﻥ ﻫﺮ ﻳﻚ ﺍﺯ ﺑﺨﺶﻫﺎﻱ ﺗﺼﺎﻭﻳﺮ ﻭ ﭼﺮﺧﺶ ١٨٠oﺁﻧﻬﺎ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. : ٣-١ﺁﻧﺎﺗﻮﻣﻲ ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ :ﺷﺎﻣﻞ ٢ﻗﺴﻤﺖ ﺁﻧﺎﺗﻮﻣﻲ ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ ﺳﻄﻮﺡ Coronalﻭ Sagittalﻣﻲﺑﺎﺷﺪ. ﻭ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺟﺎﻧﺒﻲ ،ﺷﺒﻴﻪﺳﺎﺯﻱ ﮔﺎﺳﺘﺮﻭﺳﻜﻮﭘﻲ ﺑﺎ ﻗﺎﺑﻠﻴﺖ ﺣﺮﻛﺖ ﺩﺭ ﻓﻀﺎﻱ ﻣﺮﻱ ﻭ ﻣﻌﺪﻩ( 60.1
ﺗﻮﻣﻮﮔﺮﺍﻓﻲﺑﺨﺶ ﺩﻭﻡ( ﺭﺍﺩﻳﻮﻟﻮﮊﻱ: -١-١ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ CT -٢-١ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ )ﺑﺎ ﻗﺎﺑﻠﻴﺖ ﺣﺮﻛﺖﺩﺍﺩﻥ ﺳﻄﺢ ﻣﻘﻄﻊ ﻭ ﻣﺸﺎﻫﺪﻩ ﺗﺼﻮﻳﺮ ﻫﺮ ﻗﺴﻤﺖ( -٤-١ﺷﺒﻴﻪﺳﺎﺯﻱ ﻗﺴﻤﺖ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻴﻚ ﻛﺒﺪ -٣-١ﻣﻘﺎﻳﺴﻪ ﺑﻴﻦ ﺗﺼﺎﻭﻳﺮ CTﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺳﻪﺑﻌﺪﻱ ﻭ ﻣﻘﺎﻃﻊ ﻋﺮﺿﻲ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ -ﺗﺼﺎﻭﻳﺮ X-ray
ــــــ ــــــ
-٤-٢ﺗﺼﺎﻭﻳﺮ X-rayﺍﺯ ﻛﻠﻴﺔ ﺍﻧﺪﺍﻡﻫﺎ -٣-٢ﺗﺼﺎﻭﻳﺮ X-rayﺍﺯ ﺍﻧﺪﺍﻡﻫﺎﻱ ﻣﻨﻔﺮﺩ -٢-٢ﺗﺼﺎﻭﻳﺮ X-rayﺍﺯ ﺷﻜﻢ -١-٢ﺗﺼﺎﻭﻳﺮ X-rayﺍﺯ ﻗﻔﺴﺔ ﺳﻴﻨﻪ ﻣﺎﺭﻙﺩﺍﺭﻧﻤﻮﺩﻥ ﻫﺮ ﺑﺨﺶ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﻭ ﻣﻘﺎﻃﻊ ﺗﺸﺮﻳﺤﻲ ﻗﺪﺭﺕ ﺍﻓﺰﺍﻳﺶ Zoomﺗﺼﺎﻭﻳﺮ ﺍﺭﺍﺋﻪ ﺗﺼﺎﻭﻳﺮ ﺑﺎﺯﺳﺎﺯﻱﺷﺪﻩ ﻛﺎﻣ ﹰ ﻼ ﻭﺍﻗﻌﻲ ﻛﻪ ﺍﺭﺍﺋﻪ ﻓﻬﺮﺳﺖ ﻛﺎﻣﻞ ﻣﻨﺪﺭﺟﺎﺕ ﺗﺼﺎﻭﻳﺮ ﺑـﻪ ﺳـﻪ ﺯﺑـﺎﻥ ﺍﻧﮕﻠﻴﺴـﻲ ،ﺁﻟﻤـﺎﻧﻲ ﻭ ﻧﺎﻣﮕــﺬﺍﺭﻱ ﺑﺨــﺶﻫــﺎﻱ ﻣﺨﺘﻠــﻒ ﺗﺼــﺎﺋﻴﺮ ﺑﺼــﻮﺭﺕ ﻛﺎﺭﺑﺮﺩ ﺁﻣﻮﺯﺷﻲ ﺟﺬﺍﺑﻲ ﺭﺍ ﺑﻪ ﻫﻤﺮﺍﻩ ﺩﺍﺭﺩ. ﻻﺗﻴﻦ Intractive
)VOXEL-MAN 3D-Navigator Inner Organs (Regional, Systemic and Radiological Anatomy) (IMDM university Hospital Eppendorf, Hamburg )64.1 Whole Body Computed Tomography (Second Edition) (Otto H. Wegener) (Blackwell Science ﺩﺭ ﺍﻳﻦ CDﺩﺭ ﻃﻲ ٢٨ﻓﺼﻞ ﺑﻪ ﺷﺮﺡ ﺁﻧﺎﺗﻮﻣﻲ ،ﺗﻜﻨﻴﻚ ﻭ ﻓﻴﺰﻳﻚ ﻣﺮﺑﻮﻁ ﺑﻪ CT Scanﻫﻤﺮﺍﻩ ﺑﺎ ﺑﺮﺭﺳﻲ ﺟﺰﺀ ﺑﻪ ﺟﺰﺀ ﻣﺴﺎﺋﻞ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﻧﻮﺍﺣﻲ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﮔﻮﻳﺎﻱ CT Scanﭘﺮﺩﺍﺧﺘﻪ ﺷﺪﻩ ﺍﺳـﺖ .ﻓﻬﺮﺳـﺖ ﻛﻠـﻲ ﻓﺼﻮﻝ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻜﻨﻴﻜﻬﺎﻱ CT Scan ﻣﻮﺍﺩ ﺣﺎﺟﺐ ﺗﺤﻠﻴﻞ ﺗﺼﻮﻳﺮ ﺩﺭ CT Scanﺁﻧﺎﺗﻮﻣﻲ ﺩﺭ CT Scan ﻛﻠﻴﻪ ﺍﺭﮔﺎﻧﻬﺎﻱ ﺗﻨﺎﺳﻠﻲ ﺯﻥ ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻧﻲ ﻣﺪﻳﺎﺳﺘﻦ ﺭﻭﺵ ﻭ ﺍﺳﺘﺮﺍﺗﮋﻱ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭ ﻗﻠﺐ ﺭﻳﻪﻫﺎ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﺣﻔﺮﺓ ﺭﺗﺮﻭﭘﺮﻳﺘﻮﺋﻦ ﻏﺪﺩ ﻓﻮﻕ ﻛﻠﻴﻮﻱ ﺟﻨﺐ )ﭘﻠﻮﺭ( ﺩﻳﻮﺍﺭﺓ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﻛﺒﺪ ﻟﮕﻦ ﺍﺳﺘﺨﻮﺍﻧﻲ ﺳﻴﺴﺘﻢ ﺻﻔﺮﺍﻭﻱ ﻋﻀﻼﺕ ﻣﺜﺎﻧﻪ ﺗﺮﻣﻴﻨﻮﻟﻮﮊﻱ CT ﭘﺎﻧﻜﺮﺍﺱ ﺩﺳﺘﮕﺎﻩ ﮔﻮﺍﺭﺵ ﺣﻔﺮﺓ ﭘﺮﻳﺘﻮﺋﻦ ﻃﺤﺎﻝ ﭘﺮﻭﺳﺘﺎﺕ ﻭ ﺳﻤﻴﻨﺎﻝ ﻭﺯﻳﻜﻮﻝﻫﺎ ﺗﻮﻣﻮﺭﻫﺎﻱ ﻧﺴﺞ ﻧﺮﻡ 63.1
-٢ﮔﻮﺵ ،ﺣﻠﻖ ﻭ ﺑﻴﻨﻲ
ﻋﻨﻮﺍﻥ CD )Advanced Rhinoplasty Techniques Cosmetic Rhinoplasty (Rollin K. Daniel, M.D. Analysis, Marking & Anesthesia, Closed/Open Approach, Septum Exposure, Exposure & Dorsal Reduction,
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــــ
1.2
& Caudal Septum Resection, Ideal Profile Line, Open Approach, Tip Analysis, Septoplasty Septal Harvest, Grafts, Spreaser Grafts, Grural Strut, Tip Suture Technique, Closure, Nostril Sill Alar Wedge, Composite Graft, Lateral Osteotomy, Final Steps, Acknowledgments
2004 ــــــ
Advanced Therapy of OTITIS MEDIA )Atlas D'ORL Realise avec la collaboration des (Dr Michel Boucherat, Dr Jean-Robert Blondeau -Anatomie de l’oreille normale - Images pathologiques - Cas cliniques -Anatomie naso-sinusienne normale -Images pathologiques - Cas cliniques - Rappels des principes de la TDM et de l’IRM
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
2.2 3.2
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
10 ــــــ
)Atlas of Rhinoplasty Open and Endonasal Approaches (Gilbert Aiach, M.D
4.2
ــــــ
)Atlas of Head & Neck Surgery Otolaryngology (TEXTBOOK) (Byron J. Bailey, Karen H. Calhoun, Amy R. Coffey, J. Gail Neely
5.2
1- Atlas :
ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ٢٥ﺭﻭﺵ ﺟﺮﺍﺣﻲ ﺍﻧﺘﺨﺎﺑﻲ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻗﺴﻤﺖ ﺩﺍﺭﺍﻱ ٢٥ﻓﺼﻞ ﺩﺭ ﭼﻬﺎﺭ ﺑﺨﺶ ﺍﺻﻠﻲ ﺍﺳﺖ:
- Head & Neck Surgery :
ﺷﺎﻣﻞ ٦ﻋﻨﻮﺍﻥ ﺍﺻﻠﻲ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﺍﻃﻼﻋﺎﺕ ﺍﺳﺎﺳﻲ ﺭﺍﺟﻊ ﺑﻪ ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﺗﻤﻬﻴﺪﺍﺕ ﻗﺒﻞ ﺍﺯ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ،ﻭﺳﺎﻳﻞ ﻭ ﺭﻭﺵﻫﺎﻱ ﺑﻴﻬﻮﺷﻲ ﻭ ....ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ٦ .ﻋﻨﻮﺍﻥ ﺍﺻﻠﻲ ﺷﺎﻣﻞ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺳﺖ: • Thyroid & Parathyroid
• Neck & Larynx
• Ear
• Nose & maxilla
• Oral Clarity
: • Congenital Aural Base • Excision of skin Lesions
• Tran temporal Skull Base
- Otologic procedures
• Middle Ear and Ossicular Chain
- Plastic & Reconstructive Surgery : • Larygoplasty, Rhytidectomy, Rhinoplasty
• Mandibular Surgery, Local & Regional Flaps,
: • Ton Sillectomy
• Salivary Gland
- Pediatric and General Otolaryngology
• Nasal Polypectomy
ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺑﺮ ﺍﺳﺎﺱ ﻣﻮﺿﻮﻉ ،ﻛﻠﻤﺎﺕ ﻭ ﻭﺍﮊﻫﺎﻱ ﺗﺨﺼﺼﻲ ،ﻧﺎﻡ ﻧﻮﻳﺴﻨﺪﻩ ،ﺷﻤﺎﺭﺓ ﻣﺠﻠﻪ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻣﺒﺎﺣﺚ ﻣﻮﺭﺩ ﻧﻈﺮﺗﺎﻥ ﺭﺍ ﺟﺴﺘﺠﻮ ﻭ ﻣﻄﺎﻟﻌﻪ ﻧﻤﺎﺋﻴﺪ
• Frontal Sinus
2- Bilbo Med Medline :.
3- Head & Neck Surgery: - Textbook - Drug Reference - Textbook : ﺍﻳﻦ ﺑﺨﺶ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻧﻮﺷﺘﺔ ﺩﻛﺘﺮ Bailey
ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﻣﺘﻌﺪﺩ ﮔﻮﻳﺎ ﻭ ﻧﻤﻮﺩﺍﺭﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﺍﺳﺖ ﻛﻪ ﺷﺎﻣﻞ ١٨٠ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ. 1- Basic Science / General Medicine
٤ﺑﺨﺶ ﺍﺻﻠﻲ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﺍﻳﻦ ﺷﺮﺡ ﺍﺳﺖ:
)ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﮔﻮﻧﺎﮔﻮﻥ ﻭ ﺗﺨﺼﺼﻲ ﺭﺍﺟﻊ ﺑﻪ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﮔﻮﺵ ،ﺳﺮ ،ﮔﺮﺩﻥ(
2- Head & Neck :
3- Otology 4- Facial Plastic Reconstructive Surgery - Drug Reference :
ــــــ
ــــــ
ﺩﺍﺭﻭﻫﺎﻱ ﺍﺻﻠﻲ ﻭ ﮊﻧﻮﺗﻴﻚ ﺑﻪ ﺷﻜﻞ ﺍﻟﻔﺒﺎﻳﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺍﻃﻼﻋﺎﺕ ﻛﺎﻣﻞ ) ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ،ﺭﺩﺓ ﺩﺍﺭﻭﻳﻲ ،ﺍﺳﺎﻣﻲ ﺷﻴﻤﻴﺎﻳﻲ ﻭ ﺗﺠﺎﺭﺗﻲ ،ﻣﻘﺪﺍﺭ ﻣﺼﺮﻑ ﺍﺛﺮﺍﺕ ﺟﺎﻧﺒﻲ ،ﻓﺎﺭﻣﺎﻛﻮﻛﺴﻴﻚ ﺩﺍﺭﻭ ﻭ(..... )6.2 Causes of FAILURE in STAPES SURGERY (VCD I) (Howard P. House, TED N. Steffen )PITFALLS in STAPES SURGERY (VCD II )STAPEDECTOMY (Prefabricated Wire-Loop and Gelfoam Technique) (VCD III )7.2 Chirurgia Endoscopica Dei Seni Paranasali (A Cura di E. Pasquini G. Farneti 3. Aspetti radiologici
)(EIJI YANAGISAWA, MD
ــــــ 2002
1. Principi di anatomia endoscopica
2. Tecnica chirurgica
8.2 Color Atlas of Diagnostic Endoscopy in Otorhinolaryngolgy 9.2 Color Atlas of Ear Disease
)(Salekan E-book) (Richard A. Chole, MD, PhL, James W. Forsen )10.2 Cobblation Assisted Tonsillectomy (CAT) __ Cobblation Assisted Procedures (VCD) (CD I , II
ــــــ
ﺩﺭ CDﺷﻤﺎﺭﺓ ١ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺭﻭﻱ ﺗﻮﻧﺴﻴﻞﻫﺎ ﺑﺎ ﻛﻤﻚ ﺩﺳﺘﮕﺎﻩ Coblationﺑﻪ ﺷﻤﺎ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﺍﻳﻦ VCDﺷﺎﻣﻞ ﻣﻮﺍﺭﺩ ﺁﻣﻮﺯﺷﻲ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: 3- Coblation Assisted tonsilectomg
2- Lop – off "CAT" technique
1- Subtotal Cololation Assisted tonsillectomy
ﺩﺭ CDﺷﻤﺎﺭﺓ ٢ﺷﻤﺎ ﺑﺎ ﺩﺳﺘﮕﺎﻩ Coblationﻛﻪ ﺗﺤﻮﻟﻲ ﻋﻈﻴﻢ ﺩﺭ ﺣﻴﻄﻪ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ENTﺍﻳﺠﺎﺩ ﻛﺮﺩﻩ ﺍﺳﺖ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪ .ﻧﺤﻮﺓ ﻋﻤﻠﻜﺮﺩ ﺩﺳﺘﮕﺎﻩ ﺑﺮ ﺍﺳﺎﺱ ﺍﻣﻮﺍﺝ ﺭﺍﺩﻳﻮﻓﺮﻛﻮﺋﻨﺴﻲ ﺑﺎ ﻭﺍﺳﻄﻪ ﭘﻼﺳـﻤﺎ ﻣـﺎﻳﻊ ﻣـﻲﺑﺎﺷـﺪ ﻭ ﻣﺰﺍﻳـﺎﻱ ﻓﺮﺍﻭﺍﻧـﻲ ﺑـﺮ ﺩﺳـﺘﮕﺎﻫﻬﺎﻱ ﻟﻴـﺰﺭ ﻭ ﺭﺍﺩﻳﻮﻓﺮﻛﻮﺋﻨﺴﻲ ﻗﺪﻳﻤﻲ ﺩﺍﺭﺩ .ﻋﺪﻡ ﻧﻴﺎﺯ ﺑﻪ ﺑﻲﻫﻮﺷﻲ ﻋﻤﻮﻣﻲ ﻭ ﺍﻣﻜﺎﻥ ﺍﻧﺠﺎﻡ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺑﻪ ﺻﻮﺭﺕ ﺳﺮﭘﺎﻳﻲ ،ﺩﻭﺭﺍﻥ recoveryﻛﻮﺗﺎﻩ ،ﺗﺤﻤﻞ ﺑﺎﻻﻱ ﺑﻴﻤﺎﺭﺍﻥ ،ﻭﺟﻮﺩ ﺩﺭﺩ ﺑﺴﻴﺎﺭ ﻣﺨﺘﺼﺮ ﻳﺎ ﺣﺘﻲ ﻋﺪﻡ ﻭﺟﻮﺩ ﺩﺭﺩ ﭘﺲ ﺍﺯ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ،ﻇﺮﺍﻓﺖ ﻭ ﺗﻤﻴﺰﻱ ﺍﻋﻤﺎﻝ ،ﻫﻤﻮﺳـﺘﺎﺯ ﻋﺎﻟﻲ ،ﺣﺼﻮﻝ ﺳﺮﻳﻊ ﻧﺘﺎﻳﺞ ،ﺳﺮﻋﺖ ﺑﺎﻻﻱ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ﻭ ﺭﺍﺣﺘﻲ ﻓﻮﻕﺍﻟﻌﺎﺩﻩ ﺟﺮﺍﺡ ﺑﺮﺧﻲ ﺍﺯ ﻣﺰﺍﻳﺎﻱ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﺩﺳﺘﮕﺎﻩ ﻣﻲﺑﺎﺷﺪ .ﺍﺯ ﺍﻳﻦ ﺩﺳﺘﮕﺎﻩ ﺩﺭ ﺣﻴﻄﺔ ENTﺩﺭ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩ: 1- Coblation channeling of the inferior turbinate
ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﺩﺳﺘﮕﺎﻩ ﻭ ﺗﺤﺖ ﺑﻲﺣﺴﻲ ﻟﻮﻛﺎﻝ ،ﺍﻧﺴﺪﺍﺩ ﺑﻴﻨﻲ ﻧﺎﺷﻲ ﺍﺯ ﻫﻴﭙﺮﺗﺮﻭﻓﻲ ﺗﻮﺭﺑﻴﻨﻪ ﺗﺤﺘﺎﻧﻲ ﺑﻪ ﻛﻤﻚ Channelingﺗﻮﺭﺑﻴﻨﻪ ﺩﺭﻣﺎﻥ ﻣﻲﺷﻮﺩ .ﻧﺘﻴﺠﻪ ﻋﻤﻞ ﺑﻪ ﺻﻮﺭﺕ ﺭﻳﺪﺍﻛﺸﻦ ﺳﺮﻳﻊ ﺗﻮﺭﺑﻴﻨﻪ ﺑﻼﻓﺎﺻﻠﻪ ﻗﺎﺑﻞ ﻣﺸﺎﻫﺪﻩ ﺍﺳﺖ :ﺍﻳﻦ ﻋﻤﻞ ﺗﻘﺮﻳﺒﹰﺎ ﺑﻲﺩﺭﺩ ﺧﻮﺍﻫﺪ ﺑﻮﺩ. 2- Coblation channeling of the Soft palate
ﺩﺭ ﺍﻳﻦ ﻋﻤﻞ ،ﺑﺎ Channelingﻛﺎﻡ ﻧﺮﻡ ﺍﺯ ﺣﺠﻢ ﺁﻥ ﻛﺎﺳﺘﻪ ﺷﺪﻩ ﻭ ﺑﺎﻋﺚ ﺭﻓﻊ ﺧﺮﺧﺮ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﻣﻲﺷﻮﺩ .ﺍﻳﻦ ﻋﻤﻞ ﺳﺮﭘﺎﻳﻲ ﻭ ﺗﺤﺖ ﺑﻲﺣﺴﻲ ﻟﻮﻛﺎﻥ ﻭ ﺗﻘﺮﻳﺒﹰﺎ ﻓﺎﻗﺪ ﺩﺭﺩ ﺍﺳﺖ .ﻧﺘﻴﺠﺔ ﻋﻤﻞ ﻧﻴﺰ ﺑﻪ ﺳﺮﻋﺖ ﺣﺎﺩﺙ ﻣﻲﺷﻮﺩ. 3- Coblation channeling of the tonsil
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
11 . ﻧﺘﻴﺠﻪ ﺑﻪ ﺳﺮﻋﺖ ﺣﺎﺩﺙ ﺷﺪﻩ ﻭ ﻋﻤﻞ ﺗﻘﺮﻳﺒﹰﺎ ﻓﺎﻗﺪ ﺩﺭﺩ ﺍﺳﺖ. ﺑﺴﺘﻪ ﺑﻪ ﺷﺮﺍﻳﻂ ﺍﻳﻦ ﻋﻤﻞ ﻣﻲﺗﻮﺍﻧﺪ ﺳﺮﭘﺎﻳﻲ ﻳﺎ ﺗﺤﺖ ﺑﻲﻫﻮﺷﻲ ﻋﻤﻮﻣﻲ ﺑﺎﺷﺪ. ﺗﻮﻧﺴﻴﻞ ﻛﺎﺳﺘﻪ ﻣﻲﺷﻮﺩbulk ﻫﻴﭙﺮﺗﺮﻭﻧﻲ ﺗﻮﻧﺴﻴﻠﺮ ﺑﺮﻃﺮﻑ ﺷﺪﻩ ﻭ ﺍﺯ،ﺑﺎ ﺍﻳﻦ ﺭﻭﺵ 4- Coblation Assisted Tonsillectomy(CAT)
11.2 DALLAS RHINOPLASTY
. ﻭ ﺩﻭﺭﺍﻥ ﺑﻬﺒﻮﺩﻱ ﺳﺮﻳﻊ ﻣﻲﺑﺎﺷﺪ.ﻻ ﺑﺴﻴﺎﺭ ﻣﺨﺘﺼﺮ ﺍﺳﺖ ﺩﺭﺩ ﭘﺲ ﺍﺯ ﻋﻤﻞ ﻣﻌﻤﻮ ﹰ.ﺩﺭ ﺻﻮﺭﺕ ﻭﺟﻮﺩ ﺗﻮﻧﺴﻴﻞﻫﺎﻱ ﺑﺰﺭﮒ ﻳﺎ ﺗﻮﻧﺴﻴﻠﻴﺖ ﻓﺮﺽ ﺍﺯ ﺍﻳﻦ ﺭﻭﺵ ﺟﻬﺖ ﺍﻧﺠﺎﻡ ﺗﻮﻧﺴﻴﻠﻜﺘﻮﻣﻲ ﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩ
Nasal Surgery by the Masters (Reducing Tip Projection and Nostrill Show Via the Open Approach) (CD I , II)
VCD: 1 1) Cadaveric Rhinoplasty Dissection Technique 2) Role of Component Dorsal Reduction: Spreader Grafts in the Deviated Nose
2002
VCD: 2 Reducing Tip Projection and Nostril Show Via the Open Approach
: ﺑﻪ ﺷﻤﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺑﺮ ﺭﻭﻱ ﻛﺎﺭﺁﻭﺭ ﺍﺯ ﺍﺑﺘﺪﺍ ﻭ ﺩﺭ ﻏﺎﻟﺐ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﺑﻪ ﺗﺮﺗﻴﺐ ﺁﻣﻮﺯﺷﻲ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ، ﻛﻪ ﺩﺭ ﺳﭙﻮﺯﻳﻮﻡ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺩﺍﻻﺱ ﺗﻬﻴﻪ ﺷﺪﻩ ﺍﺳﺖ١ ﺷﻤﺎﺭﺓVCD ﺩﺭ 1)
Exposure/Nasal incisions A. Closed endonasal approach - Intracartilaginous (IC) incision B. Cartilage delivery technique - Infracartilaginous incision - Intercartilaginous incision C. Open Rhinoplasty approach - Transcolumellar incision
2) Tip Alteration 3) Sptal reconstraction 4) Osteotmies 5) Adjuctive techniques/Closure A. Columellar Stat placement A. Septal reconstraction A. Medial Osteotomy A. Alare base resection - Intercarural suture stabilization - Inferior tarbinate resection B. Lateral Osteotomy - Correction of alalr flaring B. Controlling dome angalation (Submacosal) C. External Osteotomy - Diminishing nostril shape and tip defining points - Septal reconstruction B. Closare - Interdomal sutures B. Modification of the dorsum C. Splints - Transdomal Satares - Component dorsum C. Correction of alar reduction pinching/notching - Spreader graft placement - lateral crural strut grafts - Alar contour grafts D. Tip grafts - Infratip graft - Onlay tip graft ﺑـﻪGunter ﺍﺯ ﻣﺼﺎﺣﺒﻪ ﺑﺎ ﺑﻴﻤﺎﺭ ﺁﻏﺎﺯ ﺷـﺪﻩ ﻭ ﺳـﭙﺲ ﺩﻛﺘـﺮVCD ﺁﻣﻮﺯﺵ ﺩﺭ ﺍﻳﻦ. ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩOpen ﺗﺤﺖ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺑﺎ ﺍﭘﺮﻭﭺGunter ﺯﻳﺎﺩ ﺗﻮﺳﻂ ﺁﻗﺎﻱ ﺩﻛﺘﺮnostril show , Projected tip ﺧﺎﻧﻢ ﺟﻮﺍﻧﻲ ﺑﺎ ﺷﻜﻞ٢ ﺷﻤﺎﺭﺓVCD ﺩﺭ
. ﺳﭙﺲ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﺑﺎ ﻇﺮﺍﻓﺖ ﻋﺎﻟﻲ ﺩﺭ ﻏﺎﻟﺐ ﻣﺮﺍﺣﻞ ﺯﻳﺮ ﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩ.ﺁﻧﺎﻟﻴﺰ ﻧﺎﺯﻭﻧﺎﺷﻴﺎﻝ ﻭﻱ ﻣﻲﭘﺮﺩﺍﺯﺩ 4) Transaction of lat Crura
3) Underminig tip Skin
2) Infracartilaginous and trans columellar incisions
1)Complete transfixion incision
8) Reduction of dorsal septum (DS) and upper lateral cartilage (ULC)
7) reduction of bony darsum (BD)
6) Preparing submucosal tunnels
5) Resection of feet of medial crura
12) Cephalic resection of lateral Crura (LC)
11) Spreader grafts
10) Medial asteomius
9) Harvesting Septal cartilages for grafting
16) Final adjustment of dorsal height
15) Lateral asteotomy Cinternal
14) Aligning the dorsum
13) Preparation for lateral crural grafts (LCSG)
19) Closure
18) Placement of lateral crural strut grafts
17) Columellar strt placemend
!! ﺗﻮﺟﻪ ﺷﻤﺎ ﺭﺍ ﺑﻪ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻭﺳﻴﻠﻪ ﺭﻳﺪﺍﻛﺸﻦ ﺩﻭﺭ ﺳﻮﻡ ﺍﺳﺘﺨﻮﺍﻧﻲ ﻧﻴﺰ ﺟﻠﺐ ﻣﻲﻛﻨﻴﻢVCD ﺩﺭ ﺍﻳﻦ.ﺩﺭ ﻧﻬﺎﻳﺖ ﺷﻤﺎ ﻧﺘﺎﻳﺞ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ ﺑﻴﻤﺎﺭ ﺩﺭ ﻓﻮﺍﺻﻞ ﻣﺨﺘﻠﻒ ﻣﺸﺎﻫﺪﻩ ﻣﻲﻛﻨﻴﺪ 12.2 EENT Welch Allyn Institute of Interactive Learning
ــــــ
13.2 Endoscopic Assisted Procedures used in Astatic Facial Plastic Surgery
(VCD) (CD I , II)
ــــــ
ﺁﻣﻮﺯﺷﻲ ﺑﻪ ﺻـﻮﺭﺕ ﻗـﺪﻡ. ﺳﭙﺲ ﺑﻪ ﺷﻤﺎ ﺗﻜﻨﻴﻚ ﺟﺮﺍﺣﻲ ﺍﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﻣﺎﻻﺭﻭﻓﺮﻭﻧﺘﺎﻝ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﻫﻨﺮﻱ ﺩﻟﻤﺎﺭ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. ﺷﺮﻛﺖ ﻛﺎﺭﻝ ﺍﺷﺘﻮﺭﺗﺰ ﭘﻴﺸﺮﻭ ﺩﺭ ﺍﺭﺍﺋﻪ ﺗﺠﻬﻴﺰﺍﺕ ﺍﻧﺪﻭﺳﻜﻮﭘﻲ ﻭ ﻣﺤﺼﻮﻻﺕ ﺁﻥ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪ، ﺍﻭﻝ ﺷﻤﺎ ﺩﺭ ﺍﺑﺘﺪﺍVCD ﺩﺭ ﺍﻳﻦ . ﺭﺍ ﺑﻪ ﻧﻤﺎﻳﺶ ﻣﻲﮔﺬﺍﺭﺩEndoscopic forehead rhytidectomy and brow elevation ﺗﻜﻨﻴﻚ ﺟﺮﺍﺣﻲGrlecory S. Keller ﺩﺭ ﻣﺮﺣﻠﺔ ﺑﻌﺪ ﺩﻛﺘﺮ.( ﺍﺩﺍﻣﻪ ﻣﻲﻳﺎﺑﺪclosure) ﺑﻪ ﻗﺪﻡ ﺍﺯ ﻧﺸﺎﻧﻪﮔﺬﺍﺭﻱ ﺭﻭﻱ ﭘﺮﺕ ﻭ ﺗﺰﺭﻳﻖ ﻭ ﺑﺮﺵﻫﺎ ﺷﺮﻭﻉ ﺷﺪﻩ ﻭ ﺗﺎ ﭘﺎﻳﺎﻥ ﻋﻤﻞ Extended Composite face Lift
Endoscopic midface Lift
Endoscopic forehead Lift
: ﺷﻤﺎ ﺑﺎ ﺍﻳﻦ ﻣﻮﺍﺭﺩEndoscopic assisted forehead and face lifting ﺩﻭﻡ ﺗﺤﺖ ﻋﻨﻮﺍﻥVCD ﺩﺭ
ﺍﺑﺰﺍﺭﺁﻻﺕ ﻻﺯﻡ ﺩﺭ ﻋﻤﻞ، ﺩﺭ ﭘﺎﻳﺎﻥ ﻧﺤﻮﺓ ﺛﺒﺖ ﺳﻪﺑﻌﺪﻱ ﺗﻐﻴﻴﺮﺍﺕ. ﻣﺎﻩ ﺑﻌﺪ( ﻫﻢ ﺑﻪ ﺷﻤﺎ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ٢) ﺩﺭ ﻫﺮ ﻣﻮﺭﺩ ﺑﺮﺍﻱ ﺷﻤﺎ ﻳﻚ ﺑﻴﻤﺎﺭ ﻣﻮﺭﺩ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﺗﻮﺳﻂ ﺁﻥ ﺗﻜﻨﻴﻚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﻧﺘﺎﻳﺞ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ.ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ ﻭ ﻓﻮﺍﻳﺪ ﻫﺮ ﺭﻭﺵ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪ .ﺟﺮﺍﺣﻲ ﻫﻢ ﺑﻪ ﺷﻤﺎ ﻣﻌﺮﻓﻲ ﻣﻲﺷﻮﺩ 14.2 Diseases of the Sinuses Diagnosis and Management (Darid W. Kennedy, MD, FRCSI, William E. Bolger, MD, FACS, S. James Zinreich, MD) . ﺍﻳﻦ ﻛﺘﺎﺏ ﺗﻘﺮﻳﺒﹰﺎ ﻣﻌﺘﺒﺮﺗﺮﻳﻦ ﺭﻓﺮﺍﻧﺲ ﺳﻴﻨﻮﻧﺎﺯﻭﻟﻮﮊﻱ ﺩﺭ ﺩﻧﻴﺎ ﻣﻲﺑﺎﺷﺪ. ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ2001 ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺳﻴﻨﻮﺱ ﺑﻪ ﺗﺎﻟﻴﻒ ﺁﻗﺎﻱ ﺩﻛﺘﺮ ﺩﻳﻮﻳﺪﻛﻨﺪﻱ ﻣﺤﺼﻮﻝ ﺳﺎﻝtext book ، CD ﺩﺭ ﺍﻳﻦ 15.2 Endoscopic Sinus Surgery (SALEKAN-eBook) ﺁﺷﻨﺎﻳﻲ ﺷﻤﺎ ﺷﺎﻣﻞ ﺍﺑﺘﺪﺍﻳﻲﺗﺮﻳﻦ ﻣﺴﺎﺋﻞ ﻣﻦﺟﻤﻠﻪ ﺍﺑﺰﺍﺭﺁﻻﺕ ﺑﻜﺎﺭ ﺭﻓﺘﻪ ﺩﺭ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺁﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﺳﻴﻨﻮﺱ ﻭ ﺣﺘﻲ ﻧﺤﻮﺓ ﺍﻳﺴﺘﺎﺩﻥ ﻳﺎ. ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﻃﺒﻘﻪﺑﻨﺪﻱ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﺷﻤﺎ ﺑﺎ ﻓﻴﻠﺪ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺁﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺳﻴﻨﻮﺳﻲ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪCD ﺩﺭ ﺍﻳﻦ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــــ ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
12 ( ﺑـﻪAtlas and textbook) ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﺟﺮﺍﺣﻲ ﺁﻧﺪﻭﺳﻜﻮﭘﻴﻚ ﺳﻴﻨﻮﺱﻫﺎﻱ ﭘﺎﺭﺍﻧﺎﺯﺍﻝ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺮﺗﺒﻂ ﺑﺎ ﺍﻧﻬﺎ ﺑﻪ ﺻﻮﺭﺕ ﻣﺘﻦ ﻭ ﮔـﺮﺍﻑ. ﻣﺒﺎﻧﻲ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻭ ﺩﺍﻳﺴﻜﺸﻦ ﺑﺮﺍﻱ ﺷﻤﺎ ﺗﺸﺮﻳﺢ ﻣﻲﺷﻮﺩ.ﻧﺸﺴﺘﻦ ﻫﻨﮕﺎﻡ ﻋﻤﻞ ﻭ ﮔﺮﻓﺘﻦ ﺍﺑﺰﺍﺭ ﺩﺭ ﺩﺳﺖ ﻫﻢ ﻣﻲﺷﻮﺩ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﻓﺼﻮﻝ ﺍﻳﻦ.ﺷﻤﺎ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ 1- Consistent and Relible Anatomical Landmarks in Endoscopic Sinus Surgery
2- Surgical Instrumentation
3- Setup and patient positioning
4- Basic Dissection
5- Advanced Dissection
16.2 ENDONASAL SINUSECTOMY WITH CORRECTION OF THE NASAL CAVITY (Rikio Ashikawe, Takashi Ohmae, Toshio Ohnisshi, Yutaka Uchida)
ــــــ
The Endonasal sinusectomy with correction of the nasal cavity (Takahash's methodn) is carried out in seven steps. 17.2 Endoscopic Sinus Surgery NEW HORIZONS (Nikhil J. Bhatt, M.D.)
ــــــ
18.2 EVIDENCE-BASED OTITIS MEDIA (Richard M. Rosenfeld, MD, MPH, Charles D. Bluestone, MD)
ــــــ
ﺩﺭﻣـﺎﻥﻫـﺎﻱ ﺩﺍﺭﻭﻳـﻲ ﻭ ﺟﺮﺍﺣـﻲ ﺁﻥ، ﺗﺸﺨﻴﺺ، ﻋﻼﺋﻢ ﻭ ﻣﺴﻴﺮ ﺑﺎﻟﻴﻨﻲ، ﺁﺷﻨﺎﻳﻲ ﺍﺯ ﻣﺴﺎﺋﻞ ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻳﻚ ﻭ ﺗﺤﻘﻴﻘﺎﺕ ﺍﻧﺠﺎﻡ ﺷﺪﻩ ﺁﻏﺎﺯ ﺷﺪﻩ ﻭ ﺩﺭ ﺍﺩﺍﻣﻪ ﺑﻪ ﻣﻮﺷﻜﺎﻓﻲ ﺩﺭ ﻣﻮﺭﺩ ﺍﻧﻮﺍﻉ ﺍﺗﻴﻮﻟﻮﮊﻱ. ﺷﻤﺎ ﺑﺎ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻭﺗﻴﺖ ﻣﺪﻳﺎ ﺑﻪ ﺻﻮﺭﺗﻲ ﺍﺻﻮﻟﻲ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪCD ﺩﺭ ﺍﻳﻦ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﻓﺼﻮﻝ ﺍﻳﻦ. ﺩﺭ ﺿﻤﻦ ﺍﺛﺮﺍﺕ ﺍﻳﻦ ﺑﻴﻤﺎﺭﻱ ﺭﻭﻱ ﺗﻜﺎﻣﻞ ﻛﻮﺩﻙ ﻭ ﻛﻴﻔﻴﺖ ﺯﻧﺪﮔﻲ ﺍﻭ ﻧﻴﺰ ﺗﺸﺮﻳﺢ ﻣﻲﮔﺮﺩﺩ. ﺩﺭ ﺍﻧﺘﻬﺎ ﻧﺘﺎﻳﺞ ﺩﺭﻣﺎﻥ ﺑﺮﺭﺳﻲ ﻣﻲﺷﻮﺩ.ﻣﻲﭘﺮﺩﺍﺯﺩ 1- Methodology
2- Clinical Management
19.2 Facial Plastic & Reconstructive Surgery 20.2 Facial Nerve Surgery (Jack L. Pulec, M.D.)
3- Consequences and Sequelae
(Terence M. Davidson, MD) (VCD I , II)
ــــــ
Otologic Medical Group, Inc. Los Angeies
ــــــ
21.2 Head and Neck Surgery (Jatin P Shah, MD, MS (Surg), FACS) (Mosby)
ــــــ
22.2 Introduction to Ear Acupuncture (Martin Franke)
2001
ﺁﻣﻮﺯﺵ ﺍﺯ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻧﻮﺍﺣﻲ ﻣﺨﺘﻠﻒ ﻣﻮﺭﺩﻧﻈﺮ ﺩﺭ ﻃﺐ ﺳﻮﺯﻧﻲ ﮔﻮﺵ ﺁﻏﺎﺯ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺑﺎ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻃـﺐ. ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﺷﻤﺎ ﺑﺎ ﺍﺻﻮﻝ ﻛﻠﻲ ﻃﺐ ﺳﻮﺯﻧﻲ ﮔﻮﺵ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪThieme ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﻣﺎﺭﺗﻴﻦ ﻓﺮﺍﻧﻚ ﺗﻬﻴﻪ ﻭ ﺗﻮﺳﻂ ﺍﻧﺘﺸﺎﺭﺍﺕ ﻣﻌﺘﺒﺮCD ﺩﺭ ﺍﻳﻦ . ﺍﺩﺍﻣﻪ ﻣﻲﻳﺎﺑﺪ ﺳﭙﺲ ﺷﻤﺎ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻧﮕﺎﻫﻲ ﺑﻪ ﻧﺘﺎﻳﺞ ﺍﻳﻦ ﺍﻋﻤﺎﻝ ﻫﻢ ﺩﺍﺷﺘﻪ ﺑﺎﺷﻴﺪ ﻭ ﺁﻧﻬﺎ ﺭﺍ ﺍﺭﺯﻳﺎﺑﻲ ﻧﻤﺎﺋﻴﺪ... ﺍﻋﺘﻴﺎﺩ ﺑﻪ ﺳﻴﮕﺎﺭ ﻭ، ﺳﺮﮔﻴﺠﻪ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺧﻮﺍﺏ،ﺳﻮﺯﻧﻲ ﺩﺭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺨﺘﻠﻒ ﻫﻤﭽﻮﻥ ﻣﻴﮕﺮﻥ 1- Localization Assignment
2- Localization Determination
3- Treatment
4- Evaluation
23.2 La Rhinoplastica Ragionata (Valerio Micheli-Pellegrini, Roberto Polselli)
ــــــ
24.2 Nasal Aesthetics and Anatomy: A Cadaver Study (Rollin K. Daniel, M.D.)
ــــــ
25.2 Open Tip Graft in Twin Patient (Rollin K. Daniel, M.D.)
ــــــ
26.2 OPEN RHINOPLASTY Cadaver Dissection Program (Dean M. Toriumi, MD.) (Vol I , II) (College of Medicine at Chicago)
ــــــ
Analysis, Operative Planning, Twins Pre and Post, Anesthesia, Transfixion Incision, Septal Harvest, Open Approach, Exposure, Tip Anatomy, Tim Strips, Graft Preparation, Radix Graft, Crural Strut, Domal Excision, Graft, Shaping, Graft, Insertion, Closure, Post Op Result, Credits 1- Access to nasal Septum - Hemitrans Fixatu incision - Havvestiong Septal Cartilage
3- Open Rhinoplasty approach - Incisions - Flap Elevation
5- Management of Middle Nasal Vault - Division of apper Lateral Cartilages from septum - Application of Spreader grafts
2- Havvestiog of Conchal Cartilage - Anterior approach for harvestiog Cartilage - Flap elevention - Cartilage excision - Closure and dressing
4- Stractural grafts used in Secondary - loteral Crural grafts - Alar Batten grafts
6- Major septal reconstruction - Reconstraction of L-Shaped Septal Strat
7- Management of Lower third of the nose - Cephalic trimming of lateral Crura - Satured – in – place Collamellar Strut - Transdomal Sutur - Sutured – in – place tip 8- Chin augmentation - Preparation of the implant - Incision and dissection - placement of Implant
27.2 Open Structure Rhinoplasty (A Case Oriented Approach)
2005
28.2 Otorhinolaryngology Head and Neck Surgery
2003
Otology and Neurotology
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(SIXTEENTH EDITION) (James B, Snow Jr, MD, John Jacob Ballenger, MD,)
Facial Plastic and Reconstructive Surgery
Pediatric Otolaryngology
Rhinology
Bronchoesphagology
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
Laryngology
Head and Neck Surgery
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
13 ــــــ
)29.2 Plastic Surgery (Fifth Edition) (Grabb and Smith's) (Salekan E-Book
ــــــ
ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻣﺸﺘﻤﻞ ﺑﺮ ٩٢ﻓﺼﻞ ﺩﺭ ٧ﻗﺴﻤﺖ ،ﻛﺘﺎﺑﻲ ﻛﺎﻣﻞ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﺩﺭ ﺗﻤﺎﻡ ﻣﺒﺎﺣﺚ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﻣﻨﻈﻮﺭ ﻋﻼﻗﻤﻨﺪﻱ ﺑﻪ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺩﺭ ﺗﻤﺎﻡ ﺳﻄﻮﺡ ﺁﻣﻮﺯﺵ ﻭ ﺩﺭﻣﺎﻥ ﭘﺰﺷﻜﻲ ﻣﻲﺑﺎﺷﺪ ﻭ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﻣﻲﺑﺎﺷﺪ .ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ﺍﻳﻦ ﻛﺘﺎﺏ ﻫﻤﭽﻨﻴﻦ ﺑﺮﺍﻱ ﺍﻣﺘﺤﺎﻧﺎﺕ ﻭ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺑﻮﺭﺩ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺁﻣﺮﻳﻜﺎ ﺳﻮﺩﻣﻨﺪ ﺍﺳﺖ. ﺑﺨﺶ ﺍﻭﻝ General Reconstruction :ﺑﻮﺩﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﺗﺮﻣﻴﻢ ﺯﺧﻢ ،ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﻭﻟﻴﺔ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺁﻧﺸﺮﻱ ، implants ،ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ flapﻭ graftﻭ ...ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ ﺩﻭﻡ :ﺑﻪ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺩﺭ ﭘﻮﺳﺖ ﻣﻲﭘﺮﺩﺍﺯﺩ ﻛﻪ ﺷﺎﻣﻞ ﭼﮕﻮﻧﮕﻲ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺗﻮﻣﻮﺭﻫﺎﻱ ﭘﻮﺳﺖ ،ﺧﺎﻝﻫﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ،ﺟﺮﺍﺣﻲ ﺑﺎ Mothsﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﺩﺭ ﭘﻮﺳﺖ ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ ﺳﻮﻡ :ﺑﻪ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﺳﺮ ﻭ ﮔﺮﺩﻥ ﻣﻲﭘﺮﺩﺍﺯﺩ ﻣﺎﻧﻨﺪ )ﺍﺻﻼﺡ ﺩﻓﺮﻳﺘﻤﻲﻫﺎﻱ ﺳﺮ ﻭ ﺻﻮﺭﺕ ،ﺍﺗﻮﭘﻼﺳﻤﻲ Reconstruction ،ﺑﻴﻨﻲ ،ﮔﻮﺵ ﻭ ﮔﻮﻧﻪ ﻭ ﻟﺐ ﻭ (...ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ ﭼﻬﺎﺭﻡ :ﺟﺮﺍﺣﻲﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ ، dermabrasion, peeling) :ﺗﺰﺭﻳﻖ ﻛﻼﮊﻥ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ،ﻟﻴﭙﻮﺳﺎﻛﺸﻦ (...endoscopic plastic surgery ،ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ ﭘﻨﺠﻢ :ﺟﺮﺍﺣﻲﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﻭ ﺗﺮﻣﻴﻤﻲ breastﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﻛﻪ ﺷﺎﻣﻞ :ﻣﺎﻣﻮﭘﻼﺳﺘﻲ ،ﻛﻤﭙﻠﻴﻜﺎﺳﻴﻮﻥ ،ﺗﺼﻴﺤﻴﺤﻲ ﮊﻳﻨﻜﻮﻣﺎﺳﺘﻲ ﻭ ...ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ. ﺑﺨﺶ ﺷﺸﻢ :ﺍﻳﻦ ﻗﺴﻤﺖ ﺑﻪ ﺟﺮﺍﺣﻲ ﺗﺮﻣﻴﻤﻲ ﺩﺳﺖ ﺍﺧﺘﺼﺎﺹ ﺩﺍﺭﺩ. ﺑﺨﺶ ﻫﻔﺘﻢ :ﻣﺮﺑﻮﻁ ﺑﻪ ﻧﺎﺣﻴﺔ ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻨﻲ ﻭ ﺗﻨﻪ ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ :ﺩﺭﻣﺎﻥ ﺯﺧﻢ ﺑﺴﺘﺮ Reconstruction ،ﺩﻳﻮﺍﺭﺓ ﺷﻜﻢ ﻭ ..... ﺑﺨﺶ ﻫﺸﺘﻢ :ﺑﺤﺚ ﻧﺎﺣﻴﺔ ﮊﻧﻴﺘﺎﻟﻴﺎ ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ :ﺩﺭﻣﺎﻥ ﻫﻴﭙﻮﺳﭙﺎﺩﻳﺎﺱ ﻭ Reconstruction of peniﻭ.... ﻣﺆﻟﻔﻴﻦ ﻛﺘﺎﺏ ﺍﺯ ﺑﺮﺟﺴﺘﻪ ﺗﺮﻳﻦ ﭘﻴﺸﮕﺎﻣﺎﻥ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﺩﺭ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﻣﻲﺑﺎﺷﻨﺪ Fitzpatrickﻭ Goldmanﻫﻤﺮﺍﻩ ﺑﺎ Alsterﺳﻪ ﺗﻦ ﺍﺯ ﻣﻄﺮﺡﺗﺮﻳﻦ ﺍﺷﺨﺎﺹ ﺩﺭ ﻣﺒﺎﺣﺚ ﻟﻴﺰﺭﻱ ﻣﻲﺑﺎﺷﻨﺪ .ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ :ﻣﺎ ﺳﻌﻲ ﻛﺮﺩﻩ ﺍﻳﻢ ﻳﻜﺒﺎﺭ ﺩﻳﮕﺮ ﺍﻛﺜﺮ ﺗﺤﻘﻴﻘـﺎﺕ ﻭ ﺩﺍﻧﺶ ﻛﺎﺭﺑﺮﺩ ﻟﻴﺰﺭ ﺩﺭ ﭘﻮﺳﺖ ﺭﺍ ﺩ ﺍﺧﻞ ﻳﻚ ﻛﺘﺎﺏ ﮔﺮﺩﺁﻭﺭﻱ ﻛﻨﻴﻢ .ﻣﺒﺎﺣﺚ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﻃﻮﺭ ﺗﺨﺼﺼﻲ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﺓ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖ ﻫﺎ ﻭ ﺟﺮﺍﺣﺎﻧﻲ ﻛﻪ ﺩﺭ ﺯﻣﻴﻨﺔ rejuvenationﭘﻮﺳﺖ ﺻﻮﺭﺕ ﻓﻌﺎﻟﻴﺖ ﺩﺍﺭﻧﺪ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺳﺖ. )30.2 Primary Rhinoplasty (Bahman Guyuron, MD, FACS, Cleveland, Ohio) (VCD ﺩﺭ ﺍﻳﻦ VCDﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﻳﻜﻲ ﺍﺯ ﺑﺰﺭﮔﺘﺮﻳﻦ ﺟﺮﺍﺣﺎﻥ ﺻﺎﺣﺐ ﻧﺎﻡ ﺩﻧﻴﺎ ،ﺍﺯ ﻛﺸﻮﺭ ﻋﺰﻳﺰﻣﺎﻥ ﺍﻳﺮﺍﻥ ،ﺑﻪ ﻧﺎﻡ ﺁﻗﺎﻱ ﺩﻛﺘﺮ ﺑﻬﻤﻦ ﻏﻴﻮﺭﺍﻥ ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩ Ohioﺗﻬﻴﻪ ﺷﺪﻩ ﺍﺳﺖ ،ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻳﻚ ﻋﻤﻞ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺍﻭﻟﻴﻪ ﺑﺎ ﺍﭘﺮﻭﺝ Openﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﻣﻮﺭﺩ ﻋﻤﻞ ﺩﺧﺘﺮ ﺟﻮﺍﻧﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ Caseﻓﻮﻕﺍﻟﻌﺎﺩﻩ ﻣﺸﻜﻠﻲ ﺩﺭ ﺯﻣﻴﻨﻪ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﻣﺤﺴﻮﺏ ﺷﺪﻩ ﻭ ﺁﻗﺎﻱ ﺩﻛﺘﺮ ﻏﻴﻮﺭﺍﻥ ﭘﺲ ﺍﺯ ﺁﻧﺎﻟﻴﺰ ﻛﺎﻣﻞ ﻧﺎﺯﻭﻓﺎﺷﻴﺎﻝ ﺟﺮﺍﺣﻲ ﺭﺍ ﺑﺎ ﻇﺮﺍﻓﺖ ﻫﺮ ﭼﻪ ﺗﻤﺎﻣﺘﺮ ﺍﺯ ﺍﺑﺘﺪﺍﻱ ﺍﻣﺮ )ﺗﺰﺭﻳﻖ ﻭ ﺑﻲﺣﺴﻲ ﺗﻮﭘﻴﻜﺎﻝ( ﺗﺎ ﺍﻧﺘﻬﺎ )ﭘﺎﻧﺴﻤﺎﻥ( ﺍﺟﺮﺍ ﻣـﻲﻛﻨﻨـﺪ .ﺩﻳـﺪﻥ ﺍﻳـﻦ VCDﺭﺍ ﺍﻛﻴﺪﹰﺍ ﺑﻪ ﻛﻠﻴﻪ ﻣﺘﺨﺼﺼﻴﻦ ﺗﻮﺻﻴﻪ ﻣﻲﻛﻨﻴﻢ. )A Practical Guide to functional and asthetic surgery of the nose (G. J. Nolst
ــــــ
31.2 RHINOPLASTY
ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﻧﻮﻟﺴﺖ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ .ﺭﺍﻫﻨﻤﺎﻳﻲ ﻋﻤﻠﻲ ﺟﻬﺖ ﺟﺮﺍﺣﻲ ﻓﺎﻧﻜﺸﻨﺎﻝ ﻭ ﺍﺳﺘﺎﺗﻴﻚ ﺑﻴﻨﻲ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺍﻳﻦ ﻓﻴﻠﻢ ﺍﺻﻮﻝ ﭘﺎﻳﻪ ﺯﻳﺒﺎﻳﻲﺷﻨﺎﺳﻲ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ ،ﺍﺯ ﻣﺮﺍﺣﻞ ﭘﺎﻳﻪ )ﺍﺯ ﺗﻜﻨﻴﻚ ﺗﺎ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ( )ﺗﺤﺖ ﺑﻲﻫﻮﺷﻲ ﻋﻤﻮﻣﻲ( ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. ﺩﺭ ﺍﻳﻦ ﻓﻴﻠﻢ ﺗﻮﺟﻪ ﺷﻤﺎ ﺭﺍ ﺑﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﺍﺳﺘﺌﻮﺗﻮﻣﻲ ﺍﺯ ﺭﺍﻩ ﭘﻮﺳﺖ ﻭ ﻧﻴﺰ ﺣﻔﻆ ﺳﺎﭘﻮﺭﺕ tipﺟﻠﺐ ﻣﻲﻛﻨﻴﻢ .ﺩﺭ ﺍﻧﺘﻬﺎ ﺍﺯ ﻏﻀﺮﻭﻑ ﻛﻮﻧﻜﺎﻱ ﮔﻮﺵ ﺑﻴﻤﺎﺭ ،ﮔﺮﺍﻓﺖ )ﺷﻴﻠﺪ ﻳﺎ ﺍﺳﺘﺮﺍﺕ ﻛﻠﻮﻣﻼ( ﺗﻬﻴﻪ ﻣﻲﺷﻮﺩ ﻭ ﺑﺮﺍﻱ ﻗﺮﺍﺭﺩﺍﺩﻥ ﺁﻥ ﺍﺯ ﺍﭘﺮﻭﭺ openﻛﻤﻚ ﮔﺮﻓﺘﻪ ﻣﻲﺷﻮﺩ. ﺩﺭ ﻫﺮ ﻓﺼﻞ ﺍﺑﺘﺪﺍ ﺑﻪ ﺻﻮﺭﺕ textﺗﻮﺿﻴﺤﺎﺗﻲ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﻭ ﻓﻴﻠﻢ ﻣﺮﺑﻮﻁ ﺑﻪ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺁﻥ ﺑﺨﺶ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻮﻝ ﺍﻳﻦ CDﺷﺎﻣﻞ: : Basic Knowledgeﺷﺎﻣﻞ ﺁﻧﺎﺗﻮﻣﻲ ،ﺯﻳﺒﺎﺋﻲﺷﻨﺎﺧﺘﻲ Pre-opﻭ Post-opﻭ ﻛﻤﭙﻠﻴﻜﺎﺳﻴﻮﻥﻫﺎ ﻭ ﻧﺤﻮﺓ ﺑﻲﺣﺴﻲ ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢ ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ. : Operative techniquesﺑـﻪ ﺷـﻴﻮﻩﻫـﺎﻱ ﻋﻤـﻞ ﺳـﭙﺘﻮﭘﻼﺳـﺘﻲ ﻭ turbinate surgeryﮔﺮﺍﻓـﺖﻫـﺎ ،Spreadergrafs modified zplasty-Nasalvalve surgery ،ﺟﺮﺍﺣـﻲ osseocartileginousﺭﻳﻨﻮﭘﻼﺳـﺘﻲ ، external rhinoplasty ، Open Wedgeresection in alar base surgeryﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ. : Capita selectaﻓﺼﻞ ﺁﺧﺮ ﺑﻪ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺳﺎﺧﺘﻤﺎﻧﻲ ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ ﻣﺎﻧﻨﺪ ﺗﺼﺤﻴﺢ ﺷﻜﺎﻑ ﻟﺐ ﻭ ﺑﻴﻨﻲ rhinosurgery ، augmentation rhinoplasty ،ﺩﺭ ﻛﻮﺩﻛﺎﻥ Revision surgery ،ﺗﺼﺤﻴﺢ Pverprojected nasel tip. Saddle noseﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ.ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ CDﺁﺳﺎﻥ ﺑﻮﺩﻩ ﻭ ﺩﺍﺭﺍﻱ Video galleryﺷﺎﻣﻞ :ﻧﺸﺎﻥ ﺩﺍﺩﻥ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﻛﻮﺩﻛﺎﻥ ﻭ ﺍﭘﺮﻭﭺﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﺮﺍﻱ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ )ﺍﻛﺴﺘﺮﻧﺎﻝ ﻭ ( ...ﻣﻴﻜﺮﻭﺍﺳﺘﺌﻮﺗﻮﻣﻲ ﻭ Conchal Cartilage harvestingﻣﻲﺑﺎﺷﺪ. ــــــ
)(ROBERT L. SIMONS, MD., NORTH MIAMI BEACH, FLORIDA) (VCD) (CD I , II
GOLDMAN TECHNIQUE
32.2 RHINOPLASTY
ﺩﺭ ﺍﻳﻦ VCDﺁﻣﻮﺯﺷﻲ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻋﻤﻞ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﺳﻴﻤﻮﻥ ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩ ﻣﻴﺎﻣﻲ ﺗﺸﺮﻳﺢ ﻣﻲﺷﻮﺩ .ﻋﻤﺪﻩ ﻫﺪﻑ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﺼﺤﻴﺢ tipﺑﻴﻤﺎﺭ ) (tip plastyﺑﺎ ﻛﻤﻚ ﺗﻜﻨﻴﻚ ﮔﻠﺪﻣﻦ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻓﻮﻕ ﺑﺮﺍﻱ ﺗﺸﺮﻳﺢ ﺗﻜﻨﻴﻚ ﻳـﻚ Caseﻛﻪ ﺧﺎﻧﻢ ٢٧ﺳﺎﻟﻪﺍﻱ ﻣﻲﺑﺎﺷﺪ ﺗﺤﺖ ﻋﻤﻞ ﺑﺎ ﺑﻲﻫﻮﺷﻲ Stand byﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩ .ﺑﻴﻨﻲ ﺑﻴﻤﺎﺭ ﺍﺯ ﻧﻮﻉ projected tipﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺍﺑﺘﺪﺍ ﻳﻚ ﺁﻧﺎﻟﻴﺰ ﻛﺎﻣﻞ ﺍﺳﺘﺎﺗﻴﻚ ﻧﺎﺯﻭﻓﺎﺷﻴﺎﻝ ﺍﺯ ﺑﻴﻤﺎﺭ ﺑﻪ ﻋﻤﻞ ﻣﻲﺁﻳﺪ. ــــــ
)33.2 Rhinoplasty The American Academy of Facial Plastic and Reconstructive Surgery (CD I, II) (E. Gaylon McCollough, M.D.) (the St. Louis Aging Face Symposium
ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﺔ ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ) (E. Gaglon McCollough M.D.ﺩﺭ ﺳﻤﭙﻮﺯﻳﻮﻡ Aging Faceﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ،ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻳﻚ ﻋﻤﻞ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺑﺮ ﺭﻭﻱ ﺑﻴﻤﺎﺭ ﻣﻴﺎﻧﺴﺎﻝ ﺗﺤﺖ ﺑﻲﻫﻮﺷﻲ Stand byﺑﻪ ﺗﻔﻜﻴﻚ ﺑﻴﺎﻥ ﻭ ﺍﺟﺮﺍ ﻣﻲﺷـﻮﺩ .ﺩﺭ ﺍﻳـﻦ ﻋﻤـﻞ ﺍﺯ ﺍﭘﺮﻭﭺ Closedﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺑﻴﺸﺘﺮﻳﻦ ﺗﻮﺟﻪ ﺭﻭﻱ tip plastyﻣﻲﺑﺎﺷﺪ .ﺑﺮ ﺭﻭﻱ tipﺑﻴﻨﻲ ﺍﻳﻦ ﺑﻴﻤﺎﺭ ،ﺍﻓﺰﺍﻳﺶ rotationﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﺍﺯ ﺭﻭﺵ deliveryﺟﻬﺖ ﺗﺮﻣﻴﻢﻛﺮﺩﻥ ﻗﺴﻤﺖ ﺳﻔﺎﻟﻴﻚ ﻏﻀﺮﻭﻑﻫﺎﻱ LLCﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩ. ﺩﺭ ﻧﻬﺎﻳﺖ ﺑﺮﺍﻱ ﺑﻴﻤﺎﺭ Alar base resectionﺍﻧﺠﺎﻡ ﺷﺪﻩ ﻭ ﭘﺎﻧﺴﻤﺎﻥ ﻣﺨﺼﻮﺹ ﻭ ﺟﺎﻟﺐ ﻣﻮﻟﻒ ﺑﺮ ﺭﻭﻱ ﺻﻮﺭﺕ ﺑﻴﻤﺎﺭ ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. )34.2 RHINOPLASTY DOUBLE DOME UNIT (CD I , II) (E. Gaylon McCollough MD, Birmingham, Albama
ــــــ
ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﺔ ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ E. Gaglon MC Collouchﺍﺯ ﺩﺍﻧﺸﮕﺎﻩ ﺑﻴﺮﻣﻨﮕﺎﻡ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ .ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻋﻤﻞ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺑﺮ ﺭﻭﻱ ﺧﺎﻧﻤﻲ ﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩ ﻛﻪ ﻣﺸﻜﻞ ﺁﻥ ﻋﻤﺪﺗﹰﺎ ﺩﺭ ﻧﺎﺣﻴﻪ tipﺑﻮﺩﻩ ﻭ ﻫﺪﻑ ﻋﻤﺪﻩ ﺟﻤﻊ ﻛﺮﺩﻥ ﺁﻥ ﺍﺳﺖ .ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻧﮕﺮﺷﻲ ﺑﻪ Double Dome Unitﻭ ﻧﺤﻮﺓ managementﺁﻥ ﺍﺳﺖ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
14 35.2 Rhinoplasty The Overly Projected Nasal Tip
(Trent W. Smith, M.D.F.A.C.S.)
ــــــ
، ﺑﻴﻨـﻲtip ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﺑﻠﻨﺪﺑﻮﺩﻥ ﻃﻮﻝ ﻣﻮﻳﺎﻝ ﻛﺮﻭﺭﺍﻫﺎ ﺑﻪ ﻋﻨﻮﺍﻥ ﻋﻠﺖ ﺑﺮﭼﺴﺘﻪ ﺑـﻮﺩﻥ. ﺑﺮﺟﺴﺘﻪ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﻋﻤﻞ ﺑﺮ ﺭﻭﻱ ﻳﻚ ﺑﻴﻤﺎﺭ ﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩtip ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﺔ ﺁﻣﻮﺯﺷﻲ ﻣﺘﺮﻭﻟﻮﮊﻱ ﻭ ﻧﺘﺎﻳﺞ ﻛﻠﻴﻨﻴﻜﻲ ﺭﻳﻨﻮﭘﻼﺳﺘﻲ ﺩﺭ ﺑﻴﻨﻲﻫﺎﻱ ﺑﺎ . ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﻮﺳﻂ ﺁﻗﺎﻱ ﺩﻛﺘﺮ ﺍﺳﻤﻴﺖ ﺍﺳﺘﺎﺩ ﻭ ﻣﺪﻳﺮ ﮔﺮﻭﻩ ﺑﺨﺶ ﮔﻮﺵ ﻭ ﺣﻠﻖ ﻭ ﺑﻴﻨﻲ ﻭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺩﺍﻧﺸﮕﺎﻩ ﺍﻭﻫﺎﻳﻮ ﺍﺭﺍﺋﻪ ﺷﻮﺩ.ﺗﻼﺵ ﺩﺭ ﺟﻬﺖ ﻛﻮﺗﺎﻩ ﺑﻮﺩﻥ ﻃﻮﻝ ﺁﻧﻬﺎ ﺩﺭ ﺟﻬﺖ ﺍﺻﻼﺡ ﺍﻳﻦ ﺑﺮﺟﺴﺘﮕﻲ ﺍﻧﺠﺎﻡ ﻣﻲﺷﻮﺩ 36.2 SURGERY of the EAR
2003
(Fifth Edition) (Glasscock-Shambaugh) (Michael E. Glasscock III, MD, FACS, Aina Julianna Gulya, MD)
: ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ. ﻛﺘﺎﺏ ﺷﺎﻣﭙﻮ ﻳﻜﻲ ﺍﺯ ﻣﻌﺘﺒﺮﺗﺮﻳﻦ ﺭﻓﺮﺍﻧﺲﻫﺎﻱ ﺟﺮﺍﺣﻲ ﮔﻮﺵ ﺩﺭ ﺩﻧﻴﺎ ﻣﻲﺑﺎﺷﺪ.( ﺑﻪ ﺷﻤﺎ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ2003) ﺍﻭﻳﺸﻦ ﭘﻨﺠﻢ، ﺟﺮﺍﺣﻲ ﮔﻮﺵ ﺷﺎﻣﭙﻮـ ﮔﻼﺳﻜﻮtextbook . CD ﺩﺭ ﺍﻳﻦ
37.2
1- Scientific Foundations
3- Clinical Evaluation
5- Fundametals of Otologic/Neurotologic Surgery
7- Surgery of the External Ear
2- Surgery of the Tympanomastoid Compartment
4- Surgery of the Inner Ear
6- Surgery of the IAC/CPA/Petrous Apex
8- Surgery of the Skull Base
The MEDPOR Lower Eyelid Spacer (James Patrinely, M.D.F.A.C.S., and Charles N.S. Soparkar, M.D., Ph.D.) (VCD)
ــــــ
. ﺍﻳﻦ ﺁﺷﻨﺎﻳﻲ ﺩﺭ ﻏﺎﻟﺐ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ. ﺷﻤﺎ ﺑﺎ ﭘﺮﻭﺗﺰﻫﺎﻱ ﻣﺪﭘﻮﺭ ﭘﻠﻚ ﺗﺤﺘﺎﻧﻲ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﺪ، ﺁﻣﻮﺯﺷﻲ ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﭘﺎﺗﺮﻳﻨﻠﻲ ﻭ ﺩﻛﺘﺮ ﺳﻮﭘﺎﺭﻛﺎﺭ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩVCD ﺩﺭ ﺍﻳﻦ 3) Medpore biomaterial
2) Addressing and management potential Complications - managing winging are edge flare - managing ridging - managing under correction - managing overcorrection - managing implant exposure - managing entropion - managing entropion - Implant exchange
1) Introduction and Surgical technique - Cartilage grafts - Non-rigid spacer grafts (hard Patale/Sclera,dermis) - Medpore Lower Lid Advantages
38.2 The MEDPOR Nasal Shell Implant (Paul O'Keefe, M.B, B.S., (SYD), F.R.C.S., F.R.A.C.S.) (VCD)
ــــــ
39.2 VCD Journal of ENT APPROACH VESTIBULAR NEURECTOMY-TRANSTEMPORAL SUPRALABYRINTHINE APPROACH
ــــــ
MICROSURGERY OF THE SKULL BASE TRANSOTIC APPROACH ACOUSTIC NEUROMA (Prof. U. Fisch Zurich) (VCD#2) 40.2 VCD Journal of ENT INFRATEMPORAL FOSSA APPROACH TYPE C
(Prof. U. Fisch Zurich) (VCD#4)
ــــــ
41.2 VCD Journal of ENT INFRATFMPORAL FOSSA APPROACH GLOMUS TEMPORALE TUMOR (Prof. U. Fisch Zurich) (VCD#1)
ــــــ
42.2 VCD Journal of ENT MICROSURGERY OF THE SKULL BASE TRANSOTIC APPROACH ACOUSTIC NEUROMA-INFRATEMPORAL FOSSA APRROACH TYPE C (Prof. U. Fisch Zurich) (VCD#3)
ــــــ
43.2 VJGS Invited Presentation: Thyroidectomy (Jon A. van Heerden, ND)
ــــــ
44.2 San Diego Classics in Soft Tissue & Cosmetic Surgery Rhinoplasty (Part 1-6) (Richard C. Webster, MD, Terence M. Davidson, Alan M. Nahum)
ﺯﻧﺎﻥ ﻭ ﻣﺎﻣﺎﺋﻲ-٣
CD ﻋﻨﻮﺍﻥ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــــ
1.3
Abdominal Colposacropexy and Vaginal Sacropinus Suspension (Harold P. Drutz MD FRCS (C) (VCD)
2.3
Adapted form Physical Examination and Health Assessment, 2/e (Carolyn Jarvis, RN, C, MSN, FNP) (W.B. Saunders Company) (VCD)
ــــــ
3.3
Advanced Colposcopy: Understanding Vessel Patterns (Dorothy M. Babo, MD) (VCD)
ــــــ
: ﺗﻐﻴﻴﺮ ﻛﻮﻟﭙﻮﺳﻜﻮﭘﻲ ﺑﻪ ﺩﻭ ﻓﺎﻛﺘﻮﺭ ﻣﻬﻢ ﻧﻴﺎﺯ ﺩﺍﺭﺩ: ﺩﺭ ﻣﻮﺭﺩVJOG ﺍﺯ ﺳﺮﻱCD ﺍﻳﻦ ﻭﻳﺪﺋﻮ . ﺩﺍﻧﺶ ﺍﻟﮕﻮﻫﺎﻱ ﻧﺮﻣﺎﻝ ﻳﺎ ﺍﺑﻨﺮﻣﺎﻝ ﺳﺮﻭﻳﻜﺲ-٢ ﻧﮕﺮﺵ ﺩﻗﻴﻖ-١ ( ﻭ ﺍﻓﺘﺮﺍﻕ ﺁﻧﻬﺎ ﺍﺯ ﻳﻜﺪﻳﮕﺮ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺿﺎﻳﻌﺎﺕ ﻫﻤﺮﺍﻩ ﺑﺎ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲ ﻭ ﺍﺳﻼﻳﺪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖ ﺩﺭ ﻗﺴـﻤﺖ ﺁﺧـﺮ..... ﻛﺮﺍﺗﻴﻦ ﻭ،ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﻓﻴﺰﻳﻚ ﺩﺳﺘﮕﺎﻩ ﻭ ﺳﭙﺲ ﻋﻮﺍﻣﻠﻲ ﻛﻪ ﺩﺭ ﻣﺸﺎﻫﺪﻩ ﺿﺎﻳﻌﺎﺕ ﻣﻮﺛﺮ ﺍﺳﺖ )ﻣﺎﻧﻨﺪ ﺑﺎﺯﺗﺎﺏ ﻧﻮﺭ ﺗﻮﺳﻂ ﻣﻮﻛﻮﺱ .ﺭﻭﺵ ﻛﺎﺭﻛﺮﺩﻥ ﺻﺤﻴﺢ ﺑﺎ ﻛﻮﻟﭙﻮﺳﻜﻮﭖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
15 Advanced Therapy of BRAST DISEASE (S. Eva Singletry, MD, Geoffrey L. Robb, MD) 5.3 American Cancer Society Atlas of Clinical Oncology (Cancer of the Female Lowe Genital Tract) (Patricia J. Eifel, M.D. Charles Levenback, M.D.)
2000
4.3
(SALEKAN E-BOOK)
2001
Cervix ﺁﺧﺮﻳﻦ ﺗﻐﻴﻴﺮﺍﺕ ﺩﺭ ﺩﺭﻣﺎﻥﻫﺎﻱ ﭘﺬﻳﺮﻓﺘﻪﺷﺪﻩ ﺑﺮﺍﻱ ﻛﺎﻧﺴﺮ ﻣﻬﺎﺟﻢ. ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺩﺭﻣﺎﻥ ﻛﺎﻧﺴﺮﻫﺎ ﺩﺳﺘﮕﺎﻩ ﺗﻨﺎﺳﻠﻲ ﺗﺤﺘﺎﻧﻲ ﺯﻧﺎﻥ ﻣﻲﺑﺎﺷﺪ، ﺗﺸﺨﻴﺺ،ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ﺑﻪ ﻣﻨﻈﻮﺭ ﻓﺮﺍﻫﻢﻛﺮﺩﻥ ﻣﺮﻭﺭ ﻭ ﺁﻧﺎﻟﻴﺰ ﺑﻴﻮﻟﻮﮊﻱ
.ﻭ ﻳﻚ ﺑﺎﺯﻧﮕﺮﻱ ﻛﻠﻲ ﺩﺭ ﻫﻤﻪ ﻣﺒﺎﺣﺚ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺷﺪﻩ ﺍﺳﺖ 17- Chemotherapy in Curative Management
13- Surgery for Vulvar Cancer
18- Post-treatment Surveillance
14- Radiation Therapy for Vulvar Cancer
19- Palliative Care
15- Acute Effects of Radiation Therapy 16- Late Complications of Pelvic Radiation Therapy
6.3
9- Surgical Treatment of Invasive Cervical Cancer 10- Radiation Therapy for Invasive Cervical Cancer 11-Radical Management of Recurrent Cervical Cancer
5- Diagnostic Imaging
1- Epidemiology
6- Screening for Neoplasms
2- Pathology
7-Treatment of Squamous Intraepithelial Lesions
3- Molecular Biology
12- Management of Vaginal Cancer
8- Invasive Carcinoma of the Cervix
4- Anatomy and Natural History
Atlas of Clinical oncology Breast Cancer (American Cancer Society ) (David J Winchester, MD, David P Winchester, MD)
2000 : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ
yGenetics, Natural History, and DNA-Based Genetic Counseling in Hereditary Brast Cancer
y Breast Cancer Risk and Management: Chemoprevention, Surgery, and Surveillance
y Screening and Diagnostic Imaging yImaging-Directed y Breast Biopsy yHistophathology of Malignant Breast Disease yUnusual Breast Pathology y Prognostic and Predictive Markers in Breast Cancer y Surgical Management of Ductal Carcinoma In Situ yEvaluation and Surgical Management of Stage I and II Breast Cancer y Locally Advanced Breast Cancer y Breast Reconstruction
7.3
ATLAS OF ENDOSCOPIC TECHNIQUES IN GYNECOLOGY (First Edition) (Jeffrey M. Goldberg, MD, Tommaso Falcone, MD) (©W.B. Saunders, Philadelphia)
2001
:ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ 1234-
8.3 9.3
Instrumentation and Pelvic Anatomy Surgery for Pelvic Support Ovarian Surgery Hysteroscopic Surgery
5- Patient Preparation 6- Surgery for Endometriosis and Pelvic Pain 7- Complications
8- Tubal Surgery 9- New Procedures 10- Uterine Surgery
Atlas of Gynecologic Surgery (3rd edition) (H.A. Hirsch, M.D., O. Käser, M.D., F.A. Iklé, M.D.) (Thieme) Atlas of Transvaginal Surgery (Second Edition) (©W.B. Saunders, Philadelphia) (VCD) - Prolene sling in the treatment of stress incontinence - Transvaginal repair of enterocele and vault prolapse - Excision of urethral diverticula
10.3 COLPOSCOPY
an Interactive
CD-ROM
- Fibro-fatty labial flap (Martius Flat) for vaginal reconstruction - Transvaginal repair of vesico-vaginal fistula using a peritoneal flap - Transvaginal repair of posterior vaginal wall prolapse
(SALEKAN E-BOOK)
- Transvaginal hysterectomy for severe prolapse - Transvaginal repair of grade IV cystocele
(Thomas V. Sedlacek, MD, Charles J. Dunton, MD)
ــــــ 2001
ــــــ
11.3 Core Curriculum in Primary Care Patient Evaluation for Non-Cardiac Surgery and Gynecology and Urology (Michael K. Rees, MD, MPH)
ــــــ
ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳـﻦ. ﺯﻧﺎﻥ ﻭ ﺍﻭﺭﻭﮊﻱ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖ، ﺣﺎﺿﺮ ﺩﺭ ﻣﻮﺭﺩ ﺟﺮﺍﺣﻲCD . ﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖHarvard ﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻧﮓ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲCD ﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯCCC ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻـﻮﺭﺕ ﻳـﻚ ﻣﻘﺎﻟـﻪ ﭼـﺎﭘﻲ ﺩﺭ. ﺳﺆﺍﻻﺕ ﻣﺮﺑﻮﻃﻪ ﺑﻪ ﺻﻮﺭﺕ ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ، ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜﻲ.ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛﺎﺭﺑﺮ ﻣﻲﺑﺎﺷﺪ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ.ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﭼﮕﻮﻧﻪ ﻳﻚ ﺑﻴﻤﺎﺭ ﺭﺍ ﺑﺮﺍﻱ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ )ﺑﺠﺰ ﺟﺮﺍﺣﻲ ﻗﻠﺐ( ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺁﻣﺎﺩﻩ ﻛﻨﻴﻢ؟-١ Male impotence ﻋﻘﻴﻤﻲ ﻣﺮﺩﺍﻥ-٣ .(AUB) ﺍﺭﺯﻳﺎﺑﻲ ﺧﻮﻧﺮﻳﺰﻱﻫﺎﻱ ﺍﺑﻨﺮﻣﺎﻝ ﺭﺣﻢ-٢ 12.3 Core Curriculum in Primary Care Gynecology
(Michael, Isaac Schiff, Keith, Thomas, Annekathryn)
13.3 Danforth's Obstetrics and Gynecology
ــــــ
(James R. Scott) (9 Edition) (SALEKAN E-BOOK) Diagnosis of Benign Breast Disease (Dorothy M. Barbo, MD) (VCD) Submitted Subject The Limits of Laparoscopy: Diapharbmatic Endometriosis (David B. Redwine, MD) 14.3 .( ﻣﻲﺑﺎﺷﺪVideo Journal ob/Gyn) VJOG ﺍﺯ ﺳﺮﻱCD ﺍﻳﻦ ﻭﻳﺪﺋﻮ ﺍﺑﺘﺪﺍ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﺳﭙﺲ ﻃﺮﺯ ﻣﻌﺎﻳﻨﻪ ﻭ ﺍﻓﺘﺮﺍﻕ ﺿﺎﻳﻌﺎﺕ ﺧﻮﺵﺧﻴﻢ ﺍﺯ ﺑﺪﺧﻴﻢ ﺍﺯ ﻃﺮﻳﻖ ﺷﺮﺡ ﺣﺎﻝ ﺑﺎﻟﻴﻨﻲ ﻭ ﻣﺎﻣﻮﮔﺮﺍﻓﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺳﭙﺲ ﺷﻜﺎﻳﺎﺕ ﺷﺎﻳﻊ ﺑﻴﻤﺎﺭﺍﻥ ﺑﻴﺎﻥ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺑﺼﻮﺭﺕ ﺍﻟﮕﻮﺭﻳﺘﻢ ﻃﺮﺯ ﺑﺮﺧﻮﺭﺩ ﻭ ﺍﻧﺠﺎﻡ ﺁﺯﻣﺎﻳﺸﺎﺕ ﻣﺮﺑﻮﻃﻪ ﺩﺭ ﻣﻮﺭﺩCD ﺍﻳﻦ ﻭﻳﺪﺋﻮ.١ . ﺑﻴﻤﺎﺭ ﺑﺎ ﺍﻧﺪﻭﻣﺘﺮﻳﻮﺯ ﻧﺎﺣﻴﻪ ﺩﻳﺎﻓﺮﺍﮔﻢ ﺑﺤﺚ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ٢ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ. ﺩﺭ ﻣﻮﺭﺩ ﻣﺤﺪﻭﺩﻳﺖﻫﺎﻱ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖCD ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ.٢ . ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖSolid ﻭ ﻳﻚ ﺗﻮﺩﻩCyst ﻭnipple discharge ، Mastodynia ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2003 ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
16 )(Suttond & diamond) (second Edition
ــــــ
)(Michael Dixon, Richarc Sainsbury) (Salekan E-book
ــــــ
15.3 Endoscopic Surgery for Gynecologists
)16.3 Handbook of disease of the breast (Second Edition
)17.3 INTERACTIVE COLOR GUIDES Obstetrics Gynecology Neonatology (David James, Mary Pillai, Janice Rymer, Andrew N. J. Fish, Warren Hye
ــــــ ﻋﻨﺎﻭﻳﻦ ﻣﻮﺟﻮﺩ ﺩﺭ
ﺍﻳﻦ CD
ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ:
9. Skin Disorders 10. Low-Birth-Weight Infants
7. Iatrogenic Lesions 8. Surgical Problems
)(Dr G. F. Stohs, MD & Dr. L. P. Johonson, MD
ــــــ
3. Birth Trauma 4. Syndromes
5. Deformations 6. Infection
1. Normal Infant 2. Congennital Abnormalities
?18.3 LAVM: Our First one Hundred Cases; What have We Learned
ﺍﻣﺮﻭﺯﻩ ﻫﻴﺴﺘﺮﻛﺘﻮﻣﻲ ﺑﻪ ﻃﺮﻳﻘﻪ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﻓﺮﺍﮔﻴﺮ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ CDﻣﻮﺭﺑﻴﺪﻳﺘﻲ ﻭ ﻣﻮﺭﺗﺎﻟﻴﺘﻲ ﻭ ﻋﻮﺍﺭﺽ ﺍﻳﺠﺎﺩ ﺷﺪﻩ ﺑﺎ ﺍﻳﻦ ﺭﻭﺵ ﺣﻴﻦ ﻋﻤﻞ ﺩﺭ ١٠٠ﺑﻴﻤﺎﺭ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ.
)Nine Month Miracle (A.D.A.M. Software, Inc.
ــــــ
3. A Child's View of Pregnancy
2. The Family Album
1. Anatomy
19.3
20.3 Obstetric Ultrasound Principles and Techniques
ــــــ
ﺩﺭ ﺍﻳﻦ CDﻣﻄﺎﻟﺐ ﺟﺎﻣﻊ ﻭ ﺍﺭﺯﻧﺪﻩﺍﻱ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﻬﺎﺭﺕﻫﺎﻱ ﻻﺯﻣﻪ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻣﺎﻣﺎﺋﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﻛﻪ ﻋﻨﺎﻭﻳﻦ ﺁﻥ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﺗﻌﻴﻴﻦ ﺳﻦ ﺣﺎﻣﻠﮕﻲ ﺑﺮ ﺍﺳﺎﺱ ﻣﻌﻴﺎﺭﻫﺎﻱ FL . BPDﻭ ACﻭ HCﻭ ﺟﺪﺍﻭﻝ ﺁﻧﻬﺎ ﺑﺮﺭﺳﻲ ﺁﻧﺎﺗﻮﻣﻲ ﺟﻨﻴﻦ ﻭ ﺁﻧﻮﻣﺎﻟﻲﻫﺎﻱ CNSﻭ Body ﺁﻧﺎﺗﻮﻣﻲ ﺭﺣﻢ ﻭ ﺁﺩﻧﻜﺲﻫﺎ ﻭ ﺍﻣﺒﺮﻳﻮ ﻭ ﻛﻴﺴﻪ ﺯﺭﺩﻩ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺍﻭﻝ ﺑﺮ ﺍﺳﺎﺱ Gsﻭ CRLﻭ ﻧﺤﻮﺓ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻧﻬﺎ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ ﺑﺮ ﺍﺳﺎﺱ ﺩﻭﺭ ﺳﺮ ﻭ ﻧﺤﻮﻩ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻥ ﺗﻌﻴﻴﻦ ﺳﻦ ﺑﺎﺭﺩﺍﺭﻱ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ ﺑﺮ ﺍﺳﺎﺱ FLﻭ ACﻭ ﻧﺤﻮﻩ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺁﻧﻬﺎ ﺗﻌﻴﻴﻦ ﻣﺤﻞ ﺟﻔﺖ ﻭ ﺣﺠﻢ ﻣﺎﻳﻊ ﺁﻣﻨﻴﻮﺗﻴﻚ ﻣﻄﺎﻟﺐ ﺟﺎﻟﺒﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺁﻧﺎﺗﻮﻣﻲ ﺟﻨﻴﻦ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ﻭ ﺳﻮﻡ )ﻣﻌﺪﻩ -ﻛﻠﻴﻪ (........ ﺗﻌﻴﻴﻦ ﻣﺤﻞ ﻻﻧﻪﮔﺰﻳﻨﻲ ﺟﻔﺖ ﻭ ﺑﺮﺭﺳﻲ ﺭﻛﻮﻟﻤﺎﻥ ﻭ ﭘﻼﻧﺘﺎﭘﺮﻭﻳﺎ ﺍﻧﻔﺎﺭﻛﺘﻮﺱ ﻭ ﻭﺍﺭﻳﺎﺳﻴﻮﻥ ﻣﺤﻞ ﺧﺮﻭﺝ ﺑﻨﺪ ﻧﺎﻑ )(Cord Insertion ﺑﺮﺭﺳﻲ ﻟﻜﻴﻨﻴﻜﺎﻝ ﻭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ Case Studyﻭ ﻣﻄﺮﺡﻛﺮﺩﻥ ﺳﺆﺍﻻﺕ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺁﻧﻬﺎ ﻭ ﭘﺎﺳﺦ ﻣﺮﺑﻮﻃﻪ ﺗﻮﺿﻴﺤﺎﺗﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ) BPPﺑﻴﻮﻓﻴﺰﻳﻜﺎﻝ ﭘﺮﻭﻓﺎﻳﻞ(21.3 Operative Obstetrics
)(Larry C. Gilstrap III) (2nd Edition) (SALEKAN E-BOOK )22.3 Safety principles for surgical techniques in minimally invasive gynecologic surgery (Dr. Samir Sawalhe) (CD I , II )(Equipment, preparation, positioning, approach alternatives, safe entry, nots on application
ــــــ ــــــ
5. Electrical morcellation
4. Approach alternatives
3. Disinfection/preparation
2. Positioning
1. Instruments/equipment
)23.3 Single Puncture Laparoscopic Technique (Marco Pelosi, MD) (VCD
ــــــ
ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ CDﺭﻭﺵ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺑﻪ ﺻﻮﺭﺕ Single punctureﺗﻮﺻﻴﻒ ﮔﺮﺩﻳﺪﻩ ﻭ ﺷﺮﺍﻳﻂ ﺍﻃﺎﻕ ﻋﻤﻞ ،ﻃﺮﻳﻘﻪ ﻭ ﻭﺳﺎﺋﻞ ﻋﻤﻞ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﻭ ﺳﭙﺲ ﻣﺰﺍﻳﺎ ﺍﻳﻦ ﺭﻭﺵ ﺑﻪ ﻧﻮﻉ multiple punctureﺑﻴﺎﻥ ﻣﻲﮔﺮﺩﺩ. )(Frances R. Batzer, MD
ــــــ
24.3 Submitted Subject: Transvaginal Sonographic Assessment of Pelvic Pathology: Preoperative Evaluation
ﺍﻳﻦ ﻭﻳﺪﺋﻮ CDﺍﺯ ٣ﺑﺨﺶ ﺯﻳﺮ ﺗﺸﻜﻴﻞ ﺷﺪﻩ ﺍﺳﺖ: )ﻓﻴﻠﻢ ﺍﻭﻝ( :ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺑﺤﺚ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺷﺮﺡ ﺣﺎﻝ ٦ﺑﻴﻤﺎﺭ ﺑﻴﺎﻥ ﺷﺪﻩ ﻭ ﺑﺎ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺗﺸﺨﻴﺺ ﻭ ﻣﺤﻞ ﺩﻗﻴﻖ ﺿﺎﻳﻌﺎﺕ ﻟﮕﻦ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺳﭙﺲ ﺑﺎ ﻫﻴﺴﺘﺮﺳﻜﻮﭘﻲ ﻭ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺿﺎﻳﻌﺎﺕ ﺟﺮﺍﺣﻲ ﻣﻲﮔﺮﺩﺩ Case .ﻫﺎﻱ ﺳﻄﺮ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ:
ﺧﺎﻧﻢ ٤٢ﺳﺎﻟﻪﺍﻱ ﺑﻪ ﻣﻨﻮﻣﺘﺮﻭﺭﺍﮊﻱ ﺑﻪ ﻣﺪﺕ ٢ﺳﺎﻝ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ﺳﺎﺏ ﻣﻮﻛﻮﺱ ﻓﻴﺒﺮﻭﻥ ← -١ﺧﺎﻧﻢ ٢٤ﺳﺎﻟﻪﺍﻱ ﺑﺎ ﺗﺎﺭﻳﺨﭽﻪ ﺧﺘﻢ ﺣﺎﻣﻠﮕﻲ ﻣﻜﺮﺭ ﺩﺭ ﺗﺮﻳﻤﺴﺘﺮ ﺩﻭﻡ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ← Septate uterusﺩﺭﻣﺎﻥHysteroscopic Resection : ﺩﺭﻣﺎﻥ
-٢ -٣ -٤ -٥ -٦
←
ﻫﻴﺴﺘﺮﻭﺳﻜﻮﭘﻴﻚ resection
ﺧﺎﻧﻢ ٣٦ﺳﺎﻟﻪ ﺑﺎ ﺗﺎﺭﻳﺨﭽﻪ ﺍﻧﺪﻭﻣﺘﺮﻳﻮﺯ ﻭ ﺩﺭﺩ ﻧﺎﮔﻬﺎﻧﻲ ﻭ ﺵ ﺩﻳﺪ ﻧﺎﺣﻴﻪ ﻟﮕﻦ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ﺍﻧﺪﻭﻣﺘﺮﻳﻮﻣﺎ ← ﺩﺭﻣﺎﻥ :ﺑﺮﺩﺍﺷﺘﻦ ﻛﻴﺴﺖ ﺑﺎ ﻻﭘﺎﺭﺍﺳﻜﻮﭖ ﺑﺎ ﻟﻴﺰﺭﻱ YA ﺧﺎﻧﻢ ٤١ﺳﺎﻟﻪ ﺑﺎ ﺩﺭﺩ ﻧﺎﺣﻴﻪ ﻟﮕﻦ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ﺩﺭﻣﻮﺋﻴﺪ ← Cystﺩﺭﻣﺎﻥ :ﺑﺮﺩﺍﺷﺘﻦ ﺩﺭﻣﻮﺋﻴﺪ ﻛﻴﺴﺖ ﺑﺎ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺧﺎﻧﻢ ٤٣ﺳﺎﻟﻪ ﺑﻄﻮﺭ ﺍﺗﻔﺎﻗﻲ ﻣﺘﻮﺟﻪ ﺑﺰﺭﮔﻲ ﺗﺨﻤﺪﺍﻥ ﻳﻜﻄﺮﻑ ﻣﻲﺷﻮﺩ ← ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ← ﻓﻮﻟﻴﻜﻮﻝ ﺩﺭ ← Cystﺩﺭﻣﺎﻥ :ﺑﺮﺩﺍﺷﺘﻦ ﺿﺎﻳﻌﻪ ﺑﺎ ﻻﭘﺎﺭﺍﺳﻜﻮﭖ
ﺧﺎﻧﻢ ٢١ﺳﺎﻟﻪﺍﻱ ﺑﺎ ﺧﻮﻧﺮﻳﺰﻱ ﻣﺪﺍﻭﻡ ﻭ ٣ LMPﻫﻔﺘﻪ ﻗﺒﻞ ﺗﺸﺨﻴﺺ ←
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﺗﺸﺨﻴﺺ ﺗﺮﺍﻧﺲ ﻭﺍﮊﻳﻨﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ectopicpregnancy
← ﺩﺭﻣﺎﻥ:
Left Salpingectomy
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
17 :()ﻓﻴﻠﻢ ﺩﻭﻡ Limiting Physician Exposure to Hepatitis B and HIV : Ob / Gyns
(R.Viscarello.MD)
. ﺩﺭ ﺗﻤﺎﺱ ﻣﻲﺑﺎﺷﺪ ﮔﻔﺘﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺭﺍﻫﻬﺎﻱ ﺻﺤﻴﺢ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻭ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﻭ ﺭﻭﺵﻫﺎﻱ ﭘﻴﺸﮕﻴﺮﻱ ﺩﺭ ﻣﻄﺐ ﻣﺘﺨﺼﺼﻴﻦ ﺯﻧﺎﻥ ﻭ ﺯﺍﻳﻤﺎﻥ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖHIV ﻳﺎHBV ﺭﺍﻩﻫﺎﻱ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﺩﺭﻣﺎﻥ ﻓﺮﺩﻱ ﻛﻪ ﺑﺎCD ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ :()ﻓﻴﻠﻢ ﺳﻮﻡ Laparoscopic Retropubic Colposuspension For Stress urinary incontinence
(Gordon. D. Davis, MD. & R.W.Lobel,MD
. ﺑﻄﺮﻳﻘﻪ ﻻﭘﺎﺭﺍﺳﻜﻮﭘﻲ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖStress incontinence ﻃﺮﻳﻘﻪ ﺍﺻﻼﺡCD ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ :()ﻓﻴﻠﻢ ﭼﻬﺎﺭﻡ Bi-polar Desiccation of Vascular Tissue: Laparoscopic Hysterectomy
(Paul, D. Indman,MD)
. ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖbi-polar desiccation ﺩﺭ ﺍﻳﻦ ﻓﻴﻠﻢ ﻃﺮﻳﻘﻪ ﺑﺮﺩﺍﺷﺘﻦ ﭘﺎﻳﻪﻫﺎﻱ ﻋﺮﻭﻗﻲ ﻛﻮﭼﻚ ﻭ ﻣﺘﻮﺳﻂ ﺩﺭ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺗﻮﺳﻂ 1999
25.3 TEXT AND ATLAS OF Female in Fertility Surgery (ROBERT B. HUNT) (Third Edition) (Mosby) (SALEKAN E-BOOK)
:ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ BASIC SCIENCE
ENERGY SOURCES
RADIOLOGIC PROCEDURES
HYSTEROSCOPY
LAPAROSCOPY
LAPAROTOMY
ENDOMETRIOSIS
ADDITIONAL CONSIDERATIONS
2002
26.3 Triplet Pregnancies and their Consequences (Louis G. Keith, MD, Isaac Blickstein, MD) (SALEKAN E-BOOK) Epidemiology and biology
Antepartum considerations
Delivery/birth considerations
The Matria database
Short-term outcomes
Prenatal diagnosis
Long-term outcomes
Preventive measures
Miscellaneous
Future dicections
Sources of information on multiple births
27.3 TVT Tension-free Vaginal – Tape
ــــــ : ﺍﺯ ﺑﺨﺶ ﺯﻳﺮ ﺗﺸﻜﻴﻞ ﺷﺪﻩ ﺍﺳﺖCD ﺍﻳﻦ
Stress Incontinence
Anatomy&Terminology
Tension-free Vaginal Tape
Indication&Patient Selection
TVT Procedure
Clinical Information
Sales Support
28.3 Urogynecology: Evaluation and Treatment of Urinary Incontinence (Bruce Rosenzweig, MD, Jeffrey S. Levy, MD, Donald R. Ostergard, MD)
ــــــ
. ﻭﺟﻮﺩ ﺩﺍﺭﺩCD ﻼ ﺭﻧﮕﻲ ﺑﻮﺩﻩ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﺑﻪ ﺻﻮﺭﺕ ﻧﻮﺷﺘﺎﺭﻱ ﻭ ﻓﺎﻳﻞ ﺻﻮﺗﻲ ﻛﻪ ﺑﺮ ﺭﻭﻱ ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﺍﻳﻦ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﺗﺼﺎﻭﻳﺮ ﻛﺎﻣ ﹰCD ﺍﻳﻦ : ﻗﺴﻤﺖ ﻣﺠﺰﺍ ﺩﺍﺭﺩ ﺷﺎﻣﻞ٤ Urogynechology Consideration for the OB/GYN Generalist
-
won surgical & surgical Management
-
Evaluation -
:ﺍﻳﻦ ﻗﺴﻤﺖ ﺧﻮﺩ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ Types of incontinernce y
incontinence awareness y
Patient misconceptions y
Introduction Definigg Incontinence
-
:Introduction & Defining Incontince (١ affected women y
incontince ﺗﺸﺨﻴﺺy
:incontinency ( ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺎ٢ Cystoscopy y uroflowmetry y Postvoid residual y Cystometrogram y Pad test y ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲy ﺗﺎﺭﻳﺨﭽﻪy Voiding diary y un , u/s y Pessary test y Multi-Channel urodynamics y
: Stress urinary incontinence ( ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﺟﺮﺍﺣﻲ ﻭ ﻏﻴﺮ ﺟﺮﺍﺣﻲ ﺩﺭ٣ .( ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ.... ﻭfunetional electrieal Stimalation ﻭ ﺩﺭﻣﺎﻥﻫﺎﻱ ﺩﺍﺭﻭﺋﻲbiofeedback, Beharioral modification)) ﺍﻳﻦ ﻗﺴﻤﺖ ﺷﺎﻣﻞ ﺍﻟﮕﻮﺭﻳﺘﻢ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻣﻲﺑﺎﺷﺪ ﻭ ﺳﭙﺲ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻏﻴﺮﺟﺮﺍﺣﻲ . ﺍﻳﻦ ﺭﻭﺵﻫﺎ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖComplication ﺩﺭ ﻗﺴﻤﺖﻫﺎﻱ ﺑﻌﺪﻱ ﻣﻘﺎﻳﺴﻪ ﺩﺭﺻﺪ ﻣﻮﻓﻘﻴﺖ ﺭﻭﺵﻫﺎ ﺫﻛﺮ ﺷﺪﻩ ﻭ ﺩﺭ ﺁﺧﺮ. ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖProcedure ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵﻫﺎﻱ ﺍﻧﺠﺎﻡ ﺟﺮﺍﺣﻲ ﺑﺤﺚ ﺷﺪﻩ ﻭ ﺳﭙﺲ:ﺭﻭﺵﻫﺎﻱ ﺟﺮﺍﺣﻲ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
18 : Consideration for the OB/Gyn Generalist (٤ ﺩﺭ ﺍﻳﻦ ﻓﺼﻞ: urogynechology as a subdiscipline y eystometry y
professional consideration y
Non surgical therapy y
Urodynamics y
incontinrence management to private patients y
Set-up requirement y
equipment cost y
Allied Staff y
ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ.
