Download
This document was uploaded by user and they confirmed that they have the permission to share it. If you are author or own the copyright of this book, please report to us by using this DMCA report form. Report DMCA
Overview
Download & View Download as PDF for free.
More details
- Words: 36,455
- Pages: 114
Loading documents preview...
Edited by Garcia-Sanchez PC
1 First Edition, 2015© Second Edition, 2016© Edited by Pablo C. Garcia-Sanchez This book pretends to be an e-book and be read through electronic devices. Think it twice if you want to print it. If you do so, be sure that it is printed using recycled paper. This book is under a Creative Commons License: Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) You are free to share — copy and redistribute the material in any medium or format. Learn more about this CC license at creativecommons.org or in our web:
physiotherapyreflectivecases.wordpress.com Notice Medical and clinical knowledge are constantly evolving and changing. Readers of this book are advised to check the most current information provided on procedures featured. It is the responsibility of the therapist, relying on their own experience and knowledge of the patient, to make diagnoses, to determine dosage and the best treatment for each patient, and to take all appropriate safety precautions. To the fullest extent of the law, the authors do not assume any liability, loss or any injury and/or damage to persons or property arising out of or related to any use of the material contained in this book. The authors
2
Edited by Pablo C. Garcia-Sanchez
3
CONTRIBUTORS Mª Dolores Alcalá 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain
4
Iscia Bertrand 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Pablo C. Garcia-Sanchez Physiotherapist, Lecturer, Department of Physiotherapy and Podiatry, School of Health and Sports, Universidad Europea de Madrid, Spain Gema Gallardo Sanchez Physiotherapist, Physiotherapy Unit, Fuenlabrada University Hospital, Spain Juan Antonio Gonzalez Garcia Physiotherapist, Physiotherapy Unit, Fuenlabrada University Hospital, Spain Rossella Guido 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Marta Javier 3th year student of Physiotherapy, Universidad Europea de Madrid, Spain
Greete Kriik 2nd year student of Physiotherapy, Metropolia University of Applied Sciences, Finland Guadalupe Pérez 3th year student of Physiotherapy, Universidad del Valle de México, México Laura Ponce 3th year student of Physiotherapy, Universidad del Valle de México, México Marie-Anne Rannou 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Andrea Tiberi 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Ainhoa Uria 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Davide Violati 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain
5
FOREWORD TO THE FIRST EDITION La asignatura “Terapia Manual Ortopédica III” pertenece al plan de estudios del Grado en Fisioterapia de la Universidad Europea de Madrid, siendo la última asignatura a cursar dentro del itinerario curricular en “Terapia Manual Ortopédica”. Las asignaturas que lo conforman son optativas y refuerzan la formación en Terapia Manual basada en la evidencia.
6
Este proyecto pretende reflejar el desarrollo del pensamiento crítico y reflexivo, tan necesario para acometer un buen diagnóstico y abordaje terapéutico del paciente a través de la Terapia Manual Ortopédica. Y qué mejor manera que comenzar con los intentos que hace el estudiante con los primeros pacientes a los que se enfrenta en la práctica clínica real. En esta experiencia vivida de forma intensa por el alumno, éste desarrolla competencias como la adaptación del tratamiento a la evolución del paciente, el replanteamiento constante de los objetivos terapéuticos, o la autocrítica, habilidades básicas para cualquier profesional de la salud. Con este proyecto no se consigue únicamente un mejor aprendizaje por parte del estudiante, sino que, nosotros los fisioterapeutas con años de experiencia clínica, tomamos conciencia y recordamos la importancia del razonamiento clínico. La metodología docente utilizada es el Método del Caso, procedimiento que se adapta especialmente bien al desarrollo de las competencias descritas anteriormente; además, la labor del docente, que ha acompañado y guiado al estudiante a través de preguntas constantes, ha permitido la adquisición de un conocimiento más profundo. Nos gustaría destacar la labor del docente, en primer lugar, por plantear este proyecto tan ambicioso y enriquecedor para todos; y en segundo lugar por acompañar y motivar permanentemente a los estudiantes. Él ha sido el motor de este proyecto, gracias a su constante inquietud en innovación de diferentes metodologías en el aula, situando siempre al alumno en el centro de su aprendizaje. Por último, nos gustaría reconocer y agradecer el esfuerzo de estos alumnos que se han implicado de forma completa y que han acometido este reto como una oportunidad de crecimiento profesional y personal; pensamos que esta actitud os permitirá tener una vida más plena. Mónica de la Cueva, Beatriz Ruiz, Raquel Díaz-Meco y PhD , Physiotherapists , Lecturers, Department of Physiotherapy and Podiatry, School of Health and Sports, Universidad Europea de Madrid, Spain
FOREWORD TO THE SECOND EDITION In this second edition of the book, we were supposed to include more case studies from the students, but the number of students attending the subject during 15-16 course were too small, that we have decided to included their work at the end of this new season. Amazing projects could be launched in Education and Health, thinking out-of-the-box, and using wisely the new tools available for physiotherapists, patients and educators. For this second edition, I have invited Juan Antonio and Gema, for writing a chapter about their lovely experience about the use of a reflective diary, and the social media in the education of our students. They are in the paramount place to teach (clinical placement) and in one of the best times to impact the student (last year of university). Thanks for accept my offering. I hope you will be delight with the reading and get inspired for your daily work. Pablo C. Garcia-Sanchez Physiotherapist, Lecturer, Department of Physiotherapy and Podiatry, School of Health and Sports, Universidad Europea de Madrid, Spain
7
8
To our beloved patients, who open their lives to us. Pablo To our teacher, to make this happen. 2015 OMT3 students
9
PART 1: INTRODUCTION
Chapter 0: Introducing the project: using case reports to improve Reflective Practice and Clinical Reasoning in Physiotherapy, Garcia-Sanchez PC. Chapter 1: Use of the reflexive diary, blog and twitter in the practicum: our experience, Gonzalez Garcia JA. and Gallardo Sanchez G. 10
INTRODUCING THE PROJECT: USING CASE REPORTS TO IMPROVE REFLECTIVE PRACTICE AND CLINICAL REASONING IN PHYSIOTHERAPY GARCIA-SANCHEZ PC.
INTRO AND CONCEPTS The ability to reflect about our actions and decisions is irrevocably linked with the basics of our improvement and learning system. This way to approach learning and practice experiences try to get beyond the bare experience as a unique improvement tool, once the therapists have
To share their own clinical experiences to teachers, clinicians and peers, could be an essential activity to develop metacognitive abilities in the learning process (Sefton, Gordon & Field, 2008). Remains in the educator to plan and create the required spaces for feedback and reflection during the course period.
started their professional work, demanding the
According to Rivett and Jones (2008) “Skills in
apprentice to critically look over their own
clinical reasoning can only be developed in the
practice, with the goal of improve it.
context of clinical cases” (Rivett, Jones, Loftus &
It is considered as a corner stone in the development of expertise within a knowledge area (Jensen, Gwyer, Hack & Shepard, 2007) and it is progressively being incorporated to the graduate and postgraduate health science curricula.
Christensen, p. 477). The use of case reports to teach clinical reasoning is well covered by Rivett and Jones in that chapter. The type of case reports carried out in this project were “written cases”, with the particularity that were peer developed with the supervision and questions prompted by another student and the educator.
Clinical reasoning and reflective practice are linked through the metacognition level of reasoning and according to Jones and Rivett (2004) reasoning could be seen as a reflective process (Jones and Rivett, 2004).
Peer learning is an educational method to improve knowledge and understanding, and is broad defined in the literature. The type of peer learning method chosen for this project was what Ladyshewsky described in 2000 and
11
developed through past century, specifically
thinking and reasoning through real cases. This
using the metacognition as a reflective method
book doesn´t intend to emulate our pioneers,
(Ladyshewsky and Jones, 2008).
and probably the depth of the student´s reflections won´t be the same compared with
THE PROJECT AND INSPIRATION
12
these well-noun physiotherapists. But these
This book is the final product of a collaborative
student´s reflections will be productive for them
project among international physiotherapy
and will give an instant insight about what is
students
Manual
happening in the therapist-mind during the
Therapy 3", an elective subject included in the
management. We hope this could be useful for
4th year of the Bachelor Degree in Physiotherapy
others.
attending
"Orthopaedic
at Universidad Europea de Madrid. As we seen, Reflexive Practice is a key skill to The completion of a reflective case was one of
develop Clinical Reasoning in manual therapies
the activities included in the final grade of these
and other disciplines. It is one of the tools these
subject, but the presence of their cases in the
students had learnt during their stage in the
book relied on their own decision. It was guided
university on the last courses, to improve their
by me as a teacher, but the decisions of the
understanding and practice. Giving support to
whole project were made by the students. It was
our clinical decisions will allow us to improve as
completed in 3 months on the spring of 2015.
professionals and as profession.
The project is inspired in the book "Clinical
We hope you´ll find this interesting for your own
Reasoning for manual therapists" (Jones and,
practice and be inspired to cultivate this wise
Rivett,
activity as a teacher, as a student or as a graduate
2004).
In
that
book
relevant
physiotherapist show us their knowledge,
physiotherapist.
REFERENCE LIST 1. Jensen, G. M., Gwyer, J., Hack, L., & Shepard, K. (2007). Expertise in physical therapy practice. 2. Jones, M. A., & Rivett, D. A. (2004). Clinical reasoning for manual therapists. Elsevier Health Sciences. 3. Ladyshewsky, R. K. (2000). Peer-assisted learning in clinical education: a review of terms and learning principles. Journal of physical therapy education, 14(2), 15. 4. Rivett, D., Jones, M. A., & Higgs, J. (2008). Using case reports to teach clinical reasoning. Clinical reasoning in the health professions. 3rd ed. Philadelphia: Elsevier, 477-484. 5. Sefton, A., Gordon, J., & Field, M. (2008). Teaching clinical reasoning to medical students. Clinical reasoning in the health professions. 3rd ed. Edinburgh: Elsevier, 469-78.
USE OF THE REFLEXIVE DIARY, BLOG AND TWITTER IN THE PRACTICUM: OUR EXPERIENCE 13 GONZÁLEZ GARCÍA JA. AND GALLARDO SÁNCHEZ G.
The essential philosophy of the EHEA is that
INTRODUCTION
the student becomes the centre of the system. The authors are clinical teachers of Practicum II in Fuenlabrada University Hospital ten years ago.
During
this
period,
elements
of
participation that assume the philosophy of the European Higher Education Area (EHEA) have been incorporated. This chapter explains our experience of promoting a model of effective learning.
The overall effort of the student is valued, not only physical presence in a class or practices in healthcare
settings,
as
well
as
the
management of tools of learning, rather than the
mere
accumulation
of
knowledge
(Universia Spain, 2016). It is intended that the future professional will be responsible for learning on their own, to locate, analyse,
Rey Juan Carlos University and University
manage, synthesize and transmit information
Hospital of Fuenlabrada work together in
by him/herself.
teaching students in clinical practice. Physical therapy students visit our unit in their fourth course. It was considered that the orientation of the training should be directed towards the imminent
inclusion
in
the
real
work
environment. This mean a promotion of
In this context the teaching guide of the subject Practicum II proposed as a teaching strategy “knowing in action”, which can be achieved with reflective practice. The teacher or tutor has the task of stimulating this reflection in action.
autonomy in the performance of patient care, integrating all their knowledge previously
If we understand learning as an active process,
acquired.
we need to take awareness of it. We must
know about the different kinds of strategies for
and themselves as learners in these different
learning, thinking, and problem solving.
contexts (Chick, 2016). Nevertheless, we know
Students should become aware of their
that it is not a question of an easy matter of
strengths and weaknesses as learners, writers,
practising, since we have not been educated in
readers, test-takers, group members, etc.
the habit of carrying out an exercise that leads
Students have to put metacognition into
us to introspection.
practice. The metacognition is a complex
14
concept
that
has
different
definitions.
Metacognition is, put simply, thinking about one’s thinking. More precisely, it refers to the processes used to plan, monitor, and assess one’s
understanding
and
performance.
Metacognition includes a critical awareness of
With these premises since the 2012-2013 we have incorporated as elements of learning and assessment a reflective diary, a blog of the subject and the use of Twitter as social network. REFLECTIVE DIARY
a) one’s thinking and learning; and b) oneself as a thinker and learner. Major and its group of study
(Labatut
Portilho,
2004)
say
metacognition is the cognition of the cognition, that is to say, the knowledge of your own knowledge. The knowledge is the object of the cognitive activity. The way a therapist clinically
With the base of the teaching guide, different aspects were incorporated as the experience was progressing and reading about other experiences was made (Martiáñez Ramírez, 2012).
reasons their findings can strongly influence
As the name suggests, it is a chronological
how the case is interpreted. It seems clinical
account of what happened every day in the
reasoning need of the sum of the thinking and
practicum. From the beginning we emphasize
decision-making processes associated with
that the diary is voluntary, although evaluable.
clinical practice (Edwards I, 2004). The way
It
how we think it will be important to make good
discoveries,
decisions and actions. Metacognitive practices
disappointments,
increase students’ abilities to transfer or adapt
expectations, events, thoughts, reflections,
their learning to new contexts and tasks. They
suggestions, explanations, etc., experienced
do this by gaining a level of awareness above
by the student. Reflection-on-action is what
the subject matter, thinking about the tasks
gives added value to the experience. It is
and contexts of different learning situations
intended
contains
that
views,
concerns,
feelings, surprises,
the
cognitive
desires, learnings, ambitions,
effort
to
remember, process, analyze and explain in
indicated that the diary demands a richer and
writing is a way to learn.
more complex cognitive effort than the simple
It is important to emphasize the consideration that the concept of Practicum has for us. According to Guijarro Martínez (2015) we prefer the term clinical education in so far as “can contribute to [the student] development not only in doing, but also in knowing, being and living “. Reasoning, critical thinking, decision making, values, attitudes, ethical behaviors and professional socialization are involved in practice and this is considered from this broader view than simply know how (Guijarro Martínez, 2015).
description. It is noted that there is an added value in this reflection that makes it necessary and, above all, useful in their present and future learning. ACTIVITIES
15
Around reflection in action and reflection deferred to the end of the day, the students carry out different activities. They search images, rating scales, variants on ways to assess and treat patients, include database search strategies, incorporate links to websites and/or videos, attach annexes with these and
TASK
other contents, etc.
The first day students are received and
In our experience the weekly reflective diary
teachers explain to them, among other things,
usually contains 6 to 12 pages. It is sent at the
the tasks to be carried out during their stay in
end of the week by email to the teacher.
the hospital. In the case of the diary they are
He/she receives two or three diaries and once
told that it has to be written on a daily basis to
read, share relevant reflections with the
achieve the objectives. They are provided with
student in writing. The teacher corrects,
information on the potential contents. They
suggests, guides or compliments. The door is
have had previous and different experiences
open to discuss all this personally, making the
with a reflective diary. Therefore, they are
process something continuous.
provided with additional written information to get what we expected.
The reflective diary is, as we said, an assessment
tool.
Since
the
2015-2016
The proposed model of reflective diary is
academic year, in an attempt to be objective, a
deliberately versatile and open. However, it
rubric based on Martiañez Ramirez et al (2015)
always contains the reflection of the students
is used.
beyond a mere description of facts. If not, we
In short, reflection is used to what we have
that has to do with something related to the
been arguing. It encourages to propose
practice. Guidelines are given and they can
alternatives, rethink what has been done, said
read some posts in health blogs as examples.
or thought, to question processes, to justify, to
Most of students did not use before this tool.
drive change, to change attitudes and values. All this means work, and time. Students have
16
to work at home for a stronger learning and a
ACTIVITIES
development of criticism. It will be useful for a
We want the students to make the writing
life-long-learning.
process, adding the advantages of Internet such as easy sharing, abundant information
BLOG
and resources and unlimited communication. The writing process consists of:
Student blogging empowers students to take charge of their learning, gives their learning
Prewriting: Plan the writing. It is a time to
purpose while helping with reading, writing,
think, brainstorm ideas and organize the topic.
digital citizenship, artistic, critical thinking,
Students have questions to consider: what do I
social skills, self-expression and creativity
want to say? How do I want to say it? Who will
(Huffaker, 2005). It could also increase
read my writing? What else do I need to know
students and teachers´ motivation and
to begin? Who can I talk to about my ideas?
relationship, as well as academic achievement (Read, 2006). In our opinion blogging is perfect to use metacognitive strategies. Our
blog
write it down. Create a rough copy of the writing. Students have question to consider:
“Practicasfisio”
(https://practicasfisio.wordpress.com)
Drafting: Write your first draft. It is a time to
has
been used as a teaching tool since 2014-2015
Are my thoughts organized? Which ideas do I want to develop? In what order do I want to say them? Who can read this?
academic year. Revising: It is a time to improve the writing. Change your write to make it better. Questions TASK
to consider: Should I add or take out parts?
Students are explained the steps to publish
Have I used the best ideas and words? Are my
their posts on the blog. They must publish two
details clear?
posts in six weeks. They can choose the topic
Edit: check your writing. Questions to
that includes informative tweets, mentions
consider: Are my spelling, capitalization and
and communications to students. The author
punctuation correct? Could I use any image to
also makes a proposal for other uses: academic
complete the text? Could I use some useful
information, enrichment of the educational
links to add information?
experience,
Publish: share the writing on the Internet. We emphasise the first part of the writing process where the student must reflect.
extension
of
contents
and
“twitoria” or tutorial via Twitter. Finally, Arroyo
also
proposes
some
dynamic
integration of Twitter in the classroom. With that background we began by creating an
We have published sixty posts with 7,825 visits
account named @practicasfisio. The teachers
till the date but very few comments.
had started the use of personal and collective accounts nearly two years before. Surely that
TWITTER
previous usages led to learn utilities and
Our interest to incorporate new teaching tools
potential applications and the knowledge of
led us to put in the social network Twitter in
reference accounts in the field of Physical
the practicum at the beginning of 2014. We did
Therapy. As Twitter inherent philosophy, we
not know prior experience in clinical settings of
intend to make public the contents whose
Physical Therapy or other health discipline.
usefulness or uselessness can be decided by anyone. This means that tweets should be
Social networks can be used as a learning tool by providing information and means for integration and communication (Moreno Badajós, 2016).
respectful to people and the information should not contain personal or health information related to any person. Our uses largely coincide with those targeted by Arroyo
The study of Arroyo Sagasta (2012) addresses
Sagasta, with some particularities proper to
the presence of Twitter in a particular high
the nature of the Practicum.
education academic environment, face-toface education and very different to a clinical setting, but it was our initial reference. Its description of the use of social network for teachers is done from a primarily qualitative approach and contains a list of applications
After two years and a half using Twitter the teachers appreciate it positively. However, against our prejudices, this network was not used on a daily basis by most students. Most of them do not participate regularly in Twitter
17
after the practicum (at least with the profiles
In the framework of the Extension of contents
with which they did in the Practicum II).
Tweets there are links to documents, articles, videos, websites, highlighting references to
TASK
professional blogs as a source of information
It is proposed, in the context of the practicum, participate with messages of different types. Students write spontaneous comments with
18
information on topics related to what happened or they have seen. They may include links to other written content, images, videos. Teachers´ participation is considered more important because of novelty and lack of
and/or debate. Questioning tweets contain questions about different dimensions of practice (methods, techniques, illnesses, etc.). Some of them encourage enquiry about ethical codes and legal aspects of professional practice. These are responded via Twitter or students are told if the answer will be in the diary or verbally.
experience in use by many students. Students are invited to participate with tweets ACTIVITIES
about the contents of the practicum, to re-
Depending on the content we can classified
tweet,
the tweets in different types.
discussions or to answer different questions
In the
to
share
information,
to
open
Information tweets the teachers use the
that appear in the practicum.
account, since the start of each rotation, with
As in the case of diary and blog, a specific
indications about tasks, linking to content
rubric evaluates various aspects of student
about reflective diary or use of blogs in
performance.
healthcare, among other things. Other uses are information about the way of publishing
CONCLUSIONS
posts in the blog of the subject, dates or
The incorporation of teaching tools described
notifications for submission of tasks, changes
in this chapter has, as their ultimate goal, to
of teachers or teachers’ absences, exam dates,
promote more lasting and deeper learning
etc. Other informations are about professional
and habits that facilitate livelong learning. For
organizations,
the authors this is an ongoing process,
announcements,
offers,
courses/conferences that may be of interest
unfinished and subject to constant revision.
for the student or for his/her
The opinion of students is a determining factor.
immersion in the profession.
imminent
We asked them and their assessment is encouraging. However, we think it is necessary
to promote continuous efforts to improve the competences of future physical therapists.
REFERENCE LIST 1. Universia España. (Junio de 2016). http://eees.universia.es/. Recuperado el 16 de Junio de 2016, de http://eees.universia.es/preguntas-frecuentes/conceptos-basicos/#4 2. Labatut Portilho, E. (2004). Aprendizaje universitario: un enfoque metacognitivo. Madrid: Universidad Complutense de Madrid. 3. Edwards I, Jones M, Carr J, Braunack-Mayer A, Jensen GM. (Abril de 2004). Clinical reasoning strategies in physical therapy. Physical Therapy, 312-30. 5. Chick, N. (2016). https://cft.vanderbilt.edu/. From https://cft.vanderbilt.edu/guides-subpages/metacognition/ 4. Martiañez Ramirez, N. (2012). El diario reflexivo académico como recurso de aprendizaje en las prácticas clínicas: una experiencia en el grado de Fisioterapia de la Universidad Europea de Madrid. IX Jornadas Internacionales de Innovación Universitaria. Villaviciosa de Odón. 5. Guijarro Martínez, M. (2015). La educación clínica del estudiante de fisioterapia desde la experiencia de los tutores y tutoras clínicas. Estudio fenomenológico descriptivo. Bilbao: Deusto. 6. Martiáñez Ramírez, N., Rubio Alonso, M., Terrón López, M., & Gallego, T. (2015). Diseño de una rúbrica para evaluar las competencias del Prácticum del Grado en Fisioterapia. Percepción de su utilidad por los estudiantes. Fisioterapia, 83-95.
19
PART 2: REFLECTIVE CLINICAL CASES
Chapter 2: A 52 yo. man who broke his arm 9 month ago and referred pain in all movement, Alcalá MA. and Uria A.
20
Chapter 3: A 32 year old woman with sore thightness in the upper posterior surface of the right leg, Bertrand I. and Rannou M-A. Chapter 4: A persistent shoulder pain and rigidity in a 51 y.o woman, Guido R. and Javier M. Chapter 5: A 45 yo. garbage collector with chronic back symptoms , Javier M. and Guido R. Chapter 6: A 23-year-old female preparing for army with lower back pain for 4 weeks , Kriik G. and Ponce l. Chapter 7: A 40 yo. man with a painful shoulder syndrome, Pérez G. and Kriik G. Chapter 8: A 16 yo. female student that suffered a 2nd grade right ankle spring, Ponce delhoyo L. and Perez-Raymundo G. Chapter 9: A 57 yo. housewife with a right hemi patellectomy and tenectomy of the patella tendon after a patella fracture and a transidesmal fracture of the right fibula bone, Rannou MA. and Bertrand I. Chapter 10: A 8-year-old boy with fractures of both legs after a fall from the eighth floor of an apartment, Tiberi A. and Violati D. Chapter 11: A too early meniscal diagnosis, Uria A. and Alcalá MA. Chapter 12: Pain causing a scapular diskinesis in a 25 yo student, Violati D. and Tiberi A.
21
A 52 YO. MAN WHO BROKE HIS ARM 9 MONTH AGO AND REFERRED PAIN IN ALL MOVEMENT ALCALÀ M.D. AND URIA, A.
22
INTRO A 52 yo. man who had a sedentary life and one day fell down from a stone 9 month ago and
for him to relax himself, not only like stop doing something but also he can’t calm his body.
broke his arm and since that he referred pain in
The accident affect his daily life activity due
all movement and his previous treatment
the impossibility to use the hand he couldn’t do
doesn’t work but he is stressed and tired about
all that things that he usually do and he was a
this because he wants be better as soon as
little bit overwhelmed and tired about this
possible.
situation.
SUBJECTIVE EXAMINATION
He went to another physiotherapist before I
When I first met P.N was two month ago, he
met him but the results weren’t the expected.
had a lot of pain on his distal part of the left arm.
He was treated by this therapist 20 sessions
He doesn’t had all the range of motion and he
but he wasn’t happy and his problem
told me that sometimes he doesn’t feel his
continued and also gets a little bit worst.
third, fourth and fifth fingers.
He use his hand and arm like he doesn’t have it,
He works as a lawyer and he is the boss of the
also because his predominant arm is the right
association, so his life is a little bit sedentary,
arm but he couldn’t continue with this pain.
he doesn’t like practice any sport but he love to go to the theatre, cinema and going out for
STUDENT REFLEXION AFTER S/E
dinner with his wife. We can say he likes doing
With this presentation of P.N I think that he
relaxing things, because in his work he had a
has neurogenic and muscular damage.
lot responsibility and he is stressed. He told me
The main problem is the fracture that he
he is very active: because he usually have a lot
suffered at the radio and the consequences are
of things to do at the same time, being difficult
the affectation of muscles and nerve. He has a
Q2: Didn’t you think about the possibility of the
long period development of the pathology so I
ulnar nerve being damaged too because of the
know that the fracture is solved but I have to
alteration in the sensibility of the fourth and fifth
work on all the tissue that are affected to mend
fingers?
the neurogenic problem. After S/E I think that the median nerve is affected so I will check at the elbow and the wrist.
A2: No, because the ulnar nerve’s test was negative and because in the electromyography we saw the damage of the median nerve.
For the flexors and extensors muscles I have to recuperate all the range of motions and then I can work out to improve the debility that he has.
TEACHER ADVICE Choosing high evidence-based tests will add to your reasoning better ingredients to make a good
My patient start the treatment very stressed because he wants to be better but he saw that the last treatment doesn’t work but now I can see
decision. Regarding to the neurodynamics issues, we need to discriminate among tests assessing roots, nerve trunks and main nerves.
how he is more animate and positive. So far, ULNT3 hasn´t demonstrate high sensibility The last treatment was about massage on the arms to relax the muscles and use ultrasound and
and specify. So, adding your inexperience, we need to take with precautions
laser therapy, but it doesn’t work. PHYSICAL EXAMINATION QUESTIONS TO IMPROVE REFLEXION
First of all my patient has a diagnosis before I met
Q1: How did you know that radio´s fracture was
him, so in part he knows what he has, but nobody
already cured, just because of the time that had
stopped one moment and tell him the exact
passed since the fracture took place or you had
information about which parts of his harm and
photographical evidence? And do you know if he
hand were damaged and the different part of the
used any orthotics after the fx and for how long?
treatment.
A1: I know it because I saw the MRI so I have the
Firstly I spend time to explain him exactly which
photographical evidence and I’m sure about the
are the tissue he had affected than I started with
consolidation of the fracture. No, he didn’t use
the P/E and with the medical diagnosis I build my
any orthotics after the fracture.
hypothesis and I started from the elbow and I
23
saw that he has all the range of motion and no
QUESTIONS TO IMPROVE REFLEXION
pain, so I passed to the wrist.
Q1: You´ve said you had all the information
In the clinical history of my patient I had all the information about ROM, BM, damage and all about the problem but I think that I had to explore all and plan my own treatment
24
because the one he has received doesn’t work. On the wrist I tested the range of motion and muscular balance.
about ROM and BM… but it´s no clear which joints are you talking about when referring to ROM or which muscles BM are you testing. A1: I referred to wrist’s joint and all the extensors and flexors muscles. Q2:
You´ve
said
you
started
physical
examination from the elbow. Why didn´t you start at a higher level, for example, from the
With neurodynamic technique I tested the
shoulder?
ulnar, median and radial nerve to see if the
because of the damage of someone of this.
A2: Because of his mobility and his pain I supposed that the shoulder shouldn’t suffer any injuries, so I decided started from the elbow.
STUDENT REFLEXION AFTER P/E
Q3: Did you assess any reflexes or sensations
The anterior diagnosis showed me which part I
apart from making neurodynamic techniques?
debility and the strange sensation he had were
had to test but I decide made my own P/E to start another time from the 0. I had no contraindications for P/E so I tested
A3: Yes, I assess the sensation with different type of touch on his arm and hand but the only think he feels is tingle sometimes on his hand so I decide to make neurodynamic techniques
without any problem and I saw that he had a restricted range of motion in all movement of
PATIENT MANAGEMENT
the wrist and some alteration of the sensibility on the hand. But the most important thing that
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
I saw is that the necessity of my patients is to
My goals are:
knows because I do one thing and no other because he was saturated and tired that people tell him what to do but not encourage
-
Improve the range of motion of the wrist
-
him and not explain him nothing.
Improve straightness of flexors and extensors muscle
-
Eliminate the pain
-
Recuperate the sensibility
-
-
Change the treatment from the
mobilizations if the pain decrease or increase
anterior
and I saw that the pain decrease.
Increase the motivation of my patient and improve self-confidence
Now I had to search a new treatment because the anterior doesn’t work.
After that I started forced the end of the movement to start improving the range of motion. To terminate the session I started stimulate
I know that my patient needs something more
the sensibility on the hand with different type
than a simple massage and I think that the
of touch and with complete extension and
ultrasound and laser didn’t have any benefice
flexion of the fingers on the active form.
in this case. After that I had to animate my patients and explain him that now we going to use new treatment and that he has to be patients and trust on me but I know that at this point maybe it can be difficult.
STUDENT REFLEXION AFTER D1 TREATMENT At the end of the session my patient referred that the pain decrease and a sort of liberation on the wrist. I saw that something change, he
First of all I focus my attention on the wrist and
was more animate than when he arrived at the
the movement of this because he had a big
session.
restriction of all movement and at the same I work on the median nerve and the sensibility.
This process was different from the previous and at the beginning the patient was a little bit
DAY_1
insecure but I could see how it works and also
I told him to take some posture of the wrist in
him could see that from the first session we
which he doesn’t feel pain and I make the same
had some results so I will continue with this
thing for the elbow to see when the pain
treatment.
appear. QUESTIONS TO IMPROVE REFLEXION After that I saw that the elbow had no restrictions and no pain so I focus on the wrist. I make mobilization fixing the radio than fixing the ulna. After that I did the mobilizations of all the bone of the hand. I make all this movement in the passive form and evaluating after all the
Q1: What happened with the sensibility? Did it improved? A1: At the moment I didn’t know because I had to wait the next sessions and see what happen in those days and text it in the next session.
25
DAY_2 Firstly I test the movement and the general state of the wrist to saw if he had maintained
days he doesn’t feel nothing strange about his fingers.
the resulted we reached in the anterior session
Now I started work on the strength of the
and it was ok.
muscles with resisted movement firstly than
After that I do the same treatment because I
26
Also the sensibility was better because in those
saw that it works, also I started work with
we use the electro stimulation of the flexors muscle with a dumbbell of 0.5 kg.
resisted movement at the same time he was
Finally I work releasing muscles in general to
with the electro stimulation and I saw that he
avoid the overload.
can do it perfectly even if with a little bit pain at the moment of mayor tension of the muscles.
On the next session I saw that the treatment work out so I continued with this and increase slowly the kg of the dumbbell.
At the end I relaxing the flexors and said him to make the same exercise at home with a little bottle of water.
I think that the prognosis is good because my patient was satisfied with this new treatment and was more animate and participate.
DAYS 3-4 After that I can say that the part of the In the next session my patient referred less
treatment
pain and more agility on the movement so I
mobilization of the ulna and radio in all
decide to continue with this treatment.
direction because after that was the moment
that
works better
was
the
in which I started to see important change in the evolution of the problem
FINAL STUDENT REFLEXION I think that at the moment in which I met my patient I had apparently all the information I need for my clinical reasoning. I had the information from the medical diagnosis, from the anterior treatment but it wasn’t enough because there was something that doesn’t work, so thanks to my examination I discovered the main point of the problem. All this means that even if you apparently had all the information you always had to search more and more to have a complete clinical reasoning that is the main point for a successful treatment.
REFERENCE LIST 1. S. Jimenez del Barrio, M. Fortun Agud, N. Pascual Lanuza. E. Bueno Garcia, E. Estebanez de Miguel and J.M. Tricas Moreno (2013). “Reliability of upper limb neurodynamic test for range of movement and symptoms localization variable”. Cuestiones de Fisioterapia 281-289.
27
A 32 YEAR OLD WOMAN WITH SORE THIGHTNESS IN THE UPPER POSTERIOR SURFACE OF THE RIGHT LEG BERTRAND I. AND RANNOU M-A.
appendix a year and a half ago and that she still
INTRO A 32 years old woman attends a physical
28
therapist due to sore tightness in the posterior surface of the right leg; ischiotibial level. High-
doesn’t feel 100 percent “good”. She feels tightness and bloated all the time in the area and has digestive discomfort since then.
level runner, the pain began and gradually
She is a very health, energetic,
worsened 8 month after being operated from
sympathetic, open minded, athletic young
the appendix.
woman
who
has
no
relevant
family
antecedents, doesn’t smoke and sporadically
SUBJECTIVE EXAMINATION
drinks alcohol in social events. She would run
A 32-year-old patient entered the
an average of 10 kilometers a day and was
consultation and started explaining her
getting ready for an important race that
condition. For a few month now, she started to
needed a lot of training. She works long hours
feel pain in the upper posterior surface of the
behind a desk and seems to be very unsatisfied
right leg while jogging; right underneath the
with her job. She loves outdoors activities and
ischium. At first she could cope with the pain
never misses an opportunity to join a group to
but as time went by it worsened to a point
participate in the event.
where it forced her to stop jogging. She would feel the pain during the terminal swing and beginning of the propulsion phase of the human running locomotion cycle and would increase when running up steep hills. The pain would also appear while she blow-dried her hair in a bending over position and occasionally, complained of lumbar pain. Continuing
to
STUDENT REFLEXION AFTER S/E About my initial hypotheses about the sources and pathobiological processes was that she could have a tendonitis of the proximal insertion of the hamstring muscle due to overuse and maybe some active trigger
gather
useful
information about her case, she mentioned that she underwent surgery to remove the
points in the gluteus area.
She didn’t present any warning for
Q3: So far, what is your thinking about the appendix-release issue in her actual clinical
examination contraindications. My first impression with her was quite optimistic. Her positive and energetic attitude
presentation? A3: It is explained further.
was quite freshening; making it easier to create a physiotherapist- patient bond of trust.
TEACHER ADVICE
Even thought I knew that her condition was
Irritability means about the property of patient´s
also affecting her psychologically, since it
current presentation reacting to any stimulus,
limited her ability to perform the activity she
and it is not directly related with the amount of
loves most well, she always managed to keep
affected activities or participation. It´s used to
a positive and open-minded attitude about it;
be more related with the severity of the
listening and cooperating with us during the
presentation. In our management it is usually
treatments and completing her “home work
linked with the quantity of mechanical stimulus
assignments”.
needed to cause patient´s symptoms and their length. This quality will suggest the extension
QUESTIONS
TO
IMPROVE
REFLEXION Q1: How does she feel about her pathology? A1:
and the level of depth of our exploration procedures.
PHYSICAL EXAMINATION
Haven’t asked her but I think she is
Although she seemed like a joyful,
annoyed about the fact that she can’t run as
optimistic and stressless person during the
long and as well as she did before and anxious
sessions, I wanted to know how she was in a
to get better.
work-like environment; to see her stress levels
Q2: So far, what is the level of severity and irritability of her clinical presentation?
and if it had an impact on her. It turned out that during her working hours she’s quite stressed out because of the bad ambience there is at
A2: The level of severity of her pathology is
work and admitted that she eats fast sugars to
minimum but the irritability is quite high since
quench her anxiety.
it’s affecting her daily life activities. I started the physical examination by palpating the right proximal insertion of the ischiotibial’s but she felt very little pain
29
compared to the one she used to while running. Like I mentioned earlier the pain appeared during the terminal swing and beginning of the propulsion phase of the human running locomotion cycle and would increase when running up steep hills. The pain also appeared while
30
performing
a
resisted
isometric
contraction of the hip in extension and of the knee flexion; to test the ischiotibial and gluteus muscle. Body chart representing her pain. She also had active trigger points in her right gluteus muscles and a blocked
STUDENT REFLEXION AFTER P/E
sacroiliac joint because of the hypertensions of
About my initial hypotheses I met
the buttocks muscles. Her pelvis was in a slight
consistent findings about the implications of
anterversion position and her body slightly
trigger points in the gluteus muscle but not
leaned forward. Sometimes she complains of
about the tendonitis of the proximal insertion
lower back pain.
of the right hamstrings.
I decided to then explore her iliopsoas,
It is clear that she has musculoskeletal
witched showed to be rather painful (both of
dysfunction for, as mentioned in the physical
them). And the scar left by the appendix’s
examination part, she has reduced muscle
surgery was ridged, fibrotic, adhered to
strength and a slight anteversion of her pelvis
connective tissues below and painful on
with a semi blocked sacroiliac joint; but I keep
palpation.
asking myself why? How is it that in less than a year, gradually, has she been feeling pain in
Muscle group
Grad (0-5)
Ischiotibial muscles
4
Hip abductors
3+
Iliopsoas
3+
the posterior part of her leg when she’s been running all her life since the age of 17? Its not like she’s not physically prepared; she is very athletic and physically strong. The pain came gradually, little by little
Muscles’ Power
since the surgery. I think that the surgery and
the scar left behind are partly the reason and
PATIENT MANAGEMENT
origin of all the simtomatology of why she is
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
complaining of isquion pain. Due to the aggression her body
I think the pain she’s is feeling on the posterior
underwent with surgery, I think she adapted
surface of the right leg is caused by an overload
analgesic positions wile running in order to
of the isquitibials muscles due to the pelvis
reduce the abdominal tension and pain
anteversion, gluteus weakness and lumbar
acquiring
pain; all of which is caused by an incorrect body
an
erroneous
body
position;
triggering an imbalance between muscle
position.
groups forcing some to work more than others. Since she is a young athletic woman her prognosis is good. She is willing, eager to get
QUESTIONS TO IMPROVE REFLEXION
better and does everything possible in order to
Q1: Was anything done with respect to her
achieve this goal. However she is very
digestive tract symptomatology?
impatient, and so whenever we achieve to reduce the pain, she forces her leg more and
A1: Yes, due to her digestive discomfort of tightness
and
bloatedness,
she
relapses.
was
recommended to take probiotics for a month
DAY_1 + 2
and to drink a lot of water in order to rebalance
The first day she came to get treated, I applied
her intestinal flora. (It was very useful) .
analgesic electrotherapy for 20 minutes on the upper posterior surface of the right leg to
TEACHER ADVICE
reduce the pain.
Facing a high irritable presentation as you suggest, involves to take some extra precautions
Afterwards I did massage therapy on the
during the physical examination. In your case,
iquioteibials muscles to relax the muscle as
probably this means to explore carefully the
much as I could to see if in doing so, the pain
myofascial trigger points, and do not stress the
would reduce.
common ischiotibialis tendon to the extent you couldn´t continue with the P/E routine.
I explained to her what I thought what going on and the biomechanical of her lesion. I asked her the next time she goes for a jog that she should take smaller strides to reduce the hip
31
flex/ext amplitude and the force exerted by the muscles.
DAYS 3- 5 Natalie, as expected, commented that the few
I ended the session with passive stretch of the
days following the treatment she noticed
isquioteibials muscles and the gluteus muscles.
improvement but then it went back to the original pain.
STUDENT REFLEXION AFTER D1+D2 TREATMENT 32
The patient was able to do the movement of bending over and touching the ground (movement that she couldn’t do without pain) with a 40% decrease of pain. I’m glad I managed to reduce her pain although I expect it wont last long since I didn’t treat any other areas due to lack of time.
So for the next few sessions I mostly insisted on working on reducing her pelvic anterversion with
manual
therapy
techniques
and
increasing the sacroiliac joint mobility. I would also work on her scar; reducing the fibrotic, adhered tissues and making it more flexible using “ventosas” and massage theray. Treating her iliopsoas was also important to relieve the tensions and reduce the back pain
QUESTIONS TO IMPROVE REFLEXION Q1: About the pelvic anteversion: Why did you
she would complain from time to time. I showed her how to stretch it and told her to stretch it as least once a day.
chose to treat only the joints and not for example, her abdominals?
For the isquiotibial, I gave her exercise to do at home to strengthen it. Eccentric exercise. And
A2: Interesting point, I didn’t think about it; but it would of have been an additional effective
strengthening
exercise
for
her
gluteus
muscles.
treatment. I will take it into consideration for next time.
STUDENT REFLEXION
TEACHER ADVICE
The pain reduces progressively. It seems that
A test-treatment will allow you to get invaluable
we are on the good path.
information about the condition of the presentation. Using the results of the treatment
QUESTIONS TO IMPROVE
as another piece of evaluation could inform you
REFLEXION
how to treat your patient properly
Q1: How does she feel about her treatment?
A1: She was very grateful. She knows the
To strength the tendon elastic properties will be
progress is slow and that she needs to be
a required goal in most tendon issues
patient. But as the sessions passed by, she
presentations. On the other hand we could not
would notice positive changes and that little by
forget the muscles power training. There are
little the pain reduces.
recent published evidence to relieve tendon pain using isometric, contraction, which should
TEACHER ADVICE
helped with your patient too (Rio et al. 2015)
33
FINAL STUDENT REFLEXION Natalie was improving slowly but surely. I think that the fact that she was really motivated actually helped a lot with the healing process. There were ups and downs during the duration of her rehabilitations but we managed to resolve all the problems and move forward to try and achieve a full recovery.
REFERENCE LIST 1. Daniel Cushman, Monica E. Rho et al (2015). “Conservative Treatment of Subacute Proximal Hamsting Thendinopathy Using Eccentric Exercise Performed With a Treadmil.” Journal of Orthopaedic and Sports Physical Therapy. 0;0(0):1-24 2. White, K. E. (2011). High hamstring tendinopathy in 3 female long distance runners. Journal of Chiropractic Medicine, 10(2), 93–99. doi:10.1016/j.jcm.2010.10.005 3. Sherry, M. (2012). Examination and Treatment of Hamstring Related Injuries. Sports Health, 4(2), 107–114. doi:10.1177/1941738111430197
4.
Rio, E., Kidgell, D., Purdam, C., Gaida, J., Moseley, G. L., Pearce, A. J., & Cook, J. (2015). Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British journal of sports medicine, bjsports-2014.
A PERSISTENT SHOULDER PAIN AND RIGIDITY IN A 51 Y.O WOMAN GUIDO R. AND JAVIER SIMON M.
34
INTRO
M. cames showing an antalgic posture that
The patient is a 51 woman that refers pain,
strikes me: aproximation and internal rotation;
especially during the night and stifness in her
holding the affected arm with the other.
left shoulder since 9 months ago. She was initially treated for a supraspinatus tendinitis, with poor results. She
came
to
consultation,
referring
a
symptom’s change and helplessness of not being able to accomplish daily things.
The symptoms have started nine months ago, when she was working in Germany. She doesn’t remember any direct trauma in the arm. She kept in mind that one day rising in the morning, she started having a not well localized acute and annoying pain in her left shoulder,
SUBJECTIVE EXAMINATION M. come to visit in November, talking about a dull and continuus pain and stifness in her left shoulder, that prevents her to carry on
especially during the night. This lack of sleep caused her a lot of tiredness and anxiety, with the consequence of not being able to work and take care at house chores.
movements of daily life, for example when she combs her hair, and paints (a passion of her).
She thought that the intake of medication was
She works as an architecht on her own and she
the only way to fight against the problem. She
is married, with a German man, for 25 years.
started taking medications (NSAIDs) to slow
Unfortunately they have no children, due to an
down the symptoms, but this forced her to be
histerectomy she underwent at 32 yo.
dependent on medications.
