Fundamentals Of Nursing (nclex-rn)
This document was uploaded by user and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this DMCA report form. Report DMCA
Overview
Download & View Fundamentals Of Nursing (nclex-rn) as PDF for free.
More details
- Words: 15,176
- Pages: 71
Loading documents preview...
Fundamentals of Nursing (NCLEX-RN) I.
CULTURAL DIVERSITY
II.
ETHICAL AND LEGAL ISSUES
III.
LEADERSHIP AND MANAGEMENT
IV.
BASIC PHARMACOLOGY (including Herbal Medicines)
V.
ASEPSIS AND INFECTION CONTROL
VI.
COMPUTATION OF DOSAGE OF MEDICATIONS
VII.
NORMAL VALUES
VIII. NUTRITION AND DIET IX.
THERAPEUTIC DIETS
X.
POSITIONS
XI.
PROCEDURES
Fundamentals of Nursing consist of: 1. Cultural Diversity 2. Ethical and Legal Issues 3. Leadership and Management Issues 4. Basic Pharmacology (Including herbal medicines, computation, IV and Blood Transfusion Therapy) 5. Asepsis and Infection Control 6. Normal Values 7. Nutrition (including Therapeutic Diets) 8. Positioning 9. Diagnostic Tests
“What is the content of NCLEX-RN examination and how does the examinee answer those questions?” Questions of the actual NCLEX-RN Examination were distributed to the following category: Safe Effective Care Environment, under this category is the following sub-category -- Management of Care -- Infection Control Health Promotion and Maintenance Physiological Integrity, under this category is the following sub-category -- Basic Care and Comfort -- Pharmacological and Parenteral Therapies -- Reduction of Risk Potential -- Physiological Adaptation
An update you must know about the actual NCLEX-RN examination: Last April 2010, the questions about Management of Care were increased and questions about Reduction of Risk Potential were decreased. And according to the newsletter disseminated by NCSBN, the passing standard also increases. But do not be disturbed with this new info at hand, if you learn how to master the different concepts of nursing, starting with this concept “Fundamentals of Nursing”. Whatever type of questions you might encounter with the actual exam, I am sure that you can answer it correctly. Processes Integrated into all Client Needs Categories
Nursing Process Caring Communication and Documentation Teaching and Learning The Test Duration is six (6) hours Minimum number of questions that you may answer is seventy five (75) And the maximum number of questions that you may answer is two hundred sixty five (265)
The computer automatically stops when: Maximum number of questions has been answered Six hours have elapsed Examinee‟s minimum level of competency has been established Examinee‟s lack of competency has been established NCLEX-RN also uses Computer Adaptive Testing (CAT) and the decision if you pass or fail is based on how many questions you answer correctly and the difficulty of the questions a candidate answers correctly. The Examination will not end until certainty of the pass/fail result is assured.
I. CULTURAL DIVERSITY African-Americans Direct eye contact with authority is viewed as rude; but it is an important part of communication among family members/significant others. Personal questions are considered intrusive during initial contact; e.g. relationships, divorce, conflicts. Touching another’s hair is offensive. Illness is believed to be caused by demons/spirit Folk healer/herbalist may be consulted before seeking medical treatments
Native Americans/American Indians silence indicate respect for the speaker eye contact as a sign of disrespect They value the practice of massage to promote bonding between mother and newborn. Rooming-in is preferred for the mother and the newborn integration of religion and healing practices is observed Illness is caused by supernatural forces and disequilibrium between person and environment.
Asian Americans Direct eye contact with authority is viewed as rude head nodding does not necessarily mean agreement saying “NO” is considered as disrespect for others do not touch member of the opposite sex illness is believed to be an imbalance between positive (+) and negative (-) energy forces Promotion of healing by Yin and Yang principle Cold foods (Yin) Hot foods (Yang) Cold foods are given for hot illness Hot foods are given for cold illness
Hispanic Americans Do not admire a child. They believe that you may afflict the child with “evil eye,” it will cause an illness to the child they avoid eye contact with authority to show respect they use embraces/handshakes; they are very tactile they believe that health results from balance between “hot/cold”, “wet/dry” forces illness is a result of God‟s punishment communicate with male head of the family especially for major decisions, like signing consent for procedures because they have patriarchal society the most valued members of the family is the children religious practices are related to treatment of illness
European (White)-Origin Americans eye contact indicates trustworthiness they primarily depend on modern western health care services Autopsy is prohibited among: Eastern Orthodox Muslims Jehovah‟s Witness (NO BLOOD TRANSFUSION) Orthodox Jews
ORGAN DONATION: Jehovah‟s Witness (prohibited) Muslims (prohibited) Buddhists (act of mercy)
CREMATION: Hindus (cast ashes in Holy River, they believe that they can join the Creator faster this way) Mormons (prohibit cremation) Eastern Orthodox (prohibit cremation) Islam/Muslims (prohibit cremation) Jews (prohibit cremation)
RELIGION AND DIETARY PRACTICES: Baptist prohibits alcohol; discourages tea and coffee Buddhist prohibits alcohol and drug use most of them are vegetarians Hinduism considered the cow as sacred animal that is why they prohibit eating of beef and veal most of them are vegetarians Islam prohibits pork, alcohol and drugs daytime fasting is practiced during the time of Ramadan Jehovah’s Witness prohibits food to which blood has been added allow animal flesh that has been drained from blood
Judaism KOSHER DIET: prohibits meat and milk combination Prohibits pork and scavenger fish (shrimps, squids, crabs, fishes with no scales) Meat is allowed if from animals that are vegetable-eaters, cloven-hoofed, and ritually slaughtered Mormon prohibits alcohol, tea and coffee practice of fasting every first Sunday of the month encourages limited consumption of meat Roman Catholicism No meat on ash Wednesday and Good Friday (abstinence) Optional fasting during lent season Seventh day Adventist prohibits alcohol, tea and coffee, meat, and scavenger fish No surgeries or any procedures during Saturdays (Sabbath Day – sundown Friday to sundown Saturday).
CULTURAL BELIEFS AND PRACTICES ON DEATH AND DYING: Chinese When a Chinese client dies, they cover him/her with mirror with white cloth Islam/Muslim A dying client must face East (Middle East) or West/Southwest (North America). The dead body will be washed by a family member of the same sex and then covered with white cloth Buddhists The dead body is blessed by Spiritual Adviser Roman Catholics Anointing of the sick is done by the priest, to a dying client
TIME FOR A SHORT QUIZ. QUESTIONS A nurse is providing discharge instructions to a Chinese client regarding prescribed dietary modifications. During the teaching session, the client continuously turns away from the nurse. Which nursing action is appropriate? Continue the instructions, verifying client understanding Walk around the client so that the nurse constantly faces the client Give the client a dietary booklet and return later to continue with the instructions Tell the client about the importance of the instructions for the maintenance of health care 2. A nurse is preparing a plan of care for a client who is Jehovah‟s Witness. The client has been told that surgery is necessary. The nurse considers the client‟s religious preferences in developing the plan of care and documents that: Faith healing is practiced primarily Medication administration is not allowed Surgery is prohibited in this religious group The administration of blood and blood products is forbidden 3. Which of the following meal trays would be appropriate for the nurse to deliver to a client of Jewish faith who follows kosher diet? Pork roast, rice, vegetables, mixed fruit, milk Crab salad on a croissant, vegetables with a dip, potato salad, milk Sweet and sour chicken with rice and vegetables, mixed fruit, juice Fettucini alfredo with shrimp and vegetables, salad, mixed fruit, iced tea 4. An ambulatory care nurse is discussing preoperative procedures with a ChineseAmerican client who is scheduled for surgery the following week. During the discussion, the client continually smiles and nods the head. The nurse interprets this nonverbal behaviour as: Reflecting a cultural value An acceptance of the treatment The client is agreeable to the required procedures The client understands the preoperative procedure
5. A Chinese-American client experiencing anemia, which is believed to be a yin disorder, is likely to treat it with: Magnetic therapy Intercessory prayer Foods considered to be yin Foods considered to be yang ANSWERS AND RATIONALE 1) A - Most Chinese maintain a formal distance with others, which is a form of respect. Many Chinese are uncomfortable with face-to-face communications, especially when eye contact is direct. If the client turns away from the nurse during a conversation, the most appropriate action is to continue with the conversation. Walking around to the client so that the nurse faces the client is in direct conflict with the cultural practice. The client may consider returning later to continue with the explanation as a rude gesture. Telling the client about the importance of the instructions for the maintenance of health care may be viewed as degrading. 2) D - Among Jehovah‟s Witnesses, surgery is not prohibited, but the administration of blood and blood products is forbidden. Faith healing is forbidden in this religious group. Administration of medication is an acceptable practice, except if the medication is derived from blood products. 3) C - In the Jewish religion, those who are kosher believe that the dairy-meat combination is not acceptable. Pork and pork products are not allowed in the traditional Jewish religion. Only fish that have scales and fins are allowed; meats that are allowed include animals that are vegetable eaters, cloven-hoofed, and ritually slaughtered. 4) A - Nodding or smiling by a Chinese-American client may reflect only the cultural value of interpersonal harmony. This nonverbal behavior may not be an indication of agreement with the speaker, an acceptance of the treatment, or an understanding of the procedure. 5) D - In the yin and yang theory, health is believed to exist when all aspects of the person are in perfect balance. Yin foods are cold and yang foods are hot. Cold foods are eaten when one has a hot illness and hot foods are eaten when one has a cold illness. Options A and B are not associated with the yin and yang theory.
II. ETHICAL AND LEGAL ISSUES Advance Directive It is a written document that provides directions concerning the provision of care when a person is unable to make his/her own treatment choices. Two types of advance directive: a) Living Will – it is the expression of the person‟s wishes regarding end-of-life care. It is prepared by a competent adult that provides direction regarding medical care in the event of the person‟s incapacitation or otherwise becoming unable to make decisions personally. b) Durable Power of Attorney – I is an authorization that enables any competent individual to name someone to exercise decision-making on his/her behalf under specific circumstances. Example, end-of-life situation.
Clarifying Unclear/Inappropriate Physician’s Order Clarify the order with the physician who gave the order Contact nurse manager/supervisor if no resolution occurs regarding the order in question
Floating It is acceptable and legal practice Nurse cannot refuse to float; but the nurse should not assume responsibility beyond level of experience or qualification The nurse should inform the supervisor of any lack of experience in caring for the type of clients on the new nursing units The nurse should be given an orientation to the new unit Floating nurse should be assigned with patients with stable conditions; or similar to his/her training or experience Floating nurse should not be assigned to patients who are for discharge and who require patient teaching
Good Samaritan Laws - These laws encourage health care professionals to assist in emergency situations without fear of being sued for the care provided
Informed Written Consent Physician not the nurse, is the primary responsible to secure written consent Nurse may sign as a witness. It attests that the client signed the consent
Written consent is legal when: The person is in legal age (18 y/o and above) The consent is secured without force, duress, or coercion The person is not under the influence of drugs or alcohol The person is not mentally incapacitated Parents or guardian can signed for minors and persons who are physically or mentally incapacitated Minors who are married or emancipated from the parents and those seeking for treatment for STD‟s can signed an informed consent Written consent can be waived in time of emergency to save the life of the person Validity of informed consent is 24 hours. If the procedure is postponed, secure another consent Secure consent for each procedure
Organ Donation Age requirement is 18 y/o and above before signing a form for organ donation Informed choice to donate an organ may be through written document signed by the client prior to death, a will, a donor card, or an advance directive Family member or legal guardian may authorize organ donation if the client is dead
Physician’s Orders Nurses is duty-bound to carry out a doctor‟s order except when the nurse believes that the order is inappropriate Nurses who carry out inaccurate order is legally responsible for his/her action
Telephone Orders Date and time the entry Repeat (read back) the order to the physician and record the order Sign the order begin with the t.o., write the doctor‟s name, and then sign the order; e.g. (t.o. Dr. Alec Tinio/ your signature RN It is necessary that the doctor countersign the order within the time frame based on the agency policy (usually 24 hours)
Use of Restraints Written consent is needed coming from relatives/significant others Secure consent for each episode of application of restraints PRN order: legally unacceptable Apply soft restraints Secure restraints at he bed frame, not on the side rails Check restraint application every 15-20 minutes Release restraints every 2 hours for 30 minutes Change restraints every 24 hours
Documentation For Narrative Documentation it should be accurate, complete, factual, and objective use a black pen document care, medications, treatments, and procedures as soon as possible, after completed document responses to interventions document consent for a refusal of treatments document calls made to other health care providers
use appropriate abbreviations in case of error, draw one line through the error, initial and date never erase any entry, do not use correction fluid do not leave blank spaces on documentation forms. Avoid judgmental or opinionated statements, such as “uncooperative client.” Do not document for others or change documentation for other individuals For Computerized Documentation use only the user identification (ID) code, name, or password maintain privacy and confidentiality of documented information printed from the computer
Principle of Confidentiality Information about a client be kept private Information in the client‟s record is accessible only to those providing care to the client No one else is entitled to that information unless the client has signed a Consent for Release of Information that identifies with whom information may be shared and for what purpose. Discussing clients outside the clinical setting, telling friends, or family about clients or even discussing clients in the elevator with other workers violates client‟s confidentiality. The clients has a right to review the records pertaining to his/her medical care and to have the information explained or interpreted as necessary, except when restricted by law
Incident Reports/Variance Reports A tool used as a means of identifying and improving care. The reports should be complete, accurate, and factual. The reports should not include opinions or interpretations. The report form should not be copied or placed in the client„s record. It is not a substitute for a complete entry in the client‟s record regarding the incident.
Controlled Substances Nurses may administered controlled substances (narcotics, depressants, stimulants, and hallucinogens), only under the directions of a physicians or other authorized providers. Controlled substances must be kept securely locked, and only authorized personnel should have access to them.
Reporting Responsibilities. The following situations need to be reported to the Local Authority. This is a LAW. Failure to report any of these situations is a malpractice.
Communicable diseases Abuse: sexual, child, wife, husband, elderly abuse. (Whenever abuse is suspected, it should be reported to the local authority. It will be the court to prove or disprove abuse.) gunshot/ stab wounds vehicular accidents assault homicides
Clients Advocacy Involves concerns and actions on behalf of another person in order to bring about change. 3 Elements of Advocacy 1. Mediate 2. Inform 3. Support
MORAL PRINCIPLES 1. Beneficence - means doing and promoting good. e.g.,
Administering pain medications. Practicing asepsis to prevent infection.
Promoting safety of restless and confused clients. Providing psychosocial support to an anxious client.
2. Nonmalefincence - means to avoid doing harm, to remove from harm, and to prevent harm. e.g., protecting the client from a practitioner who practices drug abuse. Reporting abuse prevent further victimization. 3. Autonomy – right to make one‟s own decision 4. Fidelity – being faithful to agreement and promises 5. Veracity – telling the truth 6. Justice - fairness
TORTS AND CRIMES - These are legal wrongs committed against a person or property.
CRIME - Results in prison term or fine or short jail sentence to punish offender. a. Felony - A crime of serious nature. b. Misdemeanor - An offense punishable by imprisonment of less than one year or a fine less than 1,000 dollars. Does not amount to a felony. c. Manslaughter - A second degree murder. It is unintentional killing. e.g., accidental administration of overdose narcotics that resulted to death of the clients.
TORTS - Result in civil trial to assess compensation for plaintiff 1. Intentional Torts: I.
Assault and Battery a. Assault – is the threat of touching another person without his/her consent b. Battery – is the actual carrying out of such a threat
II.
Defamation of Character - is a communication that is false or made with careless disregard for the truth, and results in injury to the reputation of the person a. Libel – defamation by means of print, writing, or pictures b. Slander - is defamation by spoken word, stating unprivileged or false words by which the reputation of the person is damaged
III.
Fraud - is the wilful, purposeful misrepresentation of self or an act that may cause harm to a person or property
IV.
Invasion of Privacy - is disclosure confidential information to an inappropriate third party (subjects the nurse to invasion of privacy even if the information is true).
V.
False Imprisonment – occurs when a client is not allowed to leave a health care facility when there is no legal justification to detain the client
2. Unintentional Torts I.
Negligence – mistake or failure to be prudent. An act of omission or commission
II. Malpractice – is negligence in the practice of profession (e.g. error in sponge counts) To prove malpractice, four elements are necessary a. a duty of the nurse to the client b. a breach of duty on the part of the nurse c. an injury to the client d. a causal relationship between the breach of duty and the client subsequent injury Potential Malpractices Situations in Nursing medication error
mistaken identity
sponge count error
loss/damage of client‟s property
burning a client
failure in reporting crimes, torts, and unsafe practice
client falls “Only the Task not the Accountability may be Delegated to another” Best Practice: Always ensure client safety
Death and Dying Right of Informed Refusal – a competent adult has the right to refuse treatment, even lifesustaining treatment Do Not Resuscitate (DNR) Order – a written order must be present and must be reviewed on a regular basis. The client or his/her legal representative must provide informed consent for the DNR status. Both DNR and cardiopulmonary resuscitation (CPR) must be clearly defined so that other treatments, not refused by the client will be continued. Euthanasia – physician or nurse-caused death (active euthanasia), deliberately hastening a person‟s death, is considered murder in all states and almost all other countries
Pronouncement of Death in some States, the nurse may pronounce death at the bed side in most States, however, the physician has the legal responsibility of pronouncing the person dead. “To be safe in answering, always choose PHYSICIAN.” Death Certificate – the physician is responsible for signing a death certificate Care of the Body – the nurse is responsible for preparing the body for the morgue or mortuary. Consider the cultural practices and wishes of the family. Treat the body with dignity. Rigor Mortis – stiffening of the body (occurs 2-4 hours) position the body, the dentures, close the mouth and eyes before RM set in Algor Mortis – decrease in body temperature (1C/hr) Livor Mortis – discoloration of the skin because of the RBC breakdown Management: make the body appear natural and comfortable allow the family to view the patient‟s body place the body in supine positions, the arms at the side and palms down place one pillow under the head and shoulder to prevent blood from discoloring the face place absorbent pads under the buttocks to take up any feces or urine apply identification tags, one on the ankle and one at the wrist wrap the body in shroud, place the third tag for identification
III. LEADERSHIP AND MANAGEMENT Priorities of Care needs that are life threatening are given highest priority actual before potential concerns consider time constraints and available resources needs that are identified as important by the client are given highest priority use Maslow‟s hierarchy of needs (physiologic before psychosocial needs) use ABC‟s; patent airway is always priority unstable before stable clients client first before equipment do not delegate client who need: to be assessed those who need health teachings those who need to be evaluated those with unstable conditions
DELEGATION transference of responsibility and authority for the performance of an activity to a competent individual Five Rights of Delegation Right Task – appropriate activities Right Circumstances – assess health status. Match complexity of activity with competency of the health care worker. Right Person Right direction and communication Right supervision/evaluation
CNA/Unlicensed Nursing Assistant Undergo certification examination May care for clients with stable conditions May perform standard nursing procedures: VS - taking Comfort measures Hygienic measures Activity, mobility, exercise Collection of specimen Enema administration Obtaining equipment LPN/LVN Undergo licensure examination (NCLEX-PN/VN) May perform standard nursing procedures and more complicated nursing procedures: Wound dressing changes Irrigation of wounds Colostomy care Enteral feedings Administration of medications (oral, subcutaneous, intramuscular) Administration of basic IV fluids (no IV meds and electrolytes added to IV fluids like Potassium Chloride) Catheterization May care for clients with stable conditions
Leadership Theories 1. Bureaucratic – relies on organization‟s rule and policy 2. Autocratic – make decision for the group 3. Laissez-faire – recognizes the group‟s need for autonomy and self-regulation; “hands-off approach” 4. Democratic – encourages group discussion and decision making
Principles of Management 1. Authority – legitimate right to direct the work to others 2. Accountability – ability to assume responsibility for one‟s action and its consequences 3. Responsibility – obligation to complete a task Principles in Rooming-In Cohorts (similar medical diagnosis or mode of transmission of disease) may be roomed-in as long as one does not have another type of contagious infection. Consider age and gender of clients. Clients of the same age group and gender may be roomed-in Clients with airborne infections should be confined in private rooms Immune-compromised clients should not be roomed-in with clients who have infections.
Case Management Assignment of health care provider to assist a patient in assessing health and social service systems to assure that all required services are obtained Who requires Case Management? age 65 with chronic diagnostic state, lives alone newly diagnosed diabetic limited income preventing prescription purchases
weakness related to CVA may require change in living arrangements may need medical equipment may need home health follow-up
confused or unstable to make decisions
admitted from board and care
Let us evaluate . . . 1. A new unit nurse manager is holding her first staff meeting. The manager greets the staff and comments that she has been employed to bring about performance improvement. The manager provides a plan that she developed, as well as a list of tasks and activities for which each staff member must volunteer to perform. In addition, she instructs staff members to report any problems directly to her. What type of leadership style do the new manager‟s characteristics suggest? autocratic
democratic
situational
laissez-faire
2. A new nursing graduate is attending an agency orientation regarding the nursing model of practice implemented in the health care facility. The nurse is told that the nursing model is a team nursing approach. The nurse understands that planning care delivery will be based on which characteristic of this type of nursing model of practice? a task approach method is used to provide care to clients managed care concepts and tools are used in providing client care an RN leads nursing personnel in providing care to a group of clients a single RN is responsible for providing nursing care to a group of clients 3. The nurse manager has implemented a change in the method of the nursing delivery system from functional to team nursing. A nursing assistant is resistant to the change and is not taking an active part in facilitating the process of change. Which of the following is the best approach in dealing with the nursing assistant? ignore the resistance exert coercion with the nursing assistant provide a positive reward system for the nursing assistant confront the nursing assistant to encourage verbalization of feelings regarding the change 4. The nurse manager of a critical care unit must speak to a staff nurse about an employment issue, tardiness. Nearly every day during the past week, the staff nurse has been from 5 to 20 minutes late, missing portions of the daily client status conferences. The manager had verbally counselled the staff nurse 3 months prior to the latest incidence of tardiness about the same issue. When they meet, the nurse manager‟s best approach to the staff nurse is to: send the staff nurse to Human Resources Department for counselling ask the staff nurse to tell the manager about the facts surrounding the tardiness inform the staff nurse that, based on unreliability caused by tardiness issues, the nurse is terminated Provide the staff nurse with a detailed notice of intent to terminate if any further incident of tardiness occurs.