ــــــ
)29.3 Video Journal of Gynecology (Vaginal Hysterectomy Wedge morcellization Technique for the Large Uterus) (The Infertile Couple) (David Olive, MD, George W. Morley MD,
ــــــ
)30.3 WOMEN'S HEALTH (MOSBY'S PRIMARY CARE
2003
ﺍﻳﻦ CDﺷﺎﻣﻞ Procedureﻫﺎﻱ ﺳﺮﭘﺎﺋﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺯﻧﺎﻥ ﻭ ﺩﺳﺘﮕﺎﻩ ﮊﻧﻴﺘﺎﻟﻬﺎﻱ ﺯﻧﺎﻥ ) (Female Genitaliaﻭ ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ Female Genitiourinary Tractﻣﻲﺑﺎﺷﺪ. ﺩﺭ ﻫﺮ ﻓﺼﻞ ﻋﻼﻭﻩ ﺑﺮ ﺭﻭﺵ ، Lﺁﻧﺎﺗﻮﻣﻲ ،ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ Lﻭ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ﻭ ﻋﻮﺍﺭﺽ ﻭ ﺗﺴﺖﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﻭ ﻏﻴﺮﻩ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ. ﺧﺼﻮﺻﻴﺖ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮﺩ ﺍﻳﻦ CDﺷﺎﻣﻞ :ﻧﺸﺎﻥ ﺩﺍﺩﻥ ﺗﻤﺎﻡ ﺭﻭﺵﻫﺎ ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢﻫﺎﻱ ﻭﻳﺪﺋﻮﺋﻲ ﺩﺭ CDﻭ ﺩﻳﮕﺮ CNGﻳﺎ ﺗﺴﺖﻫﺎﻱ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺑﺨﺶ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ: ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ : Breast examination -١ﺷﺎﻣﻞ :ﺁﻧﺎﺗﻮﻣﻲ ،ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ،ﺗﺠﻬﻴﺰﺍﺕ ،ﺁﻣﻮﺯﺵ ﺑﻪ ﺑﻴﻤﺎﺭ ،ﻓﺮﻡ ﺭﺿﺎﻳﺖ ﻧﺎﻣﻪ Pojition ،ﺑﻴﻤﺎﺭ ﺗﻜﻨﻴﻚ ﻭ ﺛﺒﺖ ﻳﺎﻓﺘﻪﻫﺎ ﻭ ﭘﺮﻭﻧﺪﻩ ﻭ ﺍﺷﻜﺎﻻﺕ ﺗﻜﻨﻴﻜﻲ ،ﺗﺸـﺨﻴﺺ ﺍﻓﺘﺮﺍﻗـﻲ ﻭ quizﺍﻧﺘﻬـﺎﻱ ﺑﺨـﺶ ﻣﻲﺑﺎﺷﺪ ﺗﻤﺎﻡ ﻣﺮﺍﺣﻞ ﺑﺎﻳﺪ ﺑﻪ ﺻﻮﺭﺕ ﺗﻤﺎﺱﻫﺎﻱ ﺭﻧﮕﻲ ﻭ ﻓﺎﻳﻞﻫﺎﻱ ﻭﻳﺪﻳﻮﺋﻲ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﺍﺳﺖ : Colposcopy -٢ﺍﺑﺘﺪﺍ ﺁﻧﺎﺗﻮﻣﻲ cervixﺑﺎ ﺷﻜﻠﻬﺎﻱ ﺗﻤﺎﻡ ﺭﻧﮕﻲ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﻻﺯﻡ ﺩﺭ ﻣﺘﻦ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺳﭙﺲ ﺩﺭ ﻣﻮﺭﺩ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻧﺎﺣﻴﻪ ﺳﺮﻭﻛﻴﻞ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﺑﺎ ﺁﻣﻮﺯﺵ ﺑﻪ ﺑﻴﻤﺎﺭ ﺗﺠﻬﻴﺰﺍﺕ ﻻﺯﻡ ، Positioning ،ﺁﻣﺎﺩﻩ ﻛﺮﺩﻥ ﻣﺤﻞ ،ﺁﻧﺴﺘﺰﻱ ،ﺗﻜﻨﻴﻚ ﺍﻧﺠﺎﻡ Procedneﻭ ﻛﻤﭙﻴﻜﺎﺳﻴﻮﻥ ،ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻭ ﺗﻐﻴﻴﺮ ﻧﺘﺎﻳﺞ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺩﺭ ﺁﺧﺮ ﻓﺼﻞ Quizﻭﺟﻮﺩ ﺩﺍﺭﺩ ٧ .ﻓﻴﻠﻢ ﺩﺭ ﻣﻮﺭﺩ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺠﺎﻡ ﺭﻭﺵ ﻛﻮﭘﻴﻮﺳﻜﻮﭘﻲ ﺩﺭ ﺍﻳﻦ ﻓﺼﻞ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. -٣ﺍﻧﺪﻭﻣﺘﺮﻳﺎﻝ ﺑﻴﻮﭘﺴﻲ :ﺍﺑﺘﺪﺍ ﻭ ﻣﻘﺪﻣﻪ ﺗﺎﺭﻳﺨﭽﻪﺍﻱ ﺍﺯ D&Cﻭ ﺑﻴﻮﭘﺴﻲ ﺁﻧﺪﻭﻣﺘﺮﻳﺎﻝ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﻗﺪﻳﻤﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﺳﭙﺲ ﺁﻧﺎﺗﻮﻣﻲ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺁﻥ ﺑـﻪ ﺗﺼـﺎﻭﻳﺮ ﺭﻧﮕـﻲ ﺷـﺮﺡ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖ.ﺳـﭙﺲ ﻣﺎﻧﻨـﺪ ﺩﻳﮕـﺮ Procedureﻫـﺎ ﺍﻧﺪﻳﻜﺎﺳـﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﻭ ﺗﻜﻨﻴﻚ ،ﺁﻣﺎﺩﮔﻲ ﺑﻴﻤﺎﺭ Position ،ﺑﻴﻤﺎﺭ ،ﺁﻧﺴﺘﺰﻱ ﻭ ....ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺁﺧﺮ ﻓﺼﻞ ﻓﻴﻠﻢﻫﺎﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﺗﺠﻬﻴﺰﺍﺕ ﻭ ﺭﻭﺵﻫﺎﻱ ﺍﻧﺠﺎﻡ ﺑﻴﻮﭘﺴﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺁﺧﺮ ﻓﺼﻞ Quizﻗﺮﺍﺭ ﺩﺍﺭﺩ. : Pelvic Examination -٤ﺑﻌﺪ ﺍﺯ ﻣﻘﺪﻣﻪ ﺩﺭ ﻣﻮﺭﺩ ﺁﻧﺎﺗﻮﻣﻲ ﻧﺎﺣﻴﻪ ﮊﻧﺘﻴﻜﻲ ) (utenes , carivx , vagina , valveﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺠﺎﻡ ﻣﻌﺎﻳﻨﻪ Position،ﺑﻴﻤﺎﺭ ،ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ،ﻛﻨﺘﺮﺍﻳﻜﺎﺳﻴﻮﻥ ﻭ ﺗﻐﻴﻴﺮ ﻳﺎﻓﺘﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻭ ﺳﭙﺲ ٦ﻓﻴﻠﻢ ﻣﻌﺎﻳﻨﻪ ﻟﮕﻨﻲ ﻛﺎﻣﻞ ،ﻣﻌﺎﻳﻨﻪ exetrnalgenifalicnﺑﺎ ﭘﺎﭖ ﺁﺳﻤﻴﺮ ،ﻣﻌﺎﻳﻨﻪ rectovaginal , bimanualﻭ ﭼﮕﻮﻧﮕﻲ ﮔﺬﺍﺷﺘﻦ ﺍﺳﭙﻜﻮﻟﻮﻡ ﻭ ﺗﺠﻬﻴﺰﺍﺕ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺁﺧﺮ Quizﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. : Pap Smear -٥ﺍﺑﺘﺪﺍ ﺑﻌﺪ ﺍﺯ ﻣﻘﺪﻣﻪﺍﻱ ﻛﻮﺗﺎﻩ ﺩﺭ ﻣﻮﺭﺩ ﺁﻧﺎﺗﻮﻣﻲ ﻣﻨﻘﻄﻊ ﻭ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﻪ ﻣﻲﺷﻮﺩ ﺑﺎ ﭘﺎﭖ ﺁﺳﻤﻴﺮ ﺑﺮﺭﺳﻲ ﻛﺮﺩ .ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ،ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ Position ،ﺭﻭﺵ ﺍﻧﺠﺎﻡ ،ﺍﺷﻜﺎﻻﺕ ﺗﻜﻨﻴﻜﻲ ،ﺗﺠﻬﻴﺰﺍﺕ ﻭ ....ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ٥ .ﻓـﻴﻠﻢ ﺍﺯ ﭼﮕﻮﻧﮕﻲ ﻣﻌﺎﻳﻨﻪ ،ﮔﺬﺍﺷﺘﻦ ﺍﺳﻴﻜﻮﻟﻮﻡ ﻭ ﺍﻧﺠﺎﻡ ﭘﺎﭖ ﺍﺳﻤﻴﺮ ﻭ ﺗﺠﻬﻴﺰﺍﺕ ﺁﻥ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ) Vaginal Secretion -٦ﺗﺮﺷﺢ ﻭﺍﮊﻳﻨﺎﻝ( :ﺩﺭ ﺍﻳﻦ ﻣﺒﺤﺚ ﺍﺑﺘﺪﺍ ﻋﻠﻞ ﺗﺮﺷﺢ ﻭﺍﮊﻳﻨﺎﻝ ﻭ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﺁﻥ ﭘﺮﺩﺍﺧﺘﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺳﭙﺲ ﺗﺠﻬﻴﺰﺍﺕ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ،ﭼﮕﻮﻧﮕﻲ ﮔﺮﻓﺘﻦ ﻛﺸﺖ ،ﺍﻧﺠﺎﻡ ﺗﺴﺖ ، KOHﻗﺮﺍﺭ ﺩﺍﺩﻥ ﺗﺮﺷﺤﺎﺕ ﺑﺮ ﺭﻭﻱ slideﻭ ﻣﺸﺎﻫﺪﻩ ﺁﻥ ﺑﺎ ﻣﻴﻜﺮﻭﺳﻜﻮﭖ ﺑﺎ ﻓﻴﻠﻢ ﻭ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ Quizﻧﻴﺰ ﺩﺭ ﺁﺧﺮ ﻓﺼﻞ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. 31.3 UTEROSALPINGOGRAPHY IN GYNECOLOGY (Hysterosalpingography) It's Application in Physiological And Pathological Conditions )(SALEKAN E-BOOK ﺍﻳﻦ CDﺣﺎﻭﻱ ﻣﻄﺎﻟﺐ ﺫﻳﻞ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ Utero Salpingographyﻣﻲﺑﺎﺷﺪ: ﺍﺻﻮﻝ ﻛﻠﻲ ﺩﺭ Uterosalpingography
-ﺳﻘﻂ ﻣﻜﺮﺭ ﻭ ﻗﺎﻋﺪﮔﻲ ﺩﺭﺩﻧﺎﻙ )ﺩﻳﺲ ﻣﻨﻮﺭﻩ(
ﻋﻤﻠﻜﺮﺩ ﺭﺣﻢ ﻭ ﻟﻮﻟﻪﻫﺎﻱ ﻓﺎﻟﻮﭖ -ﺳﻞ ﺗﻨﺎﺳﻠﻲ ﻭ ﻓﻴﺴﺘﻮﻝ ﮊﻧﻴﺘﺎﻝ
ﺁﻧﻮﻣﺎﻟﻲﻫﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ﺭﺣﻢ ﻭ ﻟﻮﻟﻪﻫﺎﻱ ﻓﺎﻟﻮﭖ -ﭘﺎﺗﻮﻟﻮﮊﻱ ﻟﻮﻟﻪﻫﺎﻱ ﻓﺎﻟﻮﭖ ،ﭘﺮﻳﺘﻮﺋﻦ ﻭ ﺗﺨﻤﺪﺍﻥﻫﺎ
-ﺗﻐﻴﻴﺮﺍﺕ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﺭﺣﻢ
ﺩﺭ CDﻓﻮﻕﺍﻟﺬﻛﺮ ﺗﺼﺎﻭﻳﺮ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﻣﺘﻌﺪﺩ ﻭﺍﺿﺤﻲ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ USGﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ. 32.3 Your Pregnancy, Your Newborn The Complete Guide for Expectant and New Mothers
ــــــ
-٤ﻋﻠﻮﻡ ﺁﺯﻣﺎﻳﺸﮕﺎﻫﻲ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــــ
ﻋﻨﻮﺍﻥ CD )(Sixth Edition) (SALEKAN E-BOOK
)(Frances Fischbach
A Manual of Laboratory & Diagnostic Tests
1.4
ﺍﻳﻦ CDﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺪﻩ ﺍﺳﺖ ﻣﺸﺘﻤﻞ ﺑﺮ ١٦ﻓﺼﻞ ﺍﺳﺖ ﻭ ﺷﺎﻣﻞ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: Stool Studies
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
Urine Studies
Blood Studies
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
Diagnostic Testing
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
19 Cbemistry Studies Cytology, Histology, and Genetic Studies Prenatal Diagnosis and Tests of Fetal Well-Being
2.4
Microbiologic Studies Endoscopic Studies Cerebrespinal Fluid Studies
Immunodiagnostic Studies Ultrasound Studies X-ray Studies
Nuclear Medicine Studies Pulmonary Functio and Blood Gas Studies Special Systems, Organ Functions, and Post Mortem Studies
2002
A Slide Atlas of ATHEROSCLEROSIS (Progression and Regression) (Herbert C. Stary) ﻣﻄﺎﻟﻌﻪ ﺍﻳﻦ ﻧﺮﻡ ﺍﻓﺰﺍﺭ ﺑﻪ ﻣﺘﺨﺼﺼﻴﻦ ﭘﺎﺗﻮﻟﻮﮊﻱ. ﺍﺳﻼﻳﺪ ﺗﺨﺼﺼﻲ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﭘﻴﺸﺮﻓﺖ ﻭ ﭘﺴﺮﻓﺖ ﺑﻴﻤﺎﺭﻱ ﺁﺗﺮﻭﺍﺳﻜﻠﺮﻭﺯﻳﺲ ﺩﺭ ﺳﻨﻴﻦ ﻣﺨﺘﻠﻒ ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺭﺍ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﻭ ﺍﻟﻜﺘﺮﻭﻧﻲ ﺑﻪ ﺯﻳﺒﺎﻳﻲ ﺑﻪ ﺗﺼﻮﻳﺮ ﻛﺸﻴﺪﻩ ﺍﺳﺖ۹۴ ﺍﻳﻦ ﻧﺮﻡ ﺍﻓﺰﺍﺭ ﺑﺎ .ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﺗﻮﺻﻴﻪ ﻣﻴﺸﻮﺩ
3.4
2002
th
American Sodiety of Hematology (CD 1-5) (44 Annual Meeting) CD-1: ALL -AML -ASH/ASCO Joint Symposium -Atypical Cellular Disorders CD-2: CLL -CML -CNS Lymphoma -Cutaneous Lymphoma -E. Donnall Thomas Lecture CD-3: Enhancing Physician/Patient Communication Regarding Hematologic Disorders -Ham-Wasserman Lecture -Hematology Grants Workshop -Hypercoagulability: Too Many Tests, Too Much Conflicting Data -Malaria and the Red Cell -Marrow Failure CD-4: Multi[ple Myeloma -Myelodysplastic Syndromes Non-Myeloablative Transplantation -Platelets: Thrombotic Thrombocytopenic -Purpura Plenary Policy Frum CD-5: Presidential Symposium Long-Term Complications
4.4
-Red Cell Antigens as Functional Molecules and Obstacles to Transfusion
-Sickle Cell Disease
-Stem Cell Transplantation: Supportive Care and
-Stem Cells: Hype and Reality Update on Epidemiology and Therapeutics for Non-Hodgkin’s Lymphoma
An Electronic Companion to Microbiology for MajorsTM (Mark L. Wheelis)
ــــــ
Reviw , Test yourself
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ What Are Microorganisms? Classification
5.4
Methods of Microbiology Prokaryotic Cell Struture
Eukaryotic Cell Struture Growth & Reproduction
Metabolism & Energy Microbial Genetics
Gene Regulation Viruses
Microbial Ecology Defenses Againses Infection
Disease
Atlas of HEMATOLOGY
ــــــ : ﺣﺎﻭﻱ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ
1. Examination of Blood Cells
2. Normal Hematopoiesis and Blood Cells
3.Dynamic Cell Morphology
4. Hematolopathology
5. Cluster of differentiation Archive
6. Self-Assessment
6.4
Atlas of Surgical Pathology (Johns Hopkins) (Jonathan I. Epstein, Neera P. Agarwal-Antal, David B. Danner, Kim M. Ruska)
7.4
Atlas of Medical Parasitology (Dr. K. Ghazvini) ﻧﺎﻗﻞ اﻧﮕﻞ و ﺳﯿﮑﻞ زﻧﺪﮔﯽ و ﺗﮑﺜﯿﺮ اﻧﮕﻞ اﺳﺖ ﮐﻪ ﺟﻬﺖ اﺳﺘﻔﺎده ﮔﺮوهﻫﺎی ﻣﺨﺘﻠﻒ رﺷﺘﻪﻫﺎی ﭘﺰﺷـﮑﯽ ﺧﺼﻮﺻـﺎً رﺷـﺘﻪ ﻋﻠـﻮم، ﺿﺎﯾﻌﺎت اﯾﺠﺎدﺷﺪه، ﺗﺼﻮﯾﺮ رﻧﮕﯽ از اﻧﻮاع اﻧﮕﻞﻫﺎی ﺑﯿﻤﺎرﯾﺰای اﻧﺴﺎﻧﯽ ﺷﺎﻣﻞ ﺗﺼﻮﯾﺮ اﻧﮕﻞ2000 ﻧﺮماﻓﺰار ﻓﻮق ﺣﺎوی ﺣﺪود ﻣﺒﺎﺣﺚ ﻣﻄﺮحﺷﺪه در اﯾﻦ ﻧﺮماﻓـﺰار. ﺑﺴﯿﺎری از ﺗﺼﺎوﯾﺮ ﻣﻮﺟﻮد در اﯾﻦ ﻣﺠﻤﻮﻋﻪ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮد ﻣﯽﺑﺎﺷﺪ. ﺗﺼﺎوﯾﺮ ﻣﺠﻤﻮﻋﻪ ﻣﺰﺑﻮر از ﻣﻨﺎﺑﻊ ﻣﺨﺘﻠﻒ ﺟﻤﻊآوری ﮔﺮدﯾﺪه اﺳﺖ ﮐﻪ ﺗﻮﺳﻂ دﮐﺘﺮ ﻗﺰوﯾﻨﯽ ﺑﺎزﻧﮕﺮی و وﯾﺮاﯾﺶ ﮔﺮدﯾﺪه اﺳﺖ.آزﻣﺎﯾﺸﮕﺎﻫﯽ ﻣﻔﯿﺪ اﺳﺖ :ﻋﺒﺎرﺗﻨﺪ از * Heart and Muscles Parasites * Lung Parasites
8.4
* Eye Parasites * Skin Parasites
Basic histology: TEXT & ATLAS IMAGE LIBRARY (Tenth Edition)
* Central Nervous System (CNS) Parasites * Liver and Biliary Tree Parasites
* Gnito-Urinary Parasites * Intestinal Parasites (Helminths)
* Intestinal Parasites (Protozoa)
(Luiz Carlos, Juhqueira, Jose CARNEIRO) (A Division of The McGraw-Hill Companies)
2000
2 - Jose CARNEIRO
1- Luiz Carlos JUNQUEIRA 9.4
* Case reports and updates in parasitology * Blood, Bone Marrow, Spleen Parasites
2003
Biochemical Interactions An electronic companion to: FUNDAMENTALS OF BIOCHEMISTRY (Donald voet, Judith G. voet, charlotte W. Pratt)
(Version 1.02)
1999
: ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﺍﻳﻦ NUCLEOTIDES AND NUCLEIC ACIDS
PROTEINS: PRIMARY STRUCTURE
PROTEIN FUNCTION
LIPIDS
BIOLOGICAL MEMBRANES
MAMMALIAN FUEL METABOLOSM: INTEGRATION AND REGULATION
GLUCOSE CATABOLISM
GLYCOGEN METABOLISM AND GLUCONEOGENESIS
DNA REPLICATION REPAIR, AND RECOMBINATION
PHOTOSYNTHESIS
LIPID METABOLISM
AMINO ACID METABOLISM
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
20 NUCLEOTIDE METABOLISM
NUCLEIC ACID STRUCTURE
CITRIC ACID CYCLE
TRANSLATION
REGULATION OF GENE EXPRESSION
ENZYME KINETICS, INHIBITION, AND REGULATION
INTROCUCTION TO METABOLISM
ELECTRON TRANSPORT AND OXIDATIVE PHOSPORYLATION
PROTEINS: THREE-DIMENSIONAL STRUCTURE
TRANSCRIPTION AND RNA PROCESSING
10.4 BIOLOGY CONCEPTS & CONNECTIONS
(Second Edition) (Richard M. Liebaert) (CAMPBELL.MITCHELL.REECE)
ــــــ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﺍﻳﻦ
1. Introduction: The Sclentific Sindy of Life
3. The Life of the Cell
2. The Evolution of Biological Diversity
4. Animals: Form & Function
11.4 BLOOD PRINCIPLES AND PRACTICE OF HEMATOLOGY
5. Cellular Repoduction & Genetics
7. Concepls of Evolution
6. Plants: Form & Function
8. Ecology
(SECOND EDITION) (ROBERT I. HANDIN SAMUEL E. LUX THOMAS P. STOSSEL)
Part I: Fundamentals of Hmatology: Tools of the trade
Part II: The Hematopoietic System
Part III: Stem Cell Disorders
Part IV: White Blood Cells
Part V: Hemostasis
Part VII: Systemic Disease
Part VIII: Hematologic Therapies
Part VIIII: Appendices
Part VI: Red Blood Cells
12.4 BRS Cell Biology CELL BIOLOGY AND HISTOLOGY (4th edition) (Leslie P. Gartner, James L. Hiatt, Judy M. Strum) (LIPPINCOTT WILLIAMS & WILKINS)
2003
2003
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ Plasma Membrane Connective Tissue Circulatory System The Urinary System Epithelia and Glands
Nucleus Cartilage and Bone Lymphoid Tissue Female Reproductive System Blood and Hemopoiesis
13.4 Cellular & Molecular Neurobiology
Cytoplasm Muscle Endocrine System Digestive System: Oral Cavity and Alimentary Tract Digestive System: Glands
Extracellular Matrix Nervous Tissue Skin Special Senses Comprehensive Exam
(Second Edition)
ــــــ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﺍﻳﻦ
1- Lonotropic and Metabotropic Receptors in Synaptic Transmission and Sensory Transduction
3- Neurons: Excitable and Secretory Cells that Establish Synapses
2- Somato-Dendritic Processing and Plasticity of Postsynaptic Potentials
4- Activity and Developmen of Networks: The Hippocampus as an Example
14.4 Clinical Hematology (A Victor Hoffbrand , John E Pettit) (Mosby) Normal Hemopoiesis and
Blood Cells
Anaemias Blood Transfusion
ــــــ
Leucocyte Abnormialities
Hemostasis and Bleeding Disorders
Bone Marrow Transplantation
Hematological Malignancies Further Reading
Coagulation Disorders Acknowledgements
Bone Marrow in Non-hemopoietic Disease
Parasitic Infections Diagnosed in Blood
15.4 Clinical Immunology
ــــــ
16.4 COMMON PROBLEMS IN CLINICAL LABORATORY MANAGEMENT (Judith A. O'brien, M.S. CLSup (NCA)) (Salekan E-Book)
ــــــ
COMPLYING WITH CLIA '88 MEETING TUBERCULOSIS CONTROL REGULATIONS WRITING MANUALS: THE STANDARD OPERATING PROCEDURE MANUAL (SOPM)
OVERCOMING OSHA'S OBST ACLES THE EXPOSURE CONTROL PLAN PROVIDING AND USING PERSONAL PROTECTIVE EQUIPMENT PASSING PROFICEINCY TEST
OVERCOMING OSHA'S OBSTACLES THE CHEMICAL HYGIENE PLAN WRITING MANUALS: THE GENERAL OPERATING PROCEDURE MANUAL ( GOPM) FULFILING QUALITY CONTROL GUIDELINES
ESTABLISHING A QUALITY ASSURANCE PROGRAM
SURVIVING INSPECTIONS AND ATTAINING ACCREDIANCE
PURSUING PERSONNEL PERSPECTIVES
ENCOURAGING EDUCATION
THE ACQUISTION AND MAINTENANCE OF LABORATORY INSTRUMENTATION
MASTERING FINANCES: BILLING AND CODING
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
TAMING TECHNOLOGY: LABORATORY INFORMATION SYSTEM (LIS) RE-ENGINEERING FOR THE FUTURE: THE CORE LABORATORY, AUTOMATION, OUTREACH NETWORKING, AND THE MILLENNIUM BUG GENERATING LABORATORY NUMBERS: STATISTICS LINEARITY, CALIBRATION, REFERENCE, AND CRITICAL VALUES: CALCULATIONS MANAGING THE PHYSICIAN OFFICE LABORATORY (POL) TAMING TECHNOLOGY: POINT OF CARE TESTING (POCT)
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
21 (A data of multiple choice question in microscopic) (Bloom & Fawcett's) (Second Edition)
17.4 Concise Histology
ــــــ
18.4 Dianostic Hematology
ــــــ
This textbook, 'Diagnostic Hematology: A pattern approach', is accompanied by a CD-ROM with three knowledge-based systems applied to 237 case studies. The 3 knowledge-based systems are: 1. Professor Petrushka for peripheral blood analysis
2. Professor Fidelio for flow cytometry immunophenotyping
3. Professor Belmonte for bone marrow interpretation
19.4 Discover Biology
ــــــ
20.4 Electronic Atlas of Parasitology
(John T. Sullivan)
2000
university of the Incarnate Word
21.4 EMBRYO (CD Color Atlas for Developmental Biology) (Gary C. Schoenwolf) Chapter 1: Frog Embryos
Chapter 2: Chick Embryos
Chapter 3: Pig Embryos
ــــــ Chapter 4: Gametogenesis
22.4 Essential Cell Biology (with the voice of Julie Theriot designed and programmed by Christopher Thorpe)
ــــــ
23.4 Fields Virology (Forth Edition) (Volume 1) (Lippincott Williams & Wilkins)
2001
Section One: General Virology
Chapter 1-22
Section Two: Specific Virus Families Chapter 23-90
24.4 Functional HISTOLOGY WHEATER'S (FOURTH EDITION) (BARBARA YOUNG, JOHN W. HEATH) (ALAN STEVENS JAMES S. LOWE) (PHILIP J. DEAKIN)
ــــــ
25.4 Genetics From Genes to Genomes (Ann Reynolds, Ph.D.) (University of Washington)
2000
5- Gen RegVlation
(... ﺳﻴﮕﻨﺎﻝ ﺗﺮﻧﺴﻼﻛﺸﻦ ﻭ،)ﻛﻨﺘﺮﻝ ﺍﻭﭘﺮﻭﻥ ﻻﻛﺘﻮﺯ 6- Poplations & Evolvtion (... )ﻣﺒﺎﺣﺚ ﺟﻤﻌﻴﺖ ﻭ ﺗﻜﺎﻣﻞ ﻭ ﻓﺮﻛﺎﺵ ﺍﻟﻜﻞﻫﺎ ﻭ ﺩﺭ ﭘﺎﻳﺎﻥ ﻫـﺮ. ﺍﺟﺮﺍ ﮔﺮﺩﺩQuick
3- Molecular Genetice
4- Chromosomes FISH
1- Transmission Genetics
( ﺗﻜﻨﻴﻚ ﻧﻘﺸﻪ ﮊﻥ،)ﻣﺒﺎﺣﺚ ﻛﺎﺭﻳﻮﺗﺎﻳﭗ
2- Gentral Dogma
time
ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﺤﺖ ﺑﺮﻧﺎﻣﺔ... ﻫﻴﭙﺮﻳﺪﺍﺳﻴﻮﻥ ﻛﻠﺮﻧﻴﻨﮓ ﻭ،DVA ﻣﻮﺗﺎﺳﻴﻮﻥ ﻭ ﺗﺮﻣﻴﻢ، ﺍﻟﻜﺘﺮﻭﻓﻮﺭﺯ،PCR، ﻣﻴﺘﻮﺯﻭ ﻣﻴﻮﺯ... ﺗﻮﺟﻪ، ﻣﻜﺎﻧﻴﺴﻢ ﺭﻭﻧﻮﻳﺲ: ﻋﺪﺩ ﻭﻳﺪﺋﻮ ﻛﻠﻴﭗ ﺑﺼﻮﺭﺕ ﺍﻧﻴﻤﻴﺸﻦ ﺍﺯ ﻣﺒﺎﺣﺜﻲ ﻫﻤﭽﻮﻥ٢٧ ﺷﺎﻣﻞCD ﺍﻳﻦ .( ﻣﻲﺑﺎﺷﺪIn teractive) ﻫﻤﭽﻨﻴﻦ ﺩﺍﺭﺍﻱ ﺗﻤﺮﻳﻨﺎﺕ ﺑﺼﻮﺭﺕ ﺩﻭ ﺟﺎﻧﺒﻪ ﻭ ﻓﻌﺎﻝ. ﺩﺍﺭﺍﻱ ﻳﻚ ﻓﺼﻞ ﻣﺮﺑﻮﻁ ﺑﻪ ﺗﻌﺮﻳﻒ ﻭ ﺗﺮﺷﺢ ﻟﻔﺎﺕ ﻣﺸﻜﻞ ﻭ ﺗﺨﺼﺼﻲ ﺍﺳﺖ.ﻓﺼﻞ ﺧﻼﺻﺔ ﻣﺒﺎﺣﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ . ﻣﻮﺟﻮﺩ ﺍﺳﺖ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩCD ﻛﻪ ﺩﺭ ﺧﻮﺩQ.t. ( ﻭ ﻧﺼﺐ ﺑﺮﻧﺎﻣﺔSetup . exe ﻻﺯﻡ ﺍﺳﺖ ﺑﻌﺪ ﺍﺯ ﻧﺼﺐ ﺁﻥ )ﺑﺎ ﺩﻭ ﺑﺎﺭ ﻛﻠﻴﻚ ﻛﺮﺩﻥ ﺑﺮ ﺭﻭﻱCD ﺑﻜﺎﺭ ﺭﻓﺘﻪ ﺍﺳﺖ ﻭ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯCD ﺁﺑﺸﻦﻫﺎﻱ ﻣﺘﻨﻮﻉ ﻭ ﺯﻳﺒﺎﻳﻲ ﺩﺭ ﺍﻳﻦ
26.4 Gram Stain TUTOR
(ANINTERACTIVE TUTORIAL THAT TEACHES THE MICROSCOPIC EXAMINATION OF URINARY SEDIMENT)
ــــــ
(Brad Cookson, MD, PHD, Ajit Limaye, MD, Lydia Matheson, BA) 1. Introduction
2. Morphology
3. Specimen Sites
4. Case Studies 5. Exam
6. Image Atlas
1999
27.4 HISTOLOGY EXPLORER
: ﺩﺭ ﻣﻮﺭﺩ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺑﺤﺚ ﻣﻲﻛﻨﺪCD ﺍﻳﻦ Microscope 3D The Cell Epithelium
Connective Tissue Proper Blood and Bone Marrow The Sketetal Tissues
Nervous Tissue The Circulatory System The Lymphoid Organs
The Digestive System The Respiratory System The Urinary System
The Reproductive System The Mammary Giands The Eye
Glands Muscular Tissue The Skin
The Endocrine Glands The Ear
28.4 HUMAN HISTOLOGY CD-ROM (Alan Stevens. James Lowe)
ــــــ
29.4 Images of Disease An image database for the teaching of Pathology (Nick Hawkins, Mark Dziegielewski)
ــــــ
ﻣـﻮﺭﺩ ﻧﻈـﺮ ﺑـﻪ ﺗﻮﺻـﻴﻒ ﻣﺎﻛﺮﻭﺳـﻜﻮﭘﻲ ﻭ ﻣﻴﻜﺮﻭﺳـﻜﻮﭘﻲ ﺿـﺎﻳﻌﻪcase ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﺗﻚ ﺗﻚ ﺑﻴﻤﺎﺭﻳﻬﺎ ﻧﻤﻮﻧﻪﻫﺎﻱ ﺑﺎﻓﺘﻲ ﺍﺭﮔﺎﻥ ﺩﺭﮔﻴﺮ ﺑﻴﻤﺎﺭﻱ ﺑﺼﻮﺭﺕ ﻣﺎﻛﺮﻭﺳﻜﻮﭘﻲ ﻭ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﻭﺍﺿﺢ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﻭ ﺿﻤﻦ ﺍﺭﺍﺋﻪ ﺷﺮﺡ ﺣﺎﻝCD ﺩﺭ ﺍﻳﻦ . ﺑﺨﺼﻮﺹ ﺑﻪ ﺩﺳﺘﻴﺎﺭﺍﻥ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻳﺴﺖ ﺩﻣﺎ ﺩﺭ ﺟﻬﺖ ﺗﺸﺨﻴﺺ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﺑﻴﻤﺎﺭﻳﻬﺎ ﻛﻤﻚ ﺷﺎﻳﺎﻥ ﻣﻲﻛﻨﺪ ﻭ ﻧﻤﺎﺩﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻣﻴﻜﺮﻭﺳﻜﻮﺑﻴﻚ ﺑﻴﻤﺎﺭﻳﻬﺎ ﺭﺍ ﺑﺼﻮﺭﺕ ﺟﺪﺍﮔﺎﻧﻪ ﻣﻮﺭﺩ ﺗﻮﺟﻪ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪCD ﺍﻳﻦ،ﻣﻲﭘﺮﺩﺍﺯﺩ 30.4 Immunology (Blackwell Science)
2000
31.4 Interactive Color Atlas of Histology (Version 1.0) (Leslie P. Gartner James L. Hiatt) (LIPPINCOTT WILLIAMS & WILKINS)
2000
32.4 Interactive Embryology The Human Embryo Program (Jay Lash Ph.D.) 33.4 Laboratory Medicine: URINALYSIS (Chemical and microscopic examination of urine Atlas of Microscopic Analysis Procedures for Urinalsis) (Pesce Kaplan Pubishers Inc.)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2000
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
22 Extensive atlas of microscopic analysis: over 50 microphotographs of urine sediment, including cells, casts, and artifacts
Method write-up for 15 chemical urinalysis procedures
Complete Specimen collection section
Interpretation of urine findings in common renal and lower urinary tract diseases
Tables reviewing results of chemical urinalyses
2000
34.4 Media Supplement for Biochemistry (FOURH EDITION) (Roy Tasker Carl Rhodes) 1. Reaction mechanisms
2. Metabolic Pathways
3. Membrane Processes
4. Protein Synthesis
5. Molecular Representations
35.4 Microbes in Motion III (Dr. Gloria Delisle and Dr. Lewis Tomalty Queen's University)
ﻭﻳﺮﻭﺱﺷﻨﺎﺳﻲ ﺍﭘﻴﺪﻭﻣﻴﻮﻟﻮﮊﻱ ﺑﺎﻛﺘﺮﻳﻮﻟﻮﮊﻱ ﻭﺍﻛﺴﻦﻫﺎ
ﺭﺍﻫﻬﺎ ﻭ ﺭﻭﺵﻫﺎﻱ ﻛﻨﺘﺮﻝ ﻭ ﻣﻬﺎﺭ ﺭﺷﺪ ﺑﺎﻛﺘﺮﻳﻬﺎ ﺍﻧﮕﻞﺷﻨﺎﺳﻲ (... ﺗﺮﺍﻧﺴﭙﻮﺯﻭﺭﻫﺎ ﻭ، DNA ﺳﺎﺧﺘﺎﺭ،ﮊﻧﺘﻴﻚ )ﺑﻴﻮﺗﻜﻨﻮﻟﻮﮊﻱ ﺑﺎﻛﺘﺮﻳﻬﺎﻱ ﮔﺮﻡ ﻣﺜﺒﺖ
ﻣﻴﻜﺮﻭﺑﻬﺎﻱ ﺑﻲﻫﻮﺍﺯﻱ ﻣﺤﻴﻄﻲ ﻣﻴﻜﺮﻭﺑﻴﻮﻟﻮﮊﻱ ﻣﺤﻴﻄﻲ ﺑﺎﻛﺘﺮﻳﻬﺎﻱ ﮔﺮﻡ ﻣﻨﻔﻲ
: ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ١٨ ﺩﺍﺭﺍﻱ ﻳﻚ ﻛﺘﺎﺑﺨﺎﻧﻪ ﺷﺎﻣﻞCD ﺍﻳﻦ ﭘﺎﺗﻮﮊﻧﺰ ﻣﺘﺎﺑﻮﻟﻴﺴﻢ ﻣﻴﻜﺮﻭﺑﻲ ﻗﺎﺭﭺﺷﻨﺎﺳﻲ
ﻋﻤﻠﻜﺮﺩ ﺿﺪ ﻣﻴﻜﺮﻭﺑﻬﺎ ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻱ ﻣﻘﺎﻭﻣﺖ ﺿﺪ ﻣﻴﻜﺮﻭﺑﻲ
Miscellaneous
2002
36.4 MICROBIOLOGY AND IMMUNOLOGY (KEN S. ROSENTHAL) (Mosby) 1.
TUTORIAL: I. Topics
II. Systems
ــــــ
2. TEST
III. Random
37.4 MICROBIOLOGY AND MICROBIAL INFECTIONS (Topley & Wilson's) (Albert Balows, Max sussman)
(NINTH EDITION)
ــــــ 1999
38.4 MODERN GENETIC ANALYSIS (Anthony J. F. Griffiths, William M. Gelbart, Jffrey H. Miller, Richard C. Lewontin)
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ Introduction
System Requirements
Getting Started
Reference
Freeman Genetics Web Site
39.4 MOLECULAR CELL BIOLOGY 4.0 (Paul Matusdaru, Amold Berk, S. lawence Zipufsky, David Baltimore, James Damell, Harey lodish) 40.4 NCCL INFOBASE Serving the World's Medical Science Community Through Voluntary Consensus
2000 2002
41.4 PATHOLOGIC BASIS OF DISESE Interactive Case Study Companion to ROBBIMS
ــــــ
Inflammation and Repair Infectious Disease Genitouinary, Breast, and Pregnancy Disorders
Fluid and Hemodynamic Disorders Cardiovascular Diseases Endocrine Diseases
Genetic Disorders Hematopatholory Disorders Skeletal Disorders
(W. B. Saunders Company) (Sixth Edition)
Diseases of Immunity Gastrointestinal Diseases Neuropathology
Neoplasia Diseases of Liver, Galbladder, and Pancreas
Systemic Pathology Diseases of Kidney
42.4 PATHOLOGY (Alan Stevens. James Lowe) 43.4 Peripheral Blood TUTOR
ــــــ
(ANINTERACTIVE TUTORIAL THAT TEACHES THE MICROSCOPIC EXAMINATION OF URINARY SEDIMENT)
ــــــ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖCD ﺍﻳﻦ
Introduction
Cell Morphologies
Disease Associations
Atlas
Overview, Smear Preparation Stain Procedure, Smear Evaluation
Cell Structure, Read Blood Cells, White Blood Cells, Platelets, Artifacts, Quiz
Red Blood Cells, White Blood Cells, Neoplastic Disorder
Cell Morphology Disease Association
44.4 PRINCIPLES OF Molecular Virology • Contents Introduciton Particles Genomes
Final Exam
2000
(THIRD EDITION) Replication
Expression
Infection
Pathogenesis
Novel Infectious Agents
• Appendices Glossary, Abbreviations and Pronounciations
Classification of Sub-Cellular Infections Agents
The History of Virology
45.4 RAPID REVIEW HISTOLOGY AND CELL BIOLOGY (E. ROBERT BURNS, M. DONALD CAVE) (MOSBY) 46.4 Samter's Immunologic Diseases (SIXTH EDITION) (K. Frank Austen, M.D, Michael M. Frank, M.D., John P. Atkinson, M.D., Harvey Cantor, M.D.)
2002 ــــ
: ﻗﺴﻤﺖ ﺍﺻﻠﻲ ﺍﺳﺖ ﻛﻪ ﻫﺮ ﻗﺴﻤﺖ ﺩﺍﺭﺍﻱ ﭼﻨﺪﻳﻦ ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ١٠ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺍﺭﺍﻱ. ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩFlash ﻭInternet explorer ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺍﺳﺖ ﻛﻪ ﺗﺤﺖ ﺑﺮﻧﺎﻣﺔCD ﺍﻳﻦ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
23 ( ﺗﺸﺨﻴﺺ ﻭ ﺷﻨﺎﺳﺎﻳﻲ )ﺍﻳﻤﻨﻲ ﺫﺍﺗﻲ ﻭ ﺍﻛﺘﺴﺎﺑﻲ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺧﺘﺼﺎﺻﻲ ﺍﻧﺪﺍﻡ-
ﻣﻜﺎﻧﻴﺰﻡﻫﺎﻱ ﻣﺆﺛﺮ ﺍﻳﻤﻨﻲ ﺩﺭ ﺍﻳﻤﻨﻲ ﺫﺍﺗﻲ ﻭ ﺍﻛﺘﺴﺎﺑﻲ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺁﻟﺮﮊﻳﻜﻲ-
ﺑﻴﻤﺎﺭﻱ ﻧﻘﺺ ﺍﻳﻤﻨﻲ ﺍﻭﻟﻴﻪ ﺳﻴﺴﺘﻢ ﺍﻳﻤﻨﻲ ﻓﻌﺎﻝ ﻭ ﻏﻴﺮ ﻣﺆﺛﺮ-
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺯﺩﻳﺎﺩ ﻭ ﺗﻜﺜﻴﺮ ﺳﻠﻮﻟﻬﺎﻱ ﺍﻳﻤﻨﻲ ﭘﻴﻮﻧﺪ ﺍﻋﻀﺎﺀ-
ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺳﻴﺴﺘﻤﻴﻚ ﺍﻳﻤﻨﻲ ﺷﻨﺎﺳﻲ ﺩﺭﻣﺎﻧﻲ-
ﻗﺪﺭﺕ ﺑﺰﺭﮔﻨﻤﺎﻳﻲ ﺗﺼﺎﻭﻳﺮ ﻭ ﻧﻤﺎﻳﺶ ﻣﻨـﺎﺑﻊ. ﺗﻮﺍﻧﺎﻳﻲ ﺟﺴﺘﺠﻮ ﻭﺍﮊﻩﻫﺎ ﻭ ﻟﻐﺎﺕ ﺗﺨﺼﺼﻲ ﻭ ﭼﺎﭖ ﻣﺘﻮﻥ ﻛﺘﺎﺏ ﺭﺍ ﺩﺍﺭﺩ. ﺩﺍﺭﺍﻱ ﻳﻚ ﻛﺘﺎﺑﺨﺎﻧﻪ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ ﻓﺼﻞ ﻭ ﻫﺮ ﻣﻮﺿﻮﻉ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺟﺪﺍﻭﻝ ﻭ ﻃﺮﺡﻭﺍﺭﻩﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﺭﺍ ﺑﻪ ﻧﻤﺎﻳﺶ ﻣﻲﮔﺬﺍﺭﺩCD ﺍﻳﻦ .ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﻛﺘﺎﺏ ﺍﺯ ﻭﻳﮋﮔﻴﻬﺎﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﻲﺑﺎﺷﺪ 47.4 The American Society of Hematology (41st Annual Meeting and Exposition)
1999
48.4 The Cell 1.0 A Molecular Approach (Many Animations, Movies, Photos, and drawn images) (Geoffrey M. Cooper)
ــــــ : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ
Cell Overview Organelles & Energy Metabolism
Humman Genetic Diseases The Cytoskeleto
Floww of Information The Plasma Membrane
The Nucleus The Extracellular Machine
The Cell Cycle Cancer-A Family od Diseases
Protein Sorting and Transport The Meiotic Divisions
49.4 THE HUMAN GENOME PROJECT
2003
50.4 The Metabolic and Molecular Bases of Inherited Disease
____
General Themes, Amino Acids, Prophyrins and Heme, Hormones: Synthesis and Action, Defense and Immune Mechanisms, Skin, Cancer and Genetics, Organic Acids, Metals, Vitamins, Connective Tissues, Intesine, Chromosomes and Autosomes, Peroxisomes, Blood and Blood Forming Tissue, Muscle, Neurogenetics, Carbohydrates, Lipoprotein and Lipid Metabolism disorders, Lysosomal Transport, Eye, Signiflcant Developments in Progress, Cancer and NEW Geneticx Update
2000
51.4 UNDERSTAND! Biochemistry (3/e Version) (Lehninger Principles of Biochemistry) 1. THE BACKGROUND 2. THE MOLECULES OF LIFE 3. PROTEINS IN ACTION
4. BIOENERGETICS 5. BIOSYNTHESIS 6. NUCLEIC ACIDS AND THEIR EXPRESSION
7. CELLULAR ARCHITECTURE AND TRAFFIC 8. THE DIVIDING CELL 9. SOME IMPORTANT TECHNIQUES
1999
52.4 UNDERSTAND! Biochemistry (VERSION 1.0)
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ - QUIZE
- INDEX
- Web links
-Minicourses:
53.4 UNDERSTAND! Biology: Biochemistry (Molecules, Cell & Genes)
ــــــ : ﻣﺸﺘﻤﻞ ﺑﺮ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ، ﻓﻮﻕCD
Basic Chemistry
Macromolecular assembly and modification
Bioenegetics
Signal transduction
Enzymology
The flow of genetic information
54.4 Urinalysis TUTOR (ANINTERACTIVE TUTORIAL THAT TEACHES THE MICROSCOPIC EXAMINATION OF URINARY SEDIMENT) (Caria M. Phillips, MLM, MT(ASCP),
Metabolism
Molecular biology techniques
Paul J. Henderson, MS, MT(ASCP), Claudia Bein, BS, MT(ASCP))
ــــــ
. ﻓﺼﻞ ﺭﻭﺵ ﺁﺯﻣﺎﻳﺸﺎﺕ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﻧﻤﻮﻧﻪﻫﺎﻱ ﺍﺩﺭﺍﺭﻱ ﺭﺍ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﺪ٥ ﺩﺭinteractive ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ( ﻋﻔﻮﻧﺖ ﻟﻮﻟﺔ ﺍﺩﺭﺍﺭﻱ، ﻓﻴﻠﻮﻧﻔﺮﻳﺖ، ﺳﻨﺪﺭﻡ ﻧﻔﺮﻭﺗﻴﻚ. ﺑﻴﻤﺎﺭﻳﻬﺎ )ﺳﻨﺪﺭﻡ ﮔﻠﻮﻣﺮﻭﻟﻮﻧﻔﺮﻳﺖ.٥ ( ﺁﺭﺗﻴﻔﻜﺖﻫﺎ، ﺍﺭﮔﺎﻧﻴﺰﻣﻬﺎ، ﻛﺮﻳﺴﺘﺎﻟﻬﺎ، ﺳﺎﺧﺘﺎﺭ ﻭ ﻣﺎﻫﻴﺖ ﺭﺳﻮﺑﺎﺕ ﺍﺩﺭﺍﺭ )ﺑﺮﺭﺳﻲ ﺳﻠﻮﻟﻬﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ ﺍﺩﺭﺍﺭ.٣
.( ﻫﺮ ﺳﺆﺍﻝ ﺑﻪ ﺷﻜﻞ ﻧﻤﺎﻳﺶ ﻳﻚ ﺗﺼﻮﻳﺮ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻣﻮﺭﺩ ﺳﺆﺍﻝ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ. ﺳﺆﺍﻻﺗﻲ ﺑﺼﻮﺭﺕ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ، ﺍﺯ ﻫﺮ ﺑﺨﺶ. ﻣﻲﺑﺎﺷﺪB ﻭA ﺍﻣﺘﺤﺎﻥ ﭘﺎﻳﺎﻧﻲ )ﺷﺎﻣﻞ ﺩﻭﺳﺮﻱ ﺍﻣﺘﺤﺎﻥ.٤
( ﻣﻜﺎﻧﻴﺴﻢ ﻋﻤﻠﻜﺮﺩ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﻭ ﻧﻤﻮﻧﻪﻫﺎﻱ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ، ﺗﻔﺴﻴﺮ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﻧﺘﺎﻳﺞ، ﻣﻘﺪﻣﻪ )ﻋﻤﻠﻜﺮﺩ ﻛﻠﻴﻪ.١ ( ﻓﻬﺮﺳﺖ ﺗﺼﺎﻭﻳﺮ )ﺗﺼﺎﻭﻳﺮ ﻓﺼﻞ ﺩﻭﻡ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺑﺼﻮﺭﺕ ﻣﺠﺰﺍ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﻣﻲﺁﻳﺪ.٢
ﻗﻠﺐ-٥
CD ﻋﻨﻮﺍﻥ 2.4
A Slide Atlas of ATHEROSCLEROSIS Progression and Regression (Herbert C. Stary, MD)
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ 2002
ﻣﻄﺎﻟﻌﻪ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﻪ. ﺍﺳﻼﻳﺪ ﺗﺨﺼﺼﻲ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﭘﻴﺸﺮﻓﺖ ﻭ ﭘﺴﺮﻓﺖ ﺑﻴﻤﺎﺭﻱ ﺁﺗﺮﻭﺍﺳﻜﻠﺮﻭﺯﻳﺲ ﺩﺭ ﺳﻨﻴﻦ ﻣﺨﺘﻠﻒ ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺭﺍ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﻭ ﺍﻟﻜﺘﺮﻭﻧﻲ ﺑﻪ ﺯﻳﺒﺎﻳﻲ ﺑﻪ ﺗﺼﻮﻳﺮ ﻛﺸﻴﺪﻩ ﺍﺳﺖ٩٤ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺎ .ﻣﺘﺨﺼﺼﻴﻦ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﺗﻮﺻﻴﻪ ﻣﻲﺷﻮﺩ 1.5
A visible improvement in angina treatment (VCD) Post-EECP stress perfusion image, Markedly improved anterior, septal, and inferior wall perfusion.
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
2.5 3.5 4.5
24 ACCSAP (Adult Clinical Cardiology Self-Assessment Program) (C. Richard Donti, MD, Richard P. Lewis, MD) (AMERICAN COLLEGE of CARDIOLOGY) Acute Heart Failure (THE CLEVELAND CLINIC FOUNDATION) (W. Frank Peacock, MD) (The Emergency Department and the Economics of Care) American Heart Associations fighting Heart Disease and Stroke Abstracts from Scientific Sessions (Augustus O. Grant, Raymond J. Gibbons)
2000 2004 2002
: ﺑﺤﺚ ﻣﻲﻛﻨﺪ ﺷﺎﻣﻞCD ﻣﺒﺎﺣﺜﻲ ﻛﻪ ﺍﻳﻦ 5.5
6.5
-Basic Science -Clinical Science -Population Science Atlas of Transesophageal Echocardiography (Navin C. Nanda, MD, Michael J. Domanski)
(Williams & Wilkins)
1. Normal Anatomy 2. Prosthetic Valves and Rings
7. Tricuspid and Pulmonary Valves 8. Congenital Heart Disease
3. Mitral Valve 4. Ischemic Heart Disease
5. Aortic Valve and Aorta 6. Cardiomyopathy
ــــــ
BEYOND HEART SOUNDS The Interactive Cardic Exam (John Michael Criley, MD) (VOL 1)
ــــــ
Introduction to anscultation Frontal Chest Anatomy The Cardinal areas of anscultation Using the stethoscope
7.5
Hemodynamics tutorial The cardiac cycle Pulse Tutorial Mitral and aortic valve flow Introduction Hemodynamic changes in disease Carotid Pulses Mitral Stenosis Jugular Venous Pulses Aortic stenosis Cardiac Catheterization, Angiography, and Intervention (SIXTH EDITION) (LIPPINCOTT WILLIAMS & WILKINS)
2000
. ﺩﻗﻴﻘﻪ ﻓﻴﻠﻢ ﺑﻮﺩﻩ ﻭ ﻛﻠﻴﻪ ﺗﺼﺎﻭﻳﺮ ﺑﻪ ﺻﻮﺭﺕ ﺭﻧﮕﻲ ﻣﻲﺑﺎﺷﺪ٣٥ ﻭGrossmam's Cadiac Cathetrization ....... ﺷﺸﻢ ﻛﺘﺎﺏedition ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞCD ﺍﻳﻦ . ﻣﻲﺑﺎﺷﺪProcerdue- related Findinig ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺒﻲ ﻭ ﻧﺮﻣﺎﻝ ﻫﻤﺮﺍﻩ ﺑﺎCase50 ﻭﺟﻪ ﻣﺸﺨﺼﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻓﻴﻠﻢ ﻭﻳﺪﺋﻮﻳﻲ ﺷﺎﻣﻞ . ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ٨ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ (.... ﻗﻠﺐ ﻭ ﻣﻘﺎﻭﻣﺖ ﻋﺮﻭﻕ ﻭoutput ﻭblood flow ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ- ﻣﻮﺍﺭﺩ ﻫﻤﻮﺩﻳﻨﺎﻣﻴﻚ )ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﻓﺸﺎﺭ-٣ ( ﻛﺎﺗﺘﺮﺍﺯﻳﺴﻮﻥ ﺗﺸﺨﻴﺼﻲ ﺩﺭ ﻛﻮﺩﻛﺎﻥ ﻭ ﻧﻮﺯﺍﺩﺍﻥ-Brachiel Cutdown – Percutaneous approuch) Basic ﺗﻜﻨﻴﻚﻫﺎﻱ-٢ ﻣﻼﺣﻈﺎﺕ ﻛﻠﻲ ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ-١ (... ﻭﻇﻴﻔﻪ ﺩﻳﺎﺳﺘﻮﻟﻲ ﻭ ﺳﻴﺴﺘﻮﻟﻲ ﺑﻄﻨﻲﻫﺎ ﻭ،Ejection Fraction ﻃﻲ ﻛﺎﺗﺘﺮﺍﺯﻳﺴﻴﻮﻥ ﻗﻠﺒﻲ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﺣﺠﻢ ﺑﻄﻦﻫﺎTest ﺍﺭﺯﻳﺎﺑﻲ ﻓﺎﻧﻜﺸﻨﺎﻝ ﻗﻠﺒﻲ )ﺍﺳﺘﺮﺱ-٥ ( ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺁﺋﻮﺭﺕ ﻭ ﺷﺮﻳﺎﻧﻬﺎﻱ ﻣﺤﻴﻄﻲ- ﺗﻜﻨﻴﻚﻫﺎﻱ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ) ﺁﻧﮋﻳﻮﻛﺮﻭﻧﺮﻱ – ﻭﻧﺘﺮﻳﻜﻮﻟﻮﮔﺮﺍﻓﻲ ﻗﻠﺒﻲ – ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﻭﭘﻮﻟﻤﻮﻧﺮﻱ-٤ ﺗﻜﻨﻴـﻚﻫـﺎﻱ ﻣﺪﺍﺧﻠـﻪﺍﻱ )ﺁﻧﺘﮋﻳﻮﭘﻼﺳـﺘﻲ ﻋـﺮﻭﻕ-٧ (... ﻭintrathoracic balloon Counter Pulsation - ﺑﺮﺍﻱ ﺩﺭﻣـﺎﻥ ﺁﺭﻳﺘﻴﻤـﻲﻫـﺎdeivce ﻗﺮﺍﺭ ﺩﺍﺩﻥ- ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ- )ﺍﻛﻮﻛﺎﺭﺩﻳﺎﻝ ﺑﻴﻮﭘﺴﻲ: Special Catheter Techniquse -٦ – )ﻃـﺮﺯ ﺷﻨﺎﺳـﺎﻳﻲ ﻭ ﻛﺎﺗﺘﺮﻳﺰﺍﺳـﻴﻮﻥ ﻭ ﺁﻧﮋﻳـﻮﮔﺮﺍﻓﻲ ﺑﻴﻤـﺎﺭﻱﻫـﺎﻱ ﺩﺭﻳﭽـﻪﺍﻱ ﻗﻠـﺐ: ﺩﺭ ﺍﺧـﺘﻼﻻﺕ ﺍﺧﺘﺼﺎﺻـﻲProfile -٨ (ﮔﺬﺍﺭﻱ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮ – ﻣﺪﺍﺧﻠﻪ ﺩﺭ ﻋﺮﻭﻕ ﻣﺤﻴﻄﻲ ﻭ ﻋﺮﻭﻕ ﻛﻮﺩﻛﺎﻥStent- ﺁﺗﺮﻭﻛﺘﻮﻣﻲ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮﻱ ﻭ ﺗﺮﻭﻣﺒﻜﺘﻮﻣﻲ-ﻛﺮﻭﻧﺮﻱ :( ﻓﻴﻠﻢﻫﺎﻱ ﻭﻳﺪﺋﻮﻳﻲ ﺷﺎﻣﻞ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ ﻭ ﺍﻗﺪﺍﻣﺎﺕ ﺩﺭﻣﺎﻧﻲ... ﺑﻴﻤﺎﺭﻱ ﺍﻣﺒﻮﻟﻲ ﺭﻳﻪ ﻭ-ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺮﺍﺋﻴﻦ ﻛﺮﻭﻧﺮﻱ ﺍﺧﺘﻼﻻﺕ ﻭﻧﺘﺮﻳﻜﻮﻟﻮﮔﺮﺍﻓﻲ ﺑﻄﻦ ﭼﭗ ﻏﻴﺮ ﺁﺗﺮﻭﺳﻜﺮﻭﺗﻴﻚCAD ﺁﻧﻮﻣﺎﻟﻴﻬﺎ ﻭBasic ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ ﺍﺧﺘﻼﻻﺕ ﺁﺋﻮﺭﺕ ﻭ ﻋﺮﻭﻕ ﻣﺤﻴﻄﻲ.( ﻣﻲﺑﺎﺷﺪ.... ﻭRotabalator ﺑﺎﻟﻮﻥﮔﺬﺍﺭﻱ ﻭ ﻭﺍﻟﻮﭘﻼﺳﺘﻲ- ﻋﻮﺍﺭﺽ- ﮔﺬﺍﺭﻱStent) ﻣﺪﺍﺧﻼﺕ ﺩﺭﻣﺎﻧﻲ ﺷﺎﻣﻞ8.5
Cardiovascular Surgery (VCD) (CD I, II, III) Excerpted from "Medical & Surgical Controversies in CV disease: The Aorta and Peripheral Vessels" Course Directors: Thoralf M. Sundt III, MD and Peter C. Spittell, MD
2004
9.5
CathSAP Cardiac Catheterization and Interventional Cardiology Self-Assessment Program (Carl J. Pepine, MD, Steven E. Nissen, MD)
ــــــ
10.5 Challenging established treatment patterns in chronic heart failure
A Satellite Symposium held during the ESC Heart Failure meeting
11.5 Clinical TRANSESOPHAGEAL ECHOCARDIOGRAPHY (A PROBLEM- ORIENTED APPROACH) (Second Edition)
(Steven N. Konstadt)
2003 2003
12.5 Clinical Utility of Contrast Echocardiography
2001
13.5 Congestive Heart Failure
ــــــ
Sonovue: An ideal contrast agent for Low MI myocardial Perfusion (Dr. Daniela Bokor, Bracco sa, Milano) What's new in cardic echography (Dr. Luciano Agati, University "La Sapienza Roma" Ischemic coronary artery disease (Dr. Harld Becher, John Radcliffe Hospital, Oxford)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(NOVARTIS) (CD I , II)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
25 ﺍﺑﺘﺪﺍ ﭘﺰﺷﻚ ﺳﺆﺍﻻﺗﻲ ﺍﺯ ﺑﻴﻤﺎﺭ ﻣﻲﻛﻨﺪ ﻭ ﺑﻴﻤﺎﺭCase report ﺩﺭ. ﻓﻴﻠﻢ ﻭﻳﺪﺋﻮﻳﻲ ﻭ ﻓﺎﻳﻞ ﺻﻮﺗﻲ ﻣﻲﺑﺎﺷﺪ،Case report ، ﺷﺎﻣﻞ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲCD ﺍﻳﻦ. ﻣﻲﺑﺎﺷﺪFrank .H.Netter ﻣﺆﻟﻒ ﻛﺘﺎﺏ. ﺩﺭ ﻣﻮﺭﺩ ﻗﻠﺐ ﻣﻲﺑﺎﺷﺪCiba ﺷﺎﻣﻞ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲCD ﺍﻳﻦ ﺩﻭ . ﻣﻲﺑﺎﺷﺪCHF ﻭ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺑﻴﻤﺎﺭﻱmultiple choice test ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ. ﺳﭙﺲ ﻣﻌﺎﻳﻨﻪ ﻓﻴﺰﻳﻜﻲ ﺑﻴﻤﺎﺭ ﺗﻮﺳﻂ ﻓﻴﻠﻢ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺍﻃﻼﻋﺎﺕ ﺑﻴﺸﺘﺮ ﺗﻮﺳﻂ ﻛﺎﺭﺑﺮ ﺑﺎ ﻛﻠﻴﻚ ﻛﺮﺩﻥ ﺑﺮ ﺭﻭﻱ ﺩﻛﻤﻪﻫﺎ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺩﺳﺖ ﺁﻭﺭﺩ.ﺑﻪ ﺳﻮﺍﻻﺕ ﺟﻮﺍﺏ ﻣﻲﺩﻫﺪ . ﻣﻲﺑﺎﺷﺪCHF ﻭ ﺩﺭﻣﺎﻥmanagement ، ﺗﺸﺨﻴﺺ.٤
CHF ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ.٣
CHF ﺍﺗﻴﻮﻟﻮﮊﻱ ﻭ ﺗﻌﺮﻳﻒ ﺑﻴﻤﺎﺭﻱ.٢
ﻋﻤﻠﻜﺮﺩ ﻧﺮﻣﺎﻝ ﻗﻠﺐ ﻭ ﺳﻴﺴﺘﻢ ﻋﺮﻭﻗﻲ.١ : ﻓﺼﻮﻝ ﻛﺘﺎﺏ ﺷﺎﻣﻞ
14.5 Coronary Heart Disease (J. Hurley Myers, Ph.D., Frank H. Netter, M.D.)
ﺁﻣﻮﺯﺵ ﺑﺎﻟﻴﻨﻲ ﻭ ﺑﻴﻤﺎﺭﻱ-٢ ﺁﻣﻮﺯﺵ ﭘﺰﺷﻜﻲ-١ :ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ﺩﻭ ﺑﺨﺶ ﻣﻲﺑﺎﺷﺪ ﺗﺸﺨﻴﺺ ﻭ ﻣﺪﻳﺮﻳﺖ ﺩﺭﻣﺎﻥ-٤ ﺍﻧﻔﺎﺭﻛﺘﻮﺱ ﻣﻴﻮﻛﺎﺭﺩ-٣ ﺁﺗﺮﻭﺍﺳﻜﻠﺮﻭﺯﻳﺲ-٢ ﺁﻧﺎﺗﻮﻣﻲ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮﻱ-١ :ﺑﺨﺶ ﺍﻭﻝ ﺷﺎﻣﻞ . ﻛﺎﺭﺑﺮ ﻣﻲﺗﻮﺍﻧﺪ ﻳﺎﺩﺩﺍﺷﺖ ﺷﺨﺼﻲ ﺧﻮﺩ ﺭﺍ ﺍﺿﺎﻓﻪ ﻭ ﺫﺧﻴﺮﻩ ﻧﻤﺎﻳﺪ، ﺩﺭ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﻣﻮﺿﻮﻋﺎﺕ.ﻫﺮ ﻳﻚ ﺍﺯ ﭼﻬﺎﺭﻓﺼﻞ ﻓﻮﻕ ﺩﺍﺭﺍﻱ ﭼﻨﺪﻳﻦ ﺯﻳﺮﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺼﻮﺭﺕ ﺗﺼﺎﻭﻳﺮ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ ﻣﺘﻨﻲ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ﻭ-٩ ﺩﺍﺭﻭ ﺩﺭﻣﺎﻧﻲ-٨ ﺭﻭﺷﻬﺎﻱ ﺗﺸﺨﻴﺼﻲ-٧ ﺍﻧﻔﺎﺭﻛﺘﻮﺱ ﻣﻴﻮﻛﺎﺭﺩ-٦ ﺁﻧﮋﻳﻦ ﺻﺪﺭﻱ-٥ ﭘﻴﮕﻴﺮﻱ ﺍﺯ ﺑﻴﻤﺎﺭﻱ ﺍﻧﺴﺪﺍﺩ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮ-٤ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺴﺪﺍﺩ ﺳﺮﺧﺮﮔﻬﺎﻱ ﺍﻛﻠﻴﻠﻲ-٣ ﻋﺮﻭﻕ ﺧﻮﻧﻲ ﻗﻠﺐ-٢ ﻣﻘﺪﻣﻪ-١ ﻣﺒﺎﺣﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺷﺎﻣﻞ:ﺩﺭ ﺑﺨﺶ ﺩﻭﻡ .ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﻋﻨﺎﻭﻳﻦ ﻓﻮﻕ ﺗﻮﺳﻂ ﮔﻮﻳﻨﺪﻩ )ﺑﺎ ﭘﺨﺶ ﺻﺪﺍ( ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ (ﻋﻤﻞ ﺟﺮﺍﺣﻲ )ﺍﻳﻦ ﺑﺨﺶ ﺩﺍﺭﺍﻱ ﻓﻴﻠﻤﻬﺎﻱ ﻛﻮﺗﺎﻩ ﺍﺯ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﻗﻠﺐ ﻣﻲﺑﺎﺷﺪ
ــــــ
15.5 Dynamic Practical Electrodiography (Lippincott Williams & Wilkins)
ــــــ
16.5 ECG (Jay W. Mason, MD)
ــــــ
17.5 ECG DIAGNOSIS MADE EASY ROMEO VEGHT ﻓﺼﻞ ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﻣـﻮﺍﺭﺩ٩ . ﺗﻮﺍﻧﺎﻳﻲ ﺟﺴﺘﺠﻮﻱ ﻧﻤﻮﺩﺍﺭﻫﺎﻱ ﻭ ﭼﺎﭖ ﻭ ﺫﺧﻴﺮﺓ ﺁﻧﻬﺎ ﻧﻴﺰ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. ﮔﻮﻧﺎﮔﻮﻥ ﺍﺳﺖECG ﻋﺪﺩ ﻧﻤﻮﺩﺍﺭ٣٥٠ ﺩﺍﺭﺍﻱ. ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩInternet explorer ﻓﺼﻞ ﺍﺳﺖ ﻭ ﺗﺤﺖ ﺑﺮﻧﺎﻣﺔ٩ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻣﺸﺘﻤﻞ ﺑﺮ :ﺯﻳﺮ ﺍﺳﺖ 1. Basic Priciples ( ﻫﺪﺍﻳﺖ ﺟﺮﻳﺎﻥ ﺍﻟﻜﺘﺮﻳﻜﻲ، ﺩﭘﻮﻻﺭﻳﺰﺍﺳﻴﻮﻥ ﻋﻀﻠﻪ، ﻣﻮﻗﻌﻴﺖ ﺍﻟﻜﺘﺮﻭﺩﻫﺎ،ﻧﺮﻣﺎﻝ 3. ECG ﻭ ﻧﺤﻮﺓ ﺿﺒﻂ....) Ischaemic (Coronary) heart disease 5. Conductin impairment 7. Rhythm disturbances 2. Hypertrophy
6. Chardiomyopathies and autoimmune disorders
4. Pericarditis, myocarditis and metabolic disorders
6. Pacemakers, ICDs and cardioversion Mixed ECG quizzes
ﺭﺍ ﻣﻲﺯﻧﻴﻢ ﻣﺴﻴﺮ ﻧﺼﺐ ﭘﺮﺳﻴﺪﻩ ﻣﻲﺷﻮﺩ ﺩﺭ ﺻﻮﺭﺕ ﺗﻮﺍﻓـﻖNext ﺳﭙﺲ. ﺭﺍ ﺍﺟﺮﺍ ﻣﻲﻛﻨﻴﻢSetup ﻓﺎﻳﻞ. ﻣﻲﺷﻮﻳﻢSetup ﺷﺪﻩ ﻭ ﺍﺯ ﺁﻧﺠﺎ ﻭﺍﺭﺩ ﺷﺎﺧﻪCD ﺑﻌﺪ ﻭﺍﺭﺩ ﺩﺭﺍﻳﻮ. ﻣﻲﺷﻮﻳﻢmy 18.5 ECG-SAP III (Jay W. Mason, MD, FACC) -Using ECG-SAP III -Standard Tracings -Syndromes 19.5
ــــــ
computer ﺭﺍ ﺩﺭﻭﻥ ﺩﺭﺍﻳﻮ ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﻭ ﺳﭙﺲ ﻭﺍﺭﺩCD ﺍﺑﺘﺪﺍ:( ﻃﺮﻳﻘﺔ ﻧﺼﺐ . ﺭﺍ ﻓﺸﺎﺭ ﻣﻲﺩﻫﻴﻢFinish ﺭﺍ ﻣﻲﺯﻧﻴﻢ ﺑﺮﻧﺎﻣﻪ ﻧﺼﺐ ﻣﻲﺷﻮﺩ ﺩﺭ ﭘﺎﻳﺎﻥNext
ــــــ -Computer Overreads
-Serial Tracings
-Stress Testing
-ECG of the Month
-Guidelines
-Utilities
Echo Lecture (VIDEO SERIES) (7CD) (Mayo) : ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢ ﻣﻲﺑﺎﺷﺪ ﺷﺮﺡ ﻋﻨﺎﻭﻳﻦ ﺁﻥ ﺑﻪ ﺻﻮﺭﺕ ﺯﻳﺮ ﺍﺳﺖCD ﺳﺮﻱ٧ ﺍﻳﻦ ﻣﺠﻤﻮﻋﻪ ﻛﻪ ﺷﺎﻣﻞ
ــــــ
1. TEE in the Operating Room (Bijoy K. Khandheria, MD) Intraoperative echocardiography has become an essential component to the surgical approach to valvular disease. Dr. Bijoy Khandheria discusses the utility of intraoperative echocardiography and its impact on the surgical management of cardiovascular disease.
2. TEE in Adult Congenital Heart Disease (James B. Seward, M.D.)
Dr. James Seward Presents Adult Congenital Heart Disease. A generation of Children Have Grown into adulthood and Present with postoperative congenital heart disease. Transesophageal echocardiography is extremely helpful but may not always be necessary in the assessment of adult congenital heart disease. Learn from the expert regarding appropriate use of transesophageal echocardiography and assessment of residua and sequela of adult congenital heart disease.
3. Understanding Operative Procedures for Patients with Univentricular Heart from Palliation to Fontan (James B. Seward, M.D.) Dr. Seward gives a detailed overview of complex anomalies and their applicable corrections. Topics included are Blalock, Mustard, Glen and Fontan corrections. Graphic depictions of each corrective procedure, possible complications and echocardiographic example are included.
4. Mitral Valve Regurgitation: Essential Measurements. Pitfalls and Limitations. (Fletcher A. Miller, Jr., MD)
Dr. Fletcher Miller discusses and presents the current approach to the quantitative evaluation of mitral valve regurgitation. This is an excellent review of current quantitative assessment of mitral valve regurgitation including pitfalls and limitations.
5. Mitral Vale Regurgitation: Evidence-Based Practice (A. Jamil Tajik, MD) A Classic presentation by Dr. A. Jamil Tajik on a change in clinical practice with regard to the quantitation of regurgitation and then a change in medical management with early surgery and repair of the mitral valve.
6. Evaluating the Patient with Prothetic Valve (Fletcher A. Miller, Jr., MD) Dr. Fletcher Miller, an expert on the echocardiographic assessment of prosthetic valves, presents a detailed in-depth review of the quantitative echo Doppler approach to the prosthetic valve. It is important to understand the hemodynamic pitfalls and limitations of the echocardiographic assessment of cardiac prosthetic valves.
7. Stress Echocardiography and Contrast (Patricia A. Pellikka, M.D.) ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
26 Stress Echocardiography and Contrast Using illustrative cases, Dr. Pellikka gives an expert presentation and discussion on the role of contrast in stress echocardiography. Pitfalls and limitations of contrast stress echocardiography are also discussed. New Horizons in Stress Echocardiography Dr. Pellikka, an expert in Stress echocardiography, discusses Dobutamine stress echocardiography and its role in preoperative risk stratification. Also discussed are new advances in stress echocardiography such as color kinesis and acoustic quantification, color Doppler imaging, and strain and strain rate imaging.
ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (UPDATE NO. 1) (TRANSESOPHAGEAL- ECHOCARDIOGRAPHY) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 1) (VCD) (ECHOCARDIOGRAPHY Normal 2-D And M-MODE EXAM)) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 10) (VCD) (CARDIAC MASSES) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 11-A,B) (VCD CD I, ii) (ECHOCARDIOGRAPHIC ASSESSMENT OF PROSTHETIC HEART VALVES) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 12) (VCD) (INTERVENTIONAL ECHOCARDIOGRAPHY) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 2) (VCD) (DOPPLER AND COLOR FLOW IMAGING: PHYSICS, INSTRUMENTATIONS AND THE NORMAL EXAM) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 4) (VCD) (ECHOCARDIOGRAPHY IN AORTIC VAL VE DISEASE) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 5) (VCD) (ECHOCARDIOGRAPHY IN CORONARY HEART DISEASE) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 6) (VCD) (ECHOCARDIOGRAPHY IN CONGENITAL HEART DISEASE IN THE ADULT) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 7) (VCD) (ECHOCARDIOGRAPHY IN CARDIOMYOPATHIES: DILATED, RESTRICTIVE AND HYPERTROPHIC) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 8) (VCD) (ECHOCARDIOGRAPHY IN PERICARDIAL DISEASE) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME 9) (VCD) (ECHOCARDIOGRAPHY IN TRICUSPID AND PULMONIC VALVE DISEASE AND DESEASES OF THE AORTA) ECHOCARDIOGRAPHY 2-D/DOPPLER WITH COLOR FLOW IMAGING (VOLUME3) (VCD) (ECHOCARDIOGRAPHY IN MITRAL VALVE DISEASE) EchoSAP III (Echocardiography Self-Assessment Program)(Echocardiography Overview: Technique and Applications) (Volume 1) 33.5 (Jemes D. Thomas, MD, Ellen Mayer-Sabik, MD)
20.5 21.5 22.5 23.5 24.5 25.5 26.5 27.5 28.5 29.5 30.5 31.5 32.5
-Introduction and Overview -Examinations -Applications -Self-Assessment Questions -Evidence-Based Medicine -Conclusions 34.5 Electronic Image Collection of Comprehensive Vascular and Endovascular Surgery (John W. Hallet, Joseph L. Mills, Jonothan J. Eamsbaw, Jim A Reekers) 1. Background 3. claudication 2. Mesenteric Syndromes 4. Renovascular disease
5. Chronic Lower Extremity Ischemia 6. Aneurysmal Disease
7. Acute Limb Ischemia 8. Cerebrovascular Disease
ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ ــــــ 2000
2004
9. Upper Extremity Problems 10. Venous Disease
35.5 ENDOVASCULAR TECHNIQUES (Abdominal Aortic Aneurysms) (Workshop) (l. Flessenkämper) (15th Endovascular Symposium Berlin)
ــــــ
36.5 ESC Congress
2004
37.5 EVOLVING ISSUES IN THE MANAGEMENT CHD SECTION 1
(National Lipid Education Council
SECTION II
TM
2002
)
SECTION III
SECTION IV
SECTION V
Emerging Evidence-Based Data From Clinical Trials PAD Lipids and Risk Inflammatory Markers: Anovel Approach Use of Genomics to discover new targets for therapy Case study: Diabetes NON-HDL-Case Secondary Targert of Therapy Lipid Management Though combination Therapy Case Study: Novel Risk Markers Examining the nonlipid effects of statins What is it's Role in clinical practice? Case Study:Combination Therapy Case Study: NON-HDL-C
38.5 HEART DISEASE (FIFTH EDITION)
A Textbook of Cardiovascular Medicine (W.B. SAUNDERS COMPANY)
. ﻛﺘﺎﺏ ﻣﺠﺰﺍ ﺗﺸﻜﻴﻞ ﺷﺪﻩ ﺍﺳﺖ٤ ( ﺍﺯe-book) ﺩﺭ ﻭﺍﻗﻊ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ (Mendelsohn) Reviwe and Assessment Book -٤ (Hennekens) Clinical Trials in Cardiovascular Disease -٣ (chien) Molecular Basis of Heart Disase -٢ (Braunwald) Heart Disease -١ )ﺟﺴﺘﺠﻮ( ﺑﺨﺼﻮﺹ ﺑﺮﺍﻱ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎﻱ ﺭﺷﺘﻪﻫﺎﻱ ﻗﻠﺐ ﻭSearch ﻗﺎﺑﻠﻴﺖCD ﺧﺼﻮﺻﻴﺖ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮﺩ ﺍﻳﻦ. ﺳﻮﺍﻝ ﻭ ﺟﻮﺍﺏ ﻣﻲﺑﺎﺷﺪ٧٠٦ ﺩﺭ ﺁﺧﺮ ﻫﺮ ﻓﺼﻞ ﺳﻮﺍﻻﺕ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﺑﺎ ﺟﻮﺍﺏ ﺗﺸﺮﻳﺤﻲ ﻭ ﺭﻓﺮﺍﻧﺲ ﻛﺘﺎﺏ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻛﻪ ﻣﺸﺘﻤﻞ ﺑﺮ ( ﻫﻤﮕﻲe-book) ﺷﻜﻞ ﻭ ﻧﻤﻮﺩﺍﺭﻫﺎﻱ ﺍﻳﻦ. ﻣﻲﺗﻮﺍﻧﺪ ﺩﺭ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺍﺭﺗﻘﺎﺀ ﻭ ﺑﻮﺭﺩ ﻭ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺩﺭﻭﻥ ﺑﺨﺸﻲ ﻛﻤﻚ ﻗﺎﺑﻞ ﺗﻮﺟﻬﻲ ﻧﻤﺎﻳﺪCD ﺳﺮﻳﻊ ﻭ ﻭﺳﻴﻊ ﺍﻳﻦSearch ﻫﻢﭼﻨﻴﻦ ﻗﺎﺑﻠﻴﺖ.ﺩﺍﺧﻠﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﭘﻴﺪﺍ ﻛﺮﺩﻥ ﻣﻮﺿﻮﻋﻲ ﻳﺎ ﺣﺘﻲ ﻛﻠﻤﺎﺕ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﻣﻲﻧﻤﺎﻳﺪ . ﺷﻮﺩCCU ﻫﺎ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺳﺎﺗﻴﺪ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎ ﻭ ﻛﺎﺭﻛﻨﺎ ﻥ ﺑﺨﺶﻫﺎﻱ ﻗﻠﺐ ﻭclub ﺭﻧﮕﻲ ﺍﺳﺖ ﻭ ﻣﻲﺗﻮﺍﻧﺪ ﺑﺮﺍﻱ ﺗﺪﺭﻳﺲ ﻭ ﻳﺎ ﻛﻨﻔﺮﺍﻧﺲ ﻭ
39.5 HEART SOUNDS
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ــــــ
ــــــ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
27 40.5 HEART SOUNDS Basic Cardiac Auscultation Version 3.0 (Leonard Werner, M.D., Brian Pitts, David Gilsdorf)
2003
41.5 Heart Sounds Basic Cardiac Auscultation CD-ROM to Accompany (M.D., F.A/C.P., Brian Pitts, M.D., David Gilsdorf) (Lippincott Williams & Wilkins)
2003
42.5 Highlights
2004
ESC Congress
43.5 HURST'S THE HEART (R. Wayne Alexander, Robert C. Schlant, Valentin Fuster)
ــــــ
. ﺩﺍﺭﺩCD ﻓﺼﻠﻲ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺮﺍﻱ ﺷﻜﻞﻫﺎ ﻭ ﻧﻤﻮﺩﺍﺭﻫﺎﻱ ﻛﺘﺎﺏ ﻭ ﻫﻢ ﭼﻨﻴﻦ ﻓﺼﻠﻲ ﺩﻳﮕﺮ ﺑﺮﺍﻱ ﺻﺪﺍﻫﺎﻱ ﻗﻠﺒﻲ ﺑﻪ ﺻﻮﺭﺕ ﻓﺎﻳﻞ ﺻﻮﺗﻲ، ﻓﺼﻞ١٦ ﻣﺸﺘﻤﻞ ﺑﺮHurst ﻛﺘﺎﺏText ﻧﻬﻢ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻋﻼﻭﻩ ﺑﺮEdition ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺣﺎﺿﺮ . ﺍﺳﺘﻔﺎﺩﻩ ﻛﺮﺩ،( ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺨﺼﻲ ﻣﻲﺗﻮﺍﻥ ﺑﺮﺍﻱ ﺗﺪﺭﻳﺲ )ﺑﺨﺼﻮﺹ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺷﻜﻞﻫﺎﻱ ﺗﻤﺎﻡ ﺭﻧﮕﻲ ﺁﻥCD ﺍﺯ ﺍﻳﻦ. ﺗﺴﺖﻫﺎﻱ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ ﻓﺼﻞ ﻫﻤﺮﺍ ﺑﺎ ﺟﻮﺍﺏ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖCDﺩﺭ ﺁﺧﺮﺍﻳﻦ 44.5 Interactive Echocardiography: A Clinical Atlas
(Th. Binder, M.D., G. Rehak,G. Porenta. M.D., Ph.D., M. Zengeneh, M.D., G. Maurer, M.D., H. Baumgartner, M.D.)
University of Vienna, Austria
45.5 Interventional Cardiology Clinical Resource (Disc 1 & 2) (Evidence . Analysis . Recommendations . Consensus Reports) 46.5 Intra-Aortic Balloon Catheter Insertion and Removal Technique 1. INTRODUCTION
2. LAB SELECTION
3. LAB PREPARATION
4. LAB INSERTION
(ARROW) 5. LAB CATHETER
PREPARATION
6. LAB CATHETER INSERTION
7. LAB REMOVAL : ﺷﺎﻣﻞCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ
47.5 Mastering Auscultation An Audio Tour to Cardiac Diagnosis Clinical Findings Diagnosis Treatment Tutorial Text Reference (Dr. Anthony Don Michael's) 48.5 MVP Video Journal of Cardilogy (Maria-Teresa Olivari, M.D., Antonio M. Gotto, M.D., D. Phill.) ﺍﻳـﻦ. ﻳﻚ ﻣﻮﺿﻮﻉ ﺑﻪ ﺷﻜﻞ ﻣﺼﺎﺣﺒﺔ ﻋﻠﻤﻲ ﺑﺎ ﻳﻚ ﻣﺘﺨﺼﺺ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤـﺎﻳﺶ ﺍﺳـﻼﻳﺪ ﻭ ﻧﻤـﻮﺩﺍﺭ ﺑﺤـﺚ ﺷـﺪﻩ ﺍﺳـﺖ، ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ. ﺩﻗﻴﻘﻪ ﺩﺭ ﺳﻪ ﻗﺴﻤﺖ ﻣﺠﺰﺍ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ٤٥ ( ﺑﻪﻣﺪﺕVCD ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ )ﺩﺭ ﻗﺎﻟﺐMVP ﻫﺎﻱ ﺁﻣﻮﺯﺷﻲCD ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺯ ﺳﺮﻱ :ﻣﻮﺿﻮﻋﺎﺕ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ
ــــــ 2003 2002 ــــــ ــــــ
1-Determination of Rejection in the Cardiac transplant Recipient
Maria-Teresa Olivari ﺩﻛﺘﺮ: ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ . ﺭﻭﺷﻬﺎﻱ ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻳﻜﻲ )ﺁﻧﺘﻲ ﻣﻴﻮﺯﻳﻦ( ﻭ ﺩﻳﮕﺮ ﺭﻭﺷﻬﺎﻱ ﻏﻴﺮﺗﻬﺎﺟﻤﻲ ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ،MRI ، ﺍﻛﻮﺩﺍﭘﻠﺮ،ﭘﻴﮕﻴﺮﻱ ﻭ ﺗﺸﺨﻴﺺ ﺭﺩ ﭘﻴﻮﻧﺪ ﻗﻠﺐ ﺑﻪ ﻛﻤﻚ ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ Antonio Gotto ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ 2- Triglycerides, HDL and coronary Heat Disease . ﻭ ﺭﻋﺎﻳﺖ ﺍﺻﻮﻝ ﺑﻬﺪﺍﺷﺘﻲ ﺩﺭ ﺯﻣﻴﻨﺔ ﻋﺎﺭﺿﺔ ﻋﺮﻭﻕ ﻛﺮﻭﻧﺮﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ، ﺑﻴﻤﺎﺭﻱ ﺩﻳﺎﺑﺖ ﻭ ﺭﻭﺷﻬﺎﻱ ﺩﺍﺭﻭﺩﺭﻣﺎﻧﻲ.ﻛﻠﻴﺔ ﺭﻳﺴﻚ ﻓﺎﻛﺘﻮﺭﻫﺎ ﻭ ﻋﻮﺍﻣﻞ ﻣﺆﺛﺮ ﺑﺮ ﺁﻧﻬﺎ ﺩﺭ ﻋﺎﺭﺿﺔ ﺭﮔﻬﺎﻱ ﻛﺮﻭﻧﺮﻱ ﻗﻠﺐ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ 3- Management of Cardiac Disease in Pregnancy Carl E. Orringer ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ ﺍﻓﺰﺍﻳﺶ، ﻛﺎﺭﺩﻳﻮﻣﻴﻮﭘﺎﺗﻲ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ، ﺩﺭﻣﺎﻥ ﺩﺍﺭﻭﻳﻲ ﺑﻴﻤﺎﺭﺍﻥ ﻗﻠﺒﻲ ﺑﺎﺭﺩﺍﺭ،... ﻭMRI ، ﺗﺸﺨﻴﺺ ﺑﻪ ﻛﻤﻚ ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ، ﺳﻤﻊ ﻗﻠﺐ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﻗﻠﺒﻲ ﺑﺎﺭﺩﺍﺭ، ﺗﻨﻔﺴﻲ- ﻋﻼﺋﻢ ﻗﻠﺒﻲ،(... ﺍﻳﺴﺖ ﻗﻠﺒﻲ ﻭ، ﺣﺠﻢ ﺿﺮﺑﻪﺍﻱ، ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻗﻠﺐ ﺩﺭ ﺯﻣﺎﻥ ﺑﺎﺭﺩﺍﺭﻱ )ﺑﺮﻭﻥﺩﻩ ﻗﻠﺒﻲ،ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ . ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﻭ ﻧﻤﻮﺩﺍﺭ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺷﺪﻩ ﺍﺳﺖ... ﻓﺸﺎﺭ ﺧﻮﻥ ﺩﺭ ﺑﺎﺭﺩﺍﺭﻱ ﻭ
49.5 MVP Video Journal of Cardiology (Anthony C. Pearson, M.D., Charles B. Higgins, M.D., William W. O'Neill, M.D.) (VCD)
ــــــ
: ﺍﻳﻦ ﻣﻮﺿﻮﻋﺎﺕ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ. ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﻳﻚ ﻣﻮﺿﻮﻉ ﺑﻪ ﺷﻜﻞ ﻣﺼﺎﺣﺒﺔ ﻋﻠﻤﻲ ﺑﺎ ﻳﻚ ﻣﺘﺨﺼﺺ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﻪ ﻭ ﻓﻴﻠﻢ ﻭ ﻧﻤﻮﺩﺍﺭ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺷﺪﻩ ﺍﺳﺖ. ﺩﻗﻴﻘﻪ ﺩﺭ ﺳﻪ ﻗﺴﻤﺖ ﺍﺭﺍﺋﻪ ﺷﺪﻩﺍﻧﺪ40 ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻣﺪﺕMVP ﻫﺎﻱ ﺁﻣﻮﺯﺷﻲCD ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺯ ﺳﺮﻱ 1- The stately Art of MR in Cardiovascuvlar Disease Charles P. Higgins ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ . ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ.... ﻭMRI ﺩﺭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻗﻠﺒﻲ ﻋﺮﻭﻗﻲ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﻭ ﺗﺼﺎﻭﻳﺮMRI ﻛﺎﺭﺑﺮﺩ، ﺭﻭﺵﻫﺎﻱ ﻣﺘﻌﺪﺩ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺩﺭ ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ، MRI ﺗﺎﺭﻳﺨﭽﺔ،ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ 2. Arguing for Angioplasy in Acute Myocardial infction William w. ONeill ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ ﺑﺮﺁﻭﺭﺩ ﺩﻳﺴﻚ ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ﻭ ﺑﻪ ﻛﻤﻚ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﻭ ﻓﻴﻠﻢ، ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥ ﺍﻧﮋﻳﻮﭘﻼﺳﺘﻲ، Lone PTCA ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ،ﺗﺎﺭﻳﺨﭽﻪ ﺍﻧﮋﻳﻮﭘﻼﺳﺘﻲ Anthony C. Pearson : ﺩﻛﺘﺮ:ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ 3- Improved understanding of cardioembolic Stroke prorided by Transesophageal Echoecardiography . ﻣﺨﺘﻠﻒ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺷﺪﻩ ﺍﺳﺖCase ﺍﺯ ﭼﻨﺪﻳﻦTEE ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﻭ ﺗﻮﺿﻴﺢ ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻡ،TEE ﻭTEE ﻣﻘﺎﻳﺴﻪ ﺭﻭﺵ،TEE ﺗﺎﺭﻳﺨﭽﻪ ﺗﻜﻨﻴﻚ،ﺗﺎﺭﻳﺨﭽﺔ ﺩﺭﻣﺎﻥ ﺁﻣﭙﻮﻟﻲﻫﺎ 50.5 MVP VIDEO JOURNAL OF CARDIOTHORACIC SURGERY (VIDEO SEGMENT I & II) Thromboexclusion for Treatment of Descending Aortic Dissection (John A. Elefteriades, MD)
ــــــ
51.5 Perioperative Transesophageal Echocardiography
2003
1. Basics of Echocardiography
(Patricia M. Applegate, Richard L. Applegate, I)
2. Clinical TEE Examination
3. Clinical Uses of Perioperative TEE
4. Unknowns
5. Perioperative
52.5 PLUMER'S PRINCIPLES & PRACTICE OF INTERAVENOUS THERAPY (SEVEN EDITION) (Sharon M. Weinstein)
ــــــ
53.5 TEE An Intractive Exam Review on CD-ROM (CD I , II) (Lippincott Williams & Wilkins)
2002
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
28 nd )54.5 TEXTBOOK OF CARDIOVASCULAR MEDICINE (2 Edition) (ERIC J. TOPOL
ــــــ
CDﺣﺎﺿﺮ ﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﻛﺘﺎﺏﻫﺎﻱ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺍﺳﺖ ﻛﻪ ﻋﻼﻭﻩ ﺑﺮ Textﺩﺍﺭﺍﻱ ﻗﺎﺑﻠﻴﺖﻫﺎﻱ ﻓﻴﻠﻢ ،ﻋﻜﺲ ﻭ ﻓﺎﻳﻞﻫﺎﻱ ﺻﻮﺗﻲ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺐ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ CDﺷﺎﻣﻞ ﻛﺘﺎﺏ ﺩﻭ ﺟﻠـﺪﻱ Text book of Cardiovascular Medicineﺍﺳـﺖ ﻛـﻪ ﻭﺟﻮﺩ ﺻﺪﻫﺎ ﻋﻜﺲ ﻭ ﻛﻠﻴﭗ ﻭﻳﺪﺋﻮﺋﻲ ﻛﺘﺎﺏ ﺭﺍ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﺠﻤﻮﻋﺔ ﺯﻧﺪﻩ ﺩﺭ ﺁﻭﺭﺩﻩ ﺍﺳﺖ) .ﺑﻪ ﻋﻨﻮﺍﻥ ﻣﺜﺎﻝ ﺩﺭ ﻣﻮﺭﺩ ﺗﻨﮕﻲ ﺩﺭﻳﭽﻪ ﻣﻴﺘﺮﺍﻝ ﺩﺭ ﺑﺨﺶ ﻣﺮﺑﻮﻃﻪ ﻋﻼﻭﻩ ﺑﺮ ﻣﺘﻦ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲ ﺩﺭ ﺿﺎﻳﻌﻪ ،ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱﻫﺎ )ﺍﻛﻮ (...ﻭ ﻓﺎﻳﻞﻫﺎﻱ ﺻﻮﺗﻲ ،ﺻﺪﺍﻱ ECG,M.Sﻭ ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ ﺁﻥ ﺑﻪ ﺻﻮﺭﺕ ﻭﻳﺪﺋﻮﻛﻠﻴﭗ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻣﺒﺎﺣﺚ ﻛﺘﺎﺏ ﺷﺎﻣﻞ : -١ﺗﺎﺭﻳﺨﭽﻪ ﻋﻠﻢ ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ -٢ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ ﭘﻴﺸﮕﻴﺮﻱ )ﺷﺎﻣﻞ :ﺑﻴﻮﻟﻮﮊﻱ ﺍﺗﺮﻭﺳﻜﻠﺮﻭﺯ ،ﺭﮊﻳﻢ ﻏﺬﺍﻳﻲ ﻭ ﭼﺎﻗﻲ ﻭ ﺍﺧﺘﻼﻻﺕ ﭼﺮﺑﻲ ،ﻭﺭﺯﺵ ،ﻓﺸﺎﺭ ﺧﻮﻥ ﻭ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺁﻥ ،ﺳﻴﮕﺎﺭ ﻛﺸﻴﺪﻥ ،ﺩﻳﺎﺑﺖ ،ﺍﺳﺘﺮﻭﮊﻥ ،ﺟﻨﺲ ﺯﻥ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺒﻲ ،ﺍﺗﺎﻧﻮﻝ ﻭ ﻗﻠﺐ ،ﺭﻓﺘﺎﺭ ﻭ ﺷﺨﺼﻴﺖ ﺑﻴﻤﺎﺭﺍﻥ ﻗﻠﺒﻲ ،ﻧﻮﺗﻮﺍﻧﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺒﻲ( -٣ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ ﺑﺎﻟﻴﻨﻲ) :ﺷﺎﻣﻞ ﺗﺎﺭﻳﺨﭽﻪ ،ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ ،ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻳﺴﻜﻤﻲ ،ﺩﺭﻳﭽﻪﺍﻱ ،ﻋﻔﻮﻧﻲ ،ﻣﺎﺩﺭﺯﺍﺩﻱ ،ﺗﻮﻣﻮﺭﺍﻝ ﻗﻠﺐ ﻭ ﭘﺮﺩﻩﻫﺎﻱ ﺁﻥ ﻣﻲﺑﺎﺷﺪ ﻫﻢ ﭼﻨﻴﻦ ﺷﺎﻣﻞ ﻗﻠﺐ ﻭ ﺣﺎﻣﻠﮕﻲ ،ﭘﻴﺮﻱ ،ﻛﻠﻴﻪ ،ﻭﺭﺯﺵ ﻭ ﺗﺮﻭﻣـﺎ ﻣـﻲﺑﺎﺷـﺪ-(. ﻣﺸﺎﻭﺭﻩ ﻧﻮﻳﺴﻲ -ﺩﺍﺭﻭﻫﺎﻱ ﻗﻠﺒﻲ -ﺍﺷﺘﺒﺎﻫﺎﺕ ﭘﺰﺷﻜﻲ -٤ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻗﻠﺒﻲ :ﺷﺎﻣﻞ ﻋﻜﺲ ﻭ ﻓﺎﻳﻞ ﺻﻮﺗﻲ ﻭ ﻭﻳﺪﺋﻮ ﻛﻠﻴﭗ) :ﺗﻔﺴـﻴﺮ ﻋﻜـﺲ ﺳـﺎﺩﻩ ﺭﻳـﻪ – ECGﺩﺭ ﺣـﻴﻦ ﻭﺭﺯﺵ – ﺍﻛﻮﻛـﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ – transthoracicﺍﺳـﺘﺮﺱ ﺍﻛﻮﻛـﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ – ﺍﺭﺯﻳـﺎﺑﻲ ﺑـﺎ ﺩﺍﭘﻠـﺮ - ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ -transesophagealﺗﻜﻨﻴﻚﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻫﺴﺘﻪﺍﻱ – CT, PET , MRIﻗﻠﺐ – ﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ -٥ .( intraoperativeﺍﻟﻜﺘﺮﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ Pacingﺷﺎﻣﻞ ) :ﻣﻜﺎﻧﻴﺴﻢ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺁﺭﻳﺘﻤـﻲﻫـﺎ ،ﺗﺴـﺖﻫـﺎﻱ ﺍﻟﻜﺘﺮﻭﻓﻴﺰﻭﻟـﻮﮊﻱECG
ﺿﺎﻳﻌﺎﺕ ﻗﻠﺒﻲ ﺍﻳﺴﻜﻤﻴﻚ ﻭ ﻏﻴﺮﺍﻳﺴﻜﻤﻴﻚ ،ﻃﺮﺯ ﮔﺬﺍﺷﺘﻦ Pacemakerﻭ ﻓﻴﺒﺮﻳﻠﻴﺘﻮﺭﻫﺎ( -٦ﻛﺎﺭﺩﻳﻮﻟﻮﮊﻱ invasiveﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ :ﺷﺎﻣﻞ ﻋﻜـﺲ ﻭ ﻓـﻴﻠﻢ )ﺁﻧﮋﻳـﻮﮔﺮﺍﻓﻲ ﻛﺮﻭﻧـﺮﻱ -ﻛﺎﺗﺘﺮﻳﺰﺍﺳـﻴﻮﻥ ﻗﻠﺒـﻲ Procedures ،Percutaneos ،ﺑـﺎﻱﭘـﺲ ﻗﻠـﺐ– -٨ﻛـﺎﺭﺩﻳﻮﻟﻮﮊﻱ ﻣﻠﻜـﻮﻟﻲ ﻼ ﺑﺎﻱﭘﺲ ﺷﺪﻩﺍﻧﺪ – ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ ﻭ ﺁﻧﮋﻳﻮﺳﻜﻮﭘﻲ ﻭ ﺍﻟﻮﻟﻮﭘﻼﺳﺘﻲ ،ﻃﺮﺯ ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ ﺩﺭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ﻗﻠﺒﻲ( -٧ﻧﺎﺭﺳﺎﻳﻲ ﻗﻠﺐ ﻭ ﭘﻴﻮﻧﺪ ﻗﻠﺐ Restenosisﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ﻭ ﺩﺭﻣﺎﻥ– approachﺑﻪ ﺑﻴﻤﺎﺭﺍﻥ ﻛﻪ ﻗﺒ ﹰ -٩ﻭﺍﺳﻜﻮﻟﺮ ﺑﻴﻮﻟﻮﮊﻱ :Multimedia -١٠ﺷﺎﻣﻞ ﻋﻜﺲ ﻭ ﺻﺪﺍﻫﺎﻱ ﻗﻠﺒﻲ )ﻧﺮﻣﺎﻝ ﻭ ﺍﺑﻨﺮﻣﺎﻝ( ﻭ ﻛﻠﻴﭗﻫﺎﻱ ﻭﻳﺪﻳﻮﺋﻲ. ﻋﻜﺲ :ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ – - CT/MRIﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ – - ECGﺍﻭﻟﺘﺮﺍﺳﻮﻧﻮﮔﺮﺍﻓﻲ – intravascularﻧﻮﻛﻠﺌﺎﺭ – ﭘﺎﺗﻮﻟﻮﮊﻱ – ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ – ﺟﺮﺍﺣﻲ -ﭼﺸﻢ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺒﻲ ﻋﺮﻭﻗﻲ. ﻭﻳﺪﺋﻮﻛﻠﻴﭗ :ﻛﺎﺗﺘﺮﻳﺰﺍﺳﻴﻮﻥ – – CT/MRIﺍﻛﻮﻛﺎﺭﺩﻳﻮﮔﺮﺍﻓﻲ – ﺍﻟﻜﺘﺮﻭﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ Pacingﻭ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ – ﺗﺼﺎﻭﻳﺮ ﻫﺴﺘﻪﺍﻱ – ﺟﺮﺍﺣﻲ. •
،Endof-Life Careﻗﻠﺐ ﻭﺭﺯﺷﻜﺎﺭﺍﻥ ،ﺍﺭﺯﻳﺎﺑﻲ ﺑﺎﻟﻴﻨﻲ ،ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﺍﺗﻮﻧﻮﻡ،
.
ﺻﺪﺍﻫﺎﻱ ﻗﻠﺒﻲ :ﻧﺮﻣﺎﻝ ﻭ ﺍﺑﻨﺮﻣﺎﻝ
ﻓﺼﻞﻫﺎﻱ ﺟﺪﻳﺪ ﻛﺘﺎﺏ ﻧﺴﺒﺖ ﺑﻪ ﻭﻳﺮﺍﻳﺶ ﻗﺒﻠﻲ ﻛﺘﺎﺏ ﻭ CD
ﺷﺎﻣﻞ:
، Percutaneous Coronaryintervantionﻣﻼﺣﻈﺎﺕ ﺟﺮﺍﺣﻲ ﺩﺭ ﺩﺭﻣﺎﻥ ﻧﺎﺭﺳﺎﺋﻲ ﻗﻠﺐ ،ﮊﻥﺗﺮﺍﭘﻲ ﻭ ﭘﻴﺸﺮﻓﺖﻫﺎﻱ ﻣﻠﻜﻮﻟﻲ ﺩﺭ ﻣﻮﺭﺩ ﻗﻠﺐ
( ﻃﺮﻳﻘﻪ ﻧﺼﺐ : TEXTBOOK OF CARDIOVASCULAR MEDICINEﺑﺮﺍﻱ ﻧﺼﺐ ﺑﺮﻧﺎﻣﺔ Cardiovascular Medicineﺍﺑﺘﺪﺍ CDﺭﺍ ﺩﺭﻭﻥ ﺩﺭﺍﻳﻮ ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﻭ ﺩﺭ ﭘﻨﺠﺮﻩ ﺍﻱ ﻛﻪ ﺑﺎ ﻋﻨﻮﺍﻥ Flashﺑﺎﺯ ﺷﺪﻩ ﺑﺮ ﺭﻭﻱ ﻛـﺎﺩﺭ ﺳـﻤﺖ ﭼـﭗ ﺗﺼـﻮﻳﺮ، ﮔﺰﻳﻨﺔ Install TOPOLﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﺮﺩﻩ ﺳﭙﺲ ﭘﻨﺠﺮﺓ ﻣﺤﺎﻭﺭﻩﺍﻱ ﺩﻳﮕﺮﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ )ﺣﺪﻭﺩﹰﺍ ٣٠-٤٠ﺛﺎﻧﻴﻪ ﺑﻌﺪ( ﻭ ﻣﺴﻴﺮ ﻧﺼﺐ ﺑﺮﻧﺎﻣﻪ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﻛﻨﺪ .ﺍﻳﻦ ﻣﺴﻴﺮ ﺑﺼﻮﺭﺕ ﭘﻴﺶ ﻓﺮﺽ C:\Program files\CardioVascularMedicineﺍﺳﺖ ﺩﺭ ﻗﺴـﻤﺖ ﭘـﺎﻳﻴﻦ ﺑﺮﺭﻭﻱ ﺩﻛﻤﺔ Installﻛﻠﻴﻚ ﻛﻨﻴﺪ )ﺍﮔﺮ ﺧﻮﺍﺳﺘﻴﺪ ﻣﺴﻴﺮ ﻓﻮﻕ ﺭﺍ ﺑﻪ ﺩﻟﺨﻮﺍﻩ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺗﻐﻴﻴﺮ ﺩﻫﻴﺪ( ﭘﺲ ﺍﺯ ﻛﻠﻴﻚ ﺑﺮﺭﻭﻱ Installﭘﻨﺠﺮﺓ ﺩﻳﮕﺮﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ ﻭ ﺑﺮﻧﺎﻣﻪ ﺧﻮﺩﺑﺨﻮﺩ ﻧﺼﺐ ﻣﻲ ﺷﻮﺩ ﭘﺲ ﺍﺯ ﺣﺪﻭﺩ ٢٠ﺛﺎﻧﻴﻪ ﭘﻨﺠﺮﺓ ﺁﺧﺮ ﺑﻨـﺎﻡ Install completeﻣـﻲ ﺁﻳـﺪ ﺑـﺮﺭﻭﻱ ﺩﻛﻤﺔ Doneﺩﺭ ﺍﻧﺘﻬﺎ ﻛﻠﻴﻚ ﻛﻨﻴﺪ .ﭘﺲ ﺍﺯ ﺁﻧﻜﻪ ﻣﺮﺍﺣﻞ ﻓﻮﻕ ﺍﻧﺠﺎﻡ ﭘﺬﻳﺮﻓﺖ ﺑﺮﻧﺎﻣﻪ ﻧﺼﺐ ﺷﺪﻩ ﺍﺳﺖ ﻭﻟﻲ ﺑﺮﺍﻱ ﺍﺟﺮﺍﻱ ﺁﻥ ﻧﻴﺎﺯ ﺍﺳﺖ ﺩﻭ ﺑﺮﻧﺎﻣﺔ ﻛﻤﻜﻲ ﺩﻳﮕﺮ ﻧﻴﺰ ﺑﺮ ﺭﻭﻱ ﺳﻴﺴﺘﻢ ﻋﺎﻣﻞ ﻧﺼﺐ ﺷﻮﺩ ﻛﻪ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ .Quick Time, Internet Explorer :ﺑﺮﺍﻱ ﻧﺼـﺐ ﺍﻳـﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺯ ﺍﻳﻨﺘﺮﻧﺖ ﺍﻛﺴﭙﻠﻮﺭﺭ ﺑﺎﻭﺭﮊﻥ 5.5ﺑﻪ ﺑﺎﻻ ﻣﻲﺗﻮﺍﻥ ﺍﺳﺘﻔﺎﺩﻩ ﻛﺮﺩ .ﺿﻤﻨﹰﺎ ﺳﻴﺴﺘﻢ ﻋﺎﻣﻠﻬﺎﻱ ﭘﻴﺸﻨﻬﺎﺩﻱ ﺑﺮﺍﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻭﻳﻨﺪﻭﺯﻫﺎﻱ 2000, NT, ME, 98, 95ﺍﺳﺖ ﻳﺎ 200 MHZﭘﺮﺩﺍﺯﺷﮕﺮ ﻭ ﺣﺪﺍﻗﻞ 32ﻣﮕﺎﺑﺎﻳﺖ ﺣﺎﻓﻈﻪ. ﺩﺭ ﭘﻨﺠﺮﻩ ﺍﻱ ﻛﻪ ﭘﻴﺶ ﺭﻭﺩﺍﺭﻳﺪ )ﺍﻭﻟﻴﻦ ﭘﻨﺠﺮﻩ ﻫﻨﮕﺎﻡ ﻗﺮﺍﺭﺩﺍﺩﻥ (CDﮔﺰﻳﻨﺔ Internet Explore 5.5ﺭﺍ ﻛﻠﻴﻚ ﻛﻨﻴﺪ .ﺩﺭ ﭘﻨﺠﺮﻩ ﺍﻱ ﻛﻪ ﭘﻴﺶ ﺭﻭﻱ ﺷﻤﺎ ﺑﺎﺯ ﻣﻲ ﺷﻮﺩ ﺩﺭ ﻗﺴﻤﺖ I accept the agreementﻛﻠﻴﻚ ﻛﻨﻴﺪ ﻭ ﺩﻛﻤﺔ Nextﺍﺯ ﭘﺎﺋﻴﻦ ﺭﺍ ﻓﺸﺎﺭ ﺩﻫﻴﺪ. ﺑﺮﻧﺎﻣﻪ ﻣﺸﻐﻮﻝ ﭼﻚ ﻛﺮﺩﻥ ﺳﻴﺴﺘﻢ ﻭ ﻣﺤﺘﻮﺍﻱ ﻓﺎﻳﻞﻫﺎ ﻣﻲﺷﻮﺩ .ﺳﭙﺲ ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ ﻛﻪ ﺑﺼﻮﺭﺕ ﭘﻴﺶ ﻓﺮﺽ ﺩﻛﻤﺔ ﺑﺎﻻﻳﻲ ﻓﻌﺎﻝ ﺍﺳﺖ ﻭ ﺷﻤﺎ ﺑﺎﻳﺪ ﺩﻛﻤﺔ Nextﺭﺍ ﻓﺸﺎﺭ ﺩﻫﻴﺪ .ﺣﺎﻝ ﺑﺎﻳﺪ ﻣﻨﺘﻈﺮ ﺑﻤﺎﻧﻴﺪ ﺗﺎ ﺑﺮﻧﺎﻣﻪ ﺑﺼـﻮﺭﺕ ﻛﺎﻣـﻞ ﻧﺼـﺐ ﮔـﺮﺩﺩ ﺳـﭙﺲ ﭘﻨﺠـﺮﺓ ﺩﻳﮕﺮﻱ ﺑﺎﺯ ﺷﺪﻩ ﺩﻭﺑﺎﺭﻩ Nextﺭﺍ ﻓﺸﺎﺭ ﺩﺍﺩﻩ ﻭ ﺩﻛﻤﺔ finishﺩﺭ ﺍﻧﺘﻬﺎ ﺯﺩﻩ ﺷﻮﺩ .ﺩﺭ ﺍﻳﻦ ﻣﻮﻗﻊ ﻭﻳﻨﺪﻭﺯ ﺧﻮﺩﺑﺨﻮﺩ restartﻣﻲﺷﻮﺩ .ﺩﻭﺑﺎﺭﻩ CDﺭﺍ ﺍﺟﺮﺍ ﻛﻨﻴﺪ )ﺍﻳﻦ ﻛﺎﺭ ﺭﺍ ﻣﻲ ﺗﻮﺍﻧﻴﺪ ﺑﺎ ﺯﺩﻥ ﺩﻛﻤﺔ Ejectﺩﺭﺍﻳﻮ CDﻭ ﻓﺸﺮﺩﻥ ﻣﺠﺪﺩ CDﺑﻪ ﺩﺭﻭﻥ ﺩﺭﺍﻳﻮ ﻭ ﻳﺎ ﺑـﺎﺯ ﻛـﺮﺩﻥ CDﻭ ﺍﺟﺮﺍﻱ ﺁﻥ ﺍﻧﺠﺎﻡ ﺩﻫﻴﺪ( ﺣﺎﻝ ﺑﻪ ﻗﺴﻤﺖ ﺳﻮﻡ ﻧﺼﺐ ﻣﻲﺭﺳﻴﻢ .ﺑﺎﻳﺪ ﺍﺯ ﭘﻨﺠﺮﺓ ﺑﺎﺯﺷﺪﻩ )ﭘﻨﺠﺮﺓ ﺍﻭﻝ ﻫﻨﮕﺎﻡ ﻗﺮﺍﺭﺩﺍﺩﻥ ( CDﺑﺮ ﺭﻭﻱ ﮔﺰﻳﻨﺔ Quick time 5ﻛﻠﻴﻚ ﻛﻨﻴﻢ .ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪﻱ ﻣﻲﺁﻳﺪ ﺩﻛﻤﺔ Nextﺭﺍ ﻓﺸﺎﺭ ﻣﻲ ﺩﻫﻴﻢ .ﭘﻨﺠﺮﺓ ﺑﻌﺪﻱ ﻫﻢ ﺑﺎﻳﺪ Nextﺭﺍ ﺑﺰﻧﻴﺪ ﺗﺎ ﭘﻨﺠﺮﺓ ﺩﻳﮕﺮﻱ ﺑﺎﺯ ﺷﻮﺩ ﺣﺎﻝ ﺩﻛﻤﺔ Agreeﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ ﻣﺴﻴﺮﻱ ﺭﺍ ﻣﻲ ﺑﻴﻨﻴﻢ ﺍﮔﺮ ﻣﻮﺍﻓﻖ ﺑﻮﺩﻳﺪ Nextﺭﺍ ﺑﺰﻧﻴﺪ ﻭ ﺩﺭ ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪ ﺑﺼﻮﺭﺕ ﭘﻴﺶ ﻓﺮﺽ ﺩﻛﻤﺔ ﺩﻭﻡ ﺍﺯ ﺑﻴﻦ ﺳﻪ ﺩﻛﻤﻪ ﺩﺭ ﺑﺎﻻﻱ ﻛﺎﺩﺭ ﻓﻌﺎﻝ ﺍﺳﺖ ﻣﺠﺪﺩﹰﺍ Nextﺭﺍ ﺑﺰﻧﻴﺪ ﻭ ﺑﺎﺯ ﻧﻴﺰ Nextﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ ﺩﺭ ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪ ﻧﻴﺰ Nextﺭﺍ ﻓﺸﺎﺭ ﺩﻫﻴﺪ ﭘﻨﺠﺮﺓ ﺑﻌﺪﻱ ﺳﺮﻳﺎﻝ ﻭ ﻧﺎﻡ ﺷﺮﻛﺖ ﺭﺍ ﻣﻲﭘﺮﺳﺪ ﻧﻴﺎﺯﻱ ﺑﻪ ﭘﺮﻛﺮﺩﻥ ﺁﻥ ﻧﻴﺴﺖ Nextﺭﺍ ﺯﺩﻩ ﺗﺎ ﺑﺮﻧﺎﻣﻪ ﻧﺼﺐ ﺷﻮﺩ ﺑﺮ ﺭﻭﻱ ﭘﻨﺠﺮﺓ ﻓﻌﺎﻝ ﻣﺎ ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ ﺁﻥ ﺭﺍ ﻧﻴﺰ Nextﺑﺰﻧﻴﺪ ﺩﻭ ﺑﺎﺭﻛﻪ Nextﻛﺮﺩﻳﺪ ﺍﻳﻦ ﭘﻨﺠﺮﻩ ﺭﺍ finishﻛﻨﻴﺪ ﺗﺎ ﺑﻪ ﭘﺎﻳﺎﻥ ﻛﺎﺭ ﺑﺮﺳﻴﻢ ﺁﺧﺮﻳﻦ ﭘﻨﺠﺮﻩ ﺭﺍ ﺑﺎ ﺑﺮﺩﺍﺷﺘﻦ ﺗﻴﻚﻫﺎﻱ ﺩﻭ ﻛﺎﺩﺭ ﺑﺎﻻ Closeﻛﻨﻴﺪ .ﺗﻤﺎﻡ ﭘﻨﺠﺮﻩ ﻫﺎ ﺭﺍ ﺑﺮﺭﻭﻱ ﺻـﻔﺤﺔ Desktopﺑﺒﻨﺪﻳـﺪ ﺑـﺮﺭﻭﻱ ﺩﻛﻤـﺔ Startﻛﻠﻴـﻚ ﻛـﺮﺩﻩ ﻭﺍﺭﺩ Programsﺷـﻮﻳﺪ ﻭ ﺍﺯ ﻣﻨـﻮﻱ Cardio Vascular Medicineﺑﺮﻧﺎﻣـﺔ Cardio Vascular CDﺭﺍ ﺍﺟﺮﺍ ﻛﻨﻴﺪ ﻭ ﺳﭙﺲ ﺑﺮﻧﺎﻣﺔ internet explorerﺭﺍ ﺑﺎﺯ ﻛﺮﺩﻩ ﻭ ﺩﺭ ﻗﺴﻤﺖ Addressﺧﻂ ﺯﻳﺮ ﺭﺍ ﺗﺎﻳﭗ ﻛﻨﻴﺪ .ﺑﺮﻧﺎﻣﻪ ﺩﺭ ﻣﺤﻴﻂ internet explorerﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ. http://127.0.0.1:83/PCIndex.htm.