She’s a busy woman, who worked around the world, especially in Germany where she was living since 6 months ago. Her husband continues to work there, and being away from him, overwhelms her a lot.
After a months of acute pain, under the advice of her husband, she decided to attend to a physiotherapist. She was treated for a supraspinatus tendinitis for two months, with poor results.
The symptoms increased over time and a arm
symptoms change could be a evolution of this
rigidity began to manifest, that prevents her
first problem.
from moving it. When I asked her if the pain, after treatment and a few months later, was always the same or if she noticed change, her response was :“At the
There is also a emotional component that compromise the evolution and the mood of the patient.
beginning the pain was severe and sharp, to the
M. is feeling alone, because her husband is not
point of crying for the pain. After the treatment
with her and the pain and rigidity prevents her to
I noticed a small change in the pain quality. It
have a normal life and to perform her hobby.
wasn’t too acute and I was able to rest a bit more.” After the failed treatment, due to family reasons, she had to come back to Spain, and even she presented symptoms, she did not intend to attend to another physiotherapist. The months passed, the pain was still present,
I don’t think the disease is related with a tissue damage, instead with a progressive disease: her problem could be a tendinitis sequel and shouldn’t be related, considering her symptoms evolution, with soft tissues and bones damage surrounding the shoulder.
and rigidity even more.
She’s very disappointed with her anterior
Desperate for being unable to move her arm,
treatment and think that her problem has not
rest and have a normal life, she decided to go to
solution.
a physioterapist practice. At the present day, the patient is not motivated and thinks that her problem has not solution. M. has hypothyroidism and take daily medicine for this problem. She has been smoking a packet of cigarettes a day for 15 years, and she is an occasional drinker. STUDENT REFLEXION AFTER S/E I think her symptoms are related with the pathology diagnosis. The supraespinatus tendinitis could be a consequence of her actual presentation and the
I need to attend emotional issues in her presentation. I’ll return considering this point after the physical examination. QUESTIONS TO IMPROVE REFLEXION Q1: Do you think that could be related with a visceral problem, for example with a lung problem, like she is a smoker, and a lung problem refers pain in the shoulder? A1: I’d have considered it in the physical examination.
She was asked to do several
35
exams for discard associated diseases and, in
literature to follow routinely. Sometimes is
particular, the chest radiography was normal.
interesting to give this list to the patient in the
I think that can’t be a reffered pain of a visceral disease: M. doesn’t have related sympthoms
waiting, before entering the assessment room and check with her later the specifics.
and she refers, in the following physical
36
examination that her pains is triggered and
PHYSICAL EXAMINATION
increase with movements.
Before the physical examination, talked to me
I will deepen this thought in the rest of the issue.
that she did, a shoulder radiograph and a chest radiograph to discard other pathologies. In both
Q2. So far, which is your hypothesis about the
cases, the radiographs were normals.
pathobiological issues and pain component? A2: My hypothesis is about a nociceptive and somatic pain that starts with an inflammation presentation. With the passage of time this
I decide to ask her other questions about her life, before starting the physical examination, specially about her hobbies.
inflammatory pain become chronic and the
M. tells me that she paints since she was 20 yo,
inflammatory symptoms make space for
and it was a very strong passion for her.
stifness and a adhesion role. She used to paint, 5/6 hours a day, with both Q3. Which could be the role of hypothyroidism in
hands alternately. She’s ambidextrous.
her presentation? I start the physical examination with the visual A3: Oliva,Berardi, Misiti, Maffulli (2013) noticed that thyroid diseases should be linked to idiopathic tendinopathies and as Sardella White and Garbe (2010) found the hypothyroidism
inspection. I detected the left shoulder higher than the other one and in antepulsion, also the protracted left scapula. Muscle atrophy of the shoulder girdle was present too.
could be a risk factor for the joint. I detects also upper trapezius hypertone. Her first tendinitis could be related to her hypothiroidism
disease,
that
could
be
considered like a predisposing factor. TEACHER ADVICE Ruling out red flags in the S/E has to be a wise option. There are several list s of questions in the
The colour of the skin in general and in particular in the shoulder area is normal. Palpation produces pain of subscapularis (VAS 6/10) and deltoid (VAS 5/10).
The passive movements exploration of
left
The active movements exploration refers similar
shoulder refers limitation in all movements with
limitations and pain: 70 degrees of flexion, 25
a not well localized pain (VAS 6/10), in particular
and 35 degrees respectively of external rotation
in abduction and external rotation.
and internal rotation and 55 degrees of abduction. (Table 1) The patient isn’t able to perfom power testing because she refers so much pain and releted weakness.
Subescapularis pain: blue
Deltoid pain: red
Subsequently I perform a provocative test for cervical radiculopathy, the Jackson’s test, and the Adson’s test to discard a thoracic outlet syndrome. Both tests were negatives. I perform also any special tests that help me to
Not well localized pain
diagnose a possible disease, like the Apley Scratch Test and the Shrug Sign as McFarland and Kim (2006) shown. The negative test performed is the O'Brien's test (to exclude SLAP lesion). After the P/E, the patient refers me to be very afraid about the diagnosis and sad. I recommend her to attend to a doctor ,with the suggest to have a MRI, to better diagnose.
In passive flexion the patient can’t move beyond 85 degrees. The external and internal rotation are respectively of 30 degrees and 40 degrees; in the abduction the patient presents 60 degrees.
37
38
ROM
F
IR
ER
ABD
Passive
85°
40°
30°
60°
Active
70°
35°
25°
55°
problem have no solution, could be a problem during the treatment and the disease prognostic. QUESTIONS TO IMPROVE REFLEXION
Table 1 (F:Flexion; IR:Internal rotation; ER:
Q1: Has your patient any red flag or yellow flag
External rotation; ABD: Abduction)
regarding the physical examination procedure?
STUDENT REFLEXION AFTER P/E I discard the possibility of a visceral and referred pain. The patient doesn’t refer any related symptoms and the radiographs were normal. An important aspect is that she’s ambidextrous. Repetitive movements with her left shoulder, associated with hypothyroidism, could be related with her disease. Passive and active motion limitation makes me think in structural changes in the periarticular structures. These changes could be the results from a combination of an initial inflammation and immobilization (caused by the pain). The positives findings show me that the patient range of motion is affected, and help me to exclude pathologies like cervical radiculopathy and SLAP lesion.
A1: No, there weren’t red flags to perform the physical examination. The yellow flags are the low motivation of the patient about the treatment, the sadness for the absence of his husband and for not being able to perform her hobby and passion. Q2: So far, which is your first hypothesis with the data coming from C/O and P/E? Which is the data supporting this hypothesis? A2:
Her associated disease, the symptoms
change, and particularly the descreased passive range of motion, makes me think in a joint pathology, started with inflammation and then became chronic. I wait the MRI result that can help me to diagnose a specific disease. TEACHER ADVICE There should be findings in these 2 first steps of the clinical encounter that have to correlate
Another aspect to take into consideration is the
among them. As S/E comes firsts, usually points
emotional role in the patient disease. After the
out which areas have to be evaluate in the P/E,
physical examination I can say that there is an
and what should expect to find there. If we don´t
emotional and no only a physical aspect that
find these relationships, we need to keep going
afflict the patient. The patient’s think that the
with new questions and proceedings until we´ll reach a point to make a clinical decision. If there
are not present any severe signs or symptoms we
DAY_1
should continue this assessment into the next
My aims for the treatment are principally
session.
to release the pain and to increase the shoulder range of motion.
PATIENT MANAGEMENT
I
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
mobilizations in all directions. During the
MRI reveals a reduced capsular volume with
pain,
absent inflammation.
mobilization, in all movements, saying
started
with
shoulder
joint
mobilization, the patient refers a lot of especially
in
the
end-range
that she wouldn’t continue with the With this ulterior test and the P/E results I can
treatment.
say that the patient is affected by adhesive capsulitis in the “frozen phase”.
After spending time to reassure the patient, I continue the treatment with a
The symptoms show me that the patient presents a degenerative and chronic disease
soft tissue massage to reduce the stress and relax her.
that started with an inflammatory stage. The first day of treatment ends here. The initial tenditinis, the repetitives movements painting and working, with her hypotiroidism
I explain her that the prognostic could be
problem, could be risk factors of the next
good only if her works actively with me,
shoulder disease.
and that I can understand the pain she feel and can help her.
To have a good prognostic I must work the emotional role of the patient, explain the
At the end, the patient promises that will
following treatment and reassuring her.
try to have a positive role during the treatment.
However, the prognostic should be positive, if the patient follows the treatment with a positive
However, the patient feels very tired and
attitude.
negative and decides to go home.
The plan starts with a progressive treatment, helping the patient to understand her disease and treat it.
39
STUDENT REFLEXION AFTER D1 TREATMENT
motivated. The emotional role of the patient is
The first day of treatment was a disaster. The
her family is an additional drive to carry out the
patient was very negative about the treatment.
treatment.
Pain at end-range in all directions, typical of
M. was more positive and the treatment
adhesive capsulitis, prevented me to continue
continued normally.
very important, and the love and the support of
the treatment in a good way. I
40 I hope she will change her negative attitude. I must insist with the treatment and teach her to understand that the pain is part of the journey toward recovery.
started
with
shoulder
intensive
joint
mobilizations, passive, active and resistive kinesiotherapy. The patient felt pain, but she was able to withstand it. The treatment keep on with shortwave, for about 10 min/session, to increase tissues
QUESTIONS TO IMPROVE REFLEXION
temperature and improve motion and elasticy.
Q1: What do you think that you can do to motivate your patient to keep adherence of her
After one week of treatment the ROM of the shoulder improved of 15 and 10 degrees in
treatment?
flexion and abduction, while in rotational A1: To motivate my patient I can express my
movementes the degrees remain unchanged.
empathy
Anyway the patient was more motivated, than
and
explain
her
the
program
treatment and the benefits of it. The patient
the first day of treatment. (Table 2)
should have, also, the support of her family, helping her to keep adherence to the treatment and feeling motivated.
In the following treatment sessions, I added Codman’s Pendulum exercise for shoulder, to improve ROM and decrease pain; closed and
DAYS 2-4
open kinetic chain exercises, like lean the hand
The following days of treatment were different
against the wall or with a ball against the wall
compared with the first one, maybe because her
doing
husband returned to Madrid, to support her
articular stability, neuromuscular control and
wife. The husband presence influenced the
coordination.
treatment, helping M. to have an active role in the treatment program and to be more
diferents
movements,
to
improve
After 20 days of treatment the shoulder passive ROM improved of 20 degress more in flexion
and abduction, 15 degrees in internal rotation
could be: in a supine position getting the arm up
and 10 degrees in external rotation. The end-
overhead while lying down, using the opposite
range pain decreased in all movements. (Table
arm to holding it; getting the arm to externally
2)
rotate while standing, opening and closenig a door; Internal rotation could be performed using
STUDENT REFLEXION
a towel behind the back, relying on the right
The treatment’s results were good. I think this
shoulder to stretch the affected one.
treatment program is adequately and efectively in the patient presentation. Also, the emotional role of the patient changes and she’s very happy for the treatment and the results.
Q2.Which part of your management do you think has worked better and why? A2: I think the part, which was worked better was the treatment plan, especially from day 2. I planned exercises that could be appropriate for
I am very motivated and satisfied about the
the patient presentation. The anamnesis and
treatment results.
the physical examination helped me to diagnose the patient disease and to produce a treatment
I think that if the treatment will continue in this way, I will be able to improve more shoulder
plan that could be good for the patient. The
motion and decreased pain definitively.
results revealed to me that the treatment plan was good. The ROM increased, the pain
QUESTIONS TO IMPROVE REFLEXION Q1: Do you think that is useful and a good idea to recommend her to do some kind of exercises in her home? A1: Now that she begins to be motivated, I think
diminished, and the patient now is more motivated and can move forward to a symptoms improvement and a better recovery. Table 2 (F:Flexion; IR:Internal rotation; ER: External Rotation; ABD: Abduction)
it’s the better time to recommend her some
P-ROM
F
IR
ER
ABD
home exercises, because she’s more prepared to
After 1 week
+15°
/
/
+10°
keep adherence to the treatment and to have a
After 20 days +20°
+15°
+10°
+20°
Present-day
55°
40°
90°
active role in the recovery. Some exercises 120°
41
FINAL STUDENT REFLEXION This clinical case made a significant contribution in my professional and human growth. I learned to have empathy with the patient. It’s important to help the person also in her emotional issues. At the beginning was complicated to analyse the patient’s symptoms, but with the physical examination and the tests I was able to diagnose the disease. The emotional role of the patient had an important influence during the treatment.
42
I learned that the family and psychological support is very important for the patient, especially in patient with a long-term disease. The treatment results makes me think that I had plan a good treatment program for the patient, although still have a long way to go before she can be considered completely cured. REFERENCE LIST 1. Sardella White, S., & Garbe, J.R. (2010). Thyroid Disease: Understanding Hypothyroidism and Hyperthyroidism. Boston: Harvard Medical School. 2. Oliva, F., Berardi, A.C., Misiti, S., & Maffulli, N. (2013). Thyroid hormones and tendon: current views 3. and future perspectives. Concise review. Muscles Ligaments Tendons J, 3(3), 201-203. 4. McFarland, E. G., & Kim, T. K. (2006). Examination of the shoulder: the complete guide. Thieme.
A 45 YO. GARBAGE COLLECTOR WITH CHRONIC BACK SYMPTOMS JAVIER SIMON M. AND GUIDO R.
INTRO My reflective clinical case is about a 45 years old male who has pain in the cervical region, lumbar region and dizziness, didn’t suffer any direct trauma, may be related to his job,
I asked him what could be the consequences of his symptoms and he told me that his job as required gain weight because it was operator of garbage. When he described his work he commented that it was not at all satisfied.
garbage collector. The symptoms could be
He commented that did not perform any
related with a slipped disc (medical diagnosis),
hobby or sports, which can lead us to think that
and may be with other aspect like mood.
their emotional level is low, because if work
SUBJECTIVE EXAMINATION
does not satisfy you and no activity that does.
The first day the patient came to the
The most relevant symptoms was neck pain,
consultation derivative of general medicine
back pain, pain in the chest area and tingling in
with sick leave.
superior limbs. Because these symptoms were chronic, he told me that he had made some
My first impression of the patient was a sad and worried person, as he sat in the waiting room without speaking to anyone. When he started to talk to me, commented that he was married and lived with his wife and
treatments before, as Pilates, and private physiotherapy, he improve a bit, but the symptoms did not quite disappear. He hadn´t pharmacological treatment, nor had any personal history that might be related.
son. Only had a family history of osteoporosis and He had pain in the cervical and lumbar from
arthritis.
several months ago. The patient described the pain as annoying, with tension and sometimes
The patient described the pain in the morning
radiated.
with a 9/10 on the VAS scale decreased throughout the day up to 5/10.
One thing that struck me about his pain was that it hurt in any position and any movement.
43
I decided to return to this sphere during and after the physical examination (P/E). QUESTIONS TO IMPROVE REFLEXION Q1: What kind of chest pain he felt and during which movements he felt it? A1: This pain was produce by a antalgic posture,
44
in the physical examination I found that the Pectoralis minor muscles was shorted and had active Miofascial trigger points, and in the visual examination the shoulder was in internal rotation. STUDENT REFLEXION AFTER S/E About my initial hypotheses the symptoms are
I know it, because he felt pain in the stretch and palpation of these muscles.
related with the medical diagnosis, but I think that are something emotional that has been
Q2: Is there any red flag in the history you have
influenced in the perpetuation of it.
to rule out first?
I don´t think that could be related with arthritis or osteoporosis because in the medical test aren´t any signs which has any relation with
A2: No there isn´t any red flags. I can consider a yellow flag the emotional feels of patient and the relation with the pathology.
patient´s symptoms. Q3: So far, which is your guess about the At that time I did not consider the patient's
relationship between the main symptoms?
posture, but because of the knowledge acquired in other subjects this year I could associated to a string anteromedial (AM), which is related to the emotions. This is the representation of the body posture explained by Godelieve Denys-Struyf, and this string could be related with some symptoms of areas of our patients. (1)
A3: In my opinion the symptoms are related with medical diagnosis, because the pain causes by the disk alteration, has provoke some compensation that development other symptoms of patient.
TEACHER ADVICE
deviation 35º and extension 50º movements of
Relationship among symptoms often provides
the trunk, and right rotation of neck 45º.
clues about irritability, severity, and spreading pattern. Drawing a timeline introducing the starting point for signs or symptoms and their evolution, also help us to focus over one area instead of others, as the source could be the same for example.
About muscle balance he didn´t have any alteration, only the shorted Pectoralis minor muscle. And active Trigger point of Trapezius, paravertebral, lumbar quadrate muscles and psoas.
45
Sometimes, the pain in the former presentation
Other test that I realized in lumbar region was
hasn´t to be the most relevant nor the origin of
thumb-ascending test; Gillet test (2) and
the syndrome.
elasticity test and I observed an anterior
PHYSICAL EXAMINATION After know the medical diagnosis, how patient
torsion of the sacro. In dorsal region I realized the Mitchell test (3) and I found a FRSd in some vertebras.
felt his symptoms, I startet with physical examination.
I too realized Adson, Eden and Wright test to kwon if patient had any vascular alteration,
Firstly I did a static inspection, where I
and this test was negative. (2)
observed a little vascular alteration under pectoral fold.
STUDENT REFLEXION AFTER P/E
So I asked him if he had any visceral alteration
Analyzing the information got from subjective
because this could have a relation with the liver
and physical examination, I think that
or stomach.
symptoms are related with that pathology, because of hernia disc and protrusion, he
His posture was important to analysed
started to felt symptoms, and went changing
because represented AM string, antalgic
his
flexion and right lateral deviation of the trunk,
compensation that activate Trigger points,
internal rotation of shoulders, flexion of neck
and decrease the activity of some muscles.
posture.
This
could
cause
some
and extension of head. But maybe the posture was the responsible of Secondly I did the functional inspection, and I
the hernia disc, because bad posture of
found an articular limitation of the left lateral
vertebral bones, cause an alteration on disk
pressure and this could the reason of patient
Q2: So far, which is your first hypothesis with the
alterations.
data coming from C/O and P/E? Which is the
In the physical examination I hadn´t performed
46
data supporting this hypothesis?
a neurodynamic test because I didn’t know
My first hypothesis is hypertonicity because of
how to do it in this moment. After one year, I
he presents Miofascial trigger point, in my
have learned the importance and how to
opinion, activated by a bad posture and stress.
realize this test to patient how present symptoms like tingling.
The data supporting this hypothesis is the presence of Miofascial trigger point in the
So maybe I lost some important information,
palpation that reproduces his symptoms and
to plan the treatment.
the information that patient give me when he
But in this clinical case, I keep thinking that symptoms are very related with emotional state of this patient.
felt pain (for example when he has to gain weight or when he is sitting are related with a nociceptive pain). TEACHER ADVICE
QUESTIONS TO IMPROVE REFLEXION Q1: Do you think that could be useful before start or during the physiotherapy treatment, to help the patient with a psychological support by an expert? A1: In my opinion is a good idea, because our principal objective with all patient are a biopsychosocial treatment, so sometimes this must be multi-disciplinary treatment that in
Our findings during the P/E have to be meaningful for the patient. A positive finding of an unknown dysfunction or pain could lead us into a wrong path if it´s not related with the general presentation. Usually if it is found in first place of the examination. We have to check if this pain is “the kind of pain that the patient used to feel” and is related with his other main complains.
this case. But I found difficult to give patient advices about pay attention to a psychologist or other therapy to changes his mood.
PATIENT MANAGEMENT DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN After analysed the information getting in the subjective
examination
and
physical
examination my diagnosis is that patient disc
herniation, he has hypotonicity in the posterior muscles of the trunk and shortening in
STUDENT REFLEXION AFTER D1 TREATMENT
Pectoralis and Psoas.
After first day, patient presented the same symptoms and the dizziness increased.
The prognosis is positive but has some negative factors like the pathology because it,
Maybe I should choose other technique that
is irreversible without surgery treatment, the
weren´t trust technique.
chronicity of symptoms and the laboral activity. Positive factors are that after others physical treatment he has improves. The plan that I design was to address the following objectives:
Firstly in a short-term the objective
So he had more pain the second day, so I decided to do a more relaxed session applying TENS and magnetic therapy. So after this day I learned to give more importance the mood of patient before choose any technique.
was decreased pain in cervical and
lumbar region.
QUESTIONS TO IMPROVE REFLEXION
Secondly to medium term was to
Q1:
increase ROM at cervical region and
manipulation?
strengthen in posterior and anterior
A1: I did manipulative techniques in order to
muscles of thorax.
get the neurophysiological changes produced
DAY_1 First day I started with an osteopathic manipulation, for the dorsal region I used the “Dog-technique” and for the sacro and lumbar region I did the “lumbar roll”. To decrease tension I did a technique to relax
Why
did
you
chose
osteopathic
by these techniques. It is sought to give a stimulus to restore the SN information about the area and get so hypoalgesia short-term changes in the structures that could be affected (4). DAYS 3-4
diaphragm and other for the Pectoralis minor
The third day my patient had lumbar and
muscles that was a muscular energy technique.
cervical pain; he felts bad and told me that he had have vomit. So I decided to do a relax treatment with manual therapy, the fifth day I did the same treatment.
47
Sixth day the patient hadn´t tingling, the
hypotheses of has a relation with the mood
dizziness had been decreased, cervical pain
my patient.
had been improved but he kept feel lumbar pain.
48
In spite of I recommended him to did some active exercise to make more powerful the
So, for this session my objective was treating
back and deep muscles, because I think that is
the lumbar pain. I used a technique to relax
very important to have a good motor control
diaphragm, I did a compression treatment for
of the lumbo-pelvic region, to decrease the
Psoas Trigger points, contract-relax stretching
back symptoms.
for psoas and a active work for the deep lumbar muscles (Transverse muscle, pelvic floor and
QUESTIONS TO IMPROVE REFLEXION
Multifidus muscles).
Q1: Do you think the patient disease could be related with neurological disorders in addition to
STUDENT REFLEXION I hadn´t the final information before the patient end the treatment but while I was treat it, he had some improves like dizziness and headaches, but the outcomes after each day aren´t very representative because each day had different symptoms, I mean one day he was better of the cervical pain and worse of the
his emotional state? I think that there could be some present peripheral entrapment because I didn´t neurodynamic test and he present numbness in the arm, but he didn’t have any entrapment of Braquial plexum because the Jackson, Adson, Eden and Wright test, were negative.
lumbar pain, and the next day on the contrary,
Q2: Which part of your management do you
so the evolution was very confused.
think has worked better and why?
For me was difficult to interpreted which was
In my opinion the best treatment for this
the problem of patient´s symptoms because
patient was the relax technique a motor
the evolution was very different and when he
control (“rana al suelo” (5) adding a good
improve one symptoms get worse other and
breathing movement to relax diaphragm) and
vice versa.
manual
So I think that I have left loss some information. Maybe I was in a wrong way or this development had relation with my first
therapy.
Because
the
active
participation of patient to get a good control motor in the lumbopelvic region, and being aware how he is relax while he gets control the breath, helps him to get better results.
And the manual therapy at the Trigger point
good decision. Regarding to the neurodynamics
helps to decrease the symptoms and the
issues, we need to discriminate among tests
muscles tensions.
assessing roots, nerve trunks and main nerves.
TEACHER ADVICE
We also have special test to investigate where
Choosing high evidence-based tests will add to your reasoning better ingredients to make a
the entrapment is and its dimension, first step in the management of these presentations.
49 FINAL STUDENT REFLEXION
To conduct further analysis of this case, after a year in which I have acquired new knowledge, has helped me to realize that parts of the exploration had not taken into account and the importance of them such as neurodynamics, spinal mobilization with postero-anterior pressures, the patient's posture that can give us information of structures that are influencing their pathology. For example, in this case with an AM chain, I could choose treatment techniques and address the same depending on the patient, such as given the mood of the patient would have been better to make more moderate techniques: muscle energy techniques rather than with impulse techniques. And remember at all times the importance of the biopsychosocial treatment as in the recovery of the patient and their adherence to treatment is influenced by many factors. And some time that is necessary to do a multidisciplinary work. This has helped me to make a more complete reasoning and relating and integrating more different fields of physiotherapy I've been studying
REFERENCE LIST 1. Lucas, E., & Ángeles, M. (2009). Análisis biomecánico de las algias de raquis y su relación con la percepción del dolor y la calidad de vida. REDUCA (Enfermería, Fisioterapia y Podología), 1(2). 2. Cleland, J. (2006). Netter, exploración clínica en ortopedia: un enfoque para fisioterapeutas basado en la evidencia. Masson. 3. Ricard, F. (2007). Tratamiento osteopático de las algias del raquis torácico. Ed. Médica
Panamericana. 4. Pickar, J. G. (2011). Efectos neurofisiológicos de la manipulación vertebral. Osteopatía científica, 6(1), 2-18. 5. Souchard, P. E. (2005). RPG. Principios de la reeducación postural global (Vol. 88). Editorial Paidotribo
50
A 23-YEAR-OLD FEMALE PREPARING FOR ARMY WITH LOWER BACK PAIN FOR 4 WEEKS KRIIK G. AND PONCE L.
INTRO My client was a 23-year-old female student with lower back pain, which had started 4 weeks earlier due to heavy weight training.
where she wasn’t able to put on shoes in the locker room when leaving the gym. After this the pain had been troubling her especially on the left side of the back. Also a tendon had started snapping on her right hip.
SUBJECTIVE EXAMINATION My client was a 23-year-old woman who was in the second year of her studies in the field of physical therapy. She was living together with her boyfriend who was studying in the military academy, and it was her goal to join the army too. Due to lower back pain resulting from extensive training she came to the clinic. Her aim was to get back on track with training again soon, because the entrance test for military studies was a few months away. She was 165 cm tall and weighed 52 kg. She hadn’t had former traumas
She had tried to relieve the pain by stretching and trying to find a painless position. During the day sitting worsened the pain, and sitting through a lecture at the university was agonising. Because of this she had started to attend the lectures standing up. At home she had exchanged the sofa for a fitness ball. The pain was most severe in the evenings and after sitting down for a long period of time. Lying down eased the pain. She had found sleeping on the side with a pillow between her legs the best position for her.
associated with the pain. During her free time she was involved in many My client had started a comprehensive weight training program a few months earlier in order to pass the entry tests for the army. A month ago she had started to experience lower back pain after training. Two weeks before coming to the clinic the pain had been intensified to an extent
kinds of activities: walking her dog, going to the gym, swimming and at times also climbing. At the gym she usually trained with free weights together with her boyfriend. They trained at a “men’s gym” without contemporary adjustable gym equipment.
51
At the gym the most pain inducing exercise was
QUESTIONS TO IMPROVE REFLEXION
deadlift, which she usually did with 20 kg weights
Q1: So far, which is the level of severity and
3 x 10 repetitions. She said that she knew she was
irritability of her presentation? How is this going to
executing
impact on your plan for P/E?
performing
the a
movement squat
wrong
deep
without
enough.
She
recognized that also in her everyday life she was moving in unfavourable ways by having a habit of
52
not bending her knees while picking things up from the floor. She suspected that she had been engaging with a training program too hard for her fitness level, because she was training at the same tempo with her boyfriend.
A1: At the time of her therapy session the severity of the pain had been decreased to a level where it presented moderately in certain positions and movements. The pain affected her movements, activities and behaviour and in order to begin the healing process I felt it was extremely important not to irritate it any further. Thus I planned to be careful with the physical
STUDENT REFLEXION AFTER S/E
examination in order to avoid provoking excess
Based on the interview and her description of the
pain.
onset of the pain I suspected a disorder in
Q2: Do you think she should rest and stop lifting
neuromuscular control in the core area. My
weights?
hypothesis was that she was training with weights too heavy for her level of fitness and
A2: Yes, in order to recover she should rest for a
technique, and while she was performing the
sufficient amount of time, and afterwards
deadlift her back extensors failed to uphold her
gradually get back to weight training.
posture, resulting in a flexion in the lumbar spine,
Q3: Did you think about other forms of getting
and creating an increased torque that caused
prepared for the army?
significant pressure to the intervertebral discs and extreme tension to the surrounding tissues.
A3: She should train by doing versatile exercises. Because she already had a good selection of
I sensed that there was pressure for her to get
other physical activities she was engaging in, I
back on track to the training routine, and thus I
especially wanted to give her an alteration for
expected a challenge in motivating her to
weight training.
patiently commit to the therapeutic exercises. TEACHER ADVICE The degree of irritability and severity will drive the deepness of the P/E procedures. If we are not
cautious, a tough physical testing could ruined the
In the forward flexion the lumbar spine rounded
remaining management if we provoke elevate or
only at the end of the flexion, and up until that
severe symptoms in a highly irritable presentation,
point it was almost completely straight. In the
that avoid proper and comfortable following
modified Schober test lumbar spine lengthened
procedures.
in forward flexion 6 cm while standing and 5 cm while seated - which is within the reference
PHYSICAL EXAMINATION Day1: I started the physical examination by assessing my client’s posture and active movements.
values, but in the low end. Especially in the first forward flexions she conducted there was a visible functional scoliosis present. Her body also flexed to the right side, over her right lower extremity.
Her ankles were in line and in her feet she had symmetrical and strong longitudinal arches. There was no pronation in the ankles. Knees were slightly asymmetrical: the right ham was slightly lower than the left one. Also the right gluteal fold was a little lower than the left one. The iliac crests were horizontally aligned. Knees were directed to the back into a locked position and the pelvis had drifted to the front and tilted anteriorly. In the lumbar spine she had a normal lordosis but the kyphosis in the thoracic spine had straightened. Scapulae were symmetrically aligned, both by their distance from the spine and the height of their position. However the scapulohumeral rhythm was slightly asymmetrical: the right scapula moved smoothly but the left one did the same abruptly. In the cervical spine she had a normal lordosis.
Lateral flexions were symmetrical and the spine flexed evenly. Lateral rotation to the right was smaller than to the left. Single leg squat revealed larger weakness in the right gluteus medius than in the left one. On the right side in the anterior part of the hip a tendon was snapping as she flexed her hip. In the movement control test for the core there was no lack of control present. However, as a physical therapy student she did know what this test was about and perhaps was able to concentrate to not show positive signs. In the Straight Leg Raise Test her left leg raised smoothly over 90° but the hamstrings in the right thigh started to strain at 90°. In the Thomas Test there was no tightness in the iliopsoas muscles presented. According to palpation during a single leg hip raise the transversus abdominis muscle activation was slightly stronger on the left side than in the right side.
53
As first aid for her condition I gave her advice
medius
about a painless position. I also advised and
quadratus lumborum was not painful. While
encouraged her to actively keep up a better
conducting a stretch to the muscle, there was no
posture in which her lower back is not under
tension present and the stretch was symmetrical
stress.
on both sides. By palpation the lumbar spine was
There
During
palpation
m.
more flexible than the thoracic spine. The tonus
Day 2:
54
weakness.
in the back extensors was symmetrical in were
aspects
that
needed
closer
transversal manipulation.
examination and due to lack of time were not examined during the first session, so I decided to
STUDENT REFLEXION AFTER P/E
make a few more tests to confirm the most
My initial hypothesis during the first therapy
accurate diagnosis and management.
session was that she had a disorder in neuromuscular control in the core area. However
During the second therapy session there were no more signs of functional scoliosis present in forward flexion. It is possible that the muscle tension present before had loosened and did not pull the spine into an asymmetrical position. Lateral flexions and rotations were symmetrical. While squatting m. transversus abdominis stayed active and the lining of the knees remained. In the single leg squat m. gluteus medius failed on both sides. In forward flexion the movement of SI-joints was symmetrical. However the left side of the hip raised while raising the left knee, while the hip stayed in place when raising the right knee. There was no pain when compressing the SI-joint.
when she didn’t present any positive signs towards the lack of control, I had to change my presumption. In our first session we had gone through different factors in the core area, but did not have time to profoundly examine the pelvic area. That is why I decided I needed to conduct more tests in the second session. Between the sessions I had gone through numerous options which could be the cause for her pain, and expected to come into a conclusion after better examining her pelvic area and movements. Before the management phase I put a lot of thought into how to make therapy appealing to her. I felt like I had to balance between exercises that were not too difficult for her in order to
In the Straight Leg Raise Test hamstring stretch
maintain the right load and the therapeutic
was symmetrical and no tension presented. In
aspect, but also challenging enough for her to
the Donatelli Drop Leg Test the leg dropped ~10
stay motivated.
cm on both sides which refers to m. gluteus
QUESTIONS TO IMPROVE REFLEXION
TEACHER ADVICE
Q1. Which is the most important piece of data
No general advice could be provide to choose the
supporting your hypothesis with this patient?
most relevant information in the P/E. It has to be a
A1: The most important piece of data was the muscle imbalance presented by her poor posture and the evident weakness of her gluteus medius muscles combined with the information about the high intensity of her training and her unstable technique. Q2: Do you think she has a preference for the right
personal decision that could be shared with the expectations and feelings of the patient. Your experience and knowledge will drive you to this part of the decision-making after performed the
55
best evidence-based tests procedures. PATIENT MANAGEMENT
side of the body at the moment she performs the
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
movements and that it makes it stronger than the
My physical therapy diagnosis was that the client
left one on the lumbar rotation?
suffered from an unbeneficial habitual posture
A2: Based on the observations and tests I believe she has a habitual imbalance in her posture - and during heavy weight training the weaknesses in certain parts of her body have provoked an
caused by muscle imbalance, and muscle tightness and weaknesses in the pelvic region, which in high intensity weight training provoked pain into the lower back.
increasingly unbeneficial posture. Her posture
The objective for therapy for her was to correct
includes dominant elements in both right and
the posture and to learn proper movement
left side of her body, but they are unsymmetrical.
control and right movement trajectories in order
Q3: What do you think you could do to avoid her not showing the positive signs of the test you asked her to perform? A3: If she is very aware of the tests and her
to be able to train with weights. After the first physical therapy session the aim was to locate a painless
position,
avoid
pain
provoking
movements and to start practicing the right kind of posture.
performance, it could prove beneficial to ask her to describe in detail if she feels weaknesses or if one movement is harder than the other. Asking her to talk could also make the movements more natural and intuitive.
After the second therapy session the objective was to strengthen the deep postural muscles and to learn a deep, relaxed way of breathing during exercise. In order to reach a strong posture gluteus medius muscles had to be strengthened.
In the early stage of therapy the aim was to cross-
These exercises she was to do with every training
strengthen the core muscles in myofascial chains
session in order to learn to sustain core activation
both in the anterior and posterior side of her
when functioning.
body.
56
In the advanced stage of therapy the goal was to
2. EXERCISES TO STABILIZE PELVIC REGION
enable weight training. The objective was to
In order to stabilize the pelvic region I gave her
comprehensively train the musculature starting
exercises to strengthen the gluteus medius
with simple technique exercises and moving
muscles.
onto wider trajectories.
-
stepping board (3 x 10 on both sides)
In order to develop a strong muscle control I gave my client exercises to strengthen her postural
lifting the hip while standing on a
-
lateral rotation of a flexed lower limb
core muscles. In order to correct her posture I
while lying on the side (3 x 10 on both
taught her an optimal position for knees and hips,
sides)
and to stabilize her pelvic area I gave her
-
abduction of the foot while standing -
exercises for strengthening gluteus medius. In
first without a resistance and later using
order to keep her motivated I composed a
a rubber band (3 x 10 on both sides)
therapeutic training program for the advanced stage so she could witness her own improvement and not get bored with a lack of options. 1. EXERCISES FOR DEEP CORE MUSCLES To strengthen the activation of postural core
In order to keep the therapeutic training interesting and appealing she was able to choose an exercise for each session. 3. EARLY STAGE In the early stage I prescriber her
muscles I instructed her following exercises: -
vertically pulling down and bouncing a rubber band (m. transversus abdominis) (10 sec activation + 10 sec rest)
-
-
-
crossover crunches (3 x 10 on both sides)
-
by turns lifting up one hand and the opposite leg on all fours (3 x 10 on both sides)
moving the body weight onto a foot stepped forward, walking backwards
4. ADVANCED STAGE
(mm. multifidi) (5 times on both sides)
I advised her to conduct the early stage exercises
relaxed and deep breathing when
as long as she had fully learned the movements
exercising (diaphragm)
and the postural control was stable. When she
would have mastered them she could move on to
shape than before, and also to keep her
more challenging exercises. This way her training
motivated and committed into. We agreed with
was as progressive and motivating as possible. In
her that she will incorporate these exercises into
the advanced stage I gave her following
her routine and exercise independently, and
exercises:
after 6 weeks, during a follow-up contact she had
-
pulling down across to the front a pulley while crunching the opposite knee up (3 x 10 on both sides)
-
pulling down across to the back a pulley
been able to start training again with a better technique and a clear knowledge about the required movement control.
while extending the opposite leg back (3
STUDENT REFLEXION AFTER TREATMENT
x 10 on both sides)
Because my client was an active young woman
I advised her to start the advanced exercises with small resistance and moving onto heavier weights while paying strict attention to her condition and movement control.
with a concrete goal in her weight training, I didn’t want to solely give her exercises for the early stage, because she might have found it boring it could have resulted in her not sticking to it. I wanted to build a bridge between her state at
5. ALTERATIONS FOR DEADLIFT
that time and the stage she wanted to be in. I was
Because deadlift was a movement she was fond
concerned whether I was able to give her all the
of, I wanted give her an alteration to make it
information and support she needed to
possible for her to safely train the muscle groups
independently conduct the therapeutic exercise
that the movement incorporates. With the
process.
alteration she would be able to train the same muscles but in a safe and technically more simple
QUESTIONS TO IMPROVE REFLEXION
way. I instructed her:
Q1: Which part of your management do you think
-
-
squat (3 x 15), and possibly later a
has worked better and why?
telemark-squat (3 x 10)
A1: Based on the feedback I received from my
rowing both bilaterally and rotating the
client after her therapeutic practice period, the
trunk
core as well as m. gluteus medius strengthening
This progressive therapeutic exercise plan aimed to return her into the training routine in a better
exercises have proven to be the most beneficial for her. Once she was able to support a firm posture she avoided provoking pain even in
57
complicated movements. A strong core has given her the possibility to enjoy life without pain.
TEACHER ADVICE As we read previously patients’ needs to have a general idea about the length of the treatment.
Q2: What about the recovering time? Did you have
Information about this point could be found in
an idea about how many weeks the treatment
clinical reports for individual patients. Despite is
would take long?
not one best researched issues in physiotherapy, there are some populations in which these findings
58
A2: I estimated it would take her 3 months to reach the advanced level in practicing if having successfully undergone the therapy.
are extremely urgent and relevant, for example in the
professional
sports
area
where
time
constraints costs lots of money to the clubs.
FINAL STUDENT REFLEXION In order for her to properly learn the optimal movements I started the therapy plan with low-intensity training (Kisner & Colby, 2012). Especially with patients with lower back pain it is important to render activation in the deep postural muscles such as m. transversus abdominis and mm. multifidi. By increasing the activation of m. transversus abdominis the risk of generating lower back pain decreases (Miura et al. 2014). Because of this I included stabilizing exercises into every training session of her plan. In her case it was also extremely important to strengthen m. gluteus medius, which is a stabilizing muscle for the pelvic area. I chose exercises that have been proven to be the most effective in creating muscle activation in m. gluteus medius. (Bolgla & Uhl, 2005. Gowda et al. 2014.) In my opinion she comprehended the instructions well and also was committed and eager to execute the plan of therapeutic exercises. I was glad to hear her positive feedback later and excited for her recovery.
REFERENCE LIST 1. Bolgla, L. and Uhl, T. (2005). Electromyographic Analysis of Hip Rehabilitation Exercises in a Group of Healthy Subjects. JOSPT Journal of Orthopaedic & Sports Physical Therapy. 2. Gowda, A., Mease, S., Donatelli, R., Zelicof, S. (2014). Gluteus medius strengthening andthe use of the Donatelli Drop Leg Test in the athlete. JOSPT Journal of Orthopaedic &Sports Physical Therapy.
3. Kisner, C., and Colby, L. (2012). Therapeutic Exercise. Foundations and techniques.. 4. Miura, T., Yamanaka, M., Ukishiro, K., Tohyama, H., Saito, H., Samukawa, M., Takumi Kobayashi, T., Ino, T., Takeda, N. (2014). Individuals with chronic low back pain do not modulate the level of transversus abdominis muscle contraction across different postures. JOSPT Journal of Orthopaedic & Sports Physical Therapy.
59
A 40 YO. MAN WITH A PAINFUL SHOULDER SYNDROME PÉREZ G. AND KRIIK G .
INTRO
60
A 40 YO man, who handle Remotely Piloted Aircraft Systems (RPAS), in Mexico, which has a
as soon as possible to return to his daily activities. He is married and they have 2 girls with who wants to play again without pain.
painful shoulder syndrome on both sides, as a
He said that the pain on his shoulders started 2
consequence of many years working at the same
years ago but he only felt kind of discomfort and
position by long working hours.
he didn´t attended it, along of time he feels only
SUBJECTIVE EXAMINATION One day a 40 YO man, with 40 years old came to the clinical rehabilitation where I was doing my practices. He was 1.78m tall and 89 kg of weight. He handles a Remotely Piloted Aircraft System (RPAS) for a company in Mexico, almost always Monday through Saturday 8 hours with an hour of break, but he was handles the drone for 3 or 4 hours with the same position without any break to stretch or eat either. He describes his position as a super video game player, stand up, arms down, elbows 90°, and loading the control with 2kg of weight.
got worse and neurological symptoms on his arms on few times. He has token NSAID, muscular relaxants & hot water fomentations, 3 weeks felt kind of better, but 2 months later the discomfort begun again harder and his wife carried him to the doctor because the pain increase each time more, presented swollen shoulder and red zone, and sometimes cannot work but he only said ¨it will pass, I´m ok! ¨. They went first with a public doctor, where he has the insurance and take a Rx to see the acromion position, and it was good, but he said the doctor´s
diagnosis
was
¨Painful
Shoulder
Syndrome¨. Then, he went to the traumatology,
He is working on that place since he was 20 years
and he said to him the same diagnosis.
old. He had taken a course for pilot the drone to
Consequently, the doctor gives to him medical
begin work, and a long of time he has been
prescriptions to decrease the inflammation and
updated until nowadays. He was born and grew
pain, relax the muscles and the numbness
up in Mexico, he´s very sympathetic, funny,
disappears, and furthermore sends him to begun
friendly, simple, positive and waiting to recover
with physical therapy sessions.
His pain becomes chronically because he didn´t
test maybe as 1UNLT & 2UNLT to be sure that he
attend at time and at the work give to him some
hasn´t any nerve entrapment.
days to rest.
He has a good prognosis because he is very
He smoke occasionally like 1 cigar each weekend
motivated and anxious to recover full ROM to
and was an occasional social drinker.
return to his normal life, he has a very positive
He presents pain on abduction, extension, flexion (less pain with elbow flexed than with elbow extended), internal and external rotation, but in adduction he doesn´t present pain. At the
attitude and perseverant. QUESTIONS TO IMPROVE REFLEXION Q1: Which were the activities that ease his symptoms?
same time he has several limited range of motion. He presents a lot pain when try to hung out his
A1: When he applies a thermal compresses, and
clothes on the closet, brush his hair, take a
when he rested a day or two of work.
shower, dress and every activity that implicate put his arms up. He feels better when his wife put to him socks with hot rice on his shoulder. STUDENT REFLEXION AFTER S/E
Q2. Which is your opinion about central sensitization component in his pain presentation? A2: I think the main component on his pain is the muscle
overload
that
causes
a
chronic
inflammation without care on time.