5. A nurse is giving a report to a nursing assistant who will be caring for a client who has hand restraints. The nurse instructs the nursing assistant to assess the skin integrity of the restrained hands every: 2 hours
4 hours
3 hours
30 minutes
ANSWERS AND RATIONALE 1) A - The autocratic leader is focused, maintains strong control, makes decisions, and, addresses all problems. Furthermore, the autocrat dominates the group and commands rather than seeks suggestions or input. In this situation, the manager addresses a problem (performance improvement) with the staff, designs a plan without input, and wants all problems reported directly back to her. A situational leader will use a combination of styles, depending on the needs of the group and the tasks to be achieved. The situational leader would work with the group to validate that the information that the leader gained as a new employee was accurate and that a problem existed, and would then take the time to get to know the group and determine which approach to change (if needed) would work best according to the needs of the group and the nature and substance of the change that was required. A democratic leader is participative and would likely meet with each staff person individually to determine the staff member‟s perception of the problem. The democratic leader would also speak with the staff about any issues and ask the staff for input with developing a plan. A laissez-faire leader is passive and nondirective. The laissez-faire leader would state what the problem was and inform the staff that the staff needed to come up with a plan to “fix it.” 2) C - In team nursing, nursing personnel are led by a registered nurse leader in providing care to a group of clients. Option A identifies functional nursing. Option B identifies a component of case management. Option D identifies primary nursing. 3) D - Confrontation is an important strategy to meet resistance head on. Face-to-face meetings to confront the issue at hand will allow verbalization of feelings, identification of problems and issues, and development of strategies to solve the problem. Option A will not address the problem. Option B may produce additional resistance. Option C may provide a temporary solution to the resistance but will not address the concern specifically. 4) D - In general, the process for corrective action begins with an oral reprimand and then a written reprimand. In addition to the written reprimand, the manager should be prepared to work with the staff nurse to develop a plan of action. The manager must notify the staff nurse, in writing, of the potential for termination based on tardiness. If this were the first instance, the manager would ask the staff nurse to describe the facts surrounding the tardiness in order for the manager to assist the staff nurse with problem-solving strategies or to examine the need for moving the staff nurse to a different shift, if indicated. Managers are expected to deal with personnel issues, and tardiness is a frequent problem that managers face. Human resources serve as a support to the actions of the manager, but do not assume the role of dealing with the employee. Managers must give notice prior to termination as a risk management strategy. 5) D - The nurse should instruct the nursing assistant to assess restraints and skin integrity every 30 minutes. Agency guidelines regarding the use of restraints should always be followed.
IV. BASIC PHARMACOLOGY (including Herbal Medicines) Types of Doctor’s Order Standing Order – it is carried out until the specified period of time or until it is discontinued by another order Single Order – it is carried out for one time only STAT Order – it is carried out at once or immediately PRN Order – it is carried out as the patient requires Parts of Legal Doctor’s Order - Name of patient - Date and time - Name of drug - Dose of drug - Route of administration - Times or frequency - Signature of the physician PRINCIPLES IN ADMINSTERING MEDICATION 1. Observe the “7 Rights” of drug administration Right drug – read the label three times Right dose – know the usual dose of the drug. Calculate the correct amount Right time – standard time may be followed in the institution Right route – check the route of administration Right patient – identify patient by: checking the ID band (most accurate patient identifier) or asking him to state his/her name (not accurate for confused clients) Right recording – sign medication sheet immediately after administration Right approach 2. Practice Asepsis – wash hands before and after preparing medications Nurses who administer medications are responsible for their own actions. Question any order that you consider incorrect (may be unclear or inappropriate) Be knowledgeable about the medications that you administer. Know the action, indication, nursing responsibilities, side effects of the drugs Fundamental Rule: “Never Administer an Unfamiliar Medication” 3. Keep narcotics in locked place
4. Use only medications that are clearly labelled container. Relabeling of drugs is the responsibility of pharmacist 5. Return liquid that are cloudy in color to the pharmacy 6. Before administering the medication, identify the client correctly 7. Do not leave the medications at the bed side. Stay with the client until he actually takes the medications 8. The nurse who prepares the drug administers it. Only the nurse who prepared the drug knows what that drug is. Do not accept endorsement of medications. 9. If the client vomits after taking the medication, report this to the nurse in charge or physician 10. Preoperative medications are usually discontinued during the postoperative period unless ordered to be continued 11. When a medication is omitted for any reason, record the fact together with the reason 12. When a medication error is made, report it immediately to the nurse in charge or physician. To implement necessary measures immediately. This may prevent any adverse effects of the drug
ROUTES OF DRUG ADMINISTRATION 1. Oral Medication - Most common method of drug administration and generally the safest route. Absorption will usually take in GIT. - Onset is slower compare to others Types of Oral Drugs a. Solid Preparation – tablets, capsules, and pills Remember: enteric-coated tablets and time-released capsules are never crushed or chewed b. Liquid Preparation – elixirs, syrups, and suspensions. They are best administered by using calibrated cup (read at the eye level). Other Oral Form Drugs a. Sublingual – drugs are placed under the tongue b. Buccal – drugs are placed in the inner cheek Rule: never swallow the drug and do not follow with water. If nitro-glycerine is given, advise patient not to smoke.
Safety in administering Oral Medications - might cause aspiration and choking (especially large capsules and tablets) - assess for gag reflex, dysphagia, or altered LOC - client who is NPO Note: if drug has offensive taste, offer oral hygiene.
2. Topical Medication - applied to the skin by spreading it over an area, soaking or medicated bath (causes either local or systemic effect depending on duration of application). Note: Nurse should done gloves when administering this type of drug.
3. Inhalation Medication Nasal inhalation – oxygen is administered by this route Oral inhalation MDI (Metered-dose inhaler) 2 inches away from the mouth Inhale 2-5 seconds Hold breath for 10 seconds Wait 1-2 minutes before each puff Note: to know if the canister is still packed with drug, simply put it in basin with water. If it floats, it is empty. Nebulizer Dilute to sterile 0.9% NaCl (2-5 ml) Attach oxygen to nebulizer (8L/min) Breathe normally through mask or mouthpiece for 5-15 minutes Note: offer Oral Hygiene
4. Eye Medication (Optic) Effects:
Miotics - pupil constriction Mydriatics – pupil dilation
Types: Liquid – 2 gtts (lower conjunctival sac) Ointment – 2 cm (inner to outer canthus) Note: no to cornea press the nasolacrimal gland if drug will cause systemic effect don‟t let the tip of the canister touch any part of the eye sitting position is required Note: Eye assessment? Dim the light prior to eye examination
5. Ear Medication (Otic) Position: lateral position Age below 3 y/o – pull the pinna down and back Above 3 y/o – pull the pinna up and back Solution - side of the ear Temp of solution – warm Press the tarsus of the ear 3 times for absorption Place earplug for 5 minutes Note: if the ear canal is obstructed by seed, don‟t flush with water. If an insect goes inside the ear, use flashlight
6. Parenteral Route – is a medication administration is by needle. Intradermal route of medication administration- it is a parenteral route of medication administration by injecting the needle under the epidermis. The site are the inner lower arm, upper chest and back, and beneath the scapula Indicated for allergy and tuberculin testing and for vaccinations Use the needle gauge 25,26,27 needle length: 3/8", 5/8", or 1/2" Needle at 10-15 degrees angle: bevel up Inject a small amount of drug slowly over 3 to 5 seconds to form a wheal or bleb Do not massage the site of injection. To prevent irritation of the site, and to prevent absorption of the drug into the subcutaneous.
I. SUBCUTANEOUS route of medication administration - for vaccines, heparin, preoperative medication, insulin, narcotics The site: - outer aspect of the upper arms - anterior aspect of the thighs - abdomen scapular areas of the upper back - ventrogluteal - dorsogluteal Only small dose of medication should be injected via SC route Rotate site of injection to minimize tissue damage Needle length and gauge are the same for ID injections Use 5/8 needle for adults when the injection is to administer at 45 degree angle; 1/2 is use at 90 degree angle For thin patients: 45 degree angle needle For obese patient: 90 degree angle needle For heparin injection: do not aspirate and do not massage the injection site to prevent hematoma formation. For insulin injection: do not massage to prevent rapid absorption which may result to hypoglycemic reaction. Always inject insulin at 90 degrees angle to administer the medication in the pocket between the subcutaneous and muscle layer. Adjust the length of the needle depending on the size of the client
II. INTRAMUSCULAR route of medication administration needle length: 1", 1 1/2", 2" to reach the muscle layer Clean the injection site with alcoholised cotton ball to reduce microorganisms in the area Inject the medication slowly to allow the tissue to accommodate volume
Sites: a. Ventrogluteal site The area contains no large nerves, or blood vessels and less fat. It is farther from the rectal area, so it is less contaminated Position the client in prone or side-lying When in prone, curl the toes inward When in side-lying, flex the knee and hip. These ensure relaxation of the gluteus muscles and minimize discomfort during injection To locate the site, place the heel of the hand over the greater trochanter, point the index finger toward the anterior superior iliac spine, and then abduct the middle(third) finger. The triangle formed by the index finger, the third finger and the crest of the ilium is the site. b. Dorsogluteal site Position the client similar to the ventrogluteal site The site should not be used in infant under 3 years old because the gluteal muscles are not well developed yet To locate the site, the nurse draws an imaginary line from the greater trochanter to the posterior superior iliac spine. The injection site is lateral and superior to this line Another method of locating this site is to imaginary divide the buttock into four quadrants. The upper most quadrant is the site of injection. Palpate the crest of the ilium to ensure that the site is high enough Avoid hitting the sciatic nerve, major blood vessel or bone by locating the site properly c. Vastus Lateralis Recommended site for infant Located at the middle third of the anterior lateral aspect of the thigh Assume back-lying or sitting position d. Rectus Femoris site Located at the middle-third, anterior aspect of the thigh
e. Deltoid site Not used often for IM injection because it is relatively small muscle and is very close to the radial nerve and radial artery To locate the site, palpate the lower edge of the acromion process and the midpoint on the lateral aspect of the arm that is in line with the axilla. This is approximately 5cm(2 in) or 2 to 3 fingerbreadths below the acromion process f. IM injection - Z tract injection Used for parenteral iron preparation. To seal the drug deep into the muscles and prevent permanent staining of the skin Retract the skin laterally, inject the medication slowly. Hold retraction of skin until the needle is withdrawn Do not massage the site to prevent leakage into the subcutaneous.
GENERAL PRINCIPLES IN PARENTERAL ADMINISTRATION 1. Check doctor's order 2. Check the expiration for medication - drug potency may increase or decrease if outdated 3. Observe verbal and non-verbal responses toward receiving injection. It can be painful, client may have anxiety, which can increase the pain 4. Practice asepsis to prevent infection. Apply disposable gloves 5. Use appropriate needle size. To minimize tissue injury 6. Plot the site of injection properly. To prevent hitting nerves, blood vessels, bones 7. Use separate needles for aspiration and injection of medications to prevent tissue irritation 8. Introduce air into the vial before aspiration. To create a positive pressure within the vial and allow easy withdrawal of the medication 9. Allow a small bubble (0.2 ml) in the syringe to push the medication that may remain 10. Introduce the needle in quick thrust to lessen discomfort 11. Either spread or pinch muscle when introducing the medication. Depending on the size of the client 12. Minimized discomfort by applying cold compress over the injection site before introduction of medication to numb nerve endings 13. Aspirate before introduction of medication. To check if blood vessel had been hit 14. Support the tissue with cotton swabs before withdrawal of the needle. To prevent discomfort of pulling tissues as needle is withdrawn 15. Massage the site of injection to haste absorption 16. Apply pressure at the site for few minutes. To prevent bleeding 17. Evaluate effectiveness of the procedure and make relevant documentation.
METHOD OF DRUG ADMINISTRATION INTAVENOUSLY 1. A mixture within large volumes of IV fluids 2. By injection of bolus, or small volume, or medication through an existing intravenous infusion line or intermittent venous access (heparin or saline lock) 3. By "piggyback" infusion of solution containing the prescribed medication and a small volume of IV fluid through an existing IV line Most rapid route of absorption of medications Predictable, therapeutic blood levels of medication can be obtained The route can be used for clients with compromised gastrointestinal function or peripheral circulation Large dose of medications can be administered by this route The nurse must closely observe the client for symptoms of adverse reactions The nurse should double-check the six rights of safe medication If the medication has an antidote, it must be available during administration When administering potent medications, the nurse assesses vital signs before, during and after infusion
NURSING INTERVENTIONS IN I.V. INFUSION a. Verify doctor's order b. Know the type, amount, and indication of IV therapy c. Practice strict asepsis d. Inform the client and explain the purpose of IV therapy to alleviate client's anxiety e. Prime IV tubing to expel air. This will prevent air embolism f. Clean the insertion site of IV needle from center to the periphery with alcoholized cotton ball to prevent infection g. Shave the area of needle insertion if hairy. Ask permission to the client h. Change the IV tubing every 72 hours. To prevent contamination i. Change IV needle insertion site every 72 hours to prevent thrombophlebitis j. Regulate IV every 15-20 mins. To ensure administration of proper volume of IV fluid as ordered k. Observe for potential complications.
THREE TYPES OF I.V. FLUIDS a. Isotonic solution - it has the same concentration as the body fluid. D5W
Plain Ringer's lactate
NaCl 0.9%
Plain normosol M
b. Hypotonic - has lower concentration than the body fluids. Too much of this fluid can swell the body's cell. NaCl 0.3% c. Hypertonic - has higher concentration than the body fluids. Too much of this fluid can make the body's cell shrink. D10W
D5LR
D50W
D5NM
COMPLICATIONS OF I.V. INFUSION 1. Infiltration - the needle is out of vein, and fluids accumulate in the subcutaneous tissues. Assessment Pain, swelling, skin is cold at needle site, pallor of the site, flow rate has decreases or stops Nursing Intervention: Change the site of the needle Apply warm compress. This will absorb edema fluids and reduce swelling 2. Circulatory Overload- this complication of I.V. infusion results from administration of excessive volume of I.V. fluids. Assessment Headache, flushed skin, rapid pulse Increase BP, weight gain, syncope and faintness Pulmonary edema, increase volume pressure Coughing, tachycardia, shock Nursing Intervention: Slow I.V. infusion to KVO - at least 10 gtts/min Place patient in high-fowler's position to enhance breathing Administer diuretic, bronchodilator as ordered.
3. Drug Overload - this complication of I.V. infusion occurs when the patient receives an excessive amount of fluid containing drugs Assessment Dizziness, shock Fainting Nursing Intervention: Slow I.V. infusion to KVO Take vital signs Notify the physician 4. Superficial Thrombophlebitis - this complication of I.V. infusion is due to overuse of a vein, irritating solution or drugs, clot formation, large bore catheters Assessment Pain along the course of vein Vein may fell hard and cordlike Edema and redness at needle insertion site Arm feels warmer than the other arm Nursing Intervention Change I.V. site every 72 hours Use large veins for irritating fluids Stabilize venipuncture at area of flexion Apply cold compress immediately to relieve pain and inflammation; later with warm compress to stimulate circulation and promotion absorption Do not irrigate the I.V. because this could push clot into the systemic circulation 5. Air Embolism - air manage to get into the circulatory system; 5 ml of air or more causes air embolism. Take note that it is a life-threatening conditio9n. Assessment Chest, shoulder or back pain Hypotension Dyspnea Cyanosis Tachycardia Increase venous pressure Loss of consciousness Nursing Intervention Do not allow the I.V. bottle to run dry Prime I.V. tubing before starting infusion Turn patient to left side in the trendelenburg position. To allow air to rise in the right side of the heart. This prevent pulmonary embolism
6. Nerve Damage - this complication of I.V. infusion result from trying the arm too tightly to the splint Assessment Numbness of fingers and hands Nursing Intervention Massage the area and move shoulder through its ROM Instruct the patient to open and close hand several times each hour Physical therapy may be required Take note: apply splint with the fingers free to move 7. Speed Shock - This complication of I.V. infusion result from administration of I.V. push medication rapidly. To avoid speed shock and possible cardiac arrest, give most I.V. push medication over 3 to 5 mins.
OBJECTIVES OF BLOOD TRANSFUSION THERAPY 1. To increase circulating blood volume after surgery, trauma, or hemorrhage 2. To increase the number of RBC's and to maintain hemoglobin levels in clients with severe anemia 3. To provide selected cellular components as replacements therapy (e.g. clotting factors, platelets, albumin) Nursing Interventions of Blood Transfusion Therapy (note: consent is needed) 1. Verify doctor's order. Inform the client and explain the purpose of the procedure 2. Check for cross matching and typing. To ensure compatibility 3. Obtain and record baseline vital signs 4. Practice strict asepsis 5. At least 2 licensed nurses check the label of the blood transfusion. Check the following: Serial number Blood component Blood type
Rh factor Expiration date
Screening test (VDRL, HBsAg, malarial smear) - to ensure that the blood is free from bloodcarried diseases and therefore, safe from transfusion 6. Warm blood at room temperature before transfusion to prevent chills 7. Identify client properly. Two nurses check the client's identification 8. Use needle gauge 18 to 19. This allow easy flow of blood 9. Use BT set with special micron mesh filter. To prevent administration of blood clots and particles 10. Start blood transfusion therapy slowly at 10 gtts/min. Remain at bedside for 15-30 mins. Adverse reaction usually occurs during the first 15 to 20 mins
11. Monitor vital signs. Altered vital signs indicate adverse reaction: Do not mix medication with blood transfusion. To prevent adverse effects Do not incorporate medication into the blood transfusion Do not use blood transfusion line for I.V. push of medication 12. Administer 0.9% NaCl before, during, or after Blood Transfusion Therapy. Never administer I.V. fluids with dextrose because it causes hemolysis 13. Administer Blood Transfusion Therapy for 4 hrs (whole blood, packed RBC). For plasma, platelets, cryoprecipitate, transfuse quickly (20 mins) clotting factor can easily destroyed.
COMPLICATIONS OF BLOOD TRANSFUSION 1 Allergic Reaction - this type of complication of blood transfusion is caused by sensitivity to plasma protein of donor antibody, which reacts with recipient antigen Assessment: Flushing Rush, hives Pruritus Laryngeal edema, difficulty of breathing 2. Febrile, Non-Hemolytic - this type of complication of blood transfusion is caused by hypersensitivity to donor white cells, platelets or plasma proteins. This is the most symptomatic complication of blood transfusion Assessment: Sudden chills and fever Flushing Headache Anxiety 3. Septic Reaction - this type of complication of blood transfusion is caused by the transfusion of blood or components contaminated with bacteria Assessment: Rapid onset of chills Vomiting Marked hypotension High fever
4. Circulatory Overload - this type of complication of blood transfusion is caused by administration of blood volume at rate greater than the circulatory system can accommodate Assessment: Rise in venous return Dyspnea Crackles or rales Distended neck vein Cough Elevated blood pressure 5. Hemolytic Reaction - this type of complication of blood transfusion is caused by infusion of incompatible blood products Assessment: Low back pain (first sign). This is due to inflammatory response of the kidneys to incompatible blood Chills Feeling of fullness Tachycardia Flushing Tachypnea Hypotension Bleeding Vascular collapse Acute renal failure NURSING INTERVENTIONS WHEN BLOOD TRANSFUSION COMPLICATIONS OCCUR 1. The first thing to do when complications in blood transfusion occurs is to STOP TRANSFUSION 2. Then start or open I.V. line (0.9%NaCl) 3. Place the client in fowler's position and administer oxygen therapy depending in the hospital protocol 4. Check vital signs as often as 5 mins 5. Notify the doctor immediately about the complications of blood transfusion 6. Carry out doctor’s order; prepare the emergency drugs like antihistamines, vasopressor, fluids as protocol 7. Obtain urine specimen and send to the laboratory to determine presence of hemoglobin as a result of RBC hemolysis 8. Blood container, tubing, attached label, and transfusion record are saved and returned to the laboratory for analysis.