2003 ــــــ
)Images from the Netter Collection (NOVARTIS )(John Michael Criley, M.D., Conrad Zalace, David Creley Catalog of Lesions yNormal yValvar Lesions yPericardial Disease
Timing of Murmurs ySystolic Murmurs yDiastolic Murmurs yContinuous Murmurs vs. “To and Fro” Murmurs
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
The Netter Presenter Cardiovascular and Renal Edition
55.5
56.5 The Physiological Orgins of HEART SOUNDS and MURMUS
Timing of Heart Sounds yValve Closure Sounds and Splitting of Sounds yOpening Sounds yThird Sounds
General Tutorials: yInspection and Palpation yIntriduction to Auscultation yEffect of Maneuvers and Perturbations
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
29 yCongenital Heart Disease yCardiomyopathies yMyxoma
ــــــ
ــــــ
yFriction Rubs
yFourth sounds yEjection Sounds yMid-Systolic Clicks
)(LAWRENCE S. COHEN, M.D, JOHN ELEFTERIADES, M.D.) (VCD
yHemoduction to Cardiac Imaging Modalities
57.5 VJC Video Journal of Cardiology
1. From a new perspective: mitral valve prolapse aortic dissections and aneurysms 2. Surgical and medical management of ascending and descending aortic dissections liporoten (A): a cardiovascular risk factor )58.5 VJC Video Journal of Cardiology (Christopher White, M.D, Michael E. Cain, M.D., Bruce D. Lindsay, M.D., Herbert Geschwind, M.D.) (VCD ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺯ ﺳﺮﻱ CDﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ VJCﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺩﺭ ﻗﺎﻟﺐ VCDﺑﻪ ﻣﺪﺕ 50ﺩﻗﻴﻘﻪ ﺩﺭ ﺳﻪ ﺑﺨﺶ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻳﻚ ﻣﻮﺿﻮﻉ ﺑﻪ ﺷﻜﻞ ﻣﺼﺎﺣﺒﺔ ﻋﻠﻤﻲ ﺑﺎ ﻳﻚ ﻣﺘﺨﺼﺺ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪ ﻭ ﻓـﻴﻠﻢ ﻭ ﻧﻤﻮﺩﺍﺭﻫـﺎﻱ ﻣﺘﻌﺪﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺷﺪﻩ ﺍﺳﺖ .ﻣﻮﺿﻮﻋﺎﺕ ﻫﺮ ﺑﺨﺶ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ: ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ :ﺩﻛﺘﺮchristoher white : 1-Cold lege : The Approach to Acvte and progressive Peripheral Vascular Disease ﻋﻮﺍﺭﺽ ﻣﺮﺑﻮﻁ ﺑﻪ ﻋﺮﻭﻕ ﻣﺤﻴﻄﻲ ﻭ ﺭﻭﺷﻬﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺁﻧﻬﺎ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ .ﻣﺮﺍﺣﻞ ﺍﻧﺠﺎﻡ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺑﻪ ﻫﻤﺮﺍﻩ ﻧﻤﺎﻳﺶ ﺗﺼﺎﻭﻳﺮ ﺁﻧﮋﻳﻮﺳﻜﻮﭘﻴﻚ ﻭ ﺁﻧﮋﻳﻮﮔﺮﺍﻡ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﻣﺼﺎﺣﻴﻪ ﺷﻮﻧﺪﻩ :ﺩﻛﺘﺮ Michael E. Cain :
Urokinase
،ﺍﺳﺘﺮﭘﺘﻮﻛﻴﻨﺎﺯ ،ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ﻟﻴﺰﺭﻱ ﻭ ....ﻧﻴﺰ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ.
2- RADiofrgvency ablation : Ablation of AVNode reentry tachycardias
ﺍﻟﻜﺘﺮﻭﻛﺎﺭﺩﻭﻳﻮﮔﺮﺍﻡ ﺑﺎﻟﻴﺪﮔﺬﺍﺭﻱﻫﺎﻱ ﻣﺨﺘﻠﻒECG ،ﻫﺎﻱ ﺩﺭ ﻓﻴﺒﺮﻳﻼﺳﻴﻮﻥ ﻭ ﺑﻠﻮﻙ AVﻭ ...ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﺍﺳﻼﻳﺪﻫﺎ ﻭ ﺭﺍﺩﻳﻮﮔﺮﺍﻡﻫﺎﻱ ﻣﺘﻌﺪﺩ ﺑﺮﺭﺳﻲ ﻭ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﺼﺎﺣﺒﻪ ﺷﻮﻧﺪﻩ :ﺩﻛﺘﺮHerbert Geschwind :
3- Laser Angioplasty for coronary Atherosclerotic Disease
ﻣﻜﺎﻧﻴﺰﻡ ﻋﻤﻞ ﺳﻴﺴﺘﻢ ﻟﻴﺰﺭ ﺩﺭ ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ،ﻛﺎﺭﺑﺮﺩ Pulserﻃﻮﻝ ﺑﺮﺝ ﺑﻬﻤﻴﻨﻪ ) ﻣﺎﻭﺭﺍﺀ ﻣﺎﺩﻭﻥ ﻗﺮﻣﺰ( ﺍﻫﺪﺍﻑ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﻧﮋﻳﻮﭘﻼﺳﺘﻲ ﻟﻴﺰﺭﻱ ﻭ ﻋﻮﺍﺭﺽ ﺁﻥ ﻣﺰﻳﺖ ﻫﺎ ﻭ ﻣﺤﺪﻭﺩﻳﺖﻫﺎ ﺍﻳﻦ ﺭﻭﺵ ﻭ ﻣﻘﺎﻳﺴﻪ ﺁﻥ ﺑﺎ PTCAﻭ ....ﻣﻮﺭﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. -٦ﭘﻮﺳﺖ ﻭ ﻣﻮ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ 2001
ﻋﻨﻮﺍﻥ CD )American Cancer Society Atlas of Clinical Oncology Skin Cancer (Arthur J. Sober, MD, Frank G. Haluka, MD, phD) (Bc Decker Inc
1.6
ﻫﻤﭽﻨﺎﻧﻜﻪ ﻭﺍﺭﺩ ﻗﺮﻥ ٢١ﻣﻲﺷﻮﻳﻢ ﺷﺎﻳﻊﺗﺮﻳﻦ ﺷﻜﻞ ﺳﺮﻃﺎﻥﻫﺎ ،ﻛﺎﻧﺴﺮﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻣﻲﺑﺎﺷﺪ ﻭ ﺑﻪ ﻋﻠﺖ ﺍﻳﻨﻜﻪ ﺑﺮ ﺧﻼﻑ ﻛﺎﻧﺴﺮﻫﺎﻱ ﺩﻳﮕﺮ ،ﻛﺎﻧﺴﺮﻫﺎﻱ ﭘﻮﺳﺖ ﺩﺭ ﻣﻌﺮﺽ ﺩﻳﺪ ﻣﻲﺑﺎﺷﺪ ﺳﺮﻳﻌﺘﺮ ﻭ ﺭﺍﺣﺖﺗﺮ ﻗﺎﺑـﻞ ﺗﺸـﺨﻴﺺ ﺍﺳـﺖ .ﺩﺭ ﻧﺘﻴﺠـﻪ ﺩﺍﻧـﺶ ﺗﺸـﺨﻴﺺ ﻭ ﺩﺭﻣـﺎﻥ ﻭ ﺟﻠﻮﮔﻴﺮﻱ ﺍﺯ ﺳﺮﻃﺎﻥﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻣﻮﺟﺐ ﻧﮕﺎﺭﺵ ﺍﻳﻦ ﻛﺘﺎﺏ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﻣﺸﺨﺼﺔ ﺍﻳﻦ ﻛﺘﺎﺏ ﺗﺄﻛﻴﺪ ﺑﺮ ﻧﻤﺎﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ Skin cancerﻣﻲﺑﺎﺷﺪ ﭼﻮﻥ ﻋﻠﻢ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﺮ ﭘﺎﻳﺔ ﻣﺸﺎﻫﺪﻩ ﺑﻨﺎ ﺷﺪﻩ ﺍﺳﺖ ،ﺑﻨﺎﺑﺮﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺍﺭﺍﻱ ﺗﺼﺎﻭﻳﺮ ﺯﻳﺎﺩ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺴﻴﺎﺭ ﺑﺎﻻﺳﺖ ﻭ ﻫﺮ ﺟﺎ ﻛﻪ ﻋﻜﺲﻫﺎ ﺩﺭ ﺍﺭﺍﺋﻪ ﻣﻄﻠﺐ ﻛﻤﻚﻛﻨﻨﺪﻩ ﻧﺒﻮﺩﻩ textﺍﺿﺎﻓﻪ ﺷﺪﻩ ﺍﺳﺖ .ﻭ ﻋﻼﻭﻩ ﺑﺮ ﺍﻳﻦ ﻧﻜﺎﺕ ﺗﺸﺨﻴﺼﻲ ،ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ،ﺩﺭﻣﺎﻧﻲ ﻭ ﭘﻴﺸﮕﻴﺮﻱ ﺩﺭ ﻛﺘﺎﺏ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ٤ﻗﺴﻤﺖ ﺗﻘﺴﻴﻢ ﺷﺪﻩ ﺍﺳﺖ: ﺑﺨﺶ Basic Concept :١ﺷﺎﻣﻞ ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ،ﮊﻧﺘﻴﻚ ﻛﺎﻧﺴﺮﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻭ ﻋﻮﺍﻣﻞ ﺧﻄﺮﺯﺍ ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ :٢ﺗﻈﺎﻫﺮﺍﺕ ﺑﺎﻟﻴﻨﻲ :ﺩﺭ ﻫﺮ ﻓﺼﻞ ﺟﺪﺍﮔﺎﻧﻪ ﻧﻤﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ (٤ﻭ ) BCEﻓﺼﻞ (٥ﻭ ) Sccﻓﺼﻞ (٦ﻟﻤﻔﻮﻡﻫﺎﻱ ﭘﻮﺳﺘﻲ )ﻓﺼﻞ (٧ﻭ ﻣﺎﻟﻴﻨﮕﻨﺎﻧﺴﻲﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻧﺎﺷﺎﻳﻊ )ﻓﺼﻞ ) Merckle cell Carcinoma (٨:١ﻓﺼﻞ ( ٨:٢ﻭ ﻛﺎﭘﻮﺳﻲ ﺳﺎﺭﻛﻮﻡ )ﻓﺼﻞ (٨:٣ﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺑﺨﺶ Management : ٣ﻛﻪ ﺷﺎﻣﻞ :ﺗﻜﻨﻴﻚ ﺑﻴﻮﭘﺴﻲ ﺍﺯ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ ، (٩ﺗﺪﺍﺑﻴﺮ ﺟﺮﺍﺣﻲ ﻣﻼﻧﻮﻡ ﭘﻮﺳﺘﻲ )ﻓﺼﻞ ،(١١ﺍﺭﺯﻳﺎﺑﻲ ﻟﻤﻒﻧﻮﺩﻫﺎ ﻭ ﺑﻴﻮﭘﺴﻲ ﺍﺯ ﻟﻤﻒﻧﻮﺩ ﺩﺭ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ adjuvant therapy ،(١١ﺩﺭ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ ،(١٢ﺍﻳﻤﻮﻧـﻮﺗﺮﺍﭘﻲ ﺩﺭ ﻣﻼﻧـﻮﻡ )ﻓﺼـﻞ (١٣ﻭ ﻛﻤـﻮﺗﺮﺍﭘﻲ ،ﺳـﻴﺘﻮﻛﻴﻦ ﺗﺮﺍﭘﻲ ﻭ ﺑﻴﻮﻛﻤﻮﺗﺮﺍﭘﻲ ﺩﺭ ﻣﻼﻧﻮﻡ )ﻓﺼﻞ (١٤ﻣﻲﺑﺎﺷﺪ .ﻫﻤﭽﻨﻴﻦ ﺩﺭﻣﺎﻥ ﻟﻤﻔﻮﻡ ﭘﻮﺳﺘﻲ ﺍﻭﻟﻴﻪ ]) [MFﻓﺼﻞ (١٧ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ : ٤ﺩﺭ ﻣﻮﺭﺩ ﭘﻴﺸﮕﻴﺮﻱ ﺍﺯ ﻛﺎﻧﺴﺮﻫﺎﻱ ﭘﻮﺳﺘﻲ ﺑﺤﺚ ﻛﺮﺩﻩ ﺍﺳﺖ. )AQUAMIDE; Poly Acryl Amide Ged (an injectable gel for correction of soft Tissue Deficiencies
ــــــ
2.6
ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ CDﺩﺭ ﻣﻮﺭﺩ ﻳﻜﻲ ﺍﺯ ﻣﻮﺍﺩ fillerﺑﻪ ﻛﺎﺭ ﺭﻓﺘﻪ ﺩﺭ Cosmetic Surgeryﺗﻮﺿﻴﺤﺎﺗﻲ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﺑﺘﺪﺍ ﺧﻮﺍﺹ ﮊﻝ Aquamideﻭ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺁﻥ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﺳﭙﺲ ﻃﺮﻳﻘﻪ ﺗﺰﺭﻳﻖ ﺍﻳﻦ ﮊﻝ ﺩﺭ ﺍﺻﻼﺡ ﭼﻴﻦ ﻧﺎﺯﻭﺑﻴﺎﻝ ،ﺗﻐﻴﻴﺮ ﺷﻜﻞ ﻧﺎﻫﻨﺠﺎﺭﻱﻫﺎﻱ ﺑﻴﻨﻲ ،ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﭼﻴﻦﻫﺎﻱ ﭘﻴﺸﺎﻧﻲ ﻭ ﺍﻃﺮﺍﻑ ﻟﺐ ،ﭘﺮﻛﺮﺩﻥ ﻭ ﺍﺻﻼﺡ ﺿﺎﻳﻌﺎﺕ ﺁﺗﺮﻭﻓﻴﻚ ﻧﺎﺷﻲ ﺍﺯ ﺍﺳﻜﺎﺭ ﺁﺑﻠﻪﻣﺮﻏﺎﻥ ﻳﺎ ﺗﺮﻭﻣﺎﻫﺎ ،ﮔﻮﻧﻪﮔﺬﺍﺭﻱ ﻭ ﺧﻂ ﻟﺐ ﺑﻪ ﺻﻮﺭﺕ ﻧﻮﺍﺭ ﻭﻳﺪﺋﻮﺋﻲ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. 2002
)ATLAS OF COSMETIC SURGERY (MICHAEL S. KAMINER, MD, JEFFREY S. DOVER, MD, FRCPC, KENNETH A. ARNDT, MD) (W.B. SAUNDERS COMPANY) (Salekan E-Book ﺍﻃﻠﺲ ﺣﺎﺿﺮ ﺗﺄﻟﻴﻒ ﺩﻳﮕﺮﻱ ﺍﺯ Dr. Kenneth. Arndtﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻣﻘﺪﻣﻪ ﻛﺘﺎﺏ ) Dr. Leffellﺍﺳﺘﺎﺩ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺩﺍﻧﺸﮕﺎﻩ (Yaleﻣﻲﻧﻮﻳﺴﺪ"' :ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻓﻮﻕﺍﻟﻌﺎﺩﻩ ﺟﻤﻊﺁﻭﺭﻱ ﺗﺠﺎﺭﺏ ﻣﺆﻟﻔﻴﻦ ﺑﻮﺩﻩ ﻭ ﺑﻴﺸﺘﺮ ﺑﻪ ﻣـﻮﺍﺭﺩ ﻛـﺎﺭﺑﺮﺩﻱ ﺍﺷـﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ ﺑﻪ ﻃﻮﺭﻳﻜﻪ ﺑﻪ ﺷﻤﺎ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ﭼﮕﻮﻧﻪ ﺑﺎ ﻣﻮﻓﻘﻴﺖ ﻳﻚ ﻋﻤﻞ Cosmeticﺭﺍ ﺑﺮ ﺭﻭﻱ ﺑﻴﻤﺎﺭ ﺧﻮﺩ ﺍﻧﺠﺎﻡ ﺩﻫﻴﺪ Dr. Arndt .ﺳﺮﺩﺑﻴﺮ ﻣﺠﻠﻪ Archives of Dermatologyﺗﻘﺮﻳﺒﹰﺎ ﺑﻪ ﻣﺪﺕ ٢٠ﺳـﺎﻝ ﺍﺣﺎﻃـﺔ ﻭﺳـﻴﻌﻲ ﺩﺭ ﺟﺮﺍﺣـﻲﻫـﺎﻱ Cosmeticﺩﺍﺷـﺘﻪ ﻭ ﺩﺭ
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
3.6
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
30 ﺷﻜﻴﻞﺑﻮﺩﻥ ﻛﺘﺎﺏ ﺳﻬﻢ ﺑﺴﺰﺍﻳﻲ ﺩﺍﺭﺩ" ﻭﻳﮋﮔﻲ ﺍﻳﻦ ﻛﺘﺎﺏ ﻧﺴﺒﺖ ﺑﻪ ﻣﻮﺍﺭﺩ ﻣﺸﺎﺑﻪ ،ﺗﺠﺮﺑﻴﺎﺕ ﻣﺆﻟﻔﻴﻦ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻫﻤﮕﻲ ﺑﻪ ﻋﻨﻮﺍﻥ ﺭﻓﺮﺍﻧﺲ ﺩﻳﮕﺮ ﻛﺘﺐ ﻭ ﻣﺠﻼﺕ ﭘﺰﺷﻜﻲ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﺩ )ﺑﺮﺍﻱ ﻣﺜﺎﻝ ﭼﮕﻮﻧﮕﻲ ﺗﺰﺭﻳﻖ Botoxﻭ ﺩﺭﻣﺎﻥ ﺍﺳـﻜﺎﺭﻫﺎﻱ ﺁﻛﻨـﻪ ﻛـﻪ ﺩﺭ ﻣﺠـﻼﺕ ﻼ ﻣﺠﻬﺰ( ﺑﻴﺎﻥ ﻧﻤﻮﺩﻩﺍﻧﺪ .ﺑﺮﺍﻱ ﻣﺜﺎﻝ ﻣﺒﺎﺣﺚ ﺗﺰﺭﻳﻖ ، Botoxﻟﻴﺰﺭﺩﺭﻣـﺎﻧﻲ Archiveﻭ 2001 AADﻭ 2002ﭼﺎﭖ ﺷﺪﻩ ﺍﺳﺖ( ﻣﺆﻟﻔﻴﻦ ﻫﺪﻑ ﺍﺯ ﺗﺄﻟﻴﻒ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﺑﻴﺎﻥ ﺗﺠﺮﺑﻴﺎﺕ ﻛﺎﺭﺑﺮﺩﻱ ﺧﻮﺩ ﺩﺭ ﺑﻴﻤﺎﺭﺳﺘﺎﻥ ) Harvardﺑﺎ ١٣ﻟﻴﺰﺭ ﭘﻮﺳﺖ ﻭ ١٢ﺍﻃﺎﻕ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﻛﺎﻣ ﹰ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﻭ Scar managementﻭ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﺍﻳﻦ ﻛﺘﺎﺏ ﻛﺎﺭﺑﺮﺩﻱﺗﺮﻳﻦ ﻭ ﺑﻪ ﺍﺫﻋﺎﻥ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺩﺳﺘﻴﺎﺭﺍﻥ ﭘﻮﺳﺖ ﺑﻬﺘﺮﻳﻦ ﻛﺘﺎﺏ ﭼﺎﭖ ﺷﺪﻩ ﺩﺭ ﺍﻳﻦ ﻣﻮﺭﺩ ﻣﻲﺑﺎﺷﺪ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺷﻜﻞﻫﺎﻱ ﺳﺎﺩﻩ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻭ ﺑﻌﻀﹰﺎ ﺭﻧﮕﻲ ﺑﻪ ﻛﻴﻔﻴﺖ ﻭ ﺭﺍﺣﺘﻲ ﺁﻣﻮﺯﺵ ﺗﻜﻨﻴﻚﻫﺎ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ﻛﺮﺩﻩ ﺍﺳﺖ .ﻛﺘﺎﺏ Laser in Dermatologyﻣﺆﻟﻒ " "Kenneth, Arndtﺑﺰﻭﺩﻱ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ .ﺍﻳﻦ ﻛﺘﺎﺏ ﻣﻨﺤﺼﺮﺑﻪ ﻓﺮﺩ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: PART III COSMETIC SURGERY PROCEDURES AND TECHNIQUES 10 Topical Skin Care 11 Lasers in the Treatment of Vascular Lesions 12 Lasers in the Treatment of Pigmented Lesions 13 Laser Hair Removal 14 Liposuction 15 Hair Transplantation 16 Soft Tissue Augmentation 17 Botulinum A Exotoxin Injections for Photoaging and Hyperhidrosis, 18 Chemical Peels 19 Lasers in Skin Resurfacing 20 Blepharoplasty 21 Surgical Rhytidectomy: Face Lifts and the Endoscopic Forehead Lift 22 Leg Vein Management: Sclerotherapy, Ambulatory Phlebectomy, and Laser Surgery 23 Scar Management: Keloid, Hypertrophic, Atrophic, and Acne Scars
PART I EVALUATION OF THE COSMETIC SURGERY PATIENT 1 The History of Cosmetic Surgery 2 The History of Cosmetic Dermatologic Surgery 3 Evaluation of the Aging Face, 4 Photoaging: Mechanisms, Consequences, and Prevention 5 Beauty and Society 6 Psychosocial Issues and Their Relevance to the Cosmetic Surgery Patient PART II ANESTHESIA 7 Regional Anesthesia for Aesthetic Surgery 8 Office-Based Sedation and Monitoring 9 Postoperative Pain and Nausea Management
)(CD I , II
ــــــ
)(SALEKAN E-BOOK
)Atlas of Dermatology (Jhon's Hopkins
4.6
ﻼ ﺟﺎﻟﺐ ﺑﺎ ﺭﺯﻭﻟﻮﺷﻦ ﺑﺎﻻ ﺩﺭ ﺧﺼﻮﺹ ﺍﻧﻮﺍﻉ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮ ﻃﺒﻖ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎ Sortﮔﺮﺩﻳﺪﻩ ﻭ ﻣﺤﺼﻮﻝ ﺳﺎﻝ ٢٠٠٣ﺩﺍﻧﺸﮕﺎﻩ Jhon's Hopkinsﻣﻲﺑﺎﺷﺪ. ﺍﻃﻠﺲ ﻓﻮﻕ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ٢٥٠٠ﺗﺼﻮﻳﺮ ﻛﺎﻣ ﹰ 1999
)Atlas of Dermatology (T.L.Diepgen, M. Simon, A. Bittorf, M. Fartasch, G. Schuler) (with the DOIA team G. Eysenbach, J. Bauer, A. Sager) (springer
5.6
ــــــ
ﺗﺎﺭﻳﺨﭽﺔ ﺍﻃﻠﺲ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﺮﻣﻲﮔﺮﺩﺩ ﺑﻪ ﺳﺎﻝ ، ١٩٩٤ﻛﻪ ﺷﺒﻜﺔ ﺳﺮﺍﺳﺮﻱ ﺟﻬﺎﻧﻲ ﺍﻧﻴﺘﺮﻧﺖ ) (wwwﺍﻳﺠﺎﺩ ﺷﺪ .ﺍﺯ ﺁﻥ ﺳﺎﻝ ﺑﻪ ﺑﻌﺪ ﺍﺯ ﺳﺮﺍﺳﺮ ﺟﻬﺎﻥ ﺗﺼﺎﻭﻳﺮ ﺿﺎﻳﻌﺎﺕ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺩﺭ ﺍﻳﻦ ﺷﺒﻜﻪ ﺩﺭ ﻣﺤﻞ (DOIA) Dermatology online Atlasﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ﺳﺎﻳﺖ ﺍﻳﻨﺘﺮﻧﺘﻲ ﻋﻼﻭﻩ ﺑﺮ ٣٠٠٠ﺗﺼﺮﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺴﻴﺎﺭ ﺑﺎﻻﻱ ﺑﻴﺶ ﺍﺯ 600 DPIﺗﺸﺨﻴﺺ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ،ﺍﺭﺍﺋﻪ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ Case report ،ﺻﻮﺗﻲ ﻭ ...ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻨﺎﺑﺮﺍﻳﻦ ﺍﻃﻠﺲ ﻓﻮﻕ ﺑﻪ ﺻـﻮﺭﺕ Offlineﺍﺯ DOIAﺗﻬﻴـﻪ ﺷـﺪﻩ ﻛـﻪ ﻗﺎﺑﻠﻴـﺖ ﺍﺗﺼﺎﻝ ﺩﺭ ﻫﺮ ﺯﻣﺎﻥ ﺑﻪ ﺻﻮﺭﺕ onlineﺭﺍ ﺩﺍﺭﺩ. )Atlas of Differential Diagnosis in DERMATOLOGY (Klaus F. Helm, M.D., James G. Marks, Jr., M.D.
6.6
2003 ــــــ
ﺍﻳﻦ CDﺑﺮ ﺧﻼﻑ ﺍﻃﻠﺲﻫﺎﻱ ﺩﻳﮕﺮ ﻛﻪ ﺑﻴﻤﺎﺭﻱﻫﺎ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎﻳﻲ ﻳﺎ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﻛﺮﺩﻩ ﺗﺄﻛﻴﺪ ﺑﻴﺸﺘﺮ ﺑﻪ ﺗﺸﺨﻴﺺ ﺑﺎﻟﻴﻨﻲ ﻭ ﺍﻓﺘﺮﺍﻕ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﺯ ﻳﻜﺪﻳﮕﺮ ﺑﻪ ﺻﻮﺭﺕ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﺩﺍﺭﺩ .ﺑﻪ ﻃﺮﻳﻜﻪ ﺩﺭ ﻣﻮﺭﺩ ﺗﺸﺨﻴﺺ ﻳـﻚ ﺑﻴﻤﺎﺭ ﺗﺼﺎﻭﻳﺮ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺩﻳﮕﺮ ﻛﻪ ﺑﺎ ﺁﻥ ﺑﻴﻤﺎﺭﻳﻴﻲ ﺍﺷﺘﺒﺎﻩ ﻣﻲﺷﻮﺩ ﮔﺮﺩﺁﻭﺭﻱ ﺷﺪﻩ ﻭ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﺍﻃﻠﺲ Problem-orientedﺗﻨﻈﻴﻢ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ CDﺭﺍﺵﻫﺎ ﻭ ﻧﺌﻮﭘﻼﺳﻢﻫﺎ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﺷﻜﻞ ﻭ ﻣﺤﻞ ﺑﻪ ١٦ﻓﺼﻞ ﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﺷﺪﻩ ﺩﺭ ﺍﻭﻝ ﻫﺮ ﻓﺼـﻞ ﺍﺑﺘـﺮﺍ ﺍﻟﮕﻮﺭﻳﺘﻢ ﺭﺳﻴﺪﻥ ﺑﻪ ﺗﺸﺨﻴﺺ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪ ﻭ ﺳﭙﺲ ﺩﺭ ﺟﺪﺍﻭﻝ ﻣﻘﺎﻳﺴﻪﺍﺱ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻴﻬﺎﻱ ﺍﻳﻦ ﺿﺎﻳﻌﺎﺕ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺳﭙﺲ ﺗﺼﺎﻭﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺑﻪ ﺻﻮﺭﺕ ﻣﻘﺎﻳﺴﻪﺍﻱ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .ﺩﺭ ﺁﺧﺮ ﻫﺮ ﻓﺼﻞ ﻧﻴﺰ ﺍﺗﻴﻮﻟﻮﮊﻱ ،ﻧﻜﺎﺕ ﻣﻬﻢ ﺑﺎﻟﻴﻨﻲ ﻭ ﺩﺭﻣـﺎﻥ ﺑﺮﺍﻱ ﻫﺮ ﺑﻴﻤﺎﺭﻱ ﺑﻪ ﺻﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ CDﺩﺭ ﺑﺮﻧﺎﻣﻪ Acrobat readerﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﺑﺘﺪﺍ ﻳﻚ ﺑﺮﻧﺎﻣﻪ ﻣﺎﻟﺘﻲ ﻣﺪﻳﺎ ) ﺑﻪ ﺻﻮﺭﺕ (animationﺑﺮﺍﻱ ﺁﺷﻨﺎﻳﻲ ﺑﺎ ﻣﺤﺘﻮﻳﺎﺕ CDﻭ ﭼﮕﻮﻧﮕﻲ ﻛﺎﺭ ﺍﺭﺍﺋﻪ ﺷـﺪﻩ ﺍﺳـﺖ .ﺩﺭ ﺍﻳـﻦ image gallery .CDﻭﺟـﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﺗﺼﺎﻭﻳﺮ ﺑﺪﻭﻥ ﺗﻮﺿﻴﺢ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﻭ ﺍﺯ ﺁﻥ ﺑﻪ ﻋﻨﻮﺍﻥ quizﻭ ﺍﺭﺯﻳﺎﺑﻲ ﺷﺨﺼﻲ ﻣﻲﺗﻮﺍﻥ ﺍﺳﺘﻔﺎﺩﻩ ﻛﺮﺩ .ﺍﺯ index inconﻛﻪ ﺑﺮ ﺍﺳﺎﺱ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎﻱ ﺍﻧﮕﻠﻴﺴﻲ ﺑﻨﺎ ﺷﺪﻩ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺭﺍﺣﺘﻲ ﺑﺮﺍﻱ ﺟﺴﺘﺠﻮﻱ ﻣﻮﺿﻮﻉ ﺑﻴﻤﺎﺭﻱ ﻛﻤﻚ ﮔﺮﻓﺖ. )Botulinum Toxin Aesthetic Indications (Mauricio de Maio, Segio Talarico, Benjamin Ascher, Nam Ho Kim South )Color Atlas and synopsis of Clinical Dermatology Common and Serious Diseases Thomas B. (Fitzpatrick, M.D. Richard Allen Johnson, M.D. Dick Suurmond, M.D
7.6 8.6
ﺍﻳﻦ ﺍﻃﻠﺲ ﺑﺎ ٦٨٠ﺗﺼﻮﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﻣﻮﺟﺐ ﻛﻤﻚ ﺩﺭ ﺗﺸﺨﻴﺺ ﺑﻪ ﻭﺳﻴﻠﺔ ﻓﺮﺍﻫﻢ ﻛﺮﺩﻥ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﺑﺰﺭﮒ ﻭ ﻛﻴﻔﻴﺖ ﻋﺎﻟﻲ ﻣﻲﺑﺎﺷﺪ .ﻫﻤﭽﻨﻴﻦ ﺧﻼﺻﻪﺍﻱ ﺍﺯ ﺗﻈﺎﻫﺮﺍﺕ ﺍﺻﻠﻲ ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ﻭ ﺍﻧﺘﻴﻮﻟﻮﮊﻱ ﻭ ﺑﻴﻤﺎﺭﻱ ﺩﺭ ﻛﻨﺎﺭ ﺗﺼﺎﻭﻳﺮ ﺩﺭﺝ ﺷﺪﻩ ﺍﺳﺖ. ــــــ
)COLOR ATLAS OF CLINICAL DERMATOLOGY COMMON AND SERIOUS DISEASES (Salekan E-Book
9.6
)(Thomas B. Fitzpatrick, MD, Richard Allen Johnson, MD, Klaus Wolff, MD, Dick Suurmond, MD
2001
)10.6 Color Atlas of Dermatoxcopy 2nd, enlarged and completely revised edition (Wilhelm Stolz. Otto Braun-Falco) (Salekan E-Book
ــــــ
11.6 Correction of Wrinkles & Augmentation of lip and cheek with Restylane & Perlane
)(Natural beauty for as long as you like
ﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ Skin fillerﻫﺎ ﺑﺮﺍﻱ ﺭﻓﻊ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎﻱ ﺻﻮﺭﺕ ﻛﻪ ﺳﺎﺯﮔﺎﺭﻱ ﺁﻥ ﺑﺎ ﺑﺎﻓﺖ ﺍﻧﺴﺎﻥ %١٠٠ﺍﺳﺖ .ﻫﻴﺎﻧﻮﺭﻭﺗﻴﻚ ﺍﺳﻴﺪ ﺗﻮﻟﻴﺪ ﺷﺪﻩ ﺗﻮﺳﻂ ﺗﻜﻨﻴﻚ recombinantﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻣﺎﺩﻩ ﺗﻮﺳﻂ ﻛﺸﻮﺭ ﺳﻮﺋﺪ ﺩﺭ ﺳﻪ ﻏﻠﻈﺖ ﺑﻪ ﻧﺎﻡﻫﺎﻱ Restyalne , Restyane fineﻭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
31 ﻼ ﻭﺍﺿﺢ ﻧﺸﺎﻥ perlaneﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮ ﺣﺴﺐ ﻧﻮﻉ ﺧﻄﻮﻁ ﺻﻮﺭﺕ )ﻇﺮﻳﻒ ﻳﺎ ﻋﻤﻴﻖ( ﺩﺭ ﺳﻄﻮﺡ ﻣﺨﺘﻠﻒ ﺩﺭﻡ ﺗﺰﺭﻳﻖ ﻣﻲﺷﻮﺩ .ﺩﺭ ﺍﻳﻦ : VCDﺍﺑﺘﺪﺍ ﻣﺮﻭﺭﻱ ﺑﺮ ﭼﮕﻮﻧﮕﻲ ﺳﺎﺧﺖ ﺍﻳﻦ ﺳﻪ ﻣﺎﺩﻩ ﺩﺍﺭﺩ ﻭ ﺳﭙﺲ ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻭ ﭼﮕﻮﻧﮕﻲ ﺗﺰﺭﻳﻖ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺗﺰﺭﻳﻖ ﺭﺍ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﻛﺎﻣ ﹰ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .٢ .ﺩﺭ ﻗﺴﻤﺖ ﺑﻌﺪﻱ ﺑﻪ ﺻﻮﺭﺕ animationﻋﻤﻖ ﻭ ﻣﺤﻞ ﺗﺰﺭﻳﻖ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﺳﻪ ﻣﺤﺼﻮﻝ ﺭﺍ ﺩﺭ ﺩﺭﻡ ﻧﺸﺎﻥ ﻣﻲﺩﻫﺪ .٣ .ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﻃﺮﻳﻘﺔ ﺑﻲﺣﺴﻲ ﻣﻮﺿﻌﻲ ﺑﻪ ﻧﻤﺎﻳﺶ ﮔﺬﺍﺷﺘﻪ ﻣﻲﺷﻮﺩ .٣ .ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺗﻜﻨﻴﻚ ﺗﺰﺭﻳﻖ Reslane fineﻭ ﻣﺤﻞ ﺗﺰﺭﻳﻖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .٤ .ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺗﻜﻨﻴﻚ ﺗﺰﺭﻳﻖ Restylanaﻭ ﻣﺤﻞ ﺗﺰﺭﻳﻖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .٥ .ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺗﻜﻨﻴﻚ ﺗﺰﺭﻳﻖ Perlaneﺑﺮﺍﻱ ﺭﻓﻊ ﭼﻴﻦﻫـﺎﻱ ﻋﻤﻘـﻲ )ﻣﺎﻧﻨـﺪ ﻧﺎﺯﻭﺷـﻴﺎﻝ( ﻭ fonciel contouringﻣﺎﻧﻨـﺪ ) Lip enhan cemenlﻭ (cheek enhancmeatﻭ ﺩﺭﻣﺎﻥ oral Commisureﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ .٦ .ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺗﺮﻛﻴﺒﻲ ﺍﺯ ﺗﺰﺭﻳﻘﺎﺕ ﺑﺎﻻ ﺭﺍ ﺩﺭ ﻳﻚ ﺑﻴﻤﺎﺭ ﻧﺸﺎﻥ ﻣﻲﺩﻫﺪ .٧ .ﺩﺭ ﺑﺨﺶ ﺍﻧﺘﻬﺎ followupﺑﻴﻤﺎﺭ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .٨ .ﺩﺭ ﺍﻧﺘﻬﺎﻱ ﻫﺮ ﻗﺴﻤﺖ ﺗﺼﺎﻭﻳﺮ ﻗﺒﻞ ﻭ ﺑﻌﺪ ﺍﺯ ﺗﺰﺭﻳﻖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺍﺳﺖ. ــــــ
12.6 Cosmetic Surgery for FACE and BODY
2000
13.6 COSMETIC LASER SURGERY
2001
)PERFECT THE TECHIQUES, REDUCE THE RISKS, AND ENJOY THE RESULTS WHEN PERFORMING COSMETIC LASER SURGERY (Richard E. Fitzpatrick Mitchel P. Goldman
)(ALAN R. SHALITA, M.D., DAVID A. NORRIS, M.D
BASIC AND CLINICAL DERMATOLOGY
An Interdisciplinory Approach
14.6 Cosmetic Surgery
ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻒ ﻛﺘﺎﺏ ﻛﻤﺘﺮ ﻛﺘﺎﺑﻲ ﺍﺳﺖ ﻛﻪ ﺗﻠﻔﻴﻘﻲ ﺍﺯ ﺩﺍﻧﺶ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ،ﻣﺎﮔﺰﻳﻠﻮﻓﺎﺷﻴﺎﻝ ﻭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺭﺍ ﺩﺭ ﺧﻮﺩ ﮔﻨﺠﺎﻧﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺣﺪﻭﺩ ١٠٠٠ﺻﻔﺤﻪﺍﻱ ،ﺁﺧـﺮﻳﻦ ﺗﻜﻨﻴـﻚﻫـﺎﻱ ﺩﺭ ﺩﺳﺘﺮﺱ ﺩﺭ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻧﻤﻮﺩﻩ ﺗﺎ ﺑﺮﺍﻱ ﻫﺮ ﺑﻴﻤﺎﺭ ﺑﻪ ﺻﻮﺭﺕ ﺍﻧﻔﺮﺍﺩﻱ ﺗﻜﻨﻴﻚ ﻣﻨﺎﺳﺐ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﻭ ﺑﻪ ﻛﺎﺭ ﺭﻭﺩ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺍﺭﺍﻱ ﻓﺼﻮﻟﻲ ﺍﺳﺖ ﻛﻪ ﺗﻮﺳﻂ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﺟﺮﺍﺣﺎﻥ ﭘﻼﺳﺘﻴﻚ ﻭ ﺟﺮﺍﺣﺎﻥ ﻓﻚ ﻭ ﺻﻮﺭﺕ ﻧﻮﺷﺘﻪ ﺷﺪﻩ ﺍﺳﺖ. ﺍﻳﻦ ﻛﺘﺎﺏ Procedureﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺭﺍ ﻗﺪﻡ ﺑﻪ ﻗﺪﻡ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﻭ ﺗﻤﺎﻡ ﺟﻨﺒﻪﻫﺎﻱ ﺗﻜﻨﻴﻚﻫـﺎﻱ ﺟﺮﺍﺣـﻲ ﺭﺍ ﺗﻮﺿـﻴﺢ ﺩﺍﺩﻩ ﺍﺳـﺖ .ﺍﻃﻼﻋـﺎﺕ Pre-opﻭ Post-opﻭ ﻓـﺮﻡ ﺭﺿـﺎﻳﺖﻧﺎﻣـﻪ ﺩﺭ ﻫـﺮ ﻓﺼـﻞ ﺁﻭﺭﺩﻩ ﺷـﺪﻩ .ﺩﺭ ﻫـﺮ ﻓﺼـﻞ ﺍﻧﺪﻳﻜﺎﺳـﻴﻮﻥ ﻭ ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎﻱ ﻫﺮ ﺗﻜﻨﻴﻚ ﺟﺮﺍﺣﻲ ﻭ ﻣﺤﺪﻭﺩﻳﺖﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﻭ ﻋﻮﺍﺭﺽ ﻭ ﺩﺭﻣﺎﻥ ﻋﻮﺍﺭﺽ ﻭ ﺩﺭﻣﺎﻥ ﻋﻮﺍﺭﺽ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻒ ﻛﺘﺎﺏ ﭼﻮﻥ ﻫﺮ ﻓﺼﻞ ﻛﺘﺎﺏ ﺗﻮﺳﻂ ﻣﺠﺮﺏﺗﺮﻥ ﺍﻓﺮﺍﺩ ﺩﺭ ﺯﻣﻴﻨﻪ ﻛﺎﺭﻱ ﺧﻮﺩ ﻧﮕﺎﺭﺵ ﻳﺎﻓﺘﻪ ﺍﺳﺖ ﻧﻜﺎﺕ ﻛﻠﻴﺪﻱ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﺧﺘﺼﺎﺻﻲ ﻭ ﺍﻃﻼﻋﺎﺕ ﻛﻮﭼﻚ ﻭﻟﻲ ﺑﺎﺍﺭﺯﺵ ﺩﺭ ﻣﻮﺭﺩ ﺗﻜﻨﻴﻚﻫﺎ ﻭ ﺭﻭﺵ ﻋﻤﻞ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ -١ﻃﺮﺍﺣﻲ ﻣﻨﺎﺳﺐ ﺑﺮﺍﻱ ﻳﻚ ﺟﺮﺍﺣﻲ ﺑﺤﺚ ﺷﺪﻩ .ﻓﺼﻞ -٢ﺁﻧﺎﻟﻴﺰ ﺯﻳﺒﺎﻳﻲ ﺷﻨﺎﺧﺘﻲ ﺩﺭ ﻣﻮﺭﺩ ﺩﺭﻣﺎﻥ ﺻﻮﺭﺕﻫﺎﻱ ﭘﻴﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ .ﻓﺼﻞ ٣ﺗﺎ Peel ٦ﺳﻄﺤﻲ ﻭ ﻋﻤﻘﻲ ﻭ ﺗﺮﻛﻴﺐ Peelﻫﺎ ﻭ ﻋﻼﻭﻩ ﺑﺮ ﺁﻥ ) total body peelﮔﺮﺩﻥ Chest .ﻭ ﺩﺳﺖﻫﺎ ﻭ ﻣﻨﺎﻃﻖ ﺩﻳﮕﺮ( ﻧﻴﺰ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ٦ﻛﻤﭙﻠﻴﻜﺎﺳﻴﻮﻥ ﻭ ﺩﺭﻣﺎﻥ ﺑﻪ ﻃﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳـﺖ .ﺩﺭ ﻓﺼـﻮﻝ ٧ﻭ ٨ﻭ ٩ﻭ ٢٢ﻭ ٢٤ﻭ ٣٧ﺩﺭ ﻣﻮﺭﺩ ﺍﻧﻮﺍﻉ ﺩﺭﻣﺎﻥﻫﺎ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻟﻴﺰﺭ ) Er: YAG, Co2ﺿﺎﻳﻌﺎﺕ ﻋﺮﻭﻗﻲ tattooﻭ ﺿﺎﻳﻌﺎﺕ ﭘﻴﮕﻤﺎﻧﺘﻪ ( hair removalﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ٩ﺩﺭ ﻣﻮﺭﺩ ﻣﺆﺛﺮ ﺑﻮﺩﻥ ﻟﻴﺰﺭﻫﺎﻱ Resurfacingﺻـﺤﺒﺖ ﻧﻤـﻮﺩﻩ ﺍﺳـﺖ. ﻓﺼﻞ ١٠ﺑﻪ Dermabrasionﺍﺧﺘﺼﺎﺹ ﺩﺍﺩﻩ ﺍﺳﺖ .ﻓﺼﻞ ١١ﺍﻟﻲ ١٦ﺩﺭ ﻣﻮﺭﺩ ﺩﻓﻊ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎ ﺗﻮﺳﻂ Skin fillerﻫﺎ ) Restiylansﻭ ، inerrall , Perlaneﻛـﻼﮊﻥ ﻭ (....ﻭ ﺗﺰﺭﻳـﻖ ﭼﺮﺑـﻲ ﻭ ﺩﺭ ﻓﺼـﻞ ١٥ﺍﺧﺘﺼﺎﺻـﹰﺎ ﺑـﻪ ﭼﮕـﻮﻧﮕﻲ ﺍﺳـﺘﻔﺎﺩﻩ ﺍﺯ Gortexﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻞ ١٧ﺑﻪ BotulinumsToxinﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١٨ﭼﮕﻮﻧﮕﻲ ﺟﺮﺍﺣﻲ ﺧﺎﻝﻫﺎ Cyst ،ﺍﺳﻜﺎﺭ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻞ ١٩ﺍﺧﺘﺼﺎﺹ ﺑﻪ ﺍﻧـﻮﺍﻉ flapﻭ Graftﻫـﺎ ﺩﺍﺭﺩ .ﻓﺼـﻮﻝ ١٢ﻭ ١٣ﻭ ٢٥ﺑـﻪ ﻟﻴﭙﻮﺳﺎﻛﺸـﻦ ﻭ ﻟﻴﭙﻮﺍﻧﻔﻮﺯﻳﻮﻥ ﻭ tumescentﺍﺧﺘﺼﺎﺹ ﺩﺍﺭﺩ .ﺩﺭ ﻓﺼﻮﻝ ٣٣ﺗﺮﻛﻴﺐ procedureﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻮﻝ fac, Neck ٢٩-٣٢ﻭ liflingﺑﺤﺚ ﺷﺪﻩ ﻭ ﺭﻭﺵﻫﺎﻱ ﺩﺭ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ Brow Reyirvenationﺁﺭﺭﺩﻩ ﺷﺪﻩ ﺍﺳـﺖ ﻭ ﺩﺭ ﻓﺼﻞ ٣١ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﭘﻠﻚ ﺑﺎﻻ ﻭ ﭘﺎﻳﻴﻦ ﺍﺯ ﺩﻳﺪ ﺍﻓﺘﺎﻟﻤﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ٢٧ﻛﺘﺎﺏ ﺭﻭﺵ ﺍﺧﺘﺼﺎﺻﻲ D. Cookﺑﻪ ﻧﺎﻡ The cook weekend Altrnative to face liftﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻞ ٣٤ﺑﻪ ﻛﺎﺷﺖ ﻣـﻮ ﻭ Alopecia Redechionﺍﺧﺘﺼﺎﺹ ﺩﺍﺭﺩ .ﻓﺼﻞ ٣٨ﻛﺘﺎﺏ ﺑﻪ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻋﻜﺎﺳﻲ ﺩﺭ ﻣﻄﺐ ﺑﺮﺍﻱ ﻛﺎﺭﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﺍﺷﺎﺭﻩ ﺩﺍﺭﺩ .ﻓﺼﻞ ٣٩ﺑﻪ ﭼﮕﻮﻧﮕﻲ ﺑﺮﺧﻮﺭﺩ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺸﻜﻞﺁﻓﺮﻳﻦ ﻭ ﻧﺎﺭﺍﺿـﻲ ﺍﺧﺘﺼـﺎﺹ ﺩﺍﺭﺩ .ﻓﺼـﻞ ٤٠ﻭ ٤١ﺍﺧﺘﺼـﺎﺹ ﺑـﻪ ﺍﻳﻤﭙﻼﻧﺖﻫﺎﻱ ﺻﻮﺭﺕ ﻭ ﻛﺎﺭﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﺟﺮﺍﺣﻲﻫﺎﻱ ﻣﺎﮔﺰﻳﻠﻮﻓﺎﺳﻴﺎﻝ ﻭ ﺩﻫﺎﻥ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. ــــــ
15.6 COSMETIC LASER SURGERY For Face and Body
ــــــ
)16.6 Cutaneous Laser Surgery (Second edition) The Art and Science of Selective Photothermolysis (Goldman, Fitzpartick Cutaneous Laser Surgeryﭼﺎﭖ ﻫﻤﻴﻦ ﻣﺆﻟﻔﻴﻦ ﻣﻲﺑﺎﺷﺪ .ﻛﺘﺎﺏ Cutaneus Laser
ﻳﻚ ﻛﺘﺎﺏ textﺩﺭ ﺯﻣﻴﻨﺔ ﻟﻴﺰﺭ ﻣﻲﺑﺎﺷﺪ ﻭ ﻫﺮ ﻧﻮﻉ ﺍﺯ ﺗﻜﻨﻮﻟﻮﮊﻱ ﻟﻴـﺰﺭ ﺑـﺮﺍﻱ
ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﻣﻜﻤﻞ ﺑﺮ ﻛﺘﺎﺏ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﺭﺍ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺍﺳﺖ ﻭﻟﻲ ﻛﺘﺎﺏ Cosmetic Laser Surgeryﻛﻤﻜﻲ ﺍﺳﺖ ﺑﺮﺍﻱ ﭘﺰﺷﻜﺎﻥ ﺑﺎ ﺗﺄﻛﻴﺪ ﺑﻴﺸﺘﺮ ﺑﺮ ﺑﺮﺧﻮﺭﺩ ﺩﺭﻣﺎﻧﻲ ﺑﺎ ﺑﻴﻤﺎﺭ. ﻓﺼﻞ ﺍﻭﻝ ﻛﺘﺎﺏ ﻣﺮﻭﺭﻱ ﺑﺮ Laser tissue interactionﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻣﻲ ﺗﻮﺍﻥ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ mini text bookﺍﺯ ﺁﻥ ﺍﺳﺘﻔﺎﺩﻩ ﻛﺮﺩ .ﻓﺼﻞ ﺩﺭﺧﺸﺎﻥ ﻛﺘﺎﺏ ﻓﺼﻞ Wuond healingﻣﻲﺑﺎﺷﺪ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﻟﻴﺰﺭﻫﺎ ﻭ ﺑﻬﺘﺮﻳﻦ ﺗﻜﻨﻴﻚ ﻫﺎ ﺑﺪﻭﻥ ﺗﻮﺟﻪ ﺑـﻪ Post procedural wound healingﻣﻨﺠﺮ ﺑﻪ ﻛﻤﺘﺮﻳﻦ ﻧﺘﻴﺠﻪ ﻣﻲﺷﻮﺩ .ﻓﺼﻞ ٣ﻭ ٤ﻭ ٥ﻭ ٦ﻭ ﺩﺭ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻭ ﺗﻮﺿﻴﺢ ﻛﻤﭙﻠﻴﻜﺎﺳﻴﻮﻥ ﺍﺯ ﻟﻴﺰﺭﻫﺎﻱ co2ﻭ Erbium:Yagﺩﺭ resurfacingﻭ Er:yagﺻﻮﺭﺕ ﻭ ﮔﺮﺩﻥ ﻭ chestﻣـﻲﺑﺎﺷـﺪ ﻭ ﻫﻤﭽﻨـﻴﻦ ﺩﺭ ﻣـﻮﺭﺩ ﺍﺳـﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴـﺰﺭ carbon Dioxide ultrapulseﻭ Er:yagﺩﺭ ﺍﻃﺮﺍﻑ ﭼﺸﻢ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻳﻜﻲ ﺍﺯ ﻓﺼﻮﻝ ﺗﺎﺯﻩ ﻛﺘﺎﺏ ﺍﺳﺘﻔﺎﺩﻩ Nonablative Laserﺩﺭ ﻣﻮﺭﺩ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙ ﻫﺎﻱ ﺻﻮﺭﺕ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻣﻘﺒﻮﻟﻴﺖ ﺭﻭﺯﺍﻓﺮﻭﻥ ﭘﻴﺪﺍ ﻛﺮﺩﻩ ﺍﺳﺖ ﻭ ﺩﺭ ﻓﺼﻞ incisional laser Surgery ٩ﺑﺮﺍﻱ ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﻭ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١٠ﻛﺘﺎﺏ Tinas.Alsterﻣﺆﻟﻒ ﻛﺘﺎﺏ manual of cutaneous laser techniquesﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﺩﺭ Scar revisionﺭﺍ ﺷﺮﺡ ﺩﺍﺩﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١١ﺟﺪﻳﺪﺗﺮﻳﻦ ﺗﻜﻨﻴﻜﻬﺎﻱ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺭ hair ] removalﻣﻘﺎﻳﺴﻪ ﺁﻧﻬﺎ ﻭ ﻃﺮﺯ ﻛﺎﺭ ﻭ ﻣﻌﺮﻓﻲ ﻟﻴﺰﺭﻫﺎﻱ ﻣﻌﺘﺒﺮ ﺍﺯ ﻛﺎﺭﺧﺎﻧﻪ ﻫﺎﻱ ﻣﻌﺘﺒﺮ[ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ ﻭﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ mtense light sourceﺩﺭ hair transplantﺻﺤﺒﺖ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١٢ﺍﺳﺘﻔﺎﺩﻩ ﺟﺪﻳﺪ ﺍﺯ ﻟﻴﺰﺭ Co2ﻭ Er:yagﺩﺭ ) hair transplantﻛﺎﺷﺖ ﻣـﻮ( ﺑﺤﺚ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ١٣ﻛﺘﺎﺏ ﺩﺭﻣﺎﻥ Leg veinﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺁﺧﺮ ،ﻣﺆﻟﻔﻴﻦ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﺑﻪ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﻟﻴﺰﺭ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺭﺍﻫﻨﻤﺎ ﺩﺭ ﺍﻧﺘﺨﺎﺏ ﻣﻨﺎﺳﺒﺘﺮﻳﻦ ﺗﻜﻨﻴﻚﻫﺎ ﺗﻮﺻﻴﻪ ﻣﻲﻧﻤﺎﻳﻨﺪ. 2001
)17.6 Cutaneous Medicine Cutaneous Manifestations of Systemic Disease (THOMAS T. PROVOST, MD, JOHN A.FLYNN, MD) (Johns Hopkins Medical Institutions Baltimore, Maryland
ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ،ﺍﻳﻦ ﻛﺘﺎﺏ ،ﺁﺭﻡ ﻭ ﻣﺸﺨﺼﻪ ﺩﭘﺎﺭﺗﻤﺎﻥ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ﺟﺎﻥ ﻫﺎﭘﻜﻴﻨﺰ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﻋﻠﻢ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻳﻚ ﻧﻈﺮ ﻛﻠﻲ ﻧﻪ ﻓﻘﻂ ﺑﻪ ﻋﻨﻮﺍﻥ ﭘﻮﺳﺖ ﻭ ﺿﻤﺎﺋﻢ ﺑﻠﻜﻪ ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﺗﻈﺎﻫﺮﺍﺕ ﺩﻳﮕﺮ ﺑﻴﻤﺎﺭﻱ ﺩﺭ ﺑﺪﻥ ﺍﺷﺎﺭﻩ ﺩﺍﺭﺩ .ﺍﻳﻦ ٧٨٢ﺻﻔﺤﻪﺍﻱ ﺑﺎ ٧٣ ﻓﺼﻞ ﺑﺎ ﻋﻜﺲﻫﺎﻱ ﺑﺎ ﻛﻴﻔﻴﺖ ﻋﺎﻟﻲ ﺑﻪ ﺭﺍﻫﻨﻤﺎﻳﻲ ﺑﺮﺍﻱ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺩﺍﺧﻠﻲ ﻣﻲﺑﺎﺷﺪ .ﻧﻜﺘﺔ ﺑﺎﺭﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺁﻭﺭﺩﻥ ﻧﻜﺎﺕ ﻣﻬﻢ ﻛﺘﺎﺏ ﺩﺭ ﺣﺎﺷﻴﻪ ﺻﻔﺤﺎﺕ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺩﺍﺧﻠﻲ ﻛﻪ ﺗﻈﺎﻫﺮﺍﺕ ﭘﻮﺳﺘﻲ ﺩﺍﺭﻧﺪ ﻭ ﺑﻴﻤﺎﺭﻱﻫـﺎﻱ ﭘﻮﺳـﺘﻲ ﻛـﻪ ﻣﻲﺗﻮﺍﻧﺪ ﻋﻼﺋﻢ ﻋﻤﻮﻣﻲ ﭘﻴﺪﺍ ﻛﻨﺪ ﺭﺍ ﺗﻮﺻﻴﻒ ﻛﺮﺩﻩ ﺍﺳﺖ .ﺗﻜﻴﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﻣﻮﺍﺭﺩ ﻛﻠﻴﺪ ﻛﻪ ﺩﺭ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ،ﻣﻲﺑﺎﺷﺪ ﻭ ﺍﺯ ﻣﺒﺎﺣﺚ ﻏﻴﺮﺿﺮﻭﺭﻱ ﺍﺟﺘﻨﺎﺏ ﻛﺮﺩﻩ ﺍﺳﺖ. Dr. Richard Dobsonﺩﺭ ﻣﺠﻠﺔ (AAD) American etcademy of Dermatologyﺩﺭ ﻣﻮﺭﺩ ﺍﻳﻦ ﻛﺘﺎﺏ ﮔﻔﺘﻪ ﺍﺳﺖ :ﺩﺭ ﮔﺬﺷﺘﺔ ﺍﻛﺜﺮ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﺑﻪ ﻋﻠﺖ ﺷﻴﻮﻉ ﺳﻴﻔﻴﻤﻴﺲ ﺑﺎ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺩﺍﺧﻠﻲ ﺁﺷﻨﺎ ﺑﻮﺗﺪﻩﺍﻧـﺪ ﺯﻳـﺮ ﺑـﻪ ﻗـﻮﻝ Sir Willamosler ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
32 ﺩﺍﻧﺴﺘﻦ ﺳﻴﻔﻴﻤﻴﺲ ﺩﺍﻧﺴﺘﻦ ﻋﻠﻢ ﭘﺰﺷﻜﻲ ﺍﺳﺖ .ﺑﺎ ﻭﺟﻮﺩ ﺍﻳﻨﺘﺮﻧﺖ Procedureﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺩﺭ ﻋﻠﻢ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﻪ ﻧﻈﺮ ﻣﻦ medical Dermatologistﺩﺭ ﺁﻳﻨﺪﻩ ﺍﺯ ﺟﺎﻳﮕﺎﻩ ﻭﻳﮋﻩﺍﻱ ﺑﺮﺧﻮﺭﺩﺍﺭ ﺧﻮﺍﻫﻨﺪ ﺑﻮﺩ ﺯﻳﺮ ﺍﺑﺎ ﻭﺟﻮﺩ ﺗﻈـﺎﻫﺮﺍﺕ ﭘﻮﺳـﺘﻲ ﺑﻴﻤـﺎﺭﻱ AIDS
ﻭ ﭘﻴﺸـﺮﻓﺖ
ﺩﺍﻧﺶ ﭘﺰﺷﻜﻲ ﺩﺭ ﻛﺎﺭﺑﺮﺩ ﺳﻴﺘﻮﻛﺴﻴﻦﻫﺎ ،ﺁﻧﺘﻲﺑﻴﻮﺗﻴﻚ ،ﻛﻤﻮﺗﺮﺍﭘﻲ ﻭ ﺍﻳﻤﻮﻧﻮﺳﺎﭘﺮﺳﻴﻮﻫﺎ ﻋﻠﻢ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﺎﻟﻴﻨﻲ ﺑﻪ ﺍﻓﺮﺍﺩﻱ ﺑﺮﺍﻱ ﭘﺮ ﻛﺮﺩﻥ ﺧﺎﻟﻲ ﺩﺭ ﻣﺮﺍﻛﺰ ﻋﻠﻤﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﺍﺣﺘﻴﺎﺝ ﺩﺍﺭﺩ. ــــــ
)18.6 Dermatology: A Multi-Media Teaching File (Disc 1,2) (Gross & Microscopic Symposium) (Mosby
2002
)19.6 EVIDENCE-BASED DERMATOLOGY (Howard I. Maibach, MD, Sagib J. Bashir, BSc (Hons), MB, ChB, Ann McKibbon, BSc, MLS ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺑﺮ ﺍﺳﺎﺱ ﻋﻠﻢ (Evidence- Based Heatlth Care) EBMCﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ EBHC .ﭼﻬﺎﺭﭼﻮﺑﻲ ﺑﺮﺍﻱ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺩﺭ ﺑﺎﻟﻴﻨﻲ ﻭ ﺗﺤﻘﻴﻘﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ .ﻭ ٥ﻣﺮﺣﻠﻪ ﺩﺍﺭﺩ:
ﺍﻳﻦ ﻛﺘﺎﺏ
-١ﺍﻳﺠﺎﺩ ﺳﺆﺍﻝ -٢ﭘﻴﺪﺍ ﻛﺮﺩﻥ ﻣﺪﺍﺭﻙ ﻣﻌﺘﺒﺮ ﺑﺮﺍﻱ ﺟﻮﺍﺏ ﺑﻪ ﺁﻥ ﺳﺆﺍﻝ -٣ﺍﺭﺯﻳﺎﺑﻲ ﺍﻳﻨﻜﻪ ﺍﻳﻦ ﻣﻨﺎﺑﻊ ﻭ ﻣﺪﺍﺭﻙ ﺁﻳﺎ ﻣﻌﺘﺒﺮﻧﺪ ﻳﺎ ﺧﻴﺮ -٤ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻣﺪﺍﺭﻙ ﺑﺮﺍﻱ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺩﺭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭ. ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﻭﺷﻲ ﻣﻨﻄﻘﻲ ﺑﺮﺍﻱ ﭘﻴﺪﺍﻛﺮﺩﻥ ﺳﺆﺍﻻﺕ ﺑﻪ ﻭﺟﻮﺩ ﺁﻣﺪﻩ ﺩﺭ ﺣﻴﻦ ﻛﺎﺭ ﺑﺎﻟﻴﻨﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ .ﺩﺭ ﻓﺼﻞ ﺍﻭﻝ ﻛﺘﺎﺏ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﻣﺮﺣﻠﻪ ﺑﻪ ﺗﻔﻀﻴﻞ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﭼﻄﻮﺭ ﻣﻲﺗﻮﺍﻥ ﻣﺘﻮﺟﻪ ﻣﻌﺘﺒﺮ ﺑﻮﺩﻥ ﻳﻚ ﻓﺮﺿﻴﻪ ﻳﺎ ﻣﻘﺎﻟﻪ ﮔﺮﺩﻳﺪ ﻭ... ﺩﺭ ﻓﺼﻞ ﺩﻭﻡ ﻛﺎﺭﺑﺮﺩ ﺍﻳﻦ ﻋﻠﻢ EBMEﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖ .ﻭ ﺩﺭ ﻓﺼﻠﻲ ﺟﺪﺍ ﻣﻨﺎﺑﻊ ﻣﻌﺘﺒﺮ ﻭ ﻗﺎﺑﻞ ﺗﻮﺟﻬﻲ ﺁﺩﺭﺱ ﺍﻳﻨﺘﺮﻧﺘﻲ ﺑﺎ ﻣﺸﺨﺼﺎﺕ ﻛﺎﻣﻞ ﺑﺮﺍﻱ ﺑﻪ ﺭﻭﺯﺑﻮﺩﻥ ﺍﻃﻼﻋﺎﺕ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻛﻪ ﺩﺭ ﻧﺸﺮ ﻛﺘﺎﺑﻲ ﺍﻳﻦ ﻣﻨﺎﺑﻊ ﺑﺎﺍﺭﺯﺵ ﻣﺸﺎﻫﺪﻩ ﻣﻲﺷﻮﺩ. ــــــ
20.6 Facial Lifting by "APTOS" threads Clinic of Plastic and Aesthetic Surgery
ــــــ
)21.6 Hair Removal with Intense Pulsed Laser (IPL
)ﻃﺮﻳﻘﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ -ﻣﺤﻞﻫﺎﻳﻲ ﻛﻪ ﺑﺮﺍﻱ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﺩ -ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ( +ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺍﻣﺮﻭﺯﻩ ﺭﻭﺵﻫﺎﻱ ﻭﻗﺖﮔﻴﺮ ﻭ ﺑﻌﻀﹰﺎ ﺑﺎ ﻋﺎﺭﺿﻪ ﺑﺮﺍﻱ ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﻣﺎﻧﻨﺪ ،sharingﻣﻮﺑﺮﻫﺎ ،ﺍﻟﻜﺘﺮﻭﻟﻴﺰ ﻭ ...ﻛﻤﺘﺮ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ .ﻟﻴﺰﺭﻫﺎﻱ ﺍﺯ ﺑﻴﻦﺑﺮﻧﺪﻩ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﺎ ﻭﻗﺖ ﻛﻤﺘﺮ ،ﻛﺎﺭﺍﺋﻲ ﺑﻴﺸﺘﺮ ﻭ ﻋﻮﺍﺭﺽ ﻣﺨﺘﺼﺮ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﺩﺭ ﻳﻚ ﺯﻧﺪﮔﻲ ﺑﺎ ﻛﻴﻔﻴﺖ ﻣﻄﻠﻮﺏ ﺑﺮﺍﻱ ﻣﺮﺍﺟﻌﻴﻦ ﺑﻪ ﭘﺰﺷﻜﺎﻥ ﺑﺨﺼﻮﺹ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﻛﻠﻴﻨﻴﻚﻫﺎﻱ ﺯﻳﺒﺎﺋﻲ ﺩﺍﺭﺩ .ﺍﺯ ﺟﻤﻠﻪ ﺟﺪﻳﺪﺗﺮﻳﻦ ﻟﻴﺰﺭﻫﺎﻱ ﺑﻜﺎﺭﺭﻓﺘﻪ ﻟﻴﺰﺭ IPLﻣﻲﺑﺎﺷﺪ .ﻓﻮﺍﺋﺪ ﺍﻳﻦ ﻟﻴﺰﺩ ﺩﺭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﻳﻦ ﻟﻴﺰﺭ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺎ Skin typeﺑﺎﻻ Spot size ،ﺑﺰﺭﮔﺘﺮ ﻭ ﺩﺭ ﻧﺘﻴﺠﻪ ﻃﻮﻝ ﻣﺪﺕ ﻛﻤﺘﺮ ﺩﺭﻣﺎﻥ Therapeatic window ،ﺑﺰﺭﮔﺘﺮ ﻛﻪ ﻣﻮﺟﺐ ﻋﺎﺭﺿﻪ ﻛﻤﺘﺮ ﻭ ﻛﺎﺭﻣﺪﻱ ﺑﻴﺸﺘﺮ ﻣﻲﺷﻮﺩ .ﺩﺭ ﺍﻳﻦ CDﻛﻪ ﺑﻪ ﺳﻔﺎﺭﺵ ﻛﻤﭙﺎﻧﻲ Ellipseﺗﻮﻟﻴﺪ ﺷﺪﻩ ﺍﺳﺖ .ﻣﻌﺮﻓﻲ ﻟﻴﺰﺭ ،IPLﭼﮕﻮﻧﮕﻲ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ،ﻓﻮﺍﺋﺪ ﻟﻴﺰﺭ ،IPLﻣﻨﺎﻃﻘﻲ ﻛﻪ ﺩﺭ ﺁﻥ ﺍﺯ ﻟﻴﺰﺭ IPLﺑﺮﺍﻱ
ﺭﻓﻊ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻛﻠﻴﭗ ﻭﻳﺪﺋﻮﺋﻲ ﺍﺯ ﺑﻴﻤﺎﺭﻳﺎﻥ ﻭ ﻧﺤﻮﻩ ﺩﺭﻣﺎﻥ ﻭ ﻧﺘﺎﻳﺞ ﺩﺭﻣﺎﻥ ﺑﺎ ﻋﻜﺲ ﻭ clipﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. )(The Art of Micrografting and Minigrafting) (Salekan E-Book
2002 ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ: TECHNIQUE
22.6 HAIR TRANSPLANTATION
PLANING AND PATIENT INSTRUCTUIONS
PATIENT EVALUATION
ANATOMY AND PHYSILOGY OF HAIR
SPECIAL APPLICATIONS
REOPERATIVE SURGERY
COMBINED FACE LIFT AND HAIR TRANSPLAYTATION
1999
)23.6 HANDBOOK OF ORAL DISEASE DIAGNOSIS AND MANAGEMENT Cripian Scully (MARTIN DUNITZ ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺷﺎﻣﻞ ٤٢٠ﺻﻔﺤﻪ ﻣﺘﻦ ﺑﻪ ﻫﻤﺮﺍﻩ ﺑﻴﺶ ﺍﺯ ٤٠٠ﺗﺼﻮﻳﺮ ﺭﻧﮕﻲ ﺍﺯ ﺿﺎﻳﻌﺎﺕ ﺩﻫﺎﻧﻲ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺭﻣﺎﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﺩﻧﺪﺍﻧﭙﺰﺷﻜﺎﻥ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﻳﻪ ﺗﻨﻬﺎ ﺑﻪ ﻋﻨـﻮﺍﻥ ﺍﻃﻠـﺲ ﺑﻠﻜـﻪ ﺍﺯ ﺟﻨﺒﺔ ﺍﺗﻴﻮﻟﻮﮊﻱ ،ﻛﻠﻴﺪﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺩﺭﻣﺎﻥ ﻭ ﺩﺭ ﺻﻮﺭﺕ ﺍﻣﻜﺎﻥ ﭘﻴﺸﮕﻴﺮﻱ ﻧﻴﺰ ﺑﻪ ﺿﺎﻳﻌﺎﺕ ﺩﻫﺎﻧﻲ ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ .ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺎﻳﻊ ﻭ ﻣﻬﻢ ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﺩﻫﺎﻧﻲ ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ ﻋﻼﻭﻩ ﺑﺮ ﺍﻳﻦ ﺗﻌﺪﺍﺩﻱ ﻣﻮﺍﺭﺩ ﻧﺎﺩﺭ ﻛﻪ ﺩﺭ ﺳﻄﺢ ﺟﻬﺎﻥ ﺭﻭ ﺑﻪ ﺍﻓﺰﺍﻳﺶ ﺍﺳﺖ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ .ﻓﺼﻞ ﺍﻭﻝ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﺑﺮﺭﺳﻲ symptom, signﺿﺎﻳﻌﺎﺕ ﺩﻫﺎﻧﻲ ﻣﻲﺑﺎﺷﺪ .ﻓﺼﻮﻝ ﺑﻌﺪﻱ ﺷﺎﻣﻞ ﺩﺭﺩﻫﺎﻱ ﻧﺎﺣﻴﺔ ﺩﻫﺎﻥ ﺑﺎ ﻣﻨﺸﺎﺀ ﻋﺮﻭﻗﻲ ﻳﺎ ﻋﺼﺒﻲ ،ﺷﻜﺎﻳﺎﺕ ﺩﻫﺎﻧﻲ ﺑﺎ ﻣﻨﺸﺎﺀ ﺭﻭﺍﻧﻲ ،ﺿﺎﻳﻌﺎﺕ ﻣﺨﺎﻃﻲ ،ﺑﺰﺍﻗﻲ ،ﺿﺎﻳﻌﺎﺕ ﻟﺜﻪﻫﺎ ،ﺿﺎﻳﻌﺎﺕ ﻟﺐ ﻭ ﻛـﺎﻡ ﻭ ﺿـﺎﻳﻌﺎﺕ ﺩﻫﺎﻧﻲ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻫﺮ ﻓﺼﻞ ﺍﺑﺘﺪﺍ ﺿﺎﻳﻌﺎﺕ ﺑﺮ ﺍﺳﺎﺱ ﺍﻟﻔﺒﺎﻱ ﺍﻧﮕﻠﻴﺴﻲ ﺗﻨﻈﻴﻢ ﻭ ﺳﭙﺲ ﺑﺮ ﺍﺳﺎﺱ management ،Diagnosis ،Clinical feature ،Aetiology ،Sexmainly affected ،Agemainly affected ،incidence ،Defintionﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﺷﺪﻩ ﺍﺳﺖ.
2000
24.6 Laser Hair Removal
)(David J. Goldman) (Martin Dunits ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﻣﺮﻭﺭﻱ ﺑﺮ ﻟﻴﺰﺭﻫﺎﻱ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺑﺮﺍﻱ ﺑﺮﺩﺍﺷﺖ ﻣﻮﻫﺎ ) (hair removalﻣﻲﺑﺎﺷﺪ .ﻧﺨﺴﺘﻴﻦ ﻓﺼﻞ ﻛﺘﺎﺏ ﺍﺧﺘﺼﺎﺹ ﺑﻪ ﺑﻴﻮﻟﻮﮊﻱ ﻣﻮ ﺩﺍﺭﺩ .ﻓﺼﻞ ﺑﻌﺪﻱ ﻛﺘﺎﺏ ﻣﺮﻭﺭﻱ ﮔﺬﺭﺍ ﺑﻪ ﻓﻴﺰﻳﻚ ﻟﻴﺰﺭ ﻭ ﻛﺎﺭﺑﺮﺩ ﺁﻥ ﺩﺭ hair removalﻣﻲﺑﺎﺷﺪ .ﻓﺼﻞ ﺑﻌﺪﻱ ﻛﺘﺎﺏ ،ﺑﻪ ﭼﮕﻮﻧﮕﻲ ﺁﻧﺠﺎﻡ ﺍﻟﻜﺘﺮﻭﻟﻴﺰ ﺩﺭ ﺭﻓﻊ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﻭ ﻣﻘﺎﻳﺴﺔ ﺁﻥ ﺑﺎ ﻟﻴﺰﺭ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺩﺭ ﻓﺼﻮﻝ ﺩﻳﮕﺮ ﻛﺘﺎﺏ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﻟﻴﺰﺭﻫﺎ ﻛﻪ ﺑﺮﺍﻱ ﺭﻓﻊ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﻧﺪ ﺑﺮﺭﺳﻲ ﻣﻲﮔﺮﺩﺩ: 5- Intense pulsed light
ND: YAG laser
4-
3- Diode laser
2- Normal mode alexandrite laser
1- Normal mode Ruby laser
ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻣﻘﺎﻻﺕ ﺗﺤﻘﻴﻘﻲ ﻭ ﻃﺮﻕ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻫﺮ ﻳﻚ ﺍﺯ ﺩﺳﺘﮕﺎﻫﻬﺎﻱ ﺍﻳﺰﺭ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﺩﺭ ﺁﺧﺮ ﻫﺮ ﻓﺼﻞ ﻧﻈﺮ ﻣﺆﻟﻒ ﺩﺭ ﺧﺼﻮﺹ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﺳﻴﺴﺘﻢﻫﺎ ﻣﻄﺮﺡ ﺷﺪﻩ ﺍﺳﺖ. ﻳﻜﻲ ﺍﺯ ﻧﻜﺎﺕ ﻣﻨﺤﺼﺮ ﺑﻪﻓﺮﺩ ﻛﺘﺎﺏ ﻣﻌﺮﻓﻲ ﻟﻴﺰﺭﻫﺎﻱ ﻣﻌﺘﺒﺮ ﺍﺯ ﺷﺮﻛﺖﻫﺎﻱ ﻣﻌﺘﺒﺮ ﻭ ﻣﻘﺎﻳﺴﺔ ﺁﻧﻬﺎ ﺑﺎ ﻳﻜﺪﻳﮕﺮ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﭘﺰﺷﻚ ﺭﺍ ﺩﺭ ﺍﻧﺘﺨﺎﺏ ﺩﺳﺘﮕﺎﻩ ﻟﻴﺰﺭ ﻣﻨﺎﺳﺐ ﻳﺎﺭﻱ ﻣﻲﻛﻨﺪ ﻛﻪ ﺩﺭ ﻧﻬﺎﻳﺖ ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﺻﺤﻴﺢ ﺑﻪ ﺣﺼﻮﻝ ﻧﺘﻴﺠﺔ ﺧﻮﺏ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﻣﻲﻧﻤﺎﻳﺪ. ــــــ
)25.6 MANAGEMENT OF FACIAL LINES AND WRINKLES (ANDREW BLITZER, WILLIAM J. BINDER, J. BRIAN BOYD ALASTAIR CARRUTHERS) (SALEKAN E-BOOK
ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺷﺎﻣﻞ ٢٢ﻓﺼﻞ ﺍﻃﻼﻋﺎﺕ ﺟﺎﻟﺒﻲ ﺩﺭ ﻣﻮﺭﺩ ﺩﺭﻣﺎﻥ ﻭ ﻧﻮﻉ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎ ) (Line 8 Wrinkleﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﺳﭙﺲ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻓﺼﻮﻝ ﻣﺠﺰﺍ exfoliantsﻳﺎ Superfical peelﻣﺮﻃﻮﺏﻛﻨﻨﺪﺓ ﺁﻧﺎﻟﻮﮒﻫﺎﻱ Chemical ، Vitaminsﺑﺎﻓﻨﻮﻝ ﻭ ، TCAﻣﻘﺎﻳﺴﻪ Peelﺷﻴﻤﻴﺎﻳﻲ ﻭ ﻟﻴﺰﺭ Dermabrasion ،ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻧﻮﺍﻉ implantﻫﺎﻱ ﺻﻮﺭﺕ ،ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ Dermal Allograftﻃﺮﻳﻘـﺔ ﮔﺬﺍﺷـﺘﻦ GORTEXﺗـﺰﺭﻱ ﻛـﻼﮊﻥ ﻭ ﭼﺮﺑﻲ Directexcision ،ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎ ﺗﺼﺤﻴﺢ ﺟﺮﺍﺣﻲ facelifting, endoscopic Browloft Skeletal frameﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ .ﻳﻚ ﻓﺼﻞ ﺍﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺧﺘﺼﺎﺹ ﺑﻪ ﻣﺮﻭﺭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ ﻛﺎﺭﺑﺮﺩ ﺩﺭﻣﺎﻥ ﺗﻮﻛﺴﻴﻦ ﺑﻮﺗﻮﻟﻴﻨﻴﻮﻡ ﺩﺭ ﭘﺰﺷﻜﻲ ﻭ ﻓﺼﻞ ﺩﻳﮕـﺮ ﺑـﻪ ﻃﺮﻳﻘـﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺗﺰﺭﻳﻖ Botulinium Toxinﺑﺮﺍﻱ ﺩﺭﻣﺎﻥ ﭼﻴﻦ ﻭ ﭼﺮﻭﻙﻫﺎ ﺑﺤﺚ ﻣﻲﻧﻤﺎﻳﺪ .ﺳﭙﺲ ﺩﺭ ﻓﺼﻞ ٢٠ﻃﺮﻳﻘﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ﻭ Botulinumtoxinﺩﺭ ﺭﻓﻊ ﺧﻄﻮﻁ ﺩﺭ ﭼﺸﻢ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ ٢١ﻃﺮﻳﻘﺔ ﻋﻜﺲ ﮔـﺮﻓﺘﻦ ﺍﺯ ﺑﻴﻤـﺎﺭ ﺑـﻪ ﻋﻨـﻮﺍﻥ ﻳـﻚ ﺳـﻨﺪ ﭘﺰﺷﻜﻲ ﻭ Computer imagingﺑﺎ ﺩﻭﺭﺑﻴﻦﻫﺎﻱ ﺩﻳﺠﻴﺘﺎﻟﻲ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
33 )26.6 MANUAL OF CUTANEOUS LASER TECHNIQUES (Second Edition) (Tinal S. Alster, M.D.) (SALEKAN E-BOOK
2000
ــــــ
ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺷﺎﻣﻞ ١٢ﻓﺼﻞ ﺍﺳﺖ ﻛﻪ ﻳﻜﻲ ﺍﺯ ﻛﺎﺭﺑﺮﺩﻱﺗﺮﻳﻦ ﻛﺘﺎﺏﻫﺎ ﺩﺭ ﺯﻣﻴﻨﺔ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﺑﺎ ﻟﻴﺰﺭ ﻣﻲﺑﺎﺷﺪ .ﻧﮕﺎﻩ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻴﺸﺘﺮ ﺑﺮ ﻧﻜﺎﺕ ﻋﻤﻠﻲ ﻟﻴﺰﺭ ﻭ ﺗﻜﻨﻴﻚﻫﺎ ﻭ ﻣﺸﻜﻼﺗﻲ ﺍﺳﺖ ﻛﻪ ﺣﻴﻦ ﻭ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ ﺍﻳﺠﺎﺩ ﻣﻲﺷﻮﺩ ،ﻣﺘﻤﺮﻛﺰ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ﺗﻮﺿﻴﺤﺎﺗﻲ ﻛﻪ ﺑﻪ ﺑﻴﻤﺎﺭ ﻗﺒﻞ ﺍﺯ ﻋﻤﻞ ﻭ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ ﺑﺎﻳﺪ ﺩﺍﺩﻩ ﺷﻮﺩ ﻭ ﻫﻤﭽﻨﻴﻦ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺘﺨﺎﺏ ﺑﻴﻤﺎﺭ ﻣﻨﺎﺳﺐ ) (Patient selectionﺑﻪ ﻃﻮﺭ ﻛﺎﻣﻞ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺑﻌﻀﻲ ﺍﺯ ﻓﺼﻮﻝ ،ﻛﺘﺎﺏ ﺑﻪ ﻣﻌﺮﻓﻲ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺑﻪ ﻛﺎﺭﮔﻴﺮﻱ ﻟﻴﺰﺭﻫﺎ ﻭ ﻣﻌﺮﻓﻲ ﺩﺳﺘﮕﺎﻩﻫﺎﻱ ﻟﻴﺰﺭﻱ ﻣﻌﺘﺒﺮ ﻭ ﻣﻘﺎﻳﺴﺔ ﺩﺳﺘﮕﺎﻫﻬﺎﻱ ﻟﻴﺰﺭ ﻭ ﺭﻭﺵ ﺍﻧﺠﺎﻡ ﻛﺎﺭ ﺑﻪ ﻃﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺮﺍﻱ ﻟﻴﺰﺭﻫﺎﻱ ﺍﺧﺘﺼﺎﺻﻲ ﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻮﻝ ﺟﺪﻳﺪ ﻛﺘﺎﺏ ﻧﺴﺒﺖ ﺑﻪ editionﻗﺒﻞ ﺷـﺎﻣﻞ erbium :YAG laserﻭ Resurfacingﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﺑﺎ ﻟﻴﺰﺭ ﻭ ﻟﻴﻔﺘﮓ ﭘﻴﺸﺎﻧﻲ ﻫﻤﺰﻣﺎﻥ ﺑﺎ ﻟﻴﺰﺭ ﻭ ﻟﻴﺰﺭﻫﺎﻱ hair removalﺍﺿﺎﻓﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺩﺭ ﻓﺼﻮﻝ ﺁﺧﺮ ﻛﺘﺎﺏ ﻋﻮﺍﺭﺽ ﻟﻴﺰﺭ ﻭ ﭼﮕﻮﻧﮕﻲ ﺩﺭﻣﺎﻥ ﺁﻧﻬﺎ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻟﻴﺰﺭ ﺑﻪ ﻃﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ. ﻣﻲﺗﻮﺍﻥ ﮔﻔﺖ ﻛﺘﺎﺏ ﺣﺎﺿﺮ ﻫﻤﺮﺍﻩ ﺑﺎ Cutaneous Laser in Medicineﻧﻮﺷﺘﺔ Fitzpatricﻭ Goldmanﻛﺎﻣﻞﺗﺮﻳﻦ ﻛﺘﺎﺏﻫﺎﻱ ﭘﺎﻳﻪ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﺩﺭ ﻋﻠﻢ ﻟﻴﺰﺭ ﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺑﻮﺩﻩ ﻭ ﺍﺻﻠﻲﺗﺮﻳﻦ ﻛﺘﺎﺑﻲ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫـﺎ ﻭ ﺟﺮﺍﺣـﺎﻥ ﺑـﺎ ﮔـﺮﺍﻳﺶ facial rejuvenationﺑﻪ ﺁﻥ ﻧﻴﺎﺯ ﺩﺍﺭﻧﺪ. )Clifford M Lawrence Neil H Cox (Joseph L Jorizzo) (SALEKAN E-BOOK )27.6 PHYSICAL SIGNS IN DERMATOLOGY (SECOND EDITION ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ٧٠٠ﺗﺼﻮﻳﺮ ﺗﻤﺎﻡ ﺭﻧﮕﺲ ﺍﺯ ﺿﺎﻳﻌﺎﺕ ﻣﺨﺘﻠﻒ ﭘﻮﺳﺘﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮ ﺍﺳﺎﺱ ﺷﻜﻞ ﻭ ﺭﻧﮓ ﻭ ﻣﺤﻞ ﺿﺎﻳﻌﺎﺕ ﺗﻘﺴﻴﻢﺑﻨﺪﻱ ﺷﺪﻩ ﻭ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻓﻲ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﺧﻮﺍﻧﻨﺪﻩ ﺍﻳﻦ ﺍﻣﻜﺎﻥ ﺭﺍ ﻣﻲﺩﻫﺪ ﻛﻪ ﺑﺎ ﺁﻧﺎﻟﻴﺰ ﺩﺭ ﻣﺸﺎﻫﺪﺓ ﺑﺎﻟﻴﻨﻲ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻌﻠﻮﻣﺎﺕ ﺑﻪ ﺗﺸﺨﻴﺺ ﺻﺤﻴﺢ ﺿﺎﻳﻌﺎﺕ ﺑﺮﺳﺪ. ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻴﻤﺎﺭﻱﻫﺎ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﻓﻴﺰﻳﻮﭘﺎﺗﻮﻟﻮﮊﻱ )ﻋﻔﻮﻧﻲ ،ﺍﺗﻮﺍﻳﻤﻮﻥ ﻭ ( ...ﺗﻘﺴﻴﻢ ﺑﻨﺪﻱ ﻧﻜﺮﺩﻩ ﺑﻠﻜﻪ ﺑﺮ ﺍﺳﺎﺱ ﺷﻜﻞ ﻭ ﻣﺤﻞ ﺿﺎﻳﻌﺎﺕ ﻓﺼﻞ ﺑﻨﺪﻱ ﺷﺪﻩ ﺍﺳﺖ .ﻛﻪ ﺑﺮﺍﻱ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻳﻚ approachﻋﻤﻠﻲ ﺑﺮﺍﻱ ﺭﺳﻴﺪﻥ ﺑﻪ ﺗﺸﺨﻴﺺ ﺿﺎﻳﻌﺎﺕ ﺭﺍ ﻓﺮﺍﻫﻢ ﻣﻲﻛﻨﺪ. ﺍﻳﻦ ﻛﺘﺎﺏ ﻫﺮ ﭼﻨﺪ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﻛﺘﺎﺏ testﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻧﻤﻲﺑﺎﺷﺪ ﻭﻟﻲ ﺗﻤﺎﻡ ﻣﺒﺎﺣﺚ ﻣﻬﻢ ﻭ ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﻣﻮﺍﺭﺩ ﻧﺎﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺩﺭ ﺁﻥ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻳﻜﻲ ﺍﺯ ﻧﻜﺎﺕ ﻣﻤﺘﺎﺯ ﺩﺭ ﻭﻳﺮﺍﻳﺶ ﺟﺪﻳﺪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺁﻭﺭﺩﻥ ﺟﺪﺍﻭﻟﻲ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺁﻧﻬﺎ ﻧﻜﺎﺕ ﻛﻠﻴﺪﻱ ﺩﺭ ﺗﺸﺨﻴﺺ ﻭ pitfallsﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺑﻴﺎﻥ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺣﻘﻴﻘﺖ ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﺍﻃﻠﺲ ﺭﻧﮕﻲ ﺿﺎﻳﻌﺎﺕ ﭘﻮﺳﺘﻲ ﻭ ﺷﺮﺡ ﻭ ﺁﻧﺎﻟﻴﺰ ﺭﺳﻴﺪﻥ ﺑﻪ ﺗﺸﺨﻴﺺ ﺿﺎﻳﻌﺎﺕ ﻭ ﺟﺪﺍﻭﻝ ﻛﻤﻚ ﻛﻨﻨﺪﻩ ﺩﺭ ﺗﺸﺨﻴﺺ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻣﻮﺟﺐ ﺷﺪﻩ ﻳﻚ ﻛﺘﺎﺏ ﺑﺎﺍﺭﺯﺵ ﻧﻪ ﺗﻨﻬﺎ ﺑﺮﺍﻱ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﺑﻠﻜﻪ ﺑﺮﺍﻱ ﺳﺎﻳﺮ ﭘﺰﺷﻜﺎﻥ ﻛﻪ ﺑﺎ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﻮﺳﺘﻲ ﻛﻤﺘﺮ ﺁﺷﻨﺎﻳﻲ ﺩﺍﺭﻧﺪ ﺑﻪ ﻛﺎﺭ ﺭﻭﺩ .ﺑﻪ ﮔﻔﺘﺔ Dr. Joav Merickﺗﺼﺎﻭﻳﺮ ﺁﻥ ﭼﻨﺎﻥ ﻛﻴﻔﻴﺘﻲ ﺩﺍﺭﻧﺪﻛﻪ ﮔﻮﻳﺎ ﺑﻴﻤﺎﺭ ﺩﺭ ﻣﻘﺎﺑﻞ ﺷﻤﺎ ﺍﻳﺴﺘﺎﺩﻩ ﺍﺳﺖ .ﺑﻪ ﻋﻠﺖ ﺍﻫﻤﻴﺖ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺎﻳﺪ ﻫﺮ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺘﻲ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﻫﻤﺮﺍﻩ ﺩﺍﺷﺘﻪ ﺑﺎﺷﺪ ﻭ ﺳﺎﻳﺮ ﺧﺎﻧﻮﺍﺩﻩﻫﺎﻱ ﭘﺮﺷﻜﻲ ،ﻣﺘﺨﺼﻴﺼﻴﻦ ﺍﻃﻔﺎﻝ ﻭ ﺩﺍﺧﻠﻲ ﺩﺭ ﻓﻌﺎﻟﻴﺖ ﺑﺎﻟﻴﻨﻲ ﺑﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺣﺘﻴﺎﺝ ﭘﻴﺪﺍ ﺧﻮﺍﻫﻨﺪ ﻛﺮﺩ .ﻫﺮ ﻛﺘﺎﺑﺨﺎﻧﺔ ﭘﺰﺷﻜﻲ ﺑﺎﻳﺪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﺩﺭ ﻗﻔﺴﻪﻫﺎﻱ ﺧﻮﺩ ﺟﺎﻱ ﺩﻫﺪ... 28.6 Practical MINOR SURGERY
ــــ 2002
)(Third Edition) (Antoinette F. Hood, Thedore H. Kwan, Martin C. Mihm, Jr., Thomas D. Horn, Bruce R. Smoller 7. Bonus Quizzes 6. Panniculus
4. Reticular Dermis 5. Appendages
29.6 Primer of Dermatopathology
3. Basement Membrane Zone, Oaoillary Dermis, and Superficial Vascular Plexus
1. Introduction 2. Epidermis
ــــــ
)Radiosurgical Treatment of Superficial Skin Lesions (S. Randolph Waldman, M.D.
30.6
ــــــ
)Radiosurgical Vaporization of Dermatologic Lesions (Dr. Stephen Chiarello
31.6
)6. Basal Cell Carcinoma (Nasal Bridge
)5. Scar Revision (Nose
)4. Basel Cell Carcinoma (Nasal Tip
)3. Scar Revision (Back
11. Tonsillectomy
10. Rhinoplasty
9. Turbinate Shrinkage
8. Radiosurgery in ENT
12. Tympanoplasty
ــــــ
)(SALEKAN E-BOOK
2- Keratosis Removal
1- Rhinophyma
)7. Scar Revision (Lower Forehead
Reconstructive Facial Plastic Surgery
32.6
)ﻃﺮﻳﻘﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ -ﻣﺤﻞﻫﺎﻳﻲ ﻛﻪ ﺑﺮﺍﻱ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﺩ -ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ( +ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺍﻣﺮﻭﺯﻩ ﺭﻭﺵﻫﺎﻱ ﻭﻗﺖﮔﻴﺮ ﻭ ﺑﻌﻀﹰﺎ ﺑﺎ ﻋﺎﺭﺿﻪ ﺑﺮﺍﻱ ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﻣﺎﻧﻨﺪ ،sharingﻣﻮﺑﺮﻫﺎ ،ﺍﻟﻜﺘﺮﻭﻟﻴﺰ ﻭ ...ﻛﻤﺘﺮ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ. ﻟﻴﺰﺭﻫﺎﻱ ﺍﺯ ﺑﻴﻦﺑﺮﻧﺪﻩ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺑﺎ ﻭﻗﺖ ﻛﻤﺘﺮ ،ﻛﺎﺭﺍﺋﻲ ﺑﻴﺸﺘﺮ ﻭ ﻋﻮﺍﺭﺽ ﻣﺨﺘﺼﺮ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﺩﺭ ﻳﻚ ﺯﻧﺪﮔﻲ ﺑﺎ ﻛﻴﻔﻴﺖ ﻣﻄﻠﻮﺏ ﺑﺮﺍﻱ ﻣﺮﺍﺟﻌﻴﻦ ﺑﻪ ﭘﺰﺷﻜﺎﻥ ﺑﺨﺼﻮﺹ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﻛﻠﻴﻨﻴﻚﻫﺎﻱ ﺯﻳﺒﺎﺋﻲ ﺩﺍﺭﺩ. ﺍﺯ ﺟﻤﻠﻪ ﺟﺪﻳﺪﺗﺮﻳﻦ ﻟﻴﺰﺭﻫﺎﻱ ﺑﻜﺎﺭﺭﻓﺘﻪ ﻟﻴﺰﺭ IPLﻣﻲﺑﺎﺷﺪ .ﻓﻮﺍﺋﺪ ﺍﻳﻦ ﻟﻴﺰﺩ ﺩﺭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﻳﻦ ﻟﻴﺰﺭ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺎ Skin typeﺑﺎﻻ Spot size ،ﺑﺰﺭﮔﺘﺮ ﻭ ﺩﺭ ﻧﺘﻴﺠﻪ ﻃﻮﻝ ﻣﺪﺕ ﻛﻤﺘﺮ ﺩﺭﻣﺎﻥ Therapeatic window ،ﺑﺰﺭﮔﺘﺮ ﻛﻪ ﻣﻮﺟﺐ ﻋﺎﺭﺿﻪ ﻛﻤﺘﺮ ﻭ ﻛﺎﺭﻣﺪﻱ ﺑﻴﺸﺘﺮ ﻣﻲﺷﻮﺩ. ﺩﺭ ﺍﻳﻦ CDﻛﻪ ﺑﻪ ﺳﻔﺎﺭﺵ ﻛﻤﭙﺎﻧﻲ Ellipseﺗﻮﻟﻴﺪ ﺷﺪﻩ ﺍﺳﺖ .ﻣﻌﺮﻓﻲ ﻟﻴﺰﺭ ،IPLﭼﮕﻮﻧﮕﻲ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻟﻴﺰﺭ ،ﻓﻮﺍﺋﺪ ﻟﻴﺰﺭ ،IPLﻣﻨﺎﻃﻘﻲ ﻛﻪ ﺩﺭ ﺁﻥ ﺍﺯ ﻟﻴﺰﺭ IPLﺑﺮﺍﻱ ﺭﻓﻊ ﻣﻮﻫﺎﻱ ﺯﺍﺋﺪ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻫﺮ ﺑﺨﺶ ﻛﻠﻴﭗ ﻭﻳـﺪﺋﻮﺋﻲ ﺍﺯ ﺑﻴﻤﺎﺭﻳـﺎﻥ ﻭ ﻧﺤـﻮﻩ ﺩﺭﻣـﺎﻥ ﻭ ﻧﺘﺎﻳﺞ ﺩﺭﻣﺎﻥ ﺑﺎ ﻋﻜﺲ ﻭ clipﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. 2002
)33.6 REFINEMENT IN HAIR TRANSPLANTATION: Micro and minigraft Megasession (Alfonso Barrera, M.D.
ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺩﺭ ﻣﻮﺭﺩ ﭘﻴﻮﻧﺪ ﻣﻮ ﺑﻪ ﺭﻭﺵ ﻣﻴﻜﺮﻭﮔﺮﺍﻓﺖ )ﮔﺮﺍﻓﺖ ١-٢ﻣﻮ( ﻭ ﻣﻴﻨﻲﮔﺮﺍﻓﺖ )ﮔﺮﺍﻓﺖ ٣-٤ﻣﻮ( ﺑﺮﺍﻱ ﻃﺎﺳﻲ ﻣﺮﺩﺍﻧﻪ ﻭ ﺩﻳﮕﺮ ﺍﺧﺘﻼﻻﺕ ﺭﻳﺰﺵ ﻣﻮ ﻣﻲﺑﺎﺷﺪ .ﻋﻼﻭﻩ ﺑﺮ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ،ﺗﺼﺎﻭﻳﺮ ﮔﺮﺍﻓﻴﻜﻲ ﺑﺮﺍﻱ ﻓﻬﻢ ﻣﻄﺎﻟﺐ ﺑﻪ ﻛﺎﺭ ﺭﻓﺘﻪ ﺍﺳﺖ. ﻓﺼﻞ -١ﺩﺭ ﻣﻮﺭﺩ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻣﻮ ﻣﻲﺑﺎﺷﺪ ﺗﺎ ﺍﻃﻼﻋﺎﺕ ﭘﺎﻳﻪﺍﻱ ﻗﺒﻞ ﺍﺯ ﺍﻧﺠﺎﻡ ﺍﻋﻤﺎﻝ ﭘﻴﻮﻧﺪ ﺑﻪ ﻧﻮﺁﻣﻮﺯﺍﻥ ﺑﺪﻫﺪ. ﻓﺼﻞ -٢ﺍﻃﻼﻋﺎﺕ ﺳﻮﺩﻣﻨﺪﻱ ﺩﺭ ﻣﻮﺭﺩ ﺍﻟﮕﻮﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺭﻳﺰﺵ ﻣﻮ ﻭ ﺟﺮﺍﺣﻲ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﻣﺸﻜﻼﺕ ﻓﺮﺩﻱ ﺑﻴﻤﺎﺭ ﻭ ﺑﻬﺘﺮﻳﻦ ﺭﻭﺵ ﺑﺮﺍﻱ ﺑﺮﻃﺮﻑﻛﺮﺩﻥ ﺭﻳﺰ ﻣﻮ ﻛﻤﻚ ﻣﻲﻛﻨﺪ. ﻓﺼﻞ -٣ﺩﺭ ﻣﻮﺭﺩ ﺗﺠﻬﻴﺰﺍﺕ ﻻﺯﻡ ﺑﺮﺍﻱ ﺍﻧﺠﺎﻡ ﭘﻴﻮﻧﺪ ﻣﻮ ﻭ ﻫﻤﭽﻨﻴﻦ ﺍﻃﻼﻋﺎﺗﻲ ﻛﻪ ﺑﺎﻳﺪ ﺑﻪ ﺑﻴﻤﺎﺭ ﻗﺒﻞ ﺍﺯ ﺍﻧﺠﺎﻡ ﺟﺮﺍﺣﻲ ﺩﺍﺩﻩ ﺷﻮﺩ. ﻓﺼﻞ -٤ﺗﻮﺿﻴﺢ ﻗﺪﻡ ﺑﻪ ﻗﺪﻡ ﺗﻮﺳﻂ ﺗﺼﺎﻭﻳﺮ ﻭﺍﻗﻌﻲ ﻭ ﮔﺮﺍﻓﻴﻜﻲ ﺍﻧﺠﺎﻡ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﭘﻴﻮﻧﺪ ﻣﻮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺗﺼﺎﻭﻳﺮ Caseﻫﺎﻱ ﺟﺮﺍﺣﻲﺷﺪﻩ ﺍﺯ ﺍﺑﺘﺪﺍ ﺗﺎ ﺍﻧﺘﻬﺎﻱ ﻋﻤﻞ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻧﺘﺎﻳﺞ ﻫﺮ ﻳﻚ ﺑﺤﺚ ﻣﻲﺷﻮﺩ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
34 ﻼ ﺗﻮﺳﻂ ﺭﻭﺵﻫﺎﻱ ﺩﻳﮕﺮ ﺑﺮﺍﻱ ﻃﺎﺳﻲ ﺳﺮ ﺟﺮﺍﺣﻲ ﺷﺪﻩﺍﻧﺪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺗﺮﻣﻴﻢ ﺁﻧﻬﺎ ﺑﻪ ﺭﻭﺵ ﻣﻴﻨﻲ ﻭ ﻣﻴﻜﺮﻭﮔﺮﺍﻓﺖ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻓﺼﻞ -٥ﺗﺮﻛﻴﺐ ﺟﺮﺍﺣﻲ ﭘﻴﻮﻧﺪ ﻣﻮ ﺑﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺩﻳﮕﺮ ﻣﺎﻧﻨﺪ face liftingﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺍﻳﻦ ﻓﺼﻞ Caseﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻛﻪ ﻗﺒ ﹰ ﻓﺼﻞ -٦ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺩﻳﮕﺮ ﻣﻴﻜﺮﻭﮔﺮﺍﻓﺖ ﻭ ﻣﻴﻨﻲﮔﺮﺍﻓﺖ ﺩﺭ ﻛﺎﺭﻫﺎﻱ ﺯﻳﺒﺎﻳﻲ ﻭ ﺟﺮﺍﺣﻲ ﭘﻼﺳﺘﻴﻚ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻓﺼﻞ -٧ﻛﺘﺎﺏ ﻛﺎﺭﺑﺮﺩ ﻣﻴﻜﺮﻭﮔﺮﺍﻓﺖ ﻭ ﻣﻴﻨﻲﮔﺮﺍﻓﺖ ﺩﺭ ﭘﻨﻬﺎﻥﻛﺮﺩﻥ ﺍﺳﻜﺎﺭﻫﺎﻱ ،Scafpﺍﺻﻼﺡ ﺧﻂ ﺭﻳﺶ ﺑﺨﺼﻮﺹ ﺑﻌﺪ ﺍﺯ ،face liftﻛﺎﺷﺖ ﺍﺑﺮﻭ ،ﺳﺒﻴﻞ ،ﺭﻳﺶ ،ﺩﺭﻣﺎﻥ ﺁﻟﭙﻮﺳﭙﻲ ﺑﻪ ﻋﻠﺖ ﺳﻮﺧﺘﮕﻲ ﻭ ﻛﺎﺷﺖ ﻣﮋﻩ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻓﺼﻞ ٧ﺑﺮﺟﺴﺘﻪﺗـﺮﻳﻦ ﻓﺼـﻞ ﻛﺘـﺎﺏ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍﺯ ﻛﺘﺐ ﻣﺸﺎﺑﻪ ﭘﻴﻮﻧﺪ ﻣﻮ ﺭﺍ ﻣﺘﻤﺎﻳﺰ ﻣﻲﻛﻨﺪ. ــــــ
)34.6 Skin Rejuvenation with skin filler (E.E.A. Derm
1998
35.6 Textbook of Dermatology (Sixth Editions) (R.H. CHAMPION, J.L. BURTON, D.A.BURNS, S.M.BREATHNACH) (ROOK) (Software c Gention I.T. Consuliants Ltd.,) Version 1.2.0 ﻭﻳﺮﺍﻳﺶ ﺷﺸﻢ ﻛﺘﺎﺏ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ Rookﺷﺎﻣﻞ ٤ﺟﻠﺪ ﻭ ٣٦٨٣ﺻﻔﺤﻪ ﻣﻲﺑﺎﺷﺪ ﺩﺭ ﺍﻳﻦ ﻭﻳﺮﺍﻳﺶ ﺗﻤﺎﻡ ﻓﺼﻞﻫﺎ ﻣﺮﻭﺭ ﺷﺪﻩ ﻭ ﺁﺧﺮﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺍﺿﺎﻓﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﻓﺼﻞﻫﺎ ﺑﺎﺯﻧﻮﻳﺴﻲ ﺷﺪﻩ ﻭ ﺩﺭ ﺣﺪﻭﺩ % ٢٥ -٣٠ﺭﻓﺮﺍﻧﺲﻫﺎ ﺟﺪﻳﺪ ﻣﻲﺑﺎﺷﻨﺪ.