About my hypothesis is a mechanical input injury,
Q3: Does he have identical pain in both of his
with possible tissue damage. He has a lot of time
shoulders? In his work, did he usually do the same
with the pain, so it comes to be a chronic disease,
task with both hands?
it could be slower to recover than a acute pain. He didn´t receive any therapy from a specialist, only the home remedies that calm a little the pain. My first impression at all was a big contracture of upper limb, back and neck. First of all, I could do explorations to verify which muscle is more damaged, and to neurological
A3: He doesn’t have the pain as a specific point he feels pain around shoulder and neck. Furthermore, he used to do the same with both hands (take a motor control). Q4: Is possible for him to work shorter periods or take a break? A4: He said that is not possible to make a break because when begin to record is hard to pause it.
61
any inflammation about bursa. And finally he
TEACHER ADVICE It´s important to cover, at least, the main issues in
refers more pain at night.
the first visit to allow you to manage all the pieces of the quiz. Missing key issues as red flags could decrease the quality of your management and set
STUDENT REFLEXION AFTER P/E About the diagnosis of doctors, I found that he has the muscles inflamed and whichever
your patient in risk
movement that he did, he presented pain,
62
PHYSICAL EXAMINATION
consequently very limited his range of motion.
He brings radiographies and the acromion
Although, he said he begun to feels better with
doesn´t indicates a possible impingement. He
de NSAID´s he want to be all right as soon as
doesn´t have a specific point with pain on his
possible. I found same kind on limited on
shoulders, so I decided realize test for the rotator
external and internal rotators (as subescapularis
cuff muscles and examine his ROM and posture.
and Infraespinatus), and on muscles as that have function of flexion, extension, abduction, the
He presents head anteversion, winged shoulder
right side has more restriction, but in adduction
blades and a little left side descending.
the rom wasn´t limited just at the end present
The range of motion on left shoulder:
pain. I think he has more restriction on his right
-Flex (L / R) 45°, 40°
shoulder because his dominant hand at business
-Left ABD (L / R) 40°, 35°
is right side, so it overloads a little bit more the
-Add (L / R) 30°, 32°
muscles. Moreover, all the test he present
-Ext (L / R) 35°,30°
positive because he continues with inflammation
-ER(L / R) 40°,40°
and overload muscles for his work , tension
-IR (L / R) 40°,40º
position and those are contributing factors. He present very good attitude and that have good
On Jobe`s test was positive both sides, Patte´s
prognosis with NSAID and therapy he going to
test was positive (same on both sides),
belly
recover but exactly I don´t know the time.
press was positive, Gerber was positive (same on
Moreover, he doesn´t presents an anatomical
both sides), Yergason was positive too (more
deformation of acromion, just muscular so it
limited on his right side). I did Neer and
becomes better for his luck.
Hawkins`s tests too, Neer was positive on both sides, but Hawkins was negative. Furthermore,
QUESTIONS TO IMPROVE REFLEXION
on the radiographies can observed that has not
Q1: Did you advise a painless position for him?
A1: He has painless when he has his arms down.
TEACHER ADVICE
Q2: Was he still working at the same time of
Getting the most reliable tests for a typical
therapy? Do you think it´ll affect your work
presentation is the key point to get a chance in
strategy?
discovering a tissue dysfunction.
A2: He continues working fewer days and fewer
PATIENT MANAGEMENT
periods of time. I think it can make slowest rehabilitation but not totally affect. Q3: Which is your second hypothesis for the data coming from P/E? Shoulder bursitis. Which is the
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN About the diagnosis of the doctors and my point of view I met consistent findings about the painful shoulder syndrome. I had doubt then with
data supporting this hypothesis?
shoulder bursitis, because the impingement Shoulder bursitis is include the alterations of
shoulder was rule out with the radiographies, but
muscles, tendons, nerves, tendon sheaths, joint
on the radiographies has not appeared.
syndrome and neurovascular entrapment and
Furthermore he made MRI and only has
more pain at night. He has pain on all
appeared inflammation of tendons. I think he
movements
as
was good because he doesn´t present any
radiographies and magnetic resonance can rule
neurological symptom last 3 months, and he is
out impingement and bursitis.
more relax on his work and his wife is supporting
Approximately 10 % of the general adult
him, physical and psychologically.
and
with
the
studies
population experiences an episode of shoulder pain in your life (Van der Heijden, 1996) shoulder pain is the third leading cause of muscle skeletal pain extends to shoulder and back (Cailliet, 1981) .The risk that the pain persists beyond acute phase seems to be related to lack of treatment, and occupational personality factors (Van der Heijden, 1999).
The plan to reduce inflammation with help of the doctor
and
some
NSAID´s,
and
TENS,
thermotherapy, relax and therapeutic exercise. DAY_1-2 Applied TENS on his shoulders and furthermore thermotherapy with hot-wet compresses at the same time to release the pain and relax the muscles, then applied ultrasound on the area with more pain. Then told to him that he should relax for all day and don´t do any heavy work. And on the afternoon he applied an NSAID on gel.
63
STUDENT REFLEXION AFTER D1 TREATMENT
on 3rd and 4th days added pendular of Codman
The patient came with a doctor prescription. And,
mobility and muscular potency, and decrease the
he feels better with thermotherapy, so it can
pain.
exercises, and laser low potency to improve the
helps to relax the muscle and psychologically too.
potency, massage and finally 2 repetitions on
QUESTIONS TO IMPROVE REFLEXION
64
5th: add pendular Codman exercises, laser low
Q1: Did you give him instructions on how to relax
finger ladder on flexion and abduction.
his muscle at home-other than NSAID? STUDENT REFLEXION A1: only the pendular exercises.
The patient was happy because he feels his
Q2: Did you have an estimate on how many therapy sessions it would take to improve
shoulder been better and won ROM con 4 sessions. Moreover, his attitude was so positive on therapy and on house because obey all
Roberto´s state?
instructions. Furthermore, he and would gladly A2: I think near of 15 sessions.
therapy because he spoke with more people, so I think that psychologically these attitudes are
TEACHER ADVICE
best for speedy recovery.
A “test-treatment” will allow you to get invaluable information
about
the
condition
of
the
presentation. Using the results of the treatment as another piece of evaluation could inform you how to treat your patient properly. If we use a huge
QUESTIONS TO IMPROVE REFLEXION Q1: Have been your management different if you didn´t have the MRI images? Were they valuable for your results?
number of techniques in this first session, we will be less sure about which has worked better.
A1: Yes, because if we had found any abnormality as a rupture of rotator cuff, bursitis
DAYS 3-5
or even a tumor should be care with those things.
For days 3, 4 and 5 applied, TENS on his shoulders and furthermore thermotherapy with hot-wet compress at the same time to release the pain and relax the muscles, then applied ultrasound on the area with more pain. Moreover
Q2: Would he only continue his treatment at home? A2: He continues with the therapy on the clinic, but I kept giving no therapy because I was moved to another patient.
FINAL STUDENT REFLEXION All the clinical case was with help of my coordinator of practices, although we add some therapies methods. But here I would like to improve on the physical examination explore the neurological examination,
Daniel´s
scale
(muscle
strength
power).
With the treatment can be helpfully to his body but a placebo effect can be influent too. The treatment in four sessions began to show results, but those results were for the good and positive attitude for the patient, discipline at home, and he toke less hours on his job. The syndrome of shoulder pain is not exactly pathology but we can rule out other possible symptoms and treat that one. The best thing to do in all people is prevent a lesion give them some recommendations and ergonomic positions, and take a few minutes to take a break and relax on the work, in addition when we feels symptoms out of common we should go to the doctor or physiotherapist to check it and not allowed to continue advancing the affection.
REFERENCE LIST 1. Cortes V., Acosta M., Armendárez M., Domínguez M. J. Romero P. (2009). Guía de Práctica Clínica, Diagnostico y Tratamiento del Síndrome de hombro doloroso en primer nivel de atención; Delegación
Cuauhtémoc,
México:
CENETEC.
http://www.cenetec.salud.gob.mx/descargas/gpc/CatalogoMaestro/085_GPC_SxHombdoloros o1NA/GPC_SHD_EVR.pdf 2. Hernández Díaz, A., Méndez, G., Orellana Molina, A., Martín Gil, J. L., & Berty Tejeda, J. (2009). Láser de baja potencia en el tratamiento de las calcificaciones de hombro. Revista de la Sociedad Española del Dolor, 16(4), 230-238. 3. SUÁREZ-SANABRIA, N. A. T. H. A. L. I. A., & OSORIO-PATIÑO, A. M. (2013). Shoulder's biomechanics and physiological basis for the Codman exercise. CES Medicina, 27(2), 205-217.
65
A 16 YO. FEMALE STUDENT THAT SUFFERED A 2 ND GRADE RIGHT ANKLE SPRING PONCE DEL-HOYO L. AND PEREZ-RAYMUNDO G.
66
INTRO A 16 yo. girl who was a football player suffered
forward position so she wanted to score the last point before the game finished.
an second grade ankle spring on the right
She was running really fast and got the ball but
limb .There had passed 3 weeks since she
suddenly one player of the other team kicked her
suffered the spring. She was immobilized during
really hard on the lateral part of her ankle and she
these 3 weeks, now she has a lot of complications
felt down and because of the velocity she was
with the functionality of her ankle.
running she felt on the ground. The pain
SUBJECTIVE EXAMINATION When my patient arrived to the clinic where I was developing my clinical stance or practices, she was using crutches because she felt pain when she supported the foot down on the floor at the moment of walking. She said on the consultation with the doctor (I was present during all the examination) that she had had an accident while she was playing football in her high school. She was part of the school’s team and she was training for the competition than is done every year between the different grades of the school. When the accident happened, the game was on the second period and her team was winning for 2-0 points, so their team was feeling kind of security against the other team. She had the
appeared just when she tried to stand up again. “I could not support my weight on my leg. Firstly I felt like if I had lost all my strength and then a lot of pain started to came to my ankle. It was insupportable. “I would not have had cried, but I could not resist, the pain was so hard” she said. When everyone noted that what had happened to was not a simple drop, all the players went to the place where she was layed dowm. They started to call the trainer and when he arrived he had already called an ambulance. He ask her what had happened but because of her crying, she said that she could not say many details of what had happened. The other player that had kicked her was how explained what had happened. Then she did not noticed exactly what happened until the ambulance arrived, and she
was taken to the hospital. In the hospital she was
proprioception, because if not, she would get
taken to the X-ray department and the
injured again. She does not have any important
traumatology discarded a possible fracture. He
antecedent. She is a healthy girl, does exercise
told her that she had had an ankle sprain and that
constantly and take a good diet. So my first
she was going to rest and take some medications.
impression was that she was going to have a
The doctor put her splint on her ankle and said
good prognostic if she follows all the therapy to
that she was going to be immobilised during 4
the letter.
weeks. She took the prescribed medications so
67
she did not feel so much pain on the next weeks.
QUESTIONS TO IMPROVE REFLEXION
The pain came back at the moment that the
Q1: Was there any deformity on her ankle?
splint was taken off. She was really surprised because her leg was so much thinner than the other one, and her foot too. She refered to had
A1: Yes, there was a relative deformity, because it was with less muscular mass and with inflammation
pain at the moment she tried to put all her weigh on his right foot. She also felt kind of restriction
Q2: Which data of the history supports your
of the movement.
hypothesis about lack of proprioception?
STUDENT REFLEXION AFTER S/E About my hypotheses of my patient´s injury is that, well she already had a certain medical diagnosis, a second grade right ankle spring. But
That she was immobilized, so she did not stand during three weeks and that makes the baroreceptors get damaged. If it is not corrected she is really exposed to have another spring.
what I could observe while she was describing
Q3: Which are going to be your precautions for the
her situation, was that she was really worry
P/E?
about if she was going to recover properly or not. She was scared because she had never seen her foot that thin and weak. I also noticed that she did not have enough proprioception because she was always seen to her ankle and moving it with her hand to be more comfortable (it due to avoid wrong positions of hes foot and avoid pain). I thought that what she needed was firstly to decrease the pain. Then gain strength and
Avoid pain is the principal precautions. The ligaments are almost recovered, (because it was a 2nd grade not 3rd) but she is still in pain. TEACHER ADVICE It´s important to remember that our physical proceedings could damage the patient. As usually passive examinations are testing tissue response, if we do not dosage them properly they could harm
that tissues. We need a proper evaluation of the
Movement
Strength
ROM
Dorsal Flexion
3
10°
Plantar Flexion
4
20°
example, missing the potential risk fall of a
Eversion
3
10°
balance test, could provoke a harsh result.
Inversion
3
10°
severity of the presentation at this point. But there are other tests for different dysfunctions that could put our patient in danger too. In
68
PHYSICAL EXAMINATION When the doctor started the physical exploration (I was just looking), the patient was kind of scare
Passive movements were the same range of movements but with a little of restriction to make the natural joint movement.
because she said that had not had a really good
He did not explore the gait because the patient
experiences with other medical processes. So
felt with insecurity at the moment of stand in
she did not wanted to know that she was going
both limbs.
to have a bar recovering. Comparing with the other limb this was the The doctor started exploring first by observation
results:
of her ankle, not her posture, because she could not stay standed up without pain. The doctor
Movement
Strength
ROM
found that the skin around the ankle was rubbish
Dorsal Flexion
5
20°
Plantar Flexion
5
40°
Eversion
5
20°
Inversion
5
35°
and warm comparing with the other ankle. Then he palpated the area, and it was swollen and inflammated. She referred her pain in level 4 in EVA scale at the moment of stand all her weight on her right foot. After that he started to evaluate the range of movements and strength in Daniel´s scale and this are the results in active mobilization:
STUDENT REFLEXION AFTER P/E I think that the Physical Exploration was kind of obvious, because the patient already had the diagnosis made at the moment she had the lesson, and it was corroborated with a radiography, so it was just to check the actual symptoms and problems she had on her ankle.
And when the doctor said the results of the test of strength, I thought it was relative, because he evaluated the movements but without causing pain, so I think the patient could have done more
TEACHER ADVICE At the end of the physical examination we need to take back a step and think for a while if data coming from S/E and P/E fits in some way.
strength even if she had felt a little of pain. If do so, it´s the moment to make out a working list The other ankle had so much more strength than the affected one because she had had to walk standing just on one foot, so she had to improve the range of movement and power of the health one to compensate the lack of the other ankle.
with the most reliable hypothesis for current patient´s presentation. At the top of this list will be the syndromes with higher likelihood to be present, and remains in the therapist ability to stablish which of them will be the working diagnostic hypothesis during the treatment session.
QUESTIONS TO IMPROVE REFLEXION Q1: Do you think your patient is going to have a fast recovering? Yes, I think she has a really good attitude and
PATIENT MANAGEMENT DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
also positive factors to get back to play football
Thinking in my hypothesis, I beat that what she
again as soon as possible.
needs is really clear. Her ankle had suffered the consequences of the immobilization, so we need
Q2: So far, which is your first hypothesis with the data coming from C/O and P/E? Which is the data supporting this hypothesis?
to recover it as soon as possible. She had had a specific diagnosis before she came to the physiotherapy treatment so, we just had to take
My hypothesis is that is clear that she needed to
her back to her normal life. She had an
gain strength and more mobility to have a
impairment to walk normally, not just for pain,
normal gait again. The atrophy of her ankle
but also for insecurity and weakness.
makes her loose stability and muscle mass. And also the pain was the main negative factor that made her feel distrust in supporting his weight on her ankle.
The prognosis I gave her was good, I supposed she would be ok in some weeks, of course only if she follow all the instructions given during the therapy. She is young and a sportive girl, so what we have to do, also is to prevent her to have another lesion on the future, and the best way of
69
doing it is trying to recover her at 100% and
one level that were not so much painful to her.
giving her some extra points to her ankle.
She had to make 10 repetitions with an isometric
She had the same treatment during 2 weeks, and on the 3er week there were some changes, because she did not feel pain anymore. She went to therapy 3 times per week.
70
WEEK 1 AND 2
contraction in eversion, inversion, dorsiflexion and extension of the ankle. She had to keep the contraction for 10 seconds and then rest for 5 seconds between each repetition. Finally I used to give her a relax massage to avoid she was in pain after the sessions.
The treatment was given for the doctor, but I applied it to her. Firstly I used ultrasound to decrease the inflammation and pain, because if
STUDENT REFLEXION AFTER WEEK 1-2 TREATMENT
she were in pain, we could not make strength
I think the patient had good results, because we
training.
could get the pain relief. O Without pain we were
After that, I applied a hot pack for around all around her ankle for 2o minutes to relax the muscles before the stretching. Then, mobilized passively all the range of movements and stretched until the pain was of 7 in EVA scale. I explained that the therapy would be painful, but it was going to worth it.
going to be able to gain a lot of strength and proprioception to retraining the gait. WEEK 3RD During the 3er week, she was not more in pain, so all the session consisted in taught her a home program to strength all the right lower limb. I also prescribed a harder proprioceptive training
When the muscles were relaxed, we began to
and functional exercises to taker her back to
make the proprioceptive training. Being in front
football game.
of the mirror, I asked her to stand in one leg and then in the other one. I used some advisements
STUDENT REFLEXION
to make the exercises harder and raise the
She had really good results. She recovered all the
difficulty (like different surfaces with instability
range of movements, so with that factor to our
or closing her eyes at the moment she did the
favor, I think the only things she needed were get
exercises).
extra points to not get injured again.
About the strength training, I began with theraband exercises to make the resistance at
QUESTIONS TO IMPROVE REFLEXION
Q1: Do you think that is useful for her to use an
A4: I think that there wouldn´t be a lot of changes,
ankle support?
maybe I would use the kinesio-tape to help the
A1: I think that it would not be necessary, but it would give her extra support when she is playing.
peroneus muscle to do the strengthening exercises, and if the patient does not complain I could use ice instead hot. The cryo-kinetics
Q2: Does she should continue doing strengthening
exercises would have been a really good option
exercises?
too.
A2: I told her than she was going to have to do
TEACHER ADVICE
71
the exercises for a long time. Just to prevent another lesson. She needs to have more strength
For the majority of the physiotherapists I know, it
than usual in her ankle, because of the spring.
is not the ideal situation to work under the orders of other therapists or doctors, having no
Q3: Will you treat her in the same way if you have another opportunity again?
opportunity to take any decisions in the treatment you perform. In these occasions, although you
A3: Yes, absolutely. I think my management was
have to follow their prescriptions, I think that rely
good enough. The clue was in the initial
on you the capacity to dose it properly and make
subjective examination…
the necessary adjustments on patient´s benefit. And of course, they should listen to your feedbacks
Q4: How different should the treatment be if you had the opportunity to prescribe it instead of the doctor?
or reports with your own thoughts and proposals, also in that situations in which you think the treatment they prescribed is not working optimally.
FINAL STUDENT REFLEXION In my conclusion, I can say that she had a good recovering. I hope she follows all my instructions for the home program to avoid having a second lesion in the future. The treatment was successful because she was treated properly since she had the injury till the therapy program finished. The ankle spring is a very common lesson in sport people, but if it is treated properly, it doesn´t have to bring future discomforts.
REFERENCE LIST
1) Stanley Hoppenfield, (2007) Exploración física de la columna vertebral y las extremidades. (1) . Madrid. Manual Moderno
A 57 YO. HOUSEWIFE WITH A RIGHT HEMI PATELLECTOMY AND TENECTOMY OF THE PATELLA TENDON AFTER A PATELLA FRACTURE AND A TRANSIDESMAL FRACTURE OF THE RIGHT FIBULA BONE RANNOU MA. AND BERTRAND I.
imperfect osteogenesis and since then, she
INTRO
became extra careful and fearful about every A 57 yo. Housewife with a right hemi
kind of physical activity. Then, she also was
patellectomy and tenectomy of the patella
diagnosed with osteoporosis and her daughter
tendon after a patella fracture in July of 2014,
with imperfect osteogenesis too.
and a transidesmal fracture of the right fibula bone.
She’s
diagnosed
with
imperfect
She had antecedents: a right ankle fracture (a
osteogenesis and osteoporosis comes to start
fibula fracture), a right patella fracture and a
her rehabilitation with me in November after
few others in the other limbs but she couldn't
her last rehabilitation doctor’s appointment in
remember exactly how many. So, she was
August of 2014.
coming to begin her physical rehabilitation
SUBJECTIVE EXAMINATION
after her second fibula fracture (transindesmal)
I met D. at the hospital where she had a surgery for her physical rehabilitation. She was a dedicated housewife, mother of an adult daughter with whom she was very
and her second patella fracture on the right side. It happened during the summer in July, five months before I met her, first she fell and broke her patella and a week later she fell again and broke her fibula. Although her ankle fracture
close, having a lifestyle rather sedentary.
didn't need surgery as it wasn't displaced, her
Many years ago, she was diagnosed with
patella was quite bashed up and it resulted in a
hemi patellectomy and a tenectomy of the
Except for her very fragile skeletal structure
patella tendon which was in this occasion re-
which would oblige me to be extra careful, she
taunted with staples.
didn't present contraindications to the examination but, facing her fear, I decided to
The doctor prescription, of four months old in
start assessing the joints mobility and muscles
August, said that the physical therapist had to
strength in the lower limbs.
concentrate in the ankle joint but she hadn't been re-examined since then. As I spoke with
My first impression of the patient was a person
her it became clear that the ankle wasn't her
with mood swings: she often passed from a
major problem, she was disabled by it and felt
motivate, trustful and joyful state of mind to
pain but the one she had in her knee was worst.
sadness, fear, pessimism and lack of confidence
She explained to me that the pain, the
in herself as in myself. She had a tendency to
discomfort and a sensation of instability and
want to lead and control the examination,
weakness in her knee lead her to fear everyday
sometimes by fear of making it too much and
life activities such as go up and down on stairs
sometimes by laziness. It also appeared that
or go for a walk all alone even if she had
the bond she had with her daughter was very
crutches.
powerful: the fact that she inherited her
She added that because of it, she depended a
mother disease made D. feel very guilty and
lot of her daughter, feeling guilty and worry
preoccupied and worry about being a weight
about it, wanting to have a quick rehabilitation
for her.
and saying that she would do everything to
I
succeed. At the same time, she insisted a lot on
psychological sphere will be something very
the fact that I had to be very careful about her
important to include in the treatment.
understood
that,
in
this
case,
the
disease even if I didn't do anything yet. STUDENT REFLEXION AFTER S/E
QUESTIONS TO IMPROVE REFLEXION Q1: Could you find in the history any data
My initial hypotheses about the sources and
supporting that the patient should has an
patho-biological processes: a mechanic pain as
alteration of the pain modulation component in
a result of damages on bone and tendon
her pain presentation?
tissues in remodelling phase in both joints.
A1: I think that her state of mind and her
I decided to override the doctor prescription
attitude could be a proof that the patient has a
and dedicated time to the knee.
central modulation of the pain, in her case, the
psychological area has a great impact on her
she felt the more pain (Tables 2 and 3). The
pain.
mobility of the patella was quite good and the
Q2: How do you think her fear of not wanting to
cicatrisation process was going on. I made her
talk about her pathology could affect her?
walk with and without her crutch but she was so
A2: I think that this fear acts as a brake for her
focused that the walk didn’t appear very
recovery. If she doesn’t know what it is, she
natural.
can’t behave correctly to improve her condition.
TEACHER ADVICE Alteration of pain modulation system and central sensitization are two components of the pain
Right ROM Associated End-feel ankle symptoms Plantar 145° No pain Elastic flexion Dorsal 75° No pain Firm flexion Table 1. Arthrocinematics of the right ankle.
mechanisms with some overlapping and could be present at the same time. But they have to be addressed in different ways. Usually, information related with both mechanisms could be found (if present) in the subjective examination.
PHYSICAL EXAMINATION
In order to really understand what was frightening her, I tried to make her talk about her disease although I knew it. I was surprised when I discover she didn’t know much about it and wasn’t very interested in knowing more. I didn’t push her further, thinking she
Right knee Flexion
ROM
Associated Endsymptoms feel 80° Pain at the Elastic end of the movement Extension 0-1° Decreased Elastic muscle power Table 2. Arthrocinematics of the right knee.
Muscle group Grade (0-5) Ischiotibial muscles 4 Quadriceps femoris 3+ Gluteus muscles 4 Iliopsoas 4+ Flexor of ankle (DF) 4 Extensor of ankle 3+ (PF) Table 3. Muscles’ Power.
eventually could tell me and I decided to start my P/E. I started with the right ankle. She didn’t feel pain but was disturbed by a sensation of fragility and instability. I assessed her range of motion and her muscles power (Tables 1 and 3). Then, I did the same with her right knee where
At this point, she had enough so I let her go to her magnetic therapy session. Before she went out, she explained that although she was happy to start her rehabilitation and expect a lot from it, she didn’t expect very good results.
As she walked away, I finally saw how she was
exercises and that we will take care of her walk.
really walking.
My main idea was to make her participate and join her own rehabilitation by herself to then
STUDENT REFLEXION AFTER P/E
progressively lead her on a good path. She
About my initial hypotheses, my observations seemed to confirm that the real issue wasn’t in the ankle but in the knee where she suffered the more damages to the tissues. The pain finds its origin in her knee as the fact that she feels pain when moving seems to show. Also, I found interesting that she felt more pain when
seemed very relieved as she went home to know that the next session wasn’t going to be long and painful. QUESTIONS TO IMPROVE REFLEXION Q1: So far, which is your first hypothesis with the data coming from C/O and P/E? Which is the data supporting this hypothesis?
moving actively than when I executed the
A1: Noticing her pain manifests when she
movement myself. The lack of power in her
moves and go away when she rests, (associated
muscles didn’t permit her to move the way she
with a decreased ROM and muscle strength),
should as well as her fear of the pain and the fall.
my first hypothesis is a mechanical pain process
It appears that she also doesn’t know how to
as a consequence of her surgeries, in order to
use a crutch.
reduce her previous fractures. I would add that
About the narrative process, at this point I
her state of mind and her mood modulate this
understood that she didn’t want to expend
pain as shown by her attitude during the
herself on her disease or hear about it although
sessions through her obvious fear.
it had a big impact on her life and she had tendency to use it as an excuse to escape the TEACHER ADVICE
physical examination. It occurs to me that I’ll have to check again her walk as it appears that she didn’t know how to use
correctly
her
crutch
making
her
movements more difficult. I started to think that in fact, she didn’t even may need it anymore and that may have been something restraining her without her knowledge. I decided to not push her and told her that we will start the next session with some easy
There should be findings in these 2 first steps of the clinical encounter that have to correlate among them. As S/E comes firsts, usually points out which areas have to be evaluate in the P/E, and what should expect to find there. After performing the suggested tests, the therapist should could check if her first hypothesis were true or not and could move on to additional tests or questions if necessary.
avoid that she only depends on it. I noticed she
PATIENT MANAGEMENT DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN About my initial hypotheses, the exploration of
was capable to support her own weight and I asked her to try to do little walks and move in her home without it.
the patient left no doubt that the major
Finally I let her go to her electrotherapy and
problem
post-surgery
magneto therapy session because she feels
consequence and a significate lack of strength
better to end with it, saying that she took that
in the lower right limb.
as a way to relax and rest before going home.
was
indeed
a
About the narrative process, I wasn’t really sure about the implication of the daughter and her influence on her mother but I was certain that
STUDENT REFLEXION AFTER D1 TREATMENT
anyways the pathology, her history and the
She didn’t feel any pain during the treatment
rehabilitation had a strong impact on her
even if she is very attentive at every move I
participation and on her daily life sending her in
make and how far I go during the mobilizations
a vicious circle: the less she does the worst she
only to relax after a few series.
feels; and the worst she feels, the less she does.
The next day, if the treatment runs, I will
So my main goal was to break this circle and
continue with the exercises adding a little more
restore
difficulties: longer series and more resistance;
her
confidence
through
the
rehabilitation to move forward. DAY_1 We started with easy exercises: firstly big range mobilizations on both joints to show her that it could be done without pain; and then, small inner range mobilizations to start gaining ROM.
and if she has improved with her crutch I plan to try working on parallel bars with obstacles and little stairs. The goal will be to work targeting the function of her upper limb and push her to be confident about going for a walk by herself and coming back to her daily life with good bases and no fear.
I also applied a very small manual resistance during short series of movements to start
DAY_2
improving her strength slowly. The main idea is
I started assessing her progresses since the last
to show her what I expect from her and that she
session (she has a session everyday but I choose
is totally capable of doing it.
to explain the progresses and treatments each
Then, I dedicate time to show her the best way
week to really show her improvements with
to use her crutch to improve her walk and to
significates observations.), and she showed an
increased strength and a decreased pain.
obstacles and the banister and her strength
Seeing those improvements, I kept the initial
improved well so I decided to start practicing
treatment, only increasing a bit the difficulty
the stairs and to do muscular strenghting’s
with the resistance exercise and longer series of
exercise with weights.
movements.
The first exercise consisted on a flexo-
Then, we practiced on obstacles where she can
extension of her knee with a 3kg weight tied on
help herself with parallels bars and started to
her ankle, her thigh being supported by a pillow
go up and down a banister. With these two
while she was laying on her back.
exercises, we try to prepare her to go up and
The second one consisted on a flexo-extension
down the stairs, working on her joints and her
of her knee, pushing against a ball while she
muscles in a functional way which would
was sitting on the couch.
improve her symptoms.
She then continued with obstacles and banister, my intention was to slowly set up a routine,
STUDENT REFLEXION AFTER D2
with warm up, which she could easily follow so
TREATMENT
if I added exercises she won’t be lost only
I see a really significate improvement with this
removing the “old” ones when the new ones
patient. But she doesn’t seem to realize how
were totally acquired.
better she was. She tries her best to be
Finally, we started to go up and down little
enthusiastic about her treatment and I think
stairs, her two hands firmly holding on the
she manages it better when the exercises are
handtrails. The first problem was to correct her
about doing things of her daily life like trying to
posture as she was coming down the stairs
go through obstacles, working on her walk…
aside and putting both feet on each stair.
I try as much as I could to keep it entertaining
D. seemed more confident every day but
as she wished her recuperation was faster but it
started to complain about the length of the
sometimes is quite difficult to manage her
treatment showing some signs of impatience.
mood swings and to motivate her, it demands
The fact that I added some exercises didn’t
patience and inventiveness to convince her to
please her, she thought that the ones she was
work out every session but it’s an interesting
doing before were enough and I had to explain
challenge.
that the key of her progress was in the variety
DAY_3 As every session’s begun, I assessed her progresses. She was doing pretty well with the
of her treatment, increasing the difficulties. She wasn’t convinced. The next session, according to the results, I plan
to continue with the stairs, trying to improve
work more on the stairs. But to start, she
her going down so she gains in autonomy (her
warmed up with her strength exercises and
own stairs only have a handrail and she can’t
auto passive movements: we worked on every
come down without any help). We also work
movement of her hip, knee and ankle, with
out on the strength in her both legs: with auto
weights and pulleys seeking to improve the
passive exercises and more weight. Finally, we
general strength of her leg, not only her
will experiment some proprioception both for
quadriceps muscles.
her knee and ankle.
Once she finished with it, we came up and down the stairs. Last time, we didn’t manage to
STUDENT REFLEXION ABOUT D_3
change the fact that she was coming down
It’s now really difficult to keep her motivated
aside, both feet on each stairs with the two
for her therapy, she doesn’t realize her
handrails. I thought that the problem wasn’t
progresses at all, and this is why I think the
mechanic as I saw her with the obstacles and
stairs will be the solution to this problem.
she hadn’t any problem to come down from
Working and improving herself on the stairs
them. It started to appear that she feared the
will show her, with something she knows well,
stairs. She was physically capable of doing it
how much she improved.
but wasn’t confident enough.
We must continue to work with the weights for
We started slowly, with only two stairs and the
her strength even if she doesn’t see the
two handrails. Showing her that it was easier to
differences but maybe if she realize that in
come down to the next stair if she put half of
order to do the stairs exercise correctly she
her foot on the side of the stair before going
must gain strength it will be easier.
with the other on the stair of after, it was only a
The main problem with D. is her lack of trust,
question of control of her quadriceps. Solving
in herself mostly and in me a little, this is why
this, she was then able to come down frontally.
one of my objective is to give her
Very excited by this improvement, she didn’t
consciousness of all the work she managed to
even realize that she used only one handrail.
do so far, giving her exercises that put it in
These results acted as a trigger and at the end,
light, like the stairs.
she wasn’t using the handrails at all. We then tried to do little proprioception. First,
DAY_4 For this session, seeing the previous results, I decided to remove the obstacles exercises to
she had to work on a mattress, walking on it varying steps: on tiptoes, on heels, aside, crossing legs…The goal was to provoke an
adaptation of her body to the changing
was difficult for her to let her crutches aside
parameters. We then tried it on a rocker device:
because she felt like she needed it. Slowly, she
she was standing on it, on her both feet and I
decided to let them go, and admitted to me
throw her a ball in various directions to provoke
later that it was in fact easier to walk without
an unbalance.
them.
Despite her apprehension, she did it very well
Q3: Do you think that, if you ignored the
and we managed to make it more difficult
psychological aspect of the treatment, it would
asking her to stand on one feet only (she had a
had the same result?
wall to lean on if needed). She didn’t managed
A3: I think that if I hadn’t, the results would
to do it so we stayed with the more stable
have been really different, it would have been
version, for this time.
worst. I imagine she would have stop her treatment, convinced that I wasn’t seeing her
STUDENT REFLEXION AFTERDAY_4
like a person but only like a joint.
This session was quite important because she finally realized that her therapy was working, after that, it was really easier to work with her and to propose her other exercises. I think that in her case, the fear of hurting herself was the biggest brake and that all the time we took was necessary to come to this result. QUESTIONS TO IMPROVE REFLEXION Q1: Which was the role of the electrotherapy in your management? A1: The electrotherapy was TENS and was prescribed to strength her quadriceps muscles. The patient was quite enthusiastic about it as she felt a relaxing effect afterwards and insisted to have it at the end of the sessions. Q2: Did she manage to walk correctly? A2: She eventually walked in a better way but it
TEACHER ADVICE Sometimes is hard to be sure about which part of the treatment has worked better, worse or not at all, also in multi-treatment modalities. It´s the same with lots of research case reports, in which patients are treat with and elevate number of techniques and no data about confounding effect is found. At least, if patient objectives are lined with outcomes, technique effects, and these are properly performed, we could have a plan to revisit after changes are seen.
FINAL STUDENT REFLEXION The final results confirmed my initials hypotheses and even if it was a long process, the patient and I managed to see the improvements. The difficulty in this case wasn’t really the diagnosis but the management of the patient. It took a lot of patience and courage for both of us to communicate and to go through the therapy. The key of the treatment was in the psychological area of the patient, once she admitted that she was improving, it became a lot easier. She didn’t stop her mood swing but she accepted better the directions I was giving. If I had to treat her again, I wouldn’t change my treatment. It worked but maybe I’d try to be firmer, to take the lead of the treatment more quickly.
Right ROM Associated End-feel ankle symptoms Plantar 150° No pain Elastic flexion Dorsal 80° No pain Firm flexion Table 4. Final assessment of the ankle ROM
Right knee
ROM
Associated End-feel symptoms Flexion 90° No pain Elastic Extension -3° No Elastic Table 5. Final assessment of the knee ROM.
REFERENCE LIST 1. RESERVES, I. and FORIN, D. (2015). Orphanet: Ostéogenèse imparfaite. [online] Orpha.net. Available at: http://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=FR&Expert=666 [Accessed 14 Jun. 2015]. 2. Root, L. (1984). The treatment of osteogenesis imperfecta. The Orthopedic clinics of North America, 15(4), 775-790.
8 YEAR OLD BOY WITH FRACTURES OF BOTH LEGS AFTER A FALL FROM THE EIGHTH FLOOR OF AN APARTMENT. TIBERI A. AND VIOLATI D.
82 The medical diagnosis was; in the left leg
INTRO
closed diafisary fracture of tibia and perone, M. is an 8 year old boy who fell off the 8th floor on the 31st of October and fractured both his legs.
treatment with a monolateral external fixator for 3 and a half months. And in the right leg open fracture of the external femoral condyle and right meseta tibial of grade IV in the Salter
SUBJECTIVE EXAMINATION
and Harris’ epifisiolisis scale. The treatment M. is an 8 year old boy who studies in a German school in Madrid. He says he doesn’t practice a particular
sport.
He
went
to
the
consists of an open reduction of the epifisiolisis with screws, cast and orthesis for the first 6 weeks.
physiotherapist the 13th of April of 2015 and says he also goes to another physiotherapist
After a MRI, it appears he had a slight
once every 2 weeks. When we met first I asked
pulmonary
how the accident happened; M. felt a little bit
neumothorax.
uncomfortable, so I decided to change the topic. After a week he confessed that on the 31st of October 2015 (Halloween night), he was playing by himself outside in the balcony, which was on the 8th floor, when he approached the border line and fell, the fall
contusion
and
a
minimum
He doesn’t present neurologic or vascular alterations, the pelvis is stable and the upper body moves without pain. He has been on a wheelchair for 5 months and after that, until today, he uses a crutch to walk. He told me he had never had any other problem before.
was diminished since he fell on a bunch of trees. He told me that that very day he went through
He does not feel any creep sensation, tingling,
surgery on both legs.
burning or allodynia; his sensibility has increased on the right knee around the patella.
He also mentions that his pain appears when
remove some fears which can interfere in the
he tries to move more the leg, and he has an
rehabilitation.
itchy sensation around the scar on the right leg. He also says he feels his legs weaker when he
QUESTIONS TO IMPROVE REFLEXION
has to walk long distances tires or taking the
Q1: Andrea, as you described, M. also has an
stairs at school
epiphysiolysis. How do you think you can deal with it?
STUDENT REFLEXION AFTER S/E M. is a little boy therefore it is complicated to get him focused for a long time, he doesn’t enjoy talking about the accident and this makes the anamnesis harder. I always try to ask
but
without
making
him
feel
uncomfortable and for that reason I was missing information during the first week in
A1: This is a point where I feel a bit doubtful, since the doctors said he has a grade IV epifisiolisis, after a few searches on this type of fractures, I saw that the prognostic is negative due to M.’s age and his growing cartilage is affected. My objectives would be to stimulate the vascularization to that zone.
the anamnesis.
Q2: What do you mean with, “a fear can
My initial hypothesis of the source and
interfere in the rehabilitation”?
pathobiological process: M. has suffered a great
trauma,
mentally and
physically.
Physically the medical diagnosis was a great help and gave a clearer picture of what he has. The fact he has a hypersensitivity or muscular weakness
could
be
related
to
the
immobilization and due to the surgery he received. I decided to evaluate only the hip and the knee of both legs and the position he has from a bipedestation. About
the narrative process, my first
impression was that M. is a Young boy and
I think that in a normal mental state where the patient feels ‘depressed’ or better said, notmotivated, due to the fear of falling for example or doing things wrong, can harden our work. If I push the line of work too much on something he does not want to do (for whichever reason), he could obtain rejection from him but at the same time if I think this line of work is appropriate but he is scared due to any reason, it can slow down the recuperation times.
luckily his improvement is faster. We have to
Q3: Which is the impact for daily life activities
pay attention to his self-confidence and try to
and participation?
84
A3: During every day activities, as we were
physiotherapists. But it doesn´t mean that a
talking, I understood that M. can do everything
wise therapist hasn´t to take it in consideration
inside certain limits. It was him who told me he
to approach these patient´s area. Disability
had difficulties to play with the other kids since
issues
he is the slowest and if he forces his legs they
presentations
start to hurt so he is scared and avoids playing.
treatment outcomes. And our work over the
The only thing he does with no problems is
dysfunction has a direct effect in disability.
being a goalkeeper during break. But generally
Physiotherapists have to know how the impact
he moves with the crutches by himself with no
is in this area and which parts of Daily Life
difficulties and can dress up by himself etc…
Activities and Participation are being affected. It
Regarding
the
is usually more significate and realistic for a
treatment M. is easily distracted, it is hard for
patient the possibility to play soccer again than
him to keep focused and he says he gets tired
to achieve the cold “knee´s full active ROM”
and doesn’t want to do certain exercises.
goal.
Q4: How was the role of his family members
PHYSICAL EXAMINATION
his
participation
during
during the anamnesis? Do they cooperate?
have
a
major
and
role
in
perspectives
patient’s for
the
One week has passed since the first time I saw
A4: The first time I met M. he was with his
M. I was at the end of the clinic’s corridor and I
grandmother; she came to me and told me in
saw him walk towards me accompanied by his
detail about M.’s accident. When I started
grandmother. After saying hello we went
talking to M. and got a bit closer he was very
inside the consult. After a few minutes talking
shy and didn’t want to answer me, so his
with his grandmother I started with the
grandmother had to answer for him. I had to
physical exploration. I ask M. if he can put his
ask his grandmother if she could leave so I
trousers, socks, shoes and shirt off, explaining
could be with M. by myself and get closer to
him that in that way I could have a clearer look
him. Since that moment he started answering
on his state. After a few jokes I asked m. if he
more questions.
could put himself on a comfortable position and look towards the front, I tried to pay
TEACHER ADVICE Following
the WHO
attention to every detail (feet position, shape the
of the tibias, height of the patellae, popliteal
International Classification of Function in 2001
hole, hip, back, and compared his muscular
(ICF),
tone). Generally he seems he goes towards a
disability
is
definitions
not
the
of
field
of
pelvic anteversion, knee flexion on the right leg,
in any other position than goalkeeper and he
and a clear division of weight towards the left
didn’t like this situation.
leg. I also evaluated his scars and the scar of the right leg, above the patella, and saw it was
STUDENT REFLEXION AFTER P/E
a queloid type; the others didn’t seem to have
When I saw M. walk I focused on his way of
any abnormal alteration.
walking, I was impressed because it looked like
- Muscle Balance:
a neurologic walk, therefore I asked my tutor for advice and he tranquilized me and told me
Right leg: grade 3/5
it wasn’t like that. My idea at first was to
Leg left: Grade 4/5
educate his walking since it looked much
- ROM the knee:
uncontrolled. After the first time I saw M. at his home, I looked for the type of fractures he
Right leg: 85 ° of flex. And 15 ° ext.
presented and made myself an idea to what I
Left Leg: Full
was dealing with. After this first P/E, I already have an idea to what I have to work with him
- VAS:
for the moment, my objectives for now is to
Right leg: by forcing the movements of
reeducate the walk, obtain a complete knee
flexion and extension reaches an 8 (not
extension, work on the pelvic anteversion,
strive wanted more) and palpation of
strengthen the muscles and mobilize the scars
scars: supra patellar and the one in the
to avoid adherences.
popliteal hole.
I told him he’d play football again and he’ll be
Left Leg: painless movements but
stronger than before. I know inside my mind
palpation of the tibia and fibula is
that I’m facing a complicated case, mostly due
painful.
to the psychological aspect rather than the
I had the occasion to ask him some more questions, but this time focusing on his feelings after the accident. I asked him if he could play with his friends in school. He said he played as a goalkeeper and that he could stop more goals with his crutches, but he can’t play
physical.