HERBAL MEDICINES Aloe Vera - treatment for minor burns, insect bites, sunburns, dandruff, oily skin, psoriasis Chamomile - relief of digestive and GI disturbances Dong Quai - treatment for menstrual cramps and to regulate the menstrual cycle Echinacea - Immune enhancer - Treatment for respiratory and urinary tract infection - Treatment for snake bites Feverfew - relief of migraine headache Garlic - To lower cholesterol and triglyceride levels - To decrease BP; decrease clotting capability of the blood Ginger - boosts the immune system - To treat stomach and digestive disorders - Relief from nausea - Relief from pain, swelling, and stiffness for arthritis Giangko - Antioxidant: peripheral vasodilatation and increase blood flow to CNS; reduces platelet aggregation - Treatment for allergic rhinitis, Alzheimer‟s disease, anxiety, stress, dementia, Raynauld‟s disease, tinnitus, vertigo, impotence, poor circulation Ginseng - Relief of stress; to boost energy; to give digestive support - supports immune system and prevents chronic infection Goldenseal - To ward off infection and promote wound healing - To treat congestion associated with common cold Kava – kava - Root promotes sleep and muscle relaxation
- Treats UTI Licorice - Effects are similar to aldostrone and corticosteroid - relieves heartburns and indigestion - treat ulcers Milk Thistle - To prevent liver damage Peppermint - stimulates appetite to eat; aids in indigestion - Treatment of bowel disorders - stimulates circulation; reduces fever; clears congestion; restores energy - Peppermint oil is used as treatment for tension headache St. John’s Wort “herbal Prozac” - Antidepressant, antiviral activity Saw Palmetto “plant catheter” - relieves symptoms of BPH and urinary conditions Valerian “herbal valium” - sleep-inducing agent Billberry - promotes healthy vision; relieves diarrhea in children - Leaf is used for diabetes, arthritis, dermatitis, gout Black Cohosh - suppresses LH; increases estrogen level - has antispasmodic, astringent, diuretic, vasodilator effects - relieves PMS, dysmenorrheal, infertility, menopausal symptoms Cranberry - Prophylaxis for UTI Evening Primrose - Natural estrogen promoter - Treatment for PMS, diabetic neuropathies, chronic inflammatory conditions Hawthorn - promotes peripheral vasodilation; increases coronary circulation, acts as an antioxidant - Treatment for early CHF, stable angina
V. ASEPSIS AND INFECTION CONTROL Handwashing – is the single, most effective practice to prevent spread of microorganisms. 4 Elements of Handwashing 1. Water 2. Friction 3. Soap 4. Time
Body Defenses against Infection - Normal flora - Intact skin - Saliva and mucus membrane - Cilia of the upper respiratory tract infection - Inflammatory process - Immune response
ASEPSIS 1. Medical Asepsis – Clean technique - reduces number of pathogens -GIT - Handwashing removes microorganism 2. Surgical Asepsis - Sterile technique - make object free of all microorganisms - Dressing, catheterization and Surgical procedures and Specimen collection
Sterile Technique Guidelines 1. Never turn your back on a sterile field 2. Avoid talking 3. Keep all sterile objects within view 4. Moisture will carry bacteria across/ through a cloth or paper barrier 5. Open all sterile packages away from the sterile field to prevent crossover and contamination
Principles and Practices of Surgical Asepsis - All objects use in the sterile field must be sterile - Sterile objects remain sterile when touched by another sterile object - Sterile objects or fields which fall out of the range of vision or below one‟s waist are considered contaminated - Sterile items become contaminated when they come in contact with microorganism transported through the air - When sterile object/field comes in contact with another surface, it becomes contaminated - The edges of the sterile field are considered unsterile
Standard Precaution - To be used in all clients in the hospital - To be used in the following situations: a. contact with blood, body fluid, excretions and secretions b. contact with non-intact skin c. contact with mucous membrane - wash hands after contact with blood, body fluids, secretions, excretions, or contaminated objects - wear gloves when touching blood, body fluids, secretions, excretions or contaminated objects - wear mask, goggles, or face shield if there is potential for splashes or sprays of blood, body fluids, secretions or excretions to prevent splashing into the eyes or mucous membranes
- Use biohazard bag for linens soiled with blood, body fluids, secretions, or excretions - Place sharps or needles in puncture-resistant container - do not recap, bend, or break needles
Airborne Precaution Measles Varicella Tuberculosis - use private room (negative airflow room) - close the door at all times
Use HEPA filters (High-Efficiency Particulate Air) - Particulate respirator/mask for health care workers - Surgical mask for patient during transport - discard tissue wipes with sputum in plastic bags
Droplet Precautions Pneumonia Meningitis Rubella Scarlet fever Diphtheria Pertussis - use surgical mask Use disposable eating utensils
Contact Precautions Herpes simplex Staphylococcal infection Hepatitis A Respiratory syncytial virus (RSV) Wound/skin infection Methicillin-resistant staphylococcal aureus (MRSA) Vancomycin-resistant enterocolitis (VRE) Rotavirus infection (most common cause of diarrhea in the U.S.) - use gloves, gown (if clothing comes in contact with patients, environmental surfaces, or items in the room, if patient has diarrhea, wound drainage, or GI surgery).
TIME FOR A SHORT QUIZ 1. Which of the following is an appropriate nursing action when implementing standard precautions? A. Consider all body substances potentially infectious B. wear gloves whenever in contact with patient C. wear gown and gloves when caring for a client in droplet precaution D. place a body substance isolation sign on the client's door
2. Which of the following clients would qualify for hospice care? A. a client with metastatic cancer B. a client with left-side after a stroke C. a client who had coronary artery bypass surgery 1 week ago D. a client who is undergoing treatment for heroin addiction
3. For a hospitalized client, which statement reflects appropriate documentation in the client's medical record? A. "client had a good day" B. "seems to be mad at the physician" C. "small pressure ulcer noted at the lower back" D. "skin moist and cool" 4. The nurse will administer the client's 9 A.M. medications. The client is away from his room for ultrasound of the liver. Which nursing action is appropriate? A. have the client skip that B. ask the client's relatives to keep the medications for the client until he returns C. lock the medications in the medicine preparation area until the client returns D. leave the medications on the drawer of the client's bedside table 5. The nurse is caring for a client receiving patient-controlled analgesia (PCA) for pain management. Which statement about PCA is true? A. the PCA pump can‟t' infuse opioids continuously B. pain relief is initiated by the client as needed C. no complications related to opioid delivery by the pump exist D. the nurse prescribes the dosage of opioid for delivery dose of medication ANSWERS AND RATIONALE 1. A - Rationale: standard precautions are based on the concepts that all body substances are potentially infectious. The nurse should wear gloves when contact with body substances is potential, not when in contact with intact skin. Mask should be used as a barrier to prevent transmission of droplet infections. Signs on door are unnecessary for standard precaution. 2. A - Rationale: hospices provide supportive, palliative care to terminally ill clients and their families 3. D - Rationale: documentation should be factual and accurate, what are heard, seen, smelled, or felt. Documentation of ulcer should include exact size and location. Interpretations, conclusions, opinions should not be documented. 4. C - Rationale: the nurse must put the medicines in the secured area. She should not leave the medications at the bedside. The nurse should not omit doses of medications without physician's order 5. B - Rationale: the client pushes a button to self-administer narcotic analgesic. The PCA pump also allows for continuous infusions of the medication. The client may still experience complications of the medication. It is the physician who prescribes the medication order
VI. COMPUTATION OF DOSAGE OF MEDICATIONS 1. Oral Medication: Solids Desired dose / stock dose = quantity of drug D/S = Q 2. Oral/Parenteral Medications: Liquids Desired dose / stock dose x dilution = quantity of drug D/S x dilution = Q 3. IV fluids Rate a. gtts/min = volume in cc x gtt factor no. of hours x 60 min b. cc/hr = volume in cc or gtts/min x 4 no. of hours c. duration in hours = volume in cc cc/hr 4. Conversion of Temperature a. C to F = (C x 1.8) + 32 note: (1.8 is 9/5) b. F to C = (F – 32) (0.55) note: (0.55 is 5/9) Time for a Short Quiz ! ! ! 1. An antihypertensive agent, minoxidil (Loniten) 5mg p.o. is ordered. Stock is 2.5 mg/tab. How many tablets should be administered? 2. The expectorant guiafenesin (Robitussin) 300 mg. p.o. has been ordered. The bottle is labeled 100 mg/5 ml. How many ml should be given? 3. The physician‟s order reads: “Administer D5LR 3L for 24 hours.” a. to how many gtts/min will you regulate the IVF? b. how many ml/hr will be infused? 4. 38.3C equals how many degrees Farenheit? 5. 108.6F equals how many degrees Celsius?
ANSWERS 1) D/S = Q 5mg . 2.5mg/tablet = 2 tablets 2) D/S x dilution = Q 300 mg x 5 ml 100 mg = 15 ml 3) a) vol. in cc x gtt factor = gtts/min no. of hours x 60 min 3,000 cc x 15 24 x 60 45,000/1440 = 31 gtts/min b) cc/hr vol in cc no. of hrs = 3,000 cc / 24 hrs = 125 cc/hr 4) C to F = C x 1.8 + 32 = (38.3 x 1.8) + 32 = 68.9 + 32 = 100.9 F 5) F to C = (F – 32) (0.55) = (108.6 – 32) (0.55) = (76.6) (0.55) = 42.1 F
VII. NORMAL VALUES 1. Complete Blood Count (CBC) RBC (erythrocytes) – 4.5 – 5.5 million/cu.mm WBC (leukocytes) – 5,000 – 10,000/cu.mm Platelet s (thrombocytes) – 150,000 – 450,000/cu.mm 2. Hemoglobin (hgb) = 12 -17 G/dL 3. Hematocrit (hct) male: 42 – 52% Female: 40 - 48% 4. Differential Count (Leukocytes) Neutrophils – 60 – 70% Eosinophils – 1 -4% Basophils – 0 – 0.5% Lymphocytes – 20 – 30% Monocytes – 2 – 6% 5. Blood Coagulation Studies Prothrombin Time (PT) = 11 – 16 sec Partial Thromboplastin Time (PTT) = 60 – 70 sec Activated Partial Thromboplastin Time (APTT) = 30 – 45 sec Bleeding Time = 1 – 9 sec Clotting Time = 8 – 15 sec 6. Blood Urea Nitrogen (BUN) = 8 -25 mg/dL 7. Blood Lipids Serum Cholesterol = 150 – 200 mg/dL Serum Triglycerides = 140 – 200 mg/dL Low Density Lipoprotein (LDL) = less than 130 mg/dL High Density Lipoprotein (HDL) = 30 – 70 mg/dL
8. Serum Enzymes Studies Aspartate Amino Transferase (AST/SGOT) = 7 – 40 U/ml Alanine Aminotransferase (ALT/SGPT) = 10 -40 U/ml Creatine Phosphokinase (CK-MB) Male: 50 – 325 mU/ml Female: 50 – 250 mU/ml 9. Troponin Troponin I = less than 0.6 ng/ml (grater than 1.5 ng/ml indicates myocardial infarction (MI) Troponin T = 0 to less than 0.1 ng/ml (greater than 0.1 – 0.2 ng/ml indicate MI) 10. Blood Uric Acid (BUA) = 2.5 – 8mg/dl 11. Serum Electrolytes Potassium (K+) = 3.5 – 5.5 mEq/L Sodium (Na+) = 135 – 145 mEq/L Calcium (Ca+) = 4.5 – 5.5 mEq/L Magnesium (Mg+) = 1.5 – 2.5 mEq/L 12. ECG Complexes P – wave = 0.04 – 0.11 sec PR interval = 0.12 – 0.20 sec QRS complex = 0.05 – 0.10 sec T – wave = not exceed 5mm amplitude 13. Central Venous Pressure (CVP) = 5 – 12 cm H2O 14. Pulmonary Artery Pressures Pulmonary Artery Pressure (PAP) = 4 – 12 mmHg Pulmonary Capillary Wedge Pressure (PCWP) = 4 – 12 mmHg 15. Serum Ammonia = 40 – 80 mcg/dL
16. Blood Glucose Level Fasting Blood Glucose (FBG) = 70 – 110 mg/dL Glycosylated Hemoglobin (HbAIc) = 4.4 – 6.4% (7.5% or less: good diabetic control) 17. Thyroid Hormone Levels Triiodothroxine (T3) = 75 = 200 ng/dL Thyroxine (T4) = 4.5 – 11.5 mcg/dL 18. Routine Urinalysis Color = amber/straw pH = 4.5 – 8 (average: 6; slightly acidic) specific gravity = 1.010 – 1.025 protein = absent RBC = 0 – 5 Pus = absent Ketones = absent Casts = 0 – 4 19. Creatinine Clearance = 100 – 120 ml/min 20. Serum Creatinine = 0.7 – 1.4 mg/dL 21. Snellen’s Test = 20/20 22. Intraocular Pressure = 11 -21 mmHg 23. Cerebrospinal Fluid (CSF) Studies Opening pressure = 0 – 15 mmHg or 75 – 180 mm H20 Glucose = 50 – 80 mg/dL Protein = 20 – 50 mg/dL 24. Arterial Blood Gas Analysis Blood pH = 7.35 – 7.45
HCO3 = 22 – 26 mEq/L
Pa O2 = 80 – 100 mmHg
O2 saturation = 95 – 100 %
paCO2 = 35 – 45 mmHg Note: O2 saturation 90% and below indicate that hypoxia is severe
25. Therapeutic Serum Medication Levels Acetaminophen = 10 – 20 mcg/dL Phenytoin (Dilantin) = 10 – 20 mcg/dL Theophylline = 10 – 20 mcg/dL Carbamazepine (tegretol) = 5 – 12 mcg/dL Gentamycin Sulfate = 5 – 10 mcg/dL Magnesium Sulfate = 4 – 7 mg/dL Digoxin = 0.5 – 2 ng/ml Lithium = 0.5 – 1.5 mEq/L Coumadin = INR: 2 – 3
VIII. NUTRITION AND DIET Macronutrients (energy nutrients) 1. Carbohydrates (Go) – provides energy Sources: cereals, fruits, vegetables, milk Caloric deficiency is referred to as Marasmus, characterized by loss of weight, skin turgor, old-man look, distended abdomen, hypotonia Nursing Considerations for Carbohydrates High: bipolar disorder, manic phase; associated in obesity; associated in colon and breast cancer; for Marasmus Low: diarrhea; gas distention; diabetes mellitus 2. Fat (Glow) – provides essential fatty acids and energy; absorbs and transports fatsoluble vitamins (A, D, E, K); protects vital body tissues; insulates body Sources: fats and oils, meats, fish, nuts, some seeds, dairy products Nursing Considerations for Fats High: dumping syndrome, ulcer, when taking ADEK Low: acne vulgaris, pancreatitis, cholecystitis, cardiac patient
3. Protein (Grow) – growth and repair of tissues; maintain fluid and acid-base balances, provides energy. Sources: meat, fish, dairy products, eggs, nuts, legumes, cereals Protein deficiency is referred to as Kwashiorkor, characterized by lethargy, inadequate growth, loss of muscular tissue, increases susceptibility to infection, EDEMA Nursing Considerations for Protein High: hepatitis, PIH, nephrotic syndrome, burn patient Low: chronic renal failure, PKU, liver cirrhosis
MICRONUTRIENTS (VITAMINS AND MINERALS) Fat – Soluble Vitamins 1. Vitamin A (Retinol) – affects vision; health of skin; growth of hair, nails, bones, and glands; prevents infection Sources: dairy product, liver, green, yellow and orange fruits and vegetables Deficiency: night blindness, xeropthalmia, poor growth, dry skin Toxicity: fetal malformations, hair loss, skin changes, bone pain Nursing Considerations for Vitamin A Not to excessive especially amongst small children, it might cause discoloration of the skin 2. Vitamin D (Ergocalciferol) – Calcium not absorbed without Vit. D. Calcium and phosphorus absorption; bone mineralization Sources: dairy products, eggs, yolks, fatty fish Deficiency: Rickets in children, Osteomalacia for adults Toxicity: growth retardation, kidney damages, calcium deposits in soft tissue Nursing Considerations for Vitamin D Breast-fed infant must be exposed to mild sunlight Must receive by those who are receiving calcium supplement
3. Vitamin E (Tocopherol) – Antioxidant: prevents cell damage Sources: vegetable oils, nuts, seeds, whole grain Deficiency: red blood cell destruction, nerve destruction Toxicity: None, no supplements with anticoagulant drugs Nursing Considerations for Vitamin E To prevent premature aging Commonly given to client with dementia 4. Vitamin K (Menadione) – blood clotting Sources: green vegetables, intestinal synthesis Deficiency: hemorrhage Toxicity: anemia, jaundice Nursing Considerations for Vitamin K Commonly given to neonate to prevent bleeding (note: neonates have sterile intestine) Antioxidant to Coumadin Water – Soluble Vitamins 1. Vitamin C (Ascorbic Acid) – required for iron absorption. Antioxidants: prevents cell damage; causes collagen formation; affects health of teeth and gums Sources: citrus fruits, guava, strawberries, tomatoes, broccoli, cabbage, greens, potatoes Deficiency: Scurvy, poor wound healing, weakness, impaired immune response, pin point hemorrhages, bleeding gums Toxicity: more than 2g can cause diarrhea, kidney stone formation. Most renal calculi thrive in acid urine. GI upsets, fatigue
2. Vitamin B1 (Thiamine) – muscle nerve function; co-enzyme for energy metabolism Sources: pork liver, organ meats, nuts, legumes, eggs, milk, whole and enriched grains. Potatoes Deficiency: Beriberi, poor coordination, edema, weakness Nursing Considerations for Vitamin B1 Those with increased metabolic rate should increase B1 (e.g. pregnant women and client with fever) Alcoholic client 3. Vitamin B2 (Riboflavin) – coenzyme for energy metabolism Sources: milk, dairy products, organ meats, lean meats, enriched grains, green leafy vegetables, fish, eggs For skin problem such as eczema and scabies
4. Vitamin B3 (Niacin) - coenzyme for energy metabolism Sources: kidney, liver, poultry, lean meat, fish, peanut butter, dried peas and greens, whole grain, nuts Deficiency: ariboflavinosis, cheilosis, glossitis, seborrheic, dermatitis, pellagra Toxicity: vasodilation, liver damage 5. Vitamin B6 (Pyridoxine) – supplemented in anti-TB therapy as drugs compete with absorption of B6. Metabolism of amino acids and protein, neurotransmitter synthesis. Sources: meats, poultry, fish, organ meats, yeast, oats, corn, peanuts, bananas, egg yolk, whole grain cereals, wheat germ, potatoes Deficiency: headache, anemia, convulsion, nausea Toxicity: nerve destruction if >2g/day Nursing Considerations for Vitamin B6 For patient who is receiving INH to prevent peripheral neuritis For those who are taking contraceptives
6. Vitamin B9 (Folacin/Folic Acid) – aids metabolism of DNA and RNA; red blood cell maturation Sources: green leafy vegetables, asparagus, organ meats, beef, fish, legumes, eggs, yeast, wheat germ, grapefruits and orange. Deficiency: megaloblastic anemia, poor growth, birth defects 7. Vitamin B12 (Cyanocobalamine) – requires intrinsic factor for absorption in the stomach. This is not absorbed in Pernicious Anemia. - Folate metabolism, nerve function. Sources: liver, kidney meat, oyster, cheese, eggs, shrimp, milk Deficiency: megaloblastic anemia, poor nerve function MINERALS 1. Potassium (K) – major intracellular cation. - given with furosemide - fluid balance, nerve and muscle function Sources: bananas, avocado, strawberries, cantaloupe, oranges, mushrooms, carrots, spinach, tomatoes, potatoes, raisins (other dried fruits), fish, beef, veal, pork Deficiency: muscular weakness, fatigue, confusion Toxicity: muscular weakness, cardiac arrest 2. Iron (Fe) – components of hemoglobin and enzymes Sources: liver, meat, dark-green vegetables, green and red beans (dried beans), egg yolk, breads, cereals, clams Deficiency: anemia, weakness, infections, fatigue, pale eye membranes Toxicity: Acute: shock, death. Chronic: liver damage, cardiac failure Nursing Considerations for Iron Must be given between meals If given per orem: black stool If liquid: use straw If injectible: don’t massage
3. Calcium (Ca) - 99% of calcium is in the bone - Major component of renal calculi - if increased, calcitonin is given - Bone and tooth formation; blood clotting; muscle function; nerve transmission; blood pressure Sources: yogurt, low fat milk and dairy products, green leafy vegetables, broccoli, carrots, seafood, nuts, legumes, whole grains, rhubarb Deficiency: stunted growth in children; bone loss (osteoporosis) in adults Toxicity: extra calcium usually excreted; possible depressed absorption of some other minerals and kidney damage 4. Sodium (Na) - Water goes to where Na is ! - given with lithium carbonate - fluid balance, nerve impulse transmission Sources: table salt, soy sauce, cured pork, milk, butter, ketchup, canned food, processed foods, white and whole wheat bread, cheese, mustard, snack foods Deficiency: muscle cramps, reduced appetite, weakness Toxicity: high blood pressure in some people
IX. THERAPEUTIC DIETS Acid-ash diet retards the formation of alkalinic renal stones indicated to patients with renal calculi (Alkaline stones) e.g. cheese, cranberries, eggs, meat, plums, prunes, whole grains Alkaline ash diet retards the formation of acid renal stones indicated to patients with renal stones (Acidic stones) e.g. fruits (except cranberries, plums, prunes), milk, vegetables
Bland diet low fiber, mechanical irritants, chemical stimulants indicated for patients with gastritis, diarrhea, biliary indigestion, and hiatal hernia BRAT diet banana, rice, apple, toast indicated for patients with diarrhea Butterball diet spare protein but high in carbohydrates indicated for patients with liver disorders Clear liquid diet to relieve thirst and help maintain fluid balance indicated for post-operative patients and following vomiting and gastroenteritis Diabetic diet well balance diet the purpose is to maintain near to normal blood glucose level indicated to patients with diabetes mellitus Full Liquid diet it serves to provide nutrition to patients who cannot chew or tolerate solid foods indicated to patients with stomach upsets, post-surgical patients, after progression from clear liquid diet Giordano diet spare protein indicated to patients who suffers from Chronic Renal Failure
Gluten free diet no to BROW - Barley, Rye, Oat, Wheat this is the diet of a patient who suffers from Celiac's disease Halal diet no pork diet diet of the Moslems High fiber diet fruits and vegetable it speeds up the passage of food to the digestive tract, softens the stool indicated to patients who are constipated, with diverticulitis, with hyperlipedemia (to initiate removal of fats) High Protein diet lean-meat, cheese, eggs indicated to patients with nephrotic syndrome Kosher diet meat and milk cannot be served simultaneously diet of the Orthodox Jews Low carbohydrate diet indicated to patients with Dumping Syndrome Low fat/cholesterol diet it serve the purpose of reducing hyperlipidemia, and to patients with intolerance to fats indicated to patients with cardiovascular diseases, patients who underwent resection of the small intestines, hypertension, cholecystitis and cholelithiasis Low residue diet reduces the bulk of stools
indicated to patients with ulcerative colitis, diverticulitis. Patients who will undergo surgery of the GI tract Low sodium diet indicated to patients with cardiovascular and renal disorder Purine restricted diet to reduce uric acid indicated to patients with gouty arthritis, renal calculi, and hyperuricemia Sodium-restricted diet indicated to patients with heart failure, hypertension, renal diseases, PIH, and steroid therapy Soft diet used to provide nutrition for those patients having problems in chewing for patients with ill-fitting dentures; transition from full-liquid to general diet, patients with gastrointestinal disturbances such as gastric ulcers and cholelithiasis Tyramine-free diet use to prevent hypertensive crisis for patients who are taking in MAOI antidepressant no to ABC's - Avocado, Banana, Canned and Processed Foods, and also, no to fermented foods Vegan diet diet of the Seventh Day Adventists vegetarian diet Yin diet Cold deserts after a surgery. It is a Chinese belief
X. POSITIONS I. Positions for clients with Respiratory Disorders After lung Biopsy: Affected Side - To apply pressure in the site and prevent bleeding During Thoracentesis: Upright or Sitting Position at the edge of the bed, arms on overbed table, leaning forward, and feet supported on a foot stool - For easy access to the site of insertion of aspiration needle. It also promotes comfort. After Thoracentesis: Unaffected side for 1 hour to prevent leakage of fluid into the thoracic cavity. Client on Oxygen Therapy: Semi-Fowler’s position - For lung expansion and ventilation. During Tracheostomy or Endotracheal Tube Suctioning: Semi-Fowler’s position - To facilitate suction catheter insertion and enhance removal of mucous membrane . After Bronchosgraphy and Bronchoscopy: Side-lying/lateral or semi-fowler’s position - To promote drainage of secretions from the mouth and prevent aspiration. COPD: Sitting Upright, leaning forward position, with arms on overbed table at shoulder level (orthopneic position) - To allow lung expansion. Epistaxis: Sitting/Upright position, leaning forward with head tipped - To prevent aspiration of blood. After Tonsillectomy: Side lying/lateral or prone position with pillow under the chest To promote drainage of mouth secretions and prevent aspiration. If client is awake, maybe placed in semi-fowler’s position. Pulmonary Edema: High-Fowler’s position with legs slightly dependent (lowered) - To relieve dyspnea. Lowering the legs reduces venous return thereby reduces cardiac workload. Pneumonectomy: Slightly towards affected side, with head elevated or Semi-Fowler’s position for lung expansion - To prevent flooding of blood coming from the affected side to the remaining lung. Slight turning prevents mediastinal shift. Flail Chest: Semi-fowler’s position, turned towards the affected side or the affected side be supported - To control paradoxical breathing and prevent hypercapnea. Child with Epiglottitis, laryngotracheobronchitis, bronchiolitis: Tripod position (sitting upright, leaning forward with hands on the bed or floor) – to facilitate breathing. SIDS (Sudden Infant Death Syndrome): Supine or Side-lying position in a firm bed during sleep. Do not place the infant in prone position during sleep. Do not place infant in soft bed or over a pillow or comforter.