CDﺣﺎﺿﺮ ،ﺭﻭﺵ ﺍﻧﺘﺨﺎﺏ ،ﺁﻧﺴﺘﺰﻱ ﻭ ﺗﺰﺭﻳﻖ Juvedermﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺍﻳﻦ ﻭﻳﺪﺋﻮ ،CDﻧﺤﻮﺓ ﺁﻧﺴﺘﺰﻱ ﺑﺪﻭﻥ ﺍﻳﻨﻜﻪ ﺁﻧﺎﺗﻮﻣﻲ ﻣﺤﻴﻂ ﻧﺎﺣﻴﻪ ﺗﺰﺭﻳﻖ ﺍﺯ ﺑﻴﻦ ﺑﺮﻭﺩ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺳﭙﺲ ﭘﺮﻛﺮﺩﻥ ﭼﻴﻦ ﻧﺎﺯﻭﺑﻴﺎﻝ ﺑﺎ Juvederm30ﻭ ﺳﭙﺲ ﺍﻓﺰﺍﻳﺶ ﺣﺠﻢ ﻟﺐ ﺑﺎ Juvederm24ﻭ ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﭼﺮﻭﻙﻫﺎﻱ ﻇﺮﻳﻒ ﺑﺎ Juvederm18ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ.
ﺩﺭ ﻫﺮ ﻓﺼﻞ ﺗﺼﺎﻭﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺳﺘﻔﺎﺩﻩﻛﻨﻨﺪﮔﺎﻥ ﺍﺯ CDﺍﻳﻦ ﻛﺘﺎﺏ ﻣﻲﺗﻮﺍﻧﻨﺪ ﺍﺯ ﻋﻜﺲﻫﺎﻱ ﻛﺘﺎﺏ ﺑﻪ ﻋﻨﻮﺍﻥ Slide Conferenceﺍﺳﺘﻔﺎﺩﻩ ﻧﻤﺎﻳﻨﺪ .ﻛﺘﺎﺏ ﺣﺎﺿﺮ ﺭﻓﺮﺍﻧﺲ ﺩﺳﺘﻴﺎﺭﻳﺎﻥ ﭘﻮﺳﺖ ﻭ Board certificationﻣﻲﺑﺎﺷﺪ. 2004 2000
2002
)36.6 Textbook of Dermatology (Rook's
)(Seven Edition) (Volume 1-4) (E-Book )37.6 Textbook of Pediatric Dermatology (JOHN HARPER ARNOLD ORANJE NEIL PROSE) (VOLUME 1 , 2 ﻛﺘﺎﺏ ﻓﻮﻕ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺩﺭ ﺧﺼﻮﺹ Pediatric dermatologyﺍﺳﺖ ﻛﻪ ﺩﺭ ﺍﻛﺜﺮ ﻛﺸﻮﺭﻫﺎ ﻳﻚ Subspecialityﺟﺪﺍﮔﺎﻧﻪ ﻣﻲﺑﺎﺷﺪ .ﻣﺆﻟﻔﻴﻦ ﺍﻳﻦ ﻛﺘﺎﺏ ﻳﻚ encyclopedic textﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﻼ ﻣﺸﺎﺑﻪ ﺑﻪ ﺭﻭﺵ ﻧﮕﺎﺭﺵ ﻛﺘﺎﺏ (RooK) text book of general dermatologyﻣﻲﺑﺎﺷﺪ. ﺍﻃﻔﺎﻝ ﺑﻪ ﻛﻤﻚ 185ﻣﺤﻘﻖ ﺍﺯ ﺳﺮﺍﺳﺮ ﺟﻬﺎﻥ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩﺍﻧﺪ ﻛﻪ ﺑﻪ ﻋﻨﻮﺍﻥ board cerificaitionﺩﺭ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺍﻃﻔﺎﻝ ﭘﺬﻳﺮﻓﺘﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺭﻭﺵ ﻧﮕﺎﺭﺵ ﻛﺘﺎﺏ ﻛﺎﻣ ﹰ ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ ﺑﺮ ﮔﻴﺮﻧﺪﺓ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺍﺯ ﺩﻭﺭﺓ ﭘﺮﻩﻧﺎﺗﺎﻝ ﺗﺎ adolescentﻣﻲﺑﺎﺷﺪ .ﻛﺘﺎﺏ ﻣﺸﺘﻤﻞ ﺑﺮ ٢٩ﻓﺼﻞ ﺑﻮﺩﻩ ﻛﻪ ﺷﺎﻣﻞ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺷﺎﻳﻊ ﻣﺎﻧﻨﺪ Psoriasisﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻧﺎﺩﺭ ﻣﻲﺑﺎﺷﺪ .ﻫﻤﭽﻨﻴﻦ ﺁﺧﺮﻳﻦ ﭘﻴﺸﺮﻓﺖ ﺩﺭ ﮊﻧﺘﻴﻚ ﻣﻠﻜﻮﻟﻲ ﻭ ﺭﻭﺵﻫـﺎﻱ ﺩﺭﻣـﺎﻧﻲ ﺩﺭ ﺍﻳـﻦ ﻛﺘﺎﺏ ﮔﻨﭽﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺑﺨﺶ ﻋﻔﻮﻧﻲ ﻛﺘﺎﺏ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﻧﺪﻣﻴﻚ ﻣﺎﻧﻨﺪ ﻟﭙﺮﻭﺯﻱ ﻭ ﻟﻴﺸﻤﺎﻧﻴﻮﺯ ﻭ ﺍﻧﺪﻣﻴﻚ ﺗﺮﭘﻮﻧﻮﻣﺎﺗﻮﺯ ﻭ ...ﻛﻪ ﺩﺭ ﻛﺘﺎﺏﻫﺎﻱ ﺩﺭﻣﺎﺗﻮﻟﻮﮊﻱ ﺩﻳﮕﺮ ﺑﻪ ﺍﺧﺘﺼﺎﺭ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ ﺗﻮﺳﻂ ﺍﻓﺮﺍﺩ ftrsthand knowledgeﺗﺤﺮﻳﺮ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺑﺨـﺶ ﻟﻴـﺰﺭ ﻛﺘﺎﺏ ﺍﺳﺘﻔﺎﺩﻩ ﻟﻴﺰﺭ ﺑﺮﺍﻱ ﺩﺭﻣﺎﻥ ﺿﺎﻳﻌﺎﺕ ﭘﻴﮕﻤﺎﻧﺘﻪ ﻭ ﻋﺮﻭﻗﻲ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺭﻭﺵﻫﺎﻱ Sedationﻭ ﺑﻴﻬﻮﺷﻲ ﺩﺭ ﺍﻃﻔﺎﻝ ﺩﺭ ﻓﺼﻞ Surgeryﻛﺘﺎﺏ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻓﺼﻞ Surgeryﺗﻜﻨﻴﻚﻫﺎﻱ ﺳﺎﺩﻩ ﻭ ﭘﻴﭽﻴﺪﺓ ﺟﺮﺍﺣـﻲ ﻣﺸـﺘﻤﻞ ﺑـﺮ tissue expansionﻭ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ،graftﻛﺸﺖ ﻛﺮﺍﺗﻴﻨﻮﺳﻴﺖﻫﺎ ،ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﻛﻠﻮﺋﻴﺪ ،ﺍﺳﻜﺎﺭ ﻭ ﺳﻮﺧﺘﮕﻲ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻣﺸﺨﺼﺔ ﻣﻨﺤﺼﺮ ﺑﻪ ﻓﺮﺩ ﻛﺘﺎﺏ ﻋﻜﺲﻫﺎﻱ ﻣﺘﻨﺎﺑﻪ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺑﻮﺩﻩ ﻛﻪ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺍﻃﻠﺲ ﭘﻮﺳﺖ ﺩﺭ Pediatric dermatologyﻛﺎﺭﺑﺮﺩ ﺩﺍﺭﺩ .ﻭ ﺑﻪ ﮔﻔﺘـﺔ ﻣﺆﻟﻔﻴﻦ ﺗﻼﺵ ﺯﻳﺎﺩ ﺷﺪﻩ ﻛﻪ ﺗﻈﺎﻫﺮﺍﺕ ﻣﺨﺘﻠﻒ ﭘﻮﺳﺘﻲ ﺩﺭ ﻧﮋﺍﺩﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺣﺪﺍﻗﻞ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺎﻳﻊ ﺟﻤﻊﺁﻭﺭﻱ ﮔﺮﺩﺩ. )(CD I , II A Systematic Approach The Aging Face (Calvin M. Johnson, Jr., Ramsey )Alsarraf 38.6 5. Closure 9. Closure -Closure
2002
4. The Procerus and frontalis 7. Fat Removal 8. The Skin Pinch
-Resuspension
-The Submental Region
CD I: y The Coronal Browlift: 1. Introduction 2. The Incision 3. The Corrugator Muscles y Blepharoplasty: 1. Uooer Lids 3. Marking and Incision 5. Skin and Muscle 2. Lower Lids 4. The Incision 6. Fant Removal CD II: -The Deep Plane Facelift -Marking and Incision -Skin Elevation -The Deep Plane
)39.6 Treatment of Skin Disease Comprehensive therapeutic Strategies (Mark G Lebwohl Warren R Heymann, John Berth-Jones, Ian Coulson) (SALEKAN E-BOOK) (MOSBY ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺣﺎﺿﺮ ﺷﺎﻣﻞ ﺍﻃﻠﺲ +ﺍﺳﺘﺮﺍﺗﮋﻱ ﺩﺭﻣﺎﻧﻲ +ﺩﺍﺭﻭﺩﺭﻣﺎﻧﻲ ﺑﻴﻤﺎﺭﻱ ﭘﻮﺳﺖ ﻣﻲﺑﺎﺷﺪ( ﻣﺸﻜﻞ ﺍﺻﻠﻲ ﭘﺰﺷﻜﺎﻥ ﺩﺭ ﻣﻮﺍﺟﻬﻪ ﺑﻪ ﻳﻚ ﺑﻴﻤﺎﺭﻱ ﺑﻌﺪ ﺍﺯ ﺗﺸﺨﻴﺺ managementﺑﻴﻤﺎﺭﻱ ﻣﻲﺑﺎﺷﺪ .ﭼﻪ ﺳﺆﺍﻻﺗﻲ ﺑﺎﻳﺪ ﺍﺯ ﺑﻴﻤﺎﺭ ﭘﺮﺳﻴﺪﻩ ﺷﻮﺩ ﻭ ﭼﻪ ﺁﺯﻣﺎﻳﺸﺎﺗﻲ ﺑﺎﻳﺪ ﺩﺭﺧﻮﺍﺳﺖ ﮔﺮﺩﺩ .ﻫﺮ ﻓﺼﻞ ﺍﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﻳﻚ ﺑﻴﻤﺎﺭﻱ )ﺑﻪ ﺗﺮﺗﻴﺐ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎ ﺑﺮﺍﻱ ﺩﺳﺘﻴﺎﺑﻲ ﺑﻪ ﺁﺳﺎﻥ ﺑﻪ ﺑﻴﻤﺎﺭﻱ( ﺑﻮﺩﻩ ﻭ ﻫﺮ ﻓﺼﻞ ﻭ ﺷﺎﻣﻞ: -٣ﺟﺪﻭﻝ ﺑﺮﺍﻱ ﺍﻳﻨﻜﻪ ﭘﺰﺷﻚ ﭼﻪ ﺁﺯﻣﺎﻳﺸﺎﺕ ﭘﺎﺭﺍﻛﻠﻴﻨﻴﻜﻲ ﺭﺍ ﺩﺭﺧﻮﺍﺳﺖ ﻛﻨﺪ )(specific investigations
-٢ﺍﺳﺘﺮﺍﮊﻱ ﺩﺭﻣﺎﻧﻲ) management strategyﺩﺭ ﺑﺎﻟﻴﻦ ﻭ ﻣﻌﺎﻳﻨﻪ ﻭ ﺷﺮﺡ ﺣﺎﻝ ﺑﺎﻳﺪ ﭼﻪ ﻧﻜﺎﺗﻲ ﺟﺴﺘﺠﻮ ﺷﻮﺩ( -١ﺧﻼﺻﻪﺍﻱ ﺍﺯ ﺑﻴﻤﺎﺭﻱ -٤ﺩﺭﻣﺎﻥ )ﺑﻪ ﺗﺮﺗﻴﺐ ﺧﻂ ﺍﻭﻝ ،ﺧﻂ ﺩﻭﻡ ،ﺧﻂ ﺳﻮﻡ ﺩﺭﻣﺎﻥ( ﻧﻜﺘﺔ ﻣﺘﻤﺎﻳﺰﻛﻨﻨﺪﻩ ﺍﻳﻦ ﻛﺘﺎﺏ ﻧﺴﺒﺖ ﺑﻪ ﻛﺘﺎﺏﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺩﻳﮕﺮ ﭘﻮﺳﺖ ﺍﻟﻮﻳﺖﺑﻨﺪﻱ ﺩﺭﻣﺎﻥ ﻣﻲﺑﺎﺷﺪ .ﺍﻳﻦ ﺍﻟﻮﻳﺖﺑﻨﺪﻱ ﺑﺮ ﺍﺳﺎﺱ evidence-Basedﻣﻲﺑﺎﺷﺪ ﻭ ﺍﻟﻮﻳﺖ ﺑﺮ ﺍﺳﺎﺱ ﻧﻮﻉ ﻣﻄﺎﻟﻌﺎﺕ ﺍﻧﺠﺎﻡﺷـﺪﻩ ﺩﺭ ﻣﻘﺎﻻﺕ ﺍﺯ A-Eﻧﺎﻡﮔﺬﺍﺭﻱ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻪ ﻋﻨﻮﺍﻥ ﻣﺜﺎﻝ ﺩﺭ ﺩﺭﻣﺎﻥ ﺁﻛﻨﻪ ﺍﺗﺮﻭﮊﺳﻦﻫﺎﻱ ﺧﻮﺭﺍﻛﻲ ) (Aﻭ ﺍﺳﭙﻴﺮﻭﻧﻮﺍﺭﻛﺘﻮﻥ ) (Bﻧﺎﻡﮔﺬﺍﺭﻱ ﺷﺪﻩ ﻛﻪ ) (Aﻣﺸﺨﺼﻪ ) (double blind studyﺑﻮﺩﻩ ﻭ ) (Bﻣﺸﺨﺼﻪ ) (Clinical trialﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﭘﺰﺷﻚ ﻛﻤـﻚ ﻣـﻲﻛﻨـﺪ ﺗـﺎ ﺑﺘﻮﺍﻧﺪ ﺍﺭﺯﺵ ﺩﺍﺭﻭﺩﺭﻣﺎﻧﻲ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﻧﻮﻉ ﻣﻄﺎﻟﻌﻪ ﺑﻴﺎﻥ ﻛﻨﺪ .ﺳﭙﺲ ﺧﻼﺻﻪ ﻣﻘﺎﻻﺕ ﺩﺭ ﺍﺩﺍﻣﻪ ﺩﺭﻣﺎﻥ ﺫﻛﺮ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ٢١٣ﺑﻴﻤﺎﺭﻱ ﻫﻤﺮﺍﻩ ﺑﺎ ﻋﻜﺲﻫﺎﻱ ﻛﺎﻣ ﹰ ﻼ ﺭﻧﮕﻲ ﻣﻲﺑﺎﺷﺪ. )(Jean Carruthers, Alastair Carruthers
2003 ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ:
40.6 USING BOTULINUM TOXINS COSMETICALLY
MID and Lower Face Perioal Rhytides
Periorbitalarea Infraorbital Orbicularis Oculi
Horizontal Forehead Lines
Introduction
MID and Lower Face Nasalis
MID and Lower Face Perioral Rhytides
Periorbitalarea Lateral Orbital Wrinkles
Brow Injections Brow Lift
Cervical Injections Horizontal Necklace Lines
MID and Lower Face Mouthe Frown and Mentalis
Acknowledgemetns
Cervical Injections Vertical Platysmal Bands
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
35 ﺍﺭﺗﻮﭘﺪﻱ-٧
CD ﻋﻨﻮﺍﻥ 1.7
A New Generation in Cemented Hip Design (VCD) (Part I , II) (David S. Hungerford, Clayton R. Perry) Segment I: Core Decomtpression
2.7 3.7
Segment II: Trauma Case Studies: Retrograde Femoral Nailing
LCP system Description Implants and instruments Application Indications Operating techniques
LCP cases Humerus Forearm Pelvis and acetabulum Femur Tibia Periprosthetic
AO Principles of Fracture Management (Thomas P. Ruedi, William M. Murphy) (CD I , II)
5.7
Atlas of Orthopaedics Surgery (Disk 1-6)
1- AO philosophy and Its basis
2- Decision making and planning
2002
Literature and studies Related Literature Study results
4.7
7.7
2001
AO Image Collection AO Principles of fracture Management (T.P. Ruedi, W.M. Murphy) AO International AO Teaching Series-LCP (Thomas P. Ruedi, Prof. Michael Wagner) Foreword-Basics Methods of osteosynthesis AO Principles Biomechanical Principles Surgical techniques
6.7
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــــ
3- Reduction and fixation techniques
2001 4- Specific fractures
5- General topics
6- Complications
Disk 1: Condylar Plate Fixation in the Distal Femur, Malleolar Fracture Fixation, Malleolar Fracture Type B, Malleolar Fracture Type C, Tension Band Wiring on the Elbow Femoral Neck Rfacture Large Cannulated System, Fracture of the Radius Shaft 3.5 LC-DCP, Screw Fixation and Plating Disk 2: Techniques of Absolute Stability, Proximal Humerus Fracture, Reduction with Clamps, Posterior Wall Fracture, Posteror + Transverse Wall Fracture, Undeamed Tibial Nail (UTN), Intraaticular Fracture of the Distal Humerus Disk 3: Fracture of the Tibiaplateau, Tibia Fracture in Foarm LEG UTN, Reduction Techniq, The Undeamed Femoral Nail System, Dynamic Condylar Screw (DCS), Dynamic Hip Screw (DHS), Pilon Tibial Fractures (Foamed Foot) Disk 4: Application of Large Distractor, AO Asif External Fixator, PC-FIX Point Contact Fixator an Internal Biologicl, The Proximal Femoral Nail (PFN), Bicondylar Fracture of Tibia Plateau, Minimal Invasive Plating of the Tibia Disk 5: Direct and Indirect Reduction Techniques, Short Oblique Radius Fracture, Small External Fixator, Intraarticular Fracture Distal Radius, Distal Radius, Open Reduction & Fractures of the Calcaneus, Postoperative Treatment, Internal Fixation of a Humeral Shaft Fracture Disk 6: High Cinematography of a Butterfly Fracture, Posterior, Pelvic Fixations Symphysis Pubis & Pubic Rami, Pelvic Fixations, Anterior Plate Fixation 53028, The Pelvic C-Clamp, Liss Less Invasive Stabilization System, LCP Locking Compression Plate
Body in Motion (Susan K. Hillman) -Anatomy -Content -Everything -Anatomy Text
2003
-Surface Anatomy Videos -Muscle Aciton Videos
CCC (Core Curriculum in Primary Care) Orthopedics/Sport Medicine Section 1- Introduction
2- Orthopedic Procedures: A Rheumatology's Perspective
3- Xercise and Aging A Prescripton for life
ــــــ
4- Foot and Ankle Problems Part Two
ــــــ
8.7
Click'X VenttoFix SynCage (J. Webb, O. Schwarzenbach J. Thalgott) (VCD) (AO ASIF OFFICIAL TAPE)
ــــــ
9.7
FRACTURES IN ADULTS (ROCKWOOD AND GREEN'S)
ــــــ
1- General Principles
2- Upper Extremity
3- Spine
4- Lower Extremity
10.7 FRACTURES IN CHILDREN General Principlse Upper Extremity Spine Lower Extremity (ROCKWOOD AND WILKINS) (James H. Beaty, James R. Kasser)
ــــــ
11.7 FRACTURES OF THE PELVIS AND ACETABULUM (G.F. Zinghi, A. Briccoli, P.Bungaro)
ــــــ
(Salekan E-Book)
12.7 Gait Analysis an introduction (Third Edition) An interactive multi-media presentation produced using polygon software (Micheal W. Whittle)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
36 ___
33.1 Imaging of Spinal Trauma in Children (Lawrence R. Kuhns, M.D.) (University of Michigan Medical Center) Principles AND TECHNIQUES Normal Spine Variants and Anatomy Mechanisms and Patterns of Injury Thoracic Spine Injuries
13.7
Interactive orthopaedics and Sport Medicine
Epidemiology Measurements Occipitocervical Injuries
ATLAS OF SPINAL INJURIES IN CHILDREN Cervcal Spine Lumbar Spine Thoracic Spine Sacrococcygeal Spine Lumbar
Special Views and Techniques Experimental and Necropsy Data Sacral Injuries
1. Interactive Spine 2. Interactive Hand 3. Interactive hand therapy 4. Interactive Hip 5. Interactive Shoulder 6. Interactive Knee 7. Sports Injuries The Knee 8. Interactive Food and Ankle 9. Interactve Skeleton
ــــــ
14.7 Internal Fixation of a Humeral Shaft Fracture with the UHN -Technical Information
-Operation
-Postoperative Concept
ــــــ
(P.M.Rommens, J. Blum)
-Poat-op –X-ray control
- Poat-op treatment
15.7 MASTER TECHNIQUES IN ORTHOPAEDIC SURGERY RECONSTRUCTIVE KNEE SURGERY Southern California Center for Sports Medicine Long Beach, California (DOUGLAS W. JACKSON, M.D.)
ــــــ
: ﺷﺎﻣﻞCD ﻣﺒﺎﺣﺚ ﺍﻳﻦ. ﻣﻄﺎﻟﺐ ﺩﺭ ﺁﻥ ﻣﻲﺑﺎﺷﺪserch ﺑﻮﺩﻩ ﻭ ﻗﺎﺑﻠﻴﺖTEXT ﮔﺮﺩﻳﺪﻩ ﻭ ﺷﺎﻣﻞ ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﻛﺘﺎﺏ ﺑﻪ ﺻﻮﺭﺕebook ﻛﻪ ﺷﺎﻣﻞ ﻛﻞ ﻣﺘﻦ ﻛﺘﺎﺏ ﻓﻮﻕﺍﻟﺬﻛﺮ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪCD ﺍﻳﻦ PART IV INTRAARTICULAR FRACTURES OF THE TIBIA AND PATELLA
Operating Room Environment
Arthroscopic Management of Intraarticular Tibial Fractures Arthroscopically-Assisted Fixation of Patella Fractures Open Reduction Internal Fixation of Intraarticular Fractures of the Tibia
PART I EXTENSOR MECHANISM PATELLOFEMORAL PROBLEMS
Arthroscopic Lateral Release of the Patella with Electrocautery Anteromedial Tibial Tubercle Transfer Patellectomy PART II MENISCUS SURGERY
PART V ARTICULAR CARTILAGE AND SYNOVIUM
Meniscus Repair: The Outside-In Technique Meniscus Repair: The Inside-Out Technique Meniscus Repair: The All-Inside Arthroscopic Technique
Arthroscopic Chondroplasty Osteochondritis Dissecans Arthroscopic Synovectomy
PART III LIGAMENT INJURIES AND INSTABILITY
Anterior Cruciate Ligament Reconstruction Arthroscope-Assisted Posterior Cruciate Ligament Repair/Reconstruction Posterolateral Corner Collateral Ligament Reconstruction Surgical Technique for Knee Dislocations High Tibial Osteotomy in Knees with Associated Chronic Ligament Deficiencies
35.1 Magnetic Resonance Imaging in Orthopedics and Sport Medicine (David W. Stoller) MRI ﺗﻬﻴﺔ ﺗﺼﺎﻭﻳﺮ-١ ﺟﻬﺖ ﺳﻴﺴﺘﻢ ﻣﻮﺳﻜﻮﻟﻮﺍﺳﻜﻠﺘﺎﻝEcho-Planar ﺍﺻﻮﻝ ﺗﺼﻮﻳﺮﺳﺎﺯﻱ-٢ ﺯﺍﻧﻮ-٣ ﺁﺭﻧﺞ-٤ Kinematic MRI -٥
MRI ﺍﺛﺮﺍﺕ ﺑﻴﻮﻟﻮﮊﻳﻚ ﻭ ﺍﻳﻤﻨﻲ ﺩﺭ-٦ ﻋﻀﺮﻭﻑ ﻣﻔﺼﻠﻲ ﻭ ﺩﮊﻧﺮﺍﺳﻴﻮﻥ ﻋﻀﺮﻭﻓﻲMRI -٧ ﻣﭻ ﭘﺎ ﻭ ﭘﺎ-٨ ﻣﭻ ﺩﺳﺖ ﻭ ﺩﺳﺖ-٩ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ-١٠
: ﺩﺭ ﺍﺭﺗﻮﭘﺪﻱ ﻭ ﻃﺐ ﻭﺭﺯﺵ ﻣﻲﺑﺎﺷﺪ ﻭ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺍﺳﺖMRI ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻛﺎﺭﺑﺮﺩ ﺳﻪﺑﻌﺪﻱMRI ﺗﻜﻨﻴﻚ ﺑﺎﺯﺳﺎﺯﻱ ﺟﻬﺖ-١١ (Hip) ﻣﻔﺼﻞ ﺭﺍﻥ-١٢ ﺷﺎﻧﻪ-١٣ (TMJ) ﻣﻔﺼﻞ ﻛﻤﭙﻮﺭﻭﻣﺎﻧﺪﻳﺒﻮﻻﺭ-١٤ ﺍﺯ ﻣﻐﺰ ﺍﺳﺘﺨﻮﺍﻥMRI ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ-١٥
(VCD) (Video-Atelier Othmar Keel AG) -CCA - Straight Shaft -CCE -Vault Pan -CCB -Socket -CBC Stem -RM Cup
ــــــ
ﺗﻮﻣﻮﺭﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻥ ﻭ ﺑﺎﻓﺖ ﻧﺮﻡ-١٦ ﺁﺳﻴﺒﻬﺎﻱ ﻋﻀﻼﻧﻲMRI -١٧
16.7 MATHYS ORTHOPAEDICS
ــــــ
17.7 MATHYS-ORTHOPAEDICS HIP PROSTHESES (VCD)
ــــــ
1. Cemented Stem-CCA
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
2. Cemented Cup-CCB
3. Cementless Steam-CBC
4. Cementless Cup-RM Cup
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
37 (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins)
18.7 Operative Arthroscopy
2003
Shoulder: Arthroscopic Cuff Repair: -Mssive U-Shaped Tear: Subscapulais, Infraspinatus and Biceps (Stephen S. Burkhar, MD San Antonio, Texas) -Partial: Repair of Oartial Articular Sufrace Rotator Cuff Tear (Stephen S. Burkhar, MD San Antonio, Texas), San Antonio, Texas Slap Lesions: -Arthroscopic Repair of the Slap Lesion (Stephen S. Burkhar, MD San Antonio, Texas) 19.7 Operative Arthroscopy (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins)
2003
Hip: Southern Sport Medicine & Orthopaedic Center Operative Hip Arthroscopy: -Dense Soft Tissue Envelope -Constrained Ball and Socket Anatomy 20.7 Operative Arthroscopy (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins)
2003
-Thick Capsule, Limited Compliance
Ankle: Ankle Arthroscopy (James Tasto M.D.) - Ankle & Subtalar Arthroscopy Operative Arthroscopy (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins) 21.7
2003
Wrist: Wrist Arthroscopy (Robert Richards MD FRCSC) -Portal Markings -Establishing the 3/4 Portal -Radiocarpal Arthroscopy Carpal Tunnel Release 22.7 Operative Arthroscopy (Third Edition) (John B. McGinty) (Lippincot, Williams & Wilkins)
2003
Knee (CD-1): Arthroscopic meniscal repair: -suture repair -implantable fixation Knee (CD-2): -ACL -Complex articular surface injuries -Fractures -Patellofemoral 23.7 Operative Arthroscopy (SECOND EDITION) (John B. McGinty)
ــــــ
1- Basic Principles
2- The Knee
24.7 Operative Orthopaedics
3- The Shoulder
4- The Elbow
5- The Wrist
6- The Foot and Ankle
7- The Temporomandibular Joint
8- The Spine
9- The Hip
1999
(Ninth Edition) (CAMPBELL'S) (S. TERRY CANALE) . ﭼﺎﭖ ﺑﺎ ﺗﻤﺎﻣﻲ ﺗﺼﺎﻭﻳﺮ ﻣﺮﺗﺒﻂ ﺑﺎ ﻛﺘﺎﺏ ﻣﻲﺑﺎﺷﺪSerch ﻛﺎﻣﻞ ﻛﺘﺎﺏ ﻛﻤﭙﻞ ﺍﺭﺗﻮﭘﺪﻱ ﻣﻲﺑﺎﺷﺪ ﻭ ﻗﺎﺑﻠﻴﺖTEXT ﺷﺎﻣﻞCD ﺍﻳﻦ
2003
25.7 OPERATIVE ORTHOPAEDICS (CAMPBELL'S)
: ﺷﺎﻣﻞCD ﻛﺘﺎﺏ ﻛﻤﭙﻞ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻓﻴﻠﻢﻫﺎﻱ ﺍﻳﻦTEXT ﺷﺎﻣﻞ ﻋﻤﻞﻫﺎﻱ ﺟﺮﺍﺣﻲ ﻣﺮﺗﺒﻂ ﺑﺎCD ﺍﻳﻦ Trochanteric osteotomy-hip revision Reconstruction nailing femoral fracture Anterior Cervical discectomy & fusion
Arthroscopic assisted ACL reconstruction Chevron osteotomy hallux valgus
Screw fixation SCFE Ligament balancing Knee arthroplasty
Intramedullary nailing forearm fracture ORIF calconeal fracture
2002
26.7 ORTHOPAEDIC SURGERY (Third Edition) (CHAPMAN) - Surgical Principles and Techniques - Sport Medicine - Skeletal Disorders
- Fractures, Dislocations, Nonunions and Malunions - Neoplastic, Infectious - The Spine
- The Hand - Neurologic and Other - Pediatric Disorders
- The Foot - Joint Reconstruction, Arthritis, and Arthroplasty
27.7 OPERATIVE ORTHOPAEDICS
(CAMPBELL'S) (Tenth Edition) (Volume 1-4) (E-Book) (S. Terry Canale, MD) 28.7 PEDIATRIC ORTHOPAEDICS (Lovell and Winter's) (Fifth edition) (Salekan E-Book) (Volume II) KYPHOSIS
THE UPPER LIMB
SPONDYLOLYSIS AND SPONDYLOLISTHESIS
DEVELOPMENTAL HIP DYSPLASIA AND DISLOCATION
THE CERVICAL SPINE
LEGG-CALVE-PERTHES SYNDROME
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
2003 2001
SLIPPED CAPITAL FEMORAL EPIPHYSIS DEVELOPMENTAL COXA VARA, TRANSIENT SYNOVITIS, AND IDIOPATHIC CHONDROLYSIS OF THE HIP THE LOWER EXTREMITY
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
38 LEG LENGTH DISCREPANCY SPORTS MEDICINE IN CHILDREN AND ADOLESCENTS
THE FOOT MANAGEMENT OF FRACTURES
THE LIMB-DEFICIENT CHILD THE ROLE OF THE ORTHOPAEDICS IN CHILD ABUSE
29.7 Photographic manual of Regional Orthopaedic and Neurological Tests
ــــ
. ﻓﺼﻮﻝ ﺑﺮ ﺍﺳﺎﺱ ﻣﺤﻞ ﻣﻮﺭﺩ ﻣﻌﺎﻳﻨﻪ ﻃﺮﺍﺣﻲ ﻭ ﻗﺴﻤﺖﺑﻨﺪﻱ ﺷﺪﻩﺍﻧـﺪ. ﺩﺭ ﻣﻮﺍﻗﻊ ﻟﺰﻭﻡ ﺗﺼﺎﻭﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻚ ﺿﺮﻭﺭﻱ ﻧﻴﺰ ﺍﺿﺎﻓﻪ ﺷﺪﻩﺍﻧﺪ. ﺗﺼﻮﻳﺮ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﺗﻤﺎﻡ ﻣﻌﺎﻳﻨﺎﺕ ﻧﻮﺭﻭﻟﻮﮊﻳﻚ ﻭ ﺍﺭﺗﻮﭘﺪﻳﻚ ﺭﺍ ﺑﺎ ﺟﺰﺋﻴﺎﺕ ﺗﻤﺎﻡ ﺭﻭﺷﻦ ﻣﻲﺳﺎﺯﺩ٨٥٠ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯCD ﺍﻳﻦ ﺩﺭ ﺿـﻤﻦ ﻳـﻚ. ﺩﺭ ﻳﻚ ﺻﻔﺤﻪ ﻳﺎ ﺩﻭ ﺻﻔﺤﻪ ﻣﻘﺎﺑﻞ ﻫﻢ ﺑﺎ ﻋﻜﺲﻫﺎﻳﻲ ﻛﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻣﻌﺎﻳﻨـﻪ ﺭﺍ ﺑﻮﺿـﻮﺡ ﻧﺸـﺎﻥ ﻣـﻲﺩﻫﻨـﺪ ﺗﻮﺿـﻴﺢ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖTest ﻫﺮ.ﻣﻌﺎﻳﻨﺎﺕ ﺍﺯ ﻓﻘﺮﺍﺕ ﮔﺮﺩﻧﻲ ﻭ ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ ﺷﺮﻭﻉ ﻭ ﺑﻪ ﻓﻘﺮﺍﺕ ﻛﻤﺮﻱ ﻭ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺗﺤﺘﺎﻧﻲ ﺧﺘﻢ ﻣﻲﺷﻮﻧﺪ . ﺍﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺩﺭ ﺑﻜﺎﺭﮔﻴﺮﻱ ﺗﺴﺖﻫﺎﻱ ﺣﺴﺎﺳﺘﺮ ﻭ ﺍﺧﺘﺼﺎﺹﺗﺮ ﻛﻤﻚ ﻓﺮﺍﻭﺍﻥ ﺑﻪ ﭘﺰﺷﻚ ﻣﻲﻧﻤﺎﻳﺪ. ﻧﻴﺰ ﺑﺮﺍﻱ ﻫﺮ ﻣﻌﺎﻳﻨﻪ ﺗﻌﺮﻳﻒ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻣﻴﺰﺍﻥ ﺣﺴﺎﺳﻴﺖ ﻭ ﻗﺎﺑﻠﻴﺖ ﺍﻋﺘﻤﺎﺩ ﺑﻪ ﺁﻥ ﻣﻌﺎﻳﻨﻪ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﺳﺎﺯﺩSensitivity/Relialility Scale 45.1 Radiology imaging Bank:
1. Section
2. History
Orthopeadic 3. Findings 4. Diagnosis
5. Images
6. Classification
30.7
Range of Motion-AO Neutral-O Method
31.7
SPINE (VCD 1-A) (J. o' Dowd, P. Moulin, E. Morscher P. Moutin, J. Webb, M. Aebi)
7. Imagenumber ــــــ ــــــ
Pedicie Identification (Conultant: J. O'Dowd)
Cervical Spine Locking Plate: Corporectomy C6 (P. Moulin)
CS-Titanium Locking Plate (E. Morscher P.Moutin)
Cervical Spine Locking Plate (P. Moulin)
Cervical Spine Locking Plate Vertebrectomy C6 (J. Webb, M. Aebi) Posterior Cervical Plate Fixation ( C2-T1) ( j.wEBB, M.Aebi)
Posterior Plating Technique C6 to T1 (J. Webb, M.Aebi)
32.7 SPINE (VCD 1-B) (M. Aebi, J. Webb, Ghr. Ulrich, J. Nothwang, B. Jeanneret, M. Aebi J. Webb, J. Webb, M. Aebi P. Bryne) AnteriorFixation of the Dens with Cannulated Screws ( M. Aebi, J. Webb Ghr. Ulrich, J. Nothwang) Cervix: Fixation C3-C7 in Presenceb of a Laminectomy ( B. Jeanneret) U.S.S: Lumbar Degenrrative Scotiosis Side-Opening Pedicte Screws (M.Aebi J.Webb)
U.S.S: Lumbosacral Stabilisation: Back-Opening Pedicte Screws (M. Aebi J. Webb) USS: Lumbosacral Fusion Sacral Implants (J. Webb M.Aebi P.Bryne)
33.7 SPINE (VCD 1-C) (J. Webb, M. Aebi, G.Wisner, J. Webb M. Aebi, J. Webb M. Aebi, J. O'Dowd) USS: Lumbosacral Stabilisation Side Opening Pedicle Screws (J.Webb, M.Aebi, G. Winsner)
Universal Spine System Thoraco - Lumbar Fractures (J. Webb M. Aebi)
ــــــ Universal Spine System:
Right Thoracic Scoliosis: Side Opening hooks & Screws (J.Webb, M.Aebi, J.O'Dowd)
34.7 SPINE (VCD 1-D) (J. Webb, O. Schwarzenbach, J. Thalgott & J. Webb, J. Webb) Click'X (J.Webb)
ــــــ
The Snterior Rod System (J.Thalgott & J.Webb)
35.7 SPINE implants
ــــــ
Contact Fusion Cage (J.Webb)
(CD I , II)
ــــ . ﻧﺤﻮﺓ ﺟﺮﺍﺣﻲ ﻭ ﺑﻪﻛﺎﺭﮔﺬﺍﺷﺘﻦ ﭘﺮﻭﺗﺰﻫﺎﻱ ﻣﻬﺮﻩ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺍﻃﻼﻋﺎﺕ ﻛﺎﻣﻠﻲ ﺭﺍﺟﻊ ﺑﻪ ﭘﺮﻭﺗﺰﻫﺎﻱ ﺟﺎﻧﺸﻴﻦ ﺟﺴﻢ ﻣﻬﺮﻩ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩCD ﺩﺭ ﺍﻳﻦ: CD I . ﺑﺮ ﺭﻭﻱ ﻣﻬﺮﻩﻫﺎﻱ ﻛﻤﺮﻱ ﺩﺭ ﺩﺭﻣﺎﻥ ﻣﻮﺍﺭﺩ ﺗﺮﻭﻣﺎﺗﻴﻚ ﻭ ﺍﺳﻜﻮﺍﻧﻴﻮﺭ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩDiapasone-hook ﻧﺤﻮﻩ ﺟﺮﺍﺣﻲ ﻭ ﺑﻜﺎﺭﮔﺬﺍﺷﺘﻦ ﺩﺳﺘﮕﺎﻩCD ﺩﺭ ﺍﻳﻦ: CD II 1999
36.7 Surgery of the Foot and Ankle (Michael J. Coughlin, Roger A. Mann) Volume One: 1. General Considerations
2. The forefoot
Volume Two: 1. Miscellaneous Disorders
2. Sports Medicine
37.7 Surgery of the Knee
3. Postural Disorders 3. Pediatrics
4. Neurologic Disorders
5. Arthritic Conditions
4. Trauma
2001
(Third Edition) (John N. Insall, W. Norman Scott)
1- VIDEO
2- PHOTOS
3- ILLUSTRATIONS
- Anatomy
-Anatomical Aberrations
4- 3D KNEE
-Biomechanics
-Imaging
5-IMAGING -Surgical Approaches
38.7 The Adult Hip On CD
ــــــ
39.7 The Shoulder (2
ــــــ
nd
Edition) (Rockwood and Matsen)
1- Disorders of the Acromiocavicular Joint
40.7 The Unreamed Femoral Nail System
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
2- Disorders of the Sternoclavicular Joint
3- Glenohumeral Instability
(N. Sudkamp P. Duwelius)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
4- Glenohumeral Arthritis and Its Management
ــــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
41.7 Video Collection Labor for Experimental Orthopaedics Surgery
VCD 1-A
( R Texhammar,
ــــــ
P Holzach)
AO/ASIF Instrumentation Care and Maintenance
VCD 1-B
39 AO/ASIF VCD (CD 1-10)
PreOperative Preparation of the Patient
Approaches to the Femur, Pelvis Knee and Elbow
(P Matter M.D., S.M. Perren, B Noesberger)
Approach to the Proximal Femur and Elbow
After-Care Following Lower Leg Surgery
Dynamic Compression Unit
Approaches to the Upper Limb
Reduction Techniques
DCP 4.5 Compression Tibial Shaft
VCD 1-C (B Noesberger, J.Stadler, P. Holzach, Th. Ruedi) DCP 4.5 Butterss Tibial Plateau
LC-DCP 4.5 for the Distal Tbia
DCP 3.5 Radius Shaft 3.5 LC-DCP
DCP 4.5 Neutralization Plate of a Spiral Fracture
Fracture of the Radius Shaft 3.5 LC-DCP with Shaft screws
VCD 2-A (S.M. Perren, K.M. Pfeiffer M.D.)
. Correctional Osteotomy (dist. Radius)
. Basic Lag Screw Techniques . Internal Fixation of a Closed Butterfly Fracture of Right Tibia (Operation Video)
VCD 2-B (Th. Ruedi, J. Mast M.D., P.E Ochsner) Fracture of the Lateral Tibiaplateau Pilon Fracture
Indirect Reduction and Plate Fixation of a Pilon Fracture Malleolar fracture Type A
Malleolar Fracture Type B Malleolar Fracture Type C
VCD 2-C (T.Ruedi, P.Holzach, Th. Ruedi M. Schuler, P. Hozach, P Regazzoni, Th. Ruedi M.D.) Proximal Humerus Fracture Distal Humerus Fracture Type C 1.3
VCD 3-A
Tension Band Wiring of the Elbow Dynamic Hip Screw
Intaarticular Type C Fracture of the Distal Humerus Dynamic Condylar Screw (DCS) Proximal Femur
Condylar Plate Fixation in the Distal Femur
(R. Ganz R.P. Jakob P.Koch, Th Ruedi M.D., P.Regazzoni)
Condylar Plate Proximal Femur
Large Cannulated Screw System
AO/ASIF External Fixator
VCD 3-B Small External Fixator Distractor Handling Consultant Seija Pearson
VCD 3-C
Using the Small Air Drill Compact Air Drive Basic Operating Procedure & Working with attachments Intramedullary Nailing with the AO/ASIF Universal Femoral Nail
(R. Frigg, D. Hontzsch, Th. Ruedi)
The Interlocking of the Universal Femoral Intramedullary Nail Opening Procedure of the Tibial Cavity for Intramedullary Nailing The Universal Tibial Nail
VCD4
AO Universal Femoral Nail With Distractor
Intramedullary Nailing of the Tibia Intramedullary Nailing of the Tibia with a Pseudarthrosis Mid-Shaft Tibial Fracture Locked Universal Nail
(R. Frigg, Ch. Krettek)
UTN Unreamed Tibial Nail
Distal Aiming Device for UTN
ﭼﺸﻢﭘﺰﺷﻜﻲ-٨
CD ﻋﻨﻮﺍﻥ 1.8
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
Atlas of Clinical Oncology Tumors of the Eye and Ocular Adnexa (American Cancer Society) (Devron H. Char, MD)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2001
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
40
ﺍﻳﻦ CDﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: 4- ORBITAL TUMORS
3- RETINAL AND OPTIC NERVEHEAD TUMORS
2- UVEAL AND INTRAOCULAR TUMORS
1- LID AND CONJUNCTIVAL TUMORS
ــــ
)ATLAS OF OPHTALMOLOGY (RICHARD K. PARRISG II) (CD I , II) (Mosby
2.8
ــــ
)ATLAS OF OPHTHALOMOLGY (SUE FORDRONALD MARSH) (Mosby ﻼ ﻣﻌﻠﻮﻡ ﻭ ﻣﺸﺨﺺ ﺑﻮﺩﻩ ،ﻣﻄﺎﻟﻌﺔ ﻛﺘﺐ textﺑﺪﻭﻥ ﻫﻤﺮﺍﻫﻲ ﺍﻃﻠﺲﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﺗﺄﺛﻴﺮ ﻭ ﻛﺎﺭﺁﺋﻲ ﻻﺯﻡ ﺭﺍ ﻧﺨﻮﺍﻫﺪ ﺩﺍﺷﺖCD .ﻫﺎﻱ ﺫﻳﻞ ﻛﻪ ﺣﺎﻭﻱ ﻣﻌﺘﺒﺮﺗـﺮﻳﻦ ﻭ ﺷـﻨﺎﺧﺘﻪﺷـﺪﻩﺗـﺮﻳﻦ ﺍﺭﺯﺵ ﻳﻚ ﺍﻃﻠﺲ ﺧﻮﺏ ﺩﺭ ﺗﻤﺎﻣﻲ ﺷﺎﺧﻪﻫﺎﻱ ﻋﻠﻢ ﭘﺰﺷﻜﻲ ﺧﺼﻮﺻﹰﺎ ﭼﺸﻢﭘﺰﺷﻜﻲ ﻛﺎﻣ ﹰ ﺍﻃﻠﺲﻫﺎﻱ ﭼﺸﻢﭘﺰﺷﻜﻲ ﻣﻲﺑﺎﺷﻨﺪ ،ﻋﻼﻭﻩ ﺑﺮ ﺗﻮﺍﻧﺎﺋﻲ ﺑﺰﺭﮔﻨﻤﺎﻳﻲ ﺗﺼﺎﻭﻳﺮ ﺗﺎ ﭼﻨﺪﻳﻦ ﺑﺮﺍﺑﺮ ﺑﺪﻭﻥ ﻛﺎﺳﺘﻪﺷﺪﻥ ﺍﺯ ﻛﻴﻔﻴﺖ ﺑﻲﻧﻈﻴﺮ ﺁﻥ ﺩﺍﺭﺍﻱ ﻗﺎﺑﻠﻴﺖ Searchﻭ ﺟﺴﺘﺠﻮﻱ Caseﻣﻮﺭﺩ ﻧﻈﺮ ﺩﺭ ﻛﻤﺘﺮﻳﻦ ﺯﻣﺎﻥ ﻣﻤﻜﻦ ﻣﻲﺑﺎﺷﻨﺪ .ﺩﺭ ﻛﻨﺎﺭﺩﺍﺷﺘﻦ ﺍﻳـﻦ ﺍﻃﻠـﺲﻫـﺎ ﭼـﻪ ﺑـﻪ ﻫﻨﮕـﺎﻡ ﺁﻣﻮﺯﺵ ﻭ ﻳﺎﺩﮔﻴﺮﻱ ﺩﺭ ﺩﻭﺭﺓ ﺩﺳﺘﻴﺎﺭﻱ ﻭ ﭼﻪ ﺑﻪ ﻫﻨﮕﺎﻡ Practiceﻭ ﻣﻮﺍﺟﻪ ﺑﻪ Caseﻫﺎﻱ ﻧﺴﺒﺘﹰﺎ ﻧﺎﺩﺭ ﺩﺭ ﻛﻠﻴﻨﻴﻚ ﺑﺴﻴﺎﺭ ﻣﻔﻴﺪ ﻭ ﻛﻤﻚﻛﻨﻨﺪﻩ ﺧﻮﺍﻫﺪ ﺑﻮﺩ.
3.8
)Basic and Clinical Science Course Retina and Vitreous (Section 12) (American Academy of Ophthalmology
4.8
ــــ
Basic Ophthalmology Physiology of the Eye )OPHTHALMOLOGY (Myron Yanoff.Jay S. Duker) (Mosby ﺍﻳﻦ CD ٣ﺑﻪ ﺗﻮﺿﻴﺢ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﭼﺸﻢ ﻭ ﺭﺍﻫﻬﺎﻱ ﺑﻴﻨﺎﺋﻲ ،ﻣﻜﺎﻧﻴﺴﻢ ﻋﻴﻮﺏ ﺍﻧﻜﺴﺎﺭﻱ ﻭ ﻧﻴﺰ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭼﺸﻢ ﺩﺭ ﺳﻄﺢ ﻧﻴﺎﺯ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﭘﺰﺷﻜﻲ ،ﭘﺰﺷﻜﺎﻥ ﻋﻤﻮﻣﻲ ﻭ ﭘﺰﺷﻜﺎﻥ ﻣﺘﺨﺼﺺ ﺩﺭ ﺳﺎﻳﺮ ﺭﺷﺘﻪﻫﺎﻱ ﭘﺰﺷﻜﻲ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺩﻳﺪﻥ ﺍﺷﻜﺎﻝ ﺷﻤﺎﺗﻴﻚ ﺯﻳﺒﺎ ﻭ ﻧﻴﺰ ﺗﺼﺎﻭﻳﺮ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﺨﺘﻠﻒ ﭼﺸﻤﻲ ﻣﻮﺟﻮﺩ ﺩﺭ ﺍﻳﻦ CDﻫﺎ ﺑﺮﺍﻱ ﻣﺘﺨﺼﺼﻴﻦ ﻣﺤﺘﺮﻡ ﭼﺸﻢﭘﺰﺷﻜﻲ ﻧﻴﺰ ﺧﺎﻟﻲ ﺍﺯ ﻟﻄﻒ ﻧﺨﻮﺍﻫﺪ ﺑﻮﺩ
5.8
ــــ
Clinical update course on Retina
2003
)(SALEKAN E-BOOK
6.8 7.8 8.8
CDﻓﻮﻕ ﺍﺯ ﺳﺮﻱ CDﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ (Lifelong education for the ophthalmologist) LEOﻣﺘﻌﻠﻖ ﺑﻪ ﺁﻛﺎﺩﻣﻲ ﭼﺸﻢﭘﺰﺷﻜﻲ ﺁﻣﺮﻳﻜﺎ ) (AAOﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ Lecture ١٥ﻭ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ،ﻣﺮﻭﺭﻱ ﺩﺍﺭﺩ ﺑﺮ ﺟﺪﻳﺪﺗﺮﻳﻦ ﻣﺘﺪﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺩﺭ ﻓﻴﻠـﺪ ﻭ ﺗﻴـﺮﻩ ﻭ ﺭﺗﻴﻦ .ﺍﺯ ﺟﻤﻠﻪ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ CDﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺷﻴﻮﻩﻫﺎﻱ ﺩﺭﻣﺎﻥ endophthalmitis ،macular hole ،BRVO ،DR ،AMDﻭ ...ﺍﺷﺎﺭﻩ ﻧﻤﻮﺩ. ــــ
)Clinical Update Course on Neuro-ophthalmology (Peter J. Savino, MD, Steven E. Feldon. MD, Barrett Katz, MD, Thmas L. Slamovits, MD ﺍﻳﻦ CDﺑﻪ ﻣﻌﺮﻓﻲ ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﮔﻠﻮﻛﻮﻡ ﻭ ﺁﺧﺮﻳﻦ ﭘﻴﺸﺮﻓﺖﻫﺎﻱ ﺣﺎﺻﻠﻪ ﺩﺭ ﺁﻧﻬﺎ ﻣﻲﭘﺮﺩﺍﺯﺩ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ Lecture ٩ﺍﺯ ﺍﺳﺘﺎﺩﺍﻥ ﺻﺎﺣﺐﻧﺎﻡ ﺍﻳﻦ ﺭﺷﺘﻪ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺯ ﺟﻤﻠﻪ ﻣﺒﺎﺣـﺚ ﻣﻬـﻢ ﺁﻣـﻮﺯﺵ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺩﺭ ﺍﻳـﻦ CDﻣـﻲﺗـﻮﺍﻥ ﺑـﻪ LTP ،Perimetryﻭ CPCﺍﺷﺎﺭﻩ ﻧﻤﻮﺩ.
ــــ
1999
)(SALEKAN E-BOOK
9.8
10.8 Complications in Phacoemulsification
ﺑﻪ ﻗﻠﻢ ﺑﺮﺟﺴﺘﻪﺗﺮﻳﻦ phacosurgenﻫﺎﻱ ﺣﺎﻝ ﺣﺎﺿﺮ ﺩﺭ ﺩﻧﻴﺎ ﻣﻦﺟﻤﻠﻪ … , H. Gimbel ، H. Fineﺗﻤﺎﻣﹰﺎ ﺑﻪ ﺗﻮﺿﻴﺢ ﺗﻜﻨﻴﻜﻬﺎﻱ ﻣﺨﺘﻠﻒ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ، Phacoﻋﻮﺍﺭﺽ ﺍﺣﺘﻤﺎﻟﻲ ،ﺷﻴﻮﺓ ﺗﺸﺨﻴﺺ ﺑﻪ ﻣﻮﻗﻊ ﻭ ﭼﮕﻮﻧﮕﻲ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺁﻧﻬﺎ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺍﺷﻜﺎﻝ ﺷـﻤﺎﺗﻴﻚ ﻭ ﺗﺼﺎﻭﻳﺮ ﺭﻧﮕﻲ ﺁﻥ ﺩﺭ ﺩﺭﻙ ﻣﻜﺎﻧﺴﻢ ﻭ ﻋﻠﺖ ﺑﺮﻭﺯ ﻋﻮﺍﺭﺽ ﻭ ﭼﮕﻮﻧﮕﻲ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﻧﻴﺰ managementﺁﻥﻫﺎ ﺑﺴﻴﺎﺭ ﻛﻤﻚﻛﻨﻨﺪﻩ ﻭ ﺩﺭ ﻧﻮﻉ ﺧﻮﺩ ﺑﻲﻧﻈﻴﺮ ﺍﺳﺖ. )11.8 CONTACT LENS COMPLICATIONS Efron Grading Morphs For the clinical assessment of contact lens complications (NATHAN EFRON, PHILIP MORGAN ﺍﻳﻦ CDﻋﻮﺍﺭﺽ ﻣﺨﺘﻠﻒ ﻧﺎﺷﻲ ﺍﺯ ﻛﺎﺭﺑﺮﺩ ﻟﻨﺰﻫﺎﻱ ﺗﻤﺎﺳﻲ ﻭ ﭼﮕﻮﻧﮕﻲ ﭘﻴﺸﺮﻓﺖ ﻭ ﺳﻴﺮ ﺁﻧﻬﺎ ﺭﺍ ﺑﻪ ﺻﻮﺭﺗﻲ ﺑﺴﻴﺎﺭ ﺯﻳﺒـﺎ ﻭ ﺑﻴﺎﺩﻣﺎﻧـﺪﻧﻲ ﻧﻤـﺎﻳﺶ ﻣـﻲﺩﻫـﺪ ﺑﻄﻮﺭﻳﻜـﻪ ﺗﺸـﺨﻴﺺ ﻭ Gradingﻋﻮﺍﺭﺿـﻲ ﭼـﻮﻥ microcystes ،epithelial polymegethism
، epithelial
papillary conjunctivitisﻭ ...ﻣﻴﺴﺮ ﻣﻲﮔﺮﺩﺩ. )12.8 Dodick Laser Photolysis (Ultra Small Incision Cataract Surgery) (Jack M. Dodik
ــــ
Journal of Cataract & Refractive Surgery Surgical Cases Provided by Photolysis System Manufacturer
2000
Department of Clinical Ophthalmology Institute of Ophthalmology University College London
)(Hamish MA Towler, Julian A Patterson, Susan Lightman
13.8 Diabetes And The Eye
ﺍﻳﻦ CDﺁﻣﻮﺯﺵ ﺟﺎﻣﻌﻲ ﺍﺯ ﻣﻘﻮﻟﺔ diabetic retinopathyﺍﺭﺍﺋﻪ ﻣﻲﻧﻤﺎﻳﺪ .ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﻣﻦﺟﻤﻠﻪ Fluorescein angiographyﻭ ﺑﺎﻻﺧﺮﻩ ﻟﻴﺰﺭﺗﺮﺍﭘﻲ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻣﻬـﻢ ﺑـﻪ ﻛﻤـﻚ ﻋﻜـﺲ ﻭ textﺁﻣـﻮﺯﺵ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖ. ﻫﻤﭽﻨﻴﻦ CDﻣﺬﻛﻮﺭ ﺩﺍﺭﺍﻱ ﻗﺎﺑﻠﻴﺖ Seff-testﺍﺯ ﻣﻄﺎﻟﺐ ﻣﻮﺟﻮﺩ ﺩﺭ ﺁﻥ ﻣﻲﺑﺎﺷﺪ. 2000
)14.8 DICTIONARY OF VISUAL SCIENCE AND RELATED CLINICAL TERMS (Henry W. Hofstetter, John R. Griffin, Morris S. Berman, Ronald W. Everson
2004
)15.8 Duane’s Ophthalmology (Foundations of clinical Ophthalmology) (LIPPINCOTT-RAVEN
ــــ
)(CD I , II
ــــ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
)(David I. Silbert, MD FAAP
16.8 Endoscopic Dacryocystorhinostomy (DCR) Advantages and Indications
Welch Allyn Institute of Interactive Learning ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
17.8 EENT
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
41 18.8 Endoscopic Laser Assisted Lacrimal Surgery (Russel S. Gonnering, MD) (VCD)
ــــ
. ﻓﻮﺍﻳﺪ ﺁﻥ ﺭﺍ ﺑﺮﺭﺳﻲ ﻣﻲﻧﻤﺎﻳﺪ، ﺑﻪ ﺁﻣﻮﺯﺵ ﺍﻳﻦ ﺷﻴﻮﻩ ﻛﻤﺘﺮ ﺗﻬﺎﺟﻤﻲ ﺩﺭ ﺟﺮﺍﺣﻲ ﻣﺠﺎﺭﻱ ﺍﺷﻜﻲ ﭘﺮﺩﺍﺧﺘﻪVCD ﺍﻳﻦ. ﺑﺤﺚﻫﺎﻱ ﺯﻳﺎﺩﻱ ﺑﺮﺍﻧﮕﻴﺨﺘﻪ ﻭ ﻣﺨﺎﻟﻔﺎﻥ ﻭ ﻣﻮﺍﻓﻘﺎﻥ ﺯﻳﺎﺩﻱ ﺩﺍﺭﺩendoscopic laser ﺟﺮﺍﺣﻲ ﺳﻴﺴﺘﻢ ﻻﻛﺮﻳﻤﺎﻝ ﺑﻪ ﻛﻤﻚ ﺗﻜﻨﻴﻚ ﻧﺴﺒﺘﹰﺎ ﺟﺪﻳﺪ Enucleation Techniques With MEDPOR Orbital Implant MCP Placement in a Vascularized MEDPOR Implant (VCD) (Charles N. S. Soparker, Peter A. D.) 19.8 Natural Movement For Artificial Eyes With MEDPOR Biomaterial Orbit Implants ans the MEDPOR MPC Motility Coupling Post (VCD) (POREX) 20.8 Orbital Floor reconstruction using MEDPOR surgical implants 21.8 ﺁﻥ ﻭ ﻗـﺮﺍﺭﺩﺍﺩﻥ ﭘﺮﻭﺗـﺰdrilling ﻭ ﺩﺭ ﺍﻧﺘﻬﺎﺏ ﺑﻪMEDPOR ﺳﭙﺲ ﺑﻪ ﻃﺮﻳﻘﺔ ﻛﺎﺷﺖ ﺍﻳﻤﭙﻼﻧﺖ،enucleation ﺍﻭﻝ ﺍﺑﺘﺪﺍ ﺑﻪ ﺭﻭﺵﻫﺎﻱCD ٢ . ﺭﺍ ﺩﺭ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺗﺮﻣﻴﻤﻲ ﺍﺭﺑﻴﺖ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﻨﺪMEDPOR ﻓﻮﻕ ﻣﺠﻤﻮﻋﹰﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻛﺎﺷﺖ ﺍﻳﻤﭙﻼﻧﺘﻬﺎﻱVCD
ــــ
٣
. ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩMEDPOR Surgical implant ﺳﻮﻡ ﭼﮕﻮﻧﮕﻲ ﺗﺮﻣﻴﻢ ﻭ ﺑﺎﺯﺳﺎﺯﻱ ﺩﻓﻜﺖﻫﺎﻱ ﻛﻒ ﺍﺭﺑﻴﺖ ﺑﻪ ﻛﻤﻚCD ﻗﺎﺑﻞ ﻗﺒﻮﻝ ﺁﻥ ﺭﺍ ﻧﻤﺎﻳﺶ ﻣﻲﺩﻫﺪ ﺩﺭMotility ﻣﻲﭘﺮﺩﺍﺯﺩ ﻭMCP ﻭimplant ﻣﺮﺑﻮﻃﻪ ﺭﻭﻱ ﻣﺠﻤﻮﻋﺔ 16.2 Facial Plastic & Reconstructive Surgery
(Terence M. Davidson, MD) (VCD I , II) FUNDAMENTALS OF CORMEAL TOPOGRAPHY 22.8 ﻫﺎﻱ ﺍﺣﺘﻤﺎﻟﻲ ﻭ ﻧﻴﺰ ﺳﻴﺮ ﺗﻐﻴﻴﺮﺍﺕ ﺗﻮﭘﻮﮔﺮﺍﻓﻲ ﻭ ﺣﺎﻻﺕ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﺨﺘﻠـﻒ ﻗﺮﻧﻴـﻪartefact ، ﺍﻧﻮﺍﻉ ﻣﻮﺍﺭﺩ ﻃﺒﻴﻌﻲ ﻭ ﻏﻴﺮﻃﺒﻴﻌﻲ، ﻧﺤﻮﺓ ﺗﻔﺴﻴﺮ ﺗﻮﭘﻮﮔﺮﺍﻓﻲ ﻗﺮﻧﻴﻪ، ﻣﻜﺎﻧﻴﺴﻢ ﻭ ﭼﮕﻮﻧﮕﻲ ﻋﻤﻠﻜﺮﺩ ﺩﺳﺘﮕﺎﻩ. ﺟﻤﻌﹰﺎ ﺁﻣﻮﺯﺵ ﻛﺎﻣﻠﻲ ﺍﺯ ﺗﻮﭘﻮﮔﺮﺍﻓﻲ ﻗﺮﻧﻴﻪ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﻨﺪCD ﺍﻳﻦ ﺩﻭ . ﺗﻮﺻﻴﻪ ﻣﻲﺷﻮﺩOSCE ﻋﻼﻭﻩ ﺑﺮ ﻛﺎﺭﺑﺮﺩ ﻛﻠﻴﻨﻴﻜﻲ ﺁﻥ ﺟﻬﺖ ﺷﺮﻛﺖ ﺩﺭ ﺍﻣﺘﺤﺎﻧﺎﺕCD ﺑﻬﺮﻩﮔﻴﺮﻱ ﺍﺯ ﺍﻳﻦ ﺩﻭ.ﺑﻄﻮﺭ ﺟﺎﻣﻊ ﻭ ﻗﺎﺑﻞ ﺍﺳﺘﻔﺎﺩﻩﺍﻱ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ
ــــــ ــــ
23.8 Glaucoma Basic and Clinical Science Course (Section 10)
2003
(Salekan E-Book)
2000
25.8 26.8 27.8 28.8 29.8 30.8 31.8 32.8
Cataract & Refractive Sugery
24.8 Hereditary Retinal Dystrophies (Ulrich Kellner, Markus Ladewing, Christoph Heinrich)
Highlights Highlights Highlights Highlights Highlights Highlights Highlights Highlights
of of of of of of of of
the the the the the the the the
ASCRS ASCRS ASCRS ASCRS ASCRS ASCRS ASCRS ASCRS
1995 1996 1997 1998 1999 2000 2001 2003
Annual Annual Annual Annual Annual Annual Annual Annual
Meeting Meeting Meeting Meeting Meeting Meeting Meeting Meeting
، I.Howard Fine ﺍﺯ ﺑﺮﺟﺴـــﺘﻪﺗـــﺮﻳﻦ ﺍﺳـــﺎﺗﻴﺪ ﻣﺎﻧﻨـــﺪCataract & refractive Surgury ﺩﺭ ﺑـــﺎﺏLecture ﻫــﺎﻱ ﻣﻘﺎﺑـــﻞ ﺣـــﺎﻭﻱ ﺩﻫﻬـــﺎCD ﺁﺧـﺮﻳﻦ، ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻛﻤﻚ ﻓـﻴﻠﻢ ﺟﺮﺍﺣـﻲﻫـﺎﻱ ﺍﻧﺠـﺎﻡﺷـﺪﻩ ﺗﻮﺳـﻂ ﺍﻳـﻦ ﺍﺳـﺘﺎﺩﺍﻥ... ﻭRobert J. Cionni ، Roger F. Steinert، Douglas D. Koch ﻫـﺎﻱCD ﻣﺠﻤﻮﻋـﻪ. ﺭﺍ ﺁﻣـﻮﺯﺵ ﻣـﻲﺩﻫـﺪPRK ﻭLASIK ﻭ ﻧﻴﺰ ﺟﺮﺍﺣﻲ ﻛﺮﺍﺗﻮﺭﻓﺮﺍﻛﺘﻴﻮ ﺷـﺎﻣﻞPhacoemulsification ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺑﺮﻭﺵ . ﻭ ﭼﻪ ﺟﻬﺖ ﺑﻪ ﺭﻭﺯﺩﺭﺁﻭﺭﺩﻥ ﺍﻃﻼﻋﺎﺕ ﻭ ﻣﻬﺎﺭﺕﻫﺎﻱ ﻗﺒﻠﻲ ﻣﻲﺑﺎﺷﺪLASIK ﻭPhaco ﭼﻪ ﺑﻪ ﻣﻨﻈﻮﺭ ﺁﻣﻮﺯﺵ ﺍﻭﻟﻴﺔ،ﻣﺬﻛﻮﺭ ﺑﻪ ﻣﻨﺰﻟﺔ ﻛﺎﺭﮔﺎﻩ ﺁﻣﻮﺯﺷﻲ ﺍﺭﺯﺷﻤﻨﺪﻱ
33.8 Highlights of the XVIIth Congress of the ESCRS VIENNA'99
(EUROPEAN SOCIETY OF CATARACT & REFRACTIVE SURGEONS)
ــــ
34.8 Highlights of the XVIIth Congress of the ESCRS VIENNA'99
(EUROPEAN SOCIETY OF CATARACT & REFRACTIVE SURGEONS)
ــــ
1. Intrastromal Corneal Rings
2. Multifocal IOLs
3. Cataract Technidues
35.8 Illustrated Tutorials Clinical Ophthalmology
4. LASIK: Muopia & Mixed Astigmatism
5. Phakic IOLs
(Jack J Kansski, Anne Bolton)
ــــ
36.8 Implantation of AcryFlex Foldable Lens (Surgery Performed by Dr. Jagdeep M Kakadla) (VCD)
ــــ
37.8 IMPLANTE MEDPOR MANDIBULAR (VCD), (AJL OPHTHALMIC, S.A.)
ــــ
38.8 IMPROVING SUCCESS IN FILTRATION SURGERY American Academy of Ophthalmology (BRADFORD J. SHINGLETON)
ــــ
ﻫﻤﭽﻨﻴﻦ ﺑﻪ ﻣﻌﺮﻓﻲ ﺩﻭ ﺷﻴﻮﺓ ﺟﺪﻳـﺪ ﺩﺭﻣـﺎﻥ ﺟﺮﺍﺣـﻲCD ﺍﻳﻦ. ﻣﻲﺑﺎﺷﺪ ﻭ ﺟﺰﺋﻴﺎﺕ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺭﻭﺵﻫﺎ ﺭﺍ ﺑﺎ ﻛﻤﻚ ﻓﻴﻠﻢﻫﺎﻱ ﺗﻬﻴﻪﺷﺪﻩ ﺍﺯ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﻣﺮﺑﻮﻃﻪ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﺪFilstratioh Surgery ﻳﻚ ﺩﻭﺭﺓ ﻛﺎﻣﻞ ﺁﻣﻮﺯﺷﻲ ﺩﺭ ﻣﻮﺭﺩ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺨﺘﻠﻒCD ﺍﻳﻦ . ﻣﻲﭘﺮﺩﺍﺯﺩViscocanalostomy ﻭDeep Sclerectomy ﺑﻴﻤﺎﺭﺍﻥ ﮔﻠﻮﻛﻮﻣﻲ ﻳﻌﻨﻲ 2000
th 39.8 Incomitant Deviatons (4 edition) a supplement chapter 17 of Pickwell's Binocular Vision Anomalies
ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻋﻼﻭﻩ ﺑﺮ ﺗﻮﺿﻴﺢ ﻭ ﺗﺸﺮﻳﺢ... ﻭBrown's ، Duane's ﻭ ﻧﻴﺰ ﺳﻨﺪﺭﻡﻫﺎﻱrectus ﻭ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
oblique ﻛﻢﻛﺎﺭﻱ ﻭ ﻓﻠﺞ ﻋﻀﻼﺕ، ﻣﻦﺟﻤﻠﻪ ﭘﺮﻛﺎﺭﻱComitant ﻣﺠﻤﻮﻋﻪﺍﻱ ﻛﻢﻧﻈﻴﺮ ﺟﻬﺖ ﻛﻤﻚ ﺑﻪ ﺩﺭﻙ ﺑﻬﺘﺮ ﻭ ﻋﻤﻴﻖﺗﺮ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﺍﻧﺤﺮﺍﻓﺎﺕ ﭼﺸﻤﻲCD
ﺍﻳﻦ . ﺑﻪ ﺻﻮﺭﺕ ﻓﻴﻠﻢ ﺑﺮﺍﻱ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺁﻧﻬﺎ ﻣﻲﭘﺮﺩﺍﺯﺩCase ﻃﺒﻘﻪﺑﻨﺪﻱ ﻭ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﻫﺮ ﻧﻮﻉ ﺍﻧﺤﺮﺍﻑ ﺑﻪ ﻣﻌﺮﻓﻲ ﭼﻨﺪﻳﻦ، ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ،ﻣﻜﺎﻧﻴﺴﻢ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
42 40.8 Intraocular Inflammation and Uveitis
(Section 9)
2003
(SALEKAN E-BOOK)
41.8 LEO Clinical Update Course on Retina (H. Michael Lambert, Charles. Arr, J. Paul Diechert, Mark W. Johnson, James S. Tiedeman)
ــــ
42.8 LEO Clinical Update Course on Cataract (Stephen S. Lane, MD, Alan S. Candall, MD, Douglas D. Koch, MD, Roger F. Steinert, MD)
ــــ
43.8 LEO Clinical Update Course on Pediatric Ophthalmology and Strabismus THE AMERICAN ACADEMY OF OPHTHALMOLOGY (American Academy of Ophthalmology)
ﻫﻤﺮﺍﻩ ﺑﺎ ﺍﺳﻼﻳﺪ ﻭ ﻓﻴﻢ ﺁﻣﻮﺯﺷـﻲ ﺍﺯ ﺍﺳـﺘﺎﺩﺍﻥ ﻣﻌﺮﻭﻓـﻲ ﻫﻤﭽـﻮﻥLecture ١٣ ( ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺷﺎﻣﻞAAO) ( ﻣﺘﻌﻠﻖ ﺑﻪ ﺁﻛﺎﺩﻣﻲ ﭼﺸﻢﭘﺰﺷﻜﻲ ﺁﻣﺮﻳﻜﺎLifelong education for the ophthalmologist)LEO ﻫﺎﻱ ﺍﺭﺯﺷﻤﻨﺪ ﻭ ﻣﻌﺘﺒﺮCD ﻓﻮﻕ ﺍﺯ ﺳﺮﻱCD . ﺍﻧﺴﺪﺍﺩ ﻣﺠﺮﺍﻱ ﺍﺷﻜﻲ ﻣﺎﺩﺭﺯﺍﺩﻱ ﻭ ﻫﻤﭽﻨﻴﻦ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﺍﻧﺤﺮﺍﻓﺎﺕ ﭼﺸﻤﻲ ﻭ ﺭﻭﺵﻫﺎﻱ ﺩﺭﻣﺎﻥ ﺁﻧﻬﺎ ﺍﺷﺎﺭﻩ ﻛﺮﺩ،ROP ، ﮔﻠﻮﻛﻮﻡ ﻭ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺍﻃﻔﺎﻝ، ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺁﻣﺒﻠﻴﻮﭘﻲCD ﺍﺯ ﺳﺮﻱ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ. ﺍﺳﺖM.X.Repka ﻭK.W.Wright Loeil Prental Endoscopie du Vitre Phaco Chop (VIDEO Media) (Roussat B. Choukroun J, Boscher C, Lebuisson DA, Amar R, Escalas P) 44.8 : ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ - Reconnaissance des structures oculaires - Lors des echographies prenatales - Possibilites et limites actuelles Roussat B, Choukroun J (Paris)
- Anatomie endoscopique normale et Pathologique de la base du vitre anterieur Boscher C, Lebuisson DA, Amar R (paris)
2000
2003
- Le Phaco Chop: Pour que les noyaux durs deviennet un plaisir Escalas P (Nantes)
45.8 MOVIMIENTQ NATURAL PARA EL OJO ARTIFICIAL (VCD), (AJL OPHTHALMIC, S.A.)
ــــ
46.8 MVP VIDEO JOURNAL OF OPHTHALMOLOGY
ــــ
47.8 New England Eye Center Imaging in Glaucoma
ــــ
. ﻭ ﻧﻴﺰ ﺑﻴﻮﻣﻴﻜﺮﻭﺳﻜﻮﭘﻲ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﺪ ﺍﺷﺎﺭﻩ ﻛﺮﺩOCT ،SLO ﺍﺯ ﺟﻤﻠﺔ ﺍﻳﻦ ﺭﻭﺵﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﻲﺗﻮﺍﻥ ﺑﻪ. ﺑﺎ ﺗﻮﺟﻪ ﻭﻳﮋﻩ ﺑﻪ ﻛﺎﺭﺑﺮﺩ ﺁﻧﻬﺎ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥ ﮔﻠﻮﻛﻮﻣﻲ ﻣﻲﭘﺮﺩﺍﺯﺩOptic nerve ﻓﻮﻕ ﺑﻪ ﻣﻌﺮﻓﻲ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺭﺗﻴﻦ ﻭCD 48.8 New England Eye Center Photorefractive Keratectomy (PRK) Course (Helen K. WU, MD, Roger F. Steinert, MD, Michael B. Raizman, MD)
ﺍﺯ ﻣﺸﺨﺼﺎﺕ ﻟﻴﺰﺭ ﺑﻪ ﻛﺎﺭPRK ﻣﻲﺑﺎﺷﺪ ﻛﻠﻴﺔ ﻣﺴﺎﺋﻞ ﻭ ﻣﺒﺎﺣﺚRoger F. Steinert ﻛﻪ ﻋﻤﺪﺗﹰﺎ ﺍﺯ ﺩﻛﺘﺮLecture ١٥ ﺑﻪ ﺷﻤﺎﺭ ﻣﻲﺭﻭﺩ ﻛﻪ ﺍﺯ ﻃﺮﻳﻖPRK ﺗﻬﻴﻪ ﻭ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﺩﺭ ﻭﺍﻗﻊ ﻳﻚ ﻛﺎﺭﮔﺎﻩ ﺁﻣﻮﺯﺷﻲNew England ﻓﻮﻕ ﻛﻪ ﺗﻮﺳﻂ ﻣﺮﻛﺰ ﭼﺸﻢﭘﺰﺷﻜﻲCD . ﺗﺎ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻋﻤﻞ ﻭ ﺑﺎﻻﺧﺮﻩ ﻋﻮﺍﺭﺽ ﺍﺣﺘﻤﺎﻟﻲ ﻭ ﺭﺍﻩﻫﺎﻱ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﺩﺭﻣﺎﻥ ﺁﻧﻬﺎ ﺭﺍ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﺍﺳﺖPatient sclection ﺭﻓﺘﻪ 49.8 OCULAR PATHOLOGY (FIFTH EDITION) (MYRON YANOFF, MD AND BEN S. FINE, MD) (Mosby) (SALEKAN E-BOOK) Basic Principles of Pathology Congenital Anomalies Cornea and Sclera Neural (Sensory) Retina Orbit Ocular Melanotic Tumors
Surgical and Nonsurgical Trauma Nongranulomatous Inflammation: Uveltis, Endophthalmitis, Panophthalmitis, and Sequelae Granulomatous Inflammation. Uvea Vitreous Diabetes Mellitus Retinoblastoma and Pseudoglioma
50.8 Ophthalmic Lenses & Dispensing
ــــ
2002
Skin and Lacrimal Drainage System Conjunctive Lens Optid Nerve Glaucoma
(Mo JALIE)
ــــ
. ﺟﺰﺋﻴﺎﺕ ﻭ ﻧﻜﺎﺕ ﻣﺮﺑﻮﻁ ﺑﻪ ﺗﺠﻮﻳﺰ ﻟﻨﺰ ﻭ ﭘﺮﻳﺴﻢ ﺟﻬﺖ ﺍﺻﻼﺡ ﻋﻴﻮﺏ ﺍﻧﻜﺴﺎﺭﻱ ﻭ ﺍﻧﺤﺮﺍﻓﺎﺕ ﭼﺸﻤﻲ ﺭﺍ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ، ﭘﺮﺩﺍﺧﺘﻪRefraction ﻭOptic ﻓﻮﻕ ﺍﺯ ﻃﺮﻳﻖ ﺗﺼﺎﻭﻳﺮ ﺷﻤﺎﺗﻴﻚ ﺑﻪ ﺁﻣﻮﺯﺵ ﻣﻔﺎﻫﻴﻢ ﭘﺎﻳﻪ ﻭ ﻛﺎﺭﺑﺮﺩﻱCD 51.8 Ophthalmic Surgery: principles and Techniques (BLACKWELL SCIENCE) (SALEKAN E-BOOK)
ــــ
52.8 Ophthalmology A multimedia tutorial for Primary care physicians and medical students (Robert Johnston FRCOpth, Jonathan Boulton MA MRCP FRCOpth)
ــــ
53.8 Orbital Floor Reconstruction Using Medpor Surgical Implant
ــــ
(Joseph M. Serletti, MD, Paul Manson, MD) (VCD)
54.8 PHACO TODAY
(The Latest Development in Phacomulsification and Small Incision Cataract Surgery) (HOWARD FINE, MD) ﺍﺷـﻜﺎﻝ. ﺭﺍ ﺁﻣﻮﺯﺵ ﻣـﻲﺩﻫـﺪphacoemulsfication ﻭIncisions ،Anesthesin ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺪﻳﺪ، ﺍﻳﺮﺍﺩﺷﺪﻩ ﺍﺳﺖ ﺳﻴﺮ ﺟﺮﺍﺣﻲ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺑﻪ ﺭﻭﺵ ﻓﻴﻜﻮ ﺭﺍ ﻣﺮﻭﺭ ﻛﺮﺩﻩI. Howard Fine ﻭ ﺍﺳﻼﻳﺪ ﻛﻪ ﻋﻤﺪﺗﹰﺎ ﺗﻮﺳﻂLecture ١٤ ﺩﺭ ﻗﺎﻟﺐCD ﺍﻳﻦ ﺗﻚ .ﺷﻤﺎﺗﻴﻚ ﻭ ﺗﺼﺎﻭﻳﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺩﺭ ﺁﻥ ﺑﻪ ﺩﺭﻙ ﺑﻬﺘﺮ ﻣﻜﺎﻧﻴﺴﻢﻫﺎ ﻭ ﺗﻜﻨﻴﻜﻬﺎﻱ ﺟﺮﺍﺣﻲ ﺩﺭ ﻓﻴﻜﻮ ﻛﻤﻚ ﺯﻳﺎﺩﻱ ﻣﻲﻧﻤﺎﻳﺪ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
43 55.8 PhcoChop (Mastering Techniques, Optimizing Technology, and Avoiding Complications) David F. Chang CD-1: Hydrodissection Pearls CD-2: Learning Phacochop CD-3: Phacodynamic Principles for PhacoChop, Vertical Chop and Cold Phaco for Brunescent Nuclel CD-4: Strategles for PC Rupture with Nucleus Present, Bimanual Chop for Cataracts with Large Zonular Defects
2004
56.8 Phacoemyulsification Cataract Surgery (Multimedia Oculosurgical Module) (Robert M. Schertzer, David X. Pang, MSE, Luanna R. Bartholomew, PhD) (Mosby) "Scleral tunnel"
ــــ
ﺑـﻪ ﻣﺜﺎﺑـﺔ ﻛﺎﺭﮔـﺎﻩ ﺁﻣﻮﺯﺷـﻲ ﻛـﻢﻧﻈﻴـﺮﻱ ﺩﺭ ﺯﻣﻴﻨـﺔ ﺟﺮﺍﺣـﻲ ﻛﺎﺗﺎﺭﺍﻛـﺖ ﺑـﺮﻭﺵCD ﺍﻳـﻦ. ﻣـﻲﺑﺎﺷـﺪMosby ( ﻣﺘﻌﻠـﻖ ﺑـﻪ ﺍﻧﺘﺸـﺎﺭﺍﺕMultimedia Oulosurgical Module) MOM ﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﻌـﺮﻭﻑ ﻭ ﻣﻌﺘﺒـﺮCD ﻓﻮﻕ ﺍﺯ ﺳﺮﻱCD
. ﻛﻠﻴﻪ ﻣﺮﺍﺣﻞ ﻋﻤﻞ ﺭﺍ ﺑﻪ ﺻﻮﺭﺗﻲ ﻛﺎﻣ ﹰﻼ ﻛﺎﺭﺑﺮﺩﻱ ﻭ ﻗﺎﺑﻞ ﺍﺳﺘﻔﺎﺩﻩ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﺪtext ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ ﻓﻴﻠﻢ ﻭphacoemulsification 57.8 Physiology of the Eye
Anatomy of the Eye 3-D Tour of the Eye Development of Vision Physics of Light & Color Illusions & Your Vision 58.8 Practical Viewing of the Optic Disc (KATHLEEN B. DIGRE, M.D., JAMES J. CORBETT, M.D. Getting Ready-Preparing to View the Opic Disc
What Should I Look for in the Normal Fundus?
Is the Disc Swollen?
Common Eye Conditions 2003
: ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ Is the Disc Pale?
Amaurosis Fugax and Not So Fugax-Vaxcular Disorders of the Eye
White Spots-What Are They?
Hemorrhage
Pigment
What is That in the Retina?
Macula
Practical Viewing in Children
What to Look for in the Aging
Viewing the Disc in Pregnancy
Practical Viewing of the Optic Disc and Retina in the Emergency Department
59.8 PROVISION INTERACTIVE: Clinical Case Studies (AAO) (Thomas A. Weingeist, MD., ph, D)
ــــ
60.8 RECONSTRUCCIÓN DE BASE ORBITAL CON IMPLANTE MEDPOR (VCD), (AJL OPHTHALMIC, S.A.)
ــــ
61.8 Refractive Surgery First interactive Symposium (Marguerite B. McDonald, MD)
ــــ
(American Academy of Ophthalmology)
Roger F. Steinert ،،Jack T. Holladay : ﺍﺯ ﺍﺳﺘﺎﺩﺍﻥ ﺻﺎﺣﺐﻧﺎﻡ ﺍﻳﻦ ﺭﺷﺘﻪ ﻣﻦﺟﻤﻠﻪLecture ﺍﺳﺖ ﻛﻪ ﺩﺭﺑﺮﮔﻴﺮﻧﺪﺓ ﺩﻫﻬﺎManus C. Kraff ﺑﻪ ﺳﺮﭘﺮﺳﺘﻲ ﺩﻛﺘﺮASCRS ﺗﻬﻴﻪ ﺷﺪﻩ ﺍﺯ ﺍﻭﻟﻴﻦ ﺳﻤﭙﻮﺯﻳﻮﻡ ﺟﺮﺍﺣﻲ ﺭﻓﺮﺍﻛﺘﻴﻮ ﺍﻧﺠﻤﻦCD
.PRK ﻭLASIK ،phacoemulsification
ﻓﻮﻕ ﻳﻜﻲ ﺍﺯ ﻣﺠﻤﻮﻋﺔ ﺩﻭCD ﻣﺠﻤﻮﻋﺔ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﺑﻪ ﻫﻤﺮﺍﻩ ﻓﻴﻠﻢ ﻭ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺍﻳﻦ ﻣﺠﻤﻮﻋﻪ ﻣﺮﻭﺭﻱ ﺩﺍﺭﺩ ﺑﺮ ﺍﺧﺮﻳﻦ ﻭ ﺟﺪﻳﺪﺗﺮﻳﻦ ﭘﻴﺸﺮﻓﺖﻫﺎ ﺩﺭ ﺯﻣﻴﻨﺔ ﺟﺮﺍﺣﻲ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺑﻪ ﺭﻭﺵ. ﻣﻲﺑﺎﺷﺪ... ﻭ ــــ
62.8 Refractive Surgery in the new millennium. 63.8 Evolution in LASIK 64.8
LASIK: Customized Ablations and Quality of Vision ﺗﺎ ﺗﻜﻨﻴﻚPatient Selection ﺑﻪ ﺷﻤﺎﺭ ﻣﻲﺭﻭﺩ ﻭ ﺷﺎﻣﻞ ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﺍﺯ ﻣﻌﺎﻳﻨﺎﺕ ﻣﻘﺪﻣﺎﺗﻲLASIK ﺩﻭﺭﺓ ﺟﺎﻣﻊ ﺁﻣﻮﺯﺵ،( ﻣﻲﺑﺎﺷﺪAAO) ( ﻣﺘﻌﻠﻖ ﺑﻪ ﺁﻛﺎﺩﻣﻲ ﭼﺸﻢﭘﺰﺷﻜﻲ ﺁﻣﺮﻳﻜﺎOphthalmology Interactive) ﻫﺎﻱ ﻣﻌﺘﺒﺮCD ﻛﻪ ﺍﺯ ﺳﺮﻱCD ٣ ﻣﺠﻤﻮﻋﺔ ﺍﻳﻦ ﺍﻧﺠﺎﻡ ﺁﻥ ﻭ ﺑﺎﻻﺧﺮﻩ ﻋﻮﺍﺭﺽ ﺍﺣﺘﻤﺎﻟﻲ ﻭ ﻃﺮﻕ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﺩﺭﻣﺎﻥ ﺁﻧﻬﺎ ﺍﺳﺖ
ــــ 2000
65.8 RETINA (Stephen J. Ryan, M.D., Thomas E. Ogden, M.D.,)
ــــ
66.8 RETINA LIBRARY
ــــ
67.8 Retina & Vitneous
ــــ
68.8 Stereoscopic Atlas of Macular Diseases: diagnosis and treatment (Fourth Edition) (J. Donald M. Gass, M.D.) (Mosby)
ــــ
69.8 Subjective Refraction: Cross Cylider Technique
ــــ
70.8 SURGICAL TECHNIQUES WITH MEDPORIMPLANTS AND THE MCP (VCD), (AJL OPHTHALMIC, S.A.)
ــــ
Hereditary retinal dystrophies ﺑـﻪCD ﺩﺍﺷﺘﻦ ﺍﻳﻦ. ﺗﺼﻮﻳﺮ ﺑﺎ ﻛﻴﻔﻴﺘﻲ ﻛﻢﻧﻈﻴﺮ ﻣﻮﺭﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪﺍﻧﺪ١٧٠٠ ﻭ ﺑﺎﻟﻎ ﺑﺮCase ٤٦٧ ﺗﻤﺎﻣﻲ ﺍﻧﻮﺍﻉ ﺩﻳﺴﺘﺮﻭﻓﻲﻫﺎﻱ ﺭﺗﻴﻦ ﺍﺯ ﺷﺎﻳﻊﺗﺮﻳﻦ ﺗﺎ ﻧﺎﺩﺭﺗﺮﻳﻦ ﺁﻧﻬﺎ ﺩﺭ ﻗﺎﻟﺐ. ﻓﻮﻕ ﻳﻜﻲ ﺍﺯ ﺟﺎﻣﻊﺗﺮﻳﻦ ﻣﺮﺍﺟﻊ ﻣﻌﺘﺒﺮ ﺩﺭ ﺑﺎﺏ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﺩﻳﺴﺘﺮﻭﻓﻲﻫﺎﻱ ﺭﺗﻴﻦ ﺍﺳﺖCD .ﻋﻨﻮﺍﻥ ﺭﻓﺮﺍﻧﺴﻲ ﻣﺼﻮﺭ ﺩﺭ ﻣﻮﺍﺟﻪ ﺑﺎ ﻣﻮﺍﺭﺩ ﮔﻮﻧﺎﮔﻮﻥ ﺩﻳﺴﺘﺮﻭﻓﻲﻫﺎﻱ ﺭﺗﻴﻦ ﺩﺭ ﻛﻠﻴﻨﻴﻚ ﺿﺮﻭﺭﻱ ﻣﻲﻧﻤﺎﻳﺪ
71.8 ADVANCED CONCEPTS IN CATARACT SURGERY The American Society of Cataract and Refractive Surgery (ASCRS)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
44 ــــ
)71.8 Clinical Update Course on Glaucoma (Mark B. Sherwood, MD, James D. Brandt, MD, Neil T. Choplin, MD, Joel S. Schuman, MD )72.8 Techniques in CLEAR CORNEAL CATARACT SURGERY OPHTHALMOLOGY Interactive 73.8
ﺗﻤﺎﻣﻲ ﻣﺮﺍﺣﻞ ﺟﺮﺍﺣﻲ ﻛﺎﺗﺎﺭﺍﻛﺖ ﺑﺮﻭﺵ "Clear cornea" Phacoemulsificationﺷﺎﻣﻞ ﺍﻧﺘﺨﺎﺏ ﺑﻴﻤﺎﺭ ،ﺑﻲﺣﺴـﻲ ﺗﺎﭘﻴﻜـﺎﻝ ﻭ ،Prep & drape ، intracameralﺍﻧﺴـﺰﻳﻮﻥ capsulorrhexis ،Clear corneaﻭ ﻇﺮﺍﻳـﻒ ﻣﺮﺑﻮﻃـﻪsetting ،hydrodissection ،
ﻓﻴﻜـﻮ ﺩﺭ ﺍﻧـﻮﺍﻉ ﻣﺨﺘﻠـﻒ
ﻛﺎﺗﺎﺭﺍﻛﺖ ،ﻛﺎﺷﺖ Foldable IOLﻭ ﺑﺎﻻﺧﺮﻩ ﻋﻮﺍﺭﺽ ﺍﺣﺘﻤﺎﻟﻲ ﻭ ﻃﺮﻳﻘﺔ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺁﻧﻬﺎ ﺩﺭ ﻣﺠﻤﻮﻋﺔ CD٣ﻓﻮﻕ ﺍﺯ ﻃﺮﻳﻖ ،Lectureﺗﺼﺎﻭﻳﺮ ﺷﻤﺎﺗﻴﻚ ﻭ ﻓﻴﻠﻢ ﺟﺮﺍﺣﻲﻫﺎﻱ ﺍﻧﺠﺎﻡﺷﺪﻩ ﺗﻮﺳﻂ ﺍﺳﺘﺎﺩﺍﻥ ﺑﻨﺎﻡ ﺍﻳﻦ ﺭﺷﺘﻪ ﺑﻄﻮﺭ ﻛﺎﻣﻞ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. )74.8 TEXBOOK OF OPHTHALMOLOGY (KENNETH W.WRIGHT )REVIEW QUESTIONS IN OPHTHALMOLOGY (KENNETHC. CHERN.KENNETH W. WRIGHT
ــــ
ــــ
ﺩﺭ ﺩﺳﺘﺮﺱ ﺑﻮﺩﻥ ﻛﺘﺐ ﻣﺮﺟﻊ ﺑﺼﻮﺭﺕ ﻟﻮﺡ ﻓﺸﺮﺩﻩ ) (CDﺍﺭﺯﺵ ﺁﻧﻬﺎ ﺭﺍ ﺩﻭ ﭼﻨﺪﺍﻥ ﻣﻲﻛﻨﺪ ﺯﻳﺮﺍ ﻋﻼﻭﻩ ﺑﺮ ﺍﺷﻐﺎﻝ ﻓﻀﺎﻱ ﻛﻤﺘﺮ ﻭ ﺣﻤﻞ ﻭ ﻧﻘﻞ ﺭﺍﺣﺘﺘﺮ ،ﺍﻣﻜﺎﻥ ﺟﺴﺘﺠﻮﻱ ﺳﺮﻳﻊ ﻣﻄﻠﺐ ﻣﻮﺭﺩ ﻧﻈﺮ ﻭ ﺍﺣﻴﺎﻧﹰﺎ ﺗﻬﻴﺔ Printﺍﺯ ﺁﻥ ﻧﻴﺰ ﻓﺮﺍﻫﻢ ﺍﺳﺖ .ﺍﺯ ﺳﻮﻱ ﺩﻳﮕﺮ ،ﺑﻬﺎﻱ CDﺣﺘﻲ ﺑﺎ ﻼ ﺑﺼﻮﺭﺕ CDﻣﻌﺮﻓﻲ ﻣﻲﮔﺮﺩﺩ ،ﺍﻧﺤﺼﺎﺭﹰﺍ ﺗﻮﺳﻂ ﺷﺮﻛﺖ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺑﺎ ﺩﻗﺘﻲ ﻭﺳﻮﺍﺱ ﮔﻮﻧﻪ ﺍﺯ ﺭﻭﻱ ﺁﺧﺮﻳﻦ ﺗﺠﺪﻳﺪﻧﻈﺮ ﻛﺘـﺐ textﺗﻬﻴـﻪ ﺷـﺪﻩ ﻛﺘﺐ textﻣﻌﺎﺩﻝ ﺁﻥ ﻛﻪ ﺩﺭ ﺩﺍﺧﻞ ﻛﺸﻮﺭ ﺍﹸﻓﺴﺖ ﺷﺪﻩ ﻗﺎﺑﻞ ﻣﻘﺎﻳﺴﻪ ﻧﻤﻲﺑﺎﺷﺪ .ﺩﻭ ﻧﻤﻮﻧﻪ ﺍﺯ ﻛﺘﺐ ﻣﺮﺟﻌﻲ ﻛﻪ ﺫﻳ ﹰ ﺍﺳﺖ ،ﺑﻄﻮﺭﻳﻜﻪ ﺗﺼﺎﻭﻳﺮ ﻭ ﻋﻜﺲﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ ﺁﻧﻬﺎ ﺩﺍﺭﺍﻱ ﻗﺎﺑﻠﻴﺖ ﺑﺰﺭﮔﻨﻤﺎﺋﻲ ﺑﻮﺩﻩ ،ﺍﺯ ﻧﻈﺮ ﻛﻴﻔﻲ ﺑﻬﻴﭻ ﻋﻨﻮﺍﻥ ﺑﺎ ﻛﺘﺐ ﺍﻓﺴﺖ ﻣﻮﺟﻮﺩ ﺩﺭ ﺩﺍﺧﻞ ﻛﺸﻮﺭ ﻗﺎﺑﻞ ﻣﻘﺎﻳﺴﻪ ﻧﻴﺴﺖ. )75.8 THE FAILING GLAUCOMA FILTER: EARLY IDENTIFICATION & TREATMENT (Bradford J. Shingleton, MD CDﻓﻮﻕ ﺗﻤﺎﻣﹰﺎ ﺑﻪ ﻣﻘﻮﻟﺔ Failing Filtration Surgeryﭘﺮﺩﺍﺧﺘﻪ ﻭ ﻋﻠﻞ ،ﻋﻮﺍﻣﻞ ﻣﺴﺘﻌﺪﻛﻨﻨﺪﻩ ،ﺭﺍﻩﻫﺎﻱ ﭘﻴﺸﮕﻴﺮﻱ ﻭ ﺑﺎﻻﺧﺮﻩ ﺩﺭﻣﺎﻥﻫﺎﻱ ﻃﺒﻲ ﻭ ﺟﺮﺍﺣﻲ ﺁﻥ ﺭﺍ ﺍﺯ ﻃﺮﻳﻖ ﭼﻨﺪﻳﻦ Lectureﻭ ﻓﻴﻠﻢﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺮﺑﻮﻃﻪ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ .ﺩﺭ ﺍﻳﻦ CDﺗﻜﻨﻴﻚﻫﺎﻳﻲ ﻣﺎﻧﻨﺪ Choroidal tapﻭ ﻼ ﺿﺮﻭﺭﻱ ﻣﻲﺑﺎﺷﺪ ﺑﺨﻮﺑﻲ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. bleb revisionﻛﻪ ﺩﺍﻧﺴﺘﻦ ﺁﻧﻬﺎ ﺑﺮﺍﻱ ﻫﺮ ﺟﺮﺍﺡ ﮔﻠﻮﻛﻮﻣﻲ ﻛﺎﻣ ﹰ
ــــ
)(MICHAEL K. SMOLEK, PH. D.
76.8 The Multimedia Atlas of Videokeratography Basics of Map Interpretation
ــــ
)77.8 The Retina ATLAS ( Yannuzzi,Green) (Mosby
)(S.LBosniak
ــــ
)78.8 THE VIDEO ATLAS OF COSMETIC BLEPHAROPLASTY (8 CDs
ﻣﺠﻤﻮﻋﺔ VCD ٨ﻓﻮﻕ ﻳﻚ ﺩﻭﺭﺓ ﻛﺎﻣﻞ ﺁﻣﻮﺯﺵ ﺟﺮﺍﺣﻲ ﭘﻠﻚ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﻮﺳﻂ ﺍﺳﺘﺎﺩ ﺑﺮﺟﺴﺘﻪ S.LBosniakﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺷﺎﻣﻞ ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﺍﺯ ﺁﻧﺎﺗﻮﻣﻲ ﭘﻠﻚ ﻭ ﺭﻭﺵﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﻲﺣﺴﻲ ﺗﺎ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺩﺭ ﺍﺻـﻼﺡ ﻭ ﺗـﺮﻣﻴﻢ ﻛﻠﻴـﺔ ﻣﺴﺎﺋﻞ ﻭ ﻣﺸﻜﻼﺕ ﭘﻠﻜﻲ ﻣﻦﺟﻤﻠﻪ ،ﺁﻧﺘﺮﻭﭘﻴﻮﻥ ،ﺍﻛﺘﺮﻭﭘﻴﻮﻥ ،ﭘﺘﻮﺯ ،ﺩﺭﻣﺎﺗﻮﺷﺎﻻﺯﻳﺲ ﻭ ...ﻣﻲﺑﺎﺷﺪ .ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻣﺠﻤﻮﻋﻪ ﺭﺍ ﺑﺎﻳﺪ ﺑﻪ ﻣﻨﺰﻟﺔ ﮔﺬﺭﺍﻧﺪﻥ ﻳﻚ ﺩﻭﺭﻩ ﻛﺎﺭﮔﺎﻩ ﺁﻣﻮﺯﺷﻲ ﺑﻠﻔﺎﺭﻭﭘﻼﺳﺘﻲ ﺩﺍﻧﺴﺖ. ــــ
)Vitreoretinal Course Bascom Palmer Eye Institute's (William E. Smiddy, Philip Rosenfeld, Patrick E. Rubsamen, Janet L.