QUESTIONS TO IMPROVE REFLEXION Q1: In the type of trauma and the postures described in the P/E, do you think that some test
pushing the femur anteriorly as the psoas iliaco or muscles that can produce this anteversion.
to assess the integrity of the nervous system
Give mobility and break scar adherences could
could be useful?
allow us obtain more elasticity in the tissues
A1: Your proposition is very interesting and in
86
work at the same time the muscles that can be
fact I thought about the same thing during the day after the exploration. Unfortunately I don’t have a lot of time to do many things, I want to focus on these types of explorations for 2
and obtain more movement of the knee. As I said earlier, always put strength work to strenghthen and reeducate the walk. I totally agree with the propioception work but it will be a line of work that I will be integrating gradually little by little according to the
reasons:
progress made on the objectives described
Because doctors said after MRI that M. has no sort of neurologic affectation in the nerve root
I think that for a kid like him it was best
earlier. Q3: Which are the positive and negative issues for the prognosis in this patient?
to do something “faster” and simpler
A3: Positive Issues: M´s is, surely, important in
for the first day of exploration. Surely
the prognosis due to the fact that it allows us
the next time I will do some test to
to advance a quicker way, the socio-economic
discard
support of the family which allows to have
possible
neurologic
affectations. Q2: Could proprioception be an accurate goal for your patient?
physiotherapy sessions every day and 3 times a week with 2 hour sessions. The absence of other types of diseases. Negative issues: lack of concentration and doesn’t want to really do
A2: Inside my head I have an idea of what the
the exercises is a factor that makes us lose a lot
objectives are and which ones I think could be
of time to make the patient listen and do what
the most important ones. I think it is very
he is asked to, fear creates a defense response
important to work all at once with him. I will
where the muscles try to block the leg and
focus on working every day on the mobility,
difficult the exercises centered on the
paying more attention to the extension since it
increment of range of articular movement. The
is the movement that allows us to have a
type of fracture of the epifisiolisis and the age
functional walk, to work on this. I will have to
in which he did it is another important factor
since there is affectation of on the growth
for the epifisiolisis with screws, plaster and
cartilage and also it’s an age where there is
ferula for the first 6 weeks.
more bone development.
Also, after a TAC we can see a light pulmonary
TEACHER ADVICE
contusion. Minimum neumothorax.
One of the typical questions asked by the patient
He doesn’t present vascular nor neurologic
after this point is “How much time does the
affectation, the pelvis is stable and the upper
treatment need to be effective?” Therapist
limb can be moved without pain.
haven´t a crystal ball in their kit. But we could guess an approximate period of time thinking in
He has been on a wheel chair for 5 months and until today. From my point of view M. presents:
the clinical pattern, the related published evidence, the pathology and your own
Pelvic anteversion
experience treating this kind of presentation.
15° knee flexion on the right leg
Not every former point weights the same; but
Queloide-type scar on the right leg above the
you could put, in a two-plate scale, positive against negative prognostic factors and provide
an estimation. PATIENT MANAGEMENT
Muscular balance o
Right leg: grade 4/5
o
Left leg: grade 5/5
ROM: o
DIAGNOSIS, PROGNOSIS, OUTCOMES
of ext.
AND PLAN o From a medical point of view the diagnosis is clear, M. presents fractures on both legs: -
Left leg – diafisary closed fracture of
Right leg: 85° of flex. and 15°
Left leg: complete
VAS: only pain when movement and palpation o
Right leg: when forcing the
tibia and perone, treatment with an external
movements of flexo-extention
monolateral fixator for 3 and a half months.
he reaches an 8 (didn’t want to force more)
-
Right leg – open fracture of external
femoral condyle and right meseta tibial of grade IV on the Salter and Harris epifisiolisis scale, treatment consists of an open reduction
o
Left leg: the movements don’t hurt but the palpation of the tibia is painful
The prognosis of M. can be good under a
In this section I focused completely on the right
functional point of view, since he is very Young
leg:
his recuperation is faster but what upsets me is the epifisiolisis that he has on the right leg. My objectives are that M. regains his confidence on himself and that he can have once again strength, mobility and more functionality than
88
before.
I asked him if he could lay down, the attention of M during the treatment was very low, he laid down in incorrect positions and when I tried to move the leg he’d pus hit on the opposite side to avoid me from moving it. I made a deal with him: he could ask me whatever he wanted if he allowed me to move his leg. I then started with
DAY_1 Before starting with the treatment I did a quick neurologic exploration to see if there could be an entrapment on a nervous level. Both mecanosensibility test as to the nervious conduction test were negative. I asked M if he
the treatment. M was laid down facing up and the left leg was resting while I had the right leg and worked with the scar with a few massages from superficial to deep in order to break adherences, always basing on the pain M had.
could lie down on the massage table sitting. I
Then I did passive mobilizations specifically on
rapidly evaluated the ROM on both legs to
the patella to the femur and on a second place,
have a comparative mean at the end of the
passive analytic mobilizations of the knee on
treatment. I explained what I was going to do
extension
and to tell me when it’ll hurt. I explained to him
component of the tibia and tractions and
to classify his pain on a scale from 0 – 10
relaxation of the knee. On second place I
calculating 10 as an unbearable pain and 0 is
started working on the flexion from a seated
when you don’t feel anything. I started the
position
test:
component of the knee. I then did the muscle
Right leg : 85° of flex. and 15° of ext.
o
adding
an
an
external
internal
rotation
rotation
treatment of the psoas iliaco from the right
ROM: o
with
Left leg: complete
side, M was on supin position and I was holding his right leg increasing the hip flexion to better go in and palpate the iliopsoas. To the palpation of this muscle we could clearly feel
The end feel was firm and was accompanied by
an increase of the tone.
a muscular spasm as a defense mechanism due to the pain.
At the end of the treatment I re-assessed the mobility and the improvement was noticeable
since I could reach with the right leg more than
element in order to obtain his attention and
95º of flexion and nearly 5º of extension.
be able to work with him on a better way.
STUDENT REFLEXION AFTER D1
DAY_2
TREATMENT
When I saw M I asked him how he felt after the
As expected it is a child and clearly bored
treatment and he told me he felt good and that
standing still in one place and also try
he didn’t feel pain during the day. I then tried
maintaining the most attention possible with
the same treatment from the first day, giving
games and history while continuing my
me time to do a few miofascial liberation
treatment. I think it's very difficult to focus on
techniques on the quadriceps with my hands
making techniques while reassuring the
crossed on top of the muscle and realizing a
patient, this makes me wonder if what I'm
traction on the opposite side as if I wanted to
doing is really the right thing, I wish you could
enlarge the muscle and adding movements
be more relaxed and understand that what I'm
that
doing here with the I do it just for him.
restrictions. At the end of the treatment I
could
go
directed
to
miofascial
spoke with him and his grandmother who was QUESTIONS TO IMPROVE REFLEXION Q1: What types of treatment did you use to assess the iliopsoas muscle?
inside the consult and I told them that the following week we would start going to the gym, dividing the treatment on 20 minutes of manual therapy, 20 minutes of gym and 40 of
A1: I applied a pumping technique of such
swimming pool.
muscle to avoid an irritation of the muscle, which would cause an increase of the pain. Q2: Which part of your management do you
DAY_3 Same as DAY_1 and DAY 2.
think has worked better and why?
DAY_4
A2: I don’t think that there has been a part
It was the first day of gym. I started treating
during the treatment that has been more
the scars and mobilizing the patella and knee
effective. I think that the set of techniques
on flexion and extension with the same leg as
have attained this improvement. I believe my
the first day, I also focused on working on the
attitude towards the patient has played a key
hamstring muscles manually doing deep passes and stopping on miofascial conflict
90
zones and on latent trigger points. Then I went
reeducation of the gait by playing with speed
to the gym with him and we started a strength
and amplitude of the gait, controlling the trunk,
program. M was lying down and we had the
another exercise consisted on him supporting
opportunity on the clinic to do some motor
his feet on the wall of the swimming pool while
control
STABILIZE
I had to hold him from behind, positioning his
apparatus. I started with a few motor control
legs separated by a few cm’s (shoulder width)
exercises on isometric for the quadriceps, I
from this position he had to bend the legs more
positioned
the
so he could then push hard (as if he wanted to
popliteous hole and explained to M that
jump) the objective was to strengthen and
according to the orders I gave him he’d have to
work on the active mobility. For last I told him
contract only the muscle on top of the thigh
to go on a little stair that sunk M’s leg until half
and buttocks and the muscles below the thigh
of the inferior part of the thigh (above the
had to be relaxed, to make the exercise easier I
patella) and from then on he had to be on a
told him top put a hand on top of the quad and
monopodal posture and hold the position for
another one on buttocks and hamstrings. At
20 seconds.
exercises
the
with
the
STABILIZER
below
first it was hard for him to differentiate the contractions between the different muscle compartments. I did the same exercises for the hamstrings positioning the STABILIZER below
DAY_4,5,6 & 7 The treatment was always the same DAY_8
the heel and telling him to push with the heel downwards. I also worked on a propioceptive
3 weeks have passed and I did again the
level and explained to him 2 exercises, the first
physical exploration, the improvements were
one consisted on standing up on top of 2 tilts
huge.
and did charge transference from a leg to the
The pelvic anteversion, managed to have a
other without pain and the second exercise
nearly full extension from the 3º of flexion on
consisted of walking on a DYNA DISC which is
the right leg. The scars remained more or less
a disc made out of rubber, I explained to him
the same, the muscular balance improved
that he had to put more charge on the heel
even though we could still see there was a
Little toe thumb. We then went to some
difference between the left and right leg, with
parallel bars in order to work on the gait. After
less strength on the range of movement:
20 minutes I went down with him to the swimming pool where we focused on the
o
Right leg: 105° of flex. and 3° of ext.
up and down the stairs. On the swimming pool
o
Left leg: complete
-
VAS: pain only to movement and
palpation o
Right
leg:
when
forcing
the
the exercises were more or less the same but we increased the intensities. AFTER A MONTH AND A HALF:
movements of flexo-extention he reaches an 8
M’s treatments are still on the same line of
but he reaches greater amplitudes (didn’t want
work but increasing little by little the
to force more)
difficulties and intensities. On the third
o
Left leg: the movements don’t hurt,
evaluation I did that day M presented:
the palpation of the tibia is less painful
-
Minimum pelvic anteversion
I started as always mobilizing the scars, rotula
-
Scar on both legs were had more
and knee. That day I focused on working more
flexibility and the queloid type of scar had
with the psoas because I think it was one of the
diminished its width.
factors which was altering the gait, so I applied
-
Muscular balance
then I did an analytic stretch of that muscle. On
o
Balance muscular of the right leg:
this section I also worked on a Global Postural
grade V
the same treatment as described before and
Reeducation technique (RPG) with the posture of the dancer to stretch the posterior muscle chain, maintaining this position for 4 minutes without M feeling any pain but a slight tenseness Garrido-Marín, A. et all. 2012. On the gym I started doing a few propioception exercises which were a bit harder, such as stability on standing position on the BOSU, on the side of the half ball, he had to maintain for
o
Left leg: grade V
-
ROM:
o
Right leg: 130° of flex. and 0° of ext.
o
Left leg: complete
-
VAS: pain on the movement and at the
palpation
20 seconds, then he had to put a leg on top of
o
the BOSU and the other one in front of the
movements of flexion around the 133º/135º he
ground, and from there flexion the leg which
reaches an 8 (didn’t want to force more)
was more anteriorized by controlling the trunk. At last we were working on the gait and going
o
Right
leg:
Left leg:
painless
when
forcing
the
palpation of the tibia is
M. I realized that with the passage of time was always hearing me more, working with is not easy because you have to be always doing something that catches your attention, but I think with these types of jobs in addition to the clear improvements at the level physical, M. has greatly improved its attitude also fear. This
92
was the last day I saw M. due to the end of my clinical practice. STUDENT REFLEXION
a complete knee extension, increase of the muscle tone: gastrocnemius, soleus, popliteus, isquio-cruralis muscles, mostly on the right leg. I chose to apply an RPG treatment due to the fact that in the article (Garrido-Marín, A. et all. 7 November 2012) the effectivity or global postural reeducation was studied versus the Propioceptive Neuromuscular Facilitation, to increase the extensibility of the hamstring muscles and it concluded that the treatment
Throughout my treatments with M. my thoughts were always to look for functional exercises while at the same time entertaining him since he used to get distracted easily. During the hours of training I always looked for
with RPG is better. Therefore I surfed the web for books that talked more in depth about this treatment and which was the RPG posture most indicated for M´s presentation (Souchard, P. E. 2005).
simple exercises to strengthen, improve the propioception and functionality in order to bring it to his daily life activities. QUESTIONS TO IMPROVE REFLEXION
TEACHER ADVICE In spite of you´ve found one paper suggesting the prevalence of RPG stretching against PNF¨s, it´s no necessary true that this method is going
Q1: On the 8th day you said that you worked
to work better with your patient. Despite the
with M. a RPG stretch, the “dancer”, what is
internal and external quality of the journal
the reason that made you believe that this was
publication, we should find those which were run
a suitable stretch for him?
within a similar population compared with our
A1: During the treatment weeks, I had the
patients. If her/his profile fits properly within the
possibility to know more of M. as the days
profile of the volunteers in a research, probably
went by. There are many reasons: limitation of
you could better guess how treatment will be with your client.
FINAL STUDENT REFLEXION I’ve reached the end of the treatment with M. The case firstly really scared due to the fact that I had to put a lot of effort in every day to make him pay attention, there were days in which he came and he was really tired therefore working with him was very hard, also the fear I had when it came to do certain exercises with him blocked me a little. I think it has been a very stimulating case for me because every day I felt obliged to make up different exercises which were directed towards my goals at the same time. It has also been my first experience on working with the swimming pool so I am very happy about that, it’s a good line of work and the possibility to be able to follow the case gave me the security that what I was doing with him was the right thing because I could constantly see the improvements. It has been a difficult case but it has made me think a lot and improve my knowledge REFERENCE LIST 1. Souchard, P. E. (2005). RPG. Principios de la reeducación postural global (Vol. 88). Editorial Paidotribo. 2. Marín, A. G., Guzón, D. R., López, P. E., Serrano, M. F., & Imedio, A. S. (2013). Efectividad de la reeducación postural global frente a la facilitación neuromuscular propioceptiva, para aumentar la extensibilidad de los isquiotibiales en sujetos sanos. Estudio piloto. Cuestiones de fisioterapia: revista universitaria de información e investigación en Fisioterapia, 42(2), 98-106.
A TOO EARLY MENISCAL DIAGNOSIS URIA A. AND ALCALA L. The pain started one month ago during a paddle-
INTRO
tennis match when he made a sudden extension 31 year old man who works as a labourer in kitchen construction who complains about a continuous
94
pain above his right patella accompanied by a sense of engagement of 1 month onset…
of his right leg, but he continued playing at the time and for the next two weeks until the pain was so strong that he decided to stop. He usually went running with his dog three days a week, but he interrupted this too. The pain hasn´t hold on since
SUBJECTIVE EXAMINATION
he first noticed but has increased to the point that A.K is a 31-year-old man who works as a labourer
it hurts even at work.
in kitchen construction. He has come to a
He needs to expend a lot of time squatting at work
patella
and he feels a continuous pain, which influences
accompanied by a sense of engagement during
him in his mood and work performance. He is
certain movements, which started one month ago
annoyed about not being able to do any of his
during a paddle- tennis. He has recently started
hobbies (jogging and paddle- tennis).
physiotherapy continuous
consultation
pain
above
his
because right
of
feeling pain in the internal part of the left patella as well as an overload sensation of his left gastrocnemius.
The pain on both legs (specially the right leg) increases at the end of the day (when walking and standing for long periods of time, squatting, when
When I first met him, he walked into the
standing from a squatting position and while
consulting room limping his right foot trying not
going up and down stairs). He usually puts his
to stand on it. I noticed he was a restless person
right leg at rest, extended and with ice at the top
when he started talking to me. He didn´t stop
of the knee to reduce pain and he feels no pain at
wondering about the diagnosis before doing any
night. But when he wakes up, he feels a bit of
physical examination. He was really scared about
stiffness and discomfort on his right leg that stops
having a meniscal injury because his father was
after heating the joint.
operated twice due to his work, which is the same as his.
He had three-ankle sprain on his right leg when he
his constant fear about being operated as his
was 14 years old.
father. But during the clinical case and after the
He has a good overall health; no respiratory or circulatory or urologic dysfunction and he had
physical examination, you will see how I am going to change my mind.
good results on his latest blood test. He has not
Q3. Which
attended any doctor and has no radiographs of his
transmission in meniscus diseases? Do you think is
knee.
high enough to lead a P/E thinking in that
He is not taking any medication, just ibuprofen occasionally when working but without effect.
is
the prevalence for genetic
possibility? A3: No, there is no scientific evidence about genetic transmission in meniscus disease but I
STUDENT REFLEXION AFTER S/E
focused on that possibility because of the
Because of his family history (his father had
triggering
undergo a meniscus operation because of his
continuous aggravating situations during his work
work), my first thought has been that the same thing was happening to the son. So I have decided
mechanism
of
injury
and
the
TEACHER ADVICE
meniscus testing without thinking in other
Illness scripts are good tools for clinicians during the
options.
decision-making process. They provide therapists with the most relevant characteristics of a
QUESTIONS TO IMPROVE REFLEXION
prototype patient within a syndrome. Despite they
Q1: Didn’t you think that the pain of the left leg is
are not always the same (they evolve as the same
caused by an overload?
time as the clinician´s experience) and there is no such a thing as a “prototype patient”, having these
A1: It was my first thought, but I first wanted to
schemas in your mind prompts you with more
know what was happening with the right leg as it
chances to discover of the patient´s presentation
was the main cause for the patient visiting the
fits in that schema or not, avoiding unnecessary
consultation and his main concern.
procedures
Q2: What about the patellar tendon and the LCA and LCP? A2: Yes, you are totally right. Meniscus testing was my first step because of his family history and
PHYSICAL EXAMINATION
During
the
dynamic
examination,
active
movements are good except medial rotation of the knee and hip in both legs (especially in the right leg). Pain has been found during right leg extension starting from a squat position. Accompanied by an engagement sensation of the knee.
96
During palpation, temperature and muscular tone are normal and there is neither articular spilling nor edema. Pain has been produced at joint line palpation of the right leg and an increase in tone has been found in the calf of the left leg. Muscular balance is 3/5 in the right quadriceps. I have started with the static examination where
Trigger points have been detected at the left leg
nothing relevant has been detected except a bit of
in the internal and external gastrocnemius.
knee hyperextension and a great base of support.
Tests: Thessaly test, McMurray test. Appley test
The main symptom is the continuous pain
and the Sensitivity test of the joint line have been
above the right patella.
performed.
The second symptom is an engagement
All of them have been negative except the last
sensation in both sides of the right joint line.
one, which has been painful during palpation.
The third symptom is the pain at the internal
Lachman test has also been performed but has
side of the left patella.
been found to be negative too. (Harrison, B. K.,
And the fourth symptom is the overload
Abell, B. E., & Gibson, T. W. (2009), (Akseki, D.,
sensation he feels at left gastrocnemius.
Özcan, Ö., Boya, H., & Pınar, H. (2004).
His associated symptoms are a right leg block sensation and articular crunch sensation. All
STUDENT REFLEXION AFTER P/E
symptoms are related. Because of the pain in the
As all meniscal tests have been negative except
right leg, left leg has made lots of compensations,
for the joint line test. I have dismissed any
and has ended up with pain too.
meniscal injury by the limited relevance of this
last test alone. As Lachman test is also negative,
A1: The truth is that I did not think of a joint wear
LCA and LCP injuries have been dismissed too.
problem because the reason for the beginning of
I now have to make a hypothesis with all the information I have: - Pain mechanism is nociceptive and mechanical and tissue is at proliferative phase (1 month).
the pain was clear and precise: making an abrupt knee extension-playing paddle. I think that a joint wear has usually no clear beginning nor an exact reason for its appearance. Q2: I think that he should make some Rx or RMN to
Trigger mechanism: was isolated playing paddle-
see if there is some micro fracture on the patella or
tennis but was aggravated after repetitive
in the joint in general because he spends a lot of
impacts and squat positions at work time.
time in squat position, or maybe some problem in the cartilage. Don’t you think?
The source of symptoms is skeletal muscle because it affects the patella and tendons and muscles that surround it.
His main functional limitations are going up and downstairs, maintaining a squat position and standing up from a sit position. The left leg is painful after walking for a long time or after work.
A2: Yes, maybe you are right. But the reason for not doing it was because I didn´t see any neither oedema nor inflammations signs to make me suspect about micro fractures. As I didn´t find any contraindications nor red flags I decided trying some physiotherapy techniques to see if symptoms were released and patient improved before any other complementary images (which I thought were not necessary for the moment).
Because of all this information, my reflection
Q3: Have you found any symptoms on the other
about his problem after subjective and physical
limb and how do link them to the right knee
examination is that he might be suffering a
presentation?
patellofemoral pain syndrome. (Thomeé, R., Augustsson, J., & Karlsson, J. (1999). QUESTIONS TO IMPROVE REFLEXION
A3: Yes, I didn´t put enough information at first, but I´ve just revised it and as I noted, the left leg was painful during joint line palpation and had some trigger points in the external an internal
Q1: Did you think that maybe the problem started because of a joint wear?
gastrocnemius. I think there is a relation with the symptoms in the right leg because of the lots of compensation made when walking or working
that has cause an overload in his left leg because
disruption of exercise and constant overload that
of trying to avoid pain in the right leg.
will occur in the joint during his work in the future will not help the recovering process.
TEACHER ADVICE So the last of my goals is to motivate my patient The development of same symptoms on the other
to achieve better and quicker results.
limb in our patients could be related with different DAY_1
hypothesis. It could be the spread of a general
98
illness; an overused provoked by the increased
My plan starts by reducing pain and strengthening
activity of the other limb; it could be a central
the right quadriceps.
sensitization; or simply activation of mirror neurons mimicking the neural activity of the other limb. It´s
-
I have first make a passive transversal
under our scope to identify the source and the
displacement of the right patella and ask my
pattern of progression to avoid wrong targets
patient to make active flexion of the knee from
during the treatment.
a standing position, meanwhile I have continued maintaining the displacement. I´ve
PATIENT MANAGEMENT DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN My patient´s main goal is pain decreasing. So my goal table includes:
asked him to do three sets of 10 repetitions. -
Taping: medial displacement of the right patella Like this we have worked the quadriceps and the movements, which caused him pain, avoiding pain because of my passive displacement of the
-
Pain releasing
-
Strengthening right quadriceps
-
Remove load and possible contractures of the left gastrocnemius
-
Flexibilize muscles within the right knee
-
Increase or keep the articular movements limited or diminished range.
-
Restore self-confidence
As regard good prognosis factors, his interest in recovering will facilitate the process, but his fear,
patella. I have decided to apply the taping because of the good results acquired during the sessions. DAYS 2-4 My patient has come up to the next consultation with less pain so I have decided to do the same exercise as in the first session. Apart from this, I have decided to work out the internal rotation of the right hip in prone position
with a 90º-knee flexion with passive movements
A1: My idea in the first session was to reduce pain
and to work out right hip extension with anterior-
during the movements that usually caused pain to
posterior movements in standing position with
my patient. I achieved it by making a transversal
the Mulligan tape as the patient does an active
passive displacement of the patella at the same
extension of the hip.
time that he actively did his painful gesture (which
I have also recommended him to start his
was making a squat from a standing position). So
exercises and to ride in static bike for 15 minutes,
despite gaining strength in the quadriceps was
3 days per week.
not my main point, it was indirectly achieved because of the exercise itself.
In the third session, the patient has come with barely no pain, with a muscular balance of 4/5 in
Q2: Why did you work on the hip? And in this way?
the right quadriceps and with an increase in hip
A2: I decided working on the hip because, as I´ve
ROM. So I have decided to continue with the last
said in the physical examination, internal rotation
program and giving him a massage in the left leg
of the right hip was limited. I worked it in this way
to release the overload sensation of the calf.
because it was easier and had better results.
STUDENT REFLEXION
Q3: Did you do reassessment?
I really think the prognosis is this case would be
A3: I reassed my patient in the next session
great because there has been a great increase
because he came 2 days per week for just 1 hour
there has been a big improvement in all signs and
treatment so we didn´t have enough time to do
symptoms in just 3 sessions and the patient is
everything in the same day.
heavily involved. But to get our treatment to be effective, we will recommend the patient to come
Q4: What did the result from DAY1 tell you about your patient presentation?
to our clinic one day a week for the next two weeks and to begin slowly with his hobbies
A4: He was presenting an acute condition that
(running, paddle…).
was aggravated because of repetitive painful movements. As pain was alleviated while making
QUESTIONS TO IMPROVE REFLEXION Q1:
Why didn´t you work on the strength of
quadriceps in the first sessions and you didn´t focus on the range of motion firstly?
a transversal patella movement and reduced during each session, I thought about a patellofemoral dysfunction
TEACHER ADVICE
Contrasting DAY_1 results with the initial assessment of DAY_2 also provides information
Results of DAY_1 treatment usually give us a valuable information about paths of relieving
about the lasting period of the changes achieved, irritability and dosage of techniques.
symptoms and dysfunctions, if you really control the neurophysiological and biomechanical effect you are dealing with.
100 FINAL STUDENT REFLEXION I think this case has helped me to improve my clinical reasoning. In my opinion, I´ve wanted to put, too fast, the name to the disease, to make a quick diagnosis. And that is the reason why I have not progressed from the beginning. I now try to stop and pay attention to every single information about the subjective and physical examination before giving a name to the dysfunction, which I´ve learned, is not that important. REFERENCE LIST 1. Thomeé, R., Augustsson, J., & Karlsson, J. (1999). Patellofemoral pain syndrome. Sports Medicine, 28(4), 245-262 2. Harrison, B. K., Abell, B. E., & Gibson, T. W. (2009). The thessaly test for detection of meniscal tears: Validation of a new physical examination technique for primary care medicine. Clinical Journal of Sport Medicine : Official Journal of the Canadian Academy of Sport Medicine, 19(1), 9-12. doi:10.1097/JSM.0b013e31818f1689 [doi] 3. Akseki, D., Özcan, Ö., Boya, H., & Pınar, H. (2004). A new weight-bearing meniscal test and a comparison with McMurray’s test and joint line tenderness. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 20(9), 951-958
PAIN CAUSING A SCAPULAR DISKINESIS IN A 25 YO STUDENT VIOLATI D. AND TIBERI A.
INTRO 25 years old woman, with an alteration of her right scapular girdle movement after a strange episode of pain and stiffness during the night.
She went to emergency immediately where she received the diagnosis of idiopathic subluxation. No reduction was performed and she was told to apply ice and use a sling “on and off” depending on the pain.
SUBJECTIVE EXAMINATION I just had finished to treat a patient at the clinic where I’m doing my last practices of the physical therapy career, when a colleague call me to help him with the exploration of a new patient. When I got at the “gym zone” the therapist told the patient to lift her arm to show me the problem even before to introduce me. When I saw her right scapula movement during the arm flexion I
She spent 4 days following the directions. The pain decreased but it was still strong so she decided to go back to the hospital at the emergency area where the doctor said to her it was a “cervical problem” and he diagnosed her a cervicobrachialgia. The treatment was diazepam, NSAID and superficial heat application. The doctor also gave her an appointment for two weeks later with the orthopaedic doctor.
got shocked cause I hadn’t seen something like this before. When she put her arm down we
During the 2 weeks before the appointment the
introduced to each other and we started talking.
pain decreased progressively. The orthopaedic doctor told her she has capsulitis and chronic
She was a 25 years old publicity student, she
instability of her shoulder.
have been living in Madrid all her life. She showed me all the medical reports and I She attended to physical therapy because the orthopaedic told her. She told me that the onset of the problem was day 15/03/2015; She had been
asked her for previous pathologies and she answered me it was the first time she has a health problem.
woken up by a very intense pain in her shoulder during the night and She felt it very stiff (while
I asked her if she was in pain and she told me:
she was telling me that, she simulated the
“The pain appears only when I lift my arm and it
position in which her arm was stacked).
is localized in the upper part of my shoulder. I’m
101
not able to lift my arm like the other, I feel loss of
were the accurate one to describe the patient
strength when I have to take or hold something
condition.
with my hand far from my body, like a glass of water or opening the door. I don’t feel comfortable when I lay down looking up because I feel my bone (scapula) pressing the sofa or the bed, but I feel a lot better then 4 weeks ago”.
I think my first hypothesis of a mechanical problem was right but I didn’t think too much about a possible first cause of this mechanical problem. If she really suffered by a subluxation maybe an alteration of the muscular activation
She hasn’t been practicing any kind of exercise
could be provoked by a neural tissue damage or
during the last 3 years.
maybe the severe pain it self could cause it.
My
first
thinking,
putting
together
the
I also didn’t considerate the loss of strength that
information that I received and the first
the patient told me about, that could also be
impression seeing her moving, was about a
related with neurogenic problem that I didn’t ask
mechanical problem because of her “on-off” pain
questions for.
related to the last degrees of shoulder movement over the 90 degrees, provoked for the clash between the humeral head and the acromion that could compromise the tissues between them. The all thing caused by her scapula that wasn’t moving in the right way. The
My brain didn’t have the flexibility to “play” more with the information. I think it stopped working from the beginning keeping mainly the image of the patient moving. I needed to much time to get to this conclusion and start to think again.
quality of the movement that I observed made
The patient looked not worried at all for her
me think about an alteration of the sequence of
condition and she was very quiet at all time and
the muscular activation during the movement.
disposed to follow directions to improve as soon as possible.
STUDENT REFLEXION AFTER S/E I think that I forgot a lot of questions that could
QUESTIONS TO IMPROVE REFLEXION
provide me a lot more information, because of a
Q1: I would like to know if you asked your patient
lack of a mental structure to formulate them
about typical symptoms of neurogenic alterations,
orderly.
like tingling or “burning sensation”… or moments
I also didn’t considerate too much the medical diagnosis because I didn’t think that any of them
of the day in which the symptoms increase, that may help you to get a clearer idea.
A1: I didn’t ask for them and I think it was a big mistake during the first interview. Fortunately I didn’t perform the physical examination the day of the subjective examination because the patient was late for an appointment so that I had the time to reflex on it. Of course before the beginning of the physical exploration it was one of the first questions I asked the patient.
TEACHER ADVICE Contributing factors could play a key role in our patients’ presentation. Therapist tend not pay much attention to them as they are not the cause of the client´s problem. But they should be under our scope, also when they are suggested by the patients as a main issues for them. Sometimes is really challenge to eliminate their influence, for
Q2: Do you think the activation of a trigger point
example anatomic and biomechanics CF. On the
could provoke the alteration in the muscular
other hand, yellow flags or ergonomic CF will be
activation sequence of her shoulder?
targets and should be dealt within patient´s management.
A2: Actually I didn’t recognise a clear active trigger point pattern in the localization of patient
PHYSICAL EXAMINATION
pain but of course I will check it out in the
The second time I saw the patient, first thing
physical examination.
she told me was that she was getting better and
Q3: Are there any other signs supporting the neurogenic hypothesis?
her attitude was very positive from the very first moment so I thought that would be very helpful to get good results.
A3: The only signs and symptoms that could make me think about an alteration in nervous system is the loss of strength. No other signs or symptoms were reported or found.
I asked her for neurogenic symptoms and I got a “not at all” as answer. I also asked more about her strength problem and she told me it was like an uncomfortable situation in which she was
Q4: Could you identify, so far, any contributing
feeling her arm falling and tightness in her
factors for both hypotheses?
medial part of the scapula.
A4: The only contributing factor that I found is
I started with the physical examination from the
the possible subluxation she suffered because it
static observation taking the most relevant
could be the cause of both hypothesis. No other
information for me:
CF or yellow flag were found thinking in the maintenance of the condition
103
Anterior view: the humeral head looked
moment I also tried to charge the neural tissue
in a slight anterior superior position
asking a neck side bending in both sides with
compared with the other one.
the results of no changing in pain and no
Posterior view: the medial borders of
presence of other symptoms.
the scapula as well as the inferior angle of the scapula was more "detached" from the rib cage
Side view: significant decrease of the dorsal curve (kyphosis)
The passives movements had a complete range of movement (ROM) and they didn’t provoke any pain or other symptoms.
I also tried to passively help the scapula movement during the active lifting of the arm with the result of reaching the full ROM with no pain detected but with the increased muscles activation described before. I also asked the patient to open a door to check the movement during one of the action in which she was complaining about the loss of strength;
In a posterior view, during the lifting movement
she repeated again that the movement was
of the right arm, the difference in the
uncomfortable; I observed that, during the arm
movement of the right scapula compared with
lifting, her scapula was separating from the rib
the contralateral was pretty clear: the medial
cage while maintaining the arm lifted and it
border of the scapula started to separate from
increase when she was trying to open the door.
the rib cage from the first degrees of movement (20 ° -30 °); during the lifting, the scapula present a big reduction of the ROM compared with the contralateral. When the scapula stopped to move appeared a significant
At the palpation I perceived an increased tone of the rhomboideus and intermediate region of trapezius muscles, but no trigger point that could reproduce the patient symptoms were found.
increasing in the activity of the upper trapezius, lower trapezius and also the elevator scapula.
I performed the muscular balance of the serratus anterior getting a 3-/5 (Daniel’s scale)
The conclusion was that the ROM of the physiological movements of the shoulder (arm lifting) was limited and the last degrees provoked by pain at the end of the ROM.
asking the patient an abduction of the scapula. During the test the scapula behave as described during the arm lifting and the patient was recruiting other muscles to complete the action
When the patient was in pain I used the VAS to
so that the quality of the movement was very
obtain the intensity of pain: VAS= 3. In that
poor.
STUDENT REFLEXION AFTER P/E After the P/E I considered my first hypothesis of a mechanical problem right: in this case I think the mechanical problem is the cause of patient pain. It appears only during the active movement and its nature bring me to think about a nociceptive mechanical pain because it appears with movement/ mechanical provocation (on-off) (Smart, Blake, Staines, A., & Doody, 2011) and it was localized in a specific
separated from the rib cage in a static rest position could be normal cause the patient dominant hand is the right one, that could provoke more protraction in the homolateral shoulder but it doesn’t explain why she started to have the sensation of her scapula pressing the bed or the sofa in a supine position. It also doesn’t give me information about the muscular status: the serratus anterior muscle is not active in a resting position.
site that “agreed” with my first hypothesis of a
I think the loss of strength could be due to a
clash between the humeral head and the
poor proximal stability (shoulder) that doesn’t
acromion.
allow a good “basement” for the transmission of
Analysing the muscular activation sequence, I
the forces needed for the action.
think the fact that the medial border of the
When I looked for myofascial trigger points I
scapula and the inferior angle separation from
tried to remember which muscle could provoke
the rib cage, could be due to a problem in the
the pain in the location in which the patient was
serratus anterior muscle. The serratus anterior is
feeling it. I didn’t look for them in the serratus
one of the responsible, with the trapezius
anterior cause I didn’t think in the possibility of
inferior and the trapezius superior, of the
their implication in the loss of strength.
scapula movement during the raise of the arm and also to maintain the scapula in a good relation with the rib cage during the movement. I also think that the increased activity of the rest of the muscles that permit the movement and the activation of the levatur scapulae muscle are intent of the body to reach the full movement supplying the poor action of the serratus anterior. I think the fact that the medial border of the scapula and the inferior angle were slightly
After all the previous consideration I started thinking about why the serratus anterior wasn’t activating in the right way so I started to think about a conduction problem, but I couldn’t
105
remember the innervation of the target muscle.
Another test I used in the P/E is the “scapular assistance test” that evaluates scapular and acromial involvement in subacromial impingent, probably the main cause of the mechanical nociceptive pain of the patient. The assistance for scapular elevation is provided by manually stabilizing the scapula and rotating the inferior border of the scapula as the arm moves. This procedure simulates the force-couple activity (coordination) of the serratus anterior and lower
Pain: red (VAS:3) Tightness: blue
trapezius
muscles,
the
elimination
or
modification of the impingement symptoms indicates that these muscles should be a major
QUESTIONS TO IMPROVE REFLEXION
focus in rehabilitation (Kibler & McMullen 2003).
Q1: I didn’t get your conclusion about what you found in the static observation; I mean, what do
TEACHER ADVICE
you think about the relation between her scapula
If we find during the S/E information suggesting
position and her feeling of her scapula pressing
the possibility of a neurology/neurodynamic
when she lay down supine cause as you said the
problem, neurology exam has to be conducted on
serratus anterior isn’t active in a resting position?
Day_1, prior to neurodynamic tests. Also it has to be ruled out any red flag related with these kind of
A1: I don’t have an answer yet. It could be due to the use of the sling that could affect the position
symptoms (i.e. Cauda equine or an Upper Motor Neuron Syndrome)
of the scapula girdle, or maybe a change of her shoulder posture as a result of the pain felt.
PATIENT MANAGEMENT
Q2: Have you found any coordination evidence-
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
based test in the literature for this muscle?
The final diagnosis was a “Scapular dyskinesis” A2: I performed the muscular balance with a
with either flexion or abduction is rated as having
test described in (Kendall, 2007) another
obvious abnormality (dysrhythmias and winging)
effective test described in the literature is the
(McClure, Tate, Kareha, Irwin, & Zlupko, 2009).
“Wall push-ups”, used to evaluate serratus anterior muscle strength.
In the literature is described that the 5% of
that the full ROM can be reached without any
scapular diskinesis can be caused by Injury to the
pain.
long thoracic nerve that can alter muscular function of the serratus anterior muscle, and injury to the spinal accessory nerve can alter function of the trapezius muscle but no evident typical postures of these problems were found in the P/E (Kibler & McMullen 2003). Usually muscles can be also inhibited as a nonspecific response to a painful condition that in my opinion is the most possible hypothesis in the case of the patient, serratus anterior and the lower trapezius muscles are the most susceptible
I also tried to activate the serratus anterior with active exercises in a standing position and in a supine position, asking for a protraction of the scapula with the shoulder positioned in a 90 degrees flexion. I re-evaluated the ROM and pain in shoulder flexion and ABD with no significant changes in the first one and a decreased pain with an EVA of 2/10
to the effect of the inhibition (Kibler & McMullen
STUDENT REFLEXION AFTER D1 TREATMENT
2003). Inhibition is seen as a decreased ability of
My first session was planned thinking in all the
the muscles to exert torque and stabilize the
information received during the S/E and the P/E.
scapula as well as disorganization of the normal
I thought the serratus anterior muscle was the
muscle firing patterns of the muscles around the
main problem so that I chose techniques to
shoulder (Kibler & McMullen 2003).
reach a better activation of this muscle.
The superior or entire medial border may be
The treatment didn’t gave me big results maybe
painful to palpation or with motion because of
cause it was the first session and it was a very
similar tightness or scar in the levator scapulae or
short one or maybe I needed more time to apply
lower trapezius insertions, or both (Kibler &
the techniques for a longer period, or maybe
McMullen 2003), this could explain the tightness
cause I simply needed more sessions to get
that patient referred in the P/E.
better outcomes.
DAY_1
The true is that I didn’t knew protocols or other
I applied the scapular assistance test, applied in
kinds of assessment for this problem so that
several series/repetitions, as treatment to
looked for articles that describe the condition
stimulate the activity of the serratus anterior
and I took out from them some ideas to plan a
muscle and also to make the patient conscious
better treatment in the following sessions.
107
After the research I found that in the first 3 weeks
neuromuscular
of treatment the first point is avoid painful arm
techniques, of the latissimus dorsi muscle and
movements and positions and establish scapular
the pectoralis minor muscle (Kibler & McMullen
motion by proximal facilitation so that my first
2003).
technique was good (Kibler & McMullen 2003). Another point was to initiate scapular motion
facilitation
stretching
I also teach her exercises of scapula protraction using body movements previously described.
exercises without arm elevation, using trunk flexion and trunk medial rotation to facilitate
STUDENT REFLEXION
scapular protraction It could be a good idea due
After checking the muscles flexibility and tone
to the fact that the patient couldn’t activate the
related with the limitation of scapula
muscle with effectiveness and quality using arm
movements (pectoralis minor, levator scapulae,
elevation exercises (Kibler & McMullen 2003)
upper trapezius, latissimus dorsi, infraspinatus, and teres minor muscles) (Kibler & McMullen
QUESTIONS TO IMPROVE REFLEXION Q1: Do you think that activate other scapula stabilizers could be a good idea to improve the
2003), I decide to treat the muscle that appears, compared with the contralateral side, to present more tone.
quality in the shoulder movement? The result of the second session was good in A1: Yes, probably I could look for some exercises
terms of active ROM (full ROM) and pain (VAS:
to activate rhomboids and medium trapezius
1) so that I decided to follow this line for the
muscles. I’m just a little worried about charging
third session in which the patient came with
to much the superior trapezius and the inferior
better sensations but still poor movement
trapezius because as we have seen in the P/E
quality of movement but maintaining the ROM
they probably are already working too much.
and pain improving, so that I wanted to see if
DAYS 2-3
the treatment could also be useful to provoke a change in the quality of the scapular
The patient came with better sensations about
movement.
her strength and she felt she could move more than before.
What I didn’t do was retest after each technique applied so that I only know that all them
After the research I repeated the first exercise performed in day 1 and I also included the evaluation and treatment, with proprioceptive
together get to patient improvement but I don’t
know if each technique alone could lead to
technique, probably the scapular assistance test
better outcomes.
used as technique is the one that worked more cause is the only exercise I used in the first 2
QUESTIONS TO IMPROVE REFLEXION Q1: why don’t you try to activate muscles like the latissimus dorsi to see if they can help you to achieve a better scapula position in an unstable position, amid range of flexion for example?
sessions getting a better ROM and less pain. TEACHER ADVICE Physiotherapy literature is full of trials measuring the “initial effects” of lots of techniques. To be “immediately effective” doesn´t mean that the
A1: It could be a good idea to see if they can help
technique is “long-lasting” or worth it at all. Or at
me to reach a better quality of scapula
least if it is going to be accurate in each case. But
movement and position in different degrees of
re-evaluating patient´s main outcomes before
movement. I’ll try it!
and after the session, will enlighten your thinking
Q2: Which part of your management do you think has worked better and why?
and support next decisions in the management. It could also be a way to give feedback to your patient about his/her progression.
A2: I’m not pretty sure about it yet because as I said in the reflexion, I didn’t retest after each FINAL STUDENT REFLEXION My diagnosis was a scapular dyskinesis with obvious abnormality (dysrhythmias and winging) during shoulder flexion and ABD (McClure, Tate, Kareha, Irwin, & Zlupko, 2009). Causing a nociceptive mechanical pain in the patient during the 2 movements (Smart, Blake, Staines, A., & Doody, 2011). I found support that a painful condition is the most possible hypothesis in causing serratus anterior inhibition (Kibler & McMullen 2003) that is in my opinion the most affected muscle in fact a poor muscular balance during the test described in the P/E was found (Kendall, 2007); so first goal to reach was “waking up” that muscle to improve the movement quality. At this point of the treatment I didn’t find anything in the literature that could clarify me the natural process of this condition, and I also didn’t find any other paper that could help me to be more consistent during the treatment planning. I think that so far I’m missing the key treatment (exercise or manual treatment…) to improve the patient quality of movement so that I’ll keep looking for it in the literature and during the treatment sessions.
109
REFERENCE LIST 1. Smart, K. M., Blake, C., Staines, A., & Doody, C. (2011). The Discriminative validity of “nociceptive,”“peripheral neuropathic,” and “central sensitization” as mechanisms-based classifications of musculoskeletal pain. The Clinical journal of pain, 27(8), 655-663. 2. Kendall, F. P. (2007). Kendall’s Músculos Pruebas Funcionales Postura y Dolor, Editorial Marbán. 3. Kibler, W. B., & McMullen, J. (2003). Scapular dyskinesis and its relation to shoulder pain. The Journal of the American Academy of Orthopaedic Surgeons, 11(2), 142-151. 4. McClure, P., Tate, A. R., Kareha, S., Irwin, D., & Zlupko, E. (2009). A clinical method for identifying scapular dyskinesis, part 1: reliability. Journal of athletic training, 44(2), 160.
