Acupuntura Laser Book
This document was uploaded by user and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this DMCA report form. Report DMCA
Overview
Download & View Acupuntura Laser Book as PDF for free.
More details
- Words: 50,717
- Pages: 234
Loading documents preview...
Gerhard Litscher and Detlef Schikora (Eds.)
LaserneedleAcupuncture Science and Practice
PABST
III
Gerhard Litscher and Detlef Schikora (Eds.)
Laserneedle - Acupuncture Science and Practice
PABST SCIENCE PUBLISHERS Lengerich, Berlin, Bremen, Miami, Riga, Viernheim, Wien, Zagreb
IV Bibliographic information published by Die Deutsche Bibliothek Die Deutsche Bibliothek lists this publication in the Deutsche Nationalbibliografie; detailed bibliographic data is available in the Internet at.
This work is subject to copyright. All rights are reserved, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in other ways, and storage in data banks. The use of registered names, trademarks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The authors and the publisher of this volume have taken care that the information and recommendations contained herein are accurate and compatible with the standards generally accepted at the time of publication. Nevertheless, it is difficult to ensure that all the information given is entirely accurate for all circumstances. The publisher disclaims any liability, loss, or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents of this volume.
Gerhard Litscher, Prof MSc PhD MDsc Medical University of Graz Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine Auenbruggerplatz 29 8036 Graz / Austria Tel. ++43 316 385-3907, -83907 Fax ++43 316 385-3908 E-mail: [email protected] Detlef Schikora, PhD University of Paderborn Faculty of Science Warburger Straße 100 33095 Paderborn / Germany Tel. ++49 5251 60-3566 Fax ++49 5251 60-3490 E-mail: [email protected]
© 2005 Pabst Science Publishers, 49525 Lengerich, Germany Printing: D+L Printpartner GmbH, 46395 Bocholt, Germany ISBN 3-89967-199-6 (Europe), ISBN 1-59326-074-1 (USA)
V
Preface This compendium of „Laserneedle-Acupuncture“ conveys scientific and first practical results from the field of laserneedle acupuncture in an abridged and concise form. Just the thought of being pricked with needles is very uncomfortable for many people. Using the new, advanced laserneedle acupuncture method up to eight laserneedles are applied to the skin simultaneously, however, without puncturing the skin. Thus, painless, non-invasive acupuncture is possible for the first time. First public presentation of the laserneedle-system was in the year 2000 at the Medica fair in Düsseldorf. Three years of intensive scientific research and developmental work preceded. The basic idea of laserneedles originated from analysis of laser acupuncture, which was developed and spread throughout Europe in the 1990´s. It was obvious, that the technique of classic acupuncture as it had been practised for centuries, namely the simultaneous stimulation of therapy-specific acupoint combinations, became to leave its natural course. Today and in the past, acupoints are stimulated one after another using laser light, even though no evidence regarding identical effects achieved with Traditional Chinese Medicine has been documented in classic or modern literature. Suddenly, the simultaneous puncturing of acupoints according to the basic scheme of Chinese acupuncture was no longer important when practicing the Western method of laserpuncture. With the development of laserneedles, the goal to maintain the fascination of acupuncture itself was pursued: the complex diagnostic systemic approach on the one hand, and the simple manner of therapeutic application and its effects on the other. Simultaneous procedures, simple, manual handling during needle acupuncture with needle-equivalent stimulation effects and stimulation characteristics were the developmental goals of our laserneedle project. The main part of this volume includes „Peer-Review“ studies and thus, represents a scientifically substantiated work dealing with laserneedle acupuncture in particular and acupuncture in general. Noted scientists and well-known users have taken part in this book and reported about the scientific investigations and use of this new, advanced method in the field of acupuncture.
VI Non-invasive laserneedle stimulation can induce specific, reproducible effects in the brain. This is expressed by changes in different parameters such as cerebral blood flow velocity, which can be objectified using modern neuromonitoring methods for the first time. The results in this book show that cerebral effects induced by the new, painless laserneedle technique lie within similar dimensions as those evoked by manual needle acupuncture. For the first time, laserneedle acupuncture allows simultaneous optical stimulation of individual acupoint combinations. At the same time, variations in acupuncture on the body, ear or hand, as performed in our first study were made possible. Based on these investigations, the cerebral effects of laserneedle stimulation could be systematically objectified, specified and optimized for the first time. These scientific findings do not only have extensive consequences in laser medicine, but also build an important bridge between traditional Eastern and innovative Western medicine. Contact between the editors of this compendium developed in a typical modern way: per e-mail. Professor Litscher from the Medical University of Graz reported his interest in performing studies with laserneedle acupuncture to the University of Paderborn. Dr. Schikora from Paderborn answered back that he was very interested. What developed from this contact is documented in this book. Currently studies with laserneedle acupuncture are being performed in several University Clinics in Germany, Austria, Switzerland and France. All of these studies will contribute to a better understanding and objectification of effects not only for acupuncture with laserneedles but also for classic acupuncture and promote the use of this comprehensive, natural medical treatment method. Scientists agree that the 21st Century will be the Century of Photons, like the 20th Century was the Century of Electrons. It is certain, that exact understanding of the elementary interaction of photons with biological molecules, will lead to new, natural medical treatment methods which will reach far beyond acupuncture. January 2005
Detlef Schikora
Gerhard Litscher
University of Paderborn
Medical University of Graz
VII
Contents 1.
Laserneedles in acupuncture ............................................................... 1 1.1 Introduction and motivation ......................................................... 1 1.2 Dose-effect relationships in acupuncture ..................................... 4 1.3 Laserneedle acupuncture as a placebo method............................. 7 1.4 Physical characteristics of laserneedles...................................... 11 1.5 Acknowledgements .................................................................... 16 1.6 References .................................................................................. 16
2.
Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography................ 18 2.1 Introduction ................................................................................ 18 2.2 Methods...................................................................................... 20 2.2.1 Non-invasive laserneedles ............................................. 20 2.2.2 Multidirectional transorbital and transtemporal Doppler sonography ...................................................... 22 2.2.3 Participants .................................................................... 23 2.2.4 Acupuncture and procedure........................................... 23 2.2.5 Statistical analysis ......................................................... 25 2.3 Results ....................................................................................... 25 2.4 Discussion .................................................................................. 27 2.5 Conclusion.................................................................................. 28 2.6 Acknowledgements .................................................................... 29 2.7 References .................................................................................. 29
3.
Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture ................................. 32 3.1 Introduction ................................................................................ 32 3.2 Methods...................................................................................... 32 3.2.1 Near-infrared spectroscopy............................................ 32 3.2.2 Laserneedle stimulation................................................. 33 3.2.3 Healthy volunteers, acupuncture, measurement procedure................................................. 34 3.2.4 Statistical analysis ......................................................... 36 3.3 Results ....................................................................................... 36 3.4 Discussion .................................................................................. 38 3.5 Acknowledgements .................................................................... 41 3.6 References .................................................................................. 41
4.
Communication between acupoint and brain proved by ultrasound ...................................................................................... 43 4.1 Introduction ................................................................................ 43 4.2 Methods and materials................................................................ 43
VIII 4.2.1
4.3 4.4 4.5 4.6
TCD monitoring of the anterior and posterior cerebral arteries with a new probe holder...................... 43 4.2.2 Participants .................................................................... 44 4.2.3 Laserneedle acupuncture ............................................... 45 4.2.4 Statistical analysis ......................................................... 48 Results ....................................................................................... 48 Discussion .................................................................................. 53 Acknowledgements .................................................................... 55 References .................................................................................. 55
5.
Histological investigations regarding micromorphological effects of laserneedle illumination. Results of an animal experiment........................................................................................... 57 5.1 Introduction ................................................................................ 57 5.2 Methods...................................................................................... 57 5.2.1 Procedure....................................................................... 57 5.2.2 Laserneedle stimulation................................................. 59 5.2.3 Laser Doppler flowmetry and temperature measurement.................................................................. 59 5.3 Results ....................................................................................... 60 5.4 Discussion .................................................................................. 61 5.5 Acknowledgements .................................................................... 62 5.6 References .................................................................................. 62
6.
Effects of laserneedle stimulation on microcirculation and skin temperature................................................................................. 64 6.1 Introduction ................................................................................ 64 6.2 Method and volunteers ............................................................... 64 6.2.1 Laser Doppler flowmetry .............................................. 64 6.2.2 Volunteers and procedure.............................................. 65 6.2.3 Statistical analysis ......................................................... 67 6.3 Results ....................................................................................... 67 6.4 Discussion .................................................................................. 70 6.5 References .................................................................................. 72
7.
Effects of acupressure, manual acupuncture and laserneedle acupuncture on EEG bispectral index (BIS) and spectral edge frequency (SEF) in healthy volunteers ...................... 73 7.1 Introduction ................................................................................ 73 7.2 Material and methods ................................................................. 73 7.2.1 Subjects ......................................................................... 73 7.2.2 Procedure and study design ........................................... 74 7.2.3 Evaluation parameters ................................................... 76 7.2.4 Statistical analysis ......................................................... 77
IX 7.3 7.4 7.5 7.6
Results ....................................................................................... 77 Discussion .................................................................................. 81 Acknowledgements .................................................................... 85 References .................................................................................. 85
8.
Acupuncture using laserneedles modulates brain function: first evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI) ................................................................................... 87 8.1 Introduction ................................................................................ 87 8.2 Methods...................................................................................... 88 8.2.1 Painless laserneedles ..................................................... 88 8.2.2 Functional multidirectional transcranial Doppler sonography (fTCD) ....................................................... 88 8.2.3 Functional magnetic resonance imaging (fMRI)........... 89 8.2.4 Participants .................................................................... 89 8.2.5 Experimental design and procedure .............................. 89 8.2.6 Evaluated parameters..................................................... 91 8.2.7 Statistical analysis ......................................................... 92 8.3 Results ....................................................................................... 92 8.4 Discussion .................................................................................. 96 8.5 Conclusions ................................................................................ 98 8.6 Acknowledgements .................................................................... 98 8.7 References .................................................................................. 98
9.
Quantification of gender specific thermal sensory and pain thresholds before and after laserneedle stimulation ............. 101 9.1 Introduction .............................................................................. 101 9.2 Method ..................................................................................... 101 9.2.1 Volunteers.................................................................... 101 9.2.2 Measurement of thermal sensitivity and thermal pain thresholds............................................................. 102 9.2.3 Laserneedle acupuncture and procedure...................... 103 9.2.4 Statistical analysis ....................................................... 105 9.3 Results ..................................................................................... 105 9.4 Discussion ................................................................................ 109 9.5 Acknowledgements .................................................................. 110 9.6 References ................................................................................ 110
10. Biological effects of painless laserneedle acupuncture a short summary of important scientific results ............................ 112 10.1 Introduction .............................................................................. 112 10.2 Methods.................................................................................... 112 10.2.1 Temperature and microcirculatory monitoring ........... 112
X
10.3 10.4 10.5 10.6 10.7
10.2.2 Functional multidirectional transcranial Dopplersonography (fTCD) ..................................................... 113 10.2.3 Functional magnetic resonance imaging (fMRI)......... 113 10.2.4 Near infrared spectroscopy (NIRS) ............................. 113 10.2.5 Laserneedle stimulation............................................... 113 10.2.6 Healthy volunteers, animal experiment and procedures.................................................................... 114 10.2.7 Statistical analysis ....................................................... 114 10.2.8 Evaluation parameters ................................................. 115 Results ..................................................................................... 115 Discussion ................................................................................ 121 Conclusion................................................................................ 122 Acknowledgements .................................................................. 122 References ................................................................................ 122
11. Increases in intracranial pressure and changes in blood flow velocity due to acupressure, needle and laserneedle acupuncture?................................................................. 124 11.1 Introduction .............................................................................. 124 11.2 Material and methods ............................................................... 124 11.2.1 Volunteers, patient, acupressure and procedure .......... 124 11.2.2 Measurement techniques, evaluation parameters and statistical analysis ................................................. 126 11.3 Results ..................................................................................... 127 11.4 Discussion ................................................................................ 131 11.5 Acknowledgements .................................................................. 133 11.6 References ................................................................................ 133 12. Laserneedle acupuncture - clinical studies..................................... 135 12.1 Introduction .............................................................................. 135 12.2 Material, patients and methods................................................. 136 12.3 Results ..................................................................................... 139 12.3.1 Lumbar, thoracic and cervical spine syndromes as well as post cervical and lumbar intervertebral disk prolapse................................................................ 139 12.3.2 Gonarthrosis, coxarthrosis, rhizarthrosis, periarthritis in the shoulder, epicondylitis, tendinitis, Morbus Bechterew and fibromyalgia-syndrome ......... 140 12.3.3 Remaining paresis after stroke .................................... 141 12.3.4 Cephalgia, migraine and trigeminal neuralgia............. 142 12.3.5 Arterial obstruction disease ......................................... 143 12.3.6 Gastropathy and bronchial asthma .............................. 143 12.3.7 Depression, anxiety, panic attacks, psychovegetative exhaustion ....................................... 143
XI 12.4 Discussion ................................................................................ 144 12.5 References ................................................................................ 145 13. Pain therapy with laserneedle acupuncture ................................... 147 13.1 Introduction .............................................................................. 147 13.2 Case reports .............................................................................. 147 13.3 Argumentation.......................................................................... 148 13.4 Discussion ................................................................................ 150 13.5 References ................................................................................ 151 14. Pain therapy of osteoarthrosis / osteoarthritis-patients using the laserneedle system in a medical practice with emphasis on rheumatology and pain therapy ................................ 152 14.1 Introduction .............................................................................. 152 14.2 Patients and method.................................................................. 152 14.3 Results ..................................................................................... 154 14.4 Discussion ................................................................................ 154 14.5 References ................................................................................ 155 15. Laserneedles in gynecology.............................................................. 156 15.1 Introduction .............................................................................. 156 15.2 Material, test persons, technique .............................................. 157 15.3 Case studies .............................................................................. 158 15.3.1 Induction of labor with laserneedles............................ 158 15.3.2 Carpal tunnel syndrome............................................... 160 15.3.3 Urogenital symptoms, back pain, hot flushes.............. 161 15.3.4 Breast cancer with mastectomy, transmission in scars 162 15.3.5 Dysmenorrhoea, lack of energy................................... 164 15.3.6 Childlessness, temperature curve, cycle regulation..... 165 15.4 Results and discussion.............................................................. 166 15.5 References ................................................................................ 168 16. Laserneedles in gynecology - a study with questionnaires ............ 169 16.1 Introduction .............................................................................. 169 16.2 Test persons.............................................................................. 169 16.3 Method ..................................................................................... 170 16.4 Results ..................................................................................... 171 16.5 Discussion ................................................................................ 177 16.6 References ................................................................................ 178 17. Laserneedle therapy in dentistry..................................................... 179 17.1 Introduction .............................................................................. 179 17.2 Methods and materials.............................................................. 179 17.3 Results ..................................................................................... 179
XII 17.3.1 Oral surgery ................................................................. 179 17.3.2 Endodontology ............................................................ 180 17.3.3 Crown - bridges ........................................................... 181 17.3.4 Pain therapy ................................................................. 181 17.3.5 Myoarthropathy ........................................................... 181 17.3.6 Neuralgia ..................................................................... 182 17.3.7 Sedation in case of dental phobias............................... 182 17.3.8 Nausea during molding................................................ 182 17.4 Discussion ................................................................................ 183 17.5 References ................................................................................ 183 18. Laserneedle stimulation as a potential additive method for post operative pain treatment.................................................... 185 18.1 Introduction .............................................................................. 185 18.2 Method ..................................................................................... 185 18.2.1 Patients and procedure................................................. 185 18.2.2 Laserneedle acupuncture ............................................. 186 18.2.3 Statistical analysis ....................................................... 187 18.3 Results ..................................................................................... 187 18.4 Discussion ................................................................................ 188 18.5 Acknowledgements .................................................................. 189 18.6 References ................................................................................ 189 19. Effects of laserneedle stimulation in the external auditory meatus on very early auditory evoked potentials .......................... 190 19.1 Introduction .............................................................................. 190 19.2 Methods.................................................................................... 190 19.2.1 Laserneedle stimulation in the external auditory meatus ........................................................... 190 19.2.2 Auditory evoked potentials of early latency................ 191 19.2.3 Volunteers and procedure............................................ 192 19.2.4 Statistical analysis ....................................................... 193 19.3 Results ..................................................................................... 193 19.4 Discussion ................................................................................ 195 19.5 Acknowledgements .................................................................. 198 19.6 References ................................................................................ 199 20. List of references............................................................................... 200 21. Websites............................................................................................. 202 Addendum................................................................................................. 203
XIII
Editors (and authors): Gerhard Litscher, Prof MSc PhD MDsc Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Detlef Schikora, PhD Faculty of Science University of Paderborn Warburger Strasse 100 33098 Paderborn / Germany
Authors: Konrad B. Borer, MD Therwilerstrasse 11 4153 Reinach BL / Switzerland Franz Ebner, Prof MD MR Research Unit and Clinical Department of Neuroradiology Medical University of Graz Auenbruggerplatz 9 8036 Graz / Austria Franz Fazekas, Prof MD Department of Neurology, Medical University of Graz Auenbruggerplatz 22 8036 Graz / Austria Rudolf Helling, MD 1st Chairman of the ‘Ärzte-Forum für Akupunktur e.V.’ Ostenallee 107 59071 Hamm / Germany Evamaria Huber Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria
XIV Knut Kolitsch, MD General practitioner and expert for special pain therapy Oelzer Straße 12 98746 Katzhütte/Thüringen / Germany Wolfgang Nemetz, MD Department of Anesthesiology for Neurosurgical and Craniofacial Surgery and Intensive Care, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Dagmar Rachbauer, MSc MDsc Department of Neurology, Medical University of Graz Auenbruggerplatz 22 8036 Graz / Austria Stefan Ropele, Prof PhD Department of Neurology and MR Research Unit Medical University of Graz Auenbruggerplatz 22 8036 Graz / Austria Matthias Saraya, MD Department of Anesthesiology for Neurosurgical and Craniofacial Surgery and Intensive Care, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Andreas Schöpfer, MD Department of Anesthesiology for Neurosurgical and Craniofacial Surgery and Intensive Care, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Gerhard Schwarz, Prof MD Department of Anesthesiology for Neurosurgical and Craniofacial Surgery and Intensive Care, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria
XV Josef Smolle, Prof MD University Clinic for Dermatology, Medical University of Graz Auenbruggerplatz 8 8036 Graz / Austria Kirsten Stähler van Amerongen, MD Gynecological Clinic Inselspital Berne University of Berne Effingerstrasse 102 3010 Bern / Switzerland Selman Uranüs, Prof MD Department of Surgical Research, University Surgical Clinic, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Lu Wang, MD Dipl. Acup. Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Michael Weber, MD Dipl. Chem. General practitioner, emergency medical aid, naturopathic treatment, acupuncture Lönsstraße 10 37697 Lauenförde / Germany Nai-Hua Yang, Prof MD University Clinic for Ophthalmology, Medical University of Graz Auenbruggerplatz 4 8036 Graz / Austria
Acknowledgements The editors thank Mrs. Ingrid Gaischek MSc (Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz) for skillful preparation of the text and illustrations and Mrs. Sonya Mendlik-Bauer for translating a major part of the manuscripts.
1
1.
Laserneedles in acupuncture D. Schikora
1.1
Introduction and motivation
In the past 30 years, acupuncture established itself in Europe and America. Patients perceive acupuncture as an effective, non-medicinal form of treatment which conforms to the increasing desire of living a natural and balanced life. Particularly in case of chronic pain, patients attested the predominantly satisfactory results of acupuncture, especially since side effects of long term drug treatment can be ruled out with this method. In 1998, a great advancement was made leading to the acceptance of acupuncture in Western medicine. After a Consensus Conference, the United States National Institute of Health concluded that acupuncture was proven effective in cases of post operative nausea and vomiting, nausea and vomiting accompanying chemotherapy, as well as post operative tooth pain [1]. Acupuncture was also rated for the following indications: addictive illnesses, menstrual pain, headaches, tennis elbow, fibromyalgia, back pain, carpal tunnel syndrome, bronchial asthma as well as for alternative or complementary treatment after stroke. At this conference, it was emphasized that side effects of competently performed acupuncture are rare and compared with conventional therapies seem to be much more favourable [2]. Even today, the acceptance of acupuncture in some fields of western medicine is problematic particularly because no objectified proof regarding the effects of acupuncture is available. Critics fail to see, that many excellent scientific studies exist, particularly regarding acupoint-analgesia, which provide a detailed picture of physiological pain reduction achieved by acupuncture treatments. Currently, over 200 scientific publications dealing with the elementary mechanisms of acupoint-analgesia exist. Especially the leading studies by Pomeranz and Chiu [3], as well as those by Mayer et al. [4] which deal with the analgesic effect of acupuncture resulting from an increased release of ß-endorphin, establish the complex picture of neurobiological basics of acupoint-analgesia [5]. A systematic overview and critical rating of the current level of knowledge regarding neurobiological mechanisms in acupoint-analgesia were recently documented by Irnich and Beyer [6]. In the meantime, the acupuncture-endorphin-hypothesis could be proven in a number of different independent animal experiments. The ability to block the analgesic effect of acupuncture by injecting an opiate antagonist in the
2 acupoint is a strong indication that the afferent nervous system plays a role in transmitting the effects of acupuncture. All of these scientific results conform to the knowledge of modern pain research regarding the role of endorphins and are described to such an extent, desirable for other wellestablished western medical methods. The fact that these scientific results are mainly obtained from animal studies, underlines their objectivity. On the clinical level, the situation is fundamentally different. Numerous single-case and controlled studies have been documented, however definite evidence for the effects could not be proven up to this day. Of course we must note that classic needle acupuncture cannot be investigated using randomised, doubleblind study designs. Neither the patient, nor therapist can be blinded, since the patient always feels the insertion or stimulation of the applied needle and the therapist always must control the position, puncture depth and angle of insertion. There is no doubt that acupuncture has to be proved in the future by objectivized, double-blind clinical trials. However, this is only possible, when an adequate placebo method for classic needle acupuncture is available. Such a method does not exist up to this date; the placebo needle used by Streitberger et al. [7] does not fulfil the requirements of a double-blind study design. The development of a real placebo method for classic needle acupuncture is definitely of initial importance for further acupuncture research and establishing acupuncture as a medical treatment method. The goal of recent extensive field studies (GERAC-Study, Model study by German private insurance companies) was to prove or refute the efficacy of acupuncture treatment in selected indications using clinically controlled methods on a statistically significant level. Objectified, clinical evidence of effects could not be obtained in these studies for the named reasons. The initial idea of laserneedles resulted from analysis of laser acupuncture, developed and spread throughout Europe in the 1990´s. It was obvious, that the century-old technique of classic acupuncture or simultaneous stimulation of therapy specific acupoint combinations began to leave its natural course. Acupoints are stimulated one after the other, even though no evidence in classic or modern literature is given, that identical effects occur. Suddenly, the puncturing of acupoints according to the basic schemes of Chinese acupuncture was no longer important in Western “Laserpuncture”. With the development of laserneedles, we tried to maintain the fascinating aspects of acupuncture: the complex diagnostic system on the one hand, the simple therapeutic procedure and the effects on the other. The simultaneous procedure, simple handling adapted to needle acupuncture, needle equivalent stimulation effects and stimulating characteristics, were the most important goals of laserneedle acupuncture. Thus, laserneedles should be applied noninvasively by direct contact between the light emitting source and the skin. It was always clear, that quantitative documented proof of the postulated equivalence between laserneedle and classical metal needles is necessary.
3 An important, but not yet investigated question concerns the connection between stimulation strength and the effects of acupuncture. We know that an inserted acupuncture needle must be moved and repositioned by the therapist to increase stimulation intensity resulting in the De-Qi sensation. This effect is not easy to quantify since the intensity of stimulation triggered by needle puncture is also not quantifiable. How the stimulation intensity at the acupoint influences the effect of acupuncture still remains an unanswered question in this context. If we assume that acupuncture is not more than a specific kind of nerve stimulation, the question arises, whether this form of acupoint stimulation correlates with the dose-effects known from the field of bio-physiology, and underlies the Weber-Fechner-Law. With laserneedles, the light dose applied at any desired acupoint combination can be measured exactly. Compared to other classic metal needles, the stimulus strength can be quantified so that determination of dosis-effect relationships is possible. A basic assumption regarding stimulation characteristics i.e. the timing factor of stimulus intensity has to be made for experimental investigation of dose-effect relationships in acupuncture. In our first approach we assumed that the nocizeptive stimulus triggered by the classic metal needle is a continuous constant stimulation which lasts as long as the needle is inserted. In order to be equivalent to this stimulation mode, the laserneedles should act in the so-called continuous wave modus. Equivalence between both needle types can only be assumed under these circumstances. Frequency-modulated laser light is generally not equivalent to the application procedure of the classic needle acupuncture. The physical characteristics of laserneedles determine their physiological influence in tissue. We have been performing theoretical studies for some time dealing with the elementary interaction between photons and complex, biological molecules. Using molecular-dynamical methods of theoretical physics, we are able to calculate and predict the interaction of electrons or photons with complex molecules, as well as the effects of molecular excitation and basic relaxation on molecular surroundings. However, this is only possible when quasi elastic scattering processes between the photons and biological molecules are the predominant interactive processes. If we assume that elementary stimulation in acupuncture is generated on a molecular level, molecular-dynamic calculation shows [8], that electrical and optical stimulation show physiologically identical results and also generate and maintain a rhythmic cascade of action potentials at the nozizeptive structures as those produced when chemical transmitters such as substance P and bradykinine are released after needle puncture. These results can define the most important physical marginal requirements for the emission characteristics of the laserneedles: the emission wave lengths should be selected in a such a way, that quasi elastic scattering processes are dominant and emission intensity at the distal output of the laserneedle should be so
4 high, that responses relevant for acupuncture can be triggered by optical stimulation.
1.2
Dose-effect relationships in acupuncture
One of the fundamental biophysiological laws, the Weber-Fechner´s Law, describes the relationship between strength of perception E of a sensory stimulus and intensity of the stimulus S. As a result, the stimulus effect and stimulus response correlate and can be described with the following logarithm: E ~ ln S This proportionality does not imply more than that the doubling of stimulus strength not automatically leads to doubling of perception or effects of the stimulus. If we illustrate this simple relationship graphically, two important characteristics become visible and are shown in Figure 1.1. 5
Reizwirkung [a.u.] stimulus effects [a.u.]
4
3
2
1
0
0
2
4
6
8
10
stimulus strength Reizstärke [a.u.][a.u.] Fig. 1.1: Relationship between stimulus strength and stimulus effects according to Weber-Fechner ´s Law.
The curve illustrates threshold characteristics of physiological stimulation. Sensory stimuli do not lead to any effects when stimulus intensity lies under
5 a critical threshold value. Weak external influences are filtered out by the organism. Moreover, the curve shows the saturation characteristics of physiological stimuli. Thus, a doubling of stimulus strength does not lead to the doubling of effects within the organism. Finally, this is an expression for the adaptability of the organism to external stimulation, whose intensities can vary over many orders of magnitude. Validity of Weber-Fechner´s Law has been proven for acoustic, thermal, chemical and mechanical stimuli. In our experiments, we investigated if this physiological law is also applicable to acupuncture, e.g. if stimulus strength at the acupoint and the resulting induced specific effects are correlated. For this purpose, laserneedles with different optical power density were used. Power densities which are effective on the skin were varied from 1.5 – 5 W/cm². In order to compare the effect of laserneedles under identical circumstances, parallel experiments using classic metal needles were also performed. The blood flow velocity in the ophthalmic artery (OA) and its changes during stimulation of an eye specific acupuncture scheme were studied in this experiments. . Preliminary studies showed that the simultaneous stimulation of acupoints Zanzhu and Yuyao, the acupoints eye and liver on the ear, as well acupoints E2 from Korean hand acupuncture and Yan Dian from Chinese Hand acupuncture led to significant and specific increases in blood flow velocity (OA) when using metal needles or laserneedles [9] (compare chapter 2). The specific effect on the visual system could be proven by the parallel measurement of blood flow velocity in the middle cerebral artery, which remained constant i.e. did not show any changes in measurement results when using this acupuncture scheme. Measurement of blood flow velocity was performed with transorbital and transtemporal Doppler sonography. Blood pressure was registered before, during and after measurement. Treatment time was 10 minutes and blood flow velocity data was monitored continuously. A randomised, cross-over study design was used and each volunteer underwent acupuncture with laserneedles, as well as with metal needles. The study protocol was approved by the ethics commission of the Medical University of Graz, reasons for exclusion of volunteers (n = 27) were treatment with medication, visual disorders, as well as neurological and psychological deficits. Figure 1.2 shows the detected dependency of blood flow velocity in the OA as a function of power density from the laserneedles.
6
change in blood flow velocity [cm/s]
metal needle
2
laserneedle - power density [W/cm ]
Fig.1.2: Change in blood flow velocity in the OA in dependence on the power density of the laserneedles during stimulation of an eye-specific acupuncture scheme. The mean changes measured in metal needle acupuncture are marked with a line.
Figure 1.2 clearly shows that acupuncture of the seven eye-specific acupoints leads to a significant increase in blood flow velocity in the OA. Metal needles yield an increase from 10 cm/s to 18 cm/s. It is obvious that changes in blood flow velocity are dependent upon the optical power densities applied when using laserneedle acupuncture. The curve conveys the best analytical adaptation of measurement values. This curve satisfies the mathematical function f (x) = c x ln (x + 0.5). This indicates that blood flow velocity in the OA is an effective parameter for acupuncture treatment and is logarithmically dependent on the stimulus intensity of the laserneedles. Thus, we can conclude, that Weber-Fechner´s Law is valid for the dose-effect relationship examined here. The threshold value I* for optical power density can be calculated from the registered and analytically determined effect curve; I* = 1.3 W/cm². This indicates that the optical power density of the laserneedles must be greater than 1.3 W/cm² in order to activate the physiological effects of acupuncture. In addition, we can see that the needle equivalence in optical power densities of the laserneedles reach I t 5 W/cm². We can assume that an increase in blood flow velocity in the OA is based on a complex cerebral reaction resulting from acupoint
7 stimulation, preceded by multi-synaptic switching of optically induced acupuncture stimulation potentials. It is noteworthy, that despite the physiological complexity, the logarithmic relationship between stimulus strength I and stimulus effect is maintained. We interpret this as obvious proof, that specific effects of acupuncture underlie these logarithmic dose-effect relationships. The existence and validity of dose-effect relationships in acupuncture could be proven for the first time using the methods described here. This statement is strictly valid only when using laserneedles which trigger continuous permanent stimulation, thus allowing exact quantification of stimulus strength. To what extent low or high frequency modulation of laserneedle light can modify proven dose-effect relationships is unclear and must be investigated in further studies. Since the postulated equivalence between metal needles and laserneedles could be clearly shown in the examined context, we can conclude that classical acupuncture and its effects also should be functionally dependent on stimulus strength according to a potency rule.
1.3
Laserneedle acupuncture as a placebo method
The requirements of an adequate placebo needle and an adequate placebo method for classical needle acupuncture are clearly to define: The requirements of a placebo needle are: 1. The placebo needle should not generate any acupuncture effect 2. The placebo needle should be of identical shape and size compared to the verum needle and therefore should not be distinguishable from a verum acupuncture needle 3. The application procedure of the verum needle and the placebo needle should be identical 4. The application procedure of the verum needle and the placebo needle should not depend on the individual experiences of the treating physician 5. The perception of the placebo needle and the verum needle at the acupoint by the patient should be identical The requirements of an acupucnture placebo method are: 1. The fundamental rules of the classic acupuncture have to be preserved, in particular the simultaneous needling of any acupoint combination should be possible with the placebo method
8 2. The direct contact between the treating physician and the patient has to be minimized by the placebo method, to exclude any healing effect by the aura of the physician If the placebo needle and the placebo method meets all this requirements, a double blind clinical study can be performed. We know that needle puncture at desired skin points also leads to effects that are similar to those resulting from stimulation of acupoints. For that reason, this type of acupuncture is called sham-acupuncture. A further demand on the placebo method would be to establish a clear definition between the categories of verum-acupuncture, placebo-acupuncture and shamacupuncture. Based on these criteria the applicability of laserneedle acupuncture as a placebo method for classic needle acupuncture can be analyzed precisely. We already mentioned that laserneedles are not inserted into the skin, but applied to the skin at the acupoint. This non-invasive method of application is an important characteristic of laserneedle acupuncture. Our studies with more than 250,000 practical applications of laserneedles show that laserneedle stimulation with distal optical power densities of about 5 W/cm² are not perceived as a stimulus sensation by the majority of patients and volunteers. Of course the threshold of laser light stimulation is different and variable from person to person, however, laserneedle stimulation with a primary emission wavelength of 685 nm at acupoints on the body is not perceivable for most patients. The cerebral effects generated by laserneedle acupuncture were investigated systematically using multi-directional functional Doppler sonography, near-infrared spectroscopy (NIRS) and functional magnetic resonance imaging [10]. In other chapters of this book we show that laserneedles with power t 5 W/cm² lead to specific changes in cerebral blood flow velocity during stimulation of visual acupoints nearly identical to those in needle acupuncture. In addition to these experimental studies, the effects of acupuncture regarding changes in cerebral oxyhaemoglobin concentrations were investigated. Here, a visual acupuncture scheme was used and in this case, non-specific cerebral parameters could be analysed. This was done using a randomized, cross-over design with direct comparison between metal needle and laserneedle stimulation. Details from these experiments are described in [11]. Measurement of cerebral concentrations of oxyhaemoglobin and desoxyhaemoglobin were done using NIRS: Figure 1.3 shows the results of these measurements dependent on the optical power of the laserneedles.
9
metal needle
laserneedle - power [mW]
Fig. 1.3: Changes in cerebral oxyhaemoglobin concentration when using a visual acupuncture scheme with metal needles and laserneedles of different optical power. The curve shows the best analytical adaptation to the measurement values of laserneedle stimulation.
The experimental data in Figure 1.3 show that laserneedle stimulation with an optical power of about 40 mW leads to changes in oxyhaemoglobin concentration, similar to the effects when using metal needles. The equivalency between metal needle stimulation and laserneedle stimulation can also be proven with these cerebral effects. These experiments also yield the best analytical adaptation of the measurement results in a logarithmic function, i.e. cerebral oxyhaemoglobin concentration parameters also underlie a physiological dose-effect relationship. The definition of verum-acupuncture, placebo-acupuncture and shamacupuncture presents a fundamentally unsolved and principally unsolvable problem for classic acupuncture with metal needles. We examined the possibilities to differentiate and define these three modalities experimentally for laserneedle acupuncture. Hereby, acupoint combinations were stimulated with laserneedles, which according to traditional Chinese medicine are coherent with the visual or olfactory system. Figure 1.4 shows the scheme of visual distant points used.
10
Fig. 1.4: Distant acupuncture points Hegu, Zusanli, Kunlun and Zhiyin of the visual system (left) and the selected sham-points (right).
Stimulation of the olfactory system was done with acupoints Yinxiang, Pianli and Hegu. Changes in blood flow velocity in the posterior cerebral artery (PCA) and anterior cerebral artery (ACA) were used for determining the effects of acupuncture stimulation and registered with functional Doppler sonography. In addition, changes in activity in the frontal area and olfactory cortex were detected using functional MR-imaging. Detailed information regarding these measurements [10] are described in chapter 8. A randomised, controlled cross-over study design was used and can be divided in the following test situations: The verum situation, characterized by activated laserneedles at the selected acupoint, the placebo-situation characterized by non-activated laserneedles at the acupoints and the sham-situation, characterized by activated laserneedles at the selected sham-points. The verum-situation showed a specific, significant increase in blood flow velocity in the PCA and ACA in our volunteers (n = 41), resulting in specific, significant activity in the occipital and olfactory cortex visible in MR-imaging. No significant changes in functional Doppler sonography and in functional MR-imaging were registered in the placebo-situation or shamsituation. From these experimental studies, we conclude that a clear differentiation between verum-acupuncture and placebo- or sham-acupuncture is possible in regard to laserneedle acupuncture. In this context, the basic difference between acupuncture with laserneedles and with metal needles becomes obvious and fulfils and important criterion for an adequate placeboacupuncture method. Since the reproducible De-Qi sensations can be
11 triggered with laserneedle acupuncture and the proven cerebral effects do not pose special demands regarding the positioning of the laserneedles, we conclude that acupuncture with laserneedles fulfils all requirements of a complete placebo experiment. We want to emphasize that the proven physiological equivalence between metal needles and laserneedles applies to all of the reports and scientific results achieved with laserneedles and in turn is also valid for classic needle acupuncture. Therefore, the use of laserneedle acupuncture, performed in randomised, double-blind studies, can be of great advantage for clinically objectifying the effects of acupuncture.
1.4
Physical characteristics of laserneedles
The laserneedles were developed at the University of Paderborn to provide a therapeutically and methodically equivalent, non-invasive instrument to the classic metal needle.
Fig. 1.5: Laserneedle for acupuncture.
Figure 1.5 shows a laserneedle. You can see that laserneedles are acupuncture needles with optical fibres that can be applied to the skin in such a way that the distal light emitting region of optical fibre is in contact with the surface of the skin. A major goal of these scientific studies was to develop photonic acupuncture needles for simultaneous stimulation of selected acupoint combinations on the body and ear which can be used in the exact same way as metal needles, The optical power densities at the distal laserneedle exit were set in such a way, that metal needle equivalent stimulation effects are guaranteed.
12
Physical foundation of stimulation effects in the numerous experimental studies is the emission of laser light with a wavelength of 685 nm (red light) as well as the complementary emission of infrared laser light with wavelengths of 880 – 950 nm. Hence, laserneedles emit “bi-chromatic“ light with a power density of 5 - 10 W/cm² at the exit of the laserneedle. Complementary, bi-chromatic emission is based on light conversion, i.e. red laser light also activates the infra-red photons in the light wave conductor. Laser light leaving the laserneedle is coherent and is routinely examined with Michelson-Interferrometry regarding its characteristics of coherence. Chronological and spatial coherence of emitted photons is immediately lost when entering the skin and diffuse scattering becomes a determining factor. The physiologically determinant power density range of 5 - 10 W/cm² is achieved by a specially developed method of optical tailoring of the fibre core. In Table 1.1 we can see that this method is very effective, when we want to reach a maximum of power density with a minimum of laser strength. Laser power
Laser-spot diameter
Optical power density
at the skin 50 mW
5 mm
0.25 W/cm²
50 mW
0.5 mm
25.5 W/cm²
50 mW
0.05 mm
2550 W/cm²
Tab. 1.1: Connection between laser power, laser-spot diameter and optical power densities.
Exemplary calculations show that a power density of 0.25 W/cm2 results when laser power of 50 mW and spot-diameter of 5 mm at the skin, commonly used in one-hand, laser-pens is applied. In order to reach the required physiological range of power density for the laserneedles, a 20 W laser must be used! As illustrated in Table 1.1, reduction of the spotdiameter by the factor 10 leads to an increase in optical power densities by a factor of 100. The emission characteristics of laserneedles described here, in particular regarding the optical power densities affecting the skin from 5 - 10 W/cm², as well as the bichromatic emissions of red and infrared laser light are based on patented technologies only realised in laser-acupuncture needles and are available under the trade name LASERneedle® [12].
13 Contact application guarantees that the applied light dose can be exactly determined and reproduced. The next figure (Fig. 1.6) graphically illustrates how much light energy is transferred from a laserneedle during acupuncture treatment into the skin.
applied light energy dose per laserneedle [J]
60 50 40 30 20 10 0
0
5
10
15
20
25
duration of treatment [min]
Fig. 1.6: Light dose of a laserneedle dependent on the duration of treatment.
In order to determine the entire optical power transferred into tissue during stimulation of acupoints, the value in the graph needs only to be multiplied with the number of laserneedles applied. Transmitted light energy of about 320 J, equivalent to about 80 cal or that contained in less than a half teaspoon of yogurt, resulted after a treatment time of 20 minutes, using 8 laserneedles. In this chapter, we have already noted, that the emission wave length of laserneedle light should be selected in such a way, that quasi elastic scattering processes in tissues are dominant and the adsorption of photons can be neglected. Figure 1.7 shows the absorption behaviour of the most important tissue structures, dependent on the emission wave length of laser light.
14
Fig. 1.7: Absorption behaviour of important tissue structures dependent on the emission wave length of laser light.
Figure 1.7 shows that all important tissue structures from the skin yield a minimum in absorption coefficients ranging from 550 -1100 nm within the electromagnetic spectrum. This is particularly true for water, oxyhaemoglobin and melanin. In this “window”, the absorption of photons and production of heat can be neglected since the scattering of photons on tissue molecules is the dominant interactive process. Therefore, this range is very suitable for optical stimulation at the surface of the skin. The depth which photons can reach with diffuse, elastic scattering processes is once again dependent on the wave length. Simple estimates show that even at a depth of 2 - 3 cm, photon densities exist, which can trigger molecular activity at nocizeptive structures. Light wave conductors available today are made of plastic (PMMA), quartz or sapphire and have comparably little absorption in the „window“ area, so that conduction losses in the optical fiber are practically neglectable. Laserneedles use semi-conductor laser diodes as a light source. Figure 1.8 shows a semi-conductor laser diode schematically.
15
Fig. 1.8: Schematic illustration of a semi-conductor laser diode.
We can see that lasers consisting of mono-crystalline (Ga, Al, In) As are about 1 x 0.5 x 0.1 mm in size, and are about as big as a salt grain. The optically active area of a semi-conductor laser diode is once again smaller by a factor of 1000 and is comprised of layers that are only a few nanometres thick. The fact that the light field emitted by a laser diode doesn’t have a circular, but rather an elliptical diameter, is of decisive importance for optical fibre laserneedles. Since the standard light wave conductors available today have a circular diameter they lead to optical losses when an elliptical light field is fenced in a round fibre core. These loses are relatively low and according to technical standings, losses in a fiber are less than 10 %. The optical power densities alone and not the primary laser strength are responsible for the physiological stimulation effects of laserneedles at the acupoint. The results from our studies show that metal needle equivalent acupuncture can only be performed within a range of 5 - 10 W/cm². Today, we attribute power densities of 10 W/cm² to the field of photodynamic therapies. The question, whether power densities in this range lead to histologic damage is of great importance and was investigated experimentally by our study group [13] (see chapter 5). In an animal study, we could prove that no micromorphologic changes occurred during 20 minute application of laserneedles with about 5 W/cm². Neither microthrombosis or extravasation could be proven, nor changes in endothelial cells of dermal blood vessels could be observed. Thermic interaction at the acupoint was determined with infrared thermography. As a result, a heating effect of laserneedle light can be neglected. We measure an increase in temperature of about 1 °C at the
16 immediate contact area during a 20 minute treatment period. If we discuss the conditions during head- and ear acupuncture with laserneedles, we must consider that light intensity in the skin decreases exponentially and is weakened to about 50 % of the initial value when it reaches the skull. Since the stratum corneum, epidermis and dermis have different refractive indexes for optical light, wave transmitting effects occur in the layers of the skin which distribute the laser light laterally over an area of about one to 2 cm². As a result, a proportional reduction in optical power densities up to two magnitudes of order and the power density of laserneedle light is reduced to physiologically unimportant values after transmission through the skin. Transmitted part of the radiation of the laserneedles is completely absorbed by the skull. Using animal experiments, we could also show that no laserneedle-radiation (continuous wave modus) at the surface of the cortex can be observed [14]. Today, the new laserneedles for acupuncture provide instruments which are extensively characterized in medical-scientific studies. About 750,000 acupuncture treatments with laserneedles are performed worldwide in the last two years. In particular, patients appreciate this painless but still effective method of acupuncture. The medical potential of this new acupuncture method is huge. At the moment, ten University Clinics in Germany, Austria, Switzerland and France are perfoming scientific studies. The goal of these studies is to study and understand the basics of acupuncture and to get a step closer to the clinical objectification of the effects of acupuncture.
1.5
Acknowledgements
The author would like to thank all of his colleagues who took part in the development of laserneedles.
1.6 [1] [2] [3] [4]
References NIH Consensus Conference (1998) Acupuncture. JAMA 280: 15181524 Yamashita H, Tsukayama H, Hori N, Kimura T, Tanno Y (2000) Incidence of adverse reactions associated with acupuncture. J Altern Complement Med 6: 345-350 Pomeranz B, Chiu D (1976) Naloxone blockade of acupuncture analgesia: endorphin implicated. Life Sci 19: 1757-1762 Mayer DJ, Price DD, Rafil A (1977) Antagonism of acupuncture analgesia in many by the narcotic antagonist naloxone. Brain Res 2: 368-372
17 [5] [6] [7] [8] [9] [10]
[11] [12] [13]
Pomeranz B (1998) Wissenschaftliche Grundlagen der Akupunktur. Springer, Berlin-Heidelberg-New York-London-Paris-Tokio-Hongkong Irnich D, Beyer A (2002) Neurobiologische Grundlagen der Akupunkturanalgesie. Schmerz 16: 93-102 Streitberger K, Kleinhenz J (1998) Introducing a placebo needle into acupuncture research. Lancet 352: 364-365 Frauenheim T, Schikora D (2003) J Med Phys, subm. Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D (2004) Die schmerzfreie Lasernadelakupunktur moduliert die Gehirnaktivität: Erste Nachweise mit funktioneller transkranieller Dopplersonographie (fTCD) und funktionellem Magnetresonanzimaging (fMRI). Schmerz & Akupunktur 1: 4-11 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Schikora D. Europäisches Patent EP01/08504 Litscher G, Nemetz W, Smolle J, Schwarz G, Schikora D, Uranüs S (2004) Histologische Untersuchungen zu mikromorphologischen Einflüssen von Lasernadelstrahlung Ergebnisse einer tierexperimentellen Untersuchung. Biomed Tech 49: 2-5
18
2.
Cerebral vascular effects of non invasive laserneedles measured by transorbital and transtemporal Doppler sonography G. Litscher, D. Schikora
2.1
Introduction
The term "acupuncture" is used to refer to the insertion of needles into the body, at special chosen sites, for the treatment or prevention of symptoms and conditions. “Laserpuncture” is known as a method to stimulate sequentially acupoints by low level laser radiation. In contrast to that "laserneedles" allow to stimulate appropriate acupoint combinations simultaneously and with higher radiation doses and therefore represent a new non invasive optical stimulation which is described in this book. The laserneedles used in this study emit red light in cw-mode with an output power of 30 - 40 mW per laserneedle, which results in a radiant exposure energy of about 2.3 kJ/cm² at each acupuncture point during a treatment time of about 10 min. Due to the well defined contact application and the possibility to stimulate simultaneously up to eight acupoints, the laserneedles allow to attribute the resulting cerebral vascular effects unambiguous and exactly to the total laser radiation dose exposed at the acupuncture point combination selected. This opens the new scientific possibility to describe the input stimulus strength of complex acupuncture treatments with well established physical parameters. The aim of this study was to provide a possible first selective evidence of specific effects of laserneedle acupuncture and needle acupuncture on brain and eye using a combination of vision related acupoints of traditional Chinese medicine, Korean hand acupuncture and ear acupuncture. Quantification of differences in cerebral effects [1] between laserneedle acupuncture and needle acupuncture was performed using a randomized cross-over study design.
19
C omputerC ontrolled A cupuncture®
C omputerC ontrolled L aserpuncture
Fig. 2.1: Computer-Controlled Acupuncture® (CCA®) [1] and Computer-Controlled Laserpuncture (CCL) with multidirectional ultrasound probe holder devices in the biomedical engineering lab of the Medical University of Graz. Details concerning the method can be found on the website http://litscher.info.
20
C omputerC ontrolled L aserpuncture
MED-UNI GR AZ
Laserneedles
Fig. 2.2: The laserneedle system is a class 3B laser system, therefore it is compulsory to wear specific laser protection glasses.
2.2 2.2.1
Methods Non invasive laserneedles
The non invasive laserneedles were constructed to fulfil two essential requirements of acupuncture [2]: (i) They allow the simultaneous stimulation of up to eight acupuncture points in any different combinations on the body, the head, the hands and the ears. (ii) The emitted laser intensity is so adjusted that a stimulus can be induced without destroying the surrounding tissue. The laser radiation of eight 55 mW - laserdiodes was coupled into eight optical fibres and the laserneedles are arranged at the distal ends of the optical fibres. Due to coupling losses the output power of each laserneedle was reduced to 30 - 40 mW. The fibre core diameter used in the study was of about 500 µm. For our experiments seven vision related acupuncture points were chosen and irradiated simultaneously. The average time of irradiation was of about 10 min resulting in an energy density of about 2.3 kJ/cm² at
21 each acupoint and a total sum of 16.1 kJ/cm² for seven acupoints. To maintain the fundamental advantage of non invasiveness, the laserneedles were fixed onto the skin but not pricked into the skin. Fig. 2.3 depicts the measured intensity profile across the optical fibre output. The insert shows a photograph of the distal laserneedle end. Due to the direct contact of the laserneedles and the skin, no loss of intensity occurs and the laser power, which affects the acupuncture points, can by exactly determined by integration of the intensity curve shown in Fig. 2.3. Actually, the output intensity of each laserneedle was determined in such a way, resulting in an average irradiance intensity at one acupoint of about 3.8 W/cm². 1
intensity [a.u.]
emission wavelength: 685 nm
laser-needle emissioncharacteristics
total output power at distal end: 30 mW
optical cladding fibre core
-2
-1
1
2
optical fibre diameter [ a.u.]
Fig. 2.3: Emission characteristics of a tailored laserneedle used in the present study (a.u. = arbitrary units). The coherence of the laser radiation at the distal output of the optical fibre was examined by Michelson-Interferometry. The inset shows a photograph of the distal end of a laserneedle.
Due to the fact that the contact area exposed to laser rays is constant and the beam divergence can be neglected, the effective laser radiation dose at the acupoints was determined directly from the output intensity of the laserneedles and the treatment duration.
22
laser energy density [ J/cm²]
3500 3000 2500 2000 1500 1000 500 0
0
200
400
600
800 1000 1200 1400
time [s] Fig 2.4: Energy density at the laser-needle contact area in dependence on the treatment time. Due to the contact type application, as well the exposed area as the laser intensity are constant and the laser radiation dose at the acupuncture point can be determined with high accuracy from treatment time.
2.2.2
Multidirectional transorbital and transtemporal Doppler sonography
Transorbital and transtemporal Doppler sonographic examinations were performed with a Multi-Dop T unit (DWL Electronic Systems GmbH, Sipplingen, Germany). A 4 MHz and a 2 MHz probe were used in a multidirectional ultrasound probe holder construction. The monitoring arrangement for simultaneous recording of Doppler sonographic signals in the ophthalmic artery (OA) and the middle cerebral artery (MCA) was stationary at the circumference of the head. Blood flow profiles in the OA were measured transorbitally with the smallest power value able to detect signals (max. 20 mW/cm²). Under acoustic control, the angle and position of the probes were adjusted until the greatest possible signal amplitude was reached. Alterations in the blood flow velocities of both arteries were registered continuously and simultaneously. In addition blood pressure was measured non invasively before, during and after stimulation (Cardiocap® CC-104, Datex Medical Electronics, Hoevelaken, The Netherlands).
23 2.2.3
Participants
The study protocol was approved by the institutional ethics committee of the Medical University of Graz (11-017 ex 00/01) and all 27 participants gave written informed consent. Fourteen female and 13 male aged 21 - 38 years (mean age 25.15 + 4.12 (Cx + SD) years) were examined. None of the subjects was under the influence of centrally active medication and had visual deficits. All persons were free of neurological or psychological disorders. They were paid for their participation.
2.2.4
Acupuncture and procedure
Seven vision related acupoints were tested in two sessions (laserneedle acupuncture and needle acupuncture) in the same persons. The acupuncture scheme consisted of two traditional Chinese acupoints: UB.2 Zanzhu (location: in the depression of the medial end of the eyebrow. Needling method: puncture transversely 0.5 - 0.8 cun) and Ex.3 Yuyao (location: at the midpoint of the eyebrow. Needling method: puncture transversely 0.3 0.5 cun). In addition two ear acupoints (eye and liver: locations see Fig. 2.5. Needling method: puncture perpendicular 0.3 cun) and two vision-related acupoints from Korean hand acupuncture (E2: location see Fig. 2.5. Needling method: puncture transversely 0.1 – 0.2 cun) and one from Chinese hand acupuncture (Yan Dian: location: on the ulnar side of the thumb distal to the first metacarpal bone. Needling method: puncture perpendicular 0.2 cun) were used [3-5]. Three different acupuncture systems were used together because the combination shows an enhanced effect of the parameters measured in the study [5].
24
Yuyao Zanzhu
Liver
Eye
E2
Yan Dian
Fig. 2.5: Vision related acupuncture points used in this study. Traditional Chinese Medicine: Zanzhu and Yuyao. Ear acupuncture: eye and liver. Korean hand acupuncture: E2. Chinese hand acupuncture: Yan Dian.
The acupoints were punctured with sterile, single-use needles after local disinfection of the skin. We used three different types of needles (body: 0.25 x 25 mm, Huan Qiu, Suzhou, China; ear: 0.2 x 13 mm, European Marco Polo Comp., Albi, France; hand: 0.1 x 8 mm, Sooji-Chim, Korea). Needle stimulation was achieved by rotating with lifting and thrusting of the needles.
25 In case of laserneedle acupuncture the acupoints were cleaned with alcohol, the laserneedles were put in contact to the skin and stable fixed by plaster stripes. The acupoint scheme was the same as described above. During the experiments the subjects were in a relaxed and comfortable position on a bed in our laboratory. Then the monitoring equipment was positioned. After a 10-minute resting period the laserneedles or acupuncture needles were applied. The choice for the initial stimulation was randomized. The mean blood flow velocity (vm) in the OA and the MCA were evaluated simultaneously and continuously [1]. Each person was studied with laserneedle acupuncture and needle acupuncture. The choice of the measuring procedure was randomized and the interval between the experiments was 20 to 30 minutes.
2.2.5
Statistical Analysis
The data were tested with Kruskal-Wallis ANOVA on ranks using the computer program SigmaStat (Jandel Scientific Corp., Erkrath, Germany). The results of the conditions before (a), during (b) and after (c) acupuncture were given as means (Cx) + standard deviation (SD) or standard error (SE). The criterion for significance was defined as p < 0.05.
2.3
Results
The demographic data, the laser- and acupuncture schemes and the measurements of mean blood flow velocity in the OA and MCA are summarized in Fig. 2.6.
26 Participants n=27 14 female, 13 male, mean age 25.15 + 4.12 (SD), range 21 – 38 years Randomized, cross-over design R
Non invasive Laserneedles
Manual Needle Acupuncture
Ophthalmic artery (OA) vm (cm/s) 20
Ophthalmic artery (OA)
15
SE
p=0.01*
10
b
20
b
a
15
p<0.001*
10
c
Middle cerebral artery (MCA)
c a
Middle cerebral artery (MCA)
b
b
60
60
50
a
c
before (a) during (b) after (c) Mean blood Laserpuncture flow velocity Cx+ SE Ophthalmic 10.33+0.88 14.67+1.15 11.33+0.96 artery (cm/s) Middle cerebral 54.93+3.28 54.56+3.26 55.07+3.50 artery (cm/s)
40
a
c
before (a) during (b) after (c) Mean blood Acupuncture flow velocity Cx+SE Ophthalmic 10.22+0.83 19.15+1.20 12.22+0.94 artery (cm/s) Middle cerebral 53.93+3.33 56.04+3.44 55.04+3.47 artery (cm/s)
*Kruskal-Wallis ANOVA on Ranks
Fig. 2.6: Subjects, acupoints, and graphical (means + standard error (SE)) as well as numeric data of the mean blood flow velocity of the ophthalmic artery (OA) and the middle cerebral artery (MCA) before (a), during (b), and after (c) stimulating with laserneedles or needling vision related acupoints in 27 healthy volunteers in a crossover design.
The results showed significant increases of vm in the OA during (b) laserneedle acupuncture (p = 0.01) and needle acupuncture (p < 0.001). At
27 the same time only minor, insignificant changes in vm were seen in the MCA. The mean arterial blood pressure (before laserneedle acupuncture: 79.2 + 6.6 (SD) mmHg; before needle acupuncture: 77.5 + 6.6 mmHg) was not significantly changed during laserneedle acupuncture (78.4 + 6.4 mmHg) or needle acupuncture (79.1 + 6.5 mmHg). The maximum amplitude of vm in the OA was detected with a delay of 10 30 sec after the initial stimulus by the needles and with a delay of 20 - 60 sec after the initial stimulus by the laserneedles.
2.4
Discussion
Important factors have led to the expanding use of laser technology in medicine. These factors are the increasing understanding of the wave-length selective interaction and associated effects of ultraviolet-infrared radiation with biologic tissues, including those of acute damage and long-term healing, the rapidly increasing availability of lasers emitting at those wavelengths that are strongly absorbed by molecular species within tissues, and the availability of both optical fiber and lens technologies [6]. Fusion of these factors has led to the development of the new laserneedle system which is described for the first time in scientific literature by our research group. Acupuncture using laserneedles has the advantage that the stimulation can hardly be felt by the patient. The operator may also be unaware of whether the laserneedle system is active, and therefore true double-blind studies can be performed, which was almost impossible up to now in acupuncture research. The new system has the added advantage that it can be used at all standard acupuncture points [32]. The effectiveness of unconventional complementary medical methods, such as laserpuncture, have previously been documented mainly as single cases. There are only few theoretical and clinical studies concerning laserpuncture in scientific literature [7-16]. Recent scientific and technological progress has truly revolutionized acupuncture. The usage of advanced exploratory tools, such as laser Doppler flowmetry [17], laser Doppler imaging [18], ultrasound [1,5,19,20] or magnetic resonance imaging [1,21], provides revealing insights and attempt to shine scientific light upon the most spectacular of the eastern medical procedures. Similar like in animal studies [22,23] we have found recently that the brain is the key to acupuncture’s and laserpuncture’s effects. New experimental
28 constructions to measure ultrasound, light and bioelectrical processes can reproducibly demonstrate effects of stimulation of acupoints in the brain [1,5,19,20,24-28]. Studies with biosensors and probes in a specially designed helmet showed that acupuncture can increase significantly and specifically the blood flow velocity in different cerebral arteries and increase the oxygen supply to the brain [1,5,19,20,24,25,27,28]. Laserpuncture and manual needle acupuncture can also lead to an increase in oxygenated hemoglobin in the tissue oxygen index [20,29]. However, laserpuncture and needling at placebo points did not produce the same effects on cerebral oxygenation. Laserpuncture has been established for many years and was reviewed by Pöntinen et al. [30]. Nonetheless, the changes of cerebral function elicited with commercially available low level lasers were in average one magnitude of order less pronounced than those elicited with conventional needle acupuncture [1,19,20,29]. Streitberger et al. [31] have reported that the stimulus strength at the acupuncture points are of decisive importance for the therapeutic efficiency of acupuncture treatments. Using placebo-needles in comparison with metal needles, it was found that the efficiency of acupuncture treatments decreases significantly, if placebo needles were used. Our present study shows that the new high optical stimulation with laserneedles can elicit reproducible cerebral effects which are in the same order (half dimension) with respect to the maximum amplitude of the mean blood flow velocity (vm) as compared to needle acupuncture. As it is shown in Fig. 2.3 the maximum blood flow velocity rate ratio 'vm (needle) / 'vm (laserneedle) for the acupuncture scheme selected is of about 2. Regarding the stimulus dynamics we found that the delay time between the initial stimulus and the occurrence of the maximum amplitude of vm is in the order of 10 - 60 sec for both methods. This allows to conclude that obviously the basic mechanism of signal activation and transmission are comparable for both acupuncture methods. Interestingly, the maximum flow rate for laserneedles was obtained after exposing a total (sum of seven acupoints) laser ray dose of about 1.6 kJ/cm².
2.5
Conclusion
In conclusion, the results of the laserneedle applications for acupuncture demonstrate specific, significant alterations in blood flow velocity of the ophthalmic artery after stimulating vision-related acupoints on the body, ear
29 and hand. At the same time blood flow velocity in the middle cerebral artery did not change significantly. For needle acupuncture qualitatively the same behavior was observed. The cerebral effects of the laserneedles were comparable to the alterations of the needle acupuncture, they differ absolutely by a factor of ~ 2. This is a significant improvement compared to the common low-level-handylaser (LLLT) acupuncture (cerebral effects factor ~ 10 lower as for needle acupuncture). Further studies using different laser stimulus intensities and wavelengths are in progress, to optimize the adjustment of the new noninvasive laserneedles and to clarify the elementary excitations at the acupoints.
2.6
Acknowledgements
The present report is the product of many co-workers. We are especially indebted to Ms. Lu Wang MD, Evamaria Huber, Ms. Petra Petz MSc and Ms. Ingrid Gaischek MSc (all Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz / Austria) for their support to this study. We would also express our thanks to Dr. Leopold Dorfer, President of the Austrian Society for Controlled Acupuncture and to Dr. Michael Weber, Member of the EGFAA for their help. We thank Petra Thöne, Tanja Prohaska, Marianne Hubbert and Jörg Reitemeyer for technical support.
2.7 [1] [2] [3] [4] [5]
[6] [7]
References Litscher G, Cho ZH (Eds) (2000) Computer-Controlled Acupuncture®. Pabst Science Publishers, Lengerich-Berlin-Rom-Riga-Wien-Zagreb Schikora D. European Patent Nr. PCT/EP 01/08504 König G, Wancura I (1989) Neue Chinesische Akupunktur. Lehrbuch und Atlas der Akupunkturpunkte. Wilhelm Maudrich, Wien-MünchenBern Yoo TW (2001) Koryo hand therapy - Korean hand acupuncture. Eum Yang Mek Jin Publishing Co, Seoul Litscher G (2002) Computer-based quantification of traditional Chinese-, ear- and Korean hand acupuncture: Needle-induced changes of regional cerebral blood flow velocity. Neurol Res 24: 377380 Judy MM (1995) Biomedical lasers. In: Bronzino JD. (Ed) The Biomedical Engineering Handbook. CRC Press, IEEE Press, Boca Raton (USA), pp. 1333-1345 Fargas-Babjak A (2001) Acupuncture, transcutaneous electrical nerve stimulation, an laser therapy in chronic pain. Clin J Pain 17 (4. Suppl): 105-113
30 [8] [9]
[10] [11] [12] [13]
[14] [15] [16] [17]
[18]
[19] [20] [21] [22] [23]
Radmayr C, Schlager A, Studen M, Bartsch G (2001) Prospective randomized trial using laser acupuncture versus desmopressin in the treatment of nocturnal enuresis. Euro Urol 40(2): 201-205 Naeser MA (1997) Neurological rehabilitation: acupuncture and laser acupuncture to treat paralysis in stroke, other paralytic conditions, and pain in carpal tunnel syndrome. J Altern Complement Med 3(4): 425 428 Read A, Beaty P, Corner J, Sommerville Ville C (1996) Reducing naltrexone-resistant hyperphagia using laser acupuncture to increase endogenous opiates. Brain Inj 10(12): 911-919 Troshin OV (1994) A clinico-neurophysiological analysis of the single action of laser puncture. Lik Sprava 5-6: 148-153 Qin JN (1987) Laser acupuncture anaesthesia and therapy in People's Republic of China. Ann Acad Med Singapore 16(2): 261-263 Nikolaev NA (1986) Therapeutic efficacy of laser and electropuncture reflexotherapy in correcting the initial manifestations of cerebral circulatory insufficiency. Zh Nevropathol Psikhiatr Im S S Korsakova 86(1): 60-64 Omura Y (1983) Non-invasive circulatory evaluation and electroacupuncture & TES treatment of diseases difficult to treat in Western medicine. Acupunct Electrother Res 8(3-4): 177-256 Schlager A, Oehler K, Huebner KU, Schmuth M, Spoetl L (2000) Healing of burns after treatment with 670-nanometer low-power laser light. Plast Reconstr Surg 105(5): 1635-1639 Schlager A, Offer T, Baldissera I (1998) Laser stimulation of acupuncture point P6 reduces postoperative vomiting in children undergoing strabismus surgery. Br J Anaesth 81(4): 529-532 Sandner-Kiesling A, Litscher G, Voit-Augustin H, James RL, Schwarz G (2001) Laser Doppler flowmetry in combined needle acupuncture and moxibustion: a pilot study in healthy adults. Lasers Med Sci 16(3): 184-191 Litscher G, Wang L, Huber E, Nilsson G (2002) Changed skin blood perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers Med Sci 17: 1925 Litscher G, Wang L, Wiesner-Zechmeister M (2000) Specific effects of laserpuncture on the cerebral circulation. Lasers Med Sci 15: 57-62 Litscher G (2001) High-Tech Akupunktur®. Pabst Science Publishers, Lengerich-Berlin-Rom-Riga-Wien-Zagreb Cho ZH, Wong EK, Fallon J (Eds) (2001) Neuro-Acupuncture I. Neuroscience Basics. Q-Puncture Inc, Los Angeles Ji G, Zhao L, Shi R, Liu Y, Wang S, Wu F (1996) Effects of electrical acupuncture on the cerebral blood flow and the pial microcirculatory blood flow in dogs. Zhen Ci Yan Jiu 21(2): 43-46 Uchida S, Kagitani F, Suzuki A, Aikawa Y (2000) Effect of acupuncture-like stimulation on cortical cerebral blood flow in anesthetized rats. Jpn J Physiol 50(5): 495-507
31 [24] [25] [26]
[27] [28] [29] [30] [31] [32]
Litscher G, Wang L, Yang NH, Schwarz G (1999) Computer-controlled acupuncture. Quantification and separation of specific effects. Neurol Res 21(6): 530-534 Litscher G, Wang L, Yang NH, Schwarz G (1999) Ultrasoundmonitored effects of acupuncture on brain and eye. Neurol Res 21(4): 373-377 Litscher G, Yang NH, Schwarz G, Wang L (1999) Computer-controlled acupuncture. A new construction for simultaneous measurement of blood flow velocity of the supratrochlear and middle cerebral arteries. Biomed Techn 44(3): 58-63. Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I (1998) Robotic transcranial Doppler sonography probes and acupuncture. Int J Neurosci 95(1-2): 1-15 Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I, Eger E (1998) Effects of acupuncture on the oxygenation of cerebral tissue. Neurol Res 20 Suppl 1: 28-32 Litscher G, Wang L (2000) Cerebral near infrared spectroscopy and acupuncture - results of a pilot study. Biomed Technik 45(7-8): 215218 Pöntinen PJ, Pothmann R (1998) Laser in der Akupunktur. Hippokrates, Stuttgart Streitberger K, Kleinhenz J (1998) Introducing a placebo needle into acupuncture research. Lancet 352: 364-365 Litscher G, Schikora D (2002) Effects of new noninvasive laserneedles on brain function. IFMBE Proceedings, 2nd European Medical and Biological Conference (EMBEC) 4. - 8.12.2002 Vienna, pp. 996-997
32
3.
Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture G. Litscher, D. Schikora
3.1
Introduction
The connection between puncturing the body with a needle and the reaction at another area of the body is still unclear. However, it has been proven that when particular acupuncture points are stimulated with needles or laser light, specific effects in the brain can be objectivized and quantified with modern cerebral monitoring methods [1-3]. In this present study, we objectivized the systematic changes of oxygenation in the brain [4] using cerebral near-infrared spectroscopy (NIRS), after stimulating acupuncture points according to traditional Chinese medicine (TCM), Korean and Chinese hand acupuncture, ear acupuncture and combinations of these different methods. We analyzed a total of 328 recordings after manual needle and laserneedle stimulation from 88 healthy volunteers [5,6].
3.2
Methods
3.2.1
Near-infrared spectroscopy
The NIRS method allows the evaluation of changes in cerebral oxygenation through the intact skull and is also gaining importance in acupuncture research because of its non-invasive approach [6-10]. The NIRO 300 Monitor (Hamamatsu Photonics, Japan) is a new instrument in this field of research. Parameters such as changes in oxyhemoglobin ('O2Hb) and desoxyhemoglobin ('HHb) are determined by Lambert-Beer´s principle [4]. The system can measure the absolute value (µmol) of changes in parameters, but not the level (absolute concentration) at which these changes occur (in positive or negative direction). The measurement value is zero, as long as no change in concentration occurs. Placement of the sensor (emitter and near-infrared detectors) on the head with a silicone holder is easy and reproducible. Data output of 'O2Hb and 'HHb were presented on a color LCD-display and color printer.
33
In addition to the spectroscopic method, non-invasive, standard monitoring parameters such as blood pressure (Cardiocap® CC-104, Datex Medical Electronics, Hoevelaken, Netherlands) were determined before, during and after different manners of stimulation.
3.2.2
Laserneedle stimulation
The laserneedle-technique represents a new, non-invasive method for optic stimulation of acupuncture points and was first described in literature in 2002 [5,6,11,12]. Laserneedle® (Schikora D.: European Patent Nr. PCT/EP 01/08504) acupuncture allows the simultaneous stimulation of individual acupuncture point combinations. Variations and combinations of acupuncture at different areas of the body, ear or hand, as performed particularly in this study are possible (compare Fig. 3.1). Details regarding this method can also be found in preceding studies [5,6,11,12].
Fig. 3.1: Test person during laserneedle stimulation and simultaneous registration of NIRS parameters. Right bottom: single active laserneedle and application device.
Changes in near-infrared spectroscopic parameters in the frontal region of the brain were continuously registered and analyzed.
34 3.2.3
Healthy volunteers, acupuncture, measurement procedure
In this study, a total of 328 measurements on 88 healthy volunteers (50 female, 38 male) mean age 25.7 + 4.0 (Cx + SD) years (19 - 38 years) were performed. The study protocol was approved by the ethics committee of the Medical University of Graz (11-017) and all test persons gave their written consent. None of the volunteers had visual, neurological or psychological deficits or were under the influence of central nervous system effective drugs. A maximum of 7 acupuncture points in different measurement series (needle acupuncture and laserneedle acupuncture) were investigated. The acupuncture scheme included two acupuncture points from TCM: Zanzhu (localization: at the medial end of the eyebrow, perpendicular to and above the inner corner of the eye, at the foramina of the supraorbital nerve; needling: perpendicular 0.5 - 0.8 cun) and Yuyao (localization: at the middle of the eyebrow, perpendicular and above the pupil; needling: inclined 0.3 0.5 cun). In addition, 2 ear acupuncture points (eye and liver: localization see Fig. 3.2; needling: inclined 0.3 cun) and 2 eye acupuncture points from Korean hand acupuncture (E2: localization see Fig. 3.2; needling: perpendicular 0.1 – 0.2 cun) and one acupuncture point from Chinese hand acupuncture (Yan Dian: localization: on the ulnar side of the middle phalanx of the thumb; needling: inclined 0.2 cun) were included in the study [11-13]. In addition, possible responses in NIRS parameters after needling and stimulating of a placebo point (localization: lateral from the radius 6 cun above the horizontal fold of the wrist exactly on the radial ledge, lateral from the pulmonary meridian) were tested. The different acupuncture schemes were applied alone and in combination, since preliminary studies indicated that the selection of different combinations also result in different effects in the cerebral parameters to be measured (e.g. bloodflow velocity in the ophthalmic artery) [11-13] (Fig. 3.2).
35
liver
Yuyao Zanzhu eye E2
Yan Dian
Fig. 3.2: Acupuncture schemes used in this study.
Acupuncture points were needled with single-use needles after local disinfection of the skin. We used three different types of needles (body: 0.25 x 25 mm, Huan Qiu, Suzhou, China; ear: 0.2 x 13 mm, European Marco Polo Comp., Albi, France; hand: 0.1 x 8 mm, Sooji-Chim, Korea). Stimulation was performed with simultaneous rotating, pulling and thrusting movements of medium intensity. In the case of laserneedle acupuncture, the skin at the acupuncture point was cleaned with alcohol, the laserneedle was positioned at the surface of the skin and then fixated with special adhesive tape. We used the same acupuncture schemes as in the combined measurements using needle acupuncture. During the experimental phase, the test persons were positioned in a relaxed manner on a lounge. After applying the near-infrared spectroscopic sensors in the frontal area of the skull, a 10 minute resting period was observed. Then, either laserneedle stimulation was activated or the acupuncture needles were inserted and stimulated for 10 seconds. Thereafter, the laser was activated for 10 minutes or the needles were left alone. The maximum amplitude of 'O2Hb and 'HHb (phase during acupuncture) was analyzed during this period of time. Randomized selection of which technique should be started with, as well as selection of sequence of the particular type of
36 stimulation (body, ear, hand, combination) was done. The resting period between each investigation was at least 30 minutes.
3.2.4
Statistical analysis
Data was analyzed with the computer program SigmaStat (Jandel Scientific Corp., Erkrath, Germany). Results from the phases before (=zeropoint calibration), during and 5 minutes after needle acupuncture or of laserneedle acupuncture are shown in the diagrams as mean values, respectively.
3.3
Results
At the left side of Figure 3.3, the hypothetical functional curve of stimulus intensity dependent upon the treatment time is shown. This diagram gains in importance due to the actually measured, specific cerebral data in regard to changes in O2Hb and HHb shown at the right. During manual, metal needle stimulation a nearly exponential maximum increase in O2Hb and an exponential decrease to a higher level than initially, occurred, whereas the trend of O2Hb during laserneedle NIRS response remains plateau-like.
Stimulus intensity SI [a.u.]
Stimulus intensity - cerebral NIRS response O2Hb
metal needle
a
HHb O2Hb
laserneedle HHb
b time [s]
10 min
B.J., 22y, f
Fig. 3.3: Left: Stimulus intensity (SI f(t)) as a function of time (hypothesis). Right: Real measured cerebral responses of NIRS-parameters O2Hb (oxyhemoglobin) and HHb (desoxyhemoglobin) on manual, brief (20 seconds) acupuncture needle stimulation (a) and laserneedle stimulation (b) in 22-year-old female test person. The arrows indicate the beginning of stimulation.
37
Figures 3.4 and 3.5 show the mean values of maximum change in O2Hb (Fig. 3.4) and HHb (Fig. 3.5) parameters during and 5 minutes after manual needle acupuncture or laserneedle acupuncture.