79.8
CDﻓﻮﻕ ﺍﺯ ﺳﺮﻱ CDﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ (Ophthalmology interactive) OIﻣﺘﻌﻠﻖ ﺑﻪ ﺁﻛﺎﺩﻣﻲ ﭼﺸﻢﭘﺰﺷﻜﻲ ﺁﻣﺮﻳﻜﺎ ) ،(AAOﺣﺎﻭﻱ Lecture ١٦ﺑﻪ ﻫﻤﺮﺍﻩ ﺍﺳﻼﻳﺪ ﻭ ﻓﻴﻢ ﺍﺯ ﺍﺳﺘﺎﺩﺍﻥ ﺑﺮﺟﺴﺘﻪﺍﻱ ﭼﻮﻥ W.E.Smiddyﻭ H.W.Flynnﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻣﺮﻭﺭ ﻭ ﻣﻌﺮﻓﻲ ﺁﺧﺮﻳﻦ ﺩﺳﺘﺎﻭﺭﺩﻫﺎ ﺩﺭ ﻣﻮﺭﺩ ﻣﺒﺎﺣﺚ ﻣﺨﺘﻠﻒ ﺟﺮﺍﺣﻲ ﺳﮕﻤﺎﻥ ﺧﻠﻔﻲ ﭼﺸﻢ ﻣﻲﭘﺮﺩﺍﺯﺩ .ﺍﺯ ﺟﻤﻠﻪ ﻣﻮﺿﻮﻋﺎﺕ ﻣﻮﺭﺩ ﺑﺤﺚ ﺩﺭ ﺍﻳﻦ CDﻣﻲﺗﻮﺍﻥ Macular hole ،Giant retinal tear،Dislocated IOLs ،AMD , ROP ،Endophthalmitis :ﻭ ...ﺭﺍ ﻧﺎﻡ ﺑﺮﺩ. ــــ
)80.8 VJO Ophthalmology (I, I , III ,) (VCD) (Charles, H. Cozean, James S. Lewis, Richard J. Mackool
-٩ﻣﻐﺰ ﻭ ﺍﻋﺼﺎﺏ
ﻋﻨﻮﺍﻥ CD
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ 2004
)5 Minute Neurology Consult (SALEKAN E-BOOK) (D. Joanne Lynn
1.9
ﺍﻳﻦ CDﻛﻪ ﺑﺮﺍﻱ ﺍﺳﺘﻔﺎﺩﻩ ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎ ،ﺭﺯﻳﺪﻧﺖﻫﺎ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺩﺍﺧﻠﻲ ﺍﺳﺖ .ﺑﻪ ﻋﻨﻮﺍﻥ ﺭﻓﺮﺍﻧﺲ ﺳﺮﻳﻌﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ ﺳﺮﻱ 5-Minuteﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﻓﺮﻣﺖ ﺩﻭﺻﻔﺤﻪﺍﻱ ﺍﺳـﺘﻔﺎﺩﻩ ﺑﻼﻓﺎﺻـﻠﻪ ﻭ ﺳـﺮﻳﻊ ﺍﺯ ﺁﻥ ﺭﺍ ﺭﺍﺣـﺖ ﻛﺮﺩﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ٢٠٠ﺑﻴﻤﺎﺭﻱ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻛﺎﺭ ﺑﺎﻟﻴﻨﻲ ﺑﻪ ﻃﻮﺭ ﺷﺎﻳﻌﻲ ﺑﺎ ﺁﻧﻬﺎ ﻣﻮﺍﺟﻪ ﻣﻲﺷﻮﻳﻢ .ﻫﺮ ﻣﺒﺤﺚ ﺷﺎﻣﻞ Follow up ، Medications ، Management ، Diagnosis ،Basicsﻭ MiscellaneousﻣـﻲﺑﺎﺷـﺪCD . ﺷﺎﻣﻞ ﻓﺼﻮﻝ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ. -Short Topics 2003
-Neurologic Symptoms and Signs -Neurologic Diagnostic Tests -Neurologic Diseases and Disorders th )55 Annual Meeting March 29-Aprill 5, American Academy of Neurology (HAWAII
2.9
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺷﺎﻣﻞ Full textﺗﻤﺎﻡ ﻣﻘﺎﻻﺕ ﻭ Presentationﻫﺎﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺩﺭ ﻛﻨﮕﺮﻩ ﺁﻛﺎﺩﻣﻲ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺍﻣﺮﻳﻜﺎ ﺩﺭ ﺁﻭﺭﻳﻞ 2003ﺩﺭ ﻫﺎﻭﺍﻳﻲ ﻣﻲﺑﺎﺷﺪ. 2000 ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
)(Barlow/Durand's, Durand/Barlow's, Trull/Pharcs
3.9 Abnormal Psychology LIVE and interactive tutorial
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
45 2004
4.9 American Academy of Neurology 2004 Syllabi
ﺍﻳﻦ CDﻛﻪ ﺣﺎﺻﻞ ﻣﻘﺎﻻﺕ ﺁﺧﺮﻳﻦ ﻛﻨﮕﺮﻩ ﺁﻛﺎﺩﻣﻲ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺍﻣﺮﻳﻜﺎ ﺩﺭ ﺳﺎﻝ ٢٠٠٤ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ١٦٠ﻣﻮﺿﻮﻉ ﺩﺭ ﺯﻣﻴﻨﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻃﺒﺎﺑﺖ ﺑﺎﻟﻴﻨﻲ ﻧﻮﺭﻭﻟﻮﮊﻱ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻫﺮ ﻣﻮﺿﻮﻉ ﺷﺎﻣﻞ ﭼﻨﺪ ﻣﻘﺎﻟﻪ ﻭ ﻣﺒﺤﺚ ﻣﻲﮔﺮﺩﺩ .ﺑﻌﻀﻲ ﺍﺯ ﻣﻘﺎﻻﺕ ﺍﺭﺍﺋﻪﺷﺪﻩ ﻫﻤﺮﺍﻩ ﺑﺎ ﻓﺎﻳﻞﻫﺎ ﻭ ﺍﺳﻼﻳﺪﻫﺎﻱ Presentationﻧﻴﺰ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻛﺎﺭﺑﺮﺩ ﺁﻥ ﺭﺍ ﺑﺮﺍﻱ ﺗﺪﺭﻳﺲ ﻭ ﺍﺭﺍﺋﺔ ﻣﺠﺪﺩ ﺩﻭﭼﻨﺪﺍﻥ ﻣﻲﺳﺎﺯﺩ .ﻓﺎﻳﻞﻫﺎ ﺍﺯ ﻃﺮﻳﻖ Javaﻭ ﺑﻪ ﺻﻮﺭﺕ Autorunﺍﺟﺮﺍ ﻣﻲﮔﺮﺩﻧﺪ ﻗﺎﺑﻠﻴﺖ Searchﺑﺮ ﺍﺳﺎﺱ ﻣﻮﺿﻮﻉ ﻭ ﻧﻮﻳﺴﻨﺪﻩ ﺍﺯ ﻣﺰﺍﻳﺎﻱ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺍﺳﺖ. ﻣﺒﺎﺣﺚ ﻣﻬﻢ ﻣﻄﺮﺡﺷﺪﻩ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: Stroke Demyelinating dyorden
ــــ
Botutinum Toxin Injection Movement disorders
Balance and gaif disorder Clinical EMG
)Advanced Therapy of HEADACHE CONQUERING HEADACHE (SECOND REVIED EDITION) An Illustrated Guide to Understanding The Treatment and Control of Headache (Alan M. Rapoport, Fred D. Sheftell
(١ (٢ (٣
)6.9 Atlas of Functional Neuroanatomy (Dr. Walter J. Hendelman
)(Phoenix, Arizona
2003
7.9 Boehringer Ingelheim Satellite Symposium Interanational Stroke Conference
)(An interactive digital atlas designed to assist in learning human neuroanatomy
1996 ــــ
5.9
ﺍﻳﻦ CDﺷﺎﻣﻞ ﺳﻪ ﻗﺴﻤﺖ ﻣﻲﺑﺎﺷﺪ. ﻣﺘﻦ ﻓﺎﻳﻞ PDFﻛﺘﺎﺏ ) Advanced Therapy of headache (1999ﺗﻮﺳﻂ ) Alan rappaportﺍﺳﺘﺎﺩ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ) Fred sheftell ( Yaleﺍﺳﺘﺎﺩ ﺑﺨﺶ ﺭﻭﺍﻧﭙﺰﺷﻜﻲ ﺩﺍﻧﺸـﮕﺎﻩ ( Newyorkﻧﻮﺷـﺘﻪ ﺷـﺪﻩ ﺍﺳـﺖ .ﺷـﺎﻣﻞ 48ﻣﺒﺤـﺚ ﭘﺎﻳـﻪ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﺍﺻﻮﻝ ﺗﺌﻮﺭﻱ ﻭ ﻋﻤﻠﻲ ﺍﻧﻮﺍﻉ ﻣﺨﺘﻠﻒ ﺳﺮﺩﺭﺩ ﺍﺯ ﺟﻤﻠﻪ ﺗﺸﺨﻴﺺﻫﺎﻱ ﭘﻴﭽﻴﺪﻩ ،ﺩﺭﻣﺎﻥ ﺷﺎﻣﻞ ﺩﺭﻣﺎﻧﻬﺎﻱ ﺟﺪﻳﺪ ﻭ ﻧﻴﺰ managementﺑﻴﻤﺎﺭﺍﻥ ﻣﻲﺑﺎﺷﺪ. ﻣﺘﻦ ﻓﺎﻳﻞ PDFﻛﺘﺎﺏ Conquering headache 1998 2nd editionﺍﺯ ﻧﻮﻳﺴﻨﺪﮔﺎﻥ ﻓﻮﻕ ﻛﻪ ﺍﻃﻼﻋﺎﺗﻲ ﺩﺭ ﺁﻥ ﺟﻬﺖ ﻣﻘﺎﺑﻠﻪ ﺑﺎ ﺳﺮﺩﺭﺩ ﻭ ﺑﻬﺒﻮﺩ ﻧﺤﻮﺓ ﺯﻧﺪﮔﻲ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻫﻤﺮﺍﻩ ﺑﺎ ﺁﺧﺮﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺭﺍﺟﻊ ﺑﻪ ﺗﻘﺴﻴﻢ ﺑﻨﺪﻱ ﺳﺮﺩﺭﺩﻫﺎ -ﺩﺭﻣﺎﻧﻬـﺎﻱ ﺩﺍﺭﻭﻳـﻲ ﺗﺌﻮﺭﻱﻫﺎﻱ ﺟﺪﻳﺪ -ﺍﺻﻮﻝ ﺗﻐﺬﻳﻪﺍﻱ ﻭﺭﺯﺷﻲ -ﺧﻮﺍﺏ -ﺭﻭﺵﻫﺎﻱ ﻏﻴﺮ ﺩﺍﺭﻭﻳﻲ ﺩﻳﮕﺮ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ.ﻣﺘﻦ PDFﺟﻤﻠﺔ Seminars in Headache mamagementﻛﻪ ﺗﻮﺳﻂ James W.Lanceﺍﺩﺍﺭﻩ ﻣﻲﮔﺮﺩﺩ ﻭ ﺷﺎﻣﻞ ﺳﻪ ﺳﺎﻝ ﺍﺯ ﺳﺎﻝ 1996- 1998ﻣﻲﺑﺎﺷﺪ .ﻣﺒﺎﺣﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ :ﺗﺸﺨﻴﺺ -ﺩﺭﻣﺎﻥ ﺣﺎﺩ ﻣﻴﮕﺮﻥ ﻭ ﺩﺭﻣﺎﻥ ﭘﺮﻭﻓﻴﻼﻛﺘﻴﻚ ﻣﺒﺎﺣﺚ ﺳﺮﺩﺭﺩﻫﺎﻱ ﻛﻼﺳﺘﺮ – Post traumatic -ﺍﻳﺴﻜﻤﻲ ﻣﻐﺰﻱ ﻧﺎﺷﻲ ﺍﺯ ﻣﻴﮕﺮﻥ -ﻣﻴﮕﺮﻥ ﻭ ﻫﻮﺭﻣﻮﻧﻬﺎﻱ ﺟﻨﺴﻲ.
2000 ــــ
Bedside Neurology Clinical EEG
Seizure and antiepilep drugs Child Neurology
)(Version 1.52
Medical Multimedia Systems Presents
TM
!8.9 Brainiac
)Clinical Neurology (G David Perkin Fred H Hochberg Douglas C Miller
9.9
)10.9 Comprehensive Textbook of PSYCHIATRY (Seventh Edition CD-ROM) (Benjamin J. Sadock, MD – Virginia A. Sadock, MD) ( LIPPINCOTT WILLIAMS & WILKINS
ﻼ ﺍﺯ ﻭﺿﻮﺡ ﺑﺎﻻﻳﻲ ﺑﺮﺧﻮﺭﺩﺍﺭﻧﺪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻳﻚ ﻛﺘﺎﺏ ﺟﺎﻣﻊ ﻭ ﻣﺮﺟﻊ ﺩﺭ ﺯﻣﻴﻨﺔ ﺭﻭﺍﻥ ﭘﺰﺷﻜﻲ ﺍﺳـﺖ .ﺗﺼـﺎﻭﻳﺮ ﻣﺘﻌـﺪﺩ ﺁﻣﻮﺯﺷـﻲ،MRI ، ﺍﻳﻦ CDﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻚ ﻣﺸﺘﻤﻞ ﺑﺮ ٥٥ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ .ﻫﻤﭽﻨﻴﻦ ﺣﺎﻭﻱ ٦٥٠ﺗﺼﻮﻳﺮ ﺁﻣﻮﺯﺷﻲ ﻭ ﻧﻴﺰ ﺟﺪﺍﻭﻝ ﻣﺘﻌﺪﺩﻱ ﺍﺳﺖ ﻛﻪ ﻛﺎﻣ ﹰ ﻃﺮﺡﻭﺍﺭﻩﻫﺎ ﻭ ﺗﺼﺎﻭﻳﺮ ﺑﺮﺧﻲ ﺍﺯ ﺩﺍﻧﺸﻤﻨﺪﺍﻥ ﺍﻳﻦ ﺭﺷﺘﻪ ،ﺍﺭﺍﺋﻪ ﻛﺎﻣﻞ ﻣﻨﺎﺑﻊ ﺩﺭ ﭘﺎﻳﺎﻥ ﻫﺮ ﻓﺼﻞ ،ﻓﻬﺮﺳﺖ ﻛﺎﻣﻞ ﻣﻮﺿﻮﻋﺎﺕ ،ﺍﺭﺍﺋﻪ ﺩﺍﺭﻭﻫﺎﻱ ﺭﻭﺍﻧﭙﺰﺷﻜﻲ ﻭ ﺍﺷﻜﺎﻝ ﺩﺍﺭﻭﺋﻲ ﻣﺨﺘﻠﻒ ﺑﻪ ﻫﻤﺮﺍﻩ ﺗﺼﻮﻳﺮ ﺁﻧﻬﺎ ﺍﺯ ﻭﻳﮋﮔﻲﻫﺎﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﻲﺑﺎﺷﺪ .ﺑﺮﺧﻲ ﺍﺯ ﻓﺼﻮﻝ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ. -١ﺭﻭﺍﻧﭙﺰﺷﻜﻲ ﺍﻋﺼﺎﺏ ﻭ ﺭﻓﺘﺎﺭ -٢ﻋﻠﻮﻡ ﺍﻋﺼﺎﺏ -٣ﺗﺌﻮﺭﻳﻬﺎﻱ ﺷﺨﺼﻴﺖ ﻭ ﺁﺳﻴﺐﺷﻨﺎﺳﻲ ﺁﻧﻬﺎ -٤ﺭﻭﺷﻬﺎﻱ ﺗﺸﺨﻴﺺ ﺩﺭ ﺭﻭﺍﻥﭘﺰﺷﻜﻲ -٥ﻃﺒﻘﻪﺑﻨﺪﻱ ﺑﻴﻤﺎﺭﻫﺎﻱ ﻣﻐﺰﻱ -٦ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺷﻨﺎﺧﺘﻲ … -٧ ((Delirium Dementin,ﺍﺳﻜﻴﺰﻭﻓﺮﻧﻲ -٨ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺿﻄﺮﺍﺏ -٩ﺑﻴﻤﺎﺭﻳﻬﺎﻱ -١٠ Moodﺑﻴﻤﺎﺭﻫﺎﻱ ﺭﻭﺍﻧﻲ ﺧﻮﺍﺏ -١١ﺑﻴﻤﺎﺭﻳﻬﺎﻱ -١٢ Dissociativeﺧﻮﺩﻛﺸﻲﻫﺎ -١٣ﺭﻭﺍﻥ ﭘﺰﺷﻜﻲ ﺍﻃﻔﺎﻝ -١٤ﺑﻴﻤﺎﺭﻫﺎﻱ ﻳﺎﺩﮔﻴﺮﻱ -١٥ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺭﺗﺒﺎﻃﻲ -١٦ﺑﻴﻤﺎﺭﻱﻫﺎﻱ Ticﻋﺼﺒﻲ -١٧ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﺿﻄﺮﺍﺏ ﺩﺭ ﻛﻮﺩﻛﺎﻥ -١٩ Adoption -١٨ﺭﻭﺍﻧﭙﺰﺷﻜﻲ )ﮔﺬﺷﺘﻪ ﺩﺭ ﺁﻳﻨﺪﻩ( ﻭ ...ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﻮﺍﻧﺎﻳﻲ ﺟﺴﺘﺠﻮ ﺑﺮ ﺍﺳﺎﺱ ﻭﺍﮊﻩﻫﺎﻱ ﺗﺨﺼﺼﻲ ﻭ ﺍﺳﺎﻣﻲ ﺩﺍﺭﻭﻫﺎ ﺭﺍ ﺩﺍﺭﺍﺳﺖ .ﺟﺴﺘﺠﻮﻱ ﺗﺼﺎﻭﻳﺮ ،ﺗﻮﺍﻧﺎﻳﻲ ﭼﺎﭖ ﻣﺘﻦ ﻭ ﺗﺼﺎﻭﻳﺮ ،ﺍﺿﺎﻓﻪ ﻧﻤﻮﺩﻥ ﻳﺎﺩﺩﺍﺷﺖﻫﺎﻱ ﺷﺨﺼﻲ ﺍﺯ ﻭﻳﮋﮔﻴﻬﺎﻱ ﺩﻳﮕﺮ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺳﺖ. 2001
)11.9 Computational Neuroscience Realistic Modeling for Experimentalists (Erik De Schutter Introduction to Equation Solving and Parameter Fitting Modeling Networks of Signalling Pathways Modeling Local and Global Calcium Signals Using Reaction-Diffusion Equations Monte Carlo Methods for Simulating Realistic Synaptic Microphysiology Using Mcell Which Formalism to Use for Modeling voltage-Dependent Conductances? Accuate Reconstruction of Neunal Morphology Modeling Dendritic Geometry and the Development of Nerve Connections Passive Cable Modeling-A practical Introduction Modeling Simple and Complex Active Neurons Realistic Modeling of Small Neuronal Circuits Modeling of Interactions Between Neural Networks and Musculoskeletal System
2001
)12.9 CONTEMPORARY NEUROSURGERY A BIWEEKLY PUBLICATION FOR CLINICAL NEUROSURGICAL CONTINUING MEDICAL EDUCATION (Ali F. Krisht, MD
ــــ
)(Micheal K. Rees, MD, MPH, Robert Birnbaum, MD, PHD, James A.D. Otis
13.9 Core Curriculum in Primary Care Psychiatry and Pain Management Section
ﺍﻳﻦ CDﺍﺯ ﺳﺮﻱ CCCﻋﻤﺪﺗﺎﹰ ﺟﻬﺖ ﭘﺎﺳﺨﮕﻮﻳﻲ ﺑﻪ ﻧﻴﺎﺯ ﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﭘﺰﺷﻜﺎﻥ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻋﻤﺪﺓ ﻓﻌﺎﻟﻴﺘﺸﺎﻥ ﺩﺭ ﺯﻣﻴﻨﻪ ﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻭ ﺑﻴﻤﺎﺭﺍﻥ ﺳﺮﭘﺎﻳﻲ ﺍﺳﺖ ﺑﻪ ﻃﻮﺭﻳﻜﻪ ﺗﻤﺎﻡ ﻣﺒﺎﺣﺚ ﻭ ﻣﻔﺎﻫﻴﻢ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺑﺮﺍﻱ ﺍﺟﺮﺍﻱ ﻋﻤﻠﻲ ﺩﺭ ﻛﻠﻴﻨﻴﻚ ﺟﻬـﺖﺩﻫـﻲ ﺷﺪﻩﺍﻧﺪ ﻭ ﺁﺧﺮﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺑﺎﻟﻴﻨﻲ ﺭﺍ ﺑﺎ ﺷﻌﺎﺭ" "Current best Standard of therapyﺍﺭﺍﺋﻪ ﻣﻲﻧﻤﺎﻳﻨﺪ .ﺷﺎﻣﻞ ﺩﻭ ﻣﺒﺤﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
46 : ﺍﺭﺍﺋﻪ ﻣﻲﮔﺮﺩﺩ ﻭ ﺷﺎﻣﻞ ﺳﺮ ﻓﺼﻞﻫﺎﻱ ﺯﻳﺮ ﺍﺳﺖHarvard Medical School ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩRobert Birnbaum ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ: Psychopharmacology for primay Care Medicine -١ Anxiety disorder- Panic disorder- Social phobia- Specific phobia- Obcessive & Compulsire disorder- PTSD- Generalized Anxiety disorder- Depression-Dysthymia
. ﺟﺮﺍﺣﻲ( ﻣﻮﺭﺩ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ- ﺭﻭﺍﻧﺪﺭﻣﺎﻧﻲ- ﻣﺨﺪﺭ- ﺍﻧﻮﺍﻉ ﺩﺭﻣﺎﻧﻬﺎﻱ ﺩﺭﺩ )ﺩﺍﺭﻭﻳﻲ- ﺗﺸﺨﻴﺺ ﺩﺳﺘﻪﺑﻨﺪﻱ- ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ ﻭ ﺍﺭﺯﻳﺎﺑﻲBoston ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩJames A.D. otis ﻛﻪ ﺗﻮﺳﻂ ﺩﻛﺘﺮ: Pain Management -٢ . ﻗﺎﺑﻠﻴﺖ ﺍﻧﺘﺨﺎﺏ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺩﻟﺨﻮﺍﻩ ﺟﻬﺖ ﺍﺭﺍﺋﻪ ﻭ ﻛﻨﻔﺮﺍﻧﺲ ﺟﺪﺍﮔﺎﻧﻪ ﻧﻴﺰ ﻣﻲﺑﺎﺷﺪCD ﻧﺮﻡﺍﻓﺰﺍﺭ ﺍﻳﻦ. ﺗﻌﺪﺍﺩﻱ ﺳﻮﺍﻝ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﺒﺤﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﻣﻄﺮﺡ ﻭ ﭘﺎﺳﺦ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﻲﺑﺎﺷﺪprint ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﺩﺭ ﻓﺎﻳﻞ ﺟﺪﺍﮔﺎﻧﻪﺍﻱ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﻗﺎﺑﻞ 14.9 Corel Medical Series Epilepsy (Alan Guberman MD, FRCP (C)) (Professor of Neurology University of Ottawa
ــــ
ﻛﺎﻣـﻞQuiz ﺍﻧﻴﻤﻴﺸﻦ ﻭ ﻗﻄﻌـﺎﺕ ﻭﻳـﺪﺋﻮﻳﻲ ﻭ- ﺳﺮ ﻓﺼﻞﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﺁﻧﺎﻟﻴﺰ ﮔﺮﺩﺩ ﻭ ﺑﺎ ﺗﺼﺎﻭﻳﺮ: ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺳﻌﻲ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻳﻜﺴﺮﻱ ﺍﺯ ﻣﺸﻜﻼﺕ ﺷﺎﻳﻊ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ ﺻﺮﻉ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﻮﺩ. ﺍﺯ ﺩﺍﻧﺸﮕﺎﻩ ﺍﺗﺎﻭﺍ ﻃﺮﺍﺣﻲ ﻭ ﺍﺟﺮﺍ ﺷﺪﻩ ﺍﺳﺖAllan Guberman ﺗﻮﺳﻂ ﺩﻛﺘﺮ ﺷﺎﻣﻞ ﺳﺮ ﻓﺼﻞﻫﺎﻱ ﺯﻳﺮ ﺍﺳﺖ. ﺑﻮﺩﻩ ﺍﺳﺖproblem based interactive ﺑﻪ ﺻﻮﺭﺕreview ﺳﻌﻲ ﺩﺭ ﺁﻣﻮﺯﺵ ﻭ. ﺗﻤﺎﻣﻲ ﻣﻄﺎﻟﺐ ﺍﺯ ﻧﻘﺎﻁ ﻗﻮﺕ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩPrint ﺍﻃﻼﻋﺎﺕ ﺑﻴﻤﺎﺭﺍﻥ ﻭ ﺗﻮﺍﻧﺎﻳﻲ ﺑﺎﺯﮔﺸﺖ ﻣﻄﺎﻟﺐ ﻭ ﻗﺎﺑﻠﻴﺖ- ﻗﻮﻱSearch .ﮔﺮﺩﺩ Definitions
Topic index
15.9 CRANIAL NERVES
Epilepsy Notes
Patient & Family information
Epilepsy Case Study
Video
Reference list
Epilepsy Facts
What is Epilepsy
Learning Objectives
2002
in health and disease (Second Edition)
ﺷﺎﻣﻞ ﺗﺼﺎﻭﻳﺮ ﻋﺎﻟﻲ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻭ ﻃﺮﺍﺣﻲﻫﺎﻱ ﺭﻧﮕﻲ ﺍﺯ ﻣﺴﻴﺮﻫﺎﻱ ﺍﻋﺼﺎﺏ ﻛﺮﺍﻧﻴﺎﻝ ﺍﺯ ﺍﻃﺮﺍﻑ ﺑﻪ ﻣﻐﺰ ﻭ ﺍﺯ ﻣﻐﺰ ﺑﻪ. ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﻮﺳﻂ ﺟﻤﻌﻲ ﺍﺯ ﺍﺳﺎﺗﻴﺪ ﺟﺮﺍﺡ ﻭ ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖ ﺩﺍﻧﺸﮕﺎﻩﻫﺎﻱ ﻛﺎﻧﺎﺩﺍ ﻧﻮﺷﺘﻪ ﺷﺪﻩ ﺍﺳﺖ2002 ﻛﺘﺎﺏ ﻓﻮﻕ ﭼﺎﭖPDF ﺷﺎﻣﻞ ﻣﺘﻦCD ﺍﻳﻦ ﻣﻄﺮﺡ ﺷﺪﻩ ﻭ ﻟـﺬﺍ ﺑـﺮﺍﻱProblem-oriented ﺍﺻﻮﻝ ﺑﺤﺚ ﺑﺮ ﻣﺒﻨﺎﻱ. ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩﺍﻧﺪCD ﺟﻬﺖ ﺩﺭﻙ ﺑﻬﺘﺮ ﺭﻭﺍﺑﻂ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻭ ﺍﺛﺮﺍﺕ ﻓﻴﺰﻳﻮﻟﻮﮊﻳﻚ ﺩﺭanimation ﭼﻨﺪ ﺗﺼﻮﻳﺮ. ﺳﻨﺎﺭﻳﻮﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻭ ﺗﺴﺖﻫﺎﻱ ﺧﻮﺩﺁﺯﻣﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ،ﺍﻃﺮﺍﻑ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻗﺎﻟﺐ ﻣﺘﻦ . ﺩﺭ ﻗﺴﻤﺖ ﺩﻳﮕﺮ ﻓﻴﻠﻢ ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻋﺼﺎﺏ ﺑﺼﻮﺭﺕ ﺗﻚ ﺗﻚ ﮔﻨﺠﺎﻧﺪﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻭ ﭼﺸﻢ ﭘﺰﺷﻜﻲ ﺑﺴﻴﺎﺭ ﻣﻔﻴﺪ ﻭ ﺿﺮﻭﺭﻱ ﺑﻪ ﻧﻈﺮ ﻣﻲﺭﺳﺪENT ، ﺟﺮﺍﺣﻲ ﻓﻚ ﻭ ﺻﻮﺭﺕ،ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺭﺷﺘﻪﻫﺎﻱ ﻧﻮﺭﻭﻟﻮﮊﻱ 2005
16.9 Textbook of CRITICAL CARE (Salekan E-book) SECTION I RESUSCITATION AND MEDICAL EMERGENCIES SECTION II TRAUMA SECTION III IMAGING SECTION IV CELL INJURY AND CELL DEATH SECTION V INFECTIONS DISEASE SECTION VI ENDOCTINOLOGY, METABOLISM, NUTRITION, PHARMACOLOGY SECTION VII CARDIOVASCULAR SECTION VIII PULMONARY 17.9 Critical Decisions in Headache Management
(Giammarco. Edmeads. Dodick)
ــــ
(SALEKAN E-BOOK)
2002
18.9 CURRENT MANAGEMENT IN CHILD NEUROLOGY (SECOND EDITION) (Bernrd L. Maria, MD, MBA) Section 1: Clinical Practice Trends Section 2: The Office Visit Section 3: The Hospitalized Child
ــــ
19.9 DICTIONARY OF MULTIPLE SCLEROSIS (Lance D Blumgardt) (Martin Dunitz) 20.9 DISORDERS OF COGNITIVE FUNCTION
(VCD-I)
Severe Amnesic Syndrome: Anterograde and Retrograde Amnesia Left Spatial Neglect Broca's Aphasia
21.9 DISORDERS OF COGNITIVE FUNCTION Wernicke's Aphasia Negative Signs of Executive Dysfunction
Basic Mental Status Examination
Perseverative Verbal Behavior in Amnesia Eye Movements in Severe Left Spatial Neglect Lewy Bodies
Semantic Memory Loss Anosognosia for Hemiparesis Impaired Verbatim Repetition
Fluctuativng Sensorium in Dementia With Paraphasias
2002
(VCD-II) (AMERICAN ACADEMY OF NEUROLOGY) (CONTINUUM)
Dysexecutive Syndrome Prosopognosia and Visual Agnosia
22.9 DISORDERS OF COGNITIVE FUNCTION
2002
(AMERICAN ACADEMY OF NEUROLOGY) (CONTINUUM)
Disinhibited Behavior Simultanagnosia
Grasp Response and Imitation Behavior Optic Ataxia
Positive Signs of Executive Dysfunction Ocular Apraxia
Progressive Apraxia
2002
(VCD-III) (AMERICAN ACADEMY OF NEUROLOGY) (CONTINUUM)
Token Test for Auditory Comprehension
Confrontation Naming
Finger Constructions
Luria 3-Step Test
Line Cancellation
Gestural Praxis
23.9 EMG Training (Kenneth Ricker, M.D.)
ــــ
ﻣﺘﻦ ﻫﻤﺮﺍﻩ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﺩﺭ ﻣﻮﺭﺩ ﻧﺤﻮﺓ ﻛﺎﺭ. ﺑﻴﻤﺎﺭ ﻣﺨﺘﻠﻒ ﺭﺍ ﻫﻤﺎﻧﮕﻮﻧﻪ ﻛﻪ ﻣﺎﻧﻴﺘﻮﺭ ﻣﺸﺎﻫﺪﻩ ﻣﻲﮔﺮﺩﺩ ﺑﻪ ﺗﺼﻮﻳﺮ ﻛﺸﻴﺪﻩ ﻭ ﺻﺪﺍﻱ ﺁﻥ ﺭﺍ ﭘﺨﺶ ﻣﻲﻛﻨﺪ٢٧ ﺍﺯEMG ﻣﻮﺭﺩ٧٥ . ﺗﻬﻴﻪ ﺷﺪﻩ ﺍﺳﺖTOENNIES ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻛﻪ ﺟﻬﺖ ﺁﻣﻮﺯﺵ ﺍﻟﻜﺘﺮﻭﻣﻴﻮﮔﺮﺍﻓﻲ ﺗﻮﺳﻂ ﺷﺮﻛﺖ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
47 . ﺑﺮﺍﻱ ﻣﺒﺘﺪﻳﺎﻥ ﻭ ﻧﻴﺰ ﺍﻓﺮﺍﺩ ﻣﺠﺮﺏ ﺩﺭ ﺍﻳﻦ ﺯﻣﻴﻨﻪ ﺟﺎﻟﺐ ﺗﻮﺟﻪ ﺧﻮﺍﻫﺪ ﺑﻮﺩCD ﻓﺎﻳﻞﻫﺎ ﺭﺍ ﻓﺮﺍﻫﻢ ﻣﻲﺁﻭﺭﺩ ﺍﻳﻦSearch ﺍﻣﻜﺎﻥEMG glossary . ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻓﺎﻳﻞ ﻣﺴﺘﻘﻞ ﺍﺭﺍﺋﻪ ﻣﻲﮔﺮﺩﺩCase ﻫﺮ.ﺭﺍ ﺍﺭﺍﺋﻪ ﻛﺮﺩﻩ ﺍﺳﺖ ﻭ ﺳﺆﺍﻻﺗﻲ ﺭﺍ ﻣﻄﺮﺡ ﻧﻤﻮﺩﻩ ﻭ ﭘﺎﺳﺦ ﺩﺍﺩﻩ ﺍﺳﺖ 24.9 ENS Teaching Course
ــــ
ﻋﻤﺪﺓ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡﺷﺪﻩ ﺗﺤﺖ ﻋﻨﺎﻭﻳﻦ. ﻣﻲﺑﺎﺷﺪ ﺍﻃﻼﻋﺎﺕ ﺑﻪﺭﻭﺯ ﺭﺍ ﺩﺭ ﻣﻮﺭﺩ ﻣﺒﺎﺣﺚ ﻋﻤﺪﻩ ﻭ ﺑﺤﺚﺍﻧﮕﻴﺰ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺟﺪﻳﺪ ﻭ ﻧﻴﺰ ﺩﻳﺪﮔﺎﻩ ﺟﺪﻳﺪ ﻧﺴﺒﺖ ﺑﻪ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺎﻳﻊ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺭﺍ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ٢٠٠٣ ﺩﺭ ﺳﺎﻝENS ﻛﻪ ﺷﺎﻣﻞ ﻣﻘﺎﻻﺕ ﺩﻭﺭﺓ ﺁﻣﻮﺯﺷﻲ ﻛﻨﮕﺮﻩCD ﺍﻳﻦ . ﻣﺨﺘﻠﻒ ﻧﻴﺰ ﻣﻲﺑﺎﺷﺪTitle ﺯﻳﺮ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﻧﺪ ﻛﻪ ﻫﺮ ﻛﺪﺍﻡ ﺷﺎﻣﻞ ﭼﻨﺪ Dizziness and vesthg Neurogenetics for Clinicians Neuroimaging ICU in Neurology
25.9 EPILEPSY
Clinical Neurophysiology NeuroSurgery for Neurologist Neurology of Systemic disease Movement discords
The Comprehensive CD-ROM
Clinical Neuropathology Epilepsy Parkinson's diseane Neuroplathies
Sleep Disorder Multiple Sclerosis Ultrasound in Neurology Current Treatments Neurology
(Jerome Engel, Jr., M.D., Ph.D., Timothy A. Pedley, M.D.)
Stroke Muscle disorders Dementia
1999
Lippincott Williams & Wilkins
ﺗﻮﺍﻧـﺎﻳﻲ. ﮔﻨﺠﺎﻧـﺪﻩ ﺷـﺪﻩ ﺍﺳـﺖCD ﺩﺭimaging ﻋﻜـﺲ ﻭ٨٠٠ ﻫﻤﭽﻨـﻴﻦ. ﺳﺮﻓﺼـﻞ ﻣـﻲﺑﺎﺷـﺪ٢٨٩ ﻛﺘﺎﺏ ﺭﺍ ﺩﺭ ﺑﺮﻣﻲﮔﻴﺮﺩ ﻛﻪ ﻣﺸـﺘﻤﻞ ﺑـﺮFull text . ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖEpilepsy: A comprehensive textBook ﻛﻪ ﺑﺮﺍﺳﺎﺱ ﻛﺘﺎﺏCD ﺍﻳﻦ . ﺭﻓﺮﺍﻧﺲ ﻛﻪ ﺗﻮﺳﻂ ﻧﻮﻳﺴﻨﺪﻩ ﺟﻤﻊﺁﻭﺭﻱ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﺍﺯ ﻧﻘﺎﻁ ﻗﻮﺕ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩ٥٠٠ ﻭ ﺧﻼﺻﻪ ﻣﻘﺎﻻﺕ ﺑﻴﺶ ﺍﺯWeblink- Seasch 26.9 Essentials of Clinical Neurophysiology
2002
(Karl E. Misulis MD. PhD, Thomas C. Head MD)
27.9 Foundations of NEUROBIOLOGY
ــــ
28.9 Foundations of Behavioural Neuroscience
ــــ
. ﻗﺴﻤﺖ ﺯﻳﺮ ﺍﺳﺖ٥ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﺷﺎﻣﻞ، ﻭ ﺗﻜﻤﻴﻞ ﺍﻃﻼﻋﺎﺕ ﺍﻓﺮﺍﺩﻱ ﻛﻪ ﺑﺎ ﻋﻠﻮﻡ ﻣﺮﺑﻮﻁ ﺑﻪ ﺍﻋﺼﺎﺏ ﻭ ﺑﻴﻮﻟﻮﮊﻱ ﺳﺮﻭﻛﺎﺭ ﺩﺍﺭﻧﺪSelf evaluattion ﺑﻪ ﻣﻨﻈﻮﺭCD ﺍﻳﻦ . ﺧﻮﺩﺁﺯﻣﺎﻳﻲﻫﺎ ﻛﻪ ﻓﻬﺮﺳﺖﺑﻨﺪﻱ ﺷﺪﻩ ﻭ ﺟﻬﺖ ﺩﺍﺭﻧﺪ-١ ﺁﻣﺎﺩﮔﻲ ﺳﺨﻨﺮﺍﻧﻲ ﻛﻪ ﺑﻪ ﻣﺎ ﺍﻣﻜﺎﻥ ﻣﻲﺩﻫـﺪ ﺑـﺎ-٤ Expansion Module -٣ . ﺍﻧﻴﻤﻴﺸﻦﻫﺎ ﻭ ﻓﻴﻠﻢﻫﺎﻱ ﻭﻳﺪﺋﻮﻳﻲ ﺁﻣﻮﺯﻧﺪﻩ ﻭ ﺑﻴﺎﺩﻣﺎﻧﺪﻧﻲ ﺑﻪ ﻫﻤﺮﺍﻩ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺘﺒﻲ ﺭﺍﺟﻊ ﺑﻪ ﻫﺮ ﻗﻄﻌﻪ ﻓﻴﻠﻢ-٢ . ﻣﻌﺮﻓﻲ ﺷﺪﻩﺍﻧﺪ ﻭ ﻟﻴﻨﻚﻫﺎﻱ ﻣﺘﻌﺪﺩ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩﺍﻧﺪNeurobiology ﺳﺎﻳﺖﻫﺎﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﻋﻠﻮﻡ، CD ﺩﺭ ﺑﺨﺶ ﺩﻳﮕﺮﻱ ﺍﺯ. ﻣﺨﺼﻮﺹ ﺑﻪ ﺧﻮﺩ ﺭﺍ ﺳﺎﺧﺘﻪ ﻭ ﺟﻬﺖ ﺍﺭﺍﺋﻪ ﺩﺭ ﻛﻨﻔﺮﺍﻧﺲﻫﺎ ﻳﺎ ﺗﺪﺭﻳﺲ ﺍﺯ ﺁﻧﻬﺎ ﺑﻬﺮﻩ ﺑﺒﺮﻳﻢplay list ، CD ﺍﺷﻜﺎﻝ ﻭ ﻓﻴﻠﻢﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ
-Neural Communication -
. ﺑﺨﺶ ﻋﻤﺪﻩ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ٥ ﺷﺎﻣﻞCD ﺍﻳﻦ
Central Nervous system
-Research methods
-Visual System
- Control of movements
Quiz ﺩﺭ ﭼﻨﺪ ﻓﺼﻞ ﺳـﻮﺍﻻﺗﻲ ﺑـﻪ ﻋﻨـﻮﺍﻥ. ﻓﻬﺮﺳﺖ ﺩﺭﺧﺘﭽﻪﺍﻱ ﻣﻄﺎﻟﺐ ﻛﻤﻚ ﻣﻬﻤﻲ ﺑﻪ ﻳﺎﺩﮔﻴﺮﻱ ﻋﻠﻮﻡ ﭘﺎﻳﻪ ﺍﻋﺼﺎﺏ ﻣﻲﻧﻤﺎﻳﺪ. ﻛﺎﻣﻞ ﻣﻲﺑﺎﺷﺪglossary , Search ﻫﻤﺮﺍﻩ ﺑﺎ ﻣﻮﺗﻮﺭ.ﺣﺎﻭﻱ ﺗﺼﺎﻭﻳﺮﻱ ﺑﺎ ﻃﺮﺍﺣﻲ ﻋﺎﻟﻲ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺭﺍﺣﺖ ﺟﻬﺖ ﻓﻬﻢ ﺟﺰﺋﻴﺎﺕ ﭘﻴﭽﻴﺪﻩ ﻭ ﺭﻳﺰ ﺳﺎﺧﺘﻤﺎﻥﻫﺎﻱ ﻧﻮﺭﻭﻧﻲ ﻣﻲﺑﺎﺷﺪ
.ﻣﻄﺮﺡ ﺷﺪﻩﺍﻧﺪ ﻛﻪ ﺟﻬﺖ ﺗﻜﻤﻴﻞ ﺁﻣﻮﺧﺘﻪﻫﺎ ﻭ ﻳﺎﺩﮔﻴﺮﻱ ﻣﻨﺎﺳﺐ ﺍﺳﺖ 29.9 FUNDAMENTALS OF HUMAN NEURAL STRUCTURE (S. Mark Williams) (Sylvius 30.9 General depression and its pharmacological treatment (Professor Brain Leonard)
TM
ــــ
2.0)
(VCD)
31.9 Guidelines (American Academy of Neurology) (SALEKAN E-BOOK) . ﺑﺎ ﺩﺳﺘﺮﺳﻲ ﺁﺳﺎﻥ ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻛﺎﺭﺑﺮ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪOffline ﺩﺭ ﺁﻣﺪﻩ ﺍﺳﺖ ﻛﻪ ﻛﻠﻴﻪ ﻣﻘﺎﻻﺕ ﺭﺍ ﺑﻪ ﺻﻮﺭﺕSalekan E-Book ﺩﺭ ﻗﺎﻟﺐSearch ﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺩﺭﻣﺎﻧﻲ ﺁﻛﺎﺩﻣﻲ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺁﻣﺮﻳﻜﺎ ﻣﻲﺑﺎﺷﺪ ﺑﻪ ﺻﻮﺭﺕ ﻓﺎﻳﻞ ﻗﺎﺑﻞGuidline ﻛﻪ ﺷﺎﻣﻞ ﺁﺧﺮﻳﻦCD ﺍﻳﻦ - Brain Injury & Brain Death - Child Neurology
- Dementia
- Epilepsy
32.9 Human Brain Cancer: Diagnostic Decisions 33.9 Interactive Guide to Human Neuroanatomy Atlas: -Surface Anatomy of Brain Exam:I -Surface Anatomy of the Brain
- Headache - Movement Disorders - Multiple Sclerosis
(Lauren A. Langford, MD, Dr. med,)
- Neuroimaging
- Neuromuscular
- Stroke and Vascular Neurology
-Technology Assessment
American Medical Association
ــــ 2002
(Mark F. Bear, Barry W. Connors, Michael A. Paradiso)
-Cross-Sectional Anatomy of Brain -Cross-Sectional Anatomy of the Brain
2004
-The Spinal Cord -The Anatomy Nervous System -Comprehensive Exam
-The Cranial Nerves -The Blood Supply to the Brain
34.9 ICU Syllabus
ــــ
٢٠٠٤ ﺍﺯ ﻣﻨـﺎﺑﻊ ﻭ ﻣﺠـﻼﺕ ﻣﺨﺘﻠـﻒ ﺗـﺎ ﺳـﺎﻝICU Patient Care ﺁﺧﺮﻳﻦ ﻣﻘﺎﻻﺕ ﻣﻨﺘﺸﺮﻩ ﻭ ﻧﻴﺰ ﻣﻘﺎﻻﺕ ﻣﻬﻢ ﻗﺒﻠﻲ ﺩﺭ ﺯﻣﻴﻨﻪﻫﺎﻱ ﻣﺨﺘﻠـﻒ، ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ، ﺳﺮﻭﻛﺎﺭ ﺩﺍﺭﻧﺪICU ﻛﻪ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﭘﺰﺷﻜﺎﻧﻲ ﻛﻪ ﺑﺎ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺪﺣﺎﻝ ﻭ ﺑﺴﺘﺮﻱ ﺩﺭCD ﺩﺭ ﺍﻳﻦ : ﺳﺮﻓﺼﻞﻫﺎﻱ ﻋﻤﺪﻩ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ. ﻗﻮﻱ ﺍﺟﺮﺍ ﺷﺪﻩ ﺍﺳﺖSearch ﺑﺎ ﻗﺎﺑﻠﻴﺖPDF ﺟﻤﻊﺁﻭﺭﻱ ﻭ ﺑﻪ ﺻﻮﺭﺕ ﻓﺎﻳﻞ Anemia and blood Transfusion Hyperghycemia and Ihsulia Non invasive Ventilation
ARDS Hypothermia for cardiac arrest Nutritions
35.9 InterBRAIN (Martin C. hirsh) (Springer) 1. Gross Anatomy
2. Vessels and Meninges
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
3. Brain Slices
Ethics Impaired cognition Pneumonia
Fever Wokup Liver disease Pulmonary Embolism
Hemodynamics Mechanical Vetitation Renal failure
RARS Sedation Sepsis
Weaning From Mechanical Vetitation
ــــ 4. Microscopical Sections
5. Functional Systems
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
48 2003
36.9 International Symposium ON 10 Years Betaferon
CDﻓﻮﻕ ﻛﻪ ﻣﺎﺣﺼﻞ ﺳﻤﭙﻮﺯﻳﻮﻡ ﭘﺮﺍﮒ ﺩﺭ ﺳﺎﻝ ٢٠٠٣ﺩﺭ ﻣﻮﺭﺩ ﺗﺠﺮﺑﻪ ﺩﻩﺳﺎﻟﺔ ﻣﺼﺮﻑ ﺑﺘﺎﻓﺮﻭﻥﻫﺎ ﺩﺭ ﺩﺭﻣﺎﻥ MSﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ ﺗﻤﺎﻡ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ ﻛﻨﮕﺮﻩ ﺍﺳﺖ .ﻋﻨﺎﻭﻳﻦ ﻣﺒﺎﺣﺚ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺗﺰ: ﺩﺭﻣﺎﻥ ﺳﻤﭙﺘﻮﻣﺎﺗﻴﻚ ﻭ ﺗﻮﺍﻧﺒﺨﺸﻲ ﺩﺭ MS
ﺍﻓﻖﻫﺎﻱ ﺟﺪﻳﺪ
Geomics and Proteomics
ﺁﻣﻮﺧﺘﻪﻫﺎﻱ ﻣﺎﻟﻮﺯ ﻣﻄﺎﻟﻌﺎﺕ ﺑﺎﻟﻴﻨﻲ ﺩﺭﺑﺎﺭﺓ ﻓﺎﻛﺘﻮﺭﻫﺎﻱ ﭘﺮﻭﮔﻨﻮﺳﺘﻴﻚ ﺍﻳﻨﺘﺮﻓﺮﻭﻥ ﺩﻭﺯ ﺑﺎﻻ ﻳﺎ ﭘﺎﻳﻴﻦ؟
ﻧﺘﺎﻳﺞ ﻣﻄﺎﻟﻌﺎﺕ BENEFITﻭ BEYOND
ﺍﻫﻤﻴﺖ ﺑﺎﻟﻴﻨﻲ ﻳﺎﻓﺘﻪﻫﺎﻱ ﻧﺮﻭﭘﺎﺗﻮﻟﻮﮊﻳﻚ MS
ﺗﺎﺭﻳﺨﭽﺔ ﺩﺭﻣﺎﻥ ﻣﺪﺭﻥ MS
ﻧﻘﺶ Stem Cell Transplantﺩﺭ ﺩﺭﻣﺎﻥ Aggressive MS
ﺑﺘﺎﻓﺮﻭﻥ ﺩﺭ ﺩﺭﻣﺎﻥ Primary Progressive MS
37.9 MANAGING STRESS
2002 ــــ
)38.9 Manual of Pain Management (Carol A. Warfield, Hilary J. Fausett
)(Second Edition) (SALEKAN E-BOOK ﺍﻳﻦ CDﺑﺎ ﻓﺮﻣﺖ ﺧﺎﺹ ﺧﻮﺩ ﻛﻪ ﻧﺤﻮﺓ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﻥ ﺭﺍ ﺭﺍﺣﺖ ﻧﻤﻮﺩﻩ ﺍﺳﺖ .ﺯﻣﻨﻴﺔ ﻛﺎﻣﻠﻲ ﺑﺮﺍﻱ ﻣﻄﺎﻟﻌﻪ ﻧﺤﻮﺓ ﺍﺩﺍﺭﻩ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ ﺩﺭﺩﻫﺎﻱ ﻗﺴﻤﺖﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺭﺍ ﻓﺮﺍﻫﻢ ﻣﻲﺁﻭﺭﺩ .ﺩﺭ ﻓﺼﻞ ﺍﻭﻝ ﻧﻈﺮﻳﻪﻫﺎﻱ ﻋﻤﺪﺓ ﻓﻴﺰﻭﻟﻮﮊﻱ ﺩﺭﺩ ﻣﻄﺮﺡ ﺷﺪﻩ ﺍﺳﺖ. ﻋﻤﺪﻩ ﺍﻳﻦ CDﺗﻮﺻﻴﻔﻲ ﺍﺯ ﺳﻨﺪﺭﻡﻫﺎﻱ ﺷﺎﻳﻊ ﺩﺭﺩ ﺍﺳﺖ ﻛﻪ ﺑﺮ ﺍﺳﺎﺱ ﺁﻧﺎﺗﻮﻣﻲ ﺑﺎﻟﻴﻨﻲ ﻛﻼﺳﻪﺑﻨﺪﻱ ﺷﺪﻩﺍﻧﺪ .ﻓﺼﻞ ﺑﻌﺪﻱ ﺑﺮ ﺭﻭﻱ ﺩﺭﻣﺎﻥﻫﺎ ﻭ Procedureﻫﺎﻳﻲ ﻛﻪ ﺑﺮ ﺭﻭﻱ ﺑﻴﻤﺎﺭﻳﺎﻥ ﺩﺭﺩﻣﻨﺪ ﺑﻪ ﻛﺎﺭ ﻣﻲﺭﻭﻧﺪ ،ﻣﺘﻤﺮﻛﺰ ﻛﺮﺩﻩ ﺍﺳـﺖ .ﺩﺭﻣـﺎﻥ ﺩﺭﺩ ﻛﻮﺩﻛـﺎﻥ ،ﺳـﺎﻟﻤﻨﺪﺍﻥ ﻭ ﻧﻴـﺰ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ HIVﻧﻴﺰ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. -Pain Management
ــــ
-Common Painful Syndromes
)(CD I, II , III , IV
-Understanding pain
-Pain by Anatomic Location
)39.9 Microneurosurgery (M. G. Yasargil) Cassette 1 Aneurysms (VCD) (Thieme AV
2001
)40.9 Migraine Current Approaches To Treatment (Dr. Andrew Dowson
2002
)41.9 Movement Disorders Society Official Journal of The Movement Disorder Society Published by John Wiley & Sons, Ins VCD (I, II
2002
)42.9 Needle Electromyography (Daniel Dumitru, M.D., PhD. ﺍﻳﻦ CDﻛﻪ ﺑﺮ ﺍﺳﺎﺱ ﻛﺘﺎﺏ Needle EMGﻧﻮﺷﺘﺔ Daniel Dumitruﺩﺭ ﺳﺎﻝ ٢٠٠٢ﻃﺮﺍﺣﻲ ﻭ ﺍﺟﺮﺍ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ﻣﺘﻦ ﻛﺘﺎﺏ ﺑﻌﻼﻭﺓ EMG Video Libraryﺍﺳﺖ ٣٣ .ﻓﺎﻳﻞ ﻣﺨﺘﻠﻒ ﺷﺎﻣﻞ ﺍﻣﻮﺍﺝ ﻧﺮﻣﺎﻝ ﻭ ﻏﻴﺮﻧﺮﻣﺎﻝ ﻣﺨﺘﻠﻒ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ. ﺗﺼﺎﻭﻳﺮ ﺍﺭﺍﺋﻪﺷﺪﻩ ﺍﻃﻼﻋﺎﺕ ﻛﺎﻓﻲ ﺩﺭ ﻣﻮﺭﺩ ﻧﺤﻮﺓ ﺍﺟﺮﺍﻱ EMGﻭ Pitfullﻫﺎﻱ ﺁﻥ ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻗﺮﺍﺭ ﻣﻲﺩﻫﻨﺪ .ﻗﺎﺑﻠﻴﺖ Glossary , Searchﻗﻮﻱ ﻧﻴﺰ ﺍﺯ ﻣﺰﺍﻳﺎﻱ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻓﻮﻕ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩ.
1999
)43.9 NEUROANATOMY-3D-Stereoscopic Atlas of the Human Brain (Martin C. Hirsch, Thomas Kramer) (Springer ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺗﺼﺎﻭﻳﺮ ﺳﻪ ﺑﻌﺪﻱ ﻭ ﺑﺴﻴﺎﺭ ﺩﻗﻴﻘﻲ ﺍﺯ ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﻣﺮﻛﺰﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﻗﺪﺭﺕ ﺑﺎﻻﻱ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻗﺎﺩﺭﻳﻢ ﺍﺯ ﻫﺮ ﺟﻬﺖ ﺩﻟﺨﻮﺍﻩ ﺑﻪ ﺗﺼﻮﻳﺮ Grossﻣﻐﺰ ﺑﻨﮕﺮﻳﻢ .ﺑﺎ ﺩﺭﻧﻈﺮﮔﺮﻓﺘﻦ ﺍﻳﻨﻜﻪ ﺗﻚ ﺗﻚ ﺍﺟﺰﺍﻱ ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﺭﺍ ﻣﺮﺣﻠﻪ ﺑﻪ ﻣﺮﺣﻠﻪ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﺗﺼﻮﻳﺮ ﻗﺒﻠﻲ ﺍﺿﺎﻓﻪ ﻭ
ﻳﺎ ﻛﻢ ﻛﺮﺩ ،ﺟﺰﺋﻴﺎﺕ ﺍﺭﺗﺒﺎﻃﺎﺕ ﺳﻴﺴﺘﻢﻫﺎﻱ ﻋﻤﻠﻜﺮﺩﻱ ﻣﺨﺘﻠﻒ ﺑﻪ ﻭﺿﻮﺡ ﻣﺸﺨﺺ ﻣﻲﺷﻮﺩ .ﺗﺼﺎﻭﻳﺮ ﻭ ﺑﺮﺵﻫﺎ ﺑﺴﻴﺎﺭ ﻫﻮﺷﻤﻨﺪﺍﻧﻪ ﻭ ﻫﻨﺮﻣﻨﺪﺍﻧﻪ ﻃﺮﺍﺣﻲ ﮔﺸﺘﻪﺍﻧﺪ ﻭ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ،ﭘﺰﺷﻜﺎﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺩﺭﮔﻴﺮ ﺑﺎ ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﺁﻧﺮﺍ ﺗﺠﺮﺑﺔ ﺟﺪﻳﺪﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺮﺩﻩﺍﻧﺪ. ــــ
44.9 Neurofunctional Systems 3D
ــــ
)45.9 Neurological surgery (julian R. Youmans , MD Editor-in-Chief) (Fourth Edition) (Y.O.U.M.A.N.S
2001
)46.9 Neurology (Baker's clinical on CD-ROM
2002
47.9 New Analgesic Options: Overcoming Obstacles to Pain Relief -References
-Trauma
-Post Op Pain
-OA Pain
-Back Pain -Fibromyalgia
-Pharmacist Answer Sheet
- MD, NP, PA, RN Answer Sheet
25.7 Photographic manual of Regional Orthopaedic and Neurological Tests
ــــ
ﺍﻳﻦ CDﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ ٨٥٠ﺗﺼﻮﻳﺮ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﺗﻤﺎﻡ ﻣﻌﺎﻳﻨﺎﺕ ﻧﻮﺭﻭﻟﻮﮊﻳﻚ ﻭ ﺍﺭﺗﻮﭘﺪﻳﻚ ﺭﺍ ﺑﺎ ﺟﺰﺋﻴﺎﺕ ﺗﻤﺎﻡ ﺭﻭﺷﻦ ﻣﻲﺳﺎﺯﺩ .ﺩﺭ ﻣﻮﺍﻗﻊ ﻟﺰﻭﻡ ﺗﺼﺎﻭﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻚ ﺿﺮﻭﺭﻱ ﻧﻴﺰ ﺍﺿﺎﻓﻪ ﺷﺪﻩﺍﻧﺪ .ﻓﺼﻮﻝ ﺑﺮ ﺍﺳﺎﺱ ﻣﺤﻞ ﻣﻮﺭﺩ ﻣﻌﺎﻳﻨﻪ ﻃﺮﺍﺣﻲ ﻭ ﻗﺴﻤﺖﺑﻨﺪﻱ ﺷﺪﻩﺍﻧـﺪ. ﻣﻌﺎﻳﻨﺎﺕ ﺍﺯ ﻓﻘﺮﺍﺕ ﮔﺮﺩﻧﻲ ﻭ ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ ﺷﺮﻭﻉ ﻭ ﺑﻪ ﻓﻘﺮﺍﺕ ﻛﻤﺮﻱ ﻭ ﺍﻧﺪﺍﻡﻫﺎﻱ ﺗﺤﺘﺎﻧﻲ ﺧﺘﻢ ﻣﻲﺷﻮﻧﺪ .ﻫﺮ Testﺩﺭ ﻳﻚ ﺻﻔﺤﻪ ﻳﺎ ﺩﻭ ﺻﻔﺤﻪ ﻣﻘﺎﺑﻞ ﻫﻢ ﺑﺎ ﻋﻜﺲﻫﺎﻳﻲ ﻛﻪ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻣﻌﺎﻳﻨـﻪ ﺭﺍ ﺑﻮﺿـﻮﺡ ﻧﺸـﺎﻥ ﻣـﻲﺩﻫﻨـﺪ ﺗﻮﺿـﻴﺢ ﺩﺍﺩﻩ ﺷـﺪﻩ ﺍﺳـﺖ .ﺩﺭ ﺿـﻤﻦ ﻳـﻚ Sensitivity/Relialility Scaleﻧﻴﺰ ﺑﺮﺍﻱ ﻫﺮ ﻣﻌﺎﻳﻨﻪ ﺗﻌﺮﻳﻒ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻣﻴﺰﺍﻥ ﺣﺴﺎﺳﻴﺖ ﻭ ﻗﺎﺑﻠﻴﺖ ﺍﻋﺘﻤﺎﺩ ﺑﻪ ﺁﻥ ﻣﻌﺎﻳﻨﻪ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﺳﺎﺯﺩ .ﺍﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺩﺭ ﺑﻜﺎﺭﮔﻴﺮﻱ ﺗﺴﺖﻫﺎﻱ ﺣﺴﺎﺳﺘﺮ ﻭ ﺍﺧﺘﺼﺎﺹﺗﺮ ﻛﻤﻚ ﻓﺮﺍﻭﺍﻥ ﺑﻪ ﭘﺰﺷﻚ ﻣﻲﻧﻤﺎﻳﺪ. 1998
)48.9 Principles of Neurology (6th Edition) (Raymond D. Adams, M.A., M.D. 49.9 PROFESS
ــــ
ﺍﻳﻦ CDﻛﻪ ﻣﺎﺣﺼﻞ ﺳﻤﭙﻮﺯﻳﻮﻡ ﭘﻴﺸﮕﻴﺮﻱ ﺍﺯ ﺳﻜﺘﻪﻫﺎﻱ ﻣﻐﺰﻱ ﺩﺭ International Stroke Conferenceﺩﺭﺁﺭﻳﺰﻭﻧﺎﻱ ﺍﻣﺮﻳﻜﺎ ﺩﺭ ﺳﺎﻝ ٢٠٠٣ﻣﻲﺑﺎﺷﺪ ﭼﺎﻟﺶﻫﺎﻱ ﭘﻴﺶﺭﻭ ﺩﺭ ﺩﺭﻣﺎﻥ ﻭ ﭘﻴﺸﮕﻴﺮﻱ ﺍﺯ ﺳﻜﺘﻪﻫﺎﻱ ﻣﺠﺪﺩ ﻣﻐﺰﻱ ﺭﺍ ﻣﻄﺮﺡ ﻛﺮﺩﻩ ﻭ ﺁﺧﺮﻳﻦ ﺭﮊﻳﻢﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﻭﻳﺮﻭﺗﺮﻛﻞﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺭﺍ ﺩﺭ ﻗﺎﻟﺐ Lectureﻫﺎ ،ﺳﺆﺍﻝ ﻭ ﺟﻮﺍﺏ ﻭ ﺧﻼﺻﻪ ﻣﻘﺎﻻﺕ ﺍﺭﺍﺋﻪ ﻛﺮﺩﻩ ﺍﺳﺖ .ﻓﻬﺮﺳﺖ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: ﺍﻃﻼﻋﺎﺗﻲ ﻛﻪ ﺩﺭﺑﺎﺭﺓ ﺩﻳﭙﺮﻳﺪﺍﻣﻮﻝ ﻭﺟﻮﺩ ﺩﺍﺭﺩ - .ﭼﺮﺍ ﺑﺮﺧﻮﺭﺩ ﺑﺎ CVAﻣﺘﻔﺎﻭﺕ ﺍﺯ MIﺍﺳﺖ - .ﺁﻳﺎ ﺩﺭﻣﺎﻥ ﻣﺮﻛﺐ ﺁﻧﺘﻲﭘﻜﺪﺗﻲ ﺧﻄﺮﻧﺎﻙ ﺍﺳﺖ ﻳﺎ ﻣﻔﻴﺪ؟ -ﺁﻳﺎ ﺁﻧﮋﻳﻮﺗﺎﻧﻴﻦ IIﺩﻳﺴﻜﺎﻓﺎﻛﺘﻮﺭ ﻣﺴﺘﻘﻠﻲ ﺑﺮﺍﻱ ﺳﻜﺘﻪ ﺍﺳﺖ؟ -ﺭﮊﻳﻢ ﺩﺭﻣﺎﻧﻲ ﭘﻴﺸﮕﻴﺮﻱ ﺍﺯ ﺳﻜﺘﻪ ﺩﻭﻡ.ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
49 2000
50.9 Psychotropics
2001
)51.9 Recognizing Extrapyramidal Symptoms (VCD
ﺩﺍﻳﺮõﺍﻟﻤﻌﺎﺭﻑ ﻛﺎﻣﻠﻲ ﺍﺯ ﺗﻤﺎﻡ ﻣﻮﺍﺩ ﻭ ﺩﺍﺭﻭﻫﺎﻱ ﻣﻮﺛﺮ ﺑﺮ ﺳﻴﺴﺘﻢ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺷﺎﻣﻞ ﺑﺨﺸﻬﺎﻱ ﺯﻳﺮ ﻣﻲﺷﻮﺩ :ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﺭﻭﻳﻲ -ﻋﻮﺍﺭﺽ ﺟﺎﻧﺒﻲ -ﺗﺪﺍﺧﻼﺕ ﺩﺍﺭﻭﻳﻲ -ﻓﻬﺮﺳﺖ ﺍﺳﺎﻣﻲ ﺭﺍﻳﺞ ﺧﻴﺎﺑﺎﻧﻲ ﺩﺍﺭﻭﻫﺎ -ﺍﺻﻮﻝ ﺗﺮﻙ ﺩﺍﺭﻭ ،ﻣﻨﺤﻨﻲﻫﺎﻱ ﻧﻴﻤﻪ ﻋﻤﺮ ﺩﺍﺭﻭﻳﻲ -ﺍﻳﻨﺪﻛﺲ ﺑﺎ ﻣﺮﺍﺟﻌﻪ ﺑﻪ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﻣﻨﻮﮔﺮﺍﻑﻫﺎ ﻣﻲﺗﻮﺍﻥ ﺍﺯ ﺳﺎﺧﺘﻤﺎﻥ ﺷﻴﻤﻴﺎﻳﻲ -ﻓﺮﻣﻮﻝ ﺷﻴﻤﻴﺎﻳﻲ -ﻣﻮﺍﺭﺩ ﻭ ﻧﺤﻮﺓ ﺍﺳﺘﻔﺎﺩﺓ ﺑﺎﻟﻴﻨﻲ ﺷﺮﻛﺖﻫﺎﻱ ﺳﺎﺯﻧﺪﻩ ﻭ ﻧﺎﻡﻫﺎﻱ ﺗﺠﺎﺭﻱ ﻭ ﻧﻴﺰ ﺭﻓﺮﻧﺲﻫﺎﻱ ﻣﻄﺎﻟﻌﺎﺗﻲ ﻫﺮ ﻣﺎﺩﺓ ﺳﺎﻳﻜﻮﺗﺮﻭﭖ ﺍﻃﻼﻉ ﭘﻴﺪﺍ ﻛﺮﺩ. - and Tardive- Dyskinesia
ﻣﺒﺎﺣﺚ ﺍﻳﻦ CDﺷﺎﻣﻞ:
- Parkinsonism
- Akathisia
2001
- Clinical Examples of Acute Dystonia
52.9 Rune Aaslid TCD Simulator Version 2.1
ﺍﻳﻦ ﻧﺮﻡ ﺍﻓﺰﺍﺭ ﻳﻚ ﺷﺒﻴﻪ ﺳﺎﺯ ﺑﺮﺭﺳﻲﻫﺎﻱ ﺩﺍﭘﻠﺮ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻭﺍﻛﺴﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﻮﺳﻂ ﻣﺨﺘﺮﻉ ، TCDﺁﻗﺎﻱ Rune Aaslidﺩﺭ ﺍﻳﻦ CDﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ﻣﺘﻨﻲ ﺍﺳﺖ ﻛﻪ ﻧﺤﻮﺓ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ CDﺭﺍ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﺪ .ﺍﺻﻮﻝ ﺩﺍﭘﻠﺮ ﺳـﻮﻧﻮﮔﺮﺍﻓﻲ- ﺁﻧﺎﺗﻮﻣﻲ -ﻫﻤﻮﺩﻳﻨﺎﻣﻴﻚ ﻭ ﻣﻮﺍﺭﺩ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻋﺮﻭﻕ ﻣﻐﺰﻱ ﺭﺍ ﺗﻮﺿﻴﺢ ﻣﻲﺩﻫﺪ .ﻗﺎﺑﻠﻴﺖﻫﺎﻱ ﻓﺮﺍﻭﺍﻧﻲ ﺍﺯ ﺟﻤﻠﻪ ﺍﻳﻦ ﻣﻮﺍﺭﺩ ﺭﺍ ﺩﺍﺭﺍ ﺍﺳﺖ :ﻧﻤﺎﻳﺶ ﺍﺳﭙﻜﺘﺮﻭﻡ ﺩﺍﭘﻠﺮ -ﻧﻤﺎﻳﺶ ﻣﺤﻞ ﺗﺎﺑﺶ ﻭ ﺯﺍﻭﻳﻪ ﺗﺎﺑﺶ ﺍﻣﻮﺍﺝ -ﻣﻮﻧﻴﺘﻮﺭﻳﻨﮓ -ﺗﺼﻮﻳﺮ – CBFﺁﻧـﺎﺗﻮﻣﻲ ﻭ ﭘـﺎﺗﻮﻟﻮﮊﻱﻫـﺎﻱ ﻣﺨﺘﻠـﻒ، ﻛﻨﺘﺮﻝ ﻛﺎﺭﺩﻳﻮ ﻭﺍﺳﻜﻮﻻﺭ -ﺗﺄﺛﻴﺮ ﺗﻐﻴﻴﺮ ﺿﺮﺑﺎﻥ ﻗﻠﺐ -ﺗﺄﺛﻴﺮ ﺗﻐﻴﻴﺮ ﺗﻨﻔﺲ HITS -ﻭ ﺑﺎﻻﺧﺮﻩ ﺩﻳﺪ ﺳﻪ ﺑﻌﺪﻱ ﻛﻪ ﺗﺠﺴﻢ ﻣﻮﻗﻌﻴﺖ ﻓﻀﺎﻳﻲ ﻋﺮﻭﻕ ﺩﺭ ﺩﺍﺧﻞ ﺟﻤﺠﻤﻪ ﺭﺍ ﺳﻬﻞ ﻣﻲﻧﻤﺎﻳﺪ .ﺍﻳﻦ CDﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﻭ ﻣﺆﺛﺮﺗﺮﻳﻦ ﺍﺑﺰﺍﺭﻫﺎﻱ ﺁﻣﻮﺯﺵ TCDﺍﺳﺖ ﻛﻪ ﺗﻮﺳـﻂ ﺍﺳـﺎﺗﻴﺪ ﻭ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ .ﻣﻔﺎﻫﻴﻢ ﭘﻴﭽﻴﺪﻩ ﺩﺍﭘﻠﺮ ﻋﺮﻭﻕ ﻣﻐﺰﻱ ﺭﺍ ﺑﺼﻮﺭﺕ ﻣﻠﻤﻮﺱ ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻋﻼﻗﻪﻣﻨﺪﺍﻥ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ. ــــ
ــــ
53.9 Stroke Overview of Stroke: 1. Stroke in Perspective 2. Pathogenesis & Pathophysiology 3. Evaluation & Diagnosis 4. Interventions 5. Thrombolytic Therapy Studies IV Tissue Plasminogen Activator(t-PA) Studies: 1. Recent Multicenter, IV Streptokinase (SK) Studies Ultra Rapid Response: 1. Increasing Public/Professional Awareness 2. Modifying Care Patterns 3. Stroke Care Systems 4. Assessing Critical Resources Case Studies 31.7 SPINE implants )(CD I , II
: CD Iﺩﺭ ﺍﻳﻦ CDﻧﺤﻮﺓ ﺟﺮﺍﺣﻲ ﻭ ﺑﻪﻛﺎﺭﮔﺬﺍﺷﺘﻦ ﭘﺮﻭﺗﺰﻫﺎﻱ ﻣﻬﺮﻩ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﻭ ﺍﻃﻼﻋﺎﺕ ﻛﺎﻣﻠﻲ ﺭﺍﺟﻊ ﺑﻪ ﭘﺮﻭﺗﺰﻫﺎﻱ ﺟﺎﻧﺸﻴﻦ ﺟﺴﻢ ﻣﻬﺮﻩ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. : CD IIﺩﺭ ﺍﻳﻦ CDﻧﺤﻮﻩ ﺟﺮﺍﺣﻲ ﻭ ﺑﻜﺎﺭﮔﺬﺍﺷﺘﻦ ﺩﺳﺘﮕﺎﻩ Diapasone-hookﺑﺮ ﺭﻭﻱ ﻣﻬﺮﻩﻫﺎﻱ ﻛﻤﺮﻱ ﺩﺭ ﺩﺭﻣﺎﻥ ﻣﻮﺍﺭﺩ ﺗﺮﻭﻣﺎﺗﻴﻚ ﻭ ﺍﺳﻜﻮﺍﻧﻴﻮﺭ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. 1999 ــــ
)54.9 TEXTBOOK of CLINICAL NEUROLOGY (Christopher G. Goetz, MD, Eric J. Pappert, MD) (W.B. Saunders Company
)Atlas of Brain Anatomy An interactive tool for students, teachers, and researchers (Wieslaw L. Nowinski, A. Thirunavuukarasuu, R. Nick Bryan ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺗﺼﺎﻭﻳﺮ MRIﺩﺭ ﺳﻪ ﺟﻬﺖ ،ﻃﺮﺍﺣﻲﻫﺎﻱ ﺭﻧﮕﻲ ﻭ ﺳﻴﺴﺘﻢ ﻧﺎﻣﮕﺬﺍﺭﻱ ﻣﺎ ﺭﺍ ﻗﺎﺩﺭ ﻣﻲﺳﺎﺯﺩ ﺑﺮﺍﺣﺘﻲ ﻫﺮ ﺳﺎﺧﺘﻤﺎﻥ ﺩﺍﺧﻠﻲ ﻣﻐﺰﻱ ﺭﺍ ﺩﺭ ٣ﺟﻬﺖ ﺑﻄﻮﺭ ﻫﻤﺰﻣﺎﻥ ﻣﺸﺎﻫﺪﻩ ﻧﻤﺎﻳﻴﻢ .ﺟﻬﺖ ﺗﺠﺴﻢ ﻓﻀﺎﻳﻲ ﺑﻬﺘﺮ ﻭ ﻋﻤﻠﻴﺎﺕ ﺍﺳﺘﺮﺗﻮﺗﺎﻛﺴﻲ ﻣـﻲﺗـﻮﺍﻥ Gridﺧﺎﺻﻲ ﺭﺍ ﺑﺮ ﺭﻭﻱ ﺗﺼﻮﻳﺮ ﻗﺮﺍﺭ ﺩﺍﺩ ﻭ ﻓﺎﺻﻠﻪﻫﺎﻱ ﺩﻟﺨﻮﺍﻩ ﺭﺍ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﻧﻤﻮﺩ .ﺩﺭ ﻗﺴﻤﺖ ﺗﺴﺖ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕ interactiveﻭ ﺑﺴﻴﺎﺭ ﺟﺬﺍﺏ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﺍﺭﺯﻳﺎﺑﻲ ﻣﻔﺎﻫﻴﻢ ﻭ ﺁﻣﻮﺧﺘﻪﻫﺎ ﻣﻘﺪﻭﺭ ﻣﻲﮔﺮﺩﺩ .ﺩﺭ ﻗﺴﻤﺖ Glossoryﺗﻮﺿﻴﺢ ﻛﺎﻣﻠﻲ ﺭﺍﺟﻊ ﺑﻪ ﻫﺮ ﻛﺪﺍﻡ TM
55.9 The Cerefy
ﺍﺯ ﻣﻨﺎﻃﻖ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻣﻮﺭﺩ ﺍﺷﺎﺭﻩ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ CDﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺍﻓﺮﺍﺩﻳﻜﻪ ﻧﻮﺭﻭﺁﻧﺎﺗﻮﻣﻲ ،ﻧﺮﻭﻟﻮﮊﻱ -ﺟﺮﺍﺣﻲ ﺍﻋﺼﺎﺏ -ﻧﺮﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ -ﻋﻠﻮﻡ ﻧﺮﻭﺳﺎﻳﻨﺲ ﻭ ﺭﻭﺍﻧﭙﺰﺷﻜﻲ ﻣﻲﺁﻣﻮﺯﻧﺪ ﻳﺎ ﺁﻣﻮﺯﺵ ﻣﻲﺩﻫﻨﺪ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ. )56.9 The Clinical Diagnosis of Alzheimer's Disease (An Interactive Guide for Family Physician
ــــ
ﺗﻮﺳﻂ ﮔﺮﻭﻩ Alzheimer disease groupﺑﻴﻤﺎﺭﺳﺘﺎﻥ RiverViewﻛﺎﻧﺎﺩﺍ ﺗﻬﻴﻪ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﭼﻨﺪﻳﻦ ﻗﻄﻌﻪ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺭﺍﺟﻊ ﺑﻪ ﻧﺤﻮﺓ ﻣﺼﺎﺣﺒﻪ ﺑﺎ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ ﺁﻟﺰﺍﻳﻤﺮ ﻭ Flowchart
ﺗﺸﺨﻴﺺ ﺑﺎﻟﻴﻨﻲ
ﺑﺮﺭﺳﻲ ﺁﺯﻣﺎﻳﺸﮕﺎﻫﻲ
ﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ
ﻣﻌﺮﻓﻲ
ﺗﺸﺨﻴﺼﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﭼﻨﺪﻱ ﻣﻲﺑﺎﺷﺪ .ﺷﺎﻣﻞ ٨ﻣﺒﺤﺚ ﻋﻤﺪﺓ ﺯﻳﺮ ﺍﺳﺖ:
Case Studies
ﺑﺮﺭﺳﻲ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ
)(Marion Hall David Robinson
ــــ
ﺑﺮﺭﺳﻲ ﺷﻨﺎﺧﺘﻲ
ﺷﺮﺡ ﺣﺎﻝ
57.9 THE HUMAN BRAIN
ــــ
)58.9 THE HUMAN NERVOUS SYSTEM (Springer
ــــ
)59.9 The Massachusetts General Hospital Handbook of Pain Management (Second Edition
)(Jane Ballantyne, Scott M. Fishman, Salahadin Abdi) (SALEKAN-E-book II. Diagnosis of Pain III. Therapeutic Options: Pharmacologic Approaches IV. Therapeutic Options: Nonpharmacologic Approaches I. General Considerations V. Acute Pain VI. Chronic Pain VII. Pain Due to Cancer VIII. Special Situations - Apendices - Subject Index
2002
60.9 The Movement Disorder Society's Guide to Botulinum Toxin Injections
CDﺍﻭﻝ :ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺵ ﻧﺤﻮﺓ ﺗﺰﺭﻳﻖ ﺑﻮﺗﻮﻟﻴﻨﻮﻡ ﺗﻮﻛﺴﻴﻦ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﻛﺎﺩﺭ ﺍﻭﻝ ﺗﺼﻮﻳﺮ ﻛﻠﻲ ﺑﺪﻥ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﻛﻪ ﻗﺴﻤﺖ ﻣﻮﺭﺩ ﻧﻈﺮ ﺟﻬﺖ ﺗﺰﺭﻳﻖ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻣﻲﻧﻤﺎﻳﻲ .ﻋﻀﻼﺕ ﻭ ﺳﻨﺪﺭﻡﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻥ ﻗﺴﻤﺖ ﻓﻌﺎﻝ ﻣﻲﺷﻮﻧﺪ .ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﺳﻨﺪﺭﻡ ﺑﺎﻟﻴﻨﻲ ﻳـﺎ ﻋﻀـﻠﺔ ﺩﻟﺨـﻮﺍﻩ ﺍﺯ ﻟﻴﺴﺖ ،ﻓﻴﻠﻢ ﻧﺤﻮﺓ ﺗﺰﺭﻳﻖ ﺑﻬﻤﺮﺍﻩ ﺩﻳﺎﮔﺮﺍﻡ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﻣﻲﺷﻮﻧﺪ .ﺟﺰﺋﻴﺎﺕ ﺗﻜﻨﻴﻚ ﺗﺰﺭﻳﻖ ﻣﺎﻧﻨﺪ ﻧﺤﻮﺓ ﻧﺸﺴﺘﻦ ﺑﻴﻤﺎﺭ -ﻧﺤﻮﺓ ﻳﺎﻓﺘﻦ ﻋﻀﻠﻪ -ﻣﺸﺨﺼﺎﺕ ﺳﻮﺯﻥ ﻭ ﻧﺤﻮﺓ ﻓﻌﺎﻝﻛﺮﺩﻥ ﻋﻀﻠﻪ -ﻧﺤﻮﺓ ﻭﺭﻭﺩ ﺳﻮﺯﻥ -ﺗﻌﺪﺍﺩ ﺗﺰﺭﻳﻘﺎﺕ ﻭ ﺍﺣﺘﻴﺎﻃﺎﺕ ﻻﺯﻡ ﻧﻴﺰ ﺍﺭﺍﺋﻪ ﮔﺮﺩﻳﺪﻩﺍﻧﺪ. CDﺩﻭﻡ :ﻧﺮﻡﺍﻓﺰﺍﺭ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺑﻮﺗﻮﻟﻴﻨﻮﻡ ﺗﻮﻛﺴﻴﻦ ﺩﺭ ﻛﻠﻴﻨﻴﻚ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺎﻧﻚ ﺍﻃﻼﻋﺎﺗﻲ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﺑﻴﻤﺎﺭ ﺭﺍ ﺗﺸﻜﻴﻞ ﺩﺍﺩﻩ ﻭ ﺑﺎ ﻗﺎﺑﻠﻴﺖ Searchﺑﺮ ﺣﺴﺐ ﺍﻟﻔﺒﺎ ﺩﺳﺘﻴﺎﺑﻲ ﺑﻪ ﺳﻮﺍﺑﻖ ﺑﻴﻤﺎﺭ ﺭﺍ ﻣﻤﻜﻦ ﻣﻲﺳﺎﺯﺩ .ﺩﺭ ﭼﺎﺭﺕﻫﺎﻱ ﺭﻧﮕﻲ ﻣﺮﺑﻮﻁ ﺑـﻪ ﻫـﺮ ﺑﻴﻤـﺎﺭ ﻣﺤـﻞ ﻭ ﻣﻘـﺪﺍﺭ ﺗﺰﺭﻳﻖ ﻣﺸﺨﺺ ﺷﺪﻩ ﻭ ﺩﺭ ﺣﺎﻓﻈﻪ ﺫﺧﻴﺮﻩ ﻣﻲﮔﺮﺩﻧﺪ .ﻓﺎﻳﻞ PDFﺁﻣﻮﺯﺷﻲ ﺟﻬﺖ ﺭﺍﻫﻨﻤﺎﻳﻲ ﺑﻴﻤﺎﺭﺍﻥ ﻭ ﺍﻃﻼﻋﺎﺕ ﺑﻴﺸﺘﺮ ﺩﺭ CDﻣﻮﺟﻮﺩ ﺍﺳﺖ .ﺍﻳﻦ CDﺑﻪ ﭘﺰﺷﻜﺎﻥ ﺩﺭ ﺟﻤﻊﺁﻭﺭﻱ ﻳﺎﻓﺘﻪﻫﺎ ﻭ ﻛﻼﺳﻪﺑﻨﺪﻱ ﺁﻧﻬﺎ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﺑﻌﺪﻱ ﻭ ﺗﺤﻘﻴﻘﺎﺕ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﻣﻲﻛﻨﺪ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
50 2001
61.9 Thinking a head (Critical question in ms therapy) 62.9 Understanding and Diagnosing Restless Legs Syndrome
ــــ
. ﺩﺭ ﺩﺳﺘﺮﺱ ﻣﻲﺑﺎﺷﺪPDF ﺁﺧﺮﻳﻦ ﺍﻃﻼﻋﺎﺕ ﻭ ﻳﺎﻓﺘﻪﻫﺎ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱ ﺳﻨﺪﺭﻡ ﭘﺎﻫﺎﻱ ﺑﻲﻗﺮﺍﺭ ﻭ ﺭﻭﺵﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﻣﺨﺘﻠﻒ ﺍﻥ ﺑﺤﺚ ﺷﺪﻩ ﻭ ﺑﻪ ﺻﻮﺭﺕ ﻓﺎﻳﻞﻫﺎﻱ. ﻃﺮﺍﺣﻲ ﻭ ﺍﺟﺮﺍ ﺷﺪﻩ ﺍﺳﺖRLS Foundation ﻛﻪ ﺗﻮﺳﻂ ﻫﻴﺌﺖ ﻋﻠﻤﻲCD ﺩﺭ ﺍﻳﻦ . ﻳﺎﻓﺖ ﻣﻲﺷﻮﺩCD ﻫﻤﭽﻨﻴﻦ ﻳﻚ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺩﺭﺑﺎﺭﺓ ﺍﻳﻦ ﺳﻨﺪﺭﻡ ﻭ ﺗﻈﺎﻫﺮﺍﺕ ﺑﺎﻟﻴﻨﻲ ﺁﻥ ﻭ ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﻣﺨﺘﻠﻒ ﻧﻴﺰ ﺩﺭ ﺍﻳﻦ ﺩﺍﺧﻠﻲ-١٠
CD ﻋﻨﻮﺍﻥ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ 2003
1.10 (AGA Postgraduate Course) A Day and Night in the Life of a Gastroenterologist
Esophagus and Stomach Liver Pancreas and Biliary Tract 3DClinic (Version 1.0) Seeing is Understanding 2.10
Nutrition
GI Malignancy
Small Bowel and Colon
Clinical Challenge Sessions ___
ﺷﻤﺎDesktop ( ﺑﺮ ﺭﻭﻱ2D Clinic) Icon . ﻛﻨﻴﺪRestart ﺳﭙﺲ ﺳﻴﺴﺘﻢ ﺭﺍ.( ﺭﺍ ﺑﻬﻤﺮﺍﻩ ﺍﺳﻢ ﺧﻮﺩ ﻭﺍﺭﺩ ﻧﻤﺎﻳﻴﺪSN: BI-B25600000-131) ﻣﻮﺟﻮﺩ ﺍﺳﺖ ﻧﺼﺐ ﻧﻤﻮﺩﻩ ﻭ ﺳﭙﺲ ﺩﺭ ﻗﺴﻤﺖ ﺩﻭﻡCD ﺭﺍ ﻛﻪ ﺩﺭQTS ﺍﺑﺘﺪﺍAutorun ﺟﻬﺖ ﻧﺼﺐ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﻌﺪ ﺍﺯ ﺷﺮﻭﻉ ﺑﺮﻧﺎﻣﻪ ﺑﻪ ﺻﻮﺭﺕ - ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻋﻜﺲﻫﺎ ﻭ ﻓﻴﻠﻢﻫﺎﻱ ﺳﻪﺑﻌﺪﻱ ﺟﺬﺍﺏ ﻣﻔﺎﻫﻴﻢ ﻣﺨﺘﻠﻒ ﻣﺮﺑﻮﻁ ﺑﻪ ﺳﻴﺴﺘﻢﻫﺎﻱ ﻣﺨﺘﻠـﻒ ﺑـﺪﻥ ﺍﺯ ﺟﻤﻠـﻪ. ﺑﻌﺪ ﺍﺯ ﻧﺼﺐ ﺑﺮﻧﺎﻣﻪ ﺑﻪ ﻃﻮﺭ ﻛﺎﻣﻞ ﺩﺭ ﻛﺎﻣﭙﻴﻮﺗﺮ ﺣﻔﻆ ﺧﻮﺍﻫﺪ ﺷﺪ. ﻛﻪ ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﻭ ﺍﺟﺮﺍﻱ ﺁﻥ ﻣﻨﻮﻱ ﺍﺻﻠﻲ ﻇﺎﻫﺮ ﻣﻲﺷﻮﺩ.ﻇﺎﻫﺮ ﺧﻮﺍﻫﺪ ﺷﺪ ﻛﻪ ﺑﻪ ﺍﻧﺘﺨﺎﺏ ﺷﻤﺎ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ3D ﻓﻴﻠﻢﻫﺎﻱ. ﻧﺸﺎﻥ ﻣﻲﺩﻫﺪDisorder ﻭHealthy ﺭﺍ ﺩﺭ ﺩﻭ ﺣﺎﻟﺖGastrointestinal -Musculoskeletal -Respiratory -Nervous -Urinary -Sensory -Endocrine -Lymphatic -Skin ﺍﺿﺎﻓﻪﻛﺮﺩﻥ ﻧﻜﺎﺕ ﻣﻬﻢ ﺑﺎ ﻣﺎﺭﻛﺮ ﻭ ﻧﻴﺰ ﺗﺎﻳﭗ ﺑﺮ ﺭﻭﻱ ﻋﻜﺲﻫﺎ ﺍﺯ ﻗﺎﺑﻠﻴﺖﻫﺎﻱ ﺟﺎﻟﺐ ﺍﻳـﻦ، ﻗﺎﺑﻠﻴﺖ ﻧﮕﻬﺪﺍﺷﺘﻦ ﻓﻴﻠﻢ ﺩﺭ ﻟﺤﻈﻪ ﺩﻟﺨﻮﺍﻩ.ﻣﻲﺷﻮﻧﺪ ﻗﺴﻤﺖﻫﺎﻱ ﺑﺴﻴﺎﺭ ﺟﺎﻟﺐ ﻭ ﺁﻣﻮﺯﻧﺪﻩﺍﻱ ﺍﺯ ﺳﻴﺴﺘﻢﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﺩﺭ ﺣﺎﻟﺖ ﻧﺮﻣﺎﻝ ﻭ ﺑﻴﻤﺎﺭﻱ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ ﻛﻪ ﺑﻪ ﺩﺭﻙ ﺑﻬﺘﺮ ﻣﻮﺿﻮﻉ ﻛﻤﻚ ﺷﺎﻳﺎﻧﻲ ﻣﻲﻧﻤﺎﻳﺪ . ﺷﻤﺎ ﺩﺭ ﺻﻮﺭﺕ ﺗﻤﺎﻳﻞ ﻣﻲﺗﻮﺍﻧﻴﺪ ﭘﺮﻳﻨﺖ ﻭ ﺍﺳﻼﻳﺪ ﺑﺎ ﻛﻴﻔﻴﺖ ﺑﺎﻻ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﺗﻬﻴﻪ ﻓﺮﻣﺎﺋﻴﺪ.ﻧﺮﻡﺍﻓﺰﺍﺭ ﻣﻲﺑﺎﺷﺪ
-Cardiovascular
3.10 Adult Airway Management Principles & Techniques American Association
ــــ
(afael A. Ortega, M.D., Harold Arkoff, M.D.)
4.10 Advanced Therapy of INFLAMMATORY BOWEL DISEASE (Theodore M. Bayless, MD, Stephen B. Hanauer, MD) 5.10 AGA Postgraduate Course CONTROVERSIES And CLINICAL CHALLENGES in Pancreatic Diseases
2001 ــــ
(An Intensive Two-Day Course Covering A Diversity of Topics Related to the Pancreas)
6.10
-Expanded Content -Includes Results of the Q&A -Section Challenge Sessions Atlas of GASTROINTESTINAL in Health and Disease (Marvin M. Schuster, Michael D. Crowell, Kenneth L. Koch) Part 1: Physiologic Basis of Gastrointestinal Motility
Part 2: Motility Test for the Gastrointestinal Tract 2002
7.10 Atlas of GASTROINTESTINAL MOTILITY in Health and Disease (Second Edition) (Marvin M. Schuster, MD, FACP, FAPA, FACG, Michael D. Crowell, PhD, FACG, Kenneth L. Koch, MD)
Part I: Physiologic Basic of Gastrointestinal Motility Part II: Motility Tests for The Gastrointestinal Tract 8.10 Atlas of Clinical Oncology Soft Tissue Sarcomas American Cancer Sosiety (Raphael E. Pollock, MD, Phd) 9.10 Atlas of Clinical Oncology Cancer of the Lower Gastrointestinal Tract (Christopher G. Willett, MD) nd 10.10 Atlas of Clinical Rheumatology (2 Edition) (David J. Nashel, Chief, Rheumatology Section Va Medical Center, Washington, Professor of Medicine Georgetown University)
2002 2001
11.10 CANCER Principles & Practice of Oncology
ــــــ
1. Clinical Atlas of Rheumatic Diseases 2. Radiograph Intrerpretation Instructional Module
3. Physical Examination 4. Procures
5. Physical Findings Instructional Module Radiography 6. Aspiration/Injection Instructional Module
(6th Edition) (Vincent T. DeVita, Jr., Samuel Hellman, Steven A. Rosenberg)
ــــــ
12.10 Case Studies in GASTROENTEROLOGY (Second Edition) (Ingram Roberts, MD)
ــــــ
13.10 CD-ATLAS OF DIAGNOSTIC ONCOLOGY
ــــــ
14.10 Clinical Endocarinology Adrenals
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(G. Michael Besser MD, DSc, FRCP, Michael O. Thorner MB BS, DSc, FRCP) Gonads
Growth
Hormone Assay
ــــــ
Imaging Techniques
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
Pancreas
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
51 Ectopic Humoral Syndromes Gastrointestinal Tract Lipids and Lipoproteins Thyroid & Parathyroide Pituitary and Hypothalamus 15.10 Clinical Immunology PRINCIPLES AND PRACTICE (Second Edition) (Robert R Rich, Thomas A Fleisher, William T Shearer, Brain L Kotzin, Harry W Schroeder)
: ﺑﺨﺶ ﻣﻲﺑﺎﺷﺪ١١ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ. ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖRich ﻧﻮﺷﺘﺔ ﺩﻛﺘﺮClinical Immunology ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺮﺍﺳﺎﺱ ﻛﺘﺎﺏ ﺭﻭﺷﻬﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺩﺭ ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻱ-٧ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻳﻜﻲ-٦ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺁﻟﺮﮊﻳﻜﻲ-٥ ﺳﻴﺴﺘﻢ ﺩﻓﺎﻋﻲ ﺫﺍﺗﻲ ﻭ ﺍﻛﺘﺴﺎﺑﻲ-٤ ﻋﻔﻮﻧﺖ ﻭ ﺳﻴﺴﺘﻢ ﺍﻳﻤﻨﻲ-٣ ﻣﻜﺎﻧﻴﺴﻢﻫﺎﻱ ﺩﻓﺎﻋﻲ ﻣﻴﺰﺑﺎﻥ ﻭ ﺍﻟﺘﻬﺎﺏ- ٢ ﺍﺻﻮﻝ ﺗﺸﺨﻴﺼﻲ ﺍﻳﻤﻨﻲ-١ Slide ﻫﺮ ﺍﺳﻼﻳﺪ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﺩﺭ ﻳﻚ ﻓﺎﻳﻞ )ﺗﺤﺖ ﺑﺮﻧﺎﻣﺔdrag & drop ﺑﺎ ﺭﻭﺵ. ﻭﺍﮊﻩ ﻭ ﻟﻐﺎﺕ ﺭﺍ ﺩﺍﺭﺳﺖ ﻭ ﻧﻴﺰ ﺗﺼﺎﻭﻳﺮ ﻭ ﺍﺳﻼﻳﺪﻫﺎ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﭼﺎﭖ ﻧﻤﻮﺩSearch ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻗﺎﺑﻠﻴﺖ. ﺍﺳﻼﻳﺪﻫﺎﻱ ﻣﺘﻌﺪﺩﻱ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺢ ﺍﺭﺍﺋﻪ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ،ﺩﺭ ﻫﺮﺑﺨﺶ . ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩSlide vision ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ ﻭ ﺗﺤﺖAutorun ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ. ﻫﻤﭽﻨﻴﻦ ﻣﻲﺗﻮﺍﻥ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺩﻳﮕﺮﻱ ﺭﺍ ﺑﻪ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺿﺎﻓﻪ ﻳﺎ ﺣﺬﻑ ﻛﺮﺩ. ( ﺫﺧﻴﺮﻩ ﻭ ﻧﮕﻬﺪﺍﺭﻱ ﻧﻤﻮﺩvision
ــــــ
16.10 CLINICAL ONCOLOGY (Raymond E. Lenhard, J. MD, Robert T. Osteen, MD, Ted Gansler, MD)
2001
17.10 Comprehensive Clinical Endocrinology G. Michael Besser MD, DSc, FRCP, Michael O. Thorner
2000
Hypothalamus and Pituitary, Thyroid, Adrenal, Control of Blood glucose and its disturbance, gonad and growth, General conditions-basic, General conditionsclinical, Imaging, Patient Perspectives on endocrine Diseases 18.10 COMPREHENSIVE MANAGEMENT OF Chronic Obstructive Pulmonary Disease (Jean Bourbeau, MD, MSc, FRCPC, Diane Nault, RN, MSc, Elizabet Borycki)
2002
19.10 Core Curriculum in Primary Care Metabolic Diseases Section
ــــــ
20.10 Digestive Diseases
ــــــ
. ﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖHarvard ﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲCD ﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯCCC ﺳـﺆﺍﻻﺕ ﻣﺮﺑﻮﻃـﻪ ﺑـﻪ ﺻـﻮﺭﺕ، ﺩﺭ ﺁﺧـﺮ ﻫـﺮ ﺳـﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜـﻲ. ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛـﺎﺭﺑﺮ ﻣـﻲﺑﺎﺷـﺪ. ﺣﺎﺿﺮ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱ ﺩﺍﺧﻠﻲ ﻭ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖCD . ﺑﻪ ﺻﻮﺭﺕ ﺩﺭﺳﻨﺎﻣﻪ ﺁﻣﻮﺯﺷﻲ ﻣﻮﺟﻮﺩ ﺍﺳﺖCD ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺩﺭ. ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﻘﺎﻟﻪ ﭼﺎﭘﻲ ﺩﺭ ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ.ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻣﺘﺎﺑﻮﻟﻴﺴﻢ ﺁﻫﻦ-٤ ( ﻧﮕﺮﺷﻲ ﻋﻤﻠﻲ )ﻗﺴﻤﺖ ﺩﻭﻡ: ﺩﻳﺎﺑﺖ ﻣﻠﻴﺘﻮﺱ-٣ ( ﻧﮕﺮﺷﻲ ﻋﻤﻠﻲ )ﻗﺴﻤﺖ ﺍﻭﻝ: ﺩﻳﺎﺑﺖ ﻣﻠﻴﺘﻮﺱ-٢ ﻫﺎ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕLipid -١ Self-Education Program
21.10 Diseases of the Liver
(A Core Curriculum and Self-Assessment in Gastroenterology and Hepatology)
(8th Edition) (Lippincott Williams & Wilkins)
General Considerations Autoimmune Liver Disease The Liver in Pregnancy and Childhood
The Consequences of Liver Disease Alcohol and Drug-Luduced Disease Infections and Granulomatous Disorders
ــــــ The Cholestasis Disorders Genetic and Metabolic Disease Transplantation
Viral Hepatitis Vascular Disease and Trauma Benign and Malignant Tumors
Immunology of Liver
26.1 EBUS
Endo Bronchial Ultrasound (Heinrich D. Becher, MD. Fccp) - Basic Introduction -Bronchial Anatomy -Interactive Sonography -Product Information
22.10 ESAP
(Endocrinology Self-Assessment Program)
ــــــ
(Clark T. Sawin, MD, Kathryn A. Martin, MD) (The Endocrine Society)
23.10 Evidence-Based Asthma Management PATHOPHYSIOLOGY/DIAGNOSIS/MANAGEMENT (7
TH
edition)
2003 2001
ﺁﺳﻢ ﻳﻚ ﺑﻴﻤﺎﺭﻱ ﺷﺎﻳﻊ ﭘﺰﺷﻜﻲ ﺍﺳﺖ ﻛﻪ ﺷـﻴﻮﻉ ﺭﻭ. ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﻣﺘﺨﺼﺼﻴﻦ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ﺗﺎ ﺑﻬﺘﺮﻳﻦ ﺩﺭﻣﺎﻥ ﺭﺍ ﺑﺮ ﺍﺳﺎﺱ ﺩﺭﻳﺎﻓﺖ ﺷﺨﺼﻲ ﺧﻮﺩ ﺍﺯ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺩﺭﻣﺎﻥﻫﺎﻱ ﻣﻮﺟﻮﺩ ﺩﺭ ﻣﻘﺎﻻﺕ ﻭ ﻛﺘﺎﺏﻫﺎ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﺮﺩﻩ ﻭ ﺑﻪ ﻛﺎﺭ ﺑﺮﺩEvidence-Based in medicin ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺯ ﺳﺮﻱ ﻛﺘﺎﺏﻫﺎﻱ . ﺁﻣﺎﺭﮔﻴﺮﻱﻫﺎ ﻭ ﻣﻄﺎﻟﻌﺎﺕ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻛﻪ ﺍﻓﺰﺍﻳﺶ ﺷﻴﻮﻉ ﺁﺳﻢ ﻭﺍﻗﻌﻲ ﺑﻮﺩﻩ ﻭ ﺑﺎ ﺍﺯ ﻛﺎﺭﺍﻓﺘﺎﺩﮔﻲ ﺑﻴﻤﺎﺭ ﻫﻤﺮﺍﻩ ﺑﻮﺩﻩ ﻛﻪ ﻧﺸﺎﻥﺩﻫﻨﺪﻩ ﺩﺭﻣﺎﻥ ﺗﺎ ﻛﺎﻣﻞ ﺍﻳﻦ ﺑﻴﻤﺎﺭﺍﻥ ﺍﺳﺖ.ﺑﻪ ﺍﻓﺰﺍﻳﺶ ﺩﺍﺭﺩ : ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺣﺎﺿﺮ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ.ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺎ ﺁﻭﺭﺩﻥ ﻣﻘﺎﻻﺕ ﺑﺮ ﺍﺳﺎﺱ ﻣﻌﺘﺒﺮﺑﻮﺩﻥ ﻭ ﺩﺭﺟﻪﺑﻨﺪﻱ ﺍﻋﺘﺒﺎﺭ ﻣﻘﺎﻻﺕ ﭘﺰﺷﻚ ﻣﺘﺨﺼﺺ ﺭﺍ ﻛﻤﻚ ﻣﻲﻛﻨﺪ ﺗﺎ ﺩﺭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱ ﺁﺳﻢ ﺑﻬﺘﺮﻳﻦ ﻭ ﻛﻢﻋﺎﺭﺿﻪﺗﺮﻳﻦ ﺩﺭﻣﺎﻥ ﺭﺍ ﺑﺮﺍﻱ ﻫﺮ ﺑﻴﻤﺎﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﺪ 1. Natural History and Epidemiology 2. Diagnosis 3. Role of Childhood Infection 4. Management of Persistent Asthma in Childhood 5. Use of Theophylline and Anticholinergic Therapy 6. Leukotriene Modifiers 7. Acute Life-Threatening Asthma 8. Role of Asthma Education
9. Genetics of Asthma 10. Role of the Outdoor Environment 11. Diagnosis and Management of Occupational Asthma 12. Mechanisms of Action of 2-Agonists and Short-Acting 2 Therapy 13. Environmental Control and Immunotherapy 14. Alternative Anti-inflammatory Therapies 15. Management of Asthma in the Intensive Care Unit 16. Asthma Unresponsive to Usual Therapy
17. Cellular and Pathologic Characteristics 18. Role of Indoor Aeroallergens 19. Principles of Asthma Management in Adults 20. Role of Long-Acting 2-Adrenergic Agents 21. Role of Inhaled Corticosteroids 22. Exercise-Induced Bronchoconstriction 23. Severe Acute Asthma in Children 24. Measures of Outcome
24.10 EVIDENCE-BASED DIABETES CARE (Hertzel C. Gerstein, MD, R. Brain Haynes, MD,) 1- EVIDENCE 2- DEFINITION AND IMPORTANCE OF DIABETES MELLITUS 3- ETIOLOGIC CLASSIFICATION OF DIABETES
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2001
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
52 4- PREVENTION AND SCREENING FOR DIABETES MELLITUS
5- LONG-TERM CONSEQUENCES OF DIABETES
6- DELIVERY OF CARE
2001
25.10 EVIDENCE-BASED Diagnosis: A Handbook of Clinical Prediction Rules (Mark Ebell, MD, MS) (Springer-Verlag)
-Cardiovascular Diseases -Endocrinology -Gastroenterology -Gynecology and Obstetrics -Hematology/Oncology -Musculoskeletal -Neurology -Pulmonary Diseas -Renal Disease -Surgery and Trauma
-Infectious Disease 2000
26.10 Gastric Cancer Diagnosis and Treatment (An interactive Training Program) (J.R. Siewert, D.Kelsen, K. Maruyama) (Springer) 27.10 Gastroenterology
ــــ
Endoscopy (2nd Edition)
2002
th 28.10 Gastrointestinal and Liver Disease Pathophysiology/Diagnosis/Management (7 edition) (Sleisenger & Fordtran's)
Esophagus Pancreas
Liver Biliary tract
Nutrition in gastroenterology Approach to patients with symptoms and signs
Topics involving multiple organs Small and Large Intestine
Biology of the Gastrointestinal Tract and Liver Vasculature and Supporting Structures
Stomach and duodenum Psychosocial
29.10 HARRISON'S 15 McGraw-Hill presents
ــــ 1998
32.1 Imaging of Diffuse Lung Disease (David A. Lynch, MB, John D. Newell Jr, MD, FCCP, Jin Seong Lee, MD)
: ﺑﻌﻀﻲ ﻓﺼﻮﻝ ﻛﺘﺎﺏ ﺷﺎﻣﻞ.( ﺩﺭ ﺍﻃﻔﺎﻝ ﻭ ﺑﺎﻟﻐﻴﻦ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﻨﺘﺸﺮ ﺭﻳﻪ ﻣﻲﺑﺎﺷﺪ.... ﻭMRI,CT-Xray) ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻭ ﺗﻔﺴﻴﺮ ﻋﻜﺲﺑﺮﺩﺍﺭﻱ، ﺷﺮﺡ ﺣﺎﻝ، ﻛﻪ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﺷﺎﻣﻞ ﺗﻠﻔﻴﻘﻲ ﺍﺯ ﻣﻌﺎﻳﻨﻪ.( ﻣﻲﺑﺎﺷﺪDLN) ﻓﺼﻞ ﺍﺯ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻣﻨﺘﺸﺮ ﺭﻳﻪ١١ ﺣﺎﺿﺮ ﺷﺎﻣﻞCD ﺍﺭﺯﻳﺎﺑﻲ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺑﻴﻤﺎﺭﻫﺎﻱ ﺭﻳﻪ ﺁﻧﻬﺎ ﺑﻪ ﻃﻮﺭ ﻣﺠﺰﺍ ﻣﻲﺑﺎﺷﺪX-Ray,CT ﻭ ﻣﻘﺎﻳﺴﻪDLD ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ
DLDﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﻐﻠﻲ ﻭ ﻣﺤﻴﻄﻲ ﻭ
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺭﺍﻫﻬﺎﻱ ﻫﻮﺍﺋﻲ
ﭘﻴﻮﻧﺪ ﺭﻳﻪ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺁﻣﻔﻴﺰﻡ
ﺗﺼﻮﻳﺮ ﺑﺮﺩﺍﺭﻱ ﻋﺮﻭﻕ ﺭﻳﻮﻱ ﻛﻮﺩﻛﺎﻥDLD ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻧﻔﻴﻠﺘﺮﺍﺗﻴﻮ ﺭﻳﻪ
. ﻗﻠﺐ ﻭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻣﻲﺩﻫﺪ، ﺭﻳﻪ، ﺑﻮﺩﻩ ﻭ ﺑﻪ ﮔﻔﺘﻪ ﻣﺆﻟﻔﻴﻦ ﻧﮕﺎﻫﻲ ﺟﺪﻳﺪ ﺑﻪ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺭﺯﻳﺪﻧﺖﻫﺎﻱ ﺩﺍﺧﻠﻲAcrobat Reader ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ ﺑﺮﻧﺎﻣﻪ 30.10 INFECTIOUS DISEASES
(W Edmund Farrar, Martin J Wood, John A Innes, Hugh Tubbs)