111
113
Second Edition, 2016© CC BY-NC-ND 4.0
1 First Edition, 2015© Second Edition, 2016© Edited by Pablo C. Garcia-Sanchez This book pretends to be an e-book and be read through electronic devices. Think it twice if you want to print it. If you do so, be sure that it is printed using recycled paper. This book is under a Creative Commons License: Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) You are free to share — copy and redistribute the material in any medium or format. Learn more about this CC license at creativecommons.org or in our web:
physiotherapyreflectivecases.wordpress.com Notice Medical and clinical knowledge are constantly evolving and changing. Readers of this book are advised to check the most current information provided on procedures featured. It is the responsibility of the therapist, relying on their own experience and knowledge of the patient, to make diagnoses, to determine dosage and the best treatment for each patient, and to take all appropriate safety precautions. To the fullest extent of the law, the authors do not assume any liability, loss or any injury and/or damage to persons or property arising out of or related to any use of the material contained in this book. The authors
2
Edited by Pablo C. Garcia-Sanchez
3
CONTRIBUTORS Mª Dolores Alcalá 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain
4
Iscia Bertrand 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Pablo C. Garcia-Sanchez Physiotherapist, Lecturer, Department of Physiotherapy and Podiatry, School of Health and Sports, Universidad Europea de Madrid, Spain Gema Gallardo Sanchez Physiotherapist, Physiotherapy Unit, Fuenlabrada University Hospital, Spain Juan Antonio Gonzalez Garcia Physiotherapist, Physiotherapy Unit, Fuenlabrada University Hospital, Spain Rossella Guido 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Marta Javier 3th year student of Physiotherapy, Universidad Europea de Madrid, Spain
Greete Kriik 2nd year student of Physiotherapy, Metropolia University of Applied Sciences, Finland Guadalupe Pérez 3th year student of Physiotherapy, Universidad del Valle de México, México Laura Ponce 3th year student of Physiotherapy, Universidad del Valle de México, México Marie-Anne Rannou 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Andrea Tiberi 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Ainhoa Uria 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain Davide Violati 4th year student of Physiotherapy, Universidad Europea de Madrid, Spain
5
FOREWORD TO THE FIRST EDITION La asignatura “Terapia Manual Ortopédica III” pertenece al plan de estudios del Grado en Fisioterapia de la Universidad Europea de Madrid, siendo la última asignatura a cursar dentro del itinerario curricular en “Terapia Manual Ortopédica”. Las asignaturas que lo conforman son optativas y refuerzan la formación en Terapia Manual basada en la evidencia.
6
Este proyecto pretende reflejar el desarrollo del pensamiento crítico y reflexivo, tan necesario para acometer un buen diagnóstico y abordaje terapéutico del paciente a través de la Terapia Manual Ortopédica. Y qué mejor manera que comenzar con los intentos que hace el estudiante con los primeros pacientes a los que se enfrenta en la práctica clínica real. En esta experiencia vivida de forma intensa por el alumno, éste desarrolla competencias como la adaptación del tratamiento a la evolución del paciente, el replanteamiento constante de los objetivos terapéuticos, o la autocrítica, habilidades básicas para cualquier profesional de la salud. Con este proyecto no se consigue únicamente un mejor aprendizaje por parte del estudiante, sino que, nosotros los fisioterapeutas con años de experiencia clínica, tomamos conciencia y recordamos la importancia del razonamiento clínico. La metodología docente utilizada es el Método del Caso, procedimiento que se adapta especialmente bien al desarrollo de las competencias descritas anteriormente; además, la labor del docente, que ha acompañado y guiado al estudiante a través de preguntas constantes, ha permitido la adquisición de un conocimiento más profundo. Nos gustaría destacar la labor del docente, en primer lugar, por plantear este proyecto tan ambicioso y enriquecedor para todos; y en segundo lugar por acompañar y motivar permanentemente a los estudiantes. Él ha sido el motor de este proyecto, gracias a su constante inquietud en innovación de diferentes metodologías en el aula, situando siempre al alumno en el centro de su aprendizaje. Por último, nos gustaría reconocer y agradecer el esfuerzo de estos alumnos que se han implicado de forma completa y que han acometido este reto como una oportunidad de crecimiento profesional y personal; pensamos que esta actitud os permitirá tener una vida más plena. Mónica de la Cueva, Beatriz Ruiz, Raquel Díaz-Meco y PhD , Physiotherapists , Lecturers, Department of Physiotherapy and Podiatry, School of Health and Sports, Universidad Europea de Madrid, Spain
FOREWORD TO THE SECOND EDITION In this second edition of the book, we were supposed to include more case studies from the students, but the number of students attending the subject during 15-16 course were too small, that we have decided to included their work at the end of this new season. Amazing projects could be launched in Education and Health, thinking out-of-the-box, and using wisely the new tools available for physiotherapists, patients and educators. For this second edition, I have invited Juan Antonio and Gema, for writing a chapter about their lovely experience about the use of a reflective diary, and the social media in the education of our students. They are in the paramount place to teach (clinical placement) and in one of the best times to impact the student (last year of university). Thanks for accept my offering. I hope you will be delight with the reading and get inspired for your daily work. Pablo C. Garcia-Sanchez Physiotherapist, Lecturer, Department of Physiotherapy and Podiatry, School of Health and Sports, Universidad Europea de Madrid, Spain
7
8
To our beloved patients, who open their lives to us. Pablo To our teacher, to make this happen. 2015 OMT3 students
9
PART 1: INTRODUCTION
Chapter 0: Introducing the project: using case reports to improve Reflective Practice and Clinical Reasoning in Physiotherapy, Garcia-Sanchez PC. Chapter 1: Use of the reflexive diary, blog and twitter in the practicum: our experience, Gonzalez Garcia JA. and Gallardo Sanchez G. 10
INTRODUCING THE PROJECT: USING CASE REPORTS TO IMPROVE REFLECTIVE PRACTICE AND CLINICAL REASONING IN PHYSIOTHERAPY GARCIA-SANCHEZ PC.
INTRO AND CONCEPTS The ability to reflect about our actions and decisions is irrevocably linked with the basics of our improvement and learning system. This way to approach learning and practice experiences try to get beyond the bare experience as a unique improvement tool, once the therapists have
To share their own clinical experiences to teachers, clinicians and peers, could be an essential activity to develop metacognitive abilities in the learning process (Sefton, Gordon & Field, 2008). Remains in the educator to plan and create the required spaces for feedback and reflection during the course period.
started their professional work, demanding the
According to Rivett and Jones (2008) “Skills in
apprentice to critically look over their own
clinical reasoning can only be developed in the
practice, with the goal of improve it.
context of clinical cases” (Rivett, Jones, Loftus &
It is considered as a corner stone in the development of expertise within a knowledge area (Jensen, Gwyer, Hack & Shepard, 2007) and it is progressively being incorporated to the graduate and postgraduate health science curricula.
Christensen, p. 477). The use of case reports to teach clinical reasoning is well covered by Rivett and Jones in that chapter. The type of case reports carried out in this project were “written cases”, with the particularity that were peer developed with the supervision and questions prompted by another student and the educator.
Clinical reasoning and reflective practice are linked through the metacognition level of reasoning and according to Jones and Rivett (2004) reasoning could be seen as a reflective process (Jones and Rivett, 2004).
Peer learning is an educational method to improve knowledge and understanding, and is broad defined in the literature. The type of peer learning method chosen for this project was what Ladyshewsky described in 2000 and
11
developed through past century, specifically
thinking and reasoning through real cases. This
using the metacognition as a reflective method
book doesn´t intend to emulate our pioneers,
(Ladyshewsky and Jones, 2008).
and probably the depth of the student´s reflections won´t be the same compared with
THE PROJECT AND INSPIRATION
12
these well-noun physiotherapists. But these
This book is the final product of a collaborative
student´s reflections will be productive for them
project among international physiotherapy
and will give an instant insight about what is
students
Manual
happening in the therapist-mind during the
Therapy 3", an elective subject included in the
management. We hope this could be useful for
4th year of the Bachelor Degree in Physiotherapy
others.
attending
"Orthopaedic
at Universidad Europea de Madrid. As we seen, Reflexive Practice is a key skill to The completion of a reflective case was one of
develop Clinical Reasoning in manual therapies
the activities included in the final grade of these
and other disciplines. It is one of the tools these
subject, but the presence of their cases in the
students had learnt during their stage in the
book relied on their own decision. It was guided
university on the last courses, to improve their
by me as a teacher, but the decisions of the
understanding and practice. Giving support to
whole project were made by the students. It was
our clinical decisions will allow us to improve as
completed in 3 months on the spring of 2015.
professionals and as profession.
The project is inspired in the book "Clinical
We hope you´ll find this interesting for your own
Reasoning for manual therapists" (Jones and,
practice and be inspired to cultivate this wise
Rivett,
activity as a teacher, as a student or as a graduate
2004).
In
that
book
relevant
physiotherapist show us their knowledge,
physiotherapist.
REFERENCE LIST 1. Jensen, G. M., Gwyer, J., Hack, L., & Shepard, K. (2007). Expertise in physical therapy practice. 2. Jones, M. A., & Rivett, D. A. (2004). Clinical reasoning for manual therapists. Elsevier Health Sciences. 3. Ladyshewsky, R. K. (2000). Peer-assisted learning in clinical education: a review of terms and learning principles. Journal of physical therapy education, 14(2), 15. 4. Rivett, D., Jones, M. A., & Higgs, J. (2008). Using case reports to teach clinical reasoning. Clinical reasoning in the health professions. 3rd ed. Philadelphia: Elsevier, 477-484. 5. Sefton, A., Gordon, J., & Field, M. (2008). Teaching clinical reasoning to medical students. Clinical reasoning in the health professions. 3rd ed. Edinburgh: Elsevier, 469-78.
USE OF THE REFLEXIVE DIARY, BLOG AND TWITTER IN THE PRACTICUM: OUR EXPERIENCE 13 GONZÁLEZ GARCÍA JA. AND GALLARDO SÁNCHEZ G.
The essential philosophy of the EHEA is that
INTRODUCTION
the student becomes the centre of the system. The authors are clinical teachers of Practicum II in Fuenlabrada University Hospital ten years ago.
During
this
period,
elements
of
participation that assume the philosophy of the European Higher Education Area (EHEA) have been incorporated. This chapter explains our experience of promoting a model of effective learning.
The overall effort of the student is valued, not only physical presence in a class or practices in healthcare
settings,
as
well
as
the
management of tools of learning, rather than the
mere
accumulation
of
knowledge
(Universia Spain, 2016). It is intended that the future professional will be responsible for learning on their own, to locate, analyse,
Rey Juan Carlos University and University
manage, synthesize and transmit information
Hospital of Fuenlabrada work together in
by him/herself.
teaching students in clinical practice. Physical therapy students visit our unit in their fourth course. It was considered that the orientation of the training should be directed towards the imminent
inclusion
in
the
real
work
environment. This mean a promotion of
In this context the teaching guide of the subject Practicum II proposed as a teaching strategy “knowing in action”, which can be achieved with reflective practice. The teacher or tutor has the task of stimulating this reflection in action.
autonomy in the performance of patient care, integrating all their knowledge previously
If we understand learning as an active process,
acquired.
we need to take awareness of it. We must
know about the different kinds of strategies for
and themselves as learners in these different
learning, thinking, and problem solving.
contexts (Chick, 2016). Nevertheless, we know
Students should become aware of their
that it is not a question of an easy matter of
strengths and weaknesses as learners, writers,
practising, since we have not been educated in
readers, test-takers, group members, etc.
the habit of carrying out an exercise that leads
Students have to put metacognition into
us to introspection.
practice. The metacognition is a complex
14
concept
that
has
different
definitions.
Metacognition is, put simply, thinking about one’s thinking. More precisely, it refers to the processes used to plan, monitor, and assess one’s
understanding
and
performance.
Metacognition includes a critical awareness of
With these premises since the 2012-2013 we have incorporated as elements of learning and assessment a reflective diary, a blog of the subject and the use of Twitter as social network. REFLECTIVE DIARY
a) one’s thinking and learning; and b) oneself as a thinker and learner. Major and its group of study
(Labatut
Portilho,
2004)
say
metacognition is the cognition of the cognition, that is to say, the knowledge of your own knowledge. The knowledge is the object of the cognitive activity. The way a therapist clinically
With the base of the teaching guide, different aspects were incorporated as the experience was progressing and reading about other experiences was made (Martiáñez Ramírez, 2012).
reasons their findings can strongly influence
As the name suggests, it is a chronological
how the case is interpreted. It seems clinical
account of what happened every day in the
reasoning need of the sum of the thinking and
practicum. From the beginning we emphasize
decision-making processes associated with
that the diary is voluntary, although evaluable.
clinical practice (Edwards I, 2004). The way
It
how we think it will be important to make good
discoveries,
decisions and actions. Metacognitive practices
disappointments,
increase students’ abilities to transfer or adapt
expectations, events, thoughts, reflections,
their learning to new contexts and tasks. They
suggestions, explanations, etc., experienced
do this by gaining a level of awareness above
by the student. Reflection-on-action is what
the subject matter, thinking about the tasks
gives added value to the experience. It is
and contexts of different learning situations
intended
contains
that
views,
concerns,
feelings, surprises,
the
cognitive
desires, learnings, ambitions,
effort
to
remember, process, analyze and explain in
indicated that the diary demands a richer and
writing is a way to learn.
more complex cognitive effort than the simple
It is important to emphasize the consideration that the concept of Practicum has for us. According to Guijarro Martínez (2015) we prefer the term clinical education in so far as “can contribute to [the student] development not only in doing, but also in knowing, being and living “. Reasoning, critical thinking, decision making, values, attitudes, ethical behaviors and professional socialization are involved in practice and this is considered from this broader view than simply know how (Guijarro Martínez, 2015).
description. It is noted that there is an added value in this reflection that makes it necessary and, above all, useful in their present and future learning. ACTIVITIES
15
Around reflection in action and reflection deferred to the end of the day, the students carry out different activities. They search images, rating scales, variants on ways to assess and treat patients, include database search strategies, incorporate links to websites and/or videos, attach annexes with these and
TASK
other contents, etc.
The first day students are received and
In our experience the weekly reflective diary
teachers explain to them, among other things,
usually contains 6 to 12 pages. It is sent at the
the tasks to be carried out during their stay in
end of the week by email to the teacher.
the hospital. In the case of the diary they are
He/she receives two or three diaries and once
told that it has to be written on a daily basis to
read, share relevant reflections with the
achieve the objectives. They are provided with
student in writing. The teacher corrects,
information on the potential contents. They
suggests, guides or compliments. The door is
have had previous and different experiences
open to discuss all this personally, making the
with a reflective diary. Therefore, they are
process something continuous.
provided with additional written information to get what we expected.
The reflective diary is, as we said, an assessment
tool.
Since
the
2015-2016
The proposed model of reflective diary is
academic year, in an attempt to be objective, a
deliberately versatile and open. However, it
rubric based on Martiañez Ramirez et al (2015)
always contains the reflection of the students
is used.
beyond a mere description of facts. If not, we
In short, reflection is used to what we have
that has to do with something related to the
been arguing. It encourages to propose
practice. Guidelines are given and they can
alternatives, rethink what has been done, said
read some posts in health blogs as examples.
or thought, to question processes, to justify, to
Most of students did not use before this tool.
drive change, to change attitudes and values. All this means work, and time. Students have
16
to work at home for a stronger learning and a
ACTIVITIES
development of criticism. It will be useful for a
We want the students to make the writing
life-long-learning.
process, adding the advantages of Internet such as easy sharing, abundant information
BLOG
and resources and unlimited communication. The writing process consists of:
Student blogging empowers students to take charge of their learning, gives their learning
Prewriting: Plan the writing. It is a time to
purpose while helping with reading, writing,
think, brainstorm ideas and organize the topic.
digital citizenship, artistic, critical thinking,
Students have questions to consider: what do I
social skills, self-expression and creativity
want to say? How do I want to say it? Who will
(Huffaker, 2005). It could also increase
read my writing? What else do I need to know
students and teachers´ motivation and
to begin? Who can I talk to about my ideas?
relationship, as well as academic achievement (Read, 2006). In our opinion blogging is perfect to use metacognitive strategies. Our
blog
write it down. Create a rough copy of the writing. Students have question to consider:
“Practicasfisio”
(https://practicasfisio.wordpress.com)
Drafting: Write your first draft. It is a time to
has
been used as a teaching tool since 2014-2015
Are my thoughts organized? Which ideas do I want to develop? In what order do I want to say them? Who can read this?
academic year. Revising: It is a time to improve the writing. Change your write to make it better. Questions TASK
to consider: Should I add or take out parts?
Students are explained the steps to publish
Have I used the best ideas and words? Are my
their posts on the blog. They must publish two
details clear?
posts in six weeks. They can choose the topic
Edit: check your writing. Questions to
that includes informative tweets, mentions
consider: Are my spelling, capitalization and
and communications to students. The author
punctuation correct? Could I use any image to
also makes a proposal for other uses: academic
complete the text? Could I use some useful
information, enrichment of the educational
links to add information?
experience,
Publish: share the writing on the Internet. We emphasise the first part of the writing process where the student must reflect.
extension
of
contents
and
“twitoria” or tutorial via Twitter. Finally, Arroyo
also
proposes
some
dynamic
integration of Twitter in the classroom. With that background we began by creating an
We have published sixty posts with 7,825 visits
account named @practicasfisio. The teachers
till the date but very few comments.
had started the use of personal and collective accounts nearly two years before. Surely that
previous usages led to learn utilities and
Our interest to incorporate new teaching tools
potential applications and the knowledge of
led us to put in the social network Twitter in
reference accounts in the field of Physical
the practicum at the beginning of 2014. We did
Therapy. As Twitter inherent philosophy, we
not know prior experience in clinical settings of
intend to make public the contents whose
Physical Therapy or other health discipline.
usefulness or uselessness can be decided by anyone. This means that tweets should be
Social networks can be used as a learning tool by providing information and means for integration and communication (Moreno Badajós, 2016).
respectful to people and the information should not contain personal or health information related to any person. Our uses largely coincide with those targeted by Arroyo
The study of Arroyo Sagasta (2012) addresses
Sagasta, with some particularities proper to
the presence of Twitter in a particular high
the nature of the Practicum.
education academic environment, face-toface education and very different to a clinical setting, but it was our initial reference. Its description of the use of social network for teachers is done from a primarily qualitative approach and contains a list of applications
After two years and a half using Twitter the teachers appreciate it positively. However, against our prejudices, this network was not used on a daily basis by most students. Most of them do not participate regularly in Twitter
17
after the practicum (at least with the profiles
In the framework of the Extension of contents
with which they did in the Practicum II).
Tweets there are links to documents, articles, videos, websites, highlighting references to
TASK
professional blogs as a source of information
It is proposed, in the context of the practicum, participate with messages of different types. Students write spontaneous comments with
18
information on topics related to what happened or they have seen. They may include links to other written content, images, videos. Teachers´ participation is considered more important because of novelty and lack of
and/or debate. Questioning tweets contain questions about different dimensions of practice (methods, techniques, illnesses, etc.). Some of them encourage enquiry about ethical codes and legal aspects of professional practice. These are responded via Twitter or students are told if the answer will be in the diary or verbally.
experience in use by many students. Students are invited to participate with tweets ACTIVITIES
about the contents of the practicum, to re-
Depending on the content we can classified
tweet,
the tweets in different types.
discussions or to answer different questions
In the
to
share
information,
to
open
Information tweets the teachers use the
that appear in the practicum.
account, since the start of each rotation, with
As in the case of diary and blog, a specific
indications about tasks, linking to content
rubric evaluates various aspects of student
about reflective diary or use of blogs in
performance.
healthcare, among other things. Other uses are information about the way of publishing
CONCLUSIONS
posts in the blog of the subject, dates or
The incorporation of teaching tools described
notifications for submission of tasks, changes
in this chapter has, as their ultimate goal, to
of teachers or teachers’ absences, exam dates,
promote more lasting and deeper learning
etc. Other informations are about professional
and habits that facilitate livelong learning. For
organizations,
the authors this is an ongoing process,
announcements,
offers,
courses/conferences that may be of interest
unfinished and subject to constant revision.
for the student or for his/her
The opinion of students is a determining factor.
immersion in the profession.
imminent
We asked them and their assessment is encouraging. However, we think it is necessary
to promote continuous efforts to improve the competences of future physical therapists.
REFERENCE LIST 1. Universia España. (Junio de 2016). http://eees.universia.es/. Recuperado el 16 de Junio de 2016, de http://eees.universia.es/preguntas-frecuentes/conceptos-basicos/#4 2. Labatut Portilho, E. (2004). Aprendizaje universitario: un enfoque metacognitivo. Madrid: Universidad Complutense de Madrid. 3. Edwards I, Jones M, Carr J, Braunack-Mayer A, Jensen GM. (Abril de 2004). Clinical reasoning strategies in physical therapy. Physical Therapy, 312-30. 5. Chick, N. (2016). https://cft.vanderbilt.edu/. From https://cft.vanderbilt.edu/guides-subpages/metacognition/ 4. Martiañez Ramirez, N. (2012). El diario reflexivo académico como recurso de aprendizaje en las prácticas clínicas: una experiencia en el grado de Fisioterapia de la Universidad Europea de Madrid. IX Jornadas Internacionales de Innovación Universitaria. Villaviciosa de Odón. 5. Guijarro Martínez, M. (2015). La educación clínica del estudiante de fisioterapia desde la experiencia de los tutores y tutoras clínicas. Estudio fenomenológico descriptivo. Bilbao: Deusto. 6. Martiáñez Ramírez, N., Rubio Alonso, M., Terrón López, M., & Gallego, T. (2015). Diseño de una rúbrica para evaluar las competencias del Prácticum del Grado en Fisioterapia. Percepción de su utilidad por los estudiantes. Fisioterapia, 83-95.
19
PART 2: REFLECTIVE CLINICAL CASES
Chapter 2: A 52 yo. man who broke his arm 9 month ago and referred pain in all movement, Alcalá MA. and Uria A.
20
Chapter 3: A 32 year old woman with sore thightness in the upper posterior surface of the right leg, Bertrand I. and Rannou M-A. Chapter 4: A persistent shoulder pain and rigidity in a 51 y.o woman, Guido R. and Javier M. Chapter 5: A 45 yo. garbage collector with chronic back symptoms , Javier M. and Guido R. Chapter 6: A 23-year-old female preparing for army with lower back pain for 4 weeks , Kriik G. and Ponce l. Chapter 7: A 40 yo. man with a painful shoulder syndrome, Pérez G. and Kriik G. Chapter 8: A 16 yo. female student that suffered a 2nd grade right ankle spring, Ponce delhoyo L. and Perez-Raymundo G. Chapter 9: A 57 yo. housewife with a right hemi patellectomy and tenectomy of the patella tendon after a patella fracture and a transidesmal fracture of the right fibula bone, Rannou MA. and Bertrand I. Chapter 10: A 8-year-old boy with fractures of both legs after a fall from the eighth floor of an apartment, Tiberi A. and Violati D. Chapter 11: A too early meniscal diagnosis, Uria A. and Alcalá MA. Chapter 12: Pain causing a scapular diskinesis in a 25 yo student, Violati D. and Tiberi A.
21
A 52 YO. MAN WHO BROKE HIS ARM 9 MONTH AGO AND REFERRED PAIN IN ALL MOVEMENT ALCALÀ M.D. AND URIA, A.
22
INTRO A 52 yo. man who had a sedentary life and one day fell down from a stone 9 month ago and
for him to relax himself, not only like stop doing something but also he can’t calm his body.
broke his arm and since that he referred pain in
The accident affect his daily life activity due
all movement and his previous treatment
the impossibility to use the hand he couldn’t do
doesn’t work but he is stressed and tired about
all that things that he usually do and he was a
this because he wants be better as soon as
little bit overwhelmed and tired about this
possible.
situation.
SUBJECTIVE EXAMINATION
He went to another physiotherapist before I
When I first met P.N was two month ago, he
met him but the results weren’t the expected.
had a lot of pain on his distal part of the left arm.
He was treated by this therapist 20 sessions
He doesn’t had all the range of motion and he
but he wasn’t happy and his problem
told me that sometimes he doesn’t feel his
continued and also gets a little bit worst.
third, fourth and fifth fingers.
He use his hand and arm like he doesn’t have it,
He works as a lawyer and he is the boss of the
also because his predominant arm is the right
association, so his life is a little bit sedentary,
arm but he couldn’t continue with this pain.
he doesn’t like practice any sport but he love to go to the theatre, cinema and going out for
STUDENT REFLEXION AFTER S/E
dinner with his wife. We can say he likes doing
With this presentation of P.N I think that he
relaxing things, because in his work he had a
has neurogenic and muscular damage.
lot responsibility and he is stressed. He told me
The main problem is the fracture that he
he is very active: because he usually have a lot
suffered at the radio and the consequences are
of things to do at the same time, being difficult
the affectation of muscles and nerve. He has a
Q2: Didn’t you think about the possibility of the
long period development of the pathology so I
ulnar nerve being damaged too because of the
know that the fracture is solved but I have to
alteration in the sensibility of the fourth and fifth
work on all the tissue that are affected to mend
fingers?
the neurogenic problem. After S/E I think that the median nerve is affected so I will check at the elbow and the wrist.
A2: No, because the ulnar nerve’s test was negative and because in the electromyography we saw the damage of the median nerve.
For the flexors and extensors muscles I have to recuperate all the range of motions and then I can work out to improve the debility that he has.
TEACHER ADVICE Choosing high evidence-based tests will add to your reasoning better ingredients to make a good
My patient start the treatment very stressed because he wants to be better but he saw that the last treatment doesn’t work but now I can see
decision. Regarding to the neurodynamics issues, we need to discriminate among tests assessing roots, nerve trunks and main nerves.
how he is more animate and positive. So far, ULNT3 hasn´t demonstrate high sensibility The last treatment was about massage on the arms to relax the muscles and use ultrasound and
and specify. So, adding your inexperience, we need to take with precautions
laser therapy, but it doesn’t work. PHYSICAL EXAMINATION QUESTIONS TO IMPROVE REFLEXION
First of all my patient has a diagnosis before I met
Q1: How did you know that radio´s fracture was
him, so in part he knows what he has, but nobody
already cured, just because of the time that had
stopped one moment and tell him the exact
passed since the fracture took place or you had
information about which parts of his harm and
photographical evidence? And do you know if he
hand were damaged and the different part of the
used any orthotics after the fx and for how long?
treatment.
A1: I know it because I saw the MRI so I have the
Firstly I spend time to explain him exactly which
photographical evidence and I’m sure about the
are the tissue he had affected than I started with
consolidation of the fracture. No, he didn’t use
the P/E and with the medical diagnosis I build my
any orthotics after the fracture.
hypothesis and I started from the elbow and I
23
saw that he has all the range of motion and no
QUESTIONS TO IMPROVE REFLEXION
pain, so I passed to the wrist.
Q1: You´ve said you had all the information
In the clinical history of my patient I had all the information about ROM, BM, damage and all about the problem but I think that I had to explore all and plan my own treatment
24
because the one he has received doesn’t work. On the wrist I tested the range of motion and muscular balance.
about ROM and BM… but it´s no clear which joints are you talking about when referring to ROM or which muscles BM are you testing. A1: I referred to wrist’s joint and all the extensors and flexors muscles. Q2:
You´ve
said
you
started
physical
examination from the elbow. Why didn´t you start at a higher level, for example, from the
With neurodynamic technique I tested the
shoulder?
ulnar, median and radial nerve to see if the
because of the damage of someone of this.
A2: Because of his mobility and his pain I supposed that the shoulder shouldn’t suffer any injuries, so I decided started from the elbow.
STUDENT REFLEXION AFTER P/E
Q3: Did you assess any reflexes or sensations
The anterior diagnosis showed me which part I
apart from making neurodynamic techniques?
debility and the strange sensation he had were
had to test but I decide made my own P/E to start another time from the 0. I had no contraindications for P/E so I tested
A3: Yes, I assess the sensation with different type of touch on his arm and hand but the only think he feels is tingle sometimes on his hand so I decide to make neurodynamic techniques
without any problem and I saw that he had a restricted range of motion in all movement of
PATIENT MANAGEMENT
the wrist and some alteration of the sensibility on the hand. But the most important thing that
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
I saw is that the necessity of my patients is to
My goals are:
knows because I do one thing and no other because he was saturated and tired that people tell him what to do but not encourage
-
Improve the range of motion of the wrist
-
him and not explain him nothing.
Improve straightness of flexors and extensors muscle
-
Eliminate the pain
-
Recuperate the sensibility
-
-
Change the treatment from the
mobilizations if the pain decrease or increase
anterior
and I saw that the pain decrease.
Increase the motivation of my patient and improve self-confidence
Now I had to search a new treatment because the anterior doesn’t work.
After that I started forced the end of the movement to start improving the range of motion. To terminate the session I started stimulate
I know that my patient needs something more
the sensibility on the hand with different type
than a simple massage and I think that the
of touch and with complete extension and
ultrasound and laser didn’t have any benefice
flexion of the fingers on the active form.
in this case. After that I had to animate my patients and explain him that now we going to use new treatment and that he has to be patients and trust on me but I know that at this point maybe it can be difficult.
STUDENT REFLEXION AFTER D1 TREATMENT At the end of the session my patient referred that the pain decrease and a sort of liberation on the wrist. I saw that something change, he
First of all I focus my attention on the wrist and
was more animate than when he arrived at the
the movement of this because he had a big
session.
restriction of all movement and at the same I work on the median nerve and the sensibility.
This process was different from the previous and at the beginning the patient was a little bit
DAY_1
insecure but I could see how it works and also
I told him to take some posture of the wrist in
him could see that from the first session we
which he doesn’t feel pain and I make the same
had some results so I will continue with this
thing for the elbow to see when the pain
treatment.
appear. QUESTIONS TO IMPROVE REFLEXION After that I saw that the elbow had no restrictions and no pain so I focus on the wrist. I make mobilization fixing the radio than fixing the ulna. After that I did the mobilizations of all the bone of the hand. I make all this movement in the passive form and evaluating after all the
Q1: What happened with the sensibility? Did it improved? A1: At the moment I didn’t know because I had to wait the next sessions and see what happen in those days and text it in the next session.
25
DAY_2 Firstly I test the movement and the general state of the wrist to saw if he had maintained
days he doesn’t feel nothing strange about his fingers.
the resulted we reached in the anterior session
Now I started work on the strength of the
and it was ok.
muscles with resisted movement firstly than
After that I do the same treatment because I
26
Also the sensibility was better because in those
saw that it works, also I started work with
we use the electro stimulation of the flexors muscle with a dumbbell of 0.5 kg.
resisted movement at the same time he was
Finally I work releasing muscles in general to
with the electro stimulation and I saw that he
avoid the overload.
can do it perfectly even if with a little bit pain at the moment of mayor tension of the muscles.
On the next session I saw that the treatment work out so I continued with this and increase slowly the kg of the dumbbell.
At the end I relaxing the flexors and said him to make the same exercise at home with a little bottle of water.
I think that the prognosis is good because my patient was satisfied with this new treatment and was more animate and participate.
DAYS 3-4 After that I can say that the part of the In the next session my patient referred less
treatment
pain and more agility on the movement so I
mobilization of the ulna and radio in all
decide to continue with this treatment.
direction because after that was the moment
that
works better
was
the
in which I started to see important change in the evolution of the problem
FINAL STUDENT REFLEXION I think that at the moment in which I met my patient I had apparently all the information I need for my clinical reasoning. I had the information from the medical diagnosis, from the anterior treatment but it wasn’t enough because there was something that doesn’t work, so thanks to my examination I discovered the main point of the problem. All this means that even if you apparently had all the information you always had to search more and more to have a complete clinical reasoning that is the main point for a successful treatment.
REFERENCE LIST 1. S. Jimenez del Barrio, M. Fortun Agud, N. Pascual Lanuza. E. Bueno Garcia, E. Estebanez de Miguel and J.M. Tricas Moreno (2013). “Reliability of upper limb neurodynamic test for range of movement and symptoms localization variable”. Cuestiones de Fisioterapia 281-289.
27
A 32 YEAR OLD WOMAN WITH SORE THIGHTNESS IN THE UPPER POSTERIOR SURFACE OF THE RIGHT LEG BERTRAND I. AND RANNOU M-A.
appendix a year and a half ago and that she still
INTRO A 32 years old woman attends a physical
28
therapist due to sore tightness in the posterior surface of the right leg; ischiotibial level. High-
doesn’t feel 100 percent “good”. She feels tightness and bloated all the time in the area and has digestive discomfort since then.
level runner, the pain began and gradually
She is a very health, energetic,
worsened 8 month after being operated from
sympathetic, open minded, athletic young
the appendix.
woman
who
has
no
relevant
family
antecedents, doesn’t smoke and sporadically
SUBJECTIVE EXAMINATION
drinks alcohol in social events. She would run
A 32-year-old patient entered the
an average of 10 kilometers a day and was
consultation and started explaining her
getting ready for an important race that
condition. For a few month now, she started to
needed a lot of training. She works long hours
feel pain in the upper posterior surface of the
behind a desk and seems to be very unsatisfied
right leg while jogging; right underneath the
with her job. She loves outdoors activities and
ischium. At first she could cope with the pain
never misses an opportunity to join a group to
but as time went by it worsened to a point
participate in the event.
where it forced her to stop jogging. She would feel the pain during the terminal swing and beginning of the propulsion phase of the human running locomotion cycle and would increase when running up steep hills. The pain would also appear while she blow-dried her hair in a bending over position and occasionally, complained of lumbar pain. Continuing
to
STUDENT REFLEXION AFTER S/E About my initial hypotheses about the sources and pathobiological processes was that she could have a tendonitis of the proximal insertion of the hamstring muscle due to overuse and maybe some active trigger
gather
useful
information about her case, she mentioned that she underwent surgery to remove the
points in the gluteus area.
She didn’t present any warning for
Q3: So far, what is your thinking about the appendix-release issue in her actual clinical
examination contraindications. My first impression with her was quite optimistic. Her positive and energetic attitude
presentation? A3: It is explained further.
was quite freshening; making it easier to create a physiotherapist- patient bond of trust.
TEACHER ADVICE
Even thought I knew that her condition was
Irritability means about the property of patient´s
also affecting her psychologically, since it
current presentation reacting to any stimulus,
limited her ability to perform the activity she
and it is not directly related with the amount of
loves most well, she always managed to keep
affected activities or participation. It´s used to
a positive and open-minded attitude about it;
be more related with the severity of the
listening and cooperating with us during the
presentation. In our management it is usually
treatments and completing her “home work
linked with the quantity of mechanical stimulus
assignments”.
needed to cause patient´s symptoms and their length. This quality will suggest the extension
QUESTIONS
TO
IMPROVE
REFLEXION Q1: How does she feel about her pathology? A1:
and the level of depth of our exploration procedures.
PHYSICAL EXAMINATION
Haven’t asked her but I think she is
Although she seemed like a joyful,
annoyed about the fact that she can’t run as
optimistic and stressless person during the
long and as well as she did before and anxious
sessions, I wanted to know how she was in a
to get better.
work-like environment; to see her stress levels
Q2: So far, what is the level of severity and irritability of her clinical presentation?
and if it had an impact on her. It turned out that during her working hours she’s quite stressed out because of the bad ambience there is at
A2: The level of severity of her pathology is
work and admitted that she eats fast sugars to
minimum but the irritability is quite high since
quench her anxiety.
it’s affecting her daily life activities. I started the physical examination by palpating the right proximal insertion of the ischiotibial’s but she felt very little pain
29
compared to the one she used to while running. Like I mentioned earlier the pain appeared during the terminal swing and beginning of the propulsion phase of the human running locomotion cycle and would increase when running up steep hills. The pain also appeared while
30
performing
a
resisted
isometric
contraction of the hip in extension and of the knee flexion; to test the ischiotibial and gluteus muscle. Body chart representing her pain. She also had active trigger points in her right gluteus muscles and a blocked
STUDENT REFLEXION AFTER P/E
sacroiliac joint because of the hypertensions of
About my initial hypotheses I met
the buttocks muscles. Her pelvis was in a slight
consistent findings about the implications of
anterversion position and her body slightly
trigger points in the gluteus muscle but not
leaned forward. Sometimes she complains of
about the tendonitis of the proximal insertion
lower back pain.
of the right hamstrings.
I decided to then explore her iliopsoas,
It is clear that she has musculoskeletal
witched showed to be rather painful (both of
dysfunction for, as mentioned in the physical
them). And the scar left by the appendix’s
examination part, she has reduced muscle
surgery was ridged, fibrotic, adhered to
strength and a slight anteversion of her pelvis
connective tissues below and painful on
with a semi blocked sacroiliac joint; but I keep
palpation.
asking myself why? How is it that in less than a year, gradually, has she been feeling pain in
Muscle group
Grad (0-5)
Ischiotibial muscles
4
Hip abductors
3+
Iliopsoas
3+
the posterior part of her leg when she’s been running all her life since the age of 17? Its not like she’s not physically prepared; she is very athletic and physically strong. The pain came gradually, little by little
Muscles’ Power
since the surgery. I think that the surgery and
the scar left behind are partly the reason and
PATIENT MANAGEMENT
origin of all the simtomatology of why she is
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
complaining of isquion pain. Due to the aggression her body
I think the pain she’s is feeling on the posterior
underwent with surgery, I think she adapted
surface of the right leg is caused by an overload
analgesic positions wile running in order to
of the isquitibials muscles due to the pelvis
reduce the abdominal tension and pain
anteversion, gluteus weakness and lumbar
acquiring
pain; all of which is caused by an incorrect body
an
erroneous
body
position;
triggering an imbalance between muscle
position.
groups forcing some to work more than others. Since she is a young athletic woman her prognosis is good. She is willing, eager to get
QUESTIONS TO IMPROVE REFLEXION
better and does everything possible in order to
Q1: Was anything done with respect to her
achieve this goal. However she is very
digestive tract symptomatology?
impatient, and so whenever we achieve to reduce the pain, she forces her leg more and
A1: Yes, due to her digestive discomfort of tightness
and
bloatedness,
she
relapses.
was
recommended to take probiotics for a month
DAY_1 + 2
and to drink a lot of water in order to rebalance
The first day she came to get treated, I applied
her intestinal flora. (It was very useful) .
analgesic electrotherapy for 20 minutes on the upper posterior surface of the right leg to
TEACHER ADVICE
reduce the pain.
Facing a high irritable presentation as you suggest, involves to take some extra precautions
Afterwards I did massage therapy on the
during the physical examination. In your case,
iquioteibials muscles to relax the muscle as
probably this means to explore carefully the
much as I could to see if in doing so, the pain
myofascial trigger points, and do not stress the
would reduce.
common ischiotibialis tendon to the extent you couldn´t continue with the P/E routine.
I explained to her what I thought what going on and the biomechanical of her lesion. I asked her the next time she goes for a jog that she should take smaller strides to reduce the hip
31
flex/ext amplitude and the force exerted by the muscles.
DAYS 3- 5 Natalie, as expected, commented that the few
I ended the session with passive stretch of the
days following the treatment she noticed
isquioteibials muscles and the gluteus muscles.
improvement but then it went back to the original pain.
STUDENT REFLEXION AFTER D1+D2 TREATMENT 32
The patient was able to do the movement of bending over and touching the ground (movement that she couldn’t do without pain) with a 40% decrease of pain. I’m glad I managed to reduce her pain although I expect it wont last long since I didn’t treat any other areas due to lack of time.
So for the next few sessions I mostly insisted on working on reducing her pelvic anterversion with
manual
therapy
techniques
and
increasing the sacroiliac joint mobility. I would also work on her scar; reducing the fibrotic, adhered tissues and making it more flexible using “ventosas” and massage theray. Treating her iliopsoas was also important to relieve the tensions and reduce the back pain
QUESTIONS TO IMPROVE REFLEXION Q1: About the pelvic anteversion: Why did you
she would complain from time to time. I showed her how to stretch it and told her to stretch it as least once a day.
chose to treat only the joints and not for example, her abdominals?
For the isquiotibial, I gave her exercise to do at home to strengthen it. Eccentric exercise. And
A2: Interesting point, I didn’t think about it; but it would of have been an additional effective
strengthening
exercise
for
her
gluteus
muscles.
treatment. I will take it into consideration for next time.
STUDENT REFLEXION
TEACHER ADVICE
The pain reduces progressively. It seems that
A test-treatment will allow you to get invaluable
we are on the good path.
information about the condition of the presentation. Using the results of the treatment
QUESTIONS TO IMPROVE
as another piece of evaluation could inform you
REFLEXION
how to treat your patient properly
Q1: How does she feel about her treatment?
A1: She was very grateful. She knows the
To strength the tendon elastic properties will be
progress is slow and that she needs to be
a required goal in most tendon issues
patient. But as the sessions passed by, she
presentations. On the other hand we could not
would notice positive changes and that little by
forget the muscles power training. There are
little the pain reduces.
recent published evidence to relieve tendon pain using isometric, contraction, which should
TEACHER ADVICE
helped with your patient too (Rio et al. 2015)
33
FINAL STUDENT REFLEXION Natalie was improving slowly but surely. I think that the fact that she was really motivated actually helped a lot with the healing process. There were ups and downs during the duration of her rehabilitations but we managed to resolve all the problems and move forward to try and achieve a full recovery.
REFERENCE LIST 1. Daniel Cushman, Monica E. Rho et al (2015). “Conservative Treatment of Subacute Proximal Hamsting Thendinopathy Using Eccentric Exercise Performed With a Treadmil.” Journal of Orthopaedic and Sports Physical Therapy. 0;0(0):1-24 2. White, K. E. (2011). High hamstring tendinopathy in 3 female long distance runners. Journal of Chiropractic Medicine, 10(2), 93–99. doi:10.1016/j.jcm.2010.10.005 3. Sherry, M. (2012). Examination and Treatment of Hamstring Related Injuries. Sports Health, 4(2), 107–114. doi:10.1177/1941738111430197
4.
Rio, E., Kidgell, D., Purdam, C., Gaida, J., Moseley, G. L., Pearce, A. J., & Cook, J. (2015). Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British journal of sports medicine, bjsports-2014.
A PERSISTENT SHOULDER PAIN AND RIGIDITY IN A 51 Y.O WOMAN GUIDO R. AND JAVIER SIMON M.
34
INTRO
M. cames showing an antalgic posture that
The patient is a 51 woman that refers pain,
strikes me: aproximation and internal rotation;
especially during the night and stifness in her
holding the affected arm with the other.
left shoulder since 9 months ago. She was initially treated for a supraspinatus tendinitis, with poor results. She
came
to
consultation,
referring
a
symptom’s change and helplessness of not being able to accomplish daily things.
The symptoms have started nine months ago, when she was working in Germany. She doesn’t remember any direct trauma in the arm. She kept in mind that one day rising in the morning, she started having a not well localized acute and annoying pain in her left shoulder,
SUBJECTIVE EXAMINATION M. come to visit in November, talking about a dull and continuus pain and stifness in her left shoulder, that prevents her to carry on
especially during the night. This lack of sleep caused her a lot of tiredness and anxiety, with the consequence of not being able to work and take care at house chores.
movements of daily life, for example when she combs her hair, and paints (a passion of her).
She thought that the intake of medication was
She works as an architecht on her own and she
the only way to fight against the problem. She
is married, with a German man, for 25 years.
started taking medications (NSAIDs) to slow
Unfortunately they have no children, due to an
down the symptoms, but this forced her to be
histerectomy she underwent at 32 yo.
dependent on medications.
She’s a busy woman, who worked around the world, especially in Germany where she was living since 6 months ago. Her husband continues to work there, and being away from him, overwhelms her a lot.
After a months of acute pain, under the advice of her husband, she decided to attend to a physiotherapist. She was treated for a supraspinatus tendinitis for two months, with poor results.