II. Positions for clients with Cardiovascular and Hematologic Disorders Myocardial Infarction (MI): Semifowler’s position – for maximum lung expansion and improves myocardial oxygenation. Congestive Heart Failure (CHF): High-fowler’s position – it relieves dyspnea and reduces cardiac workload. When taking Nitroglycerin: Sitting or Supine position – to prevent orthostatic hypotension Arterial Insufficiency: Lower extremities slightly lower than the level of the heart (dependent position) – it promotes arterial flow Venous Insufficiency: Lower extremities elevated – it promotes venous return and relieves edema of the legs. Tetralogy of Fallot in “tet spell” (hypoxic episode): Knee-to-Chest position or Squatting position – to improve venous return, increases cardiac output and improve tissue oxygenation. Air Embolism: Left Side-lying position, Trendelenburg position – it allows the air to be absorbed in the right side of the heart thus prevents pulmonary embolism.
III. Positions for clients with Gastrointenstinal, hepato-Biliary and Pancreatic Disorders During Abdominal Examination: Dorsal recumbent position – to relax the abdominal muscles and facilitate abdominal examination. During Rectal Examination: Lateral/Side-lying position – to facilitate examination of the area. During Nasogastric tube (NGT) insertion: High-fowler’s position, with the neck hyperextended, initially. Flex the neck slightly once the tube reaches the oropharynx. During and after NGT feeding (gastric gavage) and Gastrostomy feeding: Semifowler’s position – to prevent reflux and aspiration of feeding. After insertion of Intestinal/Nasogastric Tube: Right Side-lying position – it helps advance the tube into the duodenum. During insertion of Parenteral Nutrition (TPN) Catheter: Trendelenburg position – to engorge the vein and facilitate insertion of the catheter to the subclavian vein. It also prevent air embolism. During Enema Administration: Left lateral position for adult. Dorsal Recumbent position for infant and children.
Hiatal Hernia: Upright/Sitting position during and after eating – To prevent gastroesophageal reflux. After Gastric and Biliary Surgery: Semi-fowler’s position – To promote lung expansion and ventilation and also prevents atelectasis. Dumping Syndrome: Left side-lying position – To slow down emptying of gastric content into the jejunum. Peritonitis: Semi-fowler’s position – To localize the inflammatory process in the pelvic area. Colostomy Irrigation: Semi-fowler’s position, then sitting on a bowl once ambulatory. After Hemorrhoidectomy: Side-lying position – It prevents pressure in the operated area and promote comfort. After Infant Feeding: Right side-lying position – It prevents gastroesophageal reflux and aspiration. After Cleft Lip Repair: Side-lying position – To promote drainage and prevent aspiration. No to Prone position to prevent tension on the suture line. Restraint the elbow to prevent trauma in the suture line. After Cleft Palate Repair: Side-lying and Prone position – to promote drainage and prevents aspiration. After repair of Imperforate Anus: Side-lying position or Supine with the legs suspended at the right angle – To prevent pressure in the area and minimize discomfort. During Liver Biopsy: Left Side – to facilitate approach to the liver After Liver Biopsy: Right Side with rolled towel under the puncture site – it helps apply pressure at the puncture site and prevent bleeding. During Paracentesis: Sitting/Upright position – it facilitates aspiration of abdominal fluid.
IV. Positions for clients with Fluid-Electrolyte, Acid-Base Imbalances, GenitoUrinary Disorders, Shock, Burns During insertion of Urinary Catheter: Supine with legs extended and abducted for male. Dorsal Recumbent for female. During Cyctoscopy: Lithotomy position – to promote easy insertion of cystoscope. During Renal Biopsy: Prone position – it is because the kidneys location is retroperitoneally. After Renal Biopsy: Supine position with small pillow or rolled towel under the posterior lumbar area to apply pressure and prevent bleeding. During insertion of Peritoneal Catheter: Dorsal Recumbent or Semi-fowler’s position with the knees flexed – To relax abdominal muscles and facilitates the insertion of the catheter. During Vaginal Examination: Dorsal Recumbent if she is in bed. Lithotomy position if the examination is done in the table. Shock: Modified Trendelenburg position – to increase venous return and increased force of cardiac contractility thus increases cardiac output and tissue perfusion. Burns: Supine position – To promote position of extension and prevent contractures.
V. Positions for clients with Neurologic Disorder During Lumbar Puncture: Lateral, Knee-chest position (fetal/flexed/C-position/shrimp position) – to widen intervetebral spaces and facilitate insertion of spinal needle. After Pantopaque (oil-based dye) myelogram: Lie Flat for 6 to 8 hours – to prevent spinal headache. After Metrizamide (water-based dye) myelogram: Semi-fowler’s position for 8 hours – to prevent meningeal irritation. Intracranial Pressure: Lateral, Semi-fowler’s position – to reduce the pressure, promote adequate lung expansion and improve cerebral tissue perfusion. Spinal Cord Injury: Flat/Supine position on a firm space – to maintain alignment of spine.
VI. Positions for clients with Eye and Ear Disorders After Eye Surgery: Supine position turned to the Unoperated Side – to prevent trauma to the affected eye. If the client is fully awake: Semi-fowler’s position. Retinal Detachment Preoperative: Dependent position (lower) – to prevent further detachment of the retina. Postoperative: Dependent position (upper) – to lower the sclera and choroids by gravity and allow attachment of the area of retinal detachment. After Ear Surgery: Unoperated Side – to prevent trauma to operated side.
XI. PROCEDURES ABDOMINAL ASSESSMENT Purpose - determine the presence of mass, abnormal bowel sounds, lesions, and other abnormalities in the abdominal region. Nursing Keypoints: Position: Dorsal Recumbent Sequence: (IAPP) Inspection, Auscultation, Percussion, Palpation. Start palpating from RLQ, RUQ to LUQ, to LLQ palpation is done last because it can possibly alter the bowel rhythms and may therefore give rise to abnormal sounds No to palpation to patients with Wilhm's tumor and abdominal Aortic Aneurysm
ARTERIAL BLOOD GAS ANALYSIS Purpose - to monitor the patient's response to oxygen therapy and detects the presence of acid-base imbalance. Nursing Keypoints: no to suctioning prior to obtain blood specimen assess for bleeding and hematoma at the puncture site apply firm pressure at the puncture site for 5-10 minutes specimen should be placed in iced-container Assess for metabolic alkalosis for patient with vomiting, and on the other hand, observe for signs and symptoms of metabolic acidosis for patients with diarrhea.
BARIUM ENEMA Purpose – To assess the large intestines Nursing Keypoints: provide a liquid diet before the procedure ensure that a laxative is given before the procedure to promote better visualization, and after the procedure to prevent constipation report to the doctor if bowel movement does not occur in 2 days instruct the patient to increase fluids and eat foods rich in fiber the patient should also increase intake of fluids
BARIUM SWALLOW Purpose - To assess for the esophagus, stomach, and some portion of the small intestines Nursing Alert: NPO for 6-8 hours before the procedure withhold anticholinergic and narcotics for 24 hours before test laxative is administered after the procedure to counteract the constipating effects of barium instruct patient to increase fluids and intake of fiber-riched foods
Bone Marrow Biopsy Purpose: aspirating bone marrow for laboratory studies. Preferred site is the iliac crest (proximal tibia in children), but may also use sternum, iliac spine Nursing Keypoints: administer sedative as ordered positioning (prone for iliac crest) pressure on the site for 5 to 10 minutes after aspiration placed on affected side (with sandbag underneath) assess for discomfort and bleeding at the site
CARDIAC CATHETERIZATION Purpose – To measure oxygen concentration saturation, tension and pressure in various chambers of the heart. To determine a need for cardiac surgery. Nursing Keypoints: check for informed consent assess allergy to iodine NPO for 6-8 hours before procedure check for distal pulses after the procedure check for bleeding at the arterial puncture site and apply pressure keep a 20 pounds sandbag at the bedside as a pressure instrument if bleeding occurs keep the patient flat on bed with the lower extremities hyperextended for 4-6 hours neurovascular assessment must be performed distal to the catheter insertion site and report any abnormal findings
CHEST X-RAY Purpose – To detect abnormalities of the organs in the thoracic area Nursing Keypoints: remove any metallic object before the procedure lead shield for women of childbearing age
CYSTOSCOPY Purpose – To assess the bladder and urethra Nursing Keypoints: if general anesthesia will be used, have the client on NPO; liquid diet if local anesthesia will be used monitor intake and output after the procedure, force fluids as prescribed administer sitz bath for abdominal pain pink-tinged or tea-colored urine is expected within 24-48 hours notify the doctor if bright red urine or clots occur
CT SCAN Purpose – Provides photograph of tissue densities with the use of radiation Nursing Alert: if contrast medium will be used, assess for any allergy to iodine and instruct the patient to be on NPO for 4 hours prior to procedure assess for any fear of close spaces (claustrophobia) this procedure is contraindicated to patients who are pregnant and obese (>300 lbs) Let the patient lye still during the whole course of the procedure.
CVP (CENTRAL VENOUS PRESSURE) MONITORING Purpose – It measures the pressure of the right atrium Nursing Keypoints: the nurse should place the zero level of the manometer at the level of the right atrium at the 4th intercostal space to get an accurate reading. instruct the client to avoid coughing and straining as it alters the readings normal CVP reading is 2-12 mmHg (when the tube is at the superior vena cava).
ELECTROCARDIOGRAM (ECG) Purpose – records electrical waves of the heart Nursing Keypoints: instruct the patient to lie still, breathe normally during the procedure let the patient refrain from talking during the test ST segment elevation or T wave inversion, indicates MI
ELECTROENCEPHALOGRAM (EEG) Purpose – records the electrical activity of the brain, detects intracranial hemorrhage and tumors Nursing Keypoints: advise the client to shampoo before and after the procedure. may use acetone after Withhold stimulants, antidepressant, tranquilizers, and anticonvulsants for 24-48 hours prior to the test.
FASTING BLOOD SUGAR (FBS) Purpose – detects diabetes mellitus Nursing Keypoints: normal blood sugar level is 80-120 mg/dl a blood sugar level of more than 140 mg/dl confirms diabetes
GASTRIC ANALYSIS Purposes – this test is used to detect ulcers and to rule-out pernicious anemia. It may also be done to analyze acidity, appearance and volume of gastric secretions Nursing Keypoints: in gastric ulcer, HCl is normal in duodenal ulcer, HCL is elevated refrigerate gastric samples if NOT tested within 4 hours
INTRAVENOUS PYELOGRAPHY (IVP) Purpose – visualization of the urinary tract Nursing Keypoints: NPO for 8-10 hours before the procedure administer laxative to clear bowels before the procedure check for allergy to iodine, seafood or shellfish before the procedure since the procedure requires the use of iodine based dye Keep epinephrine at the bedside to counteract possible allergic reaction. IVP requires the use of a contrast medium while KUB does not inform the patient about the possible salty taste that may be experienced during the test
LIVER BIOPSY Purpose – to determine liver disorders Nursing Keypoints: check for the consent obtain the result of blood tests before aspiration since bleeding may occur
let the patient to inhale, exhale and hold breath during the insertion of to stabilize position of the liver and prevent accidental puncture of the diaphragm position the patient on the right side after liver biopsy with pillows underneath to prevent bleeding bedside for 24 hours after the procedure
LUMBAR PUNCTURE Purpose – to withdraw CSF to determine abnormalities Nursing Keypoints: before the procedure: empty bladder and bowel position: C-position (fetal position) during the procedure: needle is inserted between L3-L4 or L4-l5 to prevent accidental puncture to the spinal cord since the spinal cord ends at L2 after: position the patient flat for 6-12 hours to prevent spinal headache increase fluid intake
MAMMOGRAPHY Purpose – detects the presence of breast tumor Nursing Keypoints: instruct the patient not to use deodorant, talcum powder, lotion, perfume or any ointment on the day of exam as these may give false-positive result let the patient know that her breasts will be compressed between 2 x-ray plates provide teachings related to self-breast examination done 7 days after menstruation Position: lying down with pillow under the shoulder of the breast being examined or sitting in front of a mirror while raising the hands of the side of the breast being examined.
MANTOUX TEST Purpose – a test to determine exposure to TB Nursing Keypoints: a positive test yields an induration of 10 mm. or more for foreign born children below 4 years old
an induration of 5 mm or more is considered positive in patients with HIV, with treated TB, and if he has had a direct exposure TB patients BCG may cause false positive reaction assess for previous history of PTB and report immediately to the doctor result is read after 48-72 hours
MRI (Magnetic Resonance Imaging) Purpose – provides cross-sectional images of brain tissues, more detailed than a CT scan Contraindications: pregnant women obesity (more than 300 lbs) claustrophobic patients patients with unstable vital signs patients with metal implants like pacemaker, hip replacements and jewelleries
PARACENTESIS Purpose – to assess the contents of the peritoneal fluid Nursing Keypoints: check for consent patient is weighed before and after procedure instruct the patient to void prior to the procedure to prevent accidental puncture of the bladder during the procedure, instruct the patient to sit up with feet resting on footstool evaluate the effect of the procedure by assessing – weight, abdominal girth, respiratory rate/pulse rate notify the physician if the urine becomes bloody, pink or red
RINNE’S TEST Purpose – used to differentiate between conductive and sensorineural hearing losses Nursing Keypoints: the vibrating tuning fork is shifted between two positions: against the mastoid bone (bone conduction) and two inches from the opening of the ear-canal (air conduction) in conductive hearing loss, bone conduction lasts longer than air conduction
SCHILLING’S TEST Purpose- used to detect Vitamin B12 absorption Nursing Keypoints: excretion of 8% - 40% of ingested radioactive Vitamin B12 withing 24 hours is normal. Excreting more than 40% indicates pernicious anemia requires 24-hour urine specimen keep the patient NPO except for water, 8-12 hours before the test
SPUTUM EXAM Purpose – determines the presence of microorganisms in the sputum Nursing Keypoints: instruct patient to rinse mouth with water ( no to mouth wash or tooth paste) specimen is collected upon rising amount required: 15 ml instruct the patient to take several deep breaths and then cough deeply
STOOL ANALYSIS Purpose – assessment of bacteria, virus, malabsorption and blood in the stool Nursing Keypoints: avoid aspirin, indomethacin, steroids, dark colored foods, red meat and Vitamin C for three days before the test as these may give a false positive result.
SUCTIONING Purpose – to obtain sputum sample and clear the airway Nursing Keypoints: hyperoxygenate the patient before and after the procedure apply intermittent suction on withdrawal of the catheter do not suction the patient for more than 15 seconds
SWAN-GANZ CATHETERIZATION Purpose – used to monitor pulmonary artery pressure (PAP) and pulmonary capillary wedge pressure (PCWP). Nursing Keyponts: the catheter has four lumen (one for CVP, one for fluid infusion and venous access for blood samples, one for monitoring PAP and PCWP and the last lumen is used for inflation and deflation of the balloon. if the fifth lumen exists, it is used for measuring oxygen saturation of the blood the normal adult PAP systolic and diastolic pressure is 20 to 30 mmHg the normal PCWP is 8-13 mmHg the only time the balloon should be inflated after it is in place is when obtaining further PCWP readings.
THORACENTESIS Purpose - aspiration of fluid and/or air from the pleural space Nursing Keypoints: check the consent position: sitting on the side of the bed with feet on a chair, leaning over a bedside table if the patient cannot sit, he lie on his affected side with hands of that side resting on opposite shoulder instruct the patient not to cough, breathe deeply or move during the procedure after the procedure: position the patient on the unaffected side/puncture site up check for bleeding at the puncture site and monitor respiratory function
notify the physician if signs of pneumothorax, air embolism and pulmonary edema
TONOMETRY Purpose – measures intraocular pressure Nursing Keypoints: normal reading is 12-21 mmHg a reading of 25 mmHg indicates glaucoma
URINALYSIS Purpose – to assess characteristics of urine Nursing Keypoints: first voided morning sample preferred: 15 ml use clean container decreased specific gravity: diabetes insipidus increased specific gravity: diabetes mellitus, dehydration, SIADH (+) protein: PIH, nephrotic syndrome (+) glucose: diabetes mellitus, infection
URINARY CATHETERIZATION Purposes – To determine residual urine and obtain sterile specimen Nursing Keypoints: the procedure is sterile maintain a close system the drainage bag must always be below the bladder to avoid back flow of urine the catheter bag should not be allowed to lie on the floor do not allow the drainage spout to touch the collection receptacle or on the toilet bowl when draining it provide urine acidification
URINE COLLECTION, 24 HOUR Purpose – determines the excretion of substances from the kidneys, adrenal glands and the stomach Nursing Keypoints: required for ACTH test and schilling‟s test discard the first voided urine
WEBER TEST Purpose – used to detect the presence of unilateral hearing loss Nursing Keypoints: the tuning fork is set into vibration and placed on the patient‟s forehead or teeth placement of the teeth is generally more reliable even when the patient has false teeth
X-RAY Purpose – provides radiological data for assessment of certain organs and bones Nursing Keypoints: assess the patients exposure level to radiation instruct the patient to remove all jewelries and other metallic objects before the procedure
CULTURAL DIVERSITY
II.
ETHICAL AND LEGAL ISSUES
III.
LEADERSHIP AND MANAGEMENT
IV.
BASIC PHARMACOLOGY (including Herbal Medicines)
V.
ASEPSIS AND INFECTION CONTROL
VI.
COMPUTATION OF DOSAGE OF MEDICATIONS
VII.