The Head and Neck The Urinary Tract Vira, Fungal and Ectoparasitic Infections
Lower Respiratory Tract The Genital Tract The Eye
The Nervous System Bones and Joints Systemic Infections
ــــ
The Gastrointestinal Tract The Cardiovascular System HIV Infection and Aids
The liver and Biliary Tract Bacterial Infections Acknowledgements
31.10 Menopausal Osteoporosis (Neill Musselwhlte, M.D., Herman Rose, M.D.)
ﺳﺆﺍﻻﺕ ﺟﺪﻳﺪ ﻣﻄﺮﺡﺷﺪﻩ ﺩﺭ ﺍﻳﻦ ﺯﻣﻴﻨﻪ-٦
ﺍﺳﺘﺌﻮﭘﺮﻭﺯ-٥
ــــــ : ﻣﻄﺎﻟﺐ ﺟﺎﻟﺒﻲ ﺩﺭ ﺭﺍﺑﻄﻪ ﺑﺎ ﻣﻨﻮﭘﻮﺯ ﻭ ﺍﺳﺘﺌﻮﭘﺮﻭﺯ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﻋﻨﺎﻭﻳﻦ ﺁﻥ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺩﺭ ﺍﻳﻦ ﻧﮕﺮﺍﻧﻲﻫﺎﻱ ﺑﻴﻤﺎﺭﻳﺎﻥ-٣ ﺭﻭﺵ ﺟﻠﻮﮔﻴﺮﻱ ﺍﺯ ﻋﻮﺍﺭﺽ ﺁﻥ-٢ ﻣﻨﻮﭘﻮﺯ ﻭ ﻧﺤﻮﺓ ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺁﻥ-١
Impact of osteobrosis -٤
2001
32.10 MKSAP® 12 (American College of Physiciance-American Sosiety Internal Medicine)
: ﺷﺎﻣﻞCD ﻋﻨﺎﻭﻳﻦ ﻣﻮﺭﺩ ﺑﺤﺚ ﺍﻳﻦ -Gastroenterology and Hepatology - Endocrinology and Metabolism -Infectious Disease Medicine - Rheumatology -Neurology
- Dermatology - Nephrology -Hospital-Based Medicine and Critical Care
- Oncology
- Hematology
- Cardiovascular Medicine
- Pulmonary Medicine
- Ambulatory Medicine
33.10 Oxford Textbook of Medicine (OTM) (Weatherall, Ledingham, Weatherall) ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻳﻚ ﻣﻨﺒﻊ ﻭ ﻣﺮﺟﻊ ﻗﻮﻱ ﺑﻪ ﻣﻨﻈﻮﺭ ﻣﺸﺎﻭﺭﻩ ﺩﺭ ﻣﻌﺎﻳﻨـﺎﺕ ﺭﻭﺯﻣـﺮﻩ ﻭ ﭘﺎﺳـﺦ. ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﻋﻠﻮﻡ ﭘﺎﻳﻪ ﻭ ﻣﻬﺎﺭﺗﻬﺎﻱ ﺑﺎﻟﻴﻨﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﻃﺐ ﺩﺍﺧﻠﻲ ﻭ ﺗﺨﺼﺺﻫﺎﻱ ﻭﺍﺑﺴﺘﻪ ﺭﺍ ﺩﺭﺑﺮ ﻣﻲﮔﻴﺮﺩCD ﺍﻳﻦ. ﺗﺼﻮﻳﺮ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ٢٥٠٠ ﺻﻔﺤﻪ ﻭ٥٠٠ ﻓﺼﻞ ﺩﺭ٣٣ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻣﺸﺘﻤﻞ ﺑﺮ : ﺍﺯ ﻣﺰﻳﺖﻫﺎﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺷﺎﺭﻩ ﻛﺮﺩ. ﻣﻘﺎﻟﻪﻧﻮﻳﺲ ﻭ ﻣﺤﻘﻖ ﻣﻌﺘﺒﺮ ﺩﺭ ﺳﺮﺗﺎﺳﺮ ﺟﻬﺎﻥ ﺍﺳﺘﻔﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ٥٨٠ ﺩﺭ ﻧﻮﺷﺘﻦ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺍﺯ. ﻣﻲﺑﺎﺷﺪ،ﺳﺆﺍﻻﺗﻲ ﻛﻪ ﺧﺎﺭﺝ ﺗﺨﺼﺺ ﭘﺰﺷﻜﺎﻥ ﻣﻄﺮﺡ ﻣﻲﺷﻮﺩ ﺩﺭ. ﺑﻴﻤﺎﺭﻳﻬـﺎﻱ ﻣﻘـﺎﺭﺑﺘﻲ، ﻣﻌﺎﻟﺠﺎﺕ ﺩﻭﺭﻩﺍﻱ، ﭘﺰﺷﻜﻲ ﭘﻴﺮﻱ، ﭘﺰﺷﻜﻲ ﻗﺎﻧﻮﻧﻲ، ﭘﺰﺷﻜﻲ ﻭﺭﺯﺷﻲ. ﺑﻴﺸﺘﺮ ﻣﻔﺎﻫﻴﻢ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻋﻔﻮﻧﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﺩﺭﺳﻨﺎﻣﻪ ﭘﺰﺷﻜﻲ ﺭﺍ ﭘﻮﺷﺶ ﻣﻲﺩﻫﺪ. ﺩﺍﻣﻨﺔ ﻣﺒﺎﺣﺚ ﻭ ﻣﻮﺿﻮﻋﺎﺕ ﺍﺯ ﻗﺒﻞ ﻭﺳﻴﻊﺗﺮ ﺷﺪﻩ ﺍﺳﺖ.ﮔﺮﺩﺁﻭﺭﻱ ﻏﻴﺮﺗﻜﺮﺍﺭﻱ ﻣﺒﺎﺣﺚ ﻋﻠﻮﻡ ﭘﺎﻳﻪ ﻭ ﻋﻠﻮﻡ ﺑﺎﻟﻴﻨﻲ . ﻣﻮﺭﺩ ﺑﺤﺚ ﺩﻗﻴﻖ ﻭ ﻣﻮﺷﻜﺎﻓﺎﻧﻪ ﻗﺮﺍﺭ ﻧﮕﺮﻓﺘﻪ ﺍﺳﺖ، ﺍﺧﺘﻼﻻﺕ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺍﻋﺘﻴﺎﺩ ﻭ ﺭﻭﺍﻥﭘﺰﺷﻜﻲ ﺩﺭ ﻣﻌﺎﻳﻨﺎﺕ ﻋﻤﻮﻣﻲ، ﺗﻐﺬﻳﻪ، ﺑﻬﺪﺍﺷﺖ ﻣﺤﻴﻂ ﻭ ﻣﺸﺎﻏﻞ. ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺑﺎﺭﺩﺍﺭﻱ،CD ﺍﻳﻦ ﻗﺪﺭﺕ ﺗﻐﻴﻴﺮ ﺍﻧﺪﺍﺯﺓ ﻗﻠﻤﻬﺎﻱ ﻣﺘﻮﻥ ﻭ ﭼﺎﭘﮕﺮ ﻭ ﻧﻴﺰ ﻗﺪﺭﺕ ﭼﺎﭖ ﻣﺘﻦ ﻭ ﺟﺴﺘﺠﻮﻱ ﻛﻠﻤـﺎﺕ ﻭ ﻭﺍﮊﻩﻫـﺎﻱ ﺗﺨﺼﺼـﻲ ﻭ ﺩﺳﺘﺮﺳـﻲ ﺁﺳـﺎﻥ ﺑـﻪ. ﺭﺍ ﻧﻴﺰ ﺟﺪﺍﮔﺎﻧﻪ ﻣﺸﺎﻫﺪﻩ ﻧﻤﻮﺩCD ﻛﻪ ﻣﻲﺗﻮﺍﻥ ﺗﻤﺎﻣﻲ ﺗﺼﺎﻭﻳﺮ، ﻫﺮ ﻓﺼﻞ ﺩﺍﺭﺍﻱ ﺗﺼﺎﻭﻳﺮﻱ ﻣﻲﺑﺎﺷﺪ. ﻣﻨﺎﺑﻊ ﺁﻥ ﻗﻴﺪ ﺷﺪﻩ ﺍﺳﺖ،ﺩﺭ ﭘﺎﻳﺎﻥ ﻫﺮ ﻓﺼﻞ ﻛﺘﺎﺏ . ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖCD ﺳﺆﺍﻻﺕ ﭼﻨﺪﮔﺰﻳﻨﻪﺍﻱ )ﻛﻪ ﺑﺼﻮﺭﺕ ﺟﺪﺍﮔﺎﻧﻪ ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ( ﻭ ﻓﻬﺮﺳﺖ ﺗﻔﺼﻴﻠﻲ ﺍﺯ ﻣﻨﺪﺭﺟﺎﺕ ﻛﺘﺎﺏ ﻧﻴﺰ ﺩﺭ ﺍﻳﻦ.ﺟﺪﺍﻭﻝ ﻭ ﺗﺼﺎﻭﻳﺮ ﺍﺯ ﻭﻳﮋﮔﻲﻫﺎﻱ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﺳﺖ
ــــ
34.10 Pre-Colonoscopy Education Program (Dr. Michael Shaw, Dr. Oliver cass Dr. James Reynolds Patricia Tomshine, Rn)
ــــ
- Reason for Colonoscopy
- The Colon and The Colonoscope
35.10 Principles & Practice of Infectious Diseases
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
- Preparations - Day of the Procedure
- About the Procedure -After the Procedur - Minor Complicaions
A Harcourt Health Sciences Company
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
- Major Complications
2000 ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
53 : ﺷﺎﻣﻞ ﺳﻪ ﺑﺨﺶ ﺍﺻﻠﻲ ﺍﺳﺖCD ﺍﻳﻦ. ﻭ ﺷﺎﻣﻞ ﺗﻤﺎﻣﻲ ﻣﻔﺎﻫﻴﻢ ﺍﺳﺎﺳﻲ ﻭ ﺟﺎﺭﻱ ﺩﺭ ﻣﻴﻜﺮﻭﺑﻴﻮﻟﻮﮊﻱ ﻭ ﺩﺭﻣﺎﻥ ﻋﻮﺍﺭﺽ ﻋﻔﻮﻧﻲ ﺍﺳﺖ. ﺗﺼﻮﻳﺮ ﻣﻲﺑﺎﺷﺪ٨٠٠ ﺟﺪﻭﻝ ﻭ٨٠٠ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﻫﻤﺮﺍﻩ ﺑﺎ ﺑﻴﺶ ﺍﺯCD ﺍﻳﻦ 1- Browse Mandell, Douglas & Bennett s .ﻛﻪ ﻣﺘﻦ ﺍﺻﻠﻲ ﻛﺘﺎﺏ ﺭﺍ ﺷﺎﻣﻞ ﻣﻲﺷﻮﺩ 2- Subject index Search: .ﺑﺮ ﺍﺳﺎﺱ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎ ﻭﺍﮊﻩﻫﺎﻱ ﺗﺨﺼﺼﻲ ﺭﺍ ﭘﻴﺪﺍ ﻧﻤﻮﺩ ﻭ ﺑﻪ ﻓﺼﻞ ﻭ ﻣﺒﺎﺣﺚ ﻣﺮﺑﻮﻁ ﺑﻪ ﺁﻥ ﺩﺭ ﻛﺘﺎﺏ ﻣﻨﺘﻘﻞ ﺷﺪ 3- Help ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖCD ﻃﺮﻳﻘﺔ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ، ﻋﺮﻭﻗﻲ- ﻋﻔﻮﻧﺖﻫﺎﻱ ﺩﺳﺘﮕﺎﻩ ﻗﻠﺒﻲ، ﻋﻔﻮﻧﺘﻬﺎﻱ ﺑﺮﻭﻧﺸﻴﻮﻟﻬﺎ، ﻋﻔﻮﻧﺘﻬﺎﻱ ﻓﻮﻗﺎﻧﻲ ﺗﻨﻔﺴﻲ،( ﻋﻼﺋﻢ ﻭ ﻧﺸﺎﻧﻪﻫﺎﻱ ﻛﻠﻴﻨﻴﻜﻲ )ﺗﺐ٢ ( ﺍﭘﻴﺪﻣﻴﻮﻟﻮﮊﻱ ﺭﻭﺷﻬﺎﻱ ﺩﺭﻣﺎﻧﻲ، ﻣﻜﺎﻧﻴﺰﻡﻫﺎﻱ ﺩﻓﺎﻋﻲ ﻣﻴﺰﺑﺎﻥ،( ﺍﺻﻮﻝ ﺍﻭﻟﻴﻪ ﺩﺭ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻋﻔﻮﻧﻲ )ﻋﻮﺍﻣﻞ ﻣﻴﻜﺮﻭﺑﻲ١ (... ﺟﺮﺍﺣﻲ ﻭ ﻋﻔﻮﻧﺘﻬﺎﻱ ﺗﺮﻭﻣﺎ ﻭ، ﻋﻔﻮﻧﺘﻬﺎﻱ ﻣﻴﺰﺑﺎﻧﻬﺎﻱ ﺧﺎﺹ، )ﻋﻔﻮﻧﺘﻬﺎﻱ ﺑﻴﻤﺎﺭﺳﺘﺎﻧﻲ،Special problems (٤ (.... ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﻴﻮﭘﻼﺳﻢﻫﺎ ﻭ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﭘﺮﻳﻮﻥﻫﺎ،( ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻋﻔﻮﻧﻲ ﻭ ﻋﻮﺍﻣﻞ ﻭ ﻋﻠﻞ ﺁﻧﻬﺎ )ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻭﻳﺮﻭﺳﻲ٣ (....... ﻋﻔﻮﻧﺘﻬﺎﻱ ﺳﻴﺴﺘﻢ ﻋﺼﺒﻲ ﻭ .( ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﻧﺪCD ﻗﺎﺑﻞ ﺍﺟﺮﺍ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﺭ ﻫﻨﮕﺎﻡ ﻧﺼﺐ ﺁﻥ ﺑﺮ ﺭﻭﻱ ﻛﺎﻣﭙﻴﻮﺗﺮ ﺷﻤﺎ )ﺍﺯ ﻃﺮﻳﻖJava VM ﻭinternet explver ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﺤﺖ 36.10 Rheumatology (John H. Klippel.Paul A Dieppe)
-Rheumatic Diseases -Regional Pain Problems
-Signs and Symptoms -Connective Tissue Disorders
37.10 TEXTBOOK OF Gastroenterology (Third Edition)
-Rheumatoid Arthritis and Spondylopathy -Disorders of Bone, Cartilage
ــــ
-Infection and Arthritis -Management of Rheumatic Disease
ــــ
ATLAS OF Gastroenterology (Second Edition) (David H. Alpers, MD, Loren Laine, MD)
2001
38.10 Textbook of Rheumatology (Kelley's) (W.B. Saunders Company) Section I BIOLOGY OF THE NORMAL JOINT Section III EVALUATION OF THE PATIENT Section V DIAGNOSTIC TESTS AND PROCEDURES Section VII CLINICAL PHARMACOLOGY Section IX SPONDYLOARTHROPATHIES Section XI VASCULITIC SYNDROMES Section XIII STRUCTURE, FUNCTION, AND DISEASE OF MUSCLE Section XV CRYSTAL-ASSOCIATED SYNOVITIS Section XVII ARTHRITIS RELATED TO INFECTION Section XIX DISORDERS OF BONE AND STRUCTURAL PROTEIN Section XXI RECONSTRUCTIVE SURGERY FOR RHEUMATIC DISEASE
Section II IMMUNE AND INFLAMMATORY RESPONSES Section IV MUSCULOSKELETAL PAIN AND EVALUATION Section VI SPECIAL ISSUES Section VIII RHEUMATOID ARTHRITIS Section X SYSTEMIC LUPUS ERYTHEMATOSUS AND RELATED SYNDROMES Section XII SCLERODERMA AND MIXED CONNECTIVE TISSUE DISEASES Section XIV RHEUMATIC DISEASES OF CHILDHOOD Section XVI OSTEOARTHRITIS, POLYCHONDRITIS, AND HERITABLE DISORDERS Section XVIII ARTHRITIS ACCOMPANYING SYSTEMIC DISORDERS Section XX TUMORS INVOLVING JOINTS
39.10 Textbook of TRAVEL MEDICINE and HEALTH (Herbert L. Dupont, M.D., Robert Steffen, M.D.) (B.C.DECKER INC)
57.9
ــــ
ﺩﺭ ﺯﻣﺎﻥ ﻣﺴﺎﻓﺮﺕ ﺑﻪ ﻣﻨﺎﻃﻖ ﻣﺨﺘﻠﻒ ﺍﻣﻜﺎﻥ ﺍﺑﺘﻼ ﺑﻪ ﺑﺮﺧﻲ ﺑﻴﻤﺎﺭﻳﻬﺎ ﺑﺎ ﺗﻮﺟﻪ ﺑـﻪ ﺷـﺮﺍﻳﻂ ﺍﭘﻴـﺪﻣﻴﻜﻲ ﻭ. ﻧﻮﺷﺘﻪ ﺷﺪﻩ ﺍﺳﺖSteffen ﻭ ﺩﻛﺘﺮDupont ﻭ ﺗﻮﺳﻂ ﺩﻛﺘﺮ. ﺻﻔﺤﻪ ﻣﻲﺑﺎﺷﺪ٣٧٠ ﻓﺼﻞ ﺩﺭ٣٤ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ﻳﻚ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺍﺳﺖ ﻛﻪ ﺷﺎﻣﻞ ﺩﺭ ﻣﺴﺎﻓﺮﺍﻥ ﻣﺨﺘﻠﻒ ﺩﺭ ﻛﺸﻮﺭﻫﺎﻱ ﮔﻮﻧﺎﮔﻮﻥ ﻣﻮﺭﺩ ﺑﺤﺚ. . . ﺍﺛﺮﺍﺕ ﻭﺍﻛﺴﻴﻨﺎﺳﻴﻮﻥ ﻭ ﺁﻣﺎﺭ ﻣﺮﮒ ﻭ ﻣﻴﺮ ﻭ، ﺷﻴﻮﻩﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻧﺎﺷﻲ ﺍﺯ ﺣﻮﺍﺩﺙ. ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﻘﺎﺭﺑﺘﻲ ﺍﺯ ﺍﻳﻦ ﺟﻤﻠﻪ ﻫﺴﺘﻨﺪ، ﻭﺑﺎ، ﺍﻳﺪﺯ، ﺗﻴﻔﻮﺋﻴﺪ، ﻫﭙﺎﺗﻴﺖ، ﺑﻴﻤﺎﺭﻳﻬﺎﻳﻲ ﻣﺜﻞ ﻣﺎﻻﺭﻳﺎ.ﺍﻧﺪﻣﻴﻚ ﺑﻴﺸﺘﺮ ﻣﻲﺷﻮﺩ . ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖCD ﻭ ﺑﺮﺭﺳﻲ ﺩﺭ ﺍﻳﻦ
The Massachusetts General Hospital Handbook of Pain Management
(Second Edition)
(Jane Ballantyne, Scott M. Fishman, Salahadin Abdi) (SALEKAN-E-book)
ــــ
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﻗﺴﻤﺖﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺍﻳﻦ I. General Considerations II. Diagnosis of Pain III. Therapeutic Options: Pharmacologic Approaches IV. Therapeutic Options: Nonpharmacologic Approaches V. Acute Pain VI. Chronic Pain VII. Pain Due to Cancer VIII. Special Situations - Apendices - Subject Index
ــــ
40.10 UEGW Gastroenterology Week 10th United European (Geneva, Switzerland)
2003
41.10 UEGW IBS: Management not myth 1. IBS: the clinician's view
2. IBS: care, cost and consequences
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ 3. Diagnosis: identigy, Probe, eliminate
42.10 Upper GI Endoscopy An Interactive Aducasional Program
4. Tegaserod: a world of experience
Video Segments of Common Pathologics of the Upper Gl tract (Iencludes Educational text)
43.10 UpToDate CLINICAL REFERENCE LIBRARY 13.1 (CD I , II) (Burton D. Rose, MD, Joseph M. Rush, MD)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
5. Chairman's summary
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــ 2005
: ﺷﺎﻣﻞCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
54 Adult Primary Care Allwrgy and Immonology Cardiology Critical Care Drug Information Enodcrinoology Family Medicine Rheumatology Women's Health Gastroenterology Gynecology Hematology Infections Disease Nephrology Oncology Pediatrics Pulmonology
44.10 YEAR BOOK of RHEUMATOLOGY, ARTHRITI, AND MUSCULOSKELETAL DISEASE
TM
(Richrd S. Panush, MD) (SALEKAN E-BOOK)
Health Sciences, Epidemiology, Economics, & Arthritis Care
Systemic Lupus Erythematosus and Related Disorders
Rheumatoid Arthritis
Vasculitis and Systemic Rheumatic Diseases and Other Related Disorders
Systemic Selerosis and Related Disorders
Osteoarthritis, Crystal-Related Arthropathies, Osteoporosis, Infectious Arthritides, and Spondyloarthropathies
Regional Pain Syndromes, Non-Articular Musculoskeletal Disorders, and Fibromyalgia
Miscellaneous Topics
2003
ﺍﻃﻔﺎﻝ-١١
CD ﻋﻨﻮﺍﻥ 1.11 A Major Contributor to Neonatal Infant Morbidity and Mortality (SURVANTA) (Part I , II) (Alan J. Gold, MD, J. Harry Gunkel, Arvin M. Overbach) 2.11 Atlas of Pediatric Gastrointestinal Disease 3.11 Basic Mechanisms of Pediatric Respiratory Disease (Second Edition) (Gabriel G. Haddad,MD, Steven H. Abman, MD) Genetic and Developmental Biology of the Respiratory System Developmental Physiology of the Respiratory System 4.11 Child Development, 9/e (John W. Santrock) 18.9 CURRENT MANAGEMENT IN CHILD NEUROLOGY
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ ــــ ــــ 2002
Structure-Function Relations of the Respiratory System During Development Inflammation and Pulmonary Defense Mechanisms (SECOND EDITION) (Bernrd L. Maria, MD, MBA)
Section 1: Clinical Practice Trends Section 2: The Office Visit Section 3: The Hospitalized Child 5.11 EVIDENCE-BASED PEDIATRICS (William Feldmam, MD, FRCPC) (B.C. Decker Inc.) 6.11 PEDIATRIC GASTROINTESTINAL DISEASE Pathophysiology . Diagnosis . Management (Third Edition) 7.11 TEXTBOOK OF NEONATAL RESUSCITATION (4TH EDITION MULTIMEDIA CD-ROM)
2001 2002 2000 ــــ ــــ
ﻋﻤﻮﻣﻲ:١٢
CD ﻋﻨﻮﺍﻥ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
1.12 1. Review for USMLE NMS® (Step 1) 2. Review for USMLE NMS® (Step 2) 3. Review for USMLE NMS® (Step 3)
ــــ
2.12 A.D.A.M. PracticePractical Review Anatomy – Create New Test – Open Existing Test
ــــ
ﺳﺆﺍﻝ ﺍﻣﺘﺤﺎﻧﻲ ﺑﻮﺩﻩ ﻛﻪ ﺑﻪﻣﻨﻈﻮﺭ ﻳﺎﺩﺁﻭﺭﻱ ﻭ ﻣﺮﻭﺭ١٥٠٠٠ ﺩﺍﺭﺍﻱ ﺑﻴﺶ ﺍﺯ.( ﻣﻲﺑﺎﺷﺪX-ray ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﻭ، ﺗﺼﻮﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ )ﺗﺼﺎﻭﻳﺮ ﻭﺍﻗﻌﻲ٥٠٠ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ﺑﻴﺶ ﺍﺯ.ﻫﺪﻑ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﺮﻭﺭ ﻣﺒﺎﺣﺚ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻣﺤﻚ ﺯﺩﻥ ﺍﻃﻼﻋﺎﺕ ﻛﺎﺭﺑﺮ ﺩﺭ ﺍﻳﻦ ﺯﻣﻴﻨﻪ ﺍﺳﺖ ﺏ( ﻣﺒﺎﺣﺚ ﻣﺮﺑﻮﻁ ﺑﻪ ﺩﺳﺘﮕﺎﻩﻫﺎﻱ ﺑﺪﻥ ﺍﻟﻒ( ﻣﺒﺎﺣﺚ ﻣﺮﺑﻮﻁ ﺑﻪ ﻧﻮﺍﺣﻲ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ : ﻗﺴﻤﺖ ﻣﺒﺎﺣﺚ ﺍﺭﺍﺋﻪ ﺷﺪﻩﺍﻧﺪ٢ ﺩﺭ،CD ﺩﺭ ﺍﻳﻦReview Anatomy ﺩﺭ ﭘﻨﺠﺮﺓ ﺍﺻﻠﻲ.ﻣﻄﺎﻟﺐ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ : ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡ ﺷﺪﻩ ﺩﺭ ﺑﺨﺶ ﻧﻮﺍﺣﻲ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﺷﺎﻣﻞ.ﻫﺮ ﻗﺴﻤﺖ ﺭﺍ ﻛﻪ ﻣﺸﺨﺺ ﻧﻤﺎﻳﻴﺪ ﺗﺼﺎﻭﻳﺮ ﻭ ﺳﺆﺍﻻﺕ ﺍﻣﺘﺤﺎﻧﻲ ﺁﻥ ﺑﺨﺶ ﺍﺭﺍﺋﻪ ﺧﻮﺍﻫﺪ ﺷﺪ . ﺁﻧﺎﺗﻮﻣﻲ ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻲ-٧ ﺁﻧﺎﺗﻮﻣﻲ ﻟﮕﻦ ﺧﺎﺻﺮﻩ-٦ ﺁﻧﺎﺗﻮﻣﻲ ﺷﻜﻢ-٥ ﺁﻧﺎﺗﻮﻣﻲ ﻗﻔﺴﻪ ﺳﻴﻨﻪ-٤ ﺁﻧﺎﺗﻮﻣﻲ ﺗﻨﻪ-٣ ﺁﻧﺎﺗﻮﻣﻲ ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ-٢ ﺁﻧﺎﺗﻮﻣﻲ ﺳﺮ ﻭ ﮔﺮﺩﻥ-١ ﻗﺪﺭﺕ ﺑﺰﺭﮔﻨﻤﺎﻳﻲ ﺗﺼﺎﻭﻳﺮ ﻭ ﻧﻴﺰ ﺣﺬﻑ ﻭ ﺍﺿﺎﻓﻪ ﻧﻤﻮﺩﻥ ﺗﺼﺎﻭﻳﺮ ﻣﻮﺭﺩ ﺩﻟﺨـﻮﺍﻩ ﻭ ﻧﻤـﺎﻳﺶ. ﺷﻤﺎ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻧﻮﻉ ﻣﻘﻄﻊ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﺭﺍ ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﻣﺸﺨﺺ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﻴﺪ. ﺑﻄﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩRelated images ﺗﺼﺎﻭﻳﺮ ﻭﺍﺑﺴﺘﻪ ﺑﻪ ﻫﺮ ﺑﺤﺚ ﺍﺯ ﻃﺮﻳﻖ ﺩﻛﻤﺔ ﭘﺎﺳﺦ ﺳﺆﺍﻻﺕ ﺑﻪShow Results ﺑﺎ ﺯﺩﻥ ﻛﻠﻴﺪ، ﻳﻚ ﺗﺼﻮﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﻣﻲﺁﻳﺪ ﻭ ﻧﺎﻡ ﺑﺨﺸﻲ ﺍﺯ ﺁﻥ ﻣﻮﺭﺩ ﺳﺆﺍﻝ ﺍﺳﺖtext ﺩﺭ ﭘﻨﺠﺮﺓStart test ﻧﺤﻮﺓ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺑﺪﻳﻦ ﺻﻮﺭﺕ ﺍﺳﺖ ﻛﻪ ﺑﺎ ﻓﻌﺎﻝ ﻧﻤﻮﺩﻥ. ﺗﺼﻮﻳﺮ ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻭﺟﻮﺩ ﺩﺍﺭﺩ٤ ﻭ٢ ،١ ﻫﻤﺰﻣﺎﻥ ﺍﺑﺘﺪﺍ ﺷﻤﺎ ﺩﺳﺘﮕﺎﻩ ﻳﺎ ﻧﺎﺣﻴﺔ، ﺩﺭ ﻧﻮﻉ ﺩﻳﮕﺮﻱ ﺍﺯ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ. ﺭﺍ ﺧﻮﺩ ﻣﻲﺗﻮﺍﻧﻴﺪ ﺑﻪ ﺩﻟﺨﻮﺍﻩ ﺗﻨﻈﻴﻢ ﻧﻤﺎﻳﻴﺪCD ﺯﻣﺎﻥ ﭘﺎﺳﺦ ﺑﻪ ﻫﺮ ﺳﺆﺍﻝ ﺩﺭ ﺍﻣﺘﺤﺎﻧﺎﺕ ﺍﻳﻦ. ﻗﺎﺑﻠﻴﺖ ﺍﺿﺎﻓﻪ ﻧﻤﻮﺩﻥ ﻳﺎﺩﺩﺍﺷﺖﻫﺎﻱ ﺷﺨﺼﻲ ﺑﻪ ﻫﺮ ﺗﺼﻮﻳﺮ ﻧﻴﺰ ﻭﺟﻮﺩ ﺩﺍﺭﺩ.ﻫﻤﺮﺍﻩ ﻧﻤﺮﺓ ﻧﻬﺎﻳﻲ ﺍﺭﺍﺋﻪ ﻣﻲﺷﻮﺩ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
55 ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﻣﻮﺭﺩﻧﻈﺮ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻣﻲﻧﻤﺎﻳﻴﺪ )ﻭ ﻧﻴﺰ ﺯﻣﺎﻥ ﭘﺎﺳﺦ ﻫﺮ ﺳﺆﺍﻝ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﻛﻨﻴﺪ( ﺑﺎ ﺯﺩﻥ ﻛﻠﻴﺪ Startﺍﻣﺘﺤﺎﻥ ﺷﺮﻭﻉ ﻣﻲﺷﻮﺩ .ﺩﺭ ﻫﺮ ﺳﺆﺍﻝ ﻧﺎﻡ ﺑﺨﺸﻲ ﺍﺯ ﻳﻚ ﺗﺼﻮﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﻣﻮﺭﺩﻧﻈﺮ ﺍﺳﺖ .ﺯﻣﺎﻥ ﺑﺎﻗﻴﻤﺎﻧﺪﻩ ﺑﺮﺍﻱ ﻫﺮ ﺳﺆﺍﻝ ﺩﺭ ﺣﻴﻦ ﺍﻣﺘﺤﺎﻥ ﺩﺭ ﺣﺎﻝ ﻧﻤﺎﻳﺶ ﺍﺳﺖ .ﺍﻳﻦ CDﻧﻮﺷﺘﺔ ﺩﻛﺘﺮ Pawlinaﻭ ﺩﻛﺘﺮ Olsonﻣﻲﺑﺎﺷﺪ ﻭ ﺑﺼﻮﺭﺕ Autorunﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ. Atlas of Clinical Medicine
3.12
Infection Cardiovascular Renal Joints and Bones Respiratory Endocrine, Metabolic and Nutritional )CECIL TEXTBOOK of MEDICINE (21st Edition
4.12
)(Version 2.0) (Forbes. Jackson
ــــ Blood Nerve and Muscle 2001
Gastrointestinal Liver and Pancreas
II SOCIAL AND ETHICAL ISSUES IN MEDICINE IV PREVENTIVE HEALTH CARE VI PRINCIPLES OF HUMAN GENETICS VIII RESPIRATORY DISEASES X RENAL AND GENITOURINARY DISEASES Part XI GASTROINTESTINAL DISEASES
Part Part Part Part Part
Part XIV ONCOLOGY Part XVI NUTRITIONAL DISEASES Part XVIII WOMEN'S HEALTH Part XX DISEASES OF THE IMMUNE SYSTEM Part XXII INFECTIOUS DISEASES Part XXIV DISEASES OF PROTOZOA AND METAZOA Part XXVI EYE, EAR, NOSE, AND THROAT DISEASES Part XXVIII LABORATORY REFERENCE INTERVALS AND VALUES
Part I MEDICINE AS A LEARNED AND HUMANE PROFESSION Part III AGING AND GERIATRIC MEDICINE Part V PRINCIPLES OF EVALUATION AND MANAGEMENT Part VII CARDIOVASCULAR DISEASES Part IX CRITICAL CARE MEDICINE Part XII DISEASES OF THE LIVER, GALLBLADDER, AND BILE DUCTS Part XIII HEMATOLOGIC DISEASES Part XV METABOLIC DISEASES Part XVII ENDOCRINE DISEASES Part XIX DISEASES OF BONE AND BONE MINERAL METABOLISM Part XXI MUSCULOSKELETAL AND CONNECTIVE TISSUE DISEASES Part XXIII HIV AND THE ACQUIRED IMMUNODEFICIENCY SYNDROME Part XXV NEUROLOGY Part XXVII SKIN DISEASES
BEST MEDICAL COLLECTION
2003
5.12
ﺍﻳﻦ CDﺩﺍﺭﺍﻱ ٧ﺑﺮﻧﺎﻣﺔ ﻣﺨﺘﻠﻒ ﻣﻲﺑﺎﺷﺪ ،ﻛﻪ ﻫﺮ ﻳﻚ ﺭﺍ ﺑﺎﻳﺪ ﺑﻄﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺍﺯ ﻓﺎﻳﻞ ﻣﺮﺑﻮﻁ ﺍﻧﺘﺨﺎﺏ ،ﻧﺼﺐ ﻭ ﺍﺟﺮﺍ ﻧﻤﻮﺩ .ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪﻫﺎ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ : -٧ﻧﺮﻡﺍﻓﺰﺍﺭ ﺳﻼﻣﺖ Health soft
-١ﺩﻳﻜﺸﻨﺮﻱ ﭘﺰﺷﻜﻲ -٢ ،ﻃﺐ ﺳﻮﺯﻧﻲ -٥ ،Health manger -٤ ،Multimedia workout -٣ ،ﺩﺍﺭﻭﻫﺎﻱ ﻧﺴﺨﻪﺍﻱ )) medical Drug Reference -٦ ،(Prescription Drugsﻣﺮﺟﻊ ﭘﺰﺷﻜﻲ ﺩﺍﺭﻭﻳﻲ( -١ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﻳﻜﺸﻨﺮﻱ ﭘﺰﺷﻜﻲ :ﻣﻔﺎﻫﻴﻢ ﻭﺍﮊﻩﻫﺎ ﻭ ﺍﺻﻄﻼﻋﺎﺕ ﭘﺰﺷﻜﻲ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﺗﻮﺳﻂ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺟﺴﺘﺠﻮ ﻧﻤﻮﺩ .ﻫﻤﭽﻨﻴﻦ ﺩﻭ ﻓﺼﻞ ﺑﺼﻮﺭﺕ :ﺍﻟﻒ( ﺳﻼﻣﺖ ﺧﺎﻧﻮﺍﺩﻩ ﺏ( ﺳﻼﻣﺖ ﻛﻮﺩﻛﺎﻥ ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﻫﺮ ﻗﺴﻤﺖ ﺩﺍﺭﺍﻱ ﻋﻨﺎﻭﻳﻦ ﻭ ﻣﻄـﺎﻟﺒﻲ ﺑﺼﻮﺭﺕ textﻣﻲﺑﺎﺷﺪ. -٢ﻃــﺐ ﺳــﻮﺯﻧﻲ :ﺷــﺎﻣﻞ ٩ﻓﺼــﻞ ﻣــﻲﺑﺎﺷــﺪ ﻛــﻪ ﺭﻭﺵ ﻛــﺎﺭ ﺑــﺎ ﻭﺳــﺎﻳﻞ ﻭ ﻧﺤــﻮﺓ ﺩﺭﻣــﺎﻥ ﺑﻴﻤﺎﺭﻳﻬــﺎ ،ﺑﺼــﻮﺭﺕ ﺗﻮﺿــﻴﺤﺎﺕ ﻣﺘﻨــﻲ ﺍﺭﺍﺋــﻪ ﺷــﺪﻩ ﺍﺳــﺖ .ﻳــﻚ ﻓــﻴﻠﻢ ﺭﺍﺟــﻊ ﺑــﻪ ﻃــﺐ ﺳــﻮﺯﻧﻲ ﻧﻴــﺰ ﻟﺤــﺎﻅ ﺷــﺪﻩ ﺍﺳــﺖ .ﺍﻳــﻦ ﺑﺮﻧﺎﻣــﻪ ﻣﺤﺼــﻮﻝ ﺷــﺮﻛﺖ Hopkins technologyﺳﺎﻝ ١٩٩٧ﻣﻲﺑﺎﺷﺪ. -٣ﺑﺮﻧﺎﻣﺔ workoutﻧﺴﺨﺔ :١ﺑﺎ ﻭﺍﺭﺩ ﻧﻤﻮﺩﻥ ﻣﺸﺨﺼﺎﺕ ﻓﺮﺩﻱ )ﺳﻦ ،ﻗﺪ ،ﻭﺯﻥ ،ﺟﻨﺴﻴﺖ ،ﻣﻴﺰﺍﻥ ﺍﻧﺮﮊﻱ ﭘﺎﻳﺔ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﻭ (...ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺭﮊﻳﻢ ﻏﺬﺍﻳﻲ ﻣﻨﺎﺳﺐ ،ﻧﻮﻉ ﻧﺮﻣﺶ ﺍﻭ ﻣﻮﺭﺩﻧﻈﺮ ﺭﺍ ﺑﻪ ﺷﻤﺎ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ .ﺍﻳـﻦ ﺑﺮﻧﺎﻣـﻪ ﻣﺤﺼـﻮﻝ ﺳـﺎﻝ ١٩٩٤ﺍﺳـﺖ ﻭ ﺩﺍﺭﺍﻱ ﭼﻨﺪﻳﻦ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﺍﺯ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻧﺮﻣﺶﻫﺎ ﻧﻴﺰ ﻣﻲﺑﺎﺷﺪ. :Health manager -٤ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺭ ﺣﻘﻴﻘﺖ ﺍﻃﻼﻋﺎﺕ ﺑﻴﻤﺎﺭﻱ ﻭ ﺳﻼﻣﺘﻲ ﺷﻐﻠﻲ ﺍﻓﺮﺍﺩ ﺭﺍ ﻣﺪﻳﺮﻳﺖ ﻣﻲﻛﻨﺪ .ﺑﺮﻧﺎﻣﻪﺍﻱ ﺍﺳﺖ ﺟﻬﺖ ﺿﺒﻂ ﻭ ﻧﮕﻬﺪﺍﺭﻱ ﻭﻗﺎﻳﻊ ﭘﺰﺷﻜﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﺷﺨﺼﻲ ،ﻟﻴﺴﺖ ﺩﺍﺭﻭﻫﺎﻱ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﺓ ﻓﺮﺩ ،ﺩﺍﺭﻭﻫـﺎﻱ ﺁﻟـﺮﮊﻱ ﻭ ﻳـﻚ ﻛﺘـﺎﺏ ﺁﺩﺭﺱ ﺍﺯ ﻣﺮﺍﻛﺰ ﻣﻬﻢ ﺑﻬﺪﺍﺷﺘﻲ ﻭ ﺩﺭﻣﺎﻧﻲ .ﺯﻣﺎﻥ ﺗﺠﺪﻳﺪ ﻭ ﺗﻌﻮﻳﺾ ﻧﺴﺨﺔ ﭘﺰﺷﻜﻲ ﻭ ﻣﺮﺍﺟﻌﻪ ﺑﻪ ﺩﻧﺪﺍﻧﭙﺰﺷﻚ ﺩﺭ ﺟﺪﺍﻭﻟﻲ ﻣﺸﺨﺺ ﻣﻲﺷﻮﺩ. -٥ﺩﺍﺭﻭﻫﺎﻱ ﻧﺴﺨﻪﺍﻱ :ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺗﻮﺿﻴﺤﺎﺕ ﻣﺨﺘﺼﺮﻱ ﺭﺍﺟﻊ ﺑﻪ ﺩﺍﺭﻭﻫﺎ ﻭ ﺍﻃﻼﻋﺎﺕ ﻓﺎﺭﻣﺎﻛﻮﻟﻮﮊﻳﻜﻲ ﻣﺮﺑﻮﻃﻪ ﺍﺭﺍﺋﻪ ﻣﻲﺩﻫﺪ .ﻣﺤﺼﻮﻝ ﺷﺮﻛﺖ Quanta Pressﺳﺎﻝ ١٩٩٢ﻣﻲﺑﺎﺷﺪ. -٦ﻣﺮﺟﻊ ﭘﺰﺷﻜﻲ ﺩﺍﺭﻭﻳﻲ ﻧﺴﺨﺔ :٢ﺍﺯ ﺳﻪ ﺭﺍﻩ ﻣﻲﺗﻮﺍﻥ ﻭﺍﺭﺩ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺪ ﻭ ﺍﺯ ﺁﻥ ﺍﺳﺘﻔﺎﺩﻩ ﻧﻤﻮﺩ: ﺏ( ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻣﻴﻠﺔ ﺟﺴﺘﺠﻮ ،ﻧﺎﻡ ﺩﺍﺭﻭ ﺭﺍ ﺗﺎﻳﭗ ﻧﻤﻮﺩﻩ ﻭ ﺁﻧﺮﺍ ﺑﻴﺎﺑﻴﺪ ﺝ( ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﻛﻠﻴﻪ ،Classﮔﺮﻭﻫﻬﺎﻱ ﺩﺍﺭﻭﻳﻲ ﻣﺨﺘﻠﻒ ﻣﻌﺮﻓﻲ ﻣﻲﮔﺮﺩﻧﺪ. ﺍﻟﻒ( ﻟﻴﺴﺖ ﺩﺍﺭﻭﻫﺎ :ﺩﺍﺭﻭﻱ ﻣﻮﺭﺩﻧﻈﺮ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻧﻤﺎﻳﻴﺪ ﻭ ﺍﻃﻼﻋﺎﺕ ﻻﺯﻡ ﺭﺍ ﺩﺭﻳﺎﻓﺖ ﻛﻨﻴﺪ. ﺩﺭﻣﻮﺭﺩ ﻫﺮ ﺩﺍﺭﻭ ،ﻣﻘﺪﺍﺭ ﻣﺼﺮﻑ ﺭﻭﺯﺍﻧﻪ ،ﺍﺛﺮﺍﺕ ﺟﺎﻧﺒﻲ ،ﺍﺷﻜﺎﻝ ﻣﺨﺘﻠﻒ ﺩﺍﺭﻭ ﻭ ﻫﺸﺪﺍﺭﻫﺎﻱ ﻻﺯﻡ ﺩﺭﻣﻮﺭﺩ ﺍﺛﺮﺍﺕ ﺳﻮﺀ ﺁﻥ ،ﺭﻭﺷﻬﺎﻱ ﻧﮕﻬﺪﺍﺭﻱ ﺩﺍﺭﻭ ﻭ . . .ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻣﺤﺼﻮﻝ ﺷﺮﻛﺖ Parsons Technologyﺳﺎﻝ ١٩٩٥ﻣﻲﺑﺎﺷﺪ. -٧ﻧﺮﻡﺍﻓﺰﺍﺭ ﺳﻼﻣﺖ ) : (Healthsoftﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺷﺎﻣﻞ ﺳﻪﺑﺨﺶ )ﺳﻪ ﺑﺮﻧﺎﻣﻪ( ﻣﺴﺘﻘﻞ ﻣﻲﺑﺎﺷﺪ: ﺍﻟﻒ( ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ﺗﻮﺿﻴﺤﺎﺗﻲ ﺭﺍﺟﻊ ﺑﻪ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ،ﻣﺮﺍﻗﺒﺖﻫﺎﻱ ﭘﺲ ﺍﺯ ﻋﻤﻞ ،ﺍﻋﻤﺎﻟﻲ ﻛﻪ ﺩﺭ ﺯﻣﺎﻥ ﺍﻭﺭﮊﺍﻧﺲ ﺑﺎﻳﺪ ﺍﻧﺠﺎﻡ ﺩﺍﺩ ﻭ . . .ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺍﺭﺍﻱ ﺗﺼﺎﻭﻳﺮ ﻣﺘﻌﺪﺩ ﻭ ﻧﻴﺰ ﺗﻠﻔﻆ ﺻﺤﻴﺢ ﺍﺻﻄﻼﺣﺎﺕ ﭘﺰﺷﻜﻲ ﻧﺎﺁﺷﻨﺎ ﻧﻴﺰ ﻣـﻲﺑﺎﺷـﺪ ،ﺑـﺎ ﺍﺳـﺘﻔﺎﺩﻩ ﺍﺯ ﻓﻬﺮﺳـﺖ ﺍﻟﻔﺒﺎﻳﻲ ﻣﻲﺗﻮﺍﻥ ﺍﻃﻼﻋﺎﺗﻲ ﺭﺍﺟﻊ ﺑﻪ ﻫﺮ ﻭﺍﮊﻩ ﺭﺍ ﭘﻴﺪﺍ ﻧﻤﻮﺩ. ﺏ( ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ،ﻋﻠﺖ ﺑﻴﻤﺎﺭﻳﻬﺎ ،ﻋﻼﺋﻢ ﻭ ﻧﺸﺎﻧﻪﻫﺎﻱ ﺑﻴﻤﺎﺭﻳﻬﺎ ،ﭘﻴﺸﮕﻴﺮﻱ ،ﻣﺮﺍﻗﺒﺖﻫﺎﻱ ﺑﻬﺪﺍﺷﺘﻲ ،ﺭﻭﺷﻬﺎﻱ ﺻﺤﻴﺢ ﻣﻌﺎﻟﺠﻪ ﻭ ﻧﻴﺰ ﺯﻣﺎﻥ ﻻﺯﻡ ﺑﺮﺍﻱ ﻣﺮﺍﺟﻌﻪ ﺑﻪ ﭘﺰﺷﻚ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
56 ﺝ( ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺍﻃﻼﻋﺎﺗﻲ ﺭﺍﺟﻊ ﺑﻪ ﺩﺍﺭﻭﻫﺎﻱ ﮊﻧﺘﻴﻚ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺛﺮﺍﺕ ﺟﺎﻧﺒﻲ ﺩﺍﺭﻭﻫﺎ ،ﻭﺍﻛﻨﺶ ﻧﺎﺳﺎﺯﮔﺎﺭﻱ ﺗﺪﺍﺧﻞ ﺩﺍﺭﻭﻳﻲ ﻭ . . .ﺩﺭ ﺍﻳﻦ CDﺍﺷﺎﺭﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻟﺒﺘﻪ ﺍﻳﻦ ﺍﻃﻼﻋﺎﺕ ﺗﻨﻬﺎ ﺟﻨﺒﺔ ﺁﮔﺎﻫﻲ ﺩﺍﺩﻥ ﺑﻪ ﻛﺎﺭﺑﺮ ﺭﺍ ﺩﺍﺷﺘﻪ ﻭ ﻧﻮﻳﺴﻨﺪﻩ ﻭ ﺷﺮﻛﺖ ﺗﻮﻟﻴﺪ ﻛﻨﻨﺪﺓ CDﻫﻴﭻ ﺗﻮﺻﻴﻪﺍﻱ ﺩﺭ ﺍﻳﻦ ﺧﺼﻮﺹ ﺍﺭﺍﺋﻪ ﻧﻤﻲﺩﻫﻨﺪ .ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻋﻼﻭﻩ ﺑﺮ ﺍﺭﺍﺋﺔ ﻧﺎﻣﻬﺎﻱ ﮊﻧﺘﻴﻚ ﻭ ﺗﺠﺎﺭﻱ ،ﮔﺮﻭﻫﻬﺎﻱ ﺩﺍﺭﻭﺋﻲ ﻭ ﻣﻮﺍﺭﺩ ﻛﺎﺭﺑﺮﺩﻱ ﺁﻧﻬﺎ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﻣﻘﺪﺍﺭ ﻣﺼﺮﻑ ﺩﺍﺭﻭ ،ﻋﻼﺋﻢ ﻭ ﻧﺸﺎﻧﻪﻫﺎﻱ Dverdoseﺩﺍﺭﻭﻫﺎ ،ﻣﻮﺍﺭﺩ ﻣﻨﻊ ﻣﺼـﺮﻑ ﺁﻧﻬـﺎ ﻭ ﺗﻠﻔﻆ ﺻﺤﻴﺢ ﻧﺎﻡ ﺩﺍﺭﻭ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. Clinical Examination
ــــــ Nervous system
Male genitalia
Heart & cardiovascular system
Respiratory system
Skin, nails & hair
Infants & children
Bones, joints & muscle
Abdomen
Femal breast & genittalia
Ear, nose & throah
CMDT CURREAT Medical Diagnosis & Treatment
7.12
Endoscopic Assessment of Esophagitis According to the Los Angeles Classification System
8.12
ــــــ ــــــ
6.12
ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ CDﺷﺎﻣﻞ :ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: y Viewing Area 1 :Slide Viewer 2: Slide Gallery 3:Video Gallery
3: Complicatins
2: Los Angeles Classification
2: On Endoscopic Assessment of Esophagitis
2002
1: Mucosal Break
y Definitions
1: International Working Group
y Quiz
GRIFFITH'S 5-MINUTE CLINICAL CONSULT
9.12
ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ،ﺍﻳﻦ CDﺑﺮﺍﻱ ﭘﺰﺷﻜﺎﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻭ ﺩﺳﺘﻲ`ﺍﺭﺍﻥ ﺑﺮﺍﻱ ﻣﺮﻭﺭ ﺳﺮﻳﻊ ﻭﻟﻲ ﺟﺎﻣﻊ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻋﻤﺪﻩ ﺩﺍﺧﻠﻲ ،ﺯﻧﺎﻥ ،ﭘﻮﺳﺖ ،ﺟﺮﺍﺣﻲ ،ﭼﺸﻢ ﻭ ENTﻭ ....ﮔﺮﺩﺁﻭﺭﻱ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻴﺶ ﺍﺯ ﻫﺰﺍﺭ ﻋﻨﻮﺍﻥ ﺑﻴﻤﺎﺭﻱ ﺑﻪ ﺗﺮﺗﻴﺐ ﺍﻟﻔﺒﺎ ﺗﺮﺗﻴﺐ ﻳﺎﻓﺘـﻪ ﺍﺳـﺖ ﻛﻪ ﺩﺭ ﻫﺮ ﻋﻨﻮﺍﻥ ﺟﺰﺋﻴﺎﺕ ﻛﺎﻓﻲ ﺑﺮﺍﻱ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﻭ ﭘﻴﮕﻴﺮﻱ ﺑﻴﻤﺎﺭﻱ ﻭﺟﻮﺩ ﺩﺍﺭﺩ .ﺑﻴﺶ ﺍﺯ ٣٣٠ﻧﻔﺮ ﻣﺘﺨﺼﺼﻴﻦ ﻣﺠﺮﺏ ﺩﺭ ﮔﺮﺩﺁﻭﺭﻱ ﺍﻳﻦ ﻣﺠﻤﻮﻋﻪ ﻫﻤﻜﺎﺭﻱ ﺩﺍﺷﺘﻪﺍﻧﺪ .ﺍﻳﻦ CDﺷﺎﻣﻞ ﺗﻮﺿﻴﺢ ﺑﻴﻤﺎﺭﻱﻫﺎ )ﺩﺭ ﺯﻳﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ( ﻭ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲ ،ﻧﻤﻮﺩﺍﺭ ﻭ ﺟﺪﻭﻝ ﻣﻲﺑﺎﺷﺪ. ﻋﻨﻮﺍﻥ ﻫﺮ ﺑﻴﻤﺎﺭﻱ ﺩﺭ ٦ﻗﺴﻤﺖ ﺍﺻﻠﻲ ﻭ ٣٦ﻗﺴﻤﺖ ﻓﺮﻋﻲ ﺑﻪ ﺗﻔﻀﻴﻞ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻣﺸﺮﻭﺡ ﻋﻨﺎﻭﻳﻦ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: 1- BASICS • Description • Genetics • Prevalence • Age • Signs and symptoms • Causes • Risk factors
2002
2000
2- DIAGNOSIS • Differential • Laboratory • Pathological findings • Special tests • Imaging
3- TREATMENT • Genral measures • Surgical measures • Activity • Diet • Patient education
4- MEDICATION • Drugs of choice • Contraindications • Precautions • Interactions • Alternate drugs
5- FOLLOW-UP • Monitoring • Prevention • Complications • Prognosis
6- MISCELLANEOUS • Associated conditions • Age-related factors • Pregnancy • Synonyms • ICD-9-CM • See also • Other notes • Abbreviations • References
)10.12 HEALTH ASSESSMENT (Gaylene Bouska Altman, RN, Ph.D., Karrin Johnson, RN, Robert W. Wallach, MD ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ٤ﺑﺨﺶ ﺭﺍﺟﻊ ﺑﻪ ﺍﺭﺯﻳﺎﺑﻲ ﺳﻼﻣﺖ ﻭ ﺁﺯﻣﺎﻳﺸﺎﺕ ﻭ ﻣﻌﺎﻳﻨﺎﺕ ﻓﻴﺰﻳﻜﻲ ﻣﻲﺑﺎﺷﺪ. ﺑﺨﺶ :١ﻣﺮﻭﺭﻱ ﺑﺮ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ :ﺷﺎﻣﻞ ١٧٥ﻗﺴﻤﺖ ﻫﻤﺮﺍﻩ ﺑﺎ ٥٩ﺗﺼﻮﻳﺮ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺯ ﺩﺳﺘﮕﺎﻫﻬﺎ ﻭ ﺍﻧﺪﺍﻣﻬﺎﻱ ﺑﺪﻥ ﺑﻪ ﻫﻤﺮﺍﻩ ﺍﻃﻼﻋﺎﺕ ﻣﺘﻨﻲ ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺗﻤﺎﻣﻲ ﻣﻄﺎﻟﺐ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﻣﺮﻭﺭ ﺷﺪﻩ ﺍﺳﺖ. ﺑﺨﺶ :٢ﺻﺪﺍﻫﺎﻱ ﻗﻠﺐ ﻭ ﺭﻳﻪ :ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺻﺪﺍﻫﺎﻱ ﻗﻠﺐ ﻭ ﺭﻳﻪ )ﺩﺭ ﺣﺎﻟﺖ ﺳﻼﻣﺘﻲ ﻭ ﺑﻴﻤﺎﺭﻱ( ﺩﺭ ﻫﻨﮕﺎﻡ ﻣﻌﺎﻳﻨﺔ ﻣﺮﻳﺾ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﻫﻤﭽﻨﻴﻦ ﻋﻤﻠﻜﺮﺩ ﻭ ﺳﺎﺧﺘﺎﺭﻫﺎﻱ ﻗﻠﺐ ﻧﻴﺰ ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ. ﺑﺨﺶ :٣ﻣﻬﺎﺭﺗﻬﺎﻱ ﺣﻴﺎﺗﻲ ﺩﺭ ﺍﺭﺯﻳﺎﺑﻲ ﺳﻼﻣﺘﻲ ﻭ ﻣﻌﺎﻳﻨﺎﺕ ﻓﻴﺰﻳﻜﻲ :ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺑﺼﻮﺭﺕ »ﺑﺮﺭﺳﻲ ﻭ ﻣﻄﺎﻟﻌﺔ ﻣﻮﺭﺩﻱ« ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ Case ٢٠ .ﻣﺨﺘﻠﻒ ﭘﺲ ﺍﺯ ﺍﺭﺍﺋﻪ ﺷﺮﺡ ﺣﺎﻝ ،ﻭﺿﻌﻴﺖ ﺑﻴﻤﺎﺭﻱ ﺁﻧﻬﺎ )ﺑﺼﻮﺭﺕ ﺳﺆﺍﻝ ﻭ ﺟﻮﺍﺏ( ﺗﻮﺳﻂ ﻛـﺎﺭﺑﺮ ﻣﺸـﺨﺺ ﻣـﻲﺷـﻮﺩ. ﻫﺪﻑ ﺍﺯ ﺍﻳﻦ ﺑﺨﺶ ﺍﻓﺰﺍﻳﺶ ﻗﺪﺭﺕ ﻭ ﻣﻬﺎﺭﺕ ﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﻧﺸﺠﻮﻳﺎﻥ ﺩﺭ ﺗﺸﺨﻴﺺ ﺑﻴﻤﺎﺭﻳﻬﺎﺳﺖ. ﺑﺨﺶ :٤ﺁﺷﻨﺎﻳﻲ ﺑﺼﺮﻱ ﺑﺎ ﻣﻌﺎﻳﻨﺎﺕ ﻓﻴﺰﻳﻜﻲ؛ ﻛﻪ ﺩﺍﺭﺍﻱ ٢Cﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ ،ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﻳﻚ ﺑﺮﻧﺎﻣﺔ ﺁﻣﻮﺯﺷﻲ ﻣﺼﻮﺭ ﻫﻤﺮﺍﻩ ﺑﺎ ﺍﺭﺍﺋﻪ ﺗﻌﺎﺭﻳﻒ ﻭ ﺍﺻﻄﻼﺣﺎﺕ ﻣﺮﺑﻮﻁ ﺑﻪ ﻣﻌﺎﻳﻨﺎﺕ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺭ ﻫﺮ ﭼﻬﺎﺭ ﺑﺨﺶ ﺍﻣﺘﺤﺎﻥ ﺑﺼﻮﺭﺕ ﺳﺆﺍﻻﺕ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﻧﻴﺰ ﻭﺟﻮﺩ ﺩﺍﺭﺩ. (11.12 MCCQE Review Nots and Lecture Series (Marcus Law & Brain Rotengberg Section Menu: Anesthesia, Cardiology, Color Atlas, Community Med, Dermatololgy, Diagnostic Imaging, Emergency, Endocrinology, Family Medicinne, Gastroenterology, General Surgery, Geriatrics, Gynecology, Hematology, Infectious Disease, Nephrology, Neurology, Neurosurgery, Obstetrics, Ophthalmology, Orthopedics, Otolaryngology, Pediatrics, Plastic Surgery, Psychiatry, Respirology, Rheumatology, Urology
2000 ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
)12.12 Medical Dictionary (Dorland's) (by W. B. Saunders ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
57 )13.12 MEDICAL Encyclopedia For Health Consumers (With Atlas TM )(The Best Internal Medicine Board Review 14.12 MedStudy
ــــ 2000
3. The Most Effective
4. The Most Talked About
2. The Most Powerful
1. The Most Board Specific
2002
)15.12 Natural Medicine Instructions for Patients (Lara U. Pizzorno, Joseph E. Pizzorno, Jr, Michael T. Murray
2002
16.12 Patient Teaching Aids ﻧﺮﻡﺍﻓﺰﺍﺭ ﺁﻣﻮﺯﺵ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﺑﻴﻤﺎﺭﺍﻥ ﻭ ﭘﺰﺷﻜﺎﻥ ﺩﺭ ﺭﺷﺘﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻃﺮﺍﺣﻲ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﺁﻣﻮﺯﺵﻫﺎﻱ ﻻﺯﻡ ﺭﺍ ﺩﺭ ﺑﺎﺑﺖ ﺍﻗﺪﺍﻣﺎﺕ ﺣﻤﺎﻳﺘﻲ ،ﺍﻗﺪﺍﻣﺎﺕ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻧﻲ ﺩﺭﺑﺮ ﺩﺍﺭﺩ .ﻣﻄﺎﻟﺐ ﺑﺮ ﺍﺳﺎﺱ ﻣﻮﺿﻮﻉ ﻭ ﺑﻴﻤﺎﺭﻱ ﺩﺳﺘﻪﺑﻨﺪﻱ ﺷﺪﻩﺍﻧﺪ ﻭ ﻫﺮ ﻣﻄﻠﺐ ﺣـﺪﻭﺩ ﻳـﻚ ﺻﻔﺤﻪ ﻣﻲﺑﺎﺷﺪ .ﺻﻔﺤﺎﺕ ﻗﺎﺑﻞ Printﻭ ﺍﺭﺍﺋﻪ ﺑﻪ ﺑﻴﻤﺎﺭﺍﻥ ﻫﺴﺘﻨﺪ .ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻧﻘﺶ ﺑﻴﻤﺎﺭ ﺭﺍ ﺩﺭ ﻓﺮﺁﻳﻨﺪ ﺩﺭﻣﺎﻥ ﺗﻘﻮﻳﺖ ﻛﺮﺩﻩ ﻭ ﺩﻳﺪﮔﺎﻩ ﻋﻠﻤﻲ ﻭ ﻣﻨﺎﺳﺒﻲ ﺑﻪ ﻭﻱ ﻣﻲﺩﻫﺪ ﻛﻪ ﺑﻪ ﺭﻭﻧﺪ ﻛﻠﻲ ﺳﻼﻣﺖ ﻭ ﺑﻬﺒﻮﺩ ﻛﻤﻚ ﺑﺴﺰﺍﻳﻲ ﺩﺍﺭﺩ .ﻗﺎﺑﻠﻴﺖ Searchﻗـﻮﻱ ﻭ ﻧﻴـﺰ ﺍﺿﺎﻓﻪﻛﺮﺩﻥ ﻧﻮﺷﺘﻪ ﺑﻪ ﻣﺘﻦ ﺍﺯ ﻣﺰﺍﻳﺎﻱ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩ .ﺣﺪﻭﺩ ٤٠٠ﺳﺮﻓﺼﻞ ﻛﻪ ﻫﺮ ﻛﺪﺍﻡ ﺷﺎﻣﻞ ﭼﻨﺪ Tapicﻋﻤﺪﻩ ﻭ ﺷﺎﻳﻊ ﻣﻲﺑﺎﺷﺪ ﺭﺍ ﻣﻲﺗﻮﺍﻥ ﺑﺮﺍﺣﺘﻲ ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻳﺎﻓﺖ. )(Third Edition
ــــ
)17.12 Practical General Practice (Guidelines for effective clinical management) (Alex Khot, Andrew Polmear
2002
)18.12 RAPID REVIEW FOR USMLE STEP 1 (Mosby y Anatomy y Behavioral Science y Biochemistry y Histology/Cell Biology y Microbiology/Immunology y Neuroscience y Pathology y Pharmocology y Physiology y Randomize All
Sciences:
2003
19.12 SPSS 12.0 for Windows
2002
)20.12 Textbook of Physical Diagnosis HISTORY AND EXAMINATION (Fourth Edition) (Mark H. Swartz, M.D.) (W.B. SAUNDERS COMPANY 21.12 The Basics for Interns
ــــ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺷﺎﻣﻞ ٦ﻓﺼﻞ ﺍﺻﻠﻲ ﺍﺳﺖ: -١ -٢ -٣ -٤ -٥ -٦
) airway Managementﺍﺭﺯﻳﺎﺑﻲ ﻣﺴﻴﺮ ﺭﺍﻫﻬﺎﻱ ﻫﻮﺍﻳﻲ ،ﻛﻨﺘﺮﻝ ﻣﺴﻴﺮ ﺭﺍﻫﻬﺎﻱ ﻫﻮﺍﻳﻲ ﺩﺭ Apneaﻭ hypoxiaﻭ ، . . .ﺍﺑﺰﺍﺭﻫﺎﻱ ﻣﻮﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺩﺭ ﻣﺴﻴﺮﻫﺎﻱ ﻫﻮﺍﻳﻲ ﺑﻴﻨﻲ ﻭ ﺩﻫﺎﻥ ،ﺭﻭﺷﻬﺎﻱ ﺑﻴﻬﻮﺷﻲ ،ﻭ ﻧﻴﺘﻼﺳﻴﻮﻥ ﻣﺎﺳﻚ ﻛﻴﺴﻪﺍﻱ ،ﻟﻮﻟﻪﮔﺬﺍﺭﻱ ﻧﺎﻱ ﺗﺮﺍﻛﻨﻮﺗﻮﻣﻲ( ﺗﻔﺴﻴﺮ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﺍﻭﻟﻴﺔ ﺗﺼﻮﻳﺮ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ )ﺷﺎﻣﻞ ﺗﺼﺎﻭﻳﺮ – Chest x-rayﺗﺼﺎﻭﻳﺮ Abdominal x-rayﻭ (CT-scan ﻣﺪﻳﺮﻳﺖ ﺟﺮﺍﺣﻲ ﺯﺧﻢﻫﺎ )ﺷﺎﻣﻞ ﻧﺦﻫﺎﻱ ﺟﺮﺍﺣﻲ – ﻣﻌﺮﻓﻲ ﺍﺑﺰﺍﺭ ﻭ ﻭﺳﺎﻳﻞ ﺟﺮﺍﺣﻲ – ﻧﻤﺎﻳﺶ ﻧﺤﻮﺓ ﺍﻧﻮﺍﻉ ﺑﺨﻴﻪ ﺯﺩﻥﻫﺎ ،ﺭﻭﺵ ﭘﺎﻧﺴﻤﺎﻥ ﺯﺧﻢﻫﺎ ( . . . ﺩﺳﺘﺮﺳﻲ ﺑﻪ ﺷﺮﻳﺎﻥﻫﺎ )ﺷﺎﻣﻞ ﺷﺮﻳﺎﻥ ﺭﺍﺩﻳﺎﻝ – ﺷﺮﻳﺎﻥ ﻓﻤﻮﺭﺍﻝ( ﺩﺳﺘﺮﺳﻲ ﻭ ﺑﻜﺎﺭﮔﻴﺮﻱ ﺳﻴﺎﻫﺮﮒﻫﺎ )ﻣﻌﺮﻓﻲ ﻭﺳﺎﻳﻞ ﺟﻬﺖ ﺩﺳﺘﺮﺳﻲ ﻃﻮﻻﻧﻲ ﻣﺪﺕ ﺑﻪ ﺳﻴﺎﻫﺮﮒﻫﺎ -ﺍﺭﺯﻳﺎﺑﻲ ﭘﻴﺶ ﺍﺯ ﻋﻤﻞ ﻭ ﺗﺪﺍﺭﻛﺎﺕ ﻻﺯﻡ – ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺑﺮﺷﻲ ﺳﻴﺎﻫﺮﮒﻫﺎ ﻭ ﺍﻳﻤﭙﻠﻨﺖﻫﺎﻱ ﺯﻳﺮﭘﻮﺳﺘﻲ ﻭ ( . . . ﺩﺭ ﻧﺎﮊ ﻭ ﺗﺨﻠﻴﻪ ﭘﻠﻮﺭﺍﻝ ) :ﻣﻮﺍﺭﺩ ﺍﺳﺘﻌﻤﺎﻝ ،ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ،ﺗﻜﻨﻴﻚ ﺗﻮﺭﺍﺳﻨﺘﺰ ،ﺗﻜﻨﻴﻚ ﺗﻴﻮﺏ ﺗﻮﺭﺍﻛﻮﺳﺘﻮﻣﻲ (
-٧
ﺗﻤﺎﻣﻲ ﻣﺒﺎﺣﺚ ﻋﻨﻮﺍﻥ ﺷﺪﻩ ﺩﺭ ﺑﺎﻻ ﺑﺼﻮﺭﺕ ﻓﻴﻠﻤﻐﻬﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻭ ﺗﺼﺎﻭﻳﺮ ﻣﺘﻌﺪﺩ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ ﮔﻮﻳﻨﺪﻩ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻓﻴﻠﻤﻐﻬﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻳﺎ ﺑﺼﻮﺭﺕ ﻭﺍﻗﻌﻲ ﺍﺳﺖ ﻭ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ﺑﺮﺭﻭﻱ ﻣﺮﻳﺾ ﺩﻗﻴﻘﹰﺎ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﻳﺎ ﺑﺼﻮﺭﺕ ﺍﻧﻴﻤﻴﺸﻦ ﺍﺳﺖ.
ــــ
)22.12 Understanding Lung Sounds (Audio CD
ــــ
)23.12 UNDERSTANDING PATHOPHYSIOLOGY (Second Edition) (Sue E. Huether, Kathryn L. McCance
ــــ
)(W.B. Saunders Company
th )24.12 Virtual Medical Office CHALLENGE (to accompany Bonewit-West Clinical Procedures for Medical Assistants, 5 Edition
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ CaseStudyﻫﺎﻱ ﻣﺘﻌﺪﺩ ﻣﻄﺮﺡﺷﺪﻩ ﻛﺎﺭﺑﺮ ﺭﺍ ﺑﻪ ﺍﺳﺘﻔﺎﺩﻩ ﺑﺎﻟﻴﻨﻲ ﺍﺯ ﺍﻃﻼﻋﺎﺕ ﺍﺭﺍﺋﻪﺷﺪﻩ ﺩﺭ ﻛﺘﺐ ﺭﻓﺮﺍﻧﺲ ﻋﺎﺩﺕ ﻣﻲﺩﻫﺪ .ﺩﺭ ﻋﻴﻦ ﺣﺎﻝ ﺷﻴﻮﺓ ﺣﻞ ﻣﺸﻜﻼﺕ ،ﻗﺪﺭﺕ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺑﻪ ﺿﺮﺍﻓﺖﻫﺎﻱ Criticalﻭ Triage ﻛﻪ ﺍﺯ ﻣﻬﻤﺘﺮﻳﻦ ﻣﻬﺎﺭﺕﻫﺎ ﺑﺎﻟﻴﻨﻲ ﭘﺰﺷﻜﺎﻥ ﻭ ﻛﺎﺩﺭ ﭘﺰﺷﻜﻲ ﻣﺤﺴﻮﺏ ﻣﻲﮔﺮﺩﺩ ،ﺩﺭ ﻃﻲ ﻣﺮﺍﺣﻞ ﻣﺘﻌﺪﺩ ﻭ ﺑﻪ ﺻﻮﺭﺕ ﻋﻤﻠﻲ ﻭ ﺳﻤﻌﻲ ﺑﺼﺮﻱ ﺁﻣﻮﺯﺵ ﻭ ﺗﻤﺮﻳﻦ ﻣﻲﮔﺮﺩﻧﺪ .ﺍﻳﻦ CDﺷﺎﻣﻞ ﭼﻬﺎﺭ ﺳﺮﻓﺼﻞ ﻋﻤﺪﻩ ﺑﻪ ﻗﺮﺍﺭ ﺯﻳﺮ ﺍﺳﺖ: -Help
- Challenge Status
- Clinical Skills
- Case Study
ﺗﻐﺬﻳﻪ 2002 ___ 2002 ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
)25.12 Contemporary Nutrition Food Wise (Food Wise, Weight Manager )26.12 Food Works (College Edition )27.12 INTRODUCTION TO NUTRIOTION AND METABOLISM (Third Edition) (DAVID A Bender ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
58 28.12 Multimedia Workout
(Jeffrey S. Smith, Joseph D. Cook)
ــــ
29.12 NUTRIENTS IN FOOD (Elizabet S. Hands)
2002
30.12 THE FOOD LOVER'S ENCYCLOPEDIA Culinary Techniques Recipes Nutrition Foods
ــــ
ﺩﺍﺭﻭﺋﻲ-١٣
CD ﻋﻨﻮﺍﻥ 1.13
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
American DRUG INDEX (FACTS AND COMPARISONS)
2.13 Appleton and Lange's Quick Review PHARMACY -Parmaceutics/Pharmokinetics
-Pharmacology
2001 ___
(Twelfth Edition) (Joyce A. Generali, Christine A. Berger)
: ﺩﺭ ﻣﻮﺭﺩ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺑﺤﺚ ﻣﻲﻛﻨﺪCD ﺍﻳﻦ
-Microbiology and Public Health
-Chemistry and Biochemistry
-Physiology/Pathology
-Clinical Pharmacy
3.13 British Pharmacopoeia (version 6.0) Vol 1: -Notices -Preface -British Pharmacopoeia Commision -Introduction -General Notices -Monographs: Meidicinal and Pharmaceutical Substances Vol 2: -Notices -General Notices -Monographs -Infrared Reference Spectra -Appendices -Supplementary Chapters British Pharmacopoeia (Veterinary): -Preface -British Pharmacopoeia Commission -Introduction -General Notices -Monographs -Infrared Reference Spectra -Appendics th 4.13 CLINICAL DRUG THERAPY Rationnales for Nursing Practice (7 Edition) (ANNE COLLINS ABRAMS) (Lippincott Williams & Wilkins) -Dosage Calc Challenge!
-Animations
-NCLEX Questions
-Monographs of 100 Most Commonly Prescribed Drug
-Preventing Medication Errors Video
2002
___
-Patient Teaching Sheets
5.13
Chem Office (Renate Buergin Schaller)
___
6.13
DERIVATIZATION REACTIONS FOR HPLC (Georgelunn, Louise C. Hellwic)
___ 2000
7.13 Dosages and Solutions CD Conpanion (Virginia Daugherty, RN, MSN, Diana Romans, RN, BSN) (Harcourt Health Sciences)
8.13
-Mathematics Review -Introducing Drug Measures -How to Read a Drug Label -Calculatin Dosages DRU ERUPTION REFERENCE MANUAL (The Parthenon Publishing Group) (Jerome Z. Litt, MD) Search by:
- Drug Name
-Reactions
9.13
DRUG CONSULT (Mosby)
10.13
Drug Identifier Find Products by: -Drug name
-Interactions
-Categories
-Company
-Multiple Search
: ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯCD ﻋﻨﺎﻭﻳﻦ ﺍﻳﻦ
-Comprehensive Posttest 2004 -Printing
-Common
-Reaciton ___ 2003
-Imprint
-NDC code
-Manufacturer name
11.13 GoodMan and Gilmans's CD-ROM
___
12.13 HERBAL MEDICINE Expanded Commission E Monographs (INTEGRATIVMEDICINE)
___
13.13 Herbal Remedy FINDER
___
14.13 HPLC and CE METHODS for Pharmaceutical Analysis
(Version 2.0)
(George Lunn) (John Wiley and ons)
15.13 Patient Education Guide to Oncology Drugs Name Search – Categories – Comparisons
2000 ___
(Gail M. Wilkes, RNC, MS, AOCN, Terri B. Ades, RN, MS, AOCN)
16.13 PDQ PHARMACOLOGY (GORDON E. JOHNSON, PHD)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
2002 ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
59 PDR® Electronic Library™ PHYSICIANS DESK REFERENCE (Thomson Medical Economics).
2004
ﺍﺭﺍﺋـﻪ ﺷـﺪﻩﺍﻧـﺪ ﺍﺯ ﻣﻌﺘﺒﺮﺗـﺮﻳﻦ ﻭ ﺟﺪﻳـﺪﺗﺮﻳﻦCD ( ﻓﺎﺭﻣﺎﻛﻮﻟﻮﮊﻱ ﻛﻪ ﺑﻪ ﺻﻮﺭﺕPDR, PDQ) ﺩﻭ ﺭﻓﺮﺍﻧﺲ. ﻭﺟﻮﺩ ﻳﻚ ﺭﻓﺮﺍﻧﺲ ﺟﺎﻣﻊ ﻭ ﻣﻌﺘﺒﺮ ﺍﻃﻼﻋﺎﺕ ﺩﺍﺭﻭﺋﻲ ﺿﺮﻭﺭﻱ ﻣﻲﻧﻤﺎﻳﺪ، ﺻﺮﻓﻨﻈﺮ ﺍﺯ ﻧﻮﻉ ﺗﺨﺼﺺ،ﺩﺭ ﻣﻄﺐ ﺭﻭﻱ ﻣﻴﺰ ﻛﺎﺭ ﻫﺮ ﭘﺰﺷﻚ . ﺭﺍ ﺑﻪ ﺩﺳﺖ ﺁﻭﺭﺩ... ﻋﻮﺍﺭﺽ ﺟﺎﻧﺒﻲ ﻭ، ﻛﻨﺘﺮﺍﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ، ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ،ﻣﺮﺍﺟﻊ ﺩﺍﺭﻭﺷﻨﺎﺳﻲ ﻣﻲﺑﺎﺷﻨﺪ ﻛﻪ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﻧﻬﺎ ﻣﻲﺗﻮﺍﻥ ﺩﺭ ﻛﻤﺘﺮﻳﻦ ﺯﻣﺎﻥ ﻣﻤﻜﻦ ﻛﻠﻴﺔ ﺍﻃﻼﻋﺎﺕ ﻻﺯﻡ ﺩﺭ ﻣﻮﺭﺩ ﺩﺍﺭﻭﻱ ﻣﻮﺭﺩ ﻧﻈﺮ ﻣﻦﺟﻤﻠﻪ ﺩﻭﺯﺍﮊ PDQ Pharmacology ( ﻃﺮﻳﻘﺔ ﻧﺼﺐ . ﻛﻨﻴﺪNext ﭘﻨﺠﺮﺓ ﺟﺪﻳﺪﻱ ﺑﺎﺯ ﻣﻲﺷﻮﺩ. ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ١ ﺑﻨﺎﺑﺮﺍﻳﻦ ﮔﺰﻳﻨﺔ. ﺭﺍ ﻧﺼﺐ ﻛﻨﻴﻢAcroba Reader ﭘﻨﺠﺮﻩﺍﻱ ﻇﺎﻫﺮ ﻣﻲﺷﻮﺩ ﺑﺮﺍﻱ ﺷﺮﻭﻉ ﻣﻲﺑﺎﻳﺴﺘﻲ ﺑﺮﻧﺎﻣﺔ. ﺑﺮﻧﺎﻣﻪ ﺑﺼﻮﺭﺕ ﺍﺗﻮﻣﺎﺗﻴﻚ ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩ، ﺭﺍ ﺩﺭﻭﻥ ﺩﺭﺍﻳﻮ ﻗﺮﺍﺭ ﻣﻲﺩﻫﻴﻢCD ﺍﺑﺘﺪﺍ Adobe ( ﺍﻳـﻦ ﺑﺮﻧﺎﻣـﻪ ﺗﺤـﺖ ﺑﺮﻧﺎﻣـﺔStart) ﺭﺍ ﺍﺯ ﺍﻭﻟـﻴﻦ ﭘﻨﺠـﺮﻩ ﺍﻧﺘﺨـﺎﺏ ﻛﻨﻴـﺪ٢ ﺑﺮﺍﻱ ﺍﺟﺮﺍﻱ ﺑﺮﻧﺎﻣﺔ ﺍﺻﻠﻲ ﮔﺰﻳﻨﺔ. ﺭﺍ ﻓﺸﺎﺭ ﺩﻫﻴﺪOK ﺩﺭ ﻧﻬﺎﻳﺖ. ﻛﻨﻴﺪNext ﭘﻨﺠﺮﺓ ﻓﻌﻠﻲ ﻣﺴﻴﺮ ﻧﺼﺐ ﺭﺍ ﻣﺸﺨﺺ ﻣﻲﻛﻨﺪ ﺩﺭ ﺻﻮﺭﺕ ﺗﻮﺍﻓﻖ ﺑﺎ ﺁﻥ . ﻗﺎﺑﻞ ﺍﺟﺮﺍ ﺍﺳﺖAerobat Reader 17.13 PHARMACOLOGY (Thomas L. Pazderink, Laszlo Kerecsen, Mrugshkumar K. Shah) (Mosby) 18.13 PHYSICANAS' CANCER CHEMOTHERAPHY DRUG MANUAL - Principles of Cancer Chemotheraphy - Common Chemotherapy Regimens in Clinical Practice
19.13 The Herbalist
-Basic Principles
(David L. Hoffman) -Human Systems
2003 2004
(Jones & Bartlett)
:ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺩﺭ ﻣﻮﺭﺩ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﺑﺤﺚ ﻣﻲﻛﻨﺪ
- Physician's Cancer Chemotherapy Drug Manual 2004 - Guidelines for Chemotherapy and Dosing Modifications - Antimetic Agents for the Treatment of Chemotherapy-Induced Nausea and Vomiting
___ -Actions
-Herbal Materia Medica
20.13 THE MERCK INDEX on CD-ROM (Version 12:3)
2000
21.13 USP 26-NF 21 Through Supplement Two (U.S. PHARMACOPEIA) (The standard of Quality)
(The United States Phamocopeial Convention, Inc)
2003
ﺯﺑﺎﻥ:١٤
CD ﻋﻨﻮﺍﻥ
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
1.14
BUILDING A MEDICAL VOCABULARY (FIFTH EDITION) (FEGGY C. LEONARD) (W.B. Saunders Company)
2001
2.14
ELECTRONIC MEDICAL DICTIONARY (STEDMAN'S) (LIPPINCOTT WILLIAMS & WILKINS)
2001
3.14
English Family (Merriam-Webster)
ــــ
4.14
Entertainment Collection
ــــ
5.14
How to Prepare for TOEFL
ــــ
6.14
Learn To Speak English Dictionary & Grammer
7.14
Mad About English Spelling (Interactive Learning)
(CD1-4)
ــــ ــــ
8.14 Medical Information on the Internet (A Guide for Health Professionals) (Second Edition) Why use the Internet? Internetive Learning The future Appendix D: Configuring TCP/IP
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
Getting Wired E-mail, discussion lists and newsgroups Appendix A: Finding more information information Appendix E: Glossary
(Robert Kiley)
ــــ
Finding what you want The quality issue Appendix B: Netscape Navigator and Internet
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
The top ten medical resources Consumer health information Appendix C: Optimising your computer
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
60 9.14
Preparation For the TOEFL (Dictionary Crossword Puzzle Matching Game)
ــــ
10.14 Preparing for the GRE Writing Assessment
ــــ
What does the GRE General Test measure? The GRE General Test is designed to measuregeneral knowledge and reasoning skills in three areas that are important for a academic achievement: Verbal Ability Quantitative Ability Analytical Ability 11.14 Speak Fluent Series
ــــ
12.14 Studying a Study Texting a Test (Fourth Edition) (Richard K. Riegelman)
ــــ
Accreditation Statement Designation Statement
Instructions to Users Target Audience
Lippincott Williams & Wilkins Test-CME Needs Assessment
Continuing Medical Education Glossary
CME User assessment Learning Objectives
Faculty Credentials/Disclosure
13.14 The AMERICAN HERITAGE® TALKING DICTIONARY (Daniel Finkel) 14.14 THE LANGUAGE OF MEDICINE (6
TH
1. Word Ports
(Chapters 1-4)
ــــ 2000
EDITION) (W.B. Saunders Company)
2.Body Systems
(Chapter 5-18)
3. Specialties
(Chapter 19-22)
15.14 TriplePlayPlus! ENGLISH (Syracuse Languag Systems)
ــــ
16.14 Users' Guides To The Medical Literature (A manual for Evidence-Based Clinical Practice) (Gordon Guyatt, MD, Drummond Rennie, MD, Robert Hayward, MD)
2002
ﺟﺮﺍﺣﻲ-١٥
CD ﻋﻨﻮﺍﻥ 1.15
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
1. Reflux Disease and Nissen Fundoplication (Philip E. Donahue, MD) (VCD)
ــــ
2. Supraceliac Aortic-Celiac Axix-Superior Mesenteric Artery Bypass (Gregorio A. Sicard, Charles B. Anderson) 2.15
Advanced Therapy in THORACIC SURGERY (Kenneth L. Franco, MD, Joe B. Putnam Jr., MD)
ــــ
3.15
Aesthetic Department
ــــ
ARTECOLL: Injectable micro-Implant, for long lasting levelling of facial wrinkles and folds M-Implants By Rofil THE BEAUTY PHILOSOPHY: M-Implantans by Rofil you and your patients with the highest quality mammary implants in every option possible. 4.15
American Collage of Surgeons ACS Surgery Principles & Practice (CDI , II)
ــــ
5.15
Aspects of Electrosurgery (Dr. Anthony C. Easty, PhD PEng CCE) Department Medical Engineering
6.15
Atlas of Liposuction (Tolbert s. Wilkinson, MD)
ــــ ــــ
7.15
Atlas of RENAL TRANSPLANTATION
8.15
-Histopathology -surgery -clinical section -imaging -immunology Basic Surgical Skills (David A. Sherris. M.D., Eugene B. Kern, M.D.) (Mayo Clinic)
9.15
Breast-Augmentation with NovagoldTM
(Prof. Legndre, Martin, Helenon, Lebranchu, Halloran, Nochy) -immunosupperssive
The PVP-Hydrogel Filled Implant
10.15 Case Presentations In Plastic Surgery (Christopher Stone, Consultant Plastic Surgeon)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ــــــ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ــــ ــــ 2004
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
61 11.15 Cholecystectomy by Laparoscopy (Department of Surgery Hospitalor Saint-Avold France) (VCD)
ــــ
12.15 Clinical Surgery (Second Edition) (Michael M. Henry, Jeremy N. Thompson)
ــــ
13.15 Core Curriculum in Primary Care Patient Evaluation for Non-Cardiac Surgery and Gynecology and Urology (Michael K. Rees, MD, MPH)
ــــ
1. Appendicectomy
2. Highly Selective Vagotomy
3. Taylor's Operation
. ﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖHarvard ﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲCD ﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯCCC ﺳـﺆﺍﻻﺕ ﻣﺮﺑﻮﻃـﻪ ﺑـﻪ، ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜﻲ. ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛﺎﺭﺑﺮ ﻣﻲﺑﺎﺷﺪ. ﺯﻧﺎﻥ ﻭ ﺍﻭﺭﻭﮊﻱ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖ، ﺣﺎﺿﺮ ﺩﺭ ﻣﻮﺭﺩ ﺟﺮﺍﺣﻲCD : ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ. ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﻘﺎﻟﻪ ﭼﺎﭘﻲ ﺩﺭ ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ.ﺻﻮﺭﺕ ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ Male impotence
ﻋﻘﻴﻤﻲ ﻣﺮﺩﺍﻥ-٣
.(AUB) ﺍﺭﺯﻳﺎﺑﻲ ﺧﻮﻧﺮﻳﺰﻱﻫﺎﻱ ﺍﺑﻨﺮﻣﺎﻝ ﺭﺣﻢ
-٢
ﭼﮕﻮﻧﻪ ﻳﻚ ﺑﻴﻤﺎﺭ ﺭﺍ ﺑﺮﺍﻱ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ )ﺑﺠﺰ ﺟﺮﺍﺣﻲ ﻗﻠﺐ( ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺁﻣﺎﺩﻩ ﻛﻨﻴﻢ؟-١ . ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖtext ﺳﺆﺍﻻﺕ ﺷﻨﻮﻧﺪﮔﺎﻥ ﻭ ﺟﻮﺍﺏ ﺳﺨﻨﺮﺍﻥ ﻧﻴﺰ ﺑﻪ ﺻﻮﺭﺕ،ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ
12.3
Core Curriculum in Primary Care Gynecology (Michael, Isaac Schiff, Keith, Thomas, Annekathryn)
14.15 Core Curriculum in Primary Care Gynecology 15.15
19.15 20.15 21.15 22.15 23.15 24.15 25.15
management of the aging face)
18.15
(A practical and systematic guide to surgical
17.15
ــــــ
(Michael, Isaac Schiff, Keith, Thomas, Annekathryn)
VCD 1: Rhinophyma (9:52) - Alloderm Lip Augmentation (14:04) - Collagen Injection Sequence COMPREHENSIVE FACIAL REJUVENATION
16.15
ــــــ
VCD 2: Full-Face Jessner’s/35% Trichloroacetic Acid Pell (31:21)
ــــ
VCD 3: Combined Resurfacing Technique for Aone Scarring (10:18) Botox Reconstitution and Injection Sequence (20:53) - Carbon Dioxide Laser Resurfacing (8:10)
ــــ 2000
VCD 4: Postoperative Care of the Chemical Peel Patient (31:21) VCD 5: Transconjunctival Lower-Lid Blepharoplasty (9:05) Skin-Muscle Flap Lower-Lid Blepharoplasty with Midface Extension (16:20)
ــــ
VCD 6: Follicular Transfer Hair Transplantation Session (30:20)
ــــ
VCD 7: Upper-Lid Blepharoplasty (11:25) - Chin Augmentation with Gore-Tex Alloplast (13:21)
ــــ
VCD 8: Minimal Incision Brow and Midface Lift (31:02)
ــــ
VCD 9: Primary Facelift (37:17)
ــــ
VCD 10: Secondary Facelift with Gore-Tex Sling (30:21)
ــــ ــــ
VCD 11: Scalp Reduction Sessions (31:47)
26.15 LAPAROTOMY (Royal Society of Medicine in association with Royal College of Surgeons of England) (VCD)
ــــ
27.15 Lipostructure (Sydncy Coleman, M.D.) (byron) (VCD)
ــــ
28.15 Lower Body Lift (Abdominoplasty) (Lockwood, M. d., Kansas Gity) (VCD) (CD I , II)
ــــ
29.15 MALAR AUGMINTATION (CLINICAL MIRASIERRA MADRID)
ــــ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
(Ulrich T. Hinderer Dr. Juan L. Del Rio) (VCD)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
62 30.15 Mammary augmention by High-Cohesive Silicon Gel Implant
ــــ
(Igar Nicchajev, Goran Jurell)
31.15 Mastery of Endoscopic & Laparoscopic Surgery (Second Edition)
2005
32.15 NMS Surgery Tutor
2000
(Dereck Mooney, T. Mack Brown, Cristian Jansenson, Denise Riedlinger)
ــــ
33.15 Open Repair of Abdominal Wall Hernias Using Prosthetic materials (Arthur I. Gilbert, M.D.)
-Small Bowel Obstrution Immediately Following Laparoscopic Herniorraphy (Karl A. Zucher, MD) -VJGS Case Study: Laparoscopic Loop Ilestomy for Temporary Fecal Diversion (Steven D. Wexner, Petachia Reissman) -VJGS Consultants Corner: Managed Care Update, Pt, III (Michael A. Wood) 34.15 Plastic and Reconstructive Breast Surgery (Second Edition) (Volume 1 , 2)
ــــ
35.15 Plug Repair for Inguinal Hernias 1- First Case: Inguinal Hernia type "Direct" 25.6 Practical MINOR SURGERY
ــــ 2- Second Case: Injuinal Hernia type "Indirect"
ــــ 2005
36.15 Principles of Surgery (Eight Edition) (Schwartz's) (E-Book) (CD I , II) Part1: Basic Considerations Part II: Specific Considerations 37.15 Single Puncture Laparoscopic Technique (Marco Pelosi, MD) (VCD)
ــــ 2004
38.15 Structural Fat Grafting (Sydney R. Caleman) (E-book & Film) 39.15 Submitted Subject: Transvaginal Sonographic Assessment of Pelvic Pathology: Preoperative Evaluation 40.15 SURGERY (John D Corson, Robin CN Willimson) -Surgical Principles and Critical Care
-Trauma
(Frances R. Batzer, MD)
(Launching Slide Vision) (Mosby)
-Gastrointestinal surgery
-Vascular Surgery
-Brast and Endoceine Surgery
-Transplantation Surgery
41.15 Surgery of the Liver & Biliary Tract 3e: Selected Operative Procedures (L.H. BLUMGART, Y. FONG)
-Allied Surgical Specialties
(W.B. Saunders)
-Hepatic Procedures -Biliary Procedures -Special Procedures The Distal Splenorenal Shunt: Effective or Obsolete? (VIDEO JOURNAL OF GENERAL SURGERY) (Layton Fredrick Rikkers, M.D.) (VCD) 42.15 - Options for Treating Portal Hypertension -HIPS Advantages
-Ideal Candidates for Distal Splenorenal Shunt -HIPS Disadvantages
ــــ ــــ 2000 ــــ
-Components of Distal Splenorenal Shunt Procedure -Distal Splenorenal Shunt Patency
43.15 The Ileana Pull-through Operative Prpcedure of Ulcerative Colitis: Eliminating the Permanent Ileostomy (Eric W. Fonkalseud, M.D.) (VCD)
ــــ
44.15 The Massachusetts General Hospital Handbook of Pain Management (Second Edition)
ــــ
- General Considerations - Acute Pain
- Diagnosis of Pain - Chronic Pain
- Therapeutic Options: Pharmacologic Approaches - Pain Due to Cancer
(Jane Ballantyne, Scott M. Fishman, Salahadin Abdi) (SALEKAN-E-book)
- Therapeutic Options: Nonpharmacologic Approaches - Special Situations - Apendices - Subject Index
45.15 TISSUE ADHESIVES In Wound Care (James V. Quinn, M.D., FACEP)
ــــ 2004
46.15 Tissue Glues in Cosmetic Surgery (RENATO SALTZ, M.D., DEAN M. TORIUMI, M.D.) 47.15 Tolaryngology Surgery for Fronatal Sinus Disease 48.15
Video Journal General Surgery
(Professor & Chairman, Bobby R. Alford, M.D.) (VCD)
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ــــ
(VCD)
1. Reflux Disease and Nissen Fundoplication (Philip E. Donahue, MD) 2. Supraceliac Aortic-Celiac Axis-Superior Mesenteric Artery Bypass
ــــ
(Gregorio, Leonardo, Brent, Charles)
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
63 ــــ
)(VCD
Video Journal General Surgery
)Open Repair of Abdominal Wall Hernias Using Prosthetic materials (Arthur I. Gilbert, M.D. )Small Bowel Obstrution Immediately Following Lapatoscopic Herniorraphy (Karl A. Zucker, MD )Laparoscopic Loop Ileostomy For Temporary Fecal Diversion (Steven D. Wxner, MD, Petachia Reissman, MD )Consultants Corner: Managed Care Update, Pt, III (Michael A. Wood
49.15
1. 2. 3. 4.
-١٦ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ
ﻋﻨﻮﺍﻥ CD
ﺳﺎﻝ ﺍﻧﺘﺸﺎﺭ
Burkect's Oral Medicine Diagnosis and Treatment
ــــ ــــ ــــ
ﭼﮕﻮﻧﮕﻲ ﺗﺸﺨﻴﺺ ﻭ Mangeﻛﺮﺩﻥ ﺑﻴﻤﺎﺭﺍﻥ -ﺍﺧﺘﻼﻻﺕ ﺗﻤﭙﻮﺭﻭﻣﻨﺪﻣﺒﻮﻻﺭ ﻭ Manageﺁﻧﻬﺎ -ﻣﻼﺣﻈﺎﺕ ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ ﺩﺭ ﺑﻴﻤﺎﺭﺍﺕ ﺩﺍﺭﺍﻱ ﺑﻴﻤﺎﺭﻱ ﺳﻴﺴﺘﻤﻴﻚth Caratera's Clinical PERIODONTOLOGY 9 Edition Textbookﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ ﻭ ﭘﺮﻳﻮﺩﻭﻧﺘﻮﻟﻮﮊﻱ -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﻟﺜﻪ ﻧﺮﻣﺎ -ﻃﺒﻘﻪﺑﻨﺪﻱ ﺑﻴﻤﺎﺭﻱ ﻟﺜﻪ ﻭ PPLﻭ – ...ﻧﺤﻮﻩ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻟﺜﻪ ﻭ PDL)COLOR ATLAS OF Dental Medicine Aesthetic Dentistry (Josef Schnidsedes
3.16
Color Atlas of Endodontics
4.16
ﻋﻨﺎﻭﻳﻦ ﻣﻬﻢ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: ﺍﻃﻠﺲ ﺭﻧﮕﻲ ﺩﺭﻣﺎﻥﻫﺎﻱ ﺩﻧﺪﺍﻧﻲ -ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ ﺯﻳﺒﺎﻳﻲ -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﻣﺘﺎﻝ ﻛﺮﺍﻭﻧﻬﺎ ﻭ ﺭﻭﺵﻫﺎﻱ ﻛﺮﺍﻭﻥﻛﺮﺩﻥ -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﺳﺮﺍﻣﻴﻚ ﻛﺮﺍﻭﻥﻫﺎ -ﺩﺭﻣﺎﻥﻫﺎﻱ ﻗﺒﻞ ﺍﺯ ﺗﺮﻣﻴﻢ -ﻛﺎﻣﭙﺎﺯﻳﺖ ﺍﻓﻴﻠﻪ )ﻣﺰﺍﻳﺎ ﻭ ﻣﻌﺎﻳﺐ( – (PFM) -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﻭﻧﻴﺮﻭ ﺭﻭﺵﻫﺎ ﻭ ﺍﺻﻮﻝ ﻭﻧﻴﺮﻛﺮﺍﻭﻥ
ــــ
1.16
-ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺺ -ﺭﻭﺵﻫﺎﻱ - Acsessﺗﺸﺨﻴﺺ ﻭ ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﻃﻮﻝ ﻛﺎﻧﺎﻝ ﺭﻳﺸﻪ
ــــ -ﺍﺭﺗﻮﺩﻭﻧﺴﻲ ﻧﻮﻳﻦ Textbook -ﺍﺭﺗﻮﺩﻭﻧﺴﻲ ﺩﺭ ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ -ﻣﺸﻜﻼﺕ ﺍﺭﺗﻮﺩﻭﻧﺴﻲ
)(William T. Johnson DDS.MS ﺁﻣﺎﺩﻩﻛﺮﺩﻥ ﻛﺎﻧﺎﻝ ﻭ – ...ﺩﺭﻣﺎﻥ ﻣﺠﺪﺩ )(RetreatmentContemporary Orthodontics PROFFIT -ﻧﺤﻮﻩ ﺗﻜﺎﻣﻞ ﺍﻳﺮﺍﺩﺍﺕ ﺍﺭﺗﻮﺩﻭﻧﺴﻲ -ﺗﺸﺨﻴﺺ ﻭ ﻃﺮﺡ ﺩﺭﻣﺎﻥ
2.16
5.16
ﻣﻜﺎﻧﻴﺴﻢﻫﺎ ﻭ ﺑﻴﻮﻣﻜﺎﻧﻴﺴﻢﻫﺎ -ﺍﺧﺘﻼﻻﺕ TMJﻭ ..Craniofacial Development
6.16
Critical Decisious in Periodoutology
7.16
ــــ
Dental Assisting ﺁﻣﻮﺯﺵ ﺑﻪ ﺻﻮﺭﺕ ﺗﺼﻮﻳﺮﻱ -ﻛﻠﻴﻪ ﺭﻭﺵﻫﺎﻱ ﻛﻨﺘﺮﻝ ﻋﻔﻮﻧﺖ ﺩﺭ ﻣﻄﺐ -ﺭﻭﺵﻫﺎﻱ ﻓﻠﻮﺭﺍﻳﺪﺗﺮﺍﭘﻲ -ﺭﻭﺵﻫﺎﻱ ﻣﻌﺎﻳﻨﻪ ﻭ Positionﺑﻴﻤﺎﺭ ﻭ ﺩﻧﺪﺍﻧﭙﺰﺷﻚ -ﺭﻭﺵ ﺻﺤﻴﺢ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ) Instromentﻗﻠﻢﻫﺎ( -ﺭﻭﺵ ﻧﺼﺐ ﺭﺍﺑﺮﺩﻡ ﻭ ﺍﺳﺘﻔﺎﺩﻩ ﺻﺤﻴﺢ ﺍﺯ ﺁﻥ ﺭﻭﺵﻫﺎﻱ ﺻﺤﻴﺢ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻲ ﮔﺮﻓﺘﻦ ﻭ ﻧﺤﻮﻩ ﻇﻬﻮﺭ ﺁﻧﻬﺎ ﻭ ﻛﻨﺘﺮﻝ ﻋﻔﻮﻧﺖ ﺗﺎﺭﻳﻜﺨﺎﻧﻪ -ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ Dessingﻭ ﻧﺤﻮﻩ ﺑﺮﺩﺍﺷﺘﻦ ﺁﻥDental Implant System -ﺍﻳﻨﺘﺮﻭﻣﻨﺖ -ﺁﻧﺎﻟﻴﺰ ﻭ ﺑﺮﺭﺳﻲ ﺭﻭﺵ ﻛﺎﺭ -ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ -ﺗﺮﻣﻴﻢ ﻭ ﺁﻣﻮﺯﺵ ﺑﻴﻤﺎﺭ
8.16
ــــ
)Dental Implant System Fixed Implant Restorations (ITI Dental Implant System) (VCD
10.16
ــــ
Endodontics
11.16
ــــ
)Endodontics 5 Edition (John I. Ingle, DDS, MSD, Leif K. Bakland, DDS
12.16
ــــ
)ESSENTIAL OF ORAL MEDICINE (Silverman, Roy Eversole, Truelove ﺑﺮﺭﺳﻲ ﺩﺭ ﺩﻫﺎﻥ ﺳﺮ ﻭ ﺻﻮﺭﺕ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺁﻣﻮﺯﺷﻲ ﻫﻤﺮﺍﻩ ﺑﺎ Caseﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻭ ﭘﺮﺳﺶ ﻭ ﭘﺎﺳﺦ ﻧﻜﺎﺕ ﺿﺮﻭﺭﻱ ﻓﺎﺭﻣﺎﻛﻮﻣﻮﺭﻋﻲ .aﺑﺮﺭﺳﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺳﻴﺴﺘﻤﻴﻚ ﻭ ﺗﻈﺎﻫﺮﺍﺕ ﺩﻫﺎﻧﻲ ﺁﻧﻬﺎ )ESTHETIC DENTISTRY 2th Edition (Dennet W. Aschheim, Barry G. Dale ﺍﺻﻮﻝ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ-١ :ﺗﺮﻣﻴﻢﻫﺎﻱ ﻛﺎﻣﭙﺎﺯﻳﺖ -٢ﺳﺮﺍﻣﻴﻚ -ﻣﺘﺎﻝ -٣ﭼﻴﻨﻲ ﻓﻮﻝﻛﺮﺍﻭﻥ -٤ﻭﻳﻨﻴﺮ ) -٥ (PFMﺭﺯﻳﻨﺖﻫﺎﻱ ﭼﺴﺒﻨﺪﻩ -٦ﺑﻠﻴﭽﻴﻨﮓ )ﺳﻔﻴﺪﻛﺮﺩﻥ ﺩﻧﺪﺍﻥﻫﺎ( -٧ﺍﻳﻤﭙﻠﻨﺖ ﻭ ﺟﺮﺍﺣﻲ ﺩﻫﺎﻥ ﻭ ﺻﻮﺭﺕ
13.16
ــــ ﺳﻴﻨﻮﺱﻫﺎﻱ ﭘﺎﺭﺍﻧﺎﺯﺍﻝ -ﻣﻨﺪﻳﺒﻮﻝ ﻭ ...ــــ -ﺑﺮﺭﺳﻲﻫﺎﻱ ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ -ﺳﺎﺑﻘﻪ ﺑﻴﻤﺎﺭ -ﻧﺤﻮﻩ ﺷﻨﺎﺳﺎﻳﻲ ﺿﺎﻳﻌﺎﺕ
ــــ
ــــ
-ﻃﺮﺡ ﺩﺭﻣﺎﻥﻫﺎﻱ ﻣﻮﺭﺩ ﻧﻴﺎﺯ
)(Walte R.B.HALL -ﺩﺭﻣﺎﻥﻫﺎﻱ ﺟﺮﺍﺣﻲ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﺩﺭ ﭘﺮﻳﻮﺩﻭﻧﺘﻴﻜﺲ ﻭ ﺯﻳﺒﺎﻳﻲ
ﺍﻳﻨﺘﺪﻭﻣﻨﺖﻫﺎﻱ ﺟﺪﻳﺪ – Shaping - Cleaningﻭ ﺁﺩﺍﭘﺘﻪﻛﺮﺩﻥ ﺭﻭﺕﻛﺎﻧﺎﻝ ﻭ ...th
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
9.16
14.16
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
64 ــــ ــــ
-١ﺟﺎﻳﮕﺰﻳﻨﻲ ﺗﻚﺩﻧﺪﺍﻧﻲ ﺑﺎ ﺍﻳﻤﭙﻠﻨﺖ ITI
)Esthetic Implant Dentistry (Daniel Buser, Hans Peter Hirt) (VCD
15.16
)ESTHETIC IMPLANT DENTISTRY (Daniel A. Bases, Urs.E.Belses
16.16
-٢ﺍﻳﻤﭙﻠﻨﺖ ﺩﻧﺪﺍﻧﻲ ﺗﻴﺘﺎﻧﻴﻮﻡ ﺑﺎ ﭘﻮﺷﺶ TPS
ﺩﺭ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻣﻞ ﻭ ﻧﺤﻮﺓ ﺟﺎﻳﮕﺬﺍﺭﻱ ﺍﻳﻤﭙﻠﻨﺖ – ﻣﺰﺍﻳﺎ ﻭ ﻣﻌﺎﻳﺐ ﺍﻧﻮﺍﻉ ﺍﻳﻤﭙﻠﻨﺖﻫﺎ -ﺑﺮﺭﺳﻲ ﺑﺎﻓﺖ ﻧﺮﻡ ﻗﺒﻞ ﺍﺯ ﺍﻧﺠﺎﻡ ﺍﻳﻤﭙﻠﻨﺖ ﻭ ﺑﺮﺭﺳﻲ ﺩﺭﺻﺪ ﻣﻮﻓﻘﻴﺖ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. )Esthetic in Dentistry (Vol 1- Vol 2
17.16
)ESTHETICS IN DENTISTRY (Second Edition
18.16
Glossary of Orthodontic Terms
19.16
)Guide to Physical Examination (Mosby
20.16
Implant Medpor Mandibular A method to Restore Skeletal Support to the Lower Face
21.16
ITI Dental Implant
22.16
)ITI TE Solution ITI TE Implant (DENTAL IMPLANT SYSTEM) (Daniel Buser) (Disk 1-3
23.16
Journal of Esthetic & Restorative Dentistry -٦ﺑﺮﺭﺳﻲ ﺭﻭﺵﻫﺎ -٧ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎ -٨ﺑﻠﻴﭽﻴﻨﮓ
24.16
)LINGUAL ORTHODONTICS (Rafi Romano) (TO EXPLORE THE CD-ROM
25.16
)Local Anesthesia in Dentistry (VCD -ﺑﺮﺭﺳﻲ ﺭﻭﺵﻫﺎﻱ ﺻﺤﻴﺢ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﺎﻭﻳﺮﻱ ﮔﻮﻳﺎ ﺑﻪ ﺻﻮﺭﺕ ﻋﻤﻠﻲ -ﺧﻄﺮﺍﺕ ﻣﻮﺟﻮﺩ ﻭ ﺍﻳﺮﺍﺩﺍﺕ
26.16
)Local Anesthesia in Dentistry (Dr. Markus D. W. Lipp Wolfgang Kelm) (VCD
27.16
My Orthodontics
28.16
Oral Disease Diagnosis & Treatment
29.16
Oral Pathology 4th edition
30.16
Orthodontics & Paediatric Dentistry
31.16
Orthodontics Priociples & Techniques 3th Edition
32.16
)Pathways of the PMP (8th Edition
33.16
)PERIODONTAL MEDICINE (L.F. Rose, R.J.Genco, B.L. Mealey, D.W. Cohen
34.16
Periodontal Surgery
35.16
ــــ -ﻣﺎﻝ ﺍﻛﻠﻮﮊﻱ
ﻣﺸﻜﻼﺕ ﺯﻳﺒﺎﻳﻲ ﺗﻚﺩﻧﺪﺍﻧﻲ -ﺍﺯ ﺩﺳﺖﺩﺍﺩﻥ ﺩﻧﺪﺍﻥ1998
PRINCIPLES COMMUNICATIONS TREATMENT METHODS
)(John Daskalogiannakis
ــــ ــــ
ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺑﺮﺭﺳﻲ ﺑﻬﺪﺍﺷﺖ ﺩﻫﺎﻧﻲ ﻭ ﺑﺮﺭﺳﻲ ﭼﻨﺪﻳﻦ Caseﻫﻤﺮﺍﻩ ﺑﺎ ﻋﻜﺲﻫﺎ ﻭ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻲﻫﺎﻱ ﺩﻫﺎﻧﻲ ﺭﺍ ﺗﻮﺿﻴﺢ ﻣﻲﺩﻫﺪ. )(Oscar M. Ramirez M.D., F.A.C.S.) (POREX) (VCD
ــــ
)(CD I , II , III
ــــ -ﻛﻠﻴﻪ ﻣﺮﺍﺣﻞ ﺁﻣﺎﺩﻩﺳﺎﺯﻱ
-ﻭﺳﺎﻳﻞ ﻣﻮﺭﺩ ﻧﻴﺎﺯ
-ﻧﺤﻮﻩ ﺟﺮﺍﺣﻲ ﻟﺜﻪ ﻭ ﻓﻚ ﻭ ﺁﻣﺎﺩﻩﺳﺎﺯﻱ ﻣﺤﻞ
2004 ــــ -١ﺑﺮﺭﺳﻲ ﻛﺎﻣﻞ ﺍﻧﻮﺍﻉ ﺍﻧﻮﺍﻉ ﺗﺮﻳﺲﻫﺎ -٢ﮊﻭﺭﻧﺎﻝ ﺩﻧﺪﺍﻧﭙﺰﺷﻜﻲ ﺗﺮﻣﻴﻤﻲ ﻭ ﺯﻳﺒﺎﻳﻲ -٩ﻋﻜﺲﻫﺎﻱ ﻛﺎﻣﻞ ﺍﺯ ﻣﺮﺍﺣﻞ ﺗﺮﻣﻴﻢ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ
-٣ﺳﺮﺍﻣﻴﻚ ﺍﻳﻨﻠﻪ ﻭ ﺍﻧﻠﻪ -٤ﻛﺎﻣﭙﺎﺯﻳﺖ ﺭﺯﻳﻦ -٥ﻛﺎﻣﭙﺎﺯﻳﺖ ﺭﺯﻳﻦ Packable Crown -١١ﺗﻤﺎﻡ ﺳﺮﺍﻣﻴﻚ Post -١٠
1998 ــــ ﺭﻭﺵﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺗﺰﺭﻳﻖ ﺑﺎ ﺍﻫﺪﺍﻑ ﻣﺘﻔﺎﻭﺕ ﺑﺮﺍﻱ ﺑﻲﺣﺴﻲ ﻧﻮﺍﺣﻲ ﻣﺨﺘﻠﻒ ﺩﻧﺪﺍﻥﻫﺎ ﻭ ﻟﺜﻪ ﻭ ﺑﺎﻓﺖ ﻧﺮﻡــــ ــــ -ﺑﺮﺭﺳﻲ ﻣﺮﺍﺣﻞ ﻣﻌﺎﻳﻨﻪ -ﻗﺒﻞ ﺍﺯ ﺩﺭﻣﺎﻥ ،ﻃﻲ ﺩﺭﻣﺎﻥ ،ﺑﻌﺪ ﺍﺯ ﺩﺭﻣﺎﻥ
-ﻧﺘﺎﻳﺞ ﺣﺎﺻﻠﻪ ﺍﺯ ﺩﺭﻣﺎﻥ ،ﻣﺮﺍﻗﺒﺖﻫﺎﻱ ﺣﻴﻦ ﺩﺭﻣﺎﻥ -ﺩﺍﺭﺍﻱ ﻟﻴﻨﻚﻫﺎﻱ ﻣﺘﻌﺪﺩ ﻭ ﺁﺩﺭﺱﻫﺎﻱ ﺟﺎﻟﺐ ﺳﺎﻳﺖﻫﺎﻱ ﺍﺭﺗﻮﺩﻭﻧﺴﻲ
ــــ ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﺿﺎﻳﻌﺎﺕ ﺩﻫﺎﻥ -ﺿﺎﻳﻌﺎﺕ ﺳﻔﻴﺪ ﺁﺑﻲ ﻗﺮﻣﺰــــ ــــ
-ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻭﺯﻳﻜﻮﻟﻮﺑﻮﻟﻮﺯ
ﺑﺮﺭﺳﻲ ﺑﻴﺶ ﺍﺯ Case ٥٠ﻣﺘﻔﺎﻭﺕ -ﺑﺮﺭﺳﻲ ﺑﻪ ﺻﻮﺭﺕ ﺁﺯﻣﻮﻥ ﻫﻤﺮﺍﻩ ﺑﺎ ﺟﻮﺍﺏ ﺻﺤﻴﺢ -ﻣﺎﻝ ﺍﻛﻠﻮﮊﻥ Mixed dentition-
-ﺷﺮﺍﻳﻂ ﺯﺧﻢﻫﺎ
-ﺍﺧﺘﻼﻻﺕ ﺭﻧﮕﺪﺍﻧﻪﺍﻱ
-ﺿﺎﻳﻌﺎﺕ ﺑﺎﻓﺖ ﻫﻤﺒﻨﺪ
-ﻣﻄﺎﻟﻌﺔ ﺟﺰﺋﻴﺎﺕ ﻭ ﻣﻼﺣﻈﺎﺕ ﻭ ﻣﺸﺨﺼﺎﺕ ﺑﻴﻤﺎﺭ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﺼﻮﻳﺮ
-ﻣﺎﻝ ﺍﻛﻠﻮﮊﻥ ﻭ ﺍﺧﺘﻼﻻﺕ TMJ
ــــ -ﺗﺸﺨﻴﺺ ﻭ ﻃﺮﺡ ﺩﺭﻣﺎﻥ ﺩﺭ ﺍﺭﺗﻮﺩﻭﻧﺴﻲ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺩﺭﻣﺎﻥ
-ﻭﺍﻛﻨﺶﻫﺎﻱ ﺑﺎﻓﺖﻫﺎ
-ﻛﻴﺴﺖﻫﺎ ﻭ ﺗﻮﻣﻮﺭﻫﺎ
-ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺍﺳﺘﺨﻮﺍﻥ -ﺍﺧﺘﻼﻻﺕ TMJﻭ ﺑﻴﻮﻣﻜﺎﻧﻴﺴﻢﻫﺎ
ــــ Part III: Related Clinical Topics
2000
Part II: The Science of Endodoutics
ــــ ﺟﺮﺍﺣﻲ ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ -ﺣﺬﻑ ﭘﺎﻛﺖ ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ -ﺑﺮﺭﺳﻲ ﺗﺤﻠﻴﻞ ﻟﺜﻪ ﺩﺭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺮﻳﻮﺩﻭﻧﺘﺎﻝ ﻛﻮﺭﺗﺎﮊ -ﺑﺮﺭﺳﻲ ﺍﻧﻮﺍﻉ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺮﻳﻮﺩﻭﻧﺸﻴﻢ -ﺩﺭﻣﺎﻥﻫﺎ ﻭ ﺁﻣﻮﺯﺵ ﺑﻬﺪﺍﺷﺖ ﭘﺲ ﺍﺯ ﺩﺭﻣﺎﻥﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
Part I: The Art of Endodoutics
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
65 ــــ
36.16
Periodontal Surgery Clinical Atlas
37.16
Removal Orthodontics Apliances
38.16
Saunders Dental Assisting (Multimedia Resource) (Second Edition) (Doni L. Bird , Debbie S. Robinson)
39.16
Strauman Dental Implant System (VCD)
40.16
The Center of Education, Teaching and Research for Oral Implant Reconstruction (Prof. Dr. Hns L. Grafelmann) (CD I , II) - Vertical Load -Pitt-Easy BIO OSS -Phase TPS Cylinder Implant
ــــ
41.16
The Entegra Dental Implant System Entegra Surgical Videos (Robert Schroering)
ــــ
42.16
The IMZ Implant System (VCD) (Dr. Karl-Ludwing Ackermann, Dr. Axel Kirsch)
ــــ
43.16
Toothcolored Restoratives
44.16
TOOTH-COLORED RESTORATIVES Ninth Edition (Principles and Techniques)
45.16
Treatment Planning in Dentistry
46.16
Treatment Planning in Dentistry (Stephen Stefanac, D.D.S., M.S.Sam Nesbit, D.D.S., M.S.)