Fig. 3.4: Changes in µmol of oxyhemoglobin (O2Hb) during needling of a placebo point, 3 hand acupuncture points, 2 ear acupuncture points, 2 acupuncture points from TCM, a combination of hand, ear and body acupuncture as well as laserneedle stimulation and an intensity-increased (+ 30 %) laserneedle acupuncture (from left to right) during and 5 minutes after acupuncture.
38
Fig. 3.5: Cerebral changes (generally decreases) in desoxyhemoglobin (HHb). For further descriptions see Fig. 3.4.
It is obvious that needling and stimulation of the placebo point does not lead to marked changes in cerebral NIRS parameters during and 5 minutes after acupuncture. Manual needling and laserneedle stimulation leads to a marked increase in O2Hb (compare Fig. 3.4) and simultaneous decrease in HHb (compare Fig. 3.5) when using the combined Korean hand acupuncture (E2) and Chinese hand acupuncture (Yan Dian), as well as TCM-body (Zhanzu and Yuyao) acupuncture, as well as combined body, ear, and hand acupuncture. This effect is still present 5 minutes after removing the needles or deactivating laserneedle stimulation. An almost negligible, but contrary behavior of O2Hb and HHb occurs when both ear points (eye and liver) are needled or stimulated with laser. None of the acupuncture stimulation methods or combinations resulted in significant changes in standard monitoring parameters (blood pressure).
3.4
Discussion
One of the main advantages of the laserneedle technique is its noninvasiveness. It is possible to apply the laser in such a manner, that the test
39 person cannot feel optical stimulation of the acupuncture point. In addition, the acupuncturer does not need to know if the system is activated or deactivated. Thus, double-blind studies using this new method are possible in acupuncture research for the first time. This method of study was already performed by our research group [14] and included simultaneous and continuous monitoring of blood flow velocity in the posterior cerebral artery and the middle cerebral artery in 17 healthy volunteers. This study showed that laserneedle stimulation of distant acupuncture points at hands and feet (Hegu, Zusanli, Kunlun, Zhiyin) is able to achieve marked and specific changes in cerebral blood flow velocity [12,14]. Even though laser puncture using Low-Level-Laser stimulation devices is an established method, measurable cerebral effects lie far below conventional needle acupuncture [15]. The results from the first studies [11,12,14] using the laserneedle system revealed significant changes in cerebral parameters (blood flow velocities), which were otherwise only achieved by manual needle acupuncture. The proportion of maximum change in blood flow velocity (needle/laserneedle) is approximately factor 2. Since Chinese medicine and acupuncture are considered an integrative part of TCM based on energetic processes, the registration of changes in the cerebral metabolism could express energetic processes in the brain and obviously plays a key role in investigating the effects of acupuncture. To date, it has not been possible to obtain non-invasive and continuous results regarding regional cerebral oxygenation. Near-infrared spectroscopy can register changes in oxygenation in the cerebral vascular region very sensitively. The advantages of transcranial oximetry are its noninvasiveness, low risks and continuity, as well as its easy and time-saving application. A wide range of indications are the result for the potential use of this spectroscopic method [4]. A number of factors which can influence adequate interpretation of data must be considered. Contamination with surrounding light, mechanical irritations, intracerebral hematoma, misplacement of optodes or other user errors are just some possibilities which should be noted [4]. A number of studies which deal with NIRS conclude that NIRS can exactly determine extremely small changes in cerebral hemodynamics, as a response to different functional stimulations. In this study [5,6], 328 systematic NIRS registrations on healthy volunteers during manual and laserneedle acupuncture stimulation were performed for the first time. The results from two preceding publications [8,9] were the reference points for this study.
40
The first study regarding acupuncture and NIRS [8] indicated that the changes in the occipital region after acupuncture stimulation in 3 healthy volunteers, was measurable and reproducible in each of the test persons. In the second study [9], NIRS-changes were measurable and reproducible at the central region after acupuncture stimulation at the Hegu point. This study showed, that reproducible changes in frontally monitored NIRS parameters could be determined, after stimulation of specific eye acupuncture points. In general, changes in NIRS parameters are unspecific and we do not know if an isolated decrease in saturation is caused by an increase in cerebral oxygenation consumption or results from a decrease in cerebral blood flow. Therefore, not only the extent of oxygenation is shown, but the interaction between oxygenation and desoxygenation is reflected. This is possible since the measurement zone is mainly dominated by the venous part of the cerebral vascular bed (~ 75 %). The arterial part (~ 20 %) or the capillary (~ 5 %) flow region is respectively smaller [4]. For these reasons, we were able to determine changes, which for example occur due to an increase in oxygenation. Which ruling mechanisms are present is still unclear. Increased desoxygenation by stimulus-induced neuronal activation, i.e. caused by changes in membrane potentials or release of neurotransmitters could be possibilities [16]. For whatever reason, acupuncture obviously influences the oxygen metabolism of the brain in healthy test persons. Similar to this study using ear acupuncture, a paradox contra-directional change in blood flow velocity (increase) and regional cerebral O2-saturation (decrease) occurred in a vascular based case of dementia, when an individually adapted acupuncture scheme was used [16]. The described case report showed that acupuncture could improve the clinical status of vascular dementia. Using NIRS and transcranial Doppler sonography, we were able to register the effects on cerebral blood flow velocity and the O2-metabolism. In combination with clinical findings, an inverse decrease in regional cerebral O2-saturation during simultaneous increase in cerebral blood flow velocity during acupuncture could be interpreted, as a sign of increased cerebral oxygenation. A decrease in regional cerebral O2-saturation does not necessarily indicate a poor condition of the O2-metabolism in the sense of reduced oxygen supply, however could also document the beneficial effects of regionally increased oxygenation, activated by acupuncture [16]. In a similar manner, the minor contradirectional regional changes in NIRS parameters using ear acupuncture could be interpreted, since the monitoring method conveys the balance between oxygenation and desoxygenation.
41 Further studies are necessary to investigate the importance of these phenomena on acupuncture, since not only the influence in general and in detail of laser acupuncture, but also the influence of combined ear and body acupuncture, are still discussed controversially. Spectroscopic methods probably are useful tools for this investigations.
3.5
Acknowledgements
The authors thank Ms. Lu Wang MD for performing the acupuncture, Ms. Evamaria Huber for help in data recording and Ms. Petra Petz MSc for her valuable support in data analysis (all Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz).
3.6
References
Litscher G (2001) High-Tech Akupunktur®. Pabst Science Publishers, Lengerich Berlin Düsseldorf [2] Litscher G, Cho ZH (Eds.) (2000) Computer-Controlled Acupuncture®. Pabst Science Publishers, Lengerich Berlin Düsseldorf Riga Scottsdale Wien Zagreb [3] Cho ZH, Wong EK, Fallon J (2001) Neuro-Acupuncture. Q-puncture, Los Angeles [4] Litscher G, Schwarz G (Eds.) (1997) Transcranial cerebral oximetry. Pabst Science Publishers, Lengerich Berlin Düsseldorf Riga Scottsdale Wien Zagreb [5] Litscher G, Schikora D (2002) Nahinfrarot-spektroskopische Untersuchungen zur Nadel- und Lasernadelakupunktur. AKU Akupunktur Theorie und Praxis 3: 140-146 [6] Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 [7] Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I, Eger E (1998) Effects of acupuncture on the oxygenation of cerebral tissue. Neurol Res 20/S1: 28-32 [8] Litscher G, Wang L (2000) Zerebrale Nahinfrarot-Spektroskopie und Akupunktur – Ergebnisse einer Pilotstudie. Biomed Technik 45: 215218 [9] Litscher G, Wang L, Huber E (2002) Veränderungen zerebraler nahinfrarot-spektroskopischer Parameter während manueller Akupunkturnadelstimulation. Biomed Technik 47: 76-79 [10] Litscher G, Wang L (2002) Computergestützte Objektivierung der Grenzen der Akupunktur. AKU Akupunktur Theorie und Praxis 30/1: 1319 [1]
42 [11] Litscher G, Schikora D (2002) Cerebral effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 [12] Litscher G, Schikora D (2002) Neue Konzepte in der experimentellen Akupunkturforschung - Computerkontrollierte Laserpunktur (CCL) mit der Laserneedle® Technik. Der Akupunkturarzt / Aurikulotherapeut 28(3): 18-28 [13] Litscher G (2002) Computer-based objectivation of traditional Chinese-, ear- and Korean hand acupuncture, Needle-induced changes of regional cerebral blood flow velocity. Neurol Res 24: 377-380 [14] Litscher G, Schikora D (2002) Effects of new noninvasive laserneedles on brain function. IFMBE Proceedings, 2nd European Medical & Biological Engineering Conference (EMBEC), Vienna, December 2002: 996-997 [15] Litscher G, Wang L, Wiesner-Zechmeister M (2000) Specific effects of laserpuncture on the cerebral circulation. Lasers Med Sci 15: 57-62 [16] Litscher G, Schwarz G, Wang L, Sandner-Kiesling A (2002) Akupunktur bei vaskulär bedingtem dementiellem Abbau. Jahrestagung der Österreichischen Alzheimer-Gesellschaft. 14. Klagenfurter Arbeitstagung für Neurologie. 24. - 25. Mai 2002, Klagenfurt / Austria
43
4.
Communication between acupoint and brain proved by ultrasound G. Litscher, L. Wang, N.H. Yang
4.1
Introduction
Transcranial Doppler ultrasonography (TCD) provides a noninvasive, rapid and continuous assessment of blood flow velocity in cerebral arteries. Using new probe holder constructions, it is possible to record blood flow patterns in various cerebral arteries simultaneously and continuously [1-4]. Acupuncture has been used as a therapeutic medical technique in China for thousands of years and is indicated for a wide variety of conditions [5,6]. However, evidence of quantitative measurable effects of acupuncture is still rare in the scientific literature. We have reported a number of quantifiable effects of acupuncture on cerebral perfusion and cerebral oxygenation [14,7-16]. In the present study we investigated the specific effects of laserneedle acupuncture of two acupuncture schemes on the mean blood flow velocity in the anterior (ACA) and posterior (PCA) cerebral arteries in a cross-over study design.
4.2 4.2.1
Methods and materials TCD monitoring of the anterior and posterior cerebral arteries with a new probe holder
Doppler sonographic signals were recorded simultaneously in the left ACA and the right PCA with a Multi-Dop T system (DWL Electronic Systems GmbH, Sipplingen, Germany). Two 2-MHz probes were used in a multidirectional ultrasound probe holder.
44
ACA - Acupuncture
Ying Xiang (LI.20)
Fig. 4.1: Monitoring of the blood flow profiles in the anterior cerebral artery (ACA) and the posterior cerebral artery (PCA) and localization of the acupuncture point Ying Xiang.
The A1 segment of the ACA was assessed in its entirety at depths between 58 and 88 mm. The direction of flow in the ACA was away from the ipsilaterally placed probe. The PCA was found by aligning the transducer slightly posteriorly and inferiorly from the bifurcation of the internal carotid artery. Between a depth of 60 to 78 mm, its P1 segment was found and showed a direction of flow toward the transducer. The mean blood flow velocity (vm) is an important parameter [1,8], because it describes the most intense mean values of Doppler frequency at every interval of the spectrum [17]. Forty vm values were averaged in each patient in five phases (a: 5 minutes before acupuncture; b - d: during laserneedle acupuncture and e: 2 minutes after stimulation). The averaged values of the five measured phases were compared for each subject.
4.2.2
Participants
Blood flow profiles in the ACA and PCA were measured before, during and after the acupuncture sessions in 22 adults (mean age 24.4 + 2.6 years; range 21 – 29 years). None of the subjects was under the influence of centrally active medication. They were fully informed about the nature of the
45 investigation and gave informed consent. During the experiments the subjects were in a relaxed and comfortable positon on a bed in our laboratory. Then the TCD monitoring equipment was positioned. After a 10minute resting period the laserneedle stimulation was activated for a duration of 20 minutes.
4.2.3
Laserneedle acupuncture
Two acupuncture schemes were tested in two sessions in the same persons. One scheme (including Yingxiang) was chosen to influence the olfactory system (Figs. 4.2 - 4.4) and one (including Zhiyin) to stimulate the optical system.
PCA ACA NIRS - sensor
Fig. 4.2: Healthy volunteer during laserneedle stimulation and TCD-registration. Additionally a sensor was placed frontally for the registration of near infraredspectroscopic signals (NIRS).
Yingxiang (LI.20) Location: Between ala nasi and nasolabial groove. Indication: Rhinitis, blocked nose, common cold, nose bleeding, facial paralysis, trigeminal neuralgia, toothache. Hegu (LI.4) Location: At the highest point of the m. adductor pollicis with the thumb and index finger adducted. Indication: The most important analgesic point; stimulation of this point relieves pain in all parts of the body. The specific effect on the
46 head, especially in headache has been verified by clinical research. Pianli (LI.6) Location: 3 cun proximal to Yangxi (LI.5) on the line connecting Yangxi with Quchi (LI.11). Indication: Dry throat, rhinitis, throat pain, redness of the eye, tinnitus, deafness, sore throat, edema. Guangming (GB.37) Location: On the anterior side of the fibula, 5 cun proximal to the malleolus lateralis. Indication: Eye disorders, headache, mental disorders. Taichong (Liv.3) Location: Between the first and second metatarsal bones, 2 cun proximal to the margin of the web. Indication: Distal point for eye disorders, pain and tension of the head and chest, urogenital, endocrine and metabolic disorders.
47
olfactory epithelium
Fig. 4.3: Schematic presentation of the olfactory epithelium (modified according to JW Karapelou, Spektrum der Wissenschaft Spezial, 4/1999).
48
Fig. 4.4: Functional magnetic resonance imaging: activation during chemical stimulation (modified according to DH Zald et al. 1997; http://james.psych.umn.edu/olfactory.html). Note the dominance on the left.
4.2.4
Statistical Analysis
The data were tested with analysis of variance (one-way repeated-measure ANOVA) with SigmaStat software (Jandel Scientific Corp., Erkrath, Germany). The results were expressed as means + standard error (Cx + SE). The criterion for significance was p < 0.05.
4.3
Results
Figure 4.5 shows an example of increased vm in the ACA during laserneedle acupuncture. Stimulation of acupoint Yingxiang was repeated and the changes in vm were reproducible.
49
Laserneedle - specific effects ACA - PCA vm (cm/s)
before
during
laserneedle-acupuncture time 1 min
Fig. 4.5: Trend of the mean blood flow velocity vm in cm/s in the left anterior cerebral artery (ACA) and the right posterior cerebral artery (PCA) before and during laserneedle acupuncture in a 24-year-old volunteer. The arrow marks the beginning of stimulation.
Figure 4.6 (middle and lower panel) summarizes the results in all 22 subjects for both acupoint schemes. The values of vm in the ACA increased significantly (p<0.001) using acupuncture scheme A (b - d) and were higher at the end of the investigation (e) than before acupuncture (a). Insignificant changes (n.s.) in vm were seen in the PCA. However, with the vision-related acupoint scheme B the same subjects showed a significant increase of vm in the PCA without significant changes in the ACA.
50 Healthy volunteers n=22 12 female, 10 male, 21 - 29 years ( 24.4 + 2.6 years; x + SD ) R
laserpuncture scheme A
laserpuncture scheme B
Anterior cerebral artery (ACA)
Anterior cerebral artery (ACA)
50
52 51
49
*)
48
50
47
49
46
48
45
n.s.
47
a
b
c
d
a
e
b
c
d
e
*) p < 0.001
Posterior cerebral artery (PCA)
Posterior cerebral artery (PCA) 47
45
46
44
45
43
*)
44
42
n.s.
41
43 42
40 a
b
c
d
e
a
b
c
d
e
*) p < 0.002
Fig. 4.6: Healthy volunteers, acupuncture points and graphic presentation (means) of the results of the mean blood flow velocity of the anterior cerebral artery (ACA) and the posterior cerebral artery (PCA) before (a), during (b - d) and after (e) laserneedle stimulation. The arrows mark the relative maximum changes during laserneedle stimulation referring to the basic value.
51
vm (cm/s) 50
Specific cerebral effects of laserneedle-acupuncture p = 0.001*
48 46 ACA PCA
44 42
n = 22
40 38
a
*
b
c
d
e
One Way Repeated Measures Analysis of Variance (Tukey Test)
Fig. 4.7: Absolute changes in vm during laserneedle acupuncture.
'vm (cm/s)
p = 0.001*
3
2,5 2 1,5 ACA
1
PCA
0,5
n = 22
0 -0,5 -1 a
*
b
c
d
e
One Way Repeated Measures Analysis of Variance (Tukey Test)
Fig. 4.8: Relative changes in vm during laserneedle acupuncture.
52
Specific cerebral effects of laserneedle-acupuncture vm (cm/s)
50
n.s.
48 46 44
ACA PCA
42
n = 22
40 38 a
b
c
d
e
Fig. 4.9: Absolute changes in vm during laserneedle acupuncture.
'vm (cm/s) 3
n.s.
2,5 2 1,5 1
ACA
0,5
PCA
0
n = 22
-0,5 -1 a
b
c
d
e
Fig. 4.10: Relative changes in vm during laserneedle acupuncture.
53
4.4
Discussion
Transcranial Doppler ultrasonography measures blood flow profiles in cerebral arteries. The technique is used to detect stenoses, emboli and malformations of intracranial arteries, assess cerebral collateral circulation before surgery, monitor cerebral vasospasm, and document cerebral circulatory arrest, as well as for intraoperative monitoring. Acupuncture is a form of traditional Chinese medicine (TCM) that has developed over thousands of years. Until now, modern Western medicine has used acupuncture mostly for complementary or supportive purposes. There are hundreds of acupoints on the human body. These are points at which according to TCM the flow of the vital force Qi can be stimulated [5,6]. In this study we used laserneedles, a new way to stimulate these points. In previous studies we have found that the brain is the key to understanding acupuncture’s effects [1-4,7-14]. New experimental constructions to measure ultrasound, light and bioelectrical processes can reproducibly demonstrate effects of acupuncture in the brain. We have shown that acupuncture with needles can increase overall cerebral blood flow. Studies with biosensors and probes in a specially designed helmet showed that acupuncture can increase the blood flow velocity in the middle cerebral artery and increase the oxygen supply to the brain. The present study is a further step to objectify the effects of acupuncture. In 22 participants we found that laserneedle acupuncture of specific acupoints increases blood flow in specific regions of the brain. An acupuncture scheme including two points in the face (Yingxiang) which TCM places in connection with the olfactory system increased mean blood flow velocity in the ACA significantly (p < 0.001). The ACA supplies most of the frontal and medial mass of the cerebrum including part of the olfactory cortex. At the same time, blood flow in the PCA stayed nearly unchanged. In contrast, an acupuncture scheme including a point on the foot (Zhiyin) which is in connection with the optic system increased blood flow in the PCA significantly (p = 0.002). Simultaneously blood flow in the ACA stayed nearly unchanged. Cho et al. [16] have described similar effects in the brain by stimulating vision-related acupoint Zhiyin with functional magnetic resonance imaging
54 and after light stimulation. Control studies with stimulation of other points on the foot did not produce specific activation in the visual cortex.
Acupuncture - fMRI
Vis. Ref.
Acup. Acup.
(light) light)
(Zhiyin)
Fig. 4.11: Functional magnetic resonance imaging (fMRI) at the Medical University of Graz (fMRI-results: Cho et al. [2]).
In our study we measured the blood flow profiles in the left ACA and the right PCA. This procedure was chosen for technical reasons and due to previous reports in the literature. Zald et al. [17] found that olfactory stimuli increased regional cerebral blood flow exactly in the left lateral orbitofrontal cortex. Cerebral blood flow in this study was measured with a slow bolus O15 water technique and positron emission tomography. We are convinced that sophisticated biomedical technology, particularly noninvasive ultrasound techniques, can objectify some effects of traditional Chinese medicine. In acupuncture the brain likely plays a key intermediate role. However, brain activity in and of itself does not explain anything about the healing power of acupuncture.
55
4.5
Acknowledgements
The authors thank Ms. Ingrid Gaischek MSc (Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz) for her valuable help.
4.6 [1] [2]
[3] [4] [5] [6] [7]
[8] [9]
[10] [11] [12]
References Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I (1998) Robotic transcranial Doppler sonography probes and acupuncture. Intern J Neurosci 95: 1-15 Litscher G, Yang NH, Schwarz G (1999) Computerkontrollierte Akupunktur®: Eine neue Konstruktion zur simultanen und kontinuierlichen Erfassung der Blutflußgeschwindigkeit in der A. supratrochlearis und A. cerebri media. Biomed Technik 44: 58-63 Litscher G, Wang L, Yang NH (1999) Ultrasound-monitored effects of acupuncture on brain and eye. Neurol Res 21: 373-377 Litscher G, Yang NH, Wang L (1998) Quantitative Separation spezifischer Akupunktureffekte von Gehirn und Auge mittels bidirektionaler Ultraschallmeßkonstruktion. AKU 26(4): 212-217 Engin I: Chinese acupuncture and moxibustion. Shanghai China, Publishing House of Shanghai College of Traditional Chinese Medicine, 1990 Mao-Liang Q (1996) Chinese acupuncture and moxibustion. Churchill Livingstone, London Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I (1997) Transkranielle Doppler-Sonographie - Robotergesteuerte Sonden zur Quantifizierung des Einflusses der Akupunktur. Biomed Technik 42: 116-122 Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I, Eger E (1998) Effects of acupuncuture on the oxygenation of cerebral tissue. Neurol Res 20(1): 28-32 Litscher G, Schwarz G, Sandner-Kiesling A (1997) Transcranial near infrared spectroscopy and transcranial Doppler sonography during acupuncture. In Litscher G, Schwarz G (Eds) (1997) Transcranial Cerebral Oximetry. Pabst Science Publishers, Lengerich, pp. 184-198 Litscher G, Wang L, Wiesner-Zechmeister M (2000) Specific effects of laserpuncture on the cerebral circulation. Lasers Med Sci 15: 57-62 Litscher G, Schwarz G, Sandner-Kiesling A (1998) Computerkontrollierte Akupunktur®. Akupunktur Theorie und Praxis 26(3): 133-142 Litscher G, Wang L, Yang NH, Schwarz G (1999) Computer-controlled acupuncture – Quantification and separation of specific effects. Neurol Res 21:530-534
56 [13] [14]
[15] [16]
[17] [18]
Litscher G, Yang NH, Wang L (1998) Ultrasound-controlled acupuncture. Internet J Anesthesiology 2/4: http://www.ispub.com/journals/IJA/Vol2N4/acu.htm Litscher G, Yang NH, Wang L (1999) Acupuntura controlada por ultrasonidos. http://www.tmed.uam.es/dpto/anesne...tas/ijae/vol2n4e/articulos/acu.h tm Litscher G, Wang L (1999) Visualisierung von peripheren Durchblutungsänderungen während der Akupunktur mittels Thermographie. Biomed Technik 44: 129, 1999 Cho ZH, Chung SC, Park JP, Park HJ, Lee HJ, Wong EK, Min BI (1998) New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci 95: 2670-2673 McCartney JP, Thomas-Lukes KM, Gomez CR (1997) Handbook of Transcranial Doppler. Springer, New York Zald DH, Pardo PJ, Pardo JV et al (1997) Left orbitofrontal activation during aversive chemical stimulation. http://james.psych.umn.edu/olfactory.html
57
5.
Histological investigations regarding micromorphological effects of laserneedle illumination. Results of an animal experiment G. Litscher, W. Nemetz, J. Smolle, G. Schwarz, D. Schikora, S. Uranüs
5.1
Introduction
For the first time, laserneedle stimulation allows simultaneous and continuous laser illumination of individual acupuncture points [3,4]. Due to the contact of the laserneedle with the skin, the illuminated area at the acupuncture point remains constant and the relevant doses can be varied exactly by altering the duration of illumination. Goal of this animal experiment was to investigate the influence of laserneedle illumination on micro morphological structures of the skin and obtain objectified information regarding the effects of characteristic densities and illumination doses for laserneedles.
5.2 5.2.1
Methods Procedure
In this animal study, we performed experiments regarding the microcirculation in the skin and surface skin temperature, before, during and after laserneedle stimulation. We used a sus scrofa domesticus, which was put under general anaesthesia in the animal surgical unit, at the Department of Surgical Research, University Clinic of Surgery (Figure 5.1). The study was performed according to the rules of the ethical commission (animal study approval number GZ 66.010/10-BRGT/2003).
58
Fig. 5.1: Animal experimental investigation with laserneedle stimulation. Illumination of the skin using 8 laserneedles (circular positioning scheme). The microcirculation and temperature sensor is located in the middle of the positioning scheme. Pre-medication was done in two steps on the day of intervention: a) Orally: Diazepam (Gewacalm®) 10 mg, Ketamin (Ketanest S®) 250 mg, Azaperom (Stresnil®) 80 mg. b) 20 min after oral pre-medication, intramuscular: Atropin 0.5 mg, Diazepam (Gewacalm®) 20 mg, Ketamin (Ketanest S®) 50 mg, Azaperom (Stresnil®) 80 mg. Anaesthesia was started 20 minutes after pre-medication: Etomidate-®Lipuro 40 mg, Fentanyl 0.5 mg i.v. Intubation was done during spontaneous respiration and muscle relaxation with Pancuroniumbromid (Pavulon®) 4 mg. Maintenance of anaesthesia was performed with: Thiopental 4 g, Fentanyl 1.5 g, Pancuroniumbromid (Pavulon®) 20 mg/500 NaCl 0.9 % as continuous instillation. Ventilation was performed instrumentally according to characteristic biometric data. At the time of excision, hemodynamic parameters (blood pressure 130/70 mmHg; heart rate 80/min; central venous pressure 5 mmHg), as well as oxygenation (SaO2 99 %) and ventilation (etCO2 38 mm) were all in the normal range. Data registration of the measurement parameter Flux (= product of mean flow velocity and concentration of red blood cells), surface skin temperature and room temperature were measured during anaesthesia. A total of five measurement values were analyzed (a = 2 min before; b = 2 min, c = 10 min, d = 18 min after beginning stimulation and e = 2 min after deactivating laserneedle stimulation; compare Figure 5.3).
59 After completing the experiment, four histological samples from the shaved cutis at the thoracic-abdominal transition were investigated, two had been illuminated with laser the other two were used as negative controls.
5.2.2
Laserneedle stimulation
Laserneedle stimulation is new optic method, which is used for stimulating acupuncture points. Illumination of different variations and combinations on the body, ear, or hand are possible. Figure 5.2 shows the characteristic emission of a fitted laserneedle, which was used in this study. The coherence of laser illumination at the distal exit point was measured with Michelsoninterferrometry. The laserneedles used (wavelength: 685 nm) emitted red light in a „continuous wave“ mode with an output of 30 - 40 mW per laserneedle, resulting in a power density of 4.6 W/cm² or an energy density of ~ 4.6 kJ/cm². The transmitted energy into the skin is 55 J per laserneedle during a treatment period of 20 minutes. 1
intensity [a.u.]
emission wavelength: 685 nm
laser-needle emissioncharacteristics
total output power at distal end: 30 mW
optical cladding fibre core
-2
-1
1
2
optical fibre diameter [ a.u.] Fig. 5.2: Emission characteristics of a laserneedle (a.u. = arbitrary units).
5.2.3
Laser Doppler flowmetry and temperature measurement
Laser Doppler signals were registered with a Laser Doppler device (DRT4), by Moor Instruments Ltd. (Devon, England). Probe output is defined as 1 mW. Laser wavelength was 780 nm, the raw signal was filtered with a digital filter from 20 Hz to 22.5 kHz. A DPIT–probe (diameter 8 mm, length
60 7 mm) was used for registration. An additional unit for measuring temperature (accuracy 0.1 °C) was integrated.
5.3
Results
Figure 5.3 shows the results from the three measurement parameters at different measurement times before (a), during (b - d) and after (e) laserneedle activation. Skin surface temperature and room temperature parameters did not show marked changes, whereas the Flux value increased significantly 2 minutes after activation (b) and reached a maximum at the end of laserneedle stimulation at measurement point (d). Thereafter, this value was reduced to its initial level. Temp. (°C) 45
Temp. R.-Temp.
Flux 40 (a.u.)
Flux
35 30 25 20 a
b
c
d
e
20 min
Fig. 5.3: Surface body temperature (Temp.), room temperature (R.-Temp.) and Flux (= product of mean flow velocity and concentration of erythrocytes) in a.u. (arbitrary units) before (a), during (b - d) and after (e) 20-minute laserneedle stimulation. Note the increase in the Flux parameter during illumination.
The examination of the four histological samples revealed the following: The hematoxylin-eosin samples of the illuminated cutis did not reveal any changes in comparison with the control biopsies. In particular, no necroses of the epidermis or single keratinocytes was evident, nor were changes in the endothelial cells of the dermal blood vessels visible. No micro thrombosis or extravasation could be detected (Figure 5.4).
61
a
b
Fig. 5.4: Histological results of the illuminated (a) and not illuminated (b) cutis. No micro morphological differences are evident.
5.4
Discussion
Laser has become a term for future technology, precision, rapidity, and achievement. Although the discovery of laser dates back to Einstein, who founded the theory of stimulated emission in 1917, the history of laser in acupuncture is still young [8]. Questions regarding tissue damage caused by certain laser power densities arise repeatedly. Border values have been determined, however are currently being discussed very differently [2,8]. Goal of this animal experimental study was to objectify whether the illumination of the cutis with a new laser system (laserneedle stimulation) leads to tissue damage when used in acupuncture. We illuminated the cutis of a sus scrofa domesticus with 8 laserneedles and simultaneously registered microcirculatory parameters and temperature values with a laser Doppler flowmetry monitor. This technique allows the objectifying of circulation in the micro-capillary region, without influencing tissue structures. It is based on the Doppler-shifting of light when it hits moving parts (erythrocytes). This technique is mainly used in pharmacology for comparing measures which influence circulation, for controlling transplants and flaps in plastic surgery and for objectifying and classifying disease stages in angiological and dermatological research, as well as in occupational medicine [1,7,9]. It can also be applied for research in the fields of anaesthesiology, intensive medicine and neurosurgery [5,6]. Even though the microcirculation parameters indicate an increase in skin circulation after an illumination time of 20 minutes, histological
62 examinations did not show any signs of alterations in the examined layers of skin tissue. We assume that this results from the minimal absorption of the most important tissue parts such as water, haemoglobin, and melatonin, which is comparatively small at the emission wavelength of 685 nm of the laserneedles. This indicates that photons entering the tissue are scattered at the tissue molecules, however do not thermically counteract, as in processes of adsorption. The skin is more or less, transparent for laser at a wavelength of 685 nm, thus thermically induced tissue changes such as coagulation, ablation and carbonisation can not take place and were not provable in our experiments. Laser illumination of 685 nm used in the laserneedles and applied in a contact mode, with power densities between 1- 5 W/cm², did not induce measurable micro morphological changes in the illuminated skin [10]. The definition of relevant critical values, in particular, determination of wavelength dependent power densities which lead to micro-morphological tissue changes, will be clarified in further studies.
5.5
Acknowledgements
The authors thank cand. med. Evamaria Huber from the Department of Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University of Graz, for her assistance in data registration.
5.6 [1]
[2] [3] [4] [5] [6]
References Fagrell B (1994) Problems using laser Doppler on the skin in clinical practice. In: Belcaro GV, Hoffmann U, Bollinger A, Nicolaides N (1994) Laser Doppler. Med-Orion Publishing Company, London Los Angeles Nicosia, 49-54 Kert J, Rose L (1989) Clinical Laser Therapy. Scandinavian Medical Laser Technology, p. 13 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schwarz G, Dalageorgos K, Neger J, Kehl G (1996) LaserDoppler-Flowmetrie - Erfahrungen aus der Intensivmedizin. Biomed Technik 41: 166-169 Litscher G, Möller KO, Stollberger R, Schwarz G, Fuchs G, Baumgartner A, Leber K, Koop T, Ascher PW (1997) Laser-Doppler-
63
[7] [8] [9] [10]
Datenanalyse während interstitieller Laserthermotherapie unter Magnetresonanz-Kontrolle im Rahmen einer tierexperimentellen Studie. Biomed Technik 42: 93-96 Öberg P (1990) Laser-Doppler flowmetry. Crit Rev Biomed Eng 18: 125-163 Pöntinen PJ, Pothmann R (1998) Laser in der Akupunktur. Grundlagen, Indikation und Technik für die AkupunkturSchwerpunktpraxis. Hippokrates, Stuttgart Tenland T, Salerud EG, Nilsson GE, Öberg PA (1983) Spatial and temporal variations in human skin blood flow. Int J Microcirc: Clin Exp 2: 81-90 Litscher G, Nemetz W, Smolle J, Schwarz G, Schikora D, Uranüs S (2004) Histologische Untersuchungen zu mikromorphologischen Einflüssen von Lasernadelstrahlung. Ergebnisse einer tierexperimentellen Untersuchung. Biomed Technik 49: 2-5
64
6.
Effects of laserneedle stimulation on microcirculation and skin temperature G. Litscher, L. Wang, E. Huber
6.1
Introduction
Laser Doppler flowmetry (LDF) is a technique particularly used in the field of pharmacology for comparing measures which influence circulation, for controlling transplants and flaps in plastic surgery and for objectifying and classifying disease stages in angiological and dermatological research and in anesthesiology and intensive care medicine [1-6]. Flux (product of mean flow velocity and the concentration of red blood cells), for example, and the concentration of moving particles (erythrocytes) in the measurement volume are calculated. Recently, some reports in literature documented, that this method can also be applied in the field of acupuncture for scientific investigations [7, 8]. In this chapter, the use of laserneedle stimulation under real circumstances is examined, based on LDF- monitoring results.
6.2 Method and volunteers 6.2.1
Laser Doppler flowmetry
A laser Doppler monitor DRT4 (Moor Instruments, Millwey, Axminster, England) was used to determine Flux and temperature. Probe output was defined with 1 mW. Edge frequencies were 20 Hz and 22.5 kHz. The temperature unit (5 °C to 50 °C) had a resolution of 0.2 °C and accuracy of 0.5 °C. In addition to an RS-232 interface, this instrument disposes of analogous signals (0 – 10 V) as an output voltage. The instrument has the following dimensions: 280 x 160 x 360 mm and weighs 8 kg. Several measurement probes are available for the DRT4 monitor. The results documented in this study were obtained with the DPIT probe (diameter 8 mm, length 7 mm) (Fig. 6.1).
65
Fig. 6.1: Laser Doppler probe.
6.2.2
Volunteers and procedure
Twenty-two healthy volunteers (12 female, 10 male), with a mean age of 24.4 + 2.6 years (21 - 29 years) were examined. At the time of measurement, none of the volunteers were under the influence of drugs. They were informed about the procedure and gave their consent. Approval of this study was obtained from the Ethical Commission of the Medical University of Graz (Laserneedle-Stimulation; 13-048 ex 02/03). Continuous measurement of microcirculation parameters and temperature was started, after a resting period of 10 minutes. After reaching the “steadystate”, the following acupuncture points on the right hand were stimulated with a laserneedle (compare Fig. 6.2): Hegu (LI.4) Localization: At the highest point of the M. adductor pollicis, when the thumb lies against the index finger. Indication: Hegu is the most important analgesic point. Pain conditions; particularly massive manual stimulation relieves pain in the entire body. Specific cerebral effects of this distant point could be proven in clinical studies.
66
Laserneedle – temperature / Flux
Fig. 6.2: Laser Doppler perfusion and temperature monitor DRT4 (Moor Instruments, Millwey, Axminster, England) and laserneedle stimulation.
The laserneedle was fixed to the skin at the acupuncture point with adhesive tape, after previous cleaning of the skin with alcohol. A semi-conductor laser with an emission wavelength of 685 nm was used as the light source. Laser intensity was 60 mW. Details regarding the stimulation method can be found in the previous chapters. The Laser Doppler probe (compare Fig. 6.1) was applied at a distance of 1 cm from the laserneedle. This distance was selected based on the given geometric dimensions of the probe holder (compare Fig. 6.1) and a supposed optic depth in the infrared range of 1 cm. Temperature at the measurement point and room temperature were determined for comparison. Figure 6.3 shows the different measurement times schematically (a - e) before, during and after laserneedle stimulation.
67 b
c
1 min
d 1 min
10 min
a
e 20 min
2 min
2 min
laserstimulation active
Fig. 6.3: Measurement profile and measurement times (a - e).
6.2.3
Statistical analysis
Data were analyzed using „Friedman Repeated Measures ANOVA on Ranks“ with the computer program SigmaStat (Jandel Scientific Corp., Erkrath, Germany). The Tukey test was used for post hoc analysis. Results from the conditions before (a), during (b - d) and after (e) laserneedle acupuncture were noted as mean values (Cx + standard error SE). The level of significance was defined as p < 0.05.
6.3
Results
Figure 6.4 summarizes the results of the three parameters; Flux, hand and room temperature at the different measurement times (compare Fig. 6.3).
68
Laserneedle – temperature and Flux p = 0.005* p = 0.002*
Temp. (°C) Flux (a.u.)
34 32 30 28
Temp. R.-Temp. Flux
26 24
n = 22
22 20
a
b
c
d
e
20 min *
Friedman Repeated Measures Analysis of Variance on Ranks (Tukey Test)
Fig. 6.4: Changes in Flux (= product of concentration and velocity of erythrocytes), skin (Temp.) and room temperature (R.-Temp.) parameters before (a), during (b - d) and after (e) laserneedle stimulation at acupuncture point Hegu.
Observe the highly significant changes in Flux (p = 0.005) as well as the increase in temperature at the measurement site (p = 0.002). Even 2 minutes after deactivating laser stimulation (measurement time e), Flux was no longer significant but still markedly higher. Temperature at the stimulation point (distance 1 cm) also showed an obvious increase, which reached its maximum at measuring time d. The nearly constant room temperature was simultaneously registered as a comparative parameter.
69
Laserneedle - microcirculation left hand
right hand
Fig. 6.5: Eight deactivated laserneedles before starting the examination.
left hand
right hand
B.A., 25y, f
Fig. 6.6: Activated laserneedles during examination procedure.
70
10 min
30 min
10 min B.A., 25y, f
s
Fig. 6.7: Changes in parameters regarding concentration of erythrocytes (c1, c2) and temperature (t1, t2) at the left, or right hand in the phases before (10 min), during (30 min) and after (10 min) laserneedle stimulation.
6.4
Discussion
The Laser Doppler technique is a suitable method for measuring the concentration and velocity of moving blood cells in surface vessels. Penetration depth is confined to about 1 mm. Laser light is usually guided to the output point via light conductors. Due to the Doppler effect, frequency shifts of scattered light take place and can be determined by measuring flow velocity. Possible advantages of this technique particularly in acupuncture research are currently being evaluated [7-13]. Negative factors regarding this method per se are the failing standardization combined with difficult interpretation of clinical data and high purchasing costs of the LDF equipment. Advantages of this method are its time-saving aspect, non-invasiveness, continuous monitoring ability and user friendliness.
71 The results from this study indicate that the energy dose emitted by a laserneedle in 20 minutes, is high enough to increase local skin temperature and subcutaneous tissue temperature (mean of 0.7 °C ; p = 0.02). Thus, the modality of periphery stimulation with laserneedles is not only optical but also thermal. Light dispersion on the skin was measured using a new device (O2C Oxygen to see, LEA Medizintechnik, Giessen, Germany). Figure 6.8 shows that even at a distance of 4 cm the laser light from the laserneedle (685 nm) can be detected.
Laserneedle stimulation 4 cm
3 cm
2 cm
1 cm
1 cm 2 cm 3 cm 4 cm
Fig. 6.8: Light dispersion on the skin. Note the peak in the spectrum at 685 nm.
In addition it is very interesting that especially Flux is significantly increased (p = 0.005) only 2 minutes after beginning laserneedle stimulation. In other words, an improvement in local, peripheral microcirculation at the stimulation point takes place. This fact could prove to be useful in dermatologic indications. The results from this study should induce further investigations regarding the evaluation of temporal and spatial (laser Doppler imaging) changes in microcirculation parameters, during and after laserneedle stimulation. Possible artifacts, as described in literature should be reduced further [4].
72
6.5 [1]
[2] [3] [4] [5] [6]
[7]
[8]
[9] [10]
[11] [12]
[13]
References Fagrell B (1994) Problems using laser Doppler on the skin in clinical practice. In: Belcaro GV, Hoffmann U, Bollinger A, Nicolaides AN (1994) Laser Doppler. Med-Orion Publishing Company, London-Los Angeles-Nicosia, 49-54 Öberg P (1990) Laser-Doppler flowmetry. Crit Rev Biomed Eng 18: 125-163 Litscher G, Schwarz G, Boggett D (1995) Laser Doppler flowmetry – Peripheral microcirculation during cessation of cerebral and cardiocirculatory function. Biomed Technik 40: 195-199 Litscher G, Schwarz G, Dalageorgos K, Neger J, Kehl G. (1996) Laser-Doppler-Flowmetrie – Erfahrungen aus der Intensivmedizin. Biomed Technik 41: 166-169 Litscher G, Möller KO, Ratzenhofer-Komenda B, Schwarz G, Koop T, Kovac H (1997) Laser Doppler flowmetry in the hyperbaric environment. Lasers Med Sci 12: 342-346 Litscher G, Möller KO, Stollberger R, Schwarz G, Fuchs G, Baumgartner A, Leber K, Koop T, Ascher PW (1997) Laser-DopplerDatenanalyse während interstitieller Laserthermotherapie unter Magnetresonanz-Kontrolle im Rahmen einer tierexperimentellen Studie. Biomed Technik 42: 93-96 Sandner-Kiesling A, Litscher G, Voit-Augustin H, James RL, Schwarz G (2001) Laser Doppler flowmetry in combined needle acupuncture and moxibustion: A pilot study in healthy adults. Lasers Med Sci 16: 184-191 Litscher G, Wang L, Huber E, Nilsson G (2002) Changed skin blood flow perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers Med Sci 17: 19-25 Litscher G, Wang L, Nilsson G (2001) Laser Doppler Imaging und Kryoglobulinämie. Biomed Technik 46: 154-157 Sprott H, Jeschonnneck M, Grohmann G, Hein G (2000) Microcirculatory changes over the tender points in fibromyalgia patients after acupuncture therapy (measured with laser-Doppler flowmetry). Wien Klin Wochenschr 112(13): 580-586 Suter B, Kistler A (1994) Does acupuncture modify skin circulation via the autonomic nervous system? Schweiz Med Wochenschr 62: 36-38 Blom M, Lundeberg T, Dawidson I, Angmar-Mansson B (1993) Effects on local blood flux of acupuncture stimulation used to treat xerostomia in patients suffering from Sjogren’s syndrome. J Oral Rehabil 20(5): 541-548 Cramp AF, Noble JG, Lowe AS, Walsh DM (2001) Transcutaneous electrical nerve stimulation (TENS): the effect of electrode placement upon cutaneous blood flow and skin temperature. Acupunct Electrother Res 26(1-2): 25-37
73
7.
Effects of acupressure, manual acupuncture and laserneedle acupuncture on EEG bispectral index (BIS) and spectral edge frequency (SEF) in healthy volunteers G. Litscher
7.1
Introduction
Noninvasive bioelectrical neuromonitoring is gaining more and more attention in anesthesia and critical care [1,2]. The bispectral index (BIS) and the spectral edge frequency (SEF) are important numerical descriptors of the EEG and both are mainly used for assessing depth of anesthesia [3]. If anesthetists rely on BIS and SEF to detect awareness, then it is very important to exclude other influences that could give false readings. It is known that a number of environmental and physiologic factors may affect BIS performance. Recently it has been reported that also nonpharmacological interventions such as acupressure can reduce BIS values significantly [4]. This study is a randomized, controlled partly blinded (laserneedle acupuncture) cross-over trial intended to investigate the effects of three nonpharmacological interventions (acupressure, manual needle acupuncture and laserneedle acupuncture) on two processed EEG variables (BIS, SEF) and a verbal stress score in healthy volunteers.
7.2 7.2.1
Material and methods Subjects
We studied 25 healthy volunteers (mean age r SD: 25.5 + 4.0 years, range 21 - 39 years; 15 women, 10 men; body weight 69.1 r 16.1 kg; height 173.5 r 9.3 cm). None of the subjects had neurological or psychological disorders and they were not taking any medication. They were partly informed about the nature of the investigation and were paid for their participation. The investigators recording EEG and sedation data were blinded to the intervention applied to the volunteers. The subjects were not informed which of the four interventions was effectively a control (acupressure on a control
74 point). The study was approved by the Ethics Committee of the Medical University of Graz (13-048 ex 02/03). Written informed consent was obtained from each subject.
7.2.2
Procedure and study design
The study was performed as a randomized, controlled cross-over trial. Four EEG electrodes (F7-Fpz, F8-Fpz, Fz = ground) and a noninvasive blood pressure cuff were attached to the volunteers after they arrived at the biomedical engineering laboratory. Two channels of spontaneous electrical activity were recorded from electroencephalographic electrodes (Zipprep™ self-prepping electrodes; Aspect Medical Systems Inc., Natick, MA, USA). The skin-electrode impedance was < 2 kOhm. Low cutoff frequency was 2 Hz and high cutoff frequency was 30 Hz. The EEG was measured continuously using an Aspect A-1000 system (Aspect Medical Systems Inc., version 3.12, Natick, MA, USA). A period of 5 min was allowed for each subject to obtain steady state BIS and SEF values. Thereafter with one of the four conditions - acupressure at the acupoint Yintang, manual needle acupuncture at Yintang, laserneedle acupuncture at Yintang or acupressure at a control point was started (Fig. 7.1). There were three treatments and additionally to investigate a possible placebo effect, we also used acupressure at a control point. The acupoint Yintang (Ex.1) is located midway between the medical ends of the two eyebrows at the root of the nose (see Fig. 7.1, a - c). To assess the reliability and validity of acupressure and manual needle acupuncture, pressure on the acupoint and the control point was applied by the same chinese medical doctor experienced in Traditional Chinese Medicine. The thumb pressure was estimated to be about 3 x 105 Pa (mean force measured ~ 30 N / 1 cm²; Pascal (Pa) = N/m²; 30/0.0001=3x105).
75
a
b
c
d
Fig. 7.1: Different conditions of the cross-over study design: (a) acupressure at the acupoint Yintang, (b) manual needle acupuncture at Yintang, (c) laserneedle acupuncture at Yintang, and (d) acupressure at a control point in a 25-year-old healthy female (with permission by the volunteer E.H.).
Manual needle acupuncture was performed using sterile single use needles 0.30 x 30 mm (Huan Qiu; Suzhou, China). After local disinfections of the skin the needling method was oblique, in caudal direction (0.5 cm) [5]. Stimulation for a duration of 20 sec in intervals of 2 minutes consisted of a combination of rotating and thrusting movements using a special manual acupuncture stimulation technique (sedation method). The needle was removed after 10 minutes. Laserneedle acupuncture at the acupoint Yintang was performed using a new method for optical stimulation. This method was reported by our research group in the scientific literature in 2002 [6,7]. The laserneedle-technique represents a new, noninvasive method for optical stimulation of acupuncture points. The laser used in this study emits red light in continuous-wave mode with an output power of 30 - 40 mW, which results in a radiant exposure energy of about 2.3 kJ/cm² at the acupuncture point during a stimulation time of 10 min [6].
76 Acupressure on the control point (location: 2 cm from lateral end of the left eyebrow; Fig. 1, d) was performed in similar manner as on the acupoint Yintang (duration 10 min). All subjects had four conditions applied (Fig. 1, a - d). The persons were in a semi-lying position with closed eyes. The choice of the stimulation procedure was randomized within a subject and the interval between the different sessions was at least 20 min.
7.2.3
Evaluation parameters
The main evaluation parameters were BIS and SEF90 during different conditions (Fig. 7.1) and time intervals (Fig. 7.2). Measurements were made at time points a - g (see Fig. 7.2). In any one condition we recorded BIS and SEF values continuously but sampled the data for subsequent analysis at 7 points. A single reading was taken at each point. The stimulation was not stopped at the time of reading. The whole study session lasted 2 – 3 hours. BIS and SEF90 represent single numbers, which should decrease continuously with decreasing level of consciousness (hypnosis). There are several review articles for methodological details of signal processing of BIS and SEF [3].
b
c
d
1 min 5 min
1 min
2.5 min
a
f
e
2.5 min
5 min
g
5 min
2 min
2 min
10 min
Fig. 7.2: Stimulation procedure and different measuring points (a=before, b f=during, g=after stimulation).
After five minutes of stimulation (Fig. 7.2, d) the subjects were asked to move their right hand to clarify that they were awake and not asleep. In addition before and after each stimulation mode the persons were asked to score the stress and tension that they had based on a verbal stress scale (VSS) from 0 (no stress) to 10 (maximum stress) [4]. Heart rate (HR) and noninvasive blood pressure (BP) were also recorded before and after
77 acupressure stimulation at Yintang (measurement points: 1 min before ‘a’ and 1 min after ‘g’ (comp. Fig. 7.2)).
7.2.4
Statistical analysis
The BIS and SEF data were tested with analysis of variance (one-way repeated measures ANOVA; similar data were found to be normally distributed in previous investigations) using SigmaStat (Jandel Scientific Corp., Erkrath, Germany). Dunnett’s method was used for post hoc analysis. VSS data were compared using paired t-test. The results were graphically presented as box plots (BIS and SEF) and as scatter plot (VSS). Changes were considered significant at a p-value < 0.05.
7.3
Results
All subjects completed the study. Figure 7.3 shows the decreases of BIS values during acupressure applied to the acupoint Yintang in all 25 healthy volunteers.
78
1
5
2
3
4
8
7
6
9
10
11
12
13
14
15
16
17
21
18
22
19
23
20
24
25
Yintang
n=25
10 min
Fig. 7.3: The trend of BIS values of 25 healthy volunteers (1 – 25) before, during and after acupressure performed on the acupoint Yintang. All subjects were awake. Note the significant decrease (min. BIS = 35; no. 14) due to acupressure.
Before the subjects were stimulated, their mean BIS values (r SD) were 97.4 (98 - 95) r 1.0 and their mean SEF values (r SD) were 23.9 r 4.1 Hz (right) and 23.5 r 4.9 Hz (left). The BIS and SEF values both decreased significantly (p < 0.001) after starting acupressure. After 5 minutes acupressure at the acupoint Yintang the mean BIS values were 62.9 (minimum 35; see no. 14 in Fig. 7.3) r 13.9, and the mean SEF values were 13.3 (minimum 2.9) r 8.1 Hz (right) and 13.8 (minimum 2.7) r 7.3 Hz (left). The release of acupressure caused an increase in BIS and SEF back to the baseline values before stimulation (compare Fig. 7.4).
79
120
100
BIS
80
60
40
p < 0.001 (b-f vs. a)
20
One Way Repeated Measures ANOVA (Dunnett‘s Method)
BIS
0 35 30 25
Hz
20 15 10 5
SEF r
p < 0.001 (b-f vs. a)
0 35
30 25
Hz
20 15 10 5 0
a
p < 0.001 (b-f vs. a)
b
c
d
SEF l
e
f
g
Fig. 7.4: Box plots of alterations of BIS and SEF values (r right, l left) in 25 healthy volunteers before (a), during (b - f), and after (g) acupressure (compare Fig. 7.2) on the acupoint Yintang. The ends of the boxes define the twenty-fifth and seventy-fifth percentiles, with a line at the median and error bars defining the tenth and ninetieth percentiles.
80 Figure 7.5 summarizes the BIS and SEF results obtained during manual needle acupuncture, laserneedle acupuncture and acupressure on the control point. Significant (p < 0.05) changes were found in BIS values during laserneedle acupuncture (measuring points d and e; compare Figs. 7.2 and 7.5) and during acupuncture on the control point (measuring points d - f). After 7.5 minutes laserneedle acupuncture at acupoint Yintang the mean BIS values (r SD) were 95.4 (minimum 81; see Fig. 7.5, middle, upper panel) r 4.1. After 5 minutes acupressure at the control point the mean BIS values (r SD) were 94.2 (minimum 77; see Fig. 7.5, right, upper panel) r 4.8. SEF did not show any significant alteration. Laserneedle - Acupuncture
Acupressure - Control
120
120
120
100
100
100
80
80
60
n.s.
20
BIS
20
One Way Repeated Measures ANOVA (Dunnett‘s Method)
BIS
35
35
35
30
30
30
25
25
25
20
20
20
15
15
10
10
n.s.
5
SEF r
10
n.s.
5
SEF r
0
35
35
35
30
30
30
25
25
25
20
20
20
Hz 15
15
10
10 5
n.s.
SEF l
0
a
b
c
d
e
f
g
n.s.
SEF r
Hz
0
5
BIS
15
Hz
0
One Way Repeated Measures ANOVA (Dunnett‘s Method)
Hz
0
Hz
0
Hz
0
5
p < 0.05 (d-f vs. a)
60
40
40
40
20
80
p < 0.05 (d,e vs. a)
60
BIS
BIS
BIS
Needle - Acupuncture
0
15 10 5
n.s.
a
SEF l
b
c
d
e
f
g
0
n.s.
a
SEF l
b
c
d
e
f
g
Fig. 7.5: Box plots of changes of BIS and SEF values (r right, l left) during manual needle acupuncture, laserneedle acupuncture and acupressure at the control point. Further explanations see Fig. 7.4.
The results of the analysis of the VSS are demonstrated in Fig. 7.6.
81 10
8
VSS
6
Acupuncture Yintang
NeedleAcupuncture
Laserneedle Acupuncture
Acupressure Control
a
a
4
a
a 2
0
b b p < 0.001
b paired t-test
b (n.s. p < 0.012)
Fig. 7.6: Mean (+ SD) values of the verbal stress score (VSS) of 25 healthy volunteers before (a) and after (b) different modalities of nonpharmacological stimulation (0 = no stress; 10 = maximum stress).
The VSS values were significantly (p < 0.001) reduced after pressure application on Yintang, needle acupuncture and laserneedle acupuncture but also after pressure application on the control point (p = 0.012). Mean baseline VSS values were insignificant lower in laserneedle and control conditions. HR and BP values (mean r SD) before and after acupressure at Yintang were calculated to be 73.2 r 12.4 1/min, 109.8 r 14.0 mmHg (systolic) and 69.3 r 10.6 mmHg (diastolic). After stimulation the values decreased to 63.7 r 11.9 1/min, 107.7 r 8.7 mmHg (systolic), and 66.8 r 8.6 mmHg (diastolic), respectively.
7.4
Discussion
The bispectral index and the spectral edge frequency are mainly used intraoperatively to monitor the hypnotic effect of anesthetic drugs. There are several studies reported in the literature proposing target values for EEG parameters to guide the depth of anesthesia. A number of authors have reported a low probability of recall and a high probability of unresponsiveness during surgery at a level of 60 for BIS [8,9]. BIS values < 50 are described as suppressing hemodynamic responses during intubation
82 [10]. In an editorial of the European Journal of Anaesthesiology Chan and Gin reported recently that statistically it would be extremely unlikely for a patient to be aware when BIS is less than 50 and, in fact, there has not been a single case of frank awareness at this level [11]. In that context our results showed that 10 of 25 awake healthy volunteers (40 %) have Yintang acupressure induced BIS values below 50 and 21 of 25 subjects (84 %) below 60. Acupressure, acupuncture, meditation, hypnosis or relaxation techniques are all considered to be forms of complementary and alternative medicine. Acupuncture has been shown to reduce medication use in a number of trials [12]. Acupressure has been studied and offered in scientific literature as a valuable treatment in improving the quality of sleep [13]. In previous studies it has also been shown that pressure on acupoints can decrease postoperative pain [14] and that Korean hand acupressure reduces postoperative nausea and vomiting after gynecological laparoscopic surgery [15]. Acupressure has also been used in some other studies for prevention of emesis [16]. There are a number of theories as to how acupressure or acupuncture works. All these hypotheses show, that the brain plays a key role in acupuncture and acupressure research [17-20]. Modulation of subcortical structures may be an important mechanism by which acupuncture and acupressure exerts its complex multisystem effects [20]. Demonstration of regionally specific, quantifiable acupuncture and acupressure effects on relevant structures of the human brain would facilitate acceptance and integration of these therapeutic modalities into the practice of modern medicine [17-20]. It has been shown in several publications that different narcotics have different influence on BIS and SEF [8-11, 21-26]. However, nonpharmacologic influences such as electromyographic activity may contribute to the low specificity of the absolute values of the electrophysiological measurement data [21]. In the majority of the cases the BIS is falsely elevated [21]. Our results appear to confirm the results of the study of Fassoulaki et al. [4] who also found that acupressure on Yintang resulted in a significant and clinically relevant reduction on BIS values and they concluded that BIS and SEF are therefore of limited clinical relevance for monitoring depth of anesthesia [22-26]. However, Fassoulaki et al. [4] did not look at the SEF, nor did they investigate the effects of manual needle acupuncture and the effects of laserneedle acupuncture (Fig. 7.7). We have shown in this study that awake volunteers subjected to acupressure at Yintang can have similar BIS and SEF values to anaesthetized patients. While it is unlikely that a patient will receive acupressure or acupuncture during surgery, the question as to what causes BIS readings below 50 in awake subjects remains. It is unlikely to be a placebo effect as we have
83 shown in several test measurements using placebo points that BIS is not affected by laserneedle stimulation per se. In the present study there were small statistically significant but not clinically important changes with needle acupuncture, laserneedle acupuncture and acupressure at control point. These findings also help confirm that the BIS and SEF reductions induced by acupressure at Yintang are not a placebo effect. Reduced electromyographic levels could be partially responsible [21] (Fig. 7.8).
Fig. 7.7: Laserneedle stimulation at Yintang (CSA = coulor spectral array; CFM = mean EEG-parameter; BIS = bispectral index; HR = heart rate; HRV = heart rate variability). Note the decrease of the BIS values during laserneedle activation.
84
EEG – EMG - HR
EMG
EEG - DELTA LaserneedleLaserneedle-Stimulation – Yintang (10 min)
Fig. 7.8: Electromyographic (EMG) and electroencephalographic Delta (EEG Delta) activities during laserneedle stimulation at Yintang.
At the moment it is also unclear to what degree system algorithms contribute to such findings. BIS is certainly affected by electrical activity nearby, especially diathermy. Therefore there could also be a possibility that local movement in the region of the recording electrode might be responsible for the EEG effects observed. These are apparently less during control point acupuncture than during Yintang acupressure, where pressure is applied to a point immediately adjacent to the Zipprep electrode. Further investigations are necessary to clarify these questions. In conclusion, we found in healthy awake volunteers that acupressure at Yintang results in statistically significant and clinically relevant reductions in BIS and SEF while needle acupuncture, laserneedle acupuncture and acupressure at a control point result in statistically significant but clinically unimportant reductions. Although the validity of BIS in anesthesia is higher than that of SEF, BIS too has to be interpreted very carefully as our results show. Our results also highlight the electroencephalographic similarities of acupressure induced sedation and anesthesia [27].
85
7.5
Acknowledgements
The author would like to express his thanks to Ms. Lu Wang MD, Ms. Petra Petz MSc and Evamaria Huber (all Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz) for their valuable help.
7.6 [1] [2]
[3] [4]
[5] [6] [7] [8]
[9] [10]
[11] [12]
References Litscher G, Schwarz G (2001) Editorial. Noninvasive bioelectrical neuromonitoring in anaesthesia and critical care. Eur J Anaesthesiol 18: 785-788 Litscher G (2000) Editorial. The future of neuromonitoring. Internet J Neuromonitoring 1(1): http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijnm/vol1n 1/editorial2.xml Rampil IJ (1998) A primer for EEG signal processing in anesthesia. Anesthesiology 89: 980-1002 Fassoulaki A, Paraskeva A, Patris K, Pourgiezi T, Kostopanagiotou G (2003) Pressure applied on the extra 1 acupuncture point reduces bispectral index values and stress in volunteers. Anesth Analg 96: 885-889 Stux G, Pomeranz B (1998) Basics of acupuncture. Springer; Berlin Heidelberg New York Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Sebel PS, Lang E, Rampil IJ, White PF, Cork R, Jopling M, Smith NT, Glas PS, Manberg P (1997) A multicenter study of bispectral electroencephalogram analysis for monitoring anesthetic effect. Anesth Analg 84: 891-899 Liu J, Singh H, White PF (1997) Electroencephalographic bispectral index correlates with intraoperative recall and depth of propofolinduced sedation. Anesth Analg 84: 185-189 Heck M, Kumle B, Boldt J, Lang J, Lehmann A, Saggau W (2000) Electroencephalogram bispectral index predicts hemodynamic and arousal reactions during induction of anesthesia in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth 14: 693-697 Chan MTV, Gin T (2000) Editorial. What does the bispectral EEG index monitor? Eur J Anaesthesiol 17: 146-148 Greif R, Laciny S, Mokhtarani M, Doufas AG, Bakhshandeh M, Dorfer L, Sessler DI (2002) Transcutaneous electrical stimulation of an
86
[13] [14] [15] [16] [17] [18] [19] [20]
[21] [22] [23]
[24] [25] [26]
[27]
auricular acupuncture point decreases anesthetic requirement. Anesthesiology 96: 306-312 Tsay SL, Chen ML (2003) Acupressure and quality of sleep in patients with end-stage renal disease - a randomized control trial. Intern J Nursing Studies 40: 1-7. Felhendler D, Lisander B (1996) Pressure on acupoints decreases postoperative pain. Clin J Pain 12: 326-329 Boehler M, Mitterschiffthaler G, Schlager A (2002) Korean hand acupressure reduces postoperative nausea and vomiting after gynecological laparaoscopic surgery. Anesth Analg 94: 872-875 Eizember FL, Tomaszewski CA, Kerns WP (2002) Acupressure for prevention of emesis in patients receiving activated charcoal. J Toxicol Clin Toxicol 40: 775-780 Cho ZH, Wong EK, Fallon JH (2000) Neuro-Acupuncture. Q-Puncture, Los Angeles Litscher G, Cho ZH (Eds.) (2000). Computer Controlled Acupuncture®. Pabst Science Publishers, Lengerich Berlin Düsseldorf Riga Scottsdale Wien Zagreb Litscher G (2001) High-Tech Akupunktur®. Pabst Science Publishers, Lengerich Berlin Düsseldorf Hui KKS, Liu J, Makris N, Gollub RL, Chen AJ, Moore CI, Kennedy DN, Rosen BR, Kwong KK (2000) Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Human Brain Mapping 9: 13-25 Bruhn J, Bouillon TW, Shafer SL (2000) Electromyographic activity falsely elevates the bispectral index. Anesthesiology 92: 1485-1487 Riess ML, Graefe UA, Goeters C, Van Aken H, Bone HG (2002) Sedation assessment in critically ill patients with bispectral index. Eur J Anaesthesiol 19: 18-22 Drummond JC (2000) Monitoring depth of anesthesia. With emphasis on the application of the bispectral index and the middle latency auditory evoked response to the prevention of recall. Anesthesiology 93: 876-882 Nieuwenhuijs D, Coleman EL, Douglas NJ, Drummond GB, Dahan A (2002) Bispectral index values and spectral edge frequency at different stages of physiologic sleep. Anesth Analg 94: 125 - 129 Kalkman CJ, Drummond JC (2002) Monitors of depth of anesthesia, quo vadis? Anesthesiology 96(4): 784-787 Bruhn J, Bouillon TW, Radulescu L, Hoeft A, Bertaccini E, Shafer SL (2003) Correlation of approximate entropy, bispectral index, and spectral edge frequency 95 (SEF95) with clinical signs of „anesthetic depth“ during coadministration of propofol and remifentanil. Anesthesiology 98: 621-627 Litscher G (2004) Effects of acupressure, manual acupuncture and Laserneedle® acupuncture on EEG bispectral index and spectral edge frequency in healthy volunteers. Eur J Anaesthesiol 21: 13-19
87
8.
Acupuncture using laserneedles modulates brain function: first evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI) G. Litscher, D. Rachbauer, S. Ropele, L. Wang, D. Schikora, F. Fazekas, F. Ebner
8.1
Introduction
A new noninvasive laserneedle system has been developed and used for the first time in acupuncture research recently [1,2]. This new optical stimulation technique has the advantage that the stimulation is absolutely painless. Moreover laserneedle acupuncture allows to stimulate appropriate acupoint combinations simultaneously and with higher radiation doses than commercially available low level hand held laser equipment. The laser radiation of eight laser diodes is coupled into eight optical fibers and the laserneedles are arranged at the distal ends of the optical fibers. Due to the direct contact of the laserneedles and the skin, no loss of intensity occurs and the laser power, which affects the acupoints, can be exactly determined [1,2]. The aim of this study was to provide evidence of specific effects of laserneedle acupuncture by stimulating a combination of vision related acupoints of traditional Chinese medicine (TCM). Quantification of cerebral effects of stimulation was performed using functional multidirectional transcranial Doppler sonographic (fTCD) in a randomized controlled doubleblind cross-over study design (fTCD). We also performed functional magnetic resonance imaging (fMRI) measurements in one volunteer using a block design. The dynamics of the metabolic mechanism that regulates cerebral blood flow has already been studied in normal human subjects using fTCD [3,4]. Blood flow velocity in the posterior cerebral artery (PCA), supplying the visual cortex, increased by 16.4 % in response to light stimulation of the retina.
88 The method of fTCD has also been used in previous studies in acupuncture and laserneedle research to investigate specific changes in blood flow velocities of different cerebral arteries [1]. Functional magnetic resonance is sensitive to subtle regional changes in the blood oxygenation level from increased neuronal activity during a specific task or stimulation. It has been successfully used to map the sites of brain activations during needle and low level laser acupuncture [5-9]. These studies report increase (positive activation) and decrease (negative activation) of the BOLD (blood oxygenation level dependent) signal. However, fMRI has not been used up to now during laserneedle stimulation.
8.2 8.2.1
Methods Painless laserneedles
For our experiments eight acupuncture points were chosen and irradiated simultaneously. The laserneedles used in this study emit red light in cwmode with an output power of 30 - 40 mW per laserneedle (wavelength: 685 nm). The fiber core diameter used in this study was about 500 µm. The time of irradiation was 20 min (fTCD measurements) resulting in an energy density of about 4.6 kJ/cm² at each acupoint and a total sum of 36.8 kJ/cm² for all acupoints. The laserneedles were fixed onto the skin using plaster stripes but not pricked into the skin.
8.2.2
Functional multidirectional sonography (fTCD)
transcranial
Doppler
Transtemporal Doppler sonographic examinations of the PCA and the middle cerebral artery (MCA) were performed simultaneously and continuously to determine alterations of cerebral blood flow velocities [4]. A Multi-Dop T unit (DWL Electronic Systems GmbH, Sipplingen, Germany) including two 2 MHz probes were used in a multidirectional ultrasound probe holder construction. Under acoustic control, the angle and position of the probes were adjusted until the greatest possible signal amplitude was reached. Alterations in the blood flow velocities of both arteries were registered continuously and simultaneously. In addition blood pressure was measured non invasively before and after stimulation (Cardiocap® CC-104, Datex Medical Electronics, Hoevelaken, The Netherlands).
89 8.2.3
Functional magnetic resonance imaging (fMRI)
Functional magnetic resonance imaging was performed using a 1.5 Tesla whole body system (Intera, Philips Medical Systems, Best, The Netherlands). Functional images sensitive to blood oxygen dependent contrast were acquired with a T2* weighted gradient echo with single shot echo planar readout (flip angle 90°, TE 50 ms, FOV 250 mm, matrix 96 x 96 interpolated to 128 x 128). Thirty axial slices with a slice thickness of 4 mm were imaged. A total of 144 volume images was obtained continuously with a repetition time of 5 seconds per volume.
8.2.4
Participants
We investigated 18 healthy volunteers (mean age r SD: 25.4 r 4.3 years; range: 21 - 30 years; 11 female, 7 male) using fTCD (n=17) and one volunteer using fMRI (27 y, female). The study protocol was approved by the institutional ethics committee of the Medical University of Graz (11-017 ex 00/01) and all 18 participants gave written informed consent. None of the subjects was under the influence of centrally active medication. All persons were free of neurological or psychological disorders including the absence of visual deficits. A honorarium was given for participation.
8.2.5
Experimental design and procedure
Eight vision related distal acupoints (Hegu, Zusanli, Kunlun, Zhiyin) [6,7,10] on both sides and 8 placebo points were tested using two schemes (fTCD measurements), each in one session in a randomized controlled double-blind cross-over study design (Fig. 8.1). The same acupoints were used for the fMRI investigation. The acupuncture scheme was selected by an expert in TCM. In addition we have seen in several test measurements that needle stimulation of this acupuncture scheme led to alterations of blood flow velocity in the PCA.
90
Vision Related Acupoints
Placebo Points
Fig. 8.1: Vision related acupuncture points and placebo points used in this study. All acupoints (left panel, from bottom to top and from right to left: Hegu, Zusanli, Kunlun, Zhiyin) and all placebo points (right panel) were stimulated bilaterally.
The acupoints were cleaned with alcohol. Then the laserneedles were put in contact with the skin and fixed by plaster stripes. During the experiments the subjects were in a relaxed and comfortable position on a bed in our laboratory (fTCD measurements) or lying in the scanner (fMRI investigation). For the fTCD investigations we started randomly with either acupoint or placebo stimulation. Acupoints Hegu (LI.4): Location: On the dorsum of the hand, between the 1st and 2nd metacarpal bones, in the middle of the 2nd metacarpal bone on the radial side. Indications: Headache, redness, swelling and pain of the eye. Zusanli (Sp.36): Location: 3 cun below Dubi (S 35), one finger-breadth from the anterior crest of the tibia. Indications: Gastric pain, abdominal distension, vomiting, diarrhea, dysentery, has tonification effect. Kunlun (UB.60): Location: In the depression between the tip of the external malleolus and tendo calcaneus. Indications: Headache, neck rigidity, dizziness.
91 Zhiyin (UB.67): Location: On the lateral side of the small toe, about 0.1 cun lateral to the corner of the nail. Indications: Headache, pain in the eye, nasal obstruction, epistaxis, malposition of fetus.
8.2.6
Evaluated parameters
The mean blood flow velocity (vm) in the PCA and the MCA were evaluated simultaneously and continuously at different measurement points (a - e in Fig. 8.2A) [10]. Each person was studied performing stimulation on vision related acupoints and placebo points. The interval between the fTCDexperiments was 20 to 30 minutes and the subjects were instructed to keep their eyes closed during the whole fTCD experiments. Similarly, during fMRI investigations the subject could not see whether the laser was off or on. The fMRI study used a block design with alternating one minute resting condition (‘R’) and one minute activation condition (‘A’) (Fig. 8.2B). The experiment started with ‘R’ followed by the laserneedle acupuncture condition (‘A’). A total of 6 ‘R’ and 6 ‘A’ intervals was registered. Altogether the fMRI data acquisition took 12 minutes. b
c
d 1 min
1 min
A
10 min
a
e
20 min Laserneedle Stimulation 2 min
2 min
Stimulation OFF
Stimulation ON
A
B
R
A R
A R
A R
A R
A R
1 min
12 min
Fig. 8.2: Measurement profiles for fTCD (A) and fMRI (B) measurements.
92 8.2.7
Statistical analysis
The fTCD data before (a), during (b - d), and after (e) laserneedle acupuncture (comp. Fig. 8.2A) were tested with Kruskal-Wallis one way ANOVA on ranks (SigmaStat, Jandel Scientific Corp., Erkrath, Germany). The criterion for significance was p < 0.05. The fMRI data were analysed using SPM 99 (SPM 99, Department of Imaging Neuroscience, London, UK). All volumes from the subject were realigned using the first volume as a reference and resliced using sincinterpolation. The functional images were spatially normalized to a standard echo planar template in Tailarach space. Functional data were spatially smoothed with a 6 mm full width at half maximum isotropic kernel. A boxcar waveform convolved with a synthetic hemodynamic response function was used as the reference waveform. A t-test was performed to identify regions showing significantly higher activation during the activation condition versus the resting condition. For significantly activated regions, a statistical threshold p < 0.05, corrected at the cluster level for multiple comparisons, was used.
8.3
Results
The results of the alterations of mean blood flow velocities in the PCA and MCA before, during, and after laserneedle and placebo acupuncture are summarized in Figure 8.3.
93
vm [cm/s]
PCA
Vision related acupoints (A)
50 + 2.5 cm/s
40
SE
MCA 50
40
vm [cm/s]
a
b
c
d
e
Placebo points (B)
PCA
50
40
SE
MCA 50
40
a
b
c
d
e
Fig. 8.3: Mean blood flow velocity (vm) of the posterior cerebral artery (PCA) and the middle cerebral artery (MCA) before (a), during (b - d), and after (e) stimulating vision related acupoints (A) and placebo points (B) with laserneedles in 17 healthy volunteers. Note the trend towards an increase (+ 2.5 cm/s) in vm in the PCA during acupoint stimulation.
The results showed a trend towards an increase of vm (insignificant changes) in the PCA during (b - d) laserneedle acupuncture at vision related acupoints (Fig. 8.3A, upper panel). At the same time only minor changes in vm were seen in the MCA (Fig. 8.3A, lower panel). The maximum amplitude of vm in the PCA was detected with a delay of 20 - 60 sec after the initial stimulus by
94 the laserneedles (vm; Cx r SE, acupoint stimulation, PCA: 42.2 r 2.5 before (a), 44.2 r 2.6 during (b - d), 42.3 r 2.4 cm/s after (e)). Stimulation at placebo points did not increase vm of the PCA and of the MCA (Fig. 8.3B), rather there was a trend towards a small decrease of mean values of the mean vm in both arteries (vm, Cx r SE, placebo point stimulation, PCA: 42.9 r 2.6 before (a), 41.7 r 2.6 during (b - d), 42.1 r 2.8 cm/s after (e)). The mean arterial blood pressure before and after laserneedle acupuncture was almost identical (76.7 r 7.6 (SD) vs. 75.8 r 6.8 mmHg). The results of the fMRI investigation are shown in Figures 8.4 and 8.5 and Table 8.1. Significant changes in brain activation were found in the occipital lobe and in the frontal lobe.
right
left
Fig. 8.4: First evidence of significant effects of changes in brain activation during laserneedle stimulation of vision related acupoints in the occipital and frontal areas in a 27-year-old healthy female using fMRI investigation.