The symptoms increased over time and a arm
symptoms change could be a evolution of this
rigidity began to manifest, that prevents her
first problem.
from moving it. When I asked her if the pain, after treatment and a few months later, was always the same or if she noticed change, her response was :“At the
There is also a emotional component that compromise the evolution and the mood of the patient.
beginning the pain was severe and sharp, to the
M. is feeling alone, because her husband is not
point of crying for the pain. After the treatment
with her and the pain and rigidity prevents her to
I noticed a small change in the pain quality. It
have a normal life and to perform her hobby.
wasn’t too acute and I was able to rest a bit more.” After the failed treatment, due to family reasons, she had to come back to Spain, and even she presented symptoms, she did not intend to attend to another physiotherapist. The months passed, the pain was still present,
I don’t think the disease is related with a tissue damage, instead with a progressive disease: her problem could be a tendinitis sequel and shouldn’t be related, considering her symptoms evolution, with soft tissues and bones damage surrounding the shoulder.
and rigidity even more.
She’s very disappointed with her anterior
Desperate for being unable to move her arm,
treatment and think that her problem has not
rest and have a normal life, she decided to go to
solution.
a physioterapist practice. At the present day, the patient is not motivated and thinks that her problem has not solution. M. has hypothyroidism and take daily medicine for this problem. She has been smoking a packet of cigarettes a day for 15 years, and she is an occasional drinker. STUDENT REFLEXION AFTER S/E I think her symptoms are related with the pathology diagnosis. The supraespinatus tendinitis could be a consequence of her actual presentation and the
I need to attend emotional issues in her presentation. I’ll return considering this point after the physical examination. QUESTIONS TO IMPROVE REFLEXION Q1: Do you think that could be related with a visceral problem, for example with a lung problem, like she is a smoker, and a lung problem refers pain in the shoulder? A1: I’d have considered it in the physical examination.
She was asked to do several
35
exams for discard associated diseases and, in
literature to follow routinely. Sometimes is
particular, the chest radiography was normal.
interesting to give this list to the patient in the
I think that can’t be a reffered pain of a visceral disease: M. doesn’t have related sympthoms
waiting, before entering the assessment room and check with her later the specifics.
and she refers, in the following physical
36
examination that her pains is triggered and
PHYSICAL EXAMINATION
increase with movements.
Before the physical examination, talked to me
I will deepen this thought in the rest of the issue.
that she did, a shoulder radiograph and a chest radiograph to discard other pathologies. In both
Q2. So far, which is your hypothesis about the
cases, the radiographs were normals.
pathobiological issues and pain component? A2: My hypothesis is about a nociceptive and somatic pain that starts with an inflammation presentation. With the passage of time this
I decide to ask her other questions about her life, before starting the physical examination, specially about her hobbies.
inflammatory pain become chronic and the
M. tells me that she paints since she was 20 yo,
inflammatory symptoms make space for
and it was a very strong passion for her.
stifness and a adhesion role. She used to paint, 5/6 hours a day, with both Q3. Which could be the role of hypothyroidism in
hands alternately. She’s ambidextrous.
her presentation? I start the physical examination with the visual A3: Oliva,Berardi, Misiti, Maffulli (2013) noticed that thyroid diseases should be linked to idiopathic tendinopathies and as Sardella White and Garbe (2010) found the hypothyroidism
inspection. I detected the left shoulder higher than the other one and in antepulsion, also the protracted left scapula. Muscle atrophy of the shoulder girdle was present too.
could be a risk factor for the joint. I detects also upper trapezius hypertone. Her first tendinitis could be related to her hypothiroidism
disease,
that
could
be
considered like a predisposing factor. TEACHER ADVICE Ruling out red flags in the S/E has to be a wise option. There are several list s of questions in the
The colour of the skin in general and in particular in the shoulder area is normal. Palpation produces pain of subscapularis (VAS 6/10) and deltoid (VAS 5/10).
The passive movements exploration of
left
The active movements exploration refers similar
shoulder refers limitation in all movements with
limitations and pain: 70 degrees of flexion, 25
a not well localized pain (VAS 6/10), in particular
and 35 degrees respectively of external rotation
in abduction and external rotation.
and internal rotation and 55 degrees of abduction. (Table 1) The patient isn’t able to perfom power testing because she refers so much pain and releted weakness.
Subescapularis pain: blue
Deltoid pain: red
Subsequently I perform a provocative test for cervical radiculopathy, the Jackson’s test, and the Adson’s test to discard a thoracic outlet syndrome. Both tests were negatives. I perform also any special tests that help me to
Not well localized pain
diagnose a possible disease, like the Apley Scratch Test and the Shrug Sign as McFarland and Kim (2006) shown. The negative test performed is the O'Brien's test (to exclude SLAP lesion). After the P/E, the patient refers me to be very afraid about the diagnosis and sad. I recommend her to attend to a doctor ,with the suggest to have a MRI, to better diagnose.
In passive flexion the patient can’t move beyond 85 degrees. The external and internal rotation are respectively of 30 degrees and 40 degrees; in the abduction the patient presents 60 degrees.
37
38
ROM
F
IR
ER
ABD
Passive
85°
40°
30°
60°
Active
70°
35°
25°
55°
problem have no solution, could be a problem during the treatment and the disease prognostic. QUESTIONS TO IMPROVE REFLEXION
Table 1 (F:Flexion; IR:Internal rotation; ER:
Q1: Has your patient any red flag or yellow flag
External rotation; ABD: Abduction)
regarding the physical examination procedure?
STUDENT REFLEXION AFTER P/E I discard the possibility of a visceral and referred pain. The patient doesn’t refer any related symptoms and the radiographs were normal. An important aspect is that she’s ambidextrous. Repetitive movements with her left shoulder, associated with hypothyroidism, could be related with her disease. Passive and active motion limitation makes me think in structural changes in the periarticular structures. These changes could be the results from a combination of an initial inflammation and immobilization (caused by the pain). The positives findings show me that the patient range of motion is affected, and help me to exclude pathologies like cervical radiculopathy and SLAP lesion.
A1: No, there weren’t red flags to perform the physical examination. The yellow flags are the low motivation of the patient about the treatment, the sadness for the absence of his husband and for not being able to perform her hobby and passion. Q2: So far, which is your first hypothesis with the data coming from C/O and P/E? Which is the data supporting this hypothesis? A2:
Her associated disease, the symptoms
change, and particularly the descreased passive range of motion, makes me think in a joint pathology, started with inflammation and then became chronic. I wait the MRI result that can help me to diagnose a specific disease. TEACHER ADVICE There should be findings in these 2 first steps of the clinical encounter that have to correlate
Another aspect to take into consideration is the
among them. As S/E comes firsts, usually points
emotional role in the patient disease. After the
out which areas have to be evaluate in the P/E,
physical examination I can say that there is an
and what should expect to find there. If we don´t
emotional and no only a physical aspect that
find these relationships, we need to keep going
afflict the patient. The patient’s think that the
with new questions and proceedings until we´ll reach a point to make a clinical decision. If there
are not present any severe signs or symptoms we
DAY_1
should continue this assessment into the next
My aims for the treatment are principally
session.
to release the pain and to increase the shoulder range of motion.
PATIENT MANAGEMENT
I
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
mobilizations in all directions. During the
MRI reveals a reduced capsular volume with
pain,
absent inflammation.
mobilization, in all movements, saying
started
with
shoulder
joint
mobilization, the patient refers a lot of especially
in
the
end-range
that she wouldn’t continue with the With this ulterior test and the P/E results I can
treatment.
say that the patient is affected by adhesive capsulitis in the “frozen phase”.
After spending time to reassure the patient, I continue the treatment with a
The symptoms show me that the patient presents a degenerative and chronic disease
soft tissue massage to reduce the stress and relax her.
that started with an inflammatory stage. The first day of treatment ends here. The initial tenditinis, the repetitives movements painting and working, with her hypotiroidism
I explain her that the prognostic could be
problem, could be risk factors of the next
good only if her works actively with me,
shoulder disease.
and that I can understand the pain she feel and can help her.
To have a good prognostic I must work the emotional role of the patient, explain the
At the end, the patient promises that will
following treatment and reassuring her.
try to have a positive role during the treatment.
However, the prognostic should be positive, if the patient follows the treatment with a positive
However, the patient feels very tired and
attitude.
negative and decides to go home.
The plan starts with a progressive treatment, helping the patient to understand her disease and treat it.
39
STUDENT REFLEXION AFTER D1 TREATMENT
motivated. The emotional role of the patient is
The first day of treatment was a disaster. The
her family is an additional drive to carry out the
patient was very negative about the treatment.
treatment.
Pain at end-range in all directions, typical of
M. was more positive and the treatment
adhesive capsulitis, prevented me to continue
continued normally.
very important, and the love and the support of
the treatment in a good way. I
40 I hope she will change her negative attitude. I must insist with the treatment and teach her to understand that the pain is part of the journey toward recovery.
started
with
shoulder
intensive
joint
mobilizations, passive, active and resistive kinesiotherapy. The patient felt pain, but she was able to withstand it. The treatment keep on with shortwave, for about 10 min/session, to increase tissues
QUESTIONS TO IMPROVE REFLEXION
temperature and improve motion and elasticy.
Q1: What do you think that you can do to motivate your patient to keep adherence of her
After one week of treatment the ROM of the shoulder improved of 15 and 10 degrees in
treatment?
flexion and abduction, while in rotational A1: To motivate my patient I can express my
movementes the degrees remain unchanged.
empathy
Anyway the patient was more motivated, than
and
explain
her
the
program
treatment and the benefits of it. The patient
the first day of treatment. (Table 2)
should have, also, the support of her family, helping her to keep adherence to the treatment and feeling motivated.
In the following treatment sessions, I added Codman’s Pendulum exercise for shoulder, to improve ROM and decrease pain; closed and
DAYS 2-4
open kinetic chain exercises, like lean the hand
The following days of treatment were different
against the wall or with a ball against the wall
compared with the first one, maybe because her
doing
husband returned to Madrid, to support her
articular stability, neuromuscular control and
wife. The husband presence influenced the
coordination.
treatment, helping M. to have an active role in the treatment program and to be more
diferents
movements,
to
improve
After 20 days of treatment the shoulder passive ROM improved of 20 degress more in flexion
and abduction, 15 degrees in internal rotation
could be: in a supine position getting the arm up
and 10 degrees in external rotation. The end-
overhead while lying down, using the opposite
range pain decreased in all movements. (Table
arm to holding it; getting the arm to externally
2)
rotate while standing, opening and closenig a door; Internal rotation could be performed using
STUDENT REFLEXION
a towel behind the back, relying on the right
The treatment’s results were good. I think this
shoulder to stretch the affected one.
treatment program is adequately and efectively in the patient presentation. Also, the emotional role of the patient changes and she’s very happy for the treatment and the results.
Q2.Which part of your management do you think has worked better and why? A2: I think the part, which was worked better was the treatment plan, especially from day 2. I planned exercises that could be appropriate for
I am very motivated and satisfied about the
the patient presentation. The anamnesis and
treatment results.
the physical examination helped me to diagnose the patient disease and to produce a treatment
I think that if the treatment will continue in this way, I will be able to improve more shoulder
plan that could be good for the patient. The
motion and decreased pain definitively.
results revealed to me that the treatment plan was good. The ROM increased, the pain
QUESTIONS TO IMPROVE REFLEXION Q1: Do you think that is useful and a good idea to recommend her to do some kind of exercises in her home? A1: Now that she begins to be motivated, I think
diminished, and the patient now is more motivated and can move forward to a symptoms improvement and a better recovery. Table 2 (F:Flexion; IR:Internal rotation; ER: External Rotation; ABD: Abduction)
it’s the better time to recommend her some
P-ROM
F
IR
ER
ABD
home exercises, because she’s more prepared to
After 1 week
+15°
/
/
+10°
keep adherence to the treatment and to have a
After 20 days +20°
+15°
+10°
+20°
Present-day
55°
40°
90°
active role in the recovery. Some exercises 120°
41
FINAL STUDENT REFLEXION This clinical case made a significant contribution in my professional and human growth. I learned to have empathy with the patient. It’s important to help the person also in her emotional issues. At the beginning was complicated to analyse the patient’s symptoms, but with the physical examination and the tests I was able to diagnose the disease. The emotional role of the patient had an important influence during the treatment.
42
I learned that the family and psychological support is very important for the patient, especially in patient with a long-term disease. The treatment results makes me think that I had plan a good treatment program for the patient, although still have a long way to go before she can be considered completely cured. REFERENCE LIST 1. Sardella White, S., & Garbe, J.R. (2010). Thyroid Disease: Understanding Hypothyroidism and Hyperthyroidism. Boston: Harvard Medical School. 2. Oliva, F., Berardi, A.C., Misiti, S., & Maffulli, N. (2013). Thyroid hormones and tendon: current views 3. and future perspectives. Concise review. Muscles Ligaments Tendons J, 3(3), 201-203. 4. McFarland, E. G., & Kim, T. K. (2006). Examination of the shoulder: the complete guide. Thieme.
A 45 YO. GARBAGE COLLECTOR WITH CHRONIC BACK SYMPTOMS JAVIER SIMON M. AND GUIDO R.
INTRO My reflective clinical case is about a 45 years old male who has pain in the cervical region, lumbar region and dizziness, didn’t suffer any direct trauma, may be related to his job,
I asked him what could be the consequences of his symptoms and he told me that his job as required gain weight because it was operator of garbage. When he described his work he commented that it was not at all satisfied.
garbage collector. The symptoms could be
He commented that did not perform any
related with a slipped disc (medical diagnosis),
hobby or sports, which can lead us to think that
and may be with other aspect like mood.
their emotional level is low, because if work
SUBJECTIVE EXAMINATION
does not satisfy you and no activity that does.
The first day the patient came to the
The most relevant symptoms was neck pain,
consultation derivative of general medicine
back pain, pain in the chest area and tingling in
with sick leave.
superior limbs. Because these symptoms were chronic, he told me that he had made some
My first impression of the patient was a sad and worried person, as he sat in the waiting room without speaking to anyone. When he started to talk to me, commented that he was married and lived with his wife and
treatments before, as Pilates, and private physiotherapy, he improve a bit, but the symptoms did not quite disappear. He hadn´t pharmacological treatment, nor had any personal history that might be related.
son. Only had a family history of osteoporosis and He had pain in the cervical and lumbar from
arthritis.
several months ago. The patient described the pain as annoying, with tension and sometimes
The patient described the pain in the morning
radiated.
with a 9/10 on the VAS scale decreased throughout the day up to 5/10.
One thing that struck me about his pain was that it hurt in any position and any movement.
43
I decided to return to this sphere during and after the physical examination (P/E). QUESTIONS TO IMPROVE REFLEXION Q1: What kind of chest pain he felt and during which movements he felt it? A1: This pain was produce by a antalgic posture,
44
in the physical examination I found that the Pectoralis minor muscles was shorted and had active Miofascial trigger points, and in the visual examination the shoulder was in internal rotation. STUDENT REFLEXION AFTER S/E About my initial hypotheses the symptoms are
I know it, because he felt pain in the stretch and palpation of these muscles.
related with the medical diagnosis, but I think that are something emotional that has been
Q2: Is there any red flag in the history you have
influenced in the perpetuation of it.
to rule out first?
I don´t think that could be related with arthritis or osteoporosis because in the medical test aren´t any signs which has any relation with
A2: No there isn´t any red flags. I can consider a yellow flag the emotional feels of patient and the relation with the pathology.
patient´s symptoms. Q3: So far, which is your guess about the At that time I did not consider the patient's
relationship between the main symptoms?
posture, but because of the knowledge acquired in other subjects this year I could associated to a string anteromedial (AM), which is related to the emotions. This is the representation of the body posture explained by Godelieve Denys-Struyf, and this string could be related with some symptoms of areas of our patients. (1)
A3: In my opinion the symptoms are related with medical diagnosis, because the pain causes by the disk alteration, has provoke some compensation that development other symptoms of patient.
TEACHER ADVICE
deviation 35º and extension 50º movements of
Relationship among symptoms often provides
the trunk, and right rotation of neck 45º.
clues about irritability, severity, and spreading pattern. Drawing a timeline introducing the starting point for signs or symptoms and their evolution, also help us to focus over one area instead of others, as the source could be the same for example.
About muscle balance he didn´t have any alteration, only the shorted Pectoralis minor muscle. And active Trigger point of Trapezius, paravertebral, lumbar quadrate muscles and psoas.
45
Sometimes, the pain in the former presentation
Other test that I realized in lumbar region was
hasn´t to be the most relevant nor the origin of
thumb-ascending test; Gillet test (2) and
the syndrome.
elasticity test and I observed an anterior
PHYSICAL EXAMINATION After know the medical diagnosis, how patient
torsion of the sacro. In dorsal region I realized the Mitchell test (3) and I found a FRSd in some vertebras.
felt his symptoms, I startet with physical examination.
I too realized Adson, Eden and Wright test to kwon if patient had any vascular alteration,
Firstly I did a static inspection, where I
and this test was negative. (2)
observed a little vascular alteration under pectoral fold.
STUDENT REFLEXION AFTER P/E
So I asked him if he had any visceral alteration
Analyzing the information got from subjective
because this could have a relation with the liver
and physical examination, I think that
or stomach.
symptoms are related with that pathology, because of hernia disc and protrusion, he
His posture was important to analysed
started to felt symptoms, and went changing
because represented AM string, antalgic
his
flexion and right lateral deviation of the trunk,
compensation that activate Trigger points,
internal rotation of shoulders, flexion of neck
and decrease the activity of some muscles.
posture.
This
could
cause
some
and extension of head. But maybe the posture was the responsible of Secondly I did the functional inspection, and I
the hernia disc, because bad posture of
found an articular limitation of the left lateral
vertebral bones, cause an alteration on disk
pressure and this could the reason of patient
Q2: So far, which is your first hypothesis with the
alterations.
data coming from C/O and P/E? Which is the
In the physical examination I hadn´t performed
46
data supporting this hypothesis?
a neurodynamic test because I didn’t know
My first hypothesis is hypertonicity because of
how to do it in this moment. After one year, I
he presents Miofascial trigger point, in my
have learned the importance and how to
opinion, activated by a bad posture and stress.
realize this test to patient how present symptoms like tingling.
The data supporting this hypothesis is the presence of Miofascial trigger point in the
So maybe I lost some important information,
palpation that reproduces his symptoms and
to plan the treatment.
the information that patient give me when he
But in this clinical case, I keep thinking that symptoms are very related with emotional state of this patient.
felt pain (for example when he has to gain weight or when he is sitting are related with a nociceptive pain). TEACHER ADVICE
QUESTIONS TO IMPROVE REFLEXION Q1: Do you think that could be useful before start or during the physiotherapy treatment, to help the patient with a psychological support by an expert? A1: In my opinion is a good idea, because our principal objective with all patient are a biopsychosocial treatment, so sometimes this must be multi-disciplinary treatment that in
Our findings during the P/E have to be meaningful for the patient. A positive finding of an unknown dysfunction or pain could lead us into a wrong path if it´s not related with the general presentation. Usually if it is found in first place of the examination. We have to check if this pain is “the kind of pain that the patient used to feel” and is related with his other main complains.
this case. But I found difficult to give patient advices about pay attention to a psychologist or other therapy to changes his mood.
PATIENT MANAGEMENT DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN After analysed the information getting in the subjective
examination
and
physical
examination my diagnosis is that patient disc
herniation, he has hypotonicity in the posterior muscles of the trunk and shortening in
STUDENT REFLEXION AFTER D1 TREATMENT
Pectoralis and Psoas.
After first day, patient presented the same symptoms and the dizziness increased.
The prognosis is positive but has some negative factors like the pathology because it,
Maybe I should choose other technique that
is irreversible without surgery treatment, the
weren´t trust technique.
chronicity of symptoms and the laboral activity. Positive factors are that after others physical treatment he has improves. The plan that I design was to address the following objectives:
Firstly in a short-term the objective
So he had more pain the second day, so I decided to do a more relaxed session applying TENS and magnetic therapy. So after this day I learned to give more importance the mood of patient before choose any technique.
was decreased pain in cervical and
lumbar region.
QUESTIONS TO IMPROVE REFLEXION
Secondly to medium term was to
Q1:
increase ROM at cervical region and
manipulation?
strengthen in posterior and anterior
A1: I did manipulative techniques in order to
muscles of thorax.
get the neurophysiological changes produced
DAY_1 First day I started with an osteopathic manipulation, for the dorsal region I used the “Dog-technique” and for the sacro and lumbar region I did the “lumbar roll”. To decrease tension I did a technique to relax
Why
did
you
chose
osteopathic
by these techniques. It is sought to give a stimulus to restore the SN information about the area and get so hypoalgesia short-term changes in the structures that could be affected (4). DAYS 3-4
diaphragm and other for the Pectoralis minor
The third day my patient had lumbar and
muscles that was a muscular energy technique.
cervical pain; he felts bad and told me that he had have vomit. So I decided to do a relax treatment with manual therapy, the fifth day I did the same treatment.
47
Sixth day the patient hadn´t tingling, the
hypotheses of has a relation with the mood
dizziness had been decreased, cervical pain
my patient.
had been improved but he kept feel lumbar pain.
48
In spite of I recommended him to did some active exercise to make more powerful the
So, for this session my objective was treating
back and deep muscles, because I think that is
the lumbar pain. I used a technique to relax
very important to have a good motor control
diaphragm, I did a compression treatment for
of the lumbo-pelvic region, to decrease the
Psoas Trigger points, contract-relax stretching
back symptoms.
for psoas and a active work for the deep lumbar muscles (Transverse muscle, pelvic floor and
QUESTIONS TO IMPROVE REFLEXION
Multifidus muscles).
Q1: Do you think the patient disease could be related with neurological disorders in addition to
STUDENT REFLEXION I hadn´t the final information before the patient end the treatment but while I was treat it, he had some improves like dizziness and headaches, but the outcomes after each day aren´t very representative because each day had different symptoms, I mean one day he was better of the cervical pain and worse of the
his emotional state? I think that there could be some present peripheral entrapment because I didn´t neurodynamic test and he present numbness in the arm, but he didn’t have any entrapment of Braquial plexum because the Jackson, Adson, Eden and Wright test, were negative.
lumbar pain, and the next day on the contrary,
Q2: Which part of your management do you
so the evolution was very confused.
think has worked better and why?
For me was difficult to interpreted which was
In my opinion the best treatment for this
the problem of patient´s symptoms because
patient was the relax technique a motor
the evolution was very different and when he
control (“rana al suelo” (5) adding a good
improve one symptoms get worse other and
breathing movement to relax diaphragm) and
vice versa.
manual
So I think that I have left loss some information. Maybe I was in a wrong way or this development had relation with my first
therapy.
Because
the
active
participation of patient to get a good control motor in the lumbopelvic region, and being aware how he is relax while he gets control the breath, helps him to get better results.
And the manual therapy at the Trigger point
good decision. Regarding to the neurodynamics
helps to decrease the symptoms and the
issues, we need to discriminate among tests
muscles tensions.
assessing roots, nerve trunks and main nerves.
TEACHER ADVICE
We also have special test to investigate where
Choosing high evidence-based tests will add to your reasoning better ingredients to make a
the entrapment is and its dimension, first step in the management of these presentations.
49 FINAL STUDENT REFLEXION
To conduct further analysis of this case, after a year in which I have acquired new knowledge, has helped me to realize that parts of the exploration had not taken into account and the importance of them such as neurodynamics, spinal mobilization with postero-anterior pressures, the patient's posture that can give us information of structures that are influencing their pathology. For example, in this case with an AM chain, I could choose treatment techniques and address the same depending on the patient, such as given the mood of the patient would have been better to make more moderate techniques: muscle energy techniques rather than with impulse techniques. And remember at all times the importance of the biopsychosocial treatment as in the recovery of the patient and their adherence to treatment is influenced by many factors. And some time that is necessary to do a multidisciplinary work. This has helped me to make a more complete reasoning and relating and integrating more different fields of physiotherapy I've been studying
REFERENCE LIST 1. Lucas, E., & Ángeles, M. (2009). Análisis biomecánico de las algias de raquis y su relación con la percepción del dolor y la calidad de vida. REDUCA (Enfermería, Fisioterapia y Podología), 1(2). 2. Cleland, J. (2006). Netter, exploración clínica en ortopedia: un enfoque para fisioterapeutas basado en la evidencia. Masson. 3. Ricard, F. (2007). Tratamiento osteopático de las algias del raquis torácico. Ed. Médica
Panamericana. 4. Pickar, J. G. (2011). Efectos neurofisiológicos de la manipulación vertebral. Osteopatía científica, 6(1), 2-18. 5. Souchard, P. E. (2005). RPG. Principios de la reeducación postural global (Vol. 88). Editorial Paidotribo
50
A 23-YEAR-OLD FEMALE PREPARING FOR ARMY WITH LOWER BACK PAIN FOR 4 WEEKS KRIIK G. AND PONCE L.
INTRO My client was a 23-year-old female student with lower back pain, which had started 4 weeks earlier due to heavy weight training.
where she wasn’t able to put on shoes in the locker room when leaving the gym. After this the pain had been troubling her especially on the left side of the back. Also a tendon had started snapping on her right hip.
SUBJECTIVE EXAMINATION My client was a 23-year-old woman who was in the second year of her studies in the field of physical therapy. She was living together with her boyfriend who was studying in the military academy, and it was her goal to join the army too. Due to lower back pain resulting from extensive training she came to the clinic. Her aim was to get back on track with training again soon, because the entrance test for military studies was a few months away. She was 165 cm tall and weighed 52 kg. She hadn’t had former traumas
She had tried to relieve the pain by stretching and trying to find a painless position. During the day sitting worsened the pain, and sitting through a lecture at the university was agonising. Because of this she had started to attend the lectures standing up. At home she had exchanged the sofa for a fitness ball. The pain was most severe in the evenings and after sitting down for a long period of time. Lying down eased the pain. She had found sleeping on the side with a pillow between her legs the best position for her.
associated with the pain. During her free time she was involved in many My client had started a comprehensive weight training program a few months earlier in order to pass the entry tests for the army. A month ago she had started to experience lower back pain after training. Two weeks before coming to the clinic the pain had been intensified to an extent
kinds of activities: walking her dog, going to the gym, swimming and at times also climbing. At the gym she usually trained with free weights together with her boyfriend. They trained at a “men’s gym” without contemporary adjustable gym equipment.
51
At the gym the most pain inducing exercise was
QUESTIONS TO IMPROVE REFLEXION
deadlift, which she usually did with 20 kg weights
Q1: So far, which is the level of severity and
3 x 10 repetitions. She said that she knew she was
irritability of her presentation? How is this going to
executing
impact on your plan for P/E?
performing
the a
movement squat
wrong
deep
without
enough.
She
recognized that also in her everyday life she was moving in unfavourable ways by having a habit of
52
not bending her knees while picking things up from the floor. She suspected that she had been engaging with a training program too hard for her fitness level, because she was training at the same tempo with her boyfriend.
A1: At the time of her therapy session the severity of the pain had been decreased to a level where it presented moderately in certain positions and movements. The pain affected her movements, activities and behaviour and in order to begin the healing process I felt it was extremely important not to irritate it any further. Thus I planned to be careful with the physical
STUDENT REFLEXION AFTER S/E
examination in order to avoid provoking excess
Based on the interview and her description of the
pain.
onset of the pain I suspected a disorder in
Q2: Do you think she should rest and stop lifting
neuromuscular control in the core area. My
weights?
hypothesis was that she was training with weights too heavy for her level of fitness and
A2: Yes, in order to recover she should rest for a
technique, and while she was performing the
sufficient amount of time, and afterwards
deadlift her back extensors failed to uphold her
gradually get back to weight training.
posture, resulting in a flexion in the lumbar spine,
Q3: Did you think about other forms of getting
and creating an increased torque that caused
prepared for the army?
significant pressure to the intervertebral discs and extreme tension to the surrounding tissues.
A3: She should train by doing versatile exercises. Because she already had a good selection of
I sensed that there was pressure for her to get
other physical activities she was engaging in, I
back on track to the training routine, and thus I
especially wanted to give her an alteration for
expected a challenge in motivating her to
weight training.
patiently commit to the therapeutic exercises. TEACHER ADVICE The degree of irritability and severity will drive the deepness of the P/E procedures. If we are not
cautious, a tough physical testing could ruined the
In the forward flexion the lumbar spine rounded
remaining management if we provoke elevate or
only at the end of the flexion, and up until that
severe symptoms in a highly irritable presentation,
point it was almost completely straight. In the
that avoid proper and comfortable following
modified Schober test lumbar spine lengthened
procedures.
in forward flexion 6 cm while standing and 5 cm while seated - which is within the reference
PHYSICAL EXAMINATION Day1: I started the physical examination by assessing my client’s posture and active movements.
values, but in the low end. Especially in the first forward flexions she conducted there was a visible functional scoliosis present. Her body also flexed to the right side, over her right lower extremity.
Her ankles were in line and in her feet she had symmetrical and strong longitudinal arches. There was no pronation in the ankles. Knees were slightly asymmetrical: the right ham was slightly lower than the left one. Also the right gluteal fold was a little lower than the left one. The iliac crests were horizontally aligned. Knees were directed to the back into a locked position and the pelvis had drifted to the front and tilted anteriorly. In the lumbar spine she had a normal lordosis but the kyphosis in the thoracic spine had straightened. Scapulae were symmetrically aligned, both by their distance from the spine and the height of their position. However the scapulohumeral rhythm was slightly asymmetrical: the right scapula moved smoothly but the left one did the same abruptly. In the cervical spine she had a normal lordosis.
Lateral flexions were symmetrical and the spine flexed evenly. Lateral rotation to the right was smaller than to the left. Single leg squat revealed larger weakness in the right gluteus medius than in the left one. On the right side in the anterior part of the hip a tendon was snapping as she flexed her hip. In the movement control test for the core there was no lack of control present. However, as a physical therapy student she did know what this test was about and perhaps was able to concentrate to not show positive signs. In the Straight Leg Raise Test her left leg raised smoothly over 90° but the hamstrings in the right thigh started to strain at 90°. In the Thomas Test there was no tightness in the iliopsoas muscles presented. According to palpation during a single leg hip raise the transversus abdominis muscle activation was slightly stronger on the left side than in the right side.
53
As first aid for her condition I gave her advice
medius
about a painless position. I also advised and
quadratus lumborum was not painful. While
encouraged her to actively keep up a better
conducting a stretch to the muscle, there was no
posture in which her lower back is not under
tension present and the stretch was symmetrical
stress.
on both sides. By palpation the lumbar spine was
There
During
palpation
m.
more flexible than the thoracic spine. The tonus
Day 2:
54
weakness.
in the back extensors was symmetrical in were
aspects
that
needed
closer
transversal manipulation.
examination and due to lack of time were not examined during the first session, so I decided to
STUDENT REFLEXION AFTER P/E
make a few more tests to confirm the most
My initial hypothesis during the first therapy
accurate diagnosis and management.
session was that she had a disorder in neuromuscular control in the core area. However
During the second therapy session there were no more signs of functional scoliosis present in forward flexion. It is possible that the muscle tension present before had loosened and did not pull the spine into an asymmetrical position. Lateral flexions and rotations were symmetrical. While squatting m. transversus abdominis stayed active and the lining of the knees remained. In the single leg squat m. gluteus medius failed on both sides. In forward flexion the movement of SI-joints was symmetrical. However the left side of the hip raised while raising the left knee, while the hip stayed in place when raising the right knee. There was no pain when compressing the SI-joint.
when she didn’t present any positive signs towards the lack of control, I had to change my presumption. In our first session we had gone through different factors in the core area, but did not have time to profoundly examine the pelvic area. That is why I decided I needed to conduct more tests in the second session. Between the sessions I had gone through numerous options which could be the cause for her pain, and expected to come into a conclusion after better examining her pelvic area and movements. Before the management phase I put a lot of thought into how to make therapy appealing to her. I felt like I had to balance between exercises that were not too difficult for her in order to
In the Straight Leg Raise Test hamstring stretch
maintain the right load and the therapeutic
was symmetrical and no tension presented. In
aspect, but also challenging enough for her to
the Donatelli Drop Leg Test the leg dropped ~10
stay motivated.
cm on both sides which refers to m. gluteus
QUESTIONS TO IMPROVE REFLEXION
TEACHER ADVICE
Q1. Which is the most important piece of data
No general advice could be provide to choose the
supporting your hypothesis with this patient?
most relevant information in the P/E. It has to be a
A1: The most important piece of data was the muscle imbalance presented by her poor posture and the evident weakness of her gluteus medius muscles combined with the information about the high intensity of her training and her unstable technique. Q2: Do you think she has a preference for the right
personal decision that could be shared with the expectations and feelings of the patient. Your experience and knowledge will drive you to this part of the decision-making after performed the
55
best evidence-based tests procedures. PATIENT MANAGEMENT
side of the body at the moment she performs the
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
movements and that it makes it stronger than the
My physical therapy diagnosis was that the client
left one on the lumbar rotation?
suffered from an unbeneficial habitual posture
A2: Based on the observations and tests I believe she has a habitual imbalance in her posture - and during heavy weight training the weaknesses in certain parts of her body have provoked an
caused by muscle imbalance, and muscle tightness and weaknesses in the pelvic region, which in high intensity weight training provoked pain into the lower back.
increasingly unbeneficial posture. Her posture
The objective for therapy for her was to correct
includes dominant elements in both right and
the posture and to learn proper movement
left side of her body, but they are unsymmetrical.
control and right movement trajectories in order
Q3: What do you think you could do to avoid her not showing the positive signs of the test you asked her to perform? A3: If she is very aware of the tests and her
to be able to train with weights. After the first physical therapy session the aim was to locate a painless
position,
avoid
pain
provoking
movements and to start practicing the right kind of posture.
performance, it could prove beneficial to ask her to describe in detail if she feels weaknesses or if one movement is harder than the other. Asking her to talk could also make the movements more natural and intuitive.
After the second therapy session the objective was to strengthen the deep postural muscles and to learn a deep, relaxed way of breathing during exercise. In order to reach a strong posture gluteus medius muscles had to be strengthened.
In the early stage of therapy the aim was to cross-
These exercises she was to do with every training
strengthen the core muscles in myofascial chains
session in order to learn to sustain core activation
both in the anterior and posterior side of her
when functioning.
body.
56
In the advanced stage of therapy the goal was to
2. EXERCISES TO STABILIZE PELVIC REGION
enable weight training. The objective was to
In order to stabilize the pelvic region I gave her
comprehensively train the musculature starting
exercises to strengthen the gluteus medius
with simple technique exercises and moving
muscles.
onto wider trajectories.
-
stepping board (3 x 10 on both sides)
In order to develop a strong muscle control I gave my client exercises to strengthen her postural
lifting the hip while standing on a
-
lateral rotation of a flexed lower limb
core muscles. In order to correct her posture I
while lying on the side (3 x 10 on both
taught her an optimal position for knees and hips,
sides)
and to stabilize her pelvic area I gave her
-
abduction of the foot while standing -
exercises for strengthening gluteus medius. In
first without a resistance and later using
order to keep her motivated I composed a
a rubber band (3 x 10 on both sides)
therapeutic training program for the advanced stage so she could witness her own improvement and not get bored with a lack of options. 1. EXERCISES FOR DEEP CORE MUSCLES To strengthen the activation of postural core
In order to keep the therapeutic training interesting and appealing she was able to choose an exercise for each session. 3. EARLY STAGE In the early stage I prescriber her
muscles I instructed her following exercises: -
vertically pulling down and bouncing a rubber band (m. transversus abdominis) (10 sec activation + 10 sec rest)
-
-
-
crossover crunches (3 x 10 on both sides)
-
by turns lifting up one hand and the opposite leg on all fours (3 x 10 on both sides)
moving the body weight onto a foot stepped forward, walking backwards
4. ADVANCED STAGE
(mm. multifidi) (5 times on both sides)
I advised her to conduct the early stage exercises
relaxed and deep breathing when
as long as she had fully learned the movements
exercising (diaphragm)
and the postural control was stable. When she
would have mastered them she could move on to
shape than before, and also to keep her
more challenging exercises. This way her training
motivated and committed into. We agreed with
was as progressive and motivating as possible. In
her that she will incorporate these exercises into
the advanced stage I gave her following
her routine and exercise independently, and
exercises:
after 6 weeks, during a follow-up contact she had
-
pulling down across to the front a pulley while crunching the opposite knee up (3 x 10 on both sides)
-
pulling down across to the back a pulley
been able to start training again with a better technique and a clear knowledge about the required movement control.
while extending the opposite leg back (3
STUDENT REFLEXION AFTER TREATMENT
x 10 on both sides)
Because my client was an active young woman
I advised her to start the advanced exercises with small resistance and moving onto heavier weights while paying strict attention to her condition and movement control.
with a concrete goal in her weight training, I didn’t want to solely give her exercises for the early stage, because she might have found it boring it could have resulted in her not sticking to it. I wanted to build a bridge between her state at
5. ALTERATIONS FOR DEADLIFT
that time and the stage she wanted to be in. I was
Because deadlift was a movement she was fond
concerned whether I was able to give her all the
of, I wanted give her an alteration to make it
information and support she needed to
possible for her to safely train the muscle groups
independently conduct the therapeutic exercise
that the movement incorporates. With the
process.
alteration she would be able to train the same muscles but in a safe and technically more simple
QUESTIONS TO IMPROVE REFLEXION
way. I instructed her:
Q1: Which part of your management do you think
-
-
squat (3 x 15), and possibly later a
has worked better and why?
telemark-squat (3 x 10)
A1: Based on the feedback I received from my
rowing both bilaterally and rotating the
client after her therapeutic practice period, the
trunk
core as well as m. gluteus medius strengthening
This progressive therapeutic exercise plan aimed to return her into the training routine in a better
exercises have proven to be the most beneficial for her. Once she was able to support a firm posture she avoided provoking pain even in
57
complicated movements. A strong core has given her the possibility to enjoy life without pain.
TEACHER ADVICE As we read previously patients’ needs to have a general idea about the length of the treatment.
Q2: What about the recovering time? Did you have
Information about this point could be found in
an idea about how many weeks the treatment
clinical reports for individual patients. Despite is
would take long?
not one best researched issues in physiotherapy, there are some populations in which these findings
58
A2: I estimated it would take her 3 months to reach the advanced level in practicing if having successfully undergone the therapy.
are extremely urgent and relevant, for example in the
professional
sports
area
where
time
constraints costs lots of money to the clubs.
FINAL STUDENT REFLEXION In order for her to properly learn the optimal movements I started the therapy plan with low-intensity training (Kisner & Colby, 2012). Especially with patients with lower back pain it is important to render activation in the deep postural muscles such as m. transversus abdominis and mm. multifidi. By increasing the activation of m. transversus abdominis the risk of generating lower back pain decreases (Miura et al. 2014). Because of this I included stabilizing exercises into every training session of her plan. In her case it was also extremely important to strengthen m. gluteus medius, which is a stabilizing muscle for the pelvic area. I chose exercises that have been proven to be the most effective in creating muscle activation in m. gluteus medius. (Bolgla & Uhl, 2005. Gowda et al. 2014.) In my opinion she comprehended the instructions well and also was committed and eager to execute the plan of therapeutic exercises. I was glad to hear her positive feedback later and excited for her recovery.
REFERENCE LIST 1. Bolgla, L. and Uhl, T. (2005). Electromyographic Analysis of Hip Rehabilitation Exercises in a Group of Healthy Subjects. JOSPT Journal of Orthopaedic & Sports Physical Therapy. 2. Gowda, A., Mease, S., Donatelli, R., Zelicof, S. (2014). Gluteus medius strengthening andthe use of the Donatelli Drop Leg Test in the athlete. JOSPT Journal of Orthopaedic &Sports Physical Therapy.
3. Kisner, C., and Colby, L. (2012). Therapeutic Exercise. Foundations and techniques.. 4. Miura, T., Yamanaka, M., Ukishiro, K., Tohyama, H., Saito, H., Samukawa, M., Takumi Kobayashi, T., Ino, T., Takeda, N. (2014). Individuals with chronic low back pain do not modulate the level of transversus abdominis muscle contraction across different postures. JOSPT Journal of Orthopaedic & Sports Physical Therapy.
59
A 40 YO. MAN WITH A PAINFUL SHOULDER SYNDROME PÉREZ G. AND KRIIK G .
INTRO
60
A 40 YO man, who handle Remotely Piloted Aircraft Systems (RPAS), in Mexico, which has a
as soon as possible to return to his daily activities. He is married and they have 2 girls with who wants to play again without pain.
painful shoulder syndrome on both sides, as a
He said that the pain on his shoulders started 2
consequence of many years working at the same
years ago but he only felt kind of discomfort and
position by long working hours.
he didn´t attended it, along of time he feels only
SUBJECTIVE EXAMINATION One day a 40 YO man, with 40 years old came to the clinical rehabilitation where I was doing my practices. He was 1.78m tall and 89 kg of weight. He handles a Remotely Piloted Aircraft System (RPAS) for a company in Mexico, almost always Monday through Saturday 8 hours with an hour of break, but he was handles the drone for 3 or 4 hours with the same position without any break to stretch or eat either. He describes his position as a super video game player, stand up, arms down, elbows 90°, and loading the control with 2kg of weight.
got worse and neurological symptoms on his arms on few times. He has token NSAID, muscular relaxants & hot water fomentations, 3 weeks felt kind of better, but 2 months later the discomfort begun again harder and his wife carried him to the doctor because the pain increase each time more, presented swollen shoulder and red zone, and sometimes cannot work but he only said ¨it will pass, I´m ok! ¨. They went first with a public doctor, where he has the insurance and take a Rx to see the acromion position, and it was good, but he said the doctor´s
diagnosis
was
¨Painful
Shoulder
Syndrome¨. Then, he went to the traumatology,
He is working on that place since he was 20 years
and he said to him the same diagnosis.
old. He had taken a course for pilot the drone to
Consequently, the doctor gives to him medical
begin work, and a long of time he has been
prescriptions to decrease the inflammation and
updated until nowadays. He was born and grew
pain, relax the muscles and the numbness
up in Mexico, he´s very sympathetic, funny,
disappears, and furthermore sends him to begun
friendly, simple, positive and waiting to recover
with physical therapy sessions.
His pain becomes chronically because he didn´t
test maybe as 1UNLT & 2UNLT to be sure that he
attend at time and at the work give to him some
hasn´t any nerve entrapment.
days to rest.
He has a good prognosis because he is very
He smoke occasionally like 1 cigar each weekend
motivated and anxious to recover full ROM to
and was an occasional social drinker.
return to his normal life, he has a very positive
He presents pain on abduction, extension, flexion (less pain with elbow flexed than with elbow extended), internal and external rotation, but in adduction he doesn´t present pain. At the
attitude and perseverant. QUESTIONS TO IMPROVE REFLEXION Q1: Which were the activities that ease his symptoms?
same time he has several limited range of motion. He presents a lot pain when try to hung out his
A1: When he applies a thermal compresses, and
clothes on the closet, brush his hair, take a
when he rested a day or two of work.
shower, dress and every activity that implicate put his arms up. He feels better when his wife put to him socks with hot rice on his shoulder. STUDENT REFLEXION AFTER S/E
Q2. Which is your opinion about central sensitization component in his pain presentation? A2: I think the main component on his pain is the muscle
overload
that
causes
a
chronic
inflammation without care on time.
About my hypothesis is a mechanical input injury,
Q3: Does he have identical pain in both of his
with possible tissue damage. He has a lot of time
shoulders? In his work, did he usually do the same
with the pain, so it comes to be a chronic disease,
task with both hands?
it could be slower to recover than a acute pain. He didn´t receive any therapy from a specialist, only the home remedies that calm a little the pain. My first impression at all was a big contracture of upper limb, back and neck. First of all, I could do explorations to verify which muscle is more damaged, and to neurological
A3: He doesn’t have the pain as a specific point he feels pain around shoulder and neck. Furthermore, he used to do the same with both hands (take a motor control). Q4: Is possible for him to work shorter periods or take a break? A4: He said that is not possible to make a break because when begin to record is hard to pause it.