ــــ
47.16
UCD Implant
ــــ
. ﻫﻤﺮﺍﻩ ﺑﺎ ﻣﺮﺍﺣﻞ ﻻﺑﺮﺍﺗﻮﺍﺭﻱ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻣﻞ ﻭ ﺗﺼﻮﻳﺮﻫﺎﻱ ﻛﺎﻣﻞ ﺍﺯ ﺗﻤﺎﻡ ﻣﺮﺍﺣﻞIII ﻭII ﻭI ﻣﺨﺘﻠﻒ ﺍﻋﻢ ﺍﺯ ﻛﻼﺱCase ﺑﺮﺭﺳﻲ ﺩﻫﻬﺎ
ــــ 2003 ــــ
ﺍﻳﻤﭙﻠﻨﺖ ﭼﻨﺪ ﺩﻧﺪﺍﻧﻲ ﻣﺎﮔﺰﻳﻠﺪ- ﭘﻴﻦﮔﺬﺍﺭﻱ ﺩﺭ ﺍﺳﺘﺨﻮﺍﻥ ﺍﻟﻮﺋﻞ- ﻧﺤﻮﻩ ﺁﻣﺎﺩﻩﺳﺎﺯﻱ ﻧﺴﺞ ﻧﺮﻡ ﻭ ﺳﺨﺖ ﺑﺮﺍﻱ ﺍﺳﺘﻘﺮﺍﺭ ﺍﻳﻤﭙﻠﻨﺖ-
(CD I , II)
ــــ
ﻭ ﺩﻧﺪﺍﻥ ﻧﻴﺎﺯﻣﻨﺪ ﺑﻪ ﺗﺮﻣﻴﻢCase ﻧﺤﻮﻩ ﺗﺸﺨﻴﺺ ﻭ ﺍﻧﺘﺨﺎﺏ-
ﺍﺻﻮﻝ ﻭ ﺗﻜﻨﻴﻚﻫﺎ-
ﺑﺮﺭﺳﻲ ﻣﻮﺍﺩ ﻣﺨﺘﻠﻒ ﺩﺭ ﺗﺮﻣﻴﻢ ﻫﻤﺮﻧﮓ ﻣﺰﺍﻳﺎ ﻭ ﻣﻌﺎﻳﺐ2002
(Harry F. Albers, DDS) ﺩﺍﺭﺍﻱ ﺁﺯﻣﻮﻥﻫﺎﻱ ﺟﺎﻟﺐ ﻭ ﻛﺎﻣﻞ-
ﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻫﻤﺮﺍﻩ ﺑﺎ ﭘﺮﻭﻧﺪﻩﻫﺎﻱ ﻛﺎﻣﻞCase ﺑﺮﺭﺳﻲ-
ــــ
... ﻧﺤﻮﻩ ﺟﺎﻳﮕﺬﺍﺭﻱ ﭘﻴﻦﻫﺎ ﻭ- ﺁﻣﺎﺩﻩﺳﺎﺯﻱ ﻧﺴﺞ ﻧﺮﻡ ﻭ ﻧﺤﻮﻩ ﺍﻳﺠﺎﺩ ﻓﻠﭗ ﻭ ﻧﺤﻮﻩ ﺁﻣﺎﺩﻩﺳﺎﺯﻱ ﻧﺴﺞ ﺍﺳﺘﺨﻮﺍﻥ- ﺭﻭﺵﻫﺎﻱ ﺑﻲﺣﺴﻲ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ:١٧
1.17 ANATOMY & PHYSIOLOGY (5 Edition) th
(Gary A. Thibodeau, Kevin T. Patton) 2.17 BODY WORKS 6.0 A 3D Journey Through The Human Anatomy 3.17 Interactive Guide to Human Neuroanatomy (Mark F. Bear, Barry W. Connors, Michael A. Paradiso) Atlas: -Surface Anatomy of Brain Exam:I -Surface Anatomy of the Brain
4.17
6.17
-The Spinal Cord -The Anatomy Nervous System -Comprehensive Exam
-The Cranial Nerves -The Blood Supply to the Brain
Interactive Physilogy MUSCULAR SYSTEM (A. D. A. M. Benjamin/Cummings) (Marvin J. Branstrom, Ph.D.) -Anatomy Review: Skeletal Muscle Tissue
5.17
-Cross-Sectional Anatomy of Brain -Cross-Sectional Anatomy of the Brain
ــــ ــــ 2002
-The Neuromuscular Junction
-Sliding Filament Theory
-Muscle Metabolism
-Contraction of Motor Units
ــــ -Contraction of Whole Musle
InterActive PHYSIOLOGY Cardiovascular System
ــــ
The Heart
Blood Vessels
Anatomy Review: The Heart Intrinsic Conduction System Cardiac Action Potential Cardiac Cycle Cardiac Output
Anatomy Review: Blood Vessel Structure and Function Measuring Blood Pressure Factors that Affect Blood Pressure
Interactive PHYSIOLOGY for Windows Urinary System
Blood Pressure Regulation Autoregulation and Capillary Dynamics
ــــ
Version 1.0
ﺏ( ﻋﺮﻭﻕ ﺧﻮﻧﻲ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ﺍﻟﻒ( ﻗﻠﺐ.ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺍﺭﺍﻱ ﺩﻭ ﻣﺒﺤﺚ ﻣﺠﺰﺍ ﻣﻲﺑﺎﺷﺪ ﻭ ﺍﻫﺪﺍﻑ ﺁﻣﻮﺯﺷﻲ ﺩﺭ ﺍﺑﺘﺪﺍﻱ ﻫﺮ ﻓﺼﻞ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
66 ﺧـﻮﺩﺗﻨﻈﻴﻤﻲ ﻭ ﺩﻳﻨﺎﻣﻴـﻚ، ﺗﻨﻈـﻴﻢ ﻓﺸـﺎﺭ ﺧـﻮﻥ، ﻓﺎﻛﺘﻮﺭﻫﺎﻱ ﻣـﺆﺛﺮ ﺑـﺮﺭﻭﻱ ﻓﺸـﺎﺭ ﺧـﻮﻥ، ﺍﻧﺪﺍﺯﻩﮔﻴﺮﻱ ﻓﺸﺎﺭ ﺧﻮﻥ، ﺳﺎﺧﺘﺎﺭ ﻭ ﻋﻤﻠﻜﺮﺩ ﻋﺮﻭﻕ ﺧﻮﻧﻲ: ﺏ( ﻋﺮﻭﻕ ﺧﻮﻧﻲ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ. ﭼﺮﺧﺔ ﻗﻠﺒﻲ ﻭ ﺑﺮﻭﻥﺩﻩ ﻗﻠﺒﻲ، ﭘﺘﺎﻧﺴﻴﻞ ﻋﻤﻞ ﻗﻠﺒﻲ، ﺳﻴﺴﺘﻢ ﻫﺪﺍﻳﺘﻲ ﻗﻠﺐ، ﺁﻧﺎﺗﻮﻣﻲ ﻗﻠﺐ:ﺍﻟﻒ( ﻗﻠﺐ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ . ﺩﺍﺭﺍﻱ ﻳﻚ ﻓﻬﺮﺳﺘﻲ ﺍﺯ ﺍﺻﻄﻼﺣﺎﺕ ﺍﺳﺖ ﻭ ﻫﺮ ﻭﺍﮊﻩ ﺭﺍ ﻣﺨﺘﺼﺮﹰﺍ ﺗﻮﺿﻴﺢ ﻣﻲﺩﻫﺪCD ﺍﻳﻦ. ﺩﺭ ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺭﺋﻮﺱ ﻣﻄﺎﻟﺐ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﮔﻮﻳﻨﺪﻩ ﺁﻧﻬﺎ ﺭﺍ ﺑﻴﺎﻥ ﻣﻲﻛﻨﺪ.ﻣﻮﻳﺮﮒﻫﺎ . ﺳﺆﺍﻻﺕ ﭼﻨﺪ ﮔﺰﻳﻨﻪﺍﻱ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﻭ ﭘﺎﺳﺦﻫﺎﻱ ﻧﺎﺻﺤﻴﺢ ﺑﺎ ﺭﻧﮓ ﻗﺮﻣﺰ ﻣﺸﺨﺺ ﻣﻲﺷﻮﻧﺪ،( ﺩﺭ ﻫﺮ ﻳﻚ ﺍﺯ ﻣﺒﺎﺣﺚ ﻓﻮﻕQuiz) ﺩﺭ ﺑﺨﺶ ﺍﻣﺘﺤﺎﻥ 7.17
Interactive Physiology RESPIRATORY SYSTEM (A. D. A. M. Benjamin/Cummings)
-Anatomy Reviw: Respiratory Structures 8.17 MedWorks Anatomy & Physilogy Anatomy Y Physiology: Overview The Endocrine System The Sensory Organs
-Pulmonary Ventilation
(Andrea K. Salmi)
-Gas Exchange
ــــ
-Gas Transport
-Control of Respiration ــــ
Cells and Tissues
The Integumentary System
Body Chemistry
The Skeletal System
The Muscula System
Cardiovascular System: The Blood Somatic and Autonomic Systems
Cardiovascular System, The Heart The Peripheral Nervous Systems
Lymphatic and Immune System
The Respiratory System The Digestive System
Inheritance
The central Nervous System
The Nervous System Organization The Urinary System
The Reproductive System
. ﺍﻧﺘﺨﺎﺏ ﻭ ﺍﺟﺮﺍ ﻛﻨﻴﺪMedwork ﺭﺍ ﺍﺯ ﻣﺴﻴﺮ ﺩﺍﻳﺮﻛﺘﻮﺭﻱSetup.exe ﻓﺎﻳﻞ،ﺑﺮﺍﻱ ﺍﺟﺮﺍ Panorama of Anatomy & Physiology Structure & Function of the Body (Eleven Edition) (Gary A. Thibodeau, Kevin T. Patton) (Time) 10.17 Range of Motion-AO Neutral-0 Method Measurement and Documentation
ــــ ــــ
9.17
2002
11.17 Sobotta (Atlas of Human Anatomy) (Urban & Schwarzenbery) 1. General Anatomy
2. Head and neck
3. Upper Limb
4. Brain and Spine Cord
Past ( ﺍﺟـﺮﺍ ﺷـﺪﻩSetup )ﻫﻤﺎﻥ ﻣﺴﻴﺮﻱ ﻛـﻪC:\Urban ﺭﺍ ﻛﭙﻲ ﻛﺮﺩﻩ ﻭ ﺩﺭSobotta 1.5Crack
5. Eye
6. Ear
7. Thoracic and Abdominal Wall
8. Thoracic Oegans
9. Lower Limb
ﻭ ﺳﭙﺲCrack ﻭﺍﺭﺩ ﺩﺍﻳﺮﻛﺘﻮﺭﻱ، ﭘﺲ ﺍﺯ ﺍﺗﻤﺎﻡ. ﺁﺑﻲﺭﻧﮓ ﺭﺍ ﺍﺟﺮﺍ ﻣﻲﻛﻨﻴﻢSetup ، English ﺟﻬﺖ ﻧﺼﺐ ﺍﻳﻦ ﻧﺮﻡﺍﻓﺰﺍﺭ ﺍﺑﺘﺪﺍ ﺍﺯ ﺩﺍﻳﺮﻛﺘﻮﺭﻱ:( ﻃﺮﻳﻘﺔ ﻧﺼﺐ . ﺣﺎﻝ ﻧﺮﻡﺍﻓﺰﺍﺭ ﻓﻮﻕ ﻗﺎﺑﻞ ﺧﻮﺍﻧﺪﻥ ﻭ ﺍﺟﺮﺍﺳﺖ.ﻣﻲﻛﻨﻴﻢ 2003 ــــــ
12.17 Student Companion CD-ROM for Principles of Anatomy & Physiology (Tenth Edition) (John Willey & Sons, INC.) 13.17 The Interactive Skeleton Tutorial 1. Head
2. Spine
3. Ribs
(Dr. peter Abrahams of cambridger University, UK.) 4. Upper Limb
5. Lower Limb
14.17 World of SPORT examined
ــــ ﭘﺮﺳﺘﺎﺭﻱ:١٨
1.18 2.18 3.18 4.18 5.18 6.18
The Oncology Nursing Society presents THE ADVANCED PRACTICE ONCOLOGY NURSING REVIEW Textbook of MEDICAL SURGUCAL NURSING (Ninth Edition) (Katherine H. Dimmock) Student Self Study Disk to Accompany BRUNNER & SUDDARTH'S Focus on Nursing Pharmacology (Lippincott Williams & Wilkins) Wongs ESSENTIALS OF Pediatric Nursing (Mosby) A Harcoun Health Sciences Company Maternal, Neonatal and Women's Health Nursing By Delmar, a division of Thomson Learning Nursing Care of Infants and Children (Seven Edition)
ــــ ــــ 2000 2001 2002 2003
: ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪCD ﺍﻳﻦ - Childre, Their Families, and the Nurse
- Family-Centered Care of the Newborn
- Family-Centered Care of the Infant
- Family-Centered Care of the Young Child - Family-Centered Care of the School-Age Child
- Family-Centered Care of the Adolescent
- Family-Centered Care of the Child with Special Needs
- The Child who is Hospitalized
- The Child with Problems Related to Transfer of Oxygen and Nutrients
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
- Assessment of the Child and Family - The Child with Disturbance of Fluid and Electrolytes
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
67 - The Child with Problems Related to Production & Circulation of Blood
- The Child with Disturbance of Regulatory Mechanisms
- The Child With a Problem that Interfers with Physical Mobility
McMinn's Interactive Clinical Anatomy 8.18 INRERACTIVE ATLAS OF CLINICAL ANATOMY (Illustrations by Frank H. Netter, M.D.) 7.18
ــــ ــــ
ﻓﻴﺰﻳﻮﺗﺮﺍﭘﻲ-١٩ 1.19 2.19 3.19
Clinical Tests for the Musculoskeletal System (Klaus Buckup, KlinikumDortmund Orthopaedic Hospital Dortmund Germany) (Salekan E-Book) DIET & FITNESS DIGITAL SHIATSU
2004 ــــ ــــ
: ﻗﺴﻤﺖ ﻣﻲ ﺑﺎﺷﺪ ﻛﻪ ﺑﻪ ﺷﺮﺡ ﺯﻳﺮ ﺍﺳﺖ٦ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺩﺍﺭﺍﻱ ﺭﺍﻫﻨﻤﺎ-
ﺍﺳﺎﺱ ﻭ ﻣﺒﺎﻧﻲ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ-
ﺟﺴﺘﺠﻮ-
(therapies) ﻣﻮﺍﺭﺩ ﻛﺎﺭﺑﺮﺩ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ-
(total body) ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﺗﻤﺎﻣﻲ ﺑﺪﻥ-
(self- shiatsu) ﺧﻮﺩ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ-
. ﺩﺭ ﺗﺼﺎﻭﻳﺮ ﻃﺮﺡﻭﺍﺭﻫﺎﻱ ﻧﻘﺎﻁ ﺣﺴﺎﺱ ﻛﻪ ﺩﺭ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﻣﻮﺭﺩ ﺗﻮﺟﻪ ﻗﺮﺍﺭ ﻣﻲﮔﻴﺮﺩ ﻧﻤﺎﻳﺶ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﺭﻭﺵ ﻣﺎﺳﺎﮊ ﺻﺤﻴﺢ ﻭ ﻋﻤﻠﻲ ﺗﻤﺎﻣﻲ ﺑﺪﻥ ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﻓﻴﻠﻢ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﮔﻮﻳﻨﺪﻩ ﻭ ﻣﺘﻦ ﭼﺎﭘﻲ ﺍﺭﺍﺋﻪ ﻣﻲ ﺷﻮﺩ-١ . ﻫﻤﺮﺍﻩ ﺑﺎ ﻧﻤﺎﻳﺶ ﻓﻴﻠﻢ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﮔﻮﻳﻨﺪﻩ ﺩﺭ ﺩﻭ ﻗﺴﻤﺖ ﺭﻭﺵ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ-٢ (... ﮔﺮﻓﺘﮕﻲ ﻭ ﻛﺮﺍﻣﭗ ﭘﺎ ﻭ، ﻗﺎﻋﺪﮔﻲ، ﺍﺳﻬﺎﻝ، ﻳﺎﺋﺴﮕﻲ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﻠﻴﻮﻱ، ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻛﺒﺪﻱ، ﺧﻮﻥ ﺩﻣﺎﻍ، ﺳﻴﻨﻮﺯﻳﺖ، ﺩﺭﺩ ﻗﻔﺴﻪ ﺳﻴﻨﻪ ﻓﻠﺞ ﺻﻮﺭﺕ، ﺁﺭﺗﺮﻳﻮﺍﺳﻜﻠﺮﻭﺯ: ) ﺷﺎﻣﻞ. ﻣﻮﺭﺩ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ٢٢ ﻣﻮﺍﺭﺩ ﻛﺎﺭﺑﺮﺩ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﺩﺭ-٣ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖNamikoshi ﺍﺻﻮﻝ ﻣﺎﺳﺎﮊ ﺩﺭﻣﺎﻧﻲ ﻭ ﺭﻭﺷﻬﺎﻱ ﻛﻼﺳﻴﻚ ﺁﻥ ﻭ ﻧﻴﺰ ﺗﺎﺭﻳﺨﭽﻪ ﻣﺘﺪ-٤ . ﺑﺮ ﺍﺳﺎﺱ ﺣﺮﻭﻑ ﺍﻟﻔﺒﺎﻳﻲ ﻣﻲ ﺗﻮﺍﻥ ﻭﺍﮊﻩﻫﺎﻱ ﺗﺨﺼﺼﻲ ﻣﻮﺭﺩ ﻧﻈﺮ ﺧﻮﺩ ﺭﺍ ﭘﻴﺪﺍ ﻧﻤﻮﺩ ﻭ ﺑﺎ ﻛﻠﻴﻚ ﻧﻤﻮﺩﻥ ﺑﺮ ﺭﻭﻱ ﺁﻥ ﺑﻪ ﺁﻥ ﻣﺒﺎﺣﺚ ﻣﻨﺘﻘﻞ ﺷﺪ-٥ . ﺍﺟﺮﺍ ﻣﻲ ﺷﻮﺩAutorun ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﻪ ﺻﻮﺭﺕ . ﻧﺼﺐ ﻣﻲ ﺷﻮﺩprogram ﺩﺭ ﮔﺰﻳﻨﻪLifestyle softuare Group ﺩﺭ ﻧﻬﺎﻳﺖ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﺑﻪ ﻧﺎﻡ، ﺩﻭ ﺑﺎﺭ ﻛﻠﻴﻚ ﻧﻤﺎﺋﻴﺪ ﻭ ﻣﺮﺍﺣﻞ ﻧﺼﺐ ﺭﺍ ﭘﻴﮕﻴﺮﻱ ﻛﻨﻴﺪSetup.exe ﺟﻬﺖ ﻧﺼﺐ ﺍﻳﻦ ﺑﺮﻧﺎﻣﻪ ﻻﺯﻡ ﺍﺳﺖ ﺑﺮ ﺭﻭﻱ ﺁﻳﻜﻮﻥ:( ﻃﺮﻳﻘﺔ ﻧﺼﺐ
. ﻛﻠﻴﻚ ﻧﻤﺎﺋﻴﺪinstall.exe ﺑﺮﺍﻱ ﻧﺼﺐ ﺁﻳﻜﻮﻥ. ﻛﺎﻣﭙﻴﻮﺗﺮ ﺷﻤﺎ ﺑﻪ ﻛﺎﺭ ﻣﻲ ﺭﻭﺩDesktop ﻧﻴﺰ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﺑﺮﺍﻱ ﺳﻔﺎﺭﺷﻲ ﻧﻤﻮﺩﻥ ﺻﻔﺤﻪJurassic Park Entertainment ﻳﻚ ﺑﺮﻧﺎﻣﻪ ﺟﺎﻧﺒﻲ ﺑﻪ ﻧﺎﻡCD ﺩﺭ ﺍﻳﻦ 4.19
EXERCISE THERAPY PREVENTION AND TREATMENT OF DISEASE ( John Gormley and Juliette Hussey)
5.19
Fibromyalgia Syndrome Bodywork Management Strategies ٥ ﺳﭙﺲ ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺩﺭﻣﺎﻥ ﻓﻴﺒﺮﻭﻣﻴﺎﻟﮋﻳﺎ ﺑﺮ ﺍﺳﺎﺱ ﭘﺮﻭﺳﻪ ﺩﺭﻣﺎﻧﻲ ﭘﻴﺸﻨﻬﺎﺩ ﺷﺪﻩ ﺁﻣﻮﺯﺵ ﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ ﺑﺪﻳﻦﺻﻮﺭﺕ ﻛﻪ ﺩﺭ ﻣﺮﺍﺣﻞ ﻣﺨﺘﻠﻒ ﺍﺭﺯﻳﺎﺑﻲ ﻛﻪ ﺷـﺎﻣﻞ. ﻛﻪ ﺩﺭ ﺯﻣﻴﻨﺔ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺩﺳﺘﻲ ﺍﺳﺖ ﻣﻌﺮﻓﻲ ﺷﺪﻩ ﺍﺳﺖLeon Chitow ﺍﺑﺘﺪﺍ ﺗﻌﺪﺍﺩﻱ ﺍﺯ ﻛﺘﺐCD ﺩﺭ ﺍﻳﻦ .ﺑﺨﺶ ﻣﻲﺑﺎﺷﺪ ﺑﺎ ﺗﺄﻛﻴﺪ ﺑﺮ ﻣﻬﺎﺭﺕﻫﺎﻱ ﻟﻤﺲ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ Assessment Methodes
6.19
Fundamentale of Sensation ad Perception (3rd Edition) (M.W. Levine)
(
- Manual Thermal Diagnosis
- Skin on Fascia Adherence
- Hyperalgesic Skin Zones reduced Skin elasticity
- Drag palpation for increased hydrosis
2005 ___
- Neuro muscular Technique Evaluation (NMT)
ــــ : ﻋﻨﻮﺍﻥ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ١٦ ﺷﺎﻣﻞCD ﻣﺤﺘﻮﺍﻱ ﺍﻳﻦ
Introduction and instructions Afterimages Depth from motion of random dots Traveling waves on the basilar membrane Gnglion Cells responding to light
Threshold experiment or Signal Detection Brain anatomy, Blink Suppression, or Cortical Cell responses Optical IIIusions and Constancies
Motion demonstrations
Retinal Cells responding to light Demonstratuins of Fourier components Color mixing or Opponent cells
Pitch and Loudness of tones
Speech sounds of Mystery phrase
Muscle spindle feedback
Motions from form of Impossible figures
Mechanics of the middle and inner ear
Taste-influenced by vision
7.19 Health & Fitness (DataSel Software, Inc) 1. Getting Started
2. The Exercise Demonstration Screen
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
3. Strength
4. Stretch
Specializations of the Vertebrate eye Cortical columns or Equiluminant demos
5. Equipment
6. Muscles
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
7. Workouts
8. Setup
9. Technical Support
ــــ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
68 8.19 Interactive Atlas of Human Anatomy
ــــ 2005 ــــــ
9.19 Introduction to Massage Therapy (Mary Beth Braum, Steplianic Simonsoon) (Salekan E-Book) 10.19 MANIPULATION OF THE SPINE, THORAX AND PELVIS An Osteopatic Perspective (Peter Gibbons, Philip Tehan)
ﺍﻳﻦ ﻓﻴﻠﻢﻫﺎ ﺩﺭ ﺩﻭ ﺑﺨﺶ ﻛﻠﻲ ﺑﻪ ﺷﺮﺡ ﺫﻳـﻞ. ﻓﻘﺴﺔ ﺳﻴﻨﻪ ﻭ ﻟﮕﻦ ﺧﺎﺻﺮﻩ ﻣﻲﺑﺎﺷﺪ، ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﺳﺘﺨﻮﺍﻧﻲ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕmanipulation ﻗﻄﻌﻪ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺷﻲ ﻛﻮﺗﺎﻩ ﺩﺭ ﺧﺼﻮﺹ ﺗﻜﻨﻴﻚﻫﺎ ﻭ ﻧﺤﻮﺓ ﻣﻌﺎﻳﻨﺔ ﻓﻴﺰﻳﻜﻲ ﻭ٣٤ ﺑﺼﻮﺭﺕ ﻧﻤﺎﻳﺶCD ﺍﻳﻦ :ﺍﺭﺍﺋﻪ ﺷﺪﻩ ﺍﺳﺖ ﺑﺨﺶ ﺍﻭﻝ: HVLA thrust techniques-spine and thorax
- Cervical and cervicothoracie spine
-Thoracic spine and rib cage
-Lumbar and thora Columbar spine
ﺑﺨﺶ ﺩﻭﻡ: HVLA thrust techniques-pelvis . ﺍﺟﺮﺍ ﻣﻲﺷﻮﺩAutorun ﺑﻪ ﺻﻮﺭﺕCD ﺍﻳﻦ. ﺭﺍ ﺑﺮ ﺭﻭﻱ ﺑﻴﻤﺎﺭ ﻧﻤﺎﻳﺶ ﻣﻲﺩﻫﺪmanipulafion ﭘﺰﺷﻚ ﻣﺘﺨﺼﺺ ﻧﺤﻮﺓ ﺍﻧﺠﺎﻡ ﻣﻌﺎﻳﻨﻪ ﻭ،ﺩﺭ ﻫﺮ ﻗﻄﻌﻪ ﻓﻴﻠﻢ 11.19 Massage Therapy Review
(interactive Edition) (Mosby)
ـــــ
12.19 Men's Health GET RID OF THAT GUT
STAGE 1: BEGINNERS LEVEL
STAGE 2: INTERMEDIATE LEVEL
13.19 MUSCLE ENERGY TECHNIQUES
STAGE 3: ADVANCED LEVEL 2001
ADVANCED SOFT TISSUE TECHNIQUES (Second Edition)
. ﺗﺼﻮﻳﺮ ﻭﻳﺪﺋﻮﺋﻲ ﻭﺟﻮﺩ ﺩﺍﺭﺩ٣٠ ﻓﺼﻞ ﺑﻪ ﻫﻤﺮﺍﻩ٨ ﻟﺌﻮﻥ ﭼﻴﺘﻮ ﻣﺸﺘﻤﻞ ﺑﺮMuscle Energy Techniques ﻣﺘﻦ ﻛﺎﻣﻞ ﻛﺘﺎﺏCD ﺩﺭ ﺍﻳﻦ ﺩﺭ ﺍﻳﻦ ﺗﻜﻨﻴﻚ ﺑﻴﻤﺎﺭ ﻧﻘﺶ ﻓﻌﺎﻟﻲ ﺩﺭ ﺍﺻﻼﺡ ﺍﺧﺘﻼﻻﺕ ﻋﻤﻠﻜﺮﺩﻱ ﺑﺮ ﻋﻬـﺪﻩ ﺩﺍﺭﺩ ﻭ. ﻳﻜﻲ ﺍﺯ ﺭﻭﺵﻫﺎﻱ ﺩﺭﻣﺎﻥ ﺩﺳﺘﻲ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺁﻥ ﺍﺯ ﺍﻧﻘﺒﺎﺽ ﺍﺭﺍﺩﻱ ﻋﻀﻠﻪ ﺩﺭ ﻳﻚ ﺟﻬﺖ ﻛﻨﺘﺮﻝ ﺷﺪﻩ ﻭ ﺩﻗﻴﻖ ﺑﺎ ﺷﺪﺕﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻭ ﺩﺭ ﺑﺮﺍﺑﺮ ﻧﻴﺮﻭﻱ ﺩﺭﻣﺎﻧﮕﺮ ﺍﺳﺘﻔﺎﺩﻩ ﻣﻲﺷﻮﺩMET : ﺍﻳﻦ ﺗﻜﻨﻴﻚ ﻛﺎﺭﺑﺮﺩ ﺑﺎﻟﻴﻨﻲ ﺯﻳﺎﺩﻱ ﺩﺍﺭﺩ ﻛﻪ ﻣﻲﺗﻮﺍﻥ ﺑﻪ ﻣﻮﺍﺭﺩ ﺯﻳﺮ ﺍﺷﺎﺭﻩ ﻛﺮﺩ. ﺑﺎﻋﺚ ﻛﺎﻫﺶ ﺗﻮﻥ ﻳﺎ ﻣﻬﺎﺭ ﻋﻀﻼﺕ ﻛﻮﺗﺎﻩﺷﺪﻩ ﻭ ﺗﻘﻮﻳﺖ ﻋﻀﻼﺕ ﺿﻌﻴﻒ ﻣﻲﺷﻮﺩReciprocal inhibtion ﻳﺎPost isometric Relaxation ﺗﺮﺍﭘﻴﺴﺖ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﮔﻴﺮﺍﻓﺘﺎﺩﮔﻲ ﻣﻨﻴﺴﻚ ﻭ ﻋﺪﻡ ﺗﻄﺎﺑﻖ ﻛﺎﻣﻞ ﺳﻄﻮﺡ، ﺍﺻﻼﺡ ﻣﻮﺍﻧﻊ ﻣﻜﺎﻧﻴﻜﻲ ﺩﺍﺧﻞ ﻣﻔﺼﻞ ﻣﺜﻞ ﺁﺭﺗﺮﻳﺖ، ﻛﺎﻫﺶ ﺍﺩﻡ ﻣﻮﺿﻌﻲ، ﺍﺯ ﺑﻴﻦﺑﺮﺩﻥ ﭼﺴﺒﻨﺪﮔﻲ ﻣﺘﻌﺎﻗﺐ ﺍﺣﺘﻘﺎﻥ ﻭﺭﻳﺪﻱ، ﺭﻓﻊ ﺍﺣﺘﻘﺎﻥﻫﺎﻱ ﻭﺭﻳﺪﻱ، ﺗﻘﻮﻳﺖ ﻋﻀﻼﺕ ﺿﻌﻴﻒ،ﻛﺸﺶ ﻋﻀﻼﺕ ﻛﻮﺗﺎﻩ ﻭ ﺍﺳﭙﺎﺳﺘﻴﻚ ﻣﻔﺼﻠﻲ ﻭ ﻫﻤﭽﻨﻴﻦ ﻣﺘﺤﺮﻙﻧﻤﻮﺩﻥ ﻣﻔﺎﺻﻞ ﻣﺤﺪﻭﺩ 14.19 Myofascial Release Techniques
(John F. Barnes, PT) (VCD I , II) 15.19 Orthopaedics for Nurses (John Ebnezar) (Salekan E-Book) 16.19 Orthopedic Massage Theory and Technique (Whitney Lowe Leon Chaitow) 17.19 Palpation Skills for Muscles and Joints
ــــــ ــــ 2003 ــــــ
18.19 Physical Education and the Study of Sport (Bob Davis, Ros Bull, Jan Roscoe, Dennis Roscoe) (Mosby)
ــــــ
1- Physical Education and the Study of Sport
2- Synoptic Questions Harcourt Health Sciences
rd 19.19 Physical Rehabilitatioon of the Injured Athlete 3 Edition
20.19 Positional Release Techniques
3- The Project Personal Performance Profile
(James R. Andrews, Gary I., Harrison, Kevin) (Salekan E-Book)
ADVANCED SOFT TISSUE TECHNIQUES (Leon Chaitow) (Harcourt) (Second Edition)
2004 ــــــ
. ﺗﺼﻮﻳﺮ ﻭﻳﺪﺋﻮﺋﻲ ﺍﺯ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﻋﻤﺎﻝﺷﺪﻩ ﻭﺟﻮﺩ ﺩﺍﺭﺩ٣١ ﻓﺼﻞ ﻫﻤﺮﺍﻩ ﺑﺎ١٢ ﻟﺌﻮﻥ ﭼﻴﺘﻮ ﻣﺸﺘﻤﻞ ﺑﺮPositional Release ﻣﺘﻦ ﻛﺎﻣﻞ ﻛﺘﺎﺏCD ﺩﺭ ﺍﻳﻦ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻜﻲ ﺍﺯ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺆﺛﺮ ﺩﺭ ﺩﺭﻣﺎﻥ ﺑﺎﻓﺖ ﻫﻤﺒﻨﺪ ﻣﻨﺎﻃﻘﻲ ﻛﻪ ﺩﺭ ﻟﻤﺲ ﻫﺎﻳﭙﺮﺗﻮﻥ ﻳﺎ ﻛﻮﺗﺎﻩ ﺷﺪﻩﺍﻧﺪ ﺑﻜﺒﺎﺭ ﻣﻲﺭﻭﺩ ﻭ ﭼﻮﻥ ﺍﺳﺎﺱ ﺁﻥ ﻗﺮﺍﺭﺩﺍﺩﻥ ﺑﺎﻓﺖ ﻫﻤﺒﻨﺪ ﻳﺎ ﻋﻀﻠﻪ ﺩﺭ ﺭﺍﺣﺖﺗﺮﻥ ﻭﺿﻌﻴﺖ ﻣﻲﺑﺎﺷﺪ ﺑﻪﻛﺎﺭﺑﺮﺩﻥ ﺁﻥ ﺩﺭ ﻣﻮﺍﺭﺩﻳﻜﻪ ﺑﻪ ﻋﻠـﺖ ﺍﺳﭙﺎﺳـﻢ ﻳـﺎ ﺍﻟﺘﻬـﺎﺏPositional Release . ﻟﺬﺍ ﺩﺭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﺍﻥ ﻣﺒﺘﻼ ﺑﻪ ﻣﺸﻜﻼﺕ ﻣﺎﺳﻜﻠﻮﺍﺳﻜﻠﺘﺎﻝ ﺑﺴﻴﺎﺭ ﻣﺆﺛﺮ ﺍﺳﺖ.ﺑﺎﻓﺖ ﻫﻤﺒﻨﺪ ﺑﺴﻴﺎﺭ ﺩﺭﺩﻧﺎﻙ ﺍﺳﺖ ﺑﺮﺍﻱ ﺑﻴﻤﺎﺭ ﻗﺎﺑﻞ ﺗﺤﻤﻞ ﻣﻲﺑﺎﺷﺪ Spontaneous Positional relese variations
The evolution of dysfunction
Unloading and Proprioceptive taping
Modified strain/counterstrain technique
Learning SCS
SCS for muscle pain (plus INTT and self-treatment)
Goodheart and Morrison's Positional release variations and lift techniques
SCS (and SCS variations) in hospital settings
The Mulligan concept: NAGs, SNAGs, MWMs, etc.
Functional technique
Facilitated Positional release (FPR)
Cranial and TMJ Positional release methods
21.19 Power Touch
ــــــ
22.19 Principles of Manual Therapy (A Manual Therapy Approach to Musculoskeletal Dyslimction) (Salekan E-Book)
2005
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
69 23.19 Surface and Living Anatomy
2002
(Gordon Joslin SOtJ)
. ﺩﺭ ﻛﻨﺎﺭ ﻫﺮ ﻳﻚ ﺍﺯ ﻣﺘﻦﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﻋﻜﺲﻫﺎﻱ ﺭﻧﮕﻲ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻛﻪ ﺑﻪ ﻭﺳﻴﻠﺔ ﻣﺎﺭﻛﺮﻫﺎﻳﻲ ﻣﻨﺎﻃﻖ ﻣﺮﺑﻮﻃﻪ ﺭﺍ ﻧﺸﺎﻥ ﻣﻲﺩﻫﻨﺪ. ﻣﻨﻄﻘﻪ ﺁﻧﺎﺗﻮﻣﻴﻜﻲ ﺭﺍ ﻣﺮﺣﻠﻪ ﺑﻪ ﻣﺮﺣﻠﻪ ﺗﻮﺿﻴﺢ ﻣﻲﺩﻫﺪ٢٢٦ ﻣﺘﻦ ﻛﺎﻣﻞ ﺁﻧﺎﺗﻮﻣﻲ ﺳﻄﺤﻲ ﻗﺴﻤﺖﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺑﺪﻥ ﻭﺟﻮﺩ ﺩﺍﺭﺩ ﻭ ﭘﻴﺪﺍﻛﺮﺩﻥCD ﺩﺭ ﺍﻳﻦ 24.19 The Complete Acupuncture
ــــ
25.19 The Principles of Harmonic Techniques
(Eyal Lederman)
(VCD)
ــــــ
ﺑﺮ ﺍﻳﻦ ﺍﺳﺎﺱ ﻛﻪ ﻫﺮ ﺳﻴﺴﺘﻤﻲ ﻳﻚ ﻓﺮﻛﺎﻧﺲ ﻧﻮﺳﺎﻥ ﻃﺒﻴﻌﻲ ﺩﺍﺭﺩ ﭼﻨﺎﻧﭽﻪ ﺍﻳﻦ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺩﺭ ﻣﺤﺪﻭﺩﺓ ﻓﺮﻛﺎﻧﺲ ﺑﺎﻓﺖﻫﺎ. ﻣﻌﺮﻓﻲ ﺷﺪEyal Lederman ﻫﺎﺭﻣﻮﻧﻴﻚ ﺗﻜﻨﻴﻚ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺗﻜﻨﻴﻚ ﺩﺭﻣﺎﻧﻲ ﻣﺆﺛﺮ ﺩﺭ ﺯﻣﻴﻨﻪ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺎﻧﻮﺍﻝ )ﺩﺳﺘﻲ( ﺑﻪ ﻭﺳﻴﻠﺔ : ﺑﺨﺶ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ٤ ﺍﺻﻮﻝ ﻭ ﺭﻭﺵ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﺗﻜﻨﻴﻚ ﺩﺭ ﻣﻔﺎﺻﻞ ﻣﺨﺘﻠﻒ ﺩﺭCD ﺩﺭ ﺍﻳﻦ.ﻭ ﺗﻮﺩﻩﻫﺎﻱ ﺑﺪﻥ ﺍﻋﻤﺎﻝ ﺷﻮﻧﺪ ﺑﺎﻋﺚ ﺍﻳﺠﺎﺩ ﺭﺯﻭﻧﺎﻧﺲ ﺷﺪﻩ ﺑﺎ ﺻﺮﻑ ﺍﻧﺮﮊﻱ ﻛﻤﺘﺮ ﺗﻮﺳﻂ ﺩﺭﻣﺎﻧﮕﺮ ﺩﺍﻣﻨﻪ ﺣﺮﻛﺘﻲ ﻣﻨﺎﺳﺐ ﺩﺭ ﺑﻴﻤﺎﺭ ﺍﻳﺠﺎﺩ ﻣﻲﺷﻮﺩ 1- The Principles of Harmonic Technique 2- The Principles of Harmonic Technique Using Thoracic Mass Oscillations
3- The Principles of Harmonic Technique Using Pelvic Mass Oscillations 4- The Principles of harmonic Technique Using Appendicular Oscillations
26.19 YOGA for YOU (Anatomy)
ــــ ﺍﻭﺭﮊﺍﻧﺲ ﻭ ﺑﻴﻬﻮﺷﻲ:٢٠
1.20 2.20
American College of Surgons ACS Surgery Principles & Pracitce (CD I , II) (E-Book) Advanced Pediatric Life Support: The Critical First Hour CPR and ACLS Review (David G. Nichols, MD)
2004 : ﺭﻳﻮﻱ ﭘﻴﺸﺮﻓﺘﻪ ﺩﺭ ﻛﻮﺩﻛﺎﻥ ﻭ ﺑﺎﻟﻐﻴﻦ ﺷﺮﺡ ﻣﻲﺩﻫﺪ- ﺩﺭ ﻣﻮﺭﺩ ﺍﺣﻴﺎﺀ ﻗﻠﺒﻲCD ﺍﻳﻦ
ــــــ
1: Initial Evaluation, 2: Airway Management, 3: Epiglottitis and Gidup, 4: Respiratory Failure, 5: Advanced Pediatric CPR, 6: Resuscitative Drugs 3.20
ANESTHESIA (Ronald D. Miller, MD) (Fifth Edition)
Anesthesiology (The Journal of the American Society of Anesthesiologists, Inc) Abstracts of Scientific Papers 5.20 Anesthesiology (The Journal of the American Society of Anesthesiologists, Inc) Abstracts of Scientific Papers 4.20 6.20 7.20
Clinical Procedures in EMERGENCY MEDICINE (4th Edition) (James R. Roberts, MD, Jerris R. Hedges, MD, MS) (E-Book) (CD I, II) Emergency Medical Training (MedEMT) Victory Technology, Inc. Presents (DISC ONE, TWO) MedEMT Overview
Emergency Medical Services (EMS)
The Well-Being of the EMT-Basic
Anatomy and Physiology-Part 1
Medical Terminology
Vital Signs and SAMPLE History
Lifting and Moving Patients
Airway Management
Patient Assessment
Medical and Behaval Care I
Medical and Behavioral Care II
Obstetric and Gynecological Care
Trauma
Infants and Children
Operations
Appendix A: Video/Animation List
Appendix B: Victory Products
1. Anatomical Fundamentals 2. Peripheral Neve Stimulation 3. Regional Anaesthesia 4. Upper, Lower Extremity 5. Peripheral Neve Blocks 11.20 The American Academy of Pediatric (David G. Nichols, MD Associate Professor of Anesthesiology and Clinical Care Medicine)
-Ventilating the Infant
-Chest Compressions
12.20 The Lipponcott-Raven Interactive Anesthesia Library on CD-ROM 13.20 The Massachusetts General Hospital Handbook of Pain Management
، ﺳﺮﻭﻛﺎﺭ ﺩﺍﺭﻧـﺪ، ﺑﻪ ﻋﻠﺖ ﺩﺳﺘﻴﺎﺑﻲ ﺭﺍﺣﺖ ﭘﺰﺷﻜﺎﻧﻲ ﻛﻪ ﺑﺎ ﺑﻴﻤﺎﺭﺍﻥ ﺩﺭﺩﻣﻨﺪPoacet
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
ــــــ
Anatomy and Physology-Part 2
8.20 EMERGENCY MEDICINE A COMPREHENSIVE STUDY GUIDE (Rosen's ) (Volume 1-3) (Sixth Edition) (Judith E. Tintinall, MD, MS) 9.20 EMT-Basic Slide Set Slide Program Guide (John A. Stouffer, EMT-P, Richard S. Bennett, RN, EMT-P, BSN) (Mosby) 10.20 Peripheral Regional Anaesthesia Tutorial in the Ulm Rehabilitation hospital (Prof. Dr. Med. H. Mehrkens) (VCD) (CD I , II)
-Intitial Steps in Resuscitation
2000 2002 2000 2004
2004 1999 ـــــ
6. Peripheral Neve Blocks
-Endotracheal Intubaion
(Version 2.0) (Paul G. Barash, MD) (Salekan E-Book)
ــــــ ـــــ ـــــ
guide ﺍﺯEdition ﺍﻳﻦ. ﺩﺭ ﺍﺧﺘﻴﺎﺭ ﻛﺎﺭﺑﺮ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ، ﺍﺟﺮﺍ ﻣﻲﮔﺮﺩﻧﺪMass.Gen
ﺩﻳﺪﮔﺎﻩ ﻛﺎﻣﻞ ﻭ ﻣﻔﻴﺪﻱ ﺍﺯ ﺍﻃﻼﻋﺎﺗﻲ ﻛﻪ ﺩﺭ ﺩﺭﻣﺎﻥ ﻣﺆﺛﺮ ﺩﺭﺩ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﻣﻲﺑﺎﺷﻨﺪ ﻭ ﺩﺭ ﺑﻴﻤﺎﺭﺍﻥCD ﺍﻳﻦ . ﻣﺰﻣﻦ ﻭ ﺩﺭﺩ ﻛﺎﻧﺴﺮ ﺭﺍ ﭘﻮﺷﺶ ﻣﻲﺩﻫﺪ، ﻣﻮﺍﻟﻴﺘﻪﺍﻱ ﺩﺭﻣﺎﻧﻲ ﻣﺨﺘﻠﻒ ﺭﺍ ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﻣﻲﺩﻫﺪ ﻭ ﺟﻨﺒﻪﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺩﺭﺩ ﺍﻋﻢ ﺍﺯ ﺣﺎﺩCD ﺍﻳﻦ، ﺑﺎ ﻣﺮﻭﺭ ﻣﺒﺎﺣﺚ ﻋﻤﺪﺓ ﺩﺭﺩ.ﻣﺸﻬﻮﺭ ﻣﻲﺑﺎﺷﺪ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
. ﺍﻃﻼﻋﺎﺕ ﺩﺍﺭﻭﻳﻲ ﻛﺎﻣﻞ ﻣﻲﺑﺎﺷﺪ48.9
70 ﺩﺭﺩ ﺻﻮﺭﺕ-
ﻣﺪﺍﺧﻼﺕ ﺭﺍﺩﻳﻮﺗﺮﺍﭘﻲ ﻭ ﺭﺍﺩﻳﻮﻓﺎﺭﻣﺎﺳﻲ ﺑﺮﺍﻱ ﺩﺭﺩﻫﺎﻱ ﻛﺎﻧﺴﺮ-
ﻣﺪﺍﺧﻼﺕ ﺟﺮﺍﺣﻲ ﻭ ﺟﺮﺍﺣﻲ ﺍﻋﺼﺎﺏ-
:ﺷﺎﻣﻞ 2002
New Analgesic Options: Overcoming Obstacles to Pain Relief - MD, NP, PA, RN Answer Sheet
-Pharmacist Answer Sheet
-Back Pain
-Fibromyalgia
-OA Pain
-Post Op Pain
-Trauma
-References
2005
11.20 Textbook of CRITICAL CARE (Salekan E-book) SECTION I RESUSCITATION AND MEDICAL EMERGENCIES SECTION II TRAUMA SECTION III IMAGING SECTION IV CELL INJURY AND CELL DEATH SECTION V INFECTIONS DISEASE SECTION VI ENDOCTINOLOGY, METABOLISM, NUTRITION, PHARMACOLOGY SECTION VII CARDIOVASCULAR SECTION VIII PULMONARY 12.20 Miller's Anesthesia (Vol I & II) (Salekan E-book)
2005
SECTION I: INTRODUCTION SECTION II: SCIENTIFIC PRINCIPLES SECTION III: ANESTHESIA VOLUME 2 SECTION IV: SUB SPECIAL TV SECTION V: CRITICAL CARE MEDICINE SECTION VI: ANCILLARY RESPONSIBILITIES AND PROBLEMS COMPANION VIDEO CD-ROM Video 1 Patient Positioning in Anesthesia Video 2 Code Blue Simulation
2004
13.20 NEW YORK SCHOOL OF REGIONAL ANESTHESIA PERIPHERAL NERVE BLOCKS PRINCIPLES AND PRACTICE -TRAINING IN PERIPHERAL NERVE BLOCKS - ESSENTIAL REGIONAL ANESTHESIA ANATOMY -EQUIPMENT AND PATIENT MONITORING IN REGIONAL ANESTHESIA -PERIPHERAL NERVE STIMULATORS AND NERVE STIMULATION -CLINICAL PHARMACOLOGY OF LOCAL ANESTHETICS -NEUROLOGIC COMPLICATIONS OF PERIPHERAL NERVE BLOCKS -KEYS TO SUCCESS WITH PERIPHERAL NERVE BLOCKS -CERVICAL PLEXUS BLOCK -INTERSCALENE BRACHIAL PLEXUS BLOCK -INFRACLAVICULAR BRACHIAL PLEXUS BLOCK -AXILLARY BRACHIAL PLEXUS BLOCK -INTRAVENOUS REGIONAL BLOCK OF THE UPPER EXTREMITY -CUTANEOUS NERVE BLOCKS OF THE UPPER EXTREMITY -THORACIC PARAVERTEBRAL BLOCK -THORACOLUMBAR PARAVERTEBRAL BLOCK -LUMBAR PLEXUS BLOCK - SCIATIC BLOCK: POSTERIOR APPROACH 234 -SCIATIC BLOCK: ANTERIOR APPROACH 252 -FEMORAL NERVE BLOCK -POPLITEAL BLOCK: INTERTENDINOUS APPROACH -POPLITEAL BLOCK: LATERAL APPROACH -ANKLE BLOCK - WRIST BLOCK -CUTANEOUS NERVE BLOCKS OF THE LOWER EXTERMITY -DIGITAL BLOCK
14.20 Interactive Regional Anesthesia
ــــــ
؛ ﺍﻭﺭﻭﻟﻮﮊﻱ٢١ 1.21
Adult and Pediatric Urology
2.21
Adult Urology Adult Urology Continued Pediatric Urology Video Library Advanced Therapy of Prostate Disease (Martin I. Resnick, MD, Ian M. Thompson, MD)
(Jay Y. Gillenwater, john T. Grayhack, Stuart S. Howards, Michael E. Mitchell)
2002 2000
. ﺭﻓﺮﺍﻧﺲﻫﺎ ﺩﺭ ﻣﻮﺭﺩ ﭼﮕﻮﻧﮕﻲ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺮﻭﺳﺘﺎﺕ ﻣﻲﺑﺎﺷﺪ. ﺑﻮﺩﻩ ﻭ ﻳﻜﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﺭﻓﺮﺍﻧﺲﻫﺎ ﺩﺭ ﻣﻮﺭﺩ ﭼﮕﻮﻧﮕﻲ ﺗﺸﺨﻴﺺ ﻭ ﺩﺭﻣﺎﻥ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺮﻭﺳﺘﺎﺕ ﻣﻲﺑﺎﺷﺪAcrobat reader ﺻﻔﺤﻪﺍﻱ ﺩﺭ ﻣﺤﻴﻂ٦٤٨ ﺍﻳﻦ ﻛﺘﺎﺏ . ﻓﺼﻞ ﻣﻲﺑﺎﺷﺪ٧١ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ ، ﻏﺮﺑــﺎﻟﮕﺮﻱ ﻛﺎﻧﺴــﺮ ﭘﺮﻭﺳــﺘﺎﺕ-٩ ﻭ١١ ﻭ١٢ ﻓﺼـﻮﻝ. ﻓﺎﻛﺘﻮﺭﻫــﺎﻱ ﻣﻠﻜـﻮﻟﻲ ﺩﺭ ﺍﺭﺯﻳــﺎﺑﻲ ﻛﺎﻧﺴــﺮ ﭘﺮﻭﺳـﺘﺎﺕ-٨ ﻓﺼــﻞ. ﺍﻟﮕــﻮﺭﻳﺘﻢ ﺍﺭﺯﻳـﺎﺑﻲ ﺧﻄــﺮ ﭘﺮﻭﺳــﺘﺎﺕ ﻛﺎﻧﺴـﺮ ﺷــﺮﺡ ﺩﺍﺩﻩ ﺷــﺪﻩ ﺍﺳـﺖ-٧ ﻓﺼــﻞ. ﺍﭘﻴــﺪﻣﻴﻮﻟﻮﮊﻱ ﻛﺎﻧﺴــﺮ ﭘﺮﻭﺳـﺘﺎﺕ ﺷــﺮﺡ ﺩﺍﺩﻩ ﺷــﺪﻩ ﺍﺳـﺖ٦-١ ﻓﺼـﻮﻝ . ﺭﺍﺩﻳﻜﺎﻝ ﭘﺮﻭﺳﺘﺎﺗﻜﺘﻮﻣﻲ:ﺁﻣﺎﺩﮔﻲ ﺑﻴﻤﺎﺭ ﺑﺮﺍﻱ-١٩ ﻓﺼﻞ، ﻛﺎﻧﺴﺮ ﭘﺮﻭﺳﺘﺎﺕstaging ﺗﺸﺨﻴﺺ ﻭ-١٧-١٨ ﻓﺼﻞ. ﺗﺎﺭﻳﺨﭽﺔ ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﭘﺮﻭﺳﺘﺎﺕ ﻭ ﺗﺎﺭﻳﺨﭽﺔ ﭘﺎﺗﻮﺑﻴﻮﻟﻮﮊﻱ ﻛﺎﻧﺴﺮ ﭘﺮﻭﺳﺘﺎﺕ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖ-١٣-١٦ ﻓﺼﻮﻝ. ﺍﺑﺰﺍﺭﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ-١٠ ﻓﺼﻞ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
71 ٢٠ﻭ ٢١ﻭ Stage -٢٢ﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺩﺭ ﺭﻭﺵﻫﺎﻱ ﺟﺮﺍﺣﻲ ﺁﻧﻬﺎ -٢٩-٢٤ .Radical Perianal Prostatectomy -٢٣ .ﺭﺍﺩﻳﻮﺗﺮﺍﭘﻲ Brachy therapy ،ﻭ ﻫﻮﺭﻣﻮﻧﺎﻝﺗﺮﺍﭘـﻲ ﻭ ﻛﺮﺍﻳﺮﺗﺮﺍﭘـﻲ ﻛﺎﻧﺴـﺮﻫﺎﻱ ﻣﺨﺘﻠـﻒ ﭘﺮﻭﺳـﺘﺎﺕ -٣٩-٣٠ﺩﺭ ﻫـﺮ ﻓﺼـﻞ (TNM) Staging
ﺟﺪﺍﮔﺎﻧﻪ ﺷﺮﺡ ﻭ ﺭﻭﺵ ﺩﺭﻣﺎﻥ ﺁﻥ ﻧﻴﺰ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ -٤٠-٤٣ﭼﮕﻮﻧﮕﻲ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﺍﻥ ﺑﻌﺪ ﺍﺯ ﻋﻤﻞ ﭘﺮﻭﺳﺘﺎﺗﻜﺘﻮﻣﻲ ﺑﺎ PSAﻭ ﻫﻮﺭﻣﻮﻥﺗﺮﺍﭘﻲ ﻭ -٤٤ ...ﺍﺳﻔﻨﻜﺘﺮ genitourinaryﺁﺭﺗﻴﻔﻴﺸﺘﺎﻝ -٤٥ﻛﻼﮊﻥﺗﺮﺍﭘﻲ ﺑﺮﺍﻱ ﺑﻲﺍﺧﺘﻴﺎﺭﻱ ﺑﻌﺪ ﺍﺯ ﻋﻤـﻞ ﺟﺮﺍﺣـﻲ ﭘﺮﻭﺳـﺘﺎﺕ -٤٧ -٤٦ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﺑﺮﺍﻱ ﻋﻮﺍﺭﺽ erctionﻭ ﺍﻧﻮﺭﻛﺘﺎﻝ -٥٠-٤٨ﺟﻠﻮﮔﻴﺮﻱ ﺍﺯ ﻋﻮﺩ ﻛﺎﻧﺴﺮ ﺑﺎ ﺷﻴﻤﻲﺩﺭﻣﺎﻧﻲ ﻭ ﺭﺍﺩﻳﻮﺗﺮﺍﭘﻲ -٥١ﻧﮕﺮﺵ ﺳﻠﻮﻟﻲ ﻭ ﻫﻮﺭﻣﻮﻧﻲ ﺑﻪ -٥٢-٥٣ . BPHﻧﺴﺒﺖ ﺍﻭﺭﻭﺩﻳﻨﺎﻣﻴﻚ ﻭ ﺍﺑﻨﺮﻣﺎﻟﻲﻫﺎﻱ ﺩﻳﮕـﺮ -٥٤ .ﭘـﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺍﻧﺴـﺪﺍﺩ ﻣﺠـﺮﺍﻱ ﺧﺮﻭﺟـﻲ ﻣﺜﺎﻧـﻪ ﻭ ﺍﺧﺘﻼﻝ ﺩﺭ -٥٥ Vodingﺟﻠﻮﮔﻴﺮﻱ ﺍﺯ ﭘﻴﺸﺮﻓﺖ ﻭ ﻋﻮﺍﺭﺽ ﺑﻠﻨﺪﻣﺪﺕ :BPH -٥٦ BPHﻛﻲ ﺑﺎﻳﺪ ﻣﺪﺍﺧﻠﻪ ﻛﺮﺩ؟ -٥٧-٥٨ﺭﻭﺵﻫﺎﻱ ﺍﺭﺯﻳﺎﺑﻲ /ﺁﻣﺎﺩﮔﻲ ﻭ ﺍﻧﺘﺨﺎﺏ ﺩﺭﻣﺎﻥ ﻣﻨﺎﺳﺐ ﺑﺮﺍﻱ -٥٩ BPHﻣﻬﺎﺭﻛﻨﻨﺪﻩﻫﺎﻱ 5αﺭﺩﻭﻛﺘﺎﺯ -٦٠-٦٦ﺭﻭﺵﻫﺎﻱ ﻣﺨﺘﻠﻒ ﺟﺮﺍﺣـﻲ ﺩﺭ BPH ﺷﺎﻣﻞ )ﺗﺮﺍﻧﺲ ﺍﻭﺭﺗﺮﺍﻝ ،needle Ablationﻟﻴﺰﺗﺮﺍﭘﻲ TUIP ،TUFP ،ﻭ ﻓﻴﺘﻮﺗﺮﺍﭘﻲ ﻭ openﭘﺮﻭﺳﺘﺎﺗﻜﺘﻮﻣﻲ( -٦٧-٧١ .ﭘﺮﻭﺳﺘﺎﺕ :ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ،ﻓﺎﻛﺘﻮﺭﻫﺎﻱ ﻣﺆﺛﺮ ﺩﺭ ﭘﺮﻭﮔﻨﻮﺯ ﻭ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺩﺭﻣﺎﻥﻫﺎ ﺩﺭ ﭘﺮﻭﺳﺘﺎﺕ. Atlas of RENAL TRANSPLANTATION
5.15
-Histopathology -surgery -clinical section -imaging -immunology AUA Vide Digest The American Urogical association (AUA) Impotence and Infertility
3.21
)(Prof. Legndre, Martin, Helenon, Lebranchu, Halloran, Nochy
ــــــ
-immunosupperssive ـــــ
ﺍﻳﻦ CDﺷﺎﻣﻞ ﻳﻜﻲ ﺍﺯ ﺳﺮﻱ ﻓﻴﻠﻢﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﺍﻧﺠﻤﻦ ﺍﻭﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎﻱ ﺁﻣﺮﻳﻜﺎ ) (AUA video digestﻣﻲﺑﺎﺷﺪ .ﻛﻪ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ Impotenceﻭ Infertiliteyﻣﻲﺑﺎﺷﺪ. ﻗﺴﻤﺖ ﺍﻭﻝ :Impotenceﺍﻟﻒ( ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﻭ ﺳﭙﺲ ﺍﻧﺘﺨﺎﺏ ﺩﺭﻣﺎﻥ ﻣﻨﺎﺳﺐ ﺁﻥ ﺑﻴﺎﻥ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﺩﺭ ﺣﻴﻦ ﻧﺸﺎﻥﺩﺍﺩﻥ ﻓﻴﻠﻢ ﺁﻣﻮﺯﺵ ﺗﻮﺳﻂ ﺍﺳﺎﺗﻴﺪ ﻣﺮﺑﻮﻃﻪ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ(Diagnosis8 treatment option) .
ﺏ( :Penile Venous Ligationﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﭼﮕﻮﻧﮕﻲ ﺍﻧﺠﺎﻡ ﻋﻤﻞ ﺟﺮﺍﺣﻲ ﺑﺎ ﺗﻮﺿﻴﺢ ﺣﻴﻦ ﻋﻤﻞ ﺑﺎ ﻓﻴﻠﻢ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻗﺴﻤﺖ ﺩﻭﻡ :Rectal Probe Electroejaculation :Infertiliryﺩﺭ ﺍﻳﻦ ﻗﺴﻤﺖ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ejaculationﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﻭ ﺳﭙﺲ ﺗﺠﻬﻴﺰﺍﺕ ﻭ ﺩﺳﺘﮕﺎﻩﻫﺎﻱ ﻣﻮﺭﺩ ﻧﻴﺎﺯ ﻭ ﻃﺮﺯ ﻛﺎﺭ ﺁﻧﻬﺎ ﺑﺎ ﻓﻴﻠﻢ ﻧﺸﺎﻥ ﺩﺍﺩﻩ ﺷﺪﻩ ﻭ ﺳﭙﺲ ﻃﺮﻳﻘﻪ ﺍﻧﺠﺎﻡ ﭘﺮﻭﺏﮔﺬﺍﺭﻱ ﻭ ﺍﻳﺠﺎﺩ ejaculationﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﺍﺳﺖ. 2004
)BLADDER BIOPSY INTERPRETATIONS (Jonathan I. Epstein, M.D., Mahul B. Amin, M.D., Victor E. Reuter, M.D.) (CD I, II) (SALEKAN E-BOOK
4.21
ﺍﻳﻦ ﻛﺘﺎﺏ ﻛﻪ ﺩﺭ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺗﺒﺪﻳﻞ ﺑﻪ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: Papillary Urothelial Neoplasms with Inverted Growth Patterns
Flat Urothelial Lesions
Normal Blodder Anatomy and Variants of Normal histology
Conventional Morphologic, Prognostic, and Predictive Factors and Reporting of Bladder Cancer Cystitis Second ary Tumors of the Bladder
Glandular Lesions Mesenchymal Tumors and Tumor-Like Lesions
Invasive Urothelial Carcinoma Squamous Lesions Miscellaneous Nontumors and Tumors
)Bristol Urological Institute (Computer Aided Learning Program
ــــــ
5.21
ﺑﻪ ﮔﻔﺘﺔ ﻣﺆﻟﻔﻴﻦ ﺍﻳﻦ CDﺑﺮﺍﻱ ﺍﻓﺰﺍﻳﺶ ﻣﻌﻠﻮﻣﺎﺕ ﺣﻔﻈﻲ ﻧﻴﺴﺖ ﺑﻠﻜﻪ ﻫﺪﻑ ﺍﻳﻦ CDﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﻧﺶ ﺍﻭﺭﻭﻟﻮﮊﻱ ﻫﺮ ﺷﺨﺺ ﻭ ﭼﮕﻮﻧﮕﻲ ﻓﻬﻢ ﻣﻄﺎﻟﺐ ﻭ ﻛﻢ ﺑﻪ ﺑﻬﺘﺮﻓﻬﻤﻴﺪﻥ ﻭ ﺗﺼﻤﻴﻢ ﮔﺮﻓﺘﻦ ﺩﺭ ﻣﻮﺭﺩ ﻣﺒﺎﺣﺚ ﺍﻭﺭﻭﻟﻮﮊﻱ ﺍﺳﺖ. ﺍﻳﻦ CDﺷﺎﻣﻞ ﺗﺴﺖﻫﺎﻱ ٤ﮔﺰﻳﻨﻪﺍﻱ ﺍﺳﺖ ﻭ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ: -١ﻣﻌﺎﻳﻨﻪ ﺑﻴﻤﺎﺭﺍﻥ ﺍﻭﺭﻭﻟﻮﮊﻱ
impotence -٢
-٣ﺗﺮﻭﻣﺎﻱ ﻛﻠﻴﻪ
-٤ﻋﻼﺋﻢ ﺩﺳﺘﮕﺎﻩ ﺍﺩﺭﺍﺭﻱ ﺗﺤﺘﺎﻧﻲ
-٥ﻫﻤﺎﺗﻮﺭﻱ
-٦ﻋﻘﻴﻤﻲ ﻣﺮﺩﺍﻥ -٧ﺳﻨﮓﻫﺎﻱ ﻛﻠﻴﻮﻱ
-٨ﺑﻲﺍﺧﺘﻴﺎﺭﻱ ﺍﺩﺭﺍﺭ
-٩ﺍﺧﺘﻼﻻﺕ ﺍﺳﻜﺮﻭﺗﻮﻡ
-١٠ﻛﺎﻧﺴﺮ ﭘﺮﻭﺳﺘﺎﺕ
-١ﺩﺭ ﻫﺮ ﻋﻨﻮﺍﻥ ﺍﺑﺘﺪﺍ ﻣﻘﺪﻣﻪﺍﻱ ﺩﺭ ﻣﻮﺭﺩ ﺑﻴﻤﺎﺭﻱ ﻭ ﺍﺧﺘﻼﻻﺕ ﻣﺮﺑﻮﻃﻪ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ -٢ .ﺳﭙﺲ ﺍﻫﺪﺍﻓﻲ ﻛﻪ ﺑﺎ ﻣﻄﺎﻟﻌﻪ ﺍﻳﻦ ﻗﺴﻤﺖ ﺍﺯ ﺑﻴﻤﺎﺭﻱ ﺑﺎﻳﺪ ﺑﻪ ﺩﺳﺖ ﺁﻭﺭﺩ ﺑﻴﺎﻥ ﺷﺪﻩ ﺍﺳﺖ -٣ .ﺩﺭ ﻗﺴﻤﺖ ﺳﻮﻡ ﺍﺑﺘﺪﺍ ﺷﺮﺡ ﺣﺎﻝ ﺑﻴﻤـﺎﺭﻱ ﻭ ﺳـﭙﺲ ﺗﺼـﺎﻭﻳﺮ ﺭﻧﮕـﻲ ،ﺭﺍﺩﻳـﻮﮔﺮﺍﻓﻲ، ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ،ﭘﺎﺗﻮﻟﻮﮊﻱ ﻫﺮ ﺍﺧﺘﻼﻝ ﺩﺭ ﺻﻔﺤﻪﺍﻱ ﺟﺪﺍﮔﺎﻧﻪ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﻭ ﺳﺆﺍﻻﺕ ٤ﺟﻮﺍﺑﻲ ﺑﺮ ﺁﻥ ﻓﺮﺍﻫﻢ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺩﺭ ﺁﺧﺮ ﻧﻴﺰ ﺑﻪ ﻣﻌﻠﻮﻣﺎﺕ ﺷﺨﺺ Scoreﺩﺍﺩﻩ ﻣﻲﺷﻮﺩ. CAMPBELL'S UROLOGY
2003 & Voiding Function Dysfunction
Infections and Inflammations of the Genitourinary Tract
Physiology, Pathology, and Management of Upper Urinary Tract Diseases
Oncology
Pediatric Urology
Sexual Function and Dysfunction
Urologic Examination and Diagnostic Techniques Reproductive Function and Dysfunction
Radiology Atlas
Pathology Atlas
Urologic Surgery
Urinary Lithiasis and Endourology Additional Media
ــــــ
)Non-Cardiac Surgery and Gynecology and Urology (Michael K. Rees, MD, MPH
Patient Evaluation for
6.21
Anatomy Benign Prostatic Hyperplasia Carcinoma of the Prostate Study Guide
Core Curriculum in Primary Care
7.21
CCCﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯ CDﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲ Harvardﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
72 CDﺣﺎﺿﺮ ﺩﺭ ﻣﻮﺭﺩ ﺟﺮﺍﺣﻲ ،ﺯﻧﺎﻥ ﻭ ﺍﻭﺭﻭﮊﻱ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖ .ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛﺎﺭﺑﺮ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜﻲ ،ﺳﺆﺍﻻﺕ ﻣﺮﺑﻮﻃﻪ ﺑﻪ ﺻﻮﺭﺕ ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑـﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﻘﺎﻟﻪ ﭼﺎﭘﻲ ﺩﺭ ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: -١ﭼﮕﻮﻧﻪ ﻳﻚ ﺑﻴﻤﺎﺭ ﺭﺍ ﺑﺮﺍﻱ ﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ )ﺑﺠﺰ ﺟﺮﺍﺣﻲ ﻗﻠﺐ( ﺍﺭﺯﻳﺎﺑﻲ ﻭ ﺁﻣﺎﺩﻩ ﻛﻨﻴﻢ؟ ــــــ
Male impotence
-٣ﻋﻘﻴﻤﻲ ﻣﺮﺩﺍﻥ -٢ﺍﺭﺯﻳﺎﺑﻲ ﺧﻮﻧﺮﻳﺰﻱﻫﺎﻱ ﺍﺑﻨﺮﻣﺎﻝ ﺭﺣﻢ ).(AUB )8.21 Core Curriculum in Primary Care Nephrology (Michael K. Rees, MD, MPH
CCCﻣﺠﻤﻮﻋﻪﺍﻱ ﺍﺯ CDﻫﺎﻳﻲ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺑﺮﺍﻱ ﺁﻣﻮﺯﺵ ﻣﺪﺍﻭﻡ ﺩﺳﺘﻴﺎﺭﺍﻥ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﻫﺮ ﺭﺷﺘﻪ ﺗﻮﺳﻂ ﺍﻋﻀﺎﺀ ﻫﻴﺌﺖ ﻋﻠﻤﻲ ﺩﺍﻧﺸﮕﺎﻩ ﭘﺰﺷﻜﻲ Harvardﺑﻨﺎ ﻧﻬﺎﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. CDﺣﺎﺿﺮ ﻣﻄﺎﻟﺒﻲ ﺍﺯ ﻧﻮﺭﻭﻟﻮﮊﻱ ﺑﻪ ﺻﻮﺭﺕ ﺍﺳﻼﻳﺪ ،ﺳﺨﻨﺮﺍﻧﻲ ،ﻧﻤﻮﺩﺍﺭ ﻭ ﺍﻟﮕﻮﺭﻳﺘﻢﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﺭﺍ ﮔﺮﺩﺁﻭﺭﻱ ﻛﺮﺩﻩ ﺍﺳﺖ. ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﺍﻳﻦ ﺳﺨﻨﺮﺍﻧﻲﻫﺎ ﻋﻼﻭﻩ ﺑﺮ ﺍﺳﻼﻳﺪﻫﺎﻱ ﺁﻣﻮﺯﺷﻲ ﻣﺘﻦ ﺳﺨﻨﺮﺍﻧﻲ ﻧﻴﺰ ﺩﺭ ﺩﺳﺘﺮﺱ ﻛﺎﺭﺑﺮ ﻣﻲﺑﺎﺷﺪ .ﺩﺭ ﺁﺧﺮ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﻭ ﻣﺒﺤﺜﻲ ،ﺳﺆﺍﻻﺕ ﻣﺮﺑﻮﻃﻪ ﺑﻪ ﺻﻮﺭﺕ ﭼﻬﺎﺭﮔﺰﻳﻨﻪﺍﻱ ﺑﺮﺍﻱ ﺍﺭﺯﻳﺎﺑﻲ ﻛﺎﺭﺑﺮ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺳﭙﺲ ﺧﻼﺻﻪ ﻫﺮ ﺳﺨﻨﺮﺍﻧﻲ ﺑﻪ ﺻﻮﺭﺕ ﻳﻚ ﻣﻘﺎﻟﻪ ﭼﺎﭘﻲ ﺩﺭ ﻣﺠﻼﺕ ﻋﻠﻤﻲ ﻭ ﺭﻭﺯﻧﺎﻣﻪﻫﺎ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. ﻣﺒﺎﺣﺚ ﺯﻳﺮ ﺩﺭ ﺍﻭﺭﻭﻟﻮﮊﻱ ﺩﺭ ﺍﻳﻦ CDﻣﻮﺟﻮﺩ ﺍﺳﺖ. 4-Clinical Application of Renal Physiology
2- Drugs vs Diet in Modifying Renal failure
3- Treatment of Mypertension-Special Case
1- How to erahcate Renal mass/Tumor
ــــــ
)Core Curriculum in Primary Care Gynecology (Michael, Isaac Schiff, Keith, Thomas, Annekathryn
12.3
ــــــ
Cystectomy and Construction an Ileocecal Neobladder for Urethral Voiding
9.21
)(John A. Libertino MD, FACS
2004
)(Roger S Kirby, Michael P O'Leary) (SALEKAN E-BOOK Erectile dysfunction and cardiovascular disease
New developments for the treatment of erectile dysfunction: Present and Future
Apoptosis in the prostate
ــــ
10.21 Hot Topics in UROLOGY Premature ejaculation Michael P O'Leary
Angiogenesis as a diagnostic and therapeutic tool in urological malignancy Chemoprevention of prostate cancer Robotic surgery and nanotechnology
Adjuvant therapy for prostate cancer
Marginally worse? Positive resection limits after radical prostatectomy
What,s hot and whats not - the medical management of BPH
I mmunotherapy for prostate
Bisphosphonates: a potential new treatment strategy in prostate cancer
Urethral stricture surgery: the state of the art
Future prospects for .. nephron conservation in renalcel I carcinoma
Three-dimensional imaging of the upper urinary tract
Laparoscopic radical prostatectomy
Management of female sexual dysfunction
Reducing medical errors in urology
Organ preserving therapies for penile carcinomas
The overactive bladder
Antisense therapy in oncology: current
)11.21 PRIMER ON KIDNEY DISEASES (Second Edition) (NATINAL KINDEY FOUNDATION SCIENTIFIC ADVISORY BOARD
ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻚ ﺩﺭ ﻣﺤﻴﻂ ﺍﻛﺮﻭﺑﺎﺕ ﺍﺟﺮﺍ ﺷﺪﻩ ﺍﺳﺖ .ﺷﺎﻣﻞ ١١ﻓﺼﻞ ﻭ ﻣﺸﺘﻤﻞ ﺑﺮ ٥١٧ﺻﻔﺤﻪ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -١ﺳﺎﺧﺘﻤﺎﻥ ﻭﻓﺎﻧﻜﺸﻦ ﻛﻠﻴﻪ ﻭ ﺍﺭﺯﻳﺎﺑﻲ ﺑﺎﻟﻴﻨﻲ ﻛﻠﻴﻪ ﺷﺎﻣﻞ :ﺁﻧﺎﺗﻮﻣﻲ ،ﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﺍﺭﺯﻳﺎﺑﻲ ﻓﺎﻧﻜﺸﻦ ﻛﻠﻴﻪ ،U/A ،ﻫﻤﺎﺗﻮﺭﻱ ،ﭘﺮﻭﺗﺌﻴﻦ ﺍﺩﺭﺍﺭﻱ ،ﺗﻜﻨﻴﻚ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺍﺯ ﻛﻠﻴﻪ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -٢ﺍﺧﺘﻼﻻﺕ ﺍﺳﻴﺪ ﻭ ﺑﺎﺯ ﻭ ﺍﻟﻜﺘﺮﻭﻧﻴﻚ ﺷﺎﻣﻞ :ﻫﻴﭙﻮﻭﻫﻴﺒﺮﻧﺎﺗﻮﻣﻲ ،ﺍﺳﻴﺪﻭﺯ ،ﺍﻟﻜﺎﻟﻮﺯﻣﺘﺎﺑﻮﻟﻴﻚ ،ﺍﺧﺘﻼﻻﺕ ﻣﺘﺎﺑﻮﻟﻴﺴﻢ ﭘﺘﺎﺳﻴﻢ ﻭ ﻛﻠﻴﺴﻴﻢ ،ﻣﻨﻴﺰﻳﻮﻡ ﻭ ﺩﻳﻮﺭﺗﻴﻚ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ Glomerular Diseuse -٣ﺷﺎﻣﻞ :ﺍﻳﻤﻮﻧﻮﭘﺎﺗﻮﮊﻧﺰ ﺑﻴﻤﺎﺭﻱ ﺍﻱ ﮔﻠﻮﻣﺮﻭﻱ MGN ،FSGN ،MPGN ،MCD ،ﻭ ﺳﻨﺪﺭﻭﻡ ﮔﻮﺩﭘﺎﺳﭽﺮ ﻭ IGAﻧﻔﺮﻭﭘﺎﺗﺎ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -٤ﻛﻠﻴﻪ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺳﻴﺴﺘﻤﻴﻚ ﻣﻲﺑﺎﺷﺪ ﺷﺎﻣﻞ :ﻛﻠﻴﻪ ﺩﺭ CHFﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﺒﺪﻱ PSGN ،ﻭ ﺍﺳﻜﻮﻟﻴﺖﻫﺎ ﻭ ﻛﻠﻴﻪ SLE ،ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺭﻭﻣﺎﺗﻴﺴﻤﻲ ﻭ ﻛﻠﻴﻪ ،ﺩﻳﺎﺑﺘﻴﻚ ﻧﻔﺮﻭﭘﺎﺗﻲ ﻭ HIVﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﻠﻴﻪ ﻭ ....ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -٥ﻧﺎﺭﺳﺎﺋﻲ ﺣﺎﺩ ﻛﻠﻴﻪ ﺷﺎﻣﻞ :ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ،ﻋﻠﻞ approach ،ﻭ ﺩﺭﻣﺎﻥ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻞ -٦ﺩﺍﺭﻭﻫﺎﻱ ﻭ ﻛﻠﻴﻪ :ﺷﺎﻣﻞ NSAIDﻭ ﻛﻠﻴﻪ ﻭ ﻣﻮﺍﺭﺩ ﺩﺍﺭﻭﻱ ﺩﺭﻣﺎﻧﻲ ﺩﺭ ﻧﺎﺭﺳﺎﺋﻲ ﻛﻠﻴﻪ ﻓﺼﻞ -٧ﺍﺧﺘﻼﻻﺕ ﺍﺭﺛﻲ ﻛﻠﻴﻪ :ﻧﻔﺮﻭﭘﺎﺗﻲ ،Sickle cellﺑﻴﻤﺎﺭﻱﻫﺎﻱ Cysticﻛﻠﻴﻪ ،ﺳﻨﺪﺭﻭﻡ Alportﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﺴﻴﺘﻴﻚ ﻛﻠﻴﻪ ﻓﺼﻞ -٨ﻧﻔﺮﻭﭘﺎﺗﻲ ﺗﻮﺑﻮﻟﻮﺍﻳﻨﺘﺮﺳﺘﻴﺸﻴﻞ ﻭ ﺍﺧﺘﻼﻻﺕ ﻣﺠﺎﺭﻱ ﺍﺩﺍﺭﻱ ﺷﺎﻣﻞ :ﺑﻴﻤﺎﺭﻱ ﻛﻠﻴﻪ ﻭ ﻟﻴﺘﻴﻮﻡ ﺳﺮﺏ ،ﺍﮔﺰﺍﻻﺕ ﺳﻨﮓﻫﺎﻱ ﻛﻠﻴﻮﻱ ،ﻋﻔﻮﻧﺖﻫﺎﻱ ﻛﻠﻴﻮﻱ ،ﻋﻔﻮﻧﺖﻫﺎﻱ ﻛﻠﻴﻮﻱ ﺍﻧﺴﺪﺍﺩ ﻣﺠﺎﺭﻱ ﻭ ﺳﺮﻃﺎﻥﻫﺎﻱ ﻛﻠﻴﻪ ﻭ ﻣﺠﺎﺭﻱ ﺁﻥ. ﻓﺼﻞ -٩ﻛﻠﻴﻪ ﻭ ﻣﻮﺍﺭﺩ ﺧﺎﺹ ﺷﺎﻣﻞ‚ ﻛﻠﻴﻪ ﺩﺭ ﻧﻮﺯﺍﺩﺍﻥ ﻭ ﻛﻮﺩﻛﺎﻥ ،ﻛﻠﻴﻪ ﺩﺭ ﺣﺎﻣﻠﮕﻲ ،ﻛﻠﻴﻪ ﺩﺭ ﭘﻴﺮﻱ. ﻓﺼﻞ -١٠ﻧﺎﺭﺳﺎﺋﻲ ﻣﺰﻣﻦ ﻛﻠﻴﻪ ﻭ ﺩﺭﻣﺎﻥ ﺷﺎﻣﻞ :ﺳﻨﺪﺭﻭﻡ ﺍﻭﺭﻣﻲ ،ﻫﻤﻮﺩﻳﺎﻟﻴﺰ ﻭ ﻫﻤﻮﻓﻴﻠﺘﺮﺍﺳﻴﻮﻥ ﺩﻳﺎﻟﻴﺰ ﺻﻔﺎﺗﻲ ،ﭘﻴﺶﺁﮔﻬﻲ ﻭ ﺗﻐﺬﻳﻪ ،CRFﺗﻈﺎﻫﺮﺍﺕ ﻗﻠﺒﻲ ،ﻋﺼﺒﻲ ،ﻫﻤﺎﺗﻮﻟﻮﮊﻱ ،ﻏﺪﺩﻱ CRFﻭ ﭘﻴﻮﻧﺪ ﻛﻠﻴﻪ ﻭ ﭼﮕﻮﻧﮕﻲ ﺩﺍﺭﻭﺩﻣﺎﻧﻲ ﺩﺭ ﺁﻧﻬﺎ. ﻓﺼﻞ -١١ﻓﺸﺎﺭ ﺧﻮﻥ ﺷﺎﻣﻞ :ﭘﺎﻧﻮﮊﻧﺰ ،ﻓﺸﺎﺭ ﺧﻮﻥ ﺍﺳﺎﺳﻲ ،ﻓﺸﺎﺭ ﺧﻮﻥ Renovascularﻭ ﺩﺭﻣﺎﻥ ﻓﺸﺎﺭ ﺧﻮﻥ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
73 )(Official Journal of the American Urological Association
2003
-CME Participant Assessment Test and Course Evaluation
)(CD I, II
)(Spring & Summer
12.21 The Journal of UROLOGY
-Urological Survey
-Investigative Urology
-Pediatric Urology
- Clinical Urology
CD I:
-Urological Survey
-Investigative Urology
-Pediatric Urology
- Clinical Urology
CD II:
)13.21 Urogynecology: Evaluation and Treatment of Urinary Incontinence (Bruce Rosenzweig, MD, Jeffrey S. Levy, MD, Donald R. Ostergard, MD
ــــــ
ﻼ ﺭﻧﮕﻲ ﺑﻮﺩﻩ ﻭ ﺗﻮﺿﻴﺤﺎﺕ ﺑﻪ ﺻﻮﺭﺕ ﻧﻮﺷﺘﺎﺭﻱ ﻭ ﻓﺎﻳﻞ ﺻﻮﺗﻲ ﻛﻪ ﺑﺮ ﺭﻭﻱ ﻫﺮ ﻗﺴﻤﺖ ﺍﺯ ﺍﻳﻦ CDﻭﺟﻮﺩ ﺩﺍﺭﺩ. ﺍﻳﻦ CDﻛﻪ ﺑﻪ ﺻﻮﺭﺕ ﺗﺼﺎﻭﻳﺮ ﻛﺎﻣ ﹰ ٤ Urogynechologyﻗﺴﻤﺖ ﻣﺠﺰﺍ ﺩﺍﺭﺩ ﺷﺎﻣﻞ:
-١
Introduction Definigg Incontinence
Evaluation -٢
:Introduction & Defining Incontince (١
-٣
won surgical & surgical Management
ﺍﻳﻦ ﻗﺴﻤﺖ ﺧﻮﺩ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ:
yﺗﺸﺨﻴﺺ incontince
-٤
Consideration for the OB/GYN Generalist
affected women y
Patient misconceptions y
Types of incontinernce y incontinence awareness y (٢ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﺍﻥ ﺑﺎ :incontinency
y Voiding diary yﺗﺎﺭﻳﺨﭽﻪ yﻣﻌﺎﻳﻨﺎﺕ ﺑﺎﻟﻴﻨﻲ
un , u/s y Multi-Channel urodynamics y
Cystoscopy y uroflowmetry y Postvoid residual y Cystometrogram y Pad test y
Pessary test y
(٣ﺗﺪﺍﺑﻴﺮ ﺩﺭﻣﺎﻧﻲ ﺟﺮﺍﺣﻲ ﻭ ﻏﻴﺮ ﺟﺮﺍﺣﻲ ﺩﺭ : Stress urinary incontinence ﺍﻳﻦ ﻗﺴﻤﺖ ﺷﺎﻣﻞ ﺍﻟﮕﻮﺭﻳﺘﻢ ﺗﺼﻤﻴﻢﮔﻴﺮﻱ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻣﻲﺑﺎﺷﺪ ﻭ ﺳﭙﺲ ﺭﻭﺵ ﺩﺭﻣﺎﻧﻲ ﻏﻴﺮﺟﺮﺍﺣﻲ )) biofeedback, Beharioral modificationﻭ ﺩﺭﻣﺎﻥﻫﺎﻱ ﺩﺍﺭﻭﺋﻲ funetional electrieal Stimalationﻭ (....ﺑﺤﺚ ﺷﺪﻩ ﺍﺳﺖ. ﺭﻭﺵﻫﺎﻱ ﺟﺮﺍﺣﻲ :ﺍﺑﺘﺪﺍ ﺩﺭ ﻣﻮﺭﺩ ﺭﻭﺵﻫﺎﻱ ﺍﻧﺠﺎﻡ ﺟﺮﺍﺣﻲ ﺑﺤﺚ ﺷﺪﻩ ﻭ ﺳﭙﺲ Procedureﺍﻋﻤﺎﻝ ﺟﺮﺍﺣﻲ ﺷﺮﺡ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺩﺭ ﻗﺴﻤﺖﻫﺎﻱ ﺑﻌﺪﻱ ﻣﻘﺎﻳﺴﻪ ﺩﺭﺻﺪ ﻣﻮﻓﻘﻴﺖ ﺭﻭﺵﻫﺎ ﺫﻛـﺮ ﺷـﺪﻩ ﻭ ﺩﺭ ﺁﺧـﺮ Complicationﺍﻳـﻦ ﺭﻭﺵﻫـﺎ ﺗﻮﺿﻴﺢ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ. : Consideration for the OB/Gyn Generalist (٤ ﺩﺭ ﺍﻳﻦ ﻓﺼﻞ: urogynechology as a subdiscipline y professional consideration y
Non surgical therapy y Urodynamics y
incontinrence management to private patients y equipment cost ySet-up requirement y
eystometry y Allied Staff y
)Seven Edition (Barry M. Brenner) (E-Book
ــــ
ﻣﻮﺭﺩ ﺑﺤﺚ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. )(Volume 1-2
14.21 The Kidney
ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻟﻜﺘﺮﻭﻧﻴﻜﻲ ﺷﺎﻣﻞ ﺩﻭ ﺟﻠﺪ ﺍﺳﺖ . ﺩﺭ ﺍﻧﺘﻬﺎﻱ ﻫﺮ ﺑﺨﺶ ﻛﺘﺎﺏ ،ﺗﺼﺎﻭﻳﺮ ﻣﺮﺑﻮﻃﻪ ﺑﺎ ﻭﺿﻮﺡ ﺑﺎﻻ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﻛﻴﻔﻴﺖ ﺑﺎﻻﻱ ﺗﺼﺎﻭﻳﺮ ،ﺍﻳﻦ ﺍﻣﻜﺎﻥ ﺭﺍ ﻓﺮﺍﻫﻤﻲ ﻣﻲﺳﺎﺯﺩ ﺗﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺁﻧﻬﺎ ﺩﺭ ﺳﻤﻴﻨﺎﺭﻫﺎ ﻭ ﻫﻤﻴﻨﻄﻮﺭ ﺟﻬﺖ ﺁﻣﻮﺯﺵ ﻣﻨﺎﺳﺐ ﺑﺎﺷﺪ .ﺍﻳﻦ ﺟﻠﺪ ﺩﺍﺭﺍﻱ ﺩﻭ ﺑﺨﺶ ﺍﺳﺖ:
-١ﻗﺴﻤﺖﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻛﻠﻴﻪ ﻃﺒﻴﻌﻲ ﻭ ﻋﻤﻠﻜﺮﺩ ﻫﺮ ﻳﻚ ﺍﺯ ﺍﻳﻦ ﺑﺨﺶﻫﺎ ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﻣﺒﺎﺣﺜﻲ ﻫﻤﭽﻮﻥ ﺁﻧﺎﺗﻮﻣﻲ ﻛﻠﻴﻪ ،ﺭﺷﺪ ﻭ ﺑﻠﻮﻍ ﻛﻠﻴﻪ ،ﺍﺻﻮﻝ ﻣﺘﺎﺑﻮﻟﻴﻚ ﺍﻧﺘﻘﺎﻝ ﻳﻮﻥ ،ﺟﺮﻳﺎﻥ ﺧﻮﻥ ﻛﻠﻴﻪ ،ﺍﻧﺘﻘﺎﻝ ﻛﻠﻴﻮﻱ ﮔﻠﻮﻛﺰ ،ﺍﺳﻴﺪ ﺁﻣﻴﻨﻪ ،ﺳﺪﻳﻢ ،....ﻛﻨﺘﺮﻝ ﺗﺮﺷﺢ ﻛﻠﻴﻮﻱ ﭘﺘﺎﺳﻴﻢ ﻭ ....ﺩﻫﻬﺎ ﻋﻨﻮﺍﻥ ﺩﻳﮕﺮ ﻣﻄﺮﺡ ﺷﺪﻩﺍﻧﺪ. -٢ﺍﺧﺘﻼﻝ ﺩﺭ ﻛﻨﺘﺮﻝ ﺣﺠﻢ ﻣﺎﻳﻊ ﺑﺪﻥ :ﻛﻨﺘﺮﻝ ﺣﺠﻢ ﺧﺎﺭﺝ ﺳﻠﻮﻟﻲ ﻭ ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺍﺩﻡ ،ﻋﻮﺍﻣﻞ ﻣﺆﺛﺮ ﺑﺮ ﻫﻤﻮﺳﺘﺎﺯ ﻣﺎﻳﻊ ،ﻓﺎﻛﺘﻮﺭﻫﺎﻱ ﻣﺆﺛﺮ ﺑﺮ ﺗﻮﺑﺮﻝ ﻛﻠﻴﻪ ،AVP ،ﭘﺮﻭﺳﺘﺎﮔﻼﻧﺪﻳﻦﻫﺎ ،ﺍﺩﻡ ﺩﺭ ﺳﻴﺮﻭﺯ ،ﺍﺩﻡ ﺩﺭ ،CHFﺩﻳﺎﺑﺖ ﺑﻲﻣﺰﻩ ﻭ ﺍﻧـﻮﺍﻉ ﺁﻥ ،ﻫﻴﭙﻮﻧـﺎﺗﺮﻣﻲ ﻭ ﺍﻳﺘﻮﻟـﻮﮊﻱﻫـﺎﻱ ﻣﺨﺘﻠﻒ ﺁﻥ ،ﺍﺧﺘﻼﻻﺕ ﺍﺳﻴﺪ ﻭ ﺑﺎﺯ ،ﺍﺧﺘﻼﻻﺕ ﺗﻮﺍﺯﻥ ﭘﺘﺎﺳﻴﻢ ،ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺑﻴﻤﺎﺭ ﻣﺒﺘﻼ ﺑﻪ ﻫﻴﭙﻮﻭﻫﻴﭙﺮﻛﺎﺳﻤﻲ ،ﺍﺧﺘﻼﻻﺕ ﻛﻠﺴﻴﻢ ﻭ ﻓﺴﻔﺮ ﻭ ....ﺩﻫﻬﺎ ﻣﻄﻠﺐ ﺩﻳﮕﺮ ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ،ﺩﺭ ﺩﺳﺘﺮﺱ ﻣﻲﺑﺎﺷﻨﺪ. ﺟﻠﺪ ٢ﻛﺘﺎﺏ ﺷﺎﻣﻞ ٣ﻗﺴﻤﺖ ﺍﺳﺖ:
ﺍﻟﻒ( ﭘﺎﺗﻮﻓﻴﺰﻳﻮﻟﻮﮊﻱ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﻠﻴﻪ :ﻣﺒﺎﺣﺜﻲ ﭼﻮﻥ :ﺍﺭﺯﻳﺎﺑﻲ ﺑﺎﻟﻴﻨﻲ ﺩﺭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﻠﻴﻪ ،ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﮔﻠﻮﻣﺮﻭﻟﻲ ﺍﻭﻟﻴﻪ ﻭ ﺛﺎﻧﻮﻳﻪ ،ﻋﻔﻮﻧﺖﻫﺎﻱ ﺍﺩﺭﺍﺭﻱ ،ﻧﻔﺮﻭﭘﺎﺗﻲ ﺗﻮﻛﺴﻴﻚ ﻭ ....ﺩﻫﻬﺎ ﻣﻄﻠﺐ ﺩﻳﮕﺮ. ﺏ( ﭘﺎﺗﻮﮊﻧﺰ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻛﻠﻴﻪ :ﻧﺌﻮﭘﻼﺯﻱ ﻛﻠﻴﻪ ،ﻫﻴﭙﺮﺗﺎﻧﺴﻴﻮﻥ )ﺍﻭﻟﻴﻪ (renovascularﺍﻭﺭﻱ ،ﺍﺳﺘﺌﻮﺩﺳﻴﺘﺮﻭﻓﻲ ﺭﻧﺎﻝ ﻭ ...ﺍﺯ ﺟﻤﻠﻪ ﻣﺒﺎﺣﺚ ﻣﻄﺮﺡ ﺷﺪﻩ ﻣﻲﺑﺎﺷﻨﺪ. ﺝ( ﺑﺮﺧﻮﺭﺩ ﺑﺎ ﺑﻴﻤﺎﺭ ﻣﺒﺘﻼ ﺑﻪ ﻧﺎﺭﺳﺎﻳﻲ ﻛﻠﻴﻮﻱ :ﺍﻧﻮﺍﻉ ﺩﻳﺎﻟﻴﺰ ،ﺍﻳﻤﻮﻧﻮﻟﻮﮊﻱ ﭘﻴﻮﻧﺪ ،ﺍﻧﻮﺍﻉ ﺩﺍﺭﻭﻫﺎﻱ ﺩﻳﻮﺭﺗﻴﻚ ﻭ ....ﺩﺭ ﺍﻳﻦ ﺑﺨﺶ ﺑﺤﺚ ﺷﺪﻫﺎﻧﺪ. 2005
)15.21 SCHWARTZ'S PRINCIPLES OF SURGERY (8th Edition) (F. Charles Brunicardi, Dana K. Andersen, Timothy R. Billiar) (Salekan e-book) (CD I, II
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
74
ﻃﺮﻳﻘﺔ ﻣﺸﺎﻫﺪﻩ ﻓﻴﻠﻢﻫﺎﻱ VCDﺗﻮﺳﻂ ﻛﺎﻣﭙﻴﻮﺗﺮ :
ﺍﺑﺘﺪﺍ ﺑﻪ my computerﺭﻓﺘﻪ ﻭ ﻭﺍﺭﺩ ﺩﺭﺍﻳﻮ CD-ROMﺩﺳﺘﮕﺎﻩ ﺷﻮﻳﺪ ﺳﭙﺲ ﺑﺎ ﺩﻭﺑﺎﺭ ﻛﻠﻴﻚ ﺑﺮ ﺭﻭﻱ Xing playerﺑﺮﻧﺎﻣﻪ Xingﺭﺍ ﻧﺼﺐ ﻛﻨﻴـﺪ .ﺍﺯ ﺭﻭﻱ Xing Mpeg Player ، desktopﺭﺍ ﺑـﺎﺯ ﻛـﺮﺩﻩ ، ﺳﭙﺲ ﺍﺯ ﺭﻭﻱ ﻣﻨﻮﻱ Open ، Fileﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ .ﺩﺭ ﻗﺴﻤﺖ Look inﺩﺭﺍﻳﻮ CD-Romﺩﺳﺘﮕﺎﻩ ﺧﻮﺩ ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﺮﺩﻩ ﻭ ﺩﺭ ﻗﺴﻤﺖ Video CD ( *.dat) . Files of typeﺭﺍ ﺍﻧﺘﺨـﺎﺏ ﻛﻨﻴـﺪ ،ﺳـﭙﺲ ﺑـﻪ ﺩﺍﻳﺮﻛﺘﻮﺭﻱ Mpegavﺭﻓﺘﻪ ﻭ Avseq01ﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﺮﺩﻩ ﻭ Openﺭﺍ ﺑﺰﻧﻴﺪ.
ﻃﺮﻳﻘﻪ ﻧﺼﺐ ﻧﺮﻡ ﺍﻓﺰﺍﺭﻫﺎﻱ : E-book
-١ -٢ -٣ -٤ -٥ -٦
ﺑﺎ ﺍﺯ ﻗﺮﺍﺭ ﺩﺍﺩﻥ ﺳﻲ ﺩﻱ E-bookﺩﺭ ﺩﺭﺍﻳﻮ CD-Romﺻﻔﺤﻪ PCA pdf book setupﺑﻪ ﺻﻮﺭﺕ Autorunﺑﺎﺯ ﻣﻲﺷﻮﺩ . ﺩﺭ ﺻﻮﺭﺗﻲ ﻛﻪ ﺍﻭﻟﻴﻦ ﺑﺎﺭ ﺍﺳﺖ ﻛﻪ CDﻫﺎﻱ E-bookﺍﻳﻦ ﺷﺮﻛﺖ ﺭﺍ ﺩﺭ ﺩﺳﺘﮕﺎﻩ ﻣﻲﮔﺬﺍﺭﻳـﺪ “ ﺑـﺎ ﺍﻧﺘﺨـﺎﺏ ﮔﺰﻳﻨـﻪ Acrobat Reader Installationﺑﺮﻧﺎﻣـﻪ Acrobatﺭﺍ ﻧﺼـﺐ ﻭ ﻣﺮﺍﺣﻞ ﺁﻥ ﺭﺍ ﺗﺎ ﺍﻧﺘﻬﺎ ﻃﻲ ﻛﻨﻴﺪ“ ﺩﺭ ﻏﻴﺮ ﺍﻳﻨﺼﻮﺭﺕ ﺑﻪ ﻣﺮﺣﻠﻪ ٣ﺑﺮﻭﻳﺪ . ﻣﻨﻮﻱ Execute The Programﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ. ﺑﺎ ﺍﻧﺘﺨﺎﺏ ﻧﺎﻡ ﻛﺘﺎﺏ ،ﮔﺰﻳﻨﻪ Viewﺭﺍ ﺍﻧﺘﺨﺎﺏ ﻛﻨﻴﺪ. ﺑﺮﻧﺎﻣﻪ Acrobatﺑﺎﺯ ﻣﻲﺷﻮﺩ ﻭ ﻛﺘﺎﺏ ﺭﺍ ﻣﻲﺗﻮﺍﻧﻴﺪ ﻣﻄﺎﻟﻌﻪ ﺑﻔﺮﻣﺎﺋﻴﺪ. ﺑﺮﺍﻱ ﺍﺟﺮﺍﻱ ﺑﺮﻧﺎﻣﻪ ﻻﺯﻡ ﺍﺳﺖ ﻛﻪ ﺩﺭﺍﻳﻮ \ C:ﺩﺳﺘﮕﺎﻫﺘﺎﻥ ﺣﺪﺍﻗﻞ 500ﻣﮕﺎﺑﺎﻳﺖ ﻓﻀﺎﻱ ﺧﺎﻟﻲ ﺩﺍﺷﺘﻪ ﺑﺎﺷﺪ ﺩﺭ ﻏﻴﺮ ﺍﻳﻨﺼﻮﺭﺕ ﺑﻌﺪ ﺍﺯ ﺯﺩﻥ Viewﺩﺳﺘﮕﺎﻩ Error 110ﺭﺍ ﻣﻲﺩﻫﺪ.