95
Signal Change Visual Cortex [a.u.]
A 3 2 1 0 -1 -2 -3
R
12 min Time [min]
Fig. 8.5: The time course of signal change correlated with the experimental fMRI paradigm. Note the signal increases during active laserneedle acupoint stimulation (A) and the signal decreases during resting condition (R).
Brain Areas Occipital Left superior occipital gyrus Frontal Right inferior frontal gyrus Right precentral gyrus Left middle frontal gyrus Left superior frontal gyrus
Brodmann Area
19
4
Coordinates in Tailarach Cluster size space (x,y,z) Z-value (mm³)
-38
-84
28
5.80
32
54
34
12
5.23
64
20
-28
64
5.43
32
-20
60
20
5.59
32
-18
56
16
5.23
32
Tab. 8.1: Regions of significant activation (occipital and frontal areas) due to laserneedle stimulation of vision related acupoints. The p-values are corrected (p < 0.05) at the cluster level for multiple comparisons. Compare Fig. 8.4.
96
8.4
Discussion
Recent scientific and technological progress especially regarding the application of modern brain function monitoring systems has truly revolutionized acupuncture research. The usage of advanced exploratory tools, such as functional multidirectional transcranial ultrasound Doppler sonography or functional magnetic resonance imaging, provides insights and attempt to shine scientific light upon the most spectacular of the eastern medical procedures [3,4]. Recently it has been attracted interest that the brain is the key to acupuncture’s and laser puncture’s effects. New experimental constructions to measure ultrasound, light and bioelectrical processes can reproducibly demonstrate effects of stimulation of acupoints in the brain [1,2,5-21]. The new laserneedle system has been described for the first time in scientific literature recently [1]. In addition previous studies from our group show that the new optical stimulation with laserneedles can elicit reproducible cerebral effects which are in the same order with respect to the maximum amplitude of the mean blood flow velocity as compared to needle acupuncture [1]. The stimulation performed within this study could not be felt by the patient. The operator was also unaware of whether the stimulation was active, and therefore a true double-blind study was performed. Moreover laserneedle is the first laser system commercially available that could be used at eight or more standard acupuncture points simultaneously. The effectiveness of unconventional complementary medical methods, such as laserpuncture, has previously been documented mainly as single cases. There are many theoretical and clinical studies concerning laserpuncture in scientific literature. For a short review see [1]. To our knowledge, laseracupuncture has not been studied in cases where more than one acupoint at time were stimulated. In our experiment, we tested four acupoints (four on both sides of the body) with laserneedle acupuncture, and measured the alterations of brain activations using fTDC and fMRI. In this study, we were not able to separate significant specific cerebral effects of blood flow velocity during laserneedle acupuncture using fTCD. However, there was a trend of an increase in vm during laserneedle stimulation of visual acupoints in the PCA. Similar significant effects have been reported after manual needle acupuncture [11,13-16]. Previous results also show that different modes of manual acupuncture stimulation differentially modulate cerebral blood flow velocity [20].
97 In addition to fTCD we used for the first time fMRI in a healthy volunteer during laserneedle stimulation of the same vision related acupoints as used for the fTCD measurements. Bilateral stimulation of the acupoints produced bilateral positive activation over the frontal cortex. A time-logged increase of the BOLD signal was also seen at the left superior occipital gyrus (Brodmann Area 19). Apparently the stimulation of vision-implicated acupoints (Kunlun, UB.60 and Zhiyin, UB.67) activated the visual cortex. These findings are in accordance with other fMRI acupuncture studies. Cho et al. [7] reported that needling of acupoints (UB.60, 65, 66 and 67) on the foot created activation in the visual cortex similar to actual visual stimuli. Needling of non-acupoints on the foot 2 to 5 cm away from the vision related acupoints as control caused no activation in the occipital lobes [7]. In traditional needle acupuncture treatment points are located at different depths and hence needle insertion is different. This is of particular importance with the points we selected because Zhiyin requires a very shallow needle insertion versus Zusanli. With the laserneedle stimulation the acupoints will receive different energy doses because of their different depths. It is possible that the effects seen with fTCD and fMRI could be due to stimulation of one of the points. Further investigation on this topic is necessary. Li et al. [6] recently also found that the application of conventional or electro-acupuncture over four vision-implicated acupoints on the right foot can modulate the activity of specific brain sites. Negative and positive activations were seen using fMRI during conventional acupuncture while positive activations, similar to our results of laserneedle stimulation, only were observed during optical stimulation and electro-acupuncture. The authors also found bilateral activations in frontal cortices [6]. It has been demonstrated using fMRI that needle acupuncture [7] and laser puncture [9] of the vision-related acupoint Zhiyin (UB.67) activates the visual cortex of the human brain. As a further study on the effect of this acupoint stimulation on the visual cortex, Lee et al. [22] examined c-Fos expression in binocularly deprived rat pups. Interestingly, acupuncture stimulation of UB.67 resulted in a significant increase in the number of cFos-positive cells in the primary visual cortex, while acupuncture stimulation of other points less important for visual function had no significant effect on c-Fos expression in the primary cortex. Other studies have shown effects of acupuncture needle manipulation of LI.4 (we also used this acupoint (Hegu) in our scheme as a general point of activation) on a network of cortical and subcortical limbic and paralimbic structures [5]. We did not find the same significant effects in our fMRI
98 experiment. In this context it is important to mention that laserneedle acupuncture allows for the first time a totally painless acupuncture stimulation. Therefore differences between electro acupuncture [23] and needle acupuncture, which often includes pain stimulation, and a painless acupuncture stimulation technique can be examined.
8.5 (a)
(b) (c)
8.6
Conclusions Using the new laserneedle acupuncture method we were able to stimulate multiple vision-associated acupuncture points at the same time. The results showed insignificant increases in cerebral blood flow velocity of the PCA after stimulation of vision-related acupoints on the foot. At the same time blood flow velocity in the MCA showed minor changes. Stimulation at placebo points did not show increases in blood flow velocity in both arteries. The fMRI results of a healthy volunteer after laserneedle stimulation of the same acupoints showed significant changes in occipital and frontal brain areas. Both techniques, fTCD and fMRI, can be used to study cerebral effects of laserneedle acupuncture in a complementary way [24].
Acknowledgements
The authors thank Evamaria Huber (Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz, Austria) and Martin Kronbichler (Department of Psychology, University of Salzburg, Austria) for their support to this study.
8.7 [1] [2] [3]
References Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Aaslid R (1987) Visually evoked dynamic blood flow response of the human cerebral circulation. Stroke 18(4): 771-775
99 [4] [5]
[6] [7]
[8]
[9]
[10] [11]
[12] [13] [14] [15] [16]
[17] [18]
Sturzenegger M, Newell DW, Aaslid R (1996) Visually evoked blood flow response assessed by simultaneous two-channel transcranial Doppler using flow velocity averaging. Stroke 27(12): 2256-2261 Hui KKS, Liu J, Makris N, Gollub RL, Chen AJW, Moore CI, Kennedy DN, Rosen BR, Kwong KK (2000) Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Map 9: 13-25 Li G, Cheung RTF, Ma QY, Yang ES (2003) Visual cortical activations on fMRI upon stimulation of the vision-implicated acupoints. NeuroReport 14: 669-673 Cho ZH, Chung SC, Jones JP, Park JB, Park HJ, Lee HJ, Wong EK, Min BI (1998) New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci USA 95: 2670-2673 Cho ZH, Oleson TD, Alimi D, Niemtzow RC (2002) Acupuncture: the search for biologic evidence with functional magnetic resonance imaging and positron emission tomography techniques. Editorial. J Altern Compl Med 8: 399-401 Siedentopf CM, Golaszewski SM, Mottaghy FM, Ruff CC, Felber S, Schlager A (2002) Functional magnetic resonance imaging detects activation of the visual association cortex during laser acupuncture of the foot in humans. Neurosci Lett 327: 53-56 Litscher G, Schikora D (2002) Effects of new noninvasive laserneedles on brain function. Proceedings of the International Federation for Medical and Biological Engineering 2: 996-997 Litscher G (2002) Computer-based quantification of traditional Chinese-, ear- and Korean hand acupuncture: Needle-induced changes of regional cerebral blood flow velocity. Neurol Res 24: 377380 Litscher G, Wang L, Wiesner-Zechmeister M (2000) Specific effects of laserpuncture on the cerebral circulation. Lasers Med Sci 15: 57-62 Litscher G (2001) High-Tech Akupunktur®. Pabst Science Publishers, Lengerich Berlin Rom Riga Wien Zagreb Litscher G, Wang L, Yang NH, Schwarz G (1999) Computer-controlled acupuncture. Quantification and separation of specific effects. Neurol Res 21(6): 530-534 Litscher G, Wang L, Yang NH, Schwarz G (1999) Ultrasoundmonitored effects of acupuncture on brain and eye. Neurol Res 21(4): 373-377 Litscher G, Yang NH, Schwarz G, Wang L (1999) Computer-controlled acupuncture. A new construction for simultaneous measurement of blood flow velocity of the supratrochlear and middle cerebral arteries. Biomed Techn 44(3): 58-63 Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I (1998) Robotic transcranial Doppler sonography probes and acupuncture. Int J Neurosci 95(1-2): 1-15 Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I, Eger E (1998) Effects of acupuncture on the oxygenation of cerebral tissue. Neurol Res 20 Suppl 1: 28-32
100 [19] [20]
[21] [22]
[23] [24]
Litscher G, Wang L (2000) Cerebral near infrared spectroscopy and acupuncture - results of a pilot study. Biomed Techn 45(7-8): 215-218 Bäcker M, Hammes MG, Valet M, Deppe M, Conrad B, Tölle TR, Dobos G (2002) Different modes of manual acupuncture stimulation differentially modulate cerebral blood flow velocity, arterial blood pressure and heart rate in human subjects. Neurosci Lett 333: 203206 Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Lee H, Park HJ, Kim SA, Lee HJ, Kim MJ, Kim CJ, Chung JH, Lee H (2002) Acupuncture stimulation of the vision-related acupoint (Bl-67) increases c-Fos expression in the visual cortex of binocularly deprived rat pups. Am J Chin Med 30: 379-385 Napadow V, Makris N, Liu J, Kettner NW, Kwong KK, Hui KKS (2005) Effects of electroacupuncture versus manual acupuncture on the human brain as measured by fMRI. Hum Brain Mapp 24: 193-205 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laser needles modulates brain function: first evidence from functional transcranial Doppler sonography and functional magnetic resonance imaging. Las Med Sci 19: 6-11
101
9.
Quantification of gender specific thermal sensory and pain thresholds before and after laserneedle stimulation G. Litscher, L. Wang, E. Huber, D. Schikora, G. Schwarz
9.1
Introduction
The quantitative determination of border values for thermal sensory and pain threshold testing has been clinically used for several years and is of great importance in the fields of neurology, psychiatry, and neurophysiology [6]. Several guidelines regarding the correct application of „Quantitative sensory testing“ (QST) were published in scientific literature [4]. QST-systems can generally be divided into instruments, which allow the application of physical-thermal, chemical or vibration specific stimuli. In addition, the general equipment required for generating electric stimulation with different frequencies and intensities can be included here. Thermal stimulation in this study was performed with a thermode (Peltier’s Principle) applied at the right palmer base of the thumb, in healthy adult volunteers. Goal of this study was to determine normal values and objectify possible gender specific differences. For the first time, QST was used, in combination with scientific tests using the new laserneedle stimulation technique, to quantify possible alterations before and after painless acupuncture with laserneedles.
9.2 9.2.1
Method Volunteers
Twenty-nine healthy adult volunteers, mean age (Cx r SD) was 24.2 r 2.7 (range from 18 to 29 years) were included in the study. Twenty volunteers were female (mean age: 23.9 r 2.7 years) and 9 were male (mean age: 24.9 r 2.8 years). The ethical committee of the Medical University of Graz (laserneedle stimulation; 13-048 ex 02/03) approved the tests and all
102 volunteers gave their written consent. None of the volunteers had neurological or psychological deficits or was under the influence of drugs.
9.2.2
Measurement of thermal sensitivity and thermal pain thresholds
A computer-controlled system was used for quantitative evaluation of small calibre nerve fibres (A-Delta and C-nerve fibres) using temperature tests (Thermal Sensory Analyser TSA-II, Medoc Advanced Medical Systems, Ramat Yishai, Israel, and Minneapolis, Minnesota, USA). The system consists of a basic unit with connection to an external notebook, a thermode with an active contact area of 30 x 30 mm (Peltier element) and a control device for input of patient reaction data. The thermode was placed on the inner side of the volunteer’s hand and can either cool or warm the skin. Adaptation temperature between 30 and 32 °C is achievable within a few seconds after skin contact, thus, the volunteer is unable to feel cold or hot sensations. The software runs with Windows, controls the system, and includes the different test methods. All parameters can be set individually. In addition to thermal sensory measurement, pain thresholds (cold pain, heat pain: 0 - 52 °C) were examined (Fig. 9.1). Cold sensation (a) and warm sensation (b) thresholds were determined first. Then, cold pain (c) and heat pain (d) thresholds were determined (compare Fig. 9.4). A resting period of at least 5 minutes was held between the single measurements.
103
2 1 3
Fig. 9.1: Set-up in the lab of the Dept. of Biomedical Research in Anaesthesia and Intensive Medicine, Medical University Graz. Thermal Sensory Analyser TSA-II (1) with Notebook-Data analysis (2) and laserneedle stimulation device (3). With generous consent from the volunteer.
9.2.3
Laserneedle acupuncture and procedure
Laserneedles are special light conductors which are placed vertically at the skin, and trigger painless stimulation at the acupoint. They offer high optical output densities regarding measurable cerebral effects compared with acupuncture needles [9 ,10], and for the first time, allow simultaneous optical activation of up to eight acupoints according to Traditional Chinese Medicine (TCM). The laserneedles used emit light with a wavelength of 685 nm in a continuous or frequency modulated wave mode. The output per laserneedle is 30 - 40 mW. Further information regarding the method and the periphery and cerebral effects of laserneedle acupuncture can be found in previous publications [8-10]. Acupuncture was performed at the acupoints shown in Figure 9.2. First, the skin was disinfected with alcohol at the acupoint, and then the laserneedles are applied and fixed to the skin with special adhesive tape. During testing, the volunteers were positioned relaxed on a bed (compare Fig. 9.1). In two
104 different tests, the laserneedles were once applied and activated for 10 minutes, or remained deactivated in an identical procedure (placebo). Which test procedure was performed first was selected at random. Each volunteer was tested with activated as well as deactivated laserneedles, whereby the volunteers were not informed about and could not perceive the respective mode being used. The resting period between both tests was at least 20 minutes. Following acupoints were used [16]: Hegu (LI.4): Localisation: Indication: Needling:
At the highest point of M. adductor pollicis, when the thumb lies against the index finger. Hegu is the most important analgesic point. Pain conditions; particularly strong manual stimulation relieves pain in the entire body. Vertical, 1 - 2 cm deep in direction Pe.8 Laogong.
Taiyuan (Lu.9): Localisation: On the radial side of the bending fold at the wrist joint, lateral from A. radialis. Indication: Pain in the wrist region, polyneuropathy at the upper extremity. Needling: Vertical or inclined, 0.3 - 1 cm deep. Quchi (LI.11): Localisation: At the lateral end of the bending fold of the elbow during right-angled bending of the lower arm. Indication: Homeostatic and immuno-stimulating point. Needling: Vertical, 2 - 3 cm deep. Shenmen (Ear point 55): Localisation: In the fossa triangularis. Indication: General sedative and analgesic point. Ear point 67: Localisation: Indication:
Between helix and anthelix in the so-called scapha. Pain, hand, wrist.
105
1 2
3
4 5 2 1
Fig. 9.2: Laserneedle stimulation at the acupoints Hegu (1), Taiyuan (2), Quchi (3), Shenmen – Ear point 55 (4) and Ear point 67 (5).
9.2.4
Statistical analysis
A „t-test“for the conditions before (I) and after (II) laserneedle stimulation and a „paired t-test“ for the placebo test, were used to determine gender specific differences. Significance was defined with p < 0.05. The results are shown graphically with box-plot illustrations (Statistical program SigmaStat; Jandel Scientific Corp., Erkrath, Germany).
9.3
Results
Figure 9.3 shows a sample „test report“. In addition to a marker at the derivation, or stimulation region („C6 right hand palmar thumb“), the measurement results (mean value of 3 tests) and differences (ǻ) before and after intervention (laserneedle stimulation or placebo test) of the respective testing mode are shown graphically in this protocol.
106
Fig. 9.3: „Quantitative Somatosensory Test Report“ from an 18-year-old volunteer. Above: laserneedle stimulation; below: placebo test.
Figure 9.4 summarizes the results from all 29 volunteers, without considering gender. No significant differences between the single tests before and after laserneedle stimulation or placebo stimulation were evident.
107 Temp. [°C] 60
laserneedle stimulation I
placebo I
II
II
50 I I
40 I
II
II
II
I I
30
II
I
II
II
20
10
0
n=29 0
1
a
2
3
b
4
5
c
6
7
d
8
9
10 11 12 13 14 15 16 17 18
a
b
c
d
Fig. 9.4: Box-plot illustration of n = 29 healthy volunteers. Cold sensation- (a) and warm sensation thresholds (b) and cold pain- (c) and heat pain thresholds (d) before (I) and after (II) laserneedle stimulation (left) and placebo (right). The horizontal line in the box indicates the position of the median. The ends of the box define the 25th and 75th percentile; the error bars mark the 10th and 90th percentiles.
Separation of the results according to gender is illustrated in Figure 9.5. Significant (p < 0.034) gender specific differences are seen in cold pain and heat pain thresholds. The border values of painful cold sensation also differs significantly between males and females (p < 0.001) as those of painful heat sensation (p = 0.009 and p = 0.034 respectively). During placebo stimulation, no obvious differences in median values are evident. However, it should be mentioned that the median tolerance of cold pain sensation after laserneedle acupuncture in females, although insignificant (p = 0.479), lies higher than before laserneedle treatment (* in Fig. 9.5A).
108 Temp. [°C]60
laserneedle stimulation I
50 I
40 I
placebo I
II
II
I
II
I
30
I
II
II
II
A
II
I
II
women *)
20
10
0
p = 0,034
p < 0,001
p = 0,009
p < 0,001
t-test
p = 0,026
n=20
Temp. [°C] I
I
II I
I I
II
II
II
II
I
I
II
B
II I
II
men
n=9 a
b
c
d
a
b
c
d
Fig. 9.5: Gender specific analysis (female (A), male (B)). In addition to the significant gender specific differences in pain sensation, note the difference (*) in median values during cold pain threshold determination before (I) and after (II) laserneedle stimulation. Further information see Fig. 9.4.
109
9.4
Discussion
There are numerous publications concerning QST reproducibility [20], the different biological effects on thermal sensor, vibration specific and pain thresholds and the gender specific differences and influence of age and body size [19]. Clinical indications for QST described in this study are the determination of sensory and pain thresholds in chronic pain disorders [17], diabetic neuropathy [3] and use in patients with multiple sclerosis [7,18]. The method for quantitative determination of different thermal thresholds used in this study has also been used in different publications in combination with other measurement techniques. For example, the comparison and correlation of somatosensory evoked potentials [14] and the supplementary or combined use with functional magnetic resonance imaging [2,5] should be mentioned. In this study, we could document significant gender specific differences in temperature sensation. A difference in gender specific thermal sensory thresholds could be proven in numerous studies [20]. In addition to these results, QST shows that cold sensations change during the female menstrual cycle dependent upon the oestrogen secretion [1]. An interesting aspect of this study design is that acupuncture subjectively relieves pain in females better than in males. This is one of the first, unpublished intermediate results of the worldwide largest controlled acupuncture study being currently performed in Germany. In a representative random sample, 1096 patients treated with acupuncture against lumbar or knee pain were questioned. Two thirds of the women, but only half of the men were satisfied with the effect of needle therapy. Sixtyone percent of the questioned persons evaluated the effect as very good or good. In contrast, 92 percent of the treating physicians were certain that this treatment was a success. Even when nine of ten patients were not satisfied with the treatment, the respective physician supposed treatment was successful. This documents the physician’s subjectivity towards the patients’ pain sensitivity and indicates the necessity of qualitative evaluation of acupuncture to objectify the potential therapy effect individually. The effects of acupuncture and laserneedle acupuncture on parameters of peripheral circulation could be scientifically proven in several studies [1113]. In many cases, moxibustion (burning of the flowering plant mugwort) intensifies the effect [15]. Measurement data determined in our study, before and after laserneedle acupuncture and placebo laserneedle acupuncture, showed no significant differences when using an acupoint scheme for acute pain. However, cold pain sensation could be reduced in women with laserneedle acupuncture. To what extent acupuncture schemes for treating
110 chronic pain with laserneedle acupuncture can lead to provable effects in the described measurement parameters should be investigated in further studies.
9.5
Acknowledgements
The authors thank Mr. Michael Magometschnigg and Mr. Ing. Stefan Wüger (both from INTEC Medizintechnik GmbH, Vienna, Austria) for their organisational and technical support with Thermal Sensory Analyser TSA-II. We also thank Ms. Ingrid Gaischek MSc. (Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University Graz) for her valuable support in data analysis and writing the manuscript.
9.6 [1] [2]
[3] [4] [5] [6] [7]
[8] [9] [10]
References Bajaj P, Arendt-Nielsen L, Bajaj P, Madsen H (2001) Sensory changes during the ovulatory phase of the menstrual cycle in healthy women. Eur J Pain 5: 135-144 Becerra LR, Breiter HC, Stojanovic M, Fishman S, Edwards A, Comite AR, Gonzalez RG, Borsook D (1999) Human brain activation under controlled thermal stimulation and habituation to noxious heat: an fMRI study. Magn Reson Med 41: 1044-1057 Bravenboer B, van Dam PS, Hop J, Steenhoven Jvd, Erkelens DW (1992) Thermal threshold testing for the assessment of small fibre dysfunction: normal values and reproducibility. Diabet Med 9: 546-549 Consensus report (1993) Quantitative sensory testing: a consensus report from the Peripheral Neuropathy Association. Neurology 43: 1050-1052 Davis KD, Kwan CL, Crawley AP, Mikulis DJ (1998) Functional MRI study of thalamic and cortical activations evoked by cutaneous heat, cold, and tactile stimuli. J Neurophysiol 80: 1533-1546 Fruhstorfer H, Lindblom U, Schmidt WC (1976) Method for quantitative estimation of thermal thresholds in patients. J Neurol Neurosurg Psychiatry 39: 1071-1075 Heijenbrok MW, Anema JR, Faes TJ, Bertelsmann FW, Heimans JJ, Polman CH (1992) Quantitative measurement of vibratory sense and temperature sense in patients with multiple sclerosis. Electromyogr Clin Neurophysiol 32: 385-388 Litscher G (2003) Cerebral and peripheral effects of laser needlestimulation. Neurol Res 25: 722-728 Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342
111 [11]
[12]
[13] [14] [15]
[16] [17]
[18] [19] [20] [21]
Litscher G, Wang L, Huber E, Nilsson G (2002) Changed skin blood perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers Med Sci 17: 1925 Litscher G, Wang L, Huber E, Nilsson G (2001) Laser Doppler Imaging – Objektivierung und Quantifizierung primärer peripherer Mikrozirkulationsänderungen durch Akupunktur. Europäische Zeitschrift für Akupunktur, Der Akupunkturarzt / Aurikulotherapeut 3: 7-17 Litscher G, Wang L, Nilsson G (2001) Laser Doppler Imaging und Kryoglobulinämie. Biomed Technik 46: 154-157 Meh D, Denislic M (2000) Correlation between temperature and vibration thresholds and somatosensory evoked potentials. Electromyogr Clin Neurophysiol 40: 131-134 Sandner-Kiesling A, Litscher G, Voit-Augustin H, James RL, Schwarz G (2001) Laser Doppler flowmetry in combined needle acupuncture and moxibustion: a pilot study in healthy adults. Lasers Med Sci 16: 184-191 Stux G, Stiller N, Pomeranz B (1999) Akupunktur. Lehrbuch und Atlas. Springer, Berlin Heidelberg New York Thimineur M, Sood P, Kravitz E, Gudin J, Kitaj M (1998) Central nervous system abnormalities in complex regional pain syndrome (CRPS): clinical and quantitative evidence of medullary dysfunction. Clin J Pain 14: 256-257 Treede RD, Hansen C, Hopf HC (1995) Paradoxical warm-sensation is a common symptom in patients with multiple sclerosis. Electroencephalogr Clin Neurophysiol 97: 125 Wiles PG, Pearce SM, Rice PF, Mitchell JM (1991) Vibration perception threshold: Influence of age, height, sex, and smoking, and calculation of accurate centile values. Diabet Med 8: 157-161 Yarnitsky D, Sprecher E, Zaslansky R, Hemli JA (1995) Heat pain thresholds: normative data and repeatability. Pain 60: 329-332 Litscher G, Wang L, Huber E, Schikora D, Schwarz G (2004) Quantitative Bestimmung geschlechtsspezifischer thermischer Empfindungsund Schmerzschwellen vor und nach Lasernadelstimulation. Biomed Technik 49: 106-110
112
10. Biological effects of painless laserneedle acupuncture - a short summary of important scientific results G. Litscher, L. Wang, D. Schikora, D. Rachbauer, G. Schwarz, A. Schöpfer, S. Ropele, E. Huber 10.1 Introduction The stimulation of acupuncture points with laser light can evoke specific effects in the periphery and in the brain. For the first time, these effects, can be objectified and quantified using modern biomedical engineering techniques. Laserneedle acupuncture represents a new, painless method for primary optical stimulation of acupuncture points [1-15]. Laserneedles, are not inserted in the skin, however, simply applied to the acupuncture point. This method allows the simultaneous stimulation of individually combined points for the first time. This study gives a current summary regarding scientific proof and innovative aspects of painless laserneedle acupuncture. We introduce studies which prove the peripheral effects using registration of temperature and laser Doppler flowmetry [8,9,13], as well as publications regarding the objectification of cerebral effects of laserneedle acupuncture aided by functional multi-directional transcranial Doppler sonography (fTCD) [13,8,9,11,12], functional magnetic resonance imaging (fMRI) [11,12] and near infrared spectroscopy (NIRS) [2,4-6,8,9].
10.2 Methods 10.2.1
Temperature and microcirculatory monitoring
The surface temperature of the skin and the measurement parameter Flux (= product of concentration and velocity of erythrocytes) were performed with the Laser-Doppler-Flowmetry Monitor DRT 4 (Moor Instruments, Millway, Axminster, England). A DPIT-probe (diameter 8 mm, length 7 mm) with a power of 1 mW was used (compare Fig. 10.1, above). The edge frequencies were 20 Hz and 22.5 kHz [8,9,13].
113 10.2.2
Functional multi-directional sonography (fTCD)
transcranial
Doppler-
The Multi-Dop T System (DWL Electronic Systems GmbH, Sipplingen, Germany), was used to measure the mean blood flow velocity in different cerebral arteries. A 4-MHz- (ophthalmic artery (OA)), as well as 2-MHz probes (posterior cerebral artery (PCA), anterior cerebral artery (ACA), middle cerebral artery (MCA)) were applied with a specially developed ultrasound probe holding construction (compare Fig. 10.2, right below).
10.2.3
Functional magnetic resonance imaging (fMRI)
The fMRI-investigations were performed using a 1.5 Tesla total body system (Intera, Philips Medical Systems, Best, Netherlands) (compare Fig. 10.4, above). The BOLD (blood oxygen level dependent) contrast sensitive images were acquired with a T2* weighted gradient echo sequence (single shot planar readout, flip angle 90°, TE 50 ms, FOV 250 mm, matrix 96 x 96 interpolated at 128 x 128, layer number 30, layer thickness 4 mm). A total of 144 volume images, were registered continuously in succession, with a repetition time of 5 seconds. The fMRI-study is based on a block design with alternating resting conditions („R“) for one minute and one minute of laserneedle activation („A“). This experiment starts with „R“, followed by the laserneedle condition „A“. A total of six „R“ and six „A“ intervals were registered. Each fMRI data registration required 12 minutes [11, 12].
10.2.4
Near infrared spectroscopy (NIRS)
Near infrared spectroscopic investigations for monitoring laserneedle acupuncture, were done with the NIRO 300 Monitor (Hamamatsu Photonics, Japan). Measurement values, and such as changes in oxyhaemoglobin (¨O2Hb) and desoxyhaemoglobin (¨HHb) were determined using LambertBeer´s principle. Alterations in parameters could be measured absolutely (µmolar) with this system, but not the level (absolute concentration) at which these changes (in a positive or negative direction) occur. As long as no change in concentration is given, the measurement value is zero. Using a silicone holder, the fixating of the sensor (emitter and near infrared detectors) on the head is easy.
10.2.5
Laserneedle stimulation
As mentioned earlier, laserneedle acupuncture (Schikora, D.: European Patent Nr. PCT/EP 01/08504) allows the simultaneous stimulation of
114 individual point combinations. Variation and combination of acupuncture points on the body are possible according to Traditional Chinese Medicine (TCM), or at the ear and hand using Korean (KHA) or Chinese (CHA) hand acupuncture. The laserneedle method is based on a multi-channel system with 8 separate semi-conductor laser diodes and emission wavelengths of 685 nm and 785 nm. The system consists of flexible optical light fibres, which conduct the laser light without loss to the laserneedle. Thus, a high optical density at the distal end of the laserneedle is achievable. The intensity of the laserneedles are optimized in such a way, so that the patient does not feel the activation of the needle (30 - 40 mW per needle; diameter 500 µm; duration 10 min; power density 2.3 kJ/cm² per acupuncture point). More details regarding this method are described in previous studies [1,6].
10.2.6
Healthy volunteers, animal experiment and procedures
This summarizing study presents a total of 511 measurements in 231 healthy test persons (129 females, 102 males) with a mean age of 25.2 r 3.5 (Cx r SD) years (18 to 38 years). Protocols were approved by the local ethic committee, Medical University of Graz (11-017 ex 00/01: Computercontrolled acupuncture; and 13-048 ex 02/03: Laserneedle-stimulation), and all test persons gave their written consent. None of the test persons had obvious visual, neurological, olfactory, or mental deficits or stood under influence of CNS active drugs. A maximum of seven acupuncture points were investigated simultaneously in different measurement series. In addition, an animal study was included in this report. The animal used was a sus scrofa domesticus, which was put under general anaesthesia in the animal surgical suite of the Department of Surgical Research at the Medical University of Graz (compare Fig. 10.1, left). This study was performed in accordance with the rules defined by the ethic committee (animal study approval number GZ 66.010/10-BRGT/2003).
10.2.7
Statistical analysis
Data was analysed with „One-way repeated measure ANOVA“ , using the computer program SigmaStat (Jandel Scientific Corp., Erkrath, Germany). The tests described in single publications were used for post hoc-analyses. The level of significance was defined as p < 0.05 when no other value was explicitly given. The fMRI-data was analysed and evaluated with SPM 99 (Statistical parametric mapping) - Software (SPM 99, Department of Imaging Neuroscience, London, England). All images of the test persons were newly
115 organized and the first picture was used as reference, whereby „sincinterpolation“ was used. Functional data were spatially smoothed with a 6 mm full width at half maximum isotropic kernel. A boxcar waveform convolved with a synthetic haemodynamic response function was used as the reference waveform. A ttest was performed to identify regions showing significantly higher activation during the activation condition versus the resting condition. For significantly activated regions, a statistical threshold p < 0,05, corrected at the cluster level for multiple comparisons, was used. The activated regions were located with help of the Tailairach-space.
10.2.8
Evaluation parameters
Temperature (surface skin temperature and room temperature), Flux, partially simultaneous and continuous measurement of mean blood flow velocity (vm) in the OA, MCA, PCA and ACA at different measurement times (a - e) were determined. A number of test persons underwent testing using different acupuncture schemes. The interval between the single experiments was 30 minutes to one day, and the test persons were instructed to keep their eyes closed during the entire active examination phase. In a similar manner to fMRI-examination, the test persons were unable to determine whether the laserneedles had been activated or deactivated.
10.3 Results Figure 10.1 shows in summary the results of an animal study [13] and a nontherapeutic biomedical engineering study with test persons [8,9] regarding the periphery effects of laserneedle acupuncture. The Flux, hand and room temperature parameters were summarized at different measurement points. The significant (p = 0.005) increase of Flux in the test persons during 20 minutes of laserneedle stimulation (b - d) must be considered. The results of the animal study show that laserneedle stimulation (wavelength: 685 nm; power density: 4.6 kJ/cm² per point; duration 20 min) can cause alterations in microcirculatory parameters of the skin, in the sense of increased circulation, however, the laser quality and intensity did not induce any micro-morphological changes in the skin [13].
116 Scientific studies - laserneedle acupuncture Peripheral effects: temperature and laser Doppler flowmetry Animal experiment (sus scrofa domesticus)
Healthy volunteers: mean age + SD: 24.4 + 2.6 yrs; 12 f, 10 m
n=1
n = 22
p = 0.005 p = 0.02
45
34
Temp. 32 (°C)
40
Temp. (°C) 35 Flux (a.u.)
30 Temp. R.-Temp. Flux
30
Flux 28 (a.u.)
Temp. R.-Temp. Flux
26 24
25
22 20
a
b
c
d
e
n=1
20 min modified from: Biomed. Technik, 2004, 49: 2-5 [13]
20
a
b
c
d
e
n = 22
20 min modified from: Neurol. Res., 2003, 25: 722-728 [9]
Fig. 10.1: Animal (left side) and human experimental (right side) studies using laserneedle stimulation. Flux (product of concentration and velocity of erythrocytes), surface skin temperature (Temp.) and room temperature (R.-Temp) before (a), during (b – d) and after (e) laserneedle activation.
Figures 10.2 and 10.3 document specific changes in cerebral blood flow velocities in different arteries. Using the laser acupuncture scheme (TCM: Zanzhu and Yuyao; ear: eye and liver; KHA: E2; CHA: Yan Dian) the blood flow velocity in the OA using a wavelength of 685 nm increases significantly (p = 0.01). However, a 30 % increase in stimulation intensity only increases vm in the OA to a mean value of 11 %. Simultaneously, no significant changes in vm occurred in the MCA. Using laserneedle acupuncture with a wavelength of 785 nm, a marked, but insignificant (p = 0.546) increase in vm in the OA during stimulus application occurred. Brief stimulation (20 sec each) of the single points with a hand-held low level laser (19 mW), did not reveal any significant (p = 0.939) differences in vm in the OA, concerning the conditions before and after stimulation.
117 Scientific studies - laserneedle acupuncture Cerebral effects: fTCD / OA - MCA Volunteers: n = 27; mean age + SD: 25.2 + 4.1 yrs, 21 - 38 yrs 14 f, 13 m Laserneedle acupuncture
Volunteers: n = 25; mean age + SD: 24.5 + 3.8 yrs, 18 - 34 yrs 14 f, 11 m Laserneedle acupuncture intensity +30 %
Laserneedle acupuncture
Ophthalmic artery (OA) 20
15
a
15
SE 10
p<0.01*
a
c
Middle cerebral artery (MCA)
b
p=0.939
15
SE
p=0.01*
60
20
p=0.546
15
10
Ophthalmic artery (OA)
20
b
b
685 nm
Ophthalmic artery (OA)
Ophthalmic artery (OA)
vm (cm/s)
Low Level Laser
785 nm
685 nm
685 nm
20
Volunteers: n = 18; mean age + SD: 24.8 + 3.3 yrs, 18 - 35 yrs 9 f, 9 m
c
10
b a
SE
SE
c
10
a
c
Middle cerebral artery (MCA)
b
60
50
a
c
40
a
c
Fig. 10.2: Specific changes in mean blood flow velocity (vm) under laserneedle acupuncture (from left to right: 685 nm, 685 nm with increased intensity (+ 30 %), 785 nm and 685 nm (19 mW)). Mean values and standard error (SE) before (a), during (b) and after (c) stimulation are shown.
Figure 10.3 shows the changes in vm in the ACA and PCA when applying different laser puncture schemes (A, B). When using laser puncture scheme A, vm increased during stimulation (b - d) significantly in the ACA (p < 0.001) and is still higher at the end of the experiment (e) than before laser puncture (a). At the same time, insignificant changes in vm occurred in the PCA. During optical stimulation of the acupuncture points in scheme B, a significant increase (p < 0.002) in vm in the PCA took place although simultaneously insignificant changes in the ACA were observed.
118 Volunteers n=22 12 female, 10 male, 21 - 29 years ( 24.4 + 2.6 years; x + SD ) R
Laser puncture scheme A
Laser puncture scheme B
Anterior cerebral artery (ACA) vm (cm/s)
Anterior cerebral artery (ACA) vm (cm/s)
50
52
49
51
*)
48
50
47
49
46
48
45
47 a
b
c
d
n.s.
e
a
b
c
d
e
*) p < 0.001
Posterior cerebral artery (PCA) 45
Posterior cerebral artery (PCA) vm (cm/s)
vm (cm/s)
47 46
44
45
43
*)
44
42
n.s.
41
43 42
40 a
b
c
d
e
a
b
c
d
e
*) p < 0.002
Fig. 10.3: Laserneedle acupuncture study in a double-blinded randomised, crossover design. Changes in blood flow vm before (a), during (b - d) and after (e) activation of laserneedles according to the specific laser puncture scheme (A or B).
119 The first fMRI-results using laserneedle acupuncture are summarized in Figure 10.4. Significant (p < 0.05) changes in brain activity were registered in the occipital and frontal regions during stimulation of distant, visual acupuncture points and near the olfactory cortex during the activation of acupuncture points, which according to Traditional Chinese Medicine, have a connection to the sense of smell. Further, significant (p < 0.001) activation after stimulating the Yintang point in the fronto-parieto-temporal region, with massive EEG-alterations (appearance of frontal Delta-activity) occurred [10]. Scientific studies - laserneedle acupuncture Cerebral effects: fMRI Vision related acupoints
H.B., 27 y, f modified from: Las. Med. Sci., 2004; 19: 6-11 [11]
Olfactory system related acupoints
L.A., 28 y, f modified from: Schmerz & Akupunktur, 2004; 1: 4-11 [12]
Yintang
E.S., 28 y, f
E.M., 29 y, m
p < 0.001 (correction for multiple comparisons)
Fig. 10.4: Functional magnetic resonance images illustrating activated cerebral regions after laserneedle stimulation. Specific cerebral activation patterns are shown according to the selected acupuncture schemes.
Figure 10.5 shows, in summary, frontal and non-invasively registered changes in O2Hb during and after needle or laserneedle acupuncture (same scheme as in Fig. 10.2). Whereas nearly no changes during acupuncture of placebo points take place, increases during laserneedle acupuncture are obvious.
120 Scientific studies - laserneedle acupuncture Cerebral effects: NIRS
Fig. 10.5: Cerebral changes in near infrared spectroscopy in µmol of oxyhaemoglobin (O2Hb) during needling of a placebo point, 3 hand acupuncture points, 2 ear acupuncture points, 2 body acupuncture points according to TCM, a combination of hand, ear and body acupuncture points, as well as laserneedle stimulation, and increased (+ 30 %) laserneedle stimulation (from left to right), during and 5 minutes after acupuncture. Modified according to [6].
Figure 10.6 at the left, shows the hypothetically assumed course of stimulus intensity, in random units of a metal and laserneedle as a function of time. At the middle and at the right, real time signals registered with NIRS and bioelectric methods (EEG - BIS) are illustrated.
121
metal needle
Stimulus intensity SI [a.u.]
hypothesis
NIRS-response
EEG-BIS-response
O2Hb 100
metal needle 90
HHb
10 min
10 min
laserneedle
Stimulus intensity SI [a.u.]
time [min]
O2Hb laserneedle
100
90
HHb time [min]
10 min
10 min
B.J., 22y, f modified from: Spectroscopy 2002; 16: 335-342 [6]
modified from: Spectroscopy 2002; 16: 335-342 [6]
H.E., 25y, f modified from: Europ. J. Anaesthesiol. 2004; 21: 13-19 [10]
Fig. 10.6: Stimulus intensity (SI) as a function of time. From left to right: hypothesis, real measured cerebral reactions of near infrared spectroscopy measurement parameters O2Hb (Oxyhaemoglobin) and HHb (Desoxyhaemoglobin), as well as the bioelectric response (BIS = Bispectral index). Modified according to [4,6,10].
10.4 Discussion The term „laser“ is very fascinating for many people today. Innovation and laser are nearly synonymous. Albert Einstein, already formulated the physical foundation for so-called light intensification with stimulated emission, in 1917. In the field of medicine, laser not only allows careful treatment for patients, but also a manifold of selective therapies in nearly all special fields. Laser has developed to be an important instrument in acupuncture when considering the treatment of small children, or patients with a phobia against needles. One goal of this study is to give a summary about previous clinical experimental studies dealing with this new method of optical acupuncture stimulation. Since the test person or patient does not feel the intervention, furthermore, the different acupuncture points can be stimulated continuously and simultaneously, it was possible to perform these double-blind randomised, controlled, cross-over studies for the first time. The studies indicate that cerebral effects of this manner of stimulation are nearly equivalent to that in needles. In addition to complex multi-directional sonography, it was also possible to provide proof regarding cerebral functional changes after laserneedle stimulation using functional magnetic
122 resonance imaging for the first time. At the same time, points “near the head” could be stimulated during fMRI examination, which was not possible thus far with acupuncture needles and hand-held laser instruments. The new scientific results may be of great importance, not only for the field of laser medicine, but also for acupuncture research in general.
10.5 Conclusion For the first time, laserneedle acupuncture allows simultaneous optical stimulation of individual puncture point combinations. Variations in acupuncture on the body, ear or hand, as performed and described in these studies are also possible. The studies were able to objectify and specify the cerebral effects of laserneedle stimulation for the first time. The cerebral effects triggered by this new, painless laserneedle technique are of similar dimension to those evoked by manual needle acupuncture. Painless laserneedle acupuncture can induce specific, reproducible changes in the brain. These can be expressed by shifts in different parameters, such as cerebral blood flow velocity [15].
10.6 Acknowledgements The authors would like to thank Ingrid Gaischek MSc (Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University of Graz) for her valuable support in this study.
10.7 References [1] [2]
[3]
Litscher G, Schikora D (2002) Cerebral effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Neue Konzepte in der experimentellen Akupunkturforschung - Computerkontrollierte Laserpunktur (CCL) mit der Laserneedle® Technik. Der Akupunkturarzt / Aurikulotherapeut 28: 18-28 Litscher G, Schikora D (2002) Effects of new noninvasive laserneedles on brain function. In: Hutten H, Krösl K, editors. EMBEC 2002. Proceedings of the 2nd European Medical & Biological Engineering Conference; 2002 Dec 4-8; Vienna, Austria. Graz; Verlag der Technischen Universität Graz, 996-997
123 [4] [5]
[6] [7] [8] [9] [10]
[11]
[12]
[13]
[14] [15]
Litscher G, Schikora D (2002) Nahinfrarot-spektroskopische Untersuchungen zur Nadel und Laserakupunktur. AKU 30: 140-146 Litscher G, Schikora D (2003) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Internet J Neuromonitoring 3(2). URL: http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijnm/vol3n 1/nirs.xml Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Litscher G (2003) Lasernadelakupunktur - Eine neue nicht-invasive optische Akupunkturstimulationsmethode. Dt. Ztschr. f. Akupunktur 1: News Litscher G (2003) Laserneedle®-Akupunktur auf dem Prüfstand der Wissenschaft. Schweizerische Z f Ganzheitsmedizin 15: 253-259 Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Litscher G (2004) Effects of acupressure, manual acupuncture and Laserneedle® acupuncture on EEG bispectral index (BIS) and spectral edge frequency (SEF) in healthy volunteers. Europ J Anaesthesiol 21: 13-19 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laserneedles modulates brain function: First evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI). Lasers Med Sci 19: 6-11 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D (2004) Die schmerzfreie Lasernadelakupunktur moduliert die Gehirnaktivität: Erste Nachweise mit funktioneller transkranieller Dopplersonographie (fTCD) und funktionellem Magnetresonanzimaging (fMRI). Schmerz & Akupunktur 1: 4-11 Litscher G, Nemetz W, Smolle J, Schwarz G, Schikora D, Uranüs S (2004) Histologische Untersuchungen zu mikromorphologischen Einflüssen von Lasernadelstrahlung. Ergebnisse einer tierexperimentellen Untersuchung. Biomed Technik 49: 2-5 Litscher G, Schikora D (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Riga Rom Viernheim Wien Zagreb Litscher G, Wang L, Schikora D, Rachbauer D, Schwarz G, Schöpfer A, Ropele S, Huber E (2004) Biological effects of painless laserneedle acupuncture. Medical Acupuncture 16(1): 24-29
124
11. Increases in intracranial pressure and changes in blood flow velocity due to acupressure, needle and laserneedle acupuncture? G. Litscher, L. Wang, G. Schwarz, D. Schikora 11.1 Introduction Acupressure of points St.7 and SJ.22 can lead to significant, reversible ICPincreases in intensive care patients with a priori elevated intracranial pressure (ICP) [1]. Our study group already documented this in 1988. These increases in intracranial pressure due to acupressure can reach a threatening extent in isolated cases. Goal of this study was to evaluate whether stimulation of the acupoints mentioned above using different stimulation techniques, also leads to changes in cerebral parameters combined with alterations in ICP, in healthy volunteers.
11.2 Material and methods 11.2.1
Volunteers, patient, acupressure and procedure
We investigated a total of 34 healthy volunteers (24 females, 10 males) and a 15-year-old intensive care patient after severe head injury. The mean age of the volunteers (Cx r SD) was 25.2 r 3.4 years (range: 20 - 35 years). The test persons were informed about the study procedure and gave their written consent. A ten minute resting period on a bed prior to investigation was observed. During this time, the measurement device was applied. The study was approved by the local Ethical Committee at the Medical University in Graz. The following acupoints [2,3] were tested on each person, during three partial unilateral (right) measurements (Fig. 11.1):
125 St.7 (Xia Guan) Localisation: In front of the articular process of the mandible, below the zygomatic arch, in a depression, it can be located when the mouth is closed. Needling: Vertical, 5 fen - 1 cun. SJ.22 (He Liao) Localisation: Ventral and cranial from SJ.23, at the beginning of the auricle, at the back edge of the temporal hairline (behind the pulse point of the temporal superficial artery). Needling: Slanted, 2 - 3 fen.
St.7
SJ.22
Fig. 11.1: Laserneedle stimulation in a volunteer during simultaneous monitoring of blood flow velocity in the right and left middle cerebral artery and frontal near infrared spectroscopy parameters (acupuncture scheme according [3]).
We used acupressure, manual needle acupuncture and laserneedle acupuncture for stimulation in all of our test persons. In order to guarantee reliability and reproducibility of acupressure and acupuncture, the stimulation in all of our volunteers, was performed by the same Chinese expert for Traditional Chinese Medicine (TCM). The thumb pressure applied to the acupoints was ~ 3 x 10.5 Pa (force ~ 30 N) determined by force and area, whereby both points were stimulated intermittently during a total time of 5 minutes.
126 Manual needle acupuncture was performed with sterile one-use needles 30 x 30 mm (Huan Qiu; Suzhou; China). Needle stimulation was done in 2 minute intervals for 20 s and included a combination of rotating, pressing and thrusting motions. After a total of 5 minutes, the needles were removed. Laserneedle stimulation is based on a multi-channel system with 8 separate semi-conductor laser diodes and emissive wavelengths from 685 to 785 nm. The system consists of flexible optic fibres, which conduct laser light to the laserneedle without loss. Thereby, a high optical density at the distal laserneedle end is achieved. The intensity of the laserneedles is optimized in such a way, that the volunteer does not feel the activation of the needle (30 40 mW per needle; diameter 500 µm; time 5 min; energy density 1.2 kJ/cm² per acupoint). For more details regarding this method, see the previous studies [4-8]. The measurement procedure scheme is illustrated in Figure 11.2 and applies to all stimulation techniques. The time between the particular stimulation techniques was at least 10 minutes and the sequence of application was performed at random.
d
3 min
5 min
b 1 min
a 1 min
Fig. 11.2: Measurement profile of the volunteer study. The measurement points were determined before (b), during (d) and after (a) stimulation. The plateau increase indicates the “active time” of acupressure, needle- and laserneedle acupuncture.
11.2.2
Measurement techniques, statistical analysis
evaluation
parameters
and
A Multi-Dop T System (DWL Electronic Systems GmbH, Sipplingen, Germany) combined with functional multi-directional transcranial Doppler sonography (TCD) were used for measuring mean blood flow velocities.
127 Two 2-MHz-probes (A. cerebri media (MCA)) were used in an ultrasound probe-holding construction (compare Fig. 11.1). We evaluated the mean blood flow velocities (vm) in the right and left MCA as well as the pulsatility index (PI = (systolic maximum value – end diastolic maximum value)/mean value) in both cerebral vessels, before, during and after the different stimulation techniques. In addition, near infrared spectroscopy (NIRS) with an INVOS 5100 cerebral oximeter (Somanetics, Troy, USA) at the frontal left as well as right, and registration of blood pressure (Cardiocap, Datex, Hoevelaken, Netherlands) were performed. Measurement values were graphically presented as box-plots and were analysed with the paired t-test (level of significance p < 0.05). The computer programs SigmaStat and SigmaPlot (Jandel Scientific Corp., Erkrath, Germany) were used.
11.3 Results Figure 11.3 exemplarily shows the registration of ICP and blood pressure (A. radialis) during bilateral as well as unilateral acupressure in a 15-year-old patient with severe head injury. During acupressure, significant and steep increases in ICP occur, which first subside after terminating stimulation.
128
mmHg 50
kPa 6.7
ICP 40
5.3
150
20
80
11
BP 10 min
Fig. 11.3: Time course of intracranial pressure (ICP) and blood pressure (BP) during acupressure of points St.7 and SJ.22 in a 15-year-old patient after severe head injury. Direction of recordings from right to left (arrow). Observe the ICP increase during bilateral (b) and left (l) or right (r) acupressure.
Figures 11.4 and 11.5 summarize the results of transcranial Doppler sonography in healthy volunteers. The results show that significant increases in blood flow velocity in both MCA´s occur during acupressure (Fig. 11.4a). These effects remain present after completing acupressure. Inverse behaviour is shown in the pulsatility index (compare Fig. 11.5a). To a certain extent, significant and similar in trend, but somewhat damped amplitudes in the response pattern can be observed in manual needle (Fig. 11.4b, 11.5b) and laserneedle acupuncture (Fig. 11.4c, 11.5c).
129 p = 0.006
vm (cm/s) 100
p = 0.003
p < 0.001
p < 0.001
80
60
a
40
20
0
left
right
n=34
paired t-test
before
during
after before Acupressure
during
after
vm (cm/s) 120
p = 0.231 (n.s.) p < 0.001
100
p = 0.003 p < 0.001
80
b
60
40
20
0
left
right
n=34
paired t-test
before
vm (cm/s)
during
after before during Needle Acupuncture
p = 0.026
100
p = 0.061 (n.s.)
after
p = 0.015 p = 0.717 (n.s.)
80
c
60
40
20
0
left
right
n=34 before
paired t-test during after before during Laserneedle Acupuncture
after
Fig. 11.4: Box plot illustration of changes in mean blood flow velocity in the right and left middle cerebral artery (MCA) in 34 healthy volunteers, before, during and after acupressure (a), needle acupuncture (b) and laserneedle acupuncture (c). The horizontal line in the box gives the position of the median. The end of the box defines the 25th and 75th percentile; the error bars mark the 10th and 90th percentile.
130 p = 0.147 (n.s.)
PI
p = 0.007
1,8
p = 0.162 (n.s.)
1,6
p = 0.007 1,4 1,2
a
1,0 0,8 0,6 0,4
left
right
0,2 0,0
paired t-test
n=34 before
PI
during
after before Acupressure
during
after
p = 0.374 (n.s.)
1,6
p = 0.044 1,4
p = 0.231 (n.s.) 1,2
p = 0.003
1,0
b
0,8 0,6 0,4
left
right
0,2 0,0
n=34
paired t-test
before
during
after before during Needle Acupuncture
after
PI 1,6
p = 0.924 (n.s.) p = 0.498 (n.s.)
1,4
p = 0.219 (n.s.) p = 0.012
1,2 1,0
c
0,8 0,6 0,4
left
right
0,2 0,0
n=34 before
paired t-test during after before during Laserneedle Acupuncture
after
Fig. 11.5: Box plot illustration of changes in pulsatility index (PI) in the right and left middle cerebral artery before, during and after acupressure (a), needle acupuncture (b) and laserneedle acupuncture (c). For further description see Fig. 11.4.
131 Regional cerebral oxygen saturation and blood pressure did not show any significant stimulation-related changes (compare Tab. 11.1).
Tab. 11.1: Regional cerebral oxygen saturation (rSO2) and blood pressure (BP sys = systolic, BP dia = diastolic and MAP = mean arterial pressure). Mean values (Cx) and standard deviation (SD) under different test circumstances are noted.
11.4 Discussion Intracranial pressure is defined as the pressure which the brain within the skull (including the subarachnoid cavities), exerts on the surrounding dura mater. This is particularly important under pathological circumstances, since it influences cerebral perfusion as well as the oxygen and nutrient supply. An increasing ICP consecutively leads to a decrease in cerebral perfusion. If brain injury or damage by bleeding occurs, ICP can increase, however the surrounding bones cannot give way. This finally can lead to further damage of the brain reaching to transtentorial herniation or in extreme cases to brain death. Investigations using auditory evoked brainstem potentials in intensive care patients with increased intracranial pressure showed that the application of headphones alone, without activating acoustic stimulation can lead to significant, and upon removal, reversible ICP-increases [1,9]. The use of acupressure with similar pressing action, could also achieve these effects (compare Fig. 11.3). We assumed that the mechanical transmission of pressure from the headphones, or finger pressure on the end cranium as a result of loss of bone stability after skull fractures or after bi-temporal osteoclastic bone trepanation could be hypothetical potential causes. Further hypothesis were the triggering of reflex mechanisms during application of the headphone holder or finger pressure above the structures in the retro-mandible region or as a result of impaired venous blood flow [9].
132 An additive hypothetical approach which suggests a possible stimulation of local acupoints was also systematically investigated in this study using TCD. The effects of the individual stimulation techniques on regional cerebral oxygen saturation could not be proven with continuous NIRS monitoring. Non-invasive, intermittent blood pressure measurement on volunteers differs methodically from continuous invasive blood pressure registration in intensive care patients regarding reproducibility and time. The missing correlation between stimulation and blood pressure cannot exclude a possible accompanying brief systemic hemodynamic reaction resulting from the measurement window of the discontinuous measurement method. TCD has its origin in the year 1842 with the discovery and description of the Doppler effect by the Austrian physicist Christian Doppler. In the 80´s of the past century, Aaslid et al. [10] used the temporal acoustic window to overcome the barrier of cranial bones. As a result, TCD has become a noninvasive method for evaluating blood flow velocity in intracranial vessels. Cerebral blood flow parameters can either be determined mathematically from the blood or cerebral pressure (cerebral perfusion pressure – corresponds to the difference resulting from the mean arterial blood pressure and transcranial pressure) or with TCD (blood flow velocity). The close correlation between TCD parameters and intracranial pressure are discussed and proven in several studies. In this manner, systemic-theoretical approaches with simultaneous analysis of blood flow velocity and arterial blood pressure enable transformation to the cerebral pressure curve with a Dirac-impulse [11]. Clinical use of this non-invasive monitoring method is being currently discussed. The systemic-theoretical combination of the parameters described above is the foundation of our studies on healthy volunteers using TCD. It allows the direct and indirect connection of measurement data with transcranial pressure measurements, in intensive care patients. Hypothetically, we must consider the following components in our explanatory models: It is possible that acupressure, acupuncture and laserneedle acupuncture at the acupoints St.7 and SJ.22 induce changes in cerebral parameters, which can increase already elevated intracranial pressure in intensive care patients. They can also induce cerebral effects in healthy volunteers which are explainable by similar mechanisms. Thus, the attributes “gentle, alternative and free of side effects”, which are associated with TCM are not weakened inconsiderably. As the results from this study show, there are some signs of possible connections to side effects
133 which can occur under particular patho-physiological pre-conditions. In other words, it is obvious that also methods of TCM require exact diagnostics, determination of indication and selection of methods.
11.5 Acknowledgements The authors thank Ms. Ingrid Gaischek MSc for her valuable help and for writing the manuscript.
11.6 References [1]
[2] [3] [4] [5]
[6] [7] [8] [9] [10] [11]
Schwarz G, Pfurtscheller G, Tritthart H, List WF (1988) Hirndruckanstieg beim Monitoring akustisch evozierter Hirnstammpotentiale mittels Kopfhörer. Neurochirurgia (Stuttg) 31: 216-218 König G, Wancura I (1989) Neue chinesische Akupunktur. Lehrbuch und Atlas der Akupunktur-Punkte, 5. Auflage. Verlag Wilhelm Maudrich, Wien-München-Bern Hecker U, Steveling A, Peuker E, Kastner J (2001) Lehrbuch und Repetitorium Akupunktur. Hippokrates, Stuttgart Litscher G, Schikora D (2002) Cerebral effects of non-invasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laserneedles modulates brain function: First evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI). Lasers Med Sci 19: 6-11 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16/3-4: 335-342 Litscher G, Schikora D (Hrsg.) (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Bremen Litscher G, Wang L, Schikora D, Rachbauer D, Schwarz G, Schöpfer A, Ropele S, Huber E (2004) Biological effects of painless laserneedle acupuncture. Medical Acupuncture 16(1): 24-29 Schwarz G (1990) Dissoziierter Hirntod. Computergestützte Verfahren in Diagnostik und Dokumentation. Springer, Berlin Heidelberg New York Aaslid R, Markwalder TM, Nornes H (1982) Non-invasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg 57: 769-774 Schmidt B (2003) Nichtinvasive Erfassung des Hirndrucks mittels des transkraniellen Dopplersignals und der Blutdruckkurve unter
134 Verwendung systemtheoretischer Methoden. Dissertation, Technische Universität Chemnitz
135
12. Laserneedle acupuncture - clinical studies M. Weber 12.1 Introduction For the first time, laserneedles using a high optical energy output were applied at multiple points allowing painless and simultaneous 8-point treatment in accordance with traditional Chinese acupuncture. The laserneedles were developed by the German company Laserneedle® systems [1] and were first introduced at the Medica-fair 2000 in Germany (Fig. 12.1).
Fig. 12.1: Front view of the laserneedle instrument with 8 optical energy outputs.
The basis of laserneedle therapy combines the positive biological stimulation of tissues with laser rays, for analgesia, muscle relaxation, promotion of microcirculation and the stimulation of the immune system, with the traditional methods of classic acupuncture. In other words, simultaneous needling using an 8 point combination is performed. During the period of study 73 patients with various illnesses were treated. A prerequisite for taking part in this study was that all other forms of conventional treatment had been tried out, including medication, physiotherapy etc. without satisfaction or cure of the patient. To assess the success-rate, two scales
136 ranging from 0 - 100 were used. First the patients noted their level of contentment and secondly their individual pain-level.
12.2 Material, patients and methods Research was performed between January and May 2001 in a general practitioner’s office; the physician was certified in both body- and ear acupuncture. The patients treated were aged between 21 and 91 years. The majority of the patients treated had chronic or a strong tendency towards chronic illnesses, partly with acute or subacute symptoms. Approximately 70 % of the patients were female, 30 % male. For body acupuncture (Fig. 12.2), 8 exactly positioned laserneedles were used simultaneously. Optimum duration of treatment was 15 minutes. For ear- and skull-acupuncture (Fig. 12.3, Fig. 12.4), the laserneedles were exactly positioned by using a special headgear for fixation. The optimum duration of treatment in these cases was 5 minutes. The acupoints were located with common methods, such as the RAC-feeler and location with a 3 Volt-hammer by Bahr, or by applying simple pressure on pain sensitive areas. Corresponding points at the ear were also determined using the RACmethod or with a pointselect apparatus. In general we note that the triggering of a distinct, acupuncture-specific De-Qi sensation is an absolute must for effective acupuncture therapy [2-4].
Fig. 12.2: Typical examples of body acupuncture with activated laserneedles.
137
Fig. 12.3: Application of a laserneedle for ear acupuncture using a special headgear for fixation.
Fig. 12.4: Typical ear acupuncture treatment after activating the laserneedle device.
138 We could show that laserneedles invoked the characteristically pleasant DeQi sensation in 450 treatments (over 90 % of all cases treated) which was described as a gentle tingling and flowing of warmth into the extremities. After treatment, the patients felt pleasantly relaxed and slightly tired. In comparison to the classic metal needles, which we have been using for acupuncture in our office for the past 10 years, the frequency of De-Qi events was significantly higher. The De-Qi feeling was achieved in all patients regardless of their illness, it was more intensive in acute cases than in chronic cases. Often, the De-Qi feeling intensified during the course of treatment, indicating an increased sensitivity towards laserneedle therapy. It is interesting to note that De-Qi events were often reached in each patient according to a defined time schedule, for example after 10 minutes in body and 1 minute in ear acupuncture. In all of the cases treated no side effects were registered. Normal complications in conjunction with traditional metal needle acupuncture such as needle collapse, bleeding, hematoma, pain, infections etc. can be completely ruled out with laserneedle therapy. In particular the following illnesses from various fields of medicine were treated (Tab. 12.1): Orthopaedics spinal syndromes herniated vertebral disk gonarthrosis coxarthrosis rhizarthrosis periarthritis of the shoulder epicondylitis humeri radialis tendinitis fibromyalgia syndrome and polyarthritis Morbus Bechterew
Neurology/Psych. paresis after stroke migraine/headache syndrome trigeminal nerve neuralgia tinnitus depression psychovegetative exhaustion
Internal medicine gastropathy AVD bronchial asthma
Tab. 12.1: Summary of the treated illness in the different medical fields.
139
12.3 Results 12.3.1
Lumbar, thoracic and cervical spine syndromes as well as post cervical and lumbar intervertebral disk prolapse
We treated local pain trigger points as well as the corresponding near points (i.e. UB.10, 11 and 13 for cervical spine syndrome, or 50, 51 and 52 for lumbar spine syndrome) and the distant acupuncture points such as UB.60 and 62, in addition, the over regional pain trigger points such as SI.3, LI.4, SJ.5 and GB.41. In case of superimposed psychic symptoms, we also used compensating points such as St.36 and Ki.6 and in stress symptoms often Liv.3. Compared with metal needle acupuncture, pain relief set in immediately after the first treatment and could be increased in each following session by means of the booster effect. Therefore, pain syndromes could be completely relieved after about 5 sessions. With simultaneous treatment of musclerelaxing and calming down points it was evident that a quick sedative, frightand stress-relieving reaction in patients was achieved. In a usual series of 10 treatment sessions, the results can be described as being exceptionally good. A large number of patients were completely free of pain or their pain was reduced to such an extent that their original quality of life returned. We could note that significant improvements in all therapy-resistant and therapied patients, particularly in those with chronic spinal problems took place. Older people achieved a higher mobility in the affected joints and enjoyed far less pain. Apparently the simultaneous effect of laser rays used in combination with the rules of classic acupuncture were responsible for this success. In most cases, analgesic and antirheumatic medication, such as ibuprofen, diclofenac or tramadol and even morphine pain killers could be either greatly reduced or completely terminated. Case example A 58-year-old female patient suffered a severe prolapse of the L5/S1 disks in December 2000 and was treated in a hospital for 4 weeks. She was discharged with therapy resistant acute pain, even after CT guided local injections and being placed on a maximum of pain medication. Further ambulatory treatment was ineffective. She was treated with laserneedles using the following point combination: UB.34, 36, 37, 40, 60 and 62 as well as St.36 and Du 2. After a few minutes, an intensive De-Qi sensation was built up during each session, and was described as a pleasant, warm tingling feeling flowing into the entire leg. After the 15-minute treatment period, pain was significantly reduced and
140 improvement in leg mobility was achieved. After 3 further sessions, the patient was able to go to parties and dance again. After 10 more sessions, only 10 % of the initial symptoms remained so that she went on holiday. Throughout treatment all pain relieving medication was gradually reduced and at the end of the therapy stopped. After 4 months this magnificent result remained unchanged. The individual pain score after the end of treatment was 20 %; the patient’s subjective satisfaction was 95 %.
12.3.2
Gonarthrosis, coxarthrosis, rhizarthrosis, periarthritis in the shoulder, epicondylitis, tendinitis, Morbus Bechterew and fibromyalgia-syndrome
Significant results were achieved after only 3 - 5 treatment sessions in the disorders mentioned above. Remarkable was the very high success rate for chronic epicondylitis during the initial phase of treatment. This illness is widespread in the general population and difficult to treat. After only a few sessions using local pain trigger points and further typical points such as SJ.5, LI.4, 11 and 12 and often additional treatment of neck rigidity with SJ.15 and cervical vertebrate points such as UB.10, the patients were able to go about their normal activities, take part in sports and other hobbies. Even chronic and impairing rhizarthrosis, which is intermittently treated with crystal-steroids, responded very well to lasering. We frequently included the corresponding local regional, local and distant trigger points (among others LI.1, 4, 5, Lu.9 and 10 as well as Pe.7). These types of disorders were also treated by the so-called TMM system (tendomuscular meridians), by additional needling of the ting- and tonus points and the equivalent reunion zones. This proved to be very useful and provides further evidence regarding the benefits of laserneedling. It is also interesting to note, that severe disorders like Morbus Bechterew and fibromyalgia, as well as chronic polyarthritis responded exceptionally well to treatment with laserneedles. In cases of year long impairment, great importance was attributed to the additional treatment of relaxing, sedating, stress relieving and energy stabilizing trigger points such as St.36, Ki.6, Ren 17, UB.60 and 62, SJ.5, GB.41, Lu.7, Liv.3 or Du 20, to compensate the psychological and depressive symptoms. We could prove that it is more effective to treat multiple points than to stimulate only single local pain points. This is particularly difficult in cases of fibromyalgia, where pain occurs throughout the entire body and constantly changes its location. The psychological background, especially in
141 fibromyalgia as well as polyarthritis is widely acknowledged and proven, thus, we have an initial point for a stabilizing treatment. In periarthritis of the shoulder, a long and impairing illness, the success rate of treatment was significant and effects were of long duration. Case example A 54-year-old male patient, suffering from Morbus Bechterew for over 20 years with partial stiffness of the lumbar vertebrae was treated with the following point combination: UB.31, 32 and 62, Du 2, Ki.6, St.36, Sp.6 and SI.3. During treatment a repeated intensive De-Qi occurred in the lumbar region and after about 10 minutes a pleasant feeling in both legs took place immediately after the first and each successive treatment. The patient was able to tie his shoelaces for the first time in years. Apparently due to relaxation of the painful muscle, the toe touching distance had improved by about 20 cm. The extreme pain described before treatment disappeared immediately, however recurred after some time, but not to the same extent as originally. The psychological condition and depressed mood as well as the sleeping disorders were greatly improved. After an observation period of 3 months the patient was without pain and could go about his hobbies and carefully increase his physical condition. The individual pain score at the end of treatment was 10 % and 100 % for the patient’s subjective well being.
12.3.3
Remaining paresis after stroke
Three patients who had suffered strokes with remaining paresis were treated in the regions of the affected extremities. A blood-flow increasing and muscle relaxing point combination was used with energy stabilizing points. In all 3 cases, a significant increase in mobility was achieved by reducing spasticity and improving the fine motor ability. Case example A 78-year-old female patient with painful, remaining paresis in her left arm was treated using the following point combination: LI.4 and 11, SI.3, Pe.6, SJ.5 and 15, Du 20 and St.36.
142 The elevation of her arm could be improved from 90 to 120 degrees after only 5 sessions. The patient was able to pull a dress over her head for the first time in 5 years. Pain reduction was achieved and fine motor ability was greatly improved. The subjective patient satisfaction was 90 %.
12.3.4
Cephalgia, migraine and trigeminal neuralgia
The necessary requirement prior to treating chronic headaches includes extensive neurological and radiological patient examination. In these indications we used local and distant trigger points. Migraine attacks could be rapidly reduced and after due course of treatment, stopped completely. Tension headaches could be treated quickly. Three patients suffering from tinnitus were treated. The results here were not as impressive as in other disorders; often the tone/noise symptoms could be reduced and sometimes stopped completely for a short time. Further longterm studies still need to be evaluated. Long-standing trigeminal nerve neuralgias were successfully treated after only 5 sessions and have not recurred to date. Employing laserneedles to the head proved to be absolutely easy, considering the location and application required. Case example A 53-year-old male patient suffering from right branch trigeminal neuralgia for over 20 years was treated with 400 mg of carbamazepin, then laserneedled with the following point combination: LI.4, SI.3, St.4, 5, 6, 36 and 44 including Ren 24. After the first session, a significant improvement was felt in the extremely painful right mouth-lip-area. After 3 further sessions no pain could be registered and carbamazepin was gradually reduced. In the following 2-month observation period, the patient remained free of pain for the first time in a decade. The pain score was rated with 0 - 5 %. The subjective patient satisfaction was 100 % in this case.
143 12.3.5
Arterial obstruction disease
Case example A patient with a persisting 10-year obstruction of the pelvis and a circulatory bypass could not be operated due to cardiac problems. After only 5 treatment sessions, his walking distance could be increased from 100 m to over 2000 m and he was free of pain. The following point combination was used: UB.40, 58 and 60, St.36 and 41, Liv.3, Ki.6, Sp.6. Obviously treatment led to an improvement in microcirculation and additional muscle relaxing effects. The subjective satisfaction was given at 95 %.
12.3.6
Gastropathy and bronchial asthma
In most cases, we are dealing with psychovegetative and other disorders, thus, a combination of organ related trigger points with sedating and stress relieving effects were of importance. In both diseases the patients’ health greatly improved after the first session. Case example A patient with a long-standing case history and diagnosis of nervous stomach was treated with the following combination of points: Pe.6, Sp.4, SI.3, Liv.3, St.36, Yintang, Ren 12 and UB.21. After a few sessions, nausea, vomiting, feeling bloated and nervous restlessness and dizziness vanished completely. The subjective satisfaction of the patient was 100 % and a 95 % symptom reduction was achieved.
12.3.7
Depression, exhaustion
anxiety,
panic
attacks,
psychovegetative
Spectacular results were achieved with laserneedles in the treatment of psychic and psychosomatic illnesses. The general practitioner’s experience shows that a large number of somatic related disorders are linked to depression. In these cases, treatment is extremely difficult and often leads to the prescription of addicting medication or psychotropic drugs. Especially younger patients frequently refuse these drugs.
144 Disorders such as burnout and exhaustion syndromes in conjunction with anxiety and panic attacks and depressive tendencies are extremely well treatable and show quick results. In general, psychotropic drugs could be stopped after only a few sessions. The same was true for pain relieving drugs in orthopaedic disorders. Patients who had been treated with sedating and anti depressive points were able to sleep better after only a few sessions. Their family life improved greatly. Laserneedle acupuncture considerably reduced illness-related absence from work. Case example A 35-year-old manager of a big company with stress-related exhaustion syndromes introduced herself to the practice. She suffered from anxiety, restlessness, sleep disturbances, headaches and sometimes vertigo. She was treated with the following combination: He.9 and 7, Lu.7, UB.62, Yintang, Liv.3, Du 20 and Ki.6. During the first session a soothing warmth flowing through the whole body was sensed, she felt very relaxed and deeply tired, which in turn led to a good night’s sleep. After only 3 sessions the patient was able to resume her high-pressure job. The patient’s subjective satisfaction was 100 %; the symptoms could be reduced by 90 %.
12.4 Discussion In this report, more than 500 acupuncture treatments were performed with the newly developed laserneedles. Limitations were reduced by using up to 8 stimulation points simultaneously on the body or ear so that all the principle point combinations, either local, loco-regional and distant acupuncture points could be activated with the laserneedles. Treatment did not have any side effects, was extremely patient orientated, pleasant and highly effective in all indications. During the study, the number of patients asking for laserneedle treatment increased considerably. Because treatment is more pleasant for the patient, no needle pricking is necessary, and better results are achieved with laserneedles, acceptance is greater. Our experience showed large groups of patients are willing to use the laserneedle method. The advantages of laserneedle treatment in pediatrics are also obvious: painlessness and the higher rate of achieved De-Qi sensations. When we consider the economical point of view, treatment costs were considerably lower due to the reduction of required treatments, thus,
145 expensive pain therapies, psychotherapy and physiotherapy became obsolete. Patients being incapable of working due to orthopaedic, psychiatric and psychosomatic disorders could also be significantly reduced. We would like to note the frequency of chronic spinal problems, which lead to great financial losses in our economy each year. Using this new laserneedle acupuncture technology, we could reduce therapy resistant complaints, especially in older patients, so that prescription of non-steroid antirheumatics could be reduced respectively. Therefore unwanted side effects such as ulcers, gastrointestinal bleeding, liver and kidney damage do not occur. The special effects laserneedle treatment has on psychiatric and psychosomatic disorders in connection with anxiety and panic disturbances should not be neglected and is also of considerable importance. These disturbances always lead to difficulties for the general practitioner because they often become chronic, are very time consuming to treat, medication therapy may be restricted and all in all are extremely difficult to treat. Patients who experience difficult phases in their lives - adolescence, mid-life crisis, senile depression, psychological exhaustion and burnout syndrome can be treated easily and successfully. These patients, who often have consulted many specialists in their ordeal, accepted laserneedle treatment exceptionally well. By presenting a new strategy they feel that their problems are being taken seriously. Naturally we suggest that acupuncture with the new laserneedle technology can only be part of a treatment concept. Before treatment is done, thorough examination and diagnosis of each patient must take place. In conclusion, acupuncture treatment with the new laserneedle technology in the general practitioner’s office is superior to the classic metal needle acupuncture methods. We must consider the therapeutical results and effects, the duration and effectiveness after treatment and the frequency of treatment. Lastly we would like to mention that remarkable results were achieved with laserneedles in fields beyond normal usage of acupuncture. Dermatological illnesses, such as crucial ulcers, chronic eczema and acute inflammation of the skin and mucous membranes etc. were treated with great success. We will report on these findings at a later date.