NORMAL VALUES
VIII. NUTRITION AND DIET IX.
THERAPEUTIC DIETS
X.
POSITIONS
XI.
PROCEDURES
Fundamentals of Nursing consist of: 1. Cultural Diversity 2. Ethical and Legal Issues 3. Leadership and Management Issues 4. Basic Pharmacology (Including herbal medicines, computation, IV and Blood Transfusion Therapy) 5. Asepsis and Infection Control 6. Normal Values 7. Nutrition (including Therapeutic Diets) 8. Positioning 9. Diagnostic Tests
“What is the content of NCLEX-RN examination and how does the examinee answer those questions?” Questions of the actual NCLEX-RN Examination were distributed to the following category: Safe Effective Care Environment, under this category is the following sub-category -- Management of Care -- Infection Control Health Promotion and Maintenance Physiological Integrity, under this category is the following sub-category -- Basic Care and Comfort -- Pharmacological and Parenteral Therapies -- Reduction of Risk Potential -- Physiological Adaptation
An update you must know about the actual NCLEX-RN examination: Last April 2010, the questions about Management of Care were increased and questions about Reduction of Risk Potential were decreased. And according to the newsletter disseminated by NCSBN, the passing standard also increases. But do not be disturbed with this new info at hand, if you learn how to master the different concepts of nursing, starting with this concept “Fundamentals of Nursing”. Whatever type of questions you might encounter with the actual exam, I am sure that you can answer it correctly. Processes Integrated into all Client Needs Categories
Nursing Process Caring Communication and Documentation Teaching and Learning The Test Duration is six (6) hours Minimum number of questions that you may answer is seventy five (75) And the maximum number of questions that you may answer is two hundred sixty five (265)
The computer automatically stops when: Maximum number of questions has been answered Six hours have elapsed Examinee‟s minimum level of competency has been established Examinee‟s lack of competency has been established NCLEX-RN also uses Computer Adaptive Testing (CAT) and the decision if you pass or fail is based on how many questions you answer correctly and the difficulty of the questions a candidate answers correctly. The Examination will not end until certainty of the pass/fail result is assured.
I. CULTURAL DIVERSITY African-Americans Direct eye contact with authority is viewed as rude; but it is an important part of communication among family members/significant others. Personal questions are considered intrusive during initial contact; e.g. relationships, divorce, conflicts. Touching another’s hair is offensive. Illness is believed to be caused by demons/spirit Folk healer/herbalist may be consulted before seeking medical treatments
Native Americans/American Indians silence indicate respect for the speaker eye contact as a sign of disrespect They value the practice of massage to promote bonding between mother and newborn. Rooming-in is preferred for the mother and the newborn integration of religion and healing practices is observed Illness is caused by supernatural forces and disequilibrium between person and environment.
Asian Americans Direct eye contact with authority is viewed as rude head nodding does not necessarily mean agreement saying “NO” is considered as disrespect for others do not touch member of the opposite sex illness is believed to be an imbalance between positive (+) and negative (-) energy forces Promotion of healing by Yin and Yang principle Cold foods (Yin) Hot foods (Yang) Cold foods are given for hot illness Hot foods are given for cold illness
Hispanic Americans Do not admire a child. They believe that you may afflict the child with “evil eye,” it will cause an illness to the child they avoid eye contact with authority to show respect they use embraces/handshakes; they are very tactile they believe that health results from balance between “hot/cold”, “wet/dry” forces illness is a result of God‟s punishment communicate with male head of the family especially for major decisions, like signing consent for procedures because they have patriarchal society the most valued members of the family is the children religious practices are related to treatment of illness
European (White)-Origin Americans eye contact indicates trustworthiness they primarily depend on modern western health care services Autopsy is prohibited among: Eastern Orthodox Muslims Jehovah‟s Witness (NO BLOOD TRANSFUSION) Orthodox Jews
ORGAN DONATION: Jehovah‟s Witness (prohibited) Muslims (prohibited) Buddhists (act of mercy)
CREMATION: Hindus (cast ashes in Holy River, they believe that they can join the Creator faster this way) Mormons (prohibit cremation) Eastern Orthodox (prohibit cremation) Islam/Muslims (prohibit cremation) Jews (prohibit cremation)
RELIGION AND DIETARY PRACTICES: Baptist prohibits alcohol; discourages tea and coffee Buddhist prohibits alcohol and drug use most of them are vegetarians Hinduism considered the cow as sacred animal that is why they prohibit eating of beef and veal most of them are vegetarians Islam prohibits pork, alcohol and drugs daytime fasting is practiced during the time of Ramadan Jehovah’s Witness prohibits food to which blood has been added allow animal flesh that has been drained from blood
Judaism KOSHER DIET: prohibits meat and milk combination Prohibits pork and scavenger fish (shrimps, squids, crabs, fishes with no scales) Meat is allowed if from animals that are vegetable-eaters, cloven-hoofed, and ritually slaughtered Mormon prohibits alcohol, tea and coffee practice of fasting every first Sunday of the month encourages limited consumption of meat Roman Catholicism No meat on ash Wednesday and Good Friday (abstinence) Optional fasting during lent season Seventh day Adventist prohibits alcohol, tea and coffee, meat, and scavenger fish No surgeries or any procedures during Saturdays (Sabbath Day – sundown Friday to sundown Saturday).
CULTURAL BELIEFS AND PRACTICES ON DEATH AND DYING: Chinese When a Chinese client dies, they cover him/her with mirror with white cloth Islam/Muslim A dying client must face East (Middle East) or West/Southwest (North America). The dead body will be washed by a family member of the same sex and then covered with white cloth Buddhists The dead body is blessed by Spiritual Adviser Roman Catholics Anointing of the sick is done by the priest, to a dying client
TIME FOR A SHORT QUIZ. QUESTIONS A nurse is providing discharge instructions to a Chinese client regarding prescribed dietary modifications. During the teaching session, the client continuously turns away from the nurse. Which nursing action is appropriate? Continue the instructions, verifying client understanding Walk around the client so that the nurse constantly faces the client Give the client a dietary booklet and return later to continue with the instructions Tell the client about the importance of the instructions for the maintenance of health care 2. A nurse is preparing a plan of care for a client who is Jehovah‟s Witness. The client has been told that surgery is necessary. The nurse considers the client‟s religious preferences in developing the plan of care and documents that: Faith healing is practiced primarily Medication administration is not allowed Surgery is prohibited in this religious group The administration of blood and blood products is forbidden 3. Which of the following meal trays would be appropriate for the nurse to deliver to a client of Jewish faith who follows kosher diet? Pork roast, rice, vegetables, mixed fruit, milk Crab salad on a croissant, vegetables with a dip, potato salad, milk Sweet and sour chicken with rice and vegetables, mixed fruit, juice Fettucini alfredo with shrimp and vegetables, salad, mixed fruit, iced tea 4. An ambulatory care nurse is discussing preoperative procedures with a ChineseAmerican client who is scheduled for surgery the following week. During the discussion, the client continually smiles and nods the head. The nurse interprets this nonverbal behaviour as: Reflecting a cultural value An acceptance of the treatment The client is agreeable to the required procedures The client understands the preoperative procedure
5. A Chinese-American client experiencing anemia, which is believed to be a yin disorder, is likely to treat it with: Magnetic therapy Intercessory prayer Foods considered to be yin Foods considered to be yang ANSWERS AND RATIONALE 1) A - Most Chinese maintain a formal distance with others, which is a form of respect. Many Chinese are uncomfortable with face-to-face communications, especially when eye contact is direct. If the client turns away from the nurse during a conversation, the most appropriate action is to continue with the conversation. Walking around to the client so that the nurse faces the client is in direct conflict with the cultural practice. The client may consider returning later to continue with the explanation as a rude gesture. Telling the client about the importance of the instructions for the maintenance of health care may be viewed as degrading. 2) D - Among Jehovah‟s Witnesses, surgery is not prohibited, but the administration of blood and blood products is forbidden. Faith healing is forbidden in this religious group. Administration of medication is an acceptable practice, except if the medication is derived from blood products. 3) C - In the Jewish religion, those who are kosher believe that the dairy-meat combination is not acceptable. Pork and pork products are not allowed in the traditional Jewish religion. Only fish that have scales and fins are allowed; meats that are allowed include animals that are vegetable eaters, cloven-hoofed, and ritually slaughtered. 4) A - Nodding or smiling by a Chinese-American client may reflect only the cultural value of interpersonal harmony. This nonverbal behavior may not be an indication of agreement with the speaker, an acceptance of the treatment, or an understanding of the procedure. 5) D - In the yin and yang theory, health is believed to exist when all aspects of the person are in perfect balance. Yin foods are cold and yang foods are hot. Cold foods are eaten when one has a hot illness and hot foods are eaten when one has a cold illness. Options A and B are not associated with the yin and yang theory.
II. ETHICAL AND LEGAL ISSUES Advance Directive It is a written document that provides directions concerning the provision of care when a person is unable to make his/her own treatment choices. Two types of advance directive: a) Living Will – it is the expression of the person‟s wishes regarding end-of-life care. It is prepared by a competent adult that provides direction regarding medical care in the event of the person‟s incapacitation or otherwise becoming unable to make decisions personally. b) Durable Power of Attorney – I is an authorization that enables any competent individual to name someone to exercise decision-making on his/her behalf under specific circumstances. Example, end-of-life situation.
Clarifying Unclear/Inappropriate Physician’s Order Clarify the order with the physician who gave the order Contact nurse manager/supervisor if no resolution occurs regarding the order in question
Floating It is acceptable and legal practice Nurse cannot refuse to float; but the nurse should not assume responsibility beyond level of experience or qualification The nurse should inform the supervisor of any lack of experience in caring for the type of clients on the new nursing units The nurse should be given an orientation to the new unit Floating nurse should be assigned with patients with stable conditions; or similar to his/her training or experience Floating nurse should not be assigned to patients who are for discharge and who require patient teaching
Good Samaritan Laws - These laws encourage health care professionals to assist in emergency situations without fear of being sued for the care provided
Informed Written Consent Physician not the nurse, is the primary responsible to secure written consent Nurse may sign as a witness. It attests that the client signed the consent
Written consent is legal when: The person is in legal age (18 y/o and above) The consent is secured without force, duress, or coercion The person is not under the influence of drugs or alcohol The person is not mentally incapacitated Parents or guardian can signed for minors and persons who are physically or mentally incapacitated Minors who are married or emancipated from the parents and those seeking for treatment for STD‟s can signed an informed consent Written consent can be waived in time of emergency to save the life of the person Validity of informed consent is 24 hours. If the procedure is postponed, secure another consent Secure consent for each procedure
Organ Donation Age requirement is 18 y/o and above before signing a form for organ donation Informed choice to donate an organ may be through written document signed by the client prior to death, a will, a donor card, or an advance directive Family member or legal guardian may authorize organ donation if the client is dead
Physician’s Orders Nurses is duty-bound to carry out a doctor‟s order except when the nurse believes that the order is inappropriate Nurses who carry out inaccurate order is legally responsible for his/her action
Telephone Orders Date and time the entry Repeat (read back) the order to the physician and record the order Sign the order begin with the t.o., write the doctor‟s name, and then sign the order; e.g. (t.o. Dr. Alec Tinio/ your signature RN It is necessary that the doctor countersign the order within the time frame based on the agency policy (usually 24 hours)
Use of Restraints Written consent is needed coming from relatives/significant others Secure consent for each episode of application of restraints PRN order: legally unacceptable Apply soft restraints Secure restraints at he bed frame, not on the side rails Check restraint application every 15-20 minutes Release restraints every 2 hours for 30 minutes Change restraints every 24 hours
Documentation For Narrative Documentation it should be accurate, complete, factual, and objective use a black pen document care, medications, treatments, and procedures as soon as possible, after completed document responses to interventions document consent for a refusal of treatments document calls made to other health care providers
use appropriate abbreviations in case of error, draw one line through the error, initial and date never erase any entry, do not use correction fluid do not leave blank spaces on documentation forms. Avoid judgmental or opinionated statements, such as “uncooperative client.” Do not document for others or change documentation for other individuals For Computerized Documentation use only the user identification (ID) code, name, or password maintain privacy and confidentiality of documented information printed from the computer
Principle of Confidentiality Information about a client be kept private Information in the client‟s record is accessible only to those providing care to the client No one else is entitled to that information unless the client has signed a Consent for Release of Information that identifies with whom information may be shared and for what purpose. Discussing clients outside the clinical setting, telling friends, or family about clients or even discussing clients in the elevator with other workers violates client‟s confidentiality. The clients has a right to review the records pertaining to his/her medical care and to have the information explained or interpreted as necessary, except when restricted by law
Incident Reports/Variance Reports A tool used as a means of identifying and improving care. The reports should be complete, accurate, and factual. The reports should not include opinions or interpretations. The report form should not be copied or placed in the client„s record. It is not a substitute for a complete entry in the client‟s record regarding the incident.
Controlled Substances Nurses may administered controlled substances (narcotics, depressants, stimulants, and hallucinogens), only under the directions of a physicians or other authorized providers. Controlled substances must be kept securely locked, and only authorized personnel should have access to them.
Reporting Responsibilities. The following situations need to be reported to the Local Authority. This is a LAW. Failure to report any of these situations is a malpractice.
Communicable diseases Abuse: sexual, child, wife, husband, elderly abuse. (Whenever abuse is suspected, it should be reported to the local authority. It will be the court to prove or disprove abuse.) gunshot/ stab wounds vehicular accidents assault homicides
Clients Advocacy Involves concerns and actions on behalf of another person in order to bring about change. 3 Elements of Advocacy 1. Mediate 2. Inform 3. Support
MORAL PRINCIPLES 1. Beneficence - means doing and promoting good. e.g.,
Administering pain medications. Practicing asepsis to prevent infection.
Promoting safety of restless and confused clients. Providing psychosocial support to an anxious client.
2. Nonmalefincence - means to avoid doing harm, to remove from harm, and to prevent harm. e.g., protecting the client from a practitioner who practices drug abuse. Reporting abuse prevent further victimization. 3. Autonomy – right to make one‟s own decision 4. Fidelity – being faithful to agreement and promises 5. Veracity – telling the truth 6. Justice - fairness
TORTS AND CRIMES - These are legal wrongs committed against a person or property.
CRIME - Results in prison term or fine or short jail sentence to punish offender. a. Felony - A crime of serious nature. b. Misdemeanor - An offense punishable by imprisonment of less than one year or a fine less than 1,000 dollars. Does not amount to a felony. c. Manslaughter - A second degree murder. It is unintentional killing. e.g., accidental administration of overdose narcotics that resulted to death of the clients.
TORTS - Result in civil trial to assess compensation for plaintiff 1. Intentional Torts: I.
Assault and Battery a. Assault – is the threat of touching another person without his/her consent b. Battery – is the actual carrying out of such a threat
II.
Defamation of Character - is a communication that is false or made with careless disregard for the truth, and results in injury to the reputation of the person a. Libel – defamation by means of print, writing, or pictures b. Slander - is defamation by spoken word, stating unprivileged or false words by which the reputation of the person is damaged
III.
Fraud - is the wilful, purposeful misrepresentation of self or an act that may cause harm to a person or property
IV.
Invasion of Privacy - is disclosure confidential information to an inappropriate third party (subjects the nurse to invasion of privacy even if the information is true).
V.
False Imprisonment – occurs when a client is not allowed to leave a health care facility when there is no legal justification to detain the client
2. Unintentional Torts I.
Negligence – mistake or failure to be prudent. An act of omission or commission
II. Malpractice – is negligence in the practice of profession (e.g. error in sponge counts) To prove malpractice, four elements are necessary a. a duty of the nurse to the client b. a breach of duty on the part of the nurse c. an injury to the client d. a causal relationship between the breach of duty and the client subsequent injury Potential Malpractices Situations in Nursing medication error
mistaken identity
sponge count error
loss/damage of client‟s property
burning a client
failure in reporting crimes, torts, and unsafe practice
client falls “Only the Task not the Accountability may be Delegated to another” Best Practice: Always ensure client safety
Death and Dying Right of Informed Refusal – a competent adult has the right to refuse treatment, even lifesustaining treatment Do Not Resuscitate (DNR) Order – a written order must be present and must be reviewed on a regular basis. The client or his/her legal representative must provide informed consent for the DNR status. Both DNR and cardiopulmonary resuscitation (CPR) must be clearly defined so that other treatments, not refused by the client will be continued. Euthanasia – physician or nurse-caused death (active euthanasia), deliberately hastening a person‟s death, is considered murder in all states and almost all other countries
Pronouncement of Death in some States, the nurse may pronounce death at the bed side in most States, however, the physician has the legal responsibility of pronouncing the person dead. “To be safe in answering, always choose PHYSICIAN.” Death Certificate – the physician is responsible for signing a death certificate Care of the Body – the nurse is responsible for preparing the body for the morgue or mortuary. Consider the cultural practices and wishes of the family. Treat the body with dignity. Rigor Mortis – stiffening of the body (occurs 2-4 hours) position the body, the dentures, close the mouth and eyes before RM set in Algor Mortis – decrease in body temperature (1C/hr) Livor Mortis – discoloration of the skin because of the RBC breakdown Management: make the body appear natural and comfortable allow the family to view the patient‟s body place the body in supine positions, the arms at the side and palms down place one pillow under the head and shoulder to prevent blood from discoloring the face place absorbent pads under the buttocks to take up any feces or urine apply identification tags, one on the ankle and one at the wrist wrap the body in shroud, place the third tag for identification
III. LEADERSHIP AND MANAGEMENT Priorities of Care needs that are life threatening are given highest priority actual before potential concerns consider time constraints and available resources needs that are identified as important by the client are given highest priority use Maslow‟s hierarchy of needs (physiologic before psychosocial needs) use ABC‟s; patent airway is always priority unstable before stable clients client first before equipment do not delegate client who need: to be assessed those who need health teachings those who need to be evaluated those with unstable conditions
DELEGATION transference of responsibility and authority for the performance of an activity to a competent individual Five Rights of Delegation Right Task – appropriate activities Right Circumstances – assess health status. Match complexity of activity with competency of the health care worker. Right Person Right direction and communication Right supervision/evaluation
CNA/Unlicensed Nursing Assistant Undergo certification examination May care for clients with stable conditions May perform standard nursing procedures: VS - taking Comfort measures Hygienic measures Activity, mobility, exercise Collection of specimen Enema administration Obtaining equipment LPN/LVN Undergo licensure examination (NCLEX-PN/VN) May perform standard nursing procedures and more complicated nursing procedures: Wound dressing changes Irrigation of wounds Colostomy care Enteral feedings Administration of medications (oral, subcutaneous, intramuscular) Administration of basic IV fluids (no IV meds and electrolytes added to IV fluids like Potassium Chloride) Catheterization May care for clients with stable conditions
Leadership Theories 1. Bureaucratic – relies on organization‟s rule and policy 2. Autocratic – make decision for the group 3. Laissez-faire – recognizes the group‟s need for autonomy and self-regulation; “hands-off approach” 4. Democratic – encourages group discussion and decision making
Principles of Management 1. Authority – legitimate right to direct the work to others 2. Accountability – ability to assume responsibility for one‟s action and its consequences 3. Responsibility – obligation to complete a task Principles in Rooming-In Cohorts (similar medical diagnosis or mode of transmission of disease) may be roomed-in as long as one does not have another type of contagious infection. Consider age and gender of clients. Clients of the same age group and gender may be roomed-in Clients with airborne infections should be confined in private rooms Immune-compromised clients should not be roomed-in with clients who have infections.
Case Management Assignment of health care provider to assist a patient in assessing health and social service systems to assure that all required services are obtained Who requires Case Management? age 65 with chronic diagnostic state, lives alone newly diagnosed diabetic limited income preventing prescription purchases
weakness related to CVA may require change in living arrangements may need medical equipment may need home health follow-up
confused or unstable to make decisions
admitted from board and care
Let us evaluate . . . 1. A new unit nurse manager is holding her first staff meeting. The manager greets the staff and comments that she has been employed to bring about performance improvement. The manager provides a plan that she developed, as well as a list of tasks and activities for which each staff member must volunteer to perform. In addition, she instructs staff members to report any problems directly to her. What type of leadership style do the new manager‟s characteristics suggest? autocratic
democratic
situational
laissez-faire
2. A new nursing graduate is attending an agency orientation regarding the nursing model of practice implemented in the health care facility. The nurse is told that the nursing model is a team nursing approach. The nurse understands that planning care delivery will be based on which characteristic of this type of nursing model of practice? a task approach method is used to provide care to clients managed care concepts and tools are used in providing client care an RN leads nursing personnel in providing care to a group of clients a single RN is responsible for providing nursing care to a group of clients 3. The nurse manager has implemented a change in the method of the nursing delivery system from functional to team nursing. A nursing assistant is resistant to the change and is not taking an active part in facilitating the process of change. Which of the following is the best approach in dealing with the nursing assistant? ignore the resistance exert coercion with the nursing assistant provide a positive reward system for the nursing assistant confront the nursing assistant to encourage verbalization of feelings regarding the change 4. The nurse manager of a critical care unit must speak to a staff nurse about an employment issue, tardiness. Nearly every day during the past week, the staff nurse has been from 5 to 20 minutes late, missing portions of the daily client status conferences. The manager had verbally counselled the staff nurse 3 months prior to the latest incidence of tardiness about the same issue. When they meet, the nurse manager‟s best approach to the staff nurse is to: send the staff nurse to Human Resources Department for counselling ask the staff nurse to tell the manager about the facts surrounding the tardiness inform the staff nurse that, based on unreliability caused by tardiness issues, the nurse is terminated Provide the staff nurse with a detailed notice of intent to terminate if any further incident of tardiness occurs.