61
any inflammation about bursa. And finally he
TEACHER ADVICE It´s important to cover, at least, the main issues in
refers more pain at night.
the first visit to allow you to manage all the pieces of the quiz. Missing key issues as red flags could decrease the quality of your management and set
STUDENT REFLEXION AFTER P/E About the diagnosis of doctors, I found that he has the muscles inflamed and whichever
your patient in risk
movement that he did, he presented pain,
62
PHYSICAL EXAMINATION
consequently very limited his range of motion.
He brings radiographies and the acromion
Although, he said he begun to feels better with
doesn´t indicates a possible impingement. He
de NSAID´s he want to be all right as soon as
doesn´t have a specific point with pain on his
possible. I found same kind on limited on
shoulders, so I decided realize test for the rotator
external and internal rotators (as subescapularis
cuff muscles and examine his ROM and posture.
and Infraespinatus), and on muscles as that have function of flexion, extension, abduction, the
He presents head anteversion, winged shoulder
right side has more restriction, but in adduction
blades and a little left side descending.
the rom wasn´t limited just at the end present
The range of motion on left shoulder:
pain. I think he has more restriction on his right
-Flex (L / R) 45°, 40°
shoulder because his dominant hand at business
-Left ABD (L / R) 40°, 35°
is right side, so it overloads a little bit more the
-Add (L / R) 30°, 32°
muscles. Moreover, all the test he present
-Ext (L / R) 35°,30°
positive because he continues with inflammation
-ER(L / R) 40°,40°
and overload muscles for his work , tension
-IR (L / R) 40°,40º
position and those are contributing factors. He present very good attitude and that have good
On Jobe`s test was positive both sides, Patte´s
prognosis with NSAID and therapy he going to
test was positive (same on both sides),
belly
recover but exactly I don´t know the time.
press was positive, Gerber was positive (same on
Moreover, he doesn´t presents an anatomical
both sides), Yergason was positive too (more
deformation of acromion, just muscular so it
limited on his right side). I did Neer and
becomes better for his luck.
Hawkins`s tests too, Neer was positive on both sides, but Hawkins was negative. Furthermore,
QUESTIONS TO IMPROVE REFLEXION
on the radiographies can observed that has not
Q1: Did you advise a painless position for him?
A1: He has painless when he has his arms down.
TEACHER ADVICE
Q2: Was he still working at the same time of
Getting the most reliable tests for a typical
therapy? Do you think it´ll affect your work
presentation is the key point to get a chance in
strategy?
discovering a tissue dysfunction.
A2: He continues working fewer days and fewer
PATIENT MANAGEMENT
periods of time. I think it can make slowest rehabilitation but not totally affect. Q3: Which is your second hypothesis for the data coming from P/E? Shoulder bursitis. Which is the
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN About the diagnosis of the doctors and my point of view I met consistent findings about the painful shoulder syndrome. I had doubt then with
data supporting this hypothesis?
shoulder bursitis, because the impingement Shoulder bursitis is include the alterations of
shoulder was rule out with the radiographies, but
muscles, tendons, nerves, tendon sheaths, joint
on the radiographies has not appeared.
syndrome and neurovascular entrapment and
Furthermore he made MRI and only has
more pain at night. He has pain on all
appeared inflammation of tendons. I think he
movements
as
was good because he doesn´t present any
radiographies and magnetic resonance can rule
neurological symptom last 3 months, and he is
out impingement and bursitis.
more relax on his work and his wife is supporting
Approximately 10 % of the general adult
him, physical and psychologically.
and
with
the
studies
population experiences an episode of shoulder pain in your life (Van der Heijden, 1996) shoulder pain is the third leading cause of muscle skeletal pain extends to shoulder and back (Cailliet, 1981) .The risk that the pain persists beyond acute phase seems to be related to lack of treatment, and occupational personality factors (Van der Heijden, 1999).
The plan to reduce inflammation with help of the doctor
and
some
NSAID´s,
and
TENS,
thermotherapy, relax and therapeutic exercise. DAY_1-2 Applied TENS on his shoulders and furthermore thermotherapy with hot-wet compresses at the same time to release the pain and relax the muscles, then applied ultrasound on the area with more pain. Then told to him that he should relax for all day and don´t do any heavy work. And on the afternoon he applied an NSAID on gel.
63
STUDENT REFLEXION AFTER D1 TREATMENT
on 3rd and 4th days added pendular of Codman
The patient came with a doctor prescription. And,
mobility and muscular potency, and decrease the
he feels better with thermotherapy, so it can
pain.
exercises, and laser low potency to improve the
helps to relax the muscle and psychologically too.
potency, massage and finally 2 repetitions on
QUESTIONS TO IMPROVE REFLEXION
64
5th: add pendular Codman exercises, laser low
Q1: Did you give him instructions on how to relax
finger ladder on flexion and abduction.
his muscle at home-other than NSAID? STUDENT REFLEXION A1: only the pendular exercises.
The patient was happy because he feels his
Q2: Did you have an estimate on how many therapy sessions it would take to improve
shoulder been better and won ROM con 4 sessions. Moreover, his attitude was so positive on therapy and on house because obey all
Roberto´s state?
instructions. Furthermore, he and would gladly A2: I think near of 15 sessions.
therapy because he spoke with more people, so I think that psychologically these attitudes are
TEACHER ADVICE
best for speedy recovery.
A “test-treatment” will allow you to get invaluable information
about
the
condition
of
the
presentation. Using the results of the treatment as another piece of evaluation could inform you how to treat your patient properly. If we use a huge
QUESTIONS TO IMPROVE REFLEXION Q1: Have been your management different if you didn´t have the MRI images? Were they valuable for your results?
number of techniques in this first session, we will be less sure about which has worked better.
A1: Yes, because if we had found any abnormality as a rupture of rotator cuff, bursitis
DAYS 3-5
or even a tumor should be care with those things.
For days 3, 4 and 5 applied, TENS on his shoulders and furthermore thermotherapy with hot-wet compress at the same time to release the pain and relax the muscles, then applied ultrasound on the area with more pain. Moreover
Q2: Would he only continue his treatment at home? A2: He continues with the therapy on the clinic, but I kept giving no therapy because I was moved to another patient.
FINAL STUDENT REFLEXION All the clinical case was with help of my coordinator of practices, although we add some therapies methods. But here I would like to improve on the physical examination explore the neurological examination,
Daniel´s
scale
(muscle
strength
power).
With the treatment can be helpfully to his body but a placebo effect can be influent too. The treatment in four sessions began to show results, but those results were for the good and positive attitude for the patient, discipline at home, and he toke less hours on his job. The syndrome of shoulder pain is not exactly pathology but we can rule out other possible symptoms and treat that one. The best thing to do in all people is prevent a lesion give them some recommendations and ergonomic positions, and take a few minutes to take a break and relax on the work, in addition when we feels symptoms out of common we should go to the doctor or physiotherapist to check it and not allowed to continue advancing the affection.
REFERENCE LIST 1. Cortes V., Acosta M., Armendárez M., Domínguez M. J. Romero P. (2009). Guía de Práctica Clínica, Diagnostico y Tratamiento del Síndrome de hombro doloroso en primer nivel de atención; Delegación
Cuauhtémoc,
México:
CENETEC.
http://www.cenetec.salud.gob.mx/descargas/gpc/CatalogoMaestro/085_GPC_SxHombdoloros o1NA/GPC_SHD_EVR.pdf 2. Hernández Díaz, A., Méndez, G., Orellana Molina, A., Martín Gil, J. L., & Berty Tejeda, J. (2009). Láser de baja potencia en el tratamiento de las calcificaciones de hombro. Revista de la Sociedad Española del Dolor, 16(4), 230-238. 3. SUÁREZ-SANABRIA, N. A. T. H. A. L. I. A., & OSORIO-PATIÑO, A. M. (2013). Shoulder's biomechanics and physiological basis for the Codman exercise. CES Medicina, 27(2), 205-217.
65
A 16 YO. FEMALE STUDENT THAT SUFFERED A 2 ND GRADE RIGHT ANKLE SPRING PONCE DEL-HOYO L. AND PEREZ-RAYMUNDO G.
66
INTRO A 16 yo. girl who was a football player suffered
forward position so she wanted to score the last point before the game finished.
an second grade ankle spring on the right
She was running really fast and got the ball but
limb .There had passed 3 weeks since she
suddenly one player of the other team kicked her
suffered the spring. She was immobilized during
really hard on the lateral part of her ankle and she
these 3 weeks, now she has a lot of complications
felt down and because of the velocity she was
with the functionality of her ankle.
running she felt on the ground. The pain
SUBJECTIVE EXAMINATION When my patient arrived to the clinic where I was developing my clinical stance or practices, she was using crutches because she felt pain when she supported the foot down on the floor at the moment of walking. She said on the consultation with the doctor (I was present during all the examination) that she had had an accident while she was playing football in her high school. She was part of the school’s team and she was training for the competition than is done every year between the different grades of the school. When the accident happened, the game was on the second period and her team was winning for 2-0 points, so their team was feeling kind of security against the other team. She had the
appeared just when she tried to stand up again. “I could not support my weight on my leg. Firstly I felt like if I had lost all my strength and then a lot of pain started to came to my ankle. It was insupportable. “I would not have had cried, but I could not resist, the pain was so hard” she said. When everyone noted that what had happened to was not a simple drop, all the players went to the place where she was layed dowm. They started to call the trainer and when he arrived he had already called an ambulance. He ask her what had happened but because of her crying, she said that she could not say many details of what had happened. The other player that had kicked her was how explained what had happened. Then she did not noticed exactly what happened until the ambulance arrived, and she
was taken to the hospital. In the hospital she was
proprioception, because if not, she would get
taken to the X-ray department and the
injured again. She does not have any important
traumatology discarded a possible fracture. He
antecedent. She is a healthy girl, does exercise
told her that she had had an ankle sprain and that
constantly and take a good diet. So my first
she was going to rest and take some medications.
impression was that she was going to have a
The doctor put her splint on her ankle and said
good prognostic if she follows all the therapy to
that she was going to be immobilised during 4
the letter.
weeks. She took the prescribed medications so
67
she did not feel so much pain on the next weeks.
QUESTIONS TO IMPROVE REFLEXION
The pain came back at the moment that the
Q1: Was there any deformity on her ankle?
splint was taken off. She was really surprised because her leg was so much thinner than the other one, and her foot too. She refered to had
A1: Yes, there was a relative deformity, because it was with less muscular mass and with inflammation
pain at the moment she tried to put all her weigh on his right foot. She also felt kind of restriction
Q2: Which data of the history supports your
of the movement.
hypothesis about lack of proprioception?
STUDENT REFLEXION AFTER S/E About my hypotheses of my patient´s injury is that, well she already had a certain medical diagnosis, a second grade right ankle spring. But
That she was immobilized, so she did not stand during three weeks and that makes the baroreceptors get damaged. If it is not corrected she is really exposed to have another spring.
what I could observe while she was describing
Q3: Which are going to be your precautions for the
her situation, was that she was really worry
P/E?
about if she was going to recover properly or not. She was scared because she had never seen her foot that thin and weak. I also noticed that she did not have enough proprioception because she was always seen to her ankle and moving it with her hand to be more comfortable (it due to avoid wrong positions of hes foot and avoid pain). I thought that what she needed was firstly to decrease the pain. Then gain strength and
Avoid pain is the principal precautions. The ligaments are almost recovered, (because it was a 2nd grade not 3rd) but she is still in pain. TEACHER ADVICE It´s important to remember that our physical proceedings could damage the patient. As usually passive examinations are testing tissue response, if we do not dosage them properly they could harm
that tissues. We need a proper evaluation of the
Movement
Strength
ROM
Dorsal Flexion
3
10°
Plantar Flexion
4
20°
example, missing the potential risk fall of a
Eversion
3
10°
balance test, could provoke a harsh result.
Inversion
3
10°
severity of the presentation at this point. But there are other tests for different dysfunctions that could put our patient in danger too. In
68
PHYSICAL EXAMINATION When the doctor started the physical exploration (I was just looking), the patient was kind of scare
Passive movements were the same range of movements but with a little of restriction to make the natural joint movement.
because she said that had not had a really good
He did not explore the gait because the patient
experiences with other medical processes. So
felt with insecurity at the moment of stand in
she did not wanted to know that she was going
both limbs.
to have a bar recovering. Comparing with the other limb this was the The doctor started exploring first by observation
results:
of her ankle, not her posture, because she could not stay standed up without pain. The doctor
Movement
Strength
ROM
found that the skin around the ankle was rubbish
Dorsal Flexion
5
20°
Plantar Flexion
5
40°
Eversion
5
20°
Inversion
5
35°
and warm comparing with the other ankle. Then he palpated the area, and it was swollen and inflammated. She referred her pain in level 4 in EVA scale at the moment of stand all her weight on her right foot. After that he started to evaluate the range of movements and strength in Daniel´s scale and this are the results in active mobilization:
STUDENT REFLEXION AFTER P/E I think that the Physical Exploration was kind of obvious, because the patient already had the diagnosis made at the moment she had the lesson, and it was corroborated with a radiography, so it was just to check the actual symptoms and problems she had on her ankle.
And when the doctor said the results of the test of strength, I thought it was relative, because he evaluated the movements but without causing pain, so I think the patient could have done more
TEACHER ADVICE At the end of the physical examination we need to take back a step and think for a while if data coming from S/E and P/E fits in some way.
strength even if she had felt a little of pain. If do so, it´s the moment to make out a working list The other ankle had so much more strength than the affected one because she had had to walk standing just on one foot, so she had to improve the range of movement and power of the health one to compensate the lack of the other ankle.
with the most reliable hypothesis for current patient´s presentation. At the top of this list will be the syndromes with higher likelihood to be present, and remains in the therapist ability to stablish which of them will be the working diagnostic hypothesis during the treatment session.
QUESTIONS TO IMPROVE REFLEXION Q1: Do you think your patient is going to have a fast recovering? Yes, I think she has a really good attitude and
PATIENT MANAGEMENT DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
also positive factors to get back to play football
Thinking in my hypothesis, I beat that what she
again as soon as possible.
needs is really clear. Her ankle had suffered the consequences of the immobilization, so we need
Q2: So far, which is your first hypothesis with the data coming from C/O and P/E? Which is the data supporting this hypothesis?
to recover it as soon as possible. She had had a specific diagnosis before she came to the physiotherapy treatment so, we just had to take
My hypothesis is that is clear that she needed to
her back to her normal life. She had an
gain strength and more mobility to have a
impairment to walk normally, not just for pain,
normal gait again. The atrophy of her ankle
but also for insecurity and weakness.
makes her loose stability and muscle mass. And also the pain was the main negative factor that made her feel distrust in supporting his weight on her ankle.
The prognosis I gave her was good, I supposed she would be ok in some weeks, of course only if she follow all the instructions given during the therapy. She is young and a sportive girl, so what we have to do, also is to prevent her to have another lesion on the future, and the best way of
69
doing it is trying to recover her at 100% and
one level that were not so much painful to her.
giving her some extra points to her ankle.
She had to make 10 repetitions with an isometric
She had the same treatment during 2 weeks, and on the 3er week there were some changes, because she did not feel pain anymore. She went to therapy 3 times per week.
70
WEEK 1 AND 2
contraction in eversion, inversion, dorsiflexion and extension of the ankle. She had to keep the contraction for 10 seconds and then rest for 5 seconds between each repetition. Finally I used to give her a relax massage to avoid she was in pain after the sessions.
The treatment was given for the doctor, but I applied it to her. Firstly I used ultrasound to decrease the inflammation and pain, because if
STUDENT REFLEXION AFTER WEEK 1-2 TREATMENT
she were in pain, we could not make strength
I think the patient had good results, because we
training.
could get the pain relief. O Without pain we were
After that, I applied a hot pack for around all around her ankle for 2o minutes to relax the muscles before the stretching. Then, mobilized passively all the range of movements and stretched until the pain was of 7 in EVA scale. I explained that the therapy would be painful, but it was going to worth it.
going to be able to gain a lot of strength and proprioception to retraining the gait. WEEK 3RD During the 3er week, she was not more in pain, so all the session consisted in taught her a home program to strength all the right lower limb. I also prescribed a harder proprioceptive training
When the muscles were relaxed, we began to
and functional exercises to taker her back to
make the proprioceptive training. Being in front
football game.
of the mirror, I asked her to stand in one leg and then in the other one. I used some advisements
STUDENT REFLEXION
to make the exercises harder and raise the
She had really good results. She recovered all the
difficulty (like different surfaces with instability
range of movements, so with that factor to our
or closing her eyes at the moment she did the
favor, I think the only things she needed were get
exercises).
extra points to not get injured again.
About the strength training, I began with theraband exercises to make the resistance at
QUESTIONS TO IMPROVE REFLEXION
Q1: Do you think that is useful for her to use an
A4: I think that there wouldn´t be a lot of changes,
ankle support?
maybe I would use the kinesio-tape to help the
A1: I think that it would not be necessary, but it would give her extra support when she is playing.
peroneus muscle to do the strengthening exercises, and if the patient does not complain I could use ice instead hot. The cryo-kinetics
Q2: Does she should continue doing strengthening
exercises would have been a really good option
exercises?
too.
A2: I told her than she was going to have to do
TEACHER ADVICE
71
the exercises for a long time. Just to prevent another lesson. She needs to have more strength
For the majority of the physiotherapists I know, it
than usual in her ankle, because of the spring.
is not the ideal situation to work under the orders of other therapists or doctors, having no
Q3: Will you treat her in the same way if you have another opportunity again?
opportunity to take any decisions in the treatment you perform. In these occasions, although you
A3: Yes, absolutely. I think my management was
have to follow their prescriptions, I think that rely
good enough. The clue was in the initial
on you the capacity to dose it properly and make
subjective examination…
the necessary adjustments on patient´s benefit. And of course, they should listen to your feedbacks
Q4: How different should the treatment be if you had the opportunity to prescribe it instead of the doctor?
or reports with your own thoughts and proposals, also in that situations in which you think the treatment they prescribed is not working optimally.
FINAL STUDENT REFLEXION In my conclusion, I can say that she had a good recovering. I hope she follows all my instructions for the home program to avoid having a second lesion in the future. The treatment was successful because she was treated properly since she had the injury till the therapy program finished. The ankle spring is a very common lesson in sport people, but if it is treated properly, it doesn´t have to bring future discomforts.
REFERENCE LIST
1) Stanley Hoppenfield, (2007) Exploración física de la columna vertebral y las extremidades. (1) . Madrid. Manual Moderno
A 57 YO. HOUSEWIFE WITH A RIGHT HEMI PATELLECTOMY AND TENECTOMY OF THE PATELLA TENDON AFTER A PATELLA FRACTURE AND A TRANSIDESMAL FRACTURE OF THE RIGHT FIBULA BONE RANNOU MA. AND BERTRAND I.
imperfect osteogenesis and since then, she
INTRO
became extra careful and fearful about every A 57 yo. Housewife with a right hemi
kind of physical activity. Then, she also was
patellectomy and tenectomy of the patella
diagnosed with osteoporosis and her daughter
tendon after a patella fracture in July of 2014,
with imperfect osteogenesis too.
and a transidesmal fracture of the right fibula bone.
She’s
diagnosed
with
imperfect
She had antecedents: a right ankle fracture (a
osteogenesis and osteoporosis comes to start
fibula fracture), a right patella fracture and a
her rehabilitation with me in November after
few others in the other limbs but she couldn't
her last rehabilitation doctor’s appointment in
remember exactly how many. So, she was
August of 2014.
coming to begin her physical rehabilitation
SUBJECTIVE EXAMINATION
after her second fibula fracture (transindesmal)
I met D. at the hospital where she had a surgery for her physical rehabilitation. She was a dedicated housewife, mother of an adult daughter with whom she was very
and her second patella fracture on the right side. It happened during the summer in July, five months before I met her, first she fell and broke her patella and a week later she fell again and broke her fibula. Although her ankle fracture
close, having a lifestyle rather sedentary.
didn't need surgery as it wasn't displaced, her
Many years ago, she was diagnosed with
patella was quite bashed up and it resulted in a
hemi patellectomy and a tenectomy of the
Except for her very fragile skeletal structure
patella tendon which was in this occasion re-
which would oblige me to be extra careful, she
taunted with staples.
didn't present contraindications to the examination but, facing her fear, I decided to
The doctor prescription, of four months old in
start assessing the joints mobility and muscles
August, said that the physical therapist had to
strength in the lower limbs.
concentrate in the ankle joint but she hadn't been re-examined since then. As I spoke with
My first impression of the patient was a person
her it became clear that the ankle wasn't her
with mood swings: she often passed from a
major problem, she was disabled by it and felt
motivate, trustful and joyful state of mind to
pain but the one she had in her knee was worst.
sadness, fear, pessimism and lack of confidence
She explained to me that the pain, the
in herself as in myself. She had a tendency to
discomfort and a sensation of instability and
want to lead and control the examination,
weakness in her knee lead her to fear everyday
sometimes by fear of making it too much and
life activities such as go up and down on stairs
sometimes by laziness. It also appeared that
or go for a walk all alone even if she had
the bond she had with her daughter was very
crutches.
powerful: the fact that she inherited her
She added that because of it, she depended a
mother disease made D. feel very guilty and
lot of her daughter, feeling guilty and worry
preoccupied and worry about being a weight
about it, wanting to have a quick rehabilitation
for her.
and saying that she would do everything to
I
succeed. At the same time, she insisted a lot on
psychological sphere will be something very
the fact that I had to be very careful about her
important to include in the treatment.
understood
that,
in
this
case,
the
disease even if I didn't do anything yet. STUDENT REFLEXION AFTER S/E
QUESTIONS TO IMPROVE REFLEXION Q1: Could you find in the history any data
My initial hypotheses about the sources and
supporting that the patient should has an
patho-biological processes: a mechanic pain as
alteration of the pain modulation component in
a result of damages on bone and tendon
her pain presentation?
tissues in remodelling phase in both joints.
A1: I think that her state of mind and her
I decided to override the doctor prescription
attitude could be a proof that the patient has a
and dedicated time to the knee.
central modulation of the pain, in her case, the
psychological area has a great impact on her
she felt the more pain (Tables 2 and 3). The
pain.
mobility of the patella was quite good and the
Q2: How do you think her fear of not wanting to
cicatrisation process was going on. I made her
talk about her pathology could affect her?
walk with and without her crutch but she was so
A2: I think that this fear acts as a brake for her
focused that the walk didn’t appear very
recovery. If she doesn’t know what it is, she
natural.
can’t behave correctly to improve her condition.
TEACHER ADVICE Alteration of pain modulation system and central sensitization are two components of the pain
Right ROM Associated End-feel ankle symptoms Plantar 145° No pain Elastic flexion Dorsal 75° No pain Firm flexion Table 1. Arthrocinematics of the right ankle.
mechanisms with some overlapping and could be present at the same time. But they have to be addressed in different ways. Usually, information related with both mechanisms could be found (if present) in the subjective examination.
PHYSICAL EXAMINATION
In order to really understand what was frightening her, I tried to make her talk about her disease although I knew it. I was surprised when I discover she didn’t know much about it and wasn’t very interested in knowing more. I didn’t push her further, thinking she
Right knee Flexion
ROM
Associated Endsymptoms feel 80° Pain at the Elastic end of the movement Extension 0-1° Decreased Elastic muscle power Table 2. Arthrocinematics of the right knee.
Muscle group Grade (0-5) Ischiotibial muscles 4 Quadriceps femoris 3+ Gluteus muscles 4 Iliopsoas 4+ Flexor of ankle (DF) 4 Extensor of ankle 3+ (PF) Table 3. Muscles’ Power.
eventually could tell me and I decided to start my P/E. I started with the right ankle. She didn’t feel pain but was disturbed by a sensation of fragility and instability. I assessed her range of motion and her muscles power (Tables 1 and 3). Then, I did the same with her right knee where
At this point, she had enough so I let her go to her magnetic therapy session. Before she went out, she explained that although she was happy to start her rehabilitation and expect a lot from it, she didn’t expect very good results.
As she walked away, I finally saw how she was
exercises and that we will take care of her walk.
really walking.
My main idea was to make her participate and join her own rehabilitation by herself to then
STUDENT REFLEXION AFTER P/E
progressively lead her on a good path. She
About my initial hypotheses, my observations seemed to confirm that the real issue wasn’t in the ankle but in the knee where she suffered the more damages to the tissues. The pain finds its origin in her knee as the fact that she feels pain when moving seems to show. Also, I found interesting that she felt more pain when
seemed very relieved as she went home to know that the next session wasn’t going to be long and painful. QUESTIONS TO IMPROVE REFLEXION Q1: So far, which is your first hypothesis with the data coming from C/O and P/E? Which is the data supporting this hypothesis?
moving actively than when I executed the
A1: Noticing her pain manifests when she
movement myself. The lack of power in her
moves and go away when she rests, (associated
muscles didn’t permit her to move the way she
with a decreased ROM and muscle strength),
should as well as her fear of the pain and the fall.
my first hypothesis is a mechanical pain process
It appears that she also doesn’t know how to
as a consequence of her surgeries, in order to
use a crutch.
reduce her previous fractures. I would add that
About the narrative process, at this point I
her state of mind and her mood modulate this
understood that she didn’t want to expend
pain as shown by her attitude during the
herself on her disease or hear about it although
sessions through her obvious fear.
it had a big impact on her life and she had tendency to use it as an excuse to escape the TEACHER ADVICE
physical examination. It occurs to me that I’ll have to check again her walk as it appears that she didn’t know how to use
correctly
her
crutch
making
her
movements more difficult. I started to think that in fact, she didn’t even may need it anymore and that may have been something restraining her without her knowledge. I decided to not push her and told her that we will start the next session with some easy
There should be findings in these 2 first steps of the clinical encounter that have to correlate among them. As S/E comes firsts, usually points out which areas have to be evaluate in the P/E, and what should expect to find there. After performing the suggested tests, the therapist should could check if her first hypothesis were true or not and could move on to additional tests or questions if necessary.
avoid that she only depends on it. I noticed she
PATIENT MANAGEMENT DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN About my initial hypotheses, the exploration of
was capable to support her own weight and I asked her to try to do little walks and move in her home without it.
the patient left no doubt that the major
Finally I let her go to her electrotherapy and
problem
post-surgery
magneto therapy session because she feels
consequence and a significate lack of strength
better to end with it, saying that she took that
in the lower right limb.
as a way to relax and rest before going home.
was
indeed
a
About the narrative process, I wasn’t really sure about the implication of the daughter and her influence on her mother but I was certain that
STUDENT REFLEXION AFTER D1 TREATMENT
anyways the pathology, her history and the
She didn’t feel any pain during the treatment
rehabilitation had a strong impact on her
even if she is very attentive at every move I
participation and on her daily life sending her in
make and how far I go during the mobilizations
a vicious circle: the less she does the worst she
only to relax after a few series.
feels; and the worst she feels, the less she does.
The next day, if the treatment runs, I will
So my main goal was to break this circle and
continue with the exercises adding a little more
restore
difficulties: longer series and more resistance;
her
confidence
through
the
rehabilitation to move forward. DAY_1 We started with easy exercises: firstly big range mobilizations on both joints to show her that it could be done without pain; and then, small inner range mobilizations to start gaining ROM.
and if she has improved with her crutch I plan to try working on parallel bars with obstacles and little stairs. The goal will be to work targeting the function of her upper limb and push her to be confident about going for a walk by herself and coming back to her daily life with good bases and no fear.
I also applied a very small manual resistance during short series of movements to start
DAY_2
improving her strength slowly. The main idea is
I started assessing her progresses since the last
to show her what I expect from her and that she
session (she has a session everyday but I choose
is totally capable of doing it.
to explain the progresses and treatments each
Then, I dedicate time to show her the best way
week to really show her improvements with
to use her crutch to improve her walk and to
significates observations.), and she showed an
increased strength and a decreased pain.
obstacles and the banister and her strength
Seeing those improvements, I kept the initial
improved well so I decided to start practicing
treatment, only increasing a bit the difficulty
the stairs and to do muscular strenghting’s
with the resistance exercise and longer series of
exercise with weights.
movements.
The first exercise consisted on a flexo-
Then, we practiced on obstacles where she can
extension of her knee with a 3kg weight tied on
help herself with parallels bars and started to
her ankle, her thigh being supported by a pillow
go up and down a banister. With these two
while she was laying on her back.
exercises, we try to prepare her to go up and
The second one consisted on a flexo-extension
down the stairs, working on her joints and her
of her knee, pushing against a ball while she
muscles in a functional way which would
was sitting on the couch.
improve her symptoms.
She then continued with obstacles and banister, my intention was to slowly set up a routine,
STUDENT REFLEXION AFTER D2
with warm up, which she could easily follow so
TREATMENT
if I added exercises she won’t be lost only
I see a really significate improvement with this
removing the “old” ones when the new ones
patient. But she doesn’t seem to realize how
were totally acquired.
better she was. She tries her best to be
Finally, we started to go up and down little
enthusiastic about her treatment and I think
stairs, her two hands firmly holding on the
she manages it better when the exercises are
handtrails. The first problem was to correct her
about doing things of her daily life like trying to
posture as she was coming down the stairs
go through obstacles, working on her walk…
aside and putting both feet on each stair.
I try as much as I could to keep it entertaining
D. seemed more confident every day but
as she wished her recuperation was faster but it
started to complain about the length of the
sometimes is quite difficult to manage her
treatment showing some signs of impatience.
mood swings and to motivate her, it demands
The fact that I added some exercises didn’t
patience and inventiveness to convince her to
please her, she thought that the ones she was
work out every session but it’s an interesting
doing before were enough and I had to explain
challenge.
that the key of her progress was in the variety
DAY_3 As every session’s begun, I assessed her progresses. She was doing pretty well with the
of her treatment, increasing the difficulties. She wasn’t convinced. The next session, according to the results, I plan
to continue with the stairs, trying to improve
work more on the stairs. But to start, she
her going down so she gains in autonomy (her
warmed up with her strength exercises and
own stairs only have a handrail and she can’t
auto passive movements: we worked on every
come down without any help). We also work
movement of her hip, knee and ankle, with
out on the strength in her both legs: with auto
weights and pulleys seeking to improve the
passive exercises and more weight. Finally, we
general strength of her leg, not only her
will experiment some proprioception both for
quadriceps muscles.
her knee and ankle.
Once she finished with it, we came up and down the stairs. Last time, we didn’t manage to
STUDENT REFLEXION ABOUT D_3
change the fact that she was coming down
It’s now really difficult to keep her motivated
aside, both feet on each stairs with the two
for her therapy, she doesn’t realize her
handrails. I thought that the problem wasn’t
progresses at all, and this is why I think the
mechanic as I saw her with the obstacles and
stairs will be the solution to this problem.
she hadn’t any problem to come down from
Working and improving herself on the stairs
them. It started to appear that she feared the
will show her, with something she knows well,
stairs. She was physically capable of doing it
how much she improved.
but wasn’t confident enough.
We must continue to work with the weights for
We started slowly, with only two stairs and the
her strength even if she doesn’t see the
two handrails. Showing her that it was easier to
differences but maybe if she realize that in
come down to the next stair if she put half of
order to do the stairs exercise correctly she
her foot on the side of the stair before going
must gain strength it will be easier.
with the other on the stair of after, it was only a
The main problem with D. is her lack of trust,
question of control of her quadriceps. Solving
in herself mostly and in me a little, this is why
this, she was then able to come down frontally.
one of my objective is to give her
Very excited by this improvement, she didn’t
consciousness of all the work she managed to
even realize that she used only one handrail.
do so far, giving her exercises that put it in
These results acted as a trigger and at the end,
light, like the stairs.
she wasn’t using the handrails at all. We then tried to do little proprioception. First,
DAY_4 For this session, seeing the previous results, I decided to remove the obstacles exercises to
she had to work on a mattress, walking on it varying steps: on tiptoes, on heels, aside, crossing legs…The goal was to provoke an
adaptation of her body to the changing
was difficult for her to let her crutches aside
parameters. We then tried it on a rocker device:
because she felt like she needed it. Slowly, she
she was standing on it, on her both feet and I
decided to let them go, and admitted to me
throw her a ball in various directions to provoke
later that it was in fact easier to walk without
an unbalance.
them.
Despite her apprehension, she did it very well
Q3: Do you think that, if you ignored the
and we managed to make it more difficult
psychological aspect of the treatment, it would
asking her to stand on one feet only (she had a
had the same result?
wall to lean on if needed). She didn’t managed
A3: I think that if I hadn’t, the results would
to do it so we stayed with the more stable
have been really different, it would have been
version, for this time.
worst. I imagine she would have stop her treatment, convinced that I wasn’t seeing her
STUDENT REFLEXION AFTERDAY_4
like a person but only like a joint.
This session was quite important because she finally realized that her therapy was working, after that, it was really easier to work with her and to propose her other exercises. I think that in her case, the fear of hurting herself was the biggest brake and that all the time we took was necessary to come to this result. QUESTIONS TO IMPROVE REFLEXION Q1: Which was the role of the electrotherapy in your management? A1: The electrotherapy was TENS and was prescribed to strength her quadriceps muscles. The patient was quite enthusiastic about it as she felt a relaxing effect afterwards and insisted to have it at the end of the sessions. Q2: Did she manage to walk correctly? A2: She eventually walked in a better way but it
TEACHER ADVICE Sometimes is hard to be sure about which part of the treatment has worked better, worse or not at all, also in multi-treatment modalities. It´s the same with lots of research case reports, in which patients are treat with and elevate number of techniques and no data about confounding effect is found. At least, if patient objectives are lined with outcomes, technique effects, and these are properly performed, we could have a plan to revisit after changes are seen.
FINAL STUDENT REFLEXION The final results confirmed my initials hypotheses and even if it was a long process, the patient and I managed to see the improvements. The difficulty in this case wasn’t really the diagnosis but the management of the patient. It took a lot of patience and courage for both of us to communicate and to go through the therapy. The key of the treatment was in the psychological area of the patient, once she admitted that she was improving, it became a lot easier. She didn’t stop her mood swing but she accepted better the directions I was giving. If I had to treat her again, I wouldn’t change my treatment. It worked but maybe I’d try to be firmer, to take the lead of the treatment more quickly.
Right ROM Associated End-feel ankle symptoms Plantar 150° No pain Elastic flexion Dorsal 80° No pain Firm flexion Table 4. Final assessment of the ankle ROM
Right knee
ROM
Associated End-feel symptoms Flexion 90° No pain Elastic Extension -3° No Elastic Table 5. Final assessment of the knee ROM.
REFERENCE LIST 1. RESERVES, I. and FORIN, D. (2015). Orphanet: Ostéogenèse imparfaite. [online] Orpha.net. Available at: http://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=FR&Expert=666 [Accessed 14 Jun. 2015]. 2. Root, L. (1984). The treatment of osteogenesis imperfecta. The Orthopedic clinics of North America, 15(4), 775-790.
8 YEAR OLD BOY WITH FRACTURES OF BOTH LEGS AFTER A FALL FROM THE EIGHTH FLOOR OF AN APARTMENT. TIBERI A. AND VIOLATI D.
82 The medical diagnosis was; in the left leg
INTRO
closed diafisary fracture of tibia and perone, M. is an 8 year old boy who fell off the 8th floor on the 31st of October and fractured both his legs.
treatment with a monolateral external fixator for 3 and a half months. And in the right leg open fracture of the external femoral condyle and right meseta tibial of grade IV in the Salter
SUBJECTIVE EXAMINATION
and Harris’ epifisiolisis scale. The treatment M. is an 8 year old boy who studies in a German school in Madrid. He says he doesn’t practice a particular
sport.
He
went
to
the
consists of an open reduction of the epifisiolisis with screws, cast and orthesis for the first 6 weeks.
physiotherapist the 13th of April of 2015 and says he also goes to another physiotherapist
After a MRI, it appears he had a slight
once every 2 weeks. When we met first I asked
pulmonary
how the accident happened; M. felt a little bit
neumothorax.
uncomfortable, so I decided to change the topic. After a week he confessed that on the 31st of October 2015 (Halloween night), he was playing by himself outside in the balcony, which was on the 8th floor, when he approached the border line and fell, the fall
contusion
and
a
minimum
He doesn’t present neurologic or vascular alterations, the pelvis is stable and the upper body moves without pain. He has been on a wheelchair for 5 months and after that, until today, he uses a crutch to walk. He told me he had never had any other problem before.
was diminished since he fell on a bunch of trees. He told me that that very day he went through
He does not feel any creep sensation, tingling,
surgery on both legs.
burning or allodynia; his sensibility has increased on the right knee around the patella.
He also mentions that his pain appears when
remove some fears which can interfere in the
he tries to move more the leg, and he has an
rehabilitation.
itchy sensation around the scar on the right leg. He also says he feels his legs weaker when he
QUESTIONS TO IMPROVE REFLEXION
has to walk long distances tires or taking the
Q1: Andrea, as you described, M. also has an
stairs at school
epiphysiolysis. How do you think you can deal with it?
STUDENT REFLEXION AFTER S/E M. is a little boy therefore it is complicated to get him focused for a long time, he doesn’t enjoy talking about the accident and this makes the anamnesis harder. I always try to ask
but
without
making
him
feel
uncomfortable and for that reason I was missing information during the first week in
A1: This is a point where I feel a bit doubtful, since the doctors said he has a grade IV epifisiolisis, after a few searches on this type of fractures, I saw that the prognostic is negative due to M.’s age and his growing cartilage is affected. My objectives would be to stimulate the vascularization to that zone.
the anamnesis.
Q2: What do you mean with, “a fear can
My initial hypothesis of the source and
interfere in the rehabilitation”?
pathobiological process: M. has suffered a great
trauma,
mentally and
physically.
Physically the medical diagnosis was a great help and gave a clearer picture of what he has. The fact he has a hypersensitivity or muscular weakness
could
be
related
to
the
immobilization and due to the surgery he received. I decided to evaluate only the hip and the knee of both legs and the position he has from a bipedestation. About
the narrative process, my first
impression was that M. is a Young boy and
I think that in a normal mental state where the patient feels ‘depressed’ or better said, notmotivated, due to the fear of falling for example or doing things wrong, can harden our work. If I push the line of work too much on something he does not want to do (for whichever reason), he could obtain rejection from him but at the same time if I think this line of work is appropriate but he is scared due to any reason, it can slow down the recuperation times.
luckily his improvement is faster. We have to
Q3: Which is the impact for daily life activities
pay attention to his self-confidence and try to
and participation?
84
A3: During every day activities, as we were
physiotherapists. But it doesn´t mean that a
talking, I understood that M. can do everything
wise therapist hasn´t to take it in consideration
inside certain limits. It was him who told me he
to approach these patient´s area. Disability
had difficulties to play with the other kids since
issues
he is the slowest and if he forces his legs they
presentations
start to hurt so he is scared and avoids playing.
treatment outcomes. And our work over the
The only thing he does with no problems is
dysfunction has a direct effect in disability.
being a goalkeeper during break. But generally
Physiotherapists have to know how the impact
he moves with the crutches by himself with no
is in this area and which parts of Daily Life
difficulties and can dress up by himself etc…
Activities and Participation are being affected. It
Regarding
the
is usually more significate and realistic for a
treatment M. is easily distracted, it is hard for
patient the possibility to play soccer again than
him to keep focused and he says he gets tired
to achieve the cold “knee´s full active ROM”
and doesn’t want to do certain exercises.
goal.
Q4: How was the role of his family members
PHYSICAL EXAMINATION
his
participation
during
during the anamnesis? Do they cooperate?
have
a
major
and
role
in
perspectives
patient’s for
the
One week has passed since the first time I saw
A4: The first time I met M. he was with his
M. I was at the end of the clinic’s corridor and I
grandmother; she came to me and told me in
saw him walk towards me accompanied by his
detail about M.’s accident. When I started
grandmother. After saying hello we went
talking to M. and got a bit closer he was very
inside the consult. After a few minutes talking
shy and didn’t want to answer me, so his
with his grandmother I started with the
grandmother had to answer for him. I had to
physical exploration. I ask M. if he can put his
ask his grandmother if she could leave so I
trousers, socks, shoes and shirt off, explaining
could be with M. by myself and get closer to
him that in that way I could have a clearer look
him. Since that moment he started answering
on his state. After a few jokes I asked m. if he
more questions.
could put himself on a comfortable position and look towards the front, I tried to pay
TEACHER ADVICE Following
the WHO
attention to every detail (feet position, shape the
of the tibias, height of the patellae, popliteal
International Classification of Function in 2001
hole, hip, back, and compared his muscular
(ICF),
tone). Generally he seems he goes towards a
disability
is
definitions
not
the
of
field
of
pelvic anteversion, knee flexion on the right leg,
in any other position than goalkeeper and he
and a clear division of weight towards the left
didn’t like this situation.
leg. I also evaluated his scars and the scar of the right leg, above the patella, and saw it was
STUDENT REFLEXION AFTER P/E
a queloid type; the others didn’t seem to have
When I saw M. walk I focused on his way of
any abnormal alteration.
walking, I was impressed because it looked like
- Muscle Balance:
a neurologic walk, therefore I asked my tutor for advice and he tranquilized me and told me
Right leg: grade 3/5
it wasn’t like that. My idea at first was to
Leg left: Grade 4/5
educate his walking since it looked much
- ROM the knee:
uncontrolled. After the first time I saw M. at his home, I looked for the type of fractures he
Right leg: 85 ° of flex. And 15 ° ext.
presented and made myself an idea to what I
Left Leg: Full
was dealing with. After this first P/E, I already have an idea to what I have to work with him
- VAS:
for the moment, my objectives for now is to
Right leg: by forcing the movements of
reeducate the walk, obtain a complete knee
flexion and extension reaches an 8 (not
extension, work on the pelvic anteversion,
strive wanted more) and palpation of
strengthen the muscles and mobilize the scars
scars: supra patellar and the one in the
to avoid adherences.
popliteal hole.
I told him he’d play football again and he’ll be
Left Leg: painless movements but
stronger than before. I know inside my mind
palpation of the tibia and fibula is
that I’m facing a complicated case, mostly due
painful.
to the psychological aspect rather than the
I had the occasion to ask him some more questions, but this time focusing on his feelings after the accident. I asked him if he could play with his friends in school. He said he played as a goalkeeper and that he could stop more goals with his crutches, but he can’t play
physical.
QUESTIONS TO IMPROVE REFLEXION Q1: In the type of trauma and the postures described in the P/E, do you think that some test
pushing the femur anteriorly as the psoas iliaco or muscles that can produce this anteversion.
to assess the integrity of the nervous system
Give mobility and break scar adherences could
could be useful?
allow us obtain more elasticity in the tissues
A1: Your proposition is very interesting and in
86
work at the same time the muscles that can be
fact I thought about the same thing during the day after the exploration. Unfortunately I don’t have a lot of time to do many things, I want to focus on these types of explorations for 2
and obtain more movement of the knee. As I said earlier, always put strength work to strenghthen and reeducate the walk. I totally agree with the propioception work but it will be a line of work that I will be integrating gradually little by little according to the
reasons:
progress made on the objectives described
Because doctors said after MRI that M. has no sort of neurologic affectation in the nerve root
I think that for a kid like him it was best
earlier. Q3: Which are the positive and negative issues for the prognosis in this patient?
to do something “faster” and simpler
A3: Positive Issues: M´s is, surely, important in
for the first day of exploration. Surely
the prognosis due to the fact that it allows us
the next time I will do some test to
to advance a quicker way, the socio-economic
discard
support of the family which allows to have
possible
neurologic
affectations. Q2: Could proprioception be an accurate goal for your patient?
physiotherapy sessions every day and 3 times a week with 2 hour sessions. The absence of other types of diseases. Negative issues: lack of concentration and doesn’t want to really do
A2: Inside my head I have an idea of what the
the exercises is a factor that makes us lose a lot
objectives are and which ones I think could be
of time to make the patient listen and do what
the most important ones. I think it is very
he is asked to, fear creates a defense response
important to work all at once with him. I will
where the muscles try to block the leg and
focus on working every day on the mobility,
difficult the exercises centered on the
paying more attention to the extension since it
increment of range of articular movement. The
is the movement that allows us to have a
type of fracture of the epifisiolisis and the age
functional walk, to work on this. I will have to
in which he did it is another important factor
since there is affectation of on the growth
for the epifisiolisis with screws, plaster and
cartilage and also it’s an age where there is
ferula for the first 6 weeks.
more bone development.