12.5 References [1]
Laserneedle systems GmbH (2001) Benutzerhandbuch Akupunkturtherapie mit Lasernadeln. http://www.laserneedle.de
zur
146 [2] [3] [4]
Kersken T (1993) Einschätzung der handwerklichen Qualität durchgeführter Akupunkturtherapie in 86 Studien. In: Bühring M, Kemper F (Eds.) (1993) Naturheilverfahren. Springer, Berlin Stux G, Stiller N, Pomeranz B (1993) Akupunktur. Lehrbuch und Atlas. Springer, Berlin Ter Riet G, Kleijnen J, Knipschild P (1990) Acupuncture and chronic pain: a criteria-based meta-analysis. J Clin Epidemiol 43/11: 11911199
147
13. Pain therapy with laserneedle acupuncture R. Helling 13.1 Introduction The cases described in this chapter do not have the same value of an actual study, however, clearly show the therapeutic effects of non-invasive laserneedle acupuncture. The cases described, were solely treated with laserneedle acupuncture.
13.2 Case reports A 48-year old female with idiopathic trigeminal neuralgia of the left second branch was treated. A specialist ruled out differential diagnostically important causes such as cranio-mandibular dysfunction, maxillary sinusitis, or post zoster neuralgia. No odontogenous disturbances were evident. Drug therapy with Carbamacepin and Baclofen® led to insignificant pain reduction, therapeutic and local anaesthetic blocks of the pterygopalatine ganglion, as well as stellate blocks only achieved pain reduction for about 2 days. Despite massive pain, the patient was not willing to undergo surgical treatment with micro vascular decompression according to Janetta´s method. Laserneedle acupuncture was performed according to standard rules of acupuncture (see Fig. 13.1). The following acupuncture points were used: contra lateral St.2 – St.4 – SJ.21 bilateral LI.4 ipsilateral St.44 and Liv.3
148
Fig. 13.1: Acupuncture points used (modified from [1]).
13.3 Argumentation In case of highly painful local processes, local points on contra lateral sides are usually selected (St.2 – St.4 – SJ.21 ), in addition to distal points ipsi- or bilateral: LI.4: LI.4 is the so-called reference point for the large intestine meridian. This is the most important distant acupuncture point for pain in the facial
149 region. According to studies by Heine, somato-sensory afferents of LI.4 at the segment level of C4/C5 to Th1/2 are switched synaptically to the sensory neurons of the dorsal horns of the spinal cord. Thus, LI.4 has control action on all afferents and efferents running through the spinal cord. Because of the unique relationship of point LI.4 to the spinal cord, acupuncture of this point not only switches the afferents at the dorsal horns cord to the bulbo-spinal and spino-thalamic tracts, but connects the spinal nucleus of the trigeminal nerve and sympathetic cilio-spinal center via interneurons in the spinal cord. Both nuclear zones reach from rostral to the lower brain stem. Here, the connection to the principle nucleus of the trigeminal nerve takes place. According to Traditional Chinese Medicine (TCM) LI.4 frees the surface from external pathogenic factors (such as wind). TCM considers trigeminal neuralgia and facial paresis to be wind diseases. Liv.3: is the reference point of the liver meridian. Combined with LI.4, this point drives the wind out of the face [2,3]. St.44 as second to last point of the stomach meridian excellently influences the other end of the meridian, which begins at the face. St.44 is often used for pain in the face, which according to TCM is triggered by climatic factors. Because of severe pain, therapy with laserneedle acupuncture was performed daily for 20 minutes during the first week. In the second week, three acupuncture sessions (each lasting 20 minutes) were performed, in the third week only 2 sessions were made. According to the patient, pain reduction of about 50 % was achieved after the third therapy session. After the eighth session, the patient was free of pain; the last two points were only performed to stabilize the therapeutic effect. During the last 2 sessions, only the distant points LI.4 – Liv.3 – St.44 were still treated with laserneedle - acupuncture, the contralateral points at the face (St.2 – St.4 – SJ.21 ) were no longer treated. During the following observation period of 8 weeks, the patient was completely free of symptoms. This is particularly notable, since the patient only had one pain free interval for two to three days in the past seven years. A 35-year-old female patient with intercostal neuralgia, underwent unexplainable left-sided rhizotomy of the sensory and motory root from Th7 to Th11 (malpractice process is currently running). Rhizotomy did not lead to lindering pain; instead, permanent pain resulted, including the zone where surgery was performed and extending under the left thorax to the left pectoral region. Only high doses of Tramal® and Novalgin® led to pain
150 reduction of about 30 %. Opiates did not show any effects, local anaesthetic, paravertebral blocks caused additional pain. In the paravertebral surgical region, treatment with laserneedle acupuncture at six highly tender points, in the region of the surgical scar, was performed. The therapy zones were not selected according to the localisation of known acupuncture points, but based on so-called A-Shi- points (tenderpoints). According to TCM all points were located along the so-called Hua Tuo – Line (one transverse finger paravertebral). Treatment was performed once a week for 20 minutes. The weekly therapy interval exists since 4 months and is still being performed currently. After being completely free of pain for one week, massive pain of the previous intensity builds up within 24 hours. Since all therapeutic methods performed by several specialists were unable to achieve the effect of laserneedle acupuncture, the patient has decided to buy her own therapy device. According to the patient, she can achieve pain free intervals lasting one week, with this painless therapy method and can live well this way.
13.4 Discussion The two cases described here do not fulfil the criteria of a study. However, they impressively show the effectiveness of laserneedle acupuncture in two therapy resistant pain disorders. Independent from the effectiveness of laserneedle acupuncture, the author finds it very important to select the acupuncture points according to the following three criteria, especially when treating pain disorders: 1. The so-called intrinsic value of the acupuncture point must correspond with the demands. 2. The combination of acupuncture points must be additive regarding their effect. 3. The effect of acupuncture points must reach the localisation of pain (goal area) [3].
151
13.5 References [1] [2] [3]
Jiangping L, Yanliang C, Renhua S (1990) Chinese acupuncture and moxibustion. Publishing House of Shanghai College of Traditional Chinese Medicine, Shanghai Deadman P (1998) Großes Handbuch der Akupunktur. Verlag für Ganzheitliche Medizin, Kötzting Maciocia G (1994) Die Grundlagen der Chinesischen Medizin. Verlag für Traditionelle Chinesische Medizin, Kötzting
152
14. Pain therapy of osteoarthrosis / osteoarthritis-patients using the laserneedle system in a medical practice with emphasis on rheumatology and pain therapy K. Kolitsch 14.1 Introduction The largest joint of the body is the knee joint. Practically no other joint has to endure greater daily stress. Complex rolling and sliding movements guarantee high flexibility as well as stability. The required flexible connection between different bones is guaranteed by the perfect cooperation of muscles, tendons and ligaments. The knee joint consists of the articular condyle and articular cavity, and is surrounded by the synovial capsule – these establish the mobile connection between the upper and lower leg. Stabilisation of the joint is secured on the side with ligaments, the meniscus acts as shock absorbers. The synovioum, combined with synovial fluid and articular cartilage provide optimum slidability. In case of arthrosis, the articular cartilage is worn down, and in advanced stages, severe pain occurs, due to friction between the bones.
14.2 Patients and method Wear and tear of the knee joint reduces the quality of life for those who are affected. Especially these patients can be found in a medical practice with emphasis on rheumatology and pain therapy. The number of patients suffering from osteoarthritis of inflammatory, as well as generative genesis shows increasing tendency. The knee joint is the clinically the most often affected joint. The changed structure of aging in the population is responsible for this phenomenon. Today we assume that every arthrosis causes accompanying symptoms of arthritis. On the other hand, arthritis leads to the triggering of arthrosis. Due to severe pain resulting from advanced loss of articular cartilage, affected patients are nearly immobile. Only few therapies seem to be promising regarding stopping or slowing the further degeneration of articular cartilage. Exactly these patients – clients develop chronified pain symptoms or a chronic pain illness.
153 Practical studies show that a dramatic deficit in caring for patients with chronic pain exists. 75 % of osteoarthrosis/osteoarthritis patients are treated by a general practitioner. About 60 % do not receive adequate pain therapy. Effective pain treatment is still a foreign word for many older osteoarthrosis/ osteoarthritis patients. An untenable condition which risks the development of a pain career. Frequent change in physicians, alternative methods without competency and irregular medication are the result. In particular, modern pain therapy methods offer a multi-modal pain therapy concept for patients with chronic pain diseases. The qualified combination of drug and non-drug treatment, in connection with psychotherapeutic strategies, leads to an optimum of therapeutic results. Most important goal of treatment is the mobilisation of patients with chronic pain diseases. Goal is a variety of physical straining of the affected knee joint without repeated, one-sided movement. Stressing of the knee joint should be avoided which doesn´t follow the natural movement patters of this joint. In particular, torsional movements should be regarded as dangerous for the knee joint. Modern pain therapy offers patients a number of options within the multimodal treatment concept. Animated by the effectiveness of laserneedle therapy compared to needle acupuncture, we performed a laser therapy on 150 patients with osteoarthrosis/osteoarthritis. Drug or pain therapy remained unchanged. The patient collective included patients with osteoarthrosis/osteoarthritis stage I and II. The technical and scientific basis of the laserneedle system were thoroughly described by Litscher and Schikora [1-3]. Within observational use of the laserneedle system in pain therapy, prescription laser acupuncture was used. The following acupuncture and extra points were applied on 150 osteoarthrosis/osteoarthritis patients: Extra points: Nu Xi Jan Xiyan (Ex.32) Heding (Ex.31) Acupuncture points: St.34 GB.43 Sp.10
St.35 Sp.9
Figure 14.1 shows a patient undergoing laserneedle treatment.
154
Fig. 14.1: Laserneedle treatment in Dr. Kolitsch´s medical practice
Duration of laserneedle therapy was 20 minutes. All patients wrote a pain diary from STK (Schmerztherapeutisches Kolloquium) as pain therapy control. The first follow-up was made after completing therapy, the second, 4 weeks later.
14.3 Results Evaluation of the treatment data after completing therapy showed pain reduction of three graduation marks on the VAS (visual analog scale) in 65 % of the osteoarthrosis/osteoarthritis patients. After follow-up 4 weeks after completing therapy the result improved to 70 %. 70 % of the patients registered a reduction pain of 3 graduation marks on the VAS. 15 % of the osteoarthrosis/osteoarthritis patients showed a decrease in pain of 2 graduation marks on the VAS.
14.4 Discussion Evidence regarding efficiency is provided by the drug-free treatment with the laserneedle system within a multimodal pain therapy concept under remaining basis and or pain treatment (WHO – graduated scheme). As a result of reduced pain intensity, an increase in mobility in chronic pain patients was achieved with laserneedle therapy. Thereby this therapeutic option achieves measurable improvement in the quality of life. Long-term observations regarding the long-time effects of laserneedle therapy will provide further effective data regarding the efficiency of this therapy.
155
14.5 References [1] [2] [3]
Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342
156
15. Laserneedles in gynecology K. Staehler van Amerongen 15.1 Introduction The laserneedle technique is a new, non-invasive method to stimulate specific acupuncture points with laser light. The method and clinical effects are described in more recent scientific literature >1@. Unlike metal needles used in common acupuncture which are inserted into the skin, Laserneedles are adhered to the desired acupoints points using small adapters and a special adhesive technique.
Fig. 15.1: Laserneedles.
After activating the device, continuous, visible red laser light with a wavelength of 685 nm is applied via an optic fiber, directly to the acupoint with the laserneedle. Intensity of the laserneedle is optimized in such a way, that the patient barely feels the activation, however still builds up vegetative stimulation at the acupuncture point. It has been documented, that laserneedles at the acupoint trigger particular stimuli that is identical to the Qi sensation of metal needles. The device has 8 exits with corresponding cables. Therefore, laserneedle acupuncture makes the simultaneous stimulation of individual point combinations possible. As a result, all combinations of body, head, and ear acupuncture application are possible. Laserneedles can be applied alone or in combination with additional traditional acupuncture needles. The acupoint is stimulated by the continuous photon flow from the laserneedle. After subtraction of scattering losses, about 40 mW optic output is achieved at the distal end of the laserneedle. The actual dose per laserneedle at the skin during acupuncture treatment is 40 – 60 J >5@. The
157 power density of a laserneedle increases with the duration of treatment >2@. Absorption in tissue is minimal at this wavelength; therefore, no warming or burning of tissue as by surgical lasers occurs. The power of the laser light leads to triggering of action potentials >4@. Continuous stimulation generates a cascade of action potentials at the acupoint.
15.2 Material, test persons, technique The investigations took place during the time period between March and October 2003. Three-hundred women between 30 and 56 years were evaluated. All patients were treated during the acupuncture consultation hours at the University gynecological clinic. Different clinical pictures from the fields of gynecology and obstetrics were treated. In most cases, single body laserneedle treatment was performed. In 40 patients, additional application of laserneedles in the ear region was done. The clinical pictures treated included 265 gynecological patients and 35 obstetric patients. The gynecological clinical pictures included menstrual problems, cycle regulation, dysmenorrheal problems, hypothalamic amenorrhea, premenstrual bleeding, premenstrual and menstrual migraine headaches, back pain during menstruation, exhaustion, burn-out, hot flushes and flush during menopause, sterility and childlessness, bladder disorders, dysuria, uro-genital symptoms, and in the oncologic field, shoulder tension after breast surgery, tension and decreased arm mobility after breast surgery. Obstetric indications were induction of labor, carpal tunnel syndrome, hyper emesis and laser application during childbirth process. Selection of acupoints on the body was done using the common traditional Chinese medicine technique and according to the pressure sensitivity of the acupoints. Ear points were partially determined with RAC-touching or with the electric Pointselector. Laserneedles were activated at the acupoints for an average of 30 minutes. Since this method is still quite new, no well-founded results can be presented due to the small number of case studies.
158
15.3 Case studies 15.3.1
Induction of labor with laserneedles
A 23-year-old patient in the 40th week of gestation, after normal course of pregnancy came to the ambulant consultation hour for acupuncture to induce labor. It was her second pregnancy. The first child was a spontaneous delivery on the awaited date of birth, 2 years earlier. Now the belly was quiet and no signs of labor were present. The child was also quiet at the beginning of treatment. The vaginal examination showed an immature finding with closed sacral mouth of the uterus. The cervix was maintained and scirrhous. The patient wanted a „natural“ induction of labor without medication. Up until this time, no measures to induce labor had been performed. After comprehensive explanation of the different possibilities, the patient decided to induce labor with laserneedles at the usual acupoints. For her, the fact that laserneedles did not cause pain was significant since she knew that acupuncture with metal needles causes some pain during insertion. At the beginning of treatment, she was positioned in a relaxed, comfortable manner on the left side. Laserneedles were applied at points LI.4, St.36, GB.34 and Liv.3 with special adhesive tape.
Fig. 15.2: Induction of labor at points LI.4, St.36, GB.34 and Liv.3.
These are the common acupoints for inducing labor. Especially LI.4 (Fig. 15.3) is an important point to stimulate labor.
159
Fig. 15.3: Laserneedle-stimulation at LI.4.
Laser emission was activated simultaneously and continuously for 30 minutes at these 8 acupoints. During treatment, the patient could feel an increase in fetal movements and a minor cramping in the belly. Towards the end of treatment, her belly was hard four times. At point LI.4 she felt the most tingling. All in all, she felt well and relaxed. After completing laser application, the cramping in the belly stopped for the time being. She returned home on that afternoon. During the night she had to go to the hospital due to beginning labor. The first stage of labor in which the mouth of the uterus opens only lasted 3 hours. The second phase only lasted 20 minutes and 4 bearing-down pains. The entire birth took 3 ½ hours which was very fast. In addition, she said she felt very well and was very relaxed. She had enough energy to bear the child and said she perceived delivery as a very nice experience. In this case, the patient delivered quickly and comfortably. Remarkable was the short first phase of labor lasting only 3 hours. The literature describes that emotional and physical stress for mother and child has a clear influence on the length of childbirth. An „allowable duration of childbirth“ in plurpara patients is usually 8 hours during the first phase, 1 hour during the second phase and half an hour for bearing down. Altogether childbirth takes 9 ½ hours >3@. In our patient, childbirth only took 3 ½ hours. If this was due to the influence of the laserneedles or if she would have delivered so well without this measure remains a speculation. Noteworthy is the quick begin of labor after laserneedle treatment, the brief first phase of childbirth and the subjectively good feeling of having enough energy to achieve childbirth easily.
160 15.3.2
Carpal tunnel syndrome
A 22-year-old mother with a 2-year-old child came to my consultation hour in the 28th week of pregnancy. I knew her from her first pregnancy as she had severe pain and edema in both hands and I treated her for carpal tunnel syndrome with acupuncture. The current pregnancy was a twin pregnancy and she had the same symptoms with tingling in the hands especially at night. She complained about severe pain and weakness in the fingers so that she could barely pick up a cup from the table. Her hands were severely edematous. The severity of the symptoms was worse in this pregnancy than in the last. In the last pregnancy, she was treated with acupuncture needles at the acupoints Pe.6 and Pe.7.
Fig. 15.4: Needle acupuncture at points Pe.6 and Pe.7.
At that time, the symptoms increased after the first treatment, but improved distinctly after the third treatment. Eight sittings using common acupuncture with metal needles were performed, first 3 times a week, then once a week. The patient experienced slight pain during needling. After appropriate explanation, the patient wanted to try acupuncture with laserneedles. Again the same two acupoints Pe.6 and Pe.7 at the inside of the wrist were selected. The laserneedles were applied at these points and illuminated with laser light for 30 minutes. Coincidently, 8 sittings were
161 necessary again. After the first treatment, again, an increase in symptoms occurred. First the pain increased however after the second treatment she could feel an obvious improvement in her symptoms. It was a positive effect for her that the fixing of the needles with adhesive tape did not cause pain, contrary to the insertion of common acupuncture needles. During laserneedle acupuncture, she felt a warming sensation. She described this as comfortable and felt better being able to move her hands slightly during treatment without moving the needles. This small freedom of movement compared to common acupuncture was positive for her. The children were quite quiet during treatment. There were no signs of labor. Cardiotocogram (CTG) registration, twice during and twice immediately after treatment, showed normal heart action in both children and no signs of labor. The carpal tunnel syndrome symptoms improved distinctly. In the 35th week of pregnancy childbirth was performed with Caesarean section.
15.3.3
Urogenital symptoms, back pain, hot flushes
A 52-year-old patient was treated with common acupuncture against her year-long symptoms. She reported a constant feeling of pressure on the bladder coming from the bladder region. Because of nycturia she had to get out of bed 2 to 3 times per night, and during the day she had to go to the toilet every hour. She could hold her urine and did not have episodes of incontinence. She experienced the constant back pain in the lumbar region as the worst symptom and had to take 2 - 4 Voltaren 50 mg per day. Walking was strenuous and she could not carry much. Despite physiotherapy and bladder training, no success could be achieved. Blood pressure was stable with medication at 120/85 mmHg. Before treatment, the patient rated her pain with 8 on a 10 point pain scale. After extensive diagnostics, the patient was treated with common acupuncture using metal needles and combined body and ear acupuncture. The acupoints UB.28, 29, 30, 40 as well as Du 20 and Ren 3 on the body and the acupoints lumbar spine, hip and bladder at the ear were selected for acupuncture. The needles remained in place for 30 minutes without stimulation. After 9 treatments with common metal needles her condition improved distinctly. She rated her pain with 3 on the pain scale and did not require any pain medication. Her blood pressure was still stable and she felt subjectively better than before acupuncture. As she heard about the new laserneedle device, she wanted to try it out. The laserneedles were applied at UB.28, 29, 30, 40 on both sides for 30 minutes. After a few minutes, the typical Qi sensation occurred during the two sittings we performed. She said that she felt a comfortable tingling sensation, which spread throughout the entire body. She rated the back trouble with 1 - 2 on the pain scale. After laserneedle treatment, she felt a direct and distinct
162 improvement in her back pain. However, her blood pressure showed diastolic peaks of 95 to 100 mmHg and she complained about extreme hot flushes. This case was mentioned in particular to attract attention to possible disadvantages of this method. I can only speculate, whether these circulatory disturbances have a direct connection to the laserneedles. My observances have indicated that the use of laserneedles in diseases with too much fullness or conditions, which are strongly influenced by the sympathicus require more caution. In particular, I noticed that hot flushes increased. I also observed this phenomenon in patients during the menopause or in oncologic patients treated with Zoladex. It is conceivable that the additional energy input, which is achieved with the laser method, can bring a system that is “too full” to “boil over”. Further controlled studies are definitely necessary to confirm this statement.
15.3.4
Breast cancer with mastectomy, transmission in scars
A 40-year-old patient had breast cancer surgery on the left two years earlier. Because of the tumor stage, a radical mastectomy and axillary lymphadenectomy had to be performed. Histology showed an invasive ductal breast cancer stage with neoplastic angiolysis and metastases in lymph nodes, estrogen and progesterone receptor positive. Thereafter, she had 6 cycles of chemotherapy as well as a anti-estrogen therapy with Tamoxifen and Zoladex. Her problem was a frozen shoulder on the left which severely restricted the mobility of her arm. The skeletal scintigraphy and CT did not reveal any metastasis. Arm movement was restricted and only sideward movement to < 45° and towards the front to < 90° was possible. Shoulder pain caused by tense muscles was rated with 7 on a 10 point pain scale. She had achieved little improvement with physical therapy exercises. In a sitting position, the patient was treated with laserneedles on both sides at the body acupoints LI.14, SJ.15, GB.21, SI.11.
163
Fig. 15.5: Laserneedle treatment at acupoints LI.14, SJ.15, GB.21 and SI.11.
The acupoints were illuminated continuously with 30 mW laser light for 30 minutes. Eight 8 sittings at 1 - 2 week intervals were performed. After this treatment interval, an obvious improvement in arm movement to < 150° to the front and < 110° sideward was achieved. She could also reach the back of her left shoulder with her left arm, a movement that was impossible before. She described her emotional and physical condition as much better and stable since laserneedle treatment. She also had more energy and was not as tired. Solely the heat sensation within the body and sweating had increased somewhat. Interestingly she describes the transmission of the laser energy directly to the scars. The needles were adhered on the back and rear shoulder region. About 5 minutes after activating the device, she felt a tingling sensation at the mastectomy scar and axillary scar. After two further minutes, she described a strange sensation in all scars on her body, even at the scar on her right knee from an old injury. The scar on the knee was located somewhat lateral from the stomach meridian. As we know, the stomach meridian runs directly over the breast. Interestingly, the scar on the knee was on the right side, the mastectomy scar on the left side of the body. Whether energy from laserneedles flows further and is stopped at scars and how far scars can be influenced with laserneedles should be discussed. According to the interference field theory, scars are very important focuses were energy is disturbed. Further studies to this topic should follow.
164 15.3.5
Dysmenorrhoea, lack of energy
A 45-year-old patient came to the consultation hour and suffered from severe pain in the lower abdomen during menstruation. Endometriosis AFS III was documented in her medical records and she had several operations because of endometriosis in the past. Dysmenorrhea was so severe, that she had to go to the hospital for treatment with strong painkillers. Menstrual blood was always clumpy and sluggish and dark in color. In addition, she had severe back pain. She also complained about changing moods, loss of libido and lack of energy. Nine sittings with laserneedles were performed once a week. Different acupoints on the body and ear were stimulated with laser light. The time of treatment was selected in such a way, that it was briefly before the beginning of menstruation. During the nine treatments, the acupoints were stimulated with laser light. After the treatment with laserneedles, the patient said that she hadn’t felt so well in the last 2 years and that she was also emotionally better balanced. She had much more energy and felt strong. Major changes had taken place with positive effects on her body and emotional condition. She was impressed. The changes in mood had also improved distinctly. Pain in the lower abdomen was almost gone and she only needed a hot-water bottle on the first day of menstruation. The color of menstrual blood was much lighter and without clumps. As she was treated one day before the awaited menstruation she reported that she already menstruated on the same day as she was treated and that she didn’t experience any pain. The blood flow was now much thinner and she didn’t experience clumpy or sluggish blood. As the acupoint Yintang (comp. Chapter 7), a point on the forehead between the eyebrows (Fig. 15.6) was treated, she described a pleasurable sensation from the acupoint over the forehead, over the eyebrows, around the eyes and to the nose.
165
Fig. 15.6: Stimulation of acupoint Yintang.
It was a relaxing feeling. She had her eyes closed during the treatment. Nevertheless, she reported feeling lightness within. After treatment, she was full of energy and felt very well.
15.3.6
Childlessness, temperature curve, cycle regulation
A 34-year-old patient with a strong wish for having children came to my acupuncture consultation hour with the question regarding alternative methods for treating sterility. She already had 2 miscarriages in the 5th and 6th week of pregnancy. She also had a consultation in the department of endocrinology. She didn’t want to take any hormones. She didn’t take contraceptives because she wanted to get pregnant. Her menstrual cycle was somewhat prolonged with 32 days. At the beginning, the menstrual blood was sluggish, clumpy, dark in color and painful. During the first days of menstruation, she always had heavy, dark red bleeding. Every morning before getting up from bed, she measured her body temperature and recorded these values on a curve. The temperature curves over 5 months, showed a zigzag picture. The values were between 36.7 and 37.5 °C. It was not a typical two-phase course with sudden increase in temperature and following higher level favorable for pregnancy. We performed 10 sittings, 4 times once a week and then 6 times every 2 weeks. Combined treatment with laserneedles on the body, and metal needles and laserneedles on the ear were performed. On the body, acupoint combinations Sp.6, Liv.3 and St.36 and Yintang were selected. First, 7 metal needles were
166 applied on the ear at the acupoints ovary, TSH, Gonadotropin. Illumination of the endocrine regions at the intertragic notch was performed 3 times. Here, the laserneedles were fastened to a head-holding device (Fig. 15.7) and the endocrine region of the ear was illuminated.
Fig. 15.7: Head-holding device for laserneedle treatment at the ear.
On the evening of the first treatment, she was very tired. Menstruation began on the very next day. She reported that the blood flow wasn’t quite so sluggish. The color of menstrual blood was still dark. During the course of treatment, the color and consistence of blood changed. It was lighter red, not as clumpy and more flowing. The menstrual cycle regulated itself to about 29 days. Pain in the lower abdomen was more tolerable. Remarkable is the nearly picture-book like temperature curve with the typical increase at the point of ovulation and the following plateau during the second cycle phase. One day she came to my consultation hour and reported her positive pregnancy test. The result was confirmed. If she would have become pregnant without laser treatment is questionable. Noteworthy is the change in the temperature curve from the initial zigzag course to the two phase course, as well as the change in color and consistency of menstrual blood.
15.4 Results and discussion This method seems to be trend setting for the future because of high patient acceptance, comfortable treatment, and good results. The special advantage compared to acupuncture with metal needles, is that insertion into the skin is
167 not necessary. Therefore, no side effects such as bleeding, haematomas, infection, or pain during insertion into the skin occur. The mothers’ fear of vegetative reactions from needle insertion is eliminated. There is no additional stress for mother and child with this method. Thus, she can „enjoy“ this method of treatment more. Furthermore, more mobility during treatment is possible. The patients do not have to remain completely still as by common acupuncture. Since the needles are not inserted into the muscle no pain occurs during slight movement. Especially in the field of obstetrics, it is desirable that the woman is relatively mobile. During childbirth, women usually make fists during labor pains. Since acupoint LI.4 at the ball of the thumb is often used to regulate labor, this can be somewhat painful. With laserneedles, stimulation of this acupoint is easily possible. At several acupoints, patients also perceive the typical Qi sensation as when using classical needle acupuncture. However, the range of sensitivity differed. When using common acupuncture, differences in sensitivity on both sides of the body were described. The Qi sensation was described as a tingling and warming feeling. Several patients reported feelings of comfortable relaxation and tiredness. The transmission of sensations along the meridians was often mentioned. In the case study with carpal tunnel syndrome, the patient reported an initial increase in symptoms after the first treatment with laserneedles, identical to that when using common acupuncture needles. This seems to indicate that the laserneedle method has similar effects as traditional acupuncture. We could observe positive results in treating gynecologic and obstetric indications with laserneedles. Cycle regulation with lighter, improved menstrual bloodflow was observed. Temperature curves also showed better results. In the field of oncology, arm mobility and reduced muscular tension could be achieved after breast cancer surgery. In case of bladder problems, dysuria was improved and an improvement in bladder capacity could be reported. After laserneedle therapy, pain was rated with better scores on the pain scale. Exhaustion and lack of energy could also be improved. In the field of obstetrics, faster phases of labor and more energy for the mother could be noted. Labor could be successfully induced by stimulating acupoint LI.4. During treatment of carpal tunnel syndrome a decrease in pain and tingling in the hands during the night could be registered. Hyper emesis with less nausea and vomiting was also achieved. The observation regarding the transmission of laser energy to the different scars on the body is noteworthy. This could further explain the transmission to the meridians. A flow of energy is perceived. This flow will probably be altered on interfering fields / scars, which very sensitive patients can perceive.
168 Scientific studies have shown that an increase in ATP takes place when using the laserneedle method. I think that this ATP is very useful during childbearing. Childbearing requires much energy from the mother and the main supplier is definitely ATP. In particular, the energy aspect is one major difference to common acupuncture. In the approx. 300 patients we have treated with laser therapy, nearly 80 % had the impression that they gained more energy through the treatment. Caution should be taken when treating patients with too much fullness or heat. Even though the laserneedle method does not lead to an increase in body temperature, one could observe that this method wasn’t appropriate for such patients as described in the case study with hot flushes. One would be cautious in patients with an already increased sympathicus. This also seems logical. You should not give a person with too much fullness additional energy. It should be clearly stated that these are reports from experience in personal treatment of patients. Further controlled studies to evaluate the effect of laserneedles are necessary.
15.5 References >1@ >2@
>3@ >4@ >5@
Litscher G, Schikora D (2002) Cerebral vascular effects of non invasive laserneedles measured by transorbital and transtemporal Doppler Sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Neue Konzepte in der experimentellen Akupunkturforschung – Computerkontrollierte Laserpunktur (CCL) mit der Laserneedle Technik. Der Akupunkturarzt / Aurikulotherapeut 28: 18-28 Martius G, Rath W (1998) Geburtshilfe und Perinatologie. Thieme Verlag, Praxis der Frauenheilkunde Band II, 1998, S. 383-384 Schikora D.: European Patent Nr. PCT/EP 01/08504 Schikora D.: Physikalische und physiologische Eigenschaften der Lasernadeln für Akupunktur, personal communication
169
16. Laserneedles in gynecology - a study with questionnaires K. Staehler van Amerongen 16.1 Introduction In the meantime, different descriptions regarding the use and effects of laserneedle acupuncture can be found in literature [1]. Goal of this study was to evaluate what patients experienced during and after treatment with laserneedles and what they knew about the technique before treatment. Using questionnaires, this current study compares the laserneedleacupuncture method with the common metal needle acupuncture method based on the patients’ perception during and after treatment.
16.2 Test persons Thirty female patients per group were questioned. All of these patients visited the acupuncture consultation hour at the University Gynecological Clinic in Bern. They were treated for gynecological disorders and came to the consultation hours with the following symptoms: Carpal tunnel syndrome, premenstrual pain, urogenital symptoms, pruritus gravis, mastodynia, chronic abdominal pain in endometriosis, induction of labor, hyper emesis gravidarum, dysmenorrhoea, breast cancer with decreased mobility of the arm, sacra-iliac joint pain during pregnancy, smoking withdrawal during pregnancy, primary sterility and preparation for childbirth. The mean age of patients in the metal needle group was 38 years (range from 18 to 73 years) and the mean age in the laserneedle group was 36 years (range from 16 to 60 years). Assignment to the laserneedle or metal needle treatment groups was done at random. Each patient took a random number from 1 - 60. The patients with even numbers were treated with metal needle acupuncture; those with uneven numbers were treated with laserneedle acupuncture.
170
16.3 Method The patients obtained questionnaires part 1 before the first treatment, part 2 after the first treatment and part 3 prior to the second treatment. The patients filled out the questionnaires voluntarily and independently. In part 1, the question “Do you know the method (metal needle acupuncture or laserneedle acupuncture)?” was asked. Two answers were possible: either yes or no. The second question was „Have you already been treated with acupuncture?” Here also the answers yes and no could be selected. The third question was “How would you evaluate your personal state of health at the moment?” The following answers were possible: very good, good, satisfactory, poor and very poor. The fourth question was „How strongly does your illness or symptoms influence you in daily life?“ Here, 5 answers were possible as follows: extremely, strongly, moderately, a little, not at all. The questionnaires were given back for evaluation. Treatment was then performed according to assignment either with metal needle or laserneedle acupuncture. Immediately after the first treatment, the patients filled out part 2 of the questionnaire for evaluation. Again, the patients filled the questionnaire out independently and without influence from others. In the second part of the questionnaire, the patients were questioned regarding their perception during treatment. The following questions were to be answered: “Did you experience pain when the needle was applied?” - “Did you experience pain during treatment?” - “Did you experience a feeling of warmth in the body during treatment?” - “Did you experience an electrical tingling sensation during treatment?” - “Did you feel something at the needle itself during treatment?” - “Did you experience a sensation in the entire body during treatment?” - “Did you experience tiredness during treatment?” - “Did you feel relaxed, comfortable during the treatment?” The following answers were possible for the questions above: extremely, strongly, moderately, a little, none. The third part of the questionnaire was filled out by the patients prior to the second treatment. Questions regarding perception after treatment were asked. The following questions were evaluated: “Did you experience pain after the treatment?” - “Were you tired after treatment?” - “Did you feel relaxed after treatment?” - “Did your symptoms improve after treatment?” “Did you feel well physically after treatment?” - “Did you feel well emotionally after treatment?” - “Did your symptom improve with treatment?” Again, several answers were possible: extremely, strongly, moderately, a little, and none.
171
16.4 Results After evaluating the question: “Do you know the method?” Thirty patients answered “no” regarding the laserneedle method and 29 “yes” regarding the acupuncture method. This shows that treatment with common metal needle acupuncture is well known among the patients; however, they have not yet been informed about laserneedle acupuncture. Already 13 of 30 patients were treated with metal needle acupuncture whereas all 30 patients in the laserneedle group had not yet been treated with this technique. The majority of patients in both groups noted their current health condition as being good to satisfactory (n=27 in the metal needle group and n=26 in the laserneedle group) (Fig. 16.1). The symptoms they had influenced them very strongly to moderately (Fig. 16.2). In the laserneedle group (n=30) 29 patients experienced no pain and 1 a little pain during application, however in the metal needle group (n=30) 3 patients experienced extreme, 3 strong, 9 moderate, 12 a little and only 3 no pain during needle insertion (Fig. 16.3). The great advantage of “painless” laserneedle-acupuncture should be noted here. In addition, none of the 30 patients experienced any pain during laserneedle acupuncture, whereas 2 patients experienced strong, 3 moderate, 4 a little and 21 no pain during metal needle acupuncture (Fig. 16.4). The question whether they felt warmth during treatment was answered by 7 patients with extremely, 17 with strongly, 5 with moderately, 1 with little and 0 with none in the laserneedle group (n=30). In the metal needle group (n=30) only 1 patient answered with extremely, 4 with strongly, 7 with moderately, 8 with a little and 10 with none (Fig. 16.5). In the laserneedle group (n=30), the question regarding tiredness during treatment was answered by 2 patients with extreme, 9 strong, 10 moderate, 6 a little and 3 none at all. In the metal needle group (n=30) 2 patients answered with extremely, 12 strongly, 8 moderately, 2 a little and 6 with none at all (Fig. 16.6). In the laserneedle group no one answered the question regarding tiredness after treatment with extreme, 1 with strong, 2 with moderate, 13 with a little and 14 with none. In the metal needle group, 4 patients were extremely tired, 8 strongly, 4 moderately, 6 a little and 8 not at all (Fig. 16.7). In the laserneedle group 2 patients said they were extremely relaxed during treatment, 13 experienced strong relaxation. Six patients experienced moderate, 6 little and 3 no relaxation. In the metal needle group, 4 noted extreme, 17 strong, 5 moderate 4 little and 0 no relaxation (Fig. 16.8). The question regarding relaxation after treatment showed similar results. In the laserneedle group 8 answered with extreme, 14 with strong, 7 with moderate,
172 1 with little and no one with none and in the metal needle group 4 answered with extreme, 18 with strong, 6 with moderate, 2 with little and no one with none (Fig. 16.9). In both groups, the patients experienced a strong feeling of relaxation during and after treatment. In both groups, most of the patients experienced a great improvement in their symptoms and felt well after treatment (Fig. 16.10 and 16.11).
number of patients (n=30) per group
How would you evaluate your personal state of health at the moment?
20
16
15
15 11
11
10 5
1
2
1
3 0
0 very good
good
satisfactory
metal needle acupuncture
poor
0
very poor
laserneedle acupuncture
Fig. 16.1: How would you evaluate your personal state of health at the moment?
number of patients (n=30) per group
How strongly does your illness or symptoms influence you in daily life? 16 14 12 10 8 6 4 2 0
15 12 10 7
6
8
1 extremely
strongly
moderately
metal needle acupuncture
1
a little
0
0
not at all
laserneedle acupuncture
Fig. 16.2: How strongly does your illness or symptoms influence you in daily life?
173
number of patients (n=30) per group
Did you experience pain when the needle was applied? 35 30 25 20 15 10 5 0
29
12
9 3
3
0
extreme
0
strong
1
0 moderate
metal needle acupuncture
a little
3 none
laserneedle acupuncture
Fig. 16.3: Did you experience pain when the needle was applied?
number of patients (n=30) per group
Did you experience pain during treatment? 35
30
30 25
21
20 15 10 5 0
0
2
0
extreme
0
strong
3
4 0
0
moderate
metal needle acupuncture
a little
none
laserneedle acupuncture
Fig. 16.4: Did you experience pain during treatment?
174
number of patients (n=30) per group
Warmth during treatment 18 16 14 12 10 8 6 4 2 0
17
10 8
7
7
5
4 1
1
extreme
strong
moderate
metal needle acupuncture
little
0 none
laserneedle acupuncture
Fig. 16.5: Warmth during treatment
number of patients (n=30) per group
Tiredness during treatment 14
12
12
9
10 8
10 8 6
6 4 2
2
2
6 3
2
0 extreme
strong
moderate
metal needle acupuncture
Fig. 16.6: Tiredness during treatment
little
none
laserneedle acupuncture
175
number of patients (n=30) per group
Tiredness after treatment 16 14 12 10 8 6 4 2 0
14
13 8
8 6
4
4
extrem e
2
1
0
strong
m oderate
metal needle acupuncture
little
none
laserneedle acupuncture
Fig. 16.7: Tiredness after treatment
Relaxation during treatment 17
number of patients (n=30) per group
18 16
13
14 12 10 8 6 4 2
5
4
6
6 4
3
2 0
0 extreme
strong
moderate
metal needle acupuncture
Fig. 16.8: Relaxation during treatment
little
none
laserneedle acupuncture
176 Relaxation after treatment
number of patients (n=30) per group
20
18
18 16
14
14 12 10
8
8 6 4
6
7
4 2
2
1
0 extrem e
strong
m oderate
metal needle acupuncture
little
0
0
none
laserneedle acupuncture
Fig. 16.9: Relaxation after treatment
number of patients (n=30) per group
Improvement of symptoms after treatment 20
18 15
15
9
10 5
7 4
3
2
2 0
0 extremely
strongly
moderately
metal needle acupuncture
a little
not at all
laserneedle acupuncture
Fig. 16.10: Improvement of symptoms after treatment
0
177
number of patients (n=30) per group
How do you feel after treatment? 25 20
20
18
15 10 5
5
6
4
5 1
1
0 very good
good
satisfactory
metal needle acupuncture
poor
0
0
very poor
laserneedle acupuncture
Fig. 16.11: How do you feel after treatment?
16.5 Discussion Our study shows that metal needle acupuncture is well known among patients but that laserneedle acupuncture requires further explanation regarding the method and possibilities of use. With the exception of one patient, no one experienced any pain during application of the needle or during treatment. The painless laserneedle method has a clear advantage compared to common metal needle acupuncture. Obvious differences in both groups regarding warming sensations can be reported. Laserneedle therapy is definitely a method in which warmth is experienced by the patient during treatment. According to temperature measurements, the body and tissue temperature does not increase during laserneedle acupuncture; however our studies show that the majority of patients perceive a warming sensation in the body. Further temperature measurements should follow. The tendency that metal needle acupuncture leads to stronger tiredness during and after treatment is obvious. On the other hand, patients treated with laserneedles were more “energetic” after treatment. Maybe laserneedles have a positive influence on less energetic persons? On the other hand, persons in our patient collective experienced a strong feeling of relaxation
178 during and after treatment. Both methods seem to be good in achieving relaxation. Most patients in both groups experienced a great improvement in their symptoms and felt well after treatment. When we view this questioning in its entirety, laserneedle acupuncture seems to be a method which according to the patients’ perception has a positive influence on symptoms and is a painless, energetic and relaxing method which leads to a warming sensation during treatment.
16.6 References [1]
Litscher G, Schikora D (Hrsg) (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Bremen
179
17. Laserneedle therapy in dentistry K. Borer 17.1 Introduction In addition to toothache and neuralgia, patients in dental practices often also suffer from anxiety and needle phobia. Experienced dentists can achieve fast relief with acupuncture therapy [1-4]. Laserneedle-technology allows new, painless acupuncture stimulation. This study is a report about the use of laserneedle acupuncture in daily routine dentistry.
17.2 Methods and materials Prerequisite for laser acupuncture treatment was the diagnostic exclusion of all obvious dental causes. For example, bite problems were treated first in the occlusion; root treatment was performed in case of gangrenous dental pulp. The positioning of the diodes was done differently according to indication: 1 – 2 diodes for direct treatment of the tooth and respective wound region, dermatologic hammer for extensive treatment (mandibular joint), application of diodes at acupuncture points according to body and ear acupuncture. Main emphasis during testing of the device was the local treatment of the problem areas.
17.3 Results 17.3.1
Oral surgery
Post operative pain with lockjaw after surgical removal of wisdom tooth: Daily treatment was done locally using the dermatologic hammer (Fig. 17.1) with eight diodes for three sittings. After the first treatment, only minor pain was present and after the third sitting, the patient could open his mouth normally.
180
Fig. 17.1: Dermatologic hammer for the treatment of jaw problems.
Massive symptoms after paradontal surgery: Local treatment with three diodes, every three days, resulted in immediate painlessness after the first sitting, thereafter, to very rapid healing (gingiva without necrotic coating, rapid resolution of the haematoma).
17.3.2
Endodontology
Toothache with new porcelain inlay: The affected tooth was treated daily, with two diodes, from the dental neck to the apex. The patient was free of pain after two sittings with positive vitality testing. Routine treatment during direct capping of open dental nerves: The corresponding area of the dental nerves were treated locally with one diode, for one minute, thereafter, a dental wound bandage was applied. In this manner, the possible death of dental nerves may be reduced.
181 17.3.3
Crown - bridges
Routine treatment of prepared pillar teeth: The prepared teeth were treated with a diode for 2 minutes. As a result, later death of the treated teeth may be avoided.
17.3.4
Pain therapy
Bite problems, sensitivity of teeth to temperature: The dental neck to the apex was treated locally with 1 – 2 diodes for about 10 minutes, every 2 – 3 days (Fig. 17.2). The reaction time until pain ceased was variable; usually 2 to 3 sittings were required.
Fig. 17.2: Treatment of the dental neck.
17.3.5
Myoarthropathy
Due to increasing stress in the population, an increase in central pressing, grinding and severely indurated jaw and neck muscles with jaw problems occur. As a result, contraction of the jaw, neck and back muscles with corresponding pain symptoms occur. Treatment was performed using the dermatologic hammer (Fig. 17.3) above the affected jaw muscles, above the cervical vertebra C0/1 and C7. Thereafter, the patients felt relaxation and a light warming sensation.
182
Fig. 17.3: Dermatologic hammer for the treatment of myoarthropathy and jaw problems.
17.3.6
Neuralgia
Based on the affected areas of the head, diodes were applied at the classic acupuncture points of the head and rest of the body. For example, Du 20 as local point, and LI.4 and Liv.3 as distant points.
17.3.7
Sedation in case of dental phobias
Acupuncture was performed 30 minutes before dental treatment. Excellent relaxation to the patient was achieved with points Ki.6, LI.1-1, Ren 17 and Ren 24.
17.3.8
Nausea during molding
Acupuncture was performed 30 minutes before taking moulds, above the acupuncture points Ren 24 (Fig. 17.4), Ki.6, LI.1-1 and Pe.6. As a result, even extremely difficult models could be made without problems.
183
Fig. 17.4: Acupuncture point Ren 24 for treatment of nausea.
17.4 Discussion Laserneedle-technology can be very well integrated into the routine dental practice. The instrument is simple to handle and can be easily delegated. A sterilizable dental adapter which survives repeated sterilization would be desirable. Laser acupuncture represents an excellent initial therapy due to its positive effects on microcirculation and relaxation. Further studies should confirm the reproducibility of these positive effects under consideration of possible relapses. Overall, the application of this technology leads to a higher efficiency in treatment. On the one hand, local therapy with good initial effects can be achieved; on the other hand, causal therapy can be performed using body acupuncture. This improves and widens the possibilities in dental medicine.
17.5 References [1] [2]
Rosted P (2000) Introduction to acupuncture in dentistry. Br Dent J 189: 136-140 Lu DP, LU GP (2003) Anatomical relevance of some acupuncture points in the head and neck region that dictate medical or dental application depending on depth of needle insertion. Acupunct Electrother Res 28: 145-156
184 [3] [4]
Thayer T (2001) Acupuncture in dentistry. SAAD Dig 18: 3-8 Lu DP, Lu GP, Reed JF 3rd (2000) Acupuncture/acupressure to treat gagging dental patients: a clinical study of anti-gagging effects. Gen Dent 48: 446-452
185
18. Laserneedle stimulation as a potential additive method for post operative pain treatment G. Litscher, G. Schwarz, A. Schöpfer, L. Wang, M. Saraya, D. Schikora 18.1 Introduction The influence of post operative pain on the entire course of treatment was underestimated for a very long time. The inadequate suppression of acute postoperative pain has a negative influence on the subjective feeling, compromises vegetative regulatory and control cycles and also plays an important role in the risk of chronification. Innovative technical developments such as laserneedle acupuncture (LNA) [1-4], provide the foundation for new, potentially additive techniques in pain treatment. At the Medical University Graz, initial indications for neuro-modulated effects of LNA could be determined on healthy volunteers using non-invasive neuromonitoring techniques and modern imaging modalities [1-4]. Goal of these preliminary examinations was to document a possible influence of the new laserneedle stimulation method on the subjective, individual need of analgesics during post-operatively controlled analgesia, within a doubleblind, randomized study.
18.2 Method 18.2.1
Patients and procedure
A total of 25 patients (13 f, 12 m) with a mean age (r SD) of 45.2 r 11.9 years, were treated with activated laserneedle stimulation. The control group comprised 19 patients (mean age (r SD): 47.3 r 11.0 years; 8 f, 11 m) and was treated with deactivated laserneedles. All patients gave their written consent and the study was approved by the local Ethical Committee at the Medical University Graz. The patients who had flavotomies (mean duration of surgery: 129.3 r 19.7 min; 104 - 161 min), were treated with laserneedle acupuncture immediately before and after surgery and during consciousness for 10 minutes. The following acupoints according to Chinese ear and body acupuncture (Fig. 18.1.) were selected on both sides: ear 55 (Shenmen), ear 40 (Lumbar spine),
186 LI.4 (Hegu) and UB.60 (Kunlun). A blind pain scale (VAS 0 - 10; 0 = free of pain - 10 = maximum pain) was used for evaluation.
Fig. 18.1: Laserneedle acupuncture as a possible additive method in postoperative pain treatment. The following acupoints were stimulated: ear point 55 (Shenmen), ear point 40 (Lumbar spine), LI.4 (Hegu), UB.60 (Kunlun) (from above to below). After intervention, the effects of pain treatment within a pre-defined observation time of 90 minutes were evaluated. At a VAS > 3, the pain therapeutic regime included intravenous bolus administration of 3 mg Piritramid (Dipidolor®) at a body weight (BW) of > 50 kg; 1.5 mg at a BW < 50. The maximum dosage of analgesics was limited according to BWs to a total of 15 mg, or 7.5 mg/h respectively. After the final administration of the opiate, the patients were observed for at least 30 more minutes. Criteria for exclusion from this study were an age > 70 years, liver and kidney diseases as well as neurological disorders.
18.2.2
Laserneedle acupuncture
After cleaning the skin with alcohol, eight laserneedles were applied to the acupoints with a special adhesive. A semi-conductor laser with an emitting wave length of 680 nm was used as the light source. Output was 30 - 40 mW per laserneedle. Duration of stimulation was 20 minutes, resulting in an energy density ~ 4.6 kJ/cm² at each single acupoint, and an average total
187 value 36.8 kJ/cm² for all. Further details regarding the method can be found in previous studies [1-4].
18.2.3
Statistical analysis
The determined data was presented graphically with box plots (SigmaStat, Jandel Scientific Corp., Erkrath, Germany). The t-test was used for statistical analysis. The level of significance was determined with p < 0.05.
18.3 Results The results of the investigations are shown in Figure 18.2. The pilot study indicated insignificant changes in the rating of subjective pain based on the VAS before and after laserneedle acupuncture. It is noteworthy, that the use of analgesics during postoperative observation was higher in the group without activated laser stimulation (t-test; p = 0.09, n.s.). Clinical side effects were not observed in any of the patients. use of analgesics (O)
VAS 12
10
10
p = 0.09 (n.s.)
p=0.619
SE
Boli
8.0 + 1.1
8 n=19
6
4
SE 6.6 + 0.7
2 n=25
0 before after before after laserneedle acupuncture
n=25
0
1 PE
2before OP 3
4 after OP 5
6 O
1 7POPD 8
5 with without laserneedle acupuncture
Fig. 18.2: Box plots of changes in the values on the pain scale (VAS) at the preliminary examination (PE), before and after surgery (OP), during postoperative observation (O) and on the first post operative day (1 POPD).
188
18.4 Discussion Adequate postoperative pain treatment fitted to the patients risks and needs by the anesthesiologist, is an absolute necessity. Corresponding immediate post and perioperative pain treatment not only helps the patient by relieving pain, but also supports the stabilization of neuro-vegetative functions and can also avoid the chronification of the pain process [5]. Dependent upon the extent and localization of surgery, postoperative pain is expected in the majority of patients. However, the difference in individual pain perception and the extent of side effects differs greatly from patient to patient. Advances in pharmacological treatment have led to treatment strategies which reduce postoperative pain to a minimum and in the best case, avoid pain altogether. In addition to oral (tablets, drops) and intramuscular administration of analgesic substances, other methods of pain treatment should be mentioned, whereby drugs with analgesic potency (opiates, local anesthetics) are applied via inserted special catheters (lumbar or thoracic epidural catheters, arm plexus catheter etc.) or with long term venous canules. These substances act either regionally or on the central nervous system. Patient-controlled analgesia can be realized with microprocessor controlled electronic perfusion and infusion devices. Transcutaneous electrical nerve stimulation is another possibility for suppressing post operative pain [6]. Moreover, scientific literature describes the use of acupuncture for perioperative pain treatment in different types of surgical interventions [7,8]. For the first time, this study applies the new laserneedle acupuncture method as a possible additive method to pharmacologic pain treatment. The use of laserneedles seems to achieve a subjective, additive suppression of pain and leads to changes in the required pain medication within a 90 minute postoperative observation period. Criterion for the required analgesics was based on the patients rating of pain intensity on a visual pain analogue scale. Non-invasive laserneedle stimulation can induce specific, reproducible changes in the brain. This leads to changes in different parameters such as cerebral blood flow velocity, and for the first time can be objectified with the newest neuromonitoring methods [1-4]. This new method of painless acupuncture has not yet been used experimentally or clinically in the field of postoperative pain treatment. Further investigations with a larger patient collective are necessary to evaluate and optimize this method before laserneedle acupuncture can be considered as an additive in routine, postoperative pain treatment.
189
18.5 Acknowledgements The authors thank Ingrid Gaischek MSc for her valuable support in data analysis and preparing the manuscript (Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University Graz).
18.6 References [1] [2] [3] [4] [5] [6]
[7]
[8]
Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Litscher G, Schikora D (Eds) (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Bremen Jage J (1997) Schmerz nach Operationen. Wissenschaftliche Verlagsgesellschaft, Stuttgart Bjordal JM, Johnson MI, Ljunggreen AE (2003) Transcutaneous electrical nerve stimulation (TENS) can reduce postoperative analgesic consumption. A meta-analysis with assessment of optimal treatment parameters for postoperative pain. Eur J Pain 7(2): 181-188 Usichenko TI, Lysenyuk VP, Groth MH, Pavlovic D (2003) Detection of ear acupuncture points by measuring the electrical skin resistance in patients before, during and after orthopedic surgery performed under general anesthesia. Acupunct Electrother Res 28(3-4): 167-173 Stener-Victorin E, Kowalski J, Lundeberg T (2002) A new highly reliable instrument for the assessment of pre- and postoperative gynecological pain. Anesth Analg 95(1): 151-157
190
19. Effects of laserneedle stimulation in the external auditory meatus on very early auditory evoked potentials G. Litscher 19.1 Introduction In the past years, several new, technical advancements in laser acupuncture have triggered an innovative jump in this field of study. In addition, scientific studies have proven that laserneedle acupuncture can achieve needle-equivalent, reproducible changes in cerebral parameters, that can be registered with modern neuromonitoring techniques [1-5]. Laser light stimulation in the external auditory canal and its effects on early (BAEP; latency: 1 - 10 ms) and very early auditory evoked potentials (SAEP; latencies: < 1 ms) have not yet been scientifically investigated. In this study, laserneedle-induced changes in biological factors of SAEP, could be determined and registered for the first time in 23 healthy volunteers using this measurement technique.
19.2 Methods 19.2.1
Laserneedle stimulation in the external auditory meatus
For application of laser stimulation in the right external auditory meatus, an adapter was developed which is similar to a spectacle construction and is fixed at the ear (see Fig. 19.1 and Fig. 19.2). A total of 4 optical fibers were conducted into the external auditory meatus using a rotating, round holder allowing different distances. These laserneedles deliver continuous or frequency-modulated laser light with a wavelength of 685 nm and an output of 30 - 40 mW per laserneedle. Duration of stimulation was 10 minutes resulting in a power density of 2.3 kJ/cm² at each laserneedle and an average total of 9.2 kJ/cm² [1-5]. In addition to laser light stimulation, a sound tube for acoustic stimulation of evoked potentials was integrated in the adapter. The entire adapter does not include any metal parts; only plastic components were used.
191
Fig. 19.1: Stimulation adapter for optical laser stimulation in the area of the external acoustic meatus. A sound tube for acoustic stimulation between the 4 laserneedles is implemented in the construction.
19.2.2
Auditory evoked potentials of early latency
Acoustic stimulation was performed with clicks of 200 µs duration and alternating polarity with a frequency of 11.1 Hz. Stimulus intensity was 105 dB nHL (normal hearing level). The contra-lateral ear was not masked. Miniature earphones (Nicolet 464-656, Nicolet Instrument Corp., Madison, WI, USA) which were connected to a sound tube were used for stimulation. Gold cup electrodes (Grass E6GH) between the vertex (Cz) and right ipsilateral mastoid (Cb2) were used on the volunteers. The ground electrode was located at the position Fz. Skin-electrode impedance was < 3 kOhm. The cup electrodes were directly connected to active electrodes for amplifying the signals in the head region enabling the registration of bioelectric cerebral activities with a minimum of artifacts [6] (compare Fig. 19.2). In each investigation, at least 2000 single clicks were averaged and each measurement was reproduced one time. A PC-based neuromonitoring system (Viking IV, Nicolet Instrument Corp., Madison, WI, USA) was used for data analysis.
192
Fig. 19.2: Experimental set-up of laser stimulation at the laboratory of Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine at the Medical University of Graz.
19.2.3
Volunteers and procedure
SAEP and BAEP were investigated in a total of 23 healthy volunteers, mean age (r SD) from 26.5 r 3.6 years (range 20 to 36 years old; 15 f, 8 m). The volunteers were informed about the procedure and gave their written consent. The study was approved by the ethical committee at the Medical University of Graz. None of the volunteers took central nervous system active medication during the study period and the neurological, mental and otological status was normal in all test persons. In addition to the amplitudes of wave I and those of the IV/V-complex in brainstem auditory evoked potentials, the amplitudes of very early AEPresponses including so-called stimulation artifacts were evaluated. Further, the tympanic temperature using a ThermoScan pro LT (Thermoscan Inc., San Diego, CA, USA) was investigated before and after the three examination phases (a) resting phase (steady state), (b) continuous laserneedle stimulation and (c) frequency-modulated (2 Hz) laserneedle stimulation.
193 19.2.4
Statistical analysis
Analysis of measurement data and graphic presentation was performed with the computer programs SigmaStat and SigmaPlot (Jandel Scientific Corp., Erkrath, Germany). The paired t-test was used for statistical evaluation and graphic illustration was done with box-plot illustrations. Criterion for significance was determined by p < 0.05.
19.3 Results The first five components of BAEP could be isolated and reproduced in all test persons and corresponded with conventional standards [7]. One example is shown in Fig. 19.3.
resting condition without stimulation
a
continuous laserstimulation
b
frequency-modulated laserstimulation (2 Hz)
c
Fig. 19.3: Early auditory evoked potentials without (a), during continuous (b) and during frequency-modulated (c) laser stimulation in a 24-year-old volunteer. Note the occurrence of very early stimulus responses and the increase in stimulation artefacts (see arrows) despite alternating stimulation modes during laser stimulation. The tables show the absolute latencies of components I, III and V in milliseconds (ms) as well as the interpeak latencies I-III, III-V and I-V in ms and the amplitude relationships (I-I’)/(V-V’).
194
The mean amplitudes of SAEP, of wave I (Ia) and of the IV/V-complex (IV/V)a during resting conditions (without stimulation; steady state), after continuous laserneedle stimulation and after frequency-modulated (2 Hz) laserneedle stimulation in all volunteers can be found in Figure 19.4.
SAEP
µV 0,4
Ia
(IV/V)a
p = 0.014 (s.)
n=23
p = 0.019 (s.) 0,3
n.s. n.s. 0,2
0,1
0,0
R
cw
S1
LN
LN
R
cw
S1
LN
LN
R
cw
S1
LN
LN
Fig. 19.4: Box-plot illustrations of very early auditory evoked potentials (SAEP), amplitudes of the wave I (Ia) and amplitude of the IV/V-wave complex (IV/V)a in µV under condition R (= resting, steady state, control measurement), cw LN (continuous laserneedle stimulation) and S1 LN (2 Hz frequency-modulated laserneedle stimulation). Note the significant increase in SAEP during laser stimulation. The horizontal line in the box shows were the median is situated. The ends of the box define the 25th and 75th percentile; error bars show the 10th and 90th percentile.
Whereas the amplitudes of wave I and those of the IV/V-complex did not reveal significant changes during laser stimulation, the mean amplitude of the stimulation artifact under continuous (p = 0.019), as well as during 2 Hzmodulated stimulation (p = 0.014) show a significant increase. The tympanic temperatures measured immediately after each phase of investigation are shown in Figure 19.5.
195 °C 38,0
normal range for ear temperature (11 - 65 years)
37,5
37,0
36,5
36,0 p < 0.001 (s.)
35,5
p < 0.001 (s.)
35,0
R
cw LN
S1 LN
Fig. 19.5: Laser stimulation related changes in temperature at the external auditory meatus. The normal range for ear temperature given by the manufacturer is shown on the right (R = resting, without stimulation; cw LN = continuous laser stimulation; S1 LN = frequency-modulated laser stimulation). For further details, see Fig. 19.4.
19.4 Discussion Laser has gained a permanent position in the field of acupuncture. Corresponding to the desired solutions, the quality of different laser systems must be applied. Future developments in laser technology will be based on the new application of laser in the field of medicine in general, and its specific use in acupuncture. Factors such as the better understanding of working mechanisms, availability of technically perfected laser constructions and the development of flexible optical transmitting systems and optical fibers all lead to technically simpler systems and will play an increasing role in the future [8]. Whereas laser technology is increasingly used in the fields of surgery, ophthalmology or gynecology, comparatively few scientific studies dealing with this topic can be found in the field of ear, nose and throat medicine. In this study, we tried to objectify peripheral and possible cerebral effects of this stimulus modality using computer-aided, bioelectric stimulus responses after performing laserneedle stimulation in the external auditory meatus.
196 Therefore auditory evoked potentials of very early latency were used. Socalled “clicks” (= rectangular impulses) with a duration of 200 µs were used as stimulus impulses. Effects on latency, amplitudes and waveforms of early auditory evoked potentials dependent on the polarity of electrical stimulation, were investigated and described in detail in the literature [9-11]. If these stimuli are presented alternately, i.e. alternating once positive and once negative, stimulus-related artifacts which occur during stimulus presentation of one polarity are averaged in the signal response. In the same manner, electro-cochleographic potentials originating in the presynaptic region in the hair cells and their support structures, cochlear microphonics and the summating potential are normally eliminated by alternating the polarity of the stimulus. Small blood vessels transport oxygen and nutrition and supply the sensory cells responsible for hearing. In case of hypo-perfusion, cells are damaged and their function is disturbed. Goal of standard medical treatment is to avoid potential sudden deafness and improve the flowing characteristics of blood. Other methods of blood cleansing or the so-called hyperbaric oxygen therapy are further possibilities. Latter leads to an increase in oxygen in blood and tissues which should result in an improved clinical picture. The treatment with laserneedles could provide a further option e.g. as tinnitus therapy. It is very interesting that changes in SAEP triggered by laser stimulation could be registered in this study. In this latency range, microphonic potentials, summating potentials and subsequently, summating active potentials of the auditory nerve could be recorded (Fig. 19.6).
197
10 µV
a
10 µV
b
CM c
0,1 µV
CM
N1 d
0,1 µV
AP
1 ms
Fig. 19.6: Very early auditory evoked potentials (SAEP) in a 20-year-old volunteer after performing positive (a) and negative (b) clicks; (c) shows microphonic potentials (CM) and (d) the summating action potential (AP = N1).
The main component, the post synaptic wave N1 (compare Fig. 19.6), represents a summating action potential of the auditory nerve and doesn’t actually originate in the cochlea [12]. However, microphonic potentials (CM) are considered as a cochlear event but do not play a major role in clinical diagnostics [12]. Our results obtained from earlier studies showed an interesting phenomenon, that definitely biologically-related changes in stimulus artifacts, despite unchanged stimulus and monitoring parameters in coma depasse occur [13,14]. During our present study, measurements with laser stimulation showed a change in SAEP in the sense of a positive increase in these components, whereas results from previous studies on comatose patients, or in the extreme case of coma depasse, indicated a contrary negative increase in activity [13,14]. Similar results, namely different early AEP-stimulation responses (wave I to V) to positive and negative auditory stimulation in healthy persons as well as
198 in pathological cases, have already been discussed in the literature [13,14]. A solution for this problem, probably lies in the mechanics of the inner ear, but is not yet in sight. More specific information regarding the actual pressure conditions within the ear would be necessary. This is difficult to determine because the insertion of a microprobe additionally alters the course of sound pressure within the ear [13,14]. A second hypothesis is based on the assumption that extra cerebral changes in functional impedance occur. Already back in 1973 [15], scientists reported irreversible functional disturbances in the brain after ischemia and after anoxia resulting in a reduction of cortical impedance compared to the initial value, whereas an increase in impedance occurred in the reticular formation. A further hypothesis can be supposed for the arising changes in SAEP under laser stimulation, which indicates that these stimulus-related depolarization processes in extra cerebral areas of the auditory system underlie altered conditions of impedance. In order to get more exact results in the future, we could use a transtympanic or extra tympanic technique to register the changes resulting from laser stimulation instead of registering induced bioelectrical activity from the mastoid, as performed in this study. The trans-tympanic technique requires the application of a thin metal needle through the ear and eardrum to the nearest area of the inner ear; the less invasive extra tympanic technique allows the registration of changes in potential by applying a needle electrode behind the ear and advancing it near the eardrum. Further investigations such as exact analysis of accompanying temperature effects are necessary before final statements regarding this topic can be made.
19.5 Acknowledgements The author thanks Ms. Ingrid Gaischek MSc and Ms. Lu Wang MD (both Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University of Graz) for their valuable support in data registration and data analysis. The author thanks Dr. Detlef Schikora (University of Paderborn) for the development of the ear adapter prototype.
199
19.6 References [1] [2] [3] [4]
[5] [6] [7] [8] [9] [10] [11] [12] [13] [14]
[15]
Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laserneedles modulates brain function: First evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI). Lasers Med Sci 19: 6-11 Litscher G, Schikora D (Eds.) (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Bremen Litscher G (1998) A mulitifunctional helmet for noninvasive neuromonitoring. J Neurosurg Anesthesiol 10(2): 116-119 Litscher G (1995) Continuous brainstem auditory evoked potential monitoring during nocturnal sleep. Int J Neurosci 82(1-2): 135-142 Albrecht H, Rohde E, Zgoda F, Müller G (2002) Lasersysteme. In: Kramme R. (Ed.) (2002) Medizintechnik. Springer, Berlin Heidelberg New York, pp. 296-318 Maurer K, Schäfer E, Leitner H (1980) The effect of varying stimulus polarity (rarefaction vs. condensation) on early auditory evoked potentials (EAEPs). Electroenceph Clin Neurophysiol 50: 332-334 Stockard JJ, Stockard JE, Sharbrough FW (1978) Non-pathologic factors influencing brainstem auditory evoked potentials. Am J EEG Technol 18: 177-209 Stockard JE, Stockard JJ, Westmoreland BF, Corfits JL (1979) Brainstem auditory-evoked responses. Normal variation as a function of stimulus and subject characteristics. Arch Neurol 39: 823-831 Maurer K, Lowitzsch K, Stöhr M (1990) Evozierte Potentiale. AEP VEP - SEP. Atlas mit Einführungen. Ferdinand Enke Verlag, Stuttgart Litscher G, Schwarz G, Kleinert R (1995) Brain-stem auditory evoked potential monitoring. Variations of stimulus artifact in brain death. Electroenceph Clin Neurophysiol 96: 413-419 Litscher G, Schwarz G, Jobstmann R, Kehl G, Kleinert R (1996) Brainstem auditory evoked potential monitoring. The increase of the stimulus artifact in the development of brain death: a biological phenomenon? Int J Neurosci 91(1-2): 95-103 Lechner H, Ott E (1973) Impedanzuntersuchungen bei reversiblen und irreversiblen Funktionsverlust des Gehirns. In: Krösl W, Scherzer E (Eds.) (1973) Die Bestimmung des Todeszeitpunktes. Maudrich, Wien, pp. 163-170
200
20. List of references Chapter 2: Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295. Chapter 3: Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16/3-4: 335-342. Chapter 5: Litscher G, Nemetz W, Smolle J, Schwarz G, Schikora D, Uranüs S (2004) Histologische Untersuchungen zu mikromorphologischen Einflüssen von Lasernadelstrahlung. Ergebnisse einer tierexperimentellen Untersuchung. Biomed Technik 49: 2-5. Chapter 6: Litscher G (2003) Laserneedle®-Akupunktur auf dem Prüfstand der Wissenschaft. Schweizerische Z f Ganzheitsmedizin 15: 253-259. Chapter 7: Litscher G (2004) Effects of acupressure, manual acupuncture and Laserneedle® acupuncture on EEG bispectral index (BIS) and spectral edge frequency (SEF) in healthy volunteers. Europ J Anaesthesiol 21: 13-19. Chapter 8: Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laserneedles modulates brain function: First evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI). Lasers Med Sci 19: 6-11. Chapter 9: Litscher G, Wang L, Huber E, Schikora D, Schwarz G (2004) Quantitative Bestimmung geschlechtsspezifischer thermischer Empfindungsund Schmerzschwellen vor und nach Lasernadelstimulation. Biomed Technik 49(5): 106-110. Chapter 10: Litscher G, Wang L, Schikora D, Rachbauer D, Schwarz G, Schöpfer A, Ropele S, Huber E (2004) Biological effects of painless laserneedle acupuncture. Medical Acupuncture 16(1): 24-29.
201 Chapter 11: Litscher G, Wang L, Schwarz G, Schikora D (2005) Intrakranieller Druckanstieg nach zerebralen Blutflussgeschwindigkeitsänderungen durch Akupressur, Nadelakupunktur und Lasernadelakupunktur? Forschende Komplementärmedizin und Klassische Naturheilkunde, subm. Chapter 18: Litscher G, Schwarz G, Schöpfer A, Wang L, Saraya M, Schikora D (2005) Laser-“Nadel”-Stimulation als potenzielle additive Methode zur postoperativen Schmerztherapie. Schmerz & Akupunktur 4: 2-5.
202
21. Websites http://www.laserneedle.ch
Laserneedle acupuncture
http://www.laserneedle.de http://www.laserneedle.at
http://litscher.info
High-Tech Acupuncture®
http://litscher.at
Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz
203
Addendum
204
Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine Medical University of Graz
Laserneedle - Stimulation
205
Laserneedle - Acupuncture ComputerComputer-based Quantification
LaserneedleLaserneedle-Acupuncture Peripheral Effects Thermography (surface temperature)
Laser Doppler Flowmetry (microcirculation)
Laser Doppler Imaging + Standard parameters
NeedleNeedle-Acupuncture Central Effects Multidirectional Transcranial UltrasoundDoppler Sonography (blood flow velocity)
Cerebral Near-infrared Spectroscopy (changes of cerebral oxygen metabolism) f MRI Bioelectrical Methods (EEG, BIS, EP)
Laserneedle – Animal Experiments
206
Laserneedle - Thermography
Laserneedle - Thermography
10:40
10:42
a
b
10:44
10:46
c
d
207
Laser Doppler Perfusion Imaging
Laser Doppler Perfusion Imaging
before
immediately after
after
208
Laserneedle - Stimulation ComputerComputer-based Quantification
Cerebral Effects
209
Laserneedle – Acupuncture Research
Ophthalmic Artery (OA)
210
Laserneedle Acupuncture - fMRI
211
Laserneedle – Stimulation Neuromonitoring
Medical University of Graz
212
Laserneedle - Acupuncture - Yintang
213
Laserneedle - Acupuncture as a potential additive method for post operative pain treatment
University Clinic for Anesthesiology and Intensive Care Medicine Graz
214
LASERneedle® - History: First Generation (1998)
Second Generation (2000)
The Laserneedle Laserneedles were developed at the University of Paderborn (1997-1999) [ Dr. D. Schikora, Dr. M. Bartels, R. Winterberg ]
Laserneedles are: fiberoptic acupuncture needles with non-invasive contact application
Goals of the development were: • needle equivalent stimulation effects • needle equivalent functioning (simultaneous stimulation of various acupuncture point combinations)
215
LASERneedle®-medical
• the most effective laser acupuncture system of our time • with 8 painless, bichromatic laserneedles, completely sufficiently for each experienced acupuncturist and each indication
LASERneedle®-frequency
• •
Diagnostics according to BAHR and NOGIER Special analgesic frequencies to increase endorphins and non-endorphinerg transmitters
216
LASERneedle® - applicators
comfortable, rapid fixation of laserneedles on acupoints using self-adhesive non-reusable applicators
Dermatology: Laser surface illumination using LASERneedle®
Acute and chronic eczema Neurodermatitis Chronic ulcer and phlebitis Psoriasis Lichen ruber planus Verruca Alopecia areata Herpes
I = 20°
I = 0° 4
x / [mm]
2 0 -2
= = = = =
d0 0.9996 0.9992 0.9990 0.9986
* * * *
d0 d0 d0 d0
4 x (B) 2 0
-4
-6
-6 -4
-2
0
2
y / [mm]
4
6
x (A)
-2
-4
-6
d d d d d
6
x / [mm]
d d d d d
6
x (C)
-6
-4
-2
0
2
y / [mm]
4
6
= 1.02 * = 1.01 * = d0 = 0.99 * = 0.98 *
d0 d0 d0 d0
217
LASERneedle®-dental
Parodontolology
Aphthae, wounds, postoperative pain therapy, pulpalgia, inflammation of the gingivae complementary: nausea-acupuncture
Endodontology
LASERneedle® - optical technologies
Laserneedlesurface-polishing procedure Computer-controlled laser fiber coupling
The ability to heal illnesses and relieve pain with light is a fascinating vision. Scientists agree that the 21st Century will be the century of photons, as the past 20th Century was that of the electrons. The laserneedles described in this compendium are characteristic for modern advancements. For the first time, they allow painless and highly effective acupuncture treatment according to traditional rules. Why this is possible is discussed in this book. Laserneedles are products from interdisciplinary and international research. Their effects open up new therapeutic dimensions beyond acupuncture whose medical-technological foundations are described here by authors from Austria, China, Germany and Switzerland.
ISBN 3-89967-199-6 (Europe) ISBN 1-59326-074-1 (USA)
www.pabst-publishers.com
LaserneedleAcupuncture Science and Practice
PABST
III
Gerhard Litscher and Detlef Schikora (Eds.)
Laserneedle - Acupuncture Science and Practice
PABST SCIENCE PUBLISHERS Lengerich, Berlin, Bremen, Miami, Riga, Viernheim, Wien, Zagreb
IV Bibliographic information published by Die Deutsche Bibliothek Die Deutsche Bibliothek lists this publication in the Deutsche Nationalbibliografie; detailed bibliographic data is available in the Internet at
This work is subject to copyright. All rights are reserved, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in other ways, and storage in data banks. The use of registered names, trademarks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. The authors and the publisher of this volume have taken care that the information and recommendations contained herein are accurate and compatible with the standards generally accepted at the time of publication. Nevertheless, it is difficult to ensure that all the information given is entirely accurate for all circumstances. The publisher disclaims any liability, loss, or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents of this volume.