5. A nurse is giving a report to a nursing assistant who will be caring for a client who has hand restraints. The nurse instructs the nursing assistant to assess the skin integrity of the restrained hands every: 2 hours
4 hours
3 hours
30 minutes
ANSWERS AND RATIONALE 1) A - The autocratic leader is focused, maintains strong control, makes decisions, and, addresses all problems. Furthermore, the autocrat dominates the group and commands rather than seeks suggestions or input. In this situation, the manager addresses a problem (performance improvement) with the staff, designs a plan without input, and wants all problems reported directly back to her. A situational leader will use a combination of styles, depending on the needs of the group and the tasks to be achieved. The situational leader would work with the group to validate that the information that the leader gained as a new employee was accurate and that a problem existed, and would then take the time to get to know the group and determine which approach to change (if needed) would work best according to the needs of the group and the nature and substance of the change that was required. A democratic leader is participative and would likely meet with each staff person individually to determine the staff member‟s perception of the problem. The democratic leader would also speak with the staff about any issues and ask the staff for input with developing a plan. A laissez-faire leader is passive and nondirective. The laissez-faire leader would state what the problem was and inform the staff that the staff needed to come up with a plan to “fix it.” 2) C - In team nursing, nursing personnel are led by a registered nurse leader in providing care to a group of clients. Option A identifies functional nursing. Option B identifies a component of case management. Option D identifies primary nursing. 3) D - Confrontation is an important strategy to meet resistance head on. Face-to-face meetings to confront the issue at hand will allow verbalization of feelings, identification of problems and issues, and development of strategies to solve the problem. Option A will not address the problem. Option B may produce additional resistance. Option C may provide a temporary solution to the resistance but will not address the concern specifically. 4) D - In general, the process for corrective action begins with an oral reprimand and then a written reprimand. In addition to the written reprimand, the manager should be prepared to work with the staff nurse to develop a plan of action. The manager must notify the staff nurse, in writing, of the potential for termination based on tardiness. If this were the first instance, the manager would ask the staff nurse to describe the facts surrounding the tardiness in order for the manager to assist the staff nurse with problem-solving strategies or to examine the need for moving the staff nurse to a different shift, if indicated. Managers are expected to deal with personnel issues, and tardiness is a frequent problem that managers face. Human resources serve as a support to the actions of the manager, but do not assume the role of dealing with the employee. Managers must give notice prior to termination as a risk management strategy. 5) D - The nurse should instruct the nursing assistant to assess restraints and skin integrity every 30 minutes. Agency guidelines regarding the use of restraints should always be followed.
IV. BASIC PHARMACOLOGY (including Herbal Medicines) Types of Doctor’s Order Standing Order – it is carried out until the specified period of time or until it is discontinued by another order Single Order – it is carried out for one time only STAT Order – it is carried out at once or immediately PRN Order – it is carried out as the patient requires Parts of Legal Doctor’s Order - Name of patient - Date and time - Name of drug - Dose of drug - Route of administration - Times or frequency - Signature of the physician PRINCIPLES IN ADMINSTERING MEDICATION 1. Observe the “7 Rights” of drug administration Right drug – read the label three times Right dose – know the usual dose of the drug. Calculate the correct amount Right time – standard time may be followed in the institution Right route – check the route of administration Right patient – identify patient by: checking the ID band (most accurate patient identifier) or asking him to state his/her name (not accurate for confused clients) Right recording – sign medication sheet immediately after administration Right approach 2. Practice Asepsis – wash hands before and after preparing medications Nurses who administer medications are responsible for their own actions. Question any order that you consider incorrect (may be unclear or inappropriate) Be knowledgeable about the medications that you administer. Know the action, indication, nursing responsibilities, side effects of the drugs Fundamental Rule: “Never Administer an Unfamiliar Medication” 3. Keep narcotics in locked place
4. Use only medications that are clearly labelled container. Relabeling of drugs is the responsibility of pharmacist 5. Return liquid that are cloudy in color to the pharmacy 6. Before administering the medication, identify the client correctly 7. Do not leave the medications at the bed side. Stay with the client until he actually takes the medications 8. The nurse who prepares the drug administers it. Only the nurse who prepared the drug knows what that drug is. Do not accept endorsement of medications. 9. If the client vomits after taking the medication, report this to the nurse in charge or physician 10. Preoperative medications are usually discontinued during the postoperative period unless ordered to be continued 11. When a medication is omitted for any reason, record the fact together with the reason 12. When a medication error is made, report it immediately to the nurse in charge or physician. To implement necessary measures immediately. This may prevent any adverse effects of the drug
ROUTES OF DRUG ADMINISTRATION 1. Oral Medication - Most common method of drug administration and generally the safest route. Absorption will usually take in GIT. - Onset is slower compare to others Types of Oral Drugs a. Solid Preparation – tablets, capsules, and pills Remember: enteric-coated tablets and time-released capsules are never crushed or chewed b. Liquid Preparation – elixirs, syrups, and suspensions. They are best administered by using calibrated cup (read at the eye level). Other Oral Form Drugs a. Sublingual – drugs are placed under the tongue b. Buccal – drugs are placed in the inner cheek Rule: never swallow the drug and do not follow with water. If nitro-glycerine is given, advise patient not to smoke.
Safety in administering Oral Medications - might cause aspiration and choking (especially large capsules and tablets) - assess for gag reflex, dysphagia, or altered LOC - client who is NPO Note: if drug has offensive taste, offer oral hygiene.
2. Topical Medication - applied to the skin by spreading it over an area, soaking or medicated bath (causes either local or systemic effect depending on duration of application). Note: Nurse should done gloves when administering this type of drug.
3. Inhalation Medication Nasal inhalation – oxygen is administered by this route Oral inhalation MDI (Metered-dose inhaler) 2 inches away from the mouth Inhale 2-5 seconds Hold breath for 10 seconds Wait 1-2 minutes before each puff Note: to know if the canister is still packed with drug, simply put it in basin with water. If it floats, it is empty. Nebulizer Dilute to sterile 0.9% NaCl (2-5 ml) Attach oxygen to nebulizer (8L/min) Breathe normally through mask or mouthpiece for 5-15 minutes Note: offer Oral Hygiene
4. Eye Medication (Optic) Effects:
Miotics - pupil constriction Mydriatics – pupil dilation
Types: Liquid – 2 gtts (lower conjunctival sac) Ointment – 2 cm (inner to outer canthus) Note: no to cornea press the nasolacrimal gland if drug will cause systemic effect don‟t let the tip of the canister touch any part of the eye sitting position is required Note: Eye assessment? Dim the light prior to eye examination
5. Ear Medication (Otic) Position: lateral position Age below 3 y/o – pull the pinna down and back Above 3 y/o – pull the pinna up and back Solution - side of the ear Temp of solution – warm Press the tarsus of the ear 3 times for absorption Place earplug for 5 minutes Note: if the ear canal is obstructed by seed, don‟t flush with water. If an insect goes inside the ear, use flashlight
6. Parenteral Route – is a medication administration is by needle. Intradermal route of medication administration- it is a parenteral route of medication administration by injecting the needle under the epidermis. The site are the inner lower arm, upper chest and back, and beneath the scapula Indicated for allergy and tuberculin testing and for vaccinations Use the needle gauge 25,26,27 needle length: 3/8", 5/8", or 1/2" Needle at 10-15 degrees angle: bevel up Inject a small amount of drug slowly over 3 to 5 seconds to form a wheal or bleb Do not massage the site of injection. To prevent irritation of the site, and to prevent absorption of the drug into the subcutaneous.
I. SUBCUTANEOUS route of medication administration - for vaccines, heparin, preoperative medication, insulin, narcotics The site: - outer aspect of the upper arms - anterior aspect of the thighs - abdomen scapular areas of the upper back - ventrogluteal - dorsogluteal Only small dose of medication should be injected via SC route Rotate site of injection to minimize tissue damage Needle length and gauge are the same for ID injections Use 5/8 needle for adults when the injection is to administer at 45 degree angle; 1/2 is use at 90 degree angle For thin patients: 45 degree angle needle For obese patient: 90 degree angle needle For heparin injection: do not aspirate and do not massage the injection site to prevent hematoma formation. For insulin injection: do not massage to prevent rapid absorption which may result to hypoglycemic reaction. Always inject insulin at 90 degrees angle to administer the medication in the pocket between the subcutaneous and muscle layer. Adjust the length of the needle depending on the size of the client
II. INTRAMUSCULAR route of medication administration needle length: 1", 1 1/2", 2" to reach the muscle layer Clean the injection site with alcoholised cotton ball to reduce microorganisms in the area Inject the medication slowly to allow the tissue to accommodate volume
Sites: a. Ventrogluteal site The area contains no large nerves, or blood vessels and less fat. It is farther from the rectal area, so it is less contaminated Position the client in prone or side-lying When in prone, curl the toes inward When in side-lying, flex the knee and hip. These ensure relaxation of the gluteus muscles and minimize discomfort during injection To locate the site, place the heel of the hand over the greater trochanter, point the index finger toward the anterior superior iliac spine, and then abduct the middle(third) finger. The triangle formed by the index finger, the third finger and the crest of the ilium is the site. b. Dorsogluteal site Position the client similar to the ventrogluteal site The site should not be used in infant under 3 years old because the gluteal muscles are not well developed yet To locate the site, the nurse draws an imaginary line from the greater trochanter to the posterior superior iliac spine. The injection site is lateral and superior to this line Another method of locating this site is to imaginary divide the buttock into four quadrants. The upper most quadrant is the site of injection. Palpate the crest of the ilium to ensure that the site is high enough Avoid hitting the sciatic nerve, major blood vessel or bone by locating the site properly c. Vastus Lateralis Recommended site for infant Located at the middle third of the anterior lateral aspect of the thigh Assume back-lying or sitting position d. Rectus Femoris site Located at the middle-third, anterior aspect of the thigh
e. Deltoid site Not used often for IM injection because it is relatively small muscle and is very close to the radial nerve and radial artery To locate the site, palpate the lower edge of the acromion process and the midpoint on the lateral aspect of the arm that is in line with the axilla. This is approximately 5cm(2 in) or 2 to 3 fingerbreadths below the acromion process f. IM injection - Z tract injection Used for parenteral iron preparation. To seal the drug deep into the muscles and prevent permanent staining of the skin Retract the skin laterally, inject the medication slowly. Hold retraction of skin until the needle is withdrawn Do not massage the site to prevent leakage into the subcutaneous.
GENERAL PRINCIPLES IN PARENTERAL ADMINISTRATION 1. Check doctor's order 2. Check the expiration for medication - drug potency may increase or decrease if outdated 3. Observe verbal and non-verbal responses toward receiving injection. It can be painful, client may have anxiety, which can increase the pain 4. Practice asepsis to prevent infection. Apply disposable gloves 5. Use appropriate needle size. To minimize tissue injury 6. Plot the site of injection properly. To prevent hitting nerves, blood vessels, bones 7. Use separate needles for aspiration and injection of medications to prevent tissue irritation 8. Introduce air into the vial before aspiration. To create a positive pressure within the vial and allow easy withdrawal of the medication 9. Allow a small bubble (0.2 ml) in the syringe to push the medication that may remain 10. Introduce the needle in quick thrust to lessen discomfort 11. Either spread or pinch muscle when introducing the medication. Depending on the size of the client 12. Minimized discomfort by applying cold compress over the injection site before introduction of medication to numb nerve endings 13. Aspirate before introduction of medication. To check if blood vessel had been hit 14. Support the tissue with cotton swabs before withdrawal of the needle. To prevent discomfort of pulling tissues as needle is withdrawn 15. Massage the site of injection to haste absorption 16. Apply pressure at the site for few minutes. To prevent bleeding 17. Evaluate effectiveness of the procedure and make relevant documentation.
METHOD OF DRUG ADMINISTRATION INTAVENOUSLY 1. A mixture within large volumes of IV fluids 2. By injection of bolus, or small volume, or medication through an existing intravenous infusion line or intermittent venous access (heparin or saline lock) 3. By "piggyback" infusion of solution containing the prescribed medication and a small volume of IV fluid through an existing IV line Most rapid route of absorption of medications Predictable, therapeutic blood levels of medication can be obtained The route can be used for clients with compromised gastrointestinal function or peripheral circulation Large dose of medications can be administered by this route The nurse must closely observe the client for symptoms of adverse reactions The nurse should double-check the six rights of safe medication If the medication has an antidote, it must be available during administration When administering potent medications, the nurse assesses vital signs before, during and after infusion
NURSING INTERVENTIONS IN I.V. INFUSION a. Verify doctor's order b. Know the type, amount, and indication of IV therapy c. Practice strict asepsis d. Inform the client and explain the purpose of IV therapy to alleviate client's anxiety e. Prime IV tubing to expel air. This will prevent air embolism f. Clean the insertion site of IV needle from center to the periphery with alcoholized cotton ball to prevent infection g. Shave the area of needle insertion if hairy. Ask permission to the client h. Change the IV tubing every 72 hours. To prevent contamination i. Change IV needle insertion site every 72 hours to prevent thrombophlebitis j. Regulate IV every 15-20 mins. To ensure administration of proper volume of IV fluid as ordered k. Observe for potential complications.
THREE TYPES OF I.V. FLUIDS a. Isotonic solution - it has the same concentration as the body fluid. D5W
Plain Ringer's lactate
NaCl 0.9%
Plain normosol M
b. Hypotonic - has lower concentration than the body fluids. Too much of this fluid can swell the body's cell. NaCl 0.3% c. Hypertonic - has higher concentration than the body fluids. Too much of this fluid can make the body's cell shrink. D10W
D5LR
D50W
D5NM
COMPLICATIONS OF I.V. INFUSION 1. Infiltration - the needle is out of vein, and fluids accumulate in the subcutaneous tissues. Assessment Pain, swelling, skin is cold at needle site, pallor of the site, flow rate has decreases or stops Nursing Intervention: Change the site of the needle Apply warm compress. This will absorb edema fluids and reduce swelling 2. Circulatory Overload- this complication of I.V. infusion results from administration of excessive volume of I.V. fluids. Assessment Headache, flushed skin, rapid pulse Increase BP, weight gain, syncope and faintness Pulmonary edema, increase volume pressure Coughing, tachycardia, shock Nursing Intervention: Slow I.V. infusion to KVO - at least 10 gtts/min Place patient in high-fowler's position to enhance breathing Administer diuretic, bronchodilator as ordered.
3. Drug Overload - this complication of I.V. infusion occurs when the patient receives an excessive amount of fluid containing drugs Assessment Dizziness, shock Fainting Nursing Intervention: Slow I.V. infusion to KVO Take vital signs Notify the physician 4. Superficial Thrombophlebitis - this complication of I.V. infusion is due to overuse of a vein, irritating solution or drugs, clot formation, large bore catheters Assessment Pain along the course of vein Vein may fell hard and cordlike Edema and redness at needle insertion site Arm feels warmer than the other arm Nursing Intervention Change I.V. site every 72 hours Use large veins for irritating fluids Stabilize venipuncture at area of flexion Apply cold compress immediately to relieve pain and inflammation; later with warm compress to stimulate circulation and promotion absorption Do not irrigate the I.V. because this could push clot into the systemic circulation 5. Air Embolism - air manage to get into the circulatory system; 5 ml of air or more causes air embolism. Take note that it is a life-threatening conditio9n. Assessment Chest, shoulder or back pain Hypotension Dyspnea Cyanosis Tachycardia Increase venous pressure Loss of consciousness Nursing Intervention Do not allow the I.V. bottle to run dry Prime I.V. tubing before starting infusion Turn patient to left side in the trendelenburg position. To allow air to rise in the right side of the heart. This prevent pulmonary embolism
6. Nerve Damage - this complication of I.V. infusion result from trying the arm too tightly to the splint Assessment Numbness of fingers and hands Nursing Intervention Massage the area and move shoulder through its ROM Instruct the patient to open and close hand several times each hour Physical therapy may be required Take note: apply splint with the fingers free to move 7. Speed Shock - This complication of I.V. infusion result from administration of I.V. push medication rapidly. To avoid speed shock and possible cardiac arrest, give most I.V. push medication over 3 to 5 mins.
OBJECTIVES OF BLOOD TRANSFUSION THERAPY 1. To increase circulating blood volume after surgery, trauma, or hemorrhage 2. To increase the number of RBC's and to maintain hemoglobin levels in clients with severe anemia 3. To provide selected cellular components as replacements therapy (e.g. clotting factors, platelets, albumin) Nursing Interventions of Blood Transfusion Therapy (note: consent is needed) 1. Verify doctor's order. Inform the client and explain the purpose of the procedure 2. Check for cross matching and typing. To ensure compatibility 3. Obtain and record baseline vital signs 4. Practice strict asepsis 5. At least 2 licensed nurses check the label of the blood transfusion. Check the following: Serial number Blood component Blood type
Rh factor Expiration date
Screening test (VDRL, HBsAg, malarial smear) - to ensure that the blood is free from bloodcarried diseases and therefore, safe from transfusion 6. Warm blood at room temperature before transfusion to prevent chills 7. Identify client properly. Two nurses check the client's identification 8. Use needle gauge 18 to 19. This allow easy flow of blood 9. Use BT set with special micron mesh filter. To prevent administration of blood clots and particles 10. Start blood transfusion therapy slowly at 10 gtts/min. Remain at bedside for 15-30 mins. Adverse reaction usually occurs during the first 15 to 20 mins
11. Monitor vital signs. Altered vital signs indicate adverse reaction: Do not mix medication with blood transfusion. To prevent adverse effects Do not incorporate medication into the blood transfusion Do not use blood transfusion line for I.V. push of medication 12. Administer 0.9% NaCl before, during, or after Blood Transfusion Therapy. Never administer I.V. fluids with dextrose because it causes hemolysis 13. Administer Blood Transfusion Therapy for 4 hrs (whole blood, packed RBC). For plasma, platelets, cryoprecipitate, transfuse quickly (20 mins) clotting factor can easily destroyed.
COMPLICATIONS OF BLOOD TRANSFUSION 1 Allergic Reaction - this type of complication of blood transfusion is caused by sensitivity to plasma protein of donor antibody, which reacts with recipient antigen Assessment: Flushing Rush, hives Pruritus Laryngeal edema, difficulty of breathing 2. Febrile, Non-Hemolytic - this type of complication of blood transfusion is caused by hypersensitivity to donor white cells, platelets or plasma proteins. This is the most symptomatic complication of blood transfusion Assessment: Sudden chills and fever Flushing Headache Anxiety 3. Septic Reaction - this type of complication of blood transfusion is caused by the transfusion of blood or components contaminated with bacteria Assessment: Rapid onset of chills Vomiting Marked hypotension High fever
4. Circulatory Overload - this type of complication of blood transfusion is caused by administration of blood volume at rate greater than the circulatory system can accommodate Assessment: Rise in venous return Dyspnea Crackles or rales Distended neck vein Cough Elevated blood pressure 5. Hemolytic Reaction - this type of complication of blood transfusion is caused by infusion of incompatible blood products Assessment: Low back pain (first sign). This is due to inflammatory response of the kidneys to incompatible blood Chills Feeling of fullness Tachycardia Flushing Tachypnea Hypotension Bleeding Vascular collapse Acute renal failure NURSING INTERVENTIONS WHEN BLOOD TRANSFUSION COMPLICATIONS OCCUR 1. The first thing to do when complications in blood transfusion occurs is to STOP TRANSFUSION 2. Then start or open I.V. line (0.9%NaCl) 3. Place the client in fowler's position and administer oxygen therapy depending in the hospital protocol 4. Check vital signs as often as 5 mins 5. Notify the doctor immediately about the complications of blood transfusion 6. Carry out doctor’s order; prepare the emergency drugs like antihistamines, vasopressor, fluids as protocol 7. Obtain urine specimen and send to the laboratory to determine presence of hemoglobin as a result of RBC hemolysis 8. Blood container, tubing, attached label, and transfusion record are saved and returned to the laboratory for analysis.