ﺍﺳﺎﻣﻲ ﻛﺘﺎﺏ/ﻧﻮﻳﺴﻨﺪﻩ
ﻗﻴﻤﺖ )ﺭﻳﺎﻝ( ﺗﻌﺪﺍﺩ ﻣﺠﻠﺪﺍﺕ
RADIOLOGY 200,000
ﺗﻚ ﺟﻠﺪﻱ
)Pediatric Radiology (The Requestions) (Hans Blickman
1.
240,000
ﺗﻚ ﺟﻠﺪﻱ
)Differential Diagnosis in Conventioanl Gastrointestinal Readiology (Francis A. Burgener, Marti Konnano
2.
500,000
ﺗﻚ ﺟﻠﺪﻱ
)Dynamic Radiology of the Abdomen: Normal and Pathologic Anatomy (Morton A. Meyers, 5 Edition Springer Verla
3.
250,000
ﺗﻚ ﺟﻠﺪﻱ
)Primary Care Radiology (Mettker, Guibert EAU. VO.SS', URBINA
4.
400,000
ﺗﻚ ﺟﻠﺪﻱ
)Textbook of Uroradiology (N. Reed Dunnick, MD, Carl M. Sandler, Md, Jeffrey H. Newhouse, MD, Estephen Amis', JR., MD
5.
400,000
ﺗﻚ ﺟﻠﺪﻱ
)Head and Neck Radiology a Teaching File (Anthony a Mancusd, Hiroya Ojiri, Ronald G. Quisling)(Lippincottt Williams & Wilkins
6.
700,000
ﺩﻭ ﺟﻠﺪﻱ
)Essentials of Skeletal Radiology (Terry R. Yochum; Lindsay J. Rowe
7.
th
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
75
)Textbook of Radiology & Imaging (David Stutton) (2003
8.
)Radiology Reviw Manual (Fourth Edition) (Wolfgang Dahnert) (2003
9.
1,400,000
ﺩﻭ ﺟﻠﺪﻱ )ﺍﻭﺭﮊﻳﻨﺎﻝ(
400,000
ﺗﻚ ﺟﻠﺪﻱ
300,000
ﺗﻚ ﺟﻠﺪﻱ
)10. Forensic Radiology (B. G. Brogdon MD
400,000
ﺗﻚ ﺟﻠﺪﻱ
)11. The Core Curriculum Neuroradiology (Mauricio Castillo) (Lippincott Williams & Wilkins
500,000
ﺗﻚ ﺟﻠﺪﻱ
)12. Diagnostic Neuroradiology (Anne G. Osborn) (Mosby
300,000
ﺗﻚ ﺟﻠﺪﻱ
)13. Bone and Joint Disorders (Conventional Radiologic Differentioal Diagnosis) (Francis A. Burgener Marti Kormano
400,000
ﺗﻚ ﺟﻠﺪﻱ
)14. Atlas of Radiologic Measurement (Theodore E. Keats, Christopher Sistrom) (Mosby
400,000
ﺗﻚ ﺟﻠﺪﻱ
)15. Radiobiology for the Radiologist (Fifthe Edition
470,000
ﺗﻚ ﺟﻠﺪﻱ
)16. Anatomy Positioning & Procedures Workbook (Steven G. Hayes
700,000
ﺗﻚ ﺟﻠﺪﻱ
)17. Atlas of Normal Roentgen Variants That May Simulate disease (Seven Edition) (Theodere E. Keats & Mark W. Anderson) (Mosby
50,000
ﺗﻚ ﺟﻠﺪﻱ
ﻣﺒﺎﻧﻲ ﺍﺳﺎﺳﻲ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﻭ ﺗﺠﻬﻴﺰﺍﺕ ﺁﻥ )ﺗﺮﺟﻤﻪ ﻭ ﮔﺮﺩﺁﻭﺭﻱ :ﺩﻛﺘﺮ ﭘﺮﻭﻳﻦ ﻋﻠﻲﭘﻮﺭ( 18.
180,000
ﺗﻚ ﺟﻠﺪﻱ
ﺍﺻﻮﻝ ﺗﺸﺨﻴﺼﻲ ﻭ ﺩﺭﻣﺎﻧﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﭘﺴﺘﺎﻥ )ﺩﻛﺘﺮ ﻣﻌﺼﻮﻣﻪ ﮔﻴﺘﻲ ،ﺩﻛﺘﺮ ﺍﻟﻬﺎﻡ ﺭﺣﻴﻤﻴﺎﻥ ،ﺩﻛﺘﺮ ﻋﻠﻲ ﻋﺮﺏ ﺧﺮﺩﻣﻨﺪ( 19.
50,000
ﺗﻚ ﺟﻠﺪﻱ
ﺷﺎﻳﻌﺘﺮﻳﻦﻫﺎ ،ﻧﺎﺩﺭﺗﺮﻳﻦﻫﺎ ،ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ،ﺑﻬﺘﺮﻳﻦ ﺭﻭﺵ ﺗﺸﺨﻴﺺ ﺑﻴﻤﺎﺭﻱﻫﺎ )ﺗﺄﻟﻴﻒ :ﺩﻛﺘﺮ ﺍﺣﻤﺪ ﻋﻠﻴﺰﺍﺩﻩ( 20.
380,000
ﺩﻭ ﺟﻠﺪﻱ
)21. Radiographic Anatomy Positioning and Procedures Workbook (Second Edition) (volume I , II) (Steven G. Hayes, Sr.
600,000
ﺗﻚ ﺟﻠﺪﻱ
250,000
ﺗﻚ ﺟﻠﺪﻱ
)23. Imaging Atlas of Human Anatomy (Third Edition) (Jamie Weir, Peter H. Abrahams) (2003
600,000
ﺗﻚ ﺟﻠﺪﻱ
)24. Pediatric Sonography (Third Edition) (Thieme) (Francis A. Burgener, Steven P. Meyers) (2004
500,000
ﺗﻚ ﺟﻠﺪﻱ
)25. Musculoskeletal Imaging Companion (Thomas H. Berquist) (2002
ﺗﻚ ﺟﻠﺪﻱ
)26. Practical Guide to Abdominal & Pelvic MRI (John R. Leyendecker, Jeffrey J. Brown
در اﯾﻦ ﮐﺘﺎب ،ﻗﺴﻤﺖ اﻋﻈﻢ ﺟﺪاول و ﻧﻤﻮدارﻫﺎی ﻣﻌﻢ ﮐﺎرﺑﺮدی ﻣﺮﺗﺒﻂ ﺑﺎ اﻧﺪازهﮔﯿﺮیﻫﺎی رادﯾﻮﻟﻮژی و ﺗﺼﻮﯾﺮﺑﺮداری در 14ﻣﺒﺤﺚ و در 630ﺻﻔﺤﻪ ﮔﺮدآوری ﮔﺮدﯾﺪه و ﻣﯽﺗﻮاﻧﺪ ﺑﻪ ﻋﻨﻮان ﯾﮏ اﺑﺰار ﺑﺴﯿﺎر ﻣﻬﻢ در ﺗﻔﺴﯿﺮ ﻧﻮاﺣﯽﻫﺎی ﻣﺨﺘﻠﻒ ﻣﻮرد اﺳﺘﻔﺎده ﻗﺮار ﮔﯿﺮد .ﻓﺼﻮل اﯾﻦ ﮐﺘﺎب ﺑﻪ ﻗﺮار ذﯾﻞ ﻣﯽﺑﺎﺷﻨﺪ: ﻣﺤﺘﻮﯾﺎت اﯾﻨﺘﺮاﮐﺮاﻧﯿﺎل -ﺟﻤﺠﻤﻪ ﺣﻔﺮه ادرﺑﯿﺖ و ﺳﯿﻨﻮسﻫﺎی ﭘﺎراﻧﺎﻣﺎل -ﻣﺤﺘﯿﺎت ادرﺑﯿﺖ ﺻﻮرت و ﮔﺮدن -ﺳﺘﻮن ﻓﻘﺮات و ﻣﺤﺘﻮﯾﺎت آن -اﻧﺪام ﻓﻮﻗﺎﻧﯽ -ﻟﮕﻦ و ﻣﻔﺎﺻﻞ - Hipاﻧﺪام ﺗﺤﺘﺎﻧﯽ ﺑﯿﻮﻣﺘﺮی و ﭘﻠﻮﺳﯿﺘﺮی در ﺟﺮﯾﺎن ﺣﺎﻣﻠﮕﯽ -ﺳﯿﺴﺘﻢ ﻋﺮوﻗﯽ و ﻟﻨﻔﺎوی ﺗﻮراﮐﺲ ،رﯾﻪﻫﺎ ،ﻣﺪﯾﺎﺳﺘﻦ و ﺟﻨﺐ -دﺳﺘﮕﺎه ﮔﻮارش -دﺳﺘﮕﺎه ادراری -ﺗﻨﺎﺳﻠﯽ ﻗﻠﺐ و ﻋﺮوق ﺑﺰرگ -ﺑﻠﻮغ اﺳﮑﻠﺘﯽ
)(Lippincott Williams & Wilkins) (2003
)(Ronald L. Eisenberg
)22. Gastrointestinal Radiology A Pattern Approach (4th Edition
اﯾﻦ ﮐﺘﺎب ﻣﺠﻤﻮﻋﮥ ﮐﺎﻣﻠﯽ از ﻣﺒﺎﺣﺚ ﻣﺨﺘﻠﻒ ﻣﺮﺗﺒﻂ ﺑﺎ ﺗﺼﻮﯾﺮﺑﺮداری دﺳﺘﮕﺎه ﮔﻮارش ﻣﯽﺑﺎﺷﺪ .ﻣﻄﺎﻟﺐ اﯾﻦ ﮐﺘﺎب در 80ﻣﺒﺤﺚ 10 ،ﻓﺼﻞ ﺗﺪوﯾﻦ ﮔﺮدﯾﺪه و ﺣﺪود 1200ﺻﻔﺤﻪ ﺣﺠﻢ دارد روش اراﺋﻪ ﻣﻄﺎﻟﺐ در اﯾﻦ ﮐﺘﺎب ﺑﻪ ﺻﻮرت Pattern Approachﺑﻮده و ﺧﻮاﻧﻨﺪه را ﻗﺎدر ﻣﯽﺳﺎزد ﺗﺎ اﻟﮕﻮﻫﺎی ﺗﺼﻮﯾﺮﺑﺮداری ﻣﺨﺘﻠﻒ دﺳﺘﮕﺎه ﮔﻮارش را دﺳﺘﻪﺑﻨﺪی ﻧﻤﻮده و ﺗﺸﺨﯿﺺﻫﺎی اﻓﺘﺮاﻗﯽ ﻫﺮ ﮐﺪام را ﺑﻪ ﺧﻮﺑﯽ از دﯾﮕﺮ اﻟﮕﻮﻫﺎ ﺗﻤﯿﺰ دﻫﺪ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
76
SONOGRAPHY 350,000
ﺗﻚ ﺟﻠﺪﻱ
)27. Ultrasonography in Urology A Practical Approach to Clinical Problems (Edward I. Bluth-Peter H.
70,000
ﺗﻚ ﺟﻠﺪﻱ
28. Seminars in Ultrasound CT and MR
1,400,000
ﺩﻭ ﺟﻠﺪﻱ
)29. Diagnostic Ultrasound (Rumack, Wilson, Charboneau) (2005 ﭼﺎپ اول اﯾﻦ ﮐﺘﺎب ﮐﻪ در ﺳﺎل 1991ﺑﻪ ﭘﺎﯾﺎن رﺳﯿﺪ و ﺑﻪ ﻋﻨﻮان راﯾﺞﺗﺮﯾﻦ ﻣﺮﺟﻊ ﺳﻮﻧﻮﮔﺮاﻓﯽ در ﺟﻬﺎن ﻣﯽﺑﺎﺷﺪ .از آﻧﺠﺎ ﮐﻪ داﻧﺶ ﺳﻮﻧﻮﮔﺮاﻓﯽ در ﻃﻮل 6ﺳﺎل ﮔﺬﺷﺘﻪ ﭘﯿﺸﺮﻓﺖﻫﺎی ﺑﺴﯿﺎری داﺷﺘﻪ اﺳﺖ ﻧﯿـﺎز ﺑـﻪ ﺑـﺎزﻧﮕﺮی در اﯾﻦ ﮐﺘﺎب اﺣﺴﺎس ﻣﯽﺷﺪ. در اﯾﻦ ﮐﺘﺎب ﺑﯿﺶ از ﯾﮑﺼﺪ ﻧﻮﯾﺴﻨﺪه ﻣﺘﺨﺼﺺ درﺳﻮﻧﻮﮔﺮاﻓﯽ ﺗﻼش ﮐﺮدهاﻧﺪ ﺗﺎ آﺧﺮﯾﻦ دﺳﺘﺎوردﻫﺎی داﻧﺶ ﺳﻮﻧﻮﮔﺮاﻓﯽ در زﻣﯿﻨﻪ ﺗﺼﻮﯾﺮﺑﺮداری ،ﺗﺸﺨﯿﺺ و ﮐﺎرﺑﺮد آﻧﻬﺎ را ﺑﻪ رﺷـﺘﻪ ﺗﺤﺮﯾـﺮ درآوردهاﻧـﺪ .ﻓﺼـﻮل ﮐﺘـﺎب ﺷـﺎﻣﻞ ﻫﯿﺴﺘﺮوﺳﻮﻧﻮﮔﺮاﻓﯽ ﻻﭘﺎروﺳﮑﻮﭘﯿﮏ ﺳﻮﻧﻮﮔﺮاﻓﯽ و ﺗﮑﻨﯿﮏﻫﺎی ﺑﯿﻮﭘﯽ ﺗﺤﺖ ﻫﺪاﯾﺖ ﺳﻮﻧﻮﮔﺮاﻓﯽ ﻧﯿﺰ ﻣﯽﺑﺎﺷﺪ .در ﮐﻠﯽ %25ﺑﻪ ﺣﺠﻢ ﮐﻠﯽ ﮐﺘﺎب اﻓﺰوده ﺷﺪه اﺳﺖ ﺑﺤﺚ ﻋﻤﺪه اﻓﺰاﯾﺶ ﺣﺠﻢ ﻣﺮﺑﻮط ﺑﻪ ﺳﻮﻧﻮﮔﺮاﻓﯽ زﻧﺎن و زاﯾﻤﺎن ﻣﯽﺑﺎﺷﺪ. ﺗﻌﺪاد زﯾﺎدی از ﺗﺼﺎوﯾﺮ ﺟﺎﯾﮕﺰﯾﻦ ﺷﺪهاﻧﺪ و ﺑﯿﺶ از 450ﺗﺼﻮﯾﺮ ﺗﻤﺎم رﻧﮕﯽ در وﯾﺮاﯾﺶ ﺟﺪﯾﺪ وﺟﻮد دارد .ﺗﻐﯿﯿﺮات ﺟﺪﯾﺪی ﺑﺮای ﺳﻬﻮﻟﺖ ﺧﻮاﻧﺪن و درک ﻣﻄﻠﺐ در ﺳﺎﺧﺘﺎر وﯾﺮاﯾﺶ اﻧﺠﺎم ﺷـﺪه اﺳـﺖ .ﮐﺪﺑﻨـﺪیﻫـﺎی رﻧﮕـﯽ ﻣﻄﺎﻟـﺐ و ﺟﺪاول highlightﺷﺪه ﺑﺮای ﻧﮑﺎت ﮐﻠﯿﺪی ﺗﺸﺨﯿﺼﯽ اﻧﺠﺎم ﺷﺪه اﺳﺖ .ﻣﻄﺎﻟﺐ ﻣﻬﻢﺗﺮ درﺷﺖﺗﺮ ﻧﻮﺷﺘﻪ ﺷﺪهاﻧﺪ و ﻣﺮاﺟﻊ اﺳﺘﻔﺎده ﺷﺪه ﺑﻪ ﺻﻮرت دﻗﯿﻖﺗﺮی ﺑﺎزﻧﻮﯾﺴﯽ ﺷﺪهاﻧﺪ .اﯾﻦ ﮐﺘﺎب در دو ﺟﻠﺪ ﻧﻮﺷﺘﻪ ﺷﺪه اﺳـﺖ .ﺟﻠـﺪ اول ﺷـﺎﻣﻞ ﭘﻨﺞ ﻓﺼﻞ ﻣﯽﺑﺎﺷﺪ ﻓﺼﻞ اول ﺷﺎﻣﻞ ﻓﯿﺰﯾﮏ و اﺛﺮات ﺑﯿﻮﻟﻮژﯾﮏ ﺳﻮﻧﻮﮔﺮاﻓﯽ و ﻣﻮاد ﺣﺎﺟﺐ در ﺳﻮﻧﻮﮔﺮاﻓﯽ ﻣﯽﺑﺎﺷﺪ .ﻓﺼﻞ دوم ﺷﺎﻣﻞ ﺳﻮﻧﻮﮔﺮاﻓﯽ ﺳﻮﻧﻮﮔﺮاﻓﯽ ﺷﮑﻢ و ﻟﮕﻦ ،ﺗﻮراﮐﺲ و روشﻫﺎی ﻣﺪاﺧﻠﻪای ) (interrcntionalﻣﯽﺑﺎﺷـﺪ. ﻓﺼﻞ ﺳﻮم ﺳﻮﻧﻮﮔﺮاﻓﯽ Intraoperativeو ﻻﭘﺎراﺳﮑﻮﭘﯿﮏ را ﺷﺮح ﻣﯽدﻫﺪ ﻓﺼﻞ ﭼﻬﺎرم ﺗﺼﻮﯾﺮﺑﺮداری اﻋﻀﺎء ﮐﻮﭼﮏ ) (small partرا اراﺋﻪ ﻣﯽﮐﻨﺪ .ﮐﻪ ﺷﺎﻣﻞ ﮐﺎروﺗﯿﺪ ،ﺷﺮﯾﺎنﻫﺎ و ورﯾﺪﻫﺎی ﻣﺤﯿﻄﯽ اﺳﺖ .ﺟﻠـﺪ دوم ﮐﺘـﺎب ﺷـﺎﻣﻞ ﻓﺼﻞ ﭘﻨﺠﻢ ﮐﻪ ﺑﺤﺚ ﮐﺎﻣﻞ ﺳﻮﻧﻮﮔﺮاﻓﯽ زﻧﺎن و ﻣﺎﻣﺎﯾﯽ اﺳﺖ و ﻧﻬﺎﯾﺘﺎً ﻓﺼﻞ ﺷﺸﻢ ﺳﻮﻧﻮﮔﺮاﻓﯽ اﻃﻔﺎل اﺳﺖ .ﺑﺨﺶ ﺟﺪﯾﺪ در ﻣﻮرد ﺳﻮﻧﻮﮔﺮاﻓﯽ داﭘﻠﺮ اﻃﻔﺎل و ﺳﻮﻧﻮﮔﺮاﻓﯽ ﻣﺪاﺧﻠﻪای در اﻃﻔﺎل ﺑﻪ اﯾﻦ ﻓﺼﻞ اﻓﺰوده ﺷﺪه اﺳﺖ .ﺧﻮاﻧﺪن اﯾـﻦ ﮐﺘﺎب ﻣﺘﺨﺼﺼﯿﻦ و دﺳﺘﯿﺎران رادﯾﻮﻟﻮژی داﻧﺸﺠﻮﯾﺎن ﭘﺰﺷﮑﯽ و ﺳﻮﻧﻮﮔﺮاﻓﻬﺎ ﺗﻮﺻﯿﻪ ﻣﯽﮔﺮدد.
ﺯﻳﺮ ﭼﺎﭖ
ﺗﻚ ﺟﻠﺪﻱ
)30. Diagnostic Ultrasound (John P. McBany Gorgon, B. Gorgon, MD) (2005
500,000
ﺗﻚ ﺟﻠﺪﻱ
)31. Ultrasound A Practical Approach to Clinical Problems (Edward Bluth, Peter H. Arger Carol B. Benson, Philip W. Rails, Marilyan) (Thieme
800,000
ﺗﻚ ﺟﻠﺪﻱ
)32. Breast Ultrasound (A. Thomas Stavros, MD, FACR) (2004
500,000
ﺗﻚ ﺟﻠﺪﻱ
)33. Musculosceletal Ultrasound (Thomas R. Nelson, Donal B. downey, Dolores H. Pretorius, A aron Fenster
400,000
ﺗﻚ ﺟﻠﺪﻱ
)34. The Core Curriculum Ultrasound (William E. Brant) (Lippincott Williams & Wilkins
800,000
ﺗﻚ ﺟﻠﺪﻱ
2005
35. Ultrasound in Obstetrics and Gynecology (Eberhard Merz) (Thieme) (Vol.1: Obstetrics )36. Color Atlas of Ultrasound Anatomy (B. Block) (Thieme) (2004
450,000 CT 250,000
ﺗﻚ ﺟﻠﺪﻱ
)37. Fundamentals of Body CT (Second Edition) (Webb & Brant & Helms
240,000
ﺗﻚ ﺟﻠﺪﻱ
38. Body CT A Practical Approach
280,000
ﺗﻚ ﺟﻠﺪﻱ
)39. High Resolution CT of the Lung (W. Richard Webb
320,000
ﺗﻚ ﺟﻠﺪﻱ
)40. High Resolution CT of the Chest Comprehensive Atlas (Second Edition) (Eric J. ster, Stephen J. Swensen)(Lippincott Williams&Wilkins
320,000
ﺗﻚ ﺟﻠﺪﻱ
)41. Pediatric Body CT (Marilyn J. Siegel
250,000
ﺗﻚ ﺟﻠﺪﻱ
)42. CT Teaching Manual (Marthias Hofer) (Thieme) (2000
550,000
ﺗﻚ ﺟﻠﺪﻱ
)43. CT Teaching Manual (A Systematic Approach to CT Reading) (Second Edition) (Thieme) (2005
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
77
44. Spiral CT (Eliot K Fishman & R. Brocke Jeffrey)
ﺗﻚ ﺟﻠﺪﻱ
400,000
45. Helical (Spiral) computed Tomography (A Practical Approach to Clinical Protocols) (Paul M. Silverman)
ﺗﻚ ﺟﻠﺪﻱ
250,000
46. Norma findings in CT and MRI (Torsten B. Moeller, EmilReif) (Thieme)
ﺗﻚ ﺟﻠﺪﻱ
300,000
47. CT and MR Imaging of the Whole Body (John R. Haaga, MD) (2003)
ﺩﻭ ﺟﻠﺪﻱ
1,000,000
48. Multidetector CT (Principles, Techniques, & Clinical Applications) (Elliot K. Fissman, R. Brooke Jeffrey, JR.)
ﺗﻚ ﺟﻠﺪﻱ
550,000
49. Spiral and Multislice Computed Tomography of the Body (Aart J. Van der Molen Cornelia M. Schaefer-Prokop) (Thieme) (2003)
ﺗﻚ ﺟﻠﺪﻱ
800,000
50. MRI of the Musculoskeletal System (Thomas H. Berquist)
ﺗﻚ ﺟﻠﺪﻱ
600,000
51. MRI of the Musculoskeletal System MRI Teaching file Series (Karence K Cahn, Mini Pathria)
ﺗﻚ ﺟﻠﺪﻱ
240,000
52. MRI of the Head and Neck MRI Teaching file Series (Jrffrey S. Ross)
ﺗﻚ ﺟﻠﺪﻱ
240,000
53. MRI of the Spine MRI Teaching file Series (Jeffrey S. Ross)
ﺗﻚ ﺟﻠﺪﻱ
240,000
54. MRI of the Brain I & II MRI Teaching file Series (Michel Brant, Zawadzki and…)
ﺩﻭ ﺟﻠﺪﻱ
480,000
55. MRI the basics fray h. Hashemi and William g. bradley, Jr.) (Williams & Wilkins)
ﺗﻚ ﺟﻠﺪﻱ
35,000
56. MRI Principles (Donald G. Mitcell, MD)
ﺗﻚ ﺟﻠﺪﻱ
190,000
57. Clinical Pelvic Imaging CT, Ultrasound, and MRI (Arnold C. Friedman, MD)
ﺗﻚ ﺟﻠﺪﻱ
300,000
58. Magnetic Resonance in Medicine The Basic Textbook of the European Magnetic Resonance Forum (Peter A. Rinck)
ﺗﻚ ﺟﻠﺪﻱ
105,000
59. Magnetic Resonance in diagnosis of C.N.S. disorders (vaso antunavic, gradimir dragutinovic, zvonimir lec) (Thieme)
ﺗﻚ ﺟﻠﺪﻱ
450,000
60. Section and MRI anatomy of the human body (slobodan marinkovic, milan milisavljevic, dieter sehellinger, vaso antunovic) (Thieme)
ﺗﻚ ﺟﻠﺪﻱ
450,000
61. PRACTICAL GUIDE TO ABDOMINAL & PELVIC MRI (JOHN R. LEYENDECHER, JEFFERY J. BROWN)
ﺗﻚ ﺟﻠﺪﻱ
450,000
62. Vascular diagnosis with Ultrasound Clinical References With Case Studies (Hennerici, Neuerburg-Heusler)(Thieme)
ﺗﻚ ﺟﻠﺪﻱ
600,000
63. Introduction to Vascular Ultrasonography (Fourth Edition) (Zwiebel) (James Saunders)
ﺗﻚ ﺟﻠﺪﻱ
600,000
MRI
Doppler
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺭﺍ ﺍﺯ ﻧﻈﺮ ﺩﻭﺭ ﻧﺪﺍﺷﺘﻪ ﻭ ﺍﻳﻦ ﺭﻭﺵ ﺭﺍ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻚ ﺷﻴﻮﻩ ﺁﻟﺘﺮﻧﺎﺗﻴﻮ ﻏﻴﺮﺗﻬﺎﺟﻤﻲ ﻛﺎﺭﺁﻣﺪ ﻣﻮﺭﺩ ﺑﺮﺭﺳﻲ ﻋﺮﻭﻕ ﺑﺪﻥ ﺩﺭ ﻛﻨـﺎﺭ ﺁﻧﮋﻳـﻮﮔﺮﺍﻓﻲ، ﭘﻴﺸﺮﻓﺖﻫﺎﻱ ﺍﺧﻴﺮ ﺩﺭ ﻋﺮﺻﻪ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺷـﺎﻣﻞ ﺳﺮﻓﺼـﻞﻫـﺎﻱ. ﻣﺒﺤﺚ ﺟﺰﺋﻲﺗﺮ( ﺑﻪ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﺁﺧﺮﻳﻦ ﺩﺳﺘﺎﻭﺭﺩﻫﺎﻱ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺩﺭ ﺗﺸﺨﻴﺺ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﺍﺭﮔﺎﻥﻫﺎﻱ ﺑﺪﻥ ﻣﻲﭘﺮﺩﺍﺯﺩ٣١ ﺑﺨﺶ ﺍﺻﻠﻲ )ﻣﺸﺘﻤﻞ ﺑﺮ٥ ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ.ﻗﺮﺍﺭ ﺩﺍﺩﻩ ﺍﺳﺖ :ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ ﻭ ﺗﺠﻬﻴﺰﺍﺕ ﻻﺯﻡB-mode ﻓﻴﺰﻳﻚ ﺩﺍﭘﻠﺮ ﻭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ.٢ ﻧﻜﺎﺕ ﻗﺎﺑﻞ ﺗﻮﺟﻪ ﻫﻤﻮﺩﻳﻨﺎﻣﻴﻚ ﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻋﺮﻭﻕ ﻣﺤﻴﻄﻲ.١ : ﺍﺻﻮﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ-ﺍﻟﻒ ﻣﻮﺍﺩ ﺣﺎﺟﺐ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ.٥ ﻧﻘﺶ ﺩﺍﭘﻠﺮ ﺭﻧﮕﻲ ﺩﺭ ﺗﺸﺨﻴﺺ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﻋﺮﻭﻗﻲ.٤ ﺁﻧﺎﻟﻴﺰ ﻃﻴﻒ )ﻣﻮﺝ( ﻓﺮﻛﺎﻧﺲ ﺩﺍﭘﻠﺮ.٣ ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
78
ﺍﺭﺯﻳﺎﺑﻲ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﭘﻼﻙ ﻛﺎﺭﻭﺗﻴﺪ.٩ ﺷﺮﺍﺋﻴﻦ ﻛﺎﺭﻭﺗﻴﺪ ﻧﺮﻣﺎﻝ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﭘﻠﺮ ﻛﺎﺭﻭﺗﻴﺪ.٨ ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ﻋﺮﻭﻕ ﻣﻐﺰﻱ.٧ ﻣﻘﻴﺎﺱ ﺩﺭ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﻋﺮﻭﻕ ﻣﻐﺰﻱ.٦ : ﻋﺮﻭﻕ ﻣﻐﺰﻱ-ﺏ (TCD) ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺗﺮﺍﻧﺲ ﻛﺮﺍﻧﻴﺎﻝ.١٣ ﺍﺭﺯﻳﺎﺑﻲ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻴﻚ ﻋﺮﻭﻕ ﻭ ﺭﺗﺒﺮﺍﻝ.١٢ ( ﺩﻳﺴﻜﻨﺴﻴﻮﻥ- ﻣﻮﺿﻮﻋﺎﺕ ﻣﺘﻔﺮﻗﻪ ﺑﺎ ﻛﺎﺭﻭﺗﻴﺪ )ﺷﺎﻣﻞ ﺍﺳﺪﺍﺩ.١١ ﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﭘﻠﺮ ﺗﻨﮕﻲ ﻛﺎﺭﻭﺗﻴﺪ.١٠ ﻧﻘﺶﻫﺎﻱ ﻓﻴﺰﻳﻮﻟﻮﮊﻳﻚ ﺟﻬﺖ ﺍﺭﺯﻳﺎﺑﻲ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺮﻳﺎﻧﻲ ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻲ.١٦ ﺁﻧﺎﺗﻮﻣﻲ ﺷﺮﻳﺎﻧﻲ ﺍﻧﺪﺍﻡﻫﺎ.١٥ ﻧﻘﺶ ﺭﻭﺵﻫﺎﻱ ﻏﻴﺮﺗﻬﺎﺟﻤﻲ ﺩﺭ ﭘﻲﮔﻴﺮﻱ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺷﺮﻳﺎﻧﻲ ﺍﻧﺪﺍﻡﻫﺎ.١٤ : ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ-ﺝ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻲ.١٨ ﺍﺭﺯﻳﺎﺑﻲ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ.١٧ ( ﺍﺭﺯﻳﺎﺑﻲ ﻭﺭﻳﺪﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ )ﺟﻨﺒﻪﻫﺎﻱ ﺗﻜﻨﻴﻜﻲ.٢٢ ﺗﺮﻣﻴﻨﻮﻟﻮﮊﻱ ﻭ ﻛﺎﺭﺍﻛﺘﺮﻫﺎﻱ ﻧﺮﻣﺎﻝ.٢١ ﺁﻧﺎﺗﻮﻣﻲ ﻭﺭﻳﺪﻱ ﺍﻧﺪﺍﻡﻫﺎ.٢٠ ﻣﻘﻴﺎﺱ ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺩﺍﭘﻠﺮ ﺩﺭ ﺍﺭﺯﻳﺎﺑﻲ ﻭﺭﻳﺪﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ.١٩ : ﻭﺭﻳﺪﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ-ﺩ ( ﻭ ﭘﺎﻣﻮﻟﻮﮊﻱ ﻏﻴﺮﻭﺭﻳﺪﻱ ﺍﻧﺪﺍﻡAVF) ﻓﻴﺴﺘﻮﻝ ﺷﺮﻳﺎﻧﻲ ﻭﺭﻳﺪﻱ.٢٤ ﺗﺮﻭﻣﺒﻮﺯ ﻭﺭﻳﺪﻱ.٢٣ ﺍﺧﺘﻼﻻﺕ ﻋﺮﻭﻗﻲ ﻛﺒﺪ.٢٩ ﺍﺭﺯﻳﺎﺑﻲ ﺍﻭﻟﺘﺮﺍﺳﻮﻧﻴﻚ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﺣﺸﺎﺋﻲ.٢٨ ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻳﻠﻴﺎﻙ، ﺁﺋﻮﺭﺕ.٢٧ ﺁﻧﺎﺗﻮﻣﻲ ﻭ ﻧﻤﺎﻫﺎﻱ ﻧﺮﻣﺎﻝ ﺳﻮﻧﻮﮔﺮﺍﻓﻴﻚ ﺩﺍﭘﻠﺮ ﻋﺮﻭﻕ ﺷﻜﻤﻲ.٢٦ : ﻋﺮﻭﻕ ﺷﻜﻤﻲ-ه Penis ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﻣﻌﻤﻮﻟﻲ ﻭ ﺩﺍﭘﻠﺮ.٣١ ( ﻭ ﻛﻠﻴﺔ ﭘﻴﻮﻧﺪﻱNative ﺍﺭﺯﻳﺎﺑﻲ ﺩﺍﭘﻠﺮ ﻋﺮﻭﻕ ﻛﻠﻴﻮﻱ )ﻣﺮﺑﻮﻁ ﺑﻪ ﻛﻠﻴﺔ.٣٠ 64. Teaching Manual of Color Duplex Sonography A Wokbook in color duplex ultrasound and echocardiographer (Matthias Hofer) (Thieme) (2005)
ﺗﻚ ﺟﻠﺪﻱ
550,000
65. Vascular Ultrasound of the Neck an Interpretive atlas (Antonio Alayon)(Lippincott Williams & Wilkins)
ﺗﻚ ﺟﻠﺪﻱ
400,000
66. Duplex Scanning in Vascular Disorders (Third Edition) (D. Eugene Strandness, Jr.)
ﺗﻚ ﺟﻠﺪﻱ
600,000
67. Doppler Ultrasound in Gynecology and Obstetrics (Christof Sohn, Hans-Joachim Voigt, Klaus Vetter) (2004)
ﺗﻚ ﺟﻠﺪﻱ
500,000
ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ
500,000
ﺗﻚ ﺟﻠﺪﻱ ﺩﻭ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ
4 00,000
Imaging 68. Skeletal Imaging Atlas of the Spine and Extremities (John A. M. Donald Resnick, MD) 69. Imaging for Surgeons 70. Imaging of the Newborn, Infant and Young Child (Fourth Edition) (Leonard E. Swischuk) (2004) 71. Thoracic Imaging A Practical Approach (Richard H. slone Fernando R. Gutier) 72. Gastrointestinal Imaging, Case Review (Peter J. Feczko, Obert d. Halperi) 73. Imaging in Hepatobiliary and Pancreatic Disease A Practical Clinical Approach (Dirk Van Leeuwen, Jacques Reeders, Joe Ariyama) 74. Aids Imaging A Practical Clinical Approach (J WA J. Reeders, J. R. Mathieson) 75. Special Procedures in diagnostic Imaging (C'lark's)(A. Stewart Whitley, Chrissie W. Alsop Adrin D. Moore) 76. Breast Imaging (Second Edition) (David B. Kopans) 77. The Core curriculum Breast Imaging (Gilda Cardenosa) 78. Neuroimaging I & II (William It. On'ison, jr) 79. Fundamentals of Neuroimaging (William w. Woodruff.M.D.) 80. Magnetic Resonance Imaging computed Tomography of the Head and Spine (C. Barrie Grossman) 81. Atlas of Musculoskeletal Imaging (Thomas Lee Pope, Jr. Stephen Loehr)(Thieme) 82. Atlas of Head and Neck Imaging (The Extracranial Head and Neck) (Suresh K. Mukherji, Vincent chong) 83. Magnetic Resonance Imaging of Orthopeadic Trauma (Stephen J. Eustace)(Lippincott Williams & Wilkins) ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
90,000 600,000 250,000 250,000 500,000 420,000 350,000 500,000 900,000 360,000 400,000 420,000 500,000 250,000
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
79
)84. Pediatric Gastrointestinal Imaging and Intervention (David A. Stringer-Paul S. Babyn MDCM
500,000
ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ ﺗﻚ ﺟﻠﺪﻱ
87. Clinical Imaging
1,100 ,000
ﺗﻚ ﺟﻠﺪﻱ
)88. Diagnostic Imaging Brain (Osborn) (2004
900,000
ﺗﻚ ﺟﻠﺪﻱ
1,000 ,000
ﺗﻚ ﺟﻠﺪﻱ
)90. Diagnostic Imaging Head and Neck (Harnsberger) (2004
1,350 ,000
ﺗﻚ ﺟﻠﺪﻱ
)91. Cranial Neuroimaging and Clinical Neuroanatomy Atlas of MR Imaging and Computed Tomography (Hans-Joachim Kretschmann
450,000
ﺗﻚ ﺟﻠﺪﻱ
)92. DIAGNOSTIC MUSCULOSKELETAL IMAGING (THEODORE T. MILLER, MARK E. SCHWEITZER) (2005
700,000
ﺗﻚ ﺟﻠﺪﻱ
)93. Orthopedic IMAGING (A Pracitcal Approach) (ADAM GREENSPAN) (Michael W. Chapman) (2004
250,000
ﺗﻚ ﺟﻠﺪﻱ
)94. Aids to RADIOLOCIAL DIFFERENTIAL DIAGNOSIS (Forth Edition) (Stephen Chapman and Richard Nakielny) (2003
260,000 500,000 580,000
)85. Modern Head and Neck Imaging Medical Radiology, Diolopy, Nostic Imaging (S. K. Mukhetji, J. A. castelijins)(Springer )86. Variants and Pitfalls in Body Imaging (Ali Shirkhoda)(Lippincot Williams & Wilkin's
ﻣﺪﺕ ﻃﻮﻻﻧﻲ ﺑﻮﺩ ﻛﻪ ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎ ،ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻳﺴﺖﻫﺎ ،ﻧﻮﺭﻭﭘﺎﺗﻮﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﺟﺮﺍﺣﺎﻥ ﺍﻋﺼﺎﺏ ﻣﻨﺘﻈﺮ ﻛﺘﺎﺏ ﺟﺪﻳﺪﻱ ﺍﺯ ﺩﻛﺘﺮ " "Ann Osbornﺑﻮﺩﻧﺪ .ﺍﻳﻦ ﻛﺎﺭ ﺟﺪﻳﺪ ﻧﻤﺎﻳﺎﻧﮕﺮﻱ ﺍﺯ ﻛﺘﺐ ﻣﺮﺟﻊ ﺩﺭ ﻗﺮﻥ ٢١ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺩﻳﮕﺮ ﻣﺎﻧﻨﺪ ﻛﺘﺎﺏﻫﺎﻱ ﻗﺪﻳﻤﻲﺗﺮ ﺍﻃﻼﻋﺎﺕ ﺑﺴﻴﺎﺭ ﺯﻳﺎﺩ ﺭﺍ ﺑﻪ ﺻﻮﺭﺕ ﻓﺸﺮﺩﻩ ﻭ ﺑﺎ ﺗﺼﺎﻭﻳﺮ ﺍﻧﺪﻙ ﺍﺭﺍﺋﻪ ﻧﻤﻲﺩﻫﺪ ﺑﻠﻜﻪ ﺑﺎ formatﻣﺪﺭﻥ ﻭ ﭘﻴﺸﺮﻓﺘﻪ ﺧﻮﺩ ﺩﻭ ﺑﺮﺍﺑﺮ ﺍﻃﻼﻋﺎﺕ ﻭ ﭼﻬﺎﺭ ﺑﺮﺍﺑﺮ ﺗﺼﺎﻭﻳﺮ ﺑﻴﺸﺘﺮﻱ ﺑﺮﺍﻱ ﻫﺮ ﺗﺸﺨﻴﺺ ﺩﺍﺭﺩ .ﻛﻴﻔﻴﺖ ﺗﺼﺎﻭﻳﺮ ﻭ ﮔﺮﺍﻓﻴـﻚﻫـﺎ ﻭﺍﻗﻌـﹰﺎ ﻋﺎﻟﻴﺴـﺖ ﻭ ﺟﻬﺖ ﺑﻬﺘﺮﻧﺸﺎﻥﺩﺍﺩﻥ ﺗﺼﺎﻭﻳﺮ ﺁﻧﺎﺗﻮﻣﻴﻚ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻳﻚ ﺍﺳﺘﻔﺎﺩﺓ ﺯﻳﺎﺩﻱ ﺍﺯ ﺭﻧﮓﻫﺎ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺑﺘﻜﺎﺭ ﺩﻳﮕﺮ ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﻳﻦ ﺍﺳﺖ ﻛﻪ ﻣﻮﺍﺭﺩ ﻭ ﺗﺼﺎﻭﻳﺮ ﻣﺸﺎﺑﻪ ﻭ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻕ ﺭﺍ ﺩﺭ ﻫﻤﺎﻥ ﻓﺼﻞ ﺟﻬﺖ ﺑﺮﺭﺳﻲ ﺑﻴﺸﺘﺮ ﺍﺭﺍﺋﻪ ﻧﻤﻮﺩﻩ ﺍﺳﺖ .ﺷﺎﻳﺪ ﺑﺘـﻮﺍﻥ ﮔﻔﺖ ﻛﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﻳﻚﺟﻠﺪﻱ "ﺍﻳﻨﺘﺮﻧﺖ" ﻧﻮﺭﻭﻟﻮﮊﻱ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ CNSﻣﻲﺑﺎﺷﺪ :ﻛﺎﻣﻞ ،ﻣﻮﺟﺮ ﻭ ﺑﺮﻭﺯ ﺑﻄﻮﺭﻳﻜﻪ ﺣﺘﻲ ﻛﻠﻤﻪﺍﻱ ﺭﺍ ﻧﻤﻲﺗﻮﺍﻥ ﻳﺎﻓﺖ ﻛﻪ ﺍﺿﺎﻓﻲ ﻧﮕﺎﺷﺘﻪ ﺷﺪﻩ ﺑﺎﺷﺪ. PART I (Pathology-based diagnoses): Congenital malformations-Trauma Sulianachnoid hemorrhage and Aneurisms-Stroke-Vascular Malformations Neoplasm's and Tumor in lesions-Primary Non-neoplastic cystsInfection and Demyelinating Disease-Metabolic/Degenerative Disorders, Inhenited-Toxic/Metabolic/Degenesative Disorders, Acquired PART II (Anatomy-based Diagnoses): Ventricles and Cysterns-Sella and Pitutary-CPA-IAC-Skull, Scalp and Meninges
ﺗﻮﺿﻴﺤﺎﺕ ﺍﺭﺍﺋﻪﺷﺪﻩ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﺑﻴﻤﺎﺭﻱ ﺷﺎﻣﻞ ﻋﻨﺎﻭﻳﻦ ﺯﻳﺮ ﻣﻲﺑﺎﺷﺪ: Terminology-Imaging Findings-Differentioal Diagnosis-Pathology Clinical Issues-Selected references-Imaging Gallery-Key Facts
ﻫﺮ ﺟﺎﻳﻲ ﻛﻪ ﻻﺯﻡ ﺑﻮﺩﻩ ﺍﺳﺖ ﺗﻮﺿﻴﺤﺎﺕ ﺿﺮﻭﺭﻱ ﺍﺯ ﺁﻧﺎﺗﻮﻣﻲ ،ﺟﻨﻴﻦﺷﻨﺎﺳﻲ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺗﺎ ﺑﻪ ﺧﻮﺍﻧﻨﺪﻩ ﺩﺭﻙ ﺗﺸﺨﻴﺺ ﻭ ﻣﻮﻗﻌﻴﺖ ﻛﻤﻚ ﻧﻤﺎﻳﺪ .ﻗﺴﻤﺖ Key Factsﺧﻼﺻﻪﺍﻱ ﺟﺎﻣﻊ ﺑﺮﺍﻱ ﻣﺮﻭﺭ ﺳﺮﻳﻊ ﻭ ﺁﺳﺎﻥ ﻣﻲﺑﺎﺷﺪ. ﺑﻪ ﻧﻈﺮ ﻣﻲﺭﺳﺪ ﻛﻪ ﻛﺘﺎﺏ " "Diagnostic Imaging Brain Osborn 2004ﻣﻨﺒﻊ ﺑﺴﻴﺎﺭ ﻏﻨﻲ ﻭ ﻣﺆﺛﺮ ﺍﺯ ﻣﻄﺎﻟﺐ ﻋﻠﻤﻲ ﺟﺪﻳﺪ ﺑـﺮﺍﻱ ﺩﺍﻧﺸـﺠﻮﻳﺎﻥ- ﺭﺯﻳﺪﻧﺖﻫﺎ ﻭ ﻣﺘﺨﺼﺼﻴﻦ ﺭﺷﺘﻪﻫﺎﻱ ﻣﺮﺑﻮﻃﻪ ﺍﻋﻢ ﺍﺯ ﻧﻮﺭﻭﻟﻮﮊﻱ ،ﺟﺮﺍﺣﻲ ﺍﻋﺼﺎﺏ ،ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱ ﺑﺎﺷﺪ.
)(Stoller.Tirman Bredella) (2004
89. Diagnostic Imaging Orthopaedics
ﺍﻳﻦ ﻛﺘﺎﺏ ﭼﺎﭖ ﺳﻮﻡ ﻛﺘﺎﺏ Cranial Neuroimaging and Clinical Neuroanatomyﺩﺭ ﺳﺎﻝ 2004ﻣﻲﺑﺎﺷﺪ .ﺗﻤﺎﻣﻲ ﻓﺼﻮﻝ ﻛﺘﺎﺏ ﺗﻐﻴﻴﺮ ﻭ ﺑﺎﺯﻧﻮﻳﺴﻲ ﺷﺪﻩ ﺍﺳﺖ .ﺑﻲﮔﻤﺎﻥ ﺑﻪ ﻋﻨﻮﺍﻥ ﻳﻲ ﺍﺯ ﺑﻬﺘﺮﻳﻦ ﻣﻨﺎﺑﻊ ﺑﺮﺍﻱ ﻓﻬـﻢ ﻭ ﺩﺭﻙ ﺁﻧـﺎﺗﻮﻣﻲ ﻣﺴـﻴﺮﻫﺎﻱ ﻋﺼﺒﻲ ﻭ ﺳﺎﺧﺘﻤﺎﻥﻫﺎﻱ ﻋﺮﻭﻗﻲ ﻣﻲﺑﺎﺷﺪ .ﺗﺼﺎﻭﻳﺮ ﺑﺰﺭﮒ ﻭ ﺻﻔﺤﻪﺁﺭﺍﻳﻲ ﺧﻮﺏ ﺁﻥ ﺍﺟﺎﺯﻩ ﺍﺳﺘﻔﺎﺩﻩ ﺁﺳﺎﻥ ﻭ ﺩﺳﺘﺮﺳﻲ ﺳﺮﻳﻊ ﺭﺍ ﻣﻴﺴﺮ ﻣﻲﺳﺎﺯﺩ. ﻣﻘﺪﻣﻪ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﺑﺤﺚ ﮔﺴﺘﺮﺩﻩﺍﻱ ﺩﺭ ﻣﻮﺭﺩ ﺁﺯﻣﻮﻥﻫﺎﻱ ﻧﻮﺭﻭﻟﻮﮊﻱ ﻭ ﺍﻧﺪﻳﻜﺎﺳﻴﻮﻥﻫﺎﻱ ﺁﻧﻬﺎﺳﺖ .ﻭ ﺭﺍﻫﻨﻤﺎﻱ ﺧﻮﺑﻲ ﺑﺮﺍﻱ ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﺟﻬﺖ ﺍﺳﺘﻔﺎﺩﻩ ﺻﺤﻴﺢ ﻭ ﺑﺠﺎ ﺍﺯ ﺁﺯﻣﻮﻥﻫﺎﻱ ﻋﺼﺒﻲ ﻣﻲﺑﺎﺷﺪ. ﭼﺎﭖ ﺟﺪﻳﺪ ﻛﺘﺎﺏ ﺣﺎﻭﻱ ﺗﺼﺎﻭﻳﺮ ﺟﺪﻳﺪ ﺩﺭ ﻣﻮﺭﺩ ﺳﺎﺧﺘﻤﺎﻥﻫﺎﻱ ﻋﺮﻭﻗﻲ ﺣﻔﺮﻩ ﺣﻠﻘﻲ ﺍﺳﺖ .ﮔﺴﺘﺮﺵ ﺳﺮﻳﻊ MRIﻭ ﺗﺼﺎﻭﻳﺮ NeuroFunctionalﻧﻴﺎﺯ ﺑﻴﺸﺘﺮ ﺑﻪ ﺍﻳﻦ ﻧﻮﻉ ﺑﺤﺚﻫﺎﻱ ﻛﺎﺭﺑﺮﺩﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺭﺍ ﺩﺍﺭﺩ ﺑـﺎ ﻣﺮﺍﺟﻌـﻪ ﺑـﻪ ﺍﻳـﻦ ﻛﺘـﺎﺏ ﻣـﻲﺗـﻮﺍﻥ ﺍﺯ ﺳﺎﺧﺘﻤﺎﻥﻫﺎﻱ ﺩﻗﻴﻖ ﻋﺮﻭﻕ ﺗﺮ ﻣﺴﻴﺮﻫﺎﻱ ﺍﻟﻴﺎﻑ ﻋﺼﺒﻲ ﻭ ﻣﺴﻴﺮ ﺍﻋﺼﺎﺏ ﻛﺮﺍﻧﻴﺎﻝ ﺁﮔﺎﻫﻲ ﻳﺎﻓﺖ ﻭ ﻋﻼﻳﻢ ﺑﺎﻟﻴﻨﻲ ﺑﺴﻴﺎﺭﻱ ﺭﺍ ﺑﺎ ﻳﺎﻓﺘﻪﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﻄﺎﺑﻘﺖ ﺩﺍﺩ .ﺗﺼﺎﻭﻳﺮ ﺳﻲﺗﻲﺍﺳﻜﻦ ﻭ MRIﺩﺭ ﻣﻘﺎﻃﻊ ﻛﺮﻭﻧﺎﻝ ،ﺍﮔﺰﻳﺎﻝ ،ﺳﺎﮊﻳﺘﺎﻝ ﺑﻪ ﻧﻤﺎﻳﺶ ﮔﺬﺍﺷﺘﻪ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﺑﺎ ﻛﺪﺑﻨﺪﻱ ﺭﻧﮕﻲ ﻭ ﺩﻳﺎﮔﺮﺍﻡﻫﺎﻱ ﺷﻤﺎﺗﻴﻚ ﻣﻄﺎﺑﻘﺖ ﺩﺍﺩﻩ ﺷﺪﻩ ﺍﺳﺖ .ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺗﻤﺎﻣﻲ ﻣﺘﺨﺼﺼﻴﻦ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ،ﻧﻮﺭﻭﻟﻮﮊﻳﺴﺖﻫﺎ ﻭ ﺟﺮﺍﺣﺎﻥ ﺍﻋﺼﺎﺏ ﺗﻮﺻﻴﻪ ﻣﻲﮔﺮﺩﺩ.
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
80
95. Teaching Atlas of Brain Imaging (Nancy J. Fischbein, William P. Dillon, A. James Barkovich)
ﺗﻚ ﺟﻠﺪﻱ
500,000
96. The Radiologic Clinics of North America Imaging of Obstructive Pulmonary Disease (W. Richard Webb.M.D.)
ﺗﻚ ﺟﻠﺪﻱ
150,000
97. The Radiologic Clinics of North America Neonatal Imaging (Janet L. ST. Rife, M.D.)
ﺗﻚ ﺟﻠﺪﻱ
115,000
98. The Radiologic Clinics of North America Lung Cancer (Claudia I. Henschke. Phil, M.D.)
ﺗﻚ ﺟﻠﺪﻱ
140,000
99. The Radiologic Clinics of North America Interventional Procedures in Musculoskeletal Radio I Interventional Techniques (Jamshid Tehranzadeh, MD)
ﺗﻚ ﺟﻠﺪﻱ
100,000
100. The Radiologic Clinics of North America Interventional Procedures in Musculoskeletal Radio II Advanced Arthrography (Jamshid Tehranzadeh)
ﺗﻚ ﺟﻠﺪﻱ
200,000
101. The Radiologic Clinics of North America Advances in Emergency Radiology I & II (Robert A. Novell)
ﺩﻭ ﺟﻠﺪﻱ
120,000
102. The Radiologic Clinics of North America Cardiac Radiology (Lawrence M. Boxt. MD)
ﺗﻚ ﺟﻠﺪﻱ
150,000
103. The Radiologic Clinics of North America Interventional Chest Radiology (Jeffrey S. Klein, M.D.)
ﺗﻚ ﺟﻠﺪﻱ
150,000
The Radiologic Clinics of North America
Imaging of the newborn, infant, and young child
(LEONARD E. SWISCHUK, M. D.) (FIFTH EDITION)
Borderlands of Normal and Early Pathological Finding in Skeletal Radiography (Juergen Freyschmidt, Joachim Brossmann, Juergen Wiens, Andreas Sternberg)
Clinical Imaging
(Ronald L. Eisenberg, Amelda County
(Fifth revised edition)
(Thieme)
)ﺭﺋﻴﺲ ﺩﭘﺎﺭﺗﻤﺎﻥ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻛﻠﻴﻨﻴﻜﺎﻝ
(an atlas of differential diagnosis) (Lippincott Williums & Wilkins)
(2004)
(Forth Edition)
ﺭﻳﺎﻝ600,000 :ﻗﻴﻤﺖ
(2003)
ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﻣﺒﺎﺣﺚ ﻻﺯﻡ ﻭ ﺩﺭ ﻋﻴﻦ ﺣﺎﻝ ﻛﺎﻣﻞ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﻧﻤﺎﻫﺎﻱ ﮔﻮﻧﺎﮔﻮﻥ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻣﻲﺑﺎﺷﺪ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻣﺨﺘﻠﻒ ﻣﺮﺑﻮﻁ ﺑﻪ ﻫﺮ ﻧﻤﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴـﻚ )ﺑﻌﻨـﻮﺍﻥ ﺍﻳـﻦ ﻛﺘـﺎﺏ ﺗﻘﺮﻳﺒـﹰﺎ ﺷـﺎﻣﻞ.( ﺗﺼﺎﻭﻳﺮ ﻣﺮﺗﺒﻂ ﺑﻪ ﻫﺮ ﺗﺸﺨﻴﺺ ﺍﻓﺘﺮﺍﻗﻲ ﺭﺍ ﺑﻄﻮﺭ ﺟﺪﺍﮔﺎﻧﻪ ﺑﻪ ﻧﻤﺎﻳﺶ ﺩﺭﺁﻣﺪﻩ ﻭ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻛﺪﺍﻡ ﻧﻴﺰ ﺗﻮﺿﻴﺤﺎﺕ ﻻﺯﻡ ﺑﺎ ﻧﮕﺎﺭﺷﻲ ﺑﺴـﻴﺎﺭ ﻗﺎﺑـﻞ ﻓﻬـﻢ ﺫﻛـﺮ ﮔﺮﺩﻳـﺪﻩ ﺍﺳـﺖmultiple Pulmonary nodules ﻼ ﻣﺜ ﹰ .( ﺩﺭ ﺁﻥ ﻟﺤﺎﻅ ﺷﺪﻩ ﺍﺳﺖ... ﻭMRI ، CTScan ، ﺳﻮﻧﻮﮔﺮﺍﻓﻲ، ﻣﻄﺎﻟﻌﺎﺕ ﺑﺎ ﻛﻨﺘﺮﺍﺳﺖ، Plain film )ﺍﺯ ﻗﺒﻴﻞImaging ﺗﺸﺨﻴﺺﻫﺎﻱ ﺍﻓﺘﺮﺍﻗﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻛﻞ ﺑﺪﻥ ﺑﻮﺩﻩ ﻭ ﺗﻜﻨﻴﻚﻫﺎﻱ ﻣﺨﺘﻠﻒ
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
81
ﻓﻬﺮﺳﺖ ﻛﻠﻲ ﻣﺮﺑﻮﻁ ﺑﻪ ﻓﺼﻮﻝ ﻣﺨﺘﻠﻒ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﻪ ﺷﺮﺡ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ: -١ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ Chest
-٦ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
-٢ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ
-٧ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺟﻤﺠﻤﻪ
-٣ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ -٨ Gastrointestinalﺑﻴﻤﺎﺭﻱﻫﺎﻱ Breastﻭ ﻣﺎﻣﻮﮔﺮﺍﻓﻲ -٤ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ Genitourinary
-٩ﺳﻮﻧﻮﮔﺮﺍﻓﻲ ﺟﻨﻴﻦ
-٥ﺍﻟﮕﻮﻫﺎﻱ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺍﺳﻜﺘﺎﻝ
ﺿﻤﻨﹰﺎ ﺩﺭ ﻣﻮﺭﺩ ﻫﺮ ﻛﺪﺍﻡ ﺍﺯ ﻓﺼﻞﻫﺎﻱ ﻓﻮﻕﺍﻟﺬﻛﺮ ،ﺩﺭ ﺍﺑﺘﺪﺍﻱ ﻫﺮ ﻓﺼﻞ ،ﻓﻬﺮﺳﺖ ﻛﺪﺩﺍﺭ ﻭﻳﮋﻩﺍﻱ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ ﻧﺸﺎﻧﻪﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﻣﺮﺑﻮﻁ ﺑﻪ ﻣﺒﺤﺚ ﻣﺬﻛﻮﺭ ﺁﻭﺭﺩﻩ ﺷﺪﻩ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﺗﺴﻬﻴﻞ ﻭ ﺗﺴﺮﻳﻊ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺴـﻴﺎﺭ ﻣـﺆﺛﺮ ﺧﻮﺍﻫـﺪ ﺑـﻮﺩ. ﻣﻄﺎﻟﻌﻪ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺭﺯﺷﻤﻨﺪ ﺑﺮﺍﻱ ﺷﺮﻛﺖ ﺩﺭ ﺍﻣﺘﺤﺎﻧﺎﻥ ﺑﺮﺩ ﺗﺨﺼﺺ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﻫﻤﭽﻨﻴﻦ ﻛﺎﺭ ﻋﻤﻠﻲ ﺩﺭ ﻣﺆﺳﺴﺎﺕ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺑﺴﻴﺎﺭ ﻣﻔﻴﺪ ﺧﻮﺍﻫﺪ ﺑﻮﺩ. ﺗﻌﺪﺍﺩ ﺻﻔﺤﺎﺕ
1307
)(Seventh Edition
)(Mosby Inc.) (2001 ﻗﻴﻤﺖ 700,000 :ﺭﻳﺎﻝ
Atlas Of Normal Roentgen Variants that may Simulate Disease )ﺩﺍﻧﺸﻴﺎﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ﻭﻳﺮﺟﻴﻨﻴﺎ , Mark W. Anderson M.d.ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ﻭﻳﺮﺟﻴﻨﻴﺎ
(Theodore E. Keats M.D.
ﺩﺭ ﺍﻳﻦ ﻛﺘﺎﺏ ،ﺑﺎ ﻛﻤﻚ ﺗﺼﺎﻭﻳﺮ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﻣﺘﻌﺪﺩ ،ﺑﺎ ﻧﻤﺎﻫﺎﻱ ﻣﺨﺘﻠﻒ ﻭﺍﺭﻳﺎﺳﻴﻮﻥﻫﺎﻱ ﻧﺮﻣﺎﻝ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺁﺷﻨﺎ ﻣﻲﺷﻮﻳﻢ ﻭ ﺑﺪﻳﻦ ﻃﺮﻳﻖ ﺍﺯ ﻣﻴﺰﺍﻥ Over diagnosisﻛﻪ ﻣﻤﻜﻦ ﺍﺳﺖ ﺩﺭ ﺟﺮﻳﺎﻥ ﮔﺰﺍﺭﺷﺎﺕ ﺭﺍﺩﻳﻮﻟﻮﮊﻳﻚ ﺍﺗﻔﺎﻕ ﺑﻴﺎﻓﺘﺪ ،ﻛﺎﺳـﺘﻪ ﺧﻮﺍﻫـﺪ ﺷﺪ. ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﺩﻭ ﺑﺨﺶ ﺍﺻﻠﻲ ﻣﻲﺑﺎﺷﺪ .ﺑﺨﺶ ﺍﻭﻝ ﻣﺮﺑﻮﻁ ﺑﻪ ﻭﺍﺭﻳﺎﺳﻴﻨﻮﺱﻫﺎﻱ ﻧﺮﻣﺎﻝ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺍﺳﺘﺨﻮﺍﻥﻫﺎ ﻭ ﺑﺨﺶ ﺩﻭﻡ ﻣﺮﺑﻮﻁ ﺑﻪ ﻭﺍﺭﻳﺎﺳﻴﻨﻮﺱﻫﺎﻱ ﻧﺮﻣﺎﻝ ﺭﺍﺩﻳﻮﮔﺮﺍﻓﻴﻚ ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﻣﻲﺑﺎﺷﺪ .ﺑﺨـﺶ ﺍﻭﻝ ﻭ ﺩﻭﻡ ﺷـﺎﻣﻞ ﻓﺼـﻮﻝ ﺫﻳـﻞ ﻣﻲﺑﺎﺷﻨﺪ: ﺑﺨﺶ ﺍﻭﻝ ﻓﺼﻞ -١ﺟﻤﺠﻤﻪ ﻓﺼﻞ -٢ﺍﺳﺘﺨﻮﺍﻥﻫﺎﻱ ﺻﻮﺭﺕ ﻓﺼﻞ -٣ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻓﺼﻞ -٤ﻛﻤﺮﺑﻨﺪ ﻟﮕﻨﻲ
ﺑﺨﺶ ﺩﻭﻡ
ﻓﺼﻞ -٥ﻛﻤﺮﺑﻨﺪ ﺷﺎﻧﻪﺍﻱ ﻭ ﻗﻔﺴﺔ ﺻﺪﺭﻱ ﻓﺼﻞ -٦ﺍﻧﺪﺍﻡ ﻓﻮﻗﺎﻧﻲ ﻓﺼﻞ -٧ﺍﻧﺪﺍﻡ ﺗﺤﺘﺎﻧﻲ
ﻗﻴﻤﺖ 500,000 :ﺭﻳﺎﻝ
ﻓﺼﻞ -٨ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﮔﺮﺩﻥ ﻓﺼﻞ -٩ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﻗﻔﺴﺔ ﺳﻴﻨﻪ ﻓﺼﻞ -١٠ﺩﻳﺎﻓﺮﺍﮔﻢ
ﺗﻌﺪﺍﺩ ﺻﻔﺤﺎﺕ:
478
)ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ Leuvenﺑﻠﮋﻳﻚ
ﻓﺼﻞ -١١ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﺷﻜﻢ ﻓﺼﻞ -١٢ﺑﺎﻓﺖﻫﺎﻱ ﻧﺮﻡ ﻟﮕﻦ ﻓﺼﻞ -١٣ﺳﻴﺴﺘﻢ ﺍﺩﺭﺍﺭﻱ ﺗﻨﺎﺳﻠﻲ
)(Springer) (2003
Magnetic Resonance Angiography
, Guy Marchal, PhD, M.D.ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ ﺍﺷﺘﺮﺕ ﮔﺎﺭﺩ ﺁﻟﻤﺎﻥ (Ingolf P. Arlart, Phd, M.D.
ﺑﺎ ﺗﻮﺟﻪ ﺑﻪ ﮔﺮﺍﻳﺶ ﺭﻭﺯﺍﻓﺰﻭﻥ ﺑﻪ ﻏﻴﺮﺗﻬﺎﺟﻤﻲﺷﺪﻥ ﺭﻭﺵﻫﺎﻱ ﺗﺸﺨﻴﺼﻲ ﭘﺰﺷﻜﻲ ﻧﻴﺎﺯ ﺑﻪ ﺩﺍﻧﺴﺘﻦ ﺗﻜﻨﻴﻚﻫﺎ ﻭ ﻫﻤﭽﻨﻴﻦ ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺑﺎ ﻛﻤﻚ ﺭﺯﻭﻧﺎﻧﺲ ﻣﻐﻨﺎﻃﻴﺴﻲ ) (MRAﺑﻴﺶ ﺍﺯ ﭘﻴﺶ ﺍﺣﺴﺎﺱ ﻣﻲﺷﻮﺩ ﻭ ﻫﺪﻑ ﺍﺻﻠﻲ ﺍﻳﻦ ﻛﺘـﺎﺏ ﻧﻴـﺰ ﺁﺷﻨﺎﻳﻲ ﺑﺎ ﺍﺻﻮﻝ ﻭ ﻣﻼﺣﻈﺎﺕ ﺗﻜﻨﻴﻜﻲ MRAﻭ ﻫﻤﭽﻨﻴﻦ ﻛﺎﺭﺑﺮﺩﻫﺎﻱ ﺑﺎﻟﻴﻨﻲ ﺍﻳﻦ ﺭﻭﺵ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺗﺸﺨﻴﺼﻲ ﻣﻲﺑﺎﺷﺪ. ﻓﺼﻮﻝ ﻋﻤﺪﺓ ﺍﻳﻦ ﻛﺘﺎﺏ ﻋﺒﺎﺭﺗﻨﺪ ﺍﺯ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
82 -١ﺳﻴﺴﺘﻢ ﻋﺮﻭﻗﻲ :ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ﻭ ﭘﺎﺗﻮﻟﻮﮊﻱﻫﺎﻱ ﻋﺮﻭﻗﻲ ﻭ ﺍﺻﻮﻝ ﻫﻤﻮﺩﻳﻨﺎﻣﻴﻚ
-٩ﺗﻜﻨﻴﻚﻫﺎﻱ ﻧﻤﺎﻳﺶ ﺗﺼﻮﻳﺮ
-١٧ﻋﺮﻭﻕ ﺭﻳﻮﻱ
-٢ﺗﻌﺮﻳﻒ ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺭﺯﻭﻧﺎﻧﺲ ﻣﻐﻨﺎﻃﻴﺴﻲ )(MRA
-١٠ﻛﻤﻴﺖ ﺟﺮﻳﺎﻥ ﺧﻮﻥ
-١٨ﺁﺋﻮﺭﺕ ﺷﻜﻤﻲ ﻭ ﺷﺎﺧﻪﻫﺎﻱ ﺁﻥ
-٣ﺍﺻﻮﻝ ﭘﺎﻳﻪ ﺭﺯﻭﻧﺎﻧﺲ ﻣﻐﻨﺎﻃﻴﺴﻲ ﻫﺴﺘﻪﺍﻱ ) (NMRﺟﻬﺖ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﭘﺰﺷﻜﻲ
-١١ﺗﺸﺮﻳﺢ ﻧﻤﺎﻳﺸﻲ ﺳﺨﺖﺍﻓﺰﺍﺭ
-١٩ﺷﺮﻳﺎﻥﻫﺎﻱ ﺍﻧﺪﺍﻡﻫﺎ
-٤ﻓﻀﺎﻱ Kﻭ Resolution
-١٢ﺁﺭﺗﻴﻔﻜﺖﻫﺎ ﻭ ﻣﺤﺪﻭﺩﻳﺖﻫﺎ
-٢٠ﻭﺭﻳﺪﻫﺎﻱ ﺑﺰﺭﮒ ﺑﺪﻥ ﻭ ﺍﻧﺪﺍﻡﻫﺎ
-٥ﺗﻜﻨﻴﻚﻫﺎﻱ Acquistionﻭﺍﺑﺴﺘﻪ ﺑﻪ ﺟﺮﻳﺎﻥ
-١٣ﻋﺮﻭﻕ ﺩﺍﺧﻞ ﺟﻤﺠﻤﻪ
-٢١ﺳﻴﺴﺘﻢ ﻭﺭﻳﺪﻱ ﺍﺳﭙﻠﻨﻮﭘﻮﺭﺗﺎﻝ
-٦ﺗﻜﻨﻴﻚﻫﺎﻱ Acquistionﻣﺴﺘﻘﻞ ﺍﺯ ﺟﺮﻳﺎﻥ
-١٤ﺷﺮﻳﺎﻥﻫﺎﻱ ﻛﺎﺭﻭﺗﻴﺪ ﻭ ﻭﺭﺗﺒﺮﺍﻝ
-٢٢ﺍﺭﺍﺋﺔ ﺭﺍﻫﻨﻤﺎ ) (Guideﺟﻬﺖ ﺭﻭﺵﻫﺎﻱ ﺩﺭﻣﺎﻧﻲ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ
Resolution -٧ﻓﻀﺎﻳﻲ ﺩﺭ ﻣﻘﺎﺑﻞ Resolutionﺯﻣﺎﻧﻲ ﺩﺭ MRAﺑﺎ ﺗﺸﺪﻳﺪ ﻛﻨﺘﺮﺍﺳﺖ
-١٥ﺁﺋﻮﺭﺕ ﺷﻜﻤﻲ ﻭ ﺷﺎﺧﻪﻫﺎﻱ ﺁﻥ
Implant -٢٣ﻫﺎﻱ ﺩﺍﺧﻞ ﻋﺮﻭﻗﻲ :ﺍﻳﻤﻨﻲ ﻭ ﺁﺭﺗﻴﻔﻜﺖﻫﺎ
-٨ﻣﺎﺩﻩ ﺣﺎﺟﺐ ﺩﺭ MRA
-١٦ﺷﺮﻳﺎﻥﻫﺎﻱ ﻛﻮﺭﻭﻧﺎﺭﻱ
)ﺗﻌﺪﺍﺩ ﺻﻔﺤﺎﺕ] 2272 :ﺩﻭﺟﻠﺪﻱ[ (
)CT and MR Imaging of the Whole Body (Mosby) (2003
ﭘﺮﻭﻓﺴﻮﺭ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﻭ ﺟﺮﺍﺣﻲ ﺍﻋﺼﺎﺏ ﺩﺍﻧﺸﮕﺎﻩ Clevelandﺍﻭﻫﺎﻳﻮ )(Charles F. Lanzieri, MD, FACR
ﺭﻳﺎﺳﺖ ﺩﭘﺎﺭﺗﻤﺎﻥ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺩﺍﻧﺸﮕﺎﻩ Clevelandﺍﻭﻫﺎﻳﻮ )(John R. Haaga, MD , FACR
ﺍﺳﺘﺎﺩ ﺑﺨﺶﻫﺎﻱ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ Thoracic , Headﺩﺍﻧﺸﮕﺎﻩ Case Western Reserveﺷﻬﺮ Clevelandﺍﻭﻫﺎﻳﻮ )(Robert C. Gilkeson, MD
ﻗﻴﻤﺖ 1000,000 :ﺭﻳﺎﻝ
ﺍﻳﻦ ﻛﺘﺎﺏ ﻳﻜﻲ ﺍﺯ ﻛﺎﻣﻠﺘﺮﻳﻦ ﻣﺮﺍﺟﻊ ﺩﺭ ﺍﺭﺗﺒﺎﻁ ﺑﺎ MRI ,CT Scanﺑﻮﺩﻩ ﻭ ﺩﺭ ﺁﻥ ﺿﻤﻦ ﺑﺤﺚ ﻛﺎﻣﻞ ﻭ ﺩﻗﻴﻖ ﺩﺭ ﻣﻮﺭﺩ ﭘﺎﺗﻮﻟﻮﮊﻱ ﻭ ﻫﻤﭽﻨﻴﻦ ﻳﺎﻓﺘﻪﻫﺎﻱ Imagingﻣﺮﺑﻮﻁ ﺑﻪ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﺨﺘﻠﻒ ،ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﮔﻮﻳـﺎ ﻭ ﺗﻴﭙﻴـﻚ ﻣﺘﻌـﺪﺩ ﻫﻤـﺮﺍﻩ ﺑـﺎ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﺑﺮﺍﻱ ﻓﻬﻢ ﻣﻄﺎﻟﺐ ﺍﺳﺘﻔﺎﺩﻩ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ ﻭ ﺍﺯ ﺗﻜﻨﻴﻜﻬﺎ ﻭ ﺟﺪﻳﺪﺗﺮﻳﻦ ﺭﻭﺷﻬﺎﻱ MRI, CT Scanﺑﻘﺪﺭ ﻛﻔﺎﻳﺖ ﺻﺤﺒﺖ ﺻﺤﺒﺖ ﺷﺪﻩ ﺍﺳﺖ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺩﺭ ﺩﻭ ﺟﻠﺪ ﺗﺪﻭﻳﻦ ﮔﺮﺩﻳﺪﻩ ﺍﺳﺖ .ﺟﻠﺪ ﺍﻭﻝ ﺍﻳﻦ ﻛﺘﺎﺏ ﺷﺎﻣﻞ ﭘﻨﺞ ﺑﺨـﺶ ﻋﻤـﺪﻩ ﻣﻲﺑﺎﺷﺪ ﻭ ﻓﻬﺮﺳﺖ ﻓﺼﻮﻝ ﺁﻥ ﺩﺭ ﺫﻳﻞ ﺁﻭﺭﺩﻩ ﺷﺪﻩﺍﻧﺪ: ﺑﺨﺶ ﺍﻭﻝ -ﺍﺻﻮﻝ MRI, CT Scan
ﺑﺨﺶ ﺩﻭﻡ -ﻣﻐﺰ ﻭ ﻣﻨﻨﮋﻫﺎ
ﺑﺨﺶ ﺳﻮﻡ -ﺗﺼﻮﻳﺮ ﺑﺮﺩﺍﺭﻱ ﺳﺮ ﻭ ﮔﺮﺩﻥ
ﺍﺻﻮﻝ ﺗﺼﻮﻳﺮ ﺑﺮﺩﺍﺭﻱ ﺩﺭ CT Scan
ﻓﺼﻞ -٤ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ MRI, CT Scanﻣﻐﺰ ﻭ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻓﺼﻞ -٥ﻧﺌﻮﭘﻼﺳﻢﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻓﺼﻞ -٦ﻋﻔﻮﻧﺘﻬﺎ ﻭ ﺍﻟﺘﻬﺎﺑﺎﺕ ﻣﻐﺰ ﻓﺼﻞ -٧ﺳﻜﺘﻪ ﻣﻐﺰﻱ ﻓﺼﻞ -٨ﻣﺎﻟﻔﻮﺭﻣﺎﺳﻴﻮﻧﻬﺎﻱ ﻋﺮﻭﻗﻲ ﻭ ﺁﻧﻮﺭﻳﺴﻤﻬﺎﻱ ﻣﻐﺰﻱ ﻓﺼﻞ -٩ﺗﺮﻭﻣﺎﻱ ﺳﻴﺴﺘﻢ ﺍﻋﺼﺎﺏ ﻣﺮﻛﺰﻱ ﻓﺼﻞ -١٠ﺍﺧﺘﻼﻻﺕ ﻧﻮﺭﻭﺩﮊﻧﺮﺍﺗﻴﻮ ﻓﺼﻞ Magnetic Resonance Spectroscopy -١١ﻣﻐﺰ ﻓﺼﻞ -١٢ﻓﺮﺁﻳﻨﺪﻫﺎﻱ ﻣﻨﻨﮋﻳﺎﻝ ﻓﺼﻞ -١٣ﻟﻮﻛﻮﺍﻧﺴﻔﺎﻟﻮﭘﺎﺗﻲﻫﺎ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﺩﻣﻴﻠﻴﻨﻴﺰﺍﻥ
ﻓﺼﻞ -١٤ﺍﻭﺭﺑﻴﺖ ﻓﺼﻞ -١٥ﺍﺳﺘﺨﻮﺍﻥ ﺗﻤﭙﻮﺭﺍﻝ ﻓﺼﻞ -١٦ﻛﺎﻭﻳﺘﻲ ﺳﻴﻨﻮﻧﺎﺯﺍﻝ ﻓﺼﻞ -١٧ﺗﻮﺩﻩﻫﺎﻱ ﻣﺮﺑﻮﻁ ﺑﻪ ﮔﺮﺩﻥ ﻭ ﺁﺩﻧﻮﭘﺎﺗﻲ ﮔﺮﺩﻧﻲ ﻓﺼﻞ -١٨ﺣﻨﺠﺮﻩ ﻓﺼﻞ -١٩ﻧﺎﺯﻭﻓﺎﺭﻧﻜﺲ ﻭ ﺍﻭﺭﻓﺎﺭﻧﻜﺲ ﻓﺼﻞ -٢٠ﻏﺪﺩ ﺗﻴﺮﻭﺋﻴﺪ ﻭ ﭘﺎﺭﺍﺗﻴﺮﻭﺋﻴﺪ ﻓﺼﻞ -٢١ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺳﺮ ﻭ ﮔﺮﺩﻥ ﺍﻃﻔﺎﻝ
ﻓﺼﻞ -١ ﻓﺼﻞ -٢ ﻓﺼﻞ -٣ﺁﻧﮋﻳﻮﮔﺮﺍﻓﻲ ﺑﺎ ﺍﺳﺘﻔﺎﺩﻩ ﺍﺯ ﺭﺯﻭﻧﺎﻧﺲ ﻣﻐﻨﺎﻃﻴﺲ ) :(MRIﺍﺻﻮﻝ ﻭ ﺗﻜﻨﻴﻜﻬﺎ ﻓﻴﺰﻳﻚ MRI
ﺑﺨﺶ ﭘﻨﺠﻢ -ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻗﻔﺴﺔ ﺳﻴﻨﻪ ﻓﺼﻞ -٢٧ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻏﻴﺮ ﻧﺌﻮﭘﻼﺳﺘﻴﻚ ﭘﺎﺭﺍﻧﺸﻴﻤﺎﻝ ﺭﻳﻪ ﻓﺼﻞ MRI, CT Scan -٣١ﺁﺋﻮﺭﺕ ﺗﻮﺭﺍﺳﻴﻚ
ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻓﺼﻞ -٢٨ﻧﺌﻮﭘﻼﺳﻢﻫﺎﻱ ﺍﻭﻟﻴﺔ ﺭﻳﻮﻱ ﻓﺼﻞ CT Scan -٣٢ﻗﻠﺐ ﻭ ﭘﺮﻳﻜﺎﺭﺩ
ﻓﺼﻞ -٢٩ﻣﺪﻳﺎﺳﺘﻦ
ﻓﺼﻞ -٣٠ﺟﻨﺐ )ﭘﻠﻮﺭ( ﻭ ﺩﻳﻮﺍﺭﺓ ﻓﻘﺴﺔ ﺻﺪﺭﻱ ﻓﺼﻞ MRI -٣٣ﻗﻠﺐ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
83
: ﺑﺨﺶ ﻋﻤﺪﻩ ﺑﻮﺩﻩ ﻭ ﻓﻬﺮﺳﺖ ﻓﺼﻮﻝ ﺁﻥ ﺑﻪ ﺗﺮﺗﻴﺐ ﺫﻳﻞ ﻣﻲﺑﺎﺷﺪ٤ ﺟﻠﺪ ﺩﻭﻡ ﻛﺘﺎﺏ ﻫﺎﮔﺎ ﺷﺎﻣﻞ ﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺍﻃﻔﺎﻝ-ﺑﺨﺶ ﻫﺸﺘﻢ ﻣﻼﺣﻈﺎﺕ ﻭﻳﮋﻩ: ﺩﺭ ﻛﻮﺩﻛﺎﻥMRI, CT Scan -٥١ ﻓﺼﻞ ﻗﻠﺐ ﻭ ﻋﺮﻭﻕ ﺑﺰﺭﮒ-٥٢ ﻓﺼﻞ ﻗﻔﺴﻪ ﺳﻴﻨﻪ-٥٣ ﻓﺼﻞ ﺳﻴﺴﺘﻢ ﻛﺒﺪﻱ ﺻﻔﺮﺍﻭﻱ-٥٤ ﻓﺼﻞ ﻃﺤﺎﻝ ﺍﻃﻔﺎﻝ-٥٥ ﻓﺼﻞ ﭘﺎﻧﻜﺮﺍﺱ-٥٦ ﻓﺼﻞ ﻛﻠﻴﻪﻫﺎ ﻭ ﻏﺪﺩ ﻓﻮﻕ ﻛﻠﻴﻮﻱ-٥٧ ﻓﺼﻞ ﺣﻔﺮﺓ ﭘﺮﻳﺘﻮﺋﻦ ﻭ ﻣﺰﺍﻧﺘﺮ، ﺩﺳﺘﮕﺎﻩ ﮔﻮﺍﺭﺵ-٥٨ ﻓﺼﻞ ﻟﮕﻦ ﻛﻮﺩﻛﺎﻥ ﻭ ﻧﻮﺟﻮﺍﻧﺎﻥ-٥٩ ﻓﺼﻞ ﺳﻴﺴﺘﻢ ﻋﻀﻼﻧﻲ ﻭ ﺍﺳﻜﻠﺘﻲ-٦٠ ﻓﺼﻞ
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺳﻴﺴﺘﻢ ﻋﻀﻼﻧﻲ ﻭ ﺍﺳﻜﻠﺘﻲ-ﺑﺨﺶ ﻫﻔﺘﻢ ﺗﻮﻣﻮﺭﻫﺎﻱ ﻣﻮﺳﻜﻮﻟﻮﺍﺳﻜﻠﺘﺎﻝ-٤٦ ﻓﺼﻞ ﭘﺎ ﻭ ﻣﭻ ﭘﺎMRI, CT Scan -٤٧ ﻓﺼﻞ ﺯﺍﻧﻮ-٤٨ ﻓﺼﻞ (Hip) ﻣﻔﺼﻞ ﺭﺍﻥ-٤٩ ﻓﺼﻞ ﺷﺎﻧﻪ-٥٠ ﻓﺼﻞ
ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﺷﻜﻢ ﻭ ﻟﮕﻦ-ﺑﺨﺶ ﺷﺸﻢ ﺩﺳﺘﮕﺎﻩ ﮔﻮﺍﺭﺵ-٣٤ ﻓﺼﻞ ﺿﺎﻳﻌﺎﺕ ﺗﻮﺩﻩﺍﻱ ﻛﺒﺪ-٣٥ ﻓﺼﻞ ﺗﻜﻨﻴﻚﻫﺎﻱ ﺗﺼﻮﻳﺮﺑﺮﺩﺍﺭﻱ ﻭ ﺑﻴﻤﺎﺭﻳﻬﺎﻱ ﻣﻨﺘﺸﺮ، ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ: ﻛﺒﺪ-٣٦ ﻓﺼﻞ ﻛﻴﺴﻪ ﺻﻔﺮﺍ ﻭ ﺳﻴﺴﺘﻢ ﺻﻔﺮﺍﻭﻱ-٣٧ ﻓﺼﻞ ﭘﺎﻧﻜﺮﺍﺱ-٣٨ ﻓﺼﻞ ﻃﺤﺎﻝ-٣٩ ﻓﺼﻞ ﻏﺪﺩ ﻓﻮﻕ ﻛﻠﻴﻮﻱ-٤٠ ﻓﺼﻞ ﻛﻠﻴﻪ-٤١ ﻓﺼﻞ ﭘﺮﻳﺘﻮﺋﻦ ﻭ ﻣﺰﺍﻧﺘﺮ-٤٢ ﻓﺼﻞ ( ﺭﺗﺮﻭﭘﺮﻳﺘﻮﺋﻦ )ﺧﻠﻒ ﺻﻔﺎﻕ-٤٣ ﻓﺼﻞ ﻟﮕﻦCT Scan -٤٤ ﻓﺼﻞ ﻟﮕﻦMRI -٤٥ ﻓﺼﻞ
Looking for the number key to the diagrams? Just fold out this page… A didactically brilliant and unprecedented approach to understanding CT imaging (Matthias Hofer, MD) Institute fo Diagnostic Radiology, MNR Clinic, Duesseldorf, Germany
Ideal for radiology residents, students and technicians, this concise manual is the perfect introduction to the practice and interpretation of computed tomography. Designed as a systematic learning tool, it introduces the use of CT scanners for all organs. Finally, self-assessment quizzes –including answers-ath the end of each chapter help the reader monitor progress and evaluate knowledge gained. Special Feature Includes detachable, pocket-sized cards containing checklists and tables of normal measurements –perfect for study or quick reference when on rounds. Contents: -Technical Aspects -Basic Rules of CT Reading -Preparing the patient -Administration of Contrast Media -Atlas of Normal and Common Pathological Findings in:the Cranium, Neck, Thorax, Abdomen, Retroperitoneum, Bones, and Lower Extremity -Interventional CT -CT-Angiography -Dose reduction -New protocols for 1-, 4-, and 16-row multislice scanners
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
84
MRI and CT Scan of Head and Spine
ﻗﻴﻤﺖ 500,000 :ﺭﻳﺎﻝ
)ﺗﻌﺪﺍﺩ ﺻﻔﺤﺎﺕ
( 810 :
)(Williams & Wilkins
)ﻓﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻳﺴﺖ ﻭ ﻣﺘﺪﻭﻟﻮﮊﻳﺴﺖ ﺩﺍﻧﺸﮕﺎﻩ (C. Barrie Grossman, M.D. Indiana
ﻛﺘﺎﺏ ﻓﻮﻕﺍﻟﺬﻛﺮ ﺩﺭ ﻣﻮﺭﺩ CT Scanﻭ MRIﺩﺭ ﺯﻣﻴﻨﺔ ﻧﻮﺭﻭﺭﺍﺩﻳﻮﻟﻮﮊﻱ ﺑﻪ ﺑﺤﺚ ﻭ ﺑﺮﺭﺳﻲ ﻣﻲﭘﺮﺩﺍﺯﺩ ﻭ ﺷﺎﻣﻞ ٤ﺑﺨﺶ ﺍﺻﻠﻲ ﺍﺳﺖ: ﺑﺨﺶ ﺍﻭﻝ :ﻣﻼﺣﻈﺎﺕ ﺗﻜﻨﻴﻜﻲ ﭘﺎﻳﻪ ﻓﺼﻞ -١
ﺑﺨﺶ ﺩﻭﻡ :ﻣﻐﺰ
ﺍﺻﻮﻝ ﻓﻴﺰﻳﻜﻲ ﻣﺮﺑﻮﻁ ﺑﻪ CT Scanﻭ MRI
ﻓﺼﻞ -٢ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺑﺎﻟﻴﻨﻲ CT Scan ﻓﺼﻞ -٣ﻣﻮﺍﺭﺩ ﺍﺳﺘﻔﺎﺩﻩ ﺑﺎﻟﻴﻨﻲ MRI
ﺑﺨﺶ ﺳﻮﻡ :ﻛﻒ ﺟﻤﺠﻤﻪ ،ﺟﻤﺠﻤﻪ ﻭ ﺻﻮﺭﺕ ﻓﺼﻞ -١١ﻧﺎﺣﻴﺔ ﺯﻳﻦ )(Sella
ﻓﺼﻞ -٤ﺁﻧﺎﺗﻮﻣﻲ ﻧﺮﻣﺎﻝ ﻣﻐﺰ ﺩﺭ CT Scanﻭ MRI
ﻓﺼﻞ -٥ﻧﺌﻮﭘﻼﺳﻢﻫﺎ ﻭ ﻛﻴﺴﺖﻫﺎﻱ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ ﻓﺼﻞ -٦ﺍﺧﺘﻼﻻﺕ ﻋﺮﻭﻗﻲ ﻣﻐﺰ ﻓﺼﻞ -٧ﺁﺳﻴﺐﻫﺎ ﻛﺮﺍﻧﻴﺎﻝ ﻭ ﺍﻳﻨﺘﺮﺍﻛﺮﺍﻧﻴﺎﻝ
ﻓﺼﻞ -٨ﻋﻔﻮﻧﺖﻫﺎ ﻭ ﺑﻴﻤﺎﺭﻱﻫﺎﻱ ﺍﻟﺘﻬﺎﺑﻲ ﻓﺼﻞ -٩ﻣﺎﻟﻔﻮﺭﻣﺎﺳﻴﻮﻥﻫﺎﻱ ﻣﺎﺩﺭﺯﺍﺩﻱ ﻣﻐﺰ ﻭ ﺍﺧﺘﻼﻻﺕ ﻧﻮﺯﺍﺩﻱ ﻓﺼﻞ -١٠ﻫﻴﺪﺭﻭﺳﻔﺎﻟﻲ ﻭ ﺍﺧﺘﻼﻻﺕ ﺩﮊﻧﺮﺍﺗﻴﻮ ﻭ ﺁﺗﺮﻭﻓﻴﻚ ﻣﻐﺰ
ﺑﺨﺶ ﭼﻬﺎﺭﻡ :ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
ﻓﺼﻞ -١٢ﻧﺎﺣﻴﻪ ﺗﻤﭙﻮﺭﺍﻝ ﻓﺼﻞ -١٣ﺟﻤﺠﻤﻪ ،ﺻﻮﺭﺕ ،ﺳﻴﻨﻮﺱﻫﺎﻱ ﭘﺎﺭﺍﻧﺎﺯﺍﻝ ﻭ ﻧﺎﺯﻭﻓﺎﺭﻧﻜﺲ ﻓﺼﻞ -١٤ﺍﻭﺭﺑﻴﺖ
ﻓﺼﻞ -١٥ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻧﺮﻣﺎﻝ ،ﺗﻜﻨﻴﮓﻫﺎﻱ ﺗﺼﻮﻳﺮ ﻓﺼﻞ -١٦ﻭﺿﻌﻴﺖﻫﺎﻱ ﺩﮊﻧﺮﺍﺗﻴﻮ ﻭ ﺗﺮﻭﻣﺎﺗﻴﻚ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ ﻓﺼﻞ -١٧ﺳﺎﻳﺮ ﭘﺎﺗﻮﻟﻮﮊﻱﻫﺎﻱ ﺳﺘﻮﻥ ﻓﻘﺮﺍﺕ
ﻻﺯﻡ ﺑﻪ ﺫﻛﺮ ﺍﺳﺖ ﻛﻪ ﺩﺭ ﻛﺘﺎﺏ ﻓﻮﻕ ،ﺑﺮﺍﻱ ﻓﻬﻢ ﺑﻬﺘﺮ ﻣﻄﺎﻟﺐ ﺍﺯ ﺗﺼﺎﻭﻳﺮ ﮔﻮﻳﺎ ﻫﻤﺮﺍﻩ ﺑﺎ ﺗﻮﺿﻴﺤﺎﺕ ﻛﺎﻓﻲ ﺍﺳﺘﻔﺎﺩﻩ ﮔﺮﺩﻳﺪﻩ ﻭ ﺑﺮﺍﻱ ﻃﺒﻘﻪﺑﻨﺪﻱ ﻧﻜﺎﺕ ﺍﺳﺎﺳﻲ ﺍﺯ ﺟﺪﺍﻭﻝ ﻣﺘﻌﺪﺩ ﺑﻬﺮﻩﮔﻴﺮﻱ ﺷﺪﻩ ﺍﺳﺖ.
HIGHLIGHTS OF OPHTHALMOLOGY INTERNATIONAL
WAVEFRONT ANALYSIS, ABERROMETERS and CORNEAL TOPOGRAPHY 1100,000R
)(2003
A. AGARWAL
B. BYOD,
ﮔﺮﭼــﻪ ﻫﻨــﻮﺯ ﻫــﻢ ﺩﺭ ﺑﺴــﻴﺎﺭﻱ ﺍﺯ ﻧﻘــﺎﻁ ﻛﺸــﻮﺭﻣﺎﻥ ﺍﻣﻜــﺎﻥ ﻋﻤــﻞ ﺟﺮﺍﺣــﻲ ﻛﺎﺗﺎﺭﺍﻛــﺖ ﺣﺘــﻲ ﺑــﻪ ﺭﻭﺵﻫــﺎﻱ ﻧﺴــﺒﺘﹰﺎ ﻗــﺪﻳﻤﻲ ﻧﻴــﺰ ﻭﺟــﻮﺩ ﻧﺪﺍﺷــﺘﻪ ،ﻋﺪﺳــﻲﻫــﺎﻱ ﺯﻳــﺎﺩﻱ ﺑــﻪ ﭘــﺎﺱ ﺧــﺪﻣﺎﺕ ﺩﺍﻧﺸــﻤﻨﺪ ﺑــﺰﺭﮒ ،ﻣﻮﺭﮔــﺎﻧﻲ ﻧــﺎﻡ ﻣــﻲﮔﻴﺮﻧــﺪ ) (!!) (Morgagnian Cataractﻟﻴﻜﻦ ﭘﻴﺸﺮﻓﺖ ﻋﻠﻢ ﻭ ﻓﻨﺎﻭﺭﻱ ﺧﺼﻮﺻﹰﺎ ﺩﺭ ﺩﻭ ﺩﻫﻪ ﺍﺧﻴﺮ ﭼﻨﺎﻥ ﺑﻮﺩﻩ ﻛﻪ ﺩﻳﮕﺮ ﺣﺪﺕ ﺑﻴﻨﺎﻳﻲ ٢٠/٢٠ﻫﺪﻑ ﻧﻬﺎﻳﻲ ﭘﺰﺷﻚ ﻭ ﺑﻴﻤﺎﺭ ﻧﺒﻮﺩﻩ ،ﻛﻴﻔﻴﺖ ﺑﻴﻨﺎﻳﻲ ﺑﺎ ﻫﻤﻪ ﺍﺑﻌﺎﺩ ﮔﺴﺘﺮﺩﻩﺍﺵ ﻣﺪ ﻧﻈﺮ ﻗﺮﺍﺭ ﮔﺮﻓﺘﻪ ﺍﺳﺖ. ﺩﺭ ﺳﺎﻝﻫﺎﻱ ﺍﺧﻴﺮ ﺑﺎ ﻭﺭﻭﺩ ﺗﻜﻨﻴﻚ Wavefront Analysisﺍﺯ ﻋﺮﺻﻪ ﻋﻠﻢ ﻧﺠﻮﻡ ﺑﻪ ﺣﻴﻄﻪ ﺟﺮﺍﺣﻲ ﻛﺮﺍﺗﻮﺭﻓﺮﺍﻛﺘﻴﻮ ﻭ ﻣﻄﺮﺡﺷﺪﻥ ، Customized LASIKﺍﻓﻖ ﺗﺎﺯﻩﺍﻱ ﺑﻪ ﻧﺎﻡ " "Super Visionﺩﺭ ﺑﺮﺍﺑﺮ ﺩﻳﺪﮔﺎﻥ ﺟﻬﺎﻧﻴﺎﻥ ﭘﺪﻳﺪﺍﺭ ﮔﺸـﺘﻪ ﺍﺳـﺖ .ﺳـﻴﺮ ﺑﺴـﻴﺎﺭ ﺳـﺮﻳﻊ ﺍﻳـﻦ ﭘﻴﺸﺮﻓﺖ ﺑﺎﻋﺚ ﺷﺪﻩ ﻛﻪ ﻛﺘﺐ Textﻣﻮﺟﻮﺩ ﻭ ﻗﺎﺑﻞ ﺩﺳﺘﺮﺳﻲ ﺩﺭ ﻛﺸﻮﺭ ﺍﺯ ﺁﻥ ﺟﺎ ﺑﻤﺎﻧﻨﺪ ﻭ ﻻﺟﺮﻡ ﺩﺍﻧﺴﺘﻪﻫﺎﻱ ﺑﺴﻴﺎﺭﻱ ﺍﺯ ﭼﺸﻢﭘﺰﺷﻜﺎﻥ ﻋﺰﻳﺰ ﻫﻢ ﺑﻪ ﺭﻭﺯ ﻧﺒﻮﺩﻩ ،ﻭ ﻳﺎ ﻣﺤﺪﻭﺩ ﺑﻪ ﺍﻃﻼﻋﺎﺕ ﭘﺮﺍﻛﻨﺪﻩ ﺑﻪ ﺩﺳﺖ ﺁﻣﺪﻩ ﺍﺯ ﻣﻘﺎﻻﺕ ﺑﺎﺷﺪ. ﻛﺘﺎﺏ ﺣﺎﺿﺮ ﻛﻪ ﺑﻪ ﻫﻤﺖ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ ﺩﺭ ﻛﻮﺗﺎﻫﺘﺮﻳﻦ ﺯﻣﺎﻥ ﻣﻤﻜﻦ ﺍﺯ ﺍﻧﺘﺸﺎﺭ ﺁﻥ ﺩﺭ ﺧﺎﺭﺝ ﺍﺯ ﻛﺸﻮﺭ ﺗﻬﻴﻪ ﺑﻪ ﺻﻮﺭﺕ ﺗﻤﺎﻡ ﺭﻧﮕﻲ ﺑﺮ ﺭﻭﻱ ﻛﺎﻏﺬ ﮔﻼﺳﺔ ﻣﺎﺕ ﻭ ﺑﺎ ﻛﻴﻔﻴﺘﻲ ﻛﻢ ﻧﻈﻴﺮ ﺑﻪ ﺯﻳﻮﺭ ﭼـﺎﭖ ﺁﺭﺍﺳـﺘﻪ ﮔﺮﺩﻳـﺪﻩ ،ﭘﺎﺳـﺨﻲ ﺍﺳـﺖ ﺩﺭ ﺟﻬﺖ ﻓﺮﻭﻧﺸﺎﻧﺪﻥ ﻋﻄﺶ ﻋﻠﻤﻲ ﻣﻮﺟﻮﺩ ﺩﺭ ﺍﻳﻦ ﺯﻣﻴﻨﻪ .ﺍﻳﻦ ﻛﺘﺎﺏ ﺑﺎ ﻋﻨﻮﺍﻥ WAVEFRONT ANALYSIS, ABERROMETERS and CORNEAL TOPOGRAPHYﺍﺯ ﺳﺮﻱ ﻛﺘﺎﺏﻫﺎﻱ ، Highlights Of Ophthalmologyﺍﺯ ﻣﻌﺪﻭﺩ ﻛﺘﺐ ﺗﻜﺴﺖ ﻣﻨﺘﺸـﺮ ﺷﺪﻩ ﻣﻲﺑﺎﺷﺪ ﻛﻪ ﺗﻤﺎﻣﹰﺎ ﺑﻪ ﻣﻘﻮﻟﻪ Wavefront Analysis, Orbscan, Topographyﻭ ﺍﺯ ﻫﻤﻪ ﻣﻬﻤﺘﺮ ﻛﺎﺭﺑﺮﺩ ﺁﻧﻬﺎ ﺩﺭ Cataract Surgery, Customized LASIK, Standard LASIKﭘﺮﺩﺍﺧﺘﻪ ﺍﺳﺖ. ﻼ ﻣﻮﺟﺰ ﻭ ﻗﺎﺑﻞ ﺩﺭﻙ ﻭ ﻛﺎﺭﺑﺮﺩﻱ ﺑﻪ ﺟﺎﻣﻌﺔ ﺟﻬﺎﻧﻲ ﭼﺸﻢﭘﺰﺷﻜﺎﻥ ﺍﺭﺍﺋﻪ ﻛﺮﺩﻩﺍﻧﺪ ﻧﻮﻳﺴﻨﺪﮔﺎﻥ ﺍﻳﻦ ﻛﺘﺎﺏ ﺍﺳﺘﺎﺩﺍﻥ ﺑﺮﺟﺴﺘﻪﺍﻱ ﺍﺯ ﻛﺸﻮﺭﻫﺎﻱ ﺁﻣﺮﻳﻜﺎ ،ﺍﺳﭙﺎﻧﻴﺎ ،ﮊﺍﭘﻦ ﻭ ﻫﻨﺪ ﻣﻲﺑﺎﺷﻨﺪ ﻛﻪ ﺑﻪ ﺳﺮﭘﺮﺳﺘﻲ Benjamin F. Boyd, M.D., FACSﺍﻳﻦ ﻛﺘﺎﺏ ﺭﺍ ﺑﻪ ﺻﻮﺭﺗﻲ ﻛﺎﻣ ﹰ ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ :ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ
ﻧﺸﺎﻧﻲ :ﺗﻬﺮﺍﻥ ،ﻡ ﺍﻧﻘﻼﺏ ،ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ ،ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ ،ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ ،ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ ،ﭘﻼﻙ ٢٣٩
ﺗﻠﻔﻦ٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :
85
AMERICAN ACADEMY OF OPHTHALMOLOGY
1 2 3 4 5 6 7 8 9 10 11 12 13
BASIC AND CLINICAL SCIENCE COURSE
ﻋﻨﻮﺍﻥ ﻛﺘﺎﺏ Section 1: Section 2: Section 3: Section 4: Section 5: Section 6: Section 7: Section 8: Section 9: Section 10: Section 11: Section 12: Section 13:
Update on General Medicine Fundamentals and Principles of Ophthalmology Optics, Refraction, and Contact Lenses Ophthalmic Pathology and Intraocular Tumors Neuro-Ophthalmolog Pediatric Ophthalmology and Strabismus Orbit, Eyelids, and Lacrimal System External Disease and Cornea Intraocular Inflammation and Uveitis Glaucoma Lens and Cataract Retina and Vitreous International Ophthalmology
ﻋﻨﻮﺍﻥ ﻛﺘﺎﺏ 14 15 16 17 18 19 20 21 22
WAVEFRONT ANALYSIS, ABERROMETERS and CORNEAL TOPOGRAPHY OPHTHALMOLOGY MONOGRAPHS Cataract Surgery and Intraocular Lenses COSMETIC OCULOPLASTIC SURGERY Eyelid, Forehead, and Facial Techniques Glaucoma THE REQUISITES IN OPHTHALMOLOGY LASIK Principles and Techniques THE GLAUCOMAS THE WILLS EYE MANUAL Office and emergency Room Deagnosis and Treatment of Eye Disease Complications in Phacoemulsification (Avoidance, Recognition, and Management) Retina and Optic Nerve Imaging (Thomas A. Ciulla, Carl D. Regillo, Alon Harris)
ﺳﺎﻝ ﻧﺸﺮ
(ﻗﻴﻤﺖ )ﺭﻳﺎﻝ
2002-2003
2002-2003
215,000 270,000 215,000 210,000 230,000 250,000 190,000 280,000 185,000 160,000 180,000 230,000 235,000
ﺳﺎﻝ ﻧﺸﺮ
(ﻗﻴﻤﺖ )ﺭﻳﺎﻝ
2003
1100,000
2001
200,000
1999
300,000
2000
200,000
1998
250,000
2000
180,000
1999
220,000
2002
400,000
2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003 2002-2003
.
٠٩١٢١٣٧٢٣٦١-٦٩٣٦٦٩٦ :ﺗﻠﻔﻦ
٢٣٩ ﭘﻼﻙ، ﺑﻦﺑﺴﺖ ﺳﻴﻤﻴﻦ، ﺑﻴﻦ ﻛﺎﺭﮔﺮ ﻭ ﺟﻤﺎﻟﺰﺍﺩﻩ، ﺥ ﻟﺒﺎﻓﻲﻧﮋﺍﺩ، ﺥ ﻛﺎﺭﮔﺮ ﺟﻨﻮﺑﻲ، ﻡ ﺍﻧﻘﻼﺏ، ﺗﻬﺮﺍﻥ:ﻧﺸﺎﻧﻲ
ﺍﺭﺍﺋﻪ ﻛﻨﻨﺪﺓ ﻛﺘﺎﺏ ﻭ ﺳﻲﺩﻱﻫﺎﻱ ﺗﺨﺼﺼﻲ ﭘﺰﺷﻜﻲ: ﻣﺮﻛﺰ ﺧﺪﻣﺎﺕ ﻓﺮﻫﻨﮕﻲ ﺳﺎﻟﻜﺎﻥ
Related Documents

Back Stability
February 2021 0
Back Pain
January 2021 2
Slope Stability Analysis
March 2021 0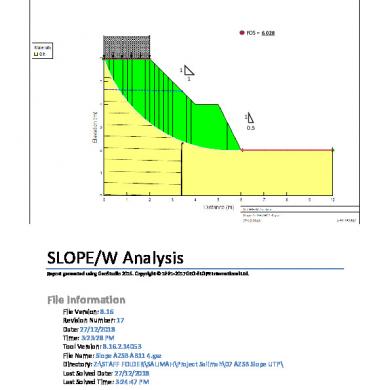
Slope Stability Analysis
March 2021 0
Back Pain
January 2021 4
Back Pain
January 2021 2More Documents from "Hardeep Chiraya"

Neck And Arm Pain Cailliet
January 2021 1
Back Stability
February 2021 0
Duvernoy En Etudes Edited Ericson
February 2021 1