Gerhard Litscher, Prof MSc PhD MDsc Medical University of Graz Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine Auenbruggerplatz 29 8036 Graz / Austria Tel. ++43 316 385-3907, -83907 Fax ++43 316 385-3908 E-mail: [email protected] Detlef Schikora, PhD University of Paderborn Faculty of Science Warburger Straße 100 33095 Paderborn / Germany Tel. ++49 5251 60-3566 Fax ++49 5251 60-3490 E-mail: [email protected]
© 2005 Pabst Science Publishers, 49525 Lengerich, Germany Printing: D+L Printpartner GmbH, 46395 Bocholt, Germany ISBN 3-89967-199-6 (Europe), ISBN 1-59326-074-1 (USA)
V
Preface This compendium of „Laserneedle-Acupuncture“ conveys scientific and first practical results from the field of laserneedle acupuncture in an abridged and concise form. Just the thought of being pricked with needles is very uncomfortable for many people. Using the new, advanced laserneedle acupuncture method up to eight laserneedles are applied to the skin simultaneously, however, without puncturing the skin. Thus, painless, non-invasive acupuncture is possible for the first time. First public presentation of the laserneedle-system was in the year 2000 at the Medica fair in Düsseldorf. Three years of intensive scientific research and developmental work preceded. The basic idea of laserneedles originated from analysis of laser acupuncture, which was developed and spread throughout Europe in the 1990´s. It was obvious, that the technique of classic acupuncture as it had been practised for centuries, namely the simultaneous stimulation of therapy-specific acupoint combinations, became to leave its natural course. Today and in the past, acupoints are stimulated one after another using laser light, even though no evidence regarding identical effects achieved with Traditional Chinese Medicine has been documented in classic or modern literature. Suddenly, the simultaneous puncturing of acupoints according to the basic scheme of Chinese acupuncture was no longer important when practicing the Western method of laserpuncture. With the development of laserneedles, the goal to maintain the fascination of acupuncture itself was pursued: the complex diagnostic systemic approach on the one hand, and the simple manner of therapeutic application and its effects on the other. Simultaneous procedures, simple, manual handling during needle acupuncture with needle-equivalent stimulation effects and stimulation characteristics were the developmental goals of our laserneedle project. The main part of this volume includes „Peer-Review“ studies and thus, represents a scientifically substantiated work dealing with laserneedle acupuncture in particular and acupuncture in general. Noted scientists and well-known users have taken part in this book and reported about the scientific investigations and use of this new, advanced method in the field of acupuncture.
VI Non-invasive laserneedle stimulation can induce specific, reproducible effects in the brain. This is expressed by changes in different parameters such as cerebral blood flow velocity, which can be objectified using modern neuromonitoring methods for the first time. The results in this book show that cerebral effects induced by the new, painless laserneedle technique lie within similar dimensions as those evoked by manual needle acupuncture. For the first time, laserneedle acupuncture allows simultaneous optical stimulation of individual acupoint combinations. At the same time, variations in acupuncture on the body, ear or hand, as performed in our first study were made possible. Based on these investigations, the cerebral effects of laserneedle stimulation could be systematically objectified, specified and optimized for the first time. These scientific findings do not only have extensive consequences in laser medicine, but also build an important bridge between traditional Eastern and innovative Western medicine. Contact between the editors of this compendium developed in a typical modern way: per e-mail. Professor Litscher from the Medical University of Graz reported his interest in performing studies with laserneedle acupuncture to the University of Paderborn. Dr. Schikora from Paderborn answered back that he was very interested. What developed from this contact is documented in this book. Currently studies with laserneedle acupuncture are being performed in several University Clinics in Germany, Austria, Switzerland and France. All of these studies will contribute to a better understanding and objectification of effects not only for acupuncture with laserneedles but also for classic acupuncture and promote the use of this comprehensive, natural medical treatment method. Scientists agree that the 21st Century will be the Century of Photons, like the 20th Century was the Century of Electrons. It is certain, that exact understanding of the elementary interaction of photons with biological molecules, will lead to new, natural medical treatment methods which will reach far beyond acupuncture. January 2005
Detlef Schikora
Gerhard Litscher
University of Paderborn
Medical University of Graz
VII
Contents 1.
Laserneedles in acupuncture ............................................................... 1 1.1 Introduction and motivation ......................................................... 1 1.2 Dose-effect relationships in acupuncture ..................................... 4 1.3 Laserneedle acupuncture as a placebo method............................. 7 1.4 Physical characteristics of laserneedles...................................... 11 1.5 Acknowledgements .................................................................... 16 1.6 References .................................................................................. 16
2.
Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography................ 18 2.1 Introduction ................................................................................ 18 2.2 Methods...................................................................................... 20 2.2.1 Non-invasive laserneedles ............................................. 20 2.2.2 Multidirectional transorbital and transtemporal Doppler sonography ...................................................... 22 2.2.3 Participants .................................................................... 23 2.2.4 Acupuncture and procedure........................................... 23 2.2.5 Statistical analysis ......................................................... 25 2.3 Results ....................................................................................... 25 2.4 Discussion .................................................................................. 27 2.5 Conclusion.................................................................................. 28 2.6 Acknowledgements .................................................................... 29 2.7 References .................................................................................. 29
3.
Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture ................................. 32 3.1 Introduction ................................................................................ 32 3.2 Methods...................................................................................... 32 3.2.1 Near-infrared spectroscopy............................................ 32 3.2.2 Laserneedle stimulation................................................. 33 3.2.3 Healthy volunteers, acupuncture, measurement procedure................................................. 34 3.2.4 Statistical analysis ......................................................... 36 3.3 Results ....................................................................................... 36 3.4 Discussion .................................................................................. 38 3.5 Acknowledgements .................................................................... 41 3.6 References .................................................................................. 41
4.
Communication between acupoint and brain proved by ultrasound ...................................................................................... 43 4.1 Introduction ................................................................................ 43 4.2 Methods and materials................................................................ 43
VIII 4.2.1
4.3 4.4 4.5 4.6
TCD monitoring of the anterior and posterior cerebral arteries with a new probe holder...................... 43 4.2.2 Participants .................................................................... 44 4.2.3 Laserneedle acupuncture ............................................... 45 4.2.4 Statistical analysis ......................................................... 48 Results ....................................................................................... 48 Discussion .................................................................................. 53 Acknowledgements .................................................................... 55 References .................................................................................. 55
5.
Histological investigations regarding micromorphological effects of laserneedle illumination. Results of an animal experiment........................................................................................... 57 5.1 Introduction ................................................................................ 57 5.2 Methods...................................................................................... 57 5.2.1 Procedure....................................................................... 57 5.2.2 Laserneedle stimulation................................................. 59 5.2.3 Laser Doppler flowmetry and temperature measurement.................................................................. 59 5.3 Results ....................................................................................... 60 5.4 Discussion .................................................................................. 61 5.5 Acknowledgements .................................................................... 62 5.6 References .................................................................................. 62
6.
Effects of laserneedle stimulation on microcirculation and skin temperature................................................................................. 64 6.1 Introduction ................................................................................ 64 6.2 Method and volunteers ............................................................... 64 6.2.1 Laser Doppler flowmetry .............................................. 64 6.2.2 Volunteers and procedure.............................................. 65 6.2.3 Statistical analysis ......................................................... 67 6.3 Results ....................................................................................... 67 6.4 Discussion .................................................................................. 70 6.5 References .................................................................................. 72
7.
Effects of acupressure, manual acupuncture and laserneedle acupuncture on EEG bispectral index (BIS) and spectral edge frequency (SEF) in healthy volunteers ...................... 73 7.1 Introduction ................................................................................ 73 7.2 Material and methods ................................................................. 73 7.2.1 Subjects ......................................................................... 73 7.2.2 Procedure and study design ........................................... 74 7.2.3 Evaluation parameters ................................................... 76 7.2.4 Statistical analysis ......................................................... 77
IX 7.3 7.4 7.5 7.6
Results ....................................................................................... 77 Discussion .................................................................................. 81 Acknowledgements .................................................................... 85 References .................................................................................. 85
8.
Acupuncture using laserneedles modulates brain function: first evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI) ................................................................................... 87 8.1 Introduction ................................................................................ 87 8.2 Methods...................................................................................... 88 8.2.1 Painless laserneedles ..................................................... 88 8.2.2 Functional multidirectional transcranial Doppler sonography (fTCD) ....................................................... 88 8.2.3 Functional magnetic resonance imaging (fMRI)........... 89 8.2.4 Participants .................................................................... 89 8.2.5 Experimental design and procedure .............................. 89 8.2.6 Evaluated parameters..................................................... 91 8.2.7 Statistical analysis ......................................................... 92 8.3 Results ....................................................................................... 92 8.4 Discussion .................................................................................. 96 8.5 Conclusions ................................................................................ 98 8.6 Acknowledgements .................................................................... 98 8.7 References .................................................................................. 98
9.
Quantification of gender specific thermal sensory and pain thresholds before and after laserneedle stimulation ............. 101 9.1 Introduction .............................................................................. 101 9.2 Method ..................................................................................... 101 9.2.1 Volunteers.................................................................... 101 9.2.2 Measurement of thermal sensitivity and thermal pain thresholds............................................................. 102 9.2.3 Laserneedle acupuncture and procedure...................... 103 9.2.4 Statistical analysis ....................................................... 105 9.3 Results ..................................................................................... 105 9.4 Discussion ................................................................................ 109 9.5 Acknowledgements .................................................................. 110 9.6 References ................................................................................ 110
10. Biological effects of painless laserneedle acupuncture a short summary of important scientific results ............................ 112 10.1 Introduction .............................................................................. 112 10.2 Methods.................................................................................... 112 10.2.1 Temperature and microcirculatory monitoring ........... 112
X
10.3 10.4 10.5 10.6 10.7
10.2.2 Functional multidirectional transcranial Dopplersonography (fTCD) ..................................................... 113 10.2.3 Functional magnetic resonance imaging (fMRI)......... 113 10.2.4 Near infrared spectroscopy (NIRS) ............................. 113 10.2.5 Laserneedle stimulation............................................... 113 10.2.6 Healthy volunteers, animal experiment and procedures.................................................................... 114 10.2.7 Statistical analysis ....................................................... 114 10.2.8 Evaluation parameters ................................................. 115 Results ..................................................................................... 115 Discussion ................................................................................ 121 Conclusion................................................................................ 122 Acknowledgements .................................................................. 122 References ................................................................................ 122
11. Increases in intracranial pressure and changes in blood flow velocity due to acupressure, needle and laserneedle acupuncture?................................................................. 124 11.1 Introduction .............................................................................. 124 11.2 Material and methods ............................................................... 124 11.2.1 Volunteers, patient, acupressure and procedure .......... 124 11.2.2 Measurement techniques, evaluation parameters and statistical analysis ................................................. 126 11.3 Results ..................................................................................... 127 11.4 Discussion ................................................................................ 131 11.5 Acknowledgements .................................................................. 133 11.6 References ................................................................................ 133 12. Laserneedle acupuncture - clinical studies..................................... 135 12.1 Introduction .............................................................................. 135 12.2 Material, patients and methods................................................. 136 12.3 Results ..................................................................................... 139 12.3.1 Lumbar, thoracic and cervical spine syndromes as well as post cervical and lumbar intervertebral disk prolapse................................................................ 139 12.3.2 Gonarthrosis, coxarthrosis, rhizarthrosis, periarthritis in the shoulder, epicondylitis, tendinitis, Morbus Bechterew and fibromyalgia-syndrome ......... 140 12.3.3 Remaining paresis after stroke .................................... 141 12.3.4 Cephalgia, migraine and trigeminal neuralgia............. 142 12.3.5 Arterial obstruction disease ......................................... 143 12.3.6 Gastropathy and bronchial asthma .............................. 143 12.3.7 Depression, anxiety, panic attacks, psychovegetative exhaustion ....................................... 143
XI 12.4 Discussion ................................................................................ 144 12.5 References ................................................................................ 145 13. Pain therapy with laserneedle acupuncture ................................... 147 13.1 Introduction .............................................................................. 147 13.2 Case reports .............................................................................. 147 13.3 Argumentation.......................................................................... 148 13.4 Discussion ................................................................................ 150 13.5 References ................................................................................ 151 14. Pain therapy of osteoarthrosis / osteoarthritis-patients using the laserneedle system in a medical practice with emphasis on rheumatology and pain therapy ................................ 152 14.1 Introduction .............................................................................. 152 14.2 Patients and method.................................................................. 152 14.3 Results ..................................................................................... 154 14.4 Discussion ................................................................................ 154 14.5 References ................................................................................ 155 15. Laserneedles in gynecology.............................................................. 156 15.1 Introduction .............................................................................. 156 15.2 Material, test persons, technique .............................................. 157 15.3 Case studies .............................................................................. 158 15.3.1 Induction of labor with laserneedles............................ 158 15.3.2 Carpal tunnel syndrome............................................... 160 15.3.3 Urogenital symptoms, back pain, hot flushes.............. 161 15.3.4 Breast cancer with mastectomy, transmission in scars 162 15.3.5 Dysmenorrhoea, lack of energy................................... 164 15.3.6 Childlessness, temperature curve, cycle regulation..... 165 15.4 Results and discussion.............................................................. 166 15.5 References ................................................................................ 168 16. Laserneedles in gynecology - a study with questionnaires ............ 169 16.1 Introduction .............................................................................. 169 16.2 Test persons.............................................................................. 169 16.3 Method ..................................................................................... 170 16.4 Results ..................................................................................... 171 16.5 Discussion ................................................................................ 177 16.6 References ................................................................................ 178 17. Laserneedle therapy in dentistry..................................................... 179 17.1 Introduction .............................................................................. 179 17.2 Methods and materials.............................................................. 179 17.3 Results ..................................................................................... 179
XII 17.3.1 Oral surgery ................................................................. 179 17.3.2 Endodontology ............................................................ 180 17.3.3 Crown - bridges ........................................................... 181 17.3.4 Pain therapy ................................................................. 181 17.3.5 Myoarthropathy ........................................................... 181 17.3.6 Neuralgia ..................................................................... 182 17.3.7 Sedation in case of dental phobias............................... 182 17.3.8 Nausea during molding................................................ 182 17.4 Discussion ................................................................................ 183 17.5 References ................................................................................ 183 18. Laserneedle stimulation as a potential additive method for post operative pain treatment.................................................... 185 18.1 Introduction .............................................................................. 185 18.2 Method ..................................................................................... 185 18.2.1 Patients and procedure................................................. 185 18.2.2 Laserneedle acupuncture ............................................. 186 18.2.3 Statistical analysis ....................................................... 187 18.3 Results ..................................................................................... 187 18.4 Discussion ................................................................................ 188 18.5 Acknowledgements .................................................................. 189 18.6 References ................................................................................ 189 19. Effects of laserneedle stimulation in the external auditory meatus on very early auditory evoked potentials .......................... 190 19.1 Introduction .............................................................................. 190 19.2 Methods.................................................................................... 190 19.2.1 Laserneedle stimulation in the external auditory meatus ........................................................... 190 19.2.2 Auditory evoked potentials of early latency................ 191 19.2.3 Volunteers and procedure............................................ 192 19.2.4 Statistical analysis ....................................................... 193 19.3 Results ..................................................................................... 193 19.4 Discussion ................................................................................ 195 19.5 Acknowledgements .................................................................. 198 19.6 References ................................................................................ 199 20. List of references............................................................................... 200 21. Websites............................................................................................. 202 Addendum................................................................................................. 203
XIII
Editors (and authors): Gerhard Litscher, Prof MSc PhD MDsc Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Detlef Schikora, PhD Faculty of Science University of Paderborn Warburger Strasse 100 33098 Paderborn / Germany
Authors: Konrad B. Borer, MD Therwilerstrasse 11 4153 Reinach BL / Switzerland Franz Ebner, Prof MD MR Research Unit and Clinical Department of Neuroradiology Medical University of Graz Auenbruggerplatz 9 8036 Graz / Austria Franz Fazekas, Prof MD Department of Neurology, Medical University of Graz Auenbruggerplatz 22 8036 Graz / Austria Rudolf Helling, MD 1st Chairman of the ‘Ärzte-Forum für Akupunktur e.V.’ Ostenallee 107 59071 Hamm / Germany Evamaria Huber Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria
XIV Knut Kolitsch, MD General practitioner and expert for special pain therapy Oelzer Straße 12 98746 Katzhütte/Thüringen / Germany Wolfgang Nemetz, MD Department of Anesthesiology for Neurosurgical and Craniofacial Surgery and Intensive Care, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Dagmar Rachbauer, MSc MDsc Department of Neurology, Medical University of Graz Auenbruggerplatz 22 8036 Graz / Austria Stefan Ropele, Prof PhD Department of Neurology and MR Research Unit Medical University of Graz Auenbruggerplatz 22 8036 Graz / Austria Matthias Saraya, MD Department of Anesthesiology for Neurosurgical and Craniofacial Surgery and Intensive Care, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Andreas Schöpfer, MD Department of Anesthesiology for Neurosurgical and Craniofacial Surgery and Intensive Care, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Gerhard Schwarz, Prof MD Department of Anesthesiology for Neurosurgical and Craniofacial Surgery and Intensive Care, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria
XV Josef Smolle, Prof MD University Clinic for Dermatology, Medical University of Graz Auenbruggerplatz 8 8036 Graz / Austria Kirsten Stähler van Amerongen, MD Gynecological Clinic Inselspital Berne University of Berne Effingerstrasse 102 3010 Bern / Switzerland Selman Uranüs, Prof MD Department of Surgical Research, University Surgical Clinic, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Lu Wang, MD Dipl. Acup. Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz Auenbruggerplatz 29 8036 Graz / Austria Michael Weber, MD Dipl. Chem. General practitioner, emergency medical aid, naturopathic treatment, acupuncture Lönsstraße 10 37697 Lauenförde / Germany Nai-Hua Yang, Prof MD University Clinic for Ophthalmology, Medical University of Graz Auenbruggerplatz 4 8036 Graz / Austria
Acknowledgements The editors thank Mrs. Ingrid Gaischek MSc (Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz) for skillful preparation of the text and illustrations and Mrs. Sonya Mendlik-Bauer for translating a major part of the manuscripts.
1
1.
Laserneedles in acupuncture D. Schikora
1.1
Introduction and motivation
In the past 30 years, acupuncture established itself in Europe and America. Patients perceive acupuncture as an effective, non-medicinal form of treatment which conforms to the increasing desire of living a natural and balanced life. Particularly in case of chronic pain, patients attested the predominantly satisfactory results of acupuncture, especially since side effects of long term drug treatment can be ruled out with this method. In 1998, a great advancement was made leading to the acceptance of acupuncture in Western medicine. After a Consensus Conference, the United States National Institute of Health concluded that acupuncture was proven effective in cases of post operative nausea and vomiting, nausea and vomiting accompanying chemotherapy, as well as post operative tooth pain [1]. Acupuncture was also rated for the following indications: addictive illnesses, menstrual pain, headaches, tennis elbow, fibromyalgia, back pain, carpal tunnel syndrome, bronchial asthma as well as for alternative or complementary treatment after stroke. At this conference, it was emphasized that side effects of competently performed acupuncture are rare and compared with conventional therapies seem to be much more favourable [2]. Even today, the acceptance of acupuncture in some fields of western medicine is problematic particularly because no objectified proof regarding the effects of acupuncture is available. Critics fail to see, that many excellent scientific studies exist, particularly regarding acupoint-analgesia, which provide a detailed picture of physiological pain reduction achieved by acupuncture treatments. Currently, over 200 scientific publications dealing with the elementary mechanisms of acupoint-analgesia exist. Especially the leading studies by Pomeranz and Chiu [3], as well as those by Mayer et al. [4] which deal with the analgesic effect of acupuncture resulting from an increased release of ß-endorphin, establish the complex picture of neurobiological basics of acupoint-analgesia [5]. A systematic overview and critical rating of the current level of knowledge regarding neurobiological mechanisms in acupoint-analgesia were recently documented by Irnich and Beyer [6]. In the meantime, the acupuncture-endorphin-hypothesis could be proven in a number of different independent animal experiments. The ability to block the analgesic effect of acupuncture by injecting an opiate antagonist in the
2 acupoint is a strong indication that the afferent nervous system plays a role in transmitting the effects of acupuncture. All of these scientific results conform to the knowledge of modern pain research regarding the role of endorphins and are described to such an extent, desirable for other wellestablished western medical methods. The fact that these scientific results are mainly obtained from animal studies, underlines their objectivity. On the clinical level, the situation is fundamentally different. Numerous single-case and controlled studies have been documented, however definite evidence for the effects could not be proven up to this day. Of course we must note that classic needle acupuncture cannot be investigated using randomised, doubleblind study designs. Neither the patient, nor therapist can be blinded, since the patient always feels the insertion or stimulation of the applied needle and the therapist always must control the position, puncture depth and angle of insertion. There is no doubt that acupuncture has to be proved in the future by objectivized, double-blind clinical trials. However, this is only possible, when an adequate placebo method for classic needle acupuncture is available. Such a method does not exist up to this date; the placebo needle used by Streitberger et al. [7] does not fulfil the requirements of a double-blind study design. The development of a real placebo method for classic needle acupuncture is definitely of initial importance for further acupuncture research and establishing acupuncture as a medical treatment method. The goal of recent extensive field studies (GERAC-Study, Model study by German private insurance companies) was to prove or refute the efficacy of acupuncture treatment in selected indications using clinically controlled methods on a statistically significant level. Objectified, clinical evidence of effects could not be obtained in these studies for the named reasons. The initial idea of laserneedles resulted from analysis of laser acupuncture, developed and spread throughout Europe in the 1990´s. It was obvious, that the century-old technique of classic acupuncture or simultaneous stimulation of therapy specific acupoint combinations began to leave its natural course. Acupoints are stimulated one after the other, even though no evidence in classic or modern literature is given, that identical effects occur. Suddenly, the puncturing of acupoints according to the basic schemes of Chinese acupuncture was no longer important in Western “Laserpuncture”. With the development of laserneedles, we tried to maintain the fascinating aspects of acupuncture: the complex diagnostic system on the one hand, the simple therapeutic procedure and the effects on the other. The simultaneous procedure, simple handling adapted to needle acupuncture, needle equivalent stimulation effects and stimulating characteristics, were the most important goals of laserneedle acupuncture. Thus, laserneedles should be applied noninvasively by direct contact between the light emitting source and the skin. It was always clear, that quantitative documented proof of the postulated equivalence between laserneedle and classical metal needles is necessary.
3 An important, but not yet investigated question concerns the connection between stimulation strength and the effects of acupuncture. We know that an inserted acupuncture needle must be moved and repositioned by the therapist to increase stimulation intensity resulting in the De-Qi sensation. This effect is not easy to quantify since the intensity of stimulation triggered by needle puncture is also not quantifiable. How the stimulation intensity at the acupoint influences the effect of acupuncture still remains an unanswered question in this context. If we assume that acupuncture is not more than a specific kind of nerve stimulation, the question arises, whether this form of acupoint stimulation correlates with the dose-effects known from the field of bio-physiology, and underlies the Weber-Fechner-Law. With laserneedles, the light dose applied at any desired acupoint combination can be measured exactly. Compared to other classic metal needles, the stimulus strength can be quantified so that determination of dosis-effect relationships is possible. A basic assumption regarding stimulation characteristics i.e. the timing factor of stimulus intensity has to be made for experimental investigation of dose-effect relationships in acupuncture. In our first approach we assumed that the nocizeptive stimulus triggered by the classic metal needle is a continuous constant stimulation which lasts as long as the needle is inserted. In order to be equivalent to this stimulation mode, the laserneedles should act in the so-called continuous wave modus. Equivalence between both needle types can only be assumed under these circumstances. Frequency-modulated laser light is generally not equivalent to the application procedure of the classic needle acupuncture. The physical characteristics of laserneedles determine their physiological influence in tissue. We have been performing theoretical studies for some time dealing with the elementary interaction between photons and complex, biological molecules. Using molecular-dynamical methods of theoretical physics, we are able to calculate and predict the interaction of electrons or photons with complex molecules, as well as the effects of molecular excitation and basic relaxation on molecular surroundings. However, this is only possible when quasi elastic scattering processes between the photons and biological molecules are the predominant interactive processes. If we assume that elementary stimulation in acupuncture is generated on a molecular level, molecular-dynamic calculation shows [8], that electrical and optical stimulation show physiologically identical results and also generate and maintain a rhythmic cascade of action potentials at the nozizeptive structures as those produced when chemical transmitters such as substance P and bradykinine are released after needle puncture. These results can define the most important physical marginal requirements for the emission characteristics of the laserneedles: the emission wave lengths should be selected in a such a way, that quasi elastic scattering processes are dominant and emission intensity at the distal output of the laserneedle should be so
4 high, that responses relevant for acupuncture can be triggered by optical stimulation.
1.2
Dose-effect relationships in acupuncture
One of the fundamental biophysiological laws, the Weber-Fechner´s Law, describes the relationship between strength of perception E of a sensory stimulus and intensity of the stimulus S. As a result, the stimulus effect and stimulus response correlate and can be described with the following logarithm: E ~ ln S This proportionality does not imply more than that the doubling of stimulus strength not automatically leads to doubling of perception or effects of the stimulus. If we illustrate this simple relationship graphically, two important characteristics become visible and are shown in Figure 1.1. 5
Reizwirkung [a.u.] stimulus effects [a.u.]
4
3
2
1
0
0
2
4
6
8
10
stimulus strength Reizstärke [a.u.][a.u.] Fig. 1.1: Relationship between stimulus strength and stimulus effects according to Weber-Fechner ´s Law.
The curve illustrates threshold characteristics of physiological stimulation. Sensory stimuli do not lead to any effects when stimulus intensity lies under
5 a critical threshold value. Weak external influences are filtered out by the organism. Moreover, the curve shows the saturation characteristics of physiological stimuli. Thus, a doubling of stimulus strength does not lead to the doubling of effects within the organism. Finally, this is an expression for the adaptability of the organism to external stimulation, whose intensities can vary over many orders of magnitude. Validity of Weber-Fechner´s Law has been proven for acoustic, thermal, chemical and mechanical stimuli. In our experiments, we investigated if this physiological law is also applicable to acupuncture, e.g. if stimulus strength at the acupoint and the resulting induced specific effects are correlated. For this purpose, laserneedles with different optical power density were used. Power densities which are effective on the skin were varied from 1.5 – 5 W/cm². In order to compare the effect of laserneedles under identical circumstances, parallel experiments using classic metal needles were also performed. The blood flow velocity in the ophthalmic artery (OA) and its changes during stimulation of an eye specific acupuncture scheme were studied in this experiments. . Preliminary studies showed that the simultaneous stimulation of acupoints Zanzhu and Yuyao, the acupoints eye and liver on the ear, as well acupoints E2 from Korean hand acupuncture and Yan Dian from Chinese Hand acupuncture led to significant and specific increases in blood flow velocity (OA) when using metal needles or laserneedles [9] (compare chapter 2). The specific effect on the visual system could be proven by the parallel measurement of blood flow velocity in the middle cerebral artery, which remained constant i.e. did not show any changes in measurement results when using this acupuncture scheme. Measurement of blood flow velocity was performed with transorbital and transtemporal Doppler sonography. Blood pressure was registered before, during and after measurement. Treatment time was 10 minutes and blood flow velocity data was monitored continuously. A randomised, cross-over study design was used and each volunteer underwent acupuncture with laserneedles, as well as with metal needles. The study protocol was approved by the ethics commission of the Medical University of Graz, reasons for exclusion of volunteers (n = 27) were treatment with medication, visual disorders, as well as neurological and psychological deficits. Figure 1.2 shows the detected dependency of blood flow velocity in the OA as a function of power density from the laserneedles.
6
change in blood flow velocity [cm/s]
metal needle
2
laserneedle - power density [W/cm ]
Fig.1.2: Change in blood flow velocity in the OA in dependence on the power density of the laserneedles during stimulation of an eye-specific acupuncture scheme. The mean changes measured in metal needle acupuncture are marked with a line.
Figure 1.2 clearly shows that acupuncture of the seven eye-specific acupoints leads to a significant increase in blood flow velocity in the OA. Metal needles yield an increase from 10 cm/s to 18 cm/s. It is obvious that changes in blood flow velocity are dependent upon the optical power densities applied when using laserneedle acupuncture. The curve conveys the best analytical adaptation of measurement values. This curve satisfies the mathematical function f (x) = c x ln (x + 0.5). This indicates that blood flow velocity in the OA is an effective parameter for acupuncture treatment and is logarithmically dependent on the stimulus intensity of the laserneedles. Thus, we can conclude, that Weber-Fechner´s Law is valid for the dose-effect relationship examined here. The threshold value I* for optical power density can be calculated from the registered and analytically determined effect curve; I* = 1.3 W/cm². This indicates that the optical power density of the laserneedles must be greater than 1.3 W/cm² in order to activate the physiological effects of acupuncture. In addition, we can see that the needle equivalence in optical power densities of the laserneedles reach I t 5 W/cm². We can assume that an increase in blood flow velocity in the OA is based on a complex cerebral reaction resulting from acupoint
7 stimulation, preceded by multi-synaptic switching of optically induced acupuncture stimulation potentials. It is noteworthy, that despite the physiological complexity, the logarithmic relationship between stimulus strength I and stimulus effect is maintained. We interpret this as obvious proof, that specific effects of acupuncture underlie these logarithmic dose-effect relationships. The existence and validity of dose-effect relationships in acupuncture could be proven for the first time using the methods described here. This statement is strictly valid only when using laserneedles which trigger continuous permanent stimulation, thus allowing exact quantification of stimulus strength. To what extent low or high frequency modulation of laserneedle light can modify proven dose-effect relationships is unclear and must be investigated in further studies. Since the postulated equivalence between metal needles and laserneedles could be clearly shown in the examined context, we can conclude that classical acupuncture and its effects also should be functionally dependent on stimulus strength according to a potency rule.
1.3
Laserneedle acupuncture as a placebo method
The requirements of an adequate placebo needle and an adequate placebo method for classical needle acupuncture are clearly to define: The requirements of a placebo needle are: 1. The placebo needle should not generate any acupuncture effect 2. The placebo needle should be of identical shape and size compared to the verum needle and therefore should not be distinguishable from a verum acupuncture needle 3. The application procedure of the verum needle and the placebo needle should be identical 4. The application procedure of the verum needle and the placebo needle should not depend on the individual experiences of the treating physician 5. The perception of the placebo needle and the verum needle at the acupoint by the patient should be identical The requirements of an acupucnture placebo method are: 1. The fundamental rules of the classic acupuncture have to be preserved, in particular the simultaneous needling of any acupoint combination should be possible with the placebo method
8 2. The direct contact between the treating physician and the patient has to be minimized by the placebo method, to exclude any healing effect by the aura of the physician If the placebo needle and the placebo method meets all this requirements, a double blind clinical study can be performed. We know that needle puncture at desired skin points also leads to effects that are similar to those resulting from stimulation of acupoints. For that reason, this type of acupuncture is called sham-acupuncture. A further demand on the placebo method would be to establish a clear definition between the categories of verum-acupuncture, placebo-acupuncture and shamacupuncture. Based on these criteria the applicability of laserneedle acupuncture as a placebo method for classic needle acupuncture can be analyzed precisely. We already mentioned that laserneedles are not inserted into the skin, but applied to the skin at the acupoint. This non-invasive method of application is an important characteristic of laserneedle acupuncture. Our studies with more than 250,000 practical applications of laserneedles show that laserneedle stimulation with distal optical power densities of about 5 W/cm² are not perceived as a stimulus sensation by the majority of patients and volunteers. Of course the threshold of laser light stimulation is different and variable from person to person, however, laserneedle stimulation with a primary emission wavelength of 685 nm at acupoints on the body is not perceivable for most patients. The cerebral effects generated by laserneedle acupuncture were investigated systematically using multi-directional functional Doppler sonography, near-infrared spectroscopy (NIRS) and functional magnetic resonance imaging [10]. In other chapters of this book we show that laserneedles with power t 5 W/cm² lead to specific changes in cerebral blood flow velocity during stimulation of visual acupoints nearly identical to those in needle acupuncture. In addition to these experimental studies, the effects of acupuncture regarding changes in cerebral oxyhaemoglobin concentrations were investigated. Here, a visual acupuncture scheme was used and in this case, non-specific cerebral parameters could be analysed. This was done using a randomized, cross-over design with direct comparison between metal needle and laserneedle stimulation. Details from these experiments are described in [11]. Measurement of cerebral concentrations of oxyhaemoglobin and desoxyhaemoglobin were done using NIRS: Figure 1.3 shows the results of these measurements dependent on the optical power of the laserneedles.
9
metal needle
laserneedle - power [mW]
Fig. 1.3: Changes in cerebral oxyhaemoglobin concentration when using a visual acupuncture scheme with metal needles and laserneedles of different optical power. The curve shows the best analytical adaptation to the measurement values of laserneedle stimulation.
The experimental data in Figure 1.3 show that laserneedle stimulation with an optical power of about 40 mW leads to changes in oxyhaemoglobin concentration, similar to the effects when using metal needles. The equivalency between metal needle stimulation and laserneedle stimulation can also be proven with these cerebral effects. These experiments also yield the best analytical adaptation of the measurement results in a logarithmic function, i.e. cerebral oxyhaemoglobin concentration parameters also underlie a physiological dose-effect relationship. The definition of verum-acupuncture, placebo-acupuncture and shamacupuncture presents a fundamentally unsolved and principally unsolvable problem for classic acupuncture with metal needles. We examined the possibilities to differentiate and define these three modalities experimentally for laserneedle acupuncture. Hereby, acupoint combinations were stimulated with laserneedles, which according to traditional Chinese medicine are coherent with the visual or olfactory system. Figure 1.4 shows the scheme of visual distant points used.
10
Fig. 1.4: Distant acupuncture points Hegu, Zusanli, Kunlun and Zhiyin of the visual system (left) and the selected sham-points (right).
Stimulation of the olfactory system was done with acupoints Yinxiang, Pianli and Hegu. Changes in blood flow velocity in the posterior cerebral artery (PCA) and anterior cerebral artery (ACA) were used for determining the effects of acupuncture stimulation and registered with functional Doppler sonography. In addition, changes in activity in the frontal area and olfactory cortex were detected using functional MR-imaging. Detailed information regarding these measurements [10] are described in chapter 8. A randomised, controlled cross-over study design was used and can be divided in the following test situations: The verum situation, characterized by activated laserneedles at the selected acupoint, the placebo-situation characterized by non-activated laserneedles at the acupoints and the sham-situation, characterized by activated laserneedles at the selected sham-points. The verum-situation showed a specific, significant increase in blood flow velocity in the PCA and ACA in our volunteers (n = 41), resulting in specific, significant activity in the occipital and olfactory cortex visible in MR-imaging. No significant changes in functional Doppler sonography and in functional MR-imaging were registered in the placebo-situation or shamsituation. From these experimental studies, we conclude that a clear differentiation between verum-acupuncture and placebo- or sham-acupuncture is possible in regard to laserneedle acupuncture. In this context, the basic difference between acupuncture with laserneedles and with metal needles becomes obvious and fulfils and important criterion for an adequate placeboacupuncture method. Since the reproducible De-Qi sensations can be
11 triggered with laserneedle acupuncture and the proven cerebral effects do not pose special demands regarding the positioning of the laserneedles, we conclude that acupuncture with laserneedles fulfils all requirements of a complete placebo experiment. We want to emphasize that the proven physiological equivalence between metal needles and laserneedles applies to all of the reports and scientific results achieved with laserneedles and in turn is also valid for classic needle acupuncture. Therefore, the use of laserneedle acupuncture, performed in randomised, double-blind studies, can be of great advantage for clinically objectifying the effects of acupuncture.
1.4
Physical characteristics of laserneedles
The laserneedles were developed at the University of Paderborn to provide a therapeutically and methodically equivalent, non-invasive instrument to the classic metal needle.
Fig. 1.5: Laserneedle for acupuncture.
Figure 1.5 shows a laserneedle. You can see that laserneedles are acupuncture needles with optical fibres that can be applied to the skin in such a way that the distal light emitting region of optical fibre is in contact with the surface of the skin. A major goal of these scientific studies was to develop photonic acupuncture needles for simultaneous stimulation of selected acupoint combinations on the body and ear which can be used in the exact same way as metal needles, The optical power densities at the distal laserneedle exit were set in such a way, that metal needle equivalent stimulation effects are guaranteed.
12
Physical foundation of stimulation effects in the numerous experimental studies is the emission of laser light with a wavelength of 685 nm (red light) as well as the complementary emission of infrared laser light with wavelengths of 880 – 950 nm. Hence, laserneedles emit “bi-chromatic“ light with a power density of 5 - 10 W/cm² at the exit of the laserneedle. Complementary, bi-chromatic emission is based on light conversion, i.e. red laser light also activates the infra-red photons in the light wave conductor. Laser light leaving the laserneedle is coherent and is routinely examined with Michelson-Interferrometry regarding its characteristics of coherence. Chronological and spatial coherence of emitted photons is immediately lost when entering the skin and diffuse scattering becomes a determining factor. The physiologically determinant power density range of 5 - 10 W/cm² is achieved by a specially developed method of optical tailoring of the fibre core. In Table 1.1 we can see that this method is very effective, when we want to reach a maximum of power density with a minimum of laser strength. Laser power
Laser-spot diameter
Optical power density
at the skin 50 mW
5 mm
0.25 W/cm²
50 mW
0.5 mm
25.5 W/cm²
50 mW
0.05 mm
2550 W/cm²
Tab. 1.1: Connection between laser power, laser-spot diameter and optical power densities.
Exemplary calculations show that a power density of 0.25 W/cm2 results when laser power of 50 mW and spot-diameter of 5 mm at the skin, commonly used in one-hand, laser-pens is applied. In order to reach the required physiological range of power density for the laserneedles, a 20 W laser must be used! As illustrated in Table 1.1, reduction of the spotdiameter by the factor 10 leads to an increase in optical power densities by a factor of 100. The emission characteristics of laserneedles described here, in particular regarding the optical power densities affecting the skin from 5 - 10 W/cm², as well as the bichromatic emissions of red and infrared laser light are based on patented technologies only realised in laser-acupuncture needles and are available under the trade name LASERneedle® [12].
13 Contact application guarantees that the applied light dose can be exactly determined and reproduced. The next figure (Fig. 1.6) graphically illustrates how much light energy is transferred from a laserneedle during acupuncture treatment into the skin.
applied light energy dose per laserneedle [J]
60 50 40 30 20 10 0
0
5
10
15
20
25
duration of treatment [min]
Fig. 1.6: Light dose of a laserneedle dependent on the duration of treatment.
In order to determine the entire optical power transferred into tissue during stimulation of acupoints, the value in the graph needs only to be multiplied with the number of laserneedles applied. Transmitted light energy of about 320 J, equivalent to about 80 cal or that contained in less than a half teaspoon of yogurt, resulted after a treatment time of 20 minutes, using 8 laserneedles. In this chapter, we have already noted, that the emission wave length of laserneedle light should be selected in such a way, that quasi elastic scattering processes in tissues are dominant and the adsorption of photons can be neglected. Figure 1.7 shows the absorption behaviour of the most important tissue structures, dependent on the emission wave length of laser light.
14
Fig. 1.7: Absorption behaviour of important tissue structures dependent on the emission wave length of laser light.
Figure 1.7 shows that all important tissue structures from the skin yield a minimum in absorption coefficients ranging from 550 -1100 nm within the electromagnetic spectrum. This is particularly true for water, oxyhaemoglobin and melanin. In this “window”, the absorption of photons and production of heat can be neglected since the scattering of photons on tissue molecules is the dominant interactive process. Therefore, this range is very suitable for optical stimulation at the surface of the skin. The depth which photons can reach with diffuse, elastic scattering processes is once again dependent on the wave length. Simple estimates show that even at a depth of 2 - 3 cm, photon densities exist, which can trigger molecular activity at nocizeptive structures. Light wave conductors available today are made of plastic (PMMA), quartz or sapphire and have comparably little absorption in the „window“ area, so that conduction losses in the optical fiber are practically neglectable. Laserneedles use semi-conductor laser diodes as a light source. Figure 1.8 shows a semi-conductor laser diode schematically.
15
Fig. 1.8: Schematic illustration of a semi-conductor laser diode.
We can see that lasers consisting of mono-crystalline (Ga, Al, In) As are about 1 x 0.5 x 0.1 mm in size, and are about as big as a salt grain. The optically active area of a semi-conductor laser diode is once again smaller by a factor of 1000 and is comprised of layers that are only a few nanometres thick. The fact that the light field emitted by a laser diode doesn’t have a circular, but rather an elliptical diameter, is of decisive importance for optical fibre laserneedles. Since the standard light wave conductors available today have a circular diameter they lead to optical losses when an elliptical light field is fenced in a round fibre core. These loses are relatively low and according to technical standings, losses in a fiber are less than 10 %. The optical power densities alone and not the primary laser strength are responsible for the physiological stimulation effects of laserneedles at the acupoint. The results from our studies show that metal needle equivalent acupuncture can only be performed within a range of 5 - 10 W/cm². Today, we attribute power densities of 10 W/cm² to the field of photodynamic therapies. The question, whether power densities in this range lead to histologic damage is of great importance and was investigated experimentally by our study group [13] (see chapter 5). In an animal study, we could prove that no micromorphologic changes occurred during 20 minute application of laserneedles with about 5 W/cm². Neither microthrombosis or extravasation could be proven, nor changes in endothelial cells of dermal blood vessels could be observed. Thermic interaction at the acupoint was determined with infrared thermography. As a result, a heating effect of laserneedle light can be neglected. We measure an increase in temperature of about 1 °C at the
16 immediate contact area during a 20 minute treatment period. If we discuss the conditions during head- and ear acupuncture with laserneedles, we must consider that light intensity in the skin decreases exponentially and is weakened to about 50 % of the initial value when it reaches the skull. Since the stratum corneum, epidermis and dermis have different refractive indexes for optical light, wave transmitting effects occur in the layers of the skin which distribute the laser light laterally over an area of about one to 2 cm². As a result, a proportional reduction in optical power densities up to two magnitudes of order and the power density of laserneedle light is reduced to physiologically unimportant values after transmission through the skin. Transmitted part of the radiation of the laserneedles is completely absorbed by the skull. Using animal experiments, we could also show that no laserneedle-radiation (continuous wave modus) at the surface of the cortex can be observed [14]. Today, the new laserneedles for acupuncture provide instruments which are extensively characterized in medical-scientific studies. About 750,000 acupuncture treatments with laserneedles are performed worldwide in the last two years. In particular, patients appreciate this painless but still effective method of acupuncture. The medical potential of this new acupuncture method is huge. At the moment, ten University Clinics in Germany, Austria, Switzerland and France are perfoming scientific studies. The goal of these studies is to study and understand the basics of acupuncture and to get a step closer to the clinical objectification of the effects of acupuncture.
1.5
Acknowledgements
The author would like to thank all of his colleagues who took part in the development of laserneedles.
1.6 [1] [2] [3] [4]
References NIH Consensus Conference (1998) Acupuncture. JAMA 280: 15181524 Yamashita H, Tsukayama H, Hori N, Kimura T, Tanno Y (2000) Incidence of adverse reactions associated with acupuncture. J Altern Complement Med 6: 345-350 Pomeranz B, Chiu D (1976) Naloxone blockade of acupuncture analgesia: endorphin implicated. Life Sci 19: 1757-1762 Mayer DJ, Price DD, Rafil A (1977) Antagonism of acupuncture analgesia in many by the narcotic antagonist naloxone. Brain Res 2: 368-372
17 [5] [6] [7] [8] [9] [10]
[11] [12] [13]
Pomeranz B (1998) Wissenschaftliche Grundlagen der Akupunktur. Springer, Berlin-Heidelberg-New York-London-Paris-Tokio-Hongkong Irnich D, Beyer A (2002) Neurobiologische Grundlagen der Akupunkturanalgesie. Schmerz 16: 93-102 Streitberger K, Kleinhenz J (1998) Introducing a placebo needle into acupuncture research. Lancet 352: 364-365 Frauenheim T, Schikora D (2003) J Med Phys, subm. Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D (2004) Die schmerzfreie Lasernadelakupunktur moduliert die Gehirnaktivität: Erste Nachweise mit funktioneller transkranieller Dopplersonographie (fTCD) und funktionellem Magnetresonanzimaging (fMRI). Schmerz & Akupunktur 1: 4-11 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Schikora D. Europäisches Patent EP01/08504 Litscher G, Nemetz W, Smolle J, Schwarz G, Schikora D, Uranüs S (2004) Histologische Untersuchungen zu mikromorphologischen Einflüssen von Lasernadelstrahlung Ergebnisse einer tierexperimentellen Untersuchung. Biomed Tech 49: 2-5
18
2.
Cerebral vascular effects of non invasive laserneedles measured by transorbital and transtemporal Doppler sonography G. Litscher, D. Schikora
2.1
Introduction
The term "acupuncture" is used to refer to the insertion of needles into the body, at special chosen sites, for the treatment or prevention of symptoms and conditions. “Laserpuncture” is known as a method to stimulate sequentially acupoints by low level laser radiation. In contrast to that "laserneedles" allow to stimulate appropriate acupoint combinations simultaneously and with higher radiation doses and therefore represent a new non invasive optical stimulation which is described in this book. The laserneedles used in this study emit red light in cw-mode with an output power of 30 - 40 mW per laserneedle, which results in a radiant exposure energy of about 2.3 kJ/cm² at each acupuncture point during a treatment time of about 10 min. Due to the well defined contact application and the possibility to stimulate simultaneously up to eight acupoints, the laserneedles allow to attribute the resulting cerebral vascular effects unambiguous and exactly to the total laser radiation dose exposed at the acupuncture point combination selected. This opens the new scientific possibility to describe the input stimulus strength of complex acupuncture treatments with well established physical parameters. The aim of this study was to provide a possible first selective evidence of specific effects of laserneedle acupuncture and needle acupuncture on brain and eye using a combination of vision related acupoints of traditional Chinese medicine, Korean hand acupuncture and ear acupuncture. Quantification of differences in cerebral effects [1] between laserneedle acupuncture and needle acupuncture was performed using a randomized cross-over study design.
19
C omputerC ontrolled A cupuncture®
C omputerC ontrolled L aserpuncture
Fig. 2.1: Computer-Controlled Acupuncture® (CCA®) [1] and Computer-Controlled Laserpuncture (CCL) with multidirectional ultrasound probe holder devices in the biomedical engineering lab of the Medical University of Graz. Details concerning the method can be found on the website http://litscher.info.
20
C omputerC ontrolled L aserpuncture
MED-UNI GR AZ
Laserneedles
Fig. 2.2: The laserneedle system is a class 3B laser system, therefore it is compulsory to wear specific laser protection glasses.
2.2 2.2.1
Methods Non invasive laserneedles
The non invasive laserneedles were constructed to fulfil two essential requirements of acupuncture [2]: (i) They allow the simultaneous stimulation of up to eight acupuncture points in any different combinations on the body, the head, the hands and the ears. (ii) The emitted laser intensity is so adjusted that a stimulus can be induced without destroying the surrounding tissue. The laser radiation of eight 55 mW - laserdiodes was coupled into eight optical fibres and the laserneedles are arranged at the distal ends of the optical fibres. Due to coupling losses the output power of each laserneedle was reduced to 30 - 40 mW. The fibre core diameter used in the study was of about 500 µm. For our experiments seven vision related acupuncture points were chosen and irradiated simultaneously. The average time of irradiation was of about 10 min resulting in an energy density of about 2.3 kJ/cm² at
21 each acupoint and a total sum of 16.1 kJ/cm² for seven acupoints. To maintain the fundamental advantage of non invasiveness, the laserneedles were fixed onto the skin but not pricked into the skin. Fig. 2.3 depicts the measured intensity profile across the optical fibre output. The insert shows a photograph of the distal laserneedle end. Due to the direct contact of the laserneedles and the skin, no loss of intensity occurs and the laser power, which affects the acupuncture points, can by exactly determined by integration of the intensity curve shown in Fig. 2.3. Actually, the output intensity of each laserneedle was determined in such a way, resulting in an average irradiance intensity at one acupoint of about 3.8 W/cm². 1
intensity [a.u.]
emission wavelength: 685 nm
laser-needle emissioncharacteristics
total output power at distal end: 30 mW
optical cladding fibre core
-2
-1
1
2
optical fibre diameter [ a.u.]
Fig. 2.3: Emission characteristics of a tailored laserneedle used in the present study (a.u. = arbitrary units). The coherence of the laser radiation at the distal output of the optical fibre was examined by Michelson-Interferometry. The inset shows a photograph of the distal end of a laserneedle.
Due to the fact that the contact area exposed to laser rays is constant and the beam divergence can be neglected, the effective laser radiation dose at the acupoints was determined directly from the output intensity of the laserneedles and the treatment duration.
22
laser energy density [ J/cm²]
3500 3000 2500 2000 1500 1000 500 0
0
200
400
600
800 1000 1200 1400
time [s] Fig 2.4: Energy density at the laser-needle contact area in dependence on the treatment time. Due to the contact type application, as well the exposed area as the laser intensity are constant and the laser radiation dose at the acupuncture point can be determined with high accuracy from treatment time.
2.2.2
Multidirectional transorbital and transtemporal Doppler sonography
Transorbital and transtemporal Doppler sonographic examinations were performed with a Multi-Dop T unit (DWL Electronic Systems GmbH, Sipplingen, Germany). A 4 MHz and a 2 MHz probe were used in a multidirectional ultrasound probe holder construction. The monitoring arrangement for simultaneous recording of Doppler sonographic signals in the ophthalmic artery (OA) and the middle cerebral artery (MCA) was stationary at the circumference of the head. Blood flow profiles in the OA were measured transorbitally with the smallest power value able to detect signals (max. 20 mW/cm²). Under acoustic control, the angle and position of the probes were adjusted until the greatest possible signal amplitude was reached. Alterations in the blood flow velocities of both arteries were registered continuously and simultaneously. In addition blood pressure was measured non invasively before, during and after stimulation (Cardiocap® CC-104, Datex Medical Electronics, Hoevelaken, The Netherlands).
23 2.2.3
Participants
The study protocol was approved by the institutional ethics committee of the Medical University of Graz (11-017 ex 00/01) and all 27 participants gave written informed consent. Fourteen female and 13 male aged 21 - 38 years (mean age 25.15 + 4.12 (Cx + SD) years) were examined. None of the subjects was under the influence of centrally active medication and had visual deficits. All persons were free of neurological or psychological disorders. They were paid for their participation.
2.2.4
Acupuncture and procedure
Seven vision related acupoints were tested in two sessions (laserneedle acupuncture and needle acupuncture) in the same persons. The acupuncture scheme consisted of two traditional Chinese acupoints: UB.2 Zanzhu (location: in the depression of the medial end of the eyebrow. Needling method: puncture transversely 0.5 - 0.8 cun) and Ex.3 Yuyao (location: at the midpoint of the eyebrow. Needling method: puncture transversely 0.3 0.5 cun). In addition two ear acupoints (eye and liver: locations see Fig. 2.5. Needling method: puncture perpendicular 0.3 cun) and two vision-related acupoints from Korean hand acupuncture (E2: location see Fig. 2.5. Needling method: puncture transversely 0.1 – 0.2 cun) and one from Chinese hand acupuncture (Yan Dian: location: on the ulnar side of the thumb distal to the first metacarpal bone. Needling method: puncture perpendicular 0.2 cun) were used [3-5]. Three different acupuncture systems were used together because the combination shows an enhanced effect of the parameters measured in the study [5].
24
Yuyao Zanzhu
Liver
Eye
E2
Yan Dian
Fig. 2.5: Vision related acupuncture points used in this study. Traditional Chinese Medicine: Zanzhu and Yuyao. Ear acupuncture: eye and liver. Korean hand acupuncture: E2. Chinese hand acupuncture: Yan Dian.
The acupoints were punctured with sterile, single-use needles after local disinfection of the skin. We used three different types of needles (body: 0.25 x 25 mm, Huan Qiu, Suzhou, China; ear: 0.2 x 13 mm, European Marco Polo Comp., Albi, France; hand: 0.1 x 8 mm, Sooji-Chim, Korea). Needle stimulation was achieved by rotating with lifting and thrusting of the needles.
25 In case of laserneedle acupuncture the acupoints were cleaned with alcohol, the laserneedles were put in contact to the skin and stable fixed by plaster stripes. The acupoint scheme was the same as described above. During the experiments the subjects were in a relaxed and comfortable position on a bed in our laboratory. Then the monitoring equipment was positioned. After a 10-minute resting period the laserneedles or acupuncture needles were applied. The choice for the initial stimulation was randomized. The mean blood flow velocity (vm) in the OA and the MCA were evaluated simultaneously and continuously [1]. Each person was studied with laserneedle acupuncture and needle acupuncture. The choice of the measuring procedure was randomized and the interval between the experiments was 20 to 30 minutes.
2.2.5
Statistical Analysis
The data were tested with Kruskal-Wallis ANOVA on ranks using the computer program SigmaStat (Jandel Scientific Corp., Erkrath, Germany). The results of the conditions before (a), during (b) and after (c) acupuncture were given as means (Cx) + standard deviation (SD) or standard error (SE). The criterion for significance was defined as p < 0.05.
2.3
Results
The demographic data, the laser- and acupuncture schemes and the measurements of mean blood flow velocity in the OA and MCA are summarized in Fig. 2.6.
26 Participants n=27 14 female, 13 male, mean age 25.15 + 4.12 (SD), range 21 – 38 years Randomized, cross-over design R
Non invasive Laserneedles
Manual Needle Acupuncture
Ophthalmic artery (OA) vm (cm/s) 20
Ophthalmic artery (OA)
15
SE
p=0.01*
10
b
20
b
a
15
p<0.001*
10
c
Middle cerebral artery (MCA)
c a
Middle cerebral artery (MCA)
b
b
60
60
50
a
c
before (a) during (b) after (c) Mean blood Laserpuncture flow velocity Cx+ SE Ophthalmic 10.33+0.88 14.67+1.15 11.33+0.96 artery (cm/s) Middle cerebral 54.93+3.28 54.56+3.26 55.07+3.50 artery (cm/s)
40
a
c
before (a) during (b) after (c) Mean blood Acupuncture flow velocity Cx+SE Ophthalmic 10.22+0.83 19.15+1.20 12.22+0.94 artery (cm/s) Middle cerebral 53.93+3.33 56.04+3.44 55.04+3.47 artery (cm/s)
*Kruskal-Wallis ANOVA on Ranks
Fig. 2.6: Subjects, acupoints, and graphical (means + standard error (SE)) as well as numeric data of the mean blood flow velocity of the ophthalmic artery (OA) and the middle cerebral artery (MCA) before (a), during (b), and after (c) stimulating with laserneedles or needling vision related acupoints in 27 healthy volunteers in a crossover design.
The results showed significant increases of vm in the OA during (b) laserneedle acupuncture (p = 0.01) and needle acupuncture (p < 0.001). At
27 the same time only minor, insignificant changes in vm were seen in the MCA. The mean arterial blood pressure (before laserneedle acupuncture: 79.2 + 6.6 (SD) mmHg; before needle acupuncture: 77.5 + 6.6 mmHg) was not significantly changed during laserneedle acupuncture (78.4 + 6.4 mmHg) or needle acupuncture (79.1 + 6.5 mmHg). The maximum amplitude of vm in the OA was detected with a delay of 10 30 sec after the initial stimulus by the needles and with a delay of 20 - 60 sec after the initial stimulus by the laserneedles.
2.4
Discussion
Important factors have led to the expanding use of laser technology in medicine. These factors are the increasing understanding of the wave-length selective interaction and associated effects of ultraviolet-infrared radiation with biologic tissues, including those of acute damage and long-term healing, the rapidly increasing availability of lasers emitting at those wavelengths that are strongly absorbed by molecular species within tissues, and the availability of both optical fiber and lens technologies [6]. Fusion of these factors has led to the development of the new laserneedle system which is described for the first time in scientific literature by our research group. Acupuncture using laserneedles has the advantage that the stimulation can hardly be felt by the patient. The operator may also be unaware of whether the laserneedle system is active, and therefore true double-blind studies can be performed, which was almost impossible up to now in acupuncture research. The new system has the added advantage that it can be used at all standard acupuncture points [32]. The effectiveness of unconventional complementary medical methods, such as laserpuncture, have previously been documented mainly as single cases. There are only few theoretical and clinical studies concerning laserpuncture in scientific literature [7-16]. Recent scientific and technological progress has truly revolutionized acupuncture. The usage of advanced exploratory tools, such as laser Doppler flowmetry [17], laser Doppler imaging [18], ultrasound [1,5,19,20] or magnetic resonance imaging [1,21], provides revealing insights and attempt to shine scientific light upon the most spectacular of the eastern medical procedures. Similar like in animal studies [22,23] we have found recently that the brain is the key to acupuncture’s and laserpuncture’s effects. New experimental
28 constructions to measure ultrasound, light and bioelectrical processes can reproducibly demonstrate effects of stimulation of acupoints in the brain [1,5,19,20,24-28]. Studies with biosensors and probes in a specially designed helmet showed that acupuncture can increase significantly and specifically the blood flow velocity in different cerebral arteries and increase the oxygen supply to the brain [1,5,19,20,24,25,27,28]. Laserpuncture and manual needle acupuncture can also lead to an increase in oxygenated hemoglobin in the tissue oxygen index [20,29]. However, laserpuncture and needling at placebo points did not produce the same effects on cerebral oxygenation. Laserpuncture has been established for many years and was reviewed by Pöntinen et al. [30]. Nonetheless, the changes of cerebral function elicited with commercially available low level lasers were in average one magnitude of order less pronounced than those elicited with conventional needle acupuncture [1,19,20,29]. Streitberger et al. [31] have reported that the stimulus strength at the acupuncture points are of decisive importance for the therapeutic efficiency of acupuncture treatments. Using placebo-needles in comparison with metal needles, it was found that the efficiency of acupuncture treatments decreases significantly, if placebo needles were used. Our present study shows that the new high optical stimulation with laserneedles can elicit reproducible cerebral effects which are in the same order (half dimension) with respect to the maximum amplitude of the mean blood flow velocity (vm) as compared to needle acupuncture. As it is shown in Fig. 2.3 the maximum blood flow velocity rate ratio 'vm (needle) / 'vm (laserneedle) for the acupuncture scheme selected is of about 2. Regarding the stimulus dynamics we found that the delay time between the initial stimulus and the occurrence of the maximum amplitude of vm is in the order of 10 - 60 sec for both methods. This allows to conclude that obviously the basic mechanism of signal activation and transmission are comparable for both acupuncture methods. Interestingly, the maximum flow rate for laserneedles was obtained after exposing a total (sum of seven acupoints) laser ray dose of about 1.6 kJ/cm².
2.5
Conclusion
In conclusion, the results of the laserneedle applications for acupuncture demonstrate specific, significant alterations in blood flow velocity of the ophthalmic artery after stimulating vision-related acupoints on the body, ear
29 and hand. At the same time blood flow velocity in the middle cerebral artery did not change significantly. For needle acupuncture qualitatively the same behavior was observed. The cerebral effects of the laserneedles were comparable to the alterations of the needle acupuncture, they differ absolutely by a factor of ~ 2. This is a significant improvement compared to the common low-level-handylaser (LLLT) acupuncture (cerebral effects factor ~ 10 lower as for needle acupuncture). Further studies using different laser stimulus intensities and wavelengths are in progress, to optimize the adjustment of the new noninvasive laserneedles and to clarify the elementary excitations at the acupoints.
2.6
Acknowledgements
The present report is the product of many co-workers. We are especially indebted to Ms. Lu Wang MD, Evamaria Huber, Ms. Petra Petz MSc and Ms. Ingrid Gaischek MSc (all Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz / Austria) for their support to this study. We would also express our thanks to Dr. Leopold Dorfer, President of the Austrian Society for Controlled Acupuncture and to Dr. Michael Weber, Member of the EGFAA for their help. We thank Petra Thöne, Tanja Prohaska, Marianne Hubbert and Jörg Reitemeyer for technical support.
2.7 [1] [2] [3] [4] [5]
[6] [7]
References Litscher G, Cho ZH (Eds) (2000) Computer-Controlled Acupuncture®. Pabst Science Publishers, Lengerich-Berlin-Rom-Riga-Wien-Zagreb Schikora D. European Patent Nr. PCT/EP 01/08504 König G, Wancura I (1989) Neue Chinesische Akupunktur. Lehrbuch und Atlas der Akupunkturpunkte. Wilhelm Maudrich, Wien-MünchenBern Yoo TW (2001) Koryo hand therapy - Korean hand acupuncture. Eum Yang Mek Jin Publishing Co, Seoul Litscher G (2002) Computer-based quantification of traditional Chinese-, ear- and Korean hand acupuncture: Needle-induced changes of regional cerebral blood flow velocity. Neurol Res 24: 377380 Judy MM (1995) Biomedical lasers. In: Bronzino JD. (Ed) The Biomedical Engineering Handbook. CRC Press, IEEE Press, Boca Raton (USA), pp. 1333-1345 Fargas-Babjak A (2001) Acupuncture, transcutaneous electrical nerve stimulation, an laser therapy in chronic pain. Clin J Pain 17 (4. Suppl): 105-113
30 [8] [9]
[10] [11] [12] [13]
[14] [15] [16] [17]
[18]
[19] [20] [21] [22] [23]
Radmayr C, Schlager A, Studen M, Bartsch G (2001) Prospective randomized trial using laser acupuncture versus desmopressin in the treatment of nocturnal enuresis. Euro Urol 40(2): 201-205 Naeser MA (1997) Neurological rehabilitation: acupuncture and laser acupuncture to treat paralysis in stroke, other paralytic conditions, and pain in carpal tunnel syndrome. J Altern Complement Med 3(4): 425 428 Read A, Beaty P, Corner J, Sommerville Ville C (1996) Reducing naltrexone-resistant hyperphagia using laser acupuncture to increase endogenous opiates. Brain Inj 10(12): 911-919 Troshin OV (1994) A clinico-neurophysiological analysis of the single action of laser puncture. Lik Sprava 5-6: 148-153 Qin JN (1987) Laser acupuncture anaesthesia and therapy in People's Republic of China. Ann Acad Med Singapore 16(2): 261-263 Nikolaev NA (1986) Therapeutic efficacy of laser and electropuncture reflexotherapy in correcting the initial manifestations of cerebral circulatory insufficiency. Zh Nevropathol Psikhiatr Im S S Korsakova 86(1): 60-64 Omura Y (1983) Non-invasive circulatory evaluation and electroacupuncture & TES treatment of diseases difficult to treat in Western medicine. Acupunct Electrother Res 8(3-4): 177-256 Schlager A, Oehler K, Huebner KU, Schmuth M, Spoetl L (2000) Healing of burns after treatment with 670-nanometer low-power laser light. Plast Reconstr Surg 105(5): 1635-1639 Schlager A, Offer T, Baldissera I (1998) Laser stimulation of acupuncture point P6 reduces postoperative vomiting in children undergoing strabismus surgery. Br J Anaesth 81(4): 529-532 Sandner-Kiesling A, Litscher G, Voit-Augustin H, James RL, Schwarz G (2001) Laser Doppler flowmetry in combined needle acupuncture and moxibustion: a pilot study in healthy adults. Lasers Med Sci 16(3): 184-191 Litscher G, Wang L, Huber E, Nilsson G (2002) Changed skin blood perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers Med Sci 17: 1925 Litscher G, Wang L, Wiesner-Zechmeister M (2000) Specific effects of laserpuncture on the cerebral circulation. Lasers Med Sci 15: 57-62 Litscher G (2001) High-Tech Akupunktur®. Pabst Science Publishers, Lengerich-Berlin-Rom-Riga-Wien-Zagreb Cho ZH, Wong EK, Fallon J (Eds) (2001) Neuro-Acupuncture I. Neuroscience Basics. Q-Puncture Inc, Los Angeles Ji G, Zhao L, Shi R, Liu Y, Wang S, Wu F (1996) Effects of electrical acupuncture on the cerebral blood flow and the pial microcirculatory blood flow in dogs. Zhen Ci Yan Jiu 21(2): 43-46 Uchida S, Kagitani F, Suzuki A, Aikawa Y (2000) Effect of acupuncture-like stimulation on cortical cerebral blood flow in anesthetized rats. Jpn J Physiol 50(5): 495-507
31 [24] [25] [26]
[27] [28] [29] [30] [31] [32]
Litscher G, Wang L, Yang NH, Schwarz G (1999) Computer-controlled acupuncture. Quantification and separation of specific effects. Neurol Res 21(6): 530-534 Litscher G, Wang L, Yang NH, Schwarz G (1999) Ultrasoundmonitored effects of acupuncture on brain and eye. Neurol Res 21(4): 373-377 Litscher G, Yang NH, Schwarz G, Wang L (1999) Computer-controlled acupuncture. A new construction for simultaneous measurement of blood flow velocity of the supratrochlear and middle cerebral arteries. Biomed Techn 44(3): 58-63. Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I (1998) Robotic transcranial Doppler sonography probes and acupuncture. Int J Neurosci 95(1-2): 1-15 Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I, Eger E (1998) Effects of acupuncture on the oxygenation of cerebral tissue. Neurol Res 20 Suppl 1: 28-32 Litscher G, Wang L (2000) Cerebral near infrared spectroscopy and acupuncture - results of a pilot study. Biomed Technik 45(7-8): 215218 Pöntinen PJ, Pothmann R (1998) Laser in der Akupunktur. Hippokrates, Stuttgart Streitberger K, Kleinhenz J (1998) Introducing a placebo needle into acupuncture research. Lancet 352: 364-365 Litscher G, Schikora D (2002) Effects of new noninvasive laserneedles on brain function. IFMBE Proceedings, 2nd European Medical and Biological Conference (EMBEC) 4. - 8.12.2002 Vienna, pp. 996-997
32
3.
Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture G. Litscher, D. Schikora
3.1
Introduction
The connection between puncturing the body with a needle and the reaction at another area of the body is still unclear. However, it has been proven that when particular acupuncture points are stimulated with needles or laser light, specific effects in the brain can be objectivized and quantified with modern cerebral monitoring methods [1-3]. In this present study, we objectivized the systematic changes of oxygenation in the brain [4] using cerebral near-infrared spectroscopy (NIRS), after stimulating acupuncture points according to traditional Chinese medicine (TCM), Korean and Chinese hand acupuncture, ear acupuncture and combinations of these different methods. We analyzed a total of 328 recordings after manual needle and laserneedle stimulation from 88 healthy volunteers [5,6].
3.2
Methods
3.2.1
Near-infrared spectroscopy
The NIRS method allows the evaluation of changes in cerebral oxygenation through the intact skull and is also gaining importance in acupuncture research because of its non-invasive approach [6-10]. The NIRO 300 Monitor (Hamamatsu Photonics, Japan) is a new instrument in this field of research. Parameters such as changes in oxyhemoglobin ('O2Hb) and desoxyhemoglobin ('HHb) are determined by Lambert-Beer´s principle [4]. The system can measure the absolute value (µmol) of changes in parameters, but not the level (absolute concentration) at which these changes occur (in positive or negative direction). The measurement value is zero, as long as no change in concentration occurs. Placement of the sensor (emitter and near-infrared detectors) on the head with a silicone holder is easy and reproducible. Data output of 'O2Hb and 'HHb were presented on a color LCD-display and color printer.
33
In addition to the spectroscopic method, non-invasive, standard monitoring parameters such as blood pressure (Cardiocap® CC-104, Datex Medical Electronics, Hoevelaken, Netherlands) were determined before, during and after different manners of stimulation.
3.2.2
Laserneedle stimulation
The laserneedle-technique represents a new, non-invasive method for optic stimulation of acupuncture points and was first described in literature in 2002 [5,6,11,12]. Laserneedle® (Schikora D.: European Patent Nr. PCT/EP 01/08504) acupuncture allows the simultaneous stimulation of individual acupuncture point combinations. Variations and combinations of acupuncture at different areas of the body, ear or hand, as performed particularly in this study are possible (compare Fig. 3.1). Details regarding this method can also be found in preceding studies [5,6,11,12].
Fig. 3.1: Test person during laserneedle stimulation and simultaneous registration of NIRS parameters. Right bottom: single active laserneedle and application device.
Changes in near-infrared spectroscopic parameters in the frontal region of the brain were continuously registered and analyzed.
34 3.2.3
Healthy volunteers, acupuncture, measurement procedure
In this study, a total of 328 measurements on 88 healthy volunteers (50 female, 38 male) mean age 25.7 + 4.0 (Cx + SD) years (19 - 38 years) were performed. The study protocol was approved by the ethics committee of the Medical University of Graz (11-017) and all test persons gave their written consent. None of the volunteers had visual, neurological or psychological deficits or were under the influence of central nervous system effective drugs. A maximum of 7 acupuncture points in different measurement series (needle acupuncture and laserneedle acupuncture) were investigated. The acupuncture scheme included two acupuncture points from TCM: Zanzhu (localization: at the medial end of the eyebrow, perpendicular to and above the inner corner of the eye, at the foramina of the supraorbital nerve; needling: perpendicular 0.5 - 0.8 cun) and Yuyao (localization: at the middle of the eyebrow, perpendicular and above the pupil; needling: inclined 0.3 0.5 cun). In addition, 2 ear acupuncture points (eye and liver: localization see Fig. 3.2; needling: inclined 0.3 cun) and 2 eye acupuncture points from Korean hand acupuncture (E2: localization see Fig. 3.2; needling: perpendicular 0.1 – 0.2 cun) and one acupuncture point from Chinese hand acupuncture (Yan Dian: localization: on the ulnar side of the middle phalanx of the thumb; needling: inclined 0.2 cun) were included in the study [11-13]. In addition, possible responses in NIRS parameters after needling and stimulating of a placebo point (localization: lateral from the radius 6 cun above the horizontal fold of the wrist exactly on the radial ledge, lateral from the pulmonary meridian) were tested. The different acupuncture schemes were applied alone and in combination, since preliminary studies indicated that the selection of different combinations also result in different effects in the cerebral parameters to be measured (e.g. bloodflow velocity in the ophthalmic artery) [11-13] (Fig. 3.2).
35
liver
Yuyao Zanzhu eye E2
Yan Dian
Fig. 3.2: Acupuncture schemes used in this study.
Acupuncture points were needled with single-use needles after local disinfection of the skin. We used three different types of needles (body: 0.25 x 25 mm, Huan Qiu, Suzhou, China; ear: 0.2 x 13 mm, European Marco Polo Comp., Albi, France; hand: 0.1 x 8 mm, Sooji-Chim, Korea). Stimulation was performed with simultaneous rotating, pulling and thrusting movements of medium intensity. In the case of laserneedle acupuncture, the skin at the acupuncture point was cleaned with alcohol, the laserneedle was positioned at the surface of the skin and then fixated with special adhesive tape. We used the same acupuncture schemes as in the combined measurements using needle acupuncture. During the experimental phase, the test persons were positioned in a relaxed manner on a lounge. After applying the near-infrared spectroscopic sensors in the frontal area of the skull, a 10 minute resting period was observed. Then, either laserneedle stimulation was activated or the acupuncture needles were inserted and stimulated for 10 seconds. Thereafter, the laser was activated for 10 minutes or the needles were left alone. The maximum amplitude of 'O2Hb and 'HHb (phase during acupuncture) was analyzed during this period of time. Randomized selection of which technique should be started with, as well as selection of sequence of the particular type of
36 stimulation (body, ear, hand, combination) was done. The resting period between each investigation was at least 30 minutes.
3.2.4
Statistical analysis
Data was analyzed with the computer program SigmaStat (Jandel Scientific Corp., Erkrath, Germany). Results from the phases before (=zeropoint calibration), during and 5 minutes after needle acupuncture or of laserneedle acupuncture are shown in the diagrams as mean values, respectively.
3.3
Results
At the left side of Figure 3.3, the hypothetical functional curve of stimulus intensity dependent upon the treatment time is shown. This diagram gains in importance due to the actually measured, specific cerebral data in regard to changes in O2Hb and HHb shown at the right. During manual, metal needle stimulation a nearly exponential maximum increase in O2Hb and an exponential decrease to a higher level than initially, occurred, whereas the trend of O2Hb during laserneedle NIRS response remains plateau-like.
Stimulus intensity SI [a.u.]
Stimulus intensity - cerebral NIRS response O2Hb
metal needle
a
HHb O2Hb
laserneedle HHb
b time [s]
10 min
B.J., 22y, f
Fig. 3.3: Left: Stimulus intensity (SI f(t)) as a function of time (hypothesis). Right: Real measured cerebral responses of NIRS-parameters O2Hb (oxyhemoglobin) and HHb (desoxyhemoglobin) on manual, brief (20 seconds) acupuncture needle stimulation (a) and laserneedle stimulation (b) in 22-year-old female test person. The arrows indicate the beginning of stimulation.
37
Figures 3.4 and 3.5 show the mean values of maximum change in O2Hb (Fig. 3.4) and HHb (Fig. 3.5) parameters during and 5 minutes after manual needle acupuncture or laserneedle acupuncture.
Fig. 3.4: Changes in µmol of oxyhemoglobin (O2Hb) during needling of a placebo point, 3 hand acupuncture points, 2 ear acupuncture points, 2 acupuncture points from TCM, a combination of hand, ear and body acupuncture as well as laserneedle stimulation and an intensity-increased (+ 30 %) laserneedle acupuncture (from left to right) during and 5 minutes after acupuncture.
38
Fig. 3.5: Cerebral changes (generally decreases) in desoxyhemoglobin (HHb). For further descriptions see Fig. 3.4.
It is obvious that needling and stimulation of the placebo point does not lead to marked changes in cerebral NIRS parameters during and 5 minutes after acupuncture. Manual needling and laserneedle stimulation leads to a marked increase in O2Hb (compare Fig. 3.4) and simultaneous decrease in HHb (compare Fig. 3.5) when using the combined Korean hand acupuncture (E2) and Chinese hand acupuncture (Yan Dian), as well as TCM-body (Zhanzu and Yuyao) acupuncture, as well as combined body, ear, and hand acupuncture. This effect is still present 5 minutes after removing the needles or deactivating laserneedle stimulation. An almost negligible, but contrary behavior of O2Hb and HHb occurs when both ear points (eye and liver) are needled or stimulated with laser. None of the acupuncture stimulation methods or combinations resulted in significant changes in standard monitoring parameters (blood pressure).