HERBAL MEDICINES Aloe Vera - treatment for minor burns, insect bites, sunburns, dandruff, oily skin, psoriasis Chamomile - relief of digestive and GI disturbances Dong Quai - treatment for menstrual cramps and to regulate the menstrual cycle Echinacea - Immune enhancer - Treatment for respiratory and urinary tract infection - Treatment for snake bites Feverfew - relief of migraine headache Garlic - To lower cholesterol and triglyceride levels - To decrease BP; decrease clotting capability of the blood Ginger - boosts the immune system - To treat stomach and digestive disorders - Relief from nausea - Relief from pain, swelling, and stiffness for arthritis Giangko - Antioxidant: peripheral vasodilatation and increase blood flow to CNS; reduces platelet aggregation - Treatment for allergic rhinitis, Alzheimer‟s disease, anxiety, stress, dementia, Raynauld‟s disease, tinnitus, vertigo, impotence, poor circulation Ginseng - Relief of stress; to boost energy; to give digestive support - supports immune system and prevents chronic infection Goldenseal - To ward off infection and promote wound healing - To treat congestion associated with common cold Kava – kava - Root promotes sleep and muscle relaxation
- Treats UTI Licorice - Effects are similar to aldostrone and corticosteroid - relieves heartburns and indigestion - treat ulcers Milk Thistle - To prevent liver damage Peppermint - stimulates appetite to eat; aids in indigestion - Treatment of bowel disorders - stimulates circulation; reduces fever; clears congestion; restores energy - Peppermint oil is used as treatment for tension headache St. John’s Wort “herbal Prozac” - Antidepressant, antiviral activity Saw Palmetto “plant catheter” - relieves symptoms of BPH and urinary conditions Valerian “herbal valium” - sleep-inducing agent Billberry - promotes healthy vision; relieves diarrhea in children - Leaf is used for diabetes, arthritis, dermatitis, gout Black Cohosh - suppresses LH; increases estrogen level - has antispasmodic, astringent, diuretic, vasodilator effects - relieves PMS, dysmenorrheal, infertility, menopausal symptoms Cranberry - Prophylaxis for UTI Evening Primrose - Natural estrogen promoter - Treatment for PMS, diabetic neuropathies, chronic inflammatory conditions Hawthorn - promotes peripheral vasodilation; increases coronary circulation, acts as an antioxidant - Treatment for early CHF, stable angina
V. ASEPSIS AND INFECTION CONTROL Handwashing – is the single, most effective practice to prevent spread of microorganisms. 4 Elements of Handwashing 1. Water 2. Friction 3. Soap 4. Time
Body Defenses against Infection - Normal flora - Intact skin - Saliva and mucus membrane - Cilia of the upper respiratory tract infection - Inflammatory process - Immune response
ASEPSIS 1. Medical Asepsis – Clean technique - reduces number of pathogens -GIT - Handwashing removes microorganism 2. Surgical Asepsis - Sterile technique - make object free of all microorganisms - Dressing, catheterization and Surgical procedures and Specimen collection
Sterile Technique Guidelines 1. Never turn your back on a sterile field 2. Avoid talking 3. Keep all sterile objects within view 4. Moisture will carry bacteria across/ through a cloth or paper barrier 5. Open all sterile packages away from the sterile field to prevent crossover and contamination
Principles and Practices of Surgical Asepsis - All objects use in the sterile field must be sterile - Sterile objects remain sterile when touched by another sterile object - Sterile objects or fields which fall out of the range of vision or below one‟s waist are considered contaminated - Sterile items become contaminated when they come in contact with microorganism transported through the air - When sterile object/field comes in contact with another surface, it becomes contaminated - The edges of the sterile field are considered unsterile
Standard Precaution - To be used in all clients in the hospital - To be used in the following situations: a. contact with blood, body fluid, excretions and secretions b. contact with non-intact skin c. contact with mucous membrane - wash hands after contact with blood, body fluids, secretions, excretions, or contaminated objects - wear gloves when touching blood, body fluids, secretions, excretions or contaminated objects - wear mask, goggles, or face shield if there is potential for splashes or sprays of blood, body fluids, secretions or excretions to prevent splashing into the eyes or mucous membranes
- Use biohazard bag for linens soiled with blood, body fluids, secretions, or excretions - Place sharps or needles in puncture-resistant container - do not recap, bend, or break needles
Airborne Precaution Measles Varicella Tuberculosis - use private room (negative airflow room) - close the door at all times
Use HEPA filters (High-Efficiency Particulate Air) - Particulate respirator/mask for health care workers - Surgical mask for patient during transport - discard tissue wipes with sputum in plastic bags
Droplet Precautions Pneumonia Meningitis Rubella Scarlet fever Diphtheria Pertussis - use surgical mask Use disposable eating utensils
Contact Precautions Herpes simplex Staphylococcal infection Hepatitis A Respiratory syncytial virus (RSV) Wound/skin infection Methicillin-resistant staphylococcal aureus (MRSA) Vancomycin-resistant enterocolitis (VRE) Rotavirus infection (most common cause of diarrhea in the U.S.) - use gloves, gown (if clothing comes in contact with patients, environmental surfaces, or items in the room, if patient has diarrhea, wound drainage, or GI surgery).
TIME FOR A SHORT QUIZ 1. Which of the following is an appropriate nursing action when implementing standard precautions? A. Consider all body substances potentially infectious B. wear gloves whenever in contact with patient C. wear gown and gloves when caring for a client in droplet precaution D. place a body substance isolation sign on the client's door
2. Which of the following clients would qualify for hospice care? A. a client with metastatic cancer B. a client with left-side after a stroke C. a client who had coronary artery bypass surgery 1 week ago D. a client who is undergoing treatment for heroin addiction
3. For a hospitalized client, which statement reflects appropriate documentation in the client's medical record? A. "client had a good day" B. "seems to be mad at the physician" C. "small pressure ulcer noted at the lower back" D. "skin moist and cool" 4. The nurse will administer the client's 9 A.M. medications. The client is away from his room for ultrasound of the liver. Which nursing action is appropriate? A. have the client skip that B. ask the client's relatives to keep the medications for the client until he returns C. lock the medications in the medicine preparation area until the client returns D. leave the medications on the drawer of the client's bedside table 5. The nurse is caring for a client receiving patient-controlled analgesia (PCA) for pain management. Which statement about PCA is true? A. the PCA pump can‟t' infuse opioids continuously B. pain relief is initiated by the client as needed C. no complications related to opioid delivery by the pump exist D. the nurse prescribes the dosage of opioid for delivery dose of medication ANSWERS AND RATIONALE 1. A - Rationale: standard precautions are based on the concepts that all body substances are potentially infectious. The nurse should wear gloves when contact with body substances is potential, not when in contact with intact skin. Mask should be used as a barrier to prevent transmission of droplet infections. Signs on door are unnecessary for standard precaution. 2. A - Rationale: hospices provide supportive, palliative care to terminally ill clients and their families 3. D - Rationale: documentation should be factual and accurate, what are heard, seen, smelled, or felt. Documentation of ulcer should include exact size and location. Interpretations, conclusions, opinions should not be documented. 4. C - Rationale: the nurse must put the medicines in the secured area. She should not leave the medications at the bedside. The nurse should not omit doses of medications without physician's order 5. B - Rationale: the client pushes a button to self-administer narcotic analgesic. The PCA pump also allows for continuous infusions of the medication. The client may still experience complications of the medication. It is the physician who prescribes the medication order
VI. COMPUTATION OF DOSAGE OF MEDICATIONS 1. Oral Medication: Solids Desired dose / stock dose = quantity of drug D/S = Q 2. Oral/Parenteral Medications: Liquids Desired dose / stock dose x dilution = quantity of drug D/S x dilution = Q 3. IV fluids Rate a. gtts/min = volume in cc x gtt factor no. of hours x 60 min b. cc/hr = volume in cc or gtts/min x 4 no. of hours c. duration in hours = volume in cc cc/hr 4. Conversion of Temperature a. C to F = (C x 1.8) + 32 note: (1.8 is 9/5) b. F to C = (F – 32) (0.55) note: (0.55 is 5/9) Time for a Short Quiz ! ! ! 1. An antihypertensive agent, minoxidil (Loniten) 5mg p.o. is ordered. Stock is 2.5 mg/tab. How many tablets should be administered? 2. The expectorant guiafenesin (Robitussin) 300 mg. p.o. has been ordered. The bottle is labeled 100 mg/5 ml. How many ml should be given? 3. The physician‟s order reads: “Administer D5LR 3L for 24 hours.” a. to how many gtts/min will you regulate the IVF? b. how many ml/hr will be infused? 4. 38.3C equals how many degrees Farenheit? 5. 108.6F equals how many degrees Celsius?
ANSWERS 1) D/S = Q 5mg . 2.5mg/tablet = 2 tablets 2) D/S x dilution = Q 300 mg x 5 ml 100 mg = 15 ml 3) a) vol. in cc x gtt factor = gtts/min no. of hours x 60 min 3,000 cc x 15 24 x 60 45,000/1440 = 31 gtts/min b) cc/hr vol in cc no. of hrs = 3,000 cc / 24 hrs = 125 cc/hr 4) C to F = C x 1.8 + 32 = (38.3 x 1.8) + 32 = 68.9 + 32 = 100.9 F 5) F to C = (F – 32) (0.55) = (108.6 – 32) (0.55) = (76.6) (0.55) = 42.1 F
VII. NORMAL VALUES 1. Complete Blood Count (CBC) RBC (erythrocytes) – 4.5 – 5.5 million/cu.mm WBC (leukocytes) – 5,000 – 10,000/cu.mm Platelet s (thrombocytes) – 150,000 – 450,000/cu.mm 2. Hemoglobin (hgb) = 12 -17 G/dL 3. Hematocrit (hct) male: 42 – 52% Female: 40 - 48% 4. Differential Count (Leukocytes) Neutrophils – 60 – 70% Eosinophils – 1 -4% Basophils – 0 – 0.5% Lymphocytes – 20 – 30% Monocytes – 2 – 6% 5. Blood Coagulation Studies Prothrombin Time (PT) = 11 – 16 sec Partial Thromboplastin Time (PTT) = 60 – 70 sec Activated Partial Thromboplastin Time (APTT) = 30 – 45 sec Bleeding Time = 1 – 9 sec Clotting Time = 8 – 15 sec 6. Blood Urea Nitrogen (BUN) = 8 -25 mg/dL 7. Blood Lipids Serum Cholesterol = 150 – 200 mg/dL Serum Triglycerides = 140 – 200 mg/dL Low Density Lipoprotein (LDL) = less than 130 mg/dL High Density Lipoprotein (HDL) = 30 – 70 mg/dL
8. Serum Enzymes Studies Aspartate Amino Transferase (AST/SGOT) = 7 – 40 U/ml Alanine Aminotransferase (ALT/SGPT) = 10 -40 U/ml Creatine Phosphokinase (CK-MB) Male: 50 – 325 mU/ml Female: 50 – 250 mU/ml 9. Troponin Troponin I = less than 0.6 ng/ml (grater than 1.5 ng/ml indicates myocardial infarction (MI) Troponin T = 0 to less than 0.1 ng/ml (greater than 0.1 – 0.2 ng/ml indicate MI) 10. Blood Uric Acid (BUA) = 2.5 – 8mg/dl 11. Serum Electrolytes Potassium (K+) = 3.5 – 5.5 mEq/L Sodium (Na+) = 135 – 145 mEq/L Calcium (Ca+) = 4.5 – 5.5 mEq/L Magnesium (Mg+) = 1.5 – 2.5 mEq/L 12. ECG Complexes P – wave = 0.04 – 0.11 sec PR interval = 0.12 – 0.20 sec QRS complex = 0.05 – 0.10 sec T – wave = not exceed 5mm amplitude 13. Central Venous Pressure (CVP) = 5 – 12 cm H2O 14. Pulmonary Artery Pressures Pulmonary Artery Pressure (PAP) = 4 – 12 mmHg Pulmonary Capillary Wedge Pressure (PCWP) = 4 – 12 mmHg 15. Serum Ammonia = 40 – 80 mcg/dL
16. Blood Glucose Level Fasting Blood Glucose (FBG) = 70 – 110 mg/dL Glycosylated Hemoglobin (HbAIc) = 4.4 – 6.4% (7.5% or less: good diabetic control) 17. Thyroid Hormone Levels Triiodothroxine (T3) = 75 = 200 ng/dL Thyroxine (T4) = 4.5 – 11.5 mcg/dL 18. Routine Urinalysis Color = amber/straw pH = 4.5 – 8 (average: 6; slightly acidic) specific gravity = 1.010 – 1.025 protein = absent RBC = 0 – 5 Pus = absent Ketones = absent Casts = 0 – 4 19. Creatinine Clearance = 100 – 120 ml/min 20. Serum Creatinine = 0.7 – 1.4 mg/dL 21. Snellen’s Test = 20/20 22. Intraocular Pressure = 11 -21 mmHg 23. Cerebrospinal Fluid (CSF) Studies Opening pressure = 0 – 15 mmHg or 75 – 180 mm H20 Glucose = 50 – 80 mg/dL Protein = 20 – 50 mg/dL 24. Arterial Blood Gas Analysis Blood pH = 7.35 – 7.45
HCO3 = 22 – 26 mEq/L
Pa O2 = 80 – 100 mmHg
O2 saturation = 95 – 100 %
paCO2 = 35 – 45 mmHg Note: O2 saturation 90% and below indicate that hypoxia is severe
25. Therapeutic Serum Medication Levels Acetaminophen = 10 – 20 mcg/dL Phenytoin (Dilantin) = 10 – 20 mcg/dL Theophylline = 10 – 20 mcg/dL Carbamazepine (tegretol) = 5 – 12 mcg/dL Gentamycin Sulfate = 5 – 10 mcg/dL Magnesium Sulfate = 4 – 7 mg/dL Digoxin = 0.5 – 2 ng/ml Lithium = 0.5 – 1.5 mEq/L Coumadin = INR: 2 – 3
VIII. NUTRITION AND DIET Macronutrients (energy nutrients) 1. Carbohydrates (Go) – provides energy Sources: cereals, fruits, vegetables, milk Caloric deficiency is referred to as Marasmus, characterized by loss of weight, skin turgor, old-man look, distended abdomen, hypotonia Nursing Considerations for Carbohydrates High: bipolar disorder, manic phase; associated in obesity; associated in colon and breast cancer; for Marasmus Low: diarrhea; gas distention; diabetes mellitus 2. Fat (Glow) – provides essential fatty acids and energy; absorbs and transports fatsoluble vitamins (A, D, E, K); protects vital body tissues; insulates body Sources: fats and oils, meats, fish, nuts, some seeds, dairy products Nursing Considerations for Fats High: dumping syndrome, ulcer, when taking ADEK Low: acne vulgaris, pancreatitis, cholecystitis, cardiac patient
3. Protein (Grow) – growth and repair of tissues; maintain fluid and acid-base balances, provides energy. Sources: meat, fish, dairy products, eggs, nuts, legumes, cereals Protein deficiency is referred to as Kwashiorkor, characterized by lethargy, inadequate growth, loss of muscular tissue, increases susceptibility to infection, EDEMA Nursing Considerations for Protein High: hepatitis, PIH, nephrotic syndrome, burn patient Low: chronic renal failure, PKU, liver cirrhosis
MICRONUTRIENTS (VITAMINS AND MINERALS) Fat – Soluble Vitamins 1. Vitamin A (Retinol) – affects vision; health of skin; growth of hair, nails, bones, and glands; prevents infection Sources: dairy product, liver, green, yellow and orange fruits and vegetables Deficiency: night blindness, xeropthalmia, poor growth, dry skin Toxicity: fetal malformations, hair loss, skin changes, bone pain Nursing Considerations for Vitamin A Not to excessive especially amongst small children, it might cause discoloration of the skin 2. Vitamin D (Ergocalciferol) – Calcium not absorbed without Vit. D. Calcium and phosphorus absorption; bone mineralization Sources: dairy products, eggs, yolks, fatty fish Deficiency: Rickets in children, Osteomalacia for adults Toxicity: growth retardation, kidney damages, calcium deposits in soft tissue Nursing Considerations for Vitamin D Breast-fed infant must be exposed to mild sunlight Must receive by those who are receiving calcium supplement
3. Vitamin E (Tocopherol) – Antioxidant: prevents cell damage Sources: vegetable oils, nuts, seeds, whole grain Deficiency: red blood cell destruction, nerve destruction Toxicity: None, no supplements with anticoagulant drugs Nursing Considerations for Vitamin E To prevent premature aging Commonly given to client with dementia 4. Vitamin K (Menadione) – blood clotting Sources: green vegetables, intestinal synthesis Deficiency: hemorrhage Toxicity: anemia, jaundice Nursing Considerations for Vitamin K Commonly given to neonate to prevent bleeding (note: neonates have sterile intestine) Antioxidant to Coumadin Water – Soluble Vitamins 1. Vitamin C (Ascorbic Acid) – required for iron absorption. Antioxidants: prevents cell damage; causes collagen formation; affects health of teeth and gums Sources: citrus fruits, guava, strawberries, tomatoes, broccoli, cabbage, greens, potatoes Deficiency: Scurvy, poor wound healing, weakness, impaired immune response, pin point hemorrhages, bleeding gums Toxicity: more than 2g can cause diarrhea, kidney stone formation. Most renal calculi thrive in acid urine. GI upsets, fatigue
2. Vitamin B1 (Thiamine) – muscle nerve function; co-enzyme for energy metabolism Sources: pork liver, organ meats, nuts, legumes, eggs, milk, whole and enriched grains. Potatoes Deficiency: Beriberi, poor coordination, edema, weakness Nursing Considerations for Vitamin B1 Those with increased metabolic rate should increase B1 (e.g. pregnant women and client with fever) Alcoholic client 3. Vitamin B2 (Riboflavin) – coenzyme for energy metabolism Sources: milk, dairy products, organ meats, lean meats, enriched grains, green leafy vegetables, fish, eggs For skin problem such as eczema and scabies
4. Vitamin B3 (Niacin) - coenzyme for energy metabolism Sources: kidney, liver, poultry, lean meat, fish, peanut butter, dried peas and greens, whole grain, nuts Deficiency: ariboflavinosis, cheilosis, glossitis, seborrheic, dermatitis, pellagra Toxicity: vasodilation, liver damage 5. Vitamin B6 (Pyridoxine) – supplemented in anti-TB therapy as drugs compete with absorption of B6. Metabolism of amino acids and protein, neurotransmitter synthesis. Sources: meats, poultry, fish, organ meats, yeast, oats, corn, peanuts, bananas, egg yolk, whole grain cereals, wheat germ, potatoes Deficiency: headache, anemia, convulsion, nausea Toxicity: nerve destruction if >2g/day Nursing Considerations for Vitamin B6 For patient who is receiving INH to prevent peripheral neuritis For those who are taking contraceptives
6. Vitamin B9 (Folacin/Folic Acid) – aids metabolism of DNA and RNA; red blood cell maturation Sources: green leafy vegetables, asparagus, organ meats, beef, fish, legumes, eggs, yeast, wheat germ, grapefruits and orange. Deficiency: megaloblastic anemia, poor growth, birth defects 7. Vitamin B12 (Cyanocobalamine) – requires intrinsic factor for absorption in the stomach. This is not absorbed in Pernicious Anemia. - Folate metabolism, nerve function. Sources: liver, kidney meat, oyster, cheese, eggs, shrimp, milk Deficiency: megaloblastic anemia, poor nerve function MINERALS 1. Potassium (K) – major intracellular cation. - given with furosemide - fluid balance, nerve and muscle function Sources: bananas, avocado, strawberries, cantaloupe, oranges, mushrooms, carrots, spinach, tomatoes, potatoes, raisins (other dried fruits), fish, beef, veal, pork Deficiency: muscular weakness, fatigue, confusion Toxicity: muscular weakness, cardiac arrest 2. Iron (Fe) – components of hemoglobin and enzymes Sources: liver, meat, dark-green vegetables, green and red beans (dried beans), egg yolk, breads, cereals, clams Deficiency: anemia, weakness, infections, fatigue, pale eye membranes Toxicity: Acute: shock, death. Chronic: liver damage, cardiac failure Nursing Considerations for Iron Must be given between meals If given per orem: black stool If liquid: use straw If injectible: don’t massage
3. Calcium (Ca) - 99% of calcium is in the bone - Major component of renal calculi - if increased, calcitonin is given - Bone and tooth formation; blood clotting; muscle function; nerve transmission; blood pressure Sources: yogurt, low fat milk and dairy products, green leafy vegetables, broccoli, carrots, seafood, nuts, legumes, whole grains, rhubarb Deficiency: stunted growth in children; bone loss (osteoporosis) in adults Toxicity: extra calcium usually excreted; possible depressed absorption of some other minerals and kidney damage 4. Sodium (Na) - Water goes to where Na is ! - given with lithium carbonate - fluid balance, nerve impulse transmission Sources: table salt, soy sauce, cured pork, milk, butter, ketchup, canned food, processed foods, white and whole wheat bread, cheese, mustard, snack foods Deficiency: muscle cramps, reduced appetite, weakness Toxicity: high blood pressure in some people
IX. THERAPEUTIC DIETS Acid-ash diet retards the formation of alkalinic renal stones indicated to patients with renal calculi (Alkaline stones) e.g. cheese, cranberries, eggs, meat, plums, prunes, whole grains Alkaline ash diet retards the formation of acid renal stones indicated to patients with renal stones (Acidic stones) e.g. fruits (except cranberries, plums, prunes), milk, vegetables
Bland diet low fiber, mechanical irritants, chemical stimulants indicated for patients with gastritis, diarrhea, biliary indigestion, and hiatal hernia BRAT diet banana, rice, apple, toast indicated for patients with diarrhea Butterball diet spare protein but high in carbohydrates indicated for patients with liver disorders Clear liquid diet to relieve thirst and help maintain fluid balance indicated for post-operative patients and following vomiting and gastroenteritis Diabetic diet well balance diet the purpose is to maintain near to normal blood glucose level indicated to patients with diabetes mellitus Full Liquid diet it serves to provide nutrition to patients who cannot chew or tolerate solid foods indicated to patients with stomach upsets, post-surgical patients, after progression from clear liquid diet Giordano diet spare protein indicated to patients who suffers from Chronic Renal Failure
Gluten free diet no to BROW - Barley, Rye, Oat, Wheat this is the diet of a patient who suffers from Celiac's disease Halal diet no pork diet diet of the Moslems High fiber diet fruits and vegetable it speeds up the passage of food to the digestive tract, softens the stool indicated to patients who are constipated, with diverticulitis, with hyperlipedemia (to initiate removal of fats) High Protein diet lean-meat, cheese, eggs indicated to patients with nephrotic syndrome Kosher diet meat and milk cannot be served simultaneously diet of the Orthodox Jews Low carbohydrate diet indicated to patients with Dumping Syndrome Low fat/cholesterol diet it serve the purpose of reducing hyperlipidemia, and to patients with intolerance to fats indicated to patients with cardiovascular diseases, patients who underwent resection of the small intestines, hypertension, cholecystitis and cholelithiasis Low residue diet reduces the bulk of stools
indicated to patients with ulcerative colitis, diverticulitis. Patients who will undergo surgery of the GI tract Low sodium diet indicated to patients with cardiovascular and renal disorder Purine restricted diet to reduce uric acid indicated to patients with gouty arthritis, renal calculi, and hyperuricemia Sodium-restricted diet indicated to patients with heart failure, hypertension, renal diseases, PIH, and steroid therapy Soft diet used to provide nutrition for those patients having problems in chewing for patients with ill-fitting dentures; transition from full-liquid to general diet, patients with gastrointestinal disturbances such as gastric ulcers and cholelithiasis Tyramine-free diet use to prevent hypertensive crisis for patients who are taking in MAOI antidepressant no to ABC's - Avocado, Banana, Canned and Processed Foods, and also, no to fermented foods Vegan diet diet of the Seventh Day Adventists vegetarian diet Yin diet Cold deserts after a surgery. It is a Chinese belief
X. POSITIONS I. Positions for clients with Respiratory Disorders After lung Biopsy: Affected Side - To apply pressure in the site and prevent bleeding During Thoracentesis: Upright or Sitting Position at the edge of the bed, arms on overbed table, leaning forward, and feet supported on a foot stool - For easy access to the site of insertion of aspiration needle. It also promotes comfort. After Thoracentesis: Unaffected side for 1 hour to prevent leakage of fluid into the thoracic cavity. Client on Oxygen Therapy: Semi-Fowler’s position - For lung expansion and ventilation. During Tracheostomy or Endotracheal Tube Suctioning: Semi-Fowler’s position - To facilitate suction catheter insertion and enhance removal of mucous membrane . After Bronchosgraphy and Bronchoscopy: Side-lying/lateral or semi-fowler’s position - To promote drainage of secretions from the mouth and prevent aspiration. COPD: Sitting Upright, leaning forward position, with arms on overbed table at shoulder level (orthopneic position) - To allow lung expansion. Epistaxis: Sitting/Upright position, leaning forward with head tipped - To prevent aspiration of blood. After Tonsillectomy: Side lying/lateral or prone position with pillow under the chest To promote drainage of mouth secretions and prevent aspiration. If client is awake, maybe placed in semi-fowler’s position. Pulmonary Edema: High-Fowler’s position with legs slightly dependent (lowered) - To relieve dyspnea. Lowering the legs reduces venous return thereby reduces cardiac workload. Pneumonectomy: Slightly towards affected side, with head elevated or Semi-Fowler’s position for lung expansion - To prevent flooding of blood coming from the affected side to the remaining lung. Slight turning prevents mediastinal shift. Flail Chest: Semi-fowler’s position, turned towards the affected side or the affected side be supported - To control paradoxical breathing and prevent hypercapnea. Child with Epiglottitis, laryngotracheobronchitis, bronchiolitis: Tripod position (sitting upright, leaning forward with hands on the bed or floor) – to facilitate breathing. SIDS (Sudden Infant Death Syndrome): Supine or Side-lying position in a firm bed during sleep. Do not place the infant in prone position during sleep. Do not place infant in soft bed or over a pillow or comforter.