Also, after a TAC we can see a light pulmonary
TEACHER ADVICE
contusion. Minimum neumothorax.
One of the typical questions asked by the patient
He doesn’t present vascular nor neurologic
after this point is “How much time does the
affectation, the pelvis is stable and the upper
treatment need to be effective?” Therapist
limb can be moved without pain.
haven´t a crystal ball in their kit. But we could guess an approximate period of time thinking in
He has been on a wheel chair for 5 months and until today. From my point of view M. presents:
the clinical pattern, the related published evidence, the pathology and your own
Pelvic anteversion
experience treating this kind of presentation.
15° knee flexion on the right leg
Not every former point weights the same; but
Queloide-type scar on the right leg above the
you could put, in a two-plate scale, positive against negative prognostic factors and provide
an estimation. PATIENT MANAGEMENT
Muscular balance o
Right leg: grade 4/5
o
Left leg: grade 5/5
ROM: o
DIAGNOSIS, PROGNOSIS, OUTCOMES
of ext.
AND PLAN o From a medical point of view the diagnosis is clear, M. presents fractures on both legs: -
Left leg – diafisary closed fracture of
Right leg: 85° of flex. and 15°
Left leg: complete
VAS: only pain when movement and palpation o
Right leg: when forcing the
tibia and perone, treatment with an external
movements of flexo-extention
monolateral fixator for 3 and a half months.
he reaches an 8 (didn’t want to force more)
-
Right leg – open fracture of external
femoral condyle and right meseta tibial of grade IV on the Salter and Harris epifisiolisis scale, treatment consists of an open reduction
o
Left leg: the movements don’t hurt but the palpation of the tibia is painful
The prognosis of M. can be good under a
In this section I focused completely on the right
functional point of view, since he is very Young
leg:
his recuperation is faster but what upsets me is the epifisiolisis that he has on the right leg. My objectives are that M. regains his confidence on himself and that he can have once again strength, mobility and more functionality than
88
before.
I asked him if he could lay down, the attention of M during the treatment was very low, he laid down in incorrect positions and when I tried to move the leg he’d pus hit on the opposite side to avoid me from moving it. I made a deal with him: he could ask me whatever he wanted if he allowed me to move his leg. I then started with
DAY_1 Before starting with the treatment I did a quick neurologic exploration to see if there could be an entrapment on a nervous level. Both mecanosensibility test as to the nervious conduction test were negative. I asked M if he
the treatment. M was laid down facing up and the left leg was resting while I had the right leg and worked with the scar with a few massages from superficial to deep in order to break adherences, always basing on the pain M had.
could lie down on the massage table sitting. I
Then I did passive mobilizations specifically on
rapidly evaluated the ROM on both legs to
the patella to the femur and on a second place,
have a comparative mean at the end of the
passive analytic mobilizations of the knee on
treatment. I explained what I was going to do
extension
and to tell me when it’ll hurt. I explained to him
component of the tibia and tractions and
to classify his pain on a scale from 0 – 10
relaxation of the knee. On second place I
calculating 10 as an unbearable pain and 0 is
started working on the flexion from a seated
when you don’t feel anything. I started the
position
test:
component of the knee. I then did the muscle
Right leg : 85° of flex. and 15° of ext.
o
adding
an
an
external
internal
rotation
rotation
treatment of the psoas iliaco from the right
ROM: o
with
Left leg: complete
side, M was on supin position and I was holding his right leg increasing the hip flexion to better go in and palpate the iliopsoas. To the palpation of this muscle we could clearly feel
The end feel was firm and was accompanied by
an increase of the tone.
a muscular spasm as a defense mechanism due to the pain.
At the end of the treatment I re-assessed the mobility and the improvement was noticeable
since I could reach with the right leg more than
element in order to obtain his attention and
95º of flexion and nearly 5º of extension.
be able to work with him on a better way.
STUDENT REFLEXION AFTER D1
DAY_2
TREATMENT
When I saw M I asked him how he felt after the
As expected it is a child and clearly bored
treatment and he told me he felt good and that
standing still in one place and also try
he didn’t feel pain during the day. I then tried
maintaining the most attention possible with
the same treatment from the first day, giving
games and history while continuing my
me time to do a few miofascial liberation
treatment. I think it's very difficult to focus on
techniques on the quadriceps with my hands
making techniques while reassuring the
crossed on top of the muscle and realizing a
patient, this makes me wonder if what I'm
traction on the opposite side as if I wanted to
doing is really the right thing, I wish you could
enlarge the muscle and adding movements
be more relaxed and understand that what I'm
that
doing here with the I do it just for him.
restrictions. At the end of the treatment I
could
go
directed
to
miofascial
spoke with him and his grandmother who was QUESTIONS TO IMPROVE REFLEXION Q1: What types of treatment did you use to assess the iliopsoas muscle?
inside the consult and I told them that the following week we would start going to the gym, dividing the treatment on 20 minutes of manual therapy, 20 minutes of gym and 40 of
A1: I applied a pumping technique of such
swimming pool.
muscle to avoid an irritation of the muscle, which would cause an increase of the pain. Q2: Which part of your management do you
DAY_3 Same as DAY_1 and DAY 2.
think has worked better and why?
DAY_4
A2: I don’t think that there has been a part
It was the first day of gym. I started treating
during the treatment that has been more
the scars and mobilizing the patella and knee
effective. I think that the set of techniques
on flexion and extension with the same leg as
have attained this improvement. I believe my
the first day, I also focused on working on the
attitude towards the patient has played a key
hamstring muscles manually doing deep passes and stopping on miofascial conflict
90
zones and on latent trigger points. Then I went
reeducation of the gait by playing with speed
to the gym with him and we started a strength
and amplitude of the gait, controlling the trunk,
program. M was lying down and we had the
another exercise consisted on him supporting
opportunity on the clinic to do some motor
his feet on the wall of the swimming pool while
control
STABILIZE
I had to hold him from behind, positioning his
apparatus. I started with a few motor control
legs separated by a few cm’s (shoulder width)
exercises on isometric for the quadriceps, I
from this position he had to bend the legs more
positioned
the
so he could then push hard (as if he wanted to
popliteous hole and explained to M that
jump) the objective was to strengthen and
according to the orders I gave him he’d have to
work on the active mobility. For last I told him
contract only the muscle on top of the thigh
to go on a little stair that sunk M’s leg until half
and buttocks and the muscles below the thigh
of the inferior part of the thigh (above the
had to be relaxed, to make the exercise easier I
patella) and from then on he had to be on a
told him top put a hand on top of the quad and
monopodal posture and hold the position for
another one on buttocks and hamstrings. At
20 seconds.
exercises
the
with
the
STABILIZER
below
first it was hard for him to differentiate the contractions between the different muscle compartments. I did the same exercises for the hamstrings positioning the STABILIZER below
DAY_4,5,6 & 7 The treatment was always the same DAY_8
the heel and telling him to push with the heel downwards. I also worked on a propioceptive
3 weeks have passed and I did again the
level and explained to him 2 exercises, the first
physical exploration, the improvements were
one consisted on standing up on top of 2 tilts
huge.
and did charge transference from a leg to the
The pelvic anteversion, managed to have a
other without pain and the second exercise
nearly full extension from the 3º of flexion on
consisted of walking on a DYNA DISC which is
the right leg. The scars remained more or less
a disc made out of rubber, I explained to him
the same, the muscular balance improved
that he had to put more charge on the heel
even though we could still see there was a
Little toe thumb. We then went to some
difference between the left and right leg, with
parallel bars in order to work on the gait. After
less strength on the range of movement:
20 minutes I went down with him to the swimming pool where we focused on the
o
Right leg: 105° of flex. and 3° of ext.
up and down the stairs. On the swimming pool
o
Left leg: complete
-
VAS: pain only to movement and
palpation o
Right
leg:
when
forcing
the
the exercises were more or less the same but we increased the intensities. AFTER A MONTH AND A HALF:
movements of flexo-extention he reaches an 8
M’s treatments are still on the same line of
but he reaches greater amplitudes (didn’t want
work but increasing little by little the
to force more)
difficulties and intensities. On the third
o
Left leg: the movements don’t hurt,
evaluation I did that day M presented:
the palpation of the tibia is less painful
-
Minimum pelvic anteversion
I started as always mobilizing the scars, rotula
-
Scar on both legs were had more
and knee. That day I focused on working more
flexibility and the queloid type of scar had
with the psoas because I think it was one of the
diminished its width.
factors which was altering the gait, so I applied
-
Muscular balance
then I did an analytic stretch of that muscle. On
o
Balance muscular of the right leg:
this section I also worked on a Global Postural
grade V
the same treatment as described before and
Reeducation technique (RPG) with the posture of the dancer to stretch the posterior muscle chain, maintaining this position for 4 minutes without M feeling any pain but a slight tenseness Garrido-Marín, A. et all. 2012. On the gym I started doing a few propioception exercises which were a bit harder, such as stability on standing position on the BOSU, on the side of the half ball, he had to maintain for
o
Left leg: grade V
-
ROM:
o
Right leg: 130° of flex. and 0° of ext.
o
Left leg: complete
-
VAS: pain on the movement and at the
palpation
20 seconds, then he had to put a leg on top of
o
the BOSU and the other one in front of the
movements of flexion around the 133º/135º he
ground, and from there flexion the leg which
reaches an 8 (didn’t want to force more)
was more anteriorized by controlling the trunk. At last we were working on the gait and going
o
Right
leg:
Left leg:
painless
when
forcing
the
palpation of the tibia is
M. I realized that with the passage of time was always hearing me more, working with is not easy because you have to be always doing something that catches your attention, but I think with these types of jobs in addition to the clear improvements at the level physical, M. has greatly improved its attitude also fear. This
92
was the last day I saw M. due to the end of my clinical practice. STUDENT REFLEXION
a complete knee extension, increase of the muscle tone: gastrocnemius, soleus, popliteus, isquio-cruralis muscles, mostly on the right leg. I chose to apply an RPG treatment due to the fact that in the article (Garrido-Marín, A. et all. 7 November 2012) the effectivity or global postural reeducation was studied versus the Propioceptive Neuromuscular Facilitation, to increase the extensibility of the hamstring muscles and it concluded that the treatment
Throughout my treatments with M. my thoughts were always to look for functional exercises while at the same time entertaining him since he used to get distracted easily. During the hours of training I always looked for
with RPG is better. Therefore I surfed the web for books that talked more in depth about this treatment and which was the RPG posture most indicated for M´s presentation (Souchard, P. E. 2005).
simple exercises to strengthen, improve the propioception and functionality in order to bring it to his daily life activities. QUESTIONS TO IMPROVE REFLEXION
TEACHER ADVICE In spite of you´ve found one paper suggesting the prevalence of RPG stretching against PNF¨s, it´s no necessary true that this method is going
Q1: On the 8th day you said that you worked
to work better with your patient. Despite the
with M. a RPG stretch, the “dancer”, what is
internal and external quality of the journal
the reason that made you believe that this was
publication, we should find those which were run
a suitable stretch for him?
within a similar population compared with our
A1: During the treatment weeks, I had the
patients. If her/his profile fits properly within the
possibility to know more of M. as the days
profile of the volunteers in a research, probably
went by. There are many reasons: limitation of
you could better guess how treatment will be with your client.
FINAL STUDENT REFLEXION I’ve reached the end of the treatment with M. The case firstly really scared due to the fact that I had to put a lot of effort in every day to make him pay attention, there were days in which he came and he was really tired therefore working with him was very hard, also the fear I had when it came to do certain exercises with him blocked me a little. I think it has been a very stimulating case for me because every day I felt obliged to make up different exercises which were directed towards my goals at the same time. It has also been my first experience on working with the swimming pool so I am very happy about that, it’s a good line of work and the possibility to be able to follow the case gave me the security that what I was doing with him was the right thing because I could constantly see the improvements. It has been a difficult case but it has made me think a lot and improve my knowledge REFERENCE LIST 1. Souchard, P. E. (2005). RPG. Principios de la reeducación postural global (Vol. 88). Editorial Paidotribo. 2. Marín, A. G., Guzón, D. R., López, P. E., Serrano, M. F., & Imedio, A. S. (2013). Efectividad de la reeducación postural global frente a la facilitación neuromuscular propioceptiva, para aumentar la extensibilidad de los isquiotibiales en sujetos sanos. Estudio piloto. Cuestiones de fisioterapia: revista universitaria de información e investigación en Fisioterapia, 42(2), 98-106.
A TOO EARLY MENISCAL DIAGNOSIS URIA A. AND ALCALA L. The pain started one month ago during a paddle-
INTRO
tennis match when he made a sudden extension 31 year old man who works as a labourer in kitchen construction who complains about a continuous
94
pain above his right patella accompanied by a sense of engagement of 1 month onset…
of his right leg, but he continued playing at the time and for the next two weeks until the pain was so strong that he decided to stop. He usually went running with his dog three days a week, but he interrupted this too. The pain hasn´t hold on since
SUBJECTIVE EXAMINATION
he first noticed but has increased to the point that A.K is a 31-year-old man who works as a labourer
it hurts even at work.
in kitchen construction. He has come to a
He needs to expend a lot of time squatting at work
patella
and he feels a continuous pain, which influences
accompanied by a sense of engagement during
him in his mood and work performance. He is
certain movements, which started one month ago
annoyed about not being able to do any of his
during a paddle- tennis. He has recently started
hobbies (jogging and paddle- tennis).
physiotherapy continuous
consultation
pain
above
his
because right
of
feeling pain in the internal part of the left patella as well as an overload sensation of his left gastrocnemius.
The pain on both legs (specially the right leg) increases at the end of the day (when walking and standing for long periods of time, squatting, when
When I first met him, he walked into the
standing from a squatting position and while
consulting room limping his right foot trying not
going up and down stairs). He usually puts his
to stand on it. I noticed he was a restless person
right leg at rest, extended and with ice at the top
when he started talking to me. He didn´t stop
of the knee to reduce pain and he feels no pain at
wondering about the diagnosis before doing any
night. But when he wakes up, he feels a bit of
physical examination. He was really scared about
stiffness and discomfort on his right leg that stops
having a meniscal injury because his father was
after heating the joint.
operated twice due to his work, which is the same as his.
He had three-ankle sprain on his right leg when he
his constant fear about being operated as his
was 14 years old.
father. But during the clinical case and after the
He has a good overall health; no respiratory or circulatory or urologic dysfunction and he had
physical examination, you will see how I am going to change my mind.
good results on his latest blood test. He has not
Q3. Which
attended any doctor and has no radiographs of his
transmission in meniscus diseases? Do you think is
knee.
high enough to lead a P/E thinking in that
He is not taking any medication, just ibuprofen occasionally when working but without effect.
is
the prevalence for genetic
possibility? A3: No, there is no scientific evidence about genetic transmission in meniscus disease but I
STUDENT REFLEXION AFTER S/E
focused on that possibility because of the
Because of his family history (his father had
triggering
undergo a meniscus operation because of his
continuous aggravating situations during his work
work), my first thought has been that the same thing was happening to the son. So I have decided
mechanism
of
injury
and
the
TEACHER ADVICE
meniscus testing without thinking in other
Illness scripts are good tools for clinicians during the
options.
decision-making process. They provide therapists with the most relevant characteristics of a
QUESTIONS TO IMPROVE REFLEXION
prototype patient within a syndrome. Despite they
Q1: Didn’t you think that the pain of the left leg is
are not always the same (they evolve as the same
caused by an overload?
time as the clinician´s experience) and there is no such a thing as a “prototype patient”, having these
A1: It was my first thought, but I first wanted to
schemas in your mind prompts you with more
know what was happening with the right leg as it
chances to discover of the patient´s presentation
was the main cause for the patient visiting the
fits in that schema or not, avoiding unnecessary
consultation and his main concern.
procedures
Q2: What about the patellar tendon and the LCA and LCP? A2: Yes, you are totally right. Meniscus testing was my first step because of his family history and
PHYSICAL EXAMINATION
During
the
dynamic
examination,
active
movements are good except medial rotation of the knee and hip in both legs (especially in the right leg). Pain has been found during right leg extension starting from a squat position. Accompanied by an engagement sensation of the knee.
96
During palpation, temperature and muscular tone are normal and there is neither articular spilling nor edema. Pain has been produced at joint line palpation of the right leg and an increase in tone has been found in the calf of the left leg. Muscular balance is 3/5 in the right quadriceps. I have started with the static examination where
Trigger points have been detected at the left leg
nothing relevant has been detected except a bit of
in the internal and external gastrocnemius.
knee hyperextension and a great base of support.
Tests: Thessaly test, McMurray test. Appley test
The main symptom is the continuous pain
and the Sensitivity test of the joint line have been
above the right patella.
performed.
The second symptom is an engagement
All of them have been negative except the last
sensation in both sides of the right joint line.
one, which has been painful during palpation.
The third symptom is the pain at the internal
Lachman test has also been performed but has
side of the left patella.
been found to be negative too. (Harrison, B. K.,
And the fourth symptom is the overload
Abell, B. E., & Gibson, T. W. (2009), (Akseki, D.,
sensation he feels at left gastrocnemius.
Özcan, Ö., Boya, H., & Pınar, H. (2004).
His associated symptoms are a right leg block sensation and articular crunch sensation. All
STUDENT REFLEXION AFTER P/E
symptoms are related. Because of the pain in the
As all meniscal tests have been negative except
right leg, left leg has made lots of compensations,
for the joint line test. I have dismissed any
and has ended up with pain too.
meniscal injury by the limited relevance of this
last test alone. As Lachman test is also negative,
A1: The truth is that I did not think of a joint wear
LCA and LCP injuries have been dismissed too.
problem because the reason for the beginning of
I now have to make a hypothesis with all the information I have: - Pain mechanism is nociceptive and mechanical and tissue is at proliferative phase (1 month).
the pain was clear and precise: making an abrupt knee extension-playing paddle. I think that a joint wear has usually no clear beginning nor an exact reason for its appearance. Q2: I think that he should make some Rx or RMN to
Trigger mechanism: was isolated playing paddle-
see if there is some micro fracture on the patella or
tennis but was aggravated after repetitive
in the joint in general because he spends a lot of
impacts and squat positions at work time.
time in squat position, or maybe some problem in the cartilage. Don’t you think?
The source of symptoms is skeletal muscle because it affects the patella and tendons and muscles that surround it.
His main functional limitations are going up and downstairs, maintaining a squat position and standing up from a sit position. The left leg is painful after walking for a long time or after work.
A2: Yes, maybe you are right. But the reason for not doing it was because I didn´t see any neither oedema nor inflammations signs to make me suspect about micro fractures. As I didn´t find any contraindications nor red flags I decided trying some physiotherapy techniques to see if symptoms were released and patient improved before any other complementary images (which I thought were not necessary for the moment).
Because of all this information, my reflection
Q3: Have you found any symptoms on the other
about his problem after subjective and physical
limb and how do link them to the right knee
examination is that he might be suffering a
presentation?
patellofemoral pain syndrome. (Thomeé, R., Augustsson, J., & Karlsson, J. (1999). QUESTIONS TO IMPROVE REFLEXION
A3: Yes, I didn´t put enough information at first, but I´ve just revised it and as I noted, the left leg was painful during joint line palpation and had some trigger points in the external an internal
Q1: Did you think that maybe the problem started because of a joint wear?
gastrocnemius. I think there is a relation with the symptoms in the right leg because of the lots of compensation made when walking or working
that has cause an overload in his left leg because
disruption of exercise and constant overload that
of trying to avoid pain in the right leg.
will occur in the joint during his work in the future will not help the recovering process.
TEACHER ADVICE So the last of my goals is to motivate my patient The development of same symptoms on the other
to achieve better and quicker results.
limb in our patients could be related with different DAY_1
hypothesis. It could be the spread of a general
98
illness; an overused provoked by the increased
My plan starts by reducing pain and strengthening
activity of the other limb; it could be a central
the right quadriceps.
sensitization; or simply activation of mirror neurons mimicking the neural activity of the other limb. It´s
-
I have first make a passive transversal
under our scope to identify the source and the
displacement of the right patella and ask my
pattern of progression to avoid wrong targets
patient to make active flexion of the knee from
during the treatment.
a standing position, meanwhile I have continued maintaining the displacement. I´ve
PATIENT MANAGEMENT DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN My patient´s main goal is pain decreasing. So my goal table includes:
asked him to do three sets of 10 repetitions. -
Taping: medial displacement of the right patella Like this we have worked the quadriceps and the movements, which caused him pain, avoiding pain because of my passive displacement of the
-
Pain releasing
-
Strengthening right quadriceps
-
Remove load and possible contractures of the left gastrocnemius
-
Flexibilize muscles within the right knee
-
Increase or keep the articular movements limited or diminished range.
-
Restore self-confidence
As regard good prognosis factors, his interest in recovering will facilitate the process, but his fear,
patella. I have decided to apply the taping because of the good results acquired during the sessions. DAYS 2-4 My patient has come up to the next consultation with less pain so I have decided to do the same exercise as in the first session. Apart from this, I have decided to work out the internal rotation of the right hip in prone position
with a 90º-knee flexion with passive movements
A1: My idea in the first session was to reduce pain
and to work out right hip extension with anterior-
during the movements that usually caused pain to
posterior movements in standing position with
my patient. I achieved it by making a transversal
the Mulligan tape as the patient does an active
passive displacement of the patella at the same
extension of the hip.
time that he actively did his painful gesture (which
I have also recommended him to start his
was making a squat from a standing position). So
exercises and to ride in static bike for 15 minutes,
despite gaining strength in the quadriceps was
3 days per week.
not my main point, it was indirectly achieved because of the exercise itself.
In the third session, the patient has come with barely no pain, with a muscular balance of 4/5 in
Q2: Why did you work on the hip? And in this way?
the right quadriceps and with an increase in hip
A2: I decided working on the hip because, as I´ve
ROM. So I have decided to continue with the last
said in the physical examination, internal rotation
program and giving him a massage in the left leg
of the right hip was limited. I worked it in this way
to release the overload sensation of the calf.
because it was easier and had better results.
STUDENT REFLEXION
Q3: Did you do reassessment?
I really think the prognosis is this case would be
A3: I reassed my patient in the next session
great because there has been a great increase
because he came 2 days per week for just 1 hour
there has been a big improvement in all signs and
treatment so we didn´t have enough time to do
symptoms in just 3 sessions and the patient is
everything in the same day.
heavily involved. But to get our treatment to be effective, we will recommend the patient to come
Q4: What did the result from DAY1 tell you about your patient presentation?
to our clinic one day a week for the next two weeks and to begin slowly with his hobbies
A4: He was presenting an acute condition that
(running, paddle…).
was aggravated because of repetitive painful movements. As pain was alleviated while making
QUESTIONS TO IMPROVE REFLEXION Q1:
Why didn´t you work on the strength of
quadriceps in the first sessions and you didn´t focus on the range of motion firstly?
a transversal patella movement and reduced during each session, I thought about a patellofemoral dysfunction
TEACHER ADVICE
Contrasting DAY_1 results with the initial assessment of DAY_2 also provides information
Results of DAY_1 treatment usually give us a valuable information about paths of relieving
about the lasting period of the changes achieved, irritability and dosage of techniques.
symptoms and dysfunctions, if you really control the neurophysiological and biomechanical effect you are dealing with.
100 FINAL STUDENT REFLEXION I think this case has helped me to improve my clinical reasoning. In my opinion, I´ve wanted to put, too fast, the name to the disease, to make a quick diagnosis. And that is the reason why I have not progressed from the beginning. I now try to stop and pay attention to every single information about the subjective and physical examination before giving a name to the dysfunction, which I´ve learned, is not that important. REFERENCE LIST 1. Thomeé, R., Augustsson, J., & Karlsson, J. (1999). Patellofemoral pain syndrome. Sports Medicine, 28(4), 245-262 2. Harrison, B. K., Abell, B. E., & Gibson, T. W. (2009). The thessaly test for detection of meniscal tears: Validation of a new physical examination technique for primary care medicine. Clinical Journal of Sport Medicine : Official Journal of the Canadian Academy of Sport Medicine, 19(1), 9-12. doi:10.1097/JSM.0b013e31818f1689 [doi] 3. Akseki, D., Özcan, Ö., Boya, H., & Pınar, H. (2004). A new weight-bearing meniscal test and a comparison with McMurray’s test and joint line tenderness. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 20(9), 951-958
PAIN CAUSING A SCAPULAR DISKINESIS IN A 25 YO STUDENT VIOLATI D. AND TIBERI A.
INTRO 25 years old woman, with an alteration of her right scapular girdle movement after a strange episode of pain and stiffness during the night.
She went to emergency immediately where she received the diagnosis of idiopathic subluxation. No reduction was performed and she was told to apply ice and use a sling “on and off” depending on the pain.
SUBJECTIVE EXAMINATION I just had finished to treat a patient at the clinic where I’m doing my last practices of the physical therapy career, when a colleague call me to help him with the exploration of a new patient. When I got at the “gym zone” the therapist told the patient to lift her arm to show me the problem even before to introduce me. When I saw her right scapula movement during the arm flexion I
She spent 4 days following the directions. The pain decreased but it was still strong so she decided to go back to the hospital at the emergency area where the doctor said to her it was a “cervical problem” and he diagnosed her a cervicobrachialgia. The treatment was diazepam, NSAID and superficial heat application. The doctor also gave her an appointment for two weeks later with the orthopaedic doctor.
got shocked cause I hadn’t seen something like this before. When she put her arm down we
During the 2 weeks before the appointment the
introduced to each other and we started talking.
pain decreased progressively. The orthopaedic doctor told her she has capsulitis and chronic
She was a 25 years old publicity student, she
instability of her shoulder.
have been living in Madrid all her life. She showed me all the medical reports and I She attended to physical therapy because the orthopaedic told her. She told me that the onset of the problem was day 15/03/2015; She had been
asked her for previous pathologies and she answered me it was the first time she has a health problem.
woken up by a very intense pain in her shoulder during the night and She felt it very stiff (while
I asked her if she was in pain and she told me:
she was telling me that, she simulated the
“The pain appears only when I lift my arm and it
position in which her arm was stacked).
is localized in the upper part of my shoulder. I’m
101
not able to lift my arm like the other, I feel loss of
were the accurate one to describe the patient
strength when I have to take or hold something
condition.
with my hand far from my body, like a glass of water or opening the door. I don’t feel comfortable when I lay down looking up because I feel my bone (scapula) pressing the sofa or the bed, but I feel a lot better then 4 weeks ago”.
I think my first hypothesis of a mechanical problem was right but I didn’t think too much about a possible first cause of this mechanical problem. If she really suffered by a subluxation maybe an alteration of the muscular activation
She hasn’t been practicing any kind of exercise
could be provoked by a neural tissue damage or
during the last 3 years.
maybe the severe pain it self could cause it.
My
first
thinking,
putting
together
the
I also didn’t considerate the loss of strength that
information that I received and the first
the patient told me about, that could also be
impression seeing her moving, was about a
related with neurogenic problem that I didn’t ask
mechanical problem because of her “on-off” pain
questions for.
related to the last degrees of shoulder movement over the 90 degrees, provoked for the clash between the humeral head and the acromion that could compromise the tissues between them. The all thing caused by her scapula that wasn’t moving in the right way. The
My brain didn’t have the flexibility to “play” more with the information. I think it stopped working from the beginning keeping mainly the image of the patient moving. I needed to much time to get to this conclusion and start to think again.
quality of the movement that I observed made
The patient looked not worried at all for her
me think about an alteration of the sequence of
condition and she was very quiet at all time and
the muscular activation during the movement.
disposed to follow directions to improve as soon as possible.
STUDENT REFLEXION AFTER S/E I think that I forgot a lot of questions that could
QUESTIONS TO IMPROVE REFLEXION
provide me a lot more information, because of a
Q1: I would like to know if you asked your patient
lack of a mental structure to formulate them
about typical symptoms of neurogenic alterations,
orderly.
like tingling or “burning sensation”… or moments
I also didn’t considerate too much the medical diagnosis because I didn’t think that any of them
of the day in which the symptoms increase, that may help you to get a clearer idea.
A1: I didn’t ask for them and I think it was a big mistake during the first interview. Fortunately I didn’t perform the physical examination the day of the subjective examination because the patient was late for an appointment so that I had the time to reflex on it. Of course before the beginning of the physical exploration it was one of the first questions I asked the patient.
TEACHER ADVICE Contributing factors could play a key role in our patients’ presentation. Therapist tend not pay much attention to them as they are not the cause of the client´s problem. But they should be under our scope, also when they are suggested by the patients as a main issues for them. Sometimes is really challenge to eliminate their influence, for
Q2: Do you think the activation of a trigger point
example anatomic and biomechanics CF. On the
could provoke the alteration in the muscular
other hand, yellow flags or ergonomic CF will be
activation sequence of her shoulder?
targets and should be dealt within patient´s management.
A2: Actually I didn’t recognise a clear active trigger point pattern in the localization of patient
PHYSICAL EXAMINATION
pain but of course I will check it out in the
The second time I saw the patient, first thing
physical examination.
she told me was that she was getting better and
Q3: Are there any other signs supporting the neurogenic hypothesis?
her attitude was very positive from the very first moment so I thought that would be very helpful to get good results.
A3: The only signs and symptoms that could make me think about an alteration in nervous system is the loss of strength. No other signs or symptoms were reported or found.
I asked her for neurogenic symptoms and I got a “not at all” as answer. I also asked more about her strength problem and she told me it was like an uncomfortable situation in which she was
Q4: Could you identify, so far, any contributing
feeling her arm falling and tightness in her
factors for both hypotheses?
medial part of the scapula.
A4: The only contributing factor that I found is
I started with the physical examination from the
the possible subluxation she suffered because it
static observation taking the most relevant
could be the cause of both hypothesis. No other
information for me:
CF or yellow flag were found thinking in the maintenance of the condition
103
Anterior view: the humeral head looked
moment I also tried to charge the neural tissue
in a slight anterior superior position
asking a neck side bending in both sides with
compared with the other one.
the results of no changing in pain and no
Posterior view: the medial borders of
presence of other symptoms.
the scapula as well as the inferior angle of the scapula was more "detached" from the rib cage
Side view: significant decrease of the dorsal curve (kyphosis)
The passives movements had a complete range of movement (ROM) and they didn’t provoke any pain or other symptoms.
I also tried to passively help the scapula movement during the active lifting of the arm with the result of reaching the full ROM with no pain detected but with the increased muscles activation described before. I also asked the patient to open a door to check the movement during one of the action in which she was complaining about the loss of strength;
In a posterior view, during the lifting movement
she repeated again that the movement was
of the right arm, the difference in the
uncomfortable; I observed that, during the arm
movement of the right scapula compared with
lifting, her scapula was separating from the rib
the contralateral was pretty clear: the medial
cage while maintaining the arm lifted and it
border of the scapula started to separate from
increase when she was trying to open the door.
the rib cage from the first degrees of movement (20 ° -30 °); during the lifting, the scapula present a big reduction of the ROM compared with the contralateral. When the scapula stopped to move appeared a significant
At the palpation I perceived an increased tone of the rhomboideus and intermediate region of trapezius muscles, but no trigger point that could reproduce the patient symptoms were found.
increasing in the activity of the upper trapezius, lower trapezius and also the elevator scapula.
I performed the muscular balance of the serratus anterior getting a 3-/5 (Daniel’s scale)
The conclusion was that the ROM of the physiological movements of the shoulder (arm lifting) was limited and the last degrees provoked by pain at the end of the ROM.
asking the patient an abduction of the scapula. During the test the scapula behave as described during the arm lifting and the patient was recruiting other muscles to complete the action
When the patient was in pain I used the VAS to
so that the quality of the movement was very
obtain the intensity of pain: VAS= 3. In that
poor.
STUDENT REFLEXION AFTER P/E After the P/E I considered my first hypothesis of a mechanical problem right: in this case I think the mechanical problem is the cause of patient pain. It appears only during the active movement and its nature bring me to think about a nociceptive mechanical pain because it appears with movement/ mechanical provocation (on-off) (Smart, Blake, Staines, A., & Doody, 2011) and it was localized in a specific
separated from the rib cage in a static rest position could be normal cause the patient dominant hand is the right one, that could provoke more protraction in the homolateral shoulder but it doesn’t explain why she started to have the sensation of her scapula pressing the bed or the sofa in a supine position. It also doesn’t give me information about the muscular status: the serratus anterior muscle is not active in a resting position.
site that “agreed” with my first hypothesis of a
I think the loss of strength could be due to a
clash between the humeral head and the
poor proximal stability (shoulder) that doesn’t
acromion.
allow a good “basement” for the transmission of
Analysing the muscular activation sequence, I
the forces needed for the action.
think the fact that the medial border of the
When I looked for myofascial trigger points I
scapula and the inferior angle separation from
tried to remember which muscle could provoke
the rib cage, could be due to a problem in the
the pain in the location in which the patient was
serratus anterior muscle. The serratus anterior is
feeling it. I didn’t look for them in the serratus
one of the responsible, with the trapezius
anterior cause I didn’t think in the possibility of
inferior and the trapezius superior, of the
their implication in the loss of strength.
scapula movement during the raise of the arm and also to maintain the scapula in a good relation with the rib cage during the movement. I also think that the increased activity of the rest of the muscles that permit the movement and the activation of the levatur scapulae muscle are intent of the body to reach the full movement supplying the poor action of the serratus anterior. I think the fact that the medial border of the scapula and the inferior angle were slightly
After all the previous consideration I started thinking about why the serratus anterior wasn’t activating in the right way so I started to think about a conduction problem, but I couldn’t
105
remember the innervation of the target muscle.
Another test I used in the P/E is the “scapular assistance test” that evaluates scapular and acromial involvement in subacromial impingent, probably the main cause of the mechanical nociceptive pain of the patient. The assistance for scapular elevation is provided by manually stabilizing the scapula and rotating the inferior border of the scapula as the arm moves. This procedure simulates the force-couple activity (coordination) of the serratus anterior and lower
Pain: red (VAS:3) Tightness: blue
trapezius
muscles,
the
elimination
or
modification of the impingement symptoms indicates that these muscles should be a major
QUESTIONS TO IMPROVE REFLEXION
focus in rehabilitation (Kibler & McMullen 2003).
Q1: I didn’t get your conclusion about what you found in the static observation; I mean, what do
TEACHER ADVICE
you think about the relation between her scapula
If we find during the S/E information suggesting
position and her feeling of her scapula pressing
the possibility of a neurology/neurodynamic
when she lay down supine cause as you said the
problem, neurology exam has to be conducted on
serratus anterior isn’t active in a resting position?
Day_1, prior to neurodynamic tests. Also it has to be ruled out any red flag related with these kind of
A1: I don’t have an answer yet. It could be due to the use of the sling that could affect the position
symptoms (i.e. Cauda equine or an Upper Motor Neuron Syndrome)
of the scapula girdle, or maybe a change of her shoulder posture as a result of the pain felt.
PATIENT MANAGEMENT
Q2: Have you found any coordination evidence-
DIAGNOSIS, PROGNOSIS, OUTCOMES AND PLAN
based test in the literature for this muscle?
The final diagnosis was a “Scapular dyskinesis” A2: I performed the muscular balance with a
with either flexion or abduction is rated as having
test described in (Kendall, 2007) another
obvious abnormality (dysrhythmias and winging)
effective test described in the literature is the
(McClure, Tate, Kareha, Irwin, & Zlupko, 2009).
“Wall push-ups”, used to evaluate serratus anterior muscle strength.
In the literature is described that the 5% of
that the full ROM can be reached without any
scapular diskinesis can be caused by Injury to the
pain.
long thoracic nerve that can alter muscular function of the serratus anterior muscle, and injury to the spinal accessory nerve can alter function of the trapezius muscle but no evident typical postures of these problems were found in the P/E (Kibler & McMullen 2003). Usually muscles can be also inhibited as a nonspecific response to a painful condition that in my opinion is the most possible hypothesis in the case of the patient, serratus anterior and the lower trapezius muscles are the most susceptible
I also tried to activate the serratus anterior with active exercises in a standing position and in a supine position, asking for a protraction of the scapula with the shoulder positioned in a 90 degrees flexion. I re-evaluated the ROM and pain in shoulder flexion and ABD with no significant changes in the first one and a decreased pain with an EVA of 2/10
to the effect of the inhibition (Kibler & McMullen
STUDENT REFLEXION AFTER D1 TREATMENT
2003). Inhibition is seen as a decreased ability of
My first session was planned thinking in all the
the muscles to exert torque and stabilize the
information received during the S/E and the P/E.
scapula as well as disorganization of the normal
I thought the serratus anterior muscle was the
muscle firing patterns of the muscles around the
main problem so that I chose techniques to
shoulder (Kibler & McMullen 2003).
reach a better activation of this muscle.
The superior or entire medial border may be
The treatment didn’t gave me big results maybe
painful to palpation or with motion because of
cause it was the first session and it was a very
similar tightness or scar in the levator scapulae or
short one or maybe I needed more time to apply
lower trapezius insertions, or both (Kibler &
the techniques for a longer period, or maybe
McMullen 2003), this could explain the tightness
cause I simply needed more sessions to get
that patient referred in the P/E.
better outcomes.
DAY_1
The true is that I didn’t knew protocols or other
I applied the scapular assistance test, applied in
kinds of assessment for this problem so that
several series/repetitions, as treatment to
looked for articles that describe the condition
stimulate the activity of the serratus anterior
and I took out from them some ideas to plan a
muscle and also to make the patient conscious
better treatment in the following sessions.
107
After the research I found that in the first 3 weeks
neuromuscular
of treatment the first point is avoid painful arm
techniques, of the latissimus dorsi muscle and
movements and positions and establish scapular
the pectoralis minor muscle (Kibler & McMullen
motion by proximal facilitation so that my first
2003).
technique was good (Kibler & McMullen 2003). Another point was to initiate scapular motion
facilitation
stretching
I also teach her exercises of scapula protraction using body movements previously described.
exercises without arm elevation, using trunk flexion and trunk medial rotation to facilitate
STUDENT REFLEXION
scapular protraction It could be a good idea due
After checking the muscles flexibility and tone
to the fact that the patient couldn’t activate the
related with the limitation of scapula
muscle with effectiveness and quality using arm
movements (pectoralis minor, levator scapulae,
elevation exercises (Kibler & McMullen 2003)
upper trapezius, latissimus dorsi, infraspinatus, and teres minor muscles) (Kibler & McMullen
QUESTIONS TO IMPROVE REFLEXION Q1: Do you think that activate other scapula stabilizers could be a good idea to improve the
2003), I decide to treat the muscle that appears, compared with the contralateral side, to present more tone.
quality in the shoulder movement? The result of the second session was good in A1: Yes, probably I could look for some exercises
terms of active ROM (full ROM) and pain (VAS:
to activate rhomboids and medium trapezius
1) so that I decided to follow this line for the
muscles. I’m just a little worried about charging
third session in which the patient came with
to much the superior trapezius and the inferior
better sensations but still poor movement
trapezius because as we have seen in the P/E
quality of movement but maintaining the ROM
they probably are already working too much.
and pain improving, so that I wanted to see if
DAYS 2-3
the treatment could also be useful to provoke a change in the quality of the scapular
The patient came with better sensations about
movement.
her strength and she felt she could move more than before.
What I didn’t do was retest after each technique applied so that I only know that all them
After the research I repeated the first exercise performed in day 1 and I also included the evaluation and treatment, with proprioceptive
together get to patient improvement but I don’t
know if each technique alone could lead to
technique, probably the scapular assistance test
better outcomes.
used as technique is the one that worked more cause is the only exercise I used in the first 2
QUESTIONS TO IMPROVE REFLEXION Q1: why don’t you try to activate muscles like the latissimus dorsi to see if they can help you to achieve a better scapula position in an unstable position, amid range of flexion for example?
sessions getting a better ROM and less pain. TEACHER ADVICE Physiotherapy literature is full of trials measuring the “initial effects” of lots of techniques. To be “immediately effective” doesn´t mean that the
A1: It could be a good idea to see if they can help
technique is “long-lasting” or worth it at all. Or at
me to reach a better quality of scapula
least if it is going to be accurate in each case. But
movement and position in different degrees of
re-evaluating patient´s main outcomes before
movement. I’ll try it!
and after the session, will enlighten your thinking
Q2: Which part of your management do you think has worked better and why?
and support next decisions in the management. It could also be a way to give feedback to your patient about his/her progression.
A2: I’m not pretty sure about it yet because as I said in the reflexion, I didn’t retest after each FINAL STUDENT REFLEXION My diagnosis was a scapular dyskinesis with obvious abnormality (dysrhythmias and winging) during shoulder flexion and ABD (McClure, Tate, Kareha, Irwin, & Zlupko, 2009). Causing a nociceptive mechanical pain in the patient during the 2 movements (Smart, Blake, Staines, A., & Doody, 2011). I found support that a painful condition is the most possible hypothesis in causing serratus anterior inhibition (Kibler & McMullen 2003) that is in my opinion the most affected muscle in fact a poor muscular balance during the test described in the P/E was found (Kendall, 2007); so first goal to reach was “waking up” that muscle to improve the movement quality. At this point of the treatment I didn’t find anything in the literature that could clarify me the natural process of this condition, and I also didn’t find any other paper that could help me to be more consistent during the treatment planning. I think that so far I’m missing the key treatment (exercise or manual treatment…) to improve the patient quality of movement so that I’ll keep looking for it in the literature and during the treatment sessions.
109
REFERENCE LIST 1. Smart, K. M., Blake, C., Staines, A., & Doody, C. (2011). The Discriminative validity of “nociceptive,”“peripheral neuropathic,” and “central sensitization” as mechanisms-based classifications of musculoskeletal pain. The Clinical journal of pain, 27(8), 655-663. 2. Kendall, F. P. (2007). Kendall’s Músculos Pruebas Funcionales Postura y Dolor, Editorial Marbán. 3. Kibler, W. B., & McMullen, J. (2003). Scapular dyskinesis and its relation to shoulder pain. The Journal of the American Academy of Orthopaedic Surgeons, 11(2), 142-151. 4. McClure, P., Tate, A. R., Kareha, S., Irwin, D., & Zlupko, E. (2009). A clinical method for identifying scapular dyskinesis, part 1: reliability. Journal of athletic training, 44(2), 160.
111
113
Second Edition, 2016© CC BY-NC-ND 4.0
Related Documents

Download
January 2021 1
Download List
January 2021 1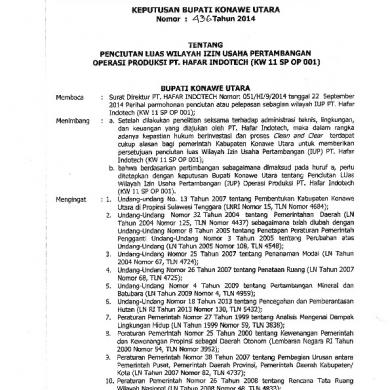
Download-1414849788298
March 2021 0
Download (6)
January 2021 1
Knjige Download
January 2021 3
Download 2
February 2021 1More Documents from "Aco Rifai"

Download
January 2021 1