3.4
Discussion
One of the main advantages of the laserneedle technique is its noninvasiveness. It is possible to apply the laser in such a manner, that the test
39 person cannot feel optical stimulation of the acupuncture point. In addition, the acupuncturer does not need to know if the system is activated or deactivated. Thus, double-blind studies using this new method are possible in acupuncture research for the first time. This method of study was already performed by our research group [14] and included simultaneous and continuous monitoring of blood flow velocity in the posterior cerebral artery and the middle cerebral artery in 17 healthy volunteers. This study showed that laserneedle stimulation of distant acupuncture points at hands and feet (Hegu, Zusanli, Kunlun, Zhiyin) is able to achieve marked and specific changes in cerebral blood flow velocity [12,14]. Even though laser puncture using Low-Level-Laser stimulation devices is an established method, measurable cerebral effects lie far below conventional needle acupuncture [15]. The results from the first studies [11,12,14] using the laserneedle system revealed significant changes in cerebral parameters (blood flow velocities), which were otherwise only achieved by manual needle acupuncture. The proportion of maximum change in blood flow velocity (needle/laserneedle) is approximately factor 2. Since Chinese medicine and acupuncture are considered an integrative part of TCM based on energetic processes, the registration of changes in the cerebral metabolism could express energetic processes in the brain and obviously plays a key role in investigating the effects of acupuncture. To date, it has not been possible to obtain non-invasive and continuous results regarding regional cerebral oxygenation. Near-infrared spectroscopy can register changes in oxygenation in the cerebral vascular region very sensitively. The advantages of transcranial oximetry are its noninvasiveness, low risks and continuity, as well as its easy and time-saving application. A wide range of indications are the result for the potential use of this spectroscopic method [4]. A number of factors which can influence adequate interpretation of data must be considered. Contamination with surrounding light, mechanical irritations, intracerebral hematoma, misplacement of optodes or other user errors are just some possibilities which should be noted [4]. A number of studies which deal with NIRS conclude that NIRS can exactly determine extremely small changes in cerebral hemodynamics, as a response to different functional stimulations. In this study [5,6], 328 systematic NIRS registrations on healthy volunteers during manual and laserneedle acupuncture stimulation were performed for the first time. The results from two preceding publications [8,9] were the reference points for this study.
40
The first study regarding acupuncture and NIRS [8] indicated that the changes in the occipital region after acupuncture stimulation in 3 healthy volunteers, was measurable and reproducible in each of the test persons. In the second study [9], NIRS-changes were measurable and reproducible at the central region after acupuncture stimulation at the Hegu point. This study showed, that reproducible changes in frontally monitored NIRS parameters could be determined, after stimulation of specific eye acupuncture points. In general, changes in NIRS parameters are unspecific and we do not know if an isolated decrease in saturation is caused by an increase in cerebral oxygenation consumption or results from a decrease in cerebral blood flow. Therefore, not only the extent of oxygenation is shown, but the interaction between oxygenation and desoxygenation is reflected. This is possible since the measurement zone is mainly dominated by the venous part of the cerebral vascular bed (~ 75 %). The arterial part (~ 20 %) or the capillary (~ 5 %) flow region is respectively smaller [4]. For these reasons, we were able to determine changes, which for example occur due to an increase in oxygenation. Which ruling mechanisms are present is still unclear. Increased desoxygenation by stimulus-induced neuronal activation, i.e. caused by changes in membrane potentials or release of neurotransmitters could be possibilities [16]. For whatever reason, acupuncture obviously influences the oxygen metabolism of the brain in healthy test persons. Similar to this study using ear acupuncture, a paradox contra-directional change in blood flow velocity (increase) and regional cerebral O2-saturation (decrease) occurred in a vascular based case of dementia, when an individually adapted acupuncture scheme was used [16]. The described case report showed that acupuncture could improve the clinical status of vascular dementia. Using NIRS and transcranial Doppler sonography, we were able to register the effects on cerebral blood flow velocity and the O2-metabolism. In combination with clinical findings, an inverse decrease in regional cerebral O2-saturation during simultaneous increase in cerebral blood flow velocity during acupuncture could be interpreted, as a sign of increased cerebral oxygenation. A decrease in regional cerebral O2-saturation does not necessarily indicate a poor condition of the O2-metabolism in the sense of reduced oxygen supply, however could also document the beneficial effects of regionally increased oxygenation, activated by acupuncture [16]. In a similar manner, the minor contradirectional regional changes in NIRS parameters using ear acupuncture could be interpreted, since the monitoring method conveys the balance between oxygenation and desoxygenation.
41 Further studies are necessary to investigate the importance of these phenomena on acupuncture, since not only the influence in general and in detail of laser acupuncture, but also the influence of combined ear and body acupuncture, are still discussed controversially. Spectroscopic methods probably are useful tools for this investigations.
3.5
Acknowledgements
The authors thank Ms. Lu Wang MD for performing the acupuncture, Ms. Evamaria Huber for help in data recording and Ms. Petra Petz MSc for her valuable support in data analysis (all Department of Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz).
3.6
References
Litscher G (2001) High-Tech Akupunktur®. Pabst Science Publishers, Lengerich Berlin Düsseldorf [2] Litscher G, Cho ZH (Eds.) (2000) Computer-Controlled Acupuncture®. Pabst Science Publishers, Lengerich Berlin Düsseldorf Riga Scottsdale Wien Zagreb [3] Cho ZH, Wong EK, Fallon J (2001) Neuro-Acupuncture. Q-puncture, Los Angeles [4] Litscher G, Schwarz G (Eds.) (1997) Transcranial cerebral oximetry. Pabst Science Publishers, Lengerich Berlin Düsseldorf Riga Scottsdale Wien Zagreb [5] Litscher G, Schikora D (2002) Nahinfrarot-spektroskopische Untersuchungen zur Nadel- und Lasernadelakupunktur. AKU Akupunktur Theorie und Praxis 3: 140-146 [6] Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 [7] Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I, Eger E (1998) Effects of acupuncture on the oxygenation of cerebral tissue. Neurol Res 20/S1: 28-32 [8] Litscher G, Wang L (2000) Zerebrale Nahinfrarot-Spektroskopie und Akupunktur – Ergebnisse einer Pilotstudie. Biomed Technik 45: 215218 [9] Litscher G, Wang L, Huber E (2002) Veränderungen zerebraler nahinfrarot-spektroskopischer Parameter während manueller Akupunkturnadelstimulation. Biomed Technik 47: 76-79 [10] Litscher G, Wang L (2002) Computergestützte Objektivierung der Grenzen der Akupunktur. AKU Akupunktur Theorie und Praxis 30/1: 1319 [1]
42 [11] Litscher G, Schikora D (2002) Cerebral effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 [12] Litscher G, Schikora D (2002) Neue Konzepte in der experimentellen Akupunkturforschung - Computerkontrollierte Laserpunktur (CCL) mit der Laserneedle® Technik. Der Akupunkturarzt / Aurikulotherapeut 28(3): 18-28 [13] Litscher G (2002) Computer-based objectivation of traditional Chinese-, ear- and Korean hand acupuncture, Needle-induced changes of regional cerebral blood flow velocity. Neurol Res 24: 377-380 [14] Litscher G, Schikora D (2002) Effects of new noninvasive laserneedles on brain function. IFMBE Proceedings, 2nd European Medical & Biological Engineering Conference (EMBEC), Vienna, December 2002: 996-997 [15] Litscher G, Wang L, Wiesner-Zechmeister M (2000) Specific effects of laserpuncture on the cerebral circulation. Lasers Med Sci 15: 57-62 [16] Litscher G, Schwarz G, Wang L, Sandner-Kiesling A (2002) Akupunktur bei vaskulär bedingtem dementiellem Abbau. Jahrestagung der Österreichischen Alzheimer-Gesellschaft. 14. Klagenfurter Arbeitstagung für Neurologie. 24. - 25. Mai 2002, Klagenfurt / Austria
43
4.
Communication between acupoint and brain proved by ultrasound G. Litscher, L. Wang, N.H. Yang
4.1
Introduction
Transcranial Doppler ultrasonography (TCD) provides a noninvasive, rapid and continuous assessment of blood flow velocity in cerebral arteries. Using new probe holder constructions, it is possible to record blood flow patterns in various cerebral arteries simultaneously and continuously [1-4]. Acupuncture has been used as a therapeutic medical technique in China for thousands of years and is indicated for a wide variety of conditions [5,6]. However, evidence of quantitative measurable effects of acupuncture is still rare in the scientific literature. We have reported a number of quantifiable effects of acupuncture on cerebral perfusion and cerebral oxygenation [14,7-16]. In the present study we investigated the specific effects of laserneedle acupuncture of two acupuncture schemes on the mean blood flow velocity in the anterior (ACA) and posterior (PCA) cerebral arteries in a cross-over study design.
4.2 4.2.1
Methods and materials TCD monitoring of the anterior and posterior cerebral arteries with a new probe holder
Doppler sonographic signals were recorded simultaneously in the left ACA and the right PCA with a Multi-Dop T system (DWL Electronic Systems GmbH, Sipplingen, Germany). Two 2-MHz probes were used in a multidirectional ultrasound probe holder.
44
ACA - Acupuncture
Ying Xiang (LI.20)
Fig. 4.1: Monitoring of the blood flow profiles in the anterior cerebral artery (ACA) and the posterior cerebral artery (PCA) and localization of the acupuncture point Ying Xiang.
The A1 segment of the ACA was assessed in its entirety at depths between 58 and 88 mm. The direction of flow in the ACA was away from the ipsilaterally placed probe. The PCA was found by aligning the transducer slightly posteriorly and inferiorly from the bifurcation of the internal carotid artery. Between a depth of 60 to 78 mm, its P1 segment was found and showed a direction of flow toward the transducer. The mean blood flow velocity (vm) is an important parameter [1,8], because it describes the most intense mean values of Doppler frequency at every interval of the spectrum [17]. Forty vm values were averaged in each patient in five phases (a: 5 minutes before acupuncture; b - d: during laserneedle acupuncture and e: 2 minutes after stimulation). The averaged values of the five measured phases were compared for each subject.
4.2.2
Participants
Blood flow profiles in the ACA and PCA were measured before, during and after the acupuncture sessions in 22 adults (mean age 24.4 + 2.6 years; range 21 – 29 years). None of the subjects was under the influence of centrally active medication. They were fully informed about the nature of the
45 investigation and gave informed consent. During the experiments the subjects were in a relaxed and comfortable positon on a bed in our laboratory. Then the TCD monitoring equipment was positioned. After a 10minute resting period the laserneedle stimulation was activated for a duration of 20 minutes.
4.2.3
Laserneedle acupuncture
Two acupuncture schemes were tested in two sessions in the same persons. One scheme (including Yingxiang) was chosen to influence the olfactory system (Figs. 4.2 - 4.4) and one (including Zhiyin) to stimulate the optical system.
PCA ACA NIRS - sensor
Fig. 4.2: Healthy volunteer during laserneedle stimulation and TCD-registration. Additionally a sensor was placed frontally for the registration of near infraredspectroscopic signals (NIRS).
Yingxiang (LI.20) Location: Between ala nasi and nasolabial groove. Indication: Rhinitis, blocked nose, common cold, nose bleeding, facial paralysis, trigeminal neuralgia, toothache. Hegu (LI.4) Location: At the highest point of the m. adductor pollicis with the thumb and index finger adducted. Indication: The most important analgesic point; stimulation of this point relieves pain in all parts of the body. The specific effect on the
46 head, especially in headache has been verified by clinical research. Pianli (LI.6) Location: 3 cun proximal to Yangxi (LI.5) on the line connecting Yangxi with Quchi (LI.11). Indication: Dry throat, rhinitis, throat pain, redness of the eye, tinnitus, deafness, sore throat, edema. Guangming (GB.37) Location: On the anterior side of the fibula, 5 cun proximal to the malleolus lateralis. Indication: Eye disorders, headache, mental disorders. Taichong (Liv.3) Location: Between the first and second metatarsal bones, 2 cun proximal to the margin of the web. Indication: Distal point for eye disorders, pain and tension of the head and chest, urogenital, endocrine and metabolic disorders.
47
olfactory epithelium
Fig. 4.3: Schematic presentation of the olfactory epithelium (modified according to JW Karapelou, Spektrum der Wissenschaft Spezial, 4/1999).
48
Fig. 4.4: Functional magnetic resonance imaging: activation during chemical stimulation (modified according to DH Zald et al. 1997; http://james.psych.umn.edu/olfactory.html). Note the dominance on the left.
4.2.4
Statistical Analysis
The data were tested with analysis of variance (one-way repeated-measure ANOVA) with SigmaStat software (Jandel Scientific Corp., Erkrath, Germany). The results were expressed as means + standard error (Cx + SE). The criterion for significance was p < 0.05.
4.3
Results
Figure 4.5 shows an example of increased vm in the ACA during laserneedle acupuncture. Stimulation of acupoint Yingxiang was repeated and the changes in vm were reproducible.
49
Laserneedle - specific effects ACA - PCA vm (cm/s)
before
during
laserneedle-acupuncture time 1 min
Fig. 4.5: Trend of the mean blood flow velocity vm in cm/s in the left anterior cerebral artery (ACA) and the right posterior cerebral artery (PCA) before and during laserneedle acupuncture in a 24-year-old volunteer. The arrow marks the beginning of stimulation.
Figure 4.6 (middle and lower panel) summarizes the results in all 22 subjects for both acupoint schemes. The values of vm in the ACA increased significantly (p<0.001) using acupuncture scheme A (b - d) and were higher at the end of the investigation (e) than before acupuncture (a). Insignificant changes (n.s.) in vm were seen in the PCA. However, with the vision-related acupoint scheme B the same subjects showed a significant increase of vm in the PCA without significant changes in the ACA.
50 Healthy volunteers n=22 12 female, 10 male, 21 - 29 years ( 24.4 + 2.6 years; x + SD ) R
laserpuncture scheme A
laserpuncture scheme B
Anterior cerebral artery (ACA)
Anterior cerebral artery (ACA)
50
52 51
49
*)
48
50
47
49
46
48
45
n.s.
47
a
b
c
d
a
e
b
c
d
e
*) p < 0.001
Posterior cerebral artery (PCA)
Posterior cerebral artery (PCA) 47
45
46
44
45
43
*)
44
42
n.s.
41
43 42
40 a
b
c
d
e
a
b
c
d
e
*) p < 0.002
Fig. 4.6: Healthy volunteers, acupuncture points and graphic presentation (means) of the results of the mean blood flow velocity of the anterior cerebral artery (ACA) and the posterior cerebral artery (PCA) before (a), during (b - d) and after (e) laserneedle stimulation. The arrows mark the relative maximum changes during laserneedle stimulation referring to the basic value.
51
vm (cm/s) 50
Specific cerebral effects of laserneedle-acupuncture p = 0.001*
48 46 ACA PCA
44 42
n = 22
40 38
a
*
b
c
d
e
One Way Repeated Measures Analysis of Variance (Tukey Test)
Fig. 4.7: Absolute changes in vm during laserneedle acupuncture.
'vm (cm/s)
p = 0.001*
3
2,5 2 1,5 ACA
1
PCA
0,5
n = 22
0 -0,5 -1 a
*
b
c
d
e
One Way Repeated Measures Analysis of Variance (Tukey Test)
Fig. 4.8: Relative changes in vm during laserneedle acupuncture.
52
Specific cerebral effects of laserneedle-acupuncture vm (cm/s)
50
n.s.
48 46 44
ACA PCA
42
n = 22
40 38 a
b
c
d
e
Fig. 4.9: Absolute changes in vm during laserneedle acupuncture.
'vm (cm/s) 3
n.s.
2,5 2 1,5 1
ACA
0,5
PCA
0
n = 22
-0,5 -1 a
b
c
d
e
Fig. 4.10: Relative changes in vm during laserneedle acupuncture.
53
4.4
Discussion
Transcranial Doppler ultrasonography measures blood flow profiles in cerebral arteries. The technique is used to detect stenoses, emboli and malformations of intracranial arteries, assess cerebral collateral circulation before surgery, monitor cerebral vasospasm, and document cerebral circulatory arrest, as well as for intraoperative monitoring. Acupuncture is a form of traditional Chinese medicine (TCM) that has developed over thousands of years. Until now, modern Western medicine has used acupuncture mostly for complementary or supportive purposes. There are hundreds of acupoints on the human body. These are points at which according to TCM the flow of the vital force Qi can be stimulated [5,6]. In this study we used laserneedles, a new way to stimulate these points. In previous studies we have found that the brain is the key to understanding acupuncture’s effects [1-4,7-14]. New experimental constructions to measure ultrasound, light and bioelectrical processes can reproducibly demonstrate effects of acupuncture in the brain. We have shown that acupuncture with needles can increase overall cerebral blood flow. Studies with biosensors and probes in a specially designed helmet showed that acupuncture can increase the blood flow velocity in the middle cerebral artery and increase the oxygen supply to the brain. The present study is a further step to objectify the effects of acupuncture. In 22 participants we found that laserneedle acupuncture of specific acupoints increases blood flow in specific regions of the brain. An acupuncture scheme including two points in the face (Yingxiang) which TCM places in connection with the olfactory system increased mean blood flow velocity in the ACA significantly (p < 0.001). The ACA supplies most of the frontal and medial mass of the cerebrum including part of the olfactory cortex. At the same time, blood flow in the PCA stayed nearly unchanged. In contrast, an acupuncture scheme including a point on the foot (Zhiyin) which is in connection with the optic system increased blood flow in the PCA significantly (p = 0.002). Simultaneously blood flow in the ACA stayed nearly unchanged. Cho et al. [16] have described similar effects in the brain by stimulating vision-related acupoint Zhiyin with functional magnetic resonance imaging
54 and after light stimulation. Control studies with stimulation of other points on the foot did not produce specific activation in the visual cortex.
Acupuncture - fMRI
Vis. Ref.
Acup. Acup.
(light) light)
(Zhiyin)
Fig. 4.11: Functional magnetic resonance imaging (fMRI) at the Medical University of Graz (fMRI-results: Cho et al. [2]).
In our study we measured the blood flow profiles in the left ACA and the right PCA. This procedure was chosen for technical reasons and due to previous reports in the literature. Zald et al. [17] found that olfactory stimuli increased regional cerebral blood flow exactly in the left lateral orbitofrontal cortex. Cerebral blood flow in this study was measured with a slow bolus O15 water technique and positron emission tomography. We are convinced that sophisticated biomedical technology, particularly noninvasive ultrasound techniques, can objectify some effects of traditional Chinese medicine. In acupuncture the brain likely plays a key intermediate role. However, brain activity in and of itself does not explain anything about the healing power of acupuncture.
55
4.5
Acknowledgements
The authors thank Ms. Ingrid Gaischek MSc (Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz) for her valuable help.
4.6 [1] [2]
[3] [4] [5] [6] [7]
[8] [9]
[10] [11] [12]
References Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I (1998) Robotic transcranial Doppler sonography probes and acupuncture. Intern J Neurosci 95: 1-15 Litscher G, Yang NH, Schwarz G (1999) Computerkontrollierte Akupunktur®: Eine neue Konstruktion zur simultanen und kontinuierlichen Erfassung der Blutflußgeschwindigkeit in der A. supratrochlearis und A. cerebri media. Biomed Technik 44: 58-63 Litscher G, Wang L, Yang NH (1999) Ultrasound-monitored effects of acupuncture on brain and eye. Neurol Res 21: 373-377 Litscher G, Yang NH, Wang L (1998) Quantitative Separation spezifischer Akupunktureffekte von Gehirn und Auge mittels bidirektionaler Ultraschallmeßkonstruktion. AKU 26(4): 212-217 Engin I: Chinese acupuncture and moxibustion. Shanghai China, Publishing House of Shanghai College of Traditional Chinese Medicine, 1990 Mao-Liang Q (1996) Chinese acupuncture and moxibustion. Churchill Livingstone, London Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I (1997) Transkranielle Doppler-Sonographie - Robotergesteuerte Sonden zur Quantifizierung des Einflusses der Akupunktur. Biomed Technik 42: 116-122 Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I, Eger E (1998) Effects of acupuncuture on the oxygenation of cerebral tissue. Neurol Res 20(1): 28-32 Litscher G, Schwarz G, Sandner-Kiesling A (1997) Transcranial near infrared spectroscopy and transcranial Doppler sonography during acupuncture. In Litscher G, Schwarz G (Eds) (1997) Transcranial Cerebral Oximetry. Pabst Science Publishers, Lengerich, pp. 184-198 Litscher G, Wang L, Wiesner-Zechmeister M (2000) Specific effects of laserpuncture on the cerebral circulation. Lasers Med Sci 15: 57-62 Litscher G, Schwarz G, Sandner-Kiesling A (1998) Computerkontrollierte Akupunktur®. Akupunktur Theorie und Praxis 26(3): 133-142 Litscher G, Wang L, Yang NH, Schwarz G (1999) Computer-controlled acupuncture – Quantification and separation of specific effects. Neurol Res 21:530-534
56 [13] [14]
[15] [16]
[17] [18]
Litscher G, Yang NH, Wang L (1998) Ultrasound-controlled acupuncture. Internet J Anesthesiology 2/4: http://www.ispub.com/journals/IJA/Vol2N4/acu.htm Litscher G, Yang NH, Wang L (1999) Acupuntura controlada por ultrasonidos. http://www.tmed.uam.es/dpto/anesne...tas/ijae/vol2n4e/articulos/acu.h tm Litscher G, Wang L (1999) Visualisierung von peripheren Durchblutungsänderungen während der Akupunktur mittels Thermographie. Biomed Technik 44: 129, 1999 Cho ZH, Chung SC, Park JP, Park HJ, Lee HJ, Wong EK, Min BI (1998) New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci 95: 2670-2673 McCartney JP, Thomas-Lukes KM, Gomez CR (1997) Handbook of Transcranial Doppler. Springer, New York Zald DH, Pardo PJ, Pardo JV et al (1997) Left orbitofrontal activation during aversive chemical stimulation. http://james.psych.umn.edu/olfactory.html
57
5.
Histological investigations regarding micromorphological effects of laserneedle illumination. Results of an animal experiment G. Litscher, W. Nemetz, J. Smolle, G. Schwarz, D. Schikora, S. Uranüs
5.1
Introduction
For the first time, laserneedle stimulation allows simultaneous and continuous laser illumination of individual acupuncture points [3,4]. Due to the contact of the laserneedle with the skin, the illuminated area at the acupuncture point remains constant and the relevant doses can be varied exactly by altering the duration of illumination. Goal of this animal experiment was to investigate the influence of laserneedle illumination on micro morphological structures of the skin and obtain objectified information regarding the effects of characteristic densities and illumination doses for laserneedles.
5.2 5.2.1
Methods Procedure
In this animal study, we performed experiments regarding the microcirculation in the skin and surface skin temperature, before, during and after laserneedle stimulation. We used a sus scrofa domesticus, which was put under general anaesthesia in the animal surgical unit, at the Department of Surgical Research, University Clinic of Surgery (Figure 5.1). The study was performed according to the rules of the ethical commission (animal study approval number GZ 66.010/10-BRGT/2003).
58
Fig. 5.1: Animal experimental investigation with laserneedle stimulation. Illumination of the skin using 8 laserneedles (circular positioning scheme). The microcirculation and temperature sensor is located in the middle of the positioning scheme. Pre-medication was done in two steps on the day of intervention: a) Orally: Diazepam (Gewacalm®) 10 mg, Ketamin (Ketanest S®) 250 mg, Azaperom (Stresnil®) 80 mg. b) 20 min after oral pre-medication, intramuscular: Atropin 0.5 mg, Diazepam (Gewacalm®) 20 mg, Ketamin (Ketanest S®) 50 mg, Azaperom (Stresnil®) 80 mg. Anaesthesia was started 20 minutes after pre-medication: Etomidate-®Lipuro 40 mg, Fentanyl 0.5 mg i.v. Intubation was done during spontaneous respiration and muscle relaxation with Pancuroniumbromid (Pavulon®) 4 mg. Maintenance of anaesthesia was performed with: Thiopental 4 g, Fentanyl 1.5 g, Pancuroniumbromid (Pavulon®) 20 mg/500 NaCl 0.9 % as continuous instillation. Ventilation was performed instrumentally according to characteristic biometric data. At the time of excision, hemodynamic parameters (blood pressure 130/70 mmHg; heart rate 80/min; central venous pressure 5 mmHg), as well as oxygenation (SaO2 99 %) and ventilation (etCO2 38 mm) were all in the normal range. Data registration of the measurement parameter Flux (= product of mean flow velocity and concentration of red blood cells), surface skin temperature and room temperature were measured during anaesthesia. A total of five measurement values were analyzed (a = 2 min before; b = 2 min, c = 10 min, d = 18 min after beginning stimulation and e = 2 min after deactivating laserneedle stimulation; compare Figure 5.3).
59 After completing the experiment, four histological samples from the shaved cutis at the thoracic-abdominal transition were investigated, two had been illuminated with laser the other two were used as negative controls.
5.2.2
Laserneedle stimulation
Laserneedle stimulation is new optic method, which is used for stimulating acupuncture points. Illumination of different variations and combinations on the body, ear, or hand are possible. Figure 5.2 shows the characteristic emission of a fitted laserneedle, which was used in this study. The coherence of laser illumination at the distal exit point was measured with Michelsoninterferrometry. The laserneedles used (wavelength: 685 nm) emitted red light in a „continuous wave“ mode with an output of 30 - 40 mW per laserneedle, resulting in a power density of 4.6 W/cm² or an energy density of ~ 4.6 kJ/cm². The transmitted energy into the skin is 55 J per laserneedle during a treatment period of 20 minutes. 1
intensity [a.u.]
emission wavelength: 685 nm
laser-needle emissioncharacteristics
total output power at distal end: 30 mW
optical cladding fibre core
-2
-1
1
2
optical fibre diameter [ a.u.] Fig. 5.2: Emission characteristics of a laserneedle (a.u. = arbitrary units).
5.2.3
Laser Doppler flowmetry and temperature measurement
Laser Doppler signals were registered with a Laser Doppler device (DRT4), by Moor Instruments Ltd. (Devon, England). Probe output is defined as 1 mW. Laser wavelength was 780 nm, the raw signal was filtered with a digital filter from 20 Hz to 22.5 kHz. A DPIT–probe (diameter 8 mm, length
60 7 mm) was used for registration. An additional unit for measuring temperature (accuracy 0.1 °C) was integrated.
5.3
Results
Figure 5.3 shows the results from the three measurement parameters at different measurement times before (a), during (b - d) and after (e) laserneedle activation. Skin surface temperature and room temperature parameters did not show marked changes, whereas the Flux value increased significantly 2 minutes after activation (b) and reached a maximum at the end of laserneedle stimulation at measurement point (d). Thereafter, this value was reduced to its initial level. Temp. (°C) 45
Temp. R.-Temp.
Flux 40 (a.u.)
Flux
35 30 25 20 a
b
c
d
e
20 min
Fig. 5.3: Surface body temperature (Temp.), room temperature (R.-Temp.) and Flux (= product of mean flow velocity and concentration of erythrocytes) in a.u. (arbitrary units) before (a), during (b - d) and after (e) 20-minute laserneedle stimulation. Note the increase in the Flux parameter during illumination.
The examination of the four histological samples revealed the following: The hematoxylin-eosin samples of the illuminated cutis did not reveal any changes in comparison with the control biopsies. In particular, no necroses of the epidermis or single keratinocytes was evident, nor were changes in the endothelial cells of the dermal blood vessels visible. No micro thrombosis or extravasation could be detected (Figure 5.4).
61
a
b
Fig. 5.4: Histological results of the illuminated (a) and not illuminated (b) cutis. No micro morphological differences are evident.
5.4
Discussion
Laser has become a term for future technology, precision, rapidity, and achievement. Although the discovery of laser dates back to Einstein, who founded the theory of stimulated emission in 1917, the history of laser in acupuncture is still young [8]. Questions regarding tissue damage caused by certain laser power densities arise repeatedly. Border values have been determined, however are currently being discussed very differently [2,8]. Goal of this animal experimental study was to objectify whether the illumination of the cutis with a new laser system (laserneedle stimulation) leads to tissue damage when used in acupuncture. We illuminated the cutis of a sus scrofa domesticus with 8 laserneedles and simultaneously registered microcirculatory parameters and temperature values with a laser Doppler flowmetry monitor. This technique allows the objectifying of circulation in the micro-capillary region, without influencing tissue structures. It is based on the Doppler-shifting of light when it hits moving parts (erythrocytes). This technique is mainly used in pharmacology for comparing measures which influence circulation, for controlling transplants and flaps in plastic surgery and for objectifying and classifying disease stages in angiological and dermatological research, as well as in occupational medicine [1,7,9]. It can also be applied for research in the fields of anaesthesiology, intensive medicine and neurosurgery [5,6]. Even though the microcirculation parameters indicate an increase in skin circulation after an illumination time of 20 minutes, histological
62 examinations did not show any signs of alterations in the examined layers of skin tissue. We assume that this results from the minimal absorption of the most important tissue parts such as water, haemoglobin, and melatonin, which is comparatively small at the emission wavelength of 685 nm of the laserneedles. This indicates that photons entering the tissue are scattered at the tissue molecules, however do not thermically counteract, as in processes of adsorption. The skin is more or less, transparent for laser at a wavelength of 685 nm, thus thermically induced tissue changes such as coagulation, ablation and carbonisation can not take place and were not provable in our experiments. Laser illumination of 685 nm used in the laserneedles and applied in a contact mode, with power densities between 1- 5 W/cm², did not induce measurable micro morphological changes in the illuminated skin [10]. The definition of relevant critical values, in particular, determination of wavelength dependent power densities which lead to micro-morphological tissue changes, will be clarified in further studies.
5.5
Acknowledgements
The authors thank cand. med. Evamaria Huber from the Department of Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University of Graz, for her assistance in data registration.
5.6 [1]
[2] [3] [4] [5] [6]
References Fagrell B (1994) Problems using laser Doppler on the skin in clinical practice. In: Belcaro GV, Hoffmann U, Bollinger A, Nicolaides N (1994) Laser Doppler. Med-Orion Publishing Company, London Los Angeles Nicosia, 49-54 Kert J, Rose L (1989) Clinical Laser Therapy. Scandinavian Medical Laser Technology, p. 13 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schwarz G, Dalageorgos K, Neger J, Kehl G (1996) LaserDoppler-Flowmetrie - Erfahrungen aus der Intensivmedizin. Biomed Technik 41: 166-169 Litscher G, Möller KO, Stollberger R, Schwarz G, Fuchs G, Baumgartner A, Leber K, Koop T, Ascher PW (1997) Laser-Doppler-
63
[7] [8] [9] [10]
Datenanalyse während interstitieller Laserthermotherapie unter Magnetresonanz-Kontrolle im Rahmen einer tierexperimentellen Studie. Biomed Technik 42: 93-96 Öberg P (1990) Laser-Doppler flowmetry. Crit Rev Biomed Eng 18: 125-163 Pöntinen PJ, Pothmann R (1998) Laser in der Akupunktur. Grundlagen, Indikation und Technik für die AkupunkturSchwerpunktpraxis. Hippokrates, Stuttgart Tenland T, Salerud EG, Nilsson GE, Öberg PA (1983) Spatial and temporal variations in human skin blood flow. Int J Microcirc: Clin Exp 2: 81-90 Litscher G, Nemetz W, Smolle J, Schwarz G, Schikora D, Uranüs S (2004) Histologische Untersuchungen zu mikromorphologischen Einflüssen von Lasernadelstrahlung. Ergebnisse einer tierexperimentellen Untersuchung. Biomed Technik 49: 2-5
64
6.
Effects of laserneedle stimulation on microcirculation and skin temperature G. Litscher, L. Wang, E. Huber
6.1
Introduction
Laser Doppler flowmetry (LDF) is a technique particularly used in the field of pharmacology for comparing measures which influence circulation, for controlling transplants and flaps in plastic surgery and for objectifying and classifying disease stages in angiological and dermatological research and in anesthesiology and intensive care medicine [1-6]. Flux (product of mean flow velocity and the concentration of red blood cells), for example, and the concentration of moving particles (erythrocytes) in the measurement volume are calculated. Recently, some reports in literature documented, that this method can also be applied in the field of acupuncture for scientific investigations [7, 8]. In this chapter, the use of laserneedle stimulation under real circumstances is examined, based on LDF- monitoring results.
6.2 Method and volunteers 6.2.1
Laser Doppler flowmetry
A laser Doppler monitor DRT4 (Moor Instruments, Millwey, Axminster, England) was used to determine Flux and temperature. Probe output was defined with 1 mW. Edge frequencies were 20 Hz and 22.5 kHz. The temperature unit (5 °C to 50 °C) had a resolution of 0.2 °C and accuracy of 0.5 °C. In addition to an RS-232 interface, this instrument disposes of analogous signals (0 – 10 V) as an output voltage. The instrument has the following dimensions: 280 x 160 x 360 mm and weighs 8 kg. Several measurement probes are available for the DRT4 monitor. The results documented in this study were obtained with the DPIT probe (diameter 8 mm, length 7 mm) (Fig. 6.1).
65
Fig. 6.1: Laser Doppler probe.
6.2.2
Volunteers and procedure
Twenty-two healthy volunteers (12 female, 10 male), with a mean age of 24.4 + 2.6 years (21 - 29 years) were examined. At the time of measurement, none of the volunteers were under the influence of drugs. They were informed about the procedure and gave their consent. Approval of this study was obtained from the Ethical Commission of the Medical University of Graz (Laserneedle-Stimulation; 13-048 ex 02/03). Continuous measurement of microcirculation parameters and temperature was started, after a resting period of 10 minutes. After reaching the “steadystate”, the following acupuncture points on the right hand were stimulated with a laserneedle (compare Fig. 6.2): Hegu (LI.4) Localization: At the highest point of the M. adductor pollicis, when the thumb lies against the index finger. Indication: Hegu is the most important analgesic point. Pain conditions; particularly massive manual stimulation relieves pain in the entire body. Specific cerebral effects of this distant point could be proven in clinical studies.
66
Laserneedle – temperature / Flux
Fig. 6.2: Laser Doppler perfusion and temperature monitor DRT4 (Moor Instruments, Millwey, Axminster, England) and laserneedle stimulation.
The laserneedle was fixed to the skin at the acupuncture point with adhesive tape, after previous cleaning of the skin with alcohol. A semi-conductor laser with an emission wavelength of 685 nm was used as the light source. Laser intensity was 60 mW. Details regarding the stimulation method can be found in the previous chapters. The Laser Doppler probe (compare Fig. 6.1) was applied at a distance of 1 cm from the laserneedle. This distance was selected based on the given geometric dimensions of the probe holder (compare Fig. 6.1) and a supposed optic depth in the infrared range of 1 cm. Temperature at the measurement point and room temperature were determined for comparison. Figure 6.3 shows the different measurement times schematically (a - e) before, during and after laserneedle stimulation.
67 b
c
1 min
d 1 min
10 min
a
e 20 min
2 min
2 min
laserstimulation active
Fig. 6.3: Measurement profile and measurement times (a - e).
6.2.3
Statistical analysis
Data were analyzed using „Friedman Repeated Measures ANOVA on Ranks“ with the computer program SigmaStat (Jandel Scientific Corp., Erkrath, Germany). The Tukey test was used for post hoc analysis. Results from the conditions before (a), during (b - d) and after (e) laserneedle acupuncture were noted as mean values (Cx + standard error SE). The level of significance was defined as p < 0.05.
6.3
Results
Figure 6.4 summarizes the results of the three parameters; Flux, hand and room temperature at the different measurement times (compare Fig. 6.3).
68
Laserneedle – temperature and Flux p = 0.005* p = 0.002*
Temp. (°C) Flux (a.u.)
34 32 30 28
Temp. R.-Temp. Flux
26 24
n = 22
22 20
a
b
c
d
e
20 min *
Friedman Repeated Measures Analysis of Variance on Ranks (Tukey Test)
Fig. 6.4: Changes in Flux (= product of concentration and velocity of erythrocytes), skin (Temp.) and room temperature (R.-Temp.) parameters before (a), during (b - d) and after (e) laserneedle stimulation at acupuncture point Hegu.
Observe the highly significant changes in Flux (p = 0.005) as well as the increase in temperature at the measurement site (p = 0.002). Even 2 minutes after deactivating laser stimulation (measurement time e), Flux was no longer significant but still markedly higher. Temperature at the stimulation point (distance 1 cm) also showed an obvious increase, which reached its maximum at measuring time d. The nearly constant room temperature was simultaneously registered as a comparative parameter.
69
Laserneedle - microcirculation left hand
right hand
Fig. 6.5: Eight deactivated laserneedles before starting the examination.
left hand
right hand
B.A., 25y, f
Fig. 6.6: Activated laserneedles during examination procedure.
70
10 min
30 min
10 min B.A., 25y, f
s
Fig. 6.7: Changes in parameters regarding concentration of erythrocytes (c1, c2) and temperature (t1, t2) at the left, or right hand in the phases before (10 min), during (30 min) and after (10 min) laserneedle stimulation.
6.4
Discussion
The Laser Doppler technique is a suitable method for measuring the concentration and velocity of moving blood cells in surface vessels. Penetration depth is confined to about 1 mm. Laser light is usually guided to the output point via light conductors. Due to the Doppler effect, frequency shifts of scattered light take place and can be determined by measuring flow velocity. Possible advantages of this technique particularly in acupuncture research are currently being evaluated [7-13]. Negative factors regarding this method per se are the failing standardization combined with difficult interpretation of clinical data and high purchasing costs of the LDF equipment. Advantages of this method are its time-saving aspect, non-invasiveness, continuous monitoring ability and user friendliness.
71 The results from this study indicate that the energy dose emitted by a laserneedle in 20 minutes, is high enough to increase local skin temperature and subcutaneous tissue temperature (mean of 0.7 °C ; p = 0.02). Thus, the modality of periphery stimulation with laserneedles is not only optical but also thermal. Light dispersion on the skin was measured using a new device (O2C Oxygen to see, LEA Medizintechnik, Giessen, Germany). Figure 6.8 shows that even at a distance of 4 cm the laser light from the laserneedle (685 nm) can be detected.
Laserneedle stimulation 4 cm
3 cm
2 cm
1 cm
1 cm 2 cm 3 cm 4 cm
Fig. 6.8: Light dispersion on the skin. Note the peak in the spectrum at 685 nm.
In addition it is very interesting that especially Flux is significantly increased (p = 0.005) only 2 minutes after beginning laserneedle stimulation. In other words, an improvement in local, peripheral microcirculation at the stimulation point takes place. This fact could prove to be useful in dermatologic indications. The results from this study should induce further investigations regarding the evaluation of temporal and spatial (laser Doppler imaging) changes in microcirculation parameters, during and after laserneedle stimulation. Possible artifacts, as described in literature should be reduced further [4].
72
6.5 [1]
[2] [3] [4] [5] [6]
[7]
[8]
[9] [10]
[11] [12]
[13]
References Fagrell B (1994) Problems using laser Doppler on the skin in clinical practice. In: Belcaro GV, Hoffmann U, Bollinger A, Nicolaides AN (1994) Laser Doppler. Med-Orion Publishing Company, London-Los Angeles-Nicosia, 49-54 Öberg P (1990) Laser-Doppler flowmetry. Crit Rev Biomed Eng 18: 125-163 Litscher G, Schwarz G, Boggett D (1995) Laser Doppler flowmetry – Peripheral microcirculation during cessation of cerebral and cardiocirculatory function. Biomed Technik 40: 195-199 Litscher G, Schwarz G, Dalageorgos K, Neger J, Kehl G. (1996) Laser-Doppler-Flowmetrie – Erfahrungen aus der Intensivmedizin. Biomed Technik 41: 166-169 Litscher G, Möller KO, Ratzenhofer-Komenda B, Schwarz G, Koop T, Kovac H (1997) Laser Doppler flowmetry in the hyperbaric environment. Lasers Med Sci 12: 342-346 Litscher G, Möller KO, Stollberger R, Schwarz G, Fuchs G, Baumgartner A, Leber K, Koop T, Ascher PW (1997) Laser-DopplerDatenanalyse während interstitieller Laserthermotherapie unter Magnetresonanz-Kontrolle im Rahmen einer tierexperimentellen Studie. Biomed Technik 42: 93-96 Sandner-Kiesling A, Litscher G, Voit-Augustin H, James RL, Schwarz G (2001) Laser Doppler flowmetry in combined needle acupuncture and moxibustion: A pilot study in healthy adults. Lasers Med Sci 16: 184-191 Litscher G, Wang L, Huber E, Nilsson G (2002) Changed skin blood flow perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers Med Sci 17: 19-25 Litscher G, Wang L, Nilsson G (2001) Laser Doppler Imaging und Kryoglobulinämie. Biomed Technik 46: 154-157 Sprott H, Jeschonnneck M, Grohmann G, Hein G (2000) Microcirculatory changes over the tender points in fibromyalgia patients after acupuncture therapy (measured with laser-Doppler flowmetry). Wien Klin Wochenschr 112(13): 580-586 Suter B, Kistler A (1994) Does acupuncture modify skin circulation via the autonomic nervous system? Schweiz Med Wochenschr 62: 36-38 Blom M, Lundeberg T, Dawidson I, Angmar-Mansson B (1993) Effects on local blood flux of acupuncture stimulation used to treat xerostomia in patients suffering from Sjogren’s syndrome. J Oral Rehabil 20(5): 541-548 Cramp AF, Noble JG, Lowe AS, Walsh DM (2001) Transcutaneous electrical nerve stimulation (TENS): the effect of electrode placement upon cutaneous blood flow and skin temperature. Acupunct Electrother Res 26(1-2): 25-37
73
7.
Effects of acupressure, manual acupuncture and laserneedle acupuncture on EEG bispectral index (BIS) and spectral edge frequency (SEF) in healthy volunteers G. Litscher
7.1
Introduction
Noninvasive bioelectrical neuromonitoring is gaining more and more attention in anesthesia and critical care [1,2]. The bispectral index (BIS) and the spectral edge frequency (SEF) are important numerical descriptors of the EEG and both are mainly used for assessing depth of anesthesia [3]. If anesthetists rely on BIS and SEF to detect awareness, then it is very important to exclude other influences that could give false readings. It is known that a number of environmental and physiologic factors may affect BIS performance. Recently it has been reported that also nonpharmacological interventions such as acupressure can reduce BIS values significantly [4]. This study is a randomized, controlled partly blinded (laserneedle acupuncture) cross-over trial intended to investigate the effects of three nonpharmacological interventions (acupressure, manual needle acupuncture and laserneedle acupuncture) on two processed EEG variables (BIS, SEF) and a verbal stress score in healthy volunteers.
7.2 7.2.1
Material and methods Subjects
We studied 25 healthy volunteers (mean age r SD: 25.5 + 4.0 years, range 21 - 39 years; 15 women, 10 men; body weight 69.1 r 16.1 kg; height 173.5 r 9.3 cm). None of the subjects had neurological or psychological disorders and they were not taking any medication. They were partly informed about the nature of the investigation and were paid for their participation. The investigators recording EEG and sedation data were blinded to the intervention applied to the volunteers. The subjects were not informed which of the four interventions was effectively a control (acupressure on a control
74 point). The study was approved by the Ethics Committee of the Medical University of Graz (13-048 ex 02/03). Written informed consent was obtained from each subject.
7.2.2
Procedure and study design
The study was performed as a randomized, controlled cross-over trial. Four EEG electrodes (F7-Fpz, F8-Fpz, Fz = ground) and a noninvasive blood pressure cuff were attached to the volunteers after they arrived at the biomedical engineering laboratory. Two channels of spontaneous electrical activity were recorded from electroencephalographic electrodes (Zipprep™ self-prepping electrodes; Aspect Medical Systems Inc., Natick, MA, USA). The skin-electrode impedance was < 2 kOhm. Low cutoff frequency was 2 Hz and high cutoff frequency was 30 Hz. The EEG was measured continuously using an Aspect A-1000 system (Aspect Medical Systems Inc., version 3.12, Natick, MA, USA). A period of 5 min was allowed for each subject to obtain steady state BIS and SEF values. Thereafter with one of the four conditions - acupressure at the acupoint Yintang, manual needle acupuncture at Yintang, laserneedle acupuncture at Yintang or acupressure at a control point was started (Fig. 7.1). There were three treatments and additionally to investigate a possible placebo effect, we also used acupressure at a control point. The acupoint Yintang (Ex.1) is located midway between the medical ends of the two eyebrows at the root of the nose (see Fig. 7.1, a - c). To assess the reliability and validity of acupressure and manual needle acupuncture, pressure on the acupoint and the control point was applied by the same chinese medical doctor experienced in Traditional Chinese Medicine. The thumb pressure was estimated to be about 3 x 105 Pa (mean force measured ~ 30 N / 1 cm²; Pascal (Pa) = N/m²; 30/0.0001=3x105).
75
a
b
c
d
Fig. 7.1: Different conditions of the cross-over study design: (a) acupressure at the acupoint Yintang, (b) manual needle acupuncture at Yintang, (c) laserneedle acupuncture at Yintang, and (d) acupressure at a control point in a 25-year-old healthy female (with permission by the volunteer E.H.).
Manual needle acupuncture was performed using sterile single use needles 0.30 x 30 mm (Huan Qiu; Suzhou, China). After local disinfections of the skin the needling method was oblique, in caudal direction (0.5 cm) [5]. Stimulation for a duration of 20 sec in intervals of 2 minutes consisted of a combination of rotating and thrusting movements using a special manual acupuncture stimulation technique (sedation method). The needle was removed after 10 minutes. Laserneedle acupuncture at the acupoint Yintang was performed using a new method for optical stimulation. This method was reported by our research group in the scientific literature in 2002 [6,7]. The laserneedle-technique represents a new, noninvasive method for optical stimulation of acupuncture points. The laser used in this study emits red light in continuous-wave mode with an output power of 30 - 40 mW, which results in a radiant exposure energy of about 2.3 kJ/cm² at the acupuncture point during a stimulation time of 10 min [6].
76 Acupressure on the control point (location: 2 cm from lateral end of the left eyebrow; Fig. 1, d) was performed in similar manner as on the acupoint Yintang (duration 10 min). All subjects had four conditions applied (Fig. 1, a - d). The persons were in a semi-lying position with closed eyes. The choice of the stimulation procedure was randomized within a subject and the interval between the different sessions was at least 20 min.
7.2.3
Evaluation parameters
The main evaluation parameters were BIS and SEF90 during different conditions (Fig. 7.1) and time intervals (Fig. 7.2). Measurements were made at time points a - g (see Fig. 7.2). In any one condition we recorded BIS and SEF values continuously but sampled the data for subsequent analysis at 7 points. A single reading was taken at each point. The stimulation was not stopped at the time of reading. The whole study session lasted 2 – 3 hours. BIS and SEF90 represent single numbers, which should decrease continuously with decreasing level of consciousness (hypnosis). There are several review articles for methodological details of signal processing of BIS and SEF [3].
b
c
d
1 min 5 min
1 min
2.5 min
a
f
e
2.5 min
5 min
g
5 min
2 min
2 min
10 min
Fig. 7.2: Stimulation procedure and different measuring points (a=before, b f=during, g=after stimulation).
After five minutes of stimulation (Fig. 7.2, d) the subjects were asked to move their right hand to clarify that they were awake and not asleep. In addition before and after each stimulation mode the persons were asked to score the stress and tension that they had based on a verbal stress scale (VSS) from 0 (no stress) to 10 (maximum stress) [4]. Heart rate (HR) and noninvasive blood pressure (BP) were also recorded before and after
77 acupressure stimulation at Yintang (measurement points: 1 min before ‘a’ and 1 min after ‘g’ (comp. Fig. 7.2)).
7.2.4
Statistical analysis
The BIS and SEF data were tested with analysis of variance (one-way repeated measures ANOVA; similar data were found to be normally distributed in previous investigations) using SigmaStat (Jandel Scientific Corp., Erkrath, Germany). Dunnett’s method was used for post hoc analysis. VSS data were compared using paired t-test. The results were graphically presented as box plots (BIS and SEF) and as scatter plot (VSS). Changes were considered significant at a p-value < 0.05.
7.3
Results
All subjects completed the study. Figure 7.3 shows the decreases of BIS values during acupressure applied to the acupoint Yintang in all 25 healthy volunteers.
78
1
5
2
3
4
8
7
6
9
10
11
12
13
14
15
16
17
21
18
22
19
23
20
24
25
Yintang
n=25
10 min
Fig. 7.3: The trend of BIS values of 25 healthy volunteers (1 – 25) before, during and after acupressure performed on the acupoint Yintang. All subjects were awake. Note the significant decrease (min. BIS = 35; no. 14) due to acupressure.
Before the subjects were stimulated, their mean BIS values (r SD) were 97.4 (98 - 95) r 1.0 and their mean SEF values (r SD) were 23.9 r 4.1 Hz (right) and 23.5 r 4.9 Hz (left). The BIS and SEF values both decreased significantly (p < 0.001) after starting acupressure. After 5 minutes acupressure at the acupoint Yintang the mean BIS values were 62.9 (minimum 35; see no. 14 in Fig. 7.3) r 13.9, and the mean SEF values were 13.3 (minimum 2.9) r 8.1 Hz (right) and 13.8 (minimum 2.7) r 7.3 Hz (left). The release of acupressure caused an increase in BIS and SEF back to the baseline values before stimulation (compare Fig. 7.4).
79
120
100
BIS
80
60
40
p < 0.001 (b-f vs. a)
20
One Way Repeated Measures ANOVA (Dunnett‘s Method)
BIS
0 35 30 25
Hz
20 15 10 5
SEF r
p < 0.001 (b-f vs. a)
0 35
30 25
Hz
20 15 10 5 0
a
p < 0.001 (b-f vs. a)
b
c
d
SEF l
e
f
g
Fig. 7.4: Box plots of alterations of BIS and SEF values (r right, l left) in 25 healthy volunteers before (a), during (b - f), and after (g) acupressure (compare Fig. 7.2) on the acupoint Yintang. The ends of the boxes define the twenty-fifth and seventy-fifth percentiles, with a line at the median and error bars defining the tenth and ninetieth percentiles.
80 Figure 7.5 summarizes the BIS and SEF results obtained during manual needle acupuncture, laserneedle acupuncture and acupressure on the control point. Significant (p < 0.05) changes were found in BIS values during laserneedle acupuncture (measuring points d and e; compare Figs. 7.2 and 7.5) and during acupuncture on the control point (measuring points d - f). After 7.5 minutes laserneedle acupuncture at acupoint Yintang the mean BIS values (r SD) were 95.4 (minimum 81; see Fig. 7.5, middle, upper panel) r 4.1. After 5 minutes acupressure at the control point the mean BIS values (r SD) were 94.2 (minimum 77; see Fig. 7.5, right, upper panel) r 4.8. SEF did not show any significant alteration. Laserneedle - Acupuncture
Acupressure - Control
120
120
120
100
100
100
80
80
60
n.s.
20
BIS
20
One Way Repeated Measures ANOVA (Dunnett‘s Method)
BIS
35
35
35
30
30
30
25
25
25
20
20
20
15
15
10
10
n.s.
5
SEF r
10
n.s.
5
SEF r
0
35
35
35
30
30
30
25
25
25
20
20
20
Hz 15
15
10
10 5
n.s.
SEF l
0
a
b
c
d
e
f
g
n.s.
SEF r
Hz
0
5
BIS
15
Hz
0
One Way Repeated Measures ANOVA (Dunnett‘s Method)
Hz
0
Hz
0
Hz
0
5
p < 0.05 (d-f vs. a)
60
40
40
40
20
80
p < 0.05 (d,e vs. a)
60
BIS
BIS
BIS
Needle - Acupuncture
0
15 10 5
n.s.
a
SEF l
b
c
d
e
f
g
0
n.s.
a
SEF l
b
c
d
e
f
g
Fig. 7.5: Box plots of changes of BIS and SEF values (r right, l left) during manual needle acupuncture, laserneedle acupuncture and acupressure at the control point. Further explanations see Fig. 7.4.
The results of the analysis of the VSS are demonstrated in Fig. 7.6.
81 10
8
VSS
6
Acupuncture Yintang
NeedleAcupuncture
Laserneedle Acupuncture
Acupressure Control
a
a
4
a
a 2
0
b b p < 0.001
b paired t-test
b (n.s. p < 0.012)
Fig. 7.6: Mean (+ SD) values of the verbal stress score (VSS) of 25 healthy volunteers before (a) and after (b) different modalities of nonpharmacological stimulation (0 = no stress; 10 = maximum stress).
The VSS values were significantly (p < 0.001) reduced after pressure application on Yintang, needle acupuncture and laserneedle acupuncture but also after pressure application on the control point (p = 0.012). Mean baseline VSS values were insignificant lower in laserneedle and control conditions. HR and BP values (mean r SD) before and after acupressure at Yintang were calculated to be 73.2 r 12.4 1/min, 109.8 r 14.0 mmHg (systolic) and 69.3 r 10.6 mmHg (diastolic). After stimulation the values decreased to 63.7 r 11.9 1/min, 107.7 r 8.7 mmHg (systolic), and 66.8 r 8.6 mmHg (diastolic), respectively.
7.4
Discussion
The bispectral index and the spectral edge frequency are mainly used intraoperatively to monitor the hypnotic effect of anesthetic drugs. There are several studies reported in the literature proposing target values for EEG parameters to guide the depth of anesthesia. A number of authors have reported a low probability of recall and a high probability of unresponsiveness during surgery at a level of 60 for BIS [8,9]. BIS values < 50 are described as suppressing hemodynamic responses during intubation
82 [10]. In an editorial of the European Journal of Anaesthesiology Chan and Gin reported recently that statistically it would be extremely unlikely for a patient to be aware when BIS is less than 50 and, in fact, there has not been a single case of frank awareness at this level [11]. In that context our results showed that 10 of 25 awake healthy volunteers (40 %) have Yintang acupressure induced BIS values below 50 and 21 of 25 subjects (84 %) below 60. Acupressure, acupuncture, meditation, hypnosis or relaxation techniques are all considered to be forms of complementary and alternative medicine. Acupuncture has been shown to reduce medication use in a number of trials [12]. Acupressure has been studied and offered in scientific literature as a valuable treatment in improving the quality of sleep [13]. In previous studies it has also been shown that pressure on acupoints can decrease postoperative pain [14] and that Korean hand acupressure reduces postoperative nausea and vomiting after gynecological laparoscopic surgery [15]. Acupressure has also been used in some other studies for prevention of emesis [16]. There are a number of theories as to how acupressure or acupuncture works. All these hypotheses show, that the brain plays a key role in acupuncture and acupressure research [17-20]. Modulation of subcortical structures may be an important mechanism by which acupuncture and acupressure exerts its complex multisystem effects [20]. Demonstration of regionally specific, quantifiable acupuncture and acupressure effects on relevant structures of the human brain would facilitate acceptance and integration of these therapeutic modalities into the practice of modern medicine [17-20]. It has been shown in several publications that different narcotics have different influence on BIS and SEF [8-11, 21-26]. However, nonpharmacologic influences such as electromyographic activity may contribute to the low specificity of the absolute values of the electrophysiological measurement data [21]. In the majority of the cases the BIS is falsely elevated [21]. Our results appear to confirm the results of the study of Fassoulaki et al. [4] who also found that acupressure on Yintang resulted in a significant and clinically relevant reduction on BIS values and they concluded that BIS and SEF are therefore of limited clinical relevance for monitoring depth of anesthesia [22-26]. However, Fassoulaki et al. [4] did not look at the SEF, nor did they investigate the effects of manual needle acupuncture and the effects of laserneedle acupuncture (Fig. 7.7). We have shown in this study that awake volunteers subjected to acupressure at Yintang can have similar BIS and SEF values to anaesthetized patients. While it is unlikely that a patient will receive acupressure or acupuncture during surgery, the question as to what causes BIS readings below 50 in awake subjects remains. It is unlikely to be a placebo effect as we have
83 shown in several test measurements using placebo points that BIS is not affected by laserneedle stimulation per se. In the present study there were small statistically significant but not clinically important changes with needle acupuncture, laserneedle acupuncture and acupressure at control point. These findings also help confirm that the BIS and SEF reductions induced by acupressure at Yintang are not a placebo effect. Reduced electromyographic levels could be partially responsible [21] (Fig. 7.8).
Fig. 7.7: Laserneedle stimulation at Yintang (CSA = coulor spectral array; CFM = mean EEG-parameter; BIS = bispectral index; HR = heart rate; HRV = heart rate variability). Note the decrease of the BIS values during laserneedle activation.
84
EEG – EMG - HR
EMG
EEG - DELTA LaserneedleLaserneedle-Stimulation – Yintang (10 min)
Fig. 7.8: Electromyographic (EMG) and electroencephalographic Delta (EEG Delta) activities during laserneedle stimulation at Yintang.
At the moment it is also unclear to what degree system algorithms contribute to such findings. BIS is certainly affected by electrical activity nearby, especially diathermy. Therefore there could also be a possibility that local movement in the region of the recording electrode might be responsible for the EEG effects observed. These are apparently less during control point acupuncture than during Yintang acupressure, where pressure is applied to a point immediately adjacent to the Zipprep electrode. Further investigations are necessary to clarify these questions. In conclusion, we found in healthy awake volunteers that acupressure at Yintang results in statistically significant and clinically relevant reductions in BIS and SEF while needle acupuncture, laserneedle acupuncture and acupressure at a control point result in statistically significant but clinically unimportant reductions. Although the validity of BIS in anesthesia is higher than that of SEF, BIS too has to be interpreted very carefully as our results show. Our results also highlight the electroencephalographic similarities of acupressure induced sedation and anesthesia [27].
85
7.5
Acknowledgements
The author would like to express his thanks to Ms. Lu Wang MD, Ms. Petra Petz MSc and Evamaria Huber (all Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz) for their valuable help.
7.6 [1] [2]
[3] [4]
[5] [6] [7] [8]
[9] [10]
[11] [12]
References Litscher G, Schwarz G (2001) Editorial. Noninvasive bioelectrical neuromonitoring in anaesthesia and critical care. Eur J Anaesthesiol 18: 785-788 Litscher G (2000) Editorial. The future of neuromonitoring. Internet J Neuromonitoring 1(1): http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijnm/vol1n 1/editorial2.xml Rampil IJ (1998) A primer for EEG signal processing in anesthesia. Anesthesiology 89: 980-1002 Fassoulaki A, Paraskeva A, Patris K, Pourgiezi T, Kostopanagiotou G (2003) Pressure applied on the extra 1 acupuncture point reduces bispectral index values and stress in volunteers. Anesth Analg 96: 885-889 Stux G, Pomeranz B (1998) Basics of acupuncture. Springer; Berlin Heidelberg New York Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Sebel PS, Lang E, Rampil IJ, White PF, Cork R, Jopling M, Smith NT, Glas PS, Manberg P (1997) A multicenter study of bispectral electroencephalogram analysis for monitoring anesthetic effect. Anesth Analg 84: 891-899 Liu J, Singh H, White PF (1997) Electroencephalographic bispectral index correlates with intraoperative recall and depth of propofolinduced sedation. Anesth Analg 84: 185-189 Heck M, Kumle B, Boldt J, Lang J, Lehmann A, Saggau W (2000) Electroencephalogram bispectral index predicts hemodynamic and arousal reactions during induction of anesthesia in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth 14: 693-697 Chan MTV, Gin T (2000) Editorial. What does the bispectral EEG index monitor? Eur J Anaesthesiol 17: 146-148 Greif R, Laciny S, Mokhtarani M, Doufas AG, Bakhshandeh M, Dorfer L, Sessler DI (2002) Transcutaneous electrical stimulation of an
86
[13] [14] [15] [16] [17] [18] [19] [20]
[21] [22] [23]
[24] [25] [26]
[27]
auricular acupuncture point decreases anesthetic requirement. Anesthesiology 96: 306-312 Tsay SL, Chen ML (2003) Acupressure and quality of sleep in patients with end-stage renal disease - a randomized control trial. Intern J Nursing Studies 40: 1-7. Felhendler D, Lisander B (1996) Pressure on acupoints decreases postoperative pain. Clin J Pain 12: 326-329 Boehler M, Mitterschiffthaler G, Schlager A (2002) Korean hand acupressure reduces postoperative nausea and vomiting after gynecological laparaoscopic surgery. Anesth Analg 94: 872-875 Eizember FL, Tomaszewski CA, Kerns WP (2002) Acupressure for prevention of emesis in patients receiving activated charcoal. J Toxicol Clin Toxicol 40: 775-780 Cho ZH, Wong EK, Fallon JH (2000) Neuro-Acupuncture. Q-Puncture, Los Angeles Litscher G, Cho ZH (Eds.) (2000). Computer Controlled Acupuncture®. Pabst Science Publishers, Lengerich Berlin Düsseldorf Riga Scottsdale Wien Zagreb Litscher G (2001) High-Tech Akupunktur®. Pabst Science Publishers, Lengerich Berlin Düsseldorf Hui KKS, Liu J, Makris N, Gollub RL, Chen AJ, Moore CI, Kennedy DN, Rosen BR, Kwong KK (2000) Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Human Brain Mapping 9: 13-25 Bruhn J, Bouillon TW, Shafer SL (2000) Electromyographic activity falsely elevates the bispectral index. Anesthesiology 92: 1485-1487 Riess ML, Graefe UA, Goeters C, Van Aken H, Bone HG (2002) Sedation assessment in critically ill patients with bispectral index. Eur J Anaesthesiol 19: 18-22 Drummond JC (2000) Monitoring depth of anesthesia. With emphasis on the application of the bispectral index and the middle latency auditory evoked response to the prevention of recall. Anesthesiology 93: 876-882 Nieuwenhuijs D, Coleman EL, Douglas NJ, Drummond GB, Dahan A (2002) Bispectral index values and spectral edge frequency at different stages of physiologic sleep. Anesth Analg 94: 125 - 129 Kalkman CJ, Drummond JC (2002) Monitors of depth of anesthesia, quo vadis? Anesthesiology 96(4): 784-787 Bruhn J, Bouillon TW, Radulescu L, Hoeft A, Bertaccini E, Shafer SL (2003) Correlation of approximate entropy, bispectral index, and spectral edge frequency 95 (SEF95) with clinical signs of „anesthetic depth“ during coadministration of propofol and remifentanil. Anesthesiology 98: 621-627 Litscher G (2004) Effects of acupressure, manual acupuncture and Laserneedle® acupuncture on EEG bispectral index and spectral edge frequency in healthy volunteers. Eur J Anaesthesiol 21: 13-19
87
8.
Acupuncture using laserneedles modulates brain function: first evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI) G. Litscher, D. Rachbauer, S. Ropele, L. Wang, D. Schikora, F. Fazekas, F. Ebner
8.1
Introduction
A new noninvasive laserneedle system has been developed and used for the first time in acupuncture research recently [1,2]. This new optical stimulation technique has the advantage that the stimulation is absolutely painless. Moreover laserneedle acupuncture allows to stimulate appropriate acupoint combinations simultaneously and with higher radiation doses than commercially available low level hand held laser equipment. The laser radiation of eight laser diodes is coupled into eight optical fibers and the laserneedles are arranged at the distal ends of the optical fibers. Due to the direct contact of the laserneedles and the skin, no loss of intensity occurs and the laser power, which affects the acupoints, can be exactly determined [1,2]. The aim of this study was to provide evidence of specific effects of laserneedle acupuncture by stimulating a combination of vision related acupoints of traditional Chinese medicine (TCM). Quantification of cerebral effects of stimulation was performed using functional multidirectional transcranial Doppler sonographic (fTCD) in a randomized controlled doubleblind cross-over study design (fTCD). We also performed functional magnetic resonance imaging (fMRI) measurements in one volunteer using a block design. The dynamics of the metabolic mechanism that regulates cerebral blood flow has already been studied in normal human subjects using fTCD [3,4]. Blood flow velocity in the posterior cerebral artery (PCA), supplying the visual cortex, increased by 16.4 % in response to light stimulation of the retina.
88 The method of fTCD has also been used in previous studies in acupuncture and laserneedle research to investigate specific changes in blood flow velocities of different cerebral arteries [1]. Functional magnetic resonance is sensitive to subtle regional changes in the blood oxygenation level from increased neuronal activity during a specific task or stimulation. It has been successfully used to map the sites of brain activations during needle and low level laser acupuncture [5-9]. These studies report increase (positive activation) and decrease (negative activation) of the BOLD (blood oxygenation level dependent) signal. However, fMRI has not been used up to now during laserneedle stimulation.
8.2 8.2.1
Methods Painless laserneedles
For our experiments eight acupuncture points were chosen and irradiated simultaneously. The laserneedles used in this study emit red light in cwmode with an output power of 30 - 40 mW per laserneedle (wavelength: 685 nm). The fiber core diameter used in this study was about 500 µm. The time of irradiation was 20 min (fTCD measurements) resulting in an energy density of about 4.6 kJ/cm² at each acupoint and a total sum of 36.8 kJ/cm² for all acupoints. The laserneedles were fixed onto the skin using plaster stripes but not pricked into the skin.
8.2.2
Functional multidirectional sonography (fTCD)
transcranial
Doppler
Transtemporal Doppler sonographic examinations of the PCA and the middle cerebral artery (MCA) were performed simultaneously and continuously to determine alterations of cerebral blood flow velocities [4]. A Multi-Dop T unit (DWL Electronic Systems GmbH, Sipplingen, Germany) including two 2 MHz probes were used in a multidirectional ultrasound probe holder construction. Under acoustic control, the angle and position of the probes were adjusted until the greatest possible signal amplitude was reached. Alterations in the blood flow velocities of both arteries were registered continuously and simultaneously. In addition blood pressure was measured non invasively before and after stimulation (Cardiocap® CC-104, Datex Medical Electronics, Hoevelaken, The Netherlands).
89 8.2.3
Functional magnetic resonance imaging (fMRI)
Functional magnetic resonance imaging was performed using a 1.5 Tesla whole body system (Intera, Philips Medical Systems, Best, The Netherlands). Functional images sensitive to blood oxygen dependent contrast were acquired with a T2* weighted gradient echo with single shot echo planar readout (flip angle 90°, TE 50 ms, FOV 250 mm, matrix 96 x 96 interpolated to 128 x 128). Thirty axial slices with a slice thickness of 4 mm were imaged. A total of 144 volume images was obtained continuously with a repetition time of 5 seconds per volume.
8.2.4
Participants
We investigated 18 healthy volunteers (mean age r SD: 25.4 r 4.3 years; range: 21 - 30 years; 11 female, 7 male) using fTCD (n=17) and one volunteer using fMRI (27 y, female). The study protocol was approved by the institutional ethics committee of the Medical University of Graz (11-017 ex 00/01) and all 18 participants gave written informed consent. None of the subjects was under the influence of centrally active medication. All persons were free of neurological or psychological disorders including the absence of visual deficits. A honorarium was given for participation.
8.2.5
Experimental design and procedure
Eight vision related distal acupoints (Hegu, Zusanli, Kunlun, Zhiyin) [6,7,10] on both sides and 8 placebo points were tested using two schemes (fTCD measurements), each in one session in a randomized controlled double-blind cross-over study design (Fig. 8.1). The same acupoints were used for the fMRI investigation. The acupuncture scheme was selected by an expert in TCM. In addition we have seen in several test measurements that needle stimulation of this acupuncture scheme led to alterations of blood flow velocity in the PCA.
90
Vision Related Acupoints
Placebo Points
Fig. 8.1: Vision related acupuncture points and placebo points used in this study. All acupoints (left panel, from bottom to top and from right to left: Hegu, Zusanli, Kunlun, Zhiyin) and all placebo points (right panel) were stimulated bilaterally.
The acupoints were cleaned with alcohol. Then the laserneedles were put in contact with the skin and fixed by plaster stripes. During the experiments the subjects were in a relaxed and comfortable position on a bed in our laboratory (fTCD measurements) or lying in the scanner (fMRI investigation). For the fTCD investigations we started randomly with either acupoint or placebo stimulation. Acupoints Hegu (LI.4): Location: On the dorsum of the hand, between the 1st and 2nd metacarpal bones, in the middle of the 2nd metacarpal bone on the radial side. Indications: Headache, redness, swelling and pain of the eye. Zusanli (Sp.36): Location: 3 cun below Dubi (S 35), one finger-breadth from the anterior crest of the tibia. Indications: Gastric pain, abdominal distension, vomiting, diarrhea, dysentery, has tonification effect. Kunlun (UB.60): Location: In the depression between the tip of the external malleolus and tendo calcaneus. Indications: Headache, neck rigidity, dizziness.
91 Zhiyin (UB.67): Location: On the lateral side of the small toe, about 0.1 cun lateral to the corner of the nail. Indications: Headache, pain in the eye, nasal obstruction, epistaxis, malposition of fetus.
8.2.6
Evaluated parameters
The mean blood flow velocity (vm) in the PCA and the MCA were evaluated simultaneously and continuously at different measurement points (a - e in Fig. 8.2A) [10]. Each person was studied performing stimulation on vision related acupoints and placebo points. The interval between the fTCDexperiments was 20 to 30 minutes and the subjects were instructed to keep their eyes closed during the whole fTCD experiments. Similarly, during fMRI investigations the subject could not see whether the laser was off or on. The fMRI study used a block design with alternating one minute resting condition (‘R’) and one minute activation condition (‘A’) (Fig. 8.2B). The experiment started with ‘R’ followed by the laserneedle acupuncture condition (‘A’). A total of 6 ‘R’ and 6 ‘A’ intervals was registered. Altogether the fMRI data acquisition took 12 minutes. b
c
d 1 min
1 min
A
10 min
a
e
20 min Laserneedle Stimulation 2 min
2 min
Stimulation OFF
Stimulation ON
A
B
R
A R
A R
A R
A R
A R
1 min
12 min
Fig. 8.2: Measurement profiles for fTCD (A) and fMRI (B) measurements.
92 8.2.7
Statistical analysis
The fTCD data before (a), during (b - d), and after (e) laserneedle acupuncture (comp. Fig. 8.2A) were tested with Kruskal-Wallis one way ANOVA on ranks (SigmaStat, Jandel Scientific Corp., Erkrath, Germany). The criterion for significance was p < 0.05. The fMRI data were analysed using SPM 99 (SPM 99, Department of Imaging Neuroscience, London, UK). All volumes from the subject were realigned using the first volume as a reference and resliced using sincinterpolation. The functional images were spatially normalized to a standard echo planar template in Tailarach space. Functional data were spatially smoothed with a 6 mm full width at half maximum isotropic kernel. A boxcar waveform convolved with a synthetic hemodynamic response function was used as the reference waveform. A t-test was performed to identify regions showing significantly higher activation during the activation condition versus the resting condition. For significantly activated regions, a statistical threshold p < 0.05, corrected at the cluster level for multiple comparisons, was used.
8.3
Results
The results of the alterations of mean blood flow velocities in the PCA and MCA before, during, and after laserneedle and placebo acupuncture are summarized in Figure 8.3.
93
vm [cm/s]
PCA
Vision related acupoints (A)
50 + 2.5 cm/s
40
SE
MCA 50
40
vm [cm/s]
a
b
c
d
e
Placebo points (B)
PCA
50
40
SE
MCA 50
40
a
b
c
d
e
Fig. 8.3: Mean blood flow velocity (vm) of the posterior cerebral artery (PCA) and the middle cerebral artery (MCA) before (a), during (b - d), and after (e) stimulating vision related acupoints (A) and placebo points (B) with laserneedles in 17 healthy volunteers. Note the trend towards an increase (+ 2.5 cm/s) in vm in the PCA during acupoint stimulation.
The results showed a trend towards an increase of vm (insignificant changes) in the PCA during (b - d) laserneedle acupuncture at vision related acupoints (Fig. 8.3A, upper panel). At the same time only minor changes in vm were seen in the MCA (Fig. 8.3A, lower panel). The maximum amplitude of vm in the PCA was detected with a delay of 20 - 60 sec after the initial stimulus by
94 the laserneedles (vm; Cx r SE, acupoint stimulation, PCA: 42.2 r 2.5 before (a), 44.2 r 2.6 during (b - d), 42.3 r 2.4 cm/s after (e)). Stimulation at placebo points did not increase vm of the PCA and of the MCA (Fig. 8.3B), rather there was a trend towards a small decrease of mean values of the mean vm in both arteries (vm, Cx r SE, placebo point stimulation, PCA: 42.9 r 2.6 before (a), 41.7 r 2.6 during (b - d), 42.1 r 2.8 cm/s after (e)). The mean arterial blood pressure before and after laserneedle acupuncture was almost identical (76.7 r 7.6 (SD) vs. 75.8 r 6.8 mmHg). The results of the fMRI investigation are shown in Figures 8.4 and 8.5 and Table 8.1. Significant changes in brain activation were found in the occipital lobe and in the frontal lobe.
right
left
Fig. 8.4: First evidence of significant effects of changes in brain activation during laserneedle stimulation of vision related acupoints in the occipital and frontal areas in a 27-year-old healthy female using fMRI investigation.
95
Signal Change Visual Cortex [a.u.]
A 3 2 1 0 -1 -2 -3
R
12 min Time [min]
Fig. 8.5: The time course of signal change correlated with the experimental fMRI paradigm. Note the signal increases during active laserneedle acupoint stimulation (A) and the signal decreases during resting condition (R).
Brain Areas Occipital Left superior occipital gyrus Frontal Right inferior frontal gyrus Right precentral gyrus Left middle frontal gyrus Left superior frontal gyrus
Brodmann Area
19
4
Coordinates in Tailarach Cluster size space (x,y,z) Z-value (mm³)
-38
-84
28
5.80
32
54
34
12
5.23
64
20
-28
64
5.43
32
-20
60
20
5.59
32
-18
56
16
5.23
32
Tab. 8.1: Regions of significant activation (occipital and frontal areas) due to laserneedle stimulation of vision related acupoints. The p-values are corrected (p < 0.05) at the cluster level for multiple comparisons. Compare Fig. 8.4.