II. Positions for clients with Cardiovascular and Hematologic Disorders Myocardial Infarction (MI): Semifowler’s position – for maximum lung expansion and improves myocardial oxygenation. Congestive Heart Failure (CHF): High-fowler’s position – it relieves dyspnea and reduces cardiac workload. When taking Nitroglycerin: Sitting or Supine position – to prevent orthostatic hypotension Arterial Insufficiency: Lower extremities slightly lower than the level of the heart (dependent position) – it promotes arterial flow Venous Insufficiency: Lower extremities elevated – it promotes venous return and relieves edema of the legs. Tetralogy of Fallot in “tet spell” (hypoxic episode): Knee-to-Chest position or Squatting position – to improve venous return, increases cardiac output and improve tissue oxygenation. Air Embolism: Left Side-lying position, Trendelenburg position – it allows the air to be absorbed in the right side of the heart thus prevents pulmonary embolism.
III. Positions for clients with Gastrointenstinal, hepato-Biliary and Pancreatic Disorders During Abdominal Examination: Dorsal recumbent position – to relax the abdominal muscles and facilitate abdominal examination. During Rectal Examination: Lateral/Side-lying position – to facilitate examination of the area. During Nasogastric tube (NGT) insertion: High-fowler’s position, with the neck hyperextended, initially. Flex the neck slightly once the tube reaches the oropharynx. During and after NGT feeding (gastric gavage) and Gastrostomy feeding: Semifowler’s position – to prevent reflux and aspiration of feeding. After insertion of Intestinal/Nasogastric Tube: Right Side-lying position – it helps advance the tube into the duodenum. During insertion of Parenteral Nutrition (TPN) Catheter: Trendelenburg position – to engorge the vein and facilitate insertion of the catheter to the subclavian vein. It also prevent air embolism. During Enema Administration: Left lateral position for adult. Dorsal Recumbent position for infant and children.
Hiatal Hernia: Upright/Sitting position during and after eating – To prevent gastroesophageal reflux. After Gastric and Biliary Surgery: Semi-fowler’s position – To promote lung expansion and ventilation and also prevents atelectasis. Dumping Syndrome: Left side-lying position – To slow down emptying of gastric content into the jejunum. Peritonitis: Semi-fowler’s position – To localize the inflammatory process in the pelvic area. Colostomy Irrigation: Semi-fowler’s position, then sitting on a bowl once ambulatory. After Hemorrhoidectomy: Side-lying position – It prevents pressure in the operated area and promote comfort. After Infant Feeding: Right side-lying position – It prevents gastroesophageal reflux and aspiration. After Cleft Lip Repair: Side-lying position – To promote drainage and prevent aspiration. No to Prone position to prevent tension on the suture line. Restraint the elbow to prevent trauma in the suture line. After Cleft Palate Repair: Side-lying and Prone position – to promote drainage and prevents aspiration. After repair of Imperforate Anus: Side-lying position or Supine with the legs suspended at the right angle – To prevent pressure in the area and minimize discomfort. During Liver Biopsy: Left Side – to facilitate approach to the liver After Liver Biopsy: Right Side with rolled towel under the puncture site – it helps apply pressure at the puncture site and prevent bleeding. During Paracentesis: Sitting/Upright position – it facilitates aspiration of abdominal fluid.
IV. Positions for clients with Fluid-Electrolyte, Acid-Base Imbalances, GenitoUrinary Disorders, Shock, Burns During insertion of Urinary Catheter: Supine with legs extended and abducted for male. Dorsal Recumbent for female. During Cyctoscopy: Lithotomy position – to promote easy insertion of cystoscope. During Renal Biopsy: Prone position – it is because the kidneys location is retroperitoneally. After Renal Biopsy: Supine position with small pillow or rolled towel under the posterior lumbar area to apply pressure and prevent bleeding. During insertion of Peritoneal Catheter: Dorsal Recumbent or Semi-fowler’s position with the knees flexed – To relax abdominal muscles and facilitates the insertion of the catheter. During Vaginal Examination: Dorsal Recumbent if she is in bed. Lithotomy position if the examination is done in the table. Shock: Modified Trendelenburg position – to increase venous return and increased force of cardiac contractility thus increases cardiac output and tissue perfusion. Burns: Supine position – To promote position of extension and prevent contractures.
V. Positions for clients with Neurologic Disorder During Lumbar Puncture: Lateral, Knee-chest position (fetal/flexed/C-position/shrimp position) – to widen intervetebral spaces and facilitate insertion of spinal needle. After Pantopaque (oil-based dye) myelogram: Lie Flat for 6 to 8 hours – to prevent spinal headache. After Metrizamide (water-based dye) myelogram: Semi-fowler’s position for 8 hours – to prevent meningeal irritation. Intracranial Pressure: Lateral, Semi-fowler’s position – to reduce the pressure, promote adequate lung expansion and improve cerebral tissue perfusion. Spinal Cord Injury: Flat/Supine position on a firm space – to maintain alignment of spine.
VI. Positions for clients with Eye and Ear Disorders After Eye Surgery: Supine position turned to the Unoperated Side – to prevent trauma to the affected eye. If the client is fully awake: Semi-fowler’s position. Retinal Detachment Preoperative: Dependent position (lower) – to prevent further detachment of the retina. Postoperative: Dependent position (upper) – to lower the sclera and choroids by gravity and allow attachment of the area of retinal detachment. After Ear Surgery: Unoperated Side – to prevent trauma to operated side.
XI. PROCEDURES ABDOMINAL ASSESSMENT Purpose - determine the presence of mass, abnormal bowel sounds, lesions, and other abnormalities in the abdominal region. Nursing Keypoints: Position: Dorsal Recumbent Sequence: (IAPP) Inspection, Auscultation, Percussion, Palpation. Start palpating from RLQ, RUQ to LUQ, to LLQ palpation is done last because it can possibly alter the bowel rhythms and may therefore give rise to abnormal sounds No to palpation to patients with Wilhm's tumor and abdominal Aortic Aneurysm
ARTERIAL BLOOD GAS ANALYSIS Purpose - to monitor the patient's response to oxygen therapy and detects the presence of acid-base imbalance. Nursing Keypoints: no to suctioning prior to obtain blood specimen assess for bleeding and hematoma at the puncture site apply firm pressure at the puncture site for 5-10 minutes specimen should be placed in iced-container Assess for metabolic alkalosis for patient with vomiting, and on the other hand, observe for signs and symptoms of metabolic acidosis for patients with diarrhea.
BARIUM ENEMA Purpose – To assess the large intestines Nursing Keypoints: provide a liquid diet before the procedure ensure that a laxative is given before the procedure to promote better visualization, and after the procedure to prevent constipation report to the doctor if bowel movement does not occur in 2 days instruct the patient to increase fluids and eat foods rich in fiber the patient should also increase intake of fluids
BARIUM SWALLOW Purpose - To assess for the esophagus, stomach, and some portion of the small intestines Nursing Alert: NPO for 6-8 hours before the procedure withhold anticholinergic and narcotics for 24 hours before test laxative is administered after the procedure to counteract the constipating effects of barium instruct patient to increase fluids and intake of fiber-riched foods
Bone Marrow Biopsy Purpose: aspirating bone marrow for laboratory studies. Preferred site is the iliac crest (proximal tibia in children), but may also use sternum, iliac spine Nursing Keypoints: administer sedative as ordered positioning (prone for iliac crest) pressure on the site for 5 to 10 minutes after aspiration placed on affected side (with sandbag underneath) assess for discomfort and bleeding at the site
CARDIAC CATHETERIZATION Purpose – To measure oxygen concentration saturation, tension and pressure in various chambers of the heart. To determine a need for cardiac surgery. Nursing Keypoints: check for informed consent assess allergy to iodine NPO for 6-8 hours before procedure check for distal pulses after the procedure check for bleeding at the arterial puncture site and apply pressure keep a 20 pounds sandbag at the bedside as a pressure instrument if bleeding occurs keep the patient flat on bed with the lower extremities hyperextended for 4-6 hours neurovascular assessment must be performed distal to the catheter insertion site and report any abnormal findings
CHEST X-RAY Purpose – To detect abnormalities of the organs in the thoracic area Nursing Keypoints: remove any metallic object before the procedure lead shield for women of childbearing age
CYSTOSCOPY Purpose – To assess the bladder and urethra Nursing Keypoints: if general anesthesia will be used, have the client on NPO; liquid diet if local anesthesia will be used monitor intake and output after the procedure, force fluids as prescribed administer sitz bath for abdominal pain pink-tinged or tea-colored urine is expected within 24-48 hours notify the doctor if bright red urine or clots occur
CT SCAN Purpose – Provides photograph of tissue densities with the use of radiation Nursing Alert: if contrast medium will be used, assess for any allergy to iodine and instruct the patient to be on NPO for 4 hours prior to procedure assess for any fear of close spaces (claustrophobia) this procedure is contraindicated to patients who are pregnant and obese (>300 lbs) Let the patient lye still during the whole course of the procedure.
CVP (CENTRAL VENOUS PRESSURE) MONITORING Purpose – It measures the pressure of the right atrium Nursing Keypoints: the nurse should place the zero level of the manometer at the level of the right atrium at the 4th intercostal space to get an accurate reading. instruct the client to avoid coughing and straining as it alters the readings normal CVP reading is 2-12 mmHg (when the tube is at the superior vena cava).
ELECTROCARDIOGRAM (ECG) Purpose – records electrical waves of the heart Nursing Keypoints: instruct the patient to lie still, breathe normally during the procedure let the patient refrain from talking during the test ST segment elevation or T wave inversion, indicates MI
ELECTROENCEPHALOGRAM (EEG) Purpose – records the electrical activity of the brain, detects intracranial hemorrhage and tumors Nursing Keypoints: advise the client to shampoo before and after the procedure. may use acetone after Withhold stimulants, antidepressant, tranquilizers, and anticonvulsants for 24-48 hours prior to the test.
FASTING BLOOD SUGAR (FBS) Purpose – detects diabetes mellitus Nursing Keypoints: normal blood sugar level is 80-120 mg/dl a blood sugar level of more than 140 mg/dl confirms diabetes
GASTRIC ANALYSIS Purposes – this test is used to detect ulcers and to rule-out pernicious anemia. It may also be done to analyze acidity, appearance and volume of gastric secretions Nursing Keypoints: in gastric ulcer, HCl is normal in duodenal ulcer, HCL is elevated refrigerate gastric samples if NOT tested within 4 hours
INTRAVENOUS PYELOGRAPHY (IVP) Purpose – visualization of the urinary tract Nursing Keypoints: NPO for 8-10 hours before the procedure administer laxative to clear bowels before the procedure check for allergy to iodine, seafood or shellfish before the procedure since the procedure requires the use of iodine based dye Keep epinephrine at the bedside to counteract possible allergic reaction. IVP requires the use of a contrast medium while KUB does not inform the patient about the possible salty taste that may be experienced during the test
LIVER BIOPSY Purpose – to determine liver disorders Nursing Keypoints: check for the consent obtain the result of blood tests before aspiration since bleeding may occur
let the patient to inhale, exhale and hold breath during the insertion of to stabilize position of the liver and prevent accidental puncture of the diaphragm position the patient on the right side after liver biopsy with pillows underneath to prevent bleeding bedside for 24 hours after the procedure
LUMBAR PUNCTURE Purpose – to withdraw CSF to determine abnormalities Nursing Keypoints: before the procedure: empty bladder and bowel position: C-position (fetal position) during the procedure: needle is inserted between L3-L4 or L4-l5 to prevent accidental puncture to the spinal cord since the spinal cord ends at L2 after: position the patient flat for 6-12 hours to prevent spinal headache increase fluid intake
MAMMOGRAPHY Purpose – detects the presence of breast tumor Nursing Keypoints: instruct the patient not to use deodorant, talcum powder, lotion, perfume or any ointment on the day of exam as these may give false-positive result let the patient know that her breasts will be compressed between 2 x-ray plates provide teachings related to self-breast examination done 7 days after menstruation Position: lying down with pillow under the shoulder of the breast being examined or sitting in front of a mirror while raising the hands of the side of the breast being examined.
MANTOUX TEST Purpose – a test to determine exposure to TB Nursing Keypoints: a positive test yields an induration of 10 mm. or more for foreign born children below 4 years old
an induration of 5 mm or more is considered positive in patients with HIV, with treated TB, and if he has had a direct exposure TB patients BCG may cause false positive reaction assess for previous history of PTB and report immediately to the doctor result is read after 48-72 hours
MRI (Magnetic Resonance Imaging) Purpose – provides cross-sectional images of brain tissues, more detailed than a CT scan Contraindications: pregnant women obesity (more than 300 lbs) claustrophobic patients patients with unstable vital signs patients with metal implants like pacemaker, hip replacements and jewelleries
PARACENTESIS Purpose – to assess the contents of the peritoneal fluid Nursing Keypoints: check for consent patient is weighed before and after procedure instruct the patient to void prior to the procedure to prevent accidental puncture of the bladder during the procedure, instruct the patient to sit up with feet resting on footstool evaluate the effect of the procedure by assessing – weight, abdominal girth, respiratory rate/pulse rate notify the physician if the urine becomes bloody, pink or red
RINNE’S TEST Purpose – used to differentiate between conductive and sensorineural hearing losses Nursing Keypoints: the vibrating tuning fork is shifted between two positions: against the mastoid bone (bone conduction) and two inches from the opening of the ear-canal (air conduction) in conductive hearing loss, bone conduction lasts longer than air conduction
SCHILLING’S TEST Purpose- used to detect Vitamin B12 absorption Nursing Keypoints: excretion of 8% - 40% of ingested radioactive Vitamin B12 withing 24 hours is normal. Excreting more than 40% indicates pernicious anemia requires 24-hour urine specimen keep the patient NPO except for water, 8-12 hours before the test
SPUTUM EXAM Purpose – determines the presence of microorganisms in the sputum Nursing Keypoints: instruct patient to rinse mouth with water ( no to mouth wash or tooth paste) specimen is collected upon rising amount required: 15 ml instruct the patient to take several deep breaths and then cough deeply
STOOL ANALYSIS Purpose – assessment of bacteria, virus, malabsorption and blood in the stool Nursing Keypoints: avoid aspirin, indomethacin, steroids, dark colored foods, red meat and Vitamin C for three days before the test as these may give a false positive result.
SUCTIONING Purpose – to obtain sputum sample and clear the airway Nursing Keypoints: hyperoxygenate the patient before and after the procedure apply intermittent suction on withdrawal of the catheter do not suction the patient for more than 15 seconds
SWAN-GANZ CATHETERIZATION Purpose – used to monitor pulmonary artery pressure (PAP) and pulmonary capillary wedge pressure (PCWP). Nursing Keyponts: the catheter has four lumen (one for CVP, one for fluid infusion and venous access for blood samples, one for monitoring PAP and PCWP and the last lumen is used for inflation and deflation of the balloon. if the fifth lumen exists, it is used for measuring oxygen saturation of the blood the normal adult PAP systolic and diastolic pressure is 20 to 30 mmHg the normal PCWP is 8-13 mmHg the only time the balloon should be inflated after it is in place is when obtaining further PCWP readings.
THORACENTESIS Purpose - aspiration of fluid and/or air from the pleural space Nursing Keypoints: check the consent position: sitting on the side of the bed with feet on a chair, leaning over a bedside table if the patient cannot sit, he lie on his affected side with hands of that side resting on opposite shoulder instruct the patient not to cough, breathe deeply or move during the procedure after the procedure: position the patient on the unaffected side/puncture site up check for bleeding at the puncture site and monitor respiratory function
notify the physician if signs of pneumothorax, air embolism and pulmonary edema
TONOMETRY Purpose – measures intraocular pressure Nursing Keypoints: normal reading is 12-21 mmHg a reading of 25 mmHg indicates glaucoma
URINALYSIS Purpose – to assess characteristics of urine Nursing Keypoints: first voided morning sample preferred: 15 ml use clean container decreased specific gravity: diabetes insipidus increased specific gravity: diabetes mellitus, dehydration, SIADH (+) protein: PIH, nephrotic syndrome (+) glucose: diabetes mellitus, infection
URINARY CATHETERIZATION Purposes – To determine residual urine and obtain sterile specimen Nursing Keypoints: the procedure is sterile maintain a close system the drainage bag must always be below the bladder to avoid back flow of urine the catheter bag should not be allowed to lie on the floor do not allow the drainage spout to touch the collection receptacle or on the toilet bowl when draining it provide urine acidification
URINE COLLECTION, 24 HOUR Purpose – determines the excretion of substances from the kidneys, adrenal glands and the stomach Nursing Keypoints: required for ACTH test and schilling‟s test discard the first voided urine
WEBER TEST Purpose – used to detect the presence of unilateral hearing loss Nursing Keypoints: the tuning fork is set into vibration and placed on the patient‟s forehead or teeth placement of the teeth is generally more reliable even when the patient has false teeth
X-RAY Purpose – provides radiological data for assessment of certain organs and bones Nursing Keypoints: assess the patients exposure level to radiation instruct the patient to remove all jewelries and other metallic objects before the procedure
Related Documents
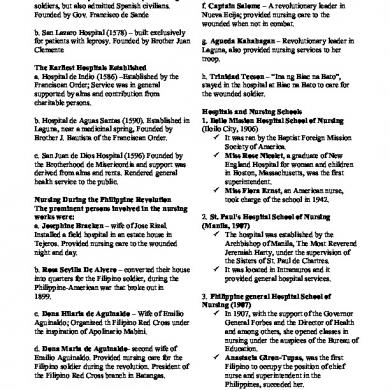
Fundamentals Of Nursing Reviewer
February 2021 1
Theoretical Foundations Of Nursing
February 2021 2
Theoretical Foundation Of Nursing
February 2021 0
Theoretical Foundations Of Nursing
February 2021 0
Fundamentals Of Astrology
January 2021 1
105174065-fundamentals-of-photonics.pdf
January 2021 0More Documents from "renatotorresa2905"

Japanese Literature: The Box Man By Kobo Abe.
January 2021 3
Star-ccm+training-ver0113-rev4.pdf
March 2021 0
Grab Hopper Dredger
February 2021 0
Wee Budget
January 2021 0