96
8.4
Discussion
Recent scientific and technological progress especially regarding the application of modern brain function monitoring systems has truly revolutionized acupuncture research. The usage of advanced exploratory tools, such as functional multidirectional transcranial ultrasound Doppler sonography or functional magnetic resonance imaging, provides insights and attempt to shine scientific light upon the most spectacular of the eastern medical procedures [3,4]. Recently it has been attracted interest that the brain is the key to acupuncture’s and laser puncture’s effects. New experimental constructions to measure ultrasound, light and bioelectrical processes can reproducibly demonstrate effects of stimulation of acupoints in the brain [1,2,5-21]. The new laserneedle system has been described for the first time in scientific literature recently [1]. In addition previous studies from our group show that the new optical stimulation with laserneedles can elicit reproducible cerebral effects which are in the same order with respect to the maximum amplitude of the mean blood flow velocity as compared to needle acupuncture [1]. The stimulation performed within this study could not be felt by the patient. The operator was also unaware of whether the stimulation was active, and therefore a true double-blind study was performed. Moreover laserneedle is the first laser system commercially available that could be used at eight or more standard acupuncture points simultaneously. The effectiveness of unconventional complementary medical methods, such as laserpuncture, has previously been documented mainly as single cases. There are many theoretical and clinical studies concerning laserpuncture in scientific literature. For a short review see [1]. To our knowledge, laseracupuncture has not been studied in cases where more than one acupoint at time were stimulated. In our experiment, we tested four acupoints (four on both sides of the body) with laserneedle acupuncture, and measured the alterations of brain activations using fTDC and fMRI. In this study, we were not able to separate significant specific cerebral effects of blood flow velocity during laserneedle acupuncture using fTCD. However, there was a trend of an increase in vm during laserneedle stimulation of visual acupoints in the PCA. Similar significant effects have been reported after manual needle acupuncture [11,13-16]. Previous results also show that different modes of manual acupuncture stimulation differentially modulate cerebral blood flow velocity [20].
97 In addition to fTCD we used for the first time fMRI in a healthy volunteer during laserneedle stimulation of the same vision related acupoints as used for the fTCD measurements. Bilateral stimulation of the acupoints produced bilateral positive activation over the frontal cortex. A time-logged increase of the BOLD signal was also seen at the left superior occipital gyrus (Brodmann Area 19). Apparently the stimulation of vision-implicated acupoints (Kunlun, UB.60 and Zhiyin, UB.67) activated the visual cortex. These findings are in accordance with other fMRI acupuncture studies. Cho et al. [7] reported that needling of acupoints (UB.60, 65, 66 and 67) on the foot created activation in the visual cortex similar to actual visual stimuli. Needling of non-acupoints on the foot 2 to 5 cm away from the vision related acupoints as control caused no activation in the occipital lobes [7]. In traditional needle acupuncture treatment points are located at different depths and hence needle insertion is different. This is of particular importance with the points we selected because Zhiyin requires a very shallow needle insertion versus Zusanli. With the laserneedle stimulation the acupoints will receive different energy doses because of their different depths. It is possible that the effects seen with fTCD and fMRI could be due to stimulation of one of the points. Further investigation on this topic is necessary. Li et al. [6] recently also found that the application of conventional or electro-acupuncture over four vision-implicated acupoints on the right foot can modulate the activity of specific brain sites. Negative and positive activations were seen using fMRI during conventional acupuncture while positive activations, similar to our results of laserneedle stimulation, only were observed during optical stimulation and electro-acupuncture. The authors also found bilateral activations in frontal cortices [6]. It has been demonstrated using fMRI that needle acupuncture [7] and laser puncture [9] of the vision-related acupoint Zhiyin (UB.67) activates the visual cortex of the human brain. As a further study on the effect of this acupoint stimulation on the visual cortex, Lee et al. [22] examined c-Fos expression in binocularly deprived rat pups. Interestingly, acupuncture stimulation of UB.67 resulted in a significant increase in the number of cFos-positive cells in the primary visual cortex, while acupuncture stimulation of other points less important for visual function had no significant effect on c-Fos expression in the primary cortex. Other studies have shown effects of acupuncture needle manipulation of LI.4 (we also used this acupoint (Hegu) in our scheme as a general point of activation) on a network of cortical and subcortical limbic and paralimbic structures [5]. We did not find the same significant effects in our fMRI
98 experiment. In this context it is important to mention that laserneedle acupuncture allows for the first time a totally painless acupuncture stimulation. Therefore differences between electro acupuncture [23] and needle acupuncture, which often includes pain stimulation, and a painless acupuncture stimulation technique can be examined.
8.5 (a)
(b) (c)
8.6
Conclusions Using the new laserneedle acupuncture method we were able to stimulate multiple vision-associated acupuncture points at the same time. The results showed insignificant increases in cerebral blood flow velocity of the PCA after stimulation of vision-related acupoints on the foot. At the same time blood flow velocity in the MCA showed minor changes. Stimulation at placebo points did not show increases in blood flow velocity in both arteries. The fMRI results of a healthy volunteer after laserneedle stimulation of the same acupoints showed significant changes in occipital and frontal brain areas. Both techniques, fTCD and fMRI, can be used to study cerebral effects of laserneedle acupuncture in a complementary way [24].
Acknowledgements
The authors thank Evamaria Huber (Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz, Austria) and Martin Kronbichler (Department of Psychology, University of Salzburg, Austria) for their support to this study.
8.7 [1] [2] [3]
References Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Aaslid R (1987) Visually evoked dynamic blood flow response of the human cerebral circulation. Stroke 18(4): 771-775
99 [4] [5]
[6] [7]
[8]
[9]
[10] [11]
[12] [13] [14] [15] [16]
[17] [18]
Sturzenegger M, Newell DW, Aaslid R (1996) Visually evoked blood flow response assessed by simultaneous two-channel transcranial Doppler using flow velocity averaging. Stroke 27(12): 2256-2261 Hui KKS, Liu J, Makris N, Gollub RL, Chen AJW, Moore CI, Kennedy DN, Rosen BR, Kwong KK (2000) Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Map 9: 13-25 Li G, Cheung RTF, Ma QY, Yang ES (2003) Visual cortical activations on fMRI upon stimulation of the vision-implicated acupoints. NeuroReport 14: 669-673 Cho ZH, Chung SC, Jones JP, Park JB, Park HJ, Lee HJ, Wong EK, Min BI (1998) New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci USA 95: 2670-2673 Cho ZH, Oleson TD, Alimi D, Niemtzow RC (2002) Acupuncture: the search for biologic evidence with functional magnetic resonance imaging and positron emission tomography techniques. Editorial. J Altern Compl Med 8: 399-401 Siedentopf CM, Golaszewski SM, Mottaghy FM, Ruff CC, Felber S, Schlager A (2002) Functional magnetic resonance imaging detects activation of the visual association cortex during laser acupuncture of the foot in humans. Neurosci Lett 327: 53-56 Litscher G, Schikora D (2002) Effects of new noninvasive laserneedles on brain function. Proceedings of the International Federation for Medical and Biological Engineering 2: 996-997 Litscher G (2002) Computer-based quantification of traditional Chinese-, ear- and Korean hand acupuncture: Needle-induced changes of regional cerebral blood flow velocity. Neurol Res 24: 377380 Litscher G, Wang L, Wiesner-Zechmeister M (2000) Specific effects of laserpuncture on the cerebral circulation. Lasers Med Sci 15: 57-62 Litscher G (2001) High-Tech Akupunktur®. Pabst Science Publishers, Lengerich Berlin Rom Riga Wien Zagreb Litscher G, Wang L, Yang NH, Schwarz G (1999) Computer-controlled acupuncture. Quantification and separation of specific effects. Neurol Res 21(6): 530-534 Litscher G, Wang L, Yang NH, Schwarz G (1999) Ultrasoundmonitored effects of acupuncture on brain and eye. Neurol Res 21(4): 373-377 Litscher G, Yang NH, Schwarz G, Wang L (1999) Computer-controlled acupuncture. A new construction for simultaneous measurement of blood flow velocity of the supratrochlear and middle cerebral arteries. Biomed Techn 44(3): 58-63 Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I (1998) Robotic transcranial Doppler sonography probes and acupuncture. Int J Neurosci 95(1-2): 1-15 Litscher G, Schwarz G, Sandner-Kiesling A, Hadolt I, Eger E (1998) Effects of acupuncture on the oxygenation of cerebral tissue. Neurol Res 20 Suppl 1: 28-32
100 [19] [20]
[21] [22]
[23] [24]
Litscher G, Wang L (2000) Cerebral near infrared spectroscopy and acupuncture - results of a pilot study. Biomed Techn 45(7-8): 215-218 Bäcker M, Hammes MG, Valet M, Deppe M, Conrad B, Tölle TR, Dobos G (2002) Different modes of manual acupuncture stimulation differentially modulate cerebral blood flow velocity, arterial blood pressure and heart rate in human subjects. Neurosci Lett 333: 203206 Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Lee H, Park HJ, Kim SA, Lee HJ, Kim MJ, Kim CJ, Chung JH, Lee H (2002) Acupuncture stimulation of the vision-related acupoint (Bl-67) increases c-Fos expression in the visual cortex of binocularly deprived rat pups. Am J Chin Med 30: 379-385 Napadow V, Makris N, Liu J, Kettner NW, Kwong KK, Hui KKS (2005) Effects of electroacupuncture versus manual acupuncture on the human brain as measured by fMRI. Hum Brain Mapp 24: 193-205 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laser needles modulates brain function: first evidence from functional transcranial Doppler sonography and functional magnetic resonance imaging. Las Med Sci 19: 6-11
101
9.
Quantification of gender specific thermal sensory and pain thresholds before and after laserneedle stimulation G. Litscher, L. Wang, E. Huber, D. Schikora, G. Schwarz
9.1
Introduction
The quantitative determination of border values for thermal sensory and pain threshold testing has been clinically used for several years and is of great importance in the fields of neurology, psychiatry, and neurophysiology [6]. Several guidelines regarding the correct application of „Quantitative sensory testing“ (QST) were published in scientific literature [4]. QST-systems can generally be divided into instruments, which allow the application of physical-thermal, chemical or vibration specific stimuli. In addition, the general equipment required for generating electric stimulation with different frequencies and intensities can be included here. Thermal stimulation in this study was performed with a thermode (Peltier’s Principle) applied at the right palmer base of the thumb, in healthy adult volunteers. Goal of this study was to determine normal values and objectify possible gender specific differences. For the first time, QST was used, in combination with scientific tests using the new laserneedle stimulation technique, to quantify possible alterations before and after painless acupuncture with laserneedles.
9.2 9.2.1
Method Volunteers
Twenty-nine healthy adult volunteers, mean age (Cx r SD) was 24.2 r 2.7 (range from 18 to 29 years) were included in the study. Twenty volunteers were female (mean age: 23.9 r 2.7 years) and 9 were male (mean age: 24.9 r 2.8 years). The ethical committee of the Medical University of Graz (laserneedle stimulation; 13-048 ex 02/03) approved the tests and all
102 volunteers gave their written consent. None of the volunteers had neurological or psychological deficits or was under the influence of drugs.
9.2.2
Measurement of thermal sensitivity and thermal pain thresholds
A computer-controlled system was used for quantitative evaluation of small calibre nerve fibres (A-Delta and C-nerve fibres) using temperature tests (Thermal Sensory Analyser TSA-II, Medoc Advanced Medical Systems, Ramat Yishai, Israel, and Minneapolis, Minnesota, USA). The system consists of a basic unit with connection to an external notebook, a thermode with an active contact area of 30 x 30 mm (Peltier element) and a control device for input of patient reaction data. The thermode was placed on the inner side of the volunteer’s hand and can either cool or warm the skin. Adaptation temperature between 30 and 32 °C is achievable within a few seconds after skin contact, thus, the volunteer is unable to feel cold or hot sensations. The software runs with Windows, controls the system, and includes the different test methods. All parameters can be set individually. In addition to thermal sensory measurement, pain thresholds (cold pain, heat pain: 0 - 52 °C) were examined (Fig. 9.1). Cold sensation (a) and warm sensation (b) thresholds were determined first. Then, cold pain (c) and heat pain (d) thresholds were determined (compare Fig. 9.4). A resting period of at least 5 minutes was held between the single measurements.
103
2 1 3
Fig. 9.1: Set-up in the lab of the Dept. of Biomedical Research in Anaesthesia and Intensive Medicine, Medical University Graz. Thermal Sensory Analyser TSA-II (1) with Notebook-Data analysis (2) and laserneedle stimulation device (3). With generous consent from the volunteer.
9.2.3
Laserneedle acupuncture and procedure
Laserneedles are special light conductors which are placed vertically at the skin, and trigger painless stimulation at the acupoint. They offer high optical output densities regarding measurable cerebral effects compared with acupuncture needles [9 ,10], and for the first time, allow simultaneous optical activation of up to eight acupoints according to Traditional Chinese Medicine (TCM). The laserneedles used emit light with a wavelength of 685 nm in a continuous or frequency modulated wave mode. The output per laserneedle is 30 - 40 mW. Further information regarding the method and the periphery and cerebral effects of laserneedle acupuncture can be found in previous publications [8-10]. Acupuncture was performed at the acupoints shown in Figure 9.2. First, the skin was disinfected with alcohol at the acupoint, and then the laserneedles are applied and fixed to the skin with special adhesive tape. During testing, the volunteers were positioned relaxed on a bed (compare Fig. 9.1). In two
104 different tests, the laserneedles were once applied and activated for 10 minutes, or remained deactivated in an identical procedure (placebo). Which test procedure was performed first was selected at random. Each volunteer was tested with activated as well as deactivated laserneedles, whereby the volunteers were not informed about and could not perceive the respective mode being used. The resting period between both tests was at least 20 minutes. Following acupoints were used [16]: Hegu (LI.4): Localisation: Indication: Needling:
At the highest point of M. adductor pollicis, when the thumb lies against the index finger. Hegu is the most important analgesic point. Pain conditions; particularly strong manual stimulation relieves pain in the entire body. Vertical, 1 - 2 cm deep in direction Pe.8 Laogong.
Taiyuan (Lu.9): Localisation: On the radial side of the bending fold at the wrist joint, lateral from A. radialis. Indication: Pain in the wrist region, polyneuropathy at the upper extremity. Needling: Vertical or inclined, 0.3 - 1 cm deep. Quchi (LI.11): Localisation: At the lateral end of the bending fold of the elbow during right-angled bending of the lower arm. Indication: Homeostatic and immuno-stimulating point. Needling: Vertical, 2 - 3 cm deep. Shenmen (Ear point 55): Localisation: In the fossa triangularis. Indication: General sedative and analgesic point. Ear point 67: Localisation: Indication:
Between helix and anthelix in the so-called scapha. Pain, hand, wrist.
105
1 2
3
4 5 2 1
Fig. 9.2: Laserneedle stimulation at the acupoints Hegu (1), Taiyuan (2), Quchi (3), Shenmen – Ear point 55 (4) and Ear point 67 (5).
9.2.4
Statistical analysis
A „t-test“for the conditions before (I) and after (II) laserneedle stimulation and a „paired t-test“ for the placebo test, were used to determine gender specific differences. Significance was defined with p < 0.05. The results are shown graphically with box-plot illustrations (Statistical program SigmaStat; Jandel Scientific Corp., Erkrath, Germany).
9.3
Results
Figure 9.3 shows a sample „test report“. In addition to a marker at the derivation, or stimulation region („C6 right hand palmar thumb“), the measurement results (mean value of 3 tests) and differences (ǻ) before and after intervention (laserneedle stimulation or placebo test) of the respective testing mode are shown graphically in this protocol.
106
Fig. 9.3: „Quantitative Somatosensory Test Report“ from an 18-year-old volunteer. Above: laserneedle stimulation; below: placebo test.
Figure 9.4 summarizes the results from all 29 volunteers, without considering gender. No significant differences between the single tests before and after laserneedle stimulation or placebo stimulation were evident.
107 Temp. [°C] 60
laserneedle stimulation I
placebo I
II
II
50 I I
40 I
II
II
II
I I
30
II
I
II
II
20
10
0
n=29 0
1
a
2
3
b
4
5
c
6
7
d
8
9
10 11 12 13 14 15 16 17 18
a
b
c
d
Fig. 9.4: Box-plot illustration of n = 29 healthy volunteers. Cold sensation- (a) and warm sensation thresholds (b) and cold pain- (c) and heat pain thresholds (d) before (I) and after (II) laserneedle stimulation (left) and placebo (right). The horizontal line in the box indicates the position of the median. The ends of the box define the 25th and 75th percentile; the error bars mark the 10th and 90th percentiles.
Separation of the results according to gender is illustrated in Figure 9.5. Significant (p < 0.034) gender specific differences are seen in cold pain and heat pain thresholds. The border values of painful cold sensation also differs significantly between males and females (p < 0.001) as those of painful heat sensation (p = 0.009 and p = 0.034 respectively). During placebo stimulation, no obvious differences in median values are evident. However, it should be mentioned that the median tolerance of cold pain sensation after laserneedle acupuncture in females, although insignificant (p = 0.479), lies higher than before laserneedle treatment (* in Fig. 9.5A).
108 Temp. [°C]60
laserneedle stimulation I
50 I
40 I
placebo I
II
II
I
II
I
30
I
II
II
II
A
II
I
II
women *)
20
10
0
p = 0,034
p < 0,001
p = 0,009
p < 0,001
t-test
p = 0,026
n=20
Temp. [°C] I
I
II I
I I
II
II
II
II
I
I
II
B
II I
II
men
n=9 a
b
c
d
a
b
c
d
Fig. 9.5: Gender specific analysis (female (A), male (B)). In addition to the significant gender specific differences in pain sensation, note the difference (*) in median values during cold pain threshold determination before (I) and after (II) laserneedle stimulation. Further information see Fig. 9.4.
109
9.4
Discussion
There are numerous publications concerning QST reproducibility [20], the different biological effects on thermal sensor, vibration specific and pain thresholds and the gender specific differences and influence of age and body size [19]. Clinical indications for QST described in this study are the determination of sensory and pain thresholds in chronic pain disorders [17], diabetic neuropathy [3] and use in patients with multiple sclerosis [7,18]. The method for quantitative determination of different thermal thresholds used in this study has also been used in different publications in combination with other measurement techniques. For example, the comparison and correlation of somatosensory evoked potentials [14] and the supplementary or combined use with functional magnetic resonance imaging [2,5] should be mentioned. In this study, we could document significant gender specific differences in temperature sensation. A difference in gender specific thermal sensory thresholds could be proven in numerous studies [20]. In addition to these results, QST shows that cold sensations change during the female menstrual cycle dependent upon the oestrogen secretion [1]. An interesting aspect of this study design is that acupuncture subjectively relieves pain in females better than in males. This is one of the first, unpublished intermediate results of the worldwide largest controlled acupuncture study being currently performed in Germany. In a representative random sample, 1096 patients treated with acupuncture against lumbar or knee pain were questioned. Two thirds of the women, but only half of the men were satisfied with the effect of needle therapy. Sixtyone percent of the questioned persons evaluated the effect as very good or good. In contrast, 92 percent of the treating physicians were certain that this treatment was a success. Even when nine of ten patients were not satisfied with the treatment, the respective physician supposed treatment was successful. This documents the physician’s subjectivity towards the patients’ pain sensitivity and indicates the necessity of qualitative evaluation of acupuncture to objectify the potential therapy effect individually. The effects of acupuncture and laserneedle acupuncture on parameters of peripheral circulation could be scientifically proven in several studies [1113]. In many cases, moxibustion (burning of the flowering plant mugwort) intensifies the effect [15]. Measurement data determined in our study, before and after laserneedle acupuncture and placebo laserneedle acupuncture, showed no significant differences when using an acupoint scheme for acute pain. However, cold pain sensation could be reduced in women with laserneedle acupuncture. To what extent acupuncture schemes for treating
110 chronic pain with laserneedle acupuncture can lead to provable effects in the described measurement parameters should be investigated in further studies.
9.5
Acknowledgements
The authors thank Mr. Michael Magometschnigg and Mr. Ing. Stefan Wüger (both from INTEC Medizintechnik GmbH, Vienna, Austria) for their organisational and technical support with Thermal Sensory Analyser TSA-II. We also thank Ms. Ingrid Gaischek MSc. (Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University Graz) for her valuable support in data analysis and writing the manuscript.
9.6 [1] [2]
[3] [4] [5] [6] [7]
[8] [9] [10]
References Bajaj P, Arendt-Nielsen L, Bajaj P, Madsen H (2001) Sensory changes during the ovulatory phase of the menstrual cycle in healthy women. Eur J Pain 5: 135-144 Becerra LR, Breiter HC, Stojanovic M, Fishman S, Edwards A, Comite AR, Gonzalez RG, Borsook D (1999) Human brain activation under controlled thermal stimulation and habituation to noxious heat: an fMRI study. Magn Reson Med 41: 1044-1057 Bravenboer B, van Dam PS, Hop J, Steenhoven Jvd, Erkelens DW (1992) Thermal threshold testing for the assessment of small fibre dysfunction: normal values and reproducibility. Diabet Med 9: 546-549 Consensus report (1993) Quantitative sensory testing: a consensus report from the Peripheral Neuropathy Association. Neurology 43: 1050-1052 Davis KD, Kwan CL, Crawley AP, Mikulis DJ (1998) Functional MRI study of thalamic and cortical activations evoked by cutaneous heat, cold, and tactile stimuli. J Neurophysiol 80: 1533-1546 Fruhstorfer H, Lindblom U, Schmidt WC (1976) Method for quantitative estimation of thermal thresholds in patients. J Neurol Neurosurg Psychiatry 39: 1071-1075 Heijenbrok MW, Anema JR, Faes TJ, Bertelsmann FW, Heimans JJ, Polman CH (1992) Quantitative measurement of vibratory sense and temperature sense in patients with multiple sclerosis. Electromyogr Clin Neurophysiol 32: 385-388 Litscher G (2003) Cerebral and peripheral effects of laser needlestimulation. Neurol Res 25: 722-728 Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342
111 [11]
[12]
[13] [14] [15]
[16] [17]
[18] [19] [20] [21]
Litscher G, Wang L, Huber E, Nilsson G (2002) Changed skin blood perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers Med Sci 17: 1925 Litscher G, Wang L, Huber E, Nilsson G (2001) Laser Doppler Imaging – Objektivierung und Quantifizierung primärer peripherer Mikrozirkulationsänderungen durch Akupunktur. Europäische Zeitschrift für Akupunktur, Der Akupunkturarzt / Aurikulotherapeut 3: 7-17 Litscher G, Wang L, Nilsson G (2001) Laser Doppler Imaging und Kryoglobulinämie. Biomed Technik 46: 154-157 Meh D, Denislic M (2000) Correlation between temperature and vibration thresholds and somatosensory evoked potentials. Electromyogr Clin Neurophysiol 40: 131-134 Sandner-Kiesling A, Litscher G, Voit-Augustin H, James RL, Schwarz G (2001) Laser Doppler flowmetry in combined needle acupuncture and moxibustion: a pilot study in healthy adults. Lasers Med Sci 16: 184-191 Stux G, Stiller N, Pomeranz B (1999) Akupunktur. Lehrbuch und Atlas. Springer, Berlin Heidelberg New York Thimineur M, Sood P, Kravitz E, Gudin J, Kitaj M (1998) Central nervous system abnormalities in complex regional pain syndrome (CRPS): clinical and quantitative evidence of medullary dysfunction. Clin J Pain 14: 256-257 Treede RD, Hansen C, Hopf HC (1995) Paradoxical warm-sensation is a common symptom in patients with multiple sclerosis. Electroencephalogr Clin Neurophysiol 97: 125 Wiles PG, Pearce SM, Rice PF, Mitchell JM (1991) Vibration perception threshold: Influence of age, height, sex, and smoking, and calculation of accurate centile values. Diabet Med 8: 157-161 Yarnitsky D, Sprecher E, Zaslansky R, Hemli JA (1995) Heat pain thresholds: normative data and repeatability. Pain 60: 329-332 Litscher G, Wang L, Huber E, Schikora D, Schwarz G (2004) Quantitative Bestimmung geschlechtsspezifischer thermischer Empfindungsund Schmerzschwellen vor und nach Lasernadelstimulation. Biomed Technik 49: 106-110
112
10. Biological effects of painless laserneedle acupuncture - a short summary of important scientific results G. Litscher, L. Wang, D. Schikora, D. Rachbauer, G. Schwarz, A. Schöpfer, S. Ropele, E. Huber 10.1 Introduction The stimulation of acupuncture points with laser light can evoke specific effects in the periphery and in the brain. For the first time, these effects, can be objectified and quantified using modern biomedical engineering techniques. Laserneedle acupuncture represents a new, painless method for primary optical stimulation of acupuncture points [1-15]. Laserneedles, are not inserted in the skin, however, simply applied to the acupuncture point. This method allows the simultaneous stimulation of individually combined points for the first time. This study gives a current summary regarding scientific proof and innovative aspects of painless laserneedle acupuncture. We introduce studies which prove the peripheral effects using registration of temperature and laser Doppler flowmetry [8,9,13], as well as publications regarding the objectification of cerebral effects of laserneedle acupuncture aided by functional multi-directional transcranial Doppler sonography (fTCD) [13,8,9,11,12], functional magnetic resonance imaging (fMRI) [11,12] and near infrared spectroscopy (NIRS) [2,4-6,8,9].
10.2 Methods 10.2.1
Temperature and microcirculatory monitoring
The surface temperature of the skin and the measurement parameter Flux (= product of concentration and velocity of erythrocytes) were performed with the Laser-Doppler-Flowmetry Monitor DRT 4 (Moor Instruments, Millway, Axminster, England). A DPIT-probe (diameter 8 mm, length 7 mm) with a power of 1 mW was used (compare Fig. 10.1, above). The edge frequencies were 20 Hz and 22.5 kHz [8,9,13].
113 10.2.2
Functional multi-directional sonography (fTCD)
transcranial
Doppler-
The Multi-Dop T System (DWL Electronic Systems GmbH, Sipplingen, Germany), was used to measure the mean blood flow velocity in different cerebral arteries. A 4-MHz- (ophthalmic artery (OA)), as well as 2-MHz probes (posterior cerebral artery (PCA), anterior cerebral artery (ACA), middle cerebral artery (MCA)) were applied with a specially developed ultrasound probe holding construction (compare Fig. 10.2, right below).
10.2.3
Functional magnetic resonance imaging (fMRI)
The fMRI-investigations were performed using a 1.5 Tesla total body system (Intera, Philips Medical Systems, Best, Netherlands) (compare Fig. 10.4, above). The BOLD (blood oxygen level dependent) contrast sensitive images were acquired with a T2* weighted gradient echo sequence (single shot planar readout, flip angle 90°, TE 50 ms, FOV 250 mm, matrix 96 x 96 interpolated at 128 x 128, layer number 30, layer thickness 4 mm). A total of 144 volume images, were registered continuously in succession, with a repetition time of 5 seconds. The fMRI-study is based on a block design with alternating resting conditions („R“) for one minute and one minute of laserneedle activation („A“). This experiment starts with „R“, followed by the laserneedle condition „A“. A total of six „R“ and six „A“ intervals were registered. Each fMRI data registration required 12 minutes [11, 12].
10.2.4
Near infrared spectroscopy (NIRS)
Near infrared spectroscopic investigations for monitoring laserneedle acupuncture, were done with the NIRO 300 Monitor (Hamamatsu Photonics, Japan). Measurement values, and such as changes in oxyhaemoglobin (¨O2Hb) and desoxyhaemoglobin (¨HHb) were determined using LambertBeer´s principle. Alterations in parameters could be measured absolutely (µmolar) with this system, but not the level (absolute concentration) at which these changes (in a positive or negative direction) occur. As long as no change in concentration is given, the measurement value is zero. Using a silicone holder, the fixating of the sensor (emitter and near infrared detectors) on the head is easy.
10.2.5
Laserneedle stimulation
As mentioned earlier, laserneedle acupuncture (Schikora, D.: European Patent Nr. PCT/EP 01/08504) allows the simultaneous stimulation of
114 individual point combinations. Variation and combination of acupuncture points on the body are possible according to Traditional Chinese Medicine (TCM), or at the ear and hand using Korean (KHA) or Chinese (CHA) hand acupuncture. The laserneedle method is based on a multi-channel system with 8 separate semi-conductor laser diodes and emission wavelengths of 685 nm and 785 nm. The system consists of flexible optical light fibres, which conduct the laser light without loss to the laserneedle. Thus, a high optical density at the distal end of the laserneedle is achievable. The intensity of the laserneedles are optimized in such a way, so that the patient does not feel the activation of the needle (30 - 40 mW per needle; diameter 500 µm; duration 10 min; power density 2.3 kJ/cm² per acupuncture point). More details regarding this method are described in previous studies [1,6].
10.2.6
Healthy volunteers, animal experiment and procedures
This summarizing study presents a total of 511 measurements in 231 healthy test persons (129 females, 102 males) with a mean age of 25.2 r 3.5 (Cx r SD) years (18 to 38 years). Protocols were approved by the local ethic committee, Medical University of Graz (11-017 ex 00/01: Computercontrolled acupuncture; and 13-048 ex 02/03: Laserneedle-stimulation), and all test persons gave their written consent. None of the test persons had obvious visual, neurological, olfactory, or mental deficits or stood under influence of CNS active drugs. A maximum of seven acupuncture points were investigated simultaneously in different measurement series. In addition, an animal study was included in this report. The animal used was a sus scrofa domesticus, which was put under general anaesthesia in the animal surgical suite of the Department of Surgical Research at the Medical University of Graz (compare Fig. 10.1, left). This study was performed in accordance with the rules defined by the ethic committee (animal study approval number GZ 66.010/10-BRGT/2003).
10.2.7
Statistical analysis
Data was analysed with „One-way repeated measure ANOVA“ , using the computer program SigmaStat (Jandel Scientific Corp., Erkrath, Germany). The tests described in single publications were used for post hoc-analyses. The level of significance was defined as p < 0.05 when no other value was explicitly given. The fMRI-data was analysed and evaluated with SPM 99 (Statistical parametric mapping) - Software (SPM 99, Department of Imaging Neuroscience, London, England). All images of the test persons were newly
115 organized and the first picture was used as reference, whereby „sincinterpolation“ was used. Functional data were spatially smoothed with a 6 mm full width at half maximum isotropic kernel. A boxcar waveform convolved with a synthetic haemodynamic response function was used as the reference waveform. A ttest was performed to identify regions showing significantly higher activation during the activation condition versus the resting condition. For significantly activated regions, a statistical threshold p < 0,05, corrected at the cluster level for multiple comparisons, was used. The activated regions were located with help of the Tailairach-space.
10.2.8
Evaluation parameters
Temperature (surface skin temperature and room temperature), Flux, partially simultaneous and continuous measurement of mean blood flow velocity (vm) in the OA, MCA, PCA and ACA at different measurement times (a - e) were determined. A number of test persons underwent testing using different acupuncture schemes. The interval between the single experiments was 30 minutes to one day, and the test persons were instructed to keep their eyes closed during the entire active examination phase. In a similar manner to fMRI-examination, the test persons were unable to determine whether the laserneedles had been activated or deactivated.
10.3 Results Figure 10.1 shows in summary the results of an animal study [13] and a nontherapeutic biomedical engineering study with test persons [8,9] regarding the periphery effects of laserneedle acupuncture. The Flux, hand and room temperature parameters were summarized at different measurement points. The significant (p = 0.005) increase of Flux in the test persons during 20 minutes of laserneedle stimulation (b - d) must be considered. The results of the animal study show that laserneedle stimulation (wavelength: 685 nm; power density: 4.6 kJ/cm² per point; duration 20 min) can cause alterations in microcirculatory parameters of the skin, in the sense of increased circulation, however, the laser quality and intensity did not induce any micro-morphological changes in the skin [13].
116 Scientific studies - laserneedle acupuncture Peripheral effects: temperature and laser Doppler flowmetry Animal experiment (sus scrofa domesticus)
Healthy volunteers: mean age + SD: 24.4 + 2.6 yrs; 12 f, 10 m
n=1
n = 22
p = 0.005 p = 0.02
45
34
Temp. 32 (°C)
40
Temp. (°C) 35 Flux (a.u.)
30 Temp. R.-Temp. Flux
30
Flux 28 (a.u.)
Temp. R.-Temp. Flux
26 24
25
22 20
a
b
c
d
e
n=1
20 min modified from: Biomed. Technik, 2004, 49: 2-5 [13]
20
a
b
c
d
e
n = 22
20 min modified from: Neurol. Res., 2003, 25: 722-728 [9]
Fig. 10.1: Animal (left side) and human experimental (right side) studies using laserneedle stimulation. Flux (product of concentration and velocity of erythrocytes), surface skin temperature (Temp.) and room temperature (R.-Temp) before (a), during (b – d) and after (e) laserneedle activation.
Figures 10.2 and 10.3 document specific changes in cerebral blood flow velocities in different arteries. Using the laser acupuncture scheme (TCM: Zanzhu and Yuyao; ear: eye and liver; KHA: E2; CHA: Yan Dian) the blood flow velocity in the OA using a wavelength of 685 nm increases significantly (p = 0.01). However, a 30 % increase in stimulation intensity only increases vm in the OA to a mean value of 11 %. Simultaneously, no significant changes in vm occurred in the MCA. Using laserneedle acupuncture with a wavelength of 785 nm, a marked, but insignificant (p = 0.546) increase in vm in the OA during stimulus application occurred. Brief stimulation (20 sec each) of the single points with a hand-held low level laser (19 mW), did not reveal any significant (p = 0.939) differences in vm in the OA, concerning the conditions before and after stimulation.
117 Scientific studies - laserneedle acupuncture Cerebral effects: fTCD / OA - MCA Volunteers: n = 27; mean age + SD: 25.2 + 4.1 yrs, 21 - 38 yrs 14 f, 13 m Laserneedle acupuncture
Volunteers: n = 25; mean age + SD: 24.5 + 3.8 yrs, 18 - 34 yrs 14 f, 11 m Laserneedle acupuncture intensity +30 %
Laserneedle acupuncture
Ophthalmic artery (OA) 20
15
a
15
SE 10
p<0.01*
a
c
Middle cerebral artery (MCA)
b
p=0.939
15
SE
p=0.01*
60
20
p=0.546
15
10
Ophthalmic artery (OA)
20
b
b
685 nm
Ophthalmic artery (OA)
Ophthalmic artery (OA)
vm (cm/s)
Low Level Laser
785 nm
685 nm
685 nm
20
Volunteers: n = 18; mean age + SD: 24.8 + 3.3 yrs, 18 - 35 yrs 9 f, 9 m
c
10
b a
SE
SE
c
10
a
c
Middle cerebral artery (MCA)
b
60
50
a
c
40
a
c
Fig. 10.2: Specific changes in mean blood flow velocity (vm) under laserneedle acupuncture (from left to right: 685 nm, 685 nm with increased intensity (+ 30 %), 785 nm and 685 nm (19 mW)). Mean values and standard error (SE) before (a), during (b) and after (c) stimulation are shown.
Figure 10.3 shows the changes in vm in the ACA and PCA when applying different laser puncture schemes (A, B). When using laser puncture scheme A, vm increased during stimulation (b - d) significantly in the ACA (p < 0.001) and is still higher at the end of the experiment (e) than before laser puncture (a). At the same time, insignificant changes in vm occurred in the PCA. During optical stimulation of the acupuncture points in scheme B, a significant increase (p < 0.002) in vm in the PCA took place although simultaneously insignificant changes in the ACA were observed.
118 Volunteers n=22 12 female, 10 male, 21 - 29 years ( 24.4 + 2.6 years; x + SD ) R
Laser puncture scheme A
Laser puncture scheme B
Anterior cerebral artery (ACA) vm (cm/s)
Anterior cerebral artery (ACA) vm (cm/s)
50
52
49
51
*)
48
50
47
49
46
48
45
47 a
b
c
d
n.s.
e
a
b
c
d
e
*) p < 0.001
Posterior cerebral artery (PCA) 45
Posterior cerebral artery (PCA) vm (cm/s)
vm (cm/s)
47 46
44
45
43
*)
44
42
n.s.
41
43 42
40 a
b
c
d
e
a
b
c
d
e
*) p < 0.002
Fig. 10.3: Laserneedle acupuncture study in a double-blinded randomised, crossover design. Changes in blood flow vm before (a), during (b - d) and after (e) activation of laserneedles according to the specific laser puncture scheme (A or B).
119 The first fMRI-results using laserneedle acupuncture are summarized in Figure 10.4. Significant (p < 0.05) changes in brain activity were registered in the occipital and frontal regions during stimulation of distant, visual acupuncture points and near the olfactory cortex during the activation of acupuncture points, which according to Traditional Chinese Medicine, have a connection to the sense of smell. Further, significant (p < 0.001) activation after stimulating the Yintang point in the fronto-parieto-temporal region, with massive EEG-alterations (appearance of frontal Delta-activity) occurred [10]. Scientific studies - laserneedle acupuncture Cerebral effects: fMRI Vision related acupoints
H.B., 27 y, f modified from: Las. Med. Sci., 2004; 19: 6-11 [11]
Olfactory system related acupoints
L.A., 28 y, f modified from: Schmerz & Akupunktur, 2004; 1: 4-11 [12]
Yintang
E.S., 28 y, f
E.M., 29 y, m
p < 0.001 (correction for multiple comparisons)
Fig. 10.4: Functional magnetic resonance images illustrating activated cerebral regions after laserneedle stimulation. Specific cerebral activation patterns are shown according to the selected acupuncture schemes.
Figure 10.5 shows, in summary, frontal and non-invasively registered changes in O2Hb during and after needle or laserneedle acupuncture (same scheme as in Fig. 10.2). Whereas nearly no changes during acupuncture of placebo points take place, increases during laserneedle acupuncture are obvious.
120 Scientific studies - laserneedle acupuncture Cerebral effects: NIRS
Fig. 10.5: Cerebral changes in near infrared spectroscopy in µmol of oxyhaemoglobin (O2Hb) during needling of a placebo point, 3 hand acupuncture points, 2 ear acupuncture points, 2 body acupuncture points according to TCM, a combination of hand, ear and body acupuncture points, as well as laserneedle stimulation, and increased (+ 30 %) laserneedle stimulation (from left to right), during and 5 minutes after acupuncture. Modified according to [6].
Figure 10.6 at the left, shows the hypothetically assumed course of stimulus intensity, in random units of a metal and laserneedle as a function of time. At the middle and at the right, real time signals registered with NIRS and bioelectric methods (EEG - BIS) are illustrated.
121
metal needle
Stimulus intensity SI [a.u.]
hypothesis
NIRS-response
EEG-BIS-response
O2Hb 100
metal needle 90
HHb
10 min
10 min
laserneedle
Stimulus intensity SI [a.u.]
time [min]
O2Hb laserneedle
100
90
HHb time [min]
10 min
10 min
B.J., 22y, f modified from: Spectroscopy 2002; 16: 335-342 [6]
modified from: Spectroscopy 2002; 16: 335-342 [6]
H.E., 25y, f modified from: Europ. J. Anaesthesiol. 2004; 21: 13-19 [10]
Fig. 10.6: Stimulus intensity (SI) as a function of time. From left to right: hypothesis, real measured cerebral reactions of near infrared spectroscopy measurement parameters O2Hb (Oxyhaemoglobin) and HHb (Desoxyhaemoglobin), as well as the bioelectric response (BIS = Bispectral index). Modified according to [4,6,10].
10.4 Discussion The term „laser“ is very fascinating for many people today. Innovation and laser are nearly synonymous. Albert Einstein, already formulated the physical foundation for so-called light intensification with stimulated emission, in 1917. In the field of medicine, laser not only allows careful treatment for patients, but also a manifold of selective therapies in nearly all special fields. Laser has developed to be an important instrument in acupuncture when considering the treatment of small children, or patients with a phobia against needles. One goal of this study is to give a summary about previous clinical experimental studies dealing with this new method of optical acupuncture stimulation. Since the test person or patient does not feel the intervention, furthermore, the different acupuncture points can be stimulated continuously and simultaneously, it was possible to perform these double-blind randomised, controlled, cross-over studies for the first time. The studies indicate that cerebral effects of this manner of stimulation are nearly equivalent to that in needles. In addition to complex multi-directional sonography, it was also possible to provide proof regarding cerebral functional changes after laserneedle stimulation using functional magnetic
122 resonance imaging for the first time. At the same time, points “near the head” could be stimulated during fMRI examination, which was not possible thus far with acupuncture needles and hand-held laser instruments. The new scientific results may be of great importance, not only for the field of laser medicine, but also for acupuncture research in general.
10.5 Conclusion For the first time, laserneedle acupuncture allows simultaneous optical stimulation of individual puncture point combinations. Variations in acupuncture on the body, ear or hand, as performed and described in these studies are also possible. The studies were able to objectify and specify the cerebral effects of laserneedle stimulation for the first time. The cerebral effects triggered by this new, painless laserneedle technique are of similar dimension to those evoked by manual needle acupuncture. Painless laserneedle acupuncture can induce specific, reproducible changes in the brain. These can be expressed by shifts in different parameters, such as cerebral blood flow velocity [15].
10.6 Acknowledgements The authors would like to thank Ingrid Gaischek MSc (Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University of Graz) for her valuable support in this study.
10.7 References [1] [2]
[3]
Litscher G, Schikora D (2002) Cerebral effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Neue Konzepte in der experimentellen Akupunkturforschung - Computerkontrollierte Laserpunktur (CCL) mit der Laserneedle® Technik. Der Akupunkturarzt / Aurikulotherapeut 28: 18-28 Litscher G, Schikora D (2002) Effects of new noninvasive laserneedles on brain function. In: Hutten H, Krösl K, editors. EMBEC 2002. Proceedings of the 2nd European Medical & Biological Engineering Conference; 2002 Dec 4-8; Vienna, Austria. Graz; Verlag der Technischen Universität Graz, 996-997
123 [4] [5]
[6] [7] [8] [9] [10]
[11]
[12]
[13]
[14] [15]
Litscher G, Schikora D (2002) Nahinfrarot-spektroskopische Untersuchungen zur Nadel und Laserakupunktur. AKU 30: 140-146 Litscher G, Schikora D (2003) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Internet J Neuromonitoring 3(2). URL: http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijnm/vol3n 1/nirs.xml Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Litscher G (2003) Lasernadelakupunktur - Eine neue nicht-invasive optische Akupunkturstimulationsmethode. Dt. Ztschr. f. Akupunktur 1: News Litscher G (2003) Laserneedle®-Akupunktur auf dem Prüfstand der Wissenschaft. Schweizerische Z f Ganzheitsmedizin 15: 253-259 Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Litscher G (2004) Effects of acupressure, manual acupuncture and Laserneedle® acupuncture on EEG bispectral index (BIS) and spectral edge frequency (SEF) in healthy volunteers. Europ J Anaesthesiol 21: 13-19 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laserneedles modulates brain function: First evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI). Lasers Med Sci 19: 6-11 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D (2004) Die schmerzfreie Lasernadelakupunktur moduliert die Gehirnaktivität: Erste Nachweise mit funktioneller transkranieller Dopplersonographie (fTCD) und funktionellem Magnetresonanzimaging (fMRI). Schmerz & Akupunktur 1: 4-11 Litscher G, Nemetz W, Smolle J, Schwarz G, Schikora D, Uranüs S (2004) Histologische Untersuchungen zu mikromorphologischen Einflüssen von Lasernadelstrahlung. Ergebnisse einer tierexperimentellen Untersuchung. Biomed Technik 49: 2-5 Litscher G, Schikora D (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Riga Rom Viernheim Wien Zagreb Litscher G, Wang L, Schikora D, Rachbauer D, Schwarz G, Schöpfer A, Ropele S, Huber E (2004) Biological effects of painless laserneedle acupuncture. Medical Acupuncture 16(1): 24-29
124
11. Increases in intracranial pressure and changes in blood flow velocity due to acupressure, needle and laserneedle acupuncture? G. Litscher, L. Wang, G. Schwarz, D. Schikora 11.1 Introduction Acupressure of points St.7 and SJ.22 can lead to significant, reversible ICPincreases in intensive care patients with a priori elevated intracranial pressure (ICP) [1]. Our study group already documented this in 1988. These increases in intracranial pressure due to acupressure can reach a threatening extent in isolated cases. Goal of this study was to evaluate whether stimulation of the acupoints mentioned above using different stimulation techniques, also leads to changes in cerebral parameters combined with alterations in ICP, in healthy volunteers.
11.2 Material and methods 11.2.1
Volunteers, patient, acupressure and procedure
We investigated a total of 34 healthy volunteers (24 females, 10 males) and a 15-year-old intensive care patient after severe head injury. The mean age of the volunteers (Cx r SD) was 25.2 r 3.4 years (range: 20 - 35 years). The test persons were informed about the study procedure and gave their written consent. A ten minute resting period on a bed prior to investigation was observed. During this time, the measurement device was applied. The study was approved by the local Ethical Committee at the Medical University in Graz. The following acupoints [2,3] were tested on each person, during three partial unilateral (right) measurements (Fig. 11.1):
125 St.7 (Xia Guan) Localisation: In front of the articular process of the mandible, below the zygomatic arch, in a depression, it can be located when the mouth is closed. Needling: Vertical, 5 fen - 1 cun. SJ.22 (He Liao) Localisation: Ventral and cranial from SJ.23, at the beginning of the auricle, at the back edge of the temporal hairline (behind the pulse point of the temporal superficial artery). Needling: Slanted, 2 - 3 fen.
St.7
SJ.22
Fig. 11.1: Laserneedle stimulation in a volunteer during simultaneous monitoring of blood flow velocity in the right and left middle cerebral artery and frontal near infrared spectroscopy parameters (acupuncture scheme according [3]).
We used acupressure, manual needle acupuncture and laserneedle acupuncture for stimulation in all of our test persons. In order to guarantee reliability and reproducibility of acupressure and acupuncture, the stimulation in all of our volunteers, was performed by the same Chinese expert for Traditional Chinese Medicine (TCM). The thumb pressure applied to the acupoints was ~ 3 x 10.5 Pa (force ~ 30 N) determined by force and area, whereby both points were stimulated intermittently during a total time of 5 minutes.
126 Manual needle acupuncture was performed with sterile one-use needles 30 x 30 mm (Huan Qiu; Suzhou; China). Needle stimulation was done in 2 minute intervals for 20 s and included a combination of rotating, pressing and thrusting motions. After a total of 5 minutes, the needles were removed. Laserneedle stimulation is based on a multi-channel system with 8 separate semi-conductor laser diodes and emissive wavelengths from 685 to 785 nm. The system consists of flexible optic fibres, which conduct laser light to the laserneedle without loss. Thereby, a high optical density at the distal laserneedle end is achieved. The intensity of the laserneedles is optimized in such a way, that the volunteer does not feel the activation of the needle (30 40 mW per needle; diameter 500 µm; time 5 min; energy density 1.2 kJ/cm² per acupoint). For more details regarding this method, see the previous studies [4-8]. The measurement procedure scheme is illustrated in Figure 11.2 and applies to all stimulation techniques. The time between the particular stimulation techniques was at least 10 minutes and the sequence of application was performed at random.
d
3 min
5 min
b 1 min
a 1 min
Fig. 11.2: Measurement profile of the volunteer study. The measurement points were determined before (b), during (d) and after (a) stimulation. The plateau increase indicates the “active time” of acupressure, needle- and laserneedle acupuncture.
11.2.2
Measurement techniques, statistical analysis
evaluation
parameters
and
A Multi-Dop T System (DWL Electronic Systems GmbH, Sipplingen, Germany) combined with functional multi-directional transcranial Doppler sonography (TCD) were used for measuring mean blood flow velocities.
127 Two 2-MHz-probes (A. cerebri media (MCA)) were used in an ultrasound probe-holding construction (compare Fig. 11.1). We evaluated the mean blood flow velocities (vm) in the right and left MCA as well as the pulsatility index (PI = (systolic maximum value – end diastolic maximum value)/mean value) in both cerebral vessels, before, during and after the different stimulation techniques. In addition, near infrared spectroscopy (NIRS) with an INVOS 5100 cerebral oximeter (Somanetics, Troy, USA) at the frontal left as well as right, and registration of blood pressure (Cardiocap, Datex, Hoevelaken, Netherlands) were performed. Measurement values were graphically presented as box-plots and were analysed with the paired t-test (level of significance p < 0.05). The computer programs SigmaStat and SigmaPlot (Jandel Scientific Corp., Erkrath, Germany) were used.
11.3 Results Figure 11.3 exemplarily shows the registration of ICP and blood pressure (A. radialis) during bilateral as well as unilateral acupressure in a 15-year-old patient with severe head injury. During acupressure, significant and steep increases in ICP occur, which first subside after terminating stimulation.
128
mmHg 50
kPa 6.7
ICP 40
5.3
150
20
80
11
BP 10 min
Fig. 11.3: Time course of intracranial pressure (ICP) and blood pressure (BP) during acupressure of points St.7 and SJ.22 in a 15-year-old patient after severe head injury. Direction of recordings from right to left (arrow). Observe the ICP increase during bilateral (b) and left (l) or right (r) acupressure.
Figures 11.4 and 11.5 summarize the results of transcranial Doppler sonography in healthy volunteers. The results show that significant increases in blood flow velocity in both MCA´s occur during acupressure (Fig. 11.4a). These effects remain present after completing acupressure. Inverse behaviour is shown in the pulsatility index (compare Fig. 11.5a). To a certain extent, significant and similar in trend, but somewhat damped amplitudes in the response pattern can be observed in manual needle (Fig. 11.4b, 11.5b) and laserneedle acupuncture (Fig. 11.4c, 11.5c).
129 p = 0.006
vm (cm/s) 100
p = 0.003
p < 0.001
p < 0.001
80
60
a
40
20
0
left
right
n=34
paired t-test
before
during
after before Acupressure
during
after
vm (cm/s) 120
p = 0.231 (n.s.) p < 0.001
100
p = 0.003 p < 0.001
80
b
60
40
20
0
left
right
n=34
paired t-test
before
vm (cm/s)
during
after before during Needle Acupuncture
p = 0.026
100
p = 0.061 (n.s.)
after
p = 0.015 p = 0.717 (n.s.)
80
c
60
40
20
0
left
right
n=34 before
paired t-test during after before during Laserneedle Acupuncture
after
Fig. 11.4: Box plot illustration of changes in mean blood flow velocity in the right and left middle cerebral artery (MCA) in 34 healthy volunteers, before, during and after acupressure (a), needle acupuncture (b) and laserneedle acupuncture (c). The horizontal line in the box gives the position of the median. The end of the box defines the 25th and 75th percentile; the error bars mark the 10th and 90th percentile.
130 p = 0.147 (n.s.)
PI
p = 0.007
1,8
p = 0.162 (n.s.)
1,6
p = 0.007 1,4 1,2
a
1,0 0,8 0,6 0,4
left
right
0,2 0,0
paired t-test
n=34 before
PI
during
after before Acupressure
during
after
p = 0.374 (n.s.)
1,6
p = 0.044 1,4
p = 0.231 (n.s.) 1,2
p = 0.003
1,0
b
0,8 0,6 0,4
left
right
0,2 0,0
n=34
paired t-test
before
during
after before during Needle Acupuncture
after
PI 1,6
p = 0.924 (n.s.) p = 0.498 (n.s.)
1,4
p = 0.219 (n.s.) p = 0.012
1,2 1,0
c
0,8 0,6 0,4
left
right
0,2 0,0
n=34 before
paired t-test during after before during Laserneedle Acupuncture
after
Fig. 11.5: Box plot illustration of changes in pulsatility index (PI) in the right and left middle cerebral artery before, during and after acupressure (a), needle acupuncture (b) and laserneedle acupuncture (c). For further description see Fig. 11.4.
131 Regional cerebral oxygen saturation and blood pressure did not show any significant stimulation-related changes (compare Tab. 11.1).
Tab. 11.1: Regional cerebral oxygen saturation (rSO2) and blood pressure (BP sys = systolic, BP dia = diastolic and MAP = mean arterial pressure). Mean values (Cx) and standard deviation (SD) under different test circumstances are noted.
11.4 Discussion Intracranial pressure is defined as the pressure which the brain within the skull (including the subarachnoid cavities), exerts on the surrounding dura mater. This is particularly important under pathological circumstances, since it influences cerebral perfusion as well as the oxygen and nutrient supply. An increasing ICP consecutively leads to a decrease in cerebral perfusion. If brain injury or damage by bleeding occurs, ICP can increase, however the surrounding bones cannot give way. This finally can lead to further damage of the brain reaching to transtentorial herniation or in extreme cases to brain death. Investigations using auditory evoked brainstem potentials in intensive care patients with increased intracranial pressure showed that the application of headphones alone, without activating acoustic stimulation can lead to significant, and upon removal, reversible ICP-increases [1,9]. The use of acupressure with similar pressing action, could also achieve these effects (compare Fig. 11.3). We assumed that the mechanical transmission of pressure from the headphones, or finger pressure on the end cranium as a result of loss of bone stability after skull fractures or after bi-temporal osteoclastic bone trepanation could be hypothetical potential causes. Further hypothesis were the triggering of reflex mechanisms during application of the headphone holder or finger pressure above the structures in the retro-mandible region or as a result of impaired venous blood flow [9].
132 An additive hypothetical approach which suggests a possible stimulation of local acupoints was also systematically investigated in this study using TCD. The effects of the individual stimulation techniques on regional cerebral oxygen saturation could not be proven with continuous NIRS monitoring. Non-invasive, intermittent blood pressure measurement on volunteers differs methodically from continuous invasive blood pressure registration in intensive care patients regarding reproducibility and time. The missing correlation between stimulation and blood pressure cannot exclude a possible accompanying brief systemic hemodynamic reaction resulting from the measurement window of the discontinuous measurement method. TCD has its origin in the year 1842 with the discovery and description of the Doppler effect by the Austrian physicist Christian Doppler. In the 80´s of the past century, Aaslid et al. [10] used the temporal acoustic window to overcome the barrier of cranial bones. As a result, TCD has become a noninvasive method for evaluating blood flow velocity in intracranial vessels. Cerebral blood flow parameters can either be determined mathematically from the blood or cerebral pressure (cerebral perfusion pressure – corresponds to the difference resulting from the mean arterial blood pressure and transcranial pressure) or with TCD (blood flow velocity). The close correlation between TCD parameters and intracranial pressure are discussed and proven in several studies. In this manner, systemic-theoretical approaches with simultaneous analysis of blood flow velocity and arterial blood pressure enable transformation to the cerebral pressure curve with a Dirac-impulse [11]. Clinical use of this non-invasive monitoring method is being currently discussed. The systemic-theoretical combination of the parameters described above is the foundation of our studies on healthy volunteers using TCD. It allows the direct and indirect connection of measurement data with transcranial pressure measurements, in intensive care patients. Hypothetically, we must consider the following components in our explanatory models: It is possible that acupressure, acupuncture and laserneedle acupuncture at the acupoints St.7 and SJ.22 induce changes in cerebral parameters, which can increase already elevated intracranial pressure in intensive care patients. They can also induce cerebral effects in healthy volunteers which are explainable by similar mechanisms. Thus, the attributes “gentle, alternative and free of side effects”, which are associated with TCM are not weakened inconsiderably. As the results from this study show, there are some signs of possible connections to side effects
133 which can occur under particular patho-physiological pre-conditions. In other words, it is obvious that also methods of TCM require exact diagnostics, determination of indication and selection of methods.
11.5 Acknowledgements The authors thank Ms. Ingrid Gaischek MSc for her valuable help and for writing the manuscript.
11.6 References [1]
[2] [3] [4] [5]
[6] [7] [8] [9] [10] [11]
Schwarz G, Pfurtscheller G, Tritthart H, List WF (1988) Hirndruckanstieg beim Monitoring akustisch evozierter Hirnstammpotentiale mittels Kopfhörer. Neurochirurgia (Stuttg) 31: 216-218 König G, Wancura I (1989) Neue chinesische Akupunktur. Lehrbuch und Atlas der Akupunktur-Punkte, 5. Auflage. Verlag Wilhelm Maudrich, Wien-München-Bern Hecker U, Steveling A, Peuker E, Kastner J (2001) Lehrbuch und Repetitorium Akupunktur. Hippokrates, Stuttgart Litscher G, Schikora D (2002) Cerebral effects of non-invasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laserneedles modulates brain function: First evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI). Lasers Med Sci 19: 6-11 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16/3-4: 335-342 Litscher G, Schikora D (Hrsg.) (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Bremen Litscher G, Wang L, Schikora D, Rachbauer D, Schwarz G, Schöpfer A, Ropele S, Huber E (2004) Biological effects of painless laserneedle acupuncture. Medical Acupuncture 16(1): 24-29 Schwarz G (1990) Dissoziierter Hirntod. Computergestützte Verfahren in Diagnostik und Dokumentation. Springer, Berlin Heidelberg New York Aaslid R, Markwalder TM, Nornes H (1982) Non-invasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg 57: 769-774 Schmidt B (2003) Nichtinvasive Erfassung des Hirndrucks mittels des transkraniellen Dopplersignals und der Blutdruckkurve unter
134 Verwendung systemtheoretischer Methoden. Dissertation, Technische Universität Chemnitz
135
12. Laserneedle acupuncture - clinical studies M. Weber 12.1 Introduction For the first time, laserneedles using a high optical energy output were applied at multiple points allowing painless and simultaneous 8-point treatment in accordance with traditional Chinese acupuncture. The laserneedles were developed by the German company Laserneedle® systems [1] and were first introduced at the Medica-fair 2000 in Germany (Fig. 12.1).
Fig. 12.1: Front view of the laserneedle instrument with 8 optical energy outputs.
The basis of laserneedle therapy combines the positive biological stimulation of tissues with laser rays, for analgesia, muscle relaxation, promotion of microcirculation and the stimulation of the immune system, with the traditional methods of classic acupuncture. In other words, simultaneous needling using an 8 point combination is performed. During the period of study 73 patients with various illnesses were treated. A prerequisite for taking part in this study was that all other forms of conventional treatment had been tried out, including medication, physiotherapy etc. without satisfaction or cure of the patient. To assess the success-rate, two scales
136 ranging from 0 - 100 were used. First the patients noted their level of contentment and secondly their individual pain-level.
12.2 Material, patients and methods Research was performed between January and May 2001 in a general practitioner’s office; the physician was certified in both body- and ear acupuncture. The patients treated were aged between 21 and 91 years. The majority of the patients treated had chronic or a strong tendency towards chronic illnesses, partly with acute or subacute symptoms. Approximately 70 % of the patients were female, 30 % male. For body acupuncture (Fig. 12.2), 8 exactly positioned laserneedles were used simultaneously. Optimum duration of treatment was 15 minutes. For ear- and skull-acupuncture (Fig. 12.3, Fig. 12.4), the laserneedles were exactly positioned by using a special headgear for fixation. The optimum duration of treatment in these cases was 5 minutes. The acupoints were located with common methods, such as the RAC-feeler and location with a 3 Volt-hammer by Bahr, or by applying simple pressure on pain sensitive areas. Corresponding points at the ear were also determined using the RACmethod or with a pointselect apparatus. In general we note that the triggering of a distinct, acupuncture-specific De-Qi sensation is an absolute must for effective acupuncture therapy [2-4].
Fig. 12.2: Typical examples of body acupuncture with activated laserneedles.
137
Fig. 12.3: Application of a laserneedle for ear acupuncture using a special headgear for fixation.
Fig. 12.4: Typical ear acupuncture treatment after activating the laserneedle device.
138 We could show that laserneedles invoked the characteristically pleasant DeQi sensation in 450 treatments (over 90 % of all cases treated) which was described as a gentle tingling and flowing of warmth into the extremities. After treatment, the patients felt pleasantly relaxed and slightly tired. In comparison to the classic metal needles, which we have been using for acupuncture in our office for the past 10 years, the frequency of De-Qi events was significantly higher. The De-Qi feeling was achieved in all patients regardless of their illness, it was more intensive in acute cases than in chronic cases. Often, the De-Qi feeling intensified during the course of treatment, indicating an increased sensitivity towards laserneedle therapy. It is interesting to note that De-Qi events were often reached in each patient according to a defined time schedule, for example after 10 minutes in body and 1 minute in ear acupuncture. In all of the cases treated no side effects were registered. Normal complications in conjunction with traditional metal needle acupuncture such as needle collapse, bleeding, hematoma, pain, infections etc. can be completely ruled out with laserneedle therapy. In particular the following illnesses from various fields of medicine were treated (Tab. 12.1): Orthopaedics spinal syndromes herniated vertebral disk gonarthrosis coxarthrosis rhizarthrosis periarthritis of the shoulder epicondylitis humeri radialis tendinitis fibromyalgia syndrome and polyarthritis Morbus Bechterew
Neurology/Psych. paresis after stroke migraine/headache syndrome trigeminal nerve neuralgia tinnitus depression psychovegetative exhaustion
Internal medicine gastropathy AVD bronchial asthma
Tab. 12.1: Summary of the treated illness in the different medical fields.
139
12.3 Results 12.3.1
Lumbar, thoracic and cervical spine syndromes as well as post cervical and lumbar intervertebral disk prolapse
We treated local pain trigger points as well as the corresponding near points (i.e. UB.10, 11 and 13 for cervical spine syndrome, or 50, 51 and 52 for lumbar spine syndrome) and the distant acupuncture points such as UB.60 and 62, in addition, the over regional pain trigger points such as SI.3, LI.4, SJ.5 and GB.41. In case of superimposed psychic symptoms, we also used compensating points such as St.36 and Ki.6 and in stress symptoms often Liv.3. Compared with metal needle acupuncture, pain relief set in immediately after the first treatment and could be increased in each following session by means of the booster effect. Therefore, pain syndromes could be completely relieved after about 5 sessions. With simultaneous treatment of musclerelaxing and calming down points it was evident that a quick sedative, frightand stress-relieving reaction in patients was achieved. In a usual series of 10 treatment sessions, the results can be described as being exceptionally good. A large number of patients were completely free of pain or their pain was reduced to such an extent that their original quality of life returned. We could note that significant improvements in all therapy-resistant and therapied patients, particularly in those with chronic spinal problems took place. Older people achieved a higher mobility in the affected joints and enjoyed far less pain. Apparently the simultaneous effect of laser rays used in combination with the rules of classic acupuncture were responsible for this success. In most cases, analgesic and antirheumatic medication, such as ibuprofen, diclofenac or tramadol and even morphine pain killers could be either greatly reduced or completely terminated. Case example A 58-year-old female patient suffered a severe prolapse of the L5/S1 disks in December 2000 and was treated in a hospital for 4 weeks. She was discharged with therapy resistant acute pain, even after CT guided local injections and being placed on a maximum of pain medication. Further ambulatory treatment was ineffective. She was treated with laserneedles using the following point combination: UB.34, 36, 37, 40, 60 and 62 as well as St.36 and Du 2. After a few minutes, an intensive De-Qi sensation was built up during each session, and was described as a pleasant, warm tingling feeling flowing into the entire leg. After the 15-minute treatment period, pain was significantly reduced and
140 improvement in leg mobility was achieved. After 3 further sessions, the patient was able to go to parties and dance again. After 10 more sessions, only 10 % of the initial symptoms remained so that she went on holiday. Throughout treatment all pain relieving medication was gradually reduced and at the end of the therapy stopped. After 4 months this magnificent result remained unchanged. The individual pain score after the end of treatment was 20 %; the patient’s subjective satisfaction was 95 %.
12.3.2
Gonarthrosis, coxarthrosis, rhizarthrosis, periarthritis in the shoulder, epicondylitis, tendinitis, Morbus Bechterew and fibromyalgia-syndrome
Significant results were achieved after only 3 - 5 treatment sessions in the disorders mentioned above. Remarkable was the very high success rate for chronic epicondylitis during the initial phase of treatment. This illness is widespread in the general population and difficult to treat. After only a few sessions using local pain trigger points and further typical points such as SJ.5, LI.4, 11 and 12 and often additional treatment of neck rigidity with SJ.15 and cervical vertebrate points such as UB.10, the patients were able to go about their normal activities, take part in sports and other hobbies. Even chronic and impairing rhizarthrosis, which is intermittently treated with crystal-steroids, responded very well to lasering. We frequently included the corresponding local regional, local and distant trigger points (among others LI.1, 4, 5, Lu.9 and 10 as well as Pe.7). These types of disorders were also treated by the so-called TMM system (tendomuscular meridians), by additional needling of the ting- and tonus points and the equivalent reunion zones. This proved to be very useful and provides further evidence regarding the benefits of laserneedling. It is also interesting to note, that severe disorders like Morbus Bechterew and fibromyalgia, as well as chronic polyarthritis responded exceptionally well to treatment with laserneedles. In cases of year long impairment, great importance was attributed to the additional treatment of relaxing, sedating, stress relieving and energy stabilizing trigger points such as St.36, Ki.6, Ren 17, UB.60 and 62, SJ.5, GB.41, Lu.7, Liv.3 or Du 20, to compensate the psychological and depressive symptoms. We could prove that it is more effective to treat multiple points than to stimulate only single local pain points. This is particularly difficult in cases of fibromyalgia, where pain occurs throughout the entire body and constantly changes its location. The psychological background, especially in
141 fibromyalgia as well as polyarthritis is widely acknowledged and proven, thus, we have an initial point for a stabilizing treatment. In periarthritis of the shoulder, a long and impairing illness, the success rate of treatment was significant and effects were of long duration. Case example A 54-year-old male patient, suffering from Morbus Bechterew for over 20 years with partial stiffness of the lumbar vertebrae was treated with the following point combination: UB.31, 32 and 62, Du 2, Ki.6, St.36, Sp.6 and SI.3. During treatment a repeated intensive De-Qi occurred in the lumbar region and after about 10 minutes a pleasant feeling in both legs took place immediately after the first and each successive treatment. The patient was able to tie his shoelaces for the first time in years. Apparently due to relaxation of the painful muscle, the toe touching distance had improved by about 20 cm. The extreme pain described before treatment disappeared immediately, however recurred after some time, but not to the same extent as originally. The psychological condition and depressed mood as well as the sleeping disorders were greatly improved. After an observation period of 3 months the patient was without pain and could go about his hobbies and carefully increase his physical condition. The individual pain score at the end of treatment was 10 % and 100 % for the patient’s subjective well being.
12.3.3
Remaining paresis after stroke
Three patients who had suffered strokes with remaining paresis were treated in the regions of the affected extremities. A blood-flow increasing and muscle relaxing point combination was used with energy stabilizing points. In all 3 cases, a significant increase in mobility was achieved by reducing spasticity and improving the fine motor ability. Case example A 78-year-old female patient with painful, remaining paresis in her left arm was treated using the following point combination: LI.4 and 11, SI.3, Pe.6, SJ.5 and 15, Du 20 and St.36.
142 The elevation of her arm could be improved from 90 to 120 degrees after only 5 sessions. The patient was able to pull a dress over her head for the first time in 5 years. Pain reduction was achieved and fine motor ability was greatly improved. The subjective patient satisfaction was 90 %.
12.3.4
Cephalgia, migraine and trigeminal neuralgia
The necessary requirement prior to treating chronic headaches includes extensive neurological and radiological patient examination. In these indications we used local and distant trigger points. Migraine attacks could be rapidly reduced and after due course of treatment, stopped completely. Tension headaches could be treated quickly. Three patients suffering from tinnitus were treated. The results here were not as impressive as in other disorders; often the tone/noise symptoms could be reduced and sometimes stopped completely for a short time. Further longterm studies still need to be evaluated. Long-standing trigeminal nerve neuralgias were successfully treated after only 5 sessions and have not recurred to date. Employing laserneedles to the head proved to be absolutely easy, considering the location and application required. Case example A 53-year-old male patient suffering from right branch trigeminal neuralgia for over 20 years was treated with 400 mg of carbamazepin, then laserneedled with the following point combination: LI.4, SI.3, St.4, 5, 6, 36 and 44 including Ren 24. After the first session, a significant improvement was felt in the extremely painful right mouth-lip-area. After 3 further sessions no pain could be registered and carbamazepin was gradually reduced. In the following 2-month observation period, the patient remained free of pain for the first time in a decade. The pain score was rated with 0 - 5 %. The subjective patient satisfaction was 100 % in this case.
143 12.3.5
Arterial obstruction disease
Case example A patient with a persisting 10-year obstruction of the pelvis and a circulatory bypass could not be operated due to cardiac problems. After only 5 treatment sessions, his walking distance could be increased from 100 m to over 2000 m and he was free of pain. The following point combination was used: UB.40, 58 and 60, St.36 and 41, Liv.3, Ki.6, Sp.6. Obviously treatment led to an improvement in microcirculation and additional muscle relaxing effects. The subjective satisfaction was given at 95 %.
12.3.6
Gastropathy and bronchial asthma
In most cases, we are dealing with psychovegetative and other disorders, thus, a combination of organ related trigger points with sedating and stress relieving effects were of importance. In both diseases the patients’ health greatly improved after the first session. Case example A patient with a long-standing case history and diagnosis of nervous stomach was treated with the following combination of points: Pe.6, Sp.4, SI.3, Liv.3, St.36, Yintang, Ren 12 and UB.21. After a few sessions, nausea, vomiting, feeling bloated and nervous restlessness and dizziness vanished completely. The subjective satisfaction of the patient was 100 % and a 95 % symptom reduction was achieved.
12.3.7
Depression, exhaustion
anxiety,
panic
attacks,
psychovegetative
Spectacular results were achieved with laserneedles in the treatment of psychic and psychosomatic illnesses. The general practitioner’s experience shows that a large number of somatic related disorders are linked to depression. In these cases, treatment is extremely difficult and often leads to the prescription of addicting medication or psychotropic drugs. Especially younger patients frequently refuse these drugs.
144 Disorders such as burnout and exhaustion syndromes in conjunction with anxiety and panic attacks and depressive tendencies are extremely well treatable and show quick results. In general, psychotropic drugs could be stopped after only a few sessions. The same was true for pain relieving drugs in orthopaedic disorders. Patients who had been treated with sedating and anti depressive points were able to sleep better after only a few sessions. Their family life improved greatly. Laserneedle acupuncture considerably reduced illness-related absence from work. Case example A 35-year-old manager of a big company with stress-related exhaustion syndromes introduced herself to the practice. She suffered from anxiety, restlessness, sleep disturbances, headaches and sometimes vertigo. She was treated with the following combination: He.9 and 7, Lu.7, UB.62, Yintang, Liv.3, Du 20 and Ki.6. During the first session a soothing warmth flowing through the whole body was sensed, she felt very relaxed and deeply tired, which in turn led to a good night’s sleep. After only 3 sessions the patient was able to resume her high-pressure job. The patient’s subjective satisfaction was 100 %; the symptoms could be reduced by 90 %.
12.4 Discussion In this report, more than 500 acupuncture treatments were performed with the newly developed laserneedles. Limitations were reduced by using up to 8 stimulation points simultaneously on the body or ear so that all the principle point combinations, either local, loco-regional and distant acupuncture points could be activated with the laserneedles. Treatment did not have any side effects, was extremely patient orientated, pleasant and highly effective in all indications. During the study, the number of patients asking for laserneedle treatment increased considerably. Because treatment is more pleasant for the patient, no needle pricking is necessary, and better results are achieved with laserneedles, acceptance is greater. Our experience showed large groups of patients are willing to use the laserneedle method. The advantages of laserneedle treatment in pediatrics are also obvious: painlessness and the higher rate of achieved De-Qi sensations. When we consider the economical point of view, treatment costs were considerably lower due to the reduction of required treatments, thus,
145 expensive pain therapies, psychotherapy and physiotherapy became obsolete. Patients being incapable of working due to orthopaedic, psychiatric and psychosomatic disorders could also be significantly reduced. We would like to note the frequency of chronic spinal problems, which lead to great financial losses in our economy each year. Using this new laserneedle acupuncture technology, we could reduce therapy resistant complaints, especially in older patients, so that prescription of non-steroid antirheumatics could be reduced respectively. Therefore unwanted side effects such as ulcers, gastrointestinal bleeding, liver and kidney damage do not occur. The special effects laserneedle treatment has on psychiatric and psychosomatic disorders in connection with anxiety and panic disturbances should not be neglected and is also of considerable importance. These disturbances always lead to difficulties for the general practitioner because they often become chronic, are very time consuming to treat, medication therapy may be restricted and all in all are extremely difficult to treat. Patients who experience difficult phases in their lives - adolescence, mid-life crisis, senile depression, psychological exhaustion and burnout syndrome can be treated easily and successfully. These patients, who often have consulted many specialists in their ordeal, accepted laserneedle treatment exceptionally well. By presenting a new strategy they feel that their problems are being taken seriously. Naturally we suggest that acupuncture with the new laserneedle technology can only be part of a treatment concept. Before treatment is done, thorough examination and diagnosis of each patient must take place. In conclusion, acupuncture treatment with the new laserneedle technology in the general practitioner’s office is superior to the classic metal needle acupuncture methods. We must consider the therapeutical results and effects, the duration and effectiveness after treatment and the frequency of treatment. Lastly we would like to mention that remarkable results were achieved with laserneedles in fields beyond normal usage of acupuncture. Dermatological illnesses, such as crucial ulcers, chronic eczema and acute inflammation of the skin and mucous membranes etc. were treated with great success. We will report on these findings at a later date.
12.5 References [1]
Laserneedle systems GmbH (2001) Benutzerhandbuch Akupunkturtherapie mit Lasernadeln. http://www.laserneedle.de
zur
146 [2] [3] [4]
Kersken T (1993) Einschätzung der handwerklichen Qualität durchgeführter Akupunkturtherapie in 86 Studien. In: Bühring M, Kemper F (Eds.) (1993) Naturheilverfahren. Springer, Berlin Stux G, Stiller N, Pomeranz B (1993) Akupunktur. Lehrbuch und Atlas. Springer, Berlin Ter Riet G, Kleijnen J, Knipschild P (1990) Acupuncture and chronic pain: a criteria-based meta-analysis. J Clin Epidemiol 43/11: 11911199
147
13. Pain therapy with laserneedle acupuncture R. Helling 13.1 Introduction The cases described in this chapter do not have the same value of an actual study, however, clearly show the therapeutic effects of non-invasive laserneedle acupuncture. The cases described, were solely treated with laserneedle acupuncture.
13.2 Case reports A 48-year old female with idiopathic trigeminal neuralgia of the left second branch was treated. A specialist ruled out differential diagnostically important causes such as cranio-mandibular dysfunction, maxillary sinusitis, or post zoster neuralgia. No odontogenous disturbances were evident. Drug therapy with Carbamacepin and Baclofen® led to insignificant pain reduction, therapeutic and local anaesthetic blocks of the pterygopalatine ganglion, as well as stellate blocks only achieved pain reduction for about 2 days. Despite massive pain, the patient was not willing to undergo surgical treatment with micro vascular decompression according to Janetta´s method. Laserneedle acupuncture was performed according to standard rules of acupuncture (see Fig. 13.1). The following acupuncture points were used: contra lateral St.2 – St.4 – SJ.21 bilateral LI.4 ipsilateral St.44 and Liv.3
148
Fig. 13.1: Acupuncture points used (modified from [1]).
13.3 Argumentation In case of highly painful local processes, local points on contra lateral sides are usually selected (St.2 – St.4 – SJ.21 ), in addition to distal points ipsi- or bilateral: LI.4: LI.4 is the so-called reference point for the large intestine meridian. This is the most important distant acupuncture point for pain in the facial
149 region. According to studies by Heine, somato-sensory afferents of LI.4 at the segment level of C4/C5 to Th1/2 are switched synaptically to the sensory neurons of the dorsal horns of the spinal cord. Thus, LI.4 has control action on all afferents and efferents running through the spinal cord. Because of the unique relationship of point LI.4 to the spinal cord, acupuncture of this point not only switches the afferents at the dorsal horns cord to the bulbo-spinal and spino-thalamic tracts, but connects the spinal nucleus of the trigeminal nerve and sympathetic cilio-spinal center via interneurons in the spinal cord. Both nuclear zones reach from rostral to the lower brain stem. Here, the connection to the principle nucleus of the trigeminal nerve takes place. According to Traditional Chinese Medicine (TCM) LI.4 frees the surface from external pathogenic factors (such as wind). TCM considers trigeminal neuralgia and facial paresis to be wind diseases. Liv.3: is the reference point of the liver meridian. Combined with LI.4, this point drives the wind out of the face [2,3]. St.44 as second to last point of the stomach meridian excellently influences the other end of the meridian, which begins at the face. St.44 is often used for pain in the face, which according to TCM is triggered by climatic factors. Because of severe pain, therapy with laserneedle acupuncture was performed daily for 20 minutes during the first week. In the second week, three acupuncture sessions (each lasting 20 minutes) were performed, in the third week only 2 sessions were made. According to the patient, pain reduction of about 50 % was achieved after the third therapy session. After the eighth session, the patient was free of pain; the last two points were only performed to stabilize the therapeutic effect. During the last 2 sessions, only the distant points LI.4 – Liv.3 – St.44 were still treated with laserneedle - acupuncture, the contralateral points at the face (St.2 – St.4 – SJ.21 ) were no longer treated. During the following observation period of 8 weeks, the patient was completely free of symptoms. This is particularly notable, since the patient only had one pain free interval for two to three days in the past seven years. A 35-year-old female patient with intercostal neuralgia, underwent unexplainable left-sided rhizotomy of the sensory and motory root from Th7 to Th11 (malpractice process is currently running). Rhizotomy did not lead to lindering pain; instead, permanent pain resulted, including the zone where surgery was performed and extending under the left thorax to the left pectoral region. Only high doses of Tramal® and Novalgin® led to pain
150 reduction of about 30 %. Opiates did not show any effects, local anaesthetic, paravertebral blocks caused additional pain. In the paravertebral surgical region, treatment with laserneedle acupuncture at six highly tender points, in the region of the surgical scar, was performed. The therapy zones were not selected according to the localisation of known acupuncture points, but based on so-called A-Shi- points (tenderpoints). According to TCM all points were located along the so-called Hua Tuo – Line (one transverse finger paravertebral). Treatment was performed once a week for 20 minutes. The weekly therapy interval exists since 4 months and is still being performed currently. After being completely free of pain for one week, massive pain of the previous intensity builds up within 24 hours. Since all therapeutic methods performed by several specialists were unable to achieve the effect of laserneedle acupuncture, the patient has decided to buy her own therapy device. According to the patient, she can achieve pain free intervals lasting one week, with this painless therapy method and can live well this way.
13.4 Discussion The two cases described here do not fulfil the criteria of a study. However, they impressively show the effectiveness of laserneedle acupuncture in two therapy resistant pain disorders. Independent from the effectiveness of laserneedle acupuncture, the author finds it very important to select the acupuncture points according to the following three criteria, especially when treating pain disorders: 1. The so-called intrinsic value of the acupuncture point must correspond with the demands. 2. The combination of acupuncture points must be additive regarding their effect. 3. The effect of acupuncture points must reach the localisation of pain (goal area) [3].
151
13.5 References [1] [2] [3]
Jiangping L, Yanliang C, Renhua S (1990) Chinese acupuncture and moxibustion. Publishing House of Shanghai College of Traditional Chinese Medicine, Shanghai Deadman P (1998) Großes Handbuch der Akupunktur. Verlag für Ganzheitliche Medizin, Kötzting Maciocia G (1994) Die Grundlagen der Chinesischen Medizin. Verlag für Traditionelle Chinesische Medizin, Kötzting
152
14. Pain therapy of osteoarthrosis / osteoarthritis-patients using the laserneedle system in a medical practice with emphasis on rheumatology and pain therapy K. Kolitsch 14.1 Introduction The largest joint of the body is the knee joint. Practically no other joint has to endure greater daily stress. Complex rolling and sliding movements guarantee high flexibility as well as stability. The required flexible connection between different bones is guaranteed by the perfect cooperation of muscles, tendons and ligaments. The knee joint consists of the articular condyle and articular cavity, and is surrounded by the synovial capsule – these establish the mobile connection between the upper and lower leg. Stabilisation of the joint is secured on the side with ligaments, the meniscus acts as shock absorbers. The synovioum, combined with synovial fluid and articular cartilage provide optimum slidability. In case of arthrosis, the articular cartilage is worn down, and in advanced stages, severe pain occurs, due to friction between the bones.
14.2 Patients and method Wear and tear of the knee joint reduces the quality of life for those who are affected. Especially these patients can be found in a medical practice with emphasis on rheumatology and pain therapy. The number of patients suffering from osteoarthritis of inflammatory, as well as generative genesis shows increasing tendency. The knee joint is the clinically the most often affected joint. The changed structure of aging in the population is responsible for this phenomenon. Today we assume that every arthrosis causes accompanying symptoms of arthritis. On the other hand, arthritis leads to the triggering of arthrosis. Due to severe pain resulting from advanced loss of articular cartilage, affected patients are nearly immobile. Only few therapies seem to be promising regarding stopping or slowing the further degeneration of articular cartilage. Exactly these patients – clients develop chronified pain symptoms or a chronic pain illness.
153 Practical studies show that a dramatic deficit in caring for patients with chronic pain exists. 75 % of osteoarthrosis/osteoarthritis patients are treated by a general practitioner. About 60 % do not receive adequate pain therapy. Effective pain treatment is still a foreign word for many older osteoarthrosis/ osteoarthritis patients. An untenable condition which risks the development of a pain career. Frequent change in physicians, alternative methods without competency and irregular medication are the result. In particular, modern pain therapy methods offer a multi-modal pain therapy concept for patients with chronic pain diseases. The qualified combination of drug and non-drug treatment, in connection with psychotherapeutic strategies, leads to an optimum of therapeutic results. Most important goal of treatment is the mobilisation of patients with chronic pain diseases. Goal is a variety of physical straining of the affected knee joint without repeated, one-sided movement. Stressing of the knee joint should be avoided which doesn´t follow the natural movement patters of this joint. In particular, torsional movements should be regarded as dangerous for the knee joint. Modern pain therapy offers patients a number of options within the multimodal treatment concept. Animated by the effectiveness of laserneedle therapy compared to needle acupuncture, we performed a laser therapy on 150 patients with osteoarthrosis/osteoarthritis. Drug or pain therapy remained unchanged. The patient collective included patients with osteoarthrosis/osteoarthritis stage I and II. The technical and scientific basis of the laserneedle system were thoroughly described by Litscher and Schikora [1-3]. Within observational use of the laserneedle system in pain therapy, prescription laser acupuncture was used. The following acupuncture and extra points were applied on 150 osteoarthrosis/osteoarthritis patients: Extra points: Nu Xi Jan Xiyan (Ex.32) Heding (Ex.31) Acupuncture points: St.34 GB.43 Sp.10
St.35 Sp.9
Figure 14.1 shows a patient undergoing laserneedle treatment.
154
Fig. 14.1: Laserneedle treatment in Dr. Kolitsch´s medical practice
Duration of laserneedle therapy was 20 minutes. All patients wrote a pain diary from STK (Schmerztherapeutisches Kolloquium) as pain therapy control. The first follow-up was made after completing therapy, the second, 4 weeks later.
14.3 Results Evaluation of the treatment data after completing therapy showed pain reduction of three graduation marks on the VAS (visual analog scale) in 65 % of the osteoarthrosis/osteoarthritis patients. After follow-up 4 weeks after completing therapy the result improved to 70 %. 70 % of the patients registered a reduction pain of 3 graduation marks on the VAS. 15 % of the osteoarthrosis/osteoarthritis patients showed a decrease in pain of 2 graduation marks on the VAS.
14.4 Discussion Evidence regarding efficiency is provided by the drug-free treatment with the laserneedle system within a multimodal pain therapy concept under remaining basis and or pain treatment (WHO – graduated scheme). As a result of reduced pain intensity, an increase in mobility in chronic pain patients was achieved with laserneedle therapy. Thereby this therapeutic option achieves measurable improvement in the quality of life. Long-term observations regarding the long-time effects of laserneedle therapy will provide further effective data regarding the efficiency of this therapy.
155
14.5 References [1] [2] [3]
Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342
156
15. Laserneedles in gynecology K. Staehler van Amerongen 15.1 Introduction The laserneedle technique is a new, non-invasive method to stimulate specific acupuncture points with laser light. The method and clinical effects are described in more recent scientific literature >1@. Unlike metal needles used in common acupuncture which are inserted into the skin, Laserneedles are adhered to the desired acupoints points using small adapters and a special adhesive technique.
Fig. 15.1: Laserneedles.
After activating the device, continuous, visible red laser light with a wavelength of 685 nm is applied via an optic fiber, directly to the acupoint with the laserneedle. Intensity of the laserneedle is optimized in such a way, that the patient barely feels the activation, however still builds up vegetative stimulation at the acupuncture point. It has been documented, that laserneedles at the acupoint trigger particular stimuli that is identical to the Qi sensation of metal needles. The device has 8 exits with corresponding cables. Therefore, laserneedle acupuncture makes the simultaneous stimulation of individual point combinations possible. As a result, all combinations of body, head, and ear acupuncture application are possible. Laserneedles can be applied alone or in combination with additional traditional acupuncture needles. The acupoint is stimulated by the continuous photon flow from the laserneedle. After subtraction of scattering losses, about 40 mW optic output is achieved at the distal end of the laserneedle. The actual dose per laserneedle at the skin during acupuncture treatment is 40 – 60 J >5@. The
157 power density of a laserneedle increases with the duration of treatment >2@. Absorption in tissue is minimal at this wavelength; therefore, no warming or burning of tissue as by surgical lasers occurs. The power of the laser light leads to triggering of action potentials >4@. Continuous stimulation generates a cascade of action potentials at the acupoint.
15.2 Material, test persons, technique The investigations took place during the time period between March and October 2003. Three-hundred women between 30 and 56 years were evaluated. All patients were treated during the acupuncture consultation hours at the University gynecological clinic. Different clinical pictures from the fields of gynecology and obstetrics were treated. In most cases, single body laserneedle treatment was performed. In 40 patients, additional application of laserneedles in the ear region was done. The clinical pictures treated included 265 gynecological patients and 35 obstetric patients. The gynecological clinical pictures included menstrual problems, cycle regulation, dysmenorrheal problems, hypothalamic amenorrhea, premenstrual bleeding, premenstrual and menstrual migraine headaches, back pain during menstruation, exhaustion, burn-out, hot flushes and flush during menopause, sterility and childlessness, bladder disorders, dysuria, uro-genital symptoms, and in the oncologic field, shoulder tension after breast surgery, tension and decreased arm mobility after breast surgery. Obstetric indications were induction of labor, carpal tunnel syndrome, hyper emesis and laser application during childbirth process. Selection of acupoints on the body was done using the common traditional Chinese medicine technique and according to the pressure sensitivity of the acupoints. Ear points were partially determined with RAC-touching or with the electric Pointselector. Laserneedles were activated at the acupoints for an average of 30 minutes. Since this method is still quite new, no well-founded results can be presented due to the small number of case studies.
158
15.3 Case studies 15.3.1
Induction of labor with laserneedles
A 23-year-old patient in the 40th week of gestation, after normal course of pregnancy came to the ambulant consultation hour for acupuncture to induce labor. It was her second pregnancy. The first child was a spontaneous delivery on the awaited date of birth, 2 years earlier. Now the belly was quiet and no signs of labor were present. The child was also quiet at the beginning of treatment. The vaginal examination showed an immature finding with closed sacral mouth of the uterus. The cervix was maintained and scirrhous. The patient wanted a „natural“ induction of labor without medication. Up until this time, no measures to induce labor had been performed. After comprehensive explanation of the different possibilities, the patient decided to induce labor with laserneedles at the usual acupoints. For her, the fact that laserneedles did not cause pain was significant since she knew that acupuncture with metal needles causes some pain during insertion. At the beginning of treatment, she was positioned in a relaxed, comfortable manner on the left side. Laserneedles were applied at points LI.4, St.36, GB.34 and Liv.3 with special adhesive tape.
Fig. 15.2: Induction of labor at points LI.4, St.36, GB.34 and Liv.3.
These are the common acupoints for inducing labor. Especially LI.4 (Fig. 15.3) is an important point to stimulate labor.
159
Fig. 15.3: Laserneedle-stimulation at LI.4.
Laser emission was activated simultaneously and continuously for 30 minutes at these 8 acupoints. During treatment, the patient could feel an increase in fetal movements and a minor cramping in the belly. Towards the end of treatment, her belly was hard four times. At point LI.4 she felt the most tingling. All in all, she felt well and relaxed. After completing laser application, the cramping in the belly stopped for the time being. She returned home on that afternoon. During the night she had to go to the hospital due to beginning labor. The first stage of labor in which the mouth of the uterus opens only lasted 3 hours. The second phase only lasted 20 minutes and 4 bearing-down pains. The entire birth took 3 ½ hours which was very fast. In addition, she said she felt very well and was very relaxed. She had enough energy to bear the child and said she perceived delivery as a very nice experience. In this case, the patient delivered quickly and comfortably. Remarkable was the short first phase of labor lasting only 3 hours. The literature describes that emotional and physical stress for mother and child has a clear influence on the length of childbirth. An „allowable duration of childbirth“ in plurpara patients is usually 8 hours during the first phase, 1 hour during the second phase and half an hour for bearing down. Altogether childbirth takes 9 ½ hours >3@. In our patient, childbirth only took 3 ½ hours. If this was due to the influence of the laserneedles or if she would have delivered so well without this measure remains a speculation. Noteworthy is the quick begin of labor after laserneedle treatment, the brief first phase of childbirth and the subjectively good feeling of having enough energy to achieve childbirth easily.
160 15.3.2
Carpal tunnel syndrome
A 22-year-old mother with a 2-year-old child came to my consultation hour in the 28th week of pregnancy. I knew her from her first pregnancy as she had severe pain and edema in both hands and I treated her for carpal tunnel syndrome with acupuncture. The current pregnancy was a twin pregnancy and she had the same symptoms with tingling in the hands especially at night. She complained about severe pain and weakness in the fingers so that she could barely pick up a cup from the table. Her hands were severely edematous. The severity of the symptoms was worse in this pregnancy than in the last. In the last pregnancy, she was treated with acupuncture needles at the acupoints Pe.6 and Pe.7.
Fig. 15.4: Needle acupuncture at points Pe.6 and Pe.7.
At that time, the symptoms increased after the first treatment, but improved distinctly after the third treatment. Eight sittings using common acupuncture with metal needles were performed, first 3 times a week, then once a week. The patient experienced slight pain during needling. After appropriate explanation, the patient wanted to try acupuncture with laserneedles. Again the same two acupoints Pe.6 and Pe.7 at the inside of the wrist were selected. The laserneedles were applied at these points and illuminated with laser light for 30 minutes. Coincidently, 8 sittings were
161 necessary again. After the first treatment, again, an increase in symptoms occurred. First the pain increased however after the second treatment she could feel an obvious improvement in her symptoms. It was a positive effect for her that the fixing of the needles with adhesive tape did not cause pain, contrary to the insertion of common acupuncture needles. During laserneedle acupuncture, she felt a warming sensation. She described this as comfortable and felt better being able to move her hands slightly during treatment without moving the needles. This small freedom of movement compared to common acupuncture was positive for her. The children were quite quiet during treatment. There were no signs of labor. Cardiotocogram (CTG) registration, twice during and twice immediately after treatment, showed normal heart action in both children and no signs of labor. The carpal tunnel syndrome symptoms improved distinctly. In the 35th week of pregnancy childbirth was performed with Caesarean section.
15.3.3
Urogenital symptoms, back pain, hot flushes
A 52-year-old patient was treated with common acupuncture against her year-long symptoms. She reported a constant feeling of pressure on the bladder coming from the bladder region. Because of nycturia she had to get out of bed 2 to 3 times per night, and during the day she had to go to the toilet every hour. She could hold her urine and did not have episodes of incontinence. She experienced the constant back pain in the lumbar region as the worst symptom and had to take 2 - 4 Voltaren 50 mg per day. Walking was strenuous and she could not carry much. Despite physiotherapy and bladder training, no success could be achieved. Blood pressure was stable with medication at 120/85 mmHg. Before treatment, the patient rated her pain with 8 on a 10 point pain scale. After extensive diagnostics, the patient was treated with common acupuncture using metal needles and combined body and ear acupuncture. The acupoints UB.28, 29, 30, 40 as well as Du 20 and Ren 3 on the body and the acupoints lumbar spine, hip and bladder at the ear were selected for acupuncture. The needles remained in place for 30 minutes without stimulation. After 9 treatments with common metal needles her condition improved distinctly. She rated her pain with 3 on the pain scale and did not require any pain medication. Her blood pressure was still stable and she felt subjectively better than before acupuncture. As she heard about the new laserneedle device, she wanted to try it out. The laserneedles were applied at UB.28, 29, 30, 40 on both sides for 30 minutes. After a few minutes, the typical Qi sensation occurred during the two sittings we performed. She said that she felt a comfortable tingling sensation, which spread throughout the entire body. She rated the back trouble with 1 - 2 on the pain scale. After laserneedle treatment, she felt a direct and distinct
162 improvement in her back pain. However, her blood pressure showed diastolic peaks of 95 to 100 mmHg and she complained about extreme hot flushes. This case was mentioned in particular to attract attention to possible disadvantages of this method. I can only speculate, whether these circulatory disturbances have a direct connection to the laserneedles. My observances have indicated that the use of laserneedles in diseases with too much fullness or conditions, which are strongly influenced by the sympathicus require more caution. In particular, I noticed that hot flushes increased. I also observed this phenomenon in patients during the menopause or in oncologic patients treated with Zoladex. It is conceivable that the additional energy input, which is achieved with the laser method, can bring a system that is “too full” to “boil over”. Further controlled studies are definitely necessary to confirm this statement.
15.3.4
Breast cancer with mastectomy, transmission in scars
A 40-year-old patient had breast cancer surgery on the left two years earlier. Because of the tumor stage, a radical mastectomy and axillary lymphadenectomy had to be performed. Histology showed an invasive ductal breast cancer stage with neoplastic angiolysis and metastases in lymph nodes, estrogen and progesterone receptor positive. Thereafter, she had 6 cycles of chemotherapy as well as a anti-estrogen therapy with Tamoxifen and Zoladex. Her problem was a frozen shoulder on the left which severely restricted the mobility of her arm. The skeletal scintigraphy and CT did not reveal any metastasis. Arm movement was restricted and only sideward movement to < 45° and towards the front to < 90° was possible. Shoulder pain caused by tense muscles was rated with 7 on a 10 point pain scale. She had achieved little improvement with physical therapy exercises. In a sitting position, the patient was treated with laserneedles on both sides at the body acupoints LI.14, SJ.15, GB.21, SI.11.
163
Fig. 15.5: Laserneedle treatment at acupoints LI.14, SJ.15, GB.21 and SI.11.
The acupoints were illuminated continuously with 30 mW laser light for 30 minutes. Eight 8 sittings at 1 - 2 week intervals were performed. After this treatment interval, an obvious improvement in arm movement to < 150° to the front and < 110° sideward was achieved. She could also reach the back of her left shoulder with her left arm, a movement that was impossible before. She described her emotional and physical condition as much better and stable since laserneedle treatment. She also had more energy and was not as tired. Solely the heat sensation within the body and sweating had increased somewhat. Interestingly she describes the transmission of the laser energy directly to the scars. The needles were adhered on the back and rear shoulder region. About 5 minutes after activating the device, she felt a tingling sensation at the mastectomy scar and axillary scar. After two further minutes, she described a strange sensation in all scars on her body, even at the scar on her right knee from an old injury. The scar on the knee was located somewhat lateral from the stomach meridian. As we know, the stomach meridian runs directly over the breast. Interestingly, the scar on the knee was on the right side, the mastectomy scar on the left side of the body. Whether energy from laserneedles flows further and is stopped at scars and how far scars can be influenced with laserneedles should be discussed. According to the interference field theory, scars are very important focuses were energy is disturbed. Further studies to this topic should follow.
164 15.3.5
Dysmenorrhoea, lack of energy
A 45-year-old patient came to the consultation hour and suffered from severe pain in the lower abdomen during menstruation. Endometriosis AFS III was documented in her medical records and she had several operations because of endometriosis in the past. Dysmenorrhea was so severe, that she had to go to the hospital for treatment with strong painkillers. Menstrual blood was always clumpy and sluggish and dark in color. In addition, she had severe back pain. She also complained about changing moods, loss of libido and lack of energy. Nine sittings with laserneedles were performed once a week. Different acupoints on the body and ear were stimulated with laser light. The time of treatment was selected in such a way, that it was briefly before the beginning of menstruation. During the nine treatments, the acupoints were stimulated with laser light. After the treatment with laserneedles, the patient said that she hadn’t felt so well in the last 2 years and that she was also emotionally better balanced. She had much more energy and felt strong. Major changes had taken place with positive effects on her body and emotional condition. She was impressed. The changes in mood had also improved distinctly. Pain in the lower abdomen was almost gone and she only needed a hot-water bottle on the first day of menstruation. The color of menstrual blood was much lighter and without clumps. As she was treated one day before the awaited menstruation she reported that she already menstruated on the same day as she was treated and that she didn’t experience any pain. The blood flow was now much thinner and she didn’t experience clumpy or sluggish blood. As the acupoint Yintang (comp. Chapter 7), a point on the forehead between the eyebrows (Fig. 15.6) was treated, she described a pleasurable sensation from the acupoint over the forehead, over the eyebrows, around the eyes and to the nose.
165
Fig. 15.6: Stimulation of acupoint Yintang.
It was a relaxing feeling. She had her eyes closed during the treatment. Nevertheless, she reported feeling lightness within. After treatment, she was full of energy and felt very well.
15.3.6
Childlessness, temperature curve, cycle regulation
A 34-year-old patient with a strong wish for having children came to my acupuncture consultation hour with the question regarding alternative methods for treating sterility. She already had 2 miscarriages in the 5th and 6th week of pregnancy. She also had a consultation in the department of endocrinology. She didn’t want to take any hormones. She didn’t take contraceptives because she wanted to get pregnant. Her menstrual cycle was somewhat prolonged with 32 days. At the beginning, the menstrual blood was sluggish, clumpy, dark in color and painful. During the first days of menstruation, she always had heavy, dark red bleeding. Every morning before getting up from bed, she measured her body temperature and recorded these values on a curve. The temperature curves over 5 months, showed a zigzag picture. The values were between 36.7 and 37.5 °C. It was not a typical two-phase course with sudden increase in temperature and following higher level favorable for pregnancy. We performed 10 sittings, 4 times once a week and then 6 times every 2 weeks. Combined treatment with laserneedles on the body, and metal needles and laserneedles on the ear were performed. On the body, acupoint combinations Sp.6, Liv.3 and St.36 and Yintang were selected. First, 7 metal needles were
166 applied on the ear at the acupoints ovary, TSH, Gonadotropin. Illumination of the endocrine regions at the intertragic notch was performed 3 times. Here, the laserneedles were fastened to a head-holding device (Fig. 15.7) and the endocrine region of the ear was illuminated.
Fig. 15.7: Head-holding device for laserneedle treatment at the ear.
On the evening of the first treatment, she was very tired. Menstruation began on the very next day. She reported that the blood flow wasn’t quite so sluggish. The color of menstrual blood was still dark. During the course of treatment, the color and consistence of blood changed. It was lighter red, not as clumpy and more flowing. The menstrual cycle regulated itself to about 29 days. Pain in the lower abdomen was more tolerable. Remarkable is the nearly picture-book like temperature curve with the typical increase at the point of ovulation and the following plateau during the second cycle phase. One day she came to my consultation hour and reported her positive pregnancy test. The result was confirmed. If she would have become pregnant without laser treatment is questionable. Noteworthy is the change in the temperature curve from the initial zigzag course to the two phase course, as well as the change in color and consistency of menstrual blood.
15.4 Results and discussion This method seems to be trend setting for the future because of high patient acceptance, comfortable treatment, and good results. The special advantage compared to acupuncture with metal needles, is that insertion into the skin is
167 not necessary. Therefore, no side effects such as bleeding, haematomas, infection, or pain during insertion into the skin occur. The mothers’ fear of vegetative reactions from needle insertion is eliminated. There is no additional stress for mother and child with this method. Thus, she can „enjoy“ this method of treatment more. Furthermore, more mobility during treatment is possible. The patients do not have to remain completely still as by common acupuncture. Since the needles are not inserted into the muscle no pain occurs during slight movement. Especially in the field of obstetrics, it is desirable that the woman is relatively mobile. During childbirth, women usually make fists during labor pains. Since acupoint LI.4 at the ball of the thumb is often used to regulate labor, this can be somewhat painful. With laserneedles, stimulation of this acupoint is easily possible. At several acupoints, patients also perceive the typical Qi sensation as when using classical needle acupuncture. However, the range of sensitivity differed. When using common acupuncture, differences in sensitivity on both sides of the body were described. The Qi sensation was described as a tingling and warming feeling. Several patients reported feelings of comfortable relaxation and tiredness. The transmission of sensations along the meridians was often mentioned. In the case study with carpal tunnel syndrome, the patient reported an initial increase in symptoms after the first treatment with laserneedles, identical to that when using common acupuncture needles. This seems to indicate that the laserneedle method has similar effects as traditional acupuncture. We could observe positive results in treating gynecologic and obstetric indications with laserneedles. Cycle regulation with lighter, improved menstrual bloodflow was observed. Temperature curves also showed better results. In the field of oncology, arm mobility and reduced muscular tension could be achieved after breast cancer surgery. In case of bladder problems, dysuria was improved and an improvement in bladder capacity could be reported. After laserneedle therapy, pain was rated with better scores on the pain scale. Exhaustion and lack of energy could also be improved. In the field of obstetrics, faster phases of labor and more energy for the mother could be noted. Labor could be successfully induced by stimulating acupoint LI.4. During treatment of carpal tunnel syndrome a decrease in pain and tingling in the hands during the night could be registered. Hyper emesis with less nausea and vomiting was also achieved. The observation regarding the transmission of laser energy to the different scars on the body is noteworthy. This could further explain the transmission to the meridians. A flow of energy is perceived. This flow will probably be altered on interfering fields / scars, which very sensitive patients can perceive.
168 Scientific studies have shown that an increase in ATP takes place when using the laserneedle method. I think that this ATP is very useful during childbearing. Childbearing requires much energy from the mother and the main supplier is definitely ATP. In particular, the energy aspect is one major difference to common acupuncture. In the approx. 300 patients we have treated with laser therapy, nearly 80 % had the impression that they gained more energy through the treatment. Caution should be taken when treating patients with too much fullness or heat. Even though the laserneedle method does not lead to an increase in body temperature, one could observe that this method wasn’t appropriate for such patients as described in the case study with hot flushes. One would be cautious in patients with an already increased sympathicus. This also seems logical. You should not give a person with too much fullness additional energy. It should be clearly stated that these are reports from experience in personal treatment of patients. Further controlled studies to evaluate the effect of laserneedles are necessary.
15.5 References >1@ >2@
>3@ >4@ >5@
Litscher G, Schikora D (2002) Cerebral vascular effects of non invasive laserneedles measured by transorbital and transtemporal Doppler Sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Neue Konzepte in der experimentellen Akupunkturforschung – Computerkontrollierte Laserpunktur (CCL) mit der Laserneedle Technik. Der Akupunkturarzt / Aurikulotherapeut 28: 18-28 Martius G, Rath W (1998) Geburtshilfe und Perinatologie. Thieme Verlag, Praxis der Frauenheilkunde Band II, 1998, S. 383-384 Schikora D.: European Patent Nr. PCT/EP 01/08504 Schikora D.: Physikalische und physiologische Eigenschaften der Lasernadeln für Akupunktur, personal communication
169
16. Laserneedles in gynecology - a study with questionnaires K. Staehler van Amerongen 16.1 Introduction In the meantime, different descriptions regarding the use and effects of laserneedle acupuncture can be found in literature [1]. Goal of this study was to evaluate what patients experienced during and after treatment with laserneedles and what they knew about the technique before treatment. Using questionnaires, this current study compares the laserneedleacupuncture method with the common metal needle acupuncture method based on the patients’ perception during and after treatment.
16.2 Test persons Thirty female patients per group were questioned. All of these patients visited the acupuncture consultation hour at the University Gynecological Clinic in Bern. They were treated for gynecological disorders and came to the consultation hours with the following symptoms: Carpal tunnel syndrome, premenstrual pain, urogenital symptoms, pruritus gravis, mastodynia, chronic abdominal pain in endometriosis, induction of labor, hyper emesis gravidarum, dysmenorrhoea, breast cancer with decreased mobility of the arm, sacra-iliac joint pain during pregnancy, smoking withdrawal during pregnancy, primary sterility and preparation for childbirth. The mean age of patients in the metal needle group was 38 years (range from 18 to 73 years) and the mean age in the laserneedle group was 36 years (range from 16 to 60 years). Assignment to the laserneedle or metal needle treatment groups was done at random. Each patient took a random number from 1 - 60. The patients with even numbers were treated with metal needle acupuncture; those with uneven numbers were treated with laserneedle acupuncture.
170
16.3 Method The patients obtained questionnaires part 1 before the first treatment, part 2 after the first treatment and part 3 prior to the second treatment. The patients filled out the questionnaires voluntarily and independently. In part 1, the question “Do you know the method (metal needle acupuncture or laserneedle acupuncture)?” was asked. Two answers were possible: either yes or no. The second question was „Have you already been treated with acupuncture?” Here also the answers yes and no could be selected. The third question was “How would you evaluate your personal state of health at the moment?” The following answers were possible: very good, good, satisfactory, poor and very poor. The fourth question was „How strongly does your illness or symptoms influence you in daily life?“ Here, 5 answers were possible as follows: extremely, strongly, moderately, a little, not at all. The questionnaires were given back for evaluation. Treatment was then performed according to assignment either with metal needle or laserneedle acupuncture. Immediately after the first treatment, the patients filled out part 2 of the questionnaire for evaluation. Again, the patients filled the questionnaire out independently and without influence from others. In the second part of the questionnaire, the patients were questioned regarding their perception during treatment. The following questions were to be answered: “Did you experience pain when the needle was applied?” - “Did you experience pain during treatment?” - “Did you experience a feeling of warmth in the body during treatment?” - “Did you experience an electrical tingling sensation during treatment?” - “Did you feel something at the needle itself during treatment?” - “Did you experience a sensation in the entire body during treatment?” - “Did you experience tiredness during treatment?” - “Did you feel relaxed, comfortable during the treatment?” The following answers were possible for the questions above: extremely, strongly, moderately, a little, none. The third part of the questionnaire was filled out by the patients prior to the second treatment. Questions regarding perception after treatment were asked. The following questions were evaluated: “Did you experience pain after the treatment?” - “Were you tired after treatment?” - “Did you feel relaxed after treatment?” - “Did your symptoms improve after treatment?” “Did you feel well physically after treatment?” - “Did you feel well emotionally after treatment?” - “Did your symptom improve with treatment?” Again, several answers were possible: extremely, strongly, moderately, a little, and none.
171
16.4 Results After evaluating the question: “Do you know the method?” Thirty patients answered “no” regarding the laserneedle method and 29 “yes” regarding the acupuncture method. This shows that treatment with common metal needle acupuncture is well known among the patients; however, they have not yet been informed about laserneedle acupuncture. Already 13 of 30 patients were treated with metal needle acupuncture whereas all 30 patients in the laserneedle group had not yet been treated with this technique. The majority of patients in both groups noted their current health condition as being good to satisfactory (n=27 in the metal needle group and n=26 in the laserneedle group) (Fig. 16.1). The symptoms they had influenced them very strongly to moderately (Fig. 16.2). In the laserneedle group (n=30) 29 patients experienced no pain and 1 a little pain during application, however in the metal needle group (n=30) 3 patients experienced extreme, 3 strong, 9 moderate, 12 a little and only 3 no pain during needle insertion (Fig. 16.3). The great advantage of “painless” laserneedle-acupuncture should be noted here. In addition, none of the 30 patients experienced any pain during laserneedle acupuncture, whereas 2 patients experienced strong, 3 moderate, 4 a little and 21 no pain during metal needle acupuncture (Fig. 16.4). The question whether they felt warmth during treatment was answered by 7 patients with extremely, 17 with strongly, 5 with moderately, 1 with little and 0 with none in the laserneedle group (n=30). In the metal needle group (n=30) only 1 patient answered with extremely, 4 with strongly, 7 with moderately, 8 with a little and 10 with none (Fig. 16.5). In the laserneedle group (n=30), the question regarding tiredness during treatment was answered by 2 patients with extreme, 9 strong, 10 moderate, 6 a little and 3 none at all. In the metal needle group (n=30) 2 patients answered with extremely, 12 strongly, 8 moderately, 2 a little and 6 with none at all (Fig. 16.6). In the laserneedle group no one answered the question regarding tiredness after treatment with extreme, 1 with strong, 2 with moderate, 13 with a little and 14 with none. In the metal needle group, 4 patients were extremely tired, 8 strongly, 4 moderately, 6 a little and 8 not at all (Fig. 16.7). In the laserneedle group 2 patients said they were extremely relaxed during treatment, 13 experienced strong relaxation. Six patients experienced moderate, 6 little and 3 no relaxation. In the metal needle group, 4 noted extreme, 17 strong, 5 moderate 4 little and 0 no relaxation (Fig. 16.8). The question regarding relaxation after treatment showed similar results. In the laserneedle group 8 answered with extreme, 14 with strong, 7 with moderate,
172 1 with little and no one with none and in the metal needle group 4 answered with extreme, 18 with strong, 6 with moderate, 2 with little and no one with none (Fig. 16.9). In both groups, the patients experienced a strong feeling of relaxation during and after treatment. In both groups, most of the patients experienced a great improvement in their symptoms and felt well after treatment (Fig. 16.10 and 16.11).
number of patients (n=30) per group
How would you evaluate your personal state of health at the moment?
20
16
15
15 11
11
10 5
1
2
1
3 0
0 very good
good
satisfactory
metal needle acupuncture
poor
0
very poor
laserneedle acupuncture
Fig. 16.1: How would you evaluate your personal state of health at the moment?
number of patients (n=30) per group
How strongly does your illness or symptoms influence you in daily life? 16 14 12 10 8 6 4 2 0
15 12 10 7
6
8
1 extremely
strongly
moderately
metal needle acupuncture
1
a little
0
0
not at all
laserneedle acupuncture
Fig. 16.2: How strongly does your illness or symptoms influence you in daily life?
173
number of patients (n=30) per group
Did you experience pain when the needle was applied? 35 30 25 20 15 10 5 0
29
12
9 3
3
0
extreme
0
strong
1
0 moderate
metal needle acupuncture
a little
3 none
laserneedle acupuncture
Fig. 16.3: Did you experience pain when the needle was applied?
number of patients (n=30) per group
Did you experience pain during treatment? 35
30
30 25
21
20 15 10 5 0
0
2
0
extreme
0
strong
3
4 0
0
moderate
metal needle acupuncture
a little
none
laserneedle acupuncture
Fig. 16.4: Did you experience pain during treatment?
174
number of patients (n=30) per group
Warmth during treatment 18 16 14 12 10 8 6 4 2 0
17
10 8
7
7
5
4 1
1
extreme
strong
moderate
metal needle acupuncture
little
0 none
laserneedle acupuncture
Fig. 16.5: Warmth during treatment
number of patients (n=30) per group
Tiredness during treatment 14
12
12
9
10 8
10 8 6
6 4 2
2
2
6 3
2
0 extreme
strong
moderate
metal needle acupuncture
Fig. 16.6: Tiredness during treatment
little
none
laserneedle acupuncture
175
number of patients (n=30) per group
Tiredness after treatment 16 14 12 10 8 6 4 2 0
14
13 8
8 6
4
4
extrem e
2
1
0
strong
m oderate
metal needle acupuncture
little
none
laserneedle acupuncture
Fig. 16.7: Tiredness after treatment
Relaxation during treatment 17
number of patients (n=30) per group
18 16
13
14 12 10 8 6 4 2
5
4
6
6 4
3
2 0
0 extreme
strong
moderate
metal needle acupuncture
Fig. 16.8: Relaxation during treatment
little
none
laserneedle acupuncture
176 Relaxation after treatment
number of patients (n=30) per group
20
18
18 16
14
14 12 10
8
8 6 4
6
7
4 2
2
1
0 extrem e
strong
m oderate
metal needle acupuncture
little
0
0
none
laserneedle acupuncture
Fig. 16.9: Relaxation after treatment
number of patients (n=30) per group
Improvement of symptoms after treatment 20
18 15
15
9
10 5
7 4
3
2
2 0
0 extremely
strongly
moderately
metal needle acupuncture
a little
not at all
laserneedle acupuncture
Fig. 16.10: Improvement of symptoms after treatment
0
177
number of patients (n=30) per group
How do you feel after treatment? 25 20
20
18
15 10 5
5
6
4
5 1
1
0 very good
good
satisfactory
metal needle acupuncture
poor
0
0
very poor
laserneedle acupuncture
Fig. 16.11: How do you feel after treatment?
16.5 Discussion Our study shows that metal needle acupuncture is well known among patients but that laserneedle acupuncture requires further explanation regarding the method and possibilities of use. With the exception of one patient, no one experienced any pain during application of the needle or during treatment. The painless laserneedle method has a clear advantage compared to common metal needle acupuncture. Obvious differences in both groups regarding warming sensations can be reported. Laserneedle therapy is definitely a method in which warmth is experienced by the patient during treatment. According to temperature measurements, the body and tissue temperature does not increase during laserneedle acupuncture; however our studies show that the majority of patients perceive a warming sensation in the body. Further temperature measurements should follow. The tendency that metal needle acupuncture leads to stronger tiredness during and after treatment is obvious. On the other hand, patients treated with laserneedles were more “energetic” after treatment. Maybe laserneedles have a positive influence on less energetic persons? On the other hand, persons in our patient collective experienced a strong feeling of relaxation
178 during and after treatment. Both methods seem to be good in achieving relaxation. Most patients in both groups experienced a great improvement in their symptoms and felt well after treatment. When we view this questioning in its entirety, laserneedle acupuncture seems to be a method which according to the patients’ perception has a positive influence on symptoms and is a painless, energetic and relaxing method which leads to a warming sensation during treatment.
16.6 References [1]
Litscher G, Schikora D (Hrsg) (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Bremen
179
17. Laserneedle therapy in dentistry K. Borer 17.1 Introduction In addition to toothache and neuralgia, patients in dental practices often also suffer from anxiety and needle phobia. Experienced dentists can achieve fast relief with acupuncture therapy [1-4]. Laserneedle-technology allows new, painless acupuncture stimulation. This study is a report about the use of laserneedle acupuncture in daily routine dentistry.
17.2 Methods and materials Prerequisite for laser acupuncture treatment was the diagnostic exclusion of all obvious dental causes. For example, bite problems were treated first in the occlusion; root treatment was performed in case of gangrenous dental pulp. The positioning of the diodes was done differently according to indication: 1 – 2 diodes for direct treatment of the tooth and respective wound region, dermatologic hammer for extensive treatment (mandibular joint), application of diodes at acupuncture points according to body and ear acupuncture. Main emphasis during testing of the device was the local treatment of the problem areas.
17.3 Results 17.3.1
Oral surgery
Post operative pain with lockjaw after surgical removal of wisdom tooth: Daily treatment was done locally using the dermatologic hammer (Fig. 17.1) with eight diodes for three sittings. After the first treatment, only minor pain was present and after the third sitting, the patient could open his mouth normally.
180
Fig. 17.1: Dermatologic hammer for the treatment of jaw problems.
Massive symptoms after paradontal surgery: Local treatment with three diodes, every three days, resulted in immediate painlessness after the first sitting, thereafter, to very rapid healing (gingiva without necrotic coating, rapid resolution of the haematoma).
17.3.2
Endodontology
Toothache with new porcelain inlay: The affected tooth was treated daily, with two diodes, from the dental neck to the apex. The patient was free of pain after two sittings with positive vitality testing. Routine treatment during direct capping of open dental nerves: The corresponding area of the dental nerves were treated locally with one diode, for one minute, thereafter, a dental wound bandage was applied. In this manner, the possible death of dental nerves may be reduced.
181 17.3.3
Crown - bridges
Routine treatment of prepared pillar teeth: The prepared teeth were treated with a diode for 2 minutes. As a result, later death of the treated teeth may be avoided.
17.3.4
Pain therapy
Bite problems, sensitivity of teeth to temperature: The dental neck to the apex was treated locally with 1 – 2 diodes for about 10 minutes, every 2 – 3 days (Fig. 17.2). The reaction time until pain ceased was variable; usually 2 to 3 sittings were required.
Fig. 17.2: Treatment of the dental neck.
17.3.5
Myoarthropathy
Due to increasing stress in the population, an increase in central pressing, grinding and severely indurated jaw and neck muscles with jaw problems occur. As a result, contraction of the jaw, neck and back muscles with corresponding pain symptoms occur. Treatment was performed using the dermatologic hammer (Fig. 17.3) above the affected jaw muscles, above the cervical vertebra C0/1 and C7. Thereafter, the patients felt relaxation and a light warming sensation.
182
Fig. 17.3: Dermatologic hammer for the treatment of myoarthropathy and jaw problems.
17.3.6
Neuralgia
Based on the affected areas of the head, diodes were applied at the classic acupuncture points of the head and rest of the body. For example, Du 20 as local point, and LI.4 and Liv.3 as distant points.
17.3.7
Sedation in case of dental phobias
Acupuncture was performed 30 minutes before dental treatment. Excellent relaxation to the patient was achieved with points Ki.6, LI.1-1, Ren 17 and Ren 24.
17.3.8
Nausea during molding
Acupuncture was performed 30 minutes before taking moulds, above the acupuncture points Ren 24 (Fig. 17.4), Ki.6, LI.1-1 and Pe.6. As a result, even extremely difficult models could be made without problems.
183
Fig. 17.4: Acupuncture point Ren 24 for treatment of nausea.
17.4 Discussion Laserneedle-technology can be very well integrated into the routine dental practice. The instrument is simple to handle and can be easily delegated. A sterilizable dental adapter which survives repeated sterilization would be desirable. Laser acupuncture represents an excellent initial therapy due to its positive effects on microcirculation and relaxation. Further studies should confirm the reproducibility of these positive effects under consideration of possible relapses. Overall, the application of this technology leads to a higher efficiency in treatment. On the one hand, local therapy with good initial effects can be achieved; on the other hand, causal therapy can be performed using body acupuncture. This improves and widens the possibilities in dental medicine.
17.5 References [1] [2]
Rosted P (2000) Introduction to acupuncture in dentistry. Br Dent J 189: 136-140 Lu DP, LU GP (2003) Anatomical relevance of some acupuncture points in the head and neck region that dictate medical or dental application depending on depth of needle insertion. Acupunct Electrother Res 28: 145-156
184 [3] [4]
Thayer T (2001) Acupuncture in dentistry. SAAD Dig 18: 3-8 Lu DP, Lu GP, Reed JF 3rd (2000) Acupuncture/acupressure to treat gagging dental patients: a clinical study of anti-gagging effects. Gen Dent 48: 446-452
185
18. Laserneedle stimulation as a potential additive method for post operative pain treatment G. Litscher, G. Schwarz, A. Schöpfer, L. Wang, M. Saraya, D. Schikora 18.1 Introduction The influence of post operative pain on the entire course of treatment was underestimated for a very long time. The inadequate suppression of acute postoperative pain has a negative influence on the subjective feeling, compromises vegetative regulatory and control cycles and also plays an important role in the risk of chronification. Innovative technical developments such as laserneedle acupuncture (LNA) [1-4], provide the foundation for new, potentially additive techniques in pain treatment. At the Medical University Graz, initial indications for neuro-modulated effects of LNA could be determined on healthy volunteers using non-invasive neuromonitoring techniques and modern imaging modalities [1-4]. Goal of these preliminary examinations was to document a possible influence of the new laserneedle stimulation method on the subjective, individual need of analgesics during post-operatively controlled analgesia, within a doubleblind, randomized study.
18.2 Method 18.2.1
Patients and procedure
A total of 25 patients (13 f, 12 m) with a mean age (r SD) of 45.2 r 11.9 years, were treated with activated laserneedle stimulation. The control group comprised 19 patients (mean age (r SD): 47.3 r 11.0 years; 8 f, 11 m) and was treated with deactivated laserneedles. All patients gave their written consent and the study was approved by the local Ethical Committee at the Medical University Graz. The patients who had flavotomies (mean duration of surgery: 129.3 r 19.7 min; 104 - 161 min), were treated with laserneedle acupuncture immediately before and after surgery and during consciousness for 10 minutes. The following acupoints according to Chinese ear and body acupuncture (Fig. 18.1.) were selected on both sides: ear 55 (Shenmen), ear 40 (Lumbar spine),
186 LI.4 (Hegu) and UB.60 (Kunlun). A blind pain scale (VAS 0 - 10; 0 = free of pain - 10 = maximum pain) was used for evaluation.
Fig. 18.1: Laserneedle acupuncture as a possible additive method in postoperative pain treatment. The following acupoints were stimulated: ear point 55 (Shenmen), ear point 40 (Lumbar spine), LI.4 (Hegu), UB.60 (Kunlun) (from above to below). After intervention, the effects of pain treatment within a pre-defined observation time of 90 minutes were evaluated. At a VAS > 3, the pain therapeutic regime included intravenous bolus administration of 3 mg Piritramid (Dipidolor®) at a body weight (BW) of > 50 kg; 1.5 mg at a BW < 50. The maximum dosage of analgesics was limited according to BWs to a total of 15 mg, or 7.5 mg/h respectively. After the final administration of the opiate, the patients were observed for at least 30 more minutes. Criteria for exclusion from this study were an age > 70 years, liver and kidney diseases as well as neurological disorders.
18.2.2
Laserneedle acupuncture
After cleaning the skin with alcohol, eight laserneedles were applied to the acupoints with a special adhesive. A semi-conductor laser with an emitting wave length of 680 nm was used as the light source. Output was 30 - 40 mW per laserneedle. Duration of stimulation was 20 minutes, resulting in an energy density ~ 4.6 kJ/cm² at each single acupoint, and an average total
187 value 36.8 kJ/cm² for all. Further details regarding the method can be found in previous studies [1-4].
18.2.3
Statistical analysis
The determined data was presented graphically with box plots (SigmaStat, Jandel Scientific Corp., Erkrath, Germany). The t-test was used for statistical analysis. The level of significance was determined with p < 0.05.
18.3 Results The results of the investigations are shown in Figure 18.2. The pilot study indicated insignificant changes in the rating of subjective pain based on the VAS before and after laserneedle acupuncture. It is noteworthy, that the use of analgesics during postoperative observation was higher in the group without activated laser stimulation (t-test; p = 0.09, n.s.). Clinical side effects were not observed in any of the patients. use of analgesics (O)
VAS 12
10
10
p = 0.09 (n.s.)
p=0.619
SE
Boli
8.0 + 1.1
8 n=19
6
4
SE 6.6 + 0.7
2 n=25
0 before after before after laserneedle acupuncture
n=25
0
1 PE
2before OP 3
4 after OP 5
6 O
1 7POPD 8
5 with without laserneedle acupuncture
Fig. 18.2: Box plots of changes in the values on the pain scale (VAS) at the preliminary examination (PE), before and after surgery (OP), during postoperative observation (O) and on the first post operative day (1 POPD).
188
18.4 Discussion Adequate postoperative pain treatment fitted to the patients risks and needs by the anesthesiologist, is an absolute necessity. Corresponding immediate post and perioperative pain treatment not only helps the patient by relieving pain, but also supports the stabilization of neuro-vegetative functions and can also avoid the chronification of the pain process [5]. Dependent upon the extent and localization of surgery, postoperative pain is expected in the majority of patients. However, the difference in individual pain perception and the extent of side effects differs greatly from patient to patient. Advances in pharmacological treatment have led to treatment strategies which reduce postoperative pain to a minimum and in the best case, avoid pain altogether. In addition to oral (tablets, drops) and intramuscular administration of analgesic substances, other methods of pain treatment should be mentioned, whereby drugs with analgesic potency (opiates, local anesthetics) are applied via inserted special catheters (lumbar or thoracic epidural catheters, arm plexus catheter etc.) or with long term venous canules. These substances act either regionally or on the central nervous system. Patient-controlled analgesia can be realized with microprocessor controlled electronic perfusion and infusion devices. Transcutaneous electrical nerve stimulation is another possibility for suppressing post operative pain [6]. Moreover, scientific literature describes the use of acupuncture for perioperative pain treatment in different types of surgical interventions [7,8]. For the first time, this study applies the new laserneedle acupuncture method as a possible additive method to pharmacologic pain treatment. The use of laserneedles seems to achieve a subjective, additive suppression of pain and leads to changes in the required pain medication within a 90 minute postoperative observation period. Criterion for the required analgesics was based on the patients rating of pain intensity on a visual pain analogue scale. Non-invasive laserneedle stimulation can induce specific, reproducible changes in the brain. This leads to changes in different parameters such as cerebral blood flow velocity, and for the first time can be objectified with the newest neuromonitoring methods [1-4]. This new method of painless acupuncture has not yet been used experimentally or clinically in the field of postoperative pain treatment. Further investigations with a larger patient collective are necessary to evaluate and optimize this method before laserneedle acupuncture can be considered as an additive in routine, postoperative pain treatment.
189
18.5 Acknowledgements The authors thank Ingrid Gaischek MSc for her valuable support in data analysis and preparing the manuscript (Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University Graz).
18.6 References [1] [2] [3] [4] [5] [6]
[7]
[8]
Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Litscher G, Schikora D (Eds) (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Bremen Jage J (1997) Schmerz nach Operationen. Wissenschaftliche Verlagsgesellschaft, Stuttgart Bjordal JM, Johnson MI, Ljunggreen AE (2003) Transcutaneous electrical nerve stimulation (TENS) can reduce postoperative analgesic consumption. A meta-analysis with assessment of optimal treatment parameters for postoperative pain. Eur J Pain 7(2): 181-188 Usichenko TI, Lysenyuk VP, Groth MH, Pavlovic D (2003) Detection of ear acupuncture points by measuring the electrical skin resistance in patients before, during and after orthopedic surgery performed under general anesthesia. Acupunct Electrother Res 28(3-4): 167-173 Stener-Victorin E, Kowalski J, Lundeberg T (2002) A new highly reliable instrument for the assessment of pre- and postoperative gynecological pain. Anesth Analg 95(1): 151-157
190
19. Effects of laserneedle stimulation in the external auditory meatus on very early auditory evoked potentials G. Litscher 19.1 Introduction In the past years, several new, technical advancements in laser acupuncture have triggered an innovative jump in this field of study. In addition, scientific studies have proven that laserneedle acupuncture can achieve needle-equivalent, reproducible changes in cerebral parameters, that can be registered with modern neuromonitoring techniques [1-5]. Laser light stimulation in the external auditory canal and its effects on early (BAEP; latency: 1 - 10 ms) and very early auditory evoked potentials (SAEP; latencies: < 1 ms) have not yet been scientifically investigated. In this study, laserneedle-induced changes in biological factors of SAEP, could be determined and registered for the first time in 23 healthy volunteers using this measurement technique.
19.2 Methods 19.2.1
Laserneedle stimulation in the external auditory meatus
For application of laser stimulation in the right external auditory meatus, an adapter was developed which is similar to a spectacle construction and is fixed at the ear (see Fig. 19.1 and Fig. 19.2). A total of 4 optical fibers were conducted into the external auditory meatus using a rotating, round holder allowing different distances. These laserneedles deliver continuous or frequency-modulated laser light with a wavelength of 685 nm and an output of 30 - 40 mW per laserneedle. Duration of stimulation was 10 minutes resulting in a power density of 2.3 kJ/cm² at each laserneedle and an average total of 9.2 kJ/cm² [1-5]. In addition to laser light stimulation, a sound tube for acoustic stimulation of evoked potentials was integrated in the adapter. The entire adapter does not include any metal parts; only plastic components were used.
191
Fig. 19.1: Stimulation adapter for optical laser stimulation in the area of the external acoustic meatus. A sound tube for acoustic stimulation between the 4 laserneedles is implemented in the construction.
19.2.2
Auditory evoked potentials of early latency
Acoustic stimulation was performed with clicks of 200 µs duration and alternating polarity with a frequency of 11.1 Hz. Stimulus intensity was 105 dB nHL (normal hearing level). The contra-lateral ear was not masked. Miniature earphones (Nicolet 464-656, Nicolet Instrument Corp., Madison, WI, USA) which were connected to a sound tube were used for stimulation. Gold cup electrodes (Grass E6GH) between the vertex (Cz) and right ipsilateral mastoid (Cb2) were used on the volunteers. The ground electrode was located at the position Fz. Skin-electrode impedance was < 3 kOhm. The cup electrodes were directly connected to active electrodes for amplifying the signals in the head region enabling the registration of bioelectric cerebral activities with a minimum of artifacts [6] (compare Fig. 19.2). In each investigation, at least 2000 single clicks were averaged and each measurement was reproduced one time. A PC-based neuromonitoring system (Viking IV, Nicolet Instrument Corp., Madison, WI, USA) was used for data analysis.
192
Fig. 19.2: Experimental set-up of laser stimulation at the laboratory of Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine at the Medical University of Graz.
19.2.3
Volunteers and procedure
SAEP and BAEP were investigated in a total of 23 healthy volunteers, mean age (r SD) from 26.5 r 3.6 years (range 20 to 36 years old; 15 f, 8 m). The volunteers were informed about the procedure and gave their written consent. The study was approved by the ethical committee at the Medical University of Graz. None of the volunteers took central nervous system active medication during the study period and the neurological, mental and otological status was normal in all test persons. In addition to the amplitudes of wave I and those of the IV/V-complex in brainstem auditory evoked potentials, the amplitudes of very early AEPresponses including so-called stimulation artifacts were evaluated. Further, the tympanic temperature using a ThermoScan pro LT (Thermoscan Inc., San Diego, CA, USA) was investigated before and after the three examination phases (a) resting phase (steady state), (b) continuous laserneedle stimulation and (c) frequency-modulated (2 Hz) laserneedle stimulation.
193 19.2.4
Statistical analysis
Analysis of measurement data and graphic presentation was performed with the computer programs SigmaStat and SigmaPlot (Jandel Scientific Corp., Erkrath, Germany). The paired t-test was used for statistical evaluation and graphic illustration was done with box-plot illustrations. Criterion for significance was determined by p < 0.05.
19.3 Results The first five components of BAEP could be isolated and reproduced in all test persons and corresponded with conventional standards [7]. One example is shown in Fig. 19.3.
resting condition without stimulation
a
continuous laserstimulation
b
frequency-modulated laserstimulation (2 Hz)
c
Fig. 19.3: Early auditory evoked potentials without (a), during continuous (b) and during frequency-modulated (c) laser stimulation in a 24-year-old volunteer. Note the occurrence of very early stimulus responses and the increase in stimulation artefacts (see arrows) despite alternating stimulation modes during laser stimulation. The tables show the absolute latencies of components I, III and V in milliseconds (ms) as well as the interpeak latencies I-III, III-V and I-V in ms and the amplitude relationships (I-I’)/(V-V’).
194
The mean amplitudes of SAEP, of wave I (Ia) and of the IV/V-complex (IV/V)a during resting conditions (without stimulation; steady state), after continuous laserneedle stimulation and after frequency-modulated (2 Hz) laserneedle stimulation in all volunteers can be found in Figure 19.4.
SAEP
µV 0,4
Ia
(IV/V)a
p = 0.014 (s.)
n=23
p = 0.019 (s.) 0,3
n.s. n.s. 0,2
0,1
0,0
R
cw
S1
LN
LN
R
cw
S1
LN
LN
R
cw
S1
LN
LN
Fig. 19.4: Box-plot illustrations of very early auditory evoked potentials (SAEP), amplitudes of the wave I (Ia) and amplitude of the IV/V-wave complex (IV/V)a in µV under condition R (= resting, steady state, control measurement), cw LN (continuous laserneedle stimulation) and S1 LN (2 Hz frequency-modulated laserneedle stimulation). Note the significant increase in SAEP during laser stimulation. The horizontal line in the box shows were the median is situated. The ends of the box define the 25th and 75th percentile; error bars show the 10th and 90th percentile.
Whereas the amplitudes of wave I and those of the IV/V-complex did not reveal significant changes during laser stimulation, the mean amplitude of the stimulation artifact under continuous (p = 0.019), as well as during 2 Hzmodulated stimulation (p = 0.014) show a significant increase. The tympanic temperatures measured immediately after each phase of investigation are shown in Figure 19.5.
195 °C 38,0
normal range for ear temperature (11 - 65 years)
37,5
37,0
36,5
36,0 p < 0.001 (s.)
35,5
p < 0.001 (s.)
35,0
R
cw LN
S1 LN
Fig. 19.5: Laser stimulation related changes in temperature at the external auditory meatus. The normal range for ear temperature given by the manufacturer is shown on the right (R = resting, without stimulation; cw LN = continuous laser stimulation; S1 LN = frequency-modulated laser stimulation). For further details, see Fig. 19.4.
19.4 Discussion Laser has gained a permanent position in the field of acupuncture. Corresponding to the desired solutions, the quality of different laser systems must be applied. Future developments in laser technology will be based on the new application of laser in the field of medicine in general, and its specific use in acupuncture. Factors such as the better understanding of working mechanisms, availability of technically perfected laser constructions and the development of flexible optical transmitting systems and optical fibers all lead to technically simpler systems and will play an increasing role in the future [8]. Whereas laser technology is increasingly used in the fields of surgery, ophthalmology or gynecology, comparatively few scientific studies dealing with this topic can be found in the field of ear, nose and throat medicine. In this study, we tried to objectify peripheral and possible cerebral effects of this stimulus modality using computer-aided, bioelectric stimulus responses after performing laserneedle stimulation in the external auditory meatus.
196 Therefore auditory evoked potentials of very early latency were used. Socalled “clicks” (= rectangular impulses) with a duration of 200 µs were used as stimulus impulses. Effects on latency, amplitudes and waveforms of early auditory evoked potentials dependent on the polarity of electrical stimulation, were investigated and described in detail in the literature [9-11]. If these stimuli are presented alternately, i.e. alternating once positive and once negative, stimulus-related artifacts which occur during stimulus presentation of one polarity are averaged in the signal response. In the same manner, electro-cochleographic potentials originating in the presynaptic region in the hair cells and their support structures, cochlear microphonics and the summating potential are normally eliminated by alternating the polarity of the stimulus. Small blood vessels transport oxygen and nutrition and supply the sensory cells responsible for hearing. In case of hypo-perfusion, cells are damaged and their function is disturbed. Goal of standard medical treatment is to avoid potential sudden deafness and improve the flowing characteristics of blood. Other methods of blood cleansing or the so-called hyperbaric oxygen therapy are further possibilities. Latter leads to an increase in oxygen in blood and tissues which should result in an improved clinical picture. The treatment with laserneedles could provide a further option e.g. as tinnitus therapy. It is very interesting that changes in SAEP triggered by laser stimulation could be registered in this study. In this latency range, microphonic potentials, summating potentials and subsequently, summating active potentials of the auditory nerve could be recorded (Fig. 19.6).
197
10 µV
a
10 µV
b
CM c
0,1 µV
CM
N1 d
0,1 µV
AP
1 ms
Fig. 19.6: Very early auditory evoked potentials (SAEP) in a 20-year-old volunteer after performing positive (a) and negative (b) clicks; (c) shows microphonic potentials (CM) and (d) the summating action potential (AP = N1).
The main component, the post synaptic wave N1 (compare Fig. 19.6), represents a summating action potential of the auditory nerve and doesn’t actually originate in the cochlea [12]. However, microphonic potentials (CM) are considered as a cochlear event but do not play a major role in clinical diagnostics [12]. Our results obtained from earlier studies showed an interesting phenomenon, that definitely biologically-related changes in stimulus artifacts, despite unchanged stimulus and monitoring parameters in coma depasse occur [13,14]. During our present study, measurements with laser stimulation showed a change in SAEP in the sense of a positive increase in these components, whereas results from previous studies on comatose patients, or in the extreme case of coma depasse, indicated a contrary negative increase in activity [13,14]. Similar results, namely different early AEP-stimulation responses (wave I to V) to positive and negative auditory stimulation in healthy persons as well as
198 in pathological cases, have already been discussed in the literature [13,14]. A solution for this problem, probably lies in the mechanics of the inner ear, but is not yet in sight. More specific information regarding the actual pressure conditions within the ear would be necessary. This is difficult to determine because the insertion of a microprobe additionally alters the course of sound pressure within the ear [13,14]. A second hypothesis is based on the assumption that extra cerebral changes in functional impedance occur. Already back in 1973 [15], scientists reported irreversible functional disturbances in the brain after ischemia and after anoxia resulting in a reduction of cortical impedance compared to the initial value, whereas an increase in impedance occurred in the reticular formation. A further hypothesis can be supposed for the arising changes in SAEP under laser stimulation, which indicates that these stimulus-related depolarization processes in extra cerebral areas of the auditory system underlie altered conditions of impedance. In order to get more exact results in the future, we could use a transtympanic or extra tympanic technique to register the changes resulting from laser stimulation instead of registering induced bioelectrical activity from the mastoid, as performed in this study. The trans-tympanic technique requires the application of a thin metal needle through the ear and eardrum to the nearest area of the inner ear; the less invasive extra tympanic technique allows the registration of changes in potential by applying a needle electrode behind the ear and advancing it near the eardrum. Further investigations such as exact analysis of accompanying temperature effects are necessary before final statements regarding this topic can be made.
19.5 Acknowledgements The author thanks Ms. Ingrid Gaischek MSc and Ms. Lu Wang MD (both Biomedical Engineering and Research in Anaesthesia and Intensive Care Medicine, Medical University of Graz) for their valuable support in data registration and data analysis. The author thanks Dr. Detlef Schikora (University of Paderborn) for the development of the ear adapter prototype.
199
19.6 References [1] [2] [3] [4]
[5] [6] [7] [8] [9] [10] [11] [12] [13] [14]
[15]
Litscher G (2003) Cerebral and peripheral effects of laserneedle®stimulation. Neurol Res 25: 722-728 Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295 Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16: 335-342 Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laserneedles modulates brain function: First evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI). Lasers Med Sci 19: 6-11 Litscher G, Schikora D (Eds.) (2004) Lasernadel-Akupunktur. Wissenschaft und Praxis. Pabst Science Publishers, Lengerich Berlin Bremen Litscher G (1998) A mulitifunctional helmet for noninvasive neuromonitoring. J Neurosurg Anesthesiol 10(2): 116-119 Litscher G (1995) Continuous brainstem auditory evoked potential monitoring during nocturnal sleep. Int J Neurosci 82(1-2): 135-142 Albrecht H, Rohde E, Zgoda F, Müller G (2002) Lasersysteme. In: Kramme R. (Ed.) (2002) Medizintechnik. Springer, Berlin Heidelberg New York, pp. 296-318 Maurer K, Schäfer E, Leitner H (1980) The effect of varying stimulus polarity (rarefaction vs. condensation) on early auditory evoked potentials (EAEPs). Electroenceph Clin Neurophysiol 50: 332-334 Stockard JJ, Stockard JE, Sharbrough FW (1978) Non-pathologic factors influencing brainstem auditory evoked potentials. Am J EEG Technol 18: 177-209 Stockard JE, Stockard JJ, Westmoreland BF, Corfits JL (1979) Brainstem auditory-evoked responses. Normal variation as a function of stimulus and subject characteristics. Arch Neurol 39: 823-831 Maurer K, Lowitzsch K, Stöhr M (1990) Evozierte Potentiale. AEP VEP - SEP. Atlas mit Einführungen. Ferdinand Enke Verlag, Stuttgart Litscher G, Schwarz G, Kleinert R (1995) Brain-stem auditory evoked potential monitoring. Variations of stimulus artifact in brain death. Electroenceph Clin Neurophysiol 96: 413-419 Litscher G, Schwarz G, Jobstmann R, Kehl G, Kleinert R (1996) Brainstem auditory evoked potential monitoring. The increase of the stimulus artifact in the development of brain death: a biological phenomenon? Int J Neurosci 91(1-2): 95-103 Lechner H, Ott E (1973) Impedanzuntersuchungen bei reversiblen und irreversiblen Funktionsverlust des Gehirns. In: Krösl W, Scherzer E (Eds.) (1973) Die Bestimmung des Todeszeitpunktes. Maudrich, Wien, pp. 163-170
200
20. List of references Chapter 2: Litscher G, Schikora D (2002) Cerebral vascular effects of noninvasive laserneedles measured by transorbital and transtemporal Doppler sonography. Lasers Med Sci 17: 289-295. Chapter 3: Litscher G, Schikora D (2002) Near-infrared spectroscopy for objectifying cerebral effects of needle and laserneedle acupuncture. Spectroscopy 16/3-4: 335-342. Chapter 5: Litscher G, Nemetz W, Smolle J, Schwarz G, Schikora D, Uranüs S (2004) Histologische Untersuchungen zu mikromorphologischen Einflüssen von Lasernadelstrahlung. Ergebnisse einer tierexperimentellen Untersuchung. Biomed Technik 49: 2-5. Chapter 6: Litscher G (2003) Laserneedle®-Akupunktur auf dem Prüfstand der Wissenschaft. Schweizerische Z f Ganzheitsmedizin 15: 253-259. Chapter 7: Litscher G (2004) Effects of acupressure, manual acupuncture and Laserneedle® acupuncture on EEG bispectral index (BIS) and spectral edge frequency (SEF) in healthy volunteers. Europ J Anaesthesiol 21: 13-19. Chapter 8: Litscher G, Rachbauer D, Ropele S, Wang L, Schikora D, Fazekas F, Ebner F (2004) Acupuncture using laserneedles modulates brain function: First evidence from functional transcranial Doppler sonography (fTCD) and functional magnetic resonance imaging (fMRI). Lasers Med Sci 19: 6-11. Chapter 9: Litscher G, Wang L, Huber E, Schikora D, Schwarz G (2004) Quantitative Bestimmung geschlechtsspezifischer thermischer Empfindungsund Schmerzschwellen vor und nach Lasernadelstimulation. Biomed Technik 49(5): 106-110. Chapter 10: Litscher G, Wang L, Schikora D, Rachbauer D, Schwarz G, Schöpfer A, Ropele S, Huber E (2004) Biological effects of painless laserneedle acupuncture. Medical Acupuncture 16(1): 24-29.
201 Chapter 11: Litscher G, Wang L, Schwarz G, Schikora D (2005) Intrakranieller Druckanstieg nach zerebralen Blutflussgeschwindigkeitsänderungen durch Akupressur, Nadelakupunktur und Lasernadelakupunktur? Forschende Komplementärmedizin und Klassische Naturheilkunde, subm. Chapter 18: Litscher G, Schwarz G, Schöpfer A, Wang L, Saraya M, Schikora D (2005) Laser-“Nadel”-Stimulation als potenzielle additive Methode zur postoperativen Schmerztherapie. Schmerz & Akupunktur 4: 2-5.
202
21. Websites http://www.laserneedle.ch
Laserneedle acupuncture
http://www.laserneedle.de http://www.laserneedle.at
http://litscher.info
High-Tech Acupuncture®
http://litscher.at
Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine, Medical University of Graz
203
Addendum
204
Biomedical Engineering and Research in Anesthesia and Intensive Care Medicine Medical University of Graz
Laserneedle - Stimulation
205
Laserneedle - Acupuncture ComputerComputer-based Quantification
LaserneedleLaserneedle-Acupuncture Peripheral Effects Thermography (surface temperature)
Laser Doppler Flowmetry (microcirculation)
Laser Doppler Imaging + Standard parameters
NeedleNeedle-Acupuncture Central Effects Multidirectional Transcranial UltrasoundDoppler Sonography (blood flow velocity)
Cerebral Near-infrared Spectroscopy (changes of cerebral oxygen metabolism) f MRI Bioelectrical Methods (EEG, BIS, EP)
Laserneedle – Animal Experiments
206
Laserneedle - Thermography
Laserneedle - Thermography
10:40
10:42
a
b
10:44
10:46
c
d
207
Laser Doppler Perfusion Imaging
Laser Doppler Perfusion Imaging
before
immediately after
after
208
Laserneedle - Stimulation ComputerComputer-based Quantification
Cerebral Effects
209
Laserneedle – Acupuncture Research
Ophthalmic Artery (OA)
210
Laserneedle Acupuncture - fMRI
211
Laserneedle – Stimulation Neuromonitoring
Medical University of Graz
212
Laserneedle - Acupuncture - Yintang
213
Laserneedle - Acupuncture as a potential additive method for post operative pain treatment
University Clinic for Anesthesiology and Intensive Care Medicine Graz
214
LASERneedle® - History: First Generation (1998)
Second Generation (2000)
The Laserneedle Laserneedles were developed at the University of Paderborn (1997-1999) [ Dr. D. Schikora, Dr. M. Bartels, R. Winterberg ]
Laserneedles are: fiberoptic acupuncture needles with non-invasive contact application
Goals of the development were: • needle equivalent stimulation effects • needle equivalent functioning (simultaneous stimulation of various acupuncture point combinations)
215
LASERneedle®-medical
• the most effective laser acupuncture system of our time • with 8 painless, bichromatic laserneedles, completely sufficiently for each experienced acupuncturist and each indication
LASERneedle®-frequency
• •
Diagnostics according to BAHR and NOGIER Special analgesic frequencies to increase endorphins and non-endorphinerg transmitters
216
LASERneedle® - applicators
comfortable, rapid fixation of laserneedles on acupoints using self-adhesive non-reusable applicators
Dermatology: Laser surface illumination using LASERneedle®
Acute and chronic eczema Neurodermatitis Chronic ulcer and phlebitis Psoriasis Lichen ruber planus Verruca Alopecia areata Herpes
I = 20°
I = 0° 4
x / [mm]
2 0 -2
= = = = =
d0 0.9996 0.9992 0.9990 0.9986
* * * *
d0 d0 d0 d0
4 x (B) 2 0
-4
-6
-6 -4
-2
0
2
y / [mm]
4
6
x (A)
-2
-4
-6
d d d d d
6
x / [mm]
d d d d d
6
x (C)
-6
-4
-2
0
2
y / [mm]
4
6
= 1.02 * = 1.01 * = d0 = 0.99 * = 0.98 *
d0 d0 d0 d0
217
LASERneedle®-dental
Parodontolology
Aphthae, wounds, postoperative pain therapy, pulpalgia, inflammation of the gingivae complementary: nausea-acupuncture
Endodontology
LASERneedle® - optical technologies
Laserneedlesurface-polishing procedure Computer-controlled laser fiber coupling
The ability to heal illnesses and relieve pain with light is a fascinating vision. Scientists agree that the 21st Century will be the century of photons, as the past 20th Century was that of the electrons. The laserneedles described in this compendium are characteristic for modern advancements. For the first time, they allow painless and highly effective acupuncture treatment according to traditional rules. Why this is possible is discussed in this book. Laserneedles are products from interdisciplinary and international research. Their effects open up new therapeutic dimensions beyond acupuncture whose medical-technological foundations are described here by authors from Austria, China, Germany and Switzerland.
ISBN 3-89967-199-6 (Europe) ISBN 1-59326-074-1 (USA)
www.pabst-publishers.com
Related Documents
Acupuntura Laser Book
January 2021 0
Manual De Acupuntura Laser
March 2021 0
Laser
March 2021 0
Acupuntura
March 2021 0
Acupuntura - Livro - Manual De Acupuntura
February 2021 0
Laser Hardening
February 2021 1More Documents from ""
Acupuntura Laser Book
January 2021 0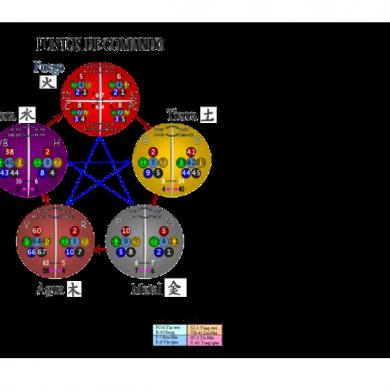
Tabla Puntos Todos
February 2021 0
In Bruges Piano Sheet
February 2021 1
Marcados Por La Uncion - Samuel Santana
February 2021 0